Obsessive-Compulsive Disorder: Diagnosis and Management
Obsessive-Compulsive Disorder: Diagnosis and Management
Obsessive-Compulsive Disorder: Diagnosis and Management
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
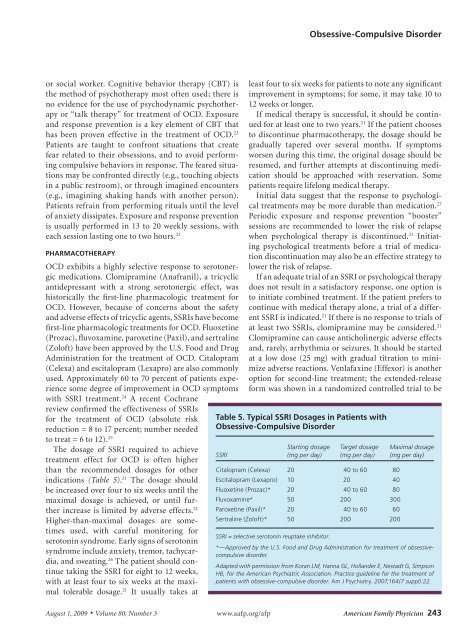
<strong>Obsessive</strong>-<strong>Compulsive</strong> <strong>Disorder</strong>or social worker. Cognitive behavior therapy (CBT) isthe method of psychotherapy most often used; there isno evidence for the use of psychodynamic psychotherapyor “talk therapy” for treatment of OCD. Exposure<strong>and</strong> response prevention is a key element of CBT thathas been proven effective in the treatment of OCD. 23Patients are taught to confront situations that createfear related to their obsessions, <strong>and</strong> to avoid performingcompulsive behaviors in response. The feared situationsmay be confronted directly (e.g., touching objectsin a public restroom), or through imagined encounters(e.g., imagining shaking h<strong>and</strong>s with another person).Patients refrain from performing rituals until the levelof anxiety dissipates. Exposure <strong>and</strong> response preventionis usually performed in 13 to 20 weekly sessions, witheach session lasting one to two hours. 21PHARMACOTHERAPYOCD exhibits a highly selective response to serotonergicmedications. Clomipramine (Anafranil), a tricyclicantidepressant with a strong serotonergic effect, washistorically the first-line pharmacologic treatment forOCD. However, because of concerns about the safety<strong>and</strong> adverse effects of tricyclic agents, SSRIs have becomefirst-line pharmacologic treatments for OCD. Fluoxetine(Prozac), fluvoxamine, paroxetine (Paxil), <strong>and</strong> sertraline(Zoloft) have been approved by the U.S. Food <strong>and</strong> DrugAdministration for the treatment of OCD. Citalopram(Celexa) <strong>and</strong> escitalopram (Lexapro) are also commonlyused. Approximately 60 to 70 percent of patients experiencesome degree of improvement in OCD symptomswith SSRI treatment. 24 A recent Cochranereview confirmed the effectiveness of SSRIsfor the treatment of OCD (absolute riskreduction = 8 to 17 percent; number neededto treat = 6 to 12). 25The dosage of SSRI required to achievetreatment effect for OCD is often higherthan the recommended dosages for otherindications (Table 5). 21 The dosage shouldbe increased over four to six weeks until themaximal dosage is achieved, or until furtherincrease is limited by adverse effects. 21Higher-than-maximal dosages are sometimesused, with careful monitoring forserotonin syndrome. Early signs of serotoninsyndrome include anxiety, tremor, tachycardia,<strong>and</strong> sweating. 26 The patient should continuetaking the SSRI for eight to 12 weeks,with at least four to six weeks at the maximaltolerable dosage. 21 It usually takes atleast four to six weeks for patients to note any significantimprovement in symptoms; for some, it may take 10 to12 weeks or longer.If medical therapy is successful, it should be continuedfor at least one to two years. 21 If the patient choosesto discontinue pharmacotherapy, the dosage should begradually tapered over several months. If symptomsworsen during this time, the original dosage should beresumed, <strong>and</strong> further attempts at discontinuing medicationshould be approached with reservation. Somepatients require lifelong medical therapy.Initial data suggest that the response to psychologicaltreatments may be more durable than medication. 27Periodic exposure <strong>and</strong> response prevention “booster”sessions are recommended to lower the risk of relapsewhen psychological therapy is discontinued. 21 Initiatingpsychological treatments before a trial of medicationdiscontinuation may also be an effective strategy tolower the risk of relapse.If an adequate trial of an SSRI or psychological therapydoes not result in a satisfactory response, one option isto initiate combined treatment. If the patient prefers tocontinue with medical therapy alone, a trial of a differentSSRI is indicated. 21 If there is no response to trials ofat least two SSRIs, clomipramine may be considered. 21Clomipramine can cause anticholinergic adverse effects<strong>and</strong>, rarely, arrhythmia or seizures. It should be startedat a low dose (25 mg) with gradual titration to minimizeadverse reactions. Venlafaxine (Effexor) is anotheroption for second-line treatment; the extended-releaseform was shown in a r<strong>and</strong>omized controlled trial to beTable 5. Typical SSRI Dosages in Patients with<strong>Obsessive</strong>-<strong>Compulsive</strong> <strong>Disorder</strong>SSRIStarting dosage(mg per day)Target dosage(mg per day)Citalopram (Celexa) 20 40 to 60 80Escitalopram (Lexapro) 10 20 40Fluoxetine (Prozac)* 20 40 to 60 80Fluvoxamine* 50 200 300Paroxetine (Paxil)* 20 40 to 60 60Sertraline (Zoloft)* 50 200 200SSRI = selective serotonin reuptake inhibitor.Maximal dosage(mg per day)*—Approved by the U.S. Food <strong>and</strong> Drug Administration for treatment of obsessivecompulsivedisorder.Adapted with permission from Koran LM, Hanna GL, Holl<strong>and</strong>er E, Nestadt G, SimpsonHB, for the American Psychiatric Association. Practice guideline for the treatment ofpatients with obsessive-compulsive disorder. Am J Psychiatry. 2007;164(7 suppl):22.August 1, 2009 ◆ Volume 80, Number 3 www.aafp.org/afp American Family Physician 243