osa related to vagal nerve stimulator therapy: a sleep center
osa related to vagal nerve stimulator therapy: a sleep center
osa related to vagal nerve stimulator therapy: a sleep center
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
13OSA RELATED TO VAGAL NERVE STIMULATOR THERAPY: A SLEEP CENTERCASE STUDY By Carolyn C. Campo, MA, RPSGT, RRTEvery so often, even the most seasoned <strong>sleep</strong> technician/technologistwill be presented with a patient who has a novel medicalhis<strong>to</strong>ry that can influence the outcome of his or her <strong>sleep</strong> study. Thisarticle provides background information on the <strong>vagal</strong> <strong>nerve</strong> and theVagal Nerve Stimula<strong>to</strong>r (VNS) device and presents a case study ofa patient with obstructive <strong>sleep</strong> apnea (OSA) <strong>related</strong> <strong>to</strong> the VNSimplant that was being used <strong>to</strong> treat her seizures.Figure 1. Vagal Nerve StimulaTOr(VNS). Copyright © 2010 Cyberonics.Image reprinted with permission.THE VAGAL (VAGUS) NERVEThe <strong>vagal</strong> <strong>nerve</strong> is just one of the 12 major cranial <strong>nerve</strong>scharged with innervation or stimulation of the viscera (gut) andskeletal muscle. It’s also called the pneumogastric <strong>nerve</strong> sinceit innervates both the lungs and the s<strong>to</strong>mach. The <strong>vagal</strong> <strong>nerve</strong>supplies mo<strong>to</strong>r parasympatheticfibers <strong>to</strong>most of the organsfrom the neck down<strong>to</strong> the second segmen<strong>to</strong>f the transversecolon. Thisincludes the heart.It’s somewhat important<strong>to</strong> rememberthat parasympathetic<strong>nerve</strong>s maintaincontrol of heart ratewhen the sympathetic<strong>nerve</strong>s (“fight orflight”) get the heartracing. Sympatheticand parasympatheticfunctions are consideredau<strong>to</strong>matic. As an interesting aside, the <strong>vagal</strong> <strong>nerve</strong> alsohas some afferent (sensory) fibers that innervate the inner (canal)portion of the outer ear. This is probably why you can feel atickling in the throat when you use a swab in the ear canal.The vagus also controls quite a few skeletal muscles - mos<strong>to</strong>f which are in the neck area, including muscles of the larynx(via recurrent laryngeal <strong>nerve</strong>) for speech production. Skeletalmuscle is often associated with voluntary movement; in thisscenario, we will associate voluntary movement with speech. Atfirst glance, speech seems au<strong>to</strong>matic; but we all had <strong>to</strong> learn <strong>to</strong>manipulate these muscles as children in order <strong>to</strong> learn <strong>to</strong> producespecific sound combinations <strong>to</strong> communicate.Carolyn C. Campo, MA,RPSGT, RRTCarolyn C. Campo, MA, RPSGT, RRT, hasbeen in the <strong>sleep</strong> field since 2000 and isDirec<strong>to</strong>r of Sleep Operations (multi-state)for Novant Healthcare based in Charlotte,N.C.To recap: The <strong>vagal</strong> <strong>nerve</strong> controls heart rate, gastrointestinalperistalsis, sweating, and quite a few muscle movements in themouth. It also keeps the larynx open for breathing.VAGAL OR VAGUS NERVE STIMULATION DEVICEThe VNS system has been around as a treatment since 1997and is very similar in appearance and function <strong>to</strong> a cardiacpacemaker in which short, regular bursts of electrical energy aresent <strong>to</strong> the brain via the vagus <strong>nerve</strong>. It is 50-55 mm in diameterand around 12-14 mm thick, making it about the size of a silverdollar. See Figure 1.INDICatioNSThe VNS is currently approved for use in adults and childrenover the age of 12 who have partial-onset seizures, which areseizures that begin in one part of the brain. Partial seizures arethe most common type of seizure experienced by people withepilepsy. Virtually any movement, sensory or emotional symp<strong>to</strong>mcan occur as part of a partial seizure, including complex visualor audi<strong>to</strong>ry hallucinations. The VNS system is intended for aperson whose seizures do not respond <strong>to</strong> medications and whoeither is not a good candidate for brain surgery or doesn’t want<strong>to</strong> have brain surgery. In 2005 it was approved for treating drugresistantcases of clinical depressionFigure 2. Vagal Nerve StimulaTOr (VNS) Implantation.Copyright © 2010 Cyberonics. Image reprinted withpermission.IMPLANTATIONWith few exceptions, VNS units are implanted on the patient’sleft side. The procedure requires two incisions: One in theneck in order <strong>to</strong> access the <strong>vagal</strong> <strong>nerve</strong> as it courses between thecarotid artery and the internal jugular vein, and another one inthe groove between the chest and the shoulder where the devicepulse genera<strong>to</strong>r (battery unit) is secured. See Figure 2. Continued on Page 14A 2Zzz 19.4 | December 2010
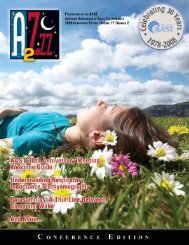
14Continued from Page 13The implantation procedure typically takes about 1.5 hours andis performed under general anesthesia. VNS is typically performedas an outpatient procedure, so patients are observed fortwo <strong>to</strong> three hours post-op and then discharged.The device is activated at low settings in the operating room atthe time of implantation and, if necessary, the doc<strong>to</strong>r will adjusthow much stimulation is being delivered, and how often. 1Exactly how VNS <strong>therapy</strong> works continues <strong>to</strong> be studied. Ifthe individual with the system feels a seizure coming on, he orshe can activate the discharge by passing a small magnet over thebattery, thus giving the patient an element of control. In somepeople, this has the effect of s<strong>to</strong>pping the seizure before it getsstarted or becomes deeply entrenched. It is also possible <strong>to</strong> turnthe device off by holding the magnet over it. This is importantlater in the case study.Although complete seizure control is seldom achieved, the majorityof people who use VNS <strong>therapy</strong> experience fewer seizures.Studies find that many people who have had the implant saythey feel better, even if their seizures continue. Many patientsreport that after a seizure they are in a better mood, feel morealert, have better memory and make fewer emergency room visitswhile using VNS <strong>therapy</strong>. 2 These mood effects explain why VNS<strong>therapy</strong> also is a treatment option for clinical depression.Most routine procedures, such as diagnostic ultrasounds orX-rays, should not affect the VNS. Anyone with a VNS implantshould tell health professionals about the implant and where it’slocated. The VNS manufacturer, Cyberonics, has a clinical/technicalsupport telephone number for health professionals <strong>to</strong> callif they have any questions about treating someone with a VNS:800-332-1375 ext. 7330.VNS THERAPY & SLEEP DISORDERED BREATHINGSide effects of VNS <strong>therapy</strong> are mostly hoarseness and occasionaldiscomfort in the throat. There may be a change in voicequality during the actual stimulation. Most notably, intermittentdecrease in respira<strong>to</strong>ry flow during <strong>sleep</strong> has consistently beendemonstrated in patients with VNS implants. 3 Clinically significant<strong>sleep</strong> disordered breathing associated with VNS <strong>therapy</strong> hasbeen described in pediatric and adult patient populations. 4,5Most patients undergoing VNS treatment experience an increasedapnea-hypopnea index (AHI) post treatment with up <strong>to</strong>approximately one third developing mild OSA post treatment. 5A small group of patients develop severe OSA <strong>related</strong> <strong>to</strong> VNS<strong>therapy</strong>. These obstructive events can be alleviated by decreasingthe frequency or intensity of VNS stimulation, by utilizingpositional <strong>therapy</strong> (<strong>sleep</strong> in non-supine position) or by applyingpositive airway pressure (PAP). 4,5VNS patients who have an increased probability for <strong>sleep</strong> disorderedbreathing will likely exhibit the usual signs and symp<strong>to</strong>ms;i.e., loud snoring or intermittent cessation of breathing at night withdaytime symp<strong>to</strong>ms such as behavioral changes, fatigue or <strong>sleep</strong>iness.Many of these patients are children who may have associated cognitivedeficits, which makes diagnosing the problem even more difficultwithout a <strong>sleep</strong> study. Thus a <strong>sleep</strong> study is required <strong>to</strong> diagnose thepresence of OSA, particularly in this population.CASE STUDYA 29-year-old female who is mentally disabled presents <strong>to</strong> the<strong>sleep</strong> <strong>center</strong> with mild snoring and a limited documented medicalhis<strong>to</strong>ry. She is obese with a body mass index (BMI) of 33.2,and she has a VNS implant for the treatment of lifelong generalizedseizures.PSG TECHNICAL FINDINGSThe patient’s respirations indicated moderate <strong>sleep</strong> disorderedbreathing with an overall AHI of 21 events per hour in all <strong>sleep</strong>positions and <strong>sleep</strong> stages. The rapid eye movement (REM)index was in the moderate category at 24. There were 128 apneasand hypopneas. Mean SaO2 during the study was 95 percentwith a nadir of 84 percent. Snoring was mild and was subjectivelyrated at three on a scale from one <strong>to</strong> 10.The patient’s EKG showed normal sinus rhythm with a heartrate range from 68 <strong>to</strong> 96 beats per minute. Periodic leg movementswith or without arousal and the spontaneous arousal indexwere all insignificant.Sleep efficiency was good at 92 percent; REM <strong>sleep</strong> and slowwave <strong>sleep</strong> constituted 21 percent and 7 percent of the <strong>to</strong>tal <strong>sleep</strong>time, respectively. REM latency was 90 minutes, and the firstREM period lasted 22 minutes.The tech who ran the study sent a note <strong>to</strong> the interpretingphysician about his suspicions regarding the timing of the apneas,which occurred approximately every four minutes. He didnot understand the role of the VNS but believed that the timingof the events coincided with the stimulation of the device.PHYSICIAN’S IMPRESSIONThere is evidence of moderate OSA with an AHI of 21 eventsper hour and desaturations as low as 84 percent. Recommendreturning for a titration study for treatment with positive airwaypressure. Elevation of head of bed, positional <strong>therapy</strong>, weightloss, ENT evaluation and elimination of sedatives and hypnotics,if applicable, are other potential treatment options. There is noevidence of significant periodic limb movement disorder. EKGis NSR. Sleep efficiency is normal.FolloW-UP TESTINGThe patient returns <strong>to</strong> the <strong>sleep</strong> <strong>center</strong> for PAP titration. Onthe night of the study the same tech consults with the physician,who requests:● Titration first <strong>to</strong> eliminate SDB● Period of testing on PAP with VNS on vs. off● Period of testing with both VNS off and PAP offPAP TECHNICAL FINDINGS:See Figure 3. The patient’s respirations without nasal CPAPand VNS turned off showed insignificant <strong>sleep</strong> disorderedbreathing with an AHI of 3.9 in all <strong>sleep</strong> stages. With CPAPapplication and the VNS turned on, the respirations were stabilizedwith an optimal nasal CPAP pressure of 7 cm H2O. At thispressure, the AHI was reduced from 24 <strong>to</strong> 3.7.Mean SaO2 at the optimal nasal CPAP pressure was 96 percentwith a nadir of 88 percent. Sleep efficiency was 88 percent.REM <strong>sleep</strong> and slow wave <strong>sleep</strong> constituted 17 percent and threepercent of <strong>to</strong>tal <strong>sleep</strong> time, respectively. REM latency was 101minutes, and the first REM period lasted 33 minutes.Since this patient required the VNS for seizure control, shewas placed on CPAP of 7 cm H2O. With education and desensitization,this patient has done very well with PAP <strong>therapy</strong>.A 2Zzz 19.4 | December 2010
– Titration first <strong>to</strong> eliminate SDB– Period of Testing with VNS On vs. Off on PAP– VNS Off and PAP Off15VNS On/PAP On ↑ VNS Off ↑VNS ON ↑ VNS Off/PAP OffFigure 3. PAP technical findings.PAP TECHNICAL FINDINGS:CONCLUSIONThe patient's respirations WITHOUT nasal 3. CPAP Malow AND BA, Edwards VNS TURNED J, Marzec M, OFF Sagher showed O, Fromes G.Patients undergoing INSIGNIFICANT VNS placement are at <strong>sleep</strong> risk for disordered developing breathing Effects with of an vagus AHI <strong>nerve</strong> of 3.9 stimulation in all <strong>sleep</strong> on respiration stages. With duringOSA <strong>related</strong> <strong>to</strong> the VNS CPAP and application should therefore and be the screened V NS clinicallyfor the presence optimal of OSA after nasal the CPAP procedure. pressure There is of some 7cm H2O. At this pressure, the apnea/hypopnea index wasTURNED ON, <strong>sleep</strong>: the a pilot respirations study. Neurology. were stabilized 2000 Nov 28;55(10):1450-4.with an4. Hsieh T, Chen M, McAfee A, Kifle Y. Sleep-<strong>related</strong>evidence that screening reduced for <strong>sleep</strong> <strong>to</strong> disordered 3.7/hr. The breathing previous in patients study, with the breathing VNS TURNED disorder in children ON showed with <strong>vagal</strong> <strong>nerve</strong> stimula<strong>to</strong>rs.with a seizure disorder MODERATE who are undergoing <strong>sleep</strong> a VNS disordered implant breathing may with Pediatr an AHI Neurol. of 2008 24/hr. Feb;38(2):99-103.be important because adequate treatment of previously undiagnosedand untreated SDB may likely result in better seizure 5. Marzec M, Edwards J, Sagher O, Fromes G, Malowcontrol. 6 CPAP <strong>therapy</strong> The is mean a viable SaO2 therapeutic at the option optimal for patients nasal CPAP pressure was 96 % with a nadir of 88 %. TheBA. Effects of vagus <strong>nerve</strong> stimulation on <strong>sleep</strong>who develop OSA <strong>related</strong> Sleep <strong>to</strong> Efficiency the VNS, and was other 88 options %. REM include <strong>sleep</strong> and Slow <strong>related</strong> Wave breathing <strong>sleep</strong> in epilepsy constituted patients. 17 Epilepsia. % and 3 2003 % ofincreasing the cycle length the Total or stimulation Sleep Time, frequency respectively. of the device.With an increase period in the lasted number 33 of minutes. patients undergoing theThe REM Jul;44(7):930-5. Latency was 101 minutes and the first REMprocedure, as well as multiple indications for use, awareness of 6. Vaughn BV, D’Cruz OF, Beach R, Messenheimer JA.this causation is important for appropriate diagnosis and treatmen<strong>to</strong>f OSA <strong>related</strong> <strong>to</strong> <strong>vagal</strong> <strong>nerve</strong> stimula<strong>to</strong>rs.obstructive placed <strong>sleep</strong> on CPAP apnoea. of Seizure. 7 cmH20. 1996 Mar;5(1):73-8. WithImprovement of epileptic seizure control with treatment ofSince this patient required the VNS for seizure control, she waseducation and desensitization, this patient has done very well with PAP <strong>therapy</strong>.REFERENCESEdi<strong>to</strong>r’s Note: Ms. Campo presented the lecture, “Vagal NerveNext is a ten-minute epoch of yet another young patient (13 y/o male w/ treatment resistant epilepsy, mildStimula<strong>to</strong>r: A Sleep Center Case Study,” June 6, 2010, during the1. Cerebral St. Louis Palsy, Children’s autism, Hospital s/p [Internet]. T&A) with Vagal VNS. <strong>nerve</strong> In this instance, Topics for the the technician Advanced Practitioner is reporting course “periodic at the AAST limb 32ndmovements” stimulation. c2010 (again [cited in purple) 2010 Aug that 08]. are, Available in fact, from: artifact from Annual the Meeting VNSin showing San An<strong>to</strong>nio, up Texas. in the leg channels as 60http://www.stlouischildrens.org/content/medservices/Hz.VagalNerveStimulation.htm.2. Epilepsy Foundation [Internet]. Vagal <strong>nerve</strong> stimulation<strong>therapy</strong>. c2010 [cited 2010 Aug 08]. Available from:http://www.epilepsyfoundation.org/answerplace/Medical/treatment/VNS/.A 2Zzz 19.4 | December 2010