PEPSI COLA Communication Pro Forma - East Midlands Cancer ...
PEPSI COLA Communication Pro Forma - East Midlands Cancer ...
PEPSI COLA Communication Pro Forma - East Midlands Cancer ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
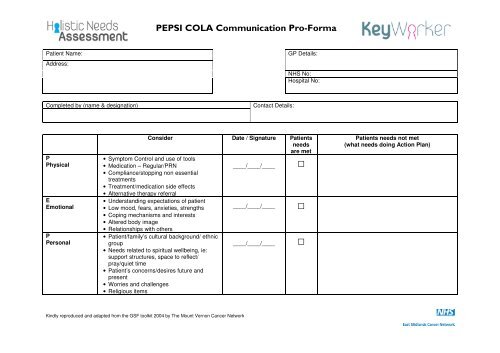
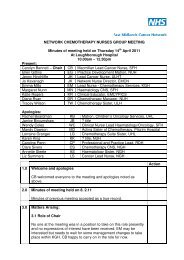
<strong>PEPSI</strong> <strong>COLA</strong> <strong>Communication</strong> <strong>Pro</strong>-<strong>Forma</strong>Patient Name:Address:GP Details:NHS No:Hospital No:Completed by (name & designation)Contact Details:PPhysicalEEmotionalPPersonalConsider Date / Signature Patientsneedsare met• Symptom Control and use of tools• Medication – Regular/PRN____/____/____ □• Compliance/stopping non essentialtreatments• Treatment/medication side effects• Alternative therapy referral• Understanding expectations of patient• Low mood, fears, anxieties, strengths ____/____/____ □• Coping mechanisms and interests• Altered body image• Relationships with others• Patient/family’s cultural background/ ethnicgroup____/____/____ □• Needs related to spiritual wellbeing, ie:support structures, space to reflect/pray/quiet time• Patient’s concerns/desires future andpresent• Worries and challenges• Religious itemsPatients needs not met(what needs doing Action Plan)Kindly reproduced and adapted from the GSF toolkit 2004 by The Mount Vernon <strong>Cancer</strong> Network
<strong>PEPSI</strong> <strong>COLA</strong> <strong>Communication</strong> <strong>Pro</strong>-<strong>Forma</strong>SSocialSupportConsider Date / Signature Patientsneedsare met• Care for carers• Practical/family support____/____/____ □• Occupational/financial welfare supportservices• Social & recreational activitiesPatients needs not met(what needs doing Action Plan)IInformation<strong>Communication</strong>• Identify the key team as per EMCN MDTpolicy• Liaison with MDT/PHCT or the receivinghealth care worker• Appropriate patient information leaflets____/____/____□CControlOOut of Hours• Discussion around patient choice• Patient dignity• Treatment options/plans discussed• Preferred place of care documented• Advanced care planning• <strong>Communication</strong> to out of hours service(OOH)• Access to drugs/equipment• Ensure continuity of care____/____/________/____/____□□LLiving withyour illness• Follow up care• Rehabilitation support• Patient/carer expectations• End of life care planning (if appropriate)• Liverpool Care Pathway• GSF register____/____/____□AAfter Care• Future support - family/patient• Discharge planning• Reassessment• Bereavement follow up____/____/____□Kindly reproduced and adapted from the GSF toolkit 2004 by The Mount Vernon <strong>Cancer</strong> Network