Brochure - Associates in Newborn Medicine
Brochure - Associates in Newborn Medicine
Brochure - Associates in Newborn Medicine
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
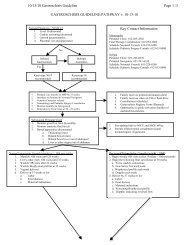
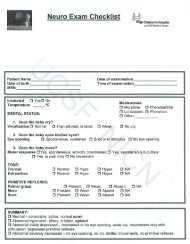
About Mild Systemic Hypothermia (MSH)• The goal of MSH is to cool the core body temperature <strong>in</strong> a rangebetween 33.5-34.5 C for 72 hours, beg<strong>in</strong>n<strong>in</strong>g as soon as possiblefollow<strong>in</strong>g successful resuscitation.• Cool<strong>in</strong>g can be achieved by us<strong>in</strong>g either a cool<strong>in</strong>g blanket(whole-body cool<strong>in</strong>g), or a cool<strong>in</strong>g cap (selective head cool<strong>in</strong>g).Both systems have been reviewed by the Federal DrugAdm<strong>in</strong>istration and have been shown effective <strong>in</strong> improv<strong>in</strong>goutcomes for <strong>in</strong>fants experienc<strong>in</strong>g HIE.Prepar<strong>in</strong>g a Baby With HIE for TransportA.Passively cool the baby as directed:– Turn off the overhead radiant warmer– Check the <strong>in</strong>fant’s rectal temperature every 30 m<strong>in</strong>utes– Place a blanket on the <strong>in</strong>fant only when the <strong>in</strong>fant’s temperature dropsto 35 C rectally– Cont<strong>in</strong>ue to check the <strong>in</strong>fants temperature every 30 m<strong>in</strong>utes– Do not let the <strong>in</strong>fant’s temperature drop below 35 C rectallyMild SystemicHypothermiaAt Children’s Hospitals and Cl<strong>in</strong>ics of M<strong>in</strong>nesotaChildren’s Hospitals and Cl<strong>in</strong>ics of M<strong>in</strong>nesota provides Mild SystemicHypothermia (MSH), or body cool<strong>in</strong>g therapy for <strong>in</strong>fants affectedby Hypoxic-ischemic Encephalopathy (HIE)—damage to cells <strong>in</strong> thecentral nervous system (the bra<strong>in</strong> and sp<strong>in</strong>al cord) from <strong>in</strong>adequateoxygen. The therapy prevents or reduces the severity of neurological<strong>in</strong>jury and improves functional outcomes for <strong>in</strong>fants.Hypothermia, achieved by selective head cool<strong>in</strong>g or whole-bodycool<strong>in</strong>g, is a new technique based on research demonstrat<strong>in</strong>greductions <strong>in</strong> bra<strong>in</strong> <strong>in</strong>jury follow<strong>in</strong>g HIE.• Published research <strong>in</strong>dicates that the sooner cool<strong>in</strong>g therapyis started <strong>in</strong> HIE <strong>in</strong>fants, the more likely it will effectivelyimprove outcomes.• After cool<strong>in</strong>g therapy has been adm<strong>in</strong>istered for more than72 hours, the patient will undergo gradual re-warm<strong>in</strong>g at no morethan 0.5 C per hour dur<strong>in</strong>g the subsequent four to six hours.Infant Care Dur<strong>in</strong>g Cool<strong>in</strong>g Therapy• Dur<strong>in</strong>g the <strong>in</strong>itial cool<strong>in</strong>g phase—before the <strong>in</strong>fant reaches thetarget body temperature—noth<strong>in</strong>g is placed between the babyand the cool<strong>in</strong>g system and the <strong>in</strong>fant wears only a diaper.• Once the <strong>in</strong>fant reaches the targeted temperature range,33.5-34.5 C, a sheet may be placed between the baby andthe cool<strong>in</strong>g system. A cloth diaper may also be placed underthe <strong>in</strong>fant’s head for comfort.B.Cont<strong>in</strong>ue discussion with NICU staff for ongo<strong>in</strong>g managementCollaborat<strong>in</strong>g With Regional Care ProvidersChildren’s neonatal team members work closely with referr<strong>in</strong>g hospitals to coord<strong>in</strong>atesafe and timely <strong>in</strong>fant transports. We work with referr<strong>in</strong>g providers to ensure the bestpossible care until transport occurs, and provide detailed status updates on all <strong>in</strong>fantreferrals. When the transport team arrives:• The family will be asked to give permission to Children’s staff to share <strong>in</strong>formationwith the referr<strong>in</strong>g hospital staff.• Providers can receive updates from Children’s neonatologists by call<strong>in</strong>g:Children’s - St. Paul NICU: (651) 220-6210Children’s - M<strong>in</strong>neapolis NICU: (612) 813-6295About Per<strong>in</strong>atal Asphyxia And Hypoxic-Ischemic Encephalopathy (HIE)• Hypoxic-ischemic events that occur around the time of birth mayresult <strong>in</strong> bra<strong>in</strong> <strong>in</strong>jury called encephalopathy.• At birth, these <strong>in</strong>fants usually have a need for resuscitationand experience neurological depression, seizures, andelectroencephalographic abnormalities.• They have an <strong>in</strong>creased risk of death or neuro-developmentalabnormalities later <strong>in</strong> <strong>in</strong>fancy if the encephalopathy seen at birthis severe.• Recent randomized trials <strong>in</strong> full-term and near full-term newbornssuggest that treatment with MSH is safe and may improve survivalwithout disabilities up to 18 months of age, but long-term efficacyand safety are yet to be established.Mild Systemic Hypothermia is a standard of care at most Level IIIneonatal centers. Children’s was the first <strong>in</strong> the state to offer MSHtreatment. Today, our comb<strong>in</strong>ation of experience and expert subspecialists—<strong>in</strong>clud<strong>in</strong>gneurologists, neurosurgeons, hematologists, andoncologists—work together to provide the best <strong>in</strong> cool<strong>in</strong>g therapy toprevent or reduce the severity of neurologic <strong>in</strong>jury associated with HIE.
Patient Eligibility Criteriafor TherapyA. Infant must be > 36 weeks gestational age, >1,800B.grams, and must have at least one of the follow<strong>in</strong>g:– Apgar score of < 5 at 10 m<strong>in</strong>utes after birth– Cont<strong>in</strong>ued need for resuscitation, <strong>in</strong>clud<strong>in</strong>gendotracheal or mask ventilation, at 10 m<strong>in</strong>utesafter birth– Acidosis def<strong>in</strong>ed as either umbilical cord pH orany arterial pH with<strong>in</strong> 60 m<strong>in</strong>utes of birth < 7.0– Base Deficit > 16 mmol/L from cord or other<strong>in</strong>fant blood sample with<strong>in</strong> 60 m<strong>in</strong>utes of birthInfant must have seizures, or alternatively, moderateto severe encephalopathy, def<strong>in</strong>ed by an alteredstate of consciousness, with at least three of thefollow<strong>in</strong>g (see chart on the right):Moderate to Severe EncephalopathyCategory Moderate Encephalopathy Severe Encephalopathy1. Level of consciousness Lethargic Stupor or coma2. Spontaneous activity Decreased activity No activity3. Posture Distal flexion, complete extension Decerebrate4. Tone Hypotonia (focal or general) Flaccid5. Primitive reflexesSuck Weak AbsentMoro Incomplete Absent6. Autonomic systemPupils Constricted Deviated, dilated, or non-reactive to lightHeart rate Bradycardia VariableRespiration Periodic breath<strong>in</strong>g ApneaN Engl J Med 2005; 353: 1574-84exclusion criteriaExclusion criteria <strong>in</strong>cludes:• Birth weight < 1,800 grams• Gestational age < 36 weeks• Condition deemed <strong>in</strong>compatible with survival• Inability to <strong>in</strong>itiate cool<strong>in</strong>g with<strong>in</strong> six hours of birth• Presence of known major congenital anomalies or recognizedchromosomal abnormalitiesPotential Harmful Effects of Cool<strong>in</strong>g• MSH has been shown as a safe, effective therapy <strong>in</strong> randomizedcontrolled trials where the targeted core body temperatureranged between 33.5-34.5 C.• No harmful side effects, with the exception of occasional benignslow<strong>in</strong>g of the heart rate, were observed <strong>in</strong> these trials.• Cool<strong>in</strong>g below a core temperature of 32 C may produceimpairment of heart functions and other problems, <strong>in</strong>clud<strong>in</strong>gneutropenia, thrombocytopenia, and hypokalemia.Cool<strong>in</strong>g should be started no laterthan six hours after birth.Therapy should be started as soonas the <strong>in</strong>fant is deemed eligible.If you are unsure whether a baby qualifies for therapy, please callthe NICU at Children’s immediately for consultation.• Children’s - St. Paul NICU: (651) 220-6650• Children’s - M<strong>in</strong>neapolis NICU: (612) 813-6295