Volume 10, Issue 1, 2011-2012 - Department of Surgery - University ...
Volume 10, Issue 1, 2011-2012 - Department of Surgery - University ...
Volume 10, Issue 1, 2011-2012 - Department of Surgery - University ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
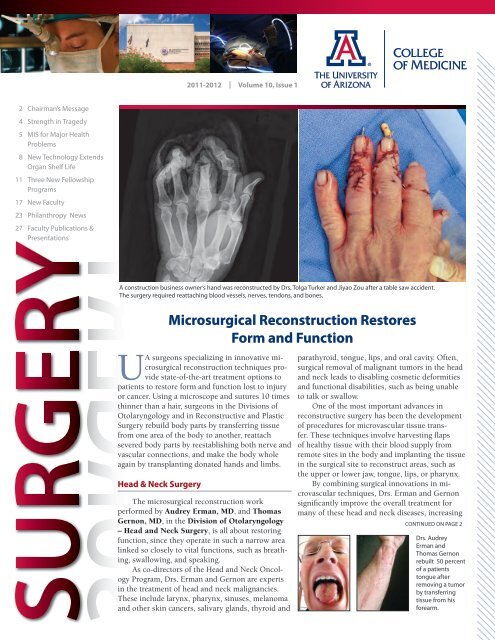
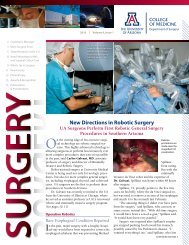
hand, or finger – cansignificantly impactquality <strong>of</strong> life. A loss<strong>of</strong> function in one<strong>of</strong> these areas is adevastating blow torecovery and to anyhope <strong>of</strong> returning toa normal life.As members <strong>of</strong>the Division <strong>of</strong> Reconstructive andPlastic <strong>Surgery</strong>, Warren BreidenbachIII, MD, Tolga Turker, MD, and JiyaoZou, MD, specialize in microsurgicaltransfer <strong>of</strong> bone, tissue, and nerve, aswell as free or pedicled skin flaps torepair wounds, injuries, or defects tothe upper extremities and to restoresensation and movement. They also aretrained to perform composite tissue allotransplants(the transplantation <strong>of</strong> tissueor limbs from deceased donors).Whether their patients come inelectively or with trauma, these surgeonshave the combined skills <strong>of</strong> reconstructive,plastic, and vascular surgeons, eliminatingthe need for multiple providersand resulting in less duplicated care andshorter recovery time. They have particularexpertise in the treatment <strong>of</strong> all types<strong>of</strong> hand surgeries, including transplantinghands and replanting severed digits.“Restoring function is our numberone priority,” said Dr. Zou. “After anaccident, we are able to save a patient’sthumb or finger by performing a replantation,which includes bone fixation andtendon, artery, and nerve repair.“We use a vein graft from the forearmin order to keep the length <strong>of</strong> thedigit. If the digit is not replantable, aswith a fingertip injury, we can salvagethe finger’s length usingdifferent kinds<strong>of</strong> flaps,” Dr. Zouexplained.Other types <strong>of</strong>miscrosurgical reconstructionon extremitiesperformed byDrs. Zou and Turkerinclude woundcoverage.“We can use both pedicled and freeflaps to cover the tissue defects. Flapcoverage can be successfully done andwill provide a better outcome with severeupper extremity injuries,” saidDr. Turker.Drs. Zou and Turker were broughton board by Dr. Breidenbach, the newchief <strong>of</strong> the Division <strong>of</strong> Reconstructiveand Plastic <strong>Surgery</strong>.Dr. Breidenbach came to the UA fromthe Christine M. Kleinert Institute forHand and Microsurgery in Louisville,Ky., where he performed the world’s firstsuccessful complete hand transplant. Heis interested in expanding the types <strong>of</strong>transplants performed at the UA to otherareas <strong>of</strong> the body, including face transplants.“There’s always been a need forthis kind <strong>of</strong> specialized microsurgicalrestoration,” Dr. Breidenbach said. “Wenow have highly qualified hand surgeonsavailable 24/7.”Breast <strong>Surgery</strong>Unlike some <strong>of</strong> the other areas <strong>of</strong> thebody where microsurgery techniques areused, form outweighs function in breastreconstruction.Ethan Larson, MD, in the Division<strong>of</strong> Reconstructive and Plastic <strong>Surgery</strong>,<strong>of</strong>fers state-<strong>of</strong>-the-art microsurgery breastreconstruction techniquesafter mastectomy to helpwomen recovering frombreast cancer begin to feelwhole again.DIEP (deep inferiorepigastric perforator) andTUG (transverse uppergracilis) flap proceduresuse skin, tissue, and tinyblood vessels taken fromeither the patient’s abdomenor inner thigh areato form a new breast. The breast reconstructionflaps are much larger than mostother flaps used in other microsurgicalprocedures, but the technical aspects arenot so different from other areas <strong>of</strong> thebody, Dr. Larson said. These particularflaps are <strong>of</strong>ten made up <strong>of</strong> the patient’sown skin and fat, without the need tosacrifice a functional muscle.“The surgery itself is quite lengthy,so completing the dissection <strong>of</strong> the flapin a timely fashion is <strong>of</strong>ten the mostdifficult portion <strong>of</strong> the procedure, alongwith the added challenge <strong>of</strong> shaping anattractive breast from abdominal tissue– one that matches a remaining breast,”he said.Dr. Larson is one <strong>of</strong> the few surgeonsin Southern Arizona to <strong>of</strong>fer microsurgicalfree-flap breast reconstruction. “I doall types <strong>of</strong> microsurgery, but breast reconstructionseems to answer the biggestneed,” he said.DIEP andTUG flapproceduresuse skin,tissue, andtiny bloodvesselstaken fromeither theabdomen orinner thighto form anew breast.3
Quality Patient Care<strong>Surgery</strong> Shows Its Strengths During Tucson’s TragedyIt’s been more than a year since theUA <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong>, The<strong>University</strong> <strong>of</strong> Arizona Medical Center,and Tucson were thrust into theinternational spotlight after the Jan.8, <strong>2011</strong> shooting that killed six andinjured 13 others, including ArizonaCongresswoman Gabrielle Giffords.It was a day <strong>of</strong> sadness for the Tucsoncommunity and a day that tested ahospital’s preparedness for dealingwith an event that captured internationalattention.As Giffords clung to life onJan. 8, media from across the globedescended on the hospital, clamoringfor updates on the condition <strong>of</strong>the congresswoman, who’d been shotthrough the left side <strong>of</strong> her brain inan assassination attempt.For Peter Rhee, MD, chief <strong>of</strong> theDivision <strong>of</strong> Trauma, Critical Care,and Emergency <strong>Surgery</strong> and a Navycombat veteran who treated soldierswith battlefield injuries in Iraq andAfghanistan before coming to the UA,mass casualties and gunshot woundsMichael Lemole, MD, chief <strong>of</strong> neurosurgery,and Peter Rhee, MD, chief <strong>of</strong> traumaare a routine part <strong>of</strong> the job. Themedia frenzy that followed on Jan. 8was not.Although the circumstancesattracting the media attention weregrim, the event also provided the UA<strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> and the hos-UA <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> chairman Rainer W.G.Gruessner, MDpital with a unique opportunity to showthe public the high-caliber <strong>of</strong> the surgeonsand staff recruited to the UA andthe high quality <strong>of</strong> care available at The<strong>University</strong> <strong>of</strong> Arizona Medical Center.Southern Arizona’s Level ITrauma CenterIt’s hard to say how the aftermath<strong>of</strong> the Jan. 8 shooting might have beendifferent had Tucson not had a Level ITrauma Center to meet the shootingvictims’ needs.“In the past four years, the <strong>University</strong><strong>of</strong> Arizona and The <strong>University</strong> <strong>of</strong>Arizona Medical Center have supportedand invested heavily in the <strong>Department</strong><strong>of</strong> <strong>Surgery</strong> and in trauma, starting withmy hiring Dr. Rhee,” said Rainer W.G.Gruessner, MD, UA <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong>chairman. “As a result, the surgerydepartment has grown since 2007 from35 faculty members to 87 faculty members.This robust expansion, rarely seentoday at public universities, permittedour instant and in-depth readiness formanaging such large-scale trauma.”“We let the world know that we areperforming at the same level as the bestin America in academic medicine,” saidMichael Lemole, MD, chief <strong>of</strong> the Division<strong>of</strong> Neurosurgery in the UA <strong>Department</strong><strong>of</strong> <strong>Surgery</strong>. “People now understandthat this is a sophisticated town with anacademic medical center and surgery departmentthat are reputable on a nationallevel.”Today, Giffords continues herrecovery. In September, she hosted aspecial dinner in Tucson for a handful<strong>of</strong> employees from The <strong>University</strong> <strong>of</strong>Arizona Medical Center – <strong>University</strong>Campus. On the one-year anniversary<strong>of</strong> the tragedy, she attended a vigil,which drew about 3,500 people, onthe UA main campus lawn.The <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> and“This is asophisticatedtown withan academicmedicalcenter anda surgerydepartmentthat arereputable ona nationallevel.”– Dr. Lemolethe trauma divisioncontinue togrow under theguidance <strong>of</strong>Dr. Gruessner andDr. Rhee, whosays he’s at aboutstage five <strong>of</strong> a<strong>10</strong>-stage expansionplan. Sincejoining the medicalcenter aboutfour years ago, Dr.Rhee has alreadygrown the divisionfrom two tonine trauma surgeons.Future plans include adding aburn unit, increasing trauma research,and building areas like the hospital’sextremity transplant and in-houserehabilitation programs.The effects <strong>of</strong> the media attentionhave been lasting. People fly into Tucsonnow for surgery from as far awayas Boston because <strong>of</strong> their confidencein the medical center. Both Dr. Rheeand Dr. Lemole continue to receiverequests to speak publicly about thehospital’s response to the tragedy, andDr. Rhee, a Korean-American, haseven been asked to help establish atrauma system in Korea modeled afterwhat’s in place at The <strong>University</strong> <strong>of</strong>Arizona Medical Center – <strong>University</strong>Campus.“I think we are going to be recognizedfor this particular event for along period <strong>of</strong> time,” Dr. Rhee said.4
One Year, <strong>10</strong>0 Kidney TransplantsFelipe Pinedo, Jr.’s surgery Dec. 13,<strong>2011</strong>, marked the <strong>University</strong> <strong>of</strong>Arizona Transplant Program’s <strong>10</strong>0thkidney transplant for the year.Pinedo’s niece, Andrea Torres, 34,donated a kidney to her 57-year-olduncle, who suffered from end-stage renaldisease due to complications <strong>of</strong> diabetes.He had been on dialysis for about threeyears. Six days after the surgery, Pinedowas “raring to go,” refusing the wheelchairride to the lobby after his releasefrom the hospital.Performed at The <strong>University</strong> <strong>of</strong>Arizona Medical Center – <strong>University</strong>Campus by Rainer W.G. Gruessner,MD, and Tun Jie, MD, the year’s <strong>10</strong>0thkidney transplant is the most the hospitalhas ever done in one year. Thetransplant program performed 90 kidneytransplants in 20<strong>10</strong> and 80 in 2009. Thenumbers <strong>of</strong> lung, pediatric liver, andintestine transplants are projected to seeincreases as well.Since the program was revitalizedin 2007, about 400 kidney transplantshave been performed, 98 from livingdonors. Dr. Gruessner, chairman <strong>of</strong> theUA <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> and chief <strong>of</strong>the Division <strong>of</strong>Abdominal Transplantation,andBruce Kaplan,MD, medicaldirector <strong>of</strong> theKidney TransplantProgram,attribute some<strong>of</strong> the growth tomore live donorkidneys,<strong>2011</strong>KIDNEY TRANSPLANTSrecent advances in immunology andtechnologies, and less invasive surgicalprocedures for the donor.“We have seen a substantial increasein living donated kidneys over the pastthree years,” said Dr. Gruessner. “Withmore people on transplant lists than everbefore, leading transplant teams like oursare turning more and more to live kidneydonation.“This is good news because the lifeexpectancy <strong>of</strong> a living donor kidneyis about 20 years on average, twice aslong as a kidney from a deceased donor.Deceased donor kidneys are in very shortsupply, and there are 90,000 people waitingfor kidney transplants.”Recent advances in immunologyand technologies have allowed centersto overcome blood type and immuneincompatibility. In the past, this incompatibilitywould rule out a donor and recipientpair. The UA transplant programhas particular expertise to <strong>of</strong>fer therapiesto increase compatibility and reduce thepossibility <strong>of</strong> organ rejection.Also, new surgical techniques,including minimally invasive kidneyextraction, are making it easier to donateSince the Transplant Program was revitalizedin 2007, UA surgeons have performed about400 kidney transplants, 98 from living donors.One-year outcomes for adult kidney transplantsare higher than the national average.ComprehensiveTransplant CenterLast May, the UA <strong>Department</strong><strong>of</strong> <strong>Surgery</strong> announcedthat the UA has one <strong>of</strong> themost comprehensive programsin all areas <strong>of</strong> adult and pediatrictransplants, including:• Solid-organ transplants,which include kidney,liver, pancreas, intestine,heart, and lung transplants• Cellular transplants,which use islet cellsto treat, or evenprevent,insulindependentdiabetes• Compositetissuetransplants,includinghandtransplantsand facetransplants,forpatientswhohavesuffered limb loss orextensive facialdisfigurementa kidney to someone in need.For patients like Pinedo, a transplantprovides a better quality <strong>of</strong> lifethan the grueling three-days-a-weekdialysis treatments. They can returnto work, travel, and spend time doingthe things they enjoy.“I run racing horses with mybrothers and before the transplantI couldn’t travel with them,” saidPinedo, a retired tire store owner.“Now I can go with them.”7
Cutting-Edge ResearchNew Technology Extends the Life <strong>of</strong> Donor Organsand Islet Cells for TransplantThe <strong>University</strong> <strong>of</strong> Arizona <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> and other highly specialized transplant centers aroundthe world are furthering the next generation <strong>of</strong> treatments for organ failure and for type 1 diabetes.New technology pioneered by researchersat the UA <strong>Department</strong> <strong>of</strong><strong>Surgery</strong> and small business collaboratorscould pr<strong>of</strong>oundly extend the viability <strong>of</strong>organs and pancreatic islet cells, expandingthe global reach <strong>of</strong> transplant centersand allowing for more critically neededtransplants.Islet cell allotransplants involve collectingislets from a donor pancreas andinfusing them into the liver <strong>of</strong> a personwith life-threatening brittle diabetes mellitus.The cells produce insulin from theliver, <strong>of</strong>ten curing the patient’s diabetes.Getting a donated pancreas and itscells to the patient in time is challenging,as the organ and its islet cells candie during transportation. The longer thetransportation process takes, the moretissue dies. Surgeons race against time,especially in cases where the organ musttravel a great distance.Klearchos K. Papas, PhD, and histeam are evaluating a relatively simplemethod <strong>of</strong> preserving organs throughimproved oxygenation. They have createdthe tools necessary to preserve andtransport not only pancreata that are tobe used to isolate and purify islet cells,but also other organs.Klearchos K. Papas, PhD, developed technology toallow donor organs and islet cells to be transportedlonger distances.“For example, this technology couldextend the life <strong>of</strong> hearts, increasing thenumber <strong>of</strong> viable organs available fortransplant,’’ said Dr. Papas, pr<strong>of</strong>essor <strong>of</strong>surgery in the Division <strong>of</strong> AbdominalTransplantation and scientific director<strong>of</strong> the Institute for Cellular Transplantation.Dr. Papas believes the technologycan extend the life <strong>of</strong> a donated heart to12 hours or more, as opposed to the fourto six hours currently acceptable, allowingfor better matches, access to morepatients, and reduced cost.Dr. Papas and his team have advancedthe technology through fundingby the National Institutes <strong>of</strong> Health(NIH) Small Business InnovationResearch Program. Dr. Papas, an engineer,came to the UA in <strong>2011</strong> from the<strong>University</strong> <strong>of</strong> Minnesota. He and his teamconducted early pro<strong>of</strong>-<strong>of</strong>-conceptresearch through seed funding from privatedonations from the Iacocca FamilyFoundation, the Carol Olson MemorialResearch Fund and the Schott Foundation.That research led to NIH funding.Oxygen is the key in extending thelife <strong>of</strong> an organ, and scientists have useda variety <strong>of</strong> methods in an attempt to sufficientlyoxygenate tissues. “Traditionally,a pancreas or other organ is placed inwhat is effectively an ice bucket, obviouslynot an ideal method <strong>of</strong> transportingan organ,’’ Dr. Papas said.Dr. Papas tapped intoexisting technology used in theSea Wolf nuclear submarine to designa portable device that can createoxygen from a small amount <strong>of</strong> waterin order to pump humidified oxygenenrichedgas through the organ’svessels during transportation, atechnique known as persufflation.The use <strong>of</strong> persufflation in preservingorgans had been limited in the pastbecause a simple method for using itduring transportation – especially by air– was lacking. The new, portable technology,which eliminates the need for gascylinders, is ready for clinical translationand will be tested in pilot human trials inEurope in <strong>2012</strong>, Dr. Papas said.The technology and tools developedby Dr. Papas and his team also couldaid in extending the life <strong>of</strong> organs fromdonors after cardiac death.“For instance, the vast majority <strong>of</strong>hearts from donors after cardiac death arenot used for transplant because currentprotocols are not able to properly preservetheir viability,” said Dr. Papas.“The longer you wait, the more theorgan dies.’’Dr. Papas and his team, through agrant from the Diabetes Research WellnessFoundation, are working with the<strong>University</strong> <strong>of</strong> Newcastle and King’s8
Athens-Geneva-Tucson ProjectKlearchos K. Papas, PhD, and his team are joining in an internationaleffort to expand islet transplants to patients in Europe with brittle diabetesmellitus.In what is known as the Athens-Geneva-Tucson Project, the UA is sendingtheir new tools, technologies, and staff to aid in an effort to bring islet transplantationto Athens.Theodore Karatzas, MD, a surgeon from Athens, hoped to provide islettransplants to his critically ill diabetic patients in Greece. However, Greece doesnot have an islet cell transplant center, which would cost millions <strong>of</strong> dollars tobuild and operate.Geneva has a very active and highly successful islet transplant program.Dr. Karatzas entered into an agreement with Dr. Thierry Berney, MD, whodirects the program at the <strong>University</strong> <strong>of</strong> Geneva, that when a donated pancreasbecomes available in Greece, it would be flown to Geneva, where the islet cellswould be isolated and flown back to Athens for transplantation.Twice an attempt was made, but twice the islet cells were <strong>of</strong> insufficientnumbers and quality after isolation in Geneva for a successful transplant, presumablybecause it took too long to get the pancreas to Geneva.Drs. Papas, Karatzas, and Berneyhave teamed up and are expected to usethe new technologies and tools to makeislet transplantation a reality in Athens.Technologies developed by Dr. Papasand his team, thanks to funds fromthe National Institutes <strong>of</strong> Health andJuvenile Diabetes Research Foundation,can better preserve the pancreas, transferislets more safely, and determine ifthe cells are viable before transplantation.A highly trained UA team is aidingin the project. Bill Scott, who is gettinghis PhD in biomedical engineering, willbe in Athens; he will board an airplanewith the equipment and the organ andCollege in London to determine whetherpersufflation can extend the viability<strong>of</strong> pancreata from donors after cardiacdeath. They also are examining whetherit could expand the viability <strong>of</strong> organs indonors over age 50.“The early data is very promising,’’Dr. Papas said.UA researchers test the persufflation device inthe U.S. in preparation for the Athens-Genevaproject.fly to Geneva. Kate Mueller, a UA research specialist, will be stationed in Genevaand will evaluate the islets. She will place them in specialized culture containersand fly with them back to Athens, where she will reevaluate them to determineif they remain viable for transplantation.The new technologies developed by Dr. Papas and his team are improvingeach step in the process, with the hope <strong>of</strong> successful long-distance transplantation.The goal is to create centers that can provide transplants using organsfrom thousands <strong>of</strong> miles away, expanding the number <strong>of</strong> successful proceduresthroughout the world.“The successfuldevelopment <strong>of</strong>this technologywill help savelives by increasingthe number<strong>of</strong> patientsreceiving transplants.”– Horacio Rilo, MDIslet Transplants at UAIslet autotransplants (self-donated)currently are performed at The <strong>University</strong><strong>of</strong> Arizona Medical Center to treatchronic pancreatitis. The UA <strong>Department</strong><strong>of</strong> <strong>Surgery</strong> Comprehensive Center forChronic Pancreatitis, in conjunctionwith the Institute for Cellular Transplantation,under the direction <strong>of</strong> HoracioRilo, MD, has performed 30 isletautotransplants to date. The UA hopesto begin islet allotransplants for patientssuffering with type 1 diabetes mellitusin <strong>2012</strong>.Islet transplants to treat patientswith type 1 diabetes mellitus are currentlyin Phase 3 clinical trials in the U.S.,sponsored by the National Institutes<strong>of</strong> Health.“The number <strong>of</strong> patients needingand waiting for a lifesaving transplantfar outpaces the supply <strong>of</strong> availableorgans,” said Dr. Rilo. “The successfuldevelopment <strong>of</strong> this technology will helpsave lives by increasing the number <strong>of</strong>patients receiving transplants.”Rainer W.G. Gruessner, MD, chief<strong>of</strong> the Division <strong>of</strong> Abdominal Transplantationand chairman, UA <strong>Department</strong><strong>of</strong> <strong>Surgery</strong>, added, “Both islet allotransplantsand pancreas transplants havebeen shown to be successful options forpatients with diabetes mellitus and itsadvanced secondary complications,such as metabolic control problems,end-stage renal disease, neuropathy,and gastropathy.“While results for pancreas transplantshave beensteadily improvingover the pastfour decades, withone-year patientsurvival rates <strong>of</strong>more than 95 percentand one-yeargraft survival rates<strong>of</strong> more than 80percent, the results<strong>of</strong> islet transplantscontinue to trailthose <strong>of</strong> pancreastransplants,” Dr. Gruessner said.“Emphasizing islet allotransplants asa research focus within the UA <strong>Department</strong><strong>of</strong> <strong>Surgery</strong> will establish the departmentas a national and internationalleader in transplant options for patientswith insulin-dependent diabetesmellitus.”9
Innovative Education12for a transplant surgery fellowship. Thetwo-year program will train one fellowevery year beginning July 2013.The fellow will be integrally involvedin all aspects <strong>of</strong> patient care:evaluation for a transplant, whether asan outpatient or under urgent inpatientcircumstances; operative and perioperativesurgical, medical, and immunosuppressivecare; and posttransplant inpatientand chronic outpatient follow-up.All applicants will have completeda general surgery residency program bythe time the fellowship begins.Minimally Invasive PostdoctorateResearch FellowshipThe Arizona Center for Endoscopic<strong>Surgery</strong> (ACES) in the UA <strong>Department</strong><strong>of</strong> <strong>Surgery</strong> Section <strong>of</strong> MinimallyInvasive and Robotic <strong>Surgery</strong> now <strong>of</strong>fersgeneral surgery residents an opportunityto participate in mentored research inthe field <strong>of</strong> minimally invasive surgery.The one-year postdoctoral scholar engagesin comprehensive research to helpevolve endoscopic surgery.Research can focus on robotic surgery,single-incision laparoscopic surgery(SILS), natural orifice translumenalendoscopic surgery (NOTES), metabolicsurgery procedures and outcomes, benignand malignant esophageal diseases,or evaluation <strong>of</strong> novel surgical devicesand procedures.The fellow participates in the surgicaleducation lab, teaching laparoscopicsurgical skills to residents and medicalstudents, and conducting researchin surgical education and minimallyinvasive surgery.ASTEC, first createdby the <strong>Department</strong> <strong>of</strong><strong>Surgery</strong>, has expandedto include all studentsand residents in theCollege <strong>of</strong> Medicine,as well as emergencypre-hospital health carepr<strong>of</strong>essionals.Digital rendering <strong>of</strong> proposed ACES training lab, which will focus on teaching surgery residents newminimally invasive and robotic surgical procedures. The <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> is fundraising for the$350,000 needed to expand the state-<strong>of</strong>-the-art simulation lab to eight stations.Larger Space forState-<strong>of</strong>-the-ArtTraining LabsArizona Center for Endoscopic<strong>Surgery</strong> (ACES)The UA <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong>’s AdvancedLaparoscopic/Robotic TrainingCourse has expanded to become theArizona Center for Endoscopic <strong>Surgery</strong>(ACES). Renovation will create a morecomprehensive program to develop andimprove surgical techniques throughanimate learning.The training center will featurestate-<strong>of</strong>-the-art facilities with the latestsimulation technologies and the mostmodern operating rooms that includerobotic, laparoscopic, and endoscopicequipment. Eight surgical stations willbe developed and will be available foruse on a year-round basis.A main focus <strong>of</strong> the center will beto provide participants with realistic andrelevant contexts in which to developtheir surgical understanding, knowledgeand competence. Medical students andsurgery residents will learn basicskills and rapidly adapt to a clinicalenvironment. The program also willserve as an interactive and dynamic wayto refine the minimally invasive and roboticsurgery skills <strong>of</strong> practiced surgeons.ACES has created successful partnershipswith industry to ensure theprogram’s sustainability. The center alsohas partnered with ASTEC (ArizonaSimulation Technology and EducationCenter) to provide a simulation-trainingmodel for instruction in minimally invasivesurgery.“The program’s expansion willlead to improved patient outcomes andrecovery and to the advancement <strong>of</strong> techniquesrequired for new types <strong>of</strong> minimallyinvasive surgical procedures,” saidCarlos Galvani, MD, associate pr<strong>of</strong>essorand director, Minimally Invasive,Robotic and Bariatric <strong>Surgery</strong>.Arizona Simulation Technologyand Education CenterThe Arizona Simulation Technologyand Education Center (ASTEC) hasmoved to a larger space in the UA College<strong>of</strong> Medicine. The expansion triplesthe size <strong>of</strong> the simulationtraining lab, which provideshigh-tech training forthousands <strong>of</strong> medical pr<strong>of</strong>essionalseach year. ASTEChas been so successful sinceits opening in 2005 that itoutgrew its previous space.Simulation-based medicaleducation uses interactivetechnologies in realistichealth care settings tohelp participants developand refine specific diagnostic,cognitive, and surgicaltechniques in a safe setting– before caring for realpatients. Simulation-based
medical education is revolutionizing theway hospitals and medical schools traindoctors and nurses and is enhancingpatient safety at the same time.The new lab features a more openenvironment for training future surgeons,including additional space forlaparoscopic training for surgery residents.The center is equipped with fiveseparate training pods that can beindividualized for all College <strong>of</strong> Medicinedepartments and provide simultaneousinstruction intended to process an entireclass <strong>of</strong> medical students in one day.ASTEC <strong>of</strong>fers training for all levelswithin the college and for regionalpre-hospital organizations. It now hasthe flexibility to transform the lab spaceto meet the needs <strong>of</strong> any size simulatedenvironment.“This is particularly beneficial forcritical trauma and/or OR simulatedevents that require multidisciplinaryteams, as well as for mass casualty exercisesthat occur in the field,” said AllanJ. Hamilton, MD, pr<strong>of</strong>essor <strong>of</strong> surgeryin the Division <strong>of</strong> Neurosurgery andASTEC director.Twelve Residents and FellowsGraduate in <strong>2011</strong>Former UA <strong>Surgery</strong> Chairman Receives<strong>Department</strong>’s Distinguished Leadership AwardThe UA <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong>honored its former chairman,Bruce E. Jarrell, MD, with the <strong>2011</strong>Distinguished Leadership Award. Theaward is presented annually to recognizeoutstanding leadership that has led toimproved surgical practices.Dr. Jarrell served as UA <strong>Department</strong><strong>of</strong> <strong>Surgery</strong> chairman from 1990 to 1997.For four years he served as chair <strong>of</strong> theboard <strong>of</strong> the UA faculty practice plan. Hewas a founding member <strong>of</strong> the UA BiomedicalEngineering Program, a joint effortbetween the <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong>and the <strong>Department</strong> <strong>of</strong> Aerospace andMechanical Engineering that was fundedby a Whitaker Foundation SpecialOpportunity Award.Dr. Jarrell went to the <strong>University</strong> <strong>of</strong>Maryland School <strong>of</strong> Medicine in 1997 aspr<strong>of</strong>essor and chair <strong>of</strong> the <strong>Department</strong> <strong>of</strong><strong>Surgery</strong> and moved to the Dean’s Officein 2003 to serve as executive vice dean.General <strong>Surgery</strong>: James J.P. Rough, MD, accepted a fellowship in plasticand reconstructive surgery at the <strong>University</strong> <strong>of</strong> California, Los Angeles; BrianK. Madigan, MD, is staying at the UA to complete a cardiothoracic surgeryfellowship; Felipe B<strong>of</strong>f Maegawa, MD, is practicing general and hepatobiliarysurgery; Sarah M. Popek, MD, has begun a colorectal surgery fellowship at the<strong>University</strong> <strong>of</strong> Southern California; Zachary C. Taylor, MD, is staying at the UA tocomplete a fellowship in vascular surgery; Norma T. Walks, MD, is now a generalsurgeon in Luverne, Minnesota.Neurosurgery: Benjamin J. Serxner, MD, started fellowship training in complexspine surgery in Colorado.Urology: Lipika R. McCauley, MD, entered private practice in Phoenix.Cardiothoracic <strong>Surgery</strong>: Aleem Siddique, MD, accepted a transplant fellowshipat Freeman Hospital in Newcastle, United Kingdom.Surgical Critical Care: Jorge Con, MD, is the first Acute Care <strong>Surgery</strong> fellow at the<strong>University</strong> <strong>of</strong> Arizona.Vascular <strong>Surgery</strong>: Layla Corral Lucas, MD, is practicing vascular surgery inTucson with an emphasis on limb salvage.Podiatric <strong>Surgery</strong>: Brian D. Lepow, DPM, has joined his family’s private practicein Houston and plans to establish a limb salvage program at Texas Medical Center.Dr. Jarrellrecently was promotedto seniorvice president andchief academic andresearch <strong>of</strong>ficerat the <strong>University</strong><strong>of</strong> Maryland. Healso is dean <strong>of</strong> theGraduate School.In his new role, Dr.Jarrell will be responsible for facilitatingthe research mission <strong>of</strong> the <strong>University</strong><strong>of</strong> Maryland, as well as function as theuniversity’s provost in matters related tothe university’s Strategic Alliance.A graduate <strong>of</strong> the <strong>University</strong> <strong>of</strong> Delawarein chemical engineering, Dr. Jarrellreceived his medical degree from JeffersonMedical College in Philadelphia. Hecompleted residency training in generalsurgery at the Medical College <strong>of</strong> Virginiaand a fellowship in renal transplantationat McGuire Veterans Affairs Hospital.Since 1986, Dr. Jarrell has beenfunded by the National Institutes <strong>of</strong>Health, the National Science Foundation(NSF), the <strong>Department</strong> <strong>of</strong> Defense, andcorporate sources. He holds 22 patents.He served on the “Journey to Mars”committee cosponsored by the NationalAeronautics and Space Administration(NASA).He currently is a co-investigator onan NSF grant to develop a Web-basedhigh school curriculum to increase interest<strong>of</strong> women and minorities in science,technology, engineering, and mathematics(STEM). The author <strong>of</strong> two populartextbooks in surgery, he has receivednumerous teaching and alumni awards.“We chose Dr. Jarrell for this year’saward because <strong>of</strong> his past leadershipas department chair at the UA and forhis academic excellence shown in hiscurrent position as the new senior vicepresident at the <strong>University</strong> <strong>of</strong> Maryland,”said Rainer W.G. Gruessner, MD, UA<strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> chairman.13
Innovative Education<strong>Surgery</strong> Residents and Fellows – PresentationsAngela Echeverria, MD, POSTGRADUATE YEAR (PGY) IISociety for Laparoendoscopic Surgeons, “Multipurpose InternalRetractor for Single Incision <strong>Surgery</strong>.”Evan Glazer, MD, PGY IIINational Podium Presentation: SWOG Cooperative Group SpringMeeting,“Prospective Validation <strong>of</strong> Karyometric Analysis <strong>of</strong>Cutaneous Squamous Cell Carcinoma,” April <strong>2011</strong>.Society <strong>of</strong> Surgical Oncology Annual Cancer Symposium, PosterPresentation: “Karyometry <strong>of</strong> Cutaneous Squamous Cell CarcinomaDiscriminates between Aggressive and Nonaggressive Phenotypes,”<strong>2011</strong>.97th Annual Clinical Congress: American College <strong>of</strong> Surgeons, PosterPresentation, “A Hands-On Experience Improves Medical StudentTrauma-Related NBME Standardized Exam Scores,” <strong>2011</strong>.SWOG Cooperative Group Meeting, Oral Presentation, “ProspectiveValidation <strong>of</strong> Karyometric Analysis <strong>of</strong> Cutaneous Squamous CellCarcinoma,” Oct <strong>2011</strong>.Pantelis Hadjizacharia, MD, PGY IV“Prothrombin Complex Concentrate: An Effective Therapy inReversing the Coagulopathy <strong>of</strong> Traumatic Brain Injury” AmericanAssociation for the <strong>Surgery</strong> <strong>of</strong> Trauma, Sept <strong>2011</strong>.Maria Michailidou, MD, PGY IAmerican Association for the <strong>Surgery</strong> <strong>of</strong> Trauma, “’BLUSH’ on CT:Often Unimportant!,” Sept <strong>2011</strong>.Wood Trauma Competition, “Video Laryngoscopy vs. DirectLaryngoscopy Trauma Patients,” Nov <strong>2011</strong>.Francisco Mora, MD, PGY IIPan American Society Conference, Asuncion, Paraguay, Nov <strong>2011</strong>.David Ritsema, MD, PGY VIAUA Annual Meeting, “Reviewing Radiographic Images with Patients:Results <strong>of</strong> a Randomized Trial on Patient Preferences, Understanding,and Satisfaction,” May <strong>2011</strong>.Arizona Urological Society Annual Meeting, “Systems-basedEvaluation <strong>of</strong> Sequential Compression Devices in Post-operativePatients,” April <strong>2011</strong>.Bernardino Rocha, MD, PGY IAmerican Association for the <strong>Surgery</strong> <strong>of</strong> Trauma, Sept <strong>2011</strong>:• “Evaluation <strong>of</strong> Multidetector Computed Tomography for NeckPenetrating Neck Injury: A Prospective Multicenter Study.”• “Prospective Evaluation <strong>of</strong> Selective Nonoperative Management <strong>of</strong>Torso Gunshot Wounds: When is it Safe to Discharge?”• “Anemia and Transfusions on Traumatic Brain Injury.”• “The Impact <strong>of</strong> Admission Hyperfibrinolysis on Mortality in TraumaPatients.”• “Assessment <strong>of</strong> an Intervention Bundle for Traumatic Brain Injury:When Are Intracranial Pressure Monitors Necessary?”Cassandra Villegas, MD, PGY I“Does Trauma Center <strong>Volume</strong> for Penetrating Trauma ImproveSurvival among Patients with Penetrating Injuries?” AmericanAssociation for the <strong>Surgery</strong> <strong>of</strong> Trauma, Sept <strong>2011</strong>.Luke X Zhan, MD, PGY IISociety <strong>of</strong> Vascular <strong>Surgery</strong>, “Comparison <strong>of</strong> Early Hemodynamicsafter Endovascular Therapy and Open Surgical Bypass in Patients withDiabetes and Critical Limb Ischemia: Does Mode <strong>of</strong> RevascularizationMatter?,” June <strong>2011</strong>.Resident Awards & Recognition14Mohammad Khreiss, MD,fifth-year general surgeryresident, received The WendellB. Whitacre OutstandingSurgical Chief ResidentAward. Presenting the awardis Wendell Whitacre, MD, long-time supporter <strong>of</strong> the <strong>Department</strong><strong>of</strong> <strong>Surgery</strong>. Dr. Whitacre, a retired surgeon, established theannual award to support resident education by recognizing andencouraging outstanding surgery residents.Ulises Garza, MD, post-doctoral research fellow in the Section <strong>of</strong>Minimally Invasive and Robotic <strong>Surgery</strong>, was invited to representhis home country <strong>of</strong> Mexico at the 3rd biennial joint conference,Collaborating Across Borders III (CAB III), “Interpr<strong>of</strong>essionalCollaboration: From Concept to Preparation to Practice,” inNovember.Maria Michailidou, MD, first-year general surgery resident, wonfirst place at the Arizona Committee on Trauma Competition inScottsdale. Her topic was “Use <strong>of</strong> a Videolaryngoscopy for TraumaPatients.”Francisco Mora, MD, second-year general surgery resident,received the International Trauma and Disaster Institute Scholarshipfrom Dr. Susan Briggs <strong>of</strong>Massachusetts General Hospital.Dr. Mora also had theopportunity to participatein the Post Traumatic StressConference as an instructorin the PTS Basic TraumaCourse, training 20 localphysicians.
<strong>Surgery</strong> Residents and Fellows – PublicationsCristina Cueto, MD, PGY V“Disparities in Treatment and Survival <strong>of</strong> White and Native AmericanPatients with Colorectal Cancer: A SEER Analysis” Journal <strong>of</strong> theAmerican College <strong>of</strong> Surgeons, Oct <strong>2011</strong>.Nazanin Ehsani-Chimeh, MD, PGY I“The Effect <strong>of</strong> Vitronectin on the Differentiation <strong>of</strong> Embryonic StemCells in a 3D Culture System” Biomaterials, Dec <strong>2011</strong>.Evan Glazer, MD, PGY III“Karyometry <strong>of</strong> Cutaneous Squamous Cell Carcinoma Discriminatesbetween Aggressive and Nonaggressive Phenotypes” Ann Surg Onc,<strong>2011</strong>.“Long-term Survival after Radi<strong>of</strong>requency Ablation for Cirrhoticswith Unresectable Hepatocellular Carcinoma” Ann Surg Onc, <strong>2011</strong>.“Nuclear Morphometry Identifies a Distinct Aggressive CellularPhenotype in Cutaneous Squamous Cell Carcinoma,” Canc Prev Res,<strong>2011</strong>, Epub ahead <strong>of</strong> press.“Bioengineered Human Arginase I with Enhanced Activity and StabilityControls, Hepatocellular and Pancreatic Carcinoma Xenografts,”Transl Oncol, <strong>2011</strong>;4(3):138-46.“Asymptomatic Lower Extremity Acrocyanosis: Report <strong>of</strong> Two Casesand Review <strong>of</strong> the Literature,” Vascular, <strong>2011</strong>, 19(2):<strong>10</strong>5-1<strong>10</strong>.“The Ongoing History <strong>of</strong> Thermal Therapy for Cancer” Peer ReviewManuscripts: Surg Oncol Clin N Am, <strong>2011</strong> April, 20(2):229-35.“Nuclear Morphometry Identifies a Distinct Aggressive CellularPhenotype in Cutaneous Squamous Cell Carcinoma” MD/Linx.com,Nov <strong>2011</strong>.Adam Hansen, Cardiothoracic <strong>Surgery</strong> Fellow“Robotic Reoperative Coronary Artery Bypass,” submitted to InteractCardiovasc and Thor Surg, Feb <strong>2011</strong>.“Postpartum Rupture <strong>of</strong> the Posteromedial Papillary Muscle,” In PressJ Cardiac Surg, Nov <strong>2011</strong>.Ioannis Konstantinidis, MD, PGY II“Twenty-three Years <strong>of</strong> the Warshaw Operation for Distal Pancreatectomywith Preservation <strong>of</strong> the Spleen,” Ann Surg, 253(6):1136-9,Jun <strong>2011</strong>.“A Duodenal Duplication Cyst Causing Recurrent Pancreatitis in aYoung Patient,” Am Surg, 77(9):1267-9, Sept <strong>2011</strong>.“Cytology Adds Value to Imging Studies for Risk Assessment <strong>of</strong> Malignancyin Pancreatic Mucinous Cysts,” Ann Surg, 254(6):977-83,Dec <strong>2011</strong>.“Gallbladder Lesions Identified on Ultrasound. Lessons from the Last<strong>10</strong> Years,” In Press: J Gastrointest Surg, Nov <strong>2011</strong>.Bernardino Rocha, MD, PGY I“The Impact <strong>of</strong> the Duration <strong>of</strong> Platelet Storage in Critically illTrauma Patients,” J Trauma, <strong>2011</strong> Dec, 71(6):1766-1774.“Optimal Positioning for Emergent Needle Thoracostomy:A Cadaver Based Study,” J Trauma, <strong>2011</strong> Nov, 71(5):<strong>10</strong>99-1<strong>10</strong>3.“Intracorporeal Use <strong>of</strong> Advanced Local Hemostatics in a DamageControl Swine Model <strong>of</strong> Grade IV Liver Injury: A RandomizedControlled Preclinical Trial,” J Trauma, <strong>2011</strong> Nov, 71(5):1312-8.“Incidence and Predictors for Fasciotomy after Extremity Trauma:A <strong>10</strong>-year Review in a Mature Level I Trauma Center,” Injury, <strong>2011</strong> Oct,42(<strong>10</strong>):1157-63.“Vascular Trauma in Geriatric Trauma Patients: A National TraumaDatabank Review,” J Trauma, <strong>2011</strong> Oct, 71(4):909-16.“Penetrating Cardiac Injury: A Survivable Injury with a High PostDischarge Complication Rate,” Arch Surg, <strong>2011</strong> Sep, 146(9):<strong>10</strong>61-6.“Effect <strong>of</strong> Age on Cervical Spine Injury on Pediatric Population: A NationalTrauma Databank Review,” J Pediatr Surg, <strong>2011</strong> Sep, 46(09):1771-6.“The Accuracy <strong>of</strong> 64-Slice Computed Tomography in Detecting ClinicallySignificant Arterial Following Pelvic Fractures,” Am Surg, Sept<strong>2011</strong>, 77(9):1176-82.“Clinical Examination is Highly Sensitive in Detecting Clinically SignificantSpinal Injuries Following Gunshot Wounds,” J Trauma, Sept <strong>2011</strong>,71(3):523-7.“The Presence <strong>of</strong> Distracting Injuries does not Affect the Initial ClinicalExamination <strong>of</strong> the Cervical Spine in Evaluable Blunt Trauma Patients:A Prospective Observational Study” J Trauma, <strong>2011</strong> Sep, 71(3):528-32.“Ten-Years <strong>of</strong> Mechanical Complications <strong>of</strong> Central Venous Catheterizationin Trauma Patients at a Level I Trauma Center,” In Print: AmSurg, <strong>2011</strong>.“The Incidence <strong>of</strong> Neurogenic Shock After Spinal Cord Injury in PatientsAdmitted to a High-<strong>Volume</strong> Level I Trauma Center,” In Print: AmSurg, <strong>2011</strong>.“The Impact <strong>of</strong> Early Hormonal Therapy in Catastrophic Brain InjuredPatients and its Effects on Organ Procurement,” In Print: Am Surg,<strong>2011</strong>.“The Need for Early Angiography in Patients with Penetrating RenalInjuries,” In Print: Eur J Trauma and Emerg Surg, <strong>2011</strong>.Raghunandan Venkat, MD, PGY I“Predicting the Risk <strong>of</strong> Perioperative Mortality in Patients UndergoingPancreaticoduodenectomy: A Novel Scoring System,” Arch Surg,146(11):1277-84, Nov <strong>2011</strong>.“Presence <strong>of</strong> Pancreatic Intraepithelial Neoplasia in the PancreaticTransection Margin does not Influence Outcome in Patients with R0Resected Pancreatic Cancer,” Ann Surg Oncol, 18(12):3493-9, Nov <strong>2011</strong>.“The Role <strong>of</strong> Preoperative Neck Ultrasounds to Assess Lymph Nodesin Patients with Suspicious or Indeterminate Thyroid Nodules,” J SurgOncol, Oct <strong>2011</strong>.15
What’s Up In SURGERYVillar Retires after 35 Years <strong>of</strong> Teaching, Research, ServiceAfter more than 35 years <strong>of</strong> dedicatedservice to the UA College <strong>of</strong>Medicine and the <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong>,Hugo Villar, MD, pr<strong>of</strong>essor and chief,Division <strong>of</strong> SurgicalOncology, retired lastJuly. A UA <strong>Department</strong><strong>of</strong> <strong>Surgery</strong> Scientific ResearchSession was heldin honor <strong>of</strong> Dr. Villarlast December.In 1977, Dr. Villarbecame a member<strong>of</strong> the Arizona CancerCenter, founded thatyear at the UA, and later its surgicaldirector. In 1983, the dean <strong>of</strong> the UAHugo Villar, MD, and Rainer W.G.Gruessner, MDCollege <strong>of</strong> Medicine appointed Dr. Villarchief <strong>of</strong> the Division <strong>of</strong> Surgical Oncology.He was named the vice chairman<strong>of</strong> the <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> in 2001,holding that position until 2004, whenhe was appointed the interim departmentchairman. After the recruitment <strong>of</strong>Rainer W.G. Gruessner, MD, to lead the<strong>Department</strong> <strong>of</strong> <strong>Surgery</strong>in 2007, Dr. Villarwas again appointedthe vice chairman <strong>of</strong>the department. In2009, Dr. Villar wasnamed chief <strong>of</strong> generalsurgery at <strong>University</strong>American College <strong>of</strong> SurgeonsThe UA <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> hosted its annual reception for alumni and friendsduring the Clinical Congress <strong>of</strong> the American College <strong>of</strong> Surgeons in San Francisco lastOctober. Save the date – this year’s reception will be held Tuesday, Oct. 2, in Chicago.Randy Wong, Mindy Wong,Brian White, CandiceJensen, Thomas HarmonPhysicians HealthcareHospital (now The<strong>University</strong> <strong>of</strong> ArizonaMedical Center – South Campus).Dr. Villar has been the recipient <strong>of</strong>numerous prestigious appointments atthe UA, serving as director <strong>of</strong> IntraoperativeRadiation Therapy, as the associatedirector <strong>of</strong> the General <strong>Surgery</strong> ResidencyProgram, and as an elected member<strong>of</strong> the Board <strong>of</strong> Directors <strong>of</strong> <strong>University</strong>Physicians Healthcare.In 2007, he was named the DistinguishedLatin American Surgeonin the United States for 2007 by theFederation <strong>of</strong> Latin American Surgeons(FELAC – Federación Latino Americanade Cirugía) for his leadership in surgicaleducation in Latin America. He helpeddevelop and implement the AmericanSociety <strong>of</strong> Clinical Oncology (ASCO)Multidisciplinary Cancer ManagementCourse in Latin America, whose purposeis to train physicians in developing countrieson a multidisciplinary approach tocancer care. He served as Chairman<strong>of</strong> the Commission on Cancer and theInternational Relations Committee <strong>of</strong> theAmerican College <strong>of</strong> Surgeons.Rose Pedersen, Elizabeth Tourville, Rainer Gruessner,Parisa MalekzadehKari Schlachtenhaufen,RockwellJackson,Sarah JacksonDiBoiseAlbert Amini, Diane Amini16Mustapha Rao<strong>of</strong>,Terence O’Keeffe, BellalJoseph, John KettelleShane Peck, Jennifer Tittensor,Kimberly Peck
New FacultyChirag S. Desai, MD,assistant pr<strong>of</strong>essor <strong>of</strong>surgery, Division <strong>of</strong>Abdominal Transplantation,comes to the UAfrom Georgetown <strong>University</strong>Hospital in Washington,DC, where hecompleted a multiorgantransplant and hepatobiliary surgery fellowship.Dr. Desai is the first fellow in the UnitedStates to be certified by the American Society<strong>of</strong> Transplant Surgeons (ASTS) for intestinetransplantation.With advanced expertise in solid-organtransplants <strong>of</strong> the liver, intestine, pancreas,and kidney, Dr. Desai also is a member <strong>of</strong> theUA <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> HepatoPancreaticoBiliary(HPB) Center team. This highlyspecialized service deals with all conditionsthat affect the liver, gallbladder, bile ducts,pancreas, and duodenum. The conditionsinclude benign and malignant tumors, inflammations,congenital abnormalities, and traumaticinjuries.Dr. Desai received his medical degreeand residency training at Seth G.S. MedicalCollege, King Edward Memorial Hospital, <strong>University</strong><strong>of</strong> Mumbai, India. He served as a livertransplant associate (Visiting Physician Program)at Mt. Sinai Hospital in New York.His research interests focus on the outcomes<strong>of</strong> liver and intestine transplantationthrough clinical research. Dr. Desai has authoredseveral publications and articles inpeer-reviewed journals.Audrey Erman, MD, isassistant pr<strong>of</strong>essor, Division<strong>of</strong> Otolaryngology– Head and Neck<strong>Surgery</strong>, and co-director<strong>of</strong> the Head and NeckOncology Program.Specializing in the treatment<strong>of</strong> head and neckmalignancies, (including melanoma and otherskin cancers, as well as salivary glands, thyroidand paratumors <strong>of</strong> the thyroid, tongue, lipsand oral cavity, larynx, pharynx, and sinuses),Dr. Erman brings to Arizona the latest microvasculartissue-transfer techniques for reconstructionfollowing surgery for head and neckcancer.Dr. Erman attended medical school atthe <strong>University</strong> <strong>of</strong> Michigan, where she waspresented the Furstenberg Award for exceptionalachievement in otolaryngology. Shecompleted her residency at the <strong>University</strong> <strong>of</strong>Michigan, the preeminent otolaryngology –head and neck surgery training program inthe country.Dr. Erman pursued fellowship training inhead and neck surgical oncology at the MassachusettsEye and Ear Infirmary, a Harvardaffiliatedhospital. She received extensivetraining in both surgical oncology and advancedreconstructive surgery for defects <strong>of</strong>the head and neck.As a result <strong>of</strong> her research on the sentinellymph node biopsy technique, which testssome <strong>of</strong> the patient’s lymph nodes to evaluatefor cancer, Dr. Erman has published thelargest single-institution review <strong>of</strong> the procedurefor use in head and neck melanoma.She has presented her research at nationalmeetings.Thomas Gernon, MD,assistant pr<strong>of</strong>essor,Division <strong>of</strong> Otolaryngology– Head andNeck <strong>Surgery</strong>, is afellowship-trained headand neck and microvascularreconstructivesurgeon specializing intransoral robotic surgery (TORS). Co-director<strong>of</strong> the Head and Neck Oncology Program, Dr.Gernon provides treatment for patients withbenign and malignant masses <strong>of</strong> the headand neck, including tumors <strong>of</strong> the tongue,lips, oral cavity, larynx, pharynx, thyroid, andparathyroid.Dr. Gernon attended the <strong>University</strong> <strong>of</strong>Washington Medical School, graduatingwith honors; he was elected to the AlphaOmega Alpha (AOA) medical honor society.He completed his residency training in otorhinolaryngology:head and neck surgery atthe <strong>University</strong> <strong>of</strong> Michigan with specializedtraining in the area <strong>of</strong> head and neck surgicaloncology.Following residency, Dr. Gernon completedthe head and neck surgical oncologyand microvascular reconstruction fellowshipat the <strong>University</strong> <strong>of</strong> Washington, wherehe worked with NealFutran, MD, one <strong>of</strong> theworld’s most renownedhead and neck oncologicand reconstructivesurgeons.U.S. Navy veteran Donald(D.J.) Green, MD,has been appointed associate pr<strong>of</strong>essor <strong>of</strong>surgery in the Division <strong>of</strong> Trauma, CriticalCare, and Emergency <strong>Surgery</strong> and medicaldirector <strong>of</strong> trauma services at the <strong>University</strong> <strong>of</strong>Arizona Medical Center – South Campus.Dr. Green served as a general surgeon for<strong>10</strong> years in the U.S. Navy, where he completedtours in Iraq and Afghanistan. He then spentsix years at the Navy Trauma Training Centerat the Los Angeles County Medical Center,preparing doctors, nurses, and other staffmembers to care for wounded soldiers in thetrauma centers in Iraq and Afghanistan.Dr. Green received his medical degree atthe <strong>University</strong> <strong>of</strong> Washington, and completedhis residency training at the <strong>University</strong> <strong>of</strong>Arizona. He completed a fellowship in surgicalcritical care at the <strong>University</strong> <strong>of</strong> SouthernCalifornia.He is a member <strong>of</strong> the American College<strong>of</strong> Surgeons, the Association for Surgical Education,and the Special Operations MedicalAssociation. He has coauthored more than 38publications. His research focuses on injuryprevention.Lynn Gries, MD, hasbeen appointed assistantpr<strong>of</strong>essor <strong>of</strong> surgeryin the Division <strong>of</strong>Trauma, Critical Care,and Emergency <strong>Surgery</strong>.Dr. Gries receivedher medical degreefrom McGill <strong>University</strong>.She completed her general surgery residencytraining at the <strong>University</strong> <strong>of</strong> Colorado HealthSciences Center, Denver.She also completed a General <strong>Surgery</strong>Basic Science Research Fellowship at DenverHealth Medical Center, <strong>University</strong> <strong>of</strong> ColoradoHealth Sciences Center, as well as a CriticalCare, Trauma, and Acute Care <strong>Surgery</strong> Fellowshipat Wake Forest <strong>University</strong> Baptist MedicalCenter, Winston-Salem, NC.Abraham Jacob, MD,has joined the Division<strong>of</strong> Otolaryngology– Head and Neck<strong>Surgery</strong> as associatepr<strong>of</strong>essor <strong>of</strong> surgeryand director <strong>of</strong> the UAEar Institute. Dr. Jacobcomes to the UA fromthe <strong>Department</strong> <strong>of</strong> Otolaryngology – Headand Neck <strong>Surgery</strong> at Ohio State <strong>University</strong> inColumbus, where he served on the faculty forfive years.17
After receiving his medical degree fromthe <strong>University</strong> <strong>of</strong> Michigan, Dr. Jacob completedhis internship in general surgery andresidency training in otolaryngology at Washington<strong>University</strong> School <strong>of</strong> Medicine andBarnes-Jewish Hospital in St. Louis. He subsequentlycompleted a fellowship in otology,neurotology, and cranial base surgery at OhioState <strong>University</strong>.Dr. Jacob specializes in the surgicalmanagement <strong>of</strong> diseases <strong>of</strong> the ear, facialnerve, and base <strong>of</strong> the skull. He is an expertin middle-ear surgery, cochlear implants,BAHA (bone-anchored hearing aid) hearingrestoration, surgically implantable hearingaids, acoustic neuromas (vestibular schwannomas),and facial nerve disorders.His ongoing research focuses on preclinicaldrug development for tumors associatedwith neur<strong>of</strong>ibromatosis type 2, such as vestibularschwannomas and meningiomas, as wellas prevention and treatment <strong>of</strong> chemotherapy-inducedhearing loss (ototoxicity). Hisresearch is funded by the National Institutes<strong>of</strong> Health.Dr. Jacob has published extensively inpeer-reviewed journals and presented at bothnational and international meetings. He is amember <strong>of</strong> the Alpha Omega Alpha medicalhonor society and has received several otolaryngologyspecialty-specific awards, includingthe Nicholas Torok Award from the AmericanNeurotology Society and the George AdamsAward from the Triological Society.NEWS BRIEFUrology Moves to<strong>University</strong> <strong>of</strong> ArizonaCancer Center – NorthCampusThe <strong>University</strong> <strong>of</strong> Arizona Cancer Center– North Campus, 3838 N. CampbellAve., is the new home <strong>of</strong> the Divison<strong>of</strong> Urology. The new facility will allowfor more patient visits and shorterwaiting time, as well as centralize andconsolidate two multidisciplinaryclinics: Genitourinary Oncology(prostate, bladder, kidney, testis,adrenal, and penile cancers), PelvicFloor Disorders, and ReconstructiveUrology (a complex subspecialtythat requires multidisciplinary careand includes all facets <strong>of</strong> urinarydysfunction in men and women).Samuel Kim, MD, assistantpr<strong>of</strong>essor, recentlyrecruited to the Division<strong>of</strong> Cardiothoracic<strong>Surgery</strong>, is the onlysurgeon in SouthernArizona <strong>of</strong>fering patientsless-invasive alternativesif they need lung tissueremoved: video-assisted thoracic surgery(VATS) and robot-assisted surgery.In traditional open-chest lung surgery,or thoracotomy, doctors cut a long incisionthrough muscle and spread apart the ribcage. VATS and robot-assisted surgery usingthe da Vinci surgical robot allow doctors toperform chest surgery through two to foursmall incisions, most less than an inch long.Patients who undergo minimally invasiveprocedures spend less time in the hospital,need less pain medication, have less scarring,and recover faster than those who undergoopen-chest surgery.Dr. Kim also specializes in minimally invasiveand robot-assisted procedures for benignand cancerous diseases <strong>of</strong> the esophagus, includingcomplex esophageal reconstruction,robot-assisted thymectomy, and trachealresection and reconstruction.Dr. Kim received his undergraduate degreewith honors in biophysics from JohnsHopkins <strong>University</strong> and his medical degreefrom Tufts <strong>University</strong> School <strong>of</strong> Medicine.He completed residency training in generalsurgery at the <strong>University</strong> <strong>of</strong> PennsylvaniaHospital and in cardiothoracic surgery at MassachusettsGeneral Hospital. In addition, hecompleted a minimally invasive esophagealsurgery training at the <strong>University</strong> <strong>of</strong>Pittsburgh and advanced thoracic surgerytraining at the Mayo Clinic.Author <strong>of</strong> several journal articles, Dr. Kimis interested in the investigation <strong>of</strong> geneticmarkers associated with improved clinicaloutcome in lung and esophageal cancerpatients and in the development <strong>of</strong> noveltargeted therapies.Ethan E. Larson, MD,has joined the Division<strong>of</strong> Reconstructive andPlastic <strong>Surgery</strong> as assistantpr<strong>of</strong>essor. Dr.Larson performs all aspects<strong>of</strong> plastic surgery,including reconstruction<strong>of</strong> traumatic, oncologic,or surgical defects, as well as breast reduction,body contouring, and cosmetic surgery.Dr. Larson has special expertise in microsurgicalreconstructive treatment optionsfor patients, including breast reconstructionfollowing mastectomy. He is one <strong>of</strong> the fewsurgeons in Southern Arizona to <strong>of</strong>fer microsurgicalbreast reconstruction with a freeDIEP (deep inferior epigastric perforator) flap,which uses skin, tissue, and tiny blood vesselstaken from the patient’s abdomen to form anew breast, while preserving the abdominalmuscle.A native <strong>of</strong> Tucson, Dr. Larson attendedthe <strong>University</strong> <strong>of</strong> Arizona, graduating summacum laude with degrees in both microbiologyand psychology. He was the senior student<strong>of</strong> the year and a NASA space-grant researchfellow. He attended the UA College <strong>of</strong> Medicineas a Dean’s Scholar. Dr. Larson completedhis internship and residency in plastic surgeryat Georgetown <strong>University</strong> in Washington, DC.He received fellowship training in microsurgeryand complex oncologic defect reconstructionunder world-famous microsurgeonPeter Neligan, MD, at the <strong>University</strong> <strong>of</strong>Washington.Valentine N. Nfonsam,MD, a specialist in colonand rectal surgery,colorectal oncology,and complex pelvicfloor disorders, has beenappointed assistant pr<strong>of</strong>essorin the Division <strong>of</strong>Surgical Oncology.Dr. Nfonsam performs surgeries for inflammatorybowel disease, anorectal disease, andbenign and malignant colorectal diseases. Heis an expert in the surgical management <strong>of</strong>pelvic floor disease, especially fecal incontinence.He also performs colonoscopies andendoscopic treatment <strong>of</strong> polyps. Dr. Nfonsamis one <strong>of</strong> just a few surgeons in the nationusing minimally invasive techniques for colonand rectal surgery, such as advanced laparoscopy,single-incision surgery, and robotassistedsurgery, which have been shown toreduce the patient’s wound infection rate,postoperative pain, length <strong>of</strong> stay in the hospital,and overall recovery time.A graduate <strong>of</strong> the <strong>University</strong> <strong>of</strong> IllinoisCollege <strong>of</strong> Medicine in Chicago, Dr. Nfonsamcompleted his surgery residency training atNorth Shore-Long Island Jewish Health Systemin New Hyde Park, NY. During his surgicaltraining, he completed a minimally invasivesurgery (MIS) research fellowship at theCleveland Clinic.Dr. Nfonsom comes to the UA from the18
Warren C. Breidenbach III, MD, has joined the UA <strong>Department</strong> <strong>of</strong><strong>Surgery</strong> as pr<strong>of</strong>essor and chief <strong>of</strong> the Division <strong>of</strong> Reconstructiveand Plastic <strong>Surgery</strong>. He is the world leader in hand and compositetissue allotransplantation (CTA). He comes to the UA from the <strong>University</strong><strong>of</strong> Louisville, where he led the team <strong>of</strong> surgeons to performthe nation’s first (and world’s first successful) hand transplant inJanuary 1999. He has since performed more hand transplants than any other surgeon inthe world. Additionally, based on his leadership and expertise in the field, he has trainedthe majority <strong>of</strong> the U.S. teams performing hand transplants.In addition to his leadership role as division chief, Dr. Breidenbach’s goal at the<strong>University</strong> <strong>of</strong> Arizona is to establish an Institute for Composite Tissue Allotransplantationand Regenerative <strong>Surgery</strong>, including hands, face, legs, and feet – the first <strong>of</strong> its kind in thenation.Dr. Breidenbach’s clinical interests are extremity surgery, peripheral nerve compressionproblems, repetitive stress disorders, and reconstructive trauma surgery.He is extensively involved in cutting-edge immunosuppression research, which hastremendous potential for those in need <strong>of</strong> transplants. In addition to CTA, his researchinterests include peripheral nerve outcomes, management <strong>of</strong> extremity pain syndrome,and animal models <strong>of</strong> tolerance induction in CTA.A graduate <strong>of</strong> the <strong>University</strong> <strong>of</strong> Calgary, Dr. Breidenbach received his postgraduatetraining at McGill <strong>University</strong>, in plastic surgery. He completed a one-year microsurgeryfellowship at the Eastern Virginia Medical School in Norfolk, followed by one year as aChristine M. Kleinert Hand Fellow at the <strong>University</strong> <strong>of</strong> Louisville.Dr. Breidenbach was appointed the first Hand Scholar with the Christine M. KleinertInstitute for Hand and Microsurgery for two years. His work on vascularized nerve graftsearned him the American Society <strong>of</strong> Plastic and Reconstructive <strong>Surgery</strong> Clinical ResearchScholarship Award. He also received the Senior Award <strong>of</strong> the American Society <strong>of</strong> Plasticand Reconstructive <strong>Surgery</strong> for his work in blood flow to nerves.He has served as president <strong>of</strong> the International Hand and Composite TissueAllotransplantation Society and is founding president <strong>of</strong> the American Society <strong>of</strong>Reconstructive Transplant. He also served on several committees <strong>of</strong> the American Societyfor <strong>Surgery</strong> <strong>of</strong> the Hand and as secretary <strong>of</strong> the American Society for Peripheral Nerve.Dr. Breidenbach has received numerous awards and honors and has published morethan 80 papers and publications.<strong>University</strong> <strong>of</strong> South Florida, Tampa, where hecompleted a two-year fellowship in colon andrectal surgery. He has taught a course in totalmesorectal excision (TME) in rectal cancertreatment, which is an essential componentin the management <strong>of</strong> rectal cancer. Dr. Nfonsam’sresearch focuses on colorectal cancer inyoung patients, inflammatory bowel disease,and the management <strong>of</strong> pelvic floor disorders.He has published articles on his researchin peer-reviewed journals and has presentedat national and international meetings.Klearchos K. Papas,PhD, MS, BChE, is pr<strong>of</strong>essor<strong>of</strong> surgery in theDivision <strong>of</strong> AbdominalTransplantation andscientific director <strong>of</strong> theInstitute for CellularTransplantation. In hisnew position, Dr. Papas directs new transplantresearch initiatives to treat patients withdiabetes.Dr. Papas is an internationally known experton retrieving, preserving, and assessinginsulin-producing islet cells. Islet transplantationinvolves extracting islet cells from thepancreas and transplanting them into theliver so they can continue to produce insulin.The loss <strong>of</strong> viable islets during the process <strong>of</strong>islet manufacturing is a major challenge inthe field <strong>of</strong> islet transplantation.Dr. Papas previously served on the facultyat the <strong>University</strong> <strong>of</strong> Minnesota, where he wasan associate pr<strong>of</strong>essor <strong>of</strong> surgery, holdingleadership positions as associate director <strong>of</strong>the Islet Transplant Program, director <strong>of</strong> IsletProcessing Research and Development, anddirector <strong>of</strong> the Islet Quality Assurance Core inthe Schulze Diabetes Institute.Dr. Papas came to the United States as aFulbright Scholar in 1986. He attended theGeorgia Institute <strong>of</strong> Technology in Atlanta,where he received his bachelor’s, master’s,and doctorate in chemical engineering, witha focus on tissue engineering for cell-basedinsulin replacement for the treatment <strong>of</strong>diabetes. He completed postdoctoral workwith Novartis Pharmaceuticals in Summit, NJ,in the area <strong>of</strong> metabolic diseases, analytics,and BioNMR (nuclear magnetic resonance).He subsequently held research positions atthe Massachusetts Institute <strong>of</strong> Technologyin the <strong>Department</strong> <strong>of</strong> Chemical Engineering,the Juvenile Diabetes Research Foundation(JDRF) Center for Islet Transplantation at HarvardMedical School, and the Howard HughesMedical Institute at Yale <strong>University</strong>.An editorial board member <strong>of</strong> the journalsCell Transplantation and Cell Medicine, Dr. Papashas published more than 50 articles (33in the past three years). He has been invitednationally and internationally to give numerouspresentations on his research studies onorgan preservation, quality assessment, andcell transplants to treat type 1 diabetes andpancreatitis.Jitesh A. Patel, MD, asurgeon specializingin minimally invasivecolon and rectal surgery,colorectal oncology, andcomplex pelvic floordisorders, has joined theDivision <strong>of</strong> SurgicalOncology as assistantpr<strong>of</strong>essor. Dr. Patel treats a wide range <strong>of</strong> diseases<strong>of</strong> the colon and rectum. He has specialexpertise in advanced minimally invasivetechniques, including transanal endoscopicmicrosurgery (TEMS) for rectal cancers andpolyps.TEMS makes it possible to excise polypsand some lesions high inside the rectumthrough the anus that otherwise would beaccessible only by major abdominal surgery.Patients who are ideal candidates for TEMSavoid a colostomy, a common fear amongthose diagnosed with rectal cancer.Dr. Patel also specializes in advanced laparoscopicsurgery for benign diseases, includinginflammatory bowel disease, diverticulitis,and other conditions <strong>of</strong> the colon, rectum,and anus, such as hemorrhoids and fissures.He also performs colon cancer screening, includingcolonoscopies.Dr. Patel received his medical degree fromthe <strong>University</strong> <strong>of</strong> Medicine and Dentistry <strong>of</strong>New Jersey – Robert Wood Johnson Medical19
Robert S. Poston, MD, nationally knownfor his work in the use <strong>of</strong> robotics for minimallyinvasive cardiac surgery, has beenappointed pr<strong>of</strong>essor and chief <strong>of</strong> the Division<strong>of</strong> Cardiothoracic <strong>Surgery</strong>. In addition,he has been named the Jack G. CopelandEndowed Chair <strong>of</strong> Cardiothoracic<strong>Surgery</strong> at the UA Sarver Heart Center.With his arrival, The <strong>University</strong> <strong>of</strong>Arizona Medical Center – <strong>University</strong>Campus is the only hospital in Arizona, andone <strong>of</strong> only a handful in the nation, to <strong>of</strong>ferrobot-assisted minimally invasive coronaryartery bypass surgery.Minimally invasive, robot-assistedbypass surgery allows physicians to gainaccess to the heart with several smallincisions (unlike conventional bypasssurgery, which requires the chest to beopened with an incision the length <strong>of</strong> thebreastbone, or sternum). With this newprocedure, the patient has smaller scars,fewer side effects and complications, lesspain, reduced risk <strong>of</strong> infection, and fasterrecovery than with conventional bypassgraft surgery. On average, hospital stay isreduced from six to three days.Dr. Poston previously served as chief <strong>of</strong>cardiac surgery at Boston Medical Center;prior to that, he was an associate pr<strong>of</strong>essor <strong>of</strong>cardiac surgery at the <strong>University</strong> <strong>of</strong> MarylandSchool <strong>of</strong> Medicine. He succeeded JackCopeland, MD, who joined the <strong>University</strong> <strong>of</strong>California, San Diego.“My aim for our division is to providedistinctive services that are highly valued bypatients and their families,” said Dr. Poston.“Robot-assisted heart surgery is a primeexample <strong>of</strong> this type <strong>of</strong> service. Similarly,our internationally renowned mechanicalassistprogram, the only one in Tucson, canimprove the quality <strong>of</strong> life for those with severecongestive heart failure.“We encourage patients who mightbe candidates to come to us for a secondopinion so they understand all their options.The emphasis on shared decision-makingwith patients by discussing these types <strong>of</strong>innovative options is a growing priority inhealth care.”Dr. Poston received his undergraduate degreein biology with highest honors from the<strong>University</strong> <strong>of</strong> Texas at Austin and his medicaldegree from the Johns Hopkins School <strong>of</strong> Medicine,as a member <strong>of</strong>the Alpha OmegaAlpha (AOA) medicalhonor society. Hecompleted a generalsurgery residency atthe <strong>University</strong> <strong>of</strong> California-San Francisco; aresearch fellowship in the <strong>Department</strong> <strong>of</strong>Cardiothoracic <strong>Surgery</strong>, CardiothoracicTransplant Laboratory, at Stanford <strong>University</strong>School <strong>of</strong> Medicine; and a cardiothoracicresidency at the <strong>University</strong> <strong>of</strong> PittsburghMedical Center.Dr. Poston has authored more than<strong>10</strong>0 scientific papers and abstracts. Heis currently the principal investigator onseveral multicenter research studies. In afive-year initiative funded by the NationalInstitutes <strong>of</strong> Health (NIH), Dr. Poston isexploring the use <strong>of</strong> high-resolutionimaging technology during heart surgeryto identify the optimal bypass graft fora patient. In another ongoing study, heis investigating the ability <strong>of</strong> roboticsurgery to accelerate the return <strong>of</strong> exercisetolerance, as compared with traditionalsurgical techniques.20School. He completed his residency in generalsurgery at Allegheny General Hospitalin Pittsburgh. During his residency, Dr. Pateldedicated an additional year to basic scienceresearch at the <strong>University</strong> <strong>of</strong> Pittsburgh. Hewent on to complete a fellowship in colonand rectal surgery at Washington <strong>University</strong>/Barnes-Jewish Hospital in St. Louis.Dr. Patel has published more than 24 articles,is an invited reviewer for The AmericanSurgeon, and serves on the editorial board<strong>of</strong> the World Journal <strong>of</strong> Gastrointestinal Endoscopy.His research interests include localexcision for the treatment <strong>of</strong> rectal cancer andinvestigation <strong>of</strong> molecular or genetic markersin determining the response to adjuvanttherapy.Dale Payne, MD, PhD,has joined the Division<strong>of</strong> Cardiothoracic <strong>Surgery</strong>as surgical director<strong>of</strong> the CardiothoracicIntensive Care Unit.Dr. Payne receivedhis doctorate and thenhis medical degree fromOhio State <strong>University</strong>. He completed generalsurgery residency training at the <strong>University</strong> <strong>of</strong>California, Los Angeles and Davis, and cardiothoracicresidency training at the <strong>University</strong><strong>of</strong> Pittsburgh.Following his residency training, Dr. Paynewas recruited to the <strong>University</strong> <strong>of</strong> North Carolinaat Chapel Hill, where he developed anddirected the first heart transplant program inthe state. He then was recruited by the LosAngeles Heart Institute at St. Vincent MedicalCenter to develop and direct its heart transplantprogram and also to direct the heartand lung transplant program at the <strong>University</strong><strong>of</strong> California, Irvine. Dr. Payne returned tothe <strong>University</strong> <strong>of</strong> Pittsburgh to develop anddirect a new open-heart teaching program atWestmoreland Regional Medical Center nearthe <strong>University</strong> Hospital.After moving to Arizona in 2000, hedeveloped a successful cardiothoracic andvascular surgery private practice, serving severalmajor hospitals in Scottsdale, Mesa, andPhoenix. He joined the UA <strong>Department</strong> <strong>of</strong><strong>Surgery</strong> to return to teaching, research, andinvolvement in cutting-edge surgical proceduresas part <strong>of</strong> a major academic surgerydepartment.Dr. Payne has expertise in many areas <strong>of</strong>cardiothoracic and vascular surgery, includingheart transplant and artificial heart devices.He has also been named director <strong>of</strong> the Cardiothoracic<strong>Surgery</strong> Robotic Lab at the <strong>University</strong><strong>of</strong> Arizona.Allen Raczkowski, MD,has joined the Division<strong>of</strong> Cardiothoracic<strong>Surgery</strong> as assistantpr<strong>of</strong>essor <strong>of</strong> surgery.Recognized as one <strong>of</strong> thepioneers in using the daVinci robot for minimallyinvasive coronary operations,Dr. Raczkowski performed hundreds<strong>of</strong> robot-assisted heart surgeries in Phoenixbefore joining the UA.Dr. Raczkowski’s practice focuses onrobot-assisted heart valve surgery, such asmitral valve repair or replacement and robotassistedaortic valve surgery. He was the firstsurgeon in the world to use the robot to donon-arrested mitral repairs in a human. Duringthis procedure, the heart continues tobeat while the valve is repaired. In Arizona, hewas the first to do endoscopic robotic mitralvalve replacement and repairs and the first todo a surgical maze procedure to treat atrial
fibrillation. During the maze surgery, thesurgeon uses small incisions, radio waves,freezing, or microwave or ultrasound energyto create scar tissue to block the abnormalelectrical signals causing the arrhythmia.The <strong>University</strong> <strong>of</strong> Arizona Medical Center– <strong>University</strong> Campus is the only hospital inArizona where mitral valve repair and replacement,aortic valve surgery, and coronary bypassprocedures are performed using theda Vinci surgical robot.Board-certified in surgery and thoracicsurgery, Dr. Raczkowski completed his generalsurgery residency and cardiothoracic surgeryfellowship at the <strong>University</strong> <strong>of</strong> Wisconsin inMadison.Sergio Rivero, MD, hasjoined the Division <strong>of</strong>Neurosurgery as associatepr<strong>of</strong>essor. Dr. Riverospecializes in complexneurosurgery <strong>of</strong> thebrain and spine, includingcervical, thoracic,and lumbar disorders;cervical and lumbar stenosis; cervical andlumbar disc herniations; tumors <strong>of</strong> the brainand spinal cord; and inclusion <strong>of</strong> spinal cordstimulation surgery and peripheral nerve surgery,including carpal tunnel surgery.Dr. Rivero attended medical school at theUniversidad Autónoma de Guadalajara, Mexico.He completed residency and fellowshiptraining at the UA College <strong>of</strong> Medicine, wherehe was one <strong>of</strong> the first residents to completethe UA’s Medical Sciences Graduate Programin Clinical Research.Dr. Rivero is a member <strong>of</strong> the AmericanAssociation <strong>of</strong> Neurological Surgeons and theCongress <strong>of</strong> Neurological Surgeons. His researchinterests focus on pain and the spine.Bruce E. Stewart, MD,has been appointedassistant pr<strong>of</strong>essor inthe Division <strong>of</strong> Otolaryngology– Head andNeck <strong>Surgery</strong>. Withmore than 20 years <strong>of</strong>experience, Dr. Stewart<strong>of</strong>fers a full range <strong>of</strong>medical and surgical services for head andneck disorders and diseases to patients <strong>of</strong> allages, from newborn infants to seniors. His servicesinclude comprehensive care <strong>of</strong> patientswith sinonasal disorders, hearing loss andchronic ear disease, obstructive sleep apnea,and masses <strong>of</strong> the thyroid, head, and neck.A descendant <strong>of</strong> an Arizona pioneer family,Dr. Stewart was born and raised in Tucson. Hereceived both his bachelor’s degree in electricalengineering and his medical degree fromthe UA, where he also received the LangeAward for Academic Excellence. He completedresidency training in otolaryngology at the<strong>University</strong> <strong>of</strong> Utah in Salt Lake City.He previously was in private practice inTucson, serving patients at Davis-Monthan AirForce Base.Dr. Stewart serves on the board <strong>of</strong> directors<strong>of</strong> the Adult Loss <strong>of</strong> Hearing Association(ALOHA), a nonpr<strong>of</strong>it support and advocacyorganization that provides hearing loss servicesfor hard-<strong>of</strong>-hearing or deaf adults. He isthe immediate past president <strong>of</strong> ALOHA andleads “Let’s Loop Tucson,” an ongoing projectto promote “looping,” a technology to helphearing aid users in public places.Sreekumar ”Kumar”Subramanian, MD, assistantpr<strong>of</strong>essor, hasjoined the Division <strong>of</strong>Cardiothoracic <strong>Surgery</strong>.Dr. Subramanian’spractice includes a broadspectrum within adultcardiac surgery, rangingfrom on-pump and beating heart coronaryartery bypass surgery to minimally invasiveheart-valve operations, surgical treatment <strong>of</strong>atrial fibrillation, and minimally invasive procedureson the aorta. While he <strong>of</strong>fers patientsmultiple minimally invasive surgical options,Dr. Subramanian also developed special expertisein reoperative and high-risk reoperativecardiovascular surgery at the ClevelandClinic Foundation.Dr. Subramanian completed a seven-yearcombined program leading to a bachelor <strong>of</strong>science degree and medical degree at UnionCollege and Albany Medical College in NewYork. He joined the U.S. Air Force and completeda six-year general surgery residencyat David Grant Medical Center in California.Subsequently stationed at Spangdahlem AirBase in Germany, he deployed to Liberia andKazakhstan, and served as a combat traumasurgeon in Balad, Iraq. He then completed hiscardiothoracic surgical training at the ClevelandClinic.Dr. Subramanian received an ArizonaHeart Institute traveling fellowship and spenttwo years working as a cardiac surgeon at theHeart Center Leipzig while doing a fellowshipin percutaneous and minimally invasive heartvalve surgery and innovations.His clinical and research interests also includeaortic valve-preserving operations andaortic surgery, including the use <strong>of</strong> hybridoperations for the descending thoracic aorta.He has authored and coauthored about 60publications, which include articles, abstracts,and book chapters.Jess L. Thompson III,MD, MSc, a cardiothoracicsurgeon specializingin the repair <strong>of</strong>congenital heart defectsin children, has joinedthe Division <strong>of</strong> Cardiothoracic<strong>Surgery</strong>as assistant pr<strong>of</strong>essor. Afourth-generation Arizona native, Dr. Thompsoncomes to the UA from Texas Children’sHospital in Houston, where he completed afellowship in congenital heart surgery. Hisclinical expertise includes repair <strong>of</strong> complexneonatal congenital heart disease and treatment<strong>of</strong> adults with congenital heart disease.Dr. Thompson attended medical school atthe <strong>University</strong> <strong>of</strong> Southern California, Los Angeles,Keck School <strong>of</strong> Medicine. He completedhis general surgery residency training andcardiothoracic training at the Mayo Clinic inRochester, MN.While at the Mayo Clinic, Dr. Thompsonparticipated in a National Institutes <strong>of</strong> HealthClinical Investigator Program, receiving amaster’s degree in biomedical sciences:clinical research. His studies centered oncomplex heart-valve disease with a specificNEWS BRIEFTrauma CenterRe-verified as Level IThe Trauma Center at The <strong>University</strong><strong>of</strong> Arizona Medical Center has beenre-verified by the American College<strong>of</strong> Surgeons as a Level I TraumaCenter. The ACS survey team visitedthe Trauma Center in November.A Level I trauma certification isthe highest national designationa hospital can receive. The TraumaCenter at The <strong>University</strong> <strong>of</strong> ArizonaMedical Center is one <strong>of</strong> eightLevel I Trauma Centers in the state,and the only one serving all <strong>of</strong>Southern Arizona.21
22emphasis on novel anticoagulants andanticoagulation strategies, as well as minimallyinvasive heart-valve repair and replacementtechniques. Dr. Thompson has published hisresearch in scientific journals and presentedat both national and international meetings.In his role at the UA, Dr. Thompson willwork closely with Michael Teodori, MD, pr<strong>of</strong>essor<strong>of</strong> surgery and director <strong>of</strong> Congenitaland Pediatric Cardiac <strong>Surgery</strong>, a renownedspecialist in surgical treatment <strong>of</strong> newbornsand children with highly complex heartproblems.Magdiel Trinidad-Hernandez, MD, hasjoined the Division <strong>of</strong>Vascular <strong>Surgery</strong> asassistant pr<strong>of</strong>essor. Hespecializes in minimallyinvasive, endovasculartreatments for the management<strong>of</strong> aortic aneurysmsand complex aortic reconstructions.Dr. Trinidad-Hernandez has trained in thelatest techniques <strong>of</strong> aortic stent grafting forendovascular repair <strong>of</strong> abdominal aortic aneurysms,other aortic abnormalities, and vascularconditions. He is an expert in advancedendovascular procedures, such as graftfenestration, hybrid operations, snorkel techniquesfor the treatment <strong>of</strong> complex aorticaneurysms, and bifurcated graft replacementfor the treatment <strong>of</strong> iliac artery aneurysms topreserve blood flow to the pelvis. In addition,Dr. Trinidad-Hernandez specializes in lowerextremitybypass and endovascular interventionsfor limb salvage as well as carotidsurgery and stenting.A native <strong>of</strong> Guadalajara, Mexico, Dr.Trinidad-Hernandez comes to the UA fromthe Mayo Clinic in Rochester, MN, where hecompleted a fellowship in vascular and endovascularsurgery. He completed his generalsurgery residency at the Metropolitan GroupHospitals <strong>of</strong> the <strong>University</strong> <strong>of</strong> Illinois at Chicago,where he also spent one year dedicatedto clinical research in the noninvasive vascularlaboratory.Dr. Trinidad-Hernandez’s research interestsinclude advanced endovascular techniquesfor complex aortic aneurysms and the surgicaltreatment <strong>of</strong> lymphedema. He has presentedpapers at national and internationalmeetings and has a number <strong>of</strong> publicationsincluding abstracts, book chapters, and originalcontributions.Tolga Turker, MD, assistantpr<strong>of</strong>essor in theDivision <strong>of</strong> Reconstructiveand Plastic<strong>Surgery</strong>, is speciallytrained to perform advancedfree or pedicledflap transfer (movingtissue from one site onthe body to another), bone and s<strong>of</strong>t tissuereconstruction, and composite tissue allotransplants(transplanting tissue or limbs fromdeceased donors).In addition, Dr. Turker treats all types <strong>of</strong>hand problems, including nerve compressionand degenerative diseases, and performs upper-extremityrepair and free-tissue transferfor trauma injuries and skin defects, vascularized-bonetransfer for fractures and deformities,and toe-to-hand transfer for thumb andfinger reconstruction.Dr. Turker earned his medical degree atIstanbul <strong>University</strong> in Turkey. After completingan orthopedic and trauma residency at CerrahpasaFaculty <strong>of</strong> Medicine <strong>Department</strong> <strong>of</strong>Orthopedic and Traumatology, Istanbul,he served in the Turkish Army as an orthopedicsurgeon and practiced at the largest armyhospital in Turkey. During his time in the army,he performed numerous trauma, hand, andmicrosurgery cases.Dr. Turker completed a three-year handand microsurgery fellowship at the ChristineM. Kleinert Institute for Hand and Microsurgeryin Louisville, KY. While at the KleinertInstitute, he was part <strong>of</strong> the surgical team fortwo hand transplant operations performedunder the direction <strong>of</strong> Dr. Warren Breidenbach,now chief <strong>of</strong> the Division <strong>of</strong> Reconstructive<strong>Surgery</strong> at the UA.Dr. Turker’s publications focus on studies<strong>of</strong> tissue and oxygen-relation models, nerveregeneration, and microsurgery education.Rebecca KleinViscusi, MD, has joinedthe breast cancer teamas assistant pr<strong>of</strong>essor inthe Division <strong>of</strong> SurgicalOncology. Dr. Viscusispecializes in surgicaltechniques that can helppatients facing a mastectomy(surgical removal <strong>of</strong> one or both breasts)have more natural-appearing reconstructedbreasts.An Arizona native, Dr. Viscusi receivedher bachelor’s degree from the UA and hermedical degree from Jefferson Medical Collegein Philadelphia. She returned to the UAto complete her general surgery residencytraining. Dr. Viscusi also completed a one-yearfellowship program in breast surgical oncologyat the <strong>University</strong> <strong>of</strong> Texas Southwesternin Dallas.Dr. Viscusi’s practice includes treatment<strong>of</strong> both benign and malignant breast-careissues. Her clinical and research interestsinvolve the care <strong>of</strong> women at high risk fordeveloping breast cancer, specifically thosewith a BRCA mutation. She participates inthe High-Risk Cancer Clinic at the UA CancerCenter.Jiyao Zou, MD, assistantpr<strong>of</strong>essor in the Division<strong>of</strong> Reconstructive andPlastic <strong>Surgery</strong>, <strong>of</strong>fersspecialized expertise inthe transplantation andreplantation <strong>of</strong> severeddigits or extremities andin microsurgical reconstruction<strong>of</strong> damaged areas <strong>of</strong> the body frominjuries or cancer.He received his medical degree fromShandong Medical <strong>University</strong> in China. Hecompleted orthopedic surgery residencytraining at one <strong>of</strong> the largest orthopedic traumaand microsurgery centers in Shandong.He performed all types <strong>of</strong> microsurgery cases,including replantation as well as free-flap andvascularized tissue transfers.Dr. Zou recently finished an orthopedictrauma fellowship at the <strong>University</strong> <strong>of</strong> Louisvilleand a hand and microsurgery fellowshipat the Christine M. Kleinert Institute for Handand Microsurgery in Louisville. He participatedin two cases <strong>of</strong> hand transplantation inLouisville, including a bilateral (double) handtransplant.Dr. Zou’s research focus is on the anatomyand clinical studies <strong>of</strong> different kinds <strong>of</strong> tissueflaps, with an emphasis on local transfer andon decreasing donor morbidities.
Philanthropy NewsFund Honors‘Father <strong>of</strong> American Lithotripsy’Endowed fund to honor UA Urology Division founder George W. Drach, MDIn 40 years as a urologist, George W. steps by becoming a minister. It was aDrach, MD, has advanced the specialtyon an international level through ognized his talent with the scalpel andzoology pr<strong>of</strong>essor at the UA who rec-his medical contributions. Dr. Drach, suggested he become a surgeon.who founded the Division <strong>of</strong> Urology at He received his medical degreethe UA <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong>, is worldrenownedfor the development <strong>of</strong> tools to in 1961, and did surgical training atfrom (Case) Western Reserve <strong>University</strong>combat kidney stones and for improved <strong>University</strong> Hospitals in Cleveland. Heurologic care for aging patients.was drawn to the field <strong>of</strong> urology afterTo honor this “boy from Arizona,” serving as chief medical <strong>of</strong>ficer in thethe UA established the George W. Navy on the USS Valley Forge during theDrach, MD, Endowed Chair for Urology,with the goal <strong>of</strong> raising $2 million. ogy residency and fellowship at WakeVietnam War. He later completed a urol-About $300,000 has been raised, much Forest <strong>University</strong>.from fraternity brothers, former residents,and patients <strong>of</strong> Dr. Drach. at the <strong>University</strong> <strong>of</strong> New Mexico, Dr.While receiving additional trainingInterest from the endowment would Drach yearned to return to Arizona. Hebenefit the division in perpetuity, supportingresearch, attracting top faculty, Here, he and his wife, Paula Drach, builtjoined the faculty at the UA in 1970.building pediatric urology, and more. the division together, providing a sense“The future is outstanding for urologybased on our aging population, and training.<strong>of</strong> family for students and residents inresearch has got to be supported so we Dr. Drach developed an interest incontinue to produce important bits <strong>of</strong> kidney stones early in his career, and becameknown as the “Father <strong>of</strong> Americanknowledge,’’ Dr. Drach said.A former UA student body president,Dr. Drach, with his affable smile lutionary device used to pulverize kidneyLithotripsy” for his research on the revo-and signature bola tie, initially planned stones with sound waves, eliminating theon following in his grandfather’s foot-continued on page 24DonationsRecognizing gifts <strong>of</strong> $1,000 ormore in <strong>2011</strong>Advanced BioHealing Inc.Aesculap Inc.Jacqueline A. and Joe AgersAir Methods Corp.Monica A. AkyolAnonymous (2)Alice and Paul BakerDavid J. BerwickLaura and Arch BrownJohn J. CampoGinny L. Clements and Tom RogersJim Click Nissan, Inc.Shauna K. and Jerrold CohenTamara CrockettMaritza and Luis F. DabdoubDr. and Mrs. Sam DeFrancescoDonal J. DraynePeggy Duckett-DrachChristina ElgartLisa EricksonMegan A. Escobar and Doug PeeryEvents Made SpecialEvergreen MortuaryFidelity Charitable FundSusan and Randall Friese, MDMartha B. Gergan<strong>of</strong>fJoseph A. GervasioDeeAnne and Gregg GibbonsNina and Nick GibsonGolden Eagle DistributorsMr. and Mrs. Joseph GootterHealthSouthDoby HillenbrandHydrite Chemical CompanyPam and Rockwell Jackson, MDDr. Bellal JosephBeth and I. Michael KasserDr. and Mrs. Daniel KlemmedsonDr. Narong KulvantunyouAllen LangerDr. and Mrs. Michael LemoleElaine LitvackLong Realty Cares FoundationElizabeth A. MacBethDr. Lori MackstallerMC Management LLC23
24Donations cont.Harold M. McNairMedEfficiency, Inc.Esther and Carlos MichanAlbert P. MichelbachRalph B. MillerDennis R. MinanoOmar MirelesDonald and Donna MositesFamily FoundationJohn Munic Enterprises Inc.Joan and John MurphyJudy and Ric MyersLaurie B. NelsonMr. and Mrs. Allan J. NorvilleNovadaq Corp.Dr. Terence O’KeeffeDr. and Mrs. Theron OvittBrian G. PrackoRaytheon Missile SystemsDr. and Mrs. Peter RheeNancy and James A. RodolphRosemont CopperRoyal Autmotive GroupSanta Cruz UrologyNeelam and Gulshan Sethi, MDHarriet A. SilvermanJudy and Vince SmedesSouthern Arizona RoadrunnersSouthern Arizona Trauma Network(SATNET)Robert and Sonia SteinbergDr. and Mrs. Andrew L. TangDrs. Janet and Michael TeodoriLouise and Al ThomasLucy ThomasTu NiditoDr. and Mrs. Evan C. UngerMarlene and Howard VolinCount and Countess FerdinandVon GalenDr. and Mrs. Ron WeinsteinAngela D. WeirWells Fargo FoundationJana and Frank WesterbekeDr. Wendell Whitacre andDr. Teresa CislerW.L. Gore & AssociatesWright Medical Technology Inc.Dr. Julie WynneAmy Zuckerman and Morey BrownZuckerman Family FoundationElizabeth J. ZukoskiLithotripsycontinued from page 23need for surgical incisions. It was one <strong>of</strong>the first minimally invasive technologiesand is used throughout the world today.His interest shifted in 1995 tourologic care for aging patients. Followingthe death <strong>of</strong> his wife and childhoodsweetheart, Dr. Drach served as visitingpr<strong>of</strong>essor <strong>of</strong> urology at the <strong>University</strong> <strong>of</strong>Texas Southwestern Medical School inDallas and directed the urology clinic atParkland Memorial Hospital in 1996-98. In 1998 he joined the <strong>University</strong> <strong>of</strong>Pennsylvania and now serves as pr<strong>of</strong>essoremeritus <strong>of</strong> urology. He and hiswife second, Margaret Duckett-Drach,Inspired to Make a DifferenceDr. Jack and Rosemary Dunn create endowment in honor <strong>of</strong> Dr. Philip Carter.Inspired by the commitment <strong>of</strong> the UA<strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> Division <strong>of</strong>Neurosurgery to research, teaching, andcompassionate patient care, neurosurgeonJack H. Dunn, MD, and his wife,Rosemary Dunn, have established theDunn Family Fund, with family andfriends supporting the effort.The endowment honors the lateDr. L. Philip Carter, a longtime UAneurosurgery faculty member and formerdivision chief who died in 20<strong>10</strong>. Itrecognizes the significant contributionsDr. Carter made in training neurosurgeonsand in the lives <strong>of</strong> his patients,Dr. Dunn said.“Dr. Carter’s personal and pr<strong>of</strong>essionallife was about making a difference.The fund will continue his legacyand make a difference to future neurosurgeonsand to neurosurgery patientsand their families,” explained Dr. Dunn.Dr. Dunn, who joined the UA in2008 with a specialty in spinal injuriesand diseases, said he and his wife havesupported institutions that impactedtheir lives, including Yale, New York<strong>University</strong>, and Wayne State <strong>University</strong>.Witnessing growth within the UADivision <strong>of</strong> Neurosurgery, under thedirection <strong>of</strong> division chief, G. MichaelLemole, Jr., MD, motivated the Dunnsto establish the endowment.“We wanted to build supportfrequently return to the UA, where hestill teaches.Dr. Drach has written more than 140journal articles and continues to inspirethe highest quality <strong>of</strong> urologic care. Herecently helped to develop surgical competenciesin the field <strong>of</strong> surgery, “somethingall surgical students and residentsshould know,’’ he said.“We are very proud <strong>of</strong> Dr. Drach,’’said Kari Schlachtenhaufen, director <strong>of</strong>development for the UA <strong>Department</strong> <strong>of</strong><strong>Surgery</strong>. “He set us on a good path. It iscritical to have endowments within the<strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> because that iswhere new surgery techniques are developed,and that research ultimately willgive patients with more complex conditionsgreater hope.’’for residents and faculty to take care<strong>of</strong> people in Arizona and around theworld,’’ Dr. Dunn said. “We train peopleto spread the knowledge they learn here.We feel this is a good place to support.’’Income from the endowment wasused most recently to support thetraining <strong>of</strong> neurosurgery residents. TheDunns will annually evaluate how fundscan best be used to support the department,through critically important research,travel to educational conferences,and other efforts.The Dunns are encouraging othersto start endowments to benefit neurosurgeryand other divisions at the UA inperpetuity.“Endowments are more valuablethan general donations,’’ Dr. Dunn said.“It’s important to put money into somethingthat makes a difference in Arizona.In neurosurgery, we are recruiting morepeople so we can provide superior neurosurgicalcare to Southern Arizona. Weare now able to do things that haven’tbeen done before in Arizona.“Our family will continue to supportthe efforts as much as we can,’’ Dr. Dunnadded.If you are interested in learning more aboutendowments at the <strong>University</strong> <strong>of</strong> Arizona,please contact Kari Schlachtenhaufen, JD,at 520-626-2222.
Raytheon MissileSystems Donates$<strong>10</strong>0,000 to UATrauma DivisionRaytheon Missile Systems has donated$<strong>10</strong>0,000 to the Division <strong>of</strong>Trauma, Critical Care, and Emergency<strong>Surgery</strong> in the UA <strong>Department</strong> <strong>of</strong><strong>Surgery</strong>. The gift will fund research onthe treatment <strong>of</strong> wounded soldiers onthe battlefield and trauma victims hereat home.Potential advancements that canbe implemented the quickest will getthe highest priority. Specific researchareas will include developing devicesto detect and treat chest injuries, newhuman-based resuscitation fluids, andnew treatments to stop bleeding. Studiesalso will focus on traumatic brain injury,tissue transplantation, and suspendedanimation.“Advancement for warfighters alsowill have an immediate impact at home,as it will be just as applicable for civiliantrauma,” said Peter Rhee, MD, chief, UADivision <strong>of</strong> Trauma, Critical Care, andEmergency <strong>Surgery</strong>. “We are excited topartner with one <strong>of</strong> Tucson’s largest employersthrough their support in traumaresearch. Research is a systematic way <strong>of</strong>improving human life now and forever.”“Raytheon is proud to provide theUA trauma division with this donationto help further the world-class workthat is already under way there,” saidTaylor W. Lawrence, PhD, RaytheonMissile Systems president. “Because ourtwo organizations have a focus on thewarfighter, we see tremendous synergybetween Raytheon and the UA Traumateam in this area.”Ranked in the top five percentnationally, the Level I Trauma Center atThe <strong>University</strong> <strong>of</strong> Arizona Medical Centeris the busiest in Arizona.Raytheon, with 20<strong>10</strong> sales <strong>of</strong> $25billion, is a technology and innovationleader specializing in defense, homelandsecurity, and other government marketsthroughout the world.Fundraising EventsM*A*S*H BashFollowing the tragic shootings onJan. 8, <strong>2011</strong>, a group <strong>of</strong> Tucsonsupporters, recognizing the critical role aLevel I Trauma Center serves in the community,created the Friends <strong>of</strong> the <strong>University</strong><strong>of</strong> Arizona Trauma Center. On Oct. 22, atthe Pima Air and Space Museum, the Friendshosted the first annual M*A*S*H Bash, afundraising event for the Level I traumacenter.The museum was transformed into a camouflaged mobile army surgicalhospital mimicking the M*A*S*H hit television series. Highlights includedspecial celebrity guests from the M*A*S*H television series Mike Farrell(B.J. Hunnicutt) and William Christopher (Father Mulcahy). Live entertainmentwas provided by a USO-style group, along with a Cab Calloway impersonatorand a “Rosie’s Bar,” serving specialty drinks in mini-canteens while the bandplayed music from WWII to the present. Guests were encouraged to dress inM*A*S*H-era or Asian-style clothing.More than 460 people attended the event. Proceeds will be used to supportan Endowed Chair in the Division <strong>of</strong> Trauma, Critical Care, and Emergency <strong>Surgery</strong>,and to purchase equipmentto support trauma research at the<strong>University</strong> <strong>of</strong> Arizona.Since 2003, The <strong>University</strong><strong>of</strong> Arizona Medical Center – <strong>University</strong>Campus has been the onlyLevel I Trauma Center servingSouthern Arizona. The cost toprovide this critical communityservice is estimated at more thanDrs. Peter Rhee, Rainer W.G. Gruessner, and RichardCarmonaM*A*S*H Bash celebrity guestsMike Farrell and William Christopher$47 million a year.The long-term vision is tobuild a freestanding traumacenter near the hospital that houses additional operating suites, a traumaintensive care unit, neurologic rehabilitation services, a burn unit, and researchlaboratories.The next M*A*S*H Bash will be held Friday, Oct. 19, <strong>2012</strong>.Sponsorship opportunities are available. For more information, contactKari Schlachtenhaufen, 520-626-2222 or karis@surgery.arizona.edu.Giving OnlineDonations can be made to each division and program in the UA <strong>Department</strong><strong>of</strong> <strong>Surgery</strong> through the <strong>University</strong> <strong>of</strong> Arizona Foundation website(www.uafoundation.org) or through the <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> website(www.arizona.surgery.edu).If you would like more information on giving opportunities or need assistance, contactKari Schlachtenhaufen, 520-626-2222 or karis@surgery.arizona.edu.25
26Awards & RecognitionUA Surgeons Among ‘Best Doctors in America’More than <strong>10</strong>0 Tucson physicians affiliated with the Arizona Health Sciences Center areincluded in the latest Best Doctors in America database, including many from the UA<strong>Department</strong> <strong>of</strong> <strong>Surgery</strong>: Alexander G. Chiu, Allan J. Hamilton, Michael F. Teodori,Khalid M. Khan, Hugo Villar, Jack H. Dunn, Mitchell H. Sokol<strong>of</strong>f, and Joseph L. Mills.Rainer W.G. Gruessner, MD, Michael Lemole,MD, and Peter Rhee, MD, were named <strong>2011</strong>Pima Medical Society Physicians <strong>of</strong> the Year. (Seephoto.)David G. Armstrong, DPM, MD, PhD, won FirstPlace, Clinical Research Award, at the Symposiumfor the Advancement <strong>of</strong> Wound Care/WoundHealing Society: Armstrong DG, Marston WA,Reyzelman AM, Kirsner RS, “Comparative Effectiveness<strong>of</strong> Mechanically and Electrically PoweredNPWT Devices: A Multicenter RandomizedControlled Trial,” Washington, DC, October <strong>2011</strong>.He also was placed on the Podiatry Management VIP List <strong>of</strong> Most Influential PodiatricPhysicians, <strong>2011</strong> (selected every 5 years). Dr. Armstrong was appointed chairman <strong>of</strong> theDiabetic Foot Commission <strong>of</strong> the International Podiatry Federation (FIP).Warren C. Breidenbach III, MD, was selected as one <strong>of</strong> America’s Top Doctors byCastle Connolly, <strong>2011</strong>.Stephen A. Goldstein, MD, was honored as the recipient <strong>of</strong> the William K. WrightAward at the annual <strong>2011</strong> American Academy <strong>of</strong> Facial Plastic and Reconstructive <strong>Surgery</strong>conference.D.J. Green, MD, has been named president <strong>of</strong> the Tucson Surgical Society, a 70-member,not-for-pr<strong>of</strong>it pr<strong>of</strong>essional organization <strong>of</strong> physician surgeons.Allan J. Hamilton, MD, received the National Award for Excellence in Fire Service-Based EMS – Career Category, presented by the Medic-Alert Foundation and the CongressionalFire Services Institute, April <strong>2011</strong>.Abraham Jacob, MD, has been awarded the <strong>2011</strong> Politzer Society Award for best basicscience paper: “AR42: A Novel Histone Deacetylase Inhibitor with High Clinical-TranslationalPotential as Treatment for NF2-Associated Tumors,” presented at the <strong>2011</strong> meetingin Athens, Greece. The Politzer Society represents a global consortium <strong>of</strong> leadingotologic/neurotologic surgeons. The society awards one basic science and one clinicalPolitzer Society Award every two years.Rifat Latifi, MD, received the Community Health Promotion Award from the URAC/Care Continuum Alliance International Health Promotion Awards (IHPA), Rome, Italy.He also received the 21st Century Achievement Award in Health by ComputerworldHonors Program, Washington, DC.Visit Us!Visit the UA <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> and learn about the latest advances in surgery,including our Class <strong>10</strong>,000 Clean Room, the Institute for Cellular Transplantation, thePediatric Liver Transplant Program, and the HepatoPancreaticoBiliary (HPB) Centerfor the treatment <strong>of</strong> pancreatic and liver diseases. Tours are regularly available forsmall groups.Contact:Kari Schlactenhaufen, 520-626-2222 or karis@surgery.arizona.edu, to schedule a tour.Michael Lemole, MD, received a CongressionalCitation by the Friends <strong>of</strong> theNational Library <strong>of</strong> Medicine at the AnnualAwards Gala in November at the GreatHall <strong>of</strong> the Library <strong>of</strong> Congress JeffersonBuilding. He also received the ArizonaBusiness Magazine 4th Annual Health CareLeadership Award; was named HonoraryCommander by the 355th Medical Group,Davis-Monthan Air Force Base, Tucson; andwas named Medscape Best Physician <strong>of</strong> theYear for <strong>2011</strong>.Joseph L. Mills, MD, received the 8thAnnual Edward James Olmos Award forAdvocacy in Amputation Prevention, March<strong>2011</strong>.Mike M. Nguyen, MD, MPH, won BestPoster for the kidney stone session at theAmerican Urological Association AnnualMeeting, Washington, DC: “Internet SearchMetrics Can Provide Real-Time Data onKidney Stone Disease in the United States.”He also won the Best Poster Award for the58th Annual Kimbrough Seminar in Seattle:“Factors Influencing Fluid Intake Behaviorin Kidney Stone Formers.”Klearchos K. Papas, PhD, has been appointedpresident-elect <strong>of</strong> the Cell TransplantationSociety (Councillor).Peter Rhee, MD, was invited to the State<strong>of</strong> the Union address as Michelle Obama’sguest in January <strong>2011</strong>. He also was invitedto the White House to attend a state dinnerin honor <strong>of</strong> South Korean President LeeMyung-Bak. He was named Grand Marshalfor the Tucson St. Patrick’s Day Parade andMedscape Best Physician <strong>of</strong> the Year for<strong>2011</strong>. He received the Arizona BusinessMagazine 4th Annual Health Care LeadershipAward; the Institute for Corean-AmericanStudies (ICAS) Liberty Award for <strong>2011</strong>;the Distinguished Leadership Award, LegalCommunity Against Violence; a Resolution<strong>of</strong> Proclamation by the Arizona IndianGaming Association; and a Proclamation bythe President <strong>of</strong> the United States: “Honoringthe Victims <strong>of</strong> the Tragedy in Tucson,Arizona.”Horacio Rilo, MD, was recognized for hiscutting-edge research at the Cure, Care &Commitment Awards Luncheon hostedby the American Diabetes Association inNovember <strong>2011</strong>.Michael F. Teodori, MD, received the <strong>2011</strong>Hon Kachina Volunteer Award for his commitmentto providing no-cost medical careand support for needy children sufferingfrom congenital heart defects.
PublicationsCopeland H, Jones M, Duran MA, Sozanski J,Poskus D, Beita O, Adamas-Rappaport WJ,“Teaching Medical Spanish on the <strong>Surgery</strong>Clerkship,” American Surgeon 77(12):1715-1717, Dec <strong>2011</strong>.Stidd D, Polonski L, Anton R, Lemole GM Jr,“Transcranial Orbitotomy for Excision <strong>of</strong> OrbitalTumors: A Case Series”; Joe S, Lemole GM Jr,“Nasoseptal Flap Harvest After Previous TransnasalTransseptal <strong>Surgery</strong>,” North AmericanSkull Base Society, 21st Annual Meeting,Scottsdale, Feb <strong>2011</strong>.Armstrong DG, editor, Up-To-Date ClinicalManagement, Wolters Kluwer Health, <strong>2011</strong>.Lavery LA, Armstrong DG, “Clinical Examinationand Risk Classification <strong>of</strong> the DiabeticFoot,” in Veves A, Giurini J, and LoGerfo F, eds,The Diabetic Foot, 3rd ed, Totowa, New Jersey,Humana Medical Press, <strong>2011</strong>.Rogers LC, Frykberg RG, Armstrong DG, BoultonAJM, Edmonds ME, Ha Van G, HartemannA, Game F, Jeffcoate W, Jirkovska A, Jude E,Morbach S, Morrison WB, Pinzur M, Pitocco D,Sanders L, Wukich D, Uccioli L, “The CharcotFoot in Diabetes,” J Amer Podiatr Med Assoc<strong>10</strong>1:437-446, <strong>2011</strong>.Armstrong DG, Cohen IK, Courric S, BhararaM, Marston W, “Diabetic Foot Ulcers and VascularInsufficiency: Our Population Has Changed,But Our Methods Have Not,” J Diabetes Sci Technol5:1591-1595, <strong>2011</strong>.Rogers LC, Frykberg RG, Armstrong DG, BoultonAJM, Edmonds ME, Ha Van G, HartemannA, Game F, Jeffcoate W, Jirkovska A, Jude E,Morbach S, Morrison WB, Pinzur M, Pitocco D,Sanders L, Wukich D, Uccioli L, “The CharcotFoot in Diabetes,” Diabetes Care 34:2123-2129,<strong>2011</strong>.Rogers LC, Frykberg RG, Armstrong DG, BoultonAJM, Edmonds ME, Ha Van G, HartemannA, Game F, Jeffcoate W, Jirkovska A, Jude E,Morbach S, Morrison WB, Pinzur M, Pitocco D,Sanders L, Wukich D, Uccioli L, “The CharcotFoot in Diabetes,” J Amer Podiatr Med Assn<strong>10</strong>1:437-446, <strong>2011</strong>.Wrobel JS, Chagares W, Crews RC, Stuck R,Weaver F, Rapacki L, Paulson, R, ArmstrongDG, “Creating a Diabetes Foot Reminder-BasedRegistry Using the Electronic Health Record,”Informatics in Primary Care 18:283-287, <strong>2011</strong>.Bhatnagar S, Bharara M, Armstrong DG, “Innovationsin Diabetic Foot Care: Prevention,Education and Treatment,” Treatment Strategies—Diabetes-CambridgeResearch Centre 3:1,62-65, <strong>2011</strong>.Fleischer AE, Wrobel JS, Leonards A, Berg S,Evans DP, Baron RL, Armstrong DG, “Post-Treatment Leukocytosis Predicts an UnfavorableClinical Response in Patients with Moderateto Severe Diabetic Foot Infections,” J FootAnkle Surg, May 26, <strong>2011</strong>, epub ahead <strong>of</strong> print.Armstrong DG, “An Overview <strong>of</strong> Foot Infectionsin Diabetes,” Diabetes Technology andTherapeutics, Jun 1, <strong>2011</strong>, epub ahead <strong>of</strong> print.Armstrong DG, Giovinco N, Mills JL, RogersLC, “Facetime for Physicians: Using Real TimeMobile Phone-Based Videoconferencing toAugment Diagnosis and Care in Telemedicine,”ePlasty 11:212-217, <strong>2011</strong>.Lepow BD, Downey M, Yurgelon J, Klassen L,Armstrong DG, “Bioengineered Tissues inWound Healing: A Progress Report,” Expert RevDermatology 6:255-262, <strong>2011</strong>.Frykberg RG, Driver VR, Lavery LA, ArmstrongDG, Isenberg RA, “The Use <strong>of</strong> PulsedRadio Frequency Energy Therapy in TreatingLower Extremity Wounds: Data from the ProvantWound Registry,” Ostomy Wound Management57:22-29, <strong>2011</strong>.Armstrong DG, Giovinco NC, “Diagnostics,Theragnostics, and the Personal Health Server:Fundamental Milestones in Technology withRevolutionary Changes in Diabetic Foot andWound Care to Come,” Foot Ankle Specialist4:54-60, <strong>2011</strong>.Gabbay R, Kaul S, Ulbrecht J, Scheffler NM,Armstrong DG, “Motivational Interviewing byPodiatric Physicians: A Method for ImprovingPatient Self-care <strong>of</strong> the Diabetic Foot,” J AmerPodiatr Med Assn <strong>10</strong>1:78-84, <strong>2011</strong>.Armstrong DG, Marston W, Reyzelman A,Kirsner R, “Comparison <strong>of</strong> Negative PressureWound Therapy with an Ultraportable Non-Electrically Powered Device vs. TraditionalElectrically Powered Device for the Treatment<strong>of</strong> Chronic Lower Extremity Ulcers: A MulticenterRandomized Controlled Trial,” WoundRepair Regen 19:173-180, <strong>2011</strong>.Armstrong DG, Fisher TK, Lepow BD, WhiteM, Mills JL, “The Diabetic Foot,” in Mechanisms<strong>of</strong> Vascular Disease: A Reference for VascularSpecialists, Fitridge R, Thompson M, eds,Cambridge <strong>University</strong> Press, 2nd ed, <strong>2011</strong>.Armstrong DG, Mills JL, “Toward a Changein Syntax in Diabetic Foot Care: PreventionEquals Remission,” J Amer Podiatr Med Assn,<strong>2011</strong>.Bharara M, Armstrong DG, “Surrogate Markersfor Inflammation in the Diabetic Foot,”Treatment Strategies Diabetes, <strong>2011</strong>.Kaufman CL, Breidenbach W, “World ExperienceAfter More Than a Decade <strong>of</strong> ClinicalHand Transplantation: Update from theLouisville Hand Transplant Program,” HandClinics 27 (4):417-21, vii-viii, Nov <strong>2011</strong>.Foroohar A, Elliott RM, Kim TW, BreidenbachW, Shaked A, Levin LS, “The History and Evolution<strong>of</strong> Hand Transplantation,” Hand Clinics27(4):405-9, vii, Nov <strong>2011</strong>.Clarkson JH, Ozyurekoglu T, Mujadzic M, IyerV, Breidenbach WC, “An Evaluation <strong>of</strong> theInformation Gained from the Use <strong>of</strong> IntraoperativeNerve Recording in the Management <strong>of</strong>Suspected Brachial Plexus Root Avulsion,” Plasticand Reconstructive <strong>Surgery</strong> 127(3):1237-43,Mar <strong>2011</strong>. Chiu A, Co-Editor,Sinonasal Tumors,Jaypee BrothersMedical Publishers:www.jaypeebrothers.com.Ransom E, Lee J,Chiu AG, “EndoscopicTranscranialand Intracranial Resection:Case Seriesand Design <strong>of</strong> a PerioperativeManagement Protocol,” Skull Base21(1), Jan <strong>2011</strong>.Becker SS, Chiu AG, “Prevention and Management<strong>of</strong> Complications in Sinus and Skull Base<strong>Surgery</strong>,” Otolaryngol Clin North Am 43(4),Aug 20<strong>10</strong>.Montone KT, Livolsi VA, Lanza DC, KennedyDW, Palmer J, Chiu AG, Feldman MD, LoevnerLA, Nachamkin I, “In Situ Hybridizationfor Specific Fungal Organisms in Acute InvasiveFungal Rhinosinusitis,” Am J Clin Pathol135(2), Feb <strong>2011</strong>.Ramakrishnan VR, Suh JD, Chiu AG, PalmerJN, “Addition <strong>of</strong> a Minimally Invasive MedialOrbital Approach in the Endoscopic Management<strong>of</strong> Advanced Sino-orbital Disease:Cadaver Study with Clinical Correlations,”Laryngoscope, <strong>2011</strong>.Goldstein-Daruech N, Cope EK, Vukovic K,K<strong>of</strong>onow J, Doghramji L, Gonzalez B, ChiuAG, et al, “Tobacco Smoke Mediated Induction<strong>of</strong> Sinonasal Microbial Bi<strong>of</strong>ilms,” PLoS ONE6(1), Jan <strong>2011</strong>.Zhang Z, K<strong>of</strong>onow JM, Finkelman BS, DoghramjiL, Chiu AG et al, “Clinical Factors Associatedwith Bacterial Bi<strong>of</strong>ilm Formation inChronic Rhinosinusitis,” Otolaryngol Head NeckSurg 144(3), Mar <strong>2011</strong>.Depoortere D, K<strong>of</strong>onow JM, Chen B, Chiu AG,Cohen NA, “Murine Ciliotoxicity and RabbitSinus Mucosal Healing by Polyhydrated Ionogen,”Otolaryngol Head Neck Surg, Mar <strong>2011</strong>.27
28Ransom E, Palmer JN, Kennedy DW, Chiu AG,“Assessing Risk/Benefit <strong>of</strong> Lumbar Drain Usefor Endoscopic Skull-Base <strong>Surgery</strong>,” Int ForumAll Rhinol 1(3), May/Jun <strong>2011</strong>.Lee JM, Ransom E, Lee JY, Palmer JN, ChiuAG, “Endoscopic Anterior Skull Base <strong>Surgery</strong>:Intraoperative Considerations <strong>of</strong> the Crista Galli,”Skull Base 21(2), Mar <strong>2011</strong>.Ramakrishnan VR, Suh JD, Chiu AG, PalmerJN, “Septal Disclocation for Endoscopic Access<strong>of</strong> the Anterolateral Maxillary Sinus and InfratemporalFossa,” Am J Rhinol Allergy 25(2), Mar<strong>2011</strong>.Chiu AG, Chen B, Palmer JN, et al, “SafetyEvaluation <strong>of</strong> Sinus Surfactant Solution on RespiratoryCilia Function,” Int Forum All Rhinol1(4), Jul/Aug <strong>2011</strong>.Smith TL, Kern RC, Palmer JN, Schlosser RJ,Chandra RK, Chiu AG, et al, “Medical Therapyvs. <strong>Surgery</strong> for Chronic Rhinosinusitis: A ProspectiveMulti-institutional Study,” Int ForumAll Rhinol 1(4), Jul/Aug <strong>2011</strong>.Adappa ND, Lee JY, Chiu AG, et al, “OlfactoryGroove Meningioma,” Otolaryngol Clin NorthAm 44(4), Aug <strong>2011</strong>.Montone KT, Livolsi VA, Landa DC, FeldmanMD, Kennedy DW, Palmer J, Chiu AG, et al,“Rapid In-situ Hybridization for DematiaceousFungi Using a Broad-Spectrum OligonucleotideDNA Probe,” Diagn Mol Pathol 20(3), Sep <strong>2011</strong>.Suh JD, Ramakrihnan VR, Zhang PJ, Wu AW,Wang MB, Palmer JN and Chiu AG, “Diagnosisand Endoscopic Management <strong>of</strong> SinonasalSchwannomas,” ORL 73 (6): 308-312, Oct<strong>2011</strong>.Ramakrishnan V R, Suh JD, Chiu AG, PalmerJN, “Reliability <strong>of</strong> Preoperative Assessment <strong>of</strong>Cerebrospinal Fluid Pressure in the Management<strong>of</strong> Spontaneous Cerebrospinal FluidLeaks and Encephaloceles,” International Forum<strong>of</strong> Allergy & Rhinology 1: 201-205, <strong>2011</strong>.Cope EK, Goldstein-Daruech N, K<strong>of</strong>onow JM,Christensen L, McDermott B, Monroy F, PalmerJN, Chiu AG, Shirtliff ME, Cohen NA, Leid JG,“Regulation <strong>of</strong> Virulence Gene Expression Resultingfrom Streptococcus Pneumonia andNontypeable Haemophilus Influenza Interactionsin Chronic Disease,” PLoS One 6(12):e28523, <strong>2011</strong>.Aouad RK, Chiu AG, “State <strong>of</strong> the Art Treatment<strong>of</strong> Nasal Polyps,” Am J Rhinol Allergy25(5): 291-298, Sep-Oct <strong>2011</strong>.Suh JD, Ramakrishnan V, Chiu AG, “The Role<strong>of</strong> Topical Therapies in the Treatment <strong>of</strong> ChronicRhinosinusitis,” Braz J Otorhinolaryngol77(6): 680-681, Dec <strong>2011</strong>.Suh JD, Ramakrishnan VR, Tarjudeen B, RegerC, Kennedy DW, Chiu AG, “Identification andTreatment <strong>of</strong> Nontuberculosis MycobacteriumSinusitis,” Am J Rhinol Allergy 25(6): 421-424,Nov-Dec <strong>2011</strong>.K<strong>of</strong>onow JM, Bhuskute A, Doghramji L, PalmerJN, Cohen NA, Chiu AG, “One-way Valve BottleContamination Rates in the Immediate PostfunctionalEndoscopic Sinus <strong>Surgery</strong> Period,”Am J Rhinol Allergy 25(6): 393-396, Nov-Dec<strong>2011</strong>.Suh J, Chiu AG, “Acute and Chronic Rhinosinusitis,”Otolaryngology, Lalwani A (eds).Lange,<strong>2011</strong>.Desai CS, Gruessner AC, Khan KM, FishbeinTM, Jie T, Rodriguez Rilo HL, GruessnerRW, “Isolated Intestinal Transplants vs. Liver-Intestinal Transplants in Adult Patients in theUnited States: 22 yr <strong>of</strong> OPTN Data,” ClinicalTransplantation, Dec <strong>2011</strong>, epub ahead <strong>of</strong> print.Desai CS, Stephenson D, Khan KM, Jie T,Gruessner AC, Rilo H, Gruessner RW, “NovelTechnique <strong>of</strong> Total Pancreatectomy before AutologousIslet Transplants in Chronic PancreatitisPatients,” Journal <strong>of</strong> American College <strong>of</strong> Surgeons213(6):e29-34, <strong>2011</strong>.Desai CS, Gruessner AC, Khan KM, Jie T, CartonM, Gruessner RW, “Isolated IntestinalTransplant vs. Multivisceral Transplants amongPediatric Patients in United States,” PediatricTransplantation 15, Supp 1: <strong>10</strong>0, Aug <strong>2011</strong>.Desai CS, Gruessner AC, Gruessner RW, JieT, Rilo H, Khan KM, “Liver Transplants forChildren with Cystic Fibrosis,” Pediatric Transplantation15, Supp 1: 95, Aug <strong>2011</strong>.Desai CS, Maybury R, Cummings LS, JohnsonLB, Fishbein TM, Neville R, Melancon J, “Autotransplantation<strong>of</strong> Solitary Kidney with RenalArtery Aneurysm Treated with LaparoscopicNephrectomy and ex vivo Repair: A Case Report,”Transplant Proc 43(7):2789-91, Sep<strong>2011</strong>.Cummings LS, Hawksworth JS, Guerra JF, DesaiCS, Girlanda R, Matsumoto CS, FishbeinTM, Johnson LB, Melancon JK, “SuccessfulABO-Incompatible Kidney Transplant After anIsolated Intestinal Transplant,” Transplantation91(<strong>10</strong>): e73-4, May <strong>2011</strong>.Melancon JK, Cummings LS, Graham J, Rosen-Bronson S, Light J, Desai CS, Girlanda R, GhasemianS, Africa J, Johnson LB, “Paired KidneyDonor Exchanges and Antibody ReductionTherapy: Novel Methods to Ameliorate DisparateAccess to Living Donor Kidney Transplantationin Ethnic Minorities,” J Am Coll Surg212(4):740-5, Apr <strong>2011</strong>.Desai CS, Gruessner R, Gruessner A, Jie T,Rilo HL, Carton MM, Khan KM, “Liver Transplantsfor Cystic Fibrosis-Related Cirrhosis:Analysis <strong>of</strong> 22 Years <strong>of</strong> the UNOS Database,”American Journal <strong>of</strong> Transplantation 11, Supp S2:198, Apr <strong>2011</strong>.Desai CS, Gruessner AC, Khan KM, Jie T,Gruessner WG, “Comparison <strong>of</strong> IntestinalTransplant (Tx) Alone (ITA) vs. Liver-Intestinaland Multiorgan Transplant (MVTx) Outcomes:An OPTN/SRTR Database Analysis,” AmericanJournal <strong>of</strong> Transplantation 11, Supp 2: 87,Jan <strong>2011</strong>.Cummings LS, Melancon JK, Guerra JF, HawksworthJ, Desai CS, Johnson LB, Girlanda R,Fishbein TM, Light J, Africa J, Ghasemain R,Orquiza M, “Utilization <strong>of</strong> a Paired Kidney Exchange,ABO-Compatible and DesensitizationProgram Has Reduced Waiting Time for Boththe Individual Recipients and the Entire CadavericWaiting List in Washington DC,” AmericanJournal <strong>of</strong> Transplantation 11, Supp 2: 69,Jan <strong>2011</strong>.Guerra JF, Cummings LS, Hawksworth JS, DesaiCS, Flanagan E, Girlanda R, Johnson LB,Melancon JK, “Use <strong>of</strong> a Desensitization Protocolin Highly Sensitized Yet ImmunocompromisedPatients Awaiting Kidney Transplantation,”American Journal <strong>of</strong> Transplantation 11, Supp 2:72, Jan <strong>2011</strong>.Desai CS, Khan KM, Gruessner AC, Jie T,Rilo H, Carton MM, Gruessner R, “IntestinalRetransplantation in Adults: Analysis <strong>of</strong> 22Years <strong>of</strong> the UNOS Database,” American Journal<strong>of</strong> Transplantation 11, Supp S2: 133, Apr <strong>2011</strong>.Cummings LS, Graham JA, Guerra J, HawksworthJS, Rosen-Bronson S, Girlanda R, DesaiCS, Johnson LB, Melancon JK, “Utilizing PairedKidney Exchange and Desensitization Programto Increase Living Donor Kidney Transplantationin African Americans,” American Journal <strong>of</strong>Transplantation 11, Supp S2: 484, Apr <strong>2011</strong>.Erman AB, Collar RM, Griffith KA, Lowe L,Sabel MS, Bichakjian CK, Wong SL, McLeanSA, Rees RS, Johnson TM, Bradford CR, “SentinelLymph Node Biopsy Is Accurate and Prognosticin Head and Neck Melanoma,” Cancer118(4):<strong>10</strong>40-7 DOI: <strong>10</strong>.<strong>10</strong>02/cncr.26288,epub Jul 19 <strong>2011</strong>.Erman AB, Griffith KG, Rees RS, Johnson TM,Bradford CR, “Sentinel Lymph Node,” Biopsyfor Head and Neck Cutaneous Melanoma, <strong>2011</strong>.Barmparas G, Inaba K, Georgiou C, HadjizachariaP, Chan L, Demetriades D, Friese R, RheeP, “Swan-Ganz Catheter Use in Trauma PatientsCan Be Reduced Without Negatively AffectingOutcomes,” World J <strong>Surgery</strong> 35(8):1809-17,<strong>2011</strong>.Galvani CA, Gallo, AS, Dylewski MR, “Robotic-AssistedHeller Myotomy for EsophagealAchalasia: Feasibility, Technique, and Short-Term Outcomes,” Journal <strong>of</strong> Robotic <strong>Surgery</strong>,<strong>2011</strong>, published online.Atunes M, Goldstein SA, “Surgical Approachto the Nasal Valves and the Midvault in Patientswith a Crooked Nose,” Facial Plastic <strong>Surgery</strong> 27(5): 422-436, Oct <strong>2011</strong>.
Bloom J, Bleier B, Goldstein SA, Carniol PJ,Palmer JN, Cohen NA, “Laser Facial NerveWelding in a Rabbit Model,” Arch Facial PlastSurg14:52-58, Dec <strong>2011</strong>.Atunes M, Goldstein SA, Chapter 4: “Anatomy<strong>of</strong> the Upper Face,” Manual <strong>of</strong> InjectableFillers, A Technical Guide to the <strong>Volume</strong>tricApproach to Whole Body Rejuvenation, <strong>2011</strong>.Goldstein SA, Ransom E, Chapter 6: “Anatomy<strong>of</strong> the Midface,” Illustrated Manual <strong>of</strong> InjectableFillers, A Technical Guide to the <strong>Volume</strong>tricApproach to Whole Body Rejuvenation , <strong>2011</strong>.Goldstein SA, Ransom E. Chapter 8: “Anatomy<strong>of</strong> the Lower Face,” Illustrated Manual <strong>of</strong>Injectable Fillers, A Technical Guide to the <strong>Volume</strong>tricApproach to Whole Body Rejuvenation,<strong>2011</strong>.Goldstein SA, Facial Plastic <strong>Surgery</strong>: TheCrooked Nose, ed, 27 (5), Oct <strong>2011</strong>.Talving P, Lustenberger T, Lam L, Inaba K,Mohseni S, Plurad D, Green DJ, DemetriadesD, “Coagulopathy After Isolated Severe TraumaticBrain Injury in Children,” J Trauma, <strong>2011</strong>Mar 21.Plurad D, Talving P, Tang A, Green D, Lam L,Inaba K, Demetriades D, “Alcohol Ingestion IsIndependently Associated With ComplicationsAfter Work Place Injuries: A National TraumaData Bank Analysis <strong>of</strong> Injury Severity And Outcomes,”J Trauma, Apr 15 <strong>2011</strong>.DuBose JJ, Putty B, Teixeira PG, Recinos G,Shiflett A, Inaba K, Green DJ, Plurad D, DemetriadesD, Belzberg H, “The RelationshipBetween Post-traumatic Ventilator-associatedPneumonia Outcomes and American College <strong>of</strong>Surgeons Trauma Center Designation,” Injury42(1):40-3, Jan <strong>2011</strong>.Inaba K, Branco BC, Reddy S, Park JJ, GreenD, Plurad D, Talving P, Lam L, Demetriades D,“Prospective Evaluation <strong>of</strong> Multidetector ComputedTomography for Extremity VascularTrauma,” J Trauma 70(4):808-15, Apr <strong>2011</strong>.Gruessner RW, Pugliese A, Reijonen HK,Gruessner S, Jie T, Desai C, Sutherland DER,Burke GW, “Development <strong>of</strong> Diabetes Mellitusin Living Pancreas Donors and Recipients,”Expert Rev Clin Immuno 7(4):543-51, Jul <strong>2011</strong>.Chisholm-Burns MA,Erickson SR, SpiveyCA, GruessnerRWG, Kaplan B,“Concurrent Validity<strong>of</strong> Three Health-RelatedQuality <strong>of</strong> LifeInstruments in RenalTransplant Recipients.Patient Preference andAdherence,” DoveMedical Press 5:517-522, <strong>2011</strong>.Gruessner, RWG, Pugliese A, Reijonen HK,Gruessner S, Jie T, Seaquist ER, SutherlandDA, Burke GW, “Development <strong>of</strong> Diabetes Mellitusin Living Pancreas Donors and Recipients,”Expert Rev <strong>of</strong> Clin Immunol7(4):543-51,Jul <strong>2011</strong>.Beebe D, Singh H, Luikart JJ, Gruessner R,Gruessner A, Belani K, “Anesthetic ComplicationsIncluding Two Cases <strong>of</strong> PostoperativeRespiratory Depression in Living Donor <strong>Surgery</strong>,”J Anaesthesiol Clinic Pharmacol 27(3):362-366, <strong>2011</strong>.Vriens MR, Weng J, Suh I, Huynh N, GuerreroMA, Shen WT, Duh QY, Clark OH, Kebebew E,“MicroRNA Expression Pr<strong>of</strong>iling is a PotentialDiagnostic Tool for Thyroid Cancer,” Cancer,<strong>2011</strong>.Guerrero MA, Clark OH, “Controversies in theManagement <strong>of</strong> Papillary Thyroid Cancer Revisited,”ISRN Oncol, Sep 16 <strong>2011</strong>.Guerrero MA, Lindsay S, Suh I, Vriens MR,Khanafshar E, Shen WT, Gosnell J, KebebewE, Duh QY, Clark OH, “Medullary ThyroidCancer: It Is a Pain in the Neck?” J Cancer,Apr 8 <strong>2011</strong>.Blakeley JO, Evans DG, Adler J, Brackmann D,Chen R, Ferner RE, Hanemann CO, Harris G,Huson SM, Jacob A, Kalamarides M, KarajannisMA, Korf BR, Mautner VF, McClatchey AI,Miao H, Plotkin SR, Slattery W 3rd, Stemmer-Rachamimov AO, Welling DB, Wen PY, WidemannB, Hunter-Schaedle K, Giovannini M,“Consensus Recommendations for CurrentTreatments and Accelerating Clinical Trials forPatients with Neur<strong>of</strong>ibromatosis Type 2,” Am JMed Genet A, Dec 2 <strong>2011</strong>, epub ahead <strong>of</strong> print.Hurtuk A, Welling DB, Dodson EE, Dome C,Wolfe K, Jacob A, “Melatonin: Can It Stop theRinging?” Ann Otol Rhinol Laryngol 120(7):433-440, Jul <strong>2011</strong>.Bush ML, Oblinger J, Brendel V, Santarelli G,Huang J, Akhmametyeva EM, Burns SS, WheelerJ, Davis J, Chaudhury AR, Kulp S, Chen C-S,Yates CW, Chang L-S, Welling DB, Jacob A,“AR42, A Novel Histone Deacetylase Inhibitor,as a Potential Therapy for Vestibular Schwannomasand Meningiomas,” Neuro Oncol 13(9):983-999, Sep <strong>2011</strong>.Jie T, Gruessner A, Khan K, Desai CS, KaplanB, Rilo H, Gruessner R, “Pancreas GraftShould Be Utilized for Transplantation WhenLiver/Intestine Are Procured from the SameDonor,” American Journal <strong>of</strong> Transplantation 11,Supp S2: 432, Apr <strong>2011</strong>.Jie T, Gruessner A, Desai CS, Khan KM, RiloH, Kaplan B, Gruessner R, “Organs fromDonation after Cardiac Death (DCD) – ASource <strong>of</strong> Potential Growth in Pancreas Transplant,”American Journal <strong>of</strong> Transplantation 11,Supp S2: 71, Apr <strong>2011</strong>.Joseph B, Kulvatunyou N, Tang A, O’KeeffeT, Wynne JL, Friese RS, Rhee P, Latifi R,“Total Parenteral Nutrition in Critically Ill andInjured Patients,” European <strong>Surgery</strong> 43(1): 19-23, <strong>2011</strong>.Con J, Joseph B, Kulvatunyou N, Tang A,O’Keeffe T, Wynne JL, Friese RS, Rhee P,Latifi R, “Evidence-based Immune-modulatingNutritional Therapy in Critically Ill and InjuredPatients,” European <strong>Surgery</strong> 43(1):13-18, <strong>2011</strong>.Rao<strong>of</strong> M, Joseph B, Friese RS, KulvatunyouN, O’Keeffe T, Tang A, Wynne J, Latifi R,Rhee P, “Organ Donation After Traumatic CardiopulmonaryArrest,” The American Journal <strong>of</strong><strong>Surgery</strong> 202(6): 701-705, <strong>2011</strong>.Menaker J, Joseph B, Stein DM, Scalea TM,“Angiointervention: High Rates <strong>of</strong> Failure FollowingBlunt Renal Injuries,” World Journal <strong>of</strong><strong>Surgery</strong> 35(3):520-7, <strong>2011</strong>.Khreiss M, Joseph B, “Packing <strong>of</strong> Liver Injurywith Damage Control Laparotomy, OperativeDictations in General and Vascular <strong>Surgery</strong>,”2nd ed, Springer; New York, <strong>2011</strong>.Hughes MG, Khan KM, Gruessner AC, SharpH, Hil M, Jie T, Kandaswamy R, Humar A,Payne WD, Gruessner RW, “Long-term Outcomein 42 Pediatric Liver Transplant Patientswith Alpha 1-Antitrypsin Deficiency: A Single-Center Experience,” Clin Transplant 25(5):731-6, <strong>2011</strong>.Klein RL, Mook JA, Euhus DM, Rao R, WynnRT, Eastman AB, Leitch AM, “Evaluation <strong>of</strong> aHydrogel Based Breast Biopsy (HydroMark) asan Alternative to Wire and Radioactive SeedLocalization for Non-Palpable Breast Lesions,”Journal <strong>of</strong> Surgical Oncology DOI: <strong>10</strong>.<strong>10</strong>02/jso.22146.Klein R, “<strong>Volume</strong> <strong>of</strong> Excision and Cosmesiswith Routine Cavity Shave Margins Technique,”Journal <strong>of</strong> Surgical Oncology DOI <strong>10</strong>.1245/s<strong>10</strong>434-011-1982-y.Knatterud ME, Book Review, I Curse the River<strong>of</strong> Time by Per Petterson, Wheat Ridge, CO:Science Editor 34(3), p <strong>10</strong>2, Jul-Sep <strong>2011</strong>.29
30Knatterud ME, Book Review, The Master ButchersSinging Club by Louise Erdrich, Wheat Ridge,CO: Science Editor,34(4), p e15, Oct-Dec <strong>2011</strong>.Knatterud ME, Book Review, The A-Z <strong>of</strong> MedicalWriting by Tim Albert, Wheat Ridge, CO:Science Editor 34(4), pp e21-e22, Oct-Dec <strong>2011</strong>.Knatterud ME, Book Review, Stylized: A SlightlyObsessive History <strong>of</strong> Strunk & White’s The Elements<strong>of</strong> Style by Mark Garvey, Wheat Ridge,CO: Science Editor 34(4), p e22, Oct-Dec <strong>2011</strong>.Hornbrook MC, Wendel CS, Coons SJ, Grant M,Herrinton LJ, Mohler MJ, Baldwin CM, McMullenCK, Green SB, Altschuler A, Rawl SM,Krouse RS, “Complications among ColorectalCancer Survivors: SF-6D Preference-WeightedQuality <strong>of</strong> Life Scores,” Med Care 49(3):321-326, Mar <strong>2011</strong>.Glazer ES, Bartels PH, Prasad AR, Yozwiak ML,Bartels HG, Einspahr JG, Alberts DS, KrouseRS, “Nuclear Morphometry Identifies a DistinctAggressive Cellular Phenotype in CutaneousSquamous Cell Carcinoma,” Ca Prev Res4(11):1770-1777, Nov <strong>2011</strong>.Badgwell BD, Contreras C, Askew RL, KrouseR, Feig B, Cormier JN, “Radiographic and ClinicalFactors Associated with Improved Outcomesin Advanced Cancer Patients with Bowel Obstruction,”J Palliat Med 14(9):990-996, Sep<strong>2011</strong>.Grant M, McMullen CK, Altschuler A, MohlerMJ, Hornbrook MC, Herrinton LJ, Wendel CS,Baldwin CM, Krouse RS, “Gender Differencesin Quality <strong>of</strong> Life among Long-term ColorectalCancer Survivors with Ostomies,” Onc Nurs Forum38(5):587-596, Sep <strong>2011</strong>.McMullen CK, Wasserman J, Altschuler A,Grant M, Hornbrook MC, Liljestrand P, BriggsC, Krouse RS, “Untreated Peristomal Skin Disordersamong Colorectal Cancer Survivors withOstomies: Lessons from a Study <strong>of</strong> Family Caregiving,”Clin J Oncol Nurs 1;15(6):644-650,Dec <strong>2011</strong>.Kulvatunyou N, Carter SN, Roberts PM, LeesJS, Bender JS, Albrecht RM, “Contrast-inducedNephropathy among Trauma Patients: Incidence,Risk Factors, and Clinical Outcome,”American Surgeon 78: 686-689, <strong>2011</strong>.Kulvatunyou N, Albrecht RM, Bender JS, FrieseRS, Joseph B, Latifi R, O’Keeffe T, WynneJL, Rhee P, “Seatbelt Triad: Severe AbdominalWall Disruption, Hollow Viscus Injury, andMajor Vascular Injury,” American Surgeon 77; 5;534-538. <strong>2011</strong>.Kulvatunyou N, “National Emergency X-RadiographyUtilization Study Criteria Are Inadequateto Rule Out Fracture after SignificantBlunt Trauma Compared with Computed Tomography,”Letter to the editor, J Trauma 71(4):<strong>10</strong>93-4, <strong>2011</strong>.Kulvatunyou N, Albrecht RM, Bender JS, FrieseRS, Joseph B, Latifi R, O’Keeffe T, WynneJL, Rhee P, “Seatbelt Triad: Severe AbdominalWall Disruption, Hollow Viscus Injury, andMajor Vascular Injury,” American Surgeon 77(5):534-538, <strong>2011</strong>.Kulvatunyou N, Joseph B, Tang A, O’KeeffeT, Wynne JL, Friese RS, Latifi R, Rhee P,“Gut Access in Critically Ill and Injured Patients:Where Have We Gone Thus Far?” European<strong>Surgery</strong> 43(1):24-29 <strong>2011</strong>.Kulvatunyou N, Rhee PM, Carter SN, RobertsPM, Lees JS, Bender JS, Albrecht R, “DefiningIncidence and Outcome <strong>of</strong> Contrast-InducedNephropathy among Trauma Patients: Is ItOverhyped?” Am Surg 77(6):686-9, <strong>2011</strong>.Kulvatunyou N, Vijayasekaran A, Hansen A,Wynne JL, O’Keeffe T, Friese RS, Joseph B,Tang A, Rhee P, “Two-Year Experience <strong>of</strong> UsingPigtail Catheters to Treat Traumatic Pneumothorax:A Changing Trend,” J Trauma71(5):1<strong>10</strong>4-1<strong>10</strong>7, Nov <strong>2011</strong>.Kulvatunyou N, Friese RS, Joseph B,O’Keeffe T, Wynne JL, Tang AL, Rhee P,“Incidence and Pattern <strong>of</strong> Cervical Spine Injuryin Blunt Assault: It Is Not How They Are Hit,But How They Fall,” J Trauma, Oct24 <strong>2011</strong>.Zibadi S, Cordova F, Slack EH, WatsonRR, Larson DF, “Leptin’s Regulation<strong>of</strong> Obesity-Induced CardiacExtracellular Matrix Remodeling,”Cardiovasc Toxicol 11(4):325-33,PMID: 21744298, Dec <strong>2011</strong>.Latifi K, Lecaj I, Bekteshi F, DashoE, Doarn CR, Merrell RC, Latifi R,“Cost-Benefit Analysis on the Use <strong>of</strong>Telemedicine Program <strong>of</strong> Kosova forContinuous Medical Education: ASustainable and Efficient Model toRebuild Medical Systems in DevelopingCountries,” Telemedicine ande-Health 17(<strong>10</strong>), 757-762, <strong>2011</strong>.Zimmerman H, Latifi R, Dehdashti B, Ong E,Jie T, Galvani C, Waer A, Wynne J, Biffar D,Gruessner R, “Intensive Laparoscopic TrainingCourse for Surgical Residents: Program Description,Initial Results, and Requirements,” SurgEndosc, <strong>2011</strong> Jun 4, epub ahead <strong>of</strong> print.Latifi R, “Partial Liver Herniation into the RightChest Following Trauma: A Delayed Presentationas Acute Injury Managed by LaparoscopicallyAssisted Minithoracotomy,” European Journal<strong>of</strong> Trauma and Emergency <strong>Surgery</strong>, online,Dec <strong>2011</strong>.Latifi R, “Nutritional Therapy in Critically Illand Injured Patients,” Surg Clin N Am 91(3):579-593, <strong>2011</strong>.Latifi R, Turegano F, “Current Management <strong>of</strong>Enterocutaneous Fistulas,” European Journal <strong>of</strong>Trauma and Emergency <strong>Surgery</strong> 37:207-208,<strong>2011</strong>.Latifi R, Gustafson M, “Abdominal Wall Reconstructionin Patients with EnterocutaneousFistulas,” Journal <strong>of</strong> Trauma and Emergency <strong>Surgery</strong>37:241-250, <strong>2011</strong>.Sakles JC, Mosier J, Hadeed GJ, Hudson M,Valenzuela T, Latifi R, “Telemedicine and Telepresencefor Prehospital and Remote HospitalTracheal Intubation Using a GlideScope Videolaryngoscope:A Model for Tele-Intubation,”Telemedicine and e-Health 17(3):185-8. epub,Mar <strong>2011</strong>.Dogjani A, Zatriqi S, Uranues S, Latifi R, “Biology-basedNutritional Support <strong>of</strong> Critically Illand Injured Patients,” European <strong>Surgery</strong> 43(1):7-12, <strong>2011</strong>.Latifi R, editorial, “Nutritional Support <strong>of</strong> CriticallyInjured Patients: Do it Early and Do itRight,” European <strong>Surgery</strong> 43(1):5-6, <strong>2011</strong>.Latifi R, Joseph B, Kulvatunyou N, WynneJL, O’Keeffe T, Tang A, Friese R, Rhee PM,“Enterocutaneous Fistulas and a Hostile Abdomen:Reoperative Surgical Approaches,” World JSurg, epublished Oct <strong>2011</strong>.Latifi R, Leppaniemi A, “Complex AbdominalWall Defects and Enterocutaneous Fistulae inthe Era <strong>of</strong> Biological Mesh: Did We Make AnyReal Progress?” World J Surg, epublished Oct<strong>2011</strong>.Luciano CJ, Banerjee PP, Bellotte NJB, LemoleGM Jr, Oh M, Charbel FT, Roitberg BZ, “LearningRetention <strong>of</strong> Thoracic Pedicle Screw PlacementUsing a High-Resolution Augmented RealitySimulator with Haptic Feedback,” Neurosurgery69 (1 Supp Operative):ons14-19, <strong>2011</strong>.Alaraj A, Lemole GM Jr, Finkle JH, YudkowskyR, Wallace A, Luciano C, Banerjee PP, Rizzi SH,Charbel FT, “Virtual Reality Training in Neurosurgery:Review <strong>of</strong> Current Status and FutureApplications,” Surg Neurol Int 2:52, <strong>2011</strong>.
Shankarraman V, Davis-Gorman G, CopelandJG, Caplan MR, McDonagh PF, “StandardizedMethods to Quantify Thrombogenicity <strong>of</strong> Blood-Contacting Materials via Thromboelastography,”J Biomed Mater Res B Appl Biomater <strong>10</strong>0(1):230-8, PMID: 22<strong>10</strong>2528, Epub Nov <strong>2011</strong>.Dokken BB, La Bonte LR, Davis-Gorman G,Teachey MK, Seaver N, McDonagh PF, “Glucagon-likePeptide-1 (GLP-1), Immediately Priorto Reperfusion, Decreases Neutrophil Activationand R myocardial Infarct Size in Rodents,” HormMetab Res 43(5):300-5PMID: 21360419, EpubFeb <strong>2011</strong>.Yassine HN, Davis-Gorman G, Stump CS,Thomson SS, Peterson J, McDonagh PF,“Effect <strong>of</strong> Glucose or Fat Challenge on AspirinResistance in Diabetes,” Int J Endocrinol20<strong>10</strong>:820876, PMID: 21318184, EpubJan <strong>2011</strong>.Lucas LC, Mills JL,“Critical Evaluation <strong>of</strong>Endovascular <strong>Surgery</strong> for Limb Salvage,”Plast Reconstr Surg 127 (Supp): 163S, <strong>2011</strong>.Rose J, Lucas LC, Bui TD, Mills JL, “EndovascularTreatment <strong>of</strong> Ruptured Axillary and LargeInternal Mammary Artery Aneurysms in a Patientwith Marfan Syndrome,” JVS 53(2):478-82,<strong>2011</strong>.Ashton JH, Mertz JA, Harper JL, Slepian MJ,Mills JL, McGrath D, VandeGeest JP, “PolymericEndoaortic Paving: Mechanical, Therm<strong>of</strong>orming,and Degradation Properties <strong>of</strong> Polycaprolactone/PolyurethaneBlends for CardiovascularApplications,” Acta Biomaterialia 7(1):287-94,<strong>2011</strong>.Eidt JF, Mills JL, Rhodes RS, Biester T, GahtanV, Jordan WD, et al, “Comparison <strong>of</strong> SurgicalOperative Experience <strong>of</strong> Trainees and PracticingVascular Surgeons: A Report from the Vascular<strong>Surgery</strong> Board <strong>of</strong> the American Board <strong>of</strong> <strong>Surgery</strong>,”J Vasc Surg 53:1130-40, <strong>2011</strong>.Mills JL, commentary: “Treatment Strategies <strong>of</strong>Arterial Steal after Arteriovenous Access, JVS54(1)167, <strong>2011</strong>.Dawson DL, Mitchell EL, Lee JT, Mills JL, LairdJR, et al, “Validation <strong>of</strong> Simulation as a Tool forAssessing Endovascular Procedural Competency,”JVS 54(2)587, Aug <strong>2011</strong>.Leon LR, Mills JL, “Off-Label Use <strong>of</strong> ReversedZenith Limb Extension Stent-Grafts to TreatDifferent Types <strong>of</strong> Aortoiliac Aneurysmal Disease,”J Endovasc Ther 18:1-3, <strong>2011</strong>.Ritter L, Davidson L, Henry M, Davis-GormanG, Morrison H, Frye J, Cohen Z, Chandler S,McDonagh P, Funk J, “Exaggerated Neutrophil-MediatedReperfusion Injury After IschemicStroke in a Rodent Model <strong>of</strong> Type 2 Diabetes,”Microcirculation 18(7): 552-561, <strong>2011</strong>.Morrison HW, Frye J, Davis-Gorman G, Mc-Donagh P, Funk J, Ritter LS, “The Contribution<strong>of</strong> Mannose Binding Lectin to CerebralReperfusion Injury after Ischemic Stroke,” CurrentNeurovascular Research 8(1): 52-63, <strong>2011</strong>.Dokken B, La Bonte L, Davis-Gorman G,Teachey M, Seaver N, McDonagh P, “Glucagon-likePeptide-1 (GLP-1) Decreases Neutrophil-Activationand Reduces Myocardial InfarctSize,” Hormone and Metabolic Research 43(5):300-305, <strong>2011</strong>.Nfonsam V, Krouse RS, “Chronicling Stridesin Understanding and Managing Rectal Cancer,”Oncol 25(14):1332-1338, Dec <strong>2011</strong>.Davis DM, Marcet JE, Frattini JC, Prather AD,Mateka JJ, Nfonsam VN, “Is It Time To Lowerthe Recommended Screening Age for ColorectalCancer?” J Am Coll Surg, <strong>2011</strong> Jul 6, epub ahead<strong>of</strong> print).Krieger BR, Davis DM, Sanchez JE, Mateka JJ,Nfonsam VN, Frattini JC, Marcet JE, “The Use<strong>of</strong> Silver Nylon in Preventing Surgical Site InfectionsFollowing Colon and Rectal <strong>Surgery</strong>,”Dis Colon Rectum 54(8): <strong>10</strong>14-9, Aug <strong>2011</strong>.Willard SD, Nguyen MM, “Internet SearchTrends Analysis Tools Can Provide Real-TimeData on Kidney Stone Disease in the UnitedStates,” Urology, <strong>2011</strong> Jun 13, epub ahead <strong>of</strong>print.Linehan JA, Bracamonte ER, Hariri LP, Sokol<strong>of</strong>fMH, Rice PS, Barton JK, Nguyen MM, “Feasibility<strong>of</strong> Optical Coherence Tomography Imagingto Characterize Renal Neoplasms: Limitationsin Resolution and Depth <strong>of</strong> Penetration,”BJU Int <strong>10</strong>8(11):1820-4, Dec <strong>2011</strong>.Hadjizacharia P, O’Keeffe T, Plurad D, GreenD, Brown C, Chan L, Demetriades D, Rhee P,“Alcohol Exposure and Outcomes in TraumaPatients,” Eur J Trauma Emerg Surg 37: 169-175,<strong>2011</strong>.Hadjizacharia P, O’Keeffe T, Brown CV, InabaK, Salim A, Chan L, Demetriades D, Rhee P,“Incidence, Risk Factors, and Outcomes forAtrial Arrhythmias in Trauma Patients,” AmSurg 77(5):634-9, <strong>2011</strong>.O’Keeffe T, Thekkkumel JJ, Friese S, Shafi S,Josephs SC, “A Policy Of Dedicated Follow-UpImproves the Rate <strong>of</strong> Removal <strong>of</strong> RetrievableInferior Vena Cava Filters in Trauma Patients,”American Journal <strong>of</strong> <strong>Surgery</strong> 77(1):<strong>10</strong>3-8, Jan<strong>2011</strong>.Erstad B, Haas CE, O’Keeffe T, Hokula CA,Parrinello K, Theodorou AA, “InterdisciplinaryPatient Care in the ICU Setting: Focus on thePharmacist,” Pharmacotherapy 31(2):128-37,<strong>2011</strong>.Gunst M, Matsushima K, Sperry J, GhaemmaghamiV, Robinson M, O’Keeffe T, Friese R,Frankel H, “Focused Bedside Echocardiographyin the Surgical Intensive Care Unit:Comparison <strong>of</strong> 3 Methods to Estimate CardiacIndex,” Journal <strong>of</strong> Intensive Care Medicine26(4):255-60, Jul-Aug <strong>2011</strong>.Aboud ET, Krisht AF, O’Keeffe T, Nader R, HassanM, Stevens CM, Ali F, Luchette FA, “NovelSimulation for Training Trauma Surgeons,” Journal<strong>of</strong> Trauma 71(6):1484-1490, Dec <strong>2011</strong>.Hansen AJ, Augenstein J, Ong ES, “Large SubcapsularLiver Hematoma Following Single-Incision Laparoscopic Cholecystectomy,” JSLS15 (1): 114-116, Jan-Mar <strong>2011</strong>.Chi A, Jang S, Welsh J, Nguyen N, Ong E,Gobar L, Komaki R, “Feasibility <strong>of</strong> Helical Tomotherapyin Stereotactic Body Radiation Therapyfor Centrally Located Early-Stage Non-SmallCell Lung Cancer or Lung Metastases,”Int J Radiat Oncol Biol Phys, Jan <strong>2011</strong>.Zou J, Banerjee B, Garcia-Uribe A, Chang C-C,Yapici MK, Kuczynski J, Ong E, Marner E,Wang L, “High-Transmission Efficiency andSide-Viewing Micro OIDRS Probe for Fast andMinimally Invasive Tumor Margin Detection,”IEEE Sensor Journal 11(4): 891-6, Apr <strong>2011</strong>.Cueto CV, Szeja S, Wertheim BC, Ong ES, TsikitisVL, “Disparities in Treatment and Survival <strong>of</strong>White and Native American Patients withColorectal Cancer: A SEER Analysis,” J Am CollSurg, Jun <strong>2011</strong> epub.Cline GW, Pongratz RL, Zhao X, Papas KK,“Rates <strong>of</strong> Insulin Secretion in INS-1 Cells AreEnhanced by Coupling to Anaplerosis andKreb’s Cycle Flux Independent <strong>of</strong> ATP Synthesis,”Biochem Biopys Re. Comm 415(1): 30-5,<strong>2011</strong>.Suszynski TM, Rizzari MD, Kidder LS, MuellerK, Chapman CS, Kitzmann JP, Pongratz RL,Cline GW, Todd PW, Kennedy D, SchuurmanH-J, O’Brien TD, Avgoustiniatos ES, Papas KK,“Paramagnetic Microparticles Are Neither Immunogenicin Mice Nor Cytotoxic to PorcinePancreatic Islets During Co-Culture,” Xenotransplantation18(4):239-44, <strong>2011</strong>.Suszynski TM, Avgoustiniatos ES, Stein SA, FaldeEJ, Hammer BE, Papas KK, “Assessment <strong>of</strong>Tissue-engineered Islet Graft Viability by FluorineMagnetic Resonance Spectroscopy,” TransplantationProceedings 43(9):3221-5, <strong>2011</strong>.Anazawa T, Matsumoto S, Yonekawa Y, LoganathanG, Wilhelm JJ, Soltani SM, Papas KK,Sutherland DER, Hering BJ, Balamurugan AN,“Prediction <strong>of</strong> Pancreatic Tissue Densities by anAnalytical Test Gradient System Before PurificationMaximizes Human Islet Recovery for IsletAuto/Allotransplantation,” Transplantation 91(5):508-14, <strong>2011</strong>.31
32Fan W, Atchison N, Brewer DD, ArunagirinathanMA, Hering BJ, Kokkoli E, Kumar S, PapasKK, Tsapatsism M, “Silica NanoparticleCoatings by Adsorption from Lys-Sil Sols onInorganic and Biological Surfaces,” AngewandteChemie 50(7):1617-21, <strong>2011</strong>.Abrahante JE, Martins K, Papas KK, HeringBJ, Schuurman H-J, Murtaugh MP, “MicrobiologicalSafety <strong>of</strong> Porcine Islets: Comparisonwith Source Pig,” Xenotransplantation 18(2):88-93, <strong>2011</strong>.Sajja VSK, Hanley TR, Gapsis H, Guernsey B,Kennedy DJ, Taylor MJ, Papas KK, Todd PW,“Application <strong>of</strong> Magnetic Particle Tracking Velocimetryto Quadrupole Magnetic Sorting <strong>of</strong>Porcine Pancreatic Islets,” Biotechnology andBioengineering <strong>10</strong>8(9):2<strong>10</strong>7-17, <strong>2011</strong>.Abouaish J, Graham M, Pakala P, LoganathanG, Yuasa T, Papas KK, Sutherland DER, Mc-Carthy RC, Hering BJ, Balamurugan AN, “SuccessfulIsolation and Transplantation <strong>of</strong> Non-Human Primate Islets Utilizing VitaCyte CIzymeCollagenase MA and CIzyme ThermolysinPurified Enzymes,” Transplantation92(8):e40-2, <strong>2011</strong>.Loganathan G, Dawra RK, Pugazhenthi S, GuoZ, Soltani SM, Wiseman A, Sanders MA, PapasKK, Kumaravel V, Saluja AK, Sutherland DER,Hering BJ, Balamurugan AN, “Insulin Degradationby Acinar-Cell Proteases Creates a DysfunctionalEnvironment for Human Islets Before/AfterTransplantation: Benefits <strong>of</strong> Alpha 1-Antitrypsin Treatment,” Transplantation92(11):1222-1230, <strong>2011</strong>.Graham ML, Bellin MD, Papas KK, Hering BJ,Schuurman H-J, “Species Incompatibilities inthe Pig-to-Macaque Islet Xenotransplant ModelAffect Transplant Outcome: A ComparisonWith Allotransplantation,” Xenotransplantation18(6):328-42, <strong>2011</strong>.Kurian D, Gorcos J, Meinke S, ThirumavalavanN, Mizrahi I, Kiani S, Desai P, Poston RS,“Change Management and an Innovative Approachto Heart Bypass <strong>Surgery</strong>,” Physician Exec37(6):30-7, PMID: 22195414, Nov-Dec <strong>2011</strong>.Kiani S, Poston R, “Is Endoscopic HarvestingBad for Saphenous Vein Graft Patency in Coronary<strong>Surgery</strong>?,” Curr Opin Cardiol 26(6):518-22, PMID: 21986399, Nov <strong>2011</strong>.Kiani S, Desai PH, Thirumvalavan N, KurianDJ, Flynn MM, Zhao X, Poston RS, “EndoscopicVenous Harvesting by InexperiencedOperators Compromises Venous Graft Remodeling,”Ann Thorac Surg 93(1):11-7; discussion17-8, PMID: 21996436,. Epub Oct <strong>2011</strong>.Desai P, Kiani S, Thiruvanthan N, Henkin S,Kurian D, Ziu P, Brown A, Patel N, Poston R,“Impact <strong>of</strong> the Learning Curve for EndoscopicVein Harvest on Conduit Quality and EarlyGraft Patency,” Ann Thorac Surg 91(5):1385-91;discussion 1391-2, PMID: 21524447, May<strong>2011</strong>.Gordy SD, Rhee P, Schreiber MA, “MilitaryApplications <strong>of</strong> Novel Hemostatic Devices,”Expert Rev Med Devices 8(1):41-7, <strong>2011</strong>.Rhee P, “Albumin,” J Trauma 70(5):S22-S24,<strong>2011</strong>.Inaba K, Rhee P, Teixeira P, Galinos B, Putty B,Branco B, Cohn S, Demetriades D, “IntracorporealUse <strong>of</strong> Advanced Local Hemostatics in aDamage-Control Swine Model <strong>of</strong> Grade IV LiverInjury: A Randomized Controlled PreclinicalTrial,” J Trauma 71(5):1312-8, Nov <strong>2011</strong>.Rhee P, Joseph B, “Hypertonic Saline Resuscitationin Trauma,” Review Article, InternationalHospital Equipment and Solutions Magazine, Pan-Global Media, Oct <strong>2011</strong>.Rodriguez-Rilo HL, Grigsby BM, GruessnerRW, “Pharmacologic Strategies for Improvement<strong>of</strong> Islet Survival: Targeting the EnterohormonalAxis,” Transpl Int 24(12):1156-8, <strong>2011</strong>.Goldman S, Sethi GK, Holman W, Thai H,McFalls E, Ward HB, Kelly RF, Rhenman B,Tobler GH, Bakaeen FG, Huh J, Soltero E,Moursi M, Haime M, Crittenden M, KasirajanV, Ratliff M, Pett S, Irimpen A, Gunnar W,Thomas D, Fremes S, Moritz T, Reda D, HarrisonL, Wagner TH, Wang Y, Planting L, MillerM, Rodriguez Y, Juneman E, Morrison D, PierceMK, Kreamer S, Shih MC, Lee K, “Radial ArteryGrafts vs Saphenous Vein Grafts in CoronaryArtery Bypass <strong>Surgery</strong>: A Randomized Trial,”JAMA 305(2):167-74, PMID: 21224458, Jan<strong>2011</strong>.Subramanian S, Seeburger J, Noack T, MohrFW, “Future Perspectives in Minimally InvasiveCardiac <strong>Surgery</strong>,” Tex Heart Inst J 38(6):678-9,<strong>2011</strong>.Subramanian S, Mohr FW, “The Case AgainstSuperspecialization in <strong>Surgery</strong>,” Semin ThoracCardiovasc Surg 23(3):171-2, Autumn <strong>2011</strong>.Schroeter T, Subramanian S, Borger MA,Mohr FW, “Staged Concept for Treatment <strong>of</strong>Severe Postsaphenectomy Wound Infection,”Case Report Med. 903839, Epub Aug <strong>2011</strong>.Pettersson GB, Subramanian S, Flynn M, NowickiER, Batizy LH, Svensson LG, BlackstoneEH, “Reoperations after the Ross Procedure inAdults: Towards Autograft-Sparing/Ross Reversal,”J Heart Valve Dis, Jul;20(4):425-32, <strong>2011</strong>.Subramanian S, Misfeld M, Rastan AJ, Letterby Subramanian et al regarding article, “ComparisonBetween Transcatheter and SurgicalProsthetic Valve Implantation in Patients withSevere Aortic Stenosis and Reduced Left VentricularEjection Fraction,” Circulation16;124(7):e206; author reply e207-8, Aug<strong>2011</strong>.Schroeter T, Subramanian S, Lehmann S,Kempfert J, Misfeld M, Mohr FW, Borger MA,“Dislocation <strong>of</strong> a Transapically Implanted AorticValve Prosthesis with a Functionally BicuspidAortic Valve and Ascending Aortic Aneurysm,”Thorac Cardiovasc Surg 59(8):503-6, Epub <strong>2011</strong>Apr, Dec <strong>2011</strong>.Schroeter T, Bittner H, Subramanian S, HänsigM, Mohr F, Borger M, “Life-threatening HemothoraxResulting from Lung Hernia after MinimallyInvasive Mitral Valve <strong>Surgery</strong>,” Thorac CardiovascSurg 59(4):252-4, Epub <strong>2011</strong> Mar 21,June <strong>2011</strong>.Tang A, Inaba K, Branco BC, Oliver M, BukurM, Salim A, Rhee P, Herrold J, Demetriades D,“Post-Discharge Complications After PenetratingCardiac Injury: A Survivable Injury with a HighPost-Discharge Complication Rate,” Arch Surg146(9):<strong>10</strong>61-<strong>10</strong>66, <strong>2011</strong>.Tang A, Wip C, Garner W, Demetriades D,“Burns,” in Demetriades D, Newton E, MandaviaD, eds, Color Atlas <strong>of</strong> Emergency Trauma, 2nd ed,Cambridge, UK: Cambridge <strong>University</strong> Press,253-270, <strong>2011</strong>.Thompson JL, Schaff HV, Dearani JA, Park SJ,Sundt TM, Suri RM, Blackhshear JL, Daly RC,“Risk <strong>of</strong> Recurrent Gastrointestinal BleedingAfter Aortic Valve Replacement in Patients withHeyde Syndrome,” Journal <strong>of</strong> Thoracic and Cardiovascular<strong>Surgery</strong> <strong>2011</strong>.Neiderer K, Walters J, Armstrong DG, “Feasibility,Safety, and Primary Efficacy <strong>of</strong> Dermastream:A Novel Continuously Streaming Devicefor Wounds,” Foot Ankle Specialist 4:222-225,<strong>2011</strong>.Engelhardt C, Curiel-Lewandrowski C,Warneke, Cranmer L, “Metastatic CutaneousSquamous Cell Carcinoma Responding toErlotinib,” J Am Acad Dermatol 65(1):237-8,Jul <strong>2011</strong>.Sosman JA, Moon J, Tuthill RJ, Warneke JA,Vetto JT, Redman BG, Liu PY, Unger JM, FlahertyLE, Sondak VK, “A Phase 2 Trial <strong>of</strong> CompleteResection for Stage IV Melanoma: Results<strong>of</strong> Southwest Oncology Group Clinical TrialS9430,” Cancer, Mar <strong>2011</strong>.Curiel-Lewandrowski C, Speetzen LS, CranmerL, Warneke JA, Loescher LJ, “Multiple PrimaryCutaneous Melanomas in Li-Fraumeni Syndrome,”Arch Dermatol 147(2):248-50, Feb<strong>2011</strong>.Stidd DA, Root B, Weinand ME, Anton R,“Granulomatous Amoebic Encephalitis Causedby Balamuthia mandrillaris in an ImmunocompetentGirl,” World Neurosurg, <strong>2011</strong> Nov 1, epubahead <strong>of</strong> print.Osbun JW, Ellenbogen RG, Chesnut RM, ChinLS, Connolly PJ, Cosgrove GR, Delashaw JB Jr,Golfinos JG, Greenlee JD, Haines SJ, Jallo J,
Muizelaar JP, Nanda A, Shaffrey M, Shah MV,Tew JM Jr, van Loveren HR, Weinand ME,White JA, Wilberger JE, “A Multicenter, Single-Blind, Prospective Randomized Trial to Evaluatethe Safety <strong>of</strong> a Polyethylene Glycol Hydrogel(Duraseal Dural Sealant System) as a DuralSealant in Cranial <strong>Surgery</strong>,” World Neurosurg,Dec <strong>2011</strong> epub ahead <strong>of</strong> print.Kanady JD, Dellinger MT, Munger SJ, WitteMH, Simon AM, “Connexin37 and Connexin43Deficiencies in Mice Disrupt LymphaticValve Development and Result in LymphaticDisorders Including Lymphedema and Chylothorax,”Developmental Biology 354: 253-266,<strong>2011</strong>.Witte M, Dellinger M, McDonald D, NathansonD, Boccardo F, Campisi C, Sleeman J, GershenwaldJ, “Lymphangiogenesis/Hemangiogenesis:Potential Targets for Therapy,” specialissue on Seminars in Surgical Oncology: The PivotalRole <strong>of</strong> the Lymphovascular System in CancerMetastasis, Leong S, guest ed, J Surg Oncol <strong>10</strong>3:489-500, <strong>2011</strong>.Witte M, “Translational/Personalized Medicine,Pharmaco/Surgico/Radiogenomics, LymphaticSpread <strong>of</strong> Cancer, and Medical Ignoromes,”J Surg Oncol <strong>10</strong>3: 501-507, <strong>2011</strong>.Leong SPL, Witte M, “Future Perspectives,Unanswered Questions and Research Agenda,”J Surg Oncol <strong>10</strong>3: 639-641, <strong>2011</strong>.Shimoda H, Bernas MJ, Witte MH, “Dysmorphogenesis<strong>of</strong> Lymph Nodes in Foxc2 HaploinsufficientMice,” Histochem Cell Biol 135:603-613, <strong>2011</strong>.Campisi C, Witte MH, Fulcheri E, Campisi C,Bellini C, Villa G, Campisi C, Santi PL, ParodiA, Murdaca G, Puppo F, Boccardo F, “General<strong>Surgery</strong>, Translational Lymphology and Lymphatic<strong>Surgery</strong>,” Int Angiol 30:504-521, <strong>2011</strong>.Dellinger M, Bernas M, Witte M, “LymphaticBiology and Pathobiology,” in Venous and LymphaticDiseases, Chapter 3, New York: McGrawHill, pp 17-35, <strong>2011</strong>.Campisi C, Boccardo F, Witte M, Bernas M,“Lymphatic <strong>Surgery</strong> and <strong>Surgery</strong> <strong>of</strong> LymphaticDisorders, ” in Venous and Lymphatic Diseases,Chapter 42, New York: McGraw Hill, pp 607-629, <strong>2011</strong>.Jones KA, Witte MH, “Hereditary and FamilialLymphedema Syndromes,” in LYMPHEDEMA:A Concise Compendium <strong>of</strong> Theory and Practice,Chapter 3, London: Springer, pp 29-39, <strong>2011</strong>.Williams W, O’Chart M, Bernas M, Witte CL,Witte MH, “Radionuclide Lymphoscintigraphy,”in LYMPHEDEMA: A Concise Compendium<strong>of</strong> Theory and Practice, Chapter 19, London:Springer, pp 145-154, <strong>2011</strong>.Douglas MJK, Flake N, Witte M, “ImprovedMethod for Chronic Cannulation <strong>of</strong> the RatThoracic Duct for Multiple Pool Kinetic Studies,”Western Student Medical Research Forum(WSMRF), Carmel, CA, Jan 27-29, <strong>2011</strong>, J InvestMed 59:177-178, <strong>2011</strong>.Witte MH, Crown P, Bernas M, Hall J, Daley S,Garcia F, “Balancing Medical Informatics andMedical ‘Ignoramics’,” Curriculum, Assessment,and the Virtual Clinical Research Center/Questionnarium, J Invest Med 59(4): 728, <strong>2011</strong>.Chen L, Yuen D, Bernas M, Witte M, GrimaldoS, “Specific Role <strong>of</strong> Angiopoietin-2 in CornealLymphangiogenesis,” Association for Researchin Vision and Ophthalmology (ARVO) annualmeeting, Ft. Lauderdale, FL, May 1-5, <strong>2011</strong>,Invest Ophthalmol Vis. Sci. <strong>2011</strong>; 52:6385.Witte MH, “Overview <strong>of</strong> Biomarkers, Pathways,and Pathology in Lymphatic and CancerDevelopment,” 4th Annual International Symposiumon Cancer Metastasis and the LymphovascularSystem: Basis for Rational Therapy;Chair: SPL Leong; New York, May 12-14,<strong>2011</strong>. Abstract Booklet, p 55.PresentationsArmstrong D, “The Diabetic Foot,” SouthernArizona Musculoskeletal Radiology Society,Tucson, Dec <strong>2011</strong>.Armstrong D, “Negative Pressure WoundTherapy: What’s New? What’s True?,” InternationalLimb Salvage Symposium / Stop theEruption <strong>of</strong> Amputations, Castellamare di Stabila,Naples, Italy, Dec <strong>2011</strong>.Armstrong D, “On Entropy, Energy and Results:Making a Difference for the Native AmericanNations,” Indian Health Services NationalWound Advisory Meeting, Phoenix, Nov <strong>2011</strong>.Armstrong D, “How to Live Forever” (expertpanelist), Pima County on Aging, <strong>University</strong> <strong>of</strong>Arizona College <strong>of</strong> Science, L<strong>of</strong>t Cinema Series,Tucson, Oct <strong>2011</strong>.Armstrong D, Keynote Address (via video),“The Diabetic Foot: Demography and Destiny,”Belgian Society <strong>of</strong> Podiatrists, Brussels, Belgium,Oct <strong>2011</strong>.Armstrong D, “Missionary vs. Mercenary: Innovation,Teamwork (and Industry?),” “BioengineeredTissue: Evidence for Regeneration?,”“The Neuroischemic Foot: Our Population HasChanged, But Our Options Haven’t,” Georgetown<strong>University</strong> Hospital Diabetic Limb SalvageSymposium, Washington, DC, Sep <strong>2011</strong>.Armstrong D, “The Diabetic Foot in the Age<strong>of</strong> Decay,” <strong>10</strong>th Anniversary Orange CountyPodiatric Medical Society Surgical Symposium,Huntington Beach, CA, Sep <strong>2011</strong>.Witte MH, “Ignorance <strong>University</strong>: A Parallel<strong>University</strong> for a Parallel Universe,” 15th InternationalThinking Conference, Belfast, Ireland,Jun 20-24, <strong>2011</strong>, Abstract Booklet, p 90.Witte MH, “Lymphology and the ISL in theReal, Virtual, and Imagined World <strong>of</strong> theFuture,”23rd International Congress on Lymphology,Malmö, Sweden, Sep 19-23, <strong>2011</strong>,Abstract Booklet, KN-01, p 22.Daley SK, Bastidas E, Washington J, Bernas MJ,Witte MH, “Foxc2 Deficiency and MelanomaSpread in a Mouse Model,” 23rd InternationalCongress on Lymphology, Malmö, Sweden, Sep19-23, <strong>2011</strong>, Abstract Booklet, P14.14, p 184.Cullinane DC, Schiller HJ, Zielinski MD, BilaniukJW, Collier BR, Como J, Holevar M, SabaterEA, Sems SA, Vassy WM, Wynne JL,“Eastern Association for the <strong>Surgery</strong> <strong>of</strong> TraumaPractice Management Guidelines for Hemorrhagein Pelvic Fracture—Update and SystematicReview,” Journal <strong>of</strong> Trauma 71(6):1850-68,Dec <strong>2011</strong>.Armstrong D, “Diabetic Foot: A World View,”“Negative Pressure Wound Therapy: Predictionsand A Philosophy,” “The Toe and FlowModel <strong>of</strong> Amputation Prevention,” 8th AsiaPacific Burn and 3rd Asia Wound Healing AssociationConferences, Bangkok, Thailand,Sep <strong>2011</strong>.Armstrong D, Visiting Pr<strong>of</strong>essor, “The DiabeticFoot: Techniques and Teamwork,” Asan MedicalCenter, <strong>Department</strong> <strong>of</strong> Plastic and Reconstructive<strong>Surgery</strong>, Seoul, Republic <strong>of</strong> Korea,Sep <strong>2011</strong>.Armstrong D, “The Diabetic Foot,” <strong>University</strong><strong>of</strong> Cardiff Visiting Pr<strong>of</strong>essor Lecture Series,Masters <strong>of</strong> Science in Tissue Repair and WoundHealing, Cardiff, Wales (via video) Sep <strong>2011</strong>.Armstrong D, Keynote Address, “DiabeticFoot, <strong>2011</strong>: The Global State <strong>of</strong> Play,” 5th JapaneseNational Diabetic Foot Conference, Saga,Japan, Aug <strong>2011</strong>.Armstrong D, “Offloading,” “Wound Classification,”“SALSA Team Approach,” Saga DiabeticFoot Symposium, Saga, Japan, Aug <strong>2011</strong>.Armstrong D, “Diabetic Foot: The Global State<strong>of</strong> Play,” American Podiatric Medical AssociationScientific Symposium, Boston, Jul <strong>2011</strong>.Armstrong D, “Wound Healing: What’s Next,”KCI/Lifecell Meet the Pr<strong>of</strong>essor / Wound HealingLecture Series, Santa Barbara, CA, Jul <strong>2011</strong>.33
34Armstrong D, Chair, Pecoraro Award Lectureand Oral Abstracts Session: Foot Care InterestGroup, 71st American Diabetes AssociationScientific Sessions, San Diego, Jun <strong>2011</strong>.Armstrong D, “The Diabetic Foot: The GlobalState <strong>of</strong> Play in <strong>2011</strong>,” “Diabetic Foot <strong>Surgery</strong>:Toward a Common Language,” Tornier Footand Ankle <strong>Surgery</strong> Course, Washington, DC,Jun <strong>2011</strong>.Armstrong D, Keynote Lecture, “The Team:Who is On It and How to Make a Difference,”“Offloading and Debriding the Diabetic Foot:New Tools for New Times,” Mexican NationalDiabetic Foot Congress, Puerto Vallarta, Mexico,Jun <strong>2011</strong>.Armstrong D, “Diabetic Foot and NPWT: TheState <strong>of</strong> Play in <strong>2011</strong>,” Expert Committee onNegative Pressure Wound Therapy (WorldUnion <strong>of</strong> Wound Healing Societies), LomaLinda/Riverside, CA, May <strong>2011</strong>.Armstrong D, “Diabetic Foot: Update, <strong>2011</strong>,”Ontario Society <strong>of</strong> Chiropodists and Podiatrists(via video from Holland), Toronto, May <strong>2011</strong>.Armstrong D, “Coming Events Cast TheirShadows Before: Quantifying Inflammation(Externally),” Co-Chair, “Surgical Reconstruction”Plenary, USA Delegate, Consensus DevelopmentConference, Noordwijkerhout, Netherlands,May <strong>2011</strong>.Armstrong D, Royal Australian College <strong>of</strong> SurgeonsMasterclass, “Pathophysiology <strong>of</strong> DiabeticFoot Complications (and what to doabout it),” 6th International Working Groupon the Diabetic Foot, Adelaide, Australia (viavideo), May <strong>2011</strong>.Armstrong D, Commencement Speaker, Barry<strong>University</strong> School <strong>of</strong> Podiatric Medicine, MiamiShores, FL, Apr <strong>2011</strong>.Armstrong D, “Making Prevention Pay,” <strong>University</strong><strong>of</strong> Arizona <strong>Department</strong> <strong>of</strong> <strong>Surgery</strong> Innovation/ Intellectual Property Retreat, Tucson,Apr <strong>2011</strong>.Armstrong D, Keynote Address, “The DiabeticFoot: Rise <strong>of</strong> the Toe and Flow,” Coney IslandHospital (via video), Brooklyn, Apr <strong>2011</strong>.Armstrong D, Kinetic Concepts VisitingPr<strong>of</strong>essor Series, “Bioengineered Tissues andRegeneration,” Boston, Apr <strong>2011</strong>.Armstrong D, Kinetic Concepts VisitingPr<strong>of</strong>essor Series, “Bioengineered Tissues andRegeneration,” Dallas, Apr <strong>2011</strong>.Armstrong D, “Global Perspectives, LocalTreatment (Chair),” “Dancing the SALSA: KeepingRhythm with Outcomes, Teamwork, andHope in the U.S. Southwest,” “Breaking theNews without Breaking the Bank (Chair),”“Toepocalypse Now: Avoiding Toetastrophywith Technical and Timely Tips (Chair),”“Achilles Heel <strong>of</strong> the Diabetic Foot (Chair),”“I SPY Healing: Theragnostic Imaging for theOR?,” International Diabetic Foot Conference,<strong>2011</strong> (DFCon11), Los Angeles, Mar <strong>2011</strong>.Armstrong D, “Coordinated Use <strong>of</strong> AdvancedModalities in Healing Diabetic Foot Wounds,”Midwest Podiatry Symposium, Chicago,Mar <strong>2011</strong>.Armstrong D, Healalliance Research Symposium:Toward a Cure (Chair), Los Angeles,Mar <strong>2011</strong>.Armstrong D, Chair/Moderator, “DiabeticFoot: Scope <strong>of</strong> the Problem,” Macrocure MD-<strong>10</strong>2 Protocol Investigator Meeting,Ft. Lauderdale, FL, Feb <strong>2011</strong>.Armstrong D, “Charcot Neuroarthropathy Is aSyndrome: Neuropathic Inflammatory CharcotSyndrome (NICS),” Joint ADA/APMA TaskForce on Charcot Arthropathy, SalpetriereHospital, Paris, Jan <strong>2011</strong>.Armstrong D, Keynote Speaker, “The Team:How to Heal Patients and Build Programs,”Connecticut Podiatric Medical AssociationAnnual Symposium, Hartford (via video),Jan <strong>2011</strong>.Armstrong D, “The Diabetic Foot,” “DiabeticFoot <strong>Surgery</strong>,” Montana Podiatric Medical AssociationAnnual Symposium, Bozeman, MT,Jan <strong>2011</strong>.Armstrong D, “Building a Team to PreventAmputations—Hows and Whys,” Meet thePr<strong>of</strong>essor, Seattle, Jan <strong>2011</strong>.Breidenbach W, Video Teleconference Presentationon Hand Transplantation, InternationalHand and Composite Tissue AllotransplantationSociety, Apr <strong>2011</strong>.Breidenbach W, Presentation on Facial Transplantation,Association in Osteosynthesis NorthAmerica Symposium: Challenges and Advancesin the Management <strong>of</strong> Craniomaxill<strong>of</strong>acial <strong>Surgery</strong>(Focus: Microsurgery), Baltimore,May <strong>2011</strong>.Breidenbach W, Presentation and Training onHand Transplantation Protocols, United Networkfor Organ Sharing (UNOS), Phoenix,Sep <strong>2011</strong>.Breidenbach W, Presentation on CompositeTissue Allotransplantation, Reaching Consensusin Reconstructive Transplantation Symposium,American Society for ReconstructiveTransplantation, Baltimore, Nov <strong>2011</strong>.Breidenbach W, Presentation on CompositeTissue Allotransplantation, Arizona Chapter,American College <strong>of</strong> Surgeons, Phoenix,Nov <strong>2011</strong>.Chiu AG, Visiting Pr<strong>of</strong>essor, Mexican ENTSociety <strong>2011</strong> Endoscopic Sinus and Skull Base<strong>Surgery</strong> Course, Mexico City, Feb <strong>2011</strong>.Chiu AG, Invited Faculty, “Management <strong>of</strong>FESS Failures,” California Sinus CenterAdvanced Endoscopic Sinus <strong>Surgery</strong> Course,Scottsdale, Feb <strong>2011</strong>.Chiu AG, “Nasal Polyposis,” North AmericanRhinology and Allergy Conference, San Juan,Puerto Rico, Feb <strong>2011</strong>.Chiu AG, Invited Faculty, “Skull Base Reconstruction,Sinonasal Tumors,” Annual Meeting<strong>of</strong> the North American Skull Base Society,Scottsdale, Mar <strong>2011</strong>.Chiu AG, Invited Guest Faculty, “FESS,” “TopicalMedications for CRS,” Penn InternationalRhinology and Skull Base Course, Philadelphia,Mar <strong>2011</strong>.Chiu AG, Invited Guest Faculty, “Frontal Sinus<strong>Surgery</strong>,” “Management <strong>of</strong> Recalcitrant ChronicRhinosinusitis,” Medical <strong>University</strong> <strong>of</strong> SouthCarolina FESS Course, Charleston, Mar <strong>2011</strong>.Chiu AG, Invited Faculty, “Sinonasal Tumors,”<strong>University</strong> <strong>of</strong> Calgary Endoscopic Sinus<strong>Surgery</strong> Course, Calgary, Jul <strong>2011</strong>.Chiu AG, “Endoscopic Management <strong>of</strong> SinonasalMalignancies,” “Tips for FESS Failures,”Annual Meeting <strong>of</strong> the American Academy <strong>of</strong>Otolaryngology – Head and Neck <strong>Surgery</strong>, InstructionalCourse, San Francisco, Sep <strong>2011</strong>.Chiu AG, Miniseminar Panelist, “Topical Therapiesfor CRS,” Annual Meeting <strong>of</strong> the AmericanAcademy <strong>of</strong> Otolaryngology – Head andNeck <strong>Surgery</strong>, San Francisco, Sep <strong>2011</strong>.Chiu AG, Keynote Lecturer, “Endoscopic Management<strong>of</strong> Benign and Malignant SinonasalLesions, FESS Failures, Tips to MaximizeFESS,” Fall Meeting <strong>of</strong> the Arizona OtolaryngologySociety, Scottsdale, Oct <strong>2011</strong>.Chiu AG, Invited Faculty, “Sinonasal Tumors,”“Complications <strong>of</strong> FESS,” Western States ResidentSinus Course, Loma Linda <strong>University</strong>,Riverside, CA, Nov <strong>2011</strong>.Chiu AG, Invited Speaker, “Chronic Rhinosinusitis,”Division <strong>of</strong> Pulmonary MedicineTeaching Conference, Tucson, Nov <strong>2011</strong>.Desai CS, Gruessner AC, Gruessner RW,Khan K, “Effect <strong>of</strong> HLA Mismatch on Long-Term Outcome <strong>of</strong> Intestinal Transplantation,”“Outcomes <strong>of</strong> Intestinal Transplants for InflammatoryBowel Diseases,” XII InternationalSmall Bowel Transplant Symposium, Washington,DC, Sep <strong>2011</strong>.Desai CS, Gruessner AC, Khan KM, Jie T,Carton M, Gruessner RW, “Isolated IntestinalTransplants vs. Multivisceral Transplantsamong Pediatric Patients in United States,”
6th Congress <strong>of</strong> the International PediatricTransplant Association, Montreal, Jun <strong>2011</strong>.Desai CS, Gruessner AC, Gruessner RW, JieT, Rilo H, Khan KM, “Liver Transplants forChildren with Cystic Fibrosis,” 6th Congress <strong>of</strong>the International Pediatric Transplant Association,Montreal, Jun <strong>2011</strong>.Desai CS, Khan KM, Gruessner AC, Jie T,Rilo H, Carton MM, Gruessner R, “IntestinalRetransplantation in Adults: Analysis <strong>of</strong> 22Years <strong>of</strong> the UNOS Database,” American TransplantCongress, Philadelphia, May <strong>2011</strong>.Cummings LS, Graham JA, Guerra J, HawksworthJS, Rosen-Bronson S, Girlanda R, DesaiCS, Johnson LB, Melancon JK, “Utilizing PairedKidney Exchange and Desensitization Programto Increase Living Donor Kidney Transplantationin African Americans,” American TransplantCongress, Philadelphia, May <strong>2011</strong>.Desai CS, Gruessner R, Gruessner A, Jie T,Rilo HL, Carton MM, Khan KM, “Liver Transplantsfor Cystic Fibrosis-Related Cirrhosis:Analysis <strong>of</strong> 22 Years <strong>of</strong> the UNOS Database,”American Transplant Congress, Philadelphia,May <strong>2011</strong>.Desai CS, Gruessner AC, Khan KM, Jie T,Gruessner RWG, Poster Presentation, “Comparison<strong>of</strong> Intestinal Transplant (Tx) Alone(ITA) vs. Liver-Intestinal and Multiorgan Transplant(MVTx) Outcomes: An OPTN/SRTR DatabaseAnalysis,” American Society <strong>of</strong> TransplantSurgeons 11th Annual State <strong>of</strong> the ArtWinter Symposium, Hollywood, FL, Jan <strong>2011</strong>.Desai CS, Khan KM, Gruessner AC, Jie T,Rilo H, Carton MM, Gruessner RW, “IntestinalRetransplantation in Adults: Analysis <strong>of</strong> 22Years <strong>of</strong> the UNOS Database,” American TransplantCongress, Philadelphia, May <strong>2011</strong>.Friese R, Bender J, O’Keeffe TA, Joseph BA,Wynne JL, Kulvatunyou N, Tang A, LatifiR, Rhee P, “Sleep Deprivation after Septic InsultTruncates Pro-Inflammatory Cytokine Releasein a Murine Model,” 41st Annual Meeting<strong>of</strong> the Western Trauma Association, Big Sky,MT, Mar <strong>2011</strong>.Galvani C, “Advances in MIS: Single-IncisionGeneral and Bariatric <strong>Surgery</strong>,” Invited GrandRounds Speaker, UMDNJ-SOM, <strong>Department</strong> <strong>of</strong><strong>Surgery</strong>, Stratford, NJ,Mar <strong>2011</strong>.Galvani C, “Medical Advancesin Weight Loss <strong>Surgery</strong>,”Invited Speaker,Sierra Vista Health Center,Sierra Vista, AZ, Mar <strong>2011</strong>.Galvani C, “Single-IncisionLaparoscopic Cholecystectomy(SIL-C) Usinga Novel Technique for Retraction<strong>of</strong> the Gallbladder: Evaluation <strong>of</strong> theInitial Experience,” Poster Session, SAGES<strong>2011</strong>, San Antonio, Mar <strong>2011</strong>.Galvani C, “Single-Incision Donor Nephrectomy,”<strong>2011</strong> World Robotic General <strong>Surgery</strong>Symposium, Miami, Jun <strong>2011</strong>.Galvani C, “Multipurpose Internal Retractorfor Single-Incision <strong>Surgery</strong> (SIS),” 20th SLSMeeting & Endo Expo, Los Angeles, Sep <strong>2011</strong>.Galvani C, “Single-Incision Laparoscopic HiatalHernia Repair with Nissen Fundoplication,”American College <strong>of</strong> Surgeons 97th AnnualClinical Congress, San Francisco, Oct <strong>2011</strong>.Galvani C, Invited Speaker, “Update <strong>of</strong> theIntracorporal Retraction Device—Experiencesin SPA,” 3rd International Round Table MeetingLaparoscopy, Freiburg-Lehen, Germany, Nov <strong>2011</strong>.Green DJ, “Thoracic Trauma,” Guardian MedicalTransport; “Emergency <strong>Department</strong> Thoracotomy,”Trauma Grand Rounds; Flagstaff MedicalCenter, Flagstaff, AZ, Jul <strong>2011</strong>.Green DJ, “Thoracic Trauma,” Pre-HospitalTrauma Update, Northwest Medical Center,Tucson, Aug <strong>2011</strong>.Green DJ, “Thoracic Trauma,” Pre-HospitalTrauma Update, Tucson Fire <strong>Department</strong>, Tucson,Sep <strong>2011</strong>.Green DJ “Trauma Update,” Rincon Valley Fire<strong>Department</strong>, Vail, AZ, Sep <strong>2011</strong>.Green DJ, “Pre-Hospital Trauma Day,” Director,Southwest Ambulance Service, Tucson, Oct<strong>2011</strong>.Green DJ, “Thoracic Trauma,” Pima CommunityCollege EMT Class, Tucson, Oct <strong>2011</strong>.Green DJ, “Tension Pneumothorax—Treatmentin the Field, the ICU, and on the BigScreen,” Special Operations Medical OperationsSymposium, Tampa, Dec <strong>2011</strong>.Green DJ, “Base Hospital EMS Trauma Update,”Davis-Monthan AFB, Tucson, Dec <strong>2011</strong>.Gruessner RWG, “Current State <strong>of</strong> AbdominalTransplantation,” Texas Tech <strong>University</strong>Health Sciences Center Grand Rounds, El Paso,Feb <strong>2011</strong>.Gruessner RWG, “Transplant Options for theTreatment or Prevention <strong>of</strong> Insulin-DependentDiabetes Mellitus,” 6th Scientific Session,Halsted Society Meeting, Baltimore, Sep <strong>2011</strong>.Gruessner RWG, “Transplant CoverageCuts—How Arizona Provides an Example,”“Emerging <strong>Issue</strong>s in Organ Transplantation:A Colloquium,” Cleveland Clinic, Cleveland,Oct <strong>2011</strong>.Vijayasekaran A, Maegawa F, Gruessner A,Guerrero MA, “Parathyroid Gland Size Limitsthe Accuracy <strong>of</strong> Bilateral Internal Jugular VeinSampling <strong>of</strong> Parathyroid Hormone in the Localization<strong>of</strong> Parathyroid Adenoma,” 63rd AnnualMeeting, Southwestern Surgical Congress, Honolulu,Apr <strong>2011</strong>.Maegawa F, Vijayasekaran A, Guerrero MA,Poster Presentation, “A Rare Finding <strong>of</strong> an EctopicParathyroid Gland Within a Cervical ThymicCyst Presenting as a Lateral Neck Mass,”63rd Annual Meeting, Southwestern SurgicalCongress, Honolulu, Apr <strong>2011</strong>.Hamilton A, Invited Speaker, “Lessons fromMedicine—Learned the Hard Way,” Chief ExecutivesRetreat, Canyon Ranch Resort, Tucson,Jan <strong>2011</strong>.Hamilton A, Invited Speaker, “Neurochemistryand the Art <strong>of</strong> the Deal,” National Women’sBusiness Association, Tucson, Feb <strong>2011</strong>.Hamilton A, Invited Speaker, “Code Blue: CanTechnology Save Us from a Tidal Wave <strong>of</strong> MedicalErrors?,” Healthcare Information and ManagementSystems Society, Elsevier Healthcare,Orlando, Feb <strong>2011</strong>.Hamilton A, Keynote Speaker, “From HospitalBedside to Hollywood Set: The Importance <strong>of</strong>the Medical Narrative,” Elsevier Healthcare,Healthcare Information and Management SystemsSociety, Orlando, Feb <strong>2011</strong>.Hamilton A, Keynote Address, “Ten SpiritualGuidelines That Can Make You a Better Neurosurgeon,”Mayfield Clinic-Cleveland ClinicWinter Clinics for Cranial & Spinal <strong>Surgery</strong>,Aspen, Mar <strong>2011</strong>.Hamilton A, Invited Speaker, “Building a SimulationThink Tank to Improve RegionalHealthcare,” Mayfield Clinic-Cleveland ClinicWinter Clinics for Cranial & Spinal <strong>Surgery</strong>,Aspen, Mar <strong>2011</strong>.Hamilton A, Invited Speaker, “How Am I EverGoing to Lose Weight If My Brain Makes MeEat?,” Canyon Ranch Resort, Tucson,Mar <strong>2011</strong>.Hamilton A, Invited Speaker, “The Neurobiology<strong>of</strong> Empathy, Compassion, and Love,” CanyonRanch Resort, Tucson, Mar <strong>2011</strong>.35
Hamilton A, Invited Guest Speaker, “The DoctorSpeaks Out: A Primer for Where Medicine’sGoing Astray,” Saddlebrooke, AZ, Mar <strong>2011</strong>.Hamilton A, Invited Speaker, “Lessons fromthe Edge: the Spiritual Side <strong>of</strong> Medicine andthe Medical Side <strong>of</strong> Spirituality,” Canyon RanchResort, Tucson, Apr <strong>2011</strong>.Hamilton A, Keynote Speaker, “Innovation:the Biologic Efficacy <strong>of</strong> Magic,” 2nd AnnualConference on Medical Innovation, Washington,DC, Oct <strong>2011</strong>.tion after Cardiac Death (DCD) Pancreas Transplant,”13th World Congress <strong>of</strong> InternationalPancreas & Islet Transplant Association,Prague, Czech Republic, Jun <strong>2011</strong>.Mbaeyi C, Rance N, Manch R, Kaplan B, BamfordC, Echevarria L, Trivedi V, Brink J, Jie T,Viscusi C, Weiss J, Farnon E, Paddock C, daSilvaA, Roy S, Zaki S, Visvesvara G, Kuehnert M,“Balamuthia mandrillaris—An Emerging PathogenTransmissible in Organ Transplantation,”American Transplant Congress, Philadelphia,May <strong>2011</strong>.Joseph B, Hadeed GJ, “Smart Technology forthe Management <strong>of</strong> Trauma and Critically IllPatients,” American Telemedicine AssociationFall Forum, Anchorage, Sep <strong>2011</strong>.Joseph B, “Smart Phone and Handheld DeviceUse in Trauma Telemedicine: Applications andHIPAA Considerations,” Indian Health ServiceChief Medical Officer’s Rounds, WebEx Seminar,Sep <strong>2011</strong>.Joseph B, “MusliArabAmer-I-Can,” Annual Reunion<strong>of</strong> Convention, Perrysberg, OH, Jul <strong>2011</strong>.Hamilton A, Invited Speaker, “The Neuroscience<strong>of</strong> Transcendence, ” 9th Annual AppliedBrilliance Conference, Four Seasons Hotel,Jackson Hole, WY, Oct <strong>2011</strong>.Hamilton A, Invited Speaker, “The HumanMirror Neuron System,” Spirituality in Pediatrics<strong>2011</strong>, Texas Children’s Hospital, Houston,Oct <strong>2011</strong>.Hamilton A, Keynote Speaker, “Simulation:Training for Moments When Humans BreakDown,” IIIrd Annual Conference CollaborationAcross Borders, Tucson, Nov <strong>2011</strong>.Jacob A, “Conductive Hearing Loss,” MedCentralHealth System Hospital Grand Rounds,MedCentral Health System, Mansfield, OH, Jan<strong>2011</strong>.Burns SS, Akhmametyeva EM, Oblinger JL,Bush ML, Huang J, Senner V, Giovannini M,Chen C-S, Jacob A, “AR-42 and AR-12Potently Inhibit the Growth <strong>of</strong> NF2-DeficientHuman Meningiomas,” <strong>2011</strong> Children’s TumorFoundation/NF Conference, Jackson Hole, WY,Jun <strong>2011</strong>.Jacob A, “AR42: A Novel Histone DeacetylaseInhibitor with High C Clinical-TranslationalPotential as Treatment for NF2-Associated Tumors,”28th Politzer Society Meeting, Athens,Greece, Sep <strong>2011</strong>.Diven C, Lee E, Mahadevan D, Tsikitis V, Jie T,Ong E, Oral Presentation, “Laparoscopic HyperthermicIntraperitoneal Chemotherapy(HIPEC) for Malignant Ascites from GastrointestinalStromal Cell Tumor (GIST),” 6th InternationalSymposium on Regional Cancer Therapies,Incline Village, NV, Feb <strong>2011</strong>.Rose J, Jie T, Ong E, Poster Presentation, “Pancreaticoduodenectomyfor Primary PancreaticLymphoma,” 63rd Annual Meeting, SouthwesternSurgical Congress, Honolulu, Apr <strong>2011</strong>.Con J, Joseph B, “Can Trauma Patient AdmissionCharacteristics Predict Rehab Outcomes?,”MacDonald Wood Arizona ACS Competition,Southwest Trauma & Acute Care Symposium,Scottsdale, Nov <strong>2011</strong>.Joseph BA, Friese RS, Kulvatunyou N,O’Keeffe T, Tang A, Wynne J, Latifi R, RheeP, Oral Presentation, “Continuous NoninvasiveHemoglobin Monitor from Pulse OX in CriticallyIll Trauma Patients,” International SurgicalWeek, International Society <strong>of</strong> <strong>Surgery</strong>, PacificoYokohama, Japan, Sep <strong>2011</strong>.Rao<strong>of</strong> M, Joseph B, Friese R, Wynne J,O’Keeffe T, Kulvatanyou N, Tang A, RheeP, “Don’t Give Up: Predictors and Prevalence <strong>of</strong>Organ Donation After Traumatic CardiopulmonaryArrest,” 63rd Annual Meeting, SouthwesternSurgical Congress, Honolulu, Apr <strong>2011</strong>.Joseph B, “Trauma and Domestic Abuse,” <strong>10</strong>thAnnual Mother’s Day Luncheon, Emerge! CenterAgainst Domestic Abuse, Westin La Paloma,Tucson, May <strong>2011</strong>.Joseph B, “Hemostasis and Resuscitation,”SWAT Medics Training, Tucson, Apr <strong>2011</strong>.Joseph B, “U <strong>of</strong> A Trauma: Past, Present, & Future,”Green Valley 260 Club, Green Valley RecreationCenter, Green Valley, AZ, Jan <strong>2011</strong>.Krouse RS, Invited Speaker, “Malignant BowelObstruction: A Clinical Conundrum”; Discussant,“Cancers <strong>of</strong> the Pancreas, Small Bowel, andHepatobiliary Tract Session,” <strong>2011</strong> GastrointestinalCancers Symposium, San Francisco,Jan <strong>2011</strong>.Campesino M, Ruiz E, Uriri Glover J, Koithan M,Saenz D, Krouse R, Larkey L, Juarez G, PosterPresentation, “Communication Challenges inCancer Care Delivery: Perspectives from Latinaand African American Breast Cancer Survivors,”Oncology Nursing Society, Los Angeles,Feb <strong>2011</strong>.McMullen CK, Grant M, Hornbrook MC,Krouse RS, Poster Presentation, “The SocialEcology <strong>of</strong> Cancer-Related Disability: Case Studies<strong>of</strong> Caregiving for Rectal Cancer Survivors,”8th Annual Conference, American PsychosocialOncology Society, Anaheim, Feb <strong>2011</strong>.36Jie T, Gruessner AC, Desai CS, Khan KM,Rilo H, Kaplan B, Gruessner RW, “Organsfrom Donation after Cardiac Death (DCD)—ASource <strong>of</strong> Potential Growth in Pancreas Transplant,”American Transplant Congress, Philadelphia,May <strong>2011</strong>.Jie T, Gruessner AC, Khan KM, Desai CS,Kaplan B, Rilo H, Gruessner R, “PancreasGraft Should Be Utilized for TransplantationWhen Liver/Intestine Are Procured from theSame Donor,” American Transplant Congress,Philadelphia, May <strong>2011</strong>.Jie T, Gruessner AC, Desai CS, Khan KM,Rilo H, Gruessner RW, “Simultaneous Procurement<strong>of</strong> Liver and Intestinal Grafts forTransplantation in the Same Donor Did NotNegatively Impact the Pancreas Graft Outcome,”“Equivalent Graft Outcomes BetweenDonation after Brain Death (DBD) and Dona-Rao<strong>of</strong> M, Joseph B, Friese RS, KulvatunyouN, O’Keeffe T, Tang A, Wynne JL, Latifi R,Rhee P, “Organ Donation Failure after TraumaticCardiopulmonary Arrest,” Poster Presentation,97th Annual Clinical Congress, AmericanCollege <strong>of</strong> Surgeons, San Francisco, Oct<strong>2011</strong>.Joseph B, Hadjizacharia P, Friese RS, KulvatunyouN, O’Keeffe T, Tang A, Wynne JL,Latifi R, Rhee P, “Prothrombin Complex Concentrate:An Effective Therapy in Reversing theCoagulopathy <strong>of</strong> Traumatic Brain Injury,” PosterPresentation, 70th Annual Meeting <strong>of</strong> theAmerican Association for the <strong>Surgery</strong> <strong>of</strong> Traumaand Clinical Congress <strong>of</strong> Acute Care <strong>Surgery</strong>,Chicago, Sep <strong>2011</strong>.Joseph B, Rhee P, “Media Involvement AfterHigh Pr<strong>of</strong>ile Injuries: Are Trauma Centers Prepared?,”Western Surgical Association, Tucson,Nov <strong>2011</strong>.Krouse RS, Invited Speaker, Survivorship Research,CC&P Outreach Harry Hynes Symposium,Southwest Oncology Group (SWOG)Semiannual Group Meeting, San Francisco,Apr <strong>2011</strong>.
Krouse RS, Invited Speaker, “SWOG S0820 ADouble-Blind Placebo-Controlled Trial <strong>of</strong> Eflornithineand Sulindac to Prevent Recurrence <strong>of</strong>High-Risk Adenomas and Second PrimaryColorectal Cancers in Patients with Stage 0-IIIColon Cancer, Phase III,” American Society <strong>of</strong>Colon and Rectal Surgeons Research Foundation<strong>2011</strong> Research Fair, ASCRS Annual Meeting,Vancouver, May <strong>2011</strong>.Krouse RS, Invited Speaker, “Quality <strong>of</strong> Lifeamong Long-Term Cancer Survivors with anOstomy”’ Norma Gill Lecturer, “Wound, Ostomy,and Continence,” 43rd Annual Conference,Nurses Society, New Orleans, Jun 4-8,<strong>2011</strong>.Kulvatunyou N, Joseph B, Friese RS,O’Keeffe T, Wynne JL, Tang AL, Rhee P,Poster Presentation, “Pattern <strong>of</strong> Cervical SpineInjury in Blunt Assault: It’s Not How They’reHit, It’s How They Fall,” SCCM, San Diego,<strong>2011</strong>.Kulvatunyou N, Vijayasekaran V, Joseph B,Friese RS, O’Keeffe T, Wynne JL, Tang AL,Rhee P, Oral Presentation, “2-Year Experience<strong>of</strong> Pigtail Catheter in the Management <strong>of</strong> TraumaticPneumothorax: A Changing Trend,”Western Trauma Association, Big Sky, MT, Feb-Mar <strong>2011</strong>.Kulvatunyou N, “Tucson Shootings,” 11thAnnual Arizona EMS Odyssey Conference,Desert Will Conference, Phoenix, Jun <strong>2011</strong>.Latifi R, Oral Presentation, “Global HealthInitiative to Strengthen Medical Systems inDeveloping Countries Using Telemedicine andAdvanced Technologies: A Sustainable Model<strong>of</strong> Surgical Volunteerism,” “Telemedicine andTelepresence in Trauma and <strong>Surgery</strong>: The NewParadigm,” “Organ Donation Failure after TraumaticCardiopulmonary Arrest,” 97th AnnualClinical Congress, American College <strong>of</strong> Surgeons,San Francisco, Oct <strong>2011</strong>.Latifi K, Lecaj I, Bekteshi F, Doarn CR, MerrellRC, Latifi R, Oral Presentation, “Cost-BenefitAnalysis <strong>of</strong> the Telemedicine Program <strong>of</strong> Kosova—ASustainable and Efficient Model to RebuildMedical Systems in Developing Countries,”American Telemedicine Association AnnualMeeting, May <strong>2011</strong>.Latifi R, Invited Speaker (via video-telepresence),“Telemedicine Program for the BalkanArea,” 1st International Conference on E-Health and Telemedicine, Nicosia, North Cyprus,Oct <strong>2011</strong>.Latifi R, Invited Speaker, “Initiate-Build-Operate-Transfer:A Strategy for Establishing SustainableTelemedicine Programs Not Only inthe Developing Countries,” ASEAN Rural ConnectivityConference for Education and Development,Hanoi, Vietnam, Sep <strong>2011</strong>.Latifi R, Invited Speaker, “Telemedicine Program<strong>of</strong> Kosova and Albania: Live InteractivePresentation <strong>of</strong> 13 Telemedicine Sites,” “Teletraumaand Telepresence for Emergency Management,”ASEAN Rural Connectivity Conferencefor Education and Development, Hanoi,Vietnam, Sep <strong>2011</strong>.Latifi R, Invited Speaker (via video-telepresence),“Initiate-Build-Operate-Transfer: A Strategyfor Establishing Sustainable TelemedicinePrograms Not Only in the Developing Countries,”Iraqi Medical Association: The 40th ScientificConference, Sulaimanya, Iraq, Sep <strong>2011</strong>.Stidd D, Dunn JH, Lemole GM Jr, Anton R,“Traumatic Thoracolumbar Fractures Treatedwith Short-Segment Pedicle Instrumentation,”AANS/CNS Section on Disorders <strong>of</strong> the Spineand Peripheral Nerves, Annual Meeting,Phoenix, Mar <strong>2011</strong>.Yudkowsky R, Luciano C, Banerjee P, Alaraj A,Lemole M, Schwartz A, Charbel F, MlinarevichN, Smith K, Gandhi S, Rizzi S, “A Library <strong>of</strong>Virtual Brains for Ventriculostomy Practice on aVR/Haptic Simulator—Initial Validity Evidence,”International Meeting for Simulation inHealthcare (IMSH), 11th Annual InternationalMeeting, New Orleans, Jan <strong>2011</strong>.Lemole GM Jr, “Neurotrauma Care: Under theMedia Microscope,” Advocate Injury InstituteSymposium, Lisle, IL, Nov <strong>2011</strong>.Lemole GM Jr, “Living in the Limelight: ANeurosurgeon’s Perspective <strong>of</strong> the Tucson Tragedy,”Western Neurosurgical Society, 57thAnnual Meeting, Kauai, HI, Sep <strong>2011</strong>.Lemole GM Jr, “Making a Difference,”Chestnut Hill Academy Cum Laude Society,Philadelphia, Apr <strong>2011</strong>.Lemole GM Jr, “Living in the Limelight,”Association <strong>of</strong> Healthcare Journalists AnnualConference, Philadelphia, Apr <strong>2011</strong>.Mills JL, “Occam’s Razor: Sometimes a Blade IsStill the Simplest Solution;” “The 8th AnnualEdward James Olmos Award for Advocacy inAmputation Prevention,” “Eschar-go: HealingHeel Ulcers (Even at a Snail’s Pace),” DFCon(Diabetic Foot Conference), Los Angeles,Mar <strong>2011</strong>.Mills JL, “The Toe/Flow Team at Arizona:Vascular <strong>Surgery</strong> and Podiatry,” “A SignificantNumber <strong>of</strong> True CLI Patients Will UltimatelyNeed Bypass for Limb Salvage Preservation,”UCSF Vascular Symposium <strong>2011</strong>, San Francisco,Apr <strong>2011</strong>.Mills JL, “Toe and Flow: Teamwork for AmputationPrevention,” <strong>University</strong> <strong>of</strong> Florida <strong>Department</strong><strong>of</strong> <strong>Surgery</strong> Grand Rounds, Apr <strong>2011</strong>.Mills JL, “Catheter-Based Intervention for InfrainguinalOcclusive Disease: Techniques andResults,” 29th Annual UCLA Symposium: AComprehensive Review and Update <strong>of</strong> What’sNew in Vascular and Endovascular <strong>Surgery</strong>,Sep <strong>2011</strong>.Mills JL, “What Is Critical Limb Ischemia andHow Should Outcomes Be Measured?,” PacificNorthwest Vascular Society, Nov <strong>2011</strong>.Mills JL, “Selecting Patients for Revascularization:Should We Be Lesionologists or Physiologists?,”“What Are the Most Exciting New Developmentsin the Treatment <strong>of</strong> Lower ExtremityIschemia: Will More or Fewer LE Bypassesbe Required than in the 25-30 Percent <strong>of</strong> CLIPatients Estimated Last Year?,” “When Do AngiosomesMatter in CLI and What To Do AboutIt?,” Veith Symposium <strong>2011</strong>, New York,Nov <strong>2011</strong>.Nguyen MM, Ahmann FR, Nagle RB, HsuChiu-Hsieh, Tangrea JA, Parnes HL, Sokol<strong>of</strong>fMH, Gretzer MB, Chow HH, “Randomized,Double-Blind, Placebo-Controlled Trial <strong>of</strong> PolyphenonE in Prostate Cancer Patients BeforeRadical Prostatectomy: Evaluation <strong>of</strong> PotentialChemopreventive Activities,” Western SectionAUA meeting, Vancouver, <strong>2011</strong>.Willard SD, Nguyen MM, “Internet SearchMetrics Can Provide Real-Time Data on KidneyStone Disease in the United States,” AmericanUrological Association Annual Meeting, Washington,DC (Best Poster Award Winner), <strong>2011</strong>.McCauley LR, Dyer AJ, Stern K, Hicks T,Nguyen MM, “Factors Influencing Fluid IntakeBehavior in Kidney Stone Formers,” 58th AnnualKimbrough Seminar, Seattle (Best PosterAward Winner), <strong>2011</strong>.Nfonsam VN, “Advances in the Management<strong>of</strong> Complex Anorectal Fistula,” <strong>Surgery</strong> GrandRounds, <strong>University</strong> <strong>of</strong> South Florida, Jun <strong>2011</strong>.Nfonsam VN, Prather A, Mateka J, Frattini JC,Marcet JE, “Outcomes <strong>of</strong> the Surgical Management<strong>of</strong> Acquired Rectourethral Fistulas: DoesTechnique Matter?,” Academic Surgical Congress,Huntington Beach, CA, <strong>2011</strong>.Nfonsam VN, Prather A, Mateka J, Frattini JC,Marcet J, “Outcomes <strong>of</strong> Treatment <strong>of</strong> PerirectalFistulas with the Anal Fistula Plug,” AmericanCollege <strong>of</strong> Surgeons Clinical Congress, Sep<strong>2011</strong>, San Francisco, <strong>2011</strong>.Nfonsam VN, Prather A, Mateka J, Frattini JC,Marcet J, “Initial Failure <strong>of</strong> Rectovaginal FistulaRepair Should Not Preclude Repeat Attempts atRepair,” <strong>University</strong> <strong>of</strong> South Florida, AmericanSociety <strong>of</strong> Colon and Rectal Surgeons AnnualMeeting (ASCRS), <strong>2011</strong>.Davis D, Horne D, Mateka J, Nfonsam V, FrattiniJ, Marcet J, “Without Warning? Characteristics<strong>of</strong> Young Colorectal Patients,” AmericanSociety <strong>of</strong> Colon and Rectal Surgeons AnnualMeeting (ASCRS), Vancouver, <strong>2011</strong>.37
38Nfonsam VN, Prather A, Mateka J, Frattini JC,Marcet J, “Colorectal Cancer in Patients withInflammatory Bowel Disease,” Society <strong>of</strong> SurgicalOncology, San Antonio, <strong>2011</strong>O’Keeffe T, “Keppra Prophylaxis for PosttraumaticBrain Injury Seizures Is Ineffective: APropensity Score Analysis,” EAST 24th AnnualScientific Assembly, Naples, FL, <strong>2011</strong>.O’Keeffe T, “Pitfalls and Limitations,” FASTUltrasound Skills Course ICU PostgraduateCourse; “How to Implement a Massive TransfusionProtocol,” Introduction to Damage ControlResuscitation Symposium; 97th Annual ClinicalCongress <strong>of</strong> the American College <strong>of</strong> Surgeons,San Francisco, Oct <strong>2011</strong>.Ong E, “Surgical Strategies to Successful Treatment<strong>of</strong> Hepatic Tumors,” “Cytoreductive <strong>Surgery</strong>and Hyperthermic Intraperitoneal Chemoperfusion(HIPEC) for Peritoneal Carcinomatosis;”1st Congress UCIMED International, SanJose, Costa Rica, Aug <strong>2011</strong>.Banerjee B, Rouse A, Tiwari P, Kuczynski J,Risi M, Gavini H, Ong ES, Jie T, Gmitro AF,“Confocal Microscopy for the Confirmation <strong>of</strong>Tumor-Free Surgical Margins in PancreaticCancer,” Digestive Disease Week <strong>2011</strong>,Chicago, May <strong>2011</strong>.Glazer ES, Gustafson M, Ong E, Joseph B,Poskus D, Adamas-Rappaport W, “ImprovingMedical Student Trauma-Related NBMEStandardized Exam Scores: A Hands-on Experience,”Poster Presentation, 97th Annual ClinicalCongress, American College <strong>of</strong> Surgeons,San Francisco, Oct <strong>2011</strong>.Taylor MJ, Baicu S, Weegman B, Papas KK,“Hypothermic Perfusion <strong>of</strong> Pancreas as an AidTowards Clinical Islet Transplantation,” HiltonHead Regenerative Medicine Workshop,Mar <strong>2011</strong>.Balamurugan AN, Loganathan G, Bellin MD,Wilhelm JJ, Yuasa T, Tiwari M, Papas KK,Vickers S, Beilman GJ, Hering BJ, SutherlandDER, “Islet Isolation Outcome from MinimalChange Chronic Pancreatitis Is Comparablewith Clinical Grade Allograft Pancreases,”American Transplant Congress, Philadelphia,Apr-May <strong>2011</strong>.Suszynski TM, Avgoustiniatos E, Stein SA, FaldeEJ, Hammer BE, Papas KK, “Assessment <strong>of</strong>Tissue-Engineered Islet Graft Viability by FluorineMagnetic Resonance Spectroscopy”; WeegmanBP, Taylor MJ, Baicu SC, Pongratz R,Mueller K, O’Brien TD, Cline G, Wilson J, PapasKK, “Biological Characterization <strong>of</strong> IsolatedJuvenile Porcine Islets as a PotentialSource <strong>of</strong> Tissue for Xenotransplantation”;Weegman BP, Taylor MJ, Baicu SC, Scott WEIII, Mueller KR, Kitzmann JP, Rizzari MD, PapasKK, “Hypothermic Perfusion Preservation<strong>of</strong> Pancreas for Islet Grafts: Validation Using aSplit-Lobe Porcine Model”; Scott WE III, RizzariMD, Stein SA, Avgoustiniatos ES, SuszynskiTM, Weegman BP, Tempelman LA, HammerBE, Papas KK, “Oxygen Persufflation <strong>of</strong> theHuman Pancreas Increases ATP Levels and ImprovesViable Islet Yields Compared with theTwo-Layer Method”; Abouaish J, Graham M,Pakala P, Loganathan G, Tiwari M, Yuasa T,Papas KK, Sutherland DER, McCarthy RC,Hering, BJ, Balamurugan AN, “A New PurifiedEnzyme Blend for Nonhuman Primate IsletIsolation”; Soltani SM, Loganathan G, BellinMD, Papas KK, Dunn TB, Vickers SM, BeilmanGJ, Hering BJ, Sutherland DER, BalamuruganAN, “Reducing the Transplantable Tissue<strong>Volume</strong> for Human Islet Autotransplantation: AHigh-Density Purification Process Differentfrom Islet Allograft Purification”; LoganathanG, Dawra RK, Pugazhenthi S, Guo Z, SoltaniSM, Wiseman A, Sanders MA, Papas KK,Saluja AK, Sutherland DER, Hering BJ, BalamuruganAN, “Acinar Cell Proteases Reduce InsulinGranules <strong>of</strong> Human Islets In Vitro andDegrade Insulin After Transplantation: PreventiveEffect <strong>of</strong> Alpha 1-Antitrypsin”; Papas KK,“Oxygen Persufflation”—all at 13th WorldCongress <strong>of</strong> the International Pancreas and IsletTransplant Association, Prague, Czech Republic,Jun <strong>2011</strong>.Papas KK, “Beta-Cell Replacement: An Engineer’sView Through the Lens <strong>of</strong> an Isletologist,”Brussels Free <strong>University</strong>, Brussels,Jun <strong>2011</strong>.Balamurugan AN, Loganathan G, Bellin MD,Papas KK, Dunn T, Vickers SM, Beilman GJ,Hering BJ, Sutherland DER, “High Islet Yieldfrom Pre-Teenage Pediatric Patients UndergoingTotal Pancreatectomy and Islet Autotransplantationfor Chronic Pancreatitis Compared toTeenage and Adult Patients,” 71st ADA ScientificSessions, San Diego, Jun <strong>2011</strong>.Rizzari M, Suszynski TM, Scott WE, WeegmanBP, Finger EB, O’Brien TD, Kidder LS, KandaswamyR, Sutherland DE, Avgoustiniatos ES,Papas KK, “Preservation via Anterograde PersufflationMay Decrease Renal Arterial Damagein a Porcine Kidney Transplant Model,” XII TTSBasic Science Symposium, Boston, Jun <strong>2011</strong>.Weegman BP, Rizzari MD, Scott III WE, TaylorMJ, Baicu SC, Suszynski TM, AvgoustiniatosES, Loughnane MH, Papas KK, “Whole-OrganOxygen Consumption Rate (WOOCR):A Novel Tool for Organ Assessment Prior toTransplant,” XII TTS Basic Science Symposium,Boston, Jun <strong>2011</strong>.Papas KK, Co-Organizer, International Workshop,“Islet Transplantation without Borders,”Athens, Greece, Dec <strong>2011</strong>.Poston RS, “Injury Incurred During EndoscopicVeins Harvesting Is Associated withCompromised Vascular Remodeling,” SouthernThoracic Surgical Association, San Antonio,Nov <strong>2011</strong>.Poston RS, “Cost <strong>of</strong> Implications Hybrid Therapy:Can We Afford It?,” Transcatheter CardiovascularTherapeutics, San Francisco,Nov <strong>2011</strong>.Poston, RS, “Venous Grafts Procured Duringthe Learning Curve for Endoscopic Veins HarvestingShow Compromised Vascular Remodeling,”Society <strong>of</strong> Thoracic Surgeons, San Diego,Jan <strong>2011</strong>.Rhee P, “Cardiac Arrest in Trauma: EmergencyPreservation and Resuscitation for Cardiac Arrestfrom Trauma,” “What’s New in ControllingHemorrhage in Trauma? New Horizons in Hemostatics,”“Incidence and Pattern <strong>of</strong> CervicalSpine Injury in Blunt Assault: It’s Not HowThey’re Hit, It’s How They Fall,” 40th CriticalCare Congress, San Diego, Jan <strong>2011</strong>.Rhee P, “Ballistics in Arizona,” Surgical GrandRounds, Cedars Sinai, Los Angeles, Feb <strong>2011</strong>.Rhee P, “Mass Casualty in Tucson and Ballistics,”Long Beach Trauma Symposium, LongBeach, CA, Feb <strong>2011</strong>.Rhee P, “Mechanics <strong>of</strong> Tissue Injury,” SessionModerator; “Mechanics <strong>of</strong> Inducing Hypothermia,”“Hemorrhagic Shock and Arrest,” <strong>2011</strong>NHLBI & DoD HYPOSTAT Workshop: Hypothermiain Trauma: A New Crossroads, NIHcampus, Bethesda, MD, Feb <strong>2011</strong>.Rhee P, “Handling the Media After a Big Event,”Special Session, 41st Annual Meeting <strong>of</strong> theWestern Trauma Association, Big Sky, MT,Mar <strong>2011</strong>.Rhee P, “Ballistics and Blast,” Keynote Speaker,Taiwan Surgical Society Annual Meeting,Formosa, Taiwan, Mar <strong>2011</strong>.Rhee P, “Is There a Role for Hypertonic Solution?:IV Fluids: Which Type?,” “Polytrauma: ATutorial,” “Damage Control <strong>Surgery</strong> Is Overutilized:Polytrauma,” “Local Hemostatics, DoThey Work?: Massive Bleeding,” “Head Trauma,”Session Moderator, “Type <strong>of</strong> Intravenous Fluids:Where is the Evidence?,” 31st InternationalSymposium on Intensive Care and EmergencyMedicine, Brussels, Belgium, Mar <strong>2011</strong>.Rhee P, “Ballistics: Myth and Facts,” SurgicalGrand Rounds, St. Raphael’s Hospital, NewHaven, CT, Mar <strong>2011</strong>.Rhee P, “Cooling for Trauma,” 13th AnnualConnecticut Trauma Conference, Ledyard, CT,Mar <strong>2011</strong>.Rhee P, “Biological and Chemical Hazards,”“Late-Breaking News—Tucson Story,” GroupFacilitator, “Triage,” Medical Disaster Response<strong>2011</strong>, Las Vegas, Apr <strong>2011</strong>.Rhee P, “New Technology—Hot or Hype?,”“Debate—Pro: Damage Control Laparotomy IsPast Its Prime,” Trauma, Critical Care & AcuteCare <strong>Surgery</strong> <strong>2011</strong>, Las Vegas, Apr <strong>2011</strong>.
Rhee P, Keynote Speaker, “How To Be anIr-Repressible Surgeon,” <strong>2011</strong> Annual SpringLuncheon, Arizona’s Asian American Faculty,Staff, and Alumni Association (AAFSAA),Tucson, Apr <strong>2011</strong>.Rhee P, Keynote Speaker, “Resuscitation HasChanged,” “Have Guns, Will Need TraumaSurgeons,” 25th Annual Midwest TraumaConference, Kansas City, May <strong>2011</strong>.Rhee P, “Mass Casualty Incidents—The ArizonaExperience,” “Rheeopardy,” 18th AnnualUSC Trauma / Critical Care Symposium,Pasadena, CA, May <strong>2011</strong>.Rhee P, “Care <strong>of</strong> Gunshot Injury in USA TraumaSystem,” 26th Annual Congress, KoreanSociety <strong>of</strong> Traumatology, Trauma Lecture, NationalMedical Center, Trauma Lecture, AsianMedical Center, Seoul, Korea, May-Jun <strong>2011</strong>.Rhee P, Introduction and Welcome Address,Controversial Case Discussion, “Trauma in Tucson,”22nd Annual Southwest Regional TraumaConference, Tucson, Aug <strong>2011</strong>.Rhee P, “Bleeding and Shock,” Tuba City, Ft.Defiance, Gallup Indian Medical Center, WhiteRiver & Summit Healthcare Regional MedicalCenter, Tour and Lectures to the Navajo IndianNation Hospitals, Aug-Sep <strong>2011</strong>.Rhee P, “Ballistics Made Easy,” Arizona TraumaResearch Consortium Grand Rounds, Sep <strong>2011</strong>.Rhee P, Address to the Annual Meeting <strong>of</strong> theAmerican College <strong>of</strong> Healthcare Executives,Arizona Chapter, Carefree, AZ, Oct <strong>2011</strong>.Rhee P, Keynote Speaker, “The Tucson Tragedy,”“Stutter: What’s Right in Health Care,”Chicago, Oct <strong>2011</strong>.Rhee P, “Penetrating Cardiac Injury: Techniques,”“New Concepts in Resuscitation,”“Call in the Gray Hairs,” American College <strong>of</strong>Surgeons Annual Conference, San Francisco,Oct <strong>2011</strong>.Rhee P, “Ballistics Made Easy: Myths andFacts,” Southwest Trauma and Acute CareSymposium, Scottsdale, Nov <strong>2011</strong>.Rhee P, Lecturer, “Damage Control Is Overratedand Overused”; Moderator, “When theBleeding Gets Going, The Going Gets Rough”;Lecturer, “I Want It to Stick: Sealants andGlues”; Panelist, “Scope <strong>of</strong> Practice / FinancialModels / Training / Future Directions”; HarvardTrauma and Critical Care Symposium, Boston,Nov <strong>2011</strong>.Rhee P, Keynote Speaker, “Leadership: What isit?,” American Academy <strong>of</strong> Medical Administrators,Scottsdale, Nov <strong>2011</strong>.Rhee P, Invited Speaker, “Trauma Services,”El Tour De Tucson Dedication Dinner, Tucson,Nov <strong>2011</strong>.Rhee P, Keynote Speaker, “Life, Liberty, andthe Pursuit <strong>of</strong> Happiness,” ICAS Annual LibertyAward Dinner, Caucus Room, Canyon Building,Capitol Hill, Washington, DC, Dec <strong>2011</strong>.Rilo H, Vardanyan M, Gruessner C, Desai CS,Jie T, Gruessner RW, Khan KM, GruessnerA, “Continuous Glucose Monitoring (CGM): ANew Tool for Evaluation <strong>of</strong> -Cell Function inClinical Islet Autotransplantation,” 13th WorldCongress <strong>of</strong> International Pancreas & IsletTransplant Association, Prague, Czech Republic,Jun <strong>2011</strong>.Nasser FS, Ritsema DF, Cheney S, Stern K, Sokol<strong>of</strong>fM, Hu CC, Nguyen MM, “ReviewingRadiographic Images with Patients: A ProspectiveRandomized Controlled Trial on PatientSatisfaction, Understanding, and Preferences,”American Urological Association AnnualMeeting, Washington, DC, <strong>2011</strong>.Leontyev S, Borger M, Trommer C, SubramanianS et al, “Early and Late Outcomes AfterAortic Valve Reconstruction in 127 Patients:A Single-Centre Experience,” Society <strong>of</strong> HeartValve Disease, Barcelona, Spain, June <strong>2011</strong>.Subramanian S, Leontyev S, Borger MA et al,“David vs. Yacoub Valve-Sparing Root Reconstructionin Acute Type A Aortic Dissection,”Houston Aortic Symposium, Houston,Mar <strong>2011</strong>.Tang A, Inaba K, et al, “Penetrating CardiacInjury: A Survivable Injury with a High Post-Discharge Complication Rate,” Oral Presentation,Pacific Coast Surgical Association, Scottsdale,Feb <strong>2011</strong>.Con J, Tang A, et al, “Fall from Ladder—AgeMatters More than Height,” Quick Shot OralPresentation, 7th Annual Academic SurgicalCongress, Las Vegas, Feb <strong>2011</strong>.Tang A, O’Keefe T, Branco B, Snyder K, FennellV, Magno A, Joseph B, Friese R, KulvatunyouN, Wynne J, Lemole M, Rhee P, “Assessment<strong>of</strong> an Intervention Bundle for TraumaticBrain Injury: When Are Intracranial PressureMonitors Necessary?,” American Associationfor the <strong>Surgery</strong> <strong>of</strong> Trauma and ClinicalCongress <strong>of</strong> Acute Care <strong>Surgery</strong>, 70th AnnualMeeting, Chicago, Sep <strong>2011</strong>.Thompson JL, Tucson Medical Center, SymposiumParticipant, 3rd Annual Cardio VascularSymposium, Tucson, Oct <strong>2011</strong>.Waer A, Glazer E, Copeland H, Ong E, SozanskiJ, Doskocil B, Poskus D, Adamas-RappaportWJ, Podium Presentation, “A Comparison<strong>of</strong> Unguided Versus Guided Case-based Instructionon the <strong>Surgery</strong> Clerkship,” Associationfor Surgical Education, Boston, Mar <strong>2011</strong>.Walks NT, Warneke JA, “S<strong>of</strong>t Tissue Zebra:A Case Report <strong>of</strong> an Extraintestinal Malt Lymphoma,”Southwestern Surgical Congress,Honolulu, Apr <strong>2011</strong>.Witte M, Poster Presentation, “K-12 VirtualClinical Research Center and Medical IgnoranceExploratorium,” NIH-NCRR-SEPA ProgramDirectors Conference, Seattle, May <strong>2011</strong>.Witte M, Co-Chair, “New Paradigms for CancerTreatment Based on the Sentinel LymphNode Clinical Trials (Panel Discussion andQ&A),” “Overlap <strong>of</strong> Lymphatic Developmentand Neoplasia: Processes, Pathways, Biomarkers,and Syndromes,” Invited Lecturer: “Overviewand Minisymposium: Sentinel LymphNodes in Breast Cancer Management, Roundtables,Future Perspectives” with Stanley Leong;Fourth International Symposium on CancerMetastasis and the Lymphovascular System:Basis for Rational Therapy, New York,May <strong>2011</strong>.Witte M, “Genetics <strong>of</strong> Lymphedema-AngiodysplasiaSyndromes and Translational Medicine,”<strong>10</strong>th Shanghai International Plastic <strong>Surgery</strong>Conference (SIPSC<strong>2011</strong>) honoring the 50thAnniversary <strong>of</strong> the Shanghai People’s Hospital<strong>Department</strong> <strong>of</strong> Plastic & Reconstructive <strong>Surgery</strong>and 20th Anniversary <strong>of</strong> Operation Smile,Shanghai, China, Jun <strong>2011</strong>.Witte M, Workshop Organizer and Leader:Ignorance <strong>University</strong>: A Parallel <strong>University</strong> for aParallel Universe, 15th International ThinkingConference, Belfast, Ireland, Jun <strong>2011</strong>.Witte M, Invited Opening Lecturer, “Lymphologyand the ISL in the Real, Virtual, and ImaginedWorld <strong>of</strong> the Future,” 23rd InternationalCongress <strong>of</strong> Lymphology, Malmö, Sweden, Sep<strong>2011</strong>.Witte M, Invited Keynote Lecturer: “ ‘Lymphatomics’as a Modern and Integrated Approachfor a Comprehensive Knowledge <strong>of</strong> LymphaticDisorders,” Joint Symposium: “TranslationalLymphology: A Full-Immersion Update,” 21stAnnual Meeting <strong>of</strong> the Mediterranean League <strong>of</strong>Angiology and Vascular <strong>Surgery</strong> (MLAVS),Genoa, Italy, Dec <strong>2011</strong>.Gustafson MR, Chavez L, Wynne JL, JosephB, O’Keeffe T, Kulvatunyou N, Friese R,Tang A, Rhee P, Latifi R, Poster Presentation,“Biologic Mesh in the Repair <strong>of</strong> Complex AbdominalWall Defects in High-Infection-RiskPatients,” 63rd Annual Meeting, SouthwesternSurgical Congress, Honolulu, Apr <strong>2011</strong>.Wynne JL, “Lighting and Electrical Injury—Hidden Damage, Underlying Trauma,” 22ndAnnual Southwest Regional Trauma Conference,Tucson, Aug <strong>2011</strong>.39
<strong>Department</strong> <strong>of</strong> <strong>Surgery</strong>PO Box 245066Tucson AZ 85724-5066NONPROFIT ORGUS POSTAGE PAIDTUCSON AZPERMIT NO. 190To refer a patient or make an appointment, call 520-694-<strong>10</strong>00Visit us online: www.surgery.arizona.edu<strong>Surgery</strong> at the <strong>University</strong> <strong>of</strong> Arizona –Advancing Care, Achieving Cures40