Concurrent validity of the parent-completed Ages and Stages ...
Concurrent validity of the parent-completed Ages and Stages ...
Concurrent validity of the parent-completed Ages and Stages ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Child: care, health <strong>and</strong> development<br />
Original Article doi:10.1111/j.1365-2214.2009.01041.x<br />
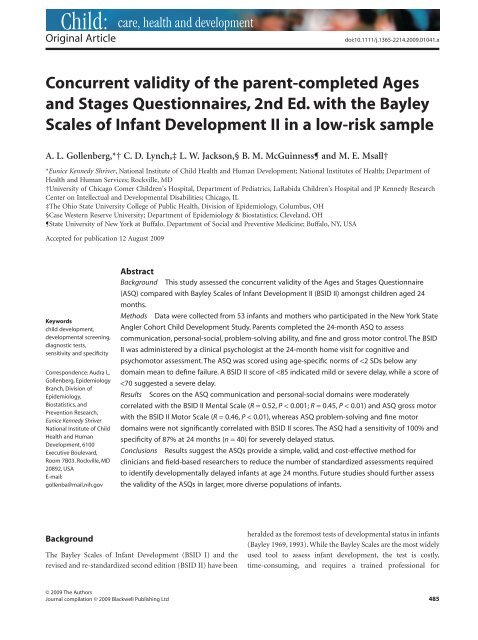
<strong>Concurrent</strong> <strong>validity</strong> <strong>of</strong> <strong>the</strong> <strong>parent</strong>-<strong>completed</strong> <strong>Ages</strong><br />
<strong>and</strong> <strong>Stages</strong> Questionnaires, 2nd Ed. with <strong>the</strong> Bayley<br />
Scales <strong>of</strong> Infant Development II in a low-risk sample<br />
A. L. Gollenberg,*† C. D. Lynch,‡ L. W. Jackson,§ B. M. McGuinness¶ <strong>and</strong> M. E. Msall†<br />
*Eunice Kennedy Shriver, National Institute <strong>of</strong> Child Health <strong>and</strong> Human Development; National Institutes <strong>of</strong> Health; Department <strong>of</strong><br />
Health <strong>and</strong> Human Services; Rockville, MD<br />
†University <strong>of</strong> Chicago Comer Children’s Hospital, Department <strong>of</strong> Pediatrics, LaRabida Children’s Hospital <strong>and</strong> JP Kennedy Research<br />
Center on Intellectual <strong>and</strong> Developmental Disabilities; Chicago, IL<br />
‡The Ohio State University College <strong>of</strong> Public Health, Division <strong>of</strong> Epidemiology, Columbus, OH<br />
§Case Western Reserve University; Department <strong>of</strong> Epidemiology & Biostatistics; Clevel<strong>and</strong>, OH<br />
¶State University <strong>of</strong> New York at Buffalo. Department <strong>of</strong> Social <strong>and</strong> Preventive Medicine; Buffalo, NY, USA<br />
Accepted for publication 12 August 2009<br />
Keywords<br />
child development,<br />
developmental screening,<br />
diagnostic tests,<br />
sensitivity <strong>and</strong> specificity<br />
Correspondence: Audra L.<br />
Gollenberg, Epidemiology<br />
Branch, Division <strong>of</strong><br />
Epidemiology,<br />
Biostatistics, <strong>and</strong><br />
Prevention Research,<br />
Eunice Kennedy Shriver<br />
National Institute <strong>of</strong> Child<br />
Health <strong>and</strong> Human<br />
Development, 6100<br />
Executive Boulevard,<br />
Room 7B03. Rockville, MD<br />
20892, USA<br />
E-mail:<br />
gollenba@mail.nih.gov<br />
Background<br />
Abstractcch_1041 485..490<br />
Background This study assessed <strong>the</strong> concurrent <strong>validity</strong> <strong>of</strong> <strong>the</strong> <strong>Ages</strong> <strong>and</strong> <strong>Stages</strong> Questionnaire<br />
(ASQ) compared with Bayley Scales <strong>of</strong> Infant Development II (BSID II) amongst children aged 24<br />
months.<br />
Methods Data were collected from 53 infants <strong>and</strong> mo<strong>the</strong>rs who participated in <strong>the</strong> New York State<br />
Angler Cohort Child Development Study. Parents <strong>completed</strong> <strong>the</strong> 24-month ASQ to assess<br />
communication, personal-social, problem-solving ability, <strong>and</strong> fine <strong>and</strong> gross motor control. The BSID<br />
II was administered by a clinical psychologist at <strong>the</strong> 24-month home visit for cognitive <strong>and</strong><br />
psychomotor assessment. The ASQ was scored using age-specific norms <strong>of</strong>
486 A.L. Gollenberg et al.<br />
administration. A screening instrument that can be administered<br />
by <strong>parent</strong>s may alleviate problems with <strong>the</strong> implementation<br />
<strong>of</strong> more costly screening programmes, like <strong>the</strong> BSID II. The<br />
<strong>Ages</strong> <strong>and</strong> <strong>Stages</strong> Questionnaires (ASQs) are a <strong>parent</strong>-<strong>completed</strong><br />
developmental monitoring system for screening large numbers<br />
<strong>of</strong> children with ease <strong>of</strong> administration, low cost, <strong>and</strong> suitability<br />
for diverse populations (Squires et al. 1999; Hix-Small et al.<br />
2007).<br />
While <strong>the</strong> ASQs have been validated against <strong>the</strong> BSID <strong>and</strong><br />
o<strong>the</strong>r st<strong>and</strong>ardized tests (Squires et al. 1997, 1998; Skellern et al.<br />
2001), a validation <strong>of</strong> <strong>the</strong> ASQs has not been conducted exclusively<br />
against <strong>the</strong> BSID II. However, one study validated <strong>the</strong><br />
ASQs against a combination <strong>of</strong> multiple developmental examinations,<br />
one <strong>of</strong> which was <strong>the</strong> BSID II (Yu et al. 2007). As part <strong>of</strong><br />
a population-based longitudinal study <strong>of</strong> infant health <strong>and</strong><br />
development, we had <strong>the</strong> opportunity to assess <strong>the</strong> <strong>validity</strong> <strong>of</strong><br />
<strong>the</strong> 24-month ASQ as compared with <strong>the</strong> BSID II amongst<br />
children aged 24 months.<br />
Methods<br />
Study population<br />
We used data from infants born to mo<strong>the</strong>rs who participated<br />
in <strong>the</strong> New York State Angler Cohort Prospective Pregnancy<br />
Study (NYSAC PPS) from 1998–2002 (Senn et al. 2005). At<br />
<strong>the</strong> time <strong>of</strong> post-partum blood collection, a research nurse<br />
informed mo<strong>the</strong>rs <strong>of</strong> <strong>the</strong> prospective child development study<br />
(NYSAC CDS) <strong>and</strong> requested informed consent for <strong>the</strong>ir<br />
child’s participation. Because <strong>of</strong> a lag in funding, some children<br />
were asked to participate after this time frame, but before<br />
<strong>the</strong>y reached age two. Data were collected via monthly diaries<br />
<strong>and</strong> ASQs, 2nd edition, <strong>completed</strong> by <strong>parent</strong>s or primary caregivers.<br />
Parents <strong>completed</strong> <strong>the</strong> ASQs, 2nd edition, at various<br />
time points, including at age 24 months for <strong>the</strong> assessment <strong>of</strong><br />
communication, socialization, fine motor control, gross motor<br />
control, <strong>and</strong> problem-solving ability. St<strong>and</strong>ardized physical,<br />
psychological, <strong>and</strong> developmental assessments were conducted<br />
by a clinical psychologist, research nurse, <strong>and</strong> developmental<br />
paediatrician during home visits at 12 <strong>and</strong> 24 months <strong>of</strong> age.<br />
The BSID II was administered to all children by <strong>the</strong> same<br />
clinical psychologist at both home visits to assess cognitive <strong>and</strong><br />
psychomotor development <strong>and</strong> behavioural status within �2<br />
weeks <strong>of</strong> <strong>the</strong> ASQ administration. The BSID II has three components,<br />
<strong>the</strong> mental scale, <strong>the</strong> motor scale, <strong>and</strong> <strong>the</strong> behaviour<br />
rating scale (BRS). The mental <strong>and</strong> motor scales are administered<br />
via a series <strong>of</strong> questions <strong>and</strong> observations conducted by a<br />
trained pr<strong>of</strong>essional. Raw scores for <strong>the</strong> mental <strong>and</strong> motor scales<br />
are converted to a st<strong>and</strong>ardized index for each age group with a<br />
mean <strong>of</strong> 100 <strong>and</strong> st<strong>and</strong>ard deviation (SD) <strong>of</strong> 15, termed <strong>the</strong><br />
Mental Development Index (MDI) <strong>and</strong> <strong>the</strong> Psychomotor Development<br />
Index (PDI), respectively. The BRS accounts for behavioural<br />
aspects <strong>of</strong> <strong>the</strong> infant during <strong>the</strong> testing session that may<br />
have affected cognitive performance, but is not used for screening<br />
purposes (Bayley 1993).<br />
In addition, <strong>the</strong> study psychologist administered <strong>the</strong><br />
Kaufman Brief Intelligence Test to mo<strong>the</strong>rs at <strong>the</strong> 12- or<br />
24-month home visit to ensure <strong>the</strong> participating <strong>parent</strong>s did not<br />
have a significant cognitive limitation. Gestational age at delivery<br />
was calculated by subtracting <strong>the</strong> last menstrual period date<br />
that was collected during <strong>the</strong> NYSAC PPS from <strong>the</strong> date <strong>of</strong><br />
delivery (Senn et al. 2005). Infant birthweight was self-reported<br />
by <strong>the</strong> mo<strong>the</strong>r at <strong>the</strong> first follow-up visit.<br />
Data analysis<br />
© 2009 The Authors<br />
Journal compilation © 2009 Blackwell Publishing Ltd, Child: care, health <strong>and</strong> development, 36, 4, 485–490<br />
Due to <strong>the</strong> missing data for <strong>the</strong> 12-month assessment resulting<br />
from <strong>the</strong> funding lag, we limited our analysis to data collected at<br />
<strong>the</strong> 24-month assessment. Agreement between <strong>the</strong> ASQs, 2nd<br />
edition, <strong>and</strong> BSID II was determined by computing Spearman<br />
rank-order correlation coefficients for ASQ domain scores<br />
versus relevant BSID II mental <strong>and</strong> motor scores, as <strong>the</strong> data<br />
were not normally distributed. ASQ communication, problemsolving,<br />
<strong>and</strong> personal/social domains were compared with <strong>the</strong><br />
BSID II MDI, <strong>and</strong> ASQ gross motor <strong>and</strong> fine motor domains<br />
were compared with <strong>the</strong> BSID II PDI.<br />
Overall <strong>validity</strong> <strong>of</strong> <strong>the</strong> ASQ, 2nd edition compared with <strong>the</strong><br />
BSID II was determined by comparing pass/fail status on each<br />
test. The ASQs were scored according to <strong>the</strong> manual (Squires<br />
et al. 1999) using age-specific norms <strong>of</strong> less than two SDs below<br />
<strong>the</strong> mean <strong>of</strong> any domain to define a failure. Failure on <strong>the</strong> BSID<br />
II MDI <strong>and</strong> PDI was defined by two cut points based on an<br />
age-st<strong>and</strong>ardized normal distribution <strong>of</strong> scores: a score <strong>of</strong> less<br />
than one SD below <strong>the</strong> mean (i.e.
except for those infants who are born
488 A.L. Gollenberg et al.<br />
Table 2. Cutpoints, median scores, <strong>and</strong> ranges for <strong>the</strong> <strong>Ages</strong> <strong>and</strong> <strong>Stages</strong><br />
Questionnaire (ASQ) domains <strong>and</strong> Bayley Scales <strong>of</strong> Infant Development<br />
II (BSID II) indices at age 24 months, New York State Angler Cohort<br />
Child Development Study (n = 40), 1998–2002<br />
24 Month assessment<br />
Pass/fail cutpoint Median Range<br />
ASQ<br />
Gross motor 36.0 60 0–60<br />
Fine motor 36.4 55 25–60<br />
Communication 36.5 60 25–60<br />
Problem-solving 32.9 50 10–60<br />
Personal/social<br />
BSID II*<br />
35.6 55 10–60<br />
Mental Index (MDI) 85; 70 98 50–140<br />
Psychomotor Index (PDI) 85; 70 96 50–110<br />
*BSID II indices have two cut points:
is developing at a typical rate, while those who fail an ASQ<br />
domain might be in need <strong>of</strong> developmental follow-up. Given<br />
<strong>the</strong> low PPV, some children who screen positive with <strong>the</strong> ASQ<br />
will be found upon fur<strong>the</strong>r testing to be developing typically.<br />
However, over-referrals in screening programmes are not<br />
necessarily a problem <strong>and</strong> can provide an opportunity to assess<br />
children’s needs for improvement as this group (i.e. falsepositives)<br />
tends to score on <strong>the</strong> lower range <strong>of</strong> screening tools<br />
<strong>and</strong> come from disadvantaged backgrounds (Glascoe 2001). To<br />
this end, <strong>the</strong> use <strong>of</strong> ASQs as a screening tool will decrease <strong>the</strong><br />
number <strong>of</strong> children requiring a full developmental assessment<br />
resulting in a cost-effective screening programme.<br />
The negligible correlation between <strong>the</strong> ASQ fine motor<br />
domain <strong>and</strong> <strong>the</strong> BSID II motor scale at 24 months was unexpected.<br />
However, previous studies have speculated <strong>the</strong> BSID II is<br />
less appropriate for assessing fine motor skills as compared with<br />
gross motor skills based on <strong>the</strong> number <strong>of</strong> applicable questions<br />
(Bayley 1993; Liao et al. 2005). Fur<strong>the</strong>rmore, <strong>the</strong> Yu et al. ASQ<br />
validation study found similar results in that <strong>the</strong> fine motor <strong>and</strong><br />
problem-solving domains contributed little to neurosensory<br />
disability detection (Yu et al. 2007), as compared with <strong>the</strong> o<strong>the</strong>r<br />
ASQ domains.<br />
The two main limitations <strong>of</strong> our study are <strong>the</strong> homogenous<br />
nature <strong>of</strong> <strong>the</strong> study population <strong>and</strong> <strong>the</strong> modest sample size <strong>of</strong> a<br />
low-risk nature. Given that <strong>the</strong> mo<strong>the</strong>rs <strong>of</strong> our study participants<br />
were white, married, <strong>and</strong> <strong>of</strong> middle to upper socioeconomic<br />
status, it was not unexpected that <strong>the</strong> distribution <strong>of</strong><br />
scores was restricted to <strong>the</strong> medium/high range on both screening<br />
tools. This may explain, in part, why so few infants failed<br />
both tests, thus limiting our ability to calculate sensitivity <strong>and</strong><br />
positive predictive value with great precision. However, since<br />
<strong>the</strong> prevalence <strong>of</strong> severe developmental delay in our study (5%)<br />
is similar to that reported by o<strong>the</strong>rs (3.5–6.5%) (Boyle et al.<br />
1994), our findings are likely generalizable to o<strong>the</strong>r low-risk US<br />
populations. While our sample size was small, a comparison <strong>of</strong><br />
selected characteristics <strong>of</strong> those included in <strong>the</strong> analysis <strong>and</strong><br />
those without assessments showed that <strong>the</strong>re were no significant<br />
differences between <strong>the</strong> groups at 24 months. Given <strong>the</strong> high<br />
costs associated with conducting in-home st<strong>and</strong>ardized assessments<br />
like <strong>the</strong> BSID II, it is not uncommon for validation<br />
studies to report small sample sizes (Skellern et al. 2001; Voigt<br />
et al. 2003; Johnson et al. 2004; Liao et al. 2005). Never<strong>the</strong>less,<br />
our findings should be interpreted with caution <strong>and</strong> should<br />
serve as an impetus for additional work in this area.<br />
It should be noted that while <strong>the</strong> BSID III became available in<br />
2006, <strong>the</strong>y do not yet appear to be widely used (Bayley 2006). In<br />
addition to providing a new overall growth score, <strong>the</strong> main<br />
difference between <strong>the</strong> BSID II <strong>and</strong> <strong>the</strong> BSID III is that <strong>the</strong> BSID<br />
III was renormed to include clinical cases in <strong>the</strong> normative<br />
sample (Bayley 2006). It has been reported that overall <strong>the</strong> BSID<br />
III index scores have been found to be 7 points higher on<br />
average as compared with <strong>the</strong> BSID II scores (likely due to <strong>the</strong><br />
renorming) (Bayley 2006).<br />
We did not formally examine intra-rater reliability for<br />
administration <strong>of</strong> <strong>the</strong> BSID II. However, one highly trained<br />
clinical psychologist administered <strong>the</strong> BSID II to all children;<br />
<strong>the</strong>refore, we do not believe that reliability was an issue in this<br />
study.<br />
In conclusion, our findings suggest that <strong>the</strong> ASQs are a valid<br />
screening tool for <strong>the</strong> identification <strong>of</strong> infants with a severe<br />
developmental delay at 24 months <strong>of</strong> age. The 24-month ASQ<br />
provides a simple, cost-effective alternative to formal st<strong>and</strong>ardized<br />
assessments for use in both screening programmes <strong>and</strong><br />
field-based research. Results <strong>of</strong> this study suggest that fur<strong>the</strong>r<br />
assessment <strong>of</strong> ASQ <strong>validity</strong> in larger, more diverse populations<br />
<strong>of</strong> infants is warranted.<br />
Acknowledgements<br />
This work was supported, in part, by grants from <strong>the</strong> Great<br />
Lakes Protection Fund (RM 791-3021), <strong>the</strong> Agency for Toxic<br />
Substances <strong>and</strong> Disease Registry (H75/ATH 298328), <strong>and</strong> <strong>the</strong><br />
Gerber Foundation as well as intramural funds from <strong>the</strong> Eunice<br />
Kennedy Shriver National Institute <strong>of</strong> Child Health <strong>and</strong> Human<br />
Development, National Institutes <strong>of</strong> Health.<br />
References<br />
Validity <strong>of</strong> <strong>Ages</strong> <strong>and</strong> <strong>Stages</strong> Questionnaires vs. BSID II 489<br />
Key messages<br />
The American Academy <strong>of</strong> Pediatrics recommends periodic<br />
screening for developmental delay.<br />
The ASQs may be more effective at screening for severe<br />
delays ra<strong>the</strong>r than mild developmental delays.<br />
The ASQs are a valid <strong>and</strong> cost-effective screening tool for<br />
developmental delay at age 24 months.<br />
Allen, M. C. & Alex<strong>and</strong>er, G. R. (1990) Gross motor milestones in<br />
preterm infants: correction for degree <strong>of</strong> prematurity. Jornal De<br />
Pediatria, 116, 955–959.<br />
Bayley, N. (1969) Bayley Scales <strong>of</strong> Infant Development. Psychological<br />
Corporation, New York.<br />
© 2009 The Authors<br />
Journal compilation © 2009 Blackwell Publishing Ltd, Child: care, health <strong>and</strong> development, 36, 4, 485–490
490 A.L. Gollenberg et al.<br />
Bayley, N. (1993) Bayley II PSychological Corporation, San Antonio.<br />
Bayley, N. (2006) Bayley Scales <strong>of</strong> Infant <strong>and</strong> Toddler Development,<br />
3rd edn. Pearson Education, Inc, San Antonio, TX.<br />
Boyle, C. A., Decoufle, P. & Yeargin-Allsop, M. (1994) Prevalence <strong>and</strong><br />
health impact <strong>of</strong> developmental disabilities in U.S. children.<br />
Pediatrics, 93, 399–403.<br />
Den, O. L., Rijken, M., Br<strong>and</strong>, R., Verloove-Vanhorick, S. P. & Ruys,<br />
J. H. (1991) Is it correct to correct? Developmental milestones in<br />
555 ‘normal’ preterm infants compared with term infants. Jornal<br />
De Pediatria, 118, 399–404.<br />
Dobrez, D., Sasso, A. L., Holl, J., Shalowitz, M., Leon, S. & Budetti, P.<br />
(2001) Estimating <strong>the</strong> cost <strong>of</strong> developmental <strong>and</strong> behavioral<br />
screening <strong>of</strong> preschool children in general pediatric practice.<br />
Pediatrics, 108, 913–922.<br />
Glascoe, F. P. (2001) Are overreferrals on developmental screening<br />
tests really a problem? Archives <strong>of</strong> Pediatrics & Adolescent Medicine,<br />
155, 54–59.<br />
Hix-Small, H., Marks, K., Squires, J. & Nickel, R. (2007) Impact <strong>of</strong><br />
implementing developmental screening at 12 <strong>and</strong> 24 months in a<br />
pediatric practice. Pediatrics, 120, 381–389.<br />
Johnson, S., Marlow, N., Wolke, D., Davidson, L., Marston, L.,<br />
O’Hare, A., Peacock, J. & Schulte, J. (2004) Validation <strong>of</strong> a <strong>parent</strong><br />
report measure <strong>of</strong> cognitive development in very preterm infants.<br />
Developmental Medicine <strong>and</strong> Child Neurology, 46, 389–397.<br />
Liao, H. F., Wang, T. M., Yao, G. & Lee, W. T. (2005) <strong>Concurrent</strong><br />
<strong>validity</strong> <strong>of</strong> <strong>the</strong> comprehensive developmental inventory for infants<br />
<strong>and</strong> toddlers with <strong>the</strong> bayley scales <strong>of</strong> infant development-II in<br />
preterm infants. Journal <strong>of</strong> <strong>the</strong> Formosan Medical Association, 104,<br />
731–737.<br />
Miller, G., Dubowitz, L. M. & Palmer, P. (1984) Follow-up <strong>of</strong><br />
pre-term infants: is correction <strong>of</strong> <strong>the</strong> developmental quotient<br />
for prematurity helpful? Early Human Development, 9,<br />
137–144.<br />
Restiffe, A. P. & Gherpelli, J. L. (2006) Comparison <strong>of</strong> chronological<br />
<strong>and</strong> corrected ages in <strong>the</strong> gross motor assessment <strong>of</strong> low-risk<br />
preterm infants during <strong>the</strong> first year <strong>of</strong> life. Arquivos De<br />
Neuro-Psiquiatria, 64, 418–425.<br />
© 2009 The Authors<br />
Journal compilation © 2009 Blackwell Publishing Ltd, Child: care, health <strong>and</strong> development, 36, 4, 485–490<br />
Senn, K. M., McGuiness, B. M., Buck, G. M., Vena, J. E., Anderson, S.<br />
& Rogers, B. T. (2005) Longitudinal study <strong>of</strong> babies born to<br />
mo<strong>the</strong>rs enrolled in a preconception prospective pregnancy study:<br />
study design <strong>and</strong> methodology, New York State Angler Cohort<br />
Study. Environmental Research, 97, 163–169.<br />
Siegel, L. S. (1983) Correction for prematurity <strong>and</strong> its consequences<br />
for <strong>the</strong> assessment <strong>of</strong> <strong>the</strong> very low birth weight infant. Child<br />
Development, 54, 1176–1188.<br />
Skellern, C. Y., Rogers, Y. & O’Callaghan, M. J. (2001) A<br />
<strong>parent</strong>-<strong>completed</strong> developmental questionnaire: follow up <strong>of</strong><br />
ex-premature infants. Journal <strong>of</strong> Paediatrics <strong>and</strong> Child Health, 37,<br />
125–129.<br />
Squires, J., Bricker, D. & Potter, L. (1997) Revision <strong>of</strong> a<br />
<strong>parent</strong>-<strong>completed</strong> development screening tool: ages <strong>and</strong> stages<br />
questionnaires. Journal <strong>of</strong> Pediatric Psychology, 22, 313–328.<br />
Squires, J., Potter, L., Bricker, D. & Lamorey, S. (1998)<br />
Parent-<strong>completed</strong> developmental questionnaires: effectiveness with<br />
low <strong>and</strong> middle income <strong>parent</strong>s. Early Childhood Research<br />
Quarterly, 13, 345–354.<br />
Squires, J., Potter, L. & Bricker, D. (1999) The <strong>Ages</strong> <strong>and</strong> <strong>Stages</strong> User’s<br />
Guide. Paul H. Brookes Publishing Co., Baltimore.<br />
Vincer, M. J., Cake, H., Graven, M., Dodds, L., McHugh, S. &<br />
Fraboni, T. (2005) A population-based study to determine <strong>the</strong><br />
performance <strong>of</strong> <strong>the</strong> Cognitive Adaptive Test/Clinical linguistic <strong>and</strong><br />
auditory milestone scale to predict <strong>the</strong> mental developmental index<br />
at 18 months on <strong>the</strong> bayley scales <strong>of</strong> infant development-II in very<br />
preterm infants. Pediatrics, 116, e864–e867.<br />
Voigt, R. G., Brown, F. R., III, Fraley, J. K., Llorente, A. M., Rozelle, J.,<br />
Turcich, M., Jensen, C. L. & Heird, W. C. (2003) <strong>Concurrent</strong> <strong>and</strong><br />
predictive <strong>validity</strong> <strong>of</strong> <strong>the</strong> cognitive adaptive test/clinical linguistic<br />
<strong>and</strong> auditory milestone scale (CAT/CLAMS) <strong>and</strong> <strong>the</strong> Mental<br />
Developmental Index <strong>of</strong> <strong>the</strong> Bayley Scales <strong>of</strong> Infant Development.<br />
Clinical Pediatrics, 42, 427–432.<br />
Yu, L. M., Hey, E., Doyle, L. W., Farrell, B., Spark, P., Altman, D. G. &<br />
Duley, L. (2007) Evaluation <strong>of</strong> <strong>the</strong> ages <strong>and</strong> stages questionnaires<br />
in identifying children with neurosensory disability in <strong>the</strong> magpie<br />
trial follow-up study. Acta Paediatrica, 96, 1803–1808.