Ocular Response Analyzer in Children Dr. Kaushik Hegde
Ocular Response Analyzer in Children Dr. Kaushik Hegde
Ocular Response Analyzer in Children Dr. Kaushik Hegde
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
CORNEA SESSION - III<br />
<strong>Ocular</strong> <strong>Response</strong> <strong>Analyzer</strong> <strong>in</strong> <strong>Children</strong><br />
<strong>Dr</strong>. <strong>Kaushik</strong> <strong>Hegde</strong>, <strong>Dr</strong>. Rohit Shetty, <strong>Dr</strong>. Ajoy V<strong>in</strong>cent, <strong>Dr</strong>. Harsha K.<br />
(Present<strong>in</strong>g Author: <strong>Dr</strong>. <strong>Kaushik</strong> Hedge)<br />
Corneal biomechanics and its relevance <strong>in</strong> the<br />
diseases of the cornea1,2 keratorefractive<br />
surgeries3,4 and measurement of Intra ocular<br />
pressure (IOP) 4,5 is an area of <strong>in</strong>tense and ongo<strong>in</strong>g<br />
research. Various techniques have been<br />
235<br />
described to measure this parameter some of<br />
them be<strong>in</strong>g the dynamic corneal imag<strong>in</strong>g 6 , high<br />
speed optical tomography 7 and more recently the<br />
ocular response analyser 3 (ORA; Reichert<br />
Ophthalmic Instruments, Depew, New York,
236 AIOC 2010 PROCEEDINGS<br />
USA).<br />
The pr<strong>in</strong>ciple of the ORA is based on non-contact<br />
tonometry (a patented bidirectional applanation<br />
event). 1 In addition to the IOP, it gives the<br />
measure of biomechanical properties of the<br />
cornea referred to as corneal hysteresis.<br />
Hysteresis refers to the energy lost dur<strong>in</strong>g the<br />
stress-stra<strong>in</strong> cycle. As with most biological<br />
materials, collagen is a viscoelastic material and<br />
therefore the cornea exhibits hysteresis.<br />
The effect of central corneal thickness (CCT) on<br />
IOP measurement is well known8,9 Corneal<br />
hysteresis may more effectively describe the<br />
contribution of corneal resistance to IOP<br />
measurements than CCT alone. 1 Prelim<strong>in</strong>ary<br />
studies have reported reduced hysteresis <strong>in</strong><br />
keratoconus, fuch’s dystrophy3 , primary open<br />
angle glaucoma and normal tension glaucoma1.<br />
Biomechanical properties of the cornea <strong>in</strong><br />
children10,11 or its contribution to the<br />
measurement of IOP12 are be<strong>in</strong>g better<br />
established.<br />
The primary aim of this study is to measure<br />
corneal hysteresis <strong>in</strong> children us<strong>in</strong>g ORA, with<br />
the <strong>in</strong>tention to provide a reference to establish<br />
the normative values and ranges of the corneal<br />
biomechanical parameters. The secondary<br />
objective is to study the correlation between the<br />
various biomechanical parameters <strong>in</strong> refractive<br />
error subgroups, and discuss the scope of its<br />
utility as a cl<strong>in</strong>ical tool.<br />
Materials and Methods<br />
Study design: Prospective, non-<strong>in</strong>terventional,<br />
cross sectional case series.<br />
Subjects and exam<strong>in</strong>ations: Informed consent<br />
was taken from the accompany<strong>in</strong>g parent or<br />
guardian, and <strong>in</strong>stitutional ethical review board<br />
clearance was obta<strong>in</strong>ed. All children(less than 16<br />
years) underwent a complete eye exam<strong>in</strong>ation.<br />
Any child with a history of ocular <strong>in</strong>fection,<br />
ocular allergy, ocular surgery and other causes<br />
known to affect the corneal hysteresis, as well as<br />
children unable to cooperate with the procedure<br />
were excluded from the study. The child was<br />
comfortably seated and asked to fixate on the<br />
green light <strong>in</strong> the <strong>in</strong>strument. ORA recorded<br />
corneal hysteresis (CH), corneal resistance factor<br />
(CRF) and two <strong>in</strong>traocular pressure<br />
measurements: <strong>in</strong>traocular pressure corneal<br />
compensated (IOPcc), which is reportedly<br />
<strong>in</strong>dependent of corneal thickness3,4 and<br />
<strong>in</strong>traocular pressure Goldmann-correlated<br />
(IOPg), which is <strong>in</strong>fluenced by corneal thickness.<br />
A m<strong>in</strong>imum of 4 read<strong>in</strong>gs were taken per eye and<br />
the best of the 4 read<strong>in</strong>gs was selected for<br />
analysis. CCT was measured us<strong>in</strong>g the IOPac<br />
Hand-Held Pachymeter (Standard, Model: 16011,<br />
Heidelberg Eng<strong>in</strong>eer<strong>in</strong>g, Inc., Germany). The<br />
probe was gently placed on the cornea <strong>in</strong> the mid<br />
pupillary plane <strong>in</strong> a perpendicular orientation, a<br />
m<strong>in</strong>imum of 20 read<strong>in</strong>gs were taken and<br />
averaged out to get the mean CCT. The children<br />
were dilated with cyclopentolate (0.5%, twice at<br />
an <strong>in</strong>terval of 30 m<strong>in</strong>utes) and refracted (NIDEK;<br />
AR-600, Japan). The spherical equivalent was<br />
noted which was verified by objective refraction.<br />
For the purpose of analysis the children were<br />
categorized <strong>in</strong>to 3 subgroups based on the<br />
refractive error (spherical equivalent) 13: >-0.50D<br />
(myopic), +2.00D to -0.50D (emmetropic),<br />
>+2.00D (hyperopic).<br />
Statistical analysis: Statistical Analysis was<br />
performed us<strong>in</strong>g Stastical Package for Social<br />
Sciences (version 10.5, SPSS Inc). Group<br />
differences for cont<strong>in</strong>uous variables were tested<br />
us<strong>in</strong>g the unpaired student t tests and one-way<br />
analysis of variance (ANOVA) for normally<br />
distributed data. Results are presented as mean<br />
± standard deviation [SD]. All statistical tests<br />
were two-tailed, and P value less than 0.05 was<br />
considered to <strong>in</strong>dicate statistical significance.<br />
Correlations between sub-groups were analyzed<br />
us<strong>in</strong>g the Pearson correlation coefficient.<br />
Results<br />
A total of 150 eyes of 76 patients with 42 male<br />
(55.3%), 34 female (44.7%), with a mean age of<br />
10.21 ± 3.2 years (range of 4 – 16 years) were<br />
exam<strong>in</strong>ed.<br />
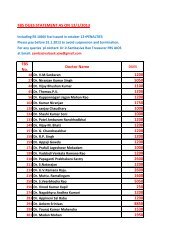
The mean CH was 10.71 ± 1.44 mm of Hg, mean<br />
CRF was 10.80 ± 1.94 mm of Hg, and the mean ±<br />
SD of the various parameters for the entire group<br />
is shown <strong>in</strong> table 1.<br />
None of the parameters showed any significant<br />
difference with age or sex with the student t test<br />
(table 2).<br />
IOPcc showed positive correlation with IOPg (r<br />
= 0.88), CRF(r = 0.4), CCT(r = 0.28) and negative<br />
correlation with CH(r = -0.25) and SE(r = -0.23).<br />
IOPg showed a positive correlation with CRF (r =<br />
0.7), CH (r = 0.2) and CCT(r = 0.5). CRF showed
CORNEA SESSION - III<br />
Table-1: Mean and Range of the various<br />
parameters of the entire sample<br />
Variables Mean ±Std. Range<br />
N= 150 Deviation (SD)<br />
IOPcc ( mm of Hg) 15.83 ± 3.30 6.7 - 24.0<br />
IOPg ( mm of Hg) 15.70 ± 3.79 8.5 - 26.8<br />
CH ( mm of Hg) 10.71 ± 1.44 6.6 - 14.3<br />
CRF ( mm of Hg) 10.80 ± 1.94 5.6 - 18.4<br />
CCT(µm)<br />
Spherical<br />
549.93 ± 33.97 474- 650<br />
equivalent (DS) 0.50 ± 3.40 -13.50 - 10.75<br />
mm of Hg: millimeter of mercury,<br />
DS: Diopter sphere.<br />
µm: micro meter,<br />
Table-2: Correlation of the various biomechanical<br />
parameters with age and sex<br />
(student t test, unpaired).<br />
Biomechanical Age Sex<br />
parameters (P value) (P value)<br />
IOPcc 0.43 0.17<br />
IOPg 0.45 0.11<br />
CH 0.97 0.68<br />
CRF 0.50 0.40<br />
CCT 0.29 0.83<br />
Spherical Equivalent 0.10 0.91<br />
a positive correlation with both CH (r = 0.64), and<br />
CCT(r = 0.64). CH showed a positive correlation<br />
with CCT(r = 0.5).<br />
The distributions of the parameters <strong>in</strong> the 3<br />
subgroup population, consist<strong>in</strong>g of myopic,<br />
emmetropic and hypermetropic children are<br />
shown <strong>in</strong> table 3.<br />
In one way ANOVA a significant difference was<br />
seen between the 3 subgroups among various<br />
parameters (table 4) except CH (P = 0.05). Post<br />
hoc test showed significant difference between<br />
emmetropic and hypermetropic groups for CRF<br />
(P = 0.02), CH (P = 0.01) and CCT (P = .007) and<br />
between myopic and hypermetropic groups for<br />
IOPcc (P = 0.006) and IOPg (P= 0.04) (table 5).<br />
Graphs 1 and 2 represent the CH (r2 = 0.022) and<br />
Table-3: Biomechanical parameters <strong>in</strong> Myopia, Emmetropia and Hypermetropia (±SD)<br />
Subgroups (DS) IOPcc IOPg CH CRF CCT<br />
(mm of Hg) (mm of Hg) (mm of Hg) (mm of Hg) (µm)<br />
> -0.5 (n = 42) 16.90 ± 3.28 16.95 ± 4.25 10.72 ± 1.27 11.11 ± 2.03 554.02 ±35.46<br />
-0.5 - 1.99 (n = 77) 15.67 ± 3.09 15.25 ± 3.74 10.49 ± 1.27 10.41 ± 1.77 542.81 ± 33.58<br />
≥+2.00 (n = 31) 14.75 ± 3.48 15.12 ± 2.86 11.23 ± 1.87 11.33 ± 2.05 562.10 ± 29.14<br />
Total (n=150) 15.83 ± 3.30 15.70 ± 3.79 10.71 ± 1.43 10.80 ± 1.93 549.93 ± 33.97<br />
237<br />
Figure-1: Shows a scatter plot of the corneal hysteresis<br />
(CH) <strong>in</strong> mm of Hg along the y-axis and the refractive<br />
error (spherical equivalent <strong>in</strong> DS) along the x- axis.<br />
Statistical analysis <strong>in</strong>dicates a weak positive correlation<br />
of CH with the refractive error, <strong>in</strong>dicat<strong>in</strong>g possibly that<br />
as the refractive error moves towards hyperopia the CH<br />
also <strong>in</strong>creases.<br />
Figure-2: Shows a scatter plot of the corneal resistance<br />
factor (CRF) <strong>in</strong> mm of Hg along the y-axis and<br />
the refractive error (spherical equivalent <strong>in</strong> DS) along<br />
the x- axis. Statistical analysis <strong>in</strong>dicates a weak positive<br />
correlation of CH with the refractive error, <strong>in</strong>dicat<strong>in</strong>g<br />
possibly that as the refractive error moves towards<br />
hyperopia the CRF also <strong>in</strong>creases.<br />
CRF (r2 = 0.002) plotted aga<strong>in</strong>st the refractive<br />
error. As the refractive error moves towards<br />
hyperopia, the biomechanical parameters also<br />
<strong>in</strong>crease, <strong>in</strong>dicat<strong>in</strong>g a weak positive correlation.
238 AIOC 2010 PROCEEDINGS<br />
Table-4: Correlation of the various biomechanical<br />
parameters with<strong>in</strong> the subgroups (student t<br />
test, unpaired)<br />
Biomechanical Significance<br />
parameter (P value)<br />
IOPcc 0.02<br />
IOPg 0.04<br />
CH 0.05<br />
CRF 0.03<br />
CCT 0.02<br />
Table-5: Comparison of corneal biomechanical<br />
parameters among refractive error subgroups<br />
Para- Sub groups Significance<br />
meters (P value)<br />
IOPcc Myopia with Emmetropia .05<br />
Myopia with Hypermetropia .006<br />
Emmetropia with Hypermetropia .18<br />
IOPg Myopia with Emmetropia .02<br />
Myopia with Hypermetropia .04<br />
Emmetropia with Hypermetropia .87<br />
CH Myopia with Emmetropia .39<br />
Myopia with Hypermetropia .13<br />
Emmetropia with Hypermetropia .02<br />
CRF Myopia with Emmetropia .06<br />
Myopia with Hypermetropia .63<br />
Emmetropia with Hypermetropia .03<br />
CCT Myopia with Emmetropia .08<br />
Myopia with Hypermetropia .31<br />
Emmetropia with Hypermetropia .007<br />
Where: Myopia (spherical equivalent > - 0.5 DS)<br />
Emmetropia (spherical equivalent between - 0.5 DS and<br />
+ 2.00 DS)<br />
Hypermetropia (spherical equivalent > + 2.00 DS)<br />
Table-6: Comparison of mean CH with other<br />
reported studies<br />
Variable Kirwan Song Indian<br />
(mean) et al10 et al11 children<br />
(our data)<br />
Age(years)<br />
CH with SD<br />
11.2(0.8) 14.7(3.2) 10.3(3.2)<br />
(mm of Hg) 12.3(1.3) 10.7(1.5) 10.70(1.3)<br />
Discussion<br />
Corneal hysteresis is thought to represent the<br />
cumulative effects of corneal thickness,<br />
hydration, rigidity, and other as yet<br />
undeterm<strong>in</strong>ed factors14. The mean CH and CRF<br />
were 10.71 ± 1.45 mm of Hg and 10.80 ± 1.90 mm<br />
of Hg respectively. In this study there was no<br />
statistically significant relationship with the<br />
student t test for both CH and CRF with age (P =<br />
0.97), (P = 0.5) or sex (P = 0.68), (P = 0.4). Earlier<br />
reported literature does mention of an <strong>in</strong>verse<br />
relationship between age and corneal<br />
biomechanics. 15,16,17 The corneal thickness <strong>in</strong><br />
children reaches adult dimensions by 5-9 years of<br />
age. 18 Physiological changes do cont<strong>in</strong>ue<br />
throughout their life. In this study the CH was<br />
similar to that reported on adults1, the authors<br />
could not f<strong>in</strong>d an <strong>in</strong>verse relationship with age<br />
possibly due to the fact that the range of age<br />
groups among whom this study was conducted<br />
was too small to establish a significant change.<br />
The results of our children were similar to those<br />
found <strong>in</strong> Asian Ch<strong>in</strong>ese children11 (Table 6), but<br />
were lesser than what was reported on Caucasian<br />
children. 10<br />
As reported by others <strong>in</strong> adults14, CRF showed a<br />
positive correlation with both CH (r = 0.67), and<br />
CCT(r = 0.64) 19, so also did CH with CCT(r =<br />
0.54) 19. This suggests that the corneal thickness<br />
is an important factor <strong>in</strong> determ<strong>in</strong><strong>in</strong>g<br />
biomechanical properties of the eye.<br />
CRF (P = 0.03) and CCT (P = 0.02) showed<br />
significant difference between the refractive error<br />
subgroups. A post hoc test revealed CH (P = 0.02)<br />
and CRF (P = 0.03) to be significantly higher <strong>in</strong><br />
hypermetropes than emmetropes. This could<br />
possibly be due to a significantly higher CCT (P<br />
= 0.007) <strong>in</strong> the hyperopes <strong>in</strong> our sample, although<br />
it is generally accepted that CCT is <strong>in</strong>dependent<br />
of the refractive error status. 20 Reported literature<br />
does <strong>in</strong>dicate that CH does not vary <strong>in</strong> myopia,<br />
or its progression. 19,21 In this study there was no<br />
significant difference <strong>in</strong> the value of CH (P = 0.13)<br />
between the myopic and hyperopic groups,<br />
though a significant difference <strong>in</strong> the value of CH<br />
was seen between emmetropic and hyperopic<br />
groups (P = 0.02). None of the reported studies<br />
had hyperopic group as a control to identify any<br />
significant association between refractive error<br />
groups.<br />
In our study there was no correlation between<br />
IOPcc and IOPg with age (P = 0.4), (P = 0.5) or sex<br />
(P = 0.2), (P = 0.1). On analyz<strong>in</strong>g the parameters<br />
across various subgroups, IOPcc and IOPg<br />
<strong>in</strong>creased <strong>in</strong> the same proportion with refractive<br />
error. In each group, measured IOP values were<br />
strongly and positively correlated with each (r =<br />
0.9, r = 0.9, r = 0.8; among myopic, emmetropic
CORNEA SESSION - III<br />
and hyperopic groups respectively). This is a<br />
little surpris<strong>in</strong>g as the IOPcc values are supposed<br />
to be <strong>in</strong>dependent of corneal parameters like<br />
CCT and corneal biomechanics, and one would<br />
ideally expect varied correlation of IOPcc with<br />
IOPg. As the IOPcc takes <strong>in</strong>to consideration the<br />
viscoelastic nature of the cornea to evaluate the<br />
‘‘corneal-compensated IOP,’’ we can expect to<br />
f<strong>in</strong>d a significant difference between IOPcc and<br />
IOPg when tissue viscous damp<strong>in</strong>g is abnormal. 22<br />
The normal range of the biomechanical<br />
parameters would probably expla<strong>in</strong> the positive<br />
correlation between the IOP values <strong>in</strong> our<br />
subgroups.<br />
IOPcc (P = 0.006) and IOPg (P = 0.04) was found<br />
to be more <strong>in</strong> myopic than hyperopic eyes (table<br />
5), although the CCT between the 2 groups <strong>in</strong> our<br />
study was not significant (P = 0.31). S<strong>in</strong>ce myopes<br />
are known to have a higher IOP23 than nonmyopes<br />
and myopia is a def<strong>in</strong>ite risk factor for<br />
the development of glaucoma23, 24, 25 the same<br />
pattern may exists <strong>in</strong> children too.<br />
CH is likely to be a useful additional<br />
measurement to assess the progression of<br />
diseases of the cornea, as it may change before<br />
topographic or cl<strong>in</strong>ical changes becomes<br />
apparent. 1,2 S<strong>in</strong>ce the CCT <strong>in</strong> Asian Indian<br />
population is known to be lesser than that found<br />
<strong>in</strong> other parts of the world, 26 and also keratoconus<br />
that is known to present itself at an earlier age<br />
1. David A. Luce. Determ<strong>in</strong><strong>in</strong>g <strong>in</strong> vivo biomechanical<br />
properties of the cornea with an ocular response<br />
analyzer. J Cataract Refract Surg 2005;31:156–62.<br />
2. Dolores Ortiz, David P<strong>in</strong>˜ ero, Mohamed H.<br />
Shabayek. Corneal biomechanical properties <strong>in</strong><br />
normal, post-laser <strong>in</strong> situ keratomileusis, and<br />
keratoconic eyes. J Cataract Refract Surg<br />
2007;33:1371–5 .<br />
3. Jun Liu, Cynthia J. Roberts. Influence of corneal<br />
biomechanical properties on <strong>in</strong>traocular pressure<br />
measurement. J Cataract Refract Surg 2005;31:146–55.<br />
4. Doughty MJ, Zaman ML. Human corneal thickness<br />
and its impact on <strong>in</strong>traocular pressure measures: a<br />
review and meta-analysis approach. Surv<br />
Ophthalmol 2000;44:367–408.<br />
5. Jay S. Pepose, Susan K. Feigenbaum, Mujtaba A.<br />
Quazi, Jeffrey P. Sanderson, and Cynthia J. Roberts.<br />
Changes <strong>in</strong> Corneal Biomechanics and Intraocular<br />
Pressure Follow<strong>in</strong>g LASIK us<strong>in</strong>g Static, Dynamic,<br />
and Noncontact Tonometry. Am J Ophthalmol<br />
2007;143:39–47.<br />
References<br />
239<br />
among Indians, 27 plann<strong>in</strong>g refractive surgery <strong>in</strong><br />
adults should <strong>in</strong>corporate CH and CRF<br />
measurements. This could also be applied to the<br />
controversial pediatric LASIK whose <strong>in</strong>dications<br />
are now be<strong>in</strong>g more clearly def<strong>in</strong>ed. 28 Keep<strong>in</strong>g<br />
these factors <strong>in</strong> m<strong>in</strong>d record<strong>in</strong>g the<br />
biomechanical parameters and monitor<strong>in</strong>g it over<br />
time would prove useful.<br />
Though the ORA is able to measure corneal<br />
biomechanical parameters; the exact area of<br />
applanation on the cornea is not well def<strong>in</strong>ed.<br />
Know<strong>in</strong>g the applanation surface may provide<br />
additional <strong>in</strong>formation about corneal behavior<br />
and corneal properties. S<strong>in</strong>ce it requires<br />
cooperation of the children, the authors found it<br />
difficult to perform ORA on children less than 5<br />
years of age.<br />
The authors found that the CH <strong>in</strong> a sample of<br />
Asian Indian children is similar to those from<br />
children and adults <strong>in</strong> other parts of the world.<br />
The corneal biomechanical parameters of CH and<br />
CRF varied with the refractive status of a child. It<br />
was higher <strong>in</strong> hyperopes. The IOPg and IOPcc<br />
correlated strongly with each other and myopes<br />
had a higher pressure when compared to the<br />
hyperopes. Thus the corneal biomechanical<br />
parameters could possibly help <strong>in</strong> understand<strong>in</strong>g<br />
disease processes of the cornea, as an aid <strong>in</strong><br />
keratorefractive surgeries, and as an IOP<br />
measurement tool <strong>in</strong> children.<br />
6. Gu¨nther Grabner, Re<strong>in</strong>hard Eilmste<strong>in</strong>er, Christian<br />
Ste<strong>in</strong>dl, Dipl-Ing, Jeef Ruckhofer, Renzo Mattioli,<br />
Dipl-Ing, and Wolfgang Hus<strong>in</strong>sky. Dynamic<br />
Corneal imag<strong>in</strong>g. J Cataract Refract Surg<br />
2005;31:163–74.<br />
7. Yan Li, Marcelo V. Netto, Raj Shekhar, Ronald R<br />
Krueger, and David Huang. A Longitud<strong>in</strong>al Study<br />
of LASIK Flap and Stromal Thickness with Highspeed<br />
Optical Coherence Tomography.<br />
Ophthalmology 2007;114:1124–32.<br />
8. Doughty MJ, Zaman ML: Human corneal thickness<br />
and its impact on <strong>in</strong>traocular pressure measures: a<br />
review and meta analysis approach. Surv<br />
Ophthalmol 2000;44:367-408.<br />
9. Kohlhaas M, Boehm AG, Spoerl E, Pursten A, Gre<strong>in</strong><br />
HJ, and Pillunat LE. Effect of central corneal<br />
thickness, corneal curvature, and axial length on<br />
applanation tonometry. Arch Ophthalmol<br />
2006;124:471–6.<br />
10. Caitriona Kirwan, Micheal O’Keefe, Bernadette<br />
Lanigan, RN. Corneal Hysteresis and Intraocular
240 AIOC 2010 PROCEEDINGS<br />
Pressure measurement <strong>in</strong> children us<strong>in</strong>g the<br />
Riechert <strong>Ocular</strong> <strong>Response</strong> analyzer. Am J Ophthalmol<br />
;142:990-2.<br />
11. Song Y, Congdon N, Li L, et al. Corneal hysteresis<br />
and axial length among Ch<strong>in</strong>ese secondary school<br />
children: The Xichang Pediatric Refractive Error<br />
Study (X-PRES) Report No. 4. Am J Ophthalmol 2008;<br />
145:819–26.<br />
12. Kelly W. Muir, J<strong>in</strong>g J<strong>in</strong>, Sharon F. Freedman .<br />
Central Corneal Thickness and Its a.Relationship to<br />
Intraocular Pressure <strong>in</strong> <strong>Children</strong>. Ophthalmology<br />
2004;111:2220-3.<br />
13. Robaei D, Kifley A, Rose KA, Mitchell P. Refractive<br />
error and patterns of spectacle use <strong>in</strong> 12-year-old<br />
Australian children. Ophthalmology 2006;113(9):<br />
1567-73.<br />
14. Sunil Shah, Mohammed Liakuzzaman, Ian Cunliffe,<br />
Sanjay Mantry. The use of ocular response analyzer<br />
to establish the relationship between ocular<br />
hysteresis, corneal resistance factor and central<br />
corneal thickness <strong>in</strong> normal eyes. Contact lens and<br />
Anterior eye 2006;29:257-62.<br />
15. Teruyo Kida, John H. K. Liu, and Robert N.<br />
We<strong>in</strong>reb. Effects of Ag<strong>in</strong>g on Corneal<br />
Biomechanical Properties and Their Impact on 24hour<br />
Measurement of Intraocular Pressure. Am J<br />
Ophthalmol 2008;146:567–72.<br />
16. Elsheikh A, Wang D, Brown M, et al: Assessment of<br />
corneal biomechanical properties and their<br />
variation with age. Curr Eye Res 32:11-19.<br />
17. Daxer A, Misof K, Grabner B, et al. Collagen fibrils<br />
<strong>in</strong> the human corneal stroma: structure and ag<strong>in</strong>g.<br />
Invest Ophthalmol Vis Sci 1998;39:644–8.<br />
18. Mohamed A.W. Husse<strong>in</strong>, Evelyn A. Paysse,<br />
Nicholas P. Bell, David K. Coats, Kathryn M. Brady<br />
McCreery, Douglas D. Koch, Silvia Orengo-nania,<br />
Darrell Bask<strong>in</strong>, and Kirk R Wilhelmus. Corneal<br />
thickness <strong>in</strong> <strong>Children</strong>. Am J Ophthalmol<br />
2004;138:744-8.<br />
19. Lim L, Gazzard G, Chan YH, Fong A, Kotecha A,<br />
Sim EL, Tan D, Tong L, and a.Saw SM. Cornea<br />
biomedical characteristics and their correlates with<br />
refractive error <strong>in</strong> S<strong>in</strong>gaporean children. Invest<br />
Ophthalmol Vis Sci. 2008;49(9):3852-7.<br />
20. N. M. Radcliffe, J. Ste<strong>in</strong> and E. Farris. Relationship<br />
between central corneal a. thickness and refractive<br />
error <strong>in</strong> Caucasian and African American Glaucoma<br />
patients. Invest Ophthalmol Vis Sci 2005;46: E-<br />
Abstract 3656@ 2005 ARVO.<br />
21. Shen M, Fan F, Xue A, Wang J, Zhou X, and Lu F.<br />
Biomechanical properties of a. the cornea <strong>in</strong> high<br />
myopia. Vision Res. 2008;48(21):2167-71.<br />
22. David Touboul, Cynthia Roberts, Julien Ke´rautret,<br />
Carol<strong>in</strong>e Garra, a. Sylvie Maurice-Tison, Elodie<br />
Saubusse and Joseph Col<strong>in</strong>. Correlations between<br />
corneal hysteresis, <strong>in</strong>traocular pressure, and corneal<br />
central pachymetry. J Cataract Refract Surg 2008;<br />
34:616–22. Q 2008 ASCRS and ESCRS.<br />
23. Mitchell P, Hourihan F, Sandbach J, Wang JJ. The<br />
relationship between glaucoma and myopia: the<br />
Blue Mounta<strong>in</strong>s Eye Study. Ophthalmology.<br />
2000;107(6):1026-7.<br />
24. Hideki Nomura, Fujiko Ando, Naoakira Ni<strong>in</strong>o,<br />
Hiroshi Shimokata and Yozo Miyake. The<br />
relationship between <strong>in</strong>traocular pressure and<br />
refractive error adjust<strong>in</strong>g for age and central corneal<br />
thickness. Ophthalmic and Physiological Optics<br />
;24:1:41–5.<br />
25. Qu<strong>in</strong>n GE, Berl<strong>in</strong> JA, Young TL, Ziylan S, Stone RA.<br />
Association of <strong>in</strong>tra ocular pressure and myopia <strong>in</strong><br />
children. Ophthalmology. 1995;102(2):180-5.<br />
26. Kathleen S. Kunert, Prashant Bhartiya, Radhika<br />
Tandon, et al. Central Corneal Thickness <strong>in</strong> Indian<br />
Patients Undergo<strong>in</strong>g LASIK for Myopia. J Cataract<br />
Refract Surg 2003;19: 378-9.<br />
27. Jagjit S Sa<strong>in</strong>i, Vandana Saroha, P S<strong>in</strong>gh et al.<br />
Keratoconus <strong>in</strong> Asian eyes at a tertiary eye care<br />
facility. Cl<strong>in</strong> Exp Optom 2004;87(2):97–101.<br />
28. William F. Astle, Peter T. Huang, April D. Ingram,<br />
R. Peter Farran. Laser- assisted subepithelial<br />
keratectomy <strong>in</strong> children. J Cataract Refract Surg<br />
2004;30:2529–35.