Hypertensive disorders of pregnancy - Australian Prescriber
Hypertensive disorders of pregnancy - Australian Prescriber
Hypertensive disorders of pregnancy - Australian Prescriber
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
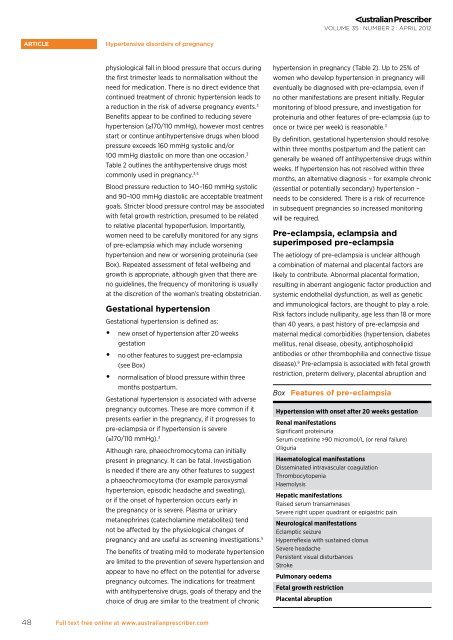
VOLUME 35 : NUMBER 2 : APRIL 2012article<strong>Hypertensive</strong> <strong>disorders</strong> <strong>of</strong> <strong>pregnancy</strong>physiological fall in blood pressure that occurs duringthe first trimester leads to normalisation without theneed for medication. There is no direct evidence thatcontinued treatment <strong>of</strong> chronic hypertension leads toa reduction in the risk <strong>of</strong> adverse <strong>pregnancy</strong> events. 3Benefits appear to be confined to reducing severehypertension (≥170/110 mmHg), however most centresstart or continue antihypertensive drugs when bloodpressure exceeds 160 mmHg systolic and/or100 mmHg diastolic on more than one occasion. 3Table 2 outlines the antihypertensive drugs mostcommonly used in <strong>pregnancy</strong>. 3,4Blood pressure reduction to 140–160 mmHg systolicand 90–100 mmHg diastolic are acceptable treatmentgoals. Stricter blood pressure control may be associatedwith fetal growth restriction, presumed to be relatedto relative placental hypoperfusion. Importantly,women need to be carefully monitored for any signs<strong>of</strong> pre-eclampsia which may include worseninghypertension and new or worsening proteinuria (seeBox). Repeated assessment <strong>of</strong> fetal wellbeing andgrowth is appropriate, although given that there areno guidelines, the frequency <strong>of</strong> monitoring is usuallyat the discretion <strong>of</strong> the woman’s treating obstetrician.Gestational hypertensionGestational hypertension is defined as:••new onset <strong>of</strong> hypertension after 20 weeksgestation••no other features to suggest pre-eclampsia(see Box)••normalisation <strong>of</strong> blood pressure within threemonths postpartum.Gestational hypertension is associated with adverse<strong>pregnancy</strong> outcomes. These are more common if itpresents earlier in the <strong>pregnancy</strong>, if it progresses topre-eclampsia or if hypertension is severe(≥170/110 mmHg). 3Although rare, phaeochromocytoma can initiallypresent in <strong>pregnancy</strong>. It can be fatal. Investigationis needed if there are any other features to suggesta phaeochromocytoma (for example paroxysmalhypertension, episodic headache and sweating),or if the onset <strong>of</strong> hypertension occurs early inthe <strong>pregnancy</strong> or is severe. Plasma or urinarymetanephrines (catecholamine metabolites) tendnot be affected by the physiological changes <strong>of</strong><strong>pregnancy</strong> and are useful as screening investigations. 5The benefits <strong>of</strong> treating mild to moderate hypertensionare limited to the prevention <strong>of</strong> severe hypertension andappear to have no effect on the potential for adverse<strong>pregnancy</strong> outcomes. The indications for treatmentwith antihypertensive drugs, goals <strong>of</strong> therapy and thechoice <strong>of</strong> drug are similar to the treatment <strong>of</strong> chronichypertension in <strong>pregnancy</strong> (Table 2). Up to 25% <strong>of</strong>women who develop hypertension in <strong>pregnancy</strong> willeventually be diagnosed with pre-eclampsia, even ifno other manifestations are present initially. Regularmonitoring <strong>of</strong> blood pressure, and investigation forproteinuria and other features <strong>of</strong> pre-eclampsia (up toonce or twice per week) is reasonable. 3By definition, gestational hypertension should resolvewithin three months postpartum and the patient cangenerally be weaned <strong>of</strong>f antihypertensive drugs withinweeks. If hypertension has not resolved within threemonths, an alternative diagnosis – for example chronic(essential or potentially secondary) hypertension –needs to be considered. There is a risk <strong>of</strong> recurrencein subsequent pregnancies so increased monitoringwill be required.Pre-eclampsia, eclampsia andsuperimposed pre-eclampsiaThe aetiology <strong>of</strong> pre-eclampsia is unclear althougha combination <strong>of</strong> maternal and placental factors arelikely to contribute. Abnormal placental formation,resulting in aberrant angiogenic factor production andsystemic endothelial dysfunction, as well as geneticand immunological factors, are thought to play a role.Risk factors include nulliparity, age less than 18 or morethan 40 years, a past history <strong>of</strong> pre-eclampsia andmaternal medical comorbidities (hypertension, diabetesmellitus, renal disease, obesity, antiphospholipidantibodies or other thrombophilia and connective tissuedisease). 6 Pre-eclampsia is associated with fetal growthrestriction, preterm delivery, placental abruption andBox Features <strong>of</strong> pre-eclampsiaHypertension with onset after 20 weeks gestationRenal manifestationsSignificant proteinuriaSerum creatinine >90 micromol/L (or renal failure)OliguriaHaematological manifestationsDisseminated intravascular coagulationThrombocytopeniaHaemolysisHepatic manifestationsRaised serum transaminasesSevere right upper quadrant or epigastric painNeurological manifestationsEclamptic seizureHyperreflexia with sustained clonusSevere headachePersistent visual disturbancesStrokePulmonary oedemaFetal growth restrictionPlacental abruption48Full text free online at www.australianprescriber.com