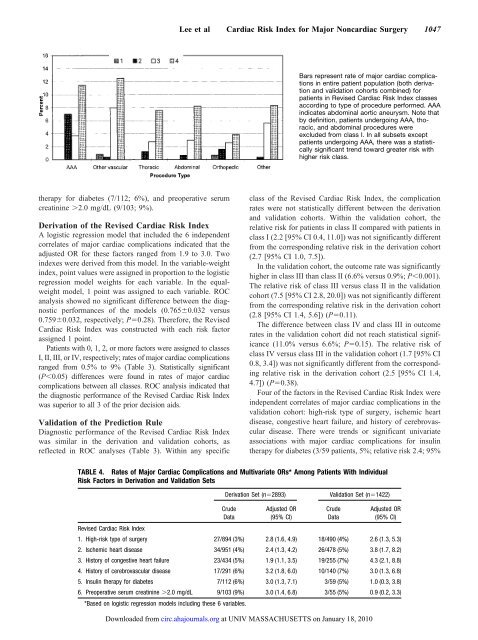
Lee et al Cardiac Risk Index for Major Noncardiac Surgery 1047Bars represent rate of major cardiac complicationsin entire patient population (both derivationand validation cohorts combined) forpatients in Revised Cardiac Risk Index classesaccording to type of procedure performed. AAAindicates abdominal aortic aneurysm. Note thatby definition, patients undergoing AAA, thoracic,and abdominal procedures wereexcluded from class I. In all subsets exceptpatients undergoing AAA, there was a statisticallysignificant trend toward greater risk withhigher risk class.therapy for diabetes (7/112; 6%), and preoperative serumcreatinine 2.0 mg/dL (9/103; 9%).Derivation of the Revised Cardiac Risk IndexA logistic regression model that included the 6 independentcorrelates of major cardiac complications indicated that theadjusted OR for these factors ranged from 1.9 to 3.0. Twoindexes were derived from this model. In the variable-weightindex, point values were assigned in proportion to the logisticregression model weights for each variable. In the equalweightmodel, 1 point was assigned to each variable. ROCanalysis showed no significant difference between the diagnosticperformances of the models (0.7650.032 versus0.7590.032, respectively; P0.28). Therefore, the RevisedCardiac Risk Index was constructed with each risk factorassigned 1 point.Patients with 0, 1, 2, or more factors were assigned to classesI, II, III, or IV, respectively; rates of major cardiac complicationsranged from 0.5% to 9% (Table 3). Statistically significant(P0.05) differences were found in rates of major cardiaccomplications between all classes. ROC analysis indicated thatthe diagnostic performance of the Revised Cardiac Risk Indexwas superior to all 3 of the prior decision aids.Validation of the Prediction RuleDiagnostic performance of the Revised Cardiac Risk Indexwas similar in the derivation and validation cohorts, asreflected in ROC analyses (Table 3). Within any specificclass of the Revised Cardiac Risk Index, the complicationrates were not statistically different between the derivationand validation cohorts. Within the validation cohort, therelative risk for patients in class II compared with patients inclass I (2.2 [95% CI 0.4, 11.0]) was not significantly differentfrom the corresponding relative risk in the derivation cohort(2.7 [95% CI 1.0, 7.5]).In the validation cohort, the outcome rate was significantlyhigher in class III than class II (6.6% versus 0.9%; P0.001).The relative risk of class III versus class II in the validationcohort (7.5 [95% CI 2.8, 20.0]) was not significantly differentfrom the corresponding relative risk in the derivation cohort(2.8 [95% CI 1.4, 5.6]) (P0.11).The difference between class IV and class III in outcomerates in the validation cohort did not reach statistical significance(11.0% versus 6.6%; P0.15). The relative risk ofclass IV versus class III in the validation cohort (1.7 [95% CI0.8, 3.4]) was not significantly different from the correspondingrelative risk in the derivation cohort (2.5 [95% CI 1.4,4.7]) (P0.38).Four of the factors in the Revised Cardiac Risk Index wereindependent correlates of major cardiac complications in thevalidation cohort: high-risk type of surgery, ischemic heartdisease, congestive heart failure, and history of cerebrovasculardisease. There were trends or significant univariateassociations with major cardiac complications for insulintherapy for diabetes (3/59 patients, 5%; relative risk 2.4; 95%TABLE 4. Rates of Major Cardiac Complications and Multivariate ORs* Among Patients With IndividualRisk Factors in Derivation and Validation SetsDerivation Set (n2893)Validation Set (n1422)CrudeDataAdjusted OR(95% CI)CrudeDataAdjusted OR(95% CI)Revised Cardiac Risk Index1. High-risk type of surgery 27/894 (3%) 2.8 (1.6, 4.9) 18/490 (4%) 2.6 (1.3, 5.3)2. Ischemic heart disease 34/951 (4%) 2.4 (1.3, 4.2) 26/478 (5%) 3.8 (1.7, 8.2)3. History of congestive heart failure 23/434 (5%) 1.9 (1.1, 3.5) 19/255 (7%) 4.3 (2.1, 8.8)4. History of cerebrovascular disease 17/291 (6%) 3.2 (1.8, 6.0) 10/140 (7%) 3.0 (1.3, 6.8)5. Insulin therapy for diabetes 7/112 (6%) 3.0 (1.3, 7.1) 3/59 (5%) 1.0 (0.3, 3.8)6. Preoperative serum creatinine 2.0 mg/dL 9/103 (9%) 3.0 (1.4, 6.8) 3/55 (5%) 0.9 (0.2, 3.3)*Based on logistic regression models including these 6 variables.Downloaded from circ.ahajournals.org at UNIV MASSACHUSETTS on January 18, 2010
1048 <strong>Circulation</strong> September 7, <strong>1999</strong>CI 1.2, 4.8) and for preoperative serum creatinine 2.0mg/dL (3/55 patients, 5%; relative risk 2.3; 95% CI 0.7, 7.1).These variables were not independent correlates of cardiaccomplications in the multivariate analysis within the validationcohort (adjusted OR 1.0 and 0.9, respectively), but theORs for major cardiac complications for these 2 variableswere not significantly different in derivation and validationcohorts.Within the validation cohort, comparisons of areas underthe ROC indicated better diagnostic performance of theRevised Cardiac Risk Index compared with the prior decisionaids (all P0.01). The Revised Cardiac Risk Index was alsocompared with a prior index for patients undergoing vascularsurgery. 2 ROC analysis indicated superior diagnostic performanceof the Revised Cardiac Risk Index in the entire patientpopulation (0.7770.023 versus 0.6450.032; P0.0001),in the validation cohort (0.8060.034 versus 0.6080.056;P0.001), and in the subset of patients undergoing vascularsurgery (0.7740.032 versus 0.6830.046; P0.05). Neitherof these indexes performed well among patients undergoingabdominal aortic aneurysm surgery (0.5430.092 forRevised Cardiac Risk Index versus 0.4840.074 for thevascular surgery index; P0.30).Finally, a version of the Revised Cardiac Risk Index with onlythe 4 variables with independent associations with complicationsin the validation cohort (excluding diabetes and renal function)yielded slightly superior diagnostic performance compared withthe 6-variable model. Complication rates in patients with none,1, 2, or more of these variables were 0.4% (2/493), 1.0% (6/579),7% (19/270), and 11% (9/80).Performance by Procedure TypePatients from both the derivation and validation cohorts werepooled for an analysis of the performance of the RevisedCardiac Risk Index within types of procedures (Figure).Except for patients undergoing abdominal aortic aneurysmsurgery, there were significant (P0.05) trends towardgreater rates of cardiac complications within higher-riskclasses within all procedure types.DiscussionIn this report of the risk of major cardiac complications withmajor nonemergent noncardiac surgery, 6 factors with approximatelyequal prognostic importance were identified. Thepresence of 2 of these factors identified patients withmoderate (7%) and high (11%) complication rates in prospectiveevaluation among 1422 patients in the validation cohort.These findings are consistent with prior research andguidelines 5,8 that have emphasized the value of clinical datain perioperative risk stratification. Other investigations havealso found increased risk among patients with cardiovasculardisease or diabetes mellitus 1,2,8,11 or with certain classes ofprocedures. 6 <strong>Ho</strong>wever, several previously identified risk factors,including advanced age, critical aortic valvular stenosis,and abnormal cardiac rhythms, did not correlate with complicationsin the present study. This finding may reflectpatient selection and increased attention to these issues.Therefore, the absence of these factors from the RevisedCardiac Risk Index should not be taken as evidence that theyare not worrisome prognostic factors; indeed, they might beimportant predictors in patients undergoing emergentoperations.There was no relationship between risk class and majorcardiac complications among the patients who underwentabdominal aortic aneurysm surgery. Because there were only110 patients who underwent this procedure in the derivationcohort, statistical power was limited in these analyses.The form and content of the Revised Cardiac Risk Indexreflect the goal of this investigation: to derive a simple indexthat might influence and be readily incorporated into routinepractice (eg, on forms for preoperative evaluations). Wetherefore emphasized in the analyses dichotomous variablesthat were either present or absent and used a scoring systemthat assigned 1 point to each variable. A more complex indexmight have achieved greater accuracy but at the expense ofease of use.<strong>Ho</strong>w the Revised Cardiac Risk Index should be used byclinicians remains to be defined. One approach is to confineroutine use of noninvasive testing to patients with moderaterisk for complications (eg, classes III or IV). 3 An alternativestrategy has been suggested by Bodenheimer, 12 who arguesthat improved outcomes are more likely to result fromcontrolling postoperative oxygen demand than additional riskstratification. This approach would support use of this indexto identify patients who should be treated with strategies toreduce oxygen consumption rather than undergo additionalnoninvasive testing.The findings from the present report should be interpretedin the context of the study design. The data were collectedfrom patients undergoing nonemergent operations at a singleteaching hospital. The Revised Cardiac Risk Index is ofuncertain generalizability in lower-risk populations, such aspatients who undergo more minor procedures, or in high-riskpopulations, such as those who undergo emergency operations.<strong>Ho</strong>wever, patients undergoing major nonemergent proceduresconstitute the population in which physicians mostoften have to consider additional testing or other strategiesbefore the patient proceeds to surgery. Other clinical factorsnot included in this index may be important for predictinglong-term prognosis and warrant attention by clinicians.Finally, although this cohort is perhaps the largest to bestudied prospectively for predictors of cardiac complicationsassociated with noncardiac surgery, the statistical power toidentify predictors of complications among specific patientsubsets was limited.Nevertheless, these findings are consistent with priorresearch, and the Revised Cardiac Risk Index appears simpleenough for easy application in patient care. Previouslypublished data on a subset of this cohort demonstrate thatpatients with at least 3 of the factors in the Revised CardiacRisk Index (history of ischemic heart disease, history ofcongestive heart failure, and diabetes mellitus) have anincreased risk for cardiovascular complications during thenext 6 months, even if they do not have major perioperativecardiac complications. 13 Hence, patients with increased perioperativerisk probably warrant closer clinical attention wellbeyond their hospital admission.Downloaded from circ.ahajournals.org at UNIV MASSACHUSETTS on January 18, 2010