May08 VS.indd - Calgary & Area Physician's Association
May08 VS.indd - Calgary & Area Physician's Association
May08 VS.indd - Calgary & Area Physician's Association
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Vital Signs is published 11 times annually (not published<br />
in August) by the <strong>Calgary</strong> & <strong>Area</strong> Physician’s <strong>Association</strong><br />
(CAPA) in partnership with the <strong>Calgary</strong> Health Region.<br />
www.capa.cc<br />
Editors:<br />
Dave Lowery, CAPA – bethere@shaw.ca<br />
Joanne Anderson, <strong>Calgary</strong> Health Region<br />
–joanne.anderson@calgaryhealthregion.ca<br />
Editorial advisory board:<br />
Dr. Mark Joyce – mjoyce@ucalgary.ca<br />
Dr. Ian Wishart – ianwishart@shaw.ca<br />
Submissions:<br />
Vital Signs welcomes submissions (articles, notices,<br />
letters to the editors, announcements, photos, etc.)<br />
from physicians in the <strong>Calgary</strong> region and from <strong>Calgary</strong><br />
Health Region staff. Please limit articles to 600 words or<br />
less.<br />
Please send any contributions for the attention of:<br />
CAPA<br />
Dave Lowery: E-mail: bethere@shaw.ca, tel: 243-9498.<br />
<strong>Calgary</strong> Health Region<br />
Joanne Anderson:<br />
E-mail joanne.anderson@calgaryhealthregion.ca<br />
tel: 943-1257<br />
Vital Signs reserves the right to edit article submissions and<br />
letters to the editor.<br />
Deadline:<br />
The deadline for article submission to Vital Signs is the 15th<br />
day of the month for distribution the fi rst week of the following<br />
month.<br />
Next deadline is May 15, 2008.<br />
Contributors:<br />
The opinions expressed in Vital Signs are those of the<br />
authors and do not necessarily refl ect the opinions or<br />
positions of the CAPA, CAPA executive or the <strong>Calgary</strong> Health<br />
Region.<br />
CAPA executive - Please feel free to contact your<br />
representative with any concerns or issues.<br />
Dr. Linda Slocombe, CAPA president<br />
Phone: 861-8423<br />
Dr. D. Glenn Comm, CAPA past president<br />
Phone: 850-0718<br />
Dr. Corinne Dyke, CGH MSA president<br />
Phone 777-3009<br />
Dr. Brendan Hughes, CGH MSA vice president & treasurer<br />
Phone 943-5461<br />
Dr. Douglas Thorson, RGH MSA president & treasurer<br />
Phone 253-7355<br />
Dr. James Janzen, RGH MSA vice president<br />
Phone 943-3410<br />
Dr. Liam Martin, FMC MSA president & treasurer<br />
Phone: 220-7725<br />
Dr. Sean Grondin, FMC MSA vice president & treasurer<br />
Phone: 944-8798<br />
Dr. Jennifer R. MacPherson, ACH MSA president<br />
Phone: 252-6651<br />
Dr. Mark Montgomery, ACH vice-president & treasurer<br />
Phone: 955-7882<br />
Dr. Patti Edgar, rural MSA president<br />
Phone: 762-4846<br />
Dr. Grant Hill, rural MSA vice-president & treasurer<br />
Phone: 938-1424<br />
Dr. Blythe K. Brown, PCPA president<br />
Phone: 269-9488<br />
Dr. Stephanie Kozma, PCPA member at large<br />
Phone: 258-3000<br />
Dr. Phillip Van Der Merwe, PCN rep<br />
Phone: 640-4320<br />
Dr. Prem Chengalath, CAPA & PCPA VP & treasurer<br />
Phone: 241-8848<br />
Dr. Inderman, H. Jadusingh CMS representative<br />
Phone: 249-0611<br />
Dr. June Bergman, PCN rep<br />
Phone: 210-9200<br />
Contributing members<br />
Dr. David Megran, CMO<br />
Phone: 943-1180<br />
Dr. Peter Jamieson, chair, medical advisory board<br />
Phone: 943-1277<br />
Dr. Robin Cox, CPSA representative<br />
Phone: 943-7260<br />
Sean Smith, director, practice management program<br />
Phone: 266-3533<br />
Dr. Brock Debenham, PARA rep<br />
Phone: 456-4338<br />
Web site: www.capa.cc<br />
Administration offi ce phone: 943-1270<br />
Administration offi ce fax: 943-1297
Columns:<br />
May 2008<br />
From the president: Sustainability . . . the new buzz word --- 4<br />
Member business alliance (MBA) update ------------------------ 6<br />
Home care update -----------------------------------------------------11<br />
Features:<br />
Form is not a four-letter word ---------------------------------------- 7<br />
Region physician helps fl ood-ravaged African villages -------- 8<br />
News:<br />
Contents<br />
Debrief provides insight into region’s effectiveness ------------ 5<br />
Connecting the dots on capacity issues -------------------------- 5<br />
New collaborative care model planned for <strong>Calgary</strong> ------------ 6<br />
New physicians receive board approval ------------------------ 10<br />
Safety learning reporting system update ------------------------11<br />
Bulletins & notices ---------------------------------------------------- 12<br />
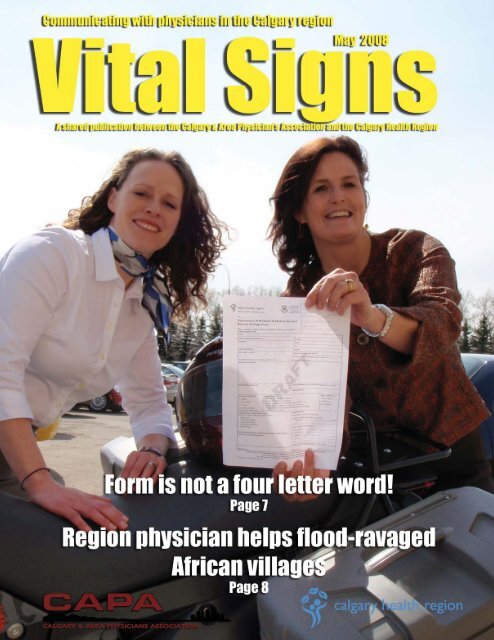
On the cover: Dr. Connie Ellis (right) with Shannon Erfl e<br />
and two “notorious” four-letter objects.<br />
Photo by Dave Lowery
Vital Signs May 2008 • Page 4<br />
From the CAPA president<br />
As you will read in this issue of Vital Signs, there is a new CHR<br />
initiative that is hoping to make form not the dreaded word it is now.<br />
Talk to any family doctor about forms and requisitions and you will<br />
likely get an earful. Talk to any specialist about the referral letters they<br />
get and you will likely also get an earful. The new medical access to<br />
services project is a good news story. At fi rst the 30 page instruction<br />
manual is a tad overwhelming but the end result is a simple one page<br />
referral form which can be used for referrals to most of the internal<br />
medicine specialities. The next challenge will be to expand this<br />
program to include other specialities and further decrease the burden<br />
of paperwork in the modern doctors offi ce. A laudable goal indeed!<br />
Since we are discussing the emotions a single word can convey,<br />
I would like to discuss the new buzzword in the medical lexicon –<br />
sustainability. We see this word being used almost ad nauseum by<br />
politicians and administrators alike. Do we really know what this<br />
word means? To quote Peter Foster in the Financial Post “it is the<br />
Orwellian dumber-down of debate.” This is certainly true in relation<br />
to healthcare. Who would advocate unsustainabililty? This brings me<br />
to the press release by the Alberta Government surrounding the action<br />
plan for healthcare. Who could argue with Minister Ron Liepert’s<br />
statement that “our top priority is to improve accessibility and the<br />
future sustainability of the health system. The outcome of the plan is a<br />
sustainable, effective and effi cient health system that provides quality<br />
patient-focused care to Albertans.”<br />
It was with real anticipation I looked forward to some concrete<br />
plans from the government to tackle the family medicine crisis,<br />
the unacceptable emergency room waits and the lack of long term<br />
care beds to name a few. Instead, we have future dates for future<br />
announcements. Funding appears to be a completely separate issue<br />
not necessarily tied to the action plans. And to use that ‘s’ word again,<br />
the provincial government has said that increases to the province’s<br />
health budget, which are often in the double digits, are not sustainable.<br />
Yet the calls for immediate action include expanding addiction and<br />
mental health services, expanding healthy lifestyle initiatives and<br />
expanding educational spaces for health care professionals. In fact, all<br />
of the calls for immediate action will involve increases in the current<br />
levels of funding. How does one promote a sustainable health system<br />
with unsustainable funding levels! The debate we should have is not<br />
whether we need a sustainable health care system but what does that<br />
mean and how do we get there.<br />
Sustainability . . . the new buzz word<br />
Dr. Linda Slocombe,<br />
CAPA president<br />
Phone: 861-8423
Debrief provides insight into region’s effectiveness<br />
By Carly Woolsey, CHR communications<br />
A recent debriefing session<br />
marked the end of the research phase<br />
and the beginning of the review<br />
process for the <strong>Calgary</strong> Health<br />
Region’s accreditation process. The Canadian Council on Health<br />
Services Accreditation (CCHSA) provided a general debrief on the<br />
results of its week-long survey where a group of health services<br />
experts assess the region on its quality and safety practices utilizing<br />
national standards.<br />
The debrief presentation provided a glimpse of the strengths and<br />
opportunities the surveyors identifi ed while speaking to front line<br />
staff, site managers, physicians, patients, corporate services and other<br />
support staff, administrators and board members.<br />
“The accreditation survey results show us what is relevant to the<br />
region today and where we are at right now, what we can do to improve<br />
and what processes are working for us,” says Val Austen-Wiebe,<br />
executive director, health outcomes.<br />
Some of the strengths identifi ed by the surveyors were related to<br />
the collaboration that they see taking place throughout the region in<br />
relation to patient fl ow and emergency preparedness. The surveyors<br />
remarked that they were impressed with programs such as chronic<br />
disease management, the patient/family safety council, and education<br />
By Carly Woolsey, CHR communications<br />
The <strong>Calgary</strong> Health Region’s<br />
GRIDLOCC (getting rid of<br />
inappropriate delays that limit our<br />
capacity to care) project celebrated<br />
its one year anniversary by refl ecting on what has been accomplished<br />
over the past year and evaluating where it is heading.<br />
The anniversary event, called Year One Review – Connecting the<br />
Dots, was held at the Red and White Club and was attended by over<br />
150 region staff and physicians. At the event, presentations were given<br />
on Lean Six Sigma initiatives that are part of the overall GRIDLOCC<br />
project.<br />
These presentations showcased how staff, physicians and quality<br />
improvement consultants have all worked together to address<br />
capacity issues faced by region sites. The Alberta Children’s Hospital<br />
emergency department team presented on their initiative which looked<br />
at decreasing the length of time it took for patients to see a physician<br />
upon entering the department by creating zones in the emergency<br />
department to stream patients. The Peter Lougheed Centre emergency<br />
department team also presented on their initiative to reduce the time<br />
and training efforts that reach deep into the organization such as the<br />
safety policy roll out.<br />
<strong>Area</strong>s identifi ed for improvement or continued focus include<br />
a region-wide review of the client consent form process to ensure<br />
compliance with region policies, and improved communication<br />
with staff and physicians on organizational issues such as capacity,<br />
access and ethics, particularly when ideas from front line staff are<br />
implemented .<br />
At the debrief, <strong>Calgary</strong> Health Region president and chief operating<br />
offi cer, Dr. Chris Eagle, said that the accreditation process is important<br />
because it is peer-reviewed learning.<br />
“Through this process we receive feedback on a lot of things to<br />
think about and improve upon. The <strong>Calgary</strong> Health Region appreciates<br />
the presence and efforts of the CCHSA surveyors as well as the<br />
participation of our staff in this process.”<br />
The accreditation process within the <strong>Calgary</strong> Health Region is a<br />
three-year sequential program which began in 1999. This year marks<br />
the beginning of a new three-year cycle. The fi nal report will be sent<br />
to the <strong>Calgary</strong> Health Region in six months.<br />
Connecting the dots on capacity issues<br />
it took to diagnose and discharge patients by streamlining the process<br />
to request old patient charts and reallocating physicians in minor<br />
treatment and RAZ (rapid access zone).<br />
The morning event was capped off by closing remarks from Dr.<br />
Rob Abernethy, vice president & associate chief medical offi cer for<br />
the <strong>Calgary</strong> Health Region. He spoke about tackling capacity issues<br />
within the region and the importance of staff and physician support<br />
of the overall GRIDLOCC project.<br />
“Our staff and physicians have risen to the occasion to make<br />
GRIDLOCC successful. It was done in the best interest of our patients<br />
and we couldn’t do it without the hard work of our frontline staff.”<br />
The upcoming year will see GRIDLOCC focus on key areas<br />
such as improving the physician consult process in the emergency<br />
department as well as spreading lean discharge best practices. An<br />
evaluation process will also take place that will look assess the success<br />
of initiatives that have taken place over the past year. This evaluation<br />
will help the regional capacity committee to focus on priority areas<br />
for improving access to services.<br />
Vital Signs May 2008 • Page 5
Vital Signs May 2008 • Page 6<br />
Member business alliance (MBA) update<br />
JustListed<strong>Calgary</strong> real estate team<br />
The JustListed<strong>Calgary</strong> real estate team is proud to partner with<br />
CAPA and offer its members substantial savings when buying and<br />
selling real estate. You will get all the benefi ts of an award winning<br />
team, extensive marketing plans, and most importantly, proven results<br />
well above the industry average. Savings in the 10-25% per cent range<br />
are being offered to all members who show their membership card.<br />
Please contact Mike Hannah with any questions or to obtain<br />
these substantial discounts.<br />
New collaborative care model planned for the <strong>Calgary</strong> Health Region<br />
By Janice Harvie, CHR communications<br />
Workforce shortages are<br />
wreaking havoc on the health care<br />
system. Some of the most visible<br />
effects are closed beds, dissatisfied patients and burned out,<br />
disillusioned staff.<br />
Aggressive recruitment and retention strategies are being<br />
implemented. In addition to ‘pumping up the volume’ with increased<br />
staff numbers, the <strong>Calgary</strong> Health Region will soon embark on a large<br />
scale system and culture change to deliver care via a collaborative<br />
care model that will ultimately take root in about 80 per cent of<br />
service areas.<br />
Dubbed the ‘workforce optimization initiative,’ the plan is to<br />
reorganize the workforce (where appropriate) to realize greater<br />
effi ciency and effectiveness in health services delivery. The initiative<br />
is fi scally neutral.<br />
“The literature supports this vision and we’ve brought a number<br />
of strategies and projects involving education, data profi ling, clinical<br />
leadership development, regulatory and HR changes and others under<br />
our umbrella to ensure the entire effort is coordinated and builds<br />
on existing good work,” says Dr. Jim Silvius, VP & associate chief<br />
medical offi cer responsible for patient care innovation and health<br />
technology, and a practicing geriatrician at Rockyview General<br />
Hospital. Dr. Silvius co-leads the initiative with Marilyn Visser,<br />
director interprofessional education and workforce utilization.<br />
The groundwork is about evaluating and addressing what’s<br />
preventing the system from working to the greatest benefi t of patients<br />
and providers. One of the key concepts within workforce optimization<br />
is collaborative practice, which represents (and requires) a major shift<br />
in thinking about our approach to patient care.<br />
“Collaborative practice is not just about practicing as a member of<br />
a team. Many of us would already say we are part of a team, but not<br />
many of us would say we work in the most effi cient system, particularly<br />
from the patient’s perspective,” says Silvius.<br />
Collaborative practice is a model in which everyone works to<br />
the full scope of their knowledge, skill and training in a process of<br />
continuous communication and shared decision-making that includes<br />
the patient and family, to achieve outcomes that could not be achieved<br />
by any one person working alone.<br />
What collaborative practice looks like in community care, in acute<br />
care and even for individual units or services is open for discussion.<br />
Because it is customizable to a certain extent in different settings,<br />
physicians are strongly encouraged to provide input when their units<br />
engage in the process and through unit councils.<br />
The implications of a new service model for physicians will be<br />
most evident in how and with whom they interact during the course<br />
of providing care. “We’ll still talk to the person most appropriate for<br />
giving or getting information about our patient, but that person may<br />
not always be the most senior nurse,” says Silvius. “We need to be part<br />
of the design in our areas because the number one principle of this is<br />
to better meet the needs of the patient. This process allows physicians<br />
to be part of developing how this is achieved in their area.”<br />
Admittedly, the collaborative practice model and other optimization<br />
strategies will not solve the region’s workforce issues. But it’s a vital<br />
step in the right direction. “Imagine how improved worklife could be<br />
if our system was functioning better, how much happier people would<br />
be if they were actually doing what they were trained to do and in a<br />
system that wasn’t so stressed,” says Silvius.<br />
The workforce optimization initiative will be piloted in six acute<br />
care units at the Foothills Medical Centre in the coming months with<br />
an enterprise-wide implementation strategy developed by the fall.
By Dave Lowery<br />
Actually, “form” and “bike . . . as in motorbike” are obviously four<br />
letter words. And a four-letter word usually has a negative connotation.<br />
But not these two four-letter words. To Dr. Connie Ellis, 42, they both<br />
elicit a lot of passion. A passion that she has had for motorbikes (she<br />
currently drives a Ducati) since she was a young girl growing up on<br />
the farm and the newly acquired passion she has for the project she<br />
has led for over two years, as liaison between the CHR department<br />
of medicine and family medicine, to condense between 3-400 forms<br />
down to maybe . . . uh . . . one!<br />
With a family practice in Bowness for the past 15 years, now<br />
specializing in travel medicine, Ellis recognized, along with numerous<br />
other family physicians over two years ago, that the number one<br />
problem back then was access to specialists in general.<br />
“We’re working on accessing specialists because it’s better patient<br />
care, specialists will be able to get the information they need and<br />
family physicians will get their patients seen in a timely fashion,”<br />
Ellis says. “Currently, the process isn’t changing for all specialties<br />
though we hope to have this someday. It will only effect specialists<br />
in the department of medicine.”<br />
The project hasn’t been cheap and initial time estimates were<br />
somewhat shorter, but Ellis says the end result will address much<br />
more than a form number reduction.<br />
“In initial meetings, we had everyone together who said ‘look at<br />
the larger issues,’” she says. “It soon became apparent that we could<br />
address them all through one form which would include triage and<br />
pertinent referral information.”<br />
And those issues included a “mess” of referral forms found in a<br />
family doctors inventory according to Shannon Erfl e, who joined the<br />
project as manager at the beginning of March after working as the CHR<br />
operations manager for living well with a chronic condition.<br />
“The family doctors had hundreds of referral forms in their offi ce<br />
and were operating in a referral system based on relationships as<br />
opposed to specialty areas,” Erfl e says. “That meant patients weren’t<br />
necessarily getting the treatment they needed and were having to wait<br />
longer. Together with family physicians, other health care providers<br />
and specialty services, we identifi ed those issues where we wanted to<br />
focus our attention. The result? We are getting the people and technical<br />
equipment in place, referral criteria have been generated and we’re<br />
committing to confi rming receipt of referral within two days and<br />
seven days for triaging. If it’s not done based on the package triage<br />
criteria, then the second triage will catch the mistake. An important<br />
change is that the specialty triage nurses will be contacting patients<br />
directly for appointments, family doctors to get more information if<br />
needed and going back to the specialist if there is anything that is<br />
questionable.”<br />
Ellis says the ultimate result will be better patient care but she is<br />
looking to expand the program.<br />
“Our next step is to include other specialties and departments,”<br />
she says. “Once they see it, I think they are going to jump on board.<br />
I would like to stress out departments and have them call us to make<br />
them part of the system. This is a plus . . . this is a good thing. We<br />
need to keep family doctors practicing and this will support good<br />
patient care.”<br />
Form is not a four-letter word<br />
What physicians need to know.<br />
1. Starts May 1, 2008<br />
2. The 30-page coil-bound instruction manual is for your<br />
staff.<br />
3. The form isn’t important. The information is.<br />
• Erfl e: “If you prefer to use a dictated letter, as long<br />
as it contains the same information and supporting<br />
documentation, then we can move forward.”<br />
4. The specialty will contact patients directly in order to<br />
confi rm and set up appointments.<br />
5. Get the forms from data group or on line from<br />
department of medicine.<br />
• Erfl e: “As we move towards a more electronic<br />
system, we are hoping to make this an easier electronic<br />
process.”<br />
6. Physician requests for a specifi c specialist will be<br />
honoured.<br />
• Erfl e: ”Most of the specialty groups haven’t made<br />
signifi cant changes in what they need, they have just<br />
put it in one place and they’ve given one central intake<br />
phone number.”<br />
For more information, please go to<br />
http://www.departmentofmedicine.com/<br />
or contact Dr. Connie Ellis P. (403) 247-9797,<br />
E-mail: ellis@bowmont.ca or Shannon Erfl e,<br />
E-mail: shannon.erfl e@calgaryhealthregion.ca<br />
Presentations can be made to your clerical team on<br />
request.<br />
Dr. Connie Ellis outside her practice in Bowness.<br />
Vital Signs May 2008 • Page 7
Region physician helps fl ood-ravaged African villages<br />
Wherever floods, fires,<br />
earthquakes or tsunamis are in the<br />
world, you may find Dr. Sandra<br />
Allaire.<br />
Allaire, the medical leader for the <strong>Calgary</strong> Health Region’s disaster<br />
services department, is also a disaster response specialist for the<br />
International Red Cross.<br />
She returned earlier this year from Africa, where she spent<br />
four weeks helping out in the fl ood-stricken southern part of the<br />
continent. She was in the fi eld for three weeks, visiting villages in a<br />
normally drought-stricken, now soggy region of Zambia, and then the<br />
waterlogged Caprivi Strip region of Namibia.<br />
In the Caprivi Strip, a 100-by-400-km long peninsula, more than<br />
400 centimetres of rain fell in January, more than double the normal<br />
amount for that time of year. The region – which is part of Namibia but<br />
is bordered by Zambia, Botswana and Zimbabwe – contains mighty<br />
rivers such as the Kavango, Kwando, Chobe and Zambezi and 90,000<br />
residents, most of whom are subsistence farmers/fi shermen who live in<br />
mud-walled huts with thatched roofs. Many of the Caprivi residents are<br />
used to moving because of the yearly fl oods but this year the rainfall<br />
was so heavy that more people than usual were forced out of their<br />
homes early before the annual river rise.<br />
Allaire, who has been working in disaster response for the Red<br />
Cross since 1991, was in charge of assessing the situation.<br />
“We went into the fi eld to the areas where the people were moving<br />
to or having to move from to assess what the situation was,” she<br />
says.<br />
“What we were looking for is how much shelter is available, how<br />
much food is available, whether there were health problems and what<br />
kind of numbers were involved. Sanitation – safe water supply and<br />
appropriate disposal of human waste, to prevent waterborne diseases<br />
– is a major concern in fl oods especially. Based on what we found, we<br />
forecasted the need and helped with the budget so the supplies could<br />
be ordered and brought in.”<br />
While Allaire’s job is mostly administrative and “big picture” – she<br />
had meetings with the premier of the Caprivi Strip in the capital city<br />
of Katima Mulilo – she is still a fi eldworker at heart.<br />
“I just love getting out in the fi eld,” she says. “You talk to the<br />
women and ask them if the kids are getting sick; more sick than the<br />
same time last year. You talk to the health offi cials and you fi nd out<br />
if there’s anything unusual and what’s being reported. You go to<br />
the clinics and talk to the nurses and see what is being reported. In<br />
Namibia, the reporting system is good.<br />
Vital Signs May 2008 • Page 8<br />
By Chris Simnett, CHR communications<br />
Dr. Sandra Allaire, right, visits African villages hit by<br />
severe fl ooding. ‘I just love getting out in the fi eld,’ says<br />
Allaire, medical director for the <strong>Calgary</strong> Health Region’s<br />
offi ce of emergency preparedness and a disaster<br />
response specialist for the International Red Cross.<br />
“I want to know the status of health in children and adults,” she<br />
adds.<br />
“I check where they get their water and use their latrines, if they<br />
exist, as part of the quality control. I want to know how their food<br />
situation is, what shelter they have and what problems they see as<br />
most important. Often, what we, in this part of the world assess as<br />
the worst problems, are not what the people themselves see as a need.<br />
Latrines, as an example, are often a ‘nice to have’ as opposed to a<br />
need. The fi elds do fi ne.”<br />
“They explain the situation to me and I will actually go in the tents<br />
or where they’re sheltered. They may say to me they don’t have any<br />
food but I like to go in and see if they have any food supplies tucked<br />
away in the corner. It’s always interesting to me to see if they have<br />
any mosquito nets because that kind of thing, they’ve had help in the<br />
past. This is not the fi rst time they’ve been visited by the Red Cross<br />
or moved by the government.”
Rainfall forced people out of their homes.<br />
Allaire, whose contract with the region permits her to be away on<br />
Red Cross relief work four weeks every year, was on vacation in South<br />
Africa when she was called to duty to deal with the fl ooding.<br />
“The day I should have fl own home from my holiday was my fi rst<br />
day of work for the Red Cross,” she says. “I had a little bit of prep<br />
work to do before that.”<br />
Her fi rst order of business was to buy equipment.<br />
“I had gone on holidays so I had shorts on and now I’m going<br />
into a fl ood zone where there are mosquitoes and it’s malaria season,”<br />
she says.<br />
“I needed to get lots of equipment – stuff that I have here – but I<br />
just didn’t take it on holidays with me.”<br />
Allaire didn’t hesitate to end her holiday prematurely.<br />
“The reason I do this is because there are people I might be able<br />
to help,” she says.<br />
“I help them now by report writing and identifying their needs. I’ve<br />
certainly worked at the frontline, seen patients, put patients through<br />
clinics, run supplies around, collected supplies and handed them out to<br />
people. One of the reasons they send me is they know I’ll do whatever<br />
is needed. If I run across a patient in the fi eld and there’s no one else,<br />
I’ll deal with it. I won’t pre-empt the local medical system but when<br />
the local medical system isn’t there, I’ll deal with it.”<br />
“There are places where there are people who are more<br />
disadvantaged and you feel good if you are able to do something<br />
for them. You can always give money here, but I<br />
prefer to actually be on the ground and working<br />
with them.”<br />
Allaire is pleased with the help she was able to<br />
provide the fl ood victims in the Caprivi Strip. But<br />
she says everything pales in comparison to her fi rst<br />
mission for the Red Cross.<br />
“When I fi rst started doing this work my fi rst<br />
mission was to Iraq after the fi rst Gulf War in<br />
1991,” says Allaire. “I was working in a refugee<br />
camp where they were dying at a rate of 10 to 15<br />
per 10,000 every day. By the time we left at the end<br />
of two and a half weeks, the death rate had come<br />
down to three to fi ve every 10,000 people so we<br />
had reduced it by one-third.<br />
“When you can see results like that, it’s<br />
pretty hard for anything else to match up to it.<br />
As a physician, I won’t ever save that many lives<br />
again.”<br />
Since then, Allaire has worked in the Darfur region of Sudan,<br />
the occupied Palestinian territories, Serbia, North Korea, Indonesia<br />
after the earthquake of May 2006 and in the Maldives after the 2004<br />
Boxing Day tsunami.<br />
Many of the Caprivi residents are used to moving<br />
because of the yearly fl oods but this year the rainfall was<br />
so heavy that more people than usual were forced out of<br />
their homes.<br />
Vital Signs May 2008 • Page 9
<strong>Calgary</strong> Health Region – board approval – March 25, 2008<br />
Dr. Shelly Bhayana internal medicine endocrinology<br />
Dr. Amy L. Gausvik rural medicine family medicine<br />
Dr. Christopher J. Irving family medicine community care<br />
Dr. M. Faisal M. Jhandir internal medicine general internal medicine<br />
Dr. Andrew S. Johnson internal medicine infectious diseases<br />
Dr. Maitreyi Kothandaraman internal medicine gastroenterology<br />
Dr. Nasrin Maiter rural medicine family medicine<br />
Dr. Melanie B. Peachell rural medicine diagnostic imaging<br />
Dr. Shannon K.T. Puloski surgery orthopedics<br />
Dr. Harald M. Schriefers rural medicine family medicine<br />
Dr. Chandra S.Sivakumar internal medicine geriatrics<br />
Dr. Leonore D. Stampa rural medicine family medicine<br />
Dr. Oliver Strohm cardiac sciences cardiology<br />
Dr. Jennifer E. Tse family medicine acute care<br />
Our recent spring snowfall may have snarled traffi c but it inspired one young patient at the Alberta Children’s<br />
Hospital to send a unique thank you to hospital staff.<br />
“It’s the little things like this that makes everything we do worthwhile,” said Dr. Brian Stewart, vice president &<br />
associate chief medical offi cer physician integration & medical leadership.<br />
Vital Signs May 2008 • Page 10
Safety learning reporting system update<br />
By Sheila Rougeau, CHR communications<br />
The <strong>Calgary</strong> Health Region<br />
launched a new online patient safety<br />
learning reporting system on March<br />
11, 2008. The new reporting system,<br />
which replaces the paper incident report forms previously used, focuses<br />
on identifying safety hazards that exist across the region and require<br />
shared solutions.<br />
The new reporting system is faster and easier to use. Reporting<br />
is confi dential (the name of the reporter is not distributed with the<br />
report), and trends identifi ed by the system are explored to determine<br />
the need for improvement.<br />
Some of the most commonly asked questions received from<br />
physicians since launching the new safety learning reporting system<br />
are below:<br />
Q: If there is no paper incident report, how am I going to fi nd out<br />
about things that have occurred with my patients?<br />
A: The most responsible physician and supervisor/manager should<br />
be notifi ed of events where their patients are involved, and the facts of<br />
an event should be charted on the patient’s chart. Reporting an event<br />
is only one part of the communication.<br />
Q: I used to “sign-off” on incidents that I needed to be aware of,<br />
and write my comments, how will I do that now?<br />
A: There is no requirement for physicians to sign-off on a safety<br />
learning report. Any documentation regarding patients should be<br />
charted on the patient record, including physician’s notes about an<br />
event. The old “incident” reports were never part of the patient’s<br />
record, so documentation on the form would not have been kept with<br />
the patient’s chart<br />
Q: Who can use the new reporting system and how can I fi nd the<br />
new report form?<br />
A: Any staff or physicians who have access to the <strong>Calgary</strong> Health<br />
Region internal web can access the new safety learning reporting<br />
system by going to the internal website and clicking on ‘submit a<br />
report’ under the safety learning reporting system banner. There is no<br />
need to login, or have a password.<br />
Q: How do I fi nd out what happened to my report?<br />
A: The online system will give you a tracking number which you<br />
cite in an email enquiry to safetylearning@calgaryhealthregion.ca<br />
Home care update<br />
DAL-ED study<br />
A 12-week concurrent study of referrals to emergency from six<br />
DAL sites is underway to examine transfers and admissions. At the<br />
mid-point, there have been 89 transfers of which 49 per cent have<br />
returned to DAL following assessment in the ED. The primary decision<br />
makers regarding transfers were site staff in 66 per cent of instances.<br />
Most common reasons for transfers were to rule out fractures and<br />
DVT, shortness of breath, abnormal behaviours, safety concerns and<br />
pain management. Most common reasons for admission were COPD<br />
exacerbation, pneumonia and UTI. Sites where there were regularly<br />
scheduled visits from a physician expressed greater satisfaction in their<br />
ability to manage emergencies. Challenges remain in communicating<br />
with physicians out of hours.<br />
DAL update<br />
The physician group met to discuss the evolving medical<br />
structure in DAL. A role description is nearly fi nalized which will<br />
guide physicians and staff as to team responsibilities. There is site<br />
RN presence at all sites now during weekdays (LPNs on a 24-hour<br />
basis). Role of home care is mostly case management. Physicians<br />
were reminded that 03.03N ($50.34) can be used for every patient<br />
visit provided the visit in the patient’s room and not in a common area<br />
or offi ce. Call 510-2518 for more information regarding working in<br />
a DAL site.<br />
Wound clinic<br />
Dr. Gene d’Archangelo has been breaking new ground with<br />
multispecialty wound rounds at the Sheldon Chumir centre on the<br />
fourth Wednesday afternoon of the month. The clinic will move to<br />
its new premises before the summer. 943-2653 to refer.<br />
Dr. Paddy Quail, medical director, home care, <strong>Calgary</strong><br />
Health Region. E-mail: quail@ucalgary.ca<br />
Vital Signs May 2008 • Page 11
Vital Signs May 2008 • Page 12<br />
Family physician – eating disorder program<br />
The eating disorder program continues to seek family physicians<br />
interested in working one or two days per week with adult outpatients<br />
who are struggling with eating disorders. The position will be based at<br />
the Richmond Road Diagnostic and Treatment Centre (former ACH)<br />
and will involve providing medical assessment and follow up with<br />
respect to the medical complications associated with this psychiatric<br />
disorder.<br />
The family physician will be a member of a dynamic<br />
multidisciplinary team made up of psychiatrists, paediatricians,<br />
family counsellors, nurses, dieticians, an occupational therapist and a<br />
recreational therapist. Training, ongoing mentoring, consultation and<br />
therapeutic support will be provided to the family physician(s).<br />
Clinics are held at the eating disorder program community based<br />
treatment located at the Richmond Road Diagnostic and Treatment<br />
Centre. There is no overhead as secretarial support and a staff nurse<br />
are included in the operation of all medical clinics. Family physicians<br />
who work with the eating disorder program will bill Alberta Health for<br />
patient visits. Sessional dollars are available to offset the cost of no<br />
shows, and to allow family physicians to participate in team meetings<br />
and educational opportunities as their time permits.<br />
If you are interested in learning more about this opportunity on a<br />
temporary or permanent basis please contact one of the following:<br />
Mark Lagimodiere<br />
manager, clinical operations<br />
eating disorder program<br />
955-7704 (w)<br />
710-3708 (cell)<br />
Carol Bentzen<br />
nurse clinician<br />
eating disorder program<br />
944-1789 (w)<br />
Brian Cram<br />
medical director<br />
eating disorder program<br />
955-7705 (w)<br />
Introducing new Canadian Tuberculosis Standards<br />
The sixth edition of the Canadian Tuberculosis Standards is now<br />
available and can be viewed at:<br />
http://www.phac-aspc.gc.ca/tbpc-latb/pubs/tbstand07-eng.php<br />
Print copies can be obtained by contacting the Alberta Lung<br />
<strong>Association</strong>.<br />
The publication is jointly produced by the Public Health<br />
Agency of Canada and the Canadian Lung <strong>Association</strong>/ Canadian<br />
Thoracic Society. The sixth edition is a much expanded version of<br />
its predecessors and is the defi nitive resource on issues pertaining to<br />
tuberculosis prevention and control in Canada.<br />
Judy MacDonald, BSc, MD, MCM, FRCPC, deputy medical<br />
offi cer of health, <strong>Calgary</strong> Health Region.<br />
Bulletins & notices<br />
Two positions: psychiatrist and family physician<br />
Location: <strong>Calgary</strong>, Alberta<br />
The Canadian Sleep Institute has been a leading national centre of<br />
sleep medicine excellence for 12 years. With a head offi ce in <strong>Calgary</strong>,<br />
we specialize in community-based clinical services, research, and<br />
corporate consulting in the area of sleep and fatigue disorders. We<br />
are an accredited full-service sleep centre, and an affi liated teaching<br />
site of the University of <strong>Calgary</strong>. CSI Research specializes in clinical<br />
trials in a spectrum of neuropsychiatric conditions, with a primary<br />
focus on sleep medicine and related mood and pain disorders. Since<br />
1996, we have completed in excess of 80 clinical trials, with a wellestablished<br />
reputation, infrastructure and team of clinical and technical<br />
research professionals.<br />
We are seeking a psychiatrist and a family physician in <strong>Calgary</strong>.<br />
This is a rewarding, varied interdisciplinary practice, in a low overhead<br />
environment. Additional training/experience in sleep medicine or<br />
clinical research is an asset, although not mandatory. We offer a<br />
combination of expanded income opportunities from fee-for-service<br />
billing, third-party private work, and remuneration for opportunities<br />
as an investigator in clinical trials.<br />
You must be licensed, or eligible for licensure in Alberta. If you<br />
are interested in exploring this exciting opportunity, we would like<br />
to hear from you.<br />
Inquiries and CVs can be forwarded by E-mail to Dr. Adam<br />
Moscovitch, MD, FRCPC, CSI medical director at<br />
adam.moscovitch@csisleep.com.