Diabetic Ketoacidosis Pathway - Children's Hospital Central California
Diabetic Ketoacidosis Pathway - Children's Hospital Central California
Diabetic Ketoacidosis Pathway - Children's Hospital Central California
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
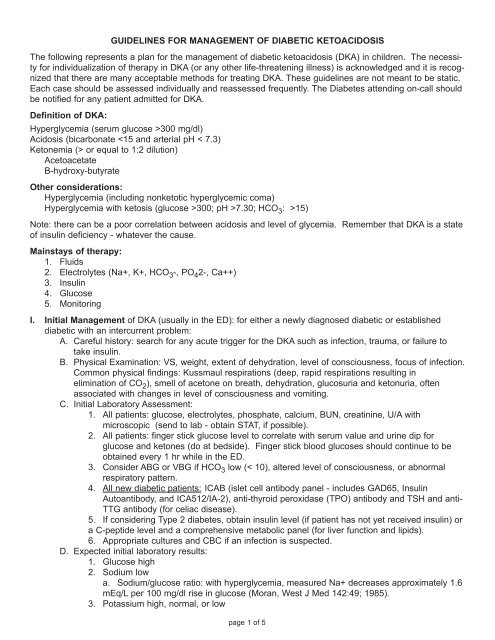
GUIDELINES FOR MANAGEMENT OF DIABETIC KETOACIDOSISThe following represents a plan for the management of diabetic ketoacidosis (DKA) in children. The necessityfor individualization of therapy in DKA (or any other life-threatening illness) is acknowledged and it is recognizedthat there are many acceptable methods for treating DKA. These guidelines are not meant to be static.Each case should be assessed individually and reassessed frequently. The Diabetes attending on-call shouldbe notified for any patient admitted for DKA.Definition of DKA:Hyperglycemia (serum glucose >300 mg/dl)Acidosis (bicarbonate or equal to 1:2 dilution)AcetoacetateB-hydroxy-butyrateOther considerations:Hyperglycemia (including nonketotic hyperglycemic coma)Hyperglycemia with ketosis (glucose >300; pH >7.30; HCO 3 : >15)Note: there can be a poor correlation between acidosis and level of glycemia. Remember that DKA is a stateof insulin deficiency - whatever the cause.Mainstays of therapy:1. Fluids2. Electrolytes (Na+, K+, HCO 3 -, PO 4 2-, Ca++)3. Insulin4. Glucose5. MonitoringI. Initial Management of DKA (usually in the ED): for either a newly diagnosed diabetic or establisheddiabetic with an intercurrent problem:A. Careful history: search for any acute trigger for the DKA such as infection, trauma, or failure totake insulin.B. Physical Examination: VS, weight, extent of dehydration, level of consciousness, focus of infection.Common physical findings: Kussmaul respirations (deep, rapid respirations resulting inelimination of CO 2 ), smell of acetone on breath, dehydration, glucosuria and ketonuria, oftenassociated with changes in level of consciousness and vomiting.C. Initial Laboratory Assessment:1. All patients: glucose, electrolytes, phosphate, calcium, BUN, creatinine, U/A withmicroscopic (send to lab - obtain STAT, if possible).2. All patients: finger stick glucose level to correlate with serum value and urine dip forglucose and ketones (do at bedside). Finger stick blood glucoses should continue to beobtained every 1 hr while in the ED.3. Consider ABG or VBG if HCO 3 low (< 10), altered level of consciousness, or abnormalrespiratory pattern.4. All new diabetic patients: ICAB (islet cell antibody panel - includes GAD65, InsulinAutoantibody, and ICA512/IA-2), anti-thyroid peroxidase (TPO) antibody and TSH and anti-TTG antibody (for celiac disease).5. If considering Type 2 diabetes, obtain insulin level (if patient has not yet received insulin) ora C-peptide level and a comprehensive metabolic panel (for liver function and lipids).6. Appropriate cultures and CBC if an infection is suspected.D. Expected initial laboratory results:1. Glucose high2. Sodium lowa. Sodium/glucose ratio: with hyperglycemia, measured Na+ decreases approximately 1.6mEq/L per 100 mg/dl rise in glucose (Moran, West J Med 142:49; 1985).3. Potassium high, normal, or lowpage 1 of 5