ABNORMAL VAGINAL BLEEDING IN PREd AND ... - Cancer Australia
ABNORMAL VAGINAL BLEEDING IN PREd AND ... - Cancer Australia
ABNORMAL VAGINAL BLEEDING IN PREd AND ... - Cancer Australia
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
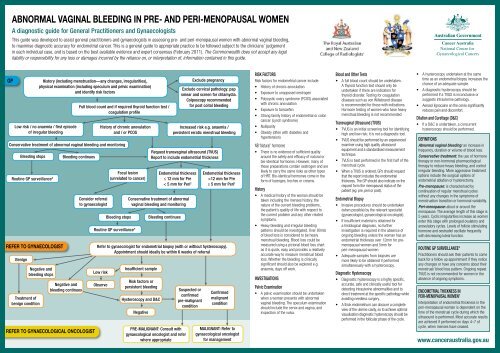
<strong>ABNORMAL</strong> <strong>VAG<strong>IN</strong>AL</strong> <strong>BLEED<strong>IN</strong>G</strong> <strong>IN</strong> PRE- <strong>AND</strong> PERI-MENOPAUSAL WOMENA diagnostic guide for General Practitioners and GynaecologistsThis guide was developed to assist general practitioners and gynaecologists in assessing pre- and peri-menopausal women with abnormal vaginal bleeding,to maximise diagnostic accuracy for endometrial cancer. This is a general guide to appropriate practice to be followed subject to the clinicians’ judgementin each individual case, and is based on the best available evidence and expert consensus (February 2011). The Commonwealth does not accept any legalliability or responsibility for any loss or damages incurred by the reliance on, or interpretation of, information contained in this guide.National Centre forGynaecological <strong>Cancer</strong>sGPRoutine GP surveillance*refer to gynaecologistHistory (including menstruation—any changes, irregularities),physical examination (including speculum and pelvic examination)and identify risk factorsLow risk / no anaemia / first episodeof irregular bleedingrefer to gynaecologiCAL ONCOLOGISTFull blood count and if required thyroid function test /coagulation profileConservative treatment of abnormal vaginal bleeding and monitoringBleeding stopsBenignTreatment ofbenign conditionNegative andbleeding stopsBleeding continuesNegative andbleeding continuesConsider referralto gynaecologistHistory of chronic anovulationand / or PCOSFocal lesion(unrelated to cancer)Bleeding stopsRoutine GP surveillance*Exclude pregnancyExclude cervical pathology: papsmear and screen for chlamydia.Colposcopy recommendedfor post coital bleedingRequest transvaginal ultrasound (TVUS)Report to include endometrial thicknessEndometrial thicknessEndometrial thickness< 5 mm for Peri † ≥ 5 mm for Peri †≤ 12 mm for Pre >12 mm for PreConservative treatment of abnormalvaginal bleeding and monitoringBleeding continuesIncreased risk e.g. anaemia /persistent erratic menstrual bleedingRefer to gynaecologist for endometrial biopsy (with or without hysteroscopy).Appointment should ideally be within 6 weeks of referralLow riskObserveInsufficient sampleRisk factors orpersistent bleedingHysteroscopy and D&CNegativePRE-MALIGNANT: Consult withgynaecological oncologist and referwhere appropriateSuspected orconfirmedpre-malignantconditionConfirmedmalignantconditionMALIGNANT: Refer togynaecological oncologistfor managementRISK FACTORSRisk factors for endometrial cancer include:• History of chronic anovulation• Exposure to unopposed oestrogen• Polycystic ovary syndrome (PCOS) associatedwith chronic anovulation• Exposure to tamoxifen• Strong family history of endometrial or coloncancer (Lynch syndrome)• Nulliparity• Obesity (often with diabetes andhypertension)NB ‘Natural’ hormones• There is no evidence of sufficient qualityaround the safety and efficacy of natural orbio-identical hormones. However, many ofthese preparations contain oestrogen and arelikely to carry the same risks as other typesof HRT. Bio-identical hormones come in theform of lozenges, troches or creams.History• A medical history of the woman should betaken including the menses history, thenature of the current bleeding problems,the patient’s quality of life with respect tothe current problem and any other relatedsymptoms.• Heavy bleeding and irregular bleedingpatterns should be investigated. Over 80mlsof blood loss is considered to be heavymenstrual bleeding. Blood loss could bemeasured using a pictorial blood loss chartas it is quick, easy and provides a relativelyaccurate way to measure menstrual bloodloss. Whether the bleeding is clinicallysignificant should also be explored e.g.anaemia, days off work.<strong>IN</strong>VESTIGATIONSPelvic Examination• A pelvic examination should be undertakenwhen a woman presents with abnormalvaginal bleeding. The speculum examinationshould include the cervix and vagina, andinspection of the vulva.Blood and Other Tests• A full blood count should be undertaken.A thyroid function test should only beundertaken if there are indicators forthyroid disorder. Testing for coagulationdiseases such as von Willebrand diseaseis recommended for those with indications.Hormone testing of women who have heavymenstrual bleeding is not recommended.Transvaginal Ultrasound (TVUS)• TVUS is an initial screening tool for identifyinghigh and low risk; it is not a diagnostic tool.• TVUS should be performed by an experiencedexaminer using high quality ultrasoundequipment and a standardised measurementtechnique.• TVUS is best performed in the first half of themenstrual cycle.• When a TVUS is ordered, GPs should requestthat the report includes the endometrialthickness. The GP should also indicate on therequest form the menopausal status of thepatient (eg. pre, peri or post).Endometrial Biopsy• Invasive procedures should be undertaken(when possible) by the relevant specialist(gynaecologist, gynaecological oncologist).• If insufficient material is obtained fora histological diagnosis, no furtherinvestigation is required in the absence ofongoing bleeding unless the woman has anendometrial thickness over 12mm for premenopausalwomen and 5mm forperi-menopausal women• Adequate samples from biopsies aremore likely to be obtained if performedsimultaneously with a hysteroscopy.Diagnostic Hysteroscopy• Diagnostic hysteroscopy is a highly specific,accurate, safe and clinically useful tool fordetecting intrauterine abnormalities and todirect treatment at the specific pathology whileavoiding needless surgery.• A thick endometrium can obscure a completeview of the uterine cavity, so to achieve optimalvisualisation diagnostic hysteroscopy should beperformed in the follicular phase of the cycle.• A hysteroscopy undertaken at the sametime as an endometrial biopsy increases thechance of an adequate sample.• A diagnostic hysteroscopy should beperformed if a TVUS is inconclusive orsuggests intrauterine pathology.• Aerosol lignocaine on the cervix significantlyreduces pain and discomfort.Dilation and Curettage (D&C)• If a D&C is undertaken, a concurrenthysteroscopy should be performed.DEF<strong>IN</strong>ITIONSAbnormal vaginal bleeding: an increase infrequency, duration or volume of blood loss.Conservative treatment: the use of hormonetherapy or non-hormonal pharmacologicaltherapy to reduce heavy bleeding, and controlirregular bleeding. More aggressive treatmentoptions include the surgical options ofendometrial ablation or hysterectomy.Pre-menopause: is characterised bycontinuation of regular menstrual cycleswithout any changes in the symptoms ofmenstruation transition or hormonal variability.Peri-menopause: about or around themenopause. The average length of this stage is5 years. Cyclic irregularities increase as womenenter this stage with prolonged ovulatory andanovulatory cycles. Levels of follicle stimulatinghormone and oestradiol oscillate frequentlywith decreasing luteal function.ROUT<strong>IN</strong>E GP SURVEILLANCE*Practitioners should ask their patients to comeback for a follow up appointment if they noticeany changes or have any concerns about theirmenstrual/ blood loss pattern. Ongoing repeatTVUS is not recommended for women in theabsence of ongoing symptoms.ENDOMETRIAL THICKNESS <strong>IN</strong>PERI-MENOPAUSAL WOMEN †Interpretation of endometrial thickness in theperi-menopausal woman is dependent on thetime of the menstrual cycle during which theultrasound is performed. Most accurate resultsare achieved if performed on days 4–7 ofcycle, when menses have ceased.www.canceraustralia.gov.au