Quality Improvement Guidelines for Recording Patient Radiation ...
Quality Improvement Guidelines for Recording Patient Radiation ...
Quality Improvement Guidelines for Recording Patient Radiation ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Quality</strong> <strong>Improvement</strong> <strong>Guidelines</strong> <strong>for</strong> <strong>Recording</strong><strong>Patient</strong> <strong>Radiation</strong> Dose in the Medical RecordDonald L. Miller, MD, Stephen Balter, PhD, Louis K. Wagner, PhD, John F. Cardella, MD,Timothy W.I. Clark, MD, MSc, Calvin D. Neithamer, Jr, MD, Marc S. Schwartzberg, MD, Timothy L. Swan, MD,Richard B. Towbin, MD, Kenneth S. Rholl, MD, and David Sacks, MD, <strong>for</strong> the SIR Standards ofPractice CommitteeJ Vasc Interv Radiol 2009; 20:S200–S207Abbreviations: CD cumulative dose, DAP dose–area–product, FDA Food and Drug Administration, IRP interventional reference point, PSD peakskin dose, TIPS transjugular intrahepatic portosystemic shuntPREAMBLETHE membership of the Society of InterventionalRadiology (SIR) Standardsof Practice Committee represents expertsin a broad spectrum of interventionalprocedures from both the privateand academic sectors of medicine. Generally,Standards of Practice Committeemembers dedicate the vast majority oftheir professional time to per<strong>for</strong>ming interventionalprocedures; as such theyFrom the Department of Interventional Radiology(D.L.M.), National Naval Medical Center, Bethesda,Maryland; Department of Medicine (S.B.), LenoxHill Hospital, New York; Department of Radiology(L.K.W.), University of Texas Houston MedicalSchool, Houston, Texas; Department of Radiology(J.F.C.), SUNY–Upstate Medical University, Syracuse,New York; Section of Vascular and InterventionalRadiology (T.W.I.C.), Department of Radiology,Hospital of the University of Pennsylvania;Department of Radiology (R.B.T.), Children’s Hospitalof Philadelphia, Philadelphia; Department ofRadiology (D.S.), Reading Hospital and MedicalCenter, Reading, Pennsylvania; Department of Radiology(C.D.N.), Inova Mount Vernon Hospital;Department of Radiology (K.S.R.), Inova AlexandriaHospital, Alexandria, Virginia; Radiology Associatesof Central Florida (M.S.S.) Leesburg, Florida;and Department of Radiology (T.L.S.), MarshfieldClinic, Marshfield, Wisconsin. Received January 23,2004; accepted January 23. Address correspondenceto SIR, 10201 Lee Highway, Suite 500, Fairfax, VA22030.None of the authors have identified a conflict ofinterest.This article first appeared in J Vasc Interv Radiol2004; 15:423–429.© SIR, 2009DOI: 10.1016/j.jvir.2009.04.005represent a valid broad expert constituencyof the subject matter under consideration<strong>for</strong> standards production.Technical documents specifying theexact consensus and literature reviewmethodologies, as well as the institutionalaffiliations and professional credentialsof the authors of this document,are available upon request fromSIR, 10201 Lee Highway Suite 500,Fairfax, VA 22030.METHODOLOGYSIR produces its Standards ofPractice documents using the followingprocess. Standards documents ofrelevance and timeliness are conceptualizedby the Standards of PracticeCommittee members. A recognizedexpert is identified to serve as theprincipal author <strong>for</strong> the standard.Additional authors may be assigneddependent upon the magnitude ofthe project.An in-depth literature search is per<strong>for</strong>medwith use of electronic medicalliterature databases. Then, a critical reviewof peer-reviewed articles is per<strong>for</strong>medwith regards to the study methodology,results, and conclusions. Thequalitative weight of these articles is assembledinto an evidence table, which isused to write the document such that itcontains evidence-based data with respectto content, rates, and thresholds.When the evidence of literature isweak, conflicting, or contradictory,consensus <strong>for</strong> the parameter is reachedby a minimum of 12 Standards ofPractice Committee members with aModified Delphi Consensus Method(1,2). For the purposes of these documents,consensus is defined as 80%Delphi participant agreement on avalue or parameter.The draft document is critically reviewedby the Standards of PracticeCommittee members, either by telephoneconference calling or face-tofacemeeting. The finalized draft fromthe Committee is sent to the SIR membership<strong>for</strong> further input/criticismduring a 30-day comment period.These comments are discussed by theStandards of Practice Committee, andappropriate revisions are made to createthe finished standards document.Prior to its publication the documentis endorsed by the SIR ExecutiveCouncil.PATIENT RADIATION DOSERECORDINGThere are no federal regulatory requirementsin the United States concerningrecording or reporting of radiationdose data <strong>for</strong> interventionalprocedures. There are recommendationsfrom the United States Food andDrug Administration (FDA) on thistopic (3–5). Regulations or guidance atthe state level are not uni<strong>for</strong>m. Only asmall number of states have addressedthis issue. If state regulations exceedthe requirements contained in thisdocument, practitioners are advised toS200
Volume 20Number 7SMiller et al • S201follow the more stringent state regulatoryguidelines. Existing guidelinesand recommendations are shown inTable 1.Fluoroscopically guided proceduresare an essential part of the contemporarypractice of medicine. In general,the risk of patient injury as a result ofradiation exposure during these proceduresis low. Some fluoroscopicallyguided procedures are associated witha risk of radiation injury to the skin(16). The frequency of injury is unknown(17,18). Koenig and colleagues(16), in a comprehensive review publishedin 2001, reported data on radiation-inducedskin injuries in 73 patients.Of these, 47 (64%) were resultsof coronary angiography and intervention,12 (16%) were results of cardiacradiofrequency catheter ablation,seven (10%) were results of transjugularintrahepatic portosystemic shunt(TIPS) creation, three (4%) were resultsof neuroradiologic interventions, andthe type of procedure was not specified<strong>for</strong> four patients. Some reportedskin injuries have been associated withrenal angioplasty, multiple hepatic/biliary procedures, or embolization(17–22).In a Public Health Advisory ofSeptember 30, 1994, the FDA recommendedthat “in<strong>for</strong>mation permittingestimation of the absorbed doseto the skin be recorded in the patient’smedical record” (3). The InternationalCommission on RadiologicalProtection (ICRP) has alsorecommended recording patient radiationdose in the medical record<strong>for</strong> certain procedures (6). Monitoringand recording patient dose data<strong>for</strong> all procedures can be valuable <strong>for</strong>quality-assurance purposes as wellas <strong>for</strong> patient safety. Feedback to theoperator may help to optimize radiationdoses overall (23).These guidelines are written <strong>for</strong> inclusionin quality-improvement programsused to manage radiation dosefrom fluoroscopically guided invasiveand interventional procedures, excludingcomputed tomographic (CT)fluoroscopy. A measurable part of theradiation management process is therecording of patient dose. The outcomemeasure or indicator <strong>for</strong> thisprocess is the compliance rate <strong>for</strong> datarecording. Outcome measures are assignedthreshold levels.DEFINITIONSAbsorbed DoseThe energy imparted per unit massby ionizing radiation to matter at aspecified point. The SI unit of absorbeddose is the joule per kilogram.The special name <strong>for</strong> this unit is theGray (Gy).Air KermaThe energy released per unit massof a small volume of air when it isirradiated by an x-ray beam. For diagnosticx-rays, air kerma is the same asthe absorbed dose delivered to the volumeof air in the absence of scatter. Airkerma is measured in Gy.Biologic VariationWith respect to radiation, the differencesamong individuals in the thresholddose required to produce a deterministiceffect, or the differences indegree of effect produced by a givendose. Biologic variation may be idiopathicor due to underlying disease.Different areas and types of skin alsodiffer in radiosensitivity.C-Arm Fluoroscopic SystemA fluoroscopic system consisting ofa mechanically coupled x-ray tube andimage receptor. Such systems typicallyhave two rotational degrees of freedom(left-right and cranial-caudal).Most such systems have an identifiablecenter of rotation called the isocenter.An object placed at the isocenterremains centered in the beam asthe C-arm is rotated.Cumulative Dose (CD)The air kerma accumulated at aspecific point in space relative to thefluoroscopic gantry (the interventionalreference point) during a procedure.CD does not include tissue backscatterand is measured in Gy. CD is sometimesreferred to as cumulative airkerma.Deterministic EffectA radiation effect characterized bya threshold dose. The effect is not observedunless the threshold dose is exceeded.(The threshold dose is subjectto biologic variation.) Once the thresholddose is exceeded in an individual,the severity of injury increases withincreasing dose. Examples of deterministiceffects include skin injury,hair loss, and cataracts.DoseAs used in this document, “dose” isthe same as the absorbed dose unlessspecified as “equivalent dose” or “effectivedose.”Dose–Area–Product (DAP)The integral of air kerma (absorbeddose to air) across the entire x-raybeam emitted from the x-ray tube.DAP is a surrogate measurement <strong>for</strong>the entire amount of energy deliveredto the patient by the beam. DAP ismeasured in Gy·cm 2 .Effective DoseThe sum, over specified tissues, ofthe products of the equivalent dose ina tissue and the tissue weighting factor<strong>for</strong> that tissue. Effective dose is measuredin Sieverts (Sv). Stochastic riskfactors are usually stated relative toeffective dose.Equivalent DoseA quantity used <strong>for</strong> radiation protectionpurposes that takes into accountthe different probability of effectsthat occur with the sameabsorbed dose delivered by radiationswith different radiation weighting factors.Effective dose is measured in Sv.Fluorographic ImageA single recorded image obtainedusing an image intensifier or flat digitalpanel as the image receptor. A digitalangiographic “run” consists of aseries of fluorographic images.Fluoroscopy TimeThe total time that fluoroscopy isused during an imaging or interventionalprocedure.
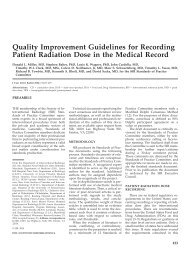
S202 • <strong>Quality</strong> <strong>Improvement</strong> <strong>Guidelines</strong> <strong>for</strong> <strong>Recording</strong> <strong>Patient</strong> <strong>Radiation</strong> Dose July 2009 JVIRTable 1Existing Recommendations <strong>for</strong> <strong>Recording</strong> <strong>Patient</strong> DoseICRP (6)ReferenceSpanish Statute (7)FDA Advisory (4)ACR (8)CRCPD, 2001 (9)Reference TypeInternationalguidelineNational law(Spain)FDA advisoryguideline(United States)ACR technicalstandard(United States)CRCPD resolution(United States)Procedures <strong>for</strong> which DoseData Should Be RecordedDetermined by dose (presumedmeasured <strong>for</strong> all cases)Mandatory <strong>for</strong> allinterventional procedures(eg, IR, cardiology);recommended <strong>for</strong> otherfluoroscopic proceduresTo be decided by each facility;should include TIPS and“percutaneous endovascularreconstruction”Determined by fluoroscopytime or expected skin dose“Procedures with a potential<strong>for</strong> producing radiationinducedinjury”When Dose Should BeRecordedPSD 1 Gy if procedurelikely to be repeated;PSD 3 Gy if procedurenot likely to be repeatedAlwaysIf skin dose equals orexceeds a threshold doseset by each facility (1–2Gy suggested asthreshold dose)Fluoroscopy time 10min or expected skindose 2GyNot specifiedDose Metrics RecordedPSD and location, skindose mapDAP (minimumrequirement);fluoroscopy time andnumber of imagesdesirableSkin dose; skin dose mapor verbal description ofsiteFor automated dosimetrysystems, dose data; <strong>for</strong>other systems,fluorosco py time; ifskin dose likely 2Gy, location of skinareas receiving dose 2GyNot specifiedCRCPD, 2003 (10) Suggested stateregulations <strong>for</strong>radiation control(United States)All All Fluoroscopy time,number of images (nospecific requirement toinclude this in patient’smedical record)Faulkner (11) Review All Always PSD and DAPO’Dea et al (12)Waite andFitzgerald (13)Miller et al (14)Miller et al (15)ObservationalstudyObservationalstudyObservationalstudyObservationalstudyGreater than 0.01% chance ofexceeding 6 Gy PSD if studynot likely to be repeated; 5% chance of exceeding 1 GyPSD if study likely to berepeated at the same skin siteFGIPsAll, if integrated dosimetryavailable; otherwise,procedures with knownpotential <strong>for</strong> high dose(embolization, TIPS, renal/visceral artery PTA and stentplacement)All if integrated dosimetryavailable; otherwise,procedures with knownpotential <strong>for</strong> high dose (allembolization, TIPS,angioplasty in abdomen orpelvis)All procedures meetingcriteriaAlways <strong>for</strong> cerebralembolization; <strong>for</strong> allcases if easily available,otherwise periodicchecks <strong>for</strong> FGIPsAll, if integrated dosimetrya vailable; otherwise,procedures with knownpotential <strong>for</strong> high doseAll, if integrated dosimetryavailable; otherwise,procedures with knownpotential <strong>for</strong> high dosePSDPSD and DAP <strong>for</strong>cerebral embolization,dap or automated PSD<strong>for</strong> all cases if easilyavailable, otherwiseperiodic checks of PSD<strong>for</strong> FGIPsPSD, CD, DAP(fluoroscopy timeacceptable only if othermetrics not available)PSD, CD, DAPNote.—ACR American College of Radiology; CRCPD Conference of <strong>Radiation</strong> Control Program Directors; FGIP fluoroscopically guided interventional procedure; ICRP International Commission on Radiological Protection; PTA percutaneous transluminal angioplasty.
S204 • <strong>Quality</strong> <strong>Improvement</strong> <strong>Guidelines</strong> <strong>for</strong> <strong>Recording</strong> <strong>Patient</strong> <strong>Radiation</strong> Dose July 2009 JVIRare based on CD tend to overstate thisrisk (15). CD is usually measured witha dosimeter integrated into the fluoroscopicunit. Relatively few fluoroscopicunits incorporate CD measurementcapability as of 2004, but this willchange as International ElectrotechnicalCommission 60601-2-43–compliant interventionalfluoroscopic systems are installed.As of March 2004, proposedFDA regulations require CD measurementcapability <strong>for</strong> all new fluoroscopicequipment.The likelihood and severity of radiation-inducedskin injury to the patient asa whole are functions of the highest radiationdose at any point on that patient’sskin—the PSD. Typically, nopoint on the patient’s skin is within theirradiated field <strong>for</strong> the entire procedure.For this reason, the PSD is usually lowerthan the CD (15). It is desirable to measurePSD during interventional radiologyprocedures, but this has proved difficultin practice (34). PSD may bemeasured with a computerized analysistool integrated into the fluoroscopic unit(35,36), with real-time point-measurementdevices applied to the patient (37–39), with thermoluminescent dosimetersapplied to the patient, or with dosimetricfilm interposed between the x-raybeam and the patient (40–42). PSD dataderived from point measurement devicesare likely to underestimate truePSD unless the measurement device isplaced at the exact site of PSD. Exactplacement of a point measurement deviceis unlikely because the PSD is usuallyconfined to a small area of skin, theprecise location of which is not knownbe<strong>for</strong>e the procedure (15,37,43).PSD measurement may be accompaniedby a display of a skin dosemap. A real-time skin dose map is anextremely valuable tool <strong>for</strong> assistingthe operator in minimizing skin dose(36). Dosimetric film may also be usedto obtain a skin dose map, albeit not inreal time (42,44). The skin dose mapmay also be added to the medicalrecord at the conclusion of the procedure,thereby indicating not only themagnitude of the skin dose, but itslocation. This satisfies the most stringentinterpretation of FDA, AmericanCollege of Radiology, and internationalrecommendations <strong>for</strong> recordingskin dose (4,6,8).A real-time skin dose map that indicatesthe site and magnitude of PSDis the ideal means <strong>for</strong> managing andrecording patient radiation dose. Un<strong>for</strong>tunately,as of March 2004, thistechnology is not commercially available.Alternative methods of dosemapping, such as dosimetric film andthermoluminescent dosimeter arrays,are rarely used.Measurement UncertaintyAll statements of patient dose containsome degree of uncertainty. Thisresults from uncertainties in the physicalmeasurement of dose and furtheruncertainties when these measurementsare used to estimate patientdose. Users of dose data should beaware of these uncertainties.For example, fluoroscopy time canbe accurately measured. However, importantuncertainties in convertingfluoroscopy time to patient dose includethe varying effects of patientsize, beam orientation, and the technicalconfiguration of the fluoroscope.Beam orientation and beam motionduring the procedure have a profoundinfluence on the precision of mostdose metrics to estimate PSD. If thebeam is fixed relative to the patientduring the entire procedure, the conversionis relatively straight<strong>for</strong>ward.However, if the beam never strikes thesame portion of the patient’s skintwice, PSD will be low. Virtually allclinical procedures are between theseextremes (45).In addition, even the most sophisticateddose-measurement instrumentationhas unavoidable uncertainties relatedto variations in instrumentresponse with changes in beam energy,dose rate, and collimator size.Converting these measurements intoskin dose introduces yet further uncertaintiesrelated to the patient’s size andposition relative to the beam. Finally, clinicallyavailable dose and DAP measurementsignore the effect of backscatter fromthe patient. Backscatter can increase skindose 10%–40%, depending on the beamarea and energy.Methods <strong>for</strong> estimating PSD can beranked from most reliable to least reliable.Peak (air) dose measuring softwareis the most reliable, followed bymeasurement of CD at a referencepoint, DAP, and finally fluoroscopytime combined with a count of thenumber of fluorography frames or images.Measurement of peak (air) dose atthe patient’s skin is probably accurateto within 50% of the actual peak airdose. This means that a reported valueof 2 Gy more precisely represents askin dose value between approximately1.3 Gy and 3.9 Gy (includingthe effect of backscatter). Dose datareconstructed from fluoroscopy timeand number of fluorographic framesare much more uncertain and, after allcorrections are factored in, are probablynot more accurate than a factor ofapproximately 130% and 70% ofthe best estimated value. For example,a 2-Gy calculated peak air dose at thepatient’s skin, reconstructed from fluoroscopytime and number of fluorographicframes, is probably more preciselystated as between 0.6 Gy and 4.6Gy. The uncertainties of estimates ofPSD derived from CD or DAP are betweenthese two extremes.How Dose Should Be MeasuredThe optimal method is measurementof PSD. Ideally, this would includereal-time skin dose mapping asa means <strong>for</strong> managing patient radiationdose. In the absence of skin dosemeasurements, other dose metricsshould be used. PSD and DAP are themost useful predictors <strong>for</strong> deterministicand stochastic injury, respectively.CD is an acceptable substitute if PSD isdifficult to measure, but it does notcorrelate well with PSD in individualcases (15). Fluoroscopy time alonedoes not correlate with PSD (45). Monitoringfluoroscopy time alone also underestimatesthe risk of radiation-inducedskin effects (12). Fluoroscopytime and number of fluorographic images,used together, can provide a betterguide to patient dose but are notthemselves measures of dose. They donot provide sufficient in<strong>for</strong>mation <strong>for</strong>dose calculations and are there<strong>for</strong>esuboptimal dose metrics. However, ifnone of the other metrics can be measured,fluoroscopy time and numberof fluorographic images, along withthe patient’s height and weight, can beused <strong>for</strong> recording patient radiationdose until other means are available.SIR recognizes that many practitionershave access only to interventionalfluoroscopic equipment with minimalor no radiation dose measurement capabilities.Facilities should be encouragedto purchase interventional fluoroscopicequipment with state-of-the-art dose-
Volume 20Number 7SMiller et al • S205Table 2Threshold Rates <strong>for</strong> <strong>Recording</strong> of Dose Metricsmeasurement and dose-managementcapabilities and to upgrade existing interventionalfluoroscopic equipmentwith after-market devices to improvedose-measurement capability. Whendeterministic effects are of concern, themost desirable capability is real-timeskin dose mapping, followed by non–real-time skin dose mapping, PSD measurement,CD measurement, and, leastvaluable, fluoroscopy time and numberof images. If stochastic effects are of concern,DAP measurement capability isalso valuable.When Dose Should Be RecordedCertain procedures are known to beassociated with relatively high patientradiation doses (14,15). <strong>Patient</strong> radiationdose data should be recorded <strong>for</strong>all instances of these procedures. Tosimplify the categorization of highdoseprocedures, SIR recommendsthat all embolization procedures, TIPSprocedures, and arterial angioplastyor stent placement procedures anywherein the abdomen or pelvisshould be considered potential highdoseprocedures (15). <strong>Patient</strong> radiationdose data should also be recorded <strong>for</strong>medium-dose procedures that are likelyto be repeated (6). Medium-dose proceduresmay be defined as procedureswith a CD of 1–3 Gy. Examples includebiliary drainage, stroke therapy, andvertebroplasty (14). Other interventionalradiology procedures such as pulmonaryangiography, inferior vena cava filterplacement, and venous access proceduresare less likely to result in highpatient radiation doses (14,45). It isnonetheless desirable to record patientradiation dose data <strong>for</strong> these procedures.<strong>Recording</strong> patient dose data <strong>for</strong>all procedures makes it less likely thatthe process will be omitted inadvertently<strong>for</strong> high-dose procedures. In addition,monitoring and recording patientdose data can be valuable <strong>for</strong>Procedure Type Threshold (%)High-dose procedures (all embolization procedures, TIPS, arterialangioplasty or stent placement at any site in the abdomen orpelvis)Other fluoroscopically-guided interventional procedures(excluding CT fluoroscopy)quality-assurance purposes as well as<strong>for</strong> patient safety. Feedback to the operatormay help to optimize radiationdoses overall (23).Published SIR guidelines <strong>for</strong> reportingand archiving of interventionalradiology procedures do notspecify where in the medical recordradiation dose data should be recorded(46). <strong>Radiation</strong> dose data maybe recorded in the immediate procedurenote, the procedure worksheet,and/or the final report. Each institutionshould specify where this in<strong>for</strong>mationis to be recorded in accordancewith the needs of its own quality-improvementprogram and its medicalrecord guidelines.DATA RECORDINGAdequate recording of dose metricsis defined as documentation in the patientrecord of at least one of the following<strong>for</strong> all interventional procedures requiringfluoroscopy (in descendingorder of desirability): skin dose mapping,PSD, CD, DAP, or fluoroscopictime/number of fluoro-graphic images(Table 2). In Table 2, all values weresupported by the weight of literatureevidence and panel consensus.Acknowledgments: Dr. Donald L. Millerauthored the first draft of this documentand served as topic leader during the subsequentrevisions of the draft. Drs. StephenBalter and Louis Wagner made significantcontributions to the content of this document.Dr. John F. Cardella is chair of theSIR Standards of Practice Committee. Dr.David Sacks is Councilor of the SIR StandardsDivision. Other members of theStandards of Practice Committee and SIRwho participated in the development ofthis clinical practice guideline are (listedalphabetically): Curtis W. Bakal, MD, JosephBonn, MD, Daniel B. Brown, MD, PatriciaE. Cole, PhD, MD, Peter Drescher,MD, Neil J. Freeman, MD, Jeffrey D. Georgia,MD, Scott C. Goodwin, MD, Clement J.9995Grassi, MD, Ziv Haskal, MD, David M.Hovsepian, MD, Curtis A. Lewis, MD,MBA, Patrick C. Malloy, MD, Louis G.Martin, MD, J. Kevin McGraw, MD, StevenG. Meranze, MD, Kenneth Murphy, MD,Albert A. Nemcek, Jr, MD, Steven B.Oglevie, MD, Reed Ali Omary, MD, NileshH. Patel, MD, Dheeraj Rajan, MD, ParvatiRamchandani, MD, Anne C. Roberts, MD,Orestes Sanchez, MD, Gary P. Siskin, MD,Harry R. Smouse, MD, Patricia E. Thorpe,MD, Thomas M. Vesely, MD, Bret N. Wiechmann,MDAPPENDIX: METHODOLOGYThresholds are derived from criticalevaluation of the literature, evaluationof empirical data from Standards ofPractice Committee member practices,and, when available, the SIR HI-IQsystem national database.Consensus on statements in thisdocument was obtained with a modifiedDelphi technique (1,2).References1. Fink A, Kosefcoff J, Chassin M, BrookRH. Consensus methods: characteristicsand guidelines <strong>for</strong> use. Am J PublicHealth 1984; 74:979.–983.2. Leape LL, Hilborne LH, Park RE, et al.The appropriateness of use of coronaryartery bypass graft surgery in NewYork State. JAMA 1993; 269:753–760.3. Food and Drug Administration. PublicHealth Advisory: avoidance of seriousx-ray-induced skin injuries to patientsduring fluoroscopically-guidedprocedures. Rockville, MD: Center <strong>for</strong>Devices and Radiological Health, 1994.4. Food and Drug Administration. <strong>Recording</strong>in<strong>for</strong>mation in the patient’smedical record that identifies the potential<strong>for</strong> serious x-ray-induced skininjuries. Rockville, MD: Center <strong>for</strong> Devicesand Radiological Health, 1995.5. Shope TB. Regulations and recommendationsrelevant to interventional radiology.In: Balter S, Shope TB, eds. Syllabus:a categorical course in physics—physicaland technical aspects of angiographyand interventional radiology. OakBrook, IL: Radiological Society of NorthAmerica, 1995;195–205.6. International Commission on RadiologicalProtection. Avoidance of radiationinjuries from medical interventionalprocedures. ICRP Publication 85.Ann ICRP 2000; 30:7–67.7. Real Decreto 1976/1999. Por el que seestablecen los criterios de calidad enradiodiagnóstico. Boletin Oficial delEstado de 29 enero de 1999; 45891–45900.8. American College of Radiology. ACRtechnical standard <strong>for</strong> management of
S206 • <strong>Quality</strong> <strong>Improvement</strong> <strong>Guidelines</strong> <strong>for</strong> <strong>Recording</strong> <strong>Patient</strong> <strong>Radiation</strong> Dose July 2009 JVIRthe use of radiation in fluoroscopicprocedures. Practice <strong>Guidelines</strong> andTechnical Standards 2003. Reston, VA:American College of Radiology, 2003;669–673.9. Conference of <strong>Radiation</strong> Control ProgramDirectors. Resolution relating toprevention of unnecessary radiationexposure to patients from fluoroscopy.Available at: http://www.crcpd.org/Positions_Resolutions/Healing_Arts/HA23-May01.htm. Accessed March15, 2004.10. Conference of <strong>Radiation</strong> Control ProgramDirectors. Suggested state regulations<strong>for</strong> control of radiation, vol. 1: ionizingradiation. Part F: diagnosticx-rays and imaging systems in thehealing arts, 2001; section F.5.I.v.Available at: http://www.crcpd.org/SSRCRs/TOC_8-2001.htm. AccessedMarch 15, 2004.11. Faulkner K. Dose displays and recordkeeping. Radiat Prot Dosimetry 2001;94:143–145.12. O’Dea TJ, Geise RA, Ritenour ER.The potential <strong>for</strong> radiation-inducedskin damage in interventional neuroradiologicalprocedures: a review of 522cases using automated dosimetry. MedPhys 1999; 26:2027–2033.13. Waite JC, Fitzgerald M. An assessmentof methods <strong>for</strong> monitoring entrancesurface dose in fluoroscopicallyguided interventional procedures. RadiatProt Dosimetry 2001; 94:89–92.14. Miller DL, Balter S, Cole PE, et al.<strong>Radiation</strong> doses in interventional radiology:the RAD-IR study. Part I: overallmeasures of dose. J Vasc Interv Radiol2003; 14:711–727.15. Miller DL, Balter S, Cole PE, et al.<strong>Radiation</strong> doses in interventional radiology:the RAD-IR study. Part II: skindose. J Vasc Interv Radiol 2003; 14:977–990.16. Koenig TR, Wolff D, Mettler FA, WagnerLK. Skin injuries from fluoroscopicallyguided procedures: part 1,characteristics of radiation injury. AJRAm J Roentgenol 2001; 177:3–11.17. Shope TB. <strong>Radiation</strong>-induced skin injuriesfrom fluoroscopy. RadioGraphics1996; 16:1195–1199.18. Koenig TR, Mettler FA, Wagner LK.Skin injuries from fluoroscopicallyguided procedures: part 2, review of 73cases and recommendations <strong>for</strong> minimizingdose delivered to the patient.AJR Am J Roentgenol 2001; 177:13–20.19. Huda W, Peters KR. <strong>Radiation</strong>-inducedtemporary epilation after a neuroradiologicallyguided embolization procedure.Radiology 1994; 193:642–644.20. Lichtenstein DA, Klapholz L, VardyDA, et al. Chronic radiodermatitisfollowing cardiac catheterization. ArchDermatol 1996; 132:663–667.21. Shope TB. <strong>Radiation</strong>-induced skin injuriesfrom fluoroscopy [abstract]. Radiology1995; 197(suppl):449.22. Vano E, Arranz L, Sastre JM, et al.Dosimetric and radiation protectionconsiderations based on some cases ofpatient skin injuries in interventionalcardiology. Br J Radiol 1998; 71:510–516.23. Vehmas T. Hawthorne effect: shorteningof fluoroscopy times during radiationmeasurement studies. Br J Radiol1997; 70:1053–1055.24. International Electrotechnical Commission.Report 60601: medical electricalequipment—part 2–43: particular requirements<strong>for</strong> the safety of x-rayequipment <strong>for</strong> interventional procedures.Geneva, Switzerland: IEC, 2000;60601-2-43.25. Balter S. Interventional fluoroscopy:physics, technology, safety. New York:Wiley-Liss, 2001.26. Servomaa A, Karppinen J. The doseareaproduct and assessment of the occupationaldose in interventional radiology.Radiat Prot Dosimetry 2001; 96:235–236.27. Wagner LK, Eifel PJ, Geise RA.Potential biological effects followinghigh x-ray dose interventional procedures.J Vasc Interv Radiol 1994; 5:71–84.28. Castellano IA, McNeill JG, Thorp NC,Dance DR, Raphael MJ. Assessmentof organ radiation doses and associatedrisk <strong>for</strong> digital bifemoral arteriography.Br J Radiol 1995; 68:502–507.29. Vehmas T. <strong>Radiation</strong> exposure duringstandard and complex interventionalprocedures. Br J Radiol 1997; 70:296–298.30. Ruiz-Cruces R, Perez-Martínez M,Flores A, Cristofol J, Martínez-MorilloM, Diez-de-los-Rios A. <strong>Patient</strong>dose in radiologically guided interventionalvascular procedures: conventionalversus digital systems. Radiology1997; 205:385–393.31. McParland BJ. A study of patient radiationdoses in interventional radiologicalprocedures. Br J Radiol 1998;71:175–185.32. Vano E, Gonzalez L, Ten JI, FernandezJM, Guibelalde E, Macaya C. Skindose and dose-area product values <strong>for</strong>interventional cardiology procedures.Br J Radiol 2001; 74:48–55.33. van de Putte S, Verhaegen F, TaeymansY, Thierens H. Correlation of patientskin doses in cardiac interventional radiologywith dose-area product. Br JRadiol 2000; 73:504–513.34. Wagner LK. You do not know whatyou are doing unless you know whatyou are doing. Radiology 2002; 225:327–328.35. den Boer A, de Feijter PJ, Serruys PW,Roelandt JRTC. Real-time quantificationand display of skin radiation duringcoronary angiography and intervention.Circulation 2001; 104:1779–1784.36. Miller DL, Balter S, Noonan PT, GeorgiaJD. Minimizing radiation-induced skininjury in interventional radiology procedures.Radiology 2002; 225:329–336.37. Geise RA, O’Dea TJ. <strong>Radiation</strong> dose ininterventional fluoroscopic procedures.Appl Radiat Isot 1999; 50: 173–184.38. Hwang E, Gaxiola E, Vlietstra RE,Brenner A, Ebersole D, Browne K.Real-time measurement of skin radiationduring cardiac catheterization.Cathet Cardiavasc Diagn 1998; 43:367–370.39. Wagner LK, Pollock JJ. Real-time portalmonitoring to estimate dose to skinof patients from high dose fluoroscopy.Br J Radiol 1999; 72:846–855.40. Balter S, Shope TB Jr, Fletcher DW,et al. Techniques to estimate radiationdose to skin during fluoroscopicallyguided procedures. In: Balter S, ChanRC, Shope TB, Jr, eds. Intravascularbrachytherapy: fluoroscopically guidedinterventions. Madison, WI: MedicalPhysics Publishing, 2002; 731–764.41. Geise RA, Ansel HJ. Radiotherapyverification film <strong>for</strong> estimating cumulativeentrance skin exposure <strong>for</strong> fluoroscopicexaminations. Health Phys1990; 59:295–298.42. Vano E, Guibelalde E, Fernandez JM,Gonzalez L, Ten JI. <strong>Patient</strong> dosimetryin interventional radiology using slowfilms. Br J Radiol 1997; 70:195–200.43. Nicholson R, Tuffee F, Uthappa MC.Skin sparing in interventional radiology:the effect of copper filtration. Br JRadiol 2000; 73:36–42.44. Fajardo LC, Geise RA, Ritenour ER. Asurvey of films <strong>for</strong> use as dosimeters ininterventional radiology. Health Phys1995; 68:595–599.45. Fletcher DW, Miller DL, Balter S, TaylorMA. Comparison of four techniquesto estimate radiation dose toskin during angiographic and interventionalradiology procedures. J VascInterv Radiol 2002; 13:391–397.46. Omary RA, Bettman MA, Cardella JF,et al. <strong>Quality</strong> improvement guidelines<strong>for</strong> the reporting and archiving ofinterventional radiology procedures. JVasc Interv Radiol 2002; 13:879–881.
Volume 20Number 7SMiller et al • S207SIR DISCLAIMERThe clinical practice guidelines of the Society of Interventional Radiology attempt to define practice principles thatgenerally should assist in producing high-quality medical care. These guidelines are voluntary and are not rules. Aphysician may deviate from these guidelines, as necessitated by the individual patient and available resources. Thesepractice guidelines should not be deemed inclusive of all proper methods of care or exclusive of other methods of carethat are reasonably directed toward the same result. Other sources of in<strong>for</strong>mation may be used in conjunction withthese principles to produce a process leading to high-quality medical care. The ultimate judgment regarding theconduct of any specific procedure or course of management must be made by the physician, who should consider allcircumstances relevant to the individual clinical situation. Adherence to the SIR <strong>Quality</strong> <strong>Improvement</strong> Program will notassure a successful outcome in every situation. It is prudent to document the rationale <strong>for</strong> any deviation from thesuggested practice guidelines in the department policies and procedure manual or in the patient’s medical record.