Cultural & EthnicHealth Disparities - Florida Academy of Family ...
Cultural & EthnicHealth Disparities - Florida Academy of Family ...
Cultural & EthnicHealth Disparities - Florida Academy of Family ...
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
OFFICERSPresidentDennis Mayeaux, MD, MiltonPresident-ElectBruce Flareau, MD, ClearwaterVice PresidentGeorge A.W. Smith, MD, PensacolaSecretary-TreasurerAmber Isley, MD, Orange ParkBoard ChairTimothy Davlantes, MD, JacksonvilleDirectorsTERMS EXPIRE 2010Marvin Dewar, MD, GainesvilleJennifer Keehbauch, MD, OrlandoMartha Price, MD, TampaGreg Sloan, MD, ChipleyAnne Waldron, MD, JacksonvilleTERMS EXPIRE 2011Gregg Gutowski, MD, Plant CityIra Pearlstine, MD, Port St. LucieMarc Rivo, MD, Miami BeachChristienne Sain, MD, TallahasseeBernd Wollschlaeger, MD, MiramarTERMS EXPIRE 2012John Gross, MD, St. PetersburgDamani Hosey, MD, MelbourneCoy Irvin, MD, Gulf BreezeRobert Raspa, MD, JacksonvilleCaroline Van Sant-Crowle, MD, Palm HarborEX-OFFICIO DIRECTORS(<strong>Family</strong> Medicine Department Chairs)H. James Brownlee, MD, TampaR. Whit Curry, MD, GainesvilleE. Robert Schwartz, MD, MiamiDaniel J. Van Durme, MD, TallahasseeGeorge Wilson, MD, Jacksonville2009-2010 – RESIDENT DIRECTORSMatt Bruneau, MD, ClearwaterCarol Mancero, MD, OrlandoPetra Townsend, MD, Jacksonville2009-2010 – STUDENT DIRECTORSAnnabella Ferrari (University <strong>of</strong> South <strong>Florida</strong>), TampaMegan Janson (University <strong>of</strong> Miami), Coral GablesDavid Lefkowitz (University <strong>of</strong> <strong>Florida</strong>), GainesvilleAlyson Lewis (<strong>Florida</strong> State University), TallahasseeDELEGATES/ALTERNATE DELEGATESDelegatesAlma Littles, MD, TallahasseeDennis Saver, MD, Vero BeachAlternate DelegatesAmber Isley, MD, Orange BeachNeil Oslos, MD, Daytona Beach<strong>Florida</strong> <strong>Family</strong> PhysicianVolume 58 • Issue 2<strong>Florida</strong> <strong>Family</strong> Physician Writing GuideThe <strong>Florida</strong> <strong>Academy</strong> <strong>of</strong> <strong>Family</strong> Physicians is seeking contributors for its <strong>of</strong>ficial quarterly journal on suchtopics as practice management and physician community involvement, as well as clinical subjects.Articles can contain up to 900 words. Photos <strong>of</strong> authors are requested but are not required. Please providereferences. Photos should be emailed as a JPG file scanned at 400 dpi. If you are unsure, e-mail us whatyou have and we will have our publisher evaluate it. We are also seeking cover photos that may accompanya feature article or simply an interesting photo with a two- or three-sentence description.The editor reserves the right to edit in a reasonable manner for grammar, spelling and punctuation. If thereare any questions regarding content or if any major changes are necessary, the editor will contact the author.If you have questions, please contact Christine Fisher, Managing Editor, cpf1219@aol.com.2010 Editorial Calendar<strong>Florida</strong> <strong>Academy</strong> <strong>of</strong> <strong>Family</strong> Physicians6720 Atlantic Boulevard • Jacksonville, <strong>Florida</strong> 32211-8730(904) 726-0944 • (800) 223-3237 • Fax (904) 726-0923 • www.fafp.orgFAFP Staff:Tad P. Fisher, Executive Vice PresidentCamille Adams, Director <strong>of</strong> CME Programs and Exhibits (camille@fafp.org)Mary Jo Griseuk, Director <strong>of</strong> Membership Development (maryjo@fafp.org)Joyce Lowe, Comptroller & Executive Assistant to the EVP (joyce@fafp.org)Annelle McClean, Director <strong>of</strong> Meeting Planning& Director <strong>of</strong> Resident & Student Relations (amcclean@fafp.org)Kathy Short, Administrative Assistant (kathy@fafp.org)FAFP Consultants:Ed Shahady, MD, Director <strong>of</strong> Centers <strong>of</strong> Office Practice Excellence (eshahady@att.net)Jim Daughton, Metz, Husband & Daughton, Legislative Consultant (jim.daughton@metzlaw.com)Christine P. Fisher, Director <strong>of</strong> Public Affairs (cpf1219@aol.com)Fernando Senra, Moore Consulting Group, Communications Consultants (fernandos@moore-pr.com)<strong>Florida</strong> <strong>Family</strong> Physician is printed on recycled paper with soy-based inks.The opinions expressed in this publication are not necessarily those <strong>of</strong> the <strong>Florida</strong> <strong>Academy</strong> <strong>of</strong> <strong>Family</strong> Physicians.Spring issue (March) copy due to FAFP by January 29, 2010Summer issue (June) copy due to FAFP by April 30, 2010Fall issue (September) due to FAFP by July 30, 2010The spring issue theme is “Patient-Centered Medical Home.” If you would like to submitan article to <strong>Florida</strong> <strong>Family</strong> Physician, please contact Managing Editor Christine P. Fisher,cpf1219@aol.com. Letters to the editor are accepted.Published December 2009FAFP FOUNDATION OFFICERSPresidentDaniel B. Lestage, MD, Orange ParkVice PresidentDennis Saver, MD, Vero BeachTad P. FisherExecutive EditorDavid Feller, MDCommunications Chair &Editor, GainesvilleChristine P. FisherManaging EditorEditorial BoardJan Larson, MDGuest EditorTanya Anim, FSU COMGuest EditorCarolyn MayeauxGuest EditorCorrection: Fall 2009 IssueIn the article “Low-IncomeSeniors” (page 27), the figurein the fifth paragraph shouldread “annual incomes below$21,855.” We apologize forthis error.<strong>Florida</strong> <strong>Family</strong> Physician 3
ContentsFeaturesPrimary Care Strategies for Reducing<strong>Disparities</strong> in Birth Outcomes .. . . . . . . . . . . . . . . . . . . . . . . . . . . . 16Closing the Gap.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18<strong>Cultural</strong> Diversity: The Attitude TowardAging and Elderly Care.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 22Old People & Loving Relationships. . . . . . . . . . . . . . . . . . . . . . . . 24<strong>Cultural</strong> Issues in Substance-AbuseEvaluation and Treatment.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26Training Medical Students to Recognize& Address Health <strong>Disparities</strong> .. . . . . . . . . . . . . . . . . . . . . . . . . . . . 28Chronic Kidney Disease Is a <strong>Family</strong> Affair. . . . . . . . . . . . . . . . . . . 30Extras103rd <strong>Family</strong> Medicine Weekend .. . . . . . . . . . . . . . . . . . . . . . . . . . 9Money Sense: Keep Your Retirement Savings on Track. . . . . . . . . 21Departments<strong>Family</strong> Medicine in the News. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6Your FAFP Foundation at Work.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10Calendar <strong>of</strong> Events. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15<strong>Florida</strong> <strong>Family</strong> Physician is published by Innovative Publishing Ink.10629 Henning Way, Suite 8 • Louisville, Kentucky 40241 • Phone 502.423.7272 • Fax 502.423.7979Innovative Publishing Ink specializes in creating custom magazines for associations. Please direct all inquiries to Aran Jackson, ajackson@ipipublishing.com.<strong>Florida</strong> <strong>Family</strong> Physician 5
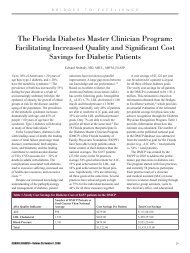
F a m i l y M e d i c i n e i n T H E N E W SPeter Rippey, MD, a second-year resident at Halifax Hospital,was named the AAFP alternate delegate representative to theAmerican Medical Association-Resident Fellow Section (AMA-RFS). He attended the AMA House <strong>of</strong> Delegates meeting inHouston in November.Alyson Lewis, FSU College <strong>of</strong> Medicine student director, hasbeen appointed by the AAFP as a <strong>Family</strong> Medicine InterestGroup regional coordinator.Carrie Jantti (Southern <strong>Family</strong> Healthcare), Debbie Schaubhut, MA, and GregSloan, MD (<strong>Family</strong> Care Associates <strong>of</strong> NW <strong>Florida</strong>)George “Scottie” Whiddon, MD, and SandyBaker, EMTDrs. Scottie Whiddon(Tallahassee) and GregSloan (Chipley) havebeen recognized bythe FAFP FoundationDiabetes Master ClinicianProgram as DiabetesMaster Clinicians, andtheir <strong>of</strong>fices have beendesignated as DiabetesCenters <strong>of</strong> Excellence.This recognition indicatesthat they have participatedin the programfor at least one year andhave demonstrated a significantincrease in thenumber <strong>of</strong> patients who are achieving evidence-based goals. Theirdedication and that <strong>of</strong> their <strong>of</strong>fice staffs have decreased the suffering<strong>of</strong> their patients and have contributed to decreased cost <strong>of</strong>diabetes. During the past year, the 84 <strong>of</strong>fices that participate in theDiabetes Master Clinician Program have created a $3.5 millionsavings for their patients. Well done!<strong>Florida</strong> <strong>Family</strong> PhysicianO ficial Publication <strong>of</strong> the <strong>Florida</strong> <strong>Academy</strong> <strong>of</strong> <strong>Family</strong> Physicians Winter 2009In This Issue<strong>Cultural</strong> & <strong>EthnicHealth</strong> <strong>Disparities</strong>To be successful in any organization,you need the right kind <strong>of</strong> help. Let ushelp you create a quality publicationthat your association can be proud <strong>of</strong>.To find out how your association canhave its own effective magazine,contact Aran Jackson at 502.423.7272or ajackson@ipipublishing.com.www.ipipublishing.com6
Rx ONLYBRIEF SUMMARY. Please see package insert forprescribing information.INDICATIONS AND USAGELEVEMIR is indicated for once- or twice-daily subcutaneousadministration for the treatment <strong>of</strong> adult and pediatric patientswith type 1 diabetes mellitus or adult patients with type 2diabetes mellitus who require basal (long acting) insulin for thecontrol <strong>of</strong> hyperglycemia.CONTRAINDICATIONSLEVEMIR is contraindicated in patients hypersensitive to insulindetemir or one <strong>of</strong> its excipients.WARNINGSHypoglycemia is the most common adverse effect <strong>of</strong>insulin therapy, including LEVEMIR. As with all insulins,the timing <strong>of</strong> hypoglycemia may differ among variousinsulin formulations.Glucose monitoring is recommended for all patientswith diabetes.LEVEMIR is not to be used in insulin infusion pumps.Any change <strong>of</strong> insulin dose should be made cautiouslyand only under medical supervision. Changes in insulinstrength, timing <strong>of</strong> dosing, manufacturer, type (e.g., regular,NPH, or insulin analogs), species (animal, human), ormethod <strong>of</strong> manufacture (rDNA versus animal-source insulin)may result in the need for a change in dosage. Concomitantoral antidiabetic treatment may need to be adjusted.PRECAUTIONSGeneralInadequate dosing or discontinuation <strong>of</strong> treatment may lead tohyperglycemia and, in patients with type 1 diabetes, diabeticketoacidosis. The first symptoms <strong>of</strong> hyperglycemia usually occurgradually over a period <strong>of</strong> hours or days. They include nausea,vomiting, drowsiness, flushed dry skin, dry mouth, increasedurination, thirst and loss <strong>of</strong> appetite as well as acetone breath.Untreated hyperglycemic events are potentially fatal.LEVEMIR is not intended for intravenous or intramuscularadministration. The prolonged duration <strong>of</strong> activity <strong>of</strong> insulindetemir is dependent on injection into subcutaneous tissue.Intravenous administration <strong>of</strong> the usual subcutaneousdose could result in severe hypoglycemia. Absorption afterintramuscular administration is both faster and more extensivethan absorption after subcutaneous administration.LEVEMIR should not be diluted or mixed with any otherinsulin preparations (see PRECAUTIONS, Mixing <strong>of</strong> Insulins).Insulin may cause sodium retention and edema, particularly ifpreviously poor metabolic control is improved by intensifiedinsulin therapy.Lipodystrophy and hypersensitivity are among potential clinicaladverse effects associated with the use <strong>of</strong> all insulins.As with all insulin preparations, the time course <strong>of</strong> LEVEMIRaction may vary in different individuals or at different times inthe same individual and is dependent on site <strong>of</strong> injection, bloodsupply, temperature, and physical activity.Adjustment <strong>of</strong> dosage <strong>of</strong> any insulin may be necessary if patientschange their physical activity or their usual meal plan.HypoglycemiaAs with all insulin preparations, hypoglycemic reactions may beassociated with the administration <strong>of</strong> LEVEMIR. Hypoglycemiais the most common adverse effect <strong>of</strong> insulins. Early warningsymptoms <strong>of</strong> hypoglycemia may be different or less pronouncedunder certain conditions, such as long duration <strong>of</strong> diabetes,diabetic nerve disease, use <strong>of</strong> medications such as beta-blockers,or intensified diabetes control (see PRECAUTIONS, DrugInteractions). Such situations may result in severe hypoglycemia(and, possibly, loss <strong>of</strong> consciousness) prior to patients’ awareness<strong>of</strong> hypoglycemia.The time <strong>of</strong> occurrence <strong>of</strong> hypoglycemia depends on the actionpr<strong>of</strong>ile <strong>of</strong> the insulins used and may, therefore, change when thetreatment regimen or timing <strong>of</strong> dosing is changed. In patientsbeing switched from other intermediate or long-acting insulinpreparations to once- or twice-daily LEVEMIR, dosages can beprescribed on a unit-to-unit basis; however, as with all insulinpreparations, dose and timing <strong>of</strong> administration may need to beadjusted to reduce the risk <strong>of</strong> hypoglycemia.Renal ImpairmentAs with other insulins, the requirements for LEVEMIR may needto be adjusted in patients with renal impairment.Hepatic ImpairmentAs with other insulins, the requirements for LEVEMIR may needto be adjusted in patients with hepatic impairment.Injection Site and Allergic ReactionsAs with any insulin therapy, lipodystrophy may occur at theinjection site and delay insulin absorption. Other injection sitereactions with insulin therapy may include redness, pain, itching,hives, swelling, and inflammation. Continuous rotation <strong>of</strong> theinjection site within a given area may help to reduce or preventthese reactions. Reactions usually resolve in a few days to a fewweeks. On rare occasions, injection site reactions may requirediscontinuation <strong>of</strong> LEVEMIR.In some instances, these reactions may be related to factorsother than insulin, such as irritants in a skin cleansing agent orpoor injection technique.Systemic allergy: Generalized allergy to insulin, which is lesscommon but potentially more serious, may cause rash (includingpruritus) over the whole body, shortness <strong>of</strong> breath, wheezing,reduction in blood pressure, rapid pulse, or sweating. Severecases <strong>of</strong> generalized allergy, including anaphylactic reaction, maybe life-threatening.Intercurrent ConditionsInsulin requirements may be altered during intercurrentconditions such as illness, emotional disturbances, or otherstresses.Information for PatientsLEVEMIR must only be used if the solution appears clear andcolorless with no visible particles. Patients should be informedabout potential risks and advantages <strong>of</strong> LEVEMIR therapy,including the possible side effects. Patients should be <strong>of</strong>feredcontinued education and advice on insulin therapies, injectiontechnique, life-style management, regular glucose monitoring,periodic glycosylated hemoglobin testing, recognition andmanagement <strong>of</strong> hypo- and hyperglycemia, adherence to mealplanning, complications <strong>of</strong> insulin therapy, timing <strong>of</strong> dosage,instruction for use <strong>of</strong> injection devices and proper storage <strong>of</strong>insulin. Patients should be informed that frequent, patientperformedblood glucose measurements are needed to achieveeffective glycemic control to avoid both hyperglycemia andhypoglycemia. Patients must be instructed on handling <strong>of</strong>special situations such as intercurrent conditions (illness, stress,or emotional disturbances), an inadequate or skipped insulindose, inadvertent administration <strong>of</strong> an increased insulin dose,inadequate food intake, or skipped meals. Refer patients to theLEVEMIR “Patient Information” circular for additional information.As with all patients who have diabetes, the ability to concentrate and/orreact may be impaired as a result <strong>of</strong> hypoglycemia or hyperglycemia.Patients with diabetes should be advised to inform their healthcare pr<strong>of</strong>essional if they are pregnant or are contemplatingpregnancy (see PRECAUTIONS, Pregnancy).Laboratory TestsAs with all insulin therapy, the therapeutic response to LEVEMIRshould be monitored by periodic blood glucose tests. Periodicmeasurement <strong>of</strong> HbA 1cis recommended for the monitoring <strong>of</strong>long-term glycemic control.Drug InteractionsA number <strong>of</strong> substances affect glucose metabolism and may requireinsulin dose adjustment and particularly close monitoring.The following are examples <strong>of</strong> substances that may reducethe blood-glucose-lowering effect <strong>of</strong> insulin: corticosteroids,danazol, diuretics, sympathomimetic agents (e.g., epinephrine,albuterol, terbutaline), isoniazid, phenothiazine derivatives,somatropin, thyroid hormones, estrogens, progestogens(e.g., in oral contraceptives).The following are examples <strong>of</strong> substances that may increasethe blood-glucose-lowering effect <strong>of</strong> insulin and susceptibilityto hypoglycemia: oral antidiabetic drugs, ACE inhibitors,disopyramide, fibrates, fluoxetine, MAO inhibitors, propoxyphene,salicylates, somatostatin analog (e.g., octreotide), andsulfonamide antibiotics.Beta-blockers, clonidine, lithium salts, and alcohol may eitherpotentiate or weaken the blood-glucose-lowering effect <strong>of</strong>insulin. Pentamidine may cause hypoglycemia, which maysometimes be followed by hyperglycemia. In addition, underthe influence <strong>of</strong> sympatholytic medicinal products such asbeta-blockers, clonidine, guanethidine, and reserpine, the signs<strong>of</strong> hypoglycemia may be reduced or absent.The results <strong>of</strong> in-vitro and in-vivo protein binding studiesdemonstrate that there is no clinically relevant interaction betweeninsulin detemir and fatty acids or other protein bound drugs.Mixing <strong>of</strong> InsulinsIf LEVEMIR is mixed with other insulin preparations, the pr<strong>of</strong>ile<strong>of</strong> action <strong>of</strong> one or both individual components may change.Mixing LEVEMIR with insulin aspart, a rapid acting insulinanalog, resulted in about 40% reduction in AUC (0-2h)and C maxfor insulin aspart compared to separate injections when theratio <strong>of</strong> insulin aspart to LEVEMIR was less than 50%.LEVEMIR should NOT be mixed or diluted with any otherinsulin preparations.Carcinogenicity, Mutagenicity, Impairment <strong>of</strong> FertilityStandard 2-year carcinogenicity studies in animals have notbeen performed. Insulin detemir tested negative for genotoxicpotential in the in-vitro reverse mutation study in bacteria,human peripheral blood lymphocyte chromosome aberrationtest, and the in-vivo mouse micronucleus test.Pregnancy: Teratogenic Effects: Pregnancy Category CIn a fertility and embryonic development study, insulin detemirwas administered to female rats before mating, during mating,and throughout pregnancy at doses up to 300 nmol/kg/day(3 times the recommended human dose, based on plasma AreaUnder the Curve (AUC) ratio). Doses <strong>of</strong> 150 and 300 nmol/kg/dayproduced numbers <strong>of</strong> litters with visceral anomalies. Doses up to900 nmol/kg/day (approximately 135 times the recommendedhuman dose based on AUC ratio) were given to rabbits duringorganogenesis. Drug-dose related increases in the incidence <strong>of</strong>fetuses with gall bladder abnormalities such as small, bilobed,bifurcated and missing gall bladders were observed at a dose <strong>of</strong>900 nmol/kg/day. The rat and rabbit embry<strong>of</strong>etal developmentstudies that included concurrent human insulin control groupsindicated that insulin detemir and human insulin had similareffects regarding embryotoxicity and teratogenicity.Nursing mothersIt is unknown whether LEVEMIR is excreted in significantamounts in human milk. For this reason, caution shouldbe exercised when LEVEMIR is administered to a nursingmother. Patients with diabetes who are lactating may requireadjustments in insulin dose, meal plan, or both.Pediatric useIn a controlled clinical study, HbA 1cconcentrations and rates <strong>of</strong>hypoglycemia were similar among patients treated with LEVEMIRand patients treated with NPH human insulin.Geriatric useOf the total number <strong>of</strong> subjects in intermediate and long-termclinical studies <strong>of</strong> LEVEMIR, 85 (type 1 studies) and 363 (type 2studies) were 65 years and older. No overall differences insafety or effectiveness were observed between these subjectsand younger subjects, and other reported clinical experiencehas not identified differences in responses between theelderly and younger patients, but greater sensitivity <strong>of</strong> someolder individuals cannot be ruled out. In elderly patients withdiabetes, the initial dosing, dose increments, and maintenancedosage should be conservative to avoid hypoglycemic reactions.Hypoglycemia may be difficult to recognize in the elderly.ADVERSE REACTIONSAdverse events commonly associated with human insulintherapy include the following:Body as Whole: allergic reactions (see PRECAUTIONS, Allergy).Skin and Appendages: lipodystrophy, pruritus, rash. Mildinjection site reactions occurred more frequently with LEVEMIRthan with NPH human insulin and usually resolved in a few daysto a few weeks (see PRECAUTIONS, Allergy).Other:Hypoglycemia: (see WARNINGS and PRECAUTIONS).In trials <strong>of</strong> up to 6 months duration in patients with type 1 andtype 2 diabetes, the incidence <strong>of</strong> severe hypoglycemia withLEVEMIR was comparable to the incidence with NPH, and, asexpected, greater overall in patients with type 1 diabetes (Table 4).Weight gain:In trials <strong>of</strong> up to 6 months duration in patients with type 1and type 2 diabetes, LEVEMIR was associated with somewhatless weight gain than NPH (Table 4). Whether these observeddifferences represent true differences in the effects <strong>of</strong> LEVEMIRand NPH insulin is not known, since these trials were notblinded and the protocols (e.g., diet and exercise instructionsand monitoring) were not specifically directed at exploringhypotheses related to weight effects <strong>of</strong> the treatmentscompared. The clinical significance <strong>of</strong> the observed differenceshas not been established.Table 4: Safety Information on Clinical StudiesWeight (kg) Hypoglycemia(events/subject/month)Treatment # <strong>of</strong> Baseline End <strong>of</strong> Major* Minor**subjectstreatmentType 1Study A LEVEMIR N=276 75.0 75.1 0.045 2.184NPH N=133 75.7 76.4 0.035 3.063Study C LEVEMIR N=492 76.5 76.3 0.029 2.397NPH N=257 76.1 76.5 0.027 2.564Study D LEVEMIR N=232 N/A N/A 0.076 2.677Pediatric NPH N=115 N/A N/A 0.083 3.203Type 2Study E LEVEMIR N=237 82.7 83.7 0.001 0.306NPH N=239 82.4 85.2 0.006 0.595Study F LEVEMIR N=195 81.8 82.3 0.003 0.193NPH N=200 79.6 80.9 0.006 0.235* Major = requires assistance <strong>of</strong> another individual because <strong>of</strong> neurologicimpairment** Minor = plasma glucose
103rd <strong>Family</strong> Medicine WeekendBuena Vista Palace, Lake Buena VistaNovember 13-15, 2009Meeting <strong>of</strong> FAFP and <strong>Florida</strong> <strong>Academy</strong> <strong>of</strong> Physician Assistants leadershipDermatology workshopTad Fisher, EVP; Sen. Durrell Peaden, MD; Alma Littles, MDMeeting Chair Dr. Amber IsleyMeeting Chair Dr. Sandra ArgenioDrs. Dennis Mayeaux and Dave Feller<strong>Florida</strong> <strong>Family</strong> Physician 9
Y O U R F A F P F O U N D A T I O N A T W O R KLessons Learned from the DiabetesMaster Clinician ProgramRecognizing and Overcoming <strong>Disparities</strong> in Diabetes-Care Challenges for the Primary Care Office Teamby Edward Shahady, MD, Medical Director, Diabetes Master Clinician Program, <strong>Florida</strong> <strong>Academy</strong> <strong>of</strong> <strong>Family</strong>Physicians Foundation“Diabetes is the most demanding chronic illness. It challenges every fiber <strong>of</strong> a patient’s bodyand spirit and demands a system <strong>of</strong> care that ministers to the biological, social and psychologicalaspects <strong>of</strong> the illness. It takes a ‘village’ to accomplish this task.” 1AbstractDiabetes is the poster child for chronic disease. It is common, costly,has well-accepted national standards for care, cost-effective treatmentchoices are available, and excellent evidence exists that treatmentreduces cost, complications and suffering. Unfortunately, despiteour knowledge <strong>of</strong> how to decrease mortality and morbidity, less than50 percent <strong>of</strong> diabetic patients are at goal for the national standards.One <strong>of</strong> the common issues cited for the gap between knowledge andperformance is disparities in care for ethnic minorities. <strong>Disparities</strong>are complex issues that are usually discussed from a perspective <strong>of</strong>cultural differences and the ability <strong>of</strong> clinicians to be competent indealing with the cultural differences. But little is discussed about the“inertia” within a primary care <strong>of</strong>fice that may impede dealing withdisparities in diabetes care. This article will share the experiencesgained from the FAFPF Diabetes Master Clinician Program duringthe last six years. Questions that will be addressed include: What isthe impact <strong>of</strong> disparities in diabetes care? What causes disparities?How do <strong>of</strong>fice staff members and clinicians feel about disparities?How does an <strong>of</strong>fice team address disparities? What are someexamples <strong>of</strong> how <strong>of</strong>fice teams addressed disparities and enhancedachievement <strong>of</strong> diabetes standards?What Is the Impact <strong>of</strong><strong>Disparities</strong> in Diabetes Care?Diabetes is one <strong>of</strong> the most common chronic diseases seen in the primarycare setting. In the United States, 10.7 percent <strong>of</strong> the populationage 20 or older and 23.1 percent <strong>of</strong> those 60 or older have diabetes. 2Significant cost and suffering is associated with diabetes. It is the sixthleading cause <strong>of</strong> death; the leading cause <strong>of</strong> end-stage renal disease,non-traumatic limb amputations and blindness; and the leading contributorto cardiovascular disease. Diabetics over age 60 are threetimes more likely to be unable to walk one-quarter <strong>of</strong> a mile, climbstairs or do housework. 2The annual cost <strong>of</strong> diabetes is $174 million. A total <strong>of</strong> $30 million <strong>of</strong>that cost is a direct burden to the patient in the form <strong>of</strong> absenteeismand presenteeism (at work but decreased productivity). 3Minority populations have an increased number <strong>of</strong> complicationscompared to non-Hispanic white Americans. Retinopathy is 46 percenthigher in blacks and 84 percent higher in Mexican-Americans.The retinopathy was more severe and the A1C level was higher in theblacks and Mexican-Americans in this study. 4 From 2001 to 2006, 58percent <strong>of</strong> white patients achieved an A1C < 7, compared to 41 percentfor black and 38 percent for U.S.-born Hispanic patients. 5 Deathrates per 100,000 are higher in minority populations. 6What Causes <strong>Disparities</strong>?Common reasons listed include: inability to pay for medication andsupplies, depression, lack <strong>of</strong> transportation, access to care, health literacy,preferred food choices, cultural values religious beliefs, lack <strong>of</strong>trust in their clinician and clinician inertia. 7, 8 But if we talk to patients,they may use a different set <strong>of</strong> words to describe the reasons why theyare not reaching their goals. Their words are what they are feelingand provide the foundation for understanding what keeps them fromreaching goals. The following are statements obtained from telephoneinterviews with patients in our diabetes registry 9 who had an averageHbA1c <strong>of</strong> 8 percent or higher.“I do not feel like I have been educated about diabetes. I am not surewhich symptoms are associated with diabetes and which ones are not.”“I am a stress-eater and a comfort-eater. I have a hard time eating theright foods. I feel frustrated because even when I try to eat right andcontrol my blood sugar, it is uncontrollable and doctors can’t seem toexplain why.”10
“I feel like I have good control <strong>of</strong> my diabetes. (HbA1c is 11.1) I amaware <strong>of</strong> diabetes complications but try not to focus on them.”“I quit taking Lipitor because it made my vision worse. I am almostblind. Once my vision improves, I will try another cholesterol medication.I hope to see an eye doctor soon.”“My doctor has never talked to me about depression, but I see a psychiatristfor mental illness.”“It doesn’t do any good to worry about my diabetes because I can’tdo anything about it.”“I am having trouble affording most <strong>of</strong> my diabetes care supplies. Iborrow test strips from a neighbor. No one has spoken to me aboutdepression but I have issues with it.”“My biggest challenge is keeping my sugar leveled <strong>of</strong>f. Getting motivatedto eat properly and exercise is hard. Trying to stay on a diet ishard. My sugar goes up and down.”“It is hard to schedule time to take my insulin during the day.Sometimes it’s hard to find foods to eat when I am hungry that won’tmake my sugar go high.”“I now take insulin but don’t do it right and forget to take it sometimes.I have breast cancer and take lots <strong>of</strong> medicine and get depressed withit all.”“I am not exercising because <strong>of</strong> back pain and swollen ankles. Wantto start walking when these issues go away.”“I don’t think my doctor and nurse like me, and I don’t reallylike them.”How Do Office Staff Membersand Clinicians Feel About <strong>Disparities</strong>?Each one <strong>of</strong> the above patient statements produces differentresponses from clinicians and <strong>of</strong>fice staff members. A commonresponse is: “this is a non-compliant patient, and little can bedone.” But what is the value <strong>of</strong> this label? “Non-compliant” isa dysfunctional term. 10 It places blame on the patient and doesnot facilitate consideration <strong>of</strong> other causes and solutions. It isa term that reflects the frustration that health care providershave when, despite all their efforts, the patient is not at goal.Other responses seek a way to discover presence <strong>of</strong> other issues.Is the patient depressed? Is there a problem with health literacy?Is there a breakdown in our system <strong>of</strong> communication or accessto care in our <strong>of</strong>fice? Are their social or cultural issues that wemight address?Shifting medical culture (physician thinking) and consideringsystems <strong>of</strong> care as the cause rather than blaming produces a lessdefensive posture and facilitates finding solutions. 11 Ability topay, transportation, insurance hassles, access to care and communicationsystems with the physician’s <strong>of</strong>fice are all systemsissues that impact ability to reach goals. Not all system issues canbe resolved in the physician’s <strong>of</strong>fice, but a model that routinelyasks about system issues, rather than routinely blaming, eitherverbally or non-verbally creates a more trusting atmosphere.Depression is present in 66 percent <strong>of</strong> diabetics, and 20 percenthave major depression. If the depression is not treated, the diabeteswill never improve. 12 Depression screening with a few simplequestions (especially for patients not at goal) aids identification<strong>of</strong> patients with depression. The warmth and attitude <strong>of</strong> the personasking the questions influences how the patient will answerdepression-screening questions.<strong>Cultural</strong> issues are not always appreciated if the clinician is froma different culture or ethnic group. The spiritual value <strong>of</strong> foodis a good example. Asking a patient not to eat a certain type <strong>of</strong>food may be perceived as more harmful than helpful. Patients have<strong>Florida</strong> <strong>Family</strong> Physician 11
a stronger relationship with physicians when they see themselves assimilar in personal beliefs, values and communication. If they sensesimilarity, there is a higher rating <strong>of</strong> trust, satisfaction and intentionto adhere. Race is the primary predictor <strong>of</strong> similarity, but use <strong>of</strong>patient-centered communication was also a significant predictor. 13Decreased health literacy is another powerful predictor <strong>of</strong>disparities and inability to reach diabetes goals. The NationalAssessment <strong>of</strong> Adult Literacy accessed literacy in three areas. 15The areas were defined as prose, document and quantitative literacy.Prose and document literacy were defined as the knowledgeand skills needed to search, comprehend and use information inbrochures, instructional materials, job applications, payroll formsand drug and food labels. Quantitative literacy or numeracy isdefined as the knowledge and skills needed to identify and usenumbers in the performance <strong>of</strong> daily activities. The survey indicatedthat 36 percent <strong>of</strong> adults have difficulty with most health literacytasks, and 59 percent <strong>of</strong> the over-65 group have below-basicliteracy skills. Blacks and Hispanics had lower literacy skills thanwhites and Asians. Quantitative or numeracy skills were belowbasic in 61 percent <strong>of</strong> the population. 15 The ability to use numbers(numeracy) may be an overlooked factor in understanding racialdisparities in glycemic control. A recent study 16 reviewed disparitiesin diabetic patients and found that lack <strong>of</strong> numeracy was morepredictive <strong>of</strong> poor glycemic control than race. Low diabetes-relatednumeracy, not African-American race, was significantly relatedto poor glycemic control. Interventions that address numeracycould help to reduce racial disparities in diabetes.How Does an Office TeamAddress <strong>Disparities</strong>?One <strong>of</strong> the major ways an <strong>of</strong>fice team can address disparitiesis through sharing patient-friendly reports that define goals,reasons for achieving the goals and level <strong>of</strong> goal achievementfor the patient. Table 1 is a sample <strong>of</strong> the patient report cardthat is generated by the diabetes registry <strong>of</strong> the <strong>Academy</strong>/Foundations Diabetes Master Clinician Program. This reportcard is given to the patient at each diabetic visit by the nurseor medical assistant before he or she is seen by the physician.The nurse or medical assistant may provide a brief explanation<strong>of</strong> the items. The physician will follow up with more extensiveself-management education using the report card to help focusthe patient. The patient takes the report card home with him orher and uses it as a guide to future care.Table 1Examples <strong>of</strong> How Office Teams Addressed <strong>Disparities</strong> andEnhanced Achievement <strong>of</strong> Diabetes StandardsAge 63 Male MR # 33749GoalNovember2009August2009Weight 235 240B/P Less than 130/80 125/80 148/88Best 120/80TestsHbA1c(sugar for 3 months)Less than 100Best if 67.0 8.5LDL(lousy cholesterol)HDL(happy cholesterol)Triglycerides(a bad fatty substance)MedicationAspirin(prevents heart attacks)ImportantYearlyActivitiesEye Check(to preventblindness)Foot Check(to check forsores andnumbness)Urine MicroAlbumin(to check forkidney failure)Flu Shot(to prevent flu)Pneumovax(to preventspecialpneumonia)SmokingStatus-SmokerLess than 100 170 165Best if 70Greater than 40 37 35Goal Status Next TestDue1 time a year Overdue1 time a year 8/22/20101 time a year 8/22/20101 time a year OverdueOnce inlifetime2 times iffirst givenbefore age 65Smoking ishazardous toyour healthLess than 150 150 250Take daily Yes YesFirst onecompletedMostRecentTest12
Table 2 is an example <strong>of</strong> how one <strong>of</strong>fice team addressed disparitiesand was able to demonstrate an increase in number <strong>of</strong> patients thatachieved diabetes goals. The strategies they used were relativelysimple. The members <strong>of</strong> the team, which included the physician, front<strong>of</strong>fice staff members and medical assistants, met to discuss how theycould improve their numbers. They developed policies for completingmissing items. The medical assistants were taught how to explain theneed for achieving the missing items on the report card, perform themon<strong>of</strong>ilament foot exam, order needed tests, and provide immunizationsif needed. The policy was part <strong>of</strong> the <strong>of</strong>fice protocol, and thephysician signed <strong>of</strong>f on all activities <strong>of</strong> the medical assistant.Table 2Change in One Practice Over an Eight-Month Period (Percentage<strong>of</strong> 140 Patients Reaching Some <strong>of</strong> the Goals Noted in AboveReport Card)February 12, 2007 October 12, 2008Eye Check 2% 59%Foot Check 10% 82%Urine Micro Albumin 6% 63%Pneumovax 32% 76%Flu Shot 1% 66%Daily Aspirin 45% 65%Table 3 is an example <strong>of</strong> how a rural practice in Quincy, <strong>Florida</strong>,made significant changes over a six-year period <strong>of</strong> time in 400 diabeticpatients. Quincy is located in a county that has large number<strong>of</strong> ethnic minorities.Table 3Changes Over Six Years in One Practice (400 Diabetic Patients)November 2003 November 2009A1C 51% 60%LDL 45% 61%B/P 38% 55%All 3 at the same time 10% 26%These changes were the result <strong>of</strong> a dedicated family physician and his<strong>of</strong>fice assistant. They made maximum use <strong>of</strong> the diabetes registry andalso conducted group visits for several <strong>of</strong> their patients.Summary<strong>Disparities</strong> in diabetes can be addressed by recognizing the causesand developing the solutions in concert with the members <strong>of</strong> the<strong>of</strong>fice team. The ability <strong>of</strong> the patient to use numbers in their dailyactivities is a major issue in diabetes. Providing the patient-centeredcare and user-friendly information to address numeracy and otherissues may decrease many <strong>of</strong> the disparities that exist in diabetes care.Empowering medical assistants to give patients diabetes report cardsis a proven method <strong>of</strong> helping patients overcome disparities. TheDiabetes Master Clinician Program <strong>of</strong> the <strong>Florida</strong> <strong>Academy</strong> <strong>of</strong> <strong>Family</strong>Physicians Foundation provides the tools for a <strong>Family</strong> Physicians<strong>of</strong>fice to overcome disparities in diabetes care.References1 Shahady EJ, Barriers to Effective Diabetes Care: How to recognize and overcome.Consultant 2009; 49:493-96.2 CDC Diabetes Fact Sheet; accessed online November 2, 2010. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf.3 Economic Costs <strong>of</strong> Diabetes in the U.S. in 2007-American DiabetesAssociation. Diabetes Care. 2008;31:1-20.4 Harris MI, Klein R, Cowie CC, Rowland M, Byrd-Holt DD. Is the risk <strong>of</strong> diabeticretinopathy greater in non-Hispanic blacks and Mexican Americans thanin non-Hispanic whites with type 2 diabetes? A U.S. population study. DiabetesCare. 1998;21(8):1230-1235.5 McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control<strong>of</strong> cardiovascular disease and diabetes by race, ethnicity, and education: U.S.trends from 1999 to 2006 and effects <strong>of</strong> Medicare coverage. Ann Intern Med.2009;150(8):505-515.6 Centers for Disease Control, National Center for Health Statistics. Mortalitytables. National Center for Health Statistics. 2009; http://www.cdc.gov/nchs/datawh/statab/unpubd/mortabs.htm. Accessed November 3, 2009.7 Shahady EJ, Barriers to care in Chronic Disease: How to bridge theTreatment Gap. Consultant 2006;46 (10):1149-1152.8 Grant RW, Cagliero E, Dubey AK, Gildesgame C, Chueh HC, Barry MJ,Singer DE, Nathan DM, Meigs JB. Clinical inertia in the management <strong>of</strong> Type2 diabetes metabolic risk factors. Diabet Med. 2004;21:150-155.9 Shahady EJ, The <strong>Florida</strong> Diabetes Master Clinician Program: FacilitatingIncreased Quality and Significant Cost Savings for Diabetic Patients, ClinDiabetes 2008 26: 29-33.10 Anderson RM, Funnell MM. Compliance and adherence are dysfunctionalconcepts in diabetes care. Diabetes Educ. 2000;26:597-604.11 Crossing the Quality Chasm, Institute <strong>of</strong> Medicine National <strong>Academy</strong>Press 2001.12 Gonzalez J, Peyrot M, McCarl L et al Depression and Diabetes TreatmentNonadherence: A Meta-Analysis. Diabetes Care 2008;31:2383-2390.13 Street RL, O’Malley KJ, Cooper LA, Haidet P Understanding Concordancein Patient-Physician Relationships: Personal and Ethnic Dimensions <strong>of</strong> SharedIdentity Ann Fam Med 2008;6:198-205.14 Literacy in Everyday Life Results from the 2003 National Assessment <strong>of</strong>Adult Literacy; accessed online.15 Kutner M, Greenberg E, JinY, Boyle B, HsuY, Dunleavy, E. (2007). Literacyin Everyday Life: Results From the 2003 National Assessment <strong>of</strong> Adult Literacy(NCES 2007-480). U.S. Department <strong>of</strong> Education Washington, D.C.: NationalCenter for Education Statistics (available online at no charge).16 Osborn CY et al Diabetes Numeracy: An overlooked factor in understandingracial disparities in glycemic control. Diabetes Care 2009;32:1614-1619.<strong>Florida</strong> <strong>Family</strong> Physician 13
C A L E N D A R O F E V E N T SHealth Awareness EventsJanuaryThyroid Awareness Monthwww.aace.comNational Birth Defects Prevention Monthwww.nbdpn.orgCervical Health Awareness Monthwww.nccc-online.org/awareness.htmlGlaucoma Awareness Monthpreventblindness.org/news/observe.htmlFebruaryAmerican Heart Monthwww.americanheart.orgNational Wise Health Consumer Monthwww.aipm.net/wiseNational Children’s Dental Health Monthwww.ada.org/pr<strong>of</strong>/events/featured/ncdhm.aspNational Donor Daywww.organdonor.gov/get_involved/nationaldonorday.htmMarchNational Nutrition Month ®www.eatright.org/cps/rde/xchg/ada/hs.xsl/NNM_2007_home.htmNational School Breakfast Weekwww.schoolnutrition.org/nsbwAmerican Diabetes Alert Daywww.diabetes.org/communityprogramsand-localevents/americandiabetesalert.jspWorld Kidney Daywww.kidney.org/news/wkd/index.cfmFAFP Future MeetingsFebruary 20, 2010Diabetes WorkshopUNF University Center, JacksonvilleApril 23-25, 2010104th <strong>Family</strong> Medicine WeekendGrand Hyatt Tampa BayJuly 9-11, 2010<strong>Family</strong> Medicine WeekendHilton OrlandoDecember 10-12, 2010<strong>Family</strong> Medicine WeekendThe Ritz-Carlton Amelia IslandJuly 15-17, 2011<strong>Family</strong> Medicine WeekendHilton OrlandoDecember 9-11, 2011<strong>Family</strong> Medicine WeekendThe Ritz-Carlton Amelia IslandJuly 13-15, 2012<strong>Family</strong> Medicine WeekendHilton OrlandoDecember 7-9, 2012<strong>Family</strong> Medicine WeekendThe Ritz-Carlton Amelia IslandJuly 19-21, 2013<strong>Family</strong> Medicine WeekendHilton OrlandoJuly 18-20, 2014<strong>Family</strong> Medicine WeekendHilton Orlando<strong>Florida</strong> <strong>Family</strong> Physician 15
Primary Care Strategies for Reducing<strong>Disparities</strong> in Birth OutcomesRacial and ethnic healthdisparities begin at birth.In <strong>Florida</strong>, like mostother parts <strong>of</strong> the country,babies born to blackmothers have more thantwice the chance <strong>of</strong>dying before their firstby Carol Brady, MA birthdays compared towhite babies. They arealso twice as likely to be stillborn or to be bornat low birth weights. <strong>Disparities</strong> among racialand ethnic groups persist despite advancesin health care and medical technology thathave reduced overall infant mortality. Newapproaches that focus on improving healthand reducing adverse social factors over thelife span recognize the critical role <strong>of</strong> familypractitioners in addressing these disparities.<strong>Florida</strong> ranks 36th out <strong>of</strong> all states in infantmortality. 1 In 2008, there were 7.2 infantdeaths (< 365 days old) for every 1,000 livebirths. The infant mortality rate for whites was5.5 deaths per 1,000 live births; for blacks, itwas 12.9 deaths per 1,000 live births (Figure1). 2 Overall, the United States ranks belowmost developed countries in birth outcomes,a trend that has remained unchanged over thelast decade. 3 In 2007, the U.S. infant mortalityrate was 6.7 deaths per 1,000 live births. 4Leading causes <strong>of</strong> death include congenitalanomalies, prematurity and low birth weightand sleep-related deaths. Health disparitiesare a primary factor impacting the state andcountry’s infant mortality rates.Infant mortality statistics tell only part <strong>of</strong> thestory. Fetal deaths (stillbirths after 20 weeks<strong>of</strong> gestation) are equal to infant deaths in mostcommunities. In 2008, <strong>Florida</strong> had a fetaldeath rate <strong>of</strong> 7.2 stillbirths per 1,000 deliveries.For whites, the fetal death rate was 5.6 per1,000 deliveries; for blacks, the rate was 13.1per 1,000 deliveries. 5 Although they have thegreatest risk <strong>of</strong> mortality at weights < 1,500grams, most babies born low birth weightsurvive. In 2008, more than 20,000 babies— 8.8 percent <strong>of</strong> all live births — were bornweighing < 2,500 grams in <strong>Florida</strong>. Thisincludes 7.4 percent <strong>of</strong> white babies and13.5 percent <strong>of</strong> black babies. 6 These babiesare at higher risk <strong>of</strong> long-term disability anddevelopmental delay.Improving access to health care duringpregnancy has been a key strategy foraddressing poor birth outcomes. Specializedprenatal and neonatal care has significantlyimproved both maternal and infant survivalrates. In <strong>Florida</strong>, expanded Medicaidbenefits are available to uninsured womenat higher income levels during pregnancy.Healthy Start and other programs workwith expectant and new families to reduceindividual risks like tobacco and substanceuse, as well as to educate parents aboutbreastfeeding, safe sleep and other positivebehaviors that can improve their chances<strong>of</strong> having a healthy baby. Despite improvementsin survival rates, the gap betweenthe outcomes <strong>of</strong> babies born to mothers <strong>of</strong>different races remains.There is growing consensus that elimination<strong>of</strong> disparities requires a broader approachthat addresses not only individual risks butalso social factors and access to health carewell before pregnancy. 7 Researchers now attributemuch <strong>of</strong> the disparity in birth outcomesto the cumulative effects <strong>of</strong> these factors overthe mother’s life course. 8 Care and servicesprovided during pregnancy or immediatelyafter birth is too late and too costly.Dr. Michael Lu and others suggest that acomplex interplay <strong>of</strong> biological, behavioral,16
psychological and social factors contributesto health outcomes across the span <strong>of</strong> aperson’s life. 9,10,11 Rather than just focusingon risks, behaviors and health care once awoman becomes pregnant, the life-coursemodel focuses on the cumulative effect <strong>of</strong>health status and life circumstances.Primary care practitioners play a criticalrole in addressing disparities in birthoutcomes using a life course approach.The U.S. Centers for Disease Control andPrevention in 2006 issued a work groupreport that attributed lack <strong>of</strong> progress inreducing low birth weight, prematurity andinfant mortality, particularly among African-Americans, to poor preconception healthand health care. 12 The importance <strong>of</strong> preconceptioncare was previously identifiedin family medicine. 13,14,15 Subsequent workby the clinical subcommittee <strong>of</strong> the SelectPanel on Preconception Health underscoredthe importance <strong>of</strong> routine primary care forwomen <strong>of</strong> reproductive age. A life-courseapproach requires “a shift from the delivery<strong>of</strong> procedure-based acute care to the provision<strong>of</strong> counseling-based preventive care.” 16A special 2008 supplement to the AmericanJournal <strong>of</strong> Obstetrics and Gynecology, producedby the subcommittee, lays out theevidence base and content <strong>of</strong> primary careinterventions to improve birth outcomes andreduce disparities. 17Beyond health and access to care, the lifecourseapproach broadens the focus <strong>of</strong>maternal and child health to include socialequity. Socioeconomic status, race and racism,educational attainment, crime and violence,environmental threats and neighborhood isolationare some <strong>of</strong> the factors that affecthealth outcomes, including infant mortality.These factors impact racial and ethnic groupsdifferently and may explain disparities inbirth outcomes even with equal access to careduring pregnancy. 18For primary care practitioners, this meansgetting involved in larger-scale communityefforts to address economic development,crime, school quality, housing, racism, accessto healthy foods and opportunities for physicalactivity that are equally critical togood birth outcomes. Pr<strong>of</strong>essional, civicand community organizations, like localHealthy Start Coalitions, provide opportunitiesfor practitioners to move beyondindividual-level interventions and advocatefor community change.References1 The Annie E. Casey Foundation Kids Count 2009Data Book. <strong>Florida</strong>’s overall rank = 36/50 (1-50 =lowest to highest or worst). Retrieved from: http://datacenter.kidscount.org/Databook/2009/OnlineBooks/StatePr<strong>of</strong>iles/AEC189%20pr<strong>of</strong>ile_<strong>Florida</strong>.pdf.2 <strong>Florida</strong> Department <strong>of</strong> Health, <strong>Florida</strong> VitalStatistics Report, 2008. Retrieved from http://www.flpublichealth.com/VSBOOK/VSBOOK.aspx.3 United States Central Intelligence Agency, TheWorld Factbook, 2009. Retrieved from https://www.cia.gov/library/publications/the-world-factbook/rankorder/2091rank.html.4 U.S. National Center for Health Statistics,“Deaths, Preliminary Data for 2007”; published19 August 2009. Retrieved from http://www.cdc.gov/nchs/data/nvsr/nvsr58/nvsr58_01.pdf.5 <strong>Florida</strong> Department <strong>of</strong> Health. Op cit.6 Ibid.7 Fine, A., Kotelchuck, M., Adess, N., Pies, C.(2009). Policy Brief: A New Agenda for MCHPolicy and Programs: Integrating a Life CoursePerspective. Retrieved from: http://www.cchealth.org/groups/lifecourse/publications.php.8 Lu, M., Halfon, N.(2003) Racial and ethnic disparitiesin birth outcomes: a life course perspective.Maternal Child Health Journal, 7: 13-30.9 Misra, D.P., Guyer, B.D., Allston, A. (2003)Integrated perinatal health framework: a multipledeterminants model with a life span approach.Am J Prev Med,25:65-75.10 Lu, M., Kotelchuck, M., Hogan, V., Jones C.P.Halfon, N. (2009). Closing the black-white gap inbirth outcomes: a life-course approach. Acceptedfor publication in Ethn Dis.11 Geronimus, A.T. (1992). The weatheringhypothesis and the health <strong>of</strong> African-Americanwomen and infants: evidence and speculations.Ethn Dis, 2:207-221.12 U.S. Centers for Disease Control & Prevention(2006). Recommendations to improve preconceptionhealth and health care – United States: areport <strong>of</strong> the CDC/ATSDR Preconception CareWork Group and the Select Panel on PreconceptionCare. MMWR 55 (No.RR-6).13 Gjerdingen DK, Fontaine P. (1991).Preconception health care: a critical task for familyphysicians. J Am Board Fam Pract, 4:237-50.14 Frey KA. (2002).Preconception care by the nonobstetricalprovider. Mayo Clin Proc, 77:469-73.15 Jack B. (1995). Preconception care (or how allfamily physicians “do” OB). Am Fam Physician.51:1807-8.16 Atrash, H., Jack, B., Johnson, K. et al (2008).Where is the “W”oman in MCH? Am J Ob Gyn.99:6 Suppl B (Dec. 2008). Retrieved from: http://www.ajog.org/issues/contents?issue_key=S0002-9378(08)X0011-0.17 Jack, B., Atrash, H. eds. (2008) PreconceptionHealth and Health Care The Clinical Content <strong>of</strong>Preconception Care. Am J Ob Gyn. 99:6 SupplB (Dec. 2008). Retrieved from: http://www.ajog.org/issues/contents?issue_key=S0002-9378(08)X0011-0.18 Lu, M., Halfon, N. (2003) op cit.About the AuthorCarol Brady, MA, is the executive director <strong>of</strong> theNortheast <strong>Florida</strong> Healthy Start Coalition, whichcovers Jacksonville-Duval and the four surroundingcounties. She is a member <strong>of</strong> the CDC SelectPanel on Preconception Health and was an invitedparticipant at the 2008 National Life CourseMeeting sponsored by the California Endowmentand Contra Costa Health Services.<strong>Florida</strong> <strong>Family</strong> Physician 17
Closing the GapReducing Health <strong>Disparities</strong> Among MinoritiesBackgroundThe Reducing Racial and Ethnic Health <strong>Disparities</strong> “Closing theGap” grant program, section 381.7351, <strong>Florida</strong> Statutes, was signedinto law on June 8, 2000. These grants are utilized to stimulate thedevelopment <strong>of</strong> community and neighborhood-based organizations toimprove health outcomes <strong>of</strong> racial and ethnic populations and promotedisease prevention activities.Projects funded through the Closing the Gap grant program helpstimulate broad-based participation and the support <strong>of</strong> both publicand private entities by:• Fostering partnerships between local governments, communitygroups and private-sector health care organizations• Helping communities address their most pressing health needs throughtargeted health screenings, education and awareness programs• Helping communities better understand the nature <strong>of</strong> health disparitiesamong ethnic and racial groups• Allowing state epidemiologists to evaluate the effectiveness <strong>of</strong> theinterventions so that identified “best practices” can be shared withother high-risk <strong>Florida</strong> communitiesPrimary benefits to the state form the Closing the Gap Act include:• Meaningful improvements in the lives <strong>of</strong> Floridians who now sufferdisproportionately from disease and disability• Development <strong>of</strong> tools and strategies that will enable <strong>Florida</strong> toeliminate these disparitiesPriority Health AreasThe “Closing the Gap” grant program targets seven priority health areas:• Cancer• Cardiovascular disease• Diabetes• Adult and Child immunizations• HIV/AIDS• Maternal and infant mortality• Oral health careIn addition, the Office <strong>of</strong> Minority Health provides leadership inimproving minority health and reducing health disparities through:• Education• Collaboration• Mobilization• CoordinationWhat Are Health <strong>Disparities</strong>?Health disparities exists when one group <strong>of</strong> people gets sick or diemore <strong>of</strong>ten than another group.For example, in <strong>Florida</strong>:• The cancer death rate is significantly higher in minorities• Black babies are twice as likely to die than white babies• Blacks make up a disproportionate number <strong>of</strong> HIV/AIDS casesin <strong>Florida</strong>• Tooth decay is the single most common chronic illness in children• Latino preschoolers have over twice the tooth decay as white childrenWhy Is Addressing Health <strong>Disparities</strong>So Important in <strong>Florida</strong>?Health disparities are associated with unhealthy communities thatcontribute to increased health care costs for all Floridians. As<strong>Florida</strong> is a very culturally diverse state, failure to address race- andethnic-based health inequities and disparities may prove devastating.The <strong>Florida</strong> Department <strong>of</strong> health monitors health disparities toreduce disease burden by identifying high-risk groups, formulatingappropriate health care policy and evaluating the state’s progress ineliminating health disparities. The <strong>Florida</strong> Office <strong>of</strong> Minority Healthserves as a focal point for the state’s efforts.What Is <strong>Florida</strong> Doing toAddress Health <strong>Disparities</strong>?The <strong>Florida</strong> Office <strong>of</strong> Minority Health works to ensure that all <strong>of</strong>the divisions and bureaus in the Department <strong>of</strong> Health are properlyaddressing minority health issues. The <strong>of</strong>fice also directly oversees theClosing the Gap Program, the State Partnership Program and <strong>Florida</strong>Healthy People 2010.From the <strong>Florida</strong> Department <strong>of</strong> Health Office <strong>of</strong> Minority Health, visit http://www.doh.state.fl.us/Minority/index.htm.18
Money SenseKeep Your Retirement Savings on Trackby Vince Grogan, Merrill LynchThe financial meltdown has dealt some<strong>of</strong> its sharpest punches to many individuals’retirement plans. Despite whatwe believe to be a temporary derailment, fourstrategies can help get your retirement savingsgoals back on track.Take stock <strong>of</strong> your situation. The first stepto developing an effective recovery plan isto gather information on all your assets.Build a holistic view <strong>of</strong> how your funds havewithstood the market thus far, and determinewhether your total asset base is allocatedeffectively for your particular plan.Consolidate accounts. The process <strong>of</strong> gatheringand reviewing all your assets may revealjust how many “savings buckets” you have tomanage. Allocating assets and managing riskcan be logistically more difficult when you’remanaging multiple pools <strong>of</strong> scattered assets.You may be able to make fewer accountswork harder for you, and you could find iteasier to respond to shifting markets.For example, if you have multiple retirementaccounts from previous employers, considerrolling them over into your current plan ora rollover IRA. Be sure to work with yourtax advisor to help assess whether a rollovermakes sense for you.Emphasize income. Consider what portion<strong>of</strong> your assets should be dedicated to providingan income stream. Bonds, treasuries andCDs can all create income, especially if youstagger maturity dates. Annuities and dividend-payingstocks are choices to consider aswell. And don’t forget, a paycheck is anotherform <strong>of</strong> regular income. Remaining in theworkforce — even if part-time — can reducethe pressure on your investments to produceincome and give you more time to save.Re-evaluate your risk exposure. With retirementsprojected to last for 20 years or more,every retirement-focused portfolio needs along-term growth component, and that usuallycomes from stocks. While it’s importantto avoid taking imprudent risks in an effort toplay catch-up, hiding in a heavy cash positionfor the long term can have you coming upshort when it’s time to depend on your savings.Work with your advisor to adjust yourasset allocations regularly.Neither Merrill Lynch nor its financial advisorsprovide tax, accounting or legal advice.Clients should review any planned financialtransactions or arrangements that may havetax, accounting or legal implications with theirpersonal pr<strong>of</strong>essional advisors.Vince Grogan is director <strong>of</strong> marketing with theRetirement Group at Merrill Lynch.For more information, contact Merrill LynchFinancial Advisor Michael Welch Jr., CRPC ® , <strong>of</strong>the Melbourne <strong>of</strong>fice at (321) 729-8630, or goto www.fa.ml.com/michael_welch.<strong>Florida</strong> <strong>Family</strong> Physician 21
<strong>Cultural</strong> Diversity:by Maria Gina Tiomico, MD, FAAFP, JacksonvilleAging is the process <strong>of</strong> becoming oldthat is genetically determined andenvironmentally modulated.Ageism is the evaluative judgment towarda person or persons simply due to theiradvancing age.In the late 1990s, the elderly population <strong>of</strong> theUnited States was 12.6 percent; 87 percent<strong>of</strong> which were non-Hispanic whites, 8 percentAfrican-Americans, 4 percent Hispanicsand 1 percent Asian-Americans. It is projectedthat by 2020, elderly non-Hispanicwhites will drop to 10 percent and theethnic minority will increase to 23 percent(African-American, Hispanics and Asian-Americans), making up 17.7 percent <strong>of</strong> thetotal population.Therefore, it is vital for physicians and otherhealth care providers to gain sensitivity andunderstanding <strong>of</strong> the cultural differences thatinfluence the family dynamics and the perception<strong>of</strong> care <strong>of</strong> the elderly patients belongingto the ethnic minority.Ethnicity is distinguished on the basis <strong>of</strong> aunique language or communication structure,common history, group-held valuesand beliefs, normative expectations andattendant customs and practices. The intergenerationaltransmission <strong>of</strong> these values— as well as the variation in social class,racial labeling and discrimination, in additionto genetic factors — may contribute toobserved ethnical differences.Most North Americans are reluctant to acceptaging and <strong>of</strong>ten hold ageist attitudes andbeliefs. This has been proven by multiplestudies done over time. One study used the“Implicit Association Test” and “RespondWindow Priming” questionnaires. It showedthat both young and old adults associated“old” with “unpleasant stimuli” more easilythan “old” and “pleasant stimuli.” There weremore “negative traits” that were associatedwith an older person, and “positive traits”were associated with a younger person. Itcannot be denied that the older one gets,the more disease entities come into play.Because this is an accepted fact by themajority, there are more realistic expectationsabout life expectancy and prognosticatingdisease processes.In receiving care, most North Americanspractice autonomy. The particular individual(the elderly) exercises his or her right to makedecisions related to medical care unless ahealth care surrogate or primary caregiver isgiven the authority by the individual to makethe decision. This produces a level <strong>of</strong> empowermentfor the individual for which egalitarianism(political doctrine that holds thatpeople should be treated as equals and havethe same political, economic, social and civilrights) can be exercised. On the other hand,in providing care for the elderly, it is expectedthat the appropriate disclosure <strong>of</strong> the illness,the treatment and the prognosis are provided.It is not customary to disclose the informationto family member(s) unless the individualprovides that authorization in writing. Theappropriate government benefits and otherformal support systems available are usuallyutilized for a more comprehensive delivery <strong>of</strong>care. In short, the overall care provided to theelderly individual is in accordance with his orher wishes and not dictated by the physicianor family member(s). This process usuallyrelieves the family member(s) <strong>of</strong> some <strong>of</strong>the stressors (e.g. economic, social burden)associated with the care. However, the directstress is usually shouldered by the elderlyspouse; thus, depression is <strong>of</strong>ten manifested.Within the African-American culture, theattitude <strong>of</strong> respect for each generation plays apart in determining family support behavior.Since more than 50 percent <strong>of</strong> the populationis unmarried, single parents, extendedfamily and kin are important in maintainingfamily cohesion. This being said, there is avery high regard for the elderly (parents/grandparents), since they provided the carefor the children/grandchildren who are nowreciprocating the care in their old age. Thegrandparents, especially the grandmother,play a crucial role in the maintenance <strong>of</strong>the African-American family. They are thestrong source <strong>of</strong> support and affection; therefore,they are more likely to be cared for bytheir family until they die. Because <strong>of</strong> suchfamily involvement, the decision regardingthe care <strong>of</strong> the elderly does not solely lieupon the individual; family members are usuallyinvolved (collectivism) and can createa conflict with the delivery <strong>of</strong> appropriatecare. The disclosure pertinent to the diseaseprocess may be requested to be withheld byfamily members in an attempt to spare theelderly <strong>of</strong> more anguish. Unfortunately, thiscan lead to a non-proactive approach in establishinga plan <strong>of</strong> care. African-Americans aremore likely to be hospitalized at the end <strong>of</strong>life and prefer to continue aggressive treatmentdespite a poor prognosis. Although theyare open in using formal services for elderlycare, they are less likely to use hospice if theelderly does not have cancer. This behavior isinfluenced by historical experience <strong>of</strong> inadequatemedical care due to low socio-economicstatus, disrespectful management aswell as religious and spiritual values. Despitethese, the caregivers are less likely to experiencecaregiver burden and/or depression.They utilize cognitive coping mechanism,providing them with increased personal andspiritual meaning in their caregiving experience,coupled with familism.The Hispanics value respect and “la familia”(the family) — the extended family. Theirfamily system is patriarchal as well as hierarchal.It revolves around a strong male figure,usually the father, who is the sole provider<strong>of</strong> the household. Household decisions areachieved by the father with strong influenceand support by the wife. In caring for theelderly parent, the spouse (sometimes) theoldest daughter or daughter-in-law is responsiblefor providing direct care, regardless <strong>of</strong>the quality <strong>of</strong> relationship the caregiver haswith the elderly parent. More <strong>of</strong>ten than not,a lot <strong>of</strong> pressure is put upon her by the rest<strong>of</strong> the family members. Additional difficultystems from the understanding that despitebeing the provider <strong>of</strong> care, the decision <strong>of</strong>22
The Attitude Toward Aging and Elderly Carethe elderly cannot be questioned or refuted,no matter how bad it may be, even if theelderly parent is demented. Dementia is notconsidered a disease but part <strong>of</strong> the normalprocess <strong>of</strong> aging. Therefore, symptoms arenot reported to the physician. Although itmay seem a torturous process and may causesome element <strong>of</strong> depression on the part <strong>of</strong> thecaregiver, the strong faith in religion (90 percent<strong>of</strong> Hispanics are Roman Catholics) providessalvation. Like Asians, some caregiversconsider the role as uplifting and become asource <strong>of</strong> self-esteem, since they have lessaccess to other valued roles (e.g. high-statusjobs). From the perspective <strong>of</strong> the health careprovider (e.g. the physician), it is important toalways consider that prevention and treatment<strong>of</strong> illnesses always has a religious component.Praying, wearing religious medals and keepingrelics in the home play a very importantrole in health. Therefore, it will be less likelyfor the elderly and the family to accept end<strong>of</strong>-lifecare in the presence <strong>of</strong> a terminal disease,and aggressive management is expecteduntil the last breath.Asian-Americans have a high regard for ageand the elderly, and they have a high obligationto the family. Hierarchal family relationshipsare prioritized over spousal relationships.Therefore, children obey and care for theirparents without question or resentment. Sincethis culture is also community-oriented, theuse <strong>of</strong> shame to control unnecessary behaviorhas been quite effective. The firstborn sonhas the greatest authority and responsibility.The care <strong>of</strong> the aging parent is delegated tothe wife <strong>of</strong> the firstborn son, regardless <strong>of</strong> thequality <strong>of</strong> relationship she has with the agingparent. In addition, all children are expectedto “repay parental sacrifice via filial piety.” Inthe absence <strong>of</strong> a firstborn son, the firstborndaughter assumes the greatest authority andresponsibility. Although the husband <strong>of</strong> thefirstborn daughter is not expected to partakein the care <strong>of</strong> the aging parent, it is expectedthat he will not compromise the level <strong>of</strong> careand respect that the daughter has for the agingparent. The spouse <strong>of</strong> the aging parent (themother) is usually sheltered from the responsibility<strong>of</strong> care. Regardless what the circumstancesmight be, the caregiver has a greaterlikelihood to develop caregiver burden anddepression, since the only mechanism utilizedis emotional and focused coping. Fromthe health care providers perspective, it isimportant to know that the decision-makingregarding care <strong>of</strong> the elderly parent is “collective,”i.e. similar to African-Americans andHispanics, rather than “individualistic,” likethe North Americans. The Asian-Americanfamily would actively protect the aging parentfrom knowledge <strong>of</strong> the medical condition.The physician should exercise caution inusing specific terminologies like “cancer”and may need to downgrade the term to amore “generic” equivalent, like “growth” or“mass,” until clarification <strong>of</strong> preference hasbeen discussed, because it can be regardedas a form <strong>of</strong> disrespect. This then posessimilar difficulty in providing the appropriateplan <strong>of</strong> care. More so, Asian-Americansare less likely to utilize formal services thatare available due to: 1) language barrier, 2)outright refusal due to shame or fear <strong>of</strong> discriminationand 3) family cohesiveness withthe mentality <strong>of</strong> “We can handle this on ourown.” Many Asian-American nurses work innursing homes, but they will never allow theiraging parent to be a part <strong>of</strong> the nursing-homesetting. Like the Hispanics, dementia is notconsidered a disease but part <strong>of</strong> the normalaging process and, therefore, is not reportedto the physician. In addition, religious faithcan complement or retard appropriate care;thus, aggressive treatment is expected regardless<strong>of</strong> prognosis, and hospice end-<strong>of</strong>-life carewould likely not be utilized.In conclusion, although the majority <strong>of</strong> theethnic minority has higher levels <strong>of</strong> illnessand disability due to previous lack <strong>of</strong> medicalcare, there continues to be the underutilization<strong>of</strong> formal support. However, theincreased level <strong>of</strong> informal support, strongfamily values, the increased level <strong>of</strong> cognitiveand religious coping and the lower probabilitythat the caregiver is the spouse afford a lowerlevel <strong>of</strong> distress overall and, therefore, manifestan increased level <strong>of</strong> positive caregivingamong the ethnic minority.References1 “Racial Differences in Hospice and In-HospitalDeath Among Medicare and Medicaid DualEligible Nursing Home Residents,” Gerontology,February 1, 2008; 48(1):32-41.2 “Ethnic Differences in Stressors, Resources &Psychological Outcome <strong>of</strong> <strong>Family</strong> Care giving”,A Meta-Analysis, Gerontology, February 1, 2005;45(1): 90-106.3 Journal <strong>of</strong> Gerontology, 1985; 40(3): 382-389.4 “<strong>Cultural</strong> Values & Care-giving Pattern AmongAsian & Pacific Islander Americans,” SocialGerontology, 1998;12(1): 155-179.5 “An Overview <strong>of</strong> Race & Marital Status in BlackFamilies,” Staples (1997), 3rd ed.:269-273.<strong>Florida</strong> <strong>Family</strong> Physician 23
y Russ Hostetler,MD, Plant CityOld People &Loving RelationshipsAnd Other Musings on Being a <strong>Family</strong> DoctorJohn was sharp. Tall and slightly overweight,he was a friendly and socially adept manwho lived his life with authenticity. John wasdiabetic, couldn’t see clearly enough to loadhis insulin syringes, and his Charcot foot andperipheral neuropathy made safe independentambulation dicey. John’s friends and family (hehad one son in Atlanta) convinced him that hewould be safer and happier in a nursing home.He acquiesced but longed for independence.Julia was quiet, thin and pale. She neveropened her blinds, and the only light in herroom was a 40-watt table lamp. Her hairwas white, and she wore on her lips a dustyrose shade that was the only real color inher otherwise black, gray and beige pallet <strong>of</strong>clothes. She had had a small CVA, which Ihad assumed made her virtually mute. Sheanswered “Yes” or “No,” but remained silentotherwise. Although, after her stroke, sherecovered nearly all physical capability, sheremained at Lynn Haven. Her only excursionswere walks between her room and the cafeteria,her eyes on the floor.On one <strong>of</strong> those walks, Julia met John. Johnhad walked into the crash bar <strong>of</strong> a proppedopen door. The end <strong>of</strong> the crash bar hookedonto his walker, and John couldn’t pull itaway. While John tried to free himself, Juliaquietly walked up, twisted the walker to freethe snagged bit, pulled it away from the barand looked at John. For a moment, Juliaseemed to study him. Then she lowered hereyes and walked on silently. John chased her athis snail’s pace, chattering away, trying to gainher attention and thanking her over and over.Mr. John usually sat with two other men inthe cafeteria, laughing at old jokes and sharedstories. But today, Mr. John didn’t sit with hisbuddies. He sat at the table where Ms. Julia sat.Julia probably did not say a word during thatfirst lunchtime together. She probably heardeverything about John: his origins, his marriage,his widower status, his son, his former occupationat Georgia Power and Light, his diabetes,his “bum foot,” his desire for freedom. Manypeople probably thought Julia’s introversionwould bore John and he’d revert to rating ladiesfrom his bench. They were wrong.John gently, quietly, patiently drew Julia fromher shell. At first, John began walking to thecafeteria at the same time as Julia. Soon, Ms.Jordan, a head nurse, noticed that Julia smiledwhen John sang John Lennon’s “Juuuuuuu leeahh” when she appeared in her doorway.I visited Lynn Haven on Wednesdays. Usually,Julia would be in bed, daydreaming. Thistime, she was gone. I would have known if“God had called her home,” but I did notknow what led to her absence that day.When I asked Ms. Jordan, she answered withrelish and detail. John would wait in his owndoorway near Julia’s room until Julia stirred.Then he’d hustle to sing her name and get herattention before she got far down the hallway.Miraculously, she waited, and they walkedtogether. It made sense that they sat togetherbecause Julia would not speak to tell him tobuzz <strong>of</strong>f. For about a week, that was theirroutine. Then Julia began appearing in herdoorway and looking toward John’s room tomake sure he was coming. Soon, she not onlylooked up, but smiled.Ms. Jordan said that about three weeks ago,Julia went with John to the day room to watchsoap operas, where Ms. Jordan had seenJohn take Julia’s hand. During the followingweeks, John coaxed Julia outside for a walk,to the canasta table, to sit with him hand inhand for the Friday-night movie, and then, asreported by a night nurse, to allow him intoher room between 10 p.m. and midnight. Asshe reported this tidbit, Ms. Jordan winked.“What they do is their business, as long assomeone doesn’t complain.”They were a cute couple. It was uplifting tosee Julia smiling as she walked with John,24
one hand on his where he grabbed his walker,or to see them cuddled on the a bench chatting.Yes, Julia could talk. But before John,she had no reason to speak.One day, John asked if I would meet with himand Mr. Wilson, the Lynn Haven administrator.I consented and went to the <strong>of</strong>fice whenI finished rounds. John and Julia were there,John conversing with Mr. Wilson, Ms. Jordanand Ms. Winetrout, the social worker. As Iwalked in, Mr. Wilson spoke.“Doc, Mr. John wonders what would beinvolved in being allowed to leave LynnHaven,” he said smiling.“Am I to assume that Mr. John and Ms. Juliawould be leaving together?” I asked.John and Julia nodded, smiling sweetly toeach other and holding hands.I reviewed Mr. John’s need to have someonedraw up his insulin for him and heard Ms.Jordan assert that Ms. Julia could performthat task. I talked about Mr. John needinghelp with foot care and lower-body dressing.I suggested that a home health aide couldcheck on their ability to obtain groceries andmanage simple food prep. The PresbyterianChurch had a program for shut-ins to helpwith buying groceries and transportation forappointments. “So...” I paused, trying to think<strong>of</strong> anything else. I looked at Ms. Winetrout,who shrugged. Then I asked Julia, “Do youhave a place to stay?”She smiled, looked at John, and spoke clearlyand simply, “John?”“I’ve been watching the classifieds,” Johnsaid. “There’s an apartment in Forsythe being<strong>of</strong>fered by a young widow who wants thecompanionship <strong>of</strong> an elderly couple. Shecould help us with groceries and gettingaround. With both <strong>of</strong> our Social Security, wecould make it just fine.”“I don’t see any problems that can’t besolved,” I said. I smiled at John and Julia,who beamed.“I’ll get started right away!” Ms.Winetrout exclaimed.Two days later, I got a message that BillWilson wanted me to attend a “family conference”the next day, a Saturday. “Turns out Ms.Julia has two daughters, and they want everybodyto meet tomorrow to discuss Mr. Johnand Ms. Julia shackin’ up together,” he said.We talked strategy; get them to sit down, letthem vent, acknowledge their feelings, butstay on the message that their mother has theright to make her own decisions and that shewas mentally sound enough to do so. Maybewe could s<strong>of</strong>ten them with renditions <strong>of</strong> thesweet courtship.It didn’t work. The daughters were loud andobnoxious. They cut <strong>of</strong>f others who tried tospeak. John’s son arrived about 20 minuteslate, right in the middle <strong>of</strong> a screaming tiradeby the oldest daughter, who was accusing Bill<strong>of</strong> running a brothel for old men. Surprised,he exclaimed, “What’s going on here?”Mr. Wilson told him that his dad and Julia hadfallen in love and decided to move in together.The daughters harrumphed, but Mr. Wilsonput out a hand to silence them. Then he askedJohn’s son, “What’s your reaction?”John’s son smiled, pumped his fist, andsaid, “Go, Dad!” Then he hugged his fatherand Julia.The daughters began screaming: “How couldyou do this to Dad?” (Ms. Julia had been widowedfor 40 years.) “What would Grandmasay if she knew you were taking up with aman out <strong>of</strong> wedlock?” In the midst <strong>of</strong> it, Juliasmiled at John, clasped his hand, and thenreturned to her room. She drew the blinds,closed the door and got in bed.She didn’t come back out.John was speechless. Herose, glaring at Julia’sdaughters with contempt.He hugged hisson, shook my handand left. He went toJulia’s room, but she would not answer thedoor, and he would not go in uninvited.John’s son berated the daughters, callingthem selfish, cruel and heartless. He askedif either were married — they were not. “Nowonder!” he said before leaving the room.He tried to comfort his dad in the hallwaynext to Julia’s room and then helped himback to his own room.When I returned to Lynn HavenWednesday, John was gone. His son hadtaken him to Atlanta.Julia was still alive and silent when I left ayear later. I imagined that, in those momentsin Bill’s <strong>of</strong>fice, she realized that she wouldalways face her daughters’ scorn. Perhapsshe thought the most loving thing to dowas to remove herself from John’s life andtake her screaming daughters with her,knowing he might feel angry with her forabandoning him.Thinking back, I imagine John in Atlanta,making his son’s children happy with hisattention and his stories. I imagine himfinally having to go to another nursinghome, and I hope that he organized anotherset <strong>of</strong> joke-telling buddies and charmedanother bevy <strong>of</strong> women there.I imagine that Julia died quietly not so manyyears later, and I imagine that, with her lastbreath, she uttered the only word I everheard her say: “John.”<strong>Florida</strong> <strong>Family</strong> Physician 25
<strong>Cultural</strong> Issuesin Substance-Abuse Evaluation and Treatmentby BerndWollschlaeger, MD,FAAFP, FASAM,Board-Certified<strong>Family</strong> Physicianand AddictionSpecialist, CertifiedMedical ReviewOfficer, MiamiFor many years, substance-abuse and other mental-health programsneglected the fact that minority groups encounter barriers to accessand utilize mental health and substance abuse treatment modalities.This results in lower and delayed health care use and subsequentlyleads to poorer quality <strong>of</strong> care.Combined, those disparities translate into millions <strong>of</strong> people sufferingneedless disability from substance abuse and dependence andother mental illnesses. Medical pr<strong>of</strong>essionals need to gain a greaterunderstanding <strong>of</strong> the cultural, economic, political and social forcesaffecting substance abuse treatment in minority populations.According to the U.S. Census Bureau, 1 the number <strong>of</strong> Hispanic-Americans, African-Americans, Asian-Americans/Pacific Islandersand American Indians/Alaska natives, the four dominant ethnicand racial minority groups, reached 102.5 million in 2007, or 34percent <strong>of</strong> the total U.S. population. Population growth is fastestamong minorities, and according to the U.S. Census Bureau estimationfor 2005, 45 percent <strong>of</strong> American children under the age<strong>of</strong> 5 are minorities. 2The heterogeneity <strong>of</strong> the members <strong>of</strong> the four major ethnicand racial minorities poses a unique challenge to renderculturally appropriate and competent care.<strong>Cultural</strong> competence is a set <strong>of</strong> academic andinterpersonal skills that allow individuals toincrease their understanding and appreciation<strong>of</strong> cultural differences and similarities within,among and between groups. 3 Unfortunately,many health care pr<strong>of</strong>essionals still lackthe skills and training to meet the growingdemand for cultural competency.This is especially evident in the area <strong>of</strong> mentalhealth care, including substance abuse, involvingthe diagnosis and treatment <strong>of</strong> complexdisease processes requiring close collaborationand communication between the patient andmultiple health care pr<strong>of</strong>essionals. In this area,cultural competence is about adapting mentalhealth care to meet the needs <strong>of</strong> consumers fromdiverse cultures. One key aim is to improve theiraccess to care. Others are to build trust and to promotetheir engagement and retention in care. A culturally competentprogram is one that demonstrates sensitivity and understanding <strong>of</strong>cultural differences in treatment and program design, implementationand evaluation.Above all, cultural competence aims to improve the quality <strong>of</strong> careand to help individuals to recover quicker and better. Its broadersocietal purpose is to reduce or eliminate all health care disparities,including mental health care, affecting disenfranchised groups. 4Members <strong>of</strong> minority groups <strong>of</strong>ten have limited access to healthcare and are, therefore, at increased risk <strong>of</strong> substance abuse and itsassociated problems, including infectious diseases, crime and interpersonalviolence. This can be attributed to several factors, amongthem, the migration experience, poverty, lack <strong>of</strong> health insurance,unemployment and cultural differences between members <strong>of</strong> minoritygroups and the society at large. We also have to understandand recognize that substantial differences exist inpatterns <strong>of</strong> substance abuse among different ethnicgroups. Highlights <strong>of</strong> the key findings discussedare derived from the 2008 National Survey onDrug Use and Health. 51. Hispanic-Americans: Among Hispanicsor Latinos, 6.2 percent used illicit drugs.Even though this is the second-lowest numberamong the four major ethnic groups,several trends are <strong>of</strong> concern. Hispanicadolescents are substantially overrepresentedamong eighth-grade students whouse drugs. This finding is alarming, givenprior findings documenting that youths whouse drugs are at significantly greater risk<strong>of</strong> experiencing a host <strong>of</strong> social, economicand health problems. The results <strong>of</strong> a multivariateanalysis showed that, for all adolescentsexcept those <strong>of</strong> other Latin American ethnicity, theestimated odds ratios predicting cocaine use werebetween 47 percent and 72 percent lower among studentsliving in households with both parents than among26
students living in households with no parent. 6 The likelihood <strong>of</strong>heavy drinking was greatest among Mexican-American, PuertoRican and Cuban-American students who lived in householdswith no parents present and lower among Mexican-Americanstudents whose first language spoken was Spanish. Treatmentadvocates have pointed out that, especially among Hispanicwomen, the guilt and shame associated with drug use <strong>of</strong>ten addsto the stigma <strong>of</strong> addiction and that this shame may also contributeto denial <strong>of</strong> their substance-abuse issues.2. African-Americans: Current illicit drug use among African-Americans amounts to 10.1 percent. Crack cocaine is the drugprompting the largest number <strong>of</strong> admissions to treatment amongyoung and early middle-aged black/African-American males andfemales. Low esteem, lack <strong>of</strong> family structure, interpersonal andfamily violence, peer pressure and exposure to and involvement indelinquent behavior are key factors that place African-Americanadolescents at a high risk <strong>of</strong> developing substance abuse. Protectivefactors that counteract the effect <strong>of</strong> risk factors include family support,religion, spirituality and community involvement. 73. Asian-Americans and Pacific Islanders (A&PI): The persistentfinding is that, compared to other populations, this group tendsto use and abuse drugs and alcohol at lower rates than othergroups, but the cultural and sociodemographic heterogeneityposes a significant challenge to understand the full extent <strong>of</strong>the substance-abuse problem. In a statewide Asian drug serviceneeds assessment survey in California, in response to the queryregarding 10 or more alcoholic drinks in their lifetime, Japanesehad the highest level <strong>of</strong> lifetime use (68.8 percent), followed byKoreans (48.6 percent), Chinese (41.8 percent), Vietnamese (43.2percent), Philipinos (39.3 percent) and Chinese-Vietnamese (38.5percent). These rates were lower than the national prevalence <strong>of</strong>85 percent. Of those who reported drinking alcohol in the pastmonth, the Chinese, Japanese, Korean and Pilipino groups tendedto drink less than either the Vietnamese or Chinese-Vietnamese. 8Hawaiians tended to have higher lifetime prevalence than otherA&PI groups for alcohol, cocaine, amphetamines and marijuana.Their alcohol lifetime prevalence was also comparable to theEuropean-American rate. Japanese and Chinese had a higherprevalence <strong>of</strong> tranquilizer use.4. American Indians and Alaska Natives: The current illicit druguse among persons aged 12 or older is 9.5 percent for AmericanIndians or Alaska natives. The high incidence <strong>of</strong> severe substanceabuse problems, especially alcoholism, has been the main stimulusfor the first alcohol treatment programs for Native Americanscreated and funded in the 1970s by the National Institute onAlcohol Abuse and Alcoholism. Alcoholism contributes to theincreased incidence <strong>of</strong> heart disease, cancer, diabetes, injuriesand death among American Indians. Members <strong>of</strong> this group alsobegin using alcohol, illicit substances and cigarettes at a youngerage, at higher rates and in combination with each other. AmericanIndian youths also frequently abuse inhalants. Obstacles tosubstance-abuse treatment include access to treatment centersand resources on reservations and the still-prevailing attitudethat such treatment approaches alienate American Indians fromtheir traditions and religion. The recognition and inclusion <strong>of</strong>traditional healing approaches (Talking Circle or Talking Stickmeeting, The Good Way, Sweat Lodge, etc.) enhances the success<strong>of</strong> and retention in treatment programs.We need to recognize that cultural themes in the development <strong>of</strong>culturally competent treatment programs will emphasize the importance<strong>of</strong> family structure, cultural healing and spiritual beliefs. Weespecially should acknowledge that, among ethnic groups, womenface significant barriers accessing appropriate care. In male dominatedsocieties, women’s substance-abuse issues are <strong>of</strong>ten belittledand ignored. Substance-abuse treatment facilities and centers shouldrespond to this double standard by utilizing female counselor andtreatment pr<strong>of</strong>essionals. 9Furthermore, understanding the minority group experiences andself-identification will assist us to identify treatment needs, culturalinterpersonal values and treatment delivery.However, we still require systematic and prospective research studiesthat document the effectiveness <strong>of</strong> specific culturally derivedtreatment interventions.References1 U.S. Census Bureau News, http://www.census.gov/Pressrelease/www/releases/archives/population/011910.html.2 Population Reference Bureau, http://www.prb.org/Articles/2006/IntheNewsUSPopulationIsNowOneThirdMinority.aspx?p=1U.S.3 Woll, C. H. (1996). What difference does culture make? Providing treatmentto women different from you. Journal <strong>of</strong> Clinical Dependency and Treatment,6(1/2), 67-85.4 Substance Abuse & Mental Health Services Administration (SAMSHA),IllnessManagement & Recovery http://download.ncadi.samhsa.gov/ken/pdf/toolkits/illness/11.IMR_<strong>Cultural</strong>.pdf.5 National Survey on Drug Use and Health. http://www.oas.samhsa.gov/nsduh/2k8nsduh/2k8Results.cfm#2.7.6 Jorge Delva, PhD, John M. Wallace Jr. PhD, Patrick M. O’Malley et al.The Epidemiology <strong>of</strong> Alcohol, Marijuana, and Cocaine Use Among MexicanAmerican, Puerto Rican, Cuban American, and Other Latin American Eighth-Grade Students in the United States: 1991–2002. Am J Public Health. 2005 April;95(4): 696–702.7 Philleo, J., Brisbane, F. L., & Epstein, L. G. (Eds.). (1997). <strong>Cultural</strong> competencein substance abuse prevention. Annapolis Jct., MD: NASW Press.8 Curriculum Asian and Pacific Islander Alcohol, Tobacco and other Drug use.http://preventiontraining.samhsa.gov/cti06/curriculum.htm.9 Women in Substance Abuse Treatment: Results from the Alcohol and DrugServices Study (ADSS) http://www.oas.samhsa.gov/WomenTX/WomenTX.htm.<strong>Florida</strong> <strong>Family</strong> Physician 27
Training Medical Students to Recognizeby Kendall M. Campbell, MD, Assistant Dean for Minority Affairs, Assistant Pr<strong>of</strong>essor,Community Health and <strong>Family</strong> Medicine, University <strong>of</strong> <strong>Florida</strong> College <strong>of</strong> Medicine, GainesvilleAs the U.S. population grows more diverse,it is becoming more and more importantfor medical schools to address health disparities,underserved populations and culturalcompetency. The growing population placesincreasing demands on our health care systemand requires our medical schools toproduce more culturally competent, healthdisparity-mindedphysicians. The 16thReport <strong>of</strong> the Council on Graduate MedicalEducation suggests that the demand forphysicians after 2015 will be greater thanthe supply. 1 The persons most impacted willbe those who are underserved.There is no standard vehicle through whichto teach cultural competence and healthdisparities. Many schools have developedcurricula that have been woven into variousaspects <strong>of</strong> the educational mission, somewith outcomes showing an improvement inawareness <strong>of</strong> these issues. Increasing awarenesscertainly is a start, but eliminatinghealth disparities requires a multi-pronged,multi-pr<strong>of</strong>essional approach that will involveongoing and evolving implementation andevaluation. Medical students are the pluripotentstem-cell recipients in this implementation,and it is our responsibility to help themdevelop and differentiate into physicianswho appreciate and recognize health disparities.Addressing health disparities in medicaleducation starts much earlier than medicalschool, involves buy-in and accountabilityfrom senior health care <strong>of</strong>ficers and <strong>of</strong>fers aunique stage for attention in family medicine.Training students to recognize and addresshealth disparities begins when young andbrilliant minds are not yet swayed by attitudes<strong>of</strong> society, which <strong>of</strong>ten minimize or placelittle emphasis on the need for addressinghealth disparities. Grade-school and undergraduateprograms have immense potentialin teaching the importance <strong>of</strong> addressinghealth disparities, and we as family physicianshave to reach far beyond our privatepractices and academic centers to the communitieswhere these young people liveto stir their desire. Platforms that lendthemselves to such schooling include summerenrichment and community outreachprograms aimed at exposing these youthto strategies that address health disparitiesand to programs that build test-taking andcritical-thinking skills. Databases shouldbe created, and these students should betracked and supported from middle andhigh school right up through undergraduatetraining and medical school. What populationsshould be targeted? It has been welldemonstrated that underrepresented groupsin medicine (URMs) tend to serve underrepresentedpopulations and those whomay be uninsured or underinsured. Thisemphasizes the need for us to supporthistorically black colleges and universities,which tend to have higher minorityenrollment, and consider these institutionsas feeders for our medical schools andresidency programs.Simply stated, where there are limited numbers<strong>of</strong> URMs in medical education, anappreciation and strategy to address healthdisparities is not as likely to exist, whetherintentional or not. Underrepresentation<strong>of</strong> URMs in our medical programs willadversely affect health disparities and boldlyunderscores the need for us to ensure culturalcompetence is taught to all enrollees,whether majority or minority. Enrichmentprograms work to create a number <strong>of</strong> applicantsfor admissions committees to consider— students who not only have theacademic ability to be successful but, moreimportantly, many who have the personalitytraits and character to become caring andcompassionate physicians.The multi-pronged approach to eliminatinghealth disparities is founded in accountability.The Liaison Committee on MedicalEducation (LCME) now requires that medi-28
& Address Health <strong>Disparities</strong>Womack ArmyMedical Centercal schools develop programs to expanddiversity in medical schools. 2 Where thereis no accountability, there is no change.Even as accountability exists from theLCME and is directly tied to accreditation,there must be buy-in for the need for thisinitiative from senior hospital and medicalschool administrators. Support from senioradministrators guarantees the life <strong>of</strong> a programand makes goal achievement possible.With support comes money and additionalresources to make the job happen.We as family physicians are on the frontlines <strong>of</strong> health disparities and owe it to ourpr<strong>of</strong>ession and to our students to ensure thatsenior administrators appreciate efforts toaddress health disparities. In stressing theimportance <strong>of</strong> addressing health disparities,it is not unreasonable to link performance toannual evaluations or performance scoring.This concept is far from the thinking in ourtraditional academic medical centers, whichcarefully evaluate and score research, medicaleducation and clinical care. The realization thathealth disparities cut across all missions andhave lasting impacts on patient care, medicaleducation and research emphasizes this needfor accountability.What is the responsibility <strong>of</strong> the family physicianin this interplay <strong>of</strong> pr<strong>of</strong>essionals poised tomeet this challenge? We, as family docs, havethe ability to drive change in this area, as thereis good evidence to show that primary careproviders have a greater desire to serve theunderserved. Change begins with perceptions,and those perceptions can’t wait to be shapedin the medical-school classroom, on the wardsor during internship. There is a belief that withstudent progression through medical training,acculturation occurs, and what may have beenperceived as a problem upon initially enteringmedical school takes on less significance astime passes. 3 This certainly may be the casein recognition <strong>of</strong> health disparities, the needfor cultural competency and mistreatment <strong>of</strong>URMs. Interestingly enough, these perceptionswere dependent on the perceiver andvaried by race, as URMs were more likelyto perceive unfair treatment. Due to underrepresentation<strong>of</strong> certain groups in medicalschools, at both student and faculty levels, itis plausible that disparities in health could beconsidered a non-issue. Our position has tobe a proactive one in which we aggressivelyteach and display the character and presence<strong>of</strong> family medicine and ways in which ourpr<strong>of</strong>ession impacts health disparities.<strong>Family</strong> physicians who serve underservedpatient populations and teach medical studentshave the ability to stimulate the biggest interestin fighting disparities. The uniqueness andrewards <strong>of</strong> caring for this group need to berealized by these trainees and the benefits andchallenges to care fully appreciated. Academiccenters must value and reward primary carephysicians who provide such a crucial and<strong>of</strong>tentimes self-sacrificing service in bothcaring for underserved patients and teachingmedical students the importance <strong>of</strong> addressinghealth disparities.In conclusion, we have discussed only three<strong>of</strong> several areas that need addressing to eliminatehealth disparities. Dialogue is a neededstart to meeting the problem, but communityoutreach, accountability and taking advantage<strong>of</strong> our unique position as family physicianscarry much more weight than talk alone. Letus all remember that disparities exist in healthcare and make it a priority to see these issuesaddressed in medical education.References1. U.S. Department <strong>of</strong> Health and Human Services,Health Resources and Services Administration(HRSA). Physician Workforce Policy Guidelines forthe United States, 2000-2020: Council on GraduateMedical Education–16th Report; 2005.2. Liaison Committee on Medical Education LCMEAccreditation Standards 2008 update on position onhealth disparities.3. Wilson, E, Grumbach K, Huebner J, Agrawal J,Bindman, A Medical student, physician and publicperceptions <strong>of</strong> health care disparities. Fam Med2004;36(10):715-21.Join the Womack Army Medical Centerteam in an exciting civilian practice atthe Army’s largest base. We <strong>of</strong>fer fullfamily practice in clinics that serve avital role supporting Army Mission andArmy Families and Retirees.Serve as a Physician, Board Certified/Board Eligible in <strong>Family</strong> Medicine,assigned to large primary care clinic atWomack Army Medical Center to providefamily medical care to beneficiaries <strong>of</strong> allages. Care for 20 to 25 patients per dayin <strong>of</strong>fice setting. No call responsibilities.Outstanding nursing and administrativeteams allow you to focus on care without<strong>of</strong>fice management burdens! Excellentpackage includes competitive salary,benefits, weekends and holidays free <strong>of</strong>clinical responsibilities.Contact Ms. Patricia Eglivitchat wamcdbocpb@amedd.army.milor call (910)907-6107.WAITING FOR THEECONOMY TO CHANGE?While you’re waiting, yourcompetitors are changing theireconomy. They’re targeting<strong>Florida</strong> <strong>Academy</strong> <strong>of</strong> <strong>Family</strong>Physicians members who makepurchasing decisions in thismulti-billion-dollar industry. Andthese members actively readthis journal like you’re doingright now.WANT TO INFLUENCETHEIR BUYING DECISION?Then contact Bob Sales at502.423.7272 or bsales@ipipublishing.com immediately!www.ipipublishing.com<strong>Florida</strong> <strong>Family</strong> Physician 29
Chronic Kidney DiseaseIs a <strong>Family</strong> AffairChronic Kidney Disease (CKD) is a generation-to-generation affair for Hispanic-Americans.If you have a blood relative who has kidney disease, you may be at risk. According to theNational Kidney Foundation, Hispanic-Americans have nearly twice the risk over non-Hispanicwhites <strong>of</strong> being diagnosed with CKD.FMQAI, the Medicare Quality Improvement Organization (QIO) for<strong>Florida</strong>, under contract with the Centers for Medicare & MedicaidServices (CMS), is one <strong>of</strong> 10 states charged with helping to identify andreduce the risk <strong>of</strong> CKD in Hispanic populations.CKD is a permanent loss <strong>of</strong> kidney function, <strong>of</strong>ten brought on by diabetesand hypertension, both <strong>of</strong> which also have a higher prevalence inHispanic populations. Of the 30 million Hispanic-Americans, approximately2.5 million have been diagnosed with diabetes. Diabetes is evenmore common among middle-aged and older Hispanic-Americans;some 25 to 30 percent <strong>of</strong> those 50 or older have diabetes. Risk factorsfor diabetes include: family history, obesity, physical inactivity and anunbalanced diet. Because Hispanic-Americans have an increased riskfor developing diabetes and CKD, they should have the following testsfor early detection <strong>of</strong> kidney disease:• Fasting blood glucose test• Non fasting blood glucose test• Blood pressure measurement• Urine test for protein• Blood test to estimate glomerular filtration (GFR)Laura Gamba, project director for the FMQAI CKD project, says:“Awareness to diabetes and high blood pressure as indicators for CKD isthe key to diagnosing the condition early on. By being aware <strong>of</strong> yoursusceptibility to diabetes and high blood pressure, you stand a greaterchance <strong>of</strong> reducing progression to CKD.” Gamba goes on to say: “It isimportant that, if you know <strong>of</strong> a family member with diabetes or highblood pressure, you see your doctor and share this important informationwith him/her. Be sure to ask about testing for diabetes and highblood pressure.”For more information about the CKD project, please go to www.fmqai.com and visit the Chronic Kidney Disease Healthcare Initiative. LauraGamba, project director, Chronic Kidney Disease, can be reached atFMQAI: (813) 354-9111 ext. 3920, or lgamba@flqio.sdps.org.This material is prepared by FMQAI, the Medicare Quality Improvement organizationfor <strong>Florida</strong>, under contract with the Centers for Medicare & MedicaidServices, an agency <strong>of</strong> the U.S. Department <strong>of</strong> Health and Human Services. Thecontents presented do not necessarily reflect CMS policy.30
Elected legislators make decisions about your financial survival and providing a medical home for your patients. These decisions aremade in the chambers <strong>of</strong> the <strong>Florida</strong> House and Senate, not in the exam room. <strong>Florida</strong>’s <strong>Family</strong>MedPAC wants to elect people whoare friendly to family physicians’ needs. To accomplish this goal, your <strong>Family</strong>MedPAC needs your help.<strong>Family</strong>MedPAC is an investment in your pr<strong>of</strong>ession. You invest in your home, family, food, clothing and transportation. You alsoinvest in your education and pr<strong>of</strong>ession merit planned investment. Make your voice strong by supporting <strong>Family</strong>MedPAC.YES, count me in — I want to help family medicine speak with astronger voice in Tallahassee!VISA # ___________________________________________________MASTERCARD # __________________________________________AMERICAN EXPRESS # ____________________________________EXPIRATION DATE ________________________________________
<strong>Florida</strong> <strong>Academy</strong> <strong>of</strong> <strong>Family</strong> Physicians6720 Atlantic BoulevardJacksonville, <strong>Florida</strong> 32211NON-PROFIT ORGUS POSTAGEPAIDLittle Rock, ARPERMIT NO. 2437