Clinical Review Packet
Clinical Review Packet
Clinical Review Packet
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
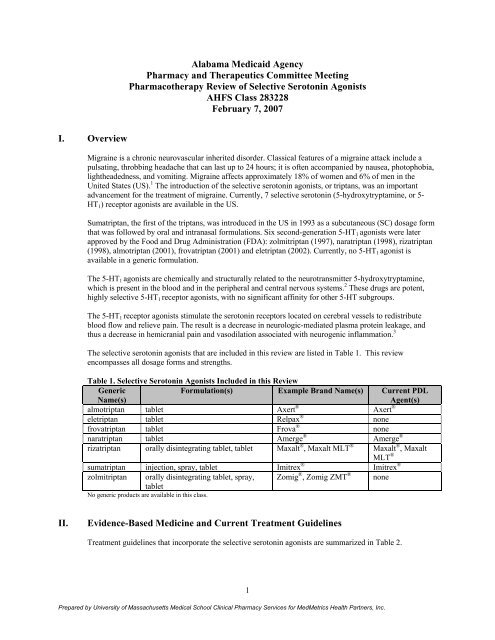
<strong>Clinical</strong> GuidelineEuropean Federation ofNeurological Societies (EFNS)Guideline on the DrugTreatment of Migraine—Reportof an EFNS Task Force 9Recommendation(s)*• Select a nonoral route of administration for patientswhose migraines present early with nausea or vomiting asa significant component of the symptom complex.• Consider self-administered rescue medication (e.g., anopioid that a patient can use at home when othertreatments have failed) for patients with severe migrainethat do not respond well to other treatments.Acute migraine attack:• First line agents (with level A 2 recommendation) for mildor moderate migraine attacks include: acetylsalicylicacid, ibuprofen, naproxen, diclofenac, paracetamol(acetaminophen), acetylsalicylic acid plus paracetamolplus caffeine.• The 5-HT 1 receptor agonists receive level A 2recommendations. 5-HT 1 receptor agonists are specificmigraine medications and should not be administered inother headache disorders except cluster headache.*Level A and Level A 1 recommendation from multiple well-designed randomized clinical trials, directly relevant to therecommendations, yielded a consistent pattern of findings. Level A 2 rating (established as useful/predictive or not useful/predictive)requires at least one convincing class I study or at least two consistent, convincing class II studies or class III studies. Level A 3recommendations are based on established scientific evidence with the highest level of proof. These include randomized, comparative,controlled trials with high statistical power and without major bias; and/or meta-analyses of randomized, comparative controlled trials;or combinations of well-conducted studies.III.IndicationsFood and Drug Administration (FDA)-approved indications for the selective serotonin agonists are noted inTable 3.Table 3. FDA-Approved Indications for the Selective Serotonin Agonists 10-17Drug(s)Migraine, Acute, with or Cluster Headachewithout AuraAlmotriptanaEletriptanaFrovatriptanaNaratriptanaRizatriptanaSumatriptan (intranasal, oral)aSumatriptan (subcutaneous) a aZolmitriptanaIV.PharmacokineticsThere are differences in the pharmacokinetic parameters of the selective serotonin agonists. Since thedevelopment of sumatriptan, alternative agents have been designed. In general, these new drugs, alsoknown as second generation selective serotonin agonists, have higher bioavailability, and a longer plasmahalf-life. Sumatriptan, rizatriptan, and zolmitriptan have the most rapid onset of action. A longer half-lifeand increased brain penetration may prevent headache recurrences. 18 The pharmacokinetic parameters forthe selective serotonin agonists are summarized in Table 4.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.3
Drug(s)Eletriptan,frovatriptan,naratriptan,rizatriptan,sumatriptan,zolmitriptanNaratriptan,rizatriptan,sumatriptan,zolmitriptanRizatriptan,sumatriptan,zolmitriptanSignificance InteractionLevel1 Ergot alkaloids(dihydroergotamine,ergotamine)MechanismThe risk of vasospastic reactions may beincreased. Possibly additive vasospasticeffects. Use of 5-HT 1 agonists within 24hours of treatment with an ergot-containingmedication is contraindicated.1 Sibutramine A “serotonin syndrome,” including CNSirritability, motor weakness, shivering,myoclonus, and altered consciousness mayoccur. The serotonergic effects of theseagents may be additive. Monitor the patientfor adverse effects if concurrent use cannotbe avoided.1 Monoamine oxidaseinhibitors (MAOIs)(isocarboxazid,phenelzine,tranylcypromine)Inhibition of metabolism via MAO,subtype-A. Use of certain 5-HT 1 agonistsconcomitantly with or within 2 weeksfollowing the discontinuation of an MAOIis contraindicated. If it is necessary to usesuch agents together, naratriptan appears tobe less likely to interact with MAOIs.Rizatriptan 2 Propranolol Rizatriptan plasma concentrations may beelevated, increasing the pharmacologic andadverse effects. Inhibition of rizatriptanmetabolism (MAO, subtype-A) bypropranolol is suspected.Significance Level 1=major severitySignificance Level 2=moderate severityPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.5
VI.Adverse Drug EventsThe most common adverse drug events reported with the selective serotonin agonists are noted in Table 6.Table 6. Adverse Drug Events (%) Reported with the Selective Serotonin Agonists 21Adverse Event(s) Almotriptan Eletriptan Frovatriptan Naratriptan Rizatriptan Sumatriptan Sumatriptan Sumatriptan ZolmitriptanInjection Nasal Spray Oral TabletsCardiovascularAngina -
Adverse Event(s) Almotriptan Eletriptan Frovatriptan Naratriptan Rizatriptan Sumatriptan Sumatriptan Sumatriptan ZolmitriptanInjection Nasal Spray Oral TabletsPulmonary- - - - -
Adverse Event(s) Almotriptan Eletriptan Frovatriptan Naratriptan Rizatriptan Sumatriptan Sumatriptan Sumatriptan ZolmitriptanInjection Nasal Spray Oral TabletsHearing loss - - - - - - - 1 -Heaviness - - - - - 7 - - -Hot/cold sensation - - 3 - - - - - -Hyperacusis - -
Adverse Event(s) Almotriptan Eletriptan Frovatriptan Naratriptan Rizatriptan Sumatriptan Sumatriptan Sumatriptan ZolmitriptanInjection Nasal Spray Oral TabletsCheilitis - -
Adverse Event(s) Almotriptan Eletriptan Frovatriptan Naratriptan Rizatriptan Sumatriptan Sumatriptan Sumatriptan ZolmitriptanInjection Nasal Spray Oral TabletsGastroesophageal - -
Adverse Event(s) Almotriptan Eletriptan Frovatriptan Naratriptan Rizatriptan Sumatriptan Sumatriptan Sumatriptan ZolmitriptanInjection Nasal Spray Oral TabletsMusculoskeletalAbnormal gait - -
Adverse Event(s) Almotriptan Eletriptan Frovatriptan Naratriptan Rizatriptan Sumatriptan Sumatriptan Sumatriptan ZolmitriptanInjection Nasal Spray Oral TabletsPharyngitis - >1
Adverse Event(s) Almotriptan Eletriptan Frovatriptan Naratriptan Rizatriptan Sumatriptan Sumatriptan Sumatriptan ZolmitriptanInjection Nasal Spray Oral TabletsNeck/throat/jaw - - - - - 2-5 - 2-3 4-10pain/tightness/pressureNeurological/- - - -
VII.Dosing and AdministrationThe usual dosing regimens for the selective serotonin agonists are summarized in Table 7.Table 7. Usual Dosing for the Selective Serotonin Agonists 10-17Drug(s)AlmotriptanEletriptanFrovatriptanNaratriptanRizatriptanSumatriptanUsual Adult DoseMigraine, with or without aura:Oral: initial, 6.25-12.5 mg, may repeatafter 2 hours; maximum 2 doses per 24hoursMigraine, acute treatment:Oral: initial, 20-40 mg, may repeat after2 hours if headache returns; maximumsingle dose, 40 mg; maximum dailydose, 80 mgMigraine:Oral: initial, 2.5 mg, may repeat after 2hours; maximum, 7.5 mg per 24 hoursMigraine, with or without aura, acutetreatment:Oral: initial, 1-2.5 mg, may repeat onceafter 4 hours; maximum, 5 mg per 24hoursMigraine, with or without aura: acutetreatment:Oral: 5 to 10 mg, may repeat after 2hours; maximum, 30 mg per 24 hoursMigraine:Oral: initial, 25-100 mg, repeat after 2hours if needed; maximum 200 mg per24 hoursSubcutaneous: initial, 6 mg, repeat in 1hour if needed; maximum 6 mg perdose and 12 mg per 24 hours; lowerdoses may be used if side effects aredose limitingNasal spray: initial, 5-20 mg, ifheadache returns may repeat dose onceafter 2 hours; maximum, 40 mg per 24hoursUsual PediatricDoseSafety and efficacyin children havenot beenestablished.Safety and efficacyin children havenot beenestablished.Safety and efficacyin children havenot beenestablished.Safety and efficacyin children havenot beenestablished.Safety and efficacyin children havenot beenestablished.Safety and efficacyin children havenot beenestablished.AvailabilityOral tablet:6.25 mg, 12.5 mgOral tablet:20 mg, 40 mgOral tablet:2.5 mgOral tablet:1 mg, 2.5 mgOral tablet:5 mg, 10 mgOral tablet,disintegrating:5 mg, 10 mgNasal spray:5 mg, 20 mgOral tablet:25 mg, 50 mg, 100mgSubcutaneousinjection:4 mg/0.5 mL, 6mg/0.5 mLCluster headache:Subcutaneous: initial, 6 mg, repeat in 1hour if needed; maximum 6 mg perdose and 12 mg per 24 hours; lowerdoses may be used if side effects aredose limitingPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.14
Drug(s)ZolmitriptanUsual Adult DoseMigraine, with or without aura, acutetreatment:Oral: initial, 2.5 mg (or lower), mayrepeat after 2 hours; maximum 10 mgper 24 hoursUsual PediatricDoseSafety and efficacyin children havenot beenestablished.AvailabilityNasal spray:5 mgOral tablet:2.5 mg, 5 mgIntranasal: initial, 5 mg into one nostril,may repeat after 2 hours; maximum 10mg per 24 hoursOral tablet,disintegrating:2.5 mg, 5 mg15Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
VIII. Effectiveness<strong>Clinical</strong> studies evaluating the safety and efficacy of the selective serotonin receptor agonists are summarized in Table 8.Table 8. Comparative <strong>Clinical</strong> Trials Using the Selective Serotonin AgonistsStudy andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationMigraine With or Without AuraCabarrocas et al. 22 OL N=747Almotriptan 12.5 mg1 yearEnd PointsPrimary:Headache responserates at 1 and 2 hoursResultsPrimary:Headache response rates at 1 and 2 hours were 43% and 73%,respectively (P value not reported).Diener et al. 23Almotriptan 12.5 mgvs.placeboAll patients were poorresponders tosumatriptan 50 mg.Pascual et al. 24Almotriptan 6.25 mgvs.almotriptan 12.5 mgRCT, PC, DB, MCEligible patients were adultsaged 18 to 65 years who hadsuffered from migraine withor without aura for at least 1year, and had experiencedunsatisfactory responses tosumatriptan on at least twooccasionsOL, DBPatients 18-65 years oldwith at least 1 year historyof migraine, with or withoutaura, all patientsexperienced 1-6 migraineattacks per month with atleast 24 hours of freedombetween attacksN=3281 attackN=7621 yearSecondary:Safety and efficacyPrimary:Relief from headacheat 2 hours after dosingSecondary:Pain-free efficacy at 2hours, and use ofrescue medicationwithin 24 hoursPrimary:The primary measureof tolerability was theincidence oftreatmentemergentadverseevents (includingabnormalities inclinical laboratorytests,electrocardiogramSecondary:The most common adverse effects were back pain, bronchitis, andflu-like symptoms (P value not reported).Primary:In the almotriptan group, 47.5% of patients achieved pain relief at2 hours after dosing which was significantly higher percentagethan in the placebo group, 23.2% (P
Study andDrug RegimenDowson et al. 25Almotriptan 12.5 mgx 1 dosevs.almotriptan 25 mgx 1 dosevs.sumatriptan 100 mgx 1 dosevs.placebox 1 doseAll study medicationswere administeredduring a migraineattack. A second dosewas allowed ifheadache relapsed in 2-Study DesignandDemographicsRCT, DB, PC, PG, MC, SDPatients 18-65 years oldwith migraine with orwithout aura for >1 yearSample Size andStudy DurationN=668Single doseEnd Points[ECG], vital signs orphysical examination)Secondary:Percent of attacksresolved (to mild orno pain) by 2 hoursafter dose (attacks ofmoderate/severebaseline intensityonly)Primary:Relief from migrainepain at 2 hours afterdosingSecondary:Relief from migrainepain at 1 hour, painfreestatus at 1 and 2hours, migrainerecurrence within 24hours postdose, needfor escape medicationResultsthose which occurred in at least 1% of patients were vomiting(2.1%), somnolence (1.7%), dizziness (1.6%), fatigue (1.4%) andnausea (1.4%) (P values not reported).Secondary:Pain relief at 2 hours after the initial dose was achieved in 84.2%of moderate/severe attacks. Patients were pain free at 2 hours afterdose in 58.2% of all attacks (P values not reported).Primary:Pain relief was higher in the treatment groups vs. placebo asfollows: almotriptan 12.5 mg=56.8% (achieved pain relief),almotriptan 25 mg=56.5%, sumatriptan 100 mg=63.7%,placebo=42.2% (P values not reported).Both doses of almotriptan were equivalent to sumatriptan 100 mgwith the 90% CI interval inside the range of the equivalenceregion.Secondary:Relief from migraine pain at 1 hour was not statistically differentfor all three treatment arms.Migraine recurrence within 24 hours postdose for patients withmoderate pain at baseline was reported as follows: almotriptan12.5 mg=22.7%, almotriptan 25 mg=14.9%, sumatriptan 100mg=22.4%, placebo=16.7% (P values not reported).Migraine recurrence within 24 hours postdose for patients withsevere pain at baseline was reported as follows: almotriptan 12.5mg=8.8%, almotriptan 25 mg=16.2%, sumatriptan 100mg=28.9%, placebo=27.3% (P values not reported).The use of escape medication was reported as follows: almotriptan12.5 mg=38.6%, almotriptan 25 mg=38.2%, sumatriptan 10017Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Study andDrug Regimen24 hours after firstdose. Escapemedication wasallowed if painpersisted beyond 2hours.Dahlof et al. 26Almotriptan 2 mgsingle dose given atonset of moderate orsevere migraine attackvs.almotriptan 6.25 mgsingle dose given atonset of moderate orsevere migraine attackvs.almotriptan 12.5 mgsingle dose given atonset of moderate orsevere migraine attackStudy DesignandDemographicsRCT, PC, DB, MC, PGPatients 18-65 years oldwith migraine with orwithout aura for >1 year,migraines occurring one-sixtimes per monthSample Size andStudy DurationN=742Single doseEnd PointsPrimary:Change in headachepain intensity at 2hours without rescuemedicationSecondary:Freedom from pain,relief from migraineassociatedsymptomsResultsmg=32.4%, placebo=55.5% (P values not reported).Primary:Almotriptan demonstrated a dose-dependent increase in thenumber of patients with improvement in headache pain intensity(58.5% and 66.5% improvement for the 12.5 and 25 mg doses,respectively, compared to 32.5% for placebo; P
Study andDrug Regimengiven at onset ofmoderate or severemigraine attackStudy DesignandDemographicsSample Size andStudy DurationEnd PointsResultsAnother dose of studydrug was allowed ifpain severity increasedwithin 2-24 hours.Escape medication wasallowed if pain did notdecrease after 2 hours.Dahlof et al. 27Almotriptan 2.0 mgvs.almotriptan 5.0 mgvs.almotriptan 6.25 mgvs.almotriptan 12.5 mgvs.almotriptan 25 mgvs.almotriptan 100 mgMeta-analysis of 4 R, PC,DB, dose comparisonstudiesMale and female patientsbetween 18 and 65 years ofage who had at leasta 6-month history ofmigraine, and experienced 1to 6 migraine attacks permonthN=2294First attackPrimary:Efficacy, speed ofonset and tolerabilityof almotriptan in theacute treatment ofmigrainePercentage(proportion) ofpatients achievingsustained pain free(SPF) with no adverseevents (SNAE): thepercentage of patientswho achieved SPF anddid not report anyadverse events (AEs)Drug vs. placebocomparisons weremade. No drug vs.drug comparisonswere made.Primary:As early as 30 minutes after dosing, almotriptan 12.5 mg wassignificantly more effective than placebo for pain relief (14.9% vs.8.2%; P
Study andDrug Regimenalmotriptan 150 mgStudy DesignandDemographicsSample Size andStudy DurationEnd PointsResultsvs.placeboColman et al. 28Almotriptan 12.5 mgvs.sumatriptan 50 mgRCT, DBPatients aged 18-71 yearswho had not been treatedpreviously with a triptan,suffering with migrainewith or without aura for >6monthsN= 1,17348 hoursPrimary:Change in treatmentsatisfaction measure,functional statusmeasure, andMigraine Quality ofLife Questionnaire(MqoLQ) values frombaseline to 48 hoursSecondary:Not reportedPrimary:There were no significant differences between the 2 treatmentgroups in terms of satisfaction with pain relief (mean score 50.85for almotriptan and 52.10 for sumatriptan; P=0.67).Functional status was not significantly different. Both groupsimproved by ~44 points on the 100-point functional status scaleafter 24 hours. Patients from both groups reported improvement infunctional status after treatment, from marginally functional atonset of migraine (mean scores for almotriptan and sumatriptan,42.54 and 42.50 respectively) to ~90% of normal (mean scores86.49 and 86.99, respectively) at 24 hours.Similarly, no difference was found between the 2 treatment groupsin a comparison of MqoLQ at 24 hours after treatment.Patients in the almotriptan group were significantly more satisfiedand experienced fewer side effects than patients receivingsumatriptan (P=0.016).Spierings et al. 29Almotriptan 12.5 mgvs.sumatriptan 50 mgR, DB, PG, MCMen and women between18 and 65 years whosuffered from migraine withor without auraN=1,25524 hoursPrimary:Headache relief frommoderate or severe tomild or no headacheand pain-free status at2 hoursSecondary:Migraine relief andfreedom fromSecondary:Not reportedPrimary:Headache relief at 2 hours was observed in 58% of patients in thealmotriptan group and 57.3% of patients in the sumatriptan groupwith no significant difference between the groups. Pain-freeresponse rate at 2 hours was observed in 17.9% of patients in thealmotriptan group and 24.6% of patients in the sumatriptan group(P=0.005) in favor of sumatriptan.Secondary:There was no significant difference between the groups with20Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Study andDrug RegimenOlesen et al. 30Eletriptan 80 mgvs.placeboR, DB, PCStudy DesignandDemographicsMale and female patientsaged 18 years and olderwith migraine with auraevery 4 weeksSample Size andStudy DurationN=12324 hoursEnd Pointsheadache pain at 0.5and 1 hours afterintake of studymedication,improvement ofmigraine associatedsymptoms, incidenceof migraine recurrenceat 24 hours afterdosing, and the use ofrescue medicationPrimary:Proportion of subjectsnot developing amigraine headache ofmoderate or severeintensity within 6hours of dosing with adouble-blind studydrugSecondary:Time to headachedevelopment, durationof aura symptoms, useof second dose,response to the seconddose, use of rescuemedication, treatmentacceptability, and timeto rescue medicationResultsregards to relief from migraine-associated symptoms of nausea,vomiting, photophobia, and phonophobia.Rescue medications were taken by 36.7% of almotriptan patientsand 33.2% of sumatriptan patients (P value not reported).Of the 343 responders in the almotriptan group, 27.4%experienced a migraine recurrence within 24 hours, compared to24.0% of the 333 responders in the sumatriptan group. Thedifferences were not statistically significant (P value not reported).Primary:Treatment with eletriptan during the aura phase was not effectivein preventing the onset of moderate-to-severe headache post-aura.There was no significant difference in the proportions of patientsdeveloping a headache on eletriptan (61%) compared with placebo(46%) (P value not reported).Secondary:Eletriptan did not increase the duration of the aura phasecompared with placebo (0.7 hour vs. 0.8 hour), nor was itassociated with a significant delay in the median time to headacheonset (1.3 hour vs. 1.0 hour) (P value not reported).A second dose of eletriptan 40 mg was permitted for patients inboth the eletriptan and placebo treatment groups who developed amoderate-to-severe headache. Response rates to the 40-mg dose ofeletriptan were similar in both (initial) treatment groups (P valuenot reported).Additional rescue medication was taken by 28% of patientsinitially randomized to eletriptan 80 mg, and by 17% of patientsinitially randomized to placebo (P value not reported).The percentage of patients rating study medication as acceptablewas comparable for both eletriptan and placebo (76% vs. 72%; Pvalue not reported).21Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Study andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationEnd PointsResultsFarkkila et al. 31Eletriptan 40 mgvs.eletriptan 80 mgvs.placeboR, DB, OG, PC, MCMale and female subjectsage ≥18 years withInternational HeadacheSociety (NAÏVE) diagnosticcriteria for migraine, withor without auraN=4463 migraine attacksPrimary:2-hour headacheresponse ratesSecondary:Onset of action, 2-hour pain-freeresponse rates,incidence of nausea,vomiting andheadache recurrence,consistency ofresponseThere was no significant difference between groups on anyefficacy measure.Primary:2-hour headache response, based on first-dose, first-attack data,was 59% for eletriptan 40 mg, 70% for eletriptan 80 mg, and 30%for placebo (P
Study andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationEnd Pointspoints; functionalstatus; headacherecurrence and timeto-headacherecurrence;use ofrescue medication andtime-to-use; sustainedheadache; sustainedpain-free response;global evaluation ofmedication;acceptability of studymedicationResultsEletriptan showed higher pain-free rates at both 2 and 4 hours(35% and 56%, respectively) compared with both naratriptan(18%; P
Study andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationEnd PointsResults(60% vs. 52%; P=0.014) and placebo (44%; P
Study andDrug RegimenDiener et al. 34Eletriptan 40 mgvseletriptan 80 mgvs.ergotamine tartrate2mg, caffeine 200 mg(Cafergot ® )vs.placeboSteiner et al. 35Eletriptan 40 mgvs.eletriptan 80 mgvs.zolmitriptan 2.5 mgvs.placeboStudy DesignandDemographicsMC, DB, R, PC, PGMale or female patientsaged 18–65 years, whoexperienced migrainewith or without aura for atleast 1 year; frequency ofmigraine attacks had to beat least 1 every 6 weeks butnot more than 6 per monthR, DB, PC, PGMale or female patientsaged 18-65 years withmigraine with or withoutauraSample Size andStudy DurationN=73324 hoursN=1,312Single migraineattackEnd PointsPrimary:Headache response(improvementfrom severe ormoderate to mild orno pain) at 2 hoursSecondary:Headache response at1 hour, pain-free ratesat 1 and 2 hours,functional hourimpairment,functional response,and presence ofmigraine-associatedsymptoms or absenceof nausea, vomiting,photophobia andphonophobiaPrimary:Headache responsewithin 2 hours oftaking the first dose ofstudy medicationSecondary :Headache-responserates at 0.5, 1 and 1.5hours, pain-free ratesat 0.5, 1, 1.5 and 2hours, absence ofassociated symptomsat 0.5, 1, 1.5 and 2hours, functionalrecovery at 1 and 2hours, headache-ResultsPrimary:Significantly more eletriptan-treated patients (80 mg, 68%;40 mg, 54%) than Cafergot ® -treated patients (33%; P< 0.001)reported headache response (improvement from moderate-tosevereto mild or no pain) at 2 hours.Substantially more eletriptan recipients reported no pain (80 mg,38%; 40 mg, 28%; Cafergot ® , 10%; placebo, 5%; P
Study andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationEnd Pointsrecurrence rate, use ofrescue medication,sustained headacheresponse, sustainedpain-free, patient'sglobal evaluation ofstudy medicationat 24 hours on a 7-point Likert scale,acceptability of studymedication5%; P
Study andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationEnd PointsResultszolmitriptan; P
vs.Study andDrug Regimeneletriptan 80 mgvs.sumatriptan 100 mgvs.placeboMandema et al. 37Eletriptan 20 mgvs.eletriptan 40 mgvs.eletriptan 80 mgvs.sumatriptan 25 mgvs.sumatriptan 50 mgvs.sumatriptan 100 mgvs.MA, PCStudy DesignandDemographicsFor inclusion in theanalysis, each trial had tomeet the following criteria:(1) randomized doubleblindplacebo controlledtrial; (2) treatment ofmoderate or severe migrainein adults within 8 hours ofonset; (3) measurement ofrelief from migraine pain ona four point categoricalscale of none, mild,moderate, severe; (4)includes efficacy results forthe first attack; (5) noremedication or rescuebefore 2 hoursSample Size andStudy DurationN≅11,400N/AEnd Pointsin headache intensityto mild or pain-freelevels from apretreatment level ofmoderate or severeSecondary:Not reportedPrimary:Proportion of patientsthat achieved migrainepain relief up to 4hours after treatmentand proportion ofpatients that becamepain freeSecondary:Not reportedResultsThere was a difference between sumatriptan 100 mg, andeletriptan 80 mg (P
Study andDrug Regimensumatriptan 200 mgvs.sumatriptan 300 mgStudy DesignandDemographicsSample Size andStudy DurationEnd PointsResultsAn absolute benefit of more than 3% of patients was maintainedfrom 1 hour up to 3 hours after treatment. No significantdifference was found between eletriptan 20 mg and sumatriptan 50mg for the fraction of patients that became pain free (P value notreported).vs.placeboNo significant effect of encapsulation of sumatriptan was found onthe time course of response up to 4 hours after treatment whencompared to commercial sumatriptan (P value not reported).Mathew et al. 38Eletriptan 40 mgvs.sumatriptan 100 mgvs.placeboSchoenen et al. 39Eletriptan 80 mgvs.sumatriptan 6 mg SCR, DB, PG, PCMen and women, aged 18 to65 years, who met the IHS(NAÏVE) criteria formigraine with or withoutauraR, OL, XOMale and female patients18–65 years of age that metthe IHS criteria for migrainewith or without aura, andsuffered at least one acuteattack every 6 weeksN=211324 hoursN=3113 migraine attacksPrimary:The primaryendpoint was 2-hourheadache responseSecondary:Headache responserates at 1 hour, painfreerates, absence ofassociated symptoms,functional response at1 and 2 hours, andsustained headacheresponsePrimary:Patient preference foreletriptan versussumatriptan SCSecondary:Change frompretreatment baselinein headache intensity;change frompretreatment baselineSecondary:Not reportedPrimary:Headache response rates at 2 hours postdose were significantlyhigher for eletriptan 40 mg (67%) than for sumatriptan 100 mg(59%; P
Study andDrug RegimenSandrini et al. 40Eletriptan 40 mgvs.eletriptan 80 mgvs.sumatriptan 50 mgvs.Study DesignandDemographicsMC, DB, DD, PC, PG RCTMen and women >18 yearsof age who were expectedto have at least one attack ofmigraine with or withoutaura, every 6 weeksSample Size andStudy DurationN=10083 attack studyEnd Pointsin a 5-point patientratedGlobalImpression ofEfficacy scale; thepresence or absence ofnausea, vomiting,photophobia andphonophobia; changein functionalimpairment scale;headache recurrence(and time to headacherecurrence), between 2and 24 hours afteringestion of studymedication; time touse of rescuemedication; sustainedrelief; acceptability ofstudy medicationPrimary:Early headacheresponse (at 1 hour)was the primaryendpoint, 2-hourheadache responseSecondary:Headache responserates, functionalimprovement, patientacceptabilityResultseach study medication, except for faster headache response andpain-free rates in favor of sumatriptan SC, and a significantlylower recurrence rate on eletriptan (25% vs. 40%; P
Study andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationEnd PointsResultssumatriptan dose. Eletriptan 40 mg was more efficacious thanboth sumatriptan doses in functional improvement (P1 year with 2 to 8migraines in the previous 2monthsN=2,67624 hours (up to 3migraine attacks)N=1652 migraine attacksPrimary:Headache response at2 hoursSecondary:Time to headacherecurrence, incidenceof patients with 24-hour headacherecurrencePrimary:The incidence of nomigraine headache 2hours post doseSecondary:Comparison of earlyvs. later use offrovatriptanThe higher efficacy of both eletriptan doses was associated withhigher rates of patient acceptability than sumatriptan 50 mg(P
Study andDrug RegimenNaratriptan 2.5 mgvs.sumatriptan 50 mgvs.placeboKlassen et al 44Naratriptan 0.1 mgvs.naratriptan 0.25 mgvs.naratriptan 1 mgvs.naratriptan 2.5 mgvs.placeboStudy DesignandDemographicsSelf-described poorsumatriptan responders, hadhistory of migraine >1 yearR, DB, PC, PGMen and women 18 to 65years of age with at least a1-year history of migrainewith or without auraSample Size andStudy DurationEnd Points2 migraine attacks moderate or severepain to mild or no painat 4 hours after the useof the double-blindtest medication for thetreatment of attack 2N=613Single migraineattackSecondary:Headache relief at 2hours and completepain relief at 4 hours,which include relief ofother components ofmigraine syndromePrimary:Percentage of patientswho experiencedheadache relief(moderate or severepain at dosing reducedto mild or no pain) 4hours after the firstdose of studymedicationSecondary:Examined at eachmeasured time pointthrough 4 hourspostdose, included theproportions of patientswith headacherelief, proportions ofpatients withmeaningful relief,proportions withheadache relief 8, 12,Resultsplacebo for the relief of headache pain (defined as mild or nopain) at 4 hours (P0.05).Primary:Headache relief 4 hours postdose was reported in 60% of patientsreceiving naratriptan 2.5 mg compared with 50%, 35%, 32%, and34% of patients receiving naratriptan 1 mg, 0.25 mg, 0.1 mg, andplacebo, respectively (P
Study andDrug RegimenGobel et al. 45Naratriptan 2.5 mgvs.sumatriptan 100 mgR, DB, COStudy DesignandDemographicsMen and women 18-65years old with >1 yearhistory of migraine with orwithout aura, randomlyassigned to treat 1 moderateor severe migraine attack ina nonclinical setting withone naratriptan 2.5 tabletand 1 attack with 1sumatriptan 100 mg tabletSample Size andStudy DurationN=25324 hoursEnd Pointsand 24 hourspostdose, theproportion takingrescue medicationwithin 24 hours ofinitial dosing, and theproportionexperiencing headacherecurrence within 24hours of initial dosingPrimary:Percent of patientswith headacherecurrence, percent ofpatients with 24-hourmaintenance ofheadache reliefSecondary:Percentage of patientsexperiencing headacherelief, the percent ofpatients using rescuemedication during the24 hours after dosing,and the percentage ofpatients that took asecond dose of studydrugResultsPrimary:Headache recurrence for naratriptan was 45% and recurrence withsumatriptan was 57% (no significant statistical difference).After 2 attacks, headache recurrence for naratriptan was 41% andfor sumatriptan was 57%. The odds ratio for not experiencingrecurrence after treatment with naratriptan relative to sumatriptanwas 1.97 (P=0.005; 95%CI, 1.24-3.15).Twenty-four hour maintenance of headache relief was reported by39% of patients given naratriptan and 34% of patients treated withsumatriptan (OR=1.26; 95%CI, 0.86-1.85; NS).Secondary:Percentage of patients experiencing headache relief was 76% forpatients treated with naratriptan 2.5 mg, and 84% in patients whoreceived sumatriptan 100 mg (not significantly different).The percent of patients who received rescue medications forinadequate relief up to 24 hours after dosing did not differsignificantly between naratriptan-treated patients (21%) andsumatriptan-treated patients (16%) (OR=1.47; 95% CI, 0.94-2.30).The percent of patients that took a second dose of study drug diddiffer significantly. Forty percent of patients treated withnaratriptan used a second dose of study medication after initialtreatment, compared with 57% for sumatriptan33Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Study andDrug RegimenAshcroft et al. 46Naratriptan 2.5 mgvs.naratriptan 1 mgvs.rizatriptan 10 mgvs.sumatriptan 100 mgvs.MAStudy DesignandDemographicsPatients suffering frommoderate or severe migraineattacksSample Size andStudy DurationN= 449Single migraineattackEnd PointsPrimary:Response rate ratiosfor headache relief,pain-free response andsustained relief (4-24hours)Secondary:Adverse events wereestimated with the rateratio (RR), riskdifference and numberneeded to harmResults(P
Study andDrug RegimenFerrari et al. 48Rizatriptan 5 mgvs.rizatriptan 10 mgvs.placeboStudy DesignandDemographicsMA of R, DBOutpatients who had at leasta 6-month history ofmigraineSample Size andStudy DurationN=4,816Single migraineattackEnd Pointsprovided a sustainedpain-free responselasting between 2 and24 hours afteradministrationPrimary:Pain relief, associatedmigraine symptomsand functionaldisability (allmeasured immediatelybefore dosing and at0.5, 1, 1.5 and 2hours), headacherecurrenceSecondary:Not reportedResultsPrimary:At 2 hours, rizatriptan 10 mg was significantly more effective thanplacebo for pain relief (71% vs. 38%, P
Study andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationEnd Points=2770ResultsPain-free response (moderate to severe pain reduced to none) attwo hours was noted as follows:Rizatriptan 5 mg: RB 3.4 (2.6 to 4.4); NNT 4.7 (4.0 to 5.7);n=1646Rizatriptan 10 mg: RB 4.8 (3.8 to 5.9); NNT 3.1 (2.9 to 3.4);n=2770Sustained relief over 24 hours (headache response at 2 hours,sustained for 24 hours with no rescue medication and no seconddose of study medication) was noted as follows:Rizatriptan 5 mg: RB 1.5 (1.3 to 1.8); NNT 8.3 (6.0 to 14);n=1450Rizatriptan 10 mg: RB 1.7 (1.5 to 2.0); NNT 5.6 (4.5 to 7.4);n=1677Kolodny et al. 50Rizatriptan 5 mgvs.rizatriptan 10 mgvs.sumatriptan 25 mgvs.sumatriptan 50 mgR, DB, PC, CO, two-attackstudyMen and women in goodhealth aged >18 years withat least 6-month history ofmigraine with or withoutauraN=1,4475 daysPrimary:Time to pain reliefduring the 2 hoursafter taking study drugSecondary:2-hour pain reliefstatus and thepresence of associatedsymptoms at 2 hoursSecondary:Not reportedPrimary:The primary efficacy variable, expressed as the hazard ratio ofrizatriptan 10 mg vs. sumatriptan 50 mg, was 1.10 (95% CI 0.96,1.26; P=0.161).Rizatriptan 5 mg was statistically (P=0.007) more efficacious thansumatriptan 25 mg; the hazard ratio of rizatriptan 5 mg vs.sumatriptan 25 mg was 1.22 (95% CI 1.06, 1.41).Secondary:Rizatriptan 10 mg-treated patients had significantly less nausea(P=0.004) compared with those treated with sumatriptan 50 mg.For all other secondary measures at 2-hours, rizatriptan 10 mg wasnot statistically different than sumatriptan 50 mg.vs.36Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Study andDrug RegimenplaceboLainez et al. 51Rizatriptan 10 mgvs.eletriptan 40 mgStudy DesignandDemographicsMC, OL, XOPatients aged 18–65 yearswith a history of at least 6months of migraine, with orwithout auraSample Size andStudy DurationN=372Single migraineattackEnd PointsPrimary:Patient preference wasanalyzed for allpatients who treatedboth attacks and whoexpressed apreference for onemedication over theotherResultsPrimary:Significantly more (P
Study andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationEnd PointsResultsMore patients taking rizatriptan had a 24-hour sustained pain-freeresponse than did patients taking other triptans.The statistical significance is noted below.Rizatriptan 10 mg vs. sumatriptan 100 mg (P=0.112)Rizatriptan 10 mg vs. sumatriptan 50 mg (P=0.015)Rizatriptan 10 mg vs. sumatriptan 25 mg (P=0.005)Rizatriptan 10 mg vs. naratriptan 2.5 mg (P=0.004)Rizatriptan 10 mg vs. zolmitriptan 2.5 mg (P=0.013)Bomhof et al. 53Rizatriptan 10 mgvs.naratriptan 2.5 mgvs.placeboR, MC, double-masked,DD, PCPatients aged 18-65 yearswho met IHS criteria formigraine with or withoutaura, a 6-month history ofmigraine and usuallyexperienced 1-8 attacks permonthN=552Single migraineattackPrimary:Time to headacherelief within 2 hoursSecondary:Headache relief andpain free up to 2hours, associatedsymptoms, functionaldisability, satisfactionwith medication at 2hours, need foradditional medicationfrom 2 to 24 hours,24-hour quality of life,safetySecondary:Incidence of drug-related adverse events were as follows:Rizatriptan 10 mg vs. sumatriptan 100 mg=33% vs. 41%(P=0.014)Rizatriptan 10 mg vs. sumatriptan 50 mg=37% vs. 35% (P=0.671)Rizatriptan 10 mg vs. sumatriptan 25 mg=37% vs. 31% (P=0.043)Rizatriptan 10 mg vs. naratriptan 2.5 mg=27% vs. 19% (P=0.079)Rizatriptan 10 mg vs. zolmitriptan 2.5 mg=25% vs. 28%(P=0.410).Primary:Rizatriptan 10 mg was more effective than naratriptan 2.5 mg onthe primary efficacy measure of time to headache relief within 2hours. HR=1.62 (95% CI, 1.26-2.09, P
Study andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationEnd PointsResultsPatients on rizatriptan were more satisfied with their medicationthan those on naratriptan at 2 hour means scores 3.55 vs. 4.21,P
vs.Study andDrug Regimenzolmitriptan 2.5 mgvs.Study DesignandDemographicsSample Size andStudy DurationEnd PointsResultsRates of treatment-emergent nausea at 2 hours ranged from 11%to 18% with placebo, from 5% to 13% with rizatriptan 10 mg, andfrom 10% to 20% with other comparator triptans.Secondary:Not reportedplaceboCady et al. 55Sumatriptan 6 mg SCvs.placeboR, PCAdult patients with historyof migraine with or withoutauraN=1,104Primary:1-hour headacheresponse rateSecondary:Complete relief ofheadache, clinicaldisability, andreduction in othermigraine symptomsPrimary:Sumatriptan 6 mg SC produced a response (defined as mild painor no pain) rate of 70%, compared with 22% for placebo(P
Study andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationEnd PointsResultsOral SumatriptanInternational Multi-Dose Study Group 57Sumatriptan 100 mgPOvs.placeboOne tablet at onset ofheadache, one tablet 2hours later if migraine,and one tablet if theheadache came backwithin 24 hoursCutler et al. 58Sumatriptan 25 mg POvs.sumatriptan 50 mg POvs.PC, DB, PGAdult patients with historyof migraine with or withoutauraR, DB, PG, PCAdult patients with historyof migraine with or withoutauraN=233 Primary:Headache relief at 2and 4 hoursN=259Single attackstudySecondary:Pain free at 2 hours,improvement inheadache severity at 1hour postdose, numberof patients needingtwo or three dosesPrimary:Headache relief by 2hoursSecondary:Headache relief by 4hoursSecondary:Not reportedPrimary:Sumatriptan was significantly more effective than placebo at 2hours (50% versus 19%; P
Study andDrug RegimenSumatriptan 1 mg INvs.sumatriptan 5 mg INvs.sumatriptan 10 mg INvs.Study DesignandDemographicsAdult patients with historyof migraine with or withoutauraSample Size andStudy DurationN=210Single attackstudyhoursEnd PointsSecondary:Not reportedResults120 minutes after doses of 10-40 mg sumatriptan compared toplacebo (P
vs.Study andDrug RegimenplaceboStudy DesignandDemographicsSample Size andStudy DurationEnd Pointspostdose,worsening pain 2hours postdose,sustained pain-freeresults from 2-24hours postdoseResultsSecondary:The proportion of patients who were migraine-free at 2 hourspostdose was 42% for sumatriptan 50 mg, 47% for sumatriptan100 mg, and 20% for placebo (P
Study andDrug RegimenLoder et al. 62Sumatriptan 50 mgtabletvs.rizatriptan orallydisintegrating tablet(ODT) 10 mgStudy DesignandDemographicsMC, RCT, OL, XOPatients aged 18 years andolderSample Size andStudy DurationN=5247 daysEnd PointsPrimary:Patient preferenceSecondary:Head pain severity,functional disability,headache recurrenceResultsPrimary:No preference for either therapy was reported in 10 of 386 patients(2.6%). Of the remaining 374 patients 57% preferred rizatriptanODT 10 mg and 43% preferred sumatriptan 50 mg tablet(P=0.009).Secondary:A significant greater percentage of patients reported pain reliefafter taking ODT than sumatriptan at 45 and 60 minutes post dose(38% vs. 29% and 58% vs. 49%, respectively; P
Study andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationEnd PointsResults50 mg (n=420), and 25 mg (n=226), respectively.Adverse events were more common with sumatriptan 100 mg thanwith placebo (risk difference [RD]=0.14 [0.09 to 0.20]; numberneeded-to-harm[NNH]=7.1 [5.0 to 11.1]; n=3172). RDs for the50- and 25-mg vs. placebo comparisons were not statisticallysignificant.Cady et al. 64Sumatriptan 25 mgPOvs.sumatriptan 50 mg POvs.sumatriptan 100 mg POvs.ergotamine 2 mg pluscaffeine 200 mgvs.aspirin 900 mg plusmetoclopramide 10 mgvs.placeboMA, DB, PCPatients with >1 headachewhich was treated earlywhen pain was mildN=92118 headachesSingle attackPrimary:Pain-free response 2and 4 hours afterdosingSecondary:Use of a second doseof medication, clinicaldisability migraineassociatedsymptoms,meaningful pain relief(patient-defined), timeto meaningful relief,sustained pain-freeresponse, andproportion of attacksin which pain hadworsened 2 and 4hours after dosing, allof which werecompared inheadaches treatedduring mild versusmoderate/severe painSecondary:Not reportedPrimary:Pain-free response was higher 2 hours after dosing withsumatriptan 50 mg (51%) or 100 mg (67%; P
Study andDrug RegimenGeraud et al. 65Zolmitriptan 5 mgvs.sumatriptan 100 mgvs.placeboUse of escapemedication waspermitted 2 hourspostdose if symptomspersisted.Study DesignandDemographicsR, MC, DB, PCTreatment naïve migrainepatients 18-65 years oldwith established diagnosisof migraine with or withoutaura for >1 yearSample Size andStudy DurationN=1,05824 hoursEnd PointsPrimary:Complete headacheresponse rates in acutetreatment (defined as areduction in headachepain frommoderate/severe atbaseline to mild or nopain 2 hours aftertaking study drug withno moderate or severerecurrences at 24hoursSecondary:Compare headacheresponses at 1, 2 and 4hours postdoseResultsplus metoclopramide 73% vs. 25%, respectively).Primary:Complete headache response (2-24 hours) was 39% forzolmitriptan, 38% for sumatriptan and 32% for placebo (nostatistical difference).In patients with moderate headache, response was greater withzolmitriptan (48%) than placebo (27%) (P=0.01).In patients with moderate headache there was no significantdifference in complete response with zolmitriptan (48%) vs.sumatriptan (40%).In patients with moderate headache, response was not statisticallydifferent with zolmitriptan (48%) vs. sumatriptan (40%).For patients with severe baseline headache, there was nosignificant difference in complete response rates between placebo(44%) and either active treatment (27% for zolmitriptan and 35%sumatriptan).Diener et al. 66Zolmitriptan 2.5 mgorally disintegratingtablet (ODT)One dose was used totreat migraineheadache; if headacherecurred, a second dosewas allowed after aninterval of at least 2OSPatients aged 9-95 yearswith migrainesN=14,5432 yearsPrimary:Efficacy evaluationSecondary:Not reportedSecondary:Active treatment groups were significantly more effective thanplacebo for 1-, 2-, and 4-hour headache response; (P
Study andDrug Regimenhours from the initialdoseSpierings et al. 67Zolmitriptan 5 mgorally disintegratingtablet (ODT)vs.placeboOne dose was used totreat migraineheadache; if there wasinadequate relief or ifthe headache returned,a second dose wasallowed 2-24 hourslaterStudy DesignandDemographicsRCT, DB, MC, PG, PCPatients aged 18-65 yearswith at least 2 migraineheadaches per month ofmoderate to severe intensityin addition to less than 10days of non-migraineheadaches per month for the3 months prior toenrollmentSample Size andStudy DurationN=6566 weeksEnd PointsPrimary:Migraine headacheresponse at 30 minutesSecondary:Speed of onset ofheadache response,duration of responseResultsPrimary:The percentages of zolmitriptan and placebo patients with reducedmigraine headache intensity (decreased from “moderate” or“severe” to “mild” or “no pain,” as assessed at 30 minutes) were16.5% (102/620 headaches) and 12.5% (81/647), respectively(P=0.048).Secondary:At the 1-hour interval, the difference in the percentages ofzolmitriptan and placebo patients with reduced migraine headacheintensity (from “moderate” or “severe” to “mild” or “no pain”)was statistically significant, with 41.1% (253/615) in thezolmitriptan group and 22.9%(147/642) in the placebo group(P
Study andDrug Regimenorally disintegratingtablet (ODT) (study C)vs.placeboStudy DesignandDemographicsSample Size andStudy DurationEnd PointsSecondary:Headache response at30 minutes (study A)Reduction ofheadache intensity(studies A and B)Pain-free rate at 2hours (studies A andC)(P
vs.Study andDrug Regimensumatriptan 50 mgtabletStudy DesignandDemographicsSample Size andStudy DurationODT)12 weeks (vs.sumatriptan)End PointsResultspatients that preferred the zolmitriptan ODT compared tosumatriptan (60.1% vs. 39.9%; P=0.013). Patients also foundzolmitriptan ODT to be more efficacious compared to sumatriptan(76.7% vs. 63.4%; P=0.006).orrizatriptan 10 mg ODTorPatient preference for zolmitriptan ODT was greater than that ofrizatriptan ODT (70% vs. 27%; P
Study andDrug RegimenDowson et al. 71Zolmitriptan 5.0 mg INStudy DesignandDemographicsDB, PG, RCT, XOPatients 18-65 years withmigraine with or withoutaura, previous participationin a dose-ranging study, 1-year history of migrainesymptoms, with an age ofonset of migraine
Study andDrug Regimeneletriptan 80 mgvs.frovatriptan 2.5 mgvs.naratriptan 2.5 mgStudy DesignandDemographicsSample Size andStudy DurationEnd PointsResultsrizatriptan 5 mg: 62.4 (60.2-64.5).5-HT 1 agonists with lower efficacy to sumatriptan 100 mgsumatriptan 25 mg: 56.0 (53.1-58.9)naratriptan 2.5 mg: 48.6 (45.7-51.4)eletriptan 20 mg: 48.9 (44.5-53.3)frovatriptan 2.5 mg: 41.5 (39.3-43.8).Pain-free results at 2 hours (mean % [95% CI]) for sumatriptan100 mg are 28.9 (27.2-30.5).vs.rizatriptan 5 mgvs.rizatriptan 10 mgvs.5-HT 1 agonists with higher rates than sumatriptan 100 mg are:almotriptan 12.5 mg: 61.2 (NA)eletriptan 80 mg: 33.0 (30.5-35.4)rizatriptan 10 mg: 40.1 (38.3-42.0).5-HT 1 agonists with lower rates than sumatriptan 100 mg are:sumatriptan 25 mg: 23.4 (21.0-25.9)naratriptan 2.5 mg: 22.4 (20.0-24.7)eletriptan 20 mg: 16.4 (13.2-19.7).sumatriptan 25 mgAll other triptans did not differ from sumatriptan 100 mg.vs.sumatriptan 50 mgvs.zolmitriptan 2.5 mgSustained pain-free results (mean % [95% CI]) for sumatriptan100 mg are 20.0 (18.2-21.3).5-HT 1 agonists with higher rates than sumatriptan 100 mg are:almotriptan 12.5 mg: 25.9 (22.7-29.1)rizatriptan 10 mg: 25.3 (23.7-26.9)eletriptan 80 mg: 25.0 (22.8-27.2).vs.zolmitriptan 5 mg5-HT 1 agonists with lower rates than sumatriptan 100 mg are:eletriptan 20 mg: 10.6 (7.7-13.5)sumatriptan 25 mg: 16.7 (14.5-18.9)naratriptan 2.5 mg: 15.9 (13.4-18.5).vs.No differences were found with other triptan doses.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.51
Study andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationEnd PointsResultssumatriptan 100 mgvs.Secondary:Adverse effects – placebo subtracted adverse effects (mean [95%CI]) for sumatriptan 100 mg: 13.2 (8.6-17.8).placebo5-HT 1 agonists with lower rates than sumatriptan 100 mg are:almotriptan 12.5 mg: 1.8 (-2.5-6.2)naratriptan 2.5 mg: 2.4 (-2.2-7.0)CNS Adverse effects-placebo subtracted adverse effects (mean[95% CI]) for sumatriptan 100 mg: 6.3 (3.2-9.5).5-HT 1 agonist with higher CNS adverse effect rates thansumatriptan 100 mg was:eletriptan 80 mg: 14.6 (10.2-19.0)Rates for all other triptans and doses largely overlap.5-HT 1 agonist with lower CNS adverse effect rates thansumatriptan 100 mg was:almotriptan 12.5 mg: -1.5 (-3.9-1.0).Menstrual MigraineAllais et al. 73Almotriptan 12.5 mgvs.zolmitriptan 2.5 mgRetrospective analysis ofMC, R, DB, PCPatients with 12-monthhistory of migraine and 2-6migraine attacks in each ofthe two moths preceding thetrialN=25524 hoursPrimary:Pain relief (fromsevere or moderate tomild or no pain) at0.5, 1, 1.5, and 2hours; pain free at 0.5,1,1.5 and 2 hours;sustained pain free 2hours with norecurrence and norescue medicationover 24 hours);recurrence within 24hours of treatment;Rates for all other triptans and doses largely overlap.Primary:In the intent-to-treat group, almotriptan did not differ significantlyfrom zolmitriptan for any of the variables tested.Two hours after dosing, 67.9% of the 136 women who tookalmotriptan and 68.6% of the women who took zolmitriptan(P=0.900) had obtained pain relief.Evolution of pain from “moderate/severe” to “mild/no pain” wasalso similar in both groups, 14.9% of almotriptan-treated womenvs. 11.9% of zolmitriptan-treated women had improved at 0.5hours (P=0.477).A pain-free state at 2 hours was reported by 44.9% of women on52Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Study andDrug RegimenStudy DesignandDemographicsSample Size andStudy DurationEnd Pointsand level of functionalimpairment beforeintake and after 0.5, 1,1.5, and 2 hoursSecondary:Tolerability defined asthe number of patientsreporting adverseevents within 24 hoursafter dosingResultsalmotriptan and 41.2% on zolmitriptan (P=0.554); 24 hours afterdosing 56.6% and 64.7% of patients, respectively, were pain free(P=0.187).Recurrences 2-24 hours postdose were reported in 32.8% and34.7% of patients respectively (P=0.833).Use of rescue medication 2-24 hours after dose was reported by21.8% of almotriptan and 25.4% of zolmitriptan (P=0.499).A sustained pain-free response was reported by 29.3% ofalmotriptan patients and 27.1% of zolmitriptan patients (P=0.698).Silberstein et al. 74Frovatriptan 2.5 mgdailyvs.frovatriptan 2.5 mgtwice dailyvs.PC, MC, DB, XOWomen migraneurs aged>18 years, >1-year historyof migraine, and an attackfrequency of at least 3 to 4(perimenstrual period)N= 4433 perimenstrualperiodsPrimary:Efficacy offrovatriptan inmenstrual migrainegiven for 6 days (2days before menses)in comparison withplaceboSecondary:Not reportedSecondary:Adverse effects in the 24 hours postdosing were reported in 19.8%of almotriptan group and 23.1% of zolmitritpan group; 13.2% and17.6% (P=0.328) respectively, were considered to be triptanrelated.Primary:The incidence of menstrual migraine was 67% (n=468) in theplacebo treated group compared with 52% (n=484; P
Study andDrug Regimendaily for up to 3 weeksStudy DesignandDemographicsCluster headache history 1-38 yearsSample Size andStudy DurationEnd Pointsepisodic and chroniccluster headaches forpreventative andtransitional therapyResults3 of 8 patients with chronic cluster headaches had complete relief.No adverse events reported.Gobel et al. 76Sumatriptan SC 6 mgMC, OLPatients 18-65 years of agewith a diagnosis of clusterheadache or episodic clusterheadacheN=521 yearSecondary:Not reportedPrimary:Efficacy of therapydefined by freedomfrom pain within 15minutes in more than90% of attacksSecondary:Not reportedPrimary:Therapy was successful in 88% of all attacks (P value notreported).Freedom from pain within 15 minutes in more than 90% of attackswas reported by 42% of patients (P value not reported).Ekbom et al. 77Sumatriptan 6 mg SCvs.sumatriptan 12 mg SCvs.MC, DB, PC, R, XOPatients 18-65 years with adiagnosis of clusterheadache or episodic clusterheadacheN=134Single dose studySecondary:Tolerability definedby adverse effectsreported by patientsPrimary:Headacheimprovement to mildor no pain at 5, 10 and15 minutesSecondary:Not reportedSecondary:Adverse events were reported by 62% of patients (P value notreported).Primary:At 10 minutes, headache relief was reported by 25% (placebo),49% (6 mg), and 63% (12 mg) of patients.At 15 minutes headache relief was reported by 35% (placebo),75% (6 mg), and 80% (12 mg). P
Study andDrug RegimenplaceboStudy DesignandDemographicswith an attack frequency of1-6 moderate or severemigraines per monthSample Size andStudy DurationEnd Pointsfor the acute relief ofmigraine headacheSecondary:Not reportedResultsasymptomatic and did not result in hemodynamic compromise.The incidence of arrhythmias was higher in the placebo-treatedpatients than frovatriptan group (11% vs. 3%, respectively).There were no differences in heart rate or diastolic or systolicblood pressure. The incidence of adverse events was similar inthe frovatriptan treated and placebo-treated groups.Fleishaker et al. 79Almotriptan 12.5 mgvs.almotriptan 25 mgvs.placeboR, DB, SD, 3-way, XOPatients with mild-tomoderatehypertensioncontrolled by medicationsN=20Single dosePrimary:Assess cardiovasculareffects of almotriptanin patients with mildto-moderatehypertensioncontrolled byantihypertensivemedicationSecondary:Assess relationshipbetween plasmaconcentrations andcardiovascular effectsin a population that ispossibly sensitive tothe vasoconstrictiveproperties of the 5-HT 1 agonistsSecondary:Not reportedPrimary:Almotriptan produced a dose-related change in systolic bloodpressure (SBP) for both 4 and 12 hours postdose. Mean changesfrom baseline from 0-4 hours were 1.59 + 3.88 , 1.85 + 5.94, and4.84 + 5.99 mm Hg for SBP and 1.38 + 6.95, 6.25 + 9.54, and11.0 + 10.6 mm Hg for diastolic blood pressure (DBP) forplacebo, almotriptan 12.5 mg, almotriptan 25 mg, respectively.Secondary:Plasma concentrations of almotriptan increased in a dose-relatedmanner. There were no statistically significant differences in doserelatedpharmacokinetic parameters between doses, indicating thatthe pharmacokinetics of almotriptan were linear for the dosagerange studied for patients with controlled hypertension.Drug regimen abbreviations: QD=once daily, BID=twice daily, IN=intranasal, SC=subcutaneous PO=oral, PRN=as needed,Study abbreviations: CI=confidence interval, CS=comparative study, DB=double-blind, MA=meta-analysis, MC=multicenter, OL=open-label, OR=odds ratio, PC=placebo-controlled, PG=parallel-group,PRO=prospective, R=randomized, RCT=randomized controlled trial, XO=crossover, NNT=numbers needed to treatMiscellaneous abbreviations: CAD=coronary artery disease, RB=relative benefitPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.55
Additional EvidenceDose SimplificationA search of Medline and Ovid did not reveal data pertinent to this topic.Stable TherapyA search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician VisitsA search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 9. Relative Cost of the Selective Serotonin AgonistsGeneric Name(s) Formulation(s) Example BrandName(s)BrandCostGenericCostalmotriptan tablet Axert ® $$$$ N/Aeletriptan tablet Relpax ® $$$$ N/Afrovatriptan tablet Frova ® $$$$ N/Anaratriptan tablet Amerge ® $$$$ N/Arizatriptan orally disintegrating Maxalt ® , Maxalt MLT ® $$$$ N/Atablet, tabletsumatriptan injection, spray, tablet Imitrex ® $$$$ N/Azolmitriptanorally disintegratingtablet, spray, tabletNo generic products are available in this class.N/A=not availableX. ConclusionsZomig ® , Zomig ZMT ® $$$$-$$$$$Migraine is a common disorder, with a one year prevalence rate in the US of approximately 13%. 80 Mostmigraine sufferers require pharmacologic treatment. Nonsteroidal anti-inflammatory drugs (NSAIDs) areconsidered first-line therapy by most organizations. The US Headache Consortium recommends migrainePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.56N/A
specific agents such as the selective serotonin agonists for patients with severe migraine and in patientswhose migraines respond poorly to NSAIDs or combination analgesics. 7,8 A nonoral medication isrecommended for patients whose migraine presents early with nausea or vomiting as a significantcomponent of the symptom complex. The Consortium does not give preference to one selective serotoninagonist over another.All of the selective serotonin agonists are approved for the acute treatment of migraine attacks with orwithout aura. The subcutaneous formulation of sumatriptan is also indicated for cluster headache.Rizatriptan and zolmitriptan are available as orally disintegrating tablets, which dissolve rapidly withoutwater. These products are not absorbed through the buccal mucosa so they have the same rate ofabsorption as the oral tablets. 79 Sumatriptan and zolmitriptan are available as nasal formulations.A meta-analysis of 53 clinical trials including over 24,000 patients concluded that all of the available oralselective serotonin agonists are effective and well tolerated. Almotriptan 12.5 mg, eletriptan 80 mg andrizatriptan 10 mg produced the most consistent success; however, eletriptan was not as tolerable assumatriptan 100 mg. 34 One should note that this meta-analysis was published prior to the reformulation ofsumatriptan tablets in January 2004.Numerous clinical trials have been conducted comparing the safety and efficacy of the selective serotoninagonists to each other. Many of the comparative studies suffer from methodological flaws and/orlimitations. For example, all selective serotonin agonist trials use patient-reported assessment systems todetermine efficacy. This system has significant shortcomings given that pain can be biased by age, gender,cultural and other factors. Another significant limitation is that the 2-hour and 4-hour postdose time period,which is commonly used, is arbitrary and may not be clinically meaningful. Still another significantshortcoming is that clinical trials have not been conducted based on stage and severity of migraine attacksin varying patient populations. Additional limitations include underdosing of the comparator drug, orenrollment of patients who have failed a comparator drug.Of the head-to-head studies that do demonstrate statistically significant differences in headache responserates, the statistical difference tends to be less than 10%. The clinical consequence of the statisticaldifference tends to be less than 10% and thus the clinical significance of this small difference is not known.Although clinical trials have compared the selective serotonin agonists head-to-head, there is insufficientclinical evidence to conclude that one 5-HT 1 agonist is safer or more efficacious than another whenadministered at equivalent doses. All selective serotonin agonists are safe, effective, and well tolerated, andthey have comparable side-effect profiles. While the selective serotonin agonists have differentpharmacokinetic properties, in general, these differences have not resulted in different clinical outcomes.There is insufficient clinical evidence to conclude that one selective serotonin agonist is safer or moreefficacious than another. Therefore, all brand products within the class reviewed are comparable to eachother and to the generics and over-the-counter products in this class and offer no significant clinicaladvantage over other alternatives in general use.XI.RecommendationsNo brand selective serotonin agonist is recommended for preferred status. Alabama Medicaid should acceptcost proposals from manufacturers to determine cost effective products and possibly designate one or morepreferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.57
References1. Adelman JU, Adelman RD. Current options for the prevention and treatment of migraine. Clin Ther.2001;23(6):772-788.2. Lance JW. 5-hydroxytryptamine and its role in migraine. Eur Neurol. 1991;31:279-281.3. Bateman DN. Sumatriptan. Lancet. 1993;341:221-224.4. Silberstein SD. Practice parameter: Evidence-based guidelines for migraine headache (an evidence-basedreview): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology.2000.55;754-762.5. Lewis D, Ashwal S, Hershey A et al. Practice Parameter: Pharmacological treatment of migraine headache inchildren and adolescents: report of the American Academy of Neurology Quality Standards Subcommittee andthe Practice Committee of the Child Neurology Society. Neurology. 2004. 63;2215-2224.6. Snow V, Weiss K, Wall EM, Mottur-Pilson C; American Academy of Family Physicians; American College ofPhysicians-American Society of Internal Medicine. Pharmacologic management of acute attacks of migraineand prevention of migraine headache. Ann Intern Med. 2002 Nov 19;137(10):840-9.7. Matchar DB, Young WB, Rosenberg JH, Pietrzak MP, Silberstein SD, Lipton RB, et al. Evidence-basedguidelines for migraine headache in the primary care setting; pharmacologic management of acute attacks.Available at www.aan.com/professionals/practice/guidelines.cfm. Accessed November 1, 2006.8. Ramadan NM, Silberstein SD, Freitag FG, Gilbert TT, Frishberg BM. Evidence-based guidelines for migraineheadache in the primary care setting: pharmacological management for prevention of migraine. Available atwww.aan.com/professionals/practic/guidelines.cfm. Accessed November 1, 2006.9. Evers S, Afra J, Frese A, Goadsby PJ, Linde M, May A, Sandor PS. EFNS guideline on the drug treatment ofmigraine - report of an EFNS task force. Eur J Neurol. 2006 Jun;13(6):560-572.10. Frova ® [package insert]. Chadds Ford, PA: Endo Pharmaceuticals Inc.; June 2006.11. Imitrex ® Tablets and Imitrex ® Nasal Spray [package inserts]. Research Triangle Park, NC: GlaxoSmithKline;June 2006.12. Imitrex ® Injection [package insert]. Research Triangle Park, NC: GlaxoSmithKline; November 2006.13. Amerge ® [package insert]. Research Triangle Park, NC: GlaxoSmithKline; June 2006.14. Axert ® [package insert]. Raritan, NJ: Ortho-McNeil Pharmaceutical, Inc.; June 2005.15. Maxalt ® , Maxalt-MLT ® Tablets and Orally Disintegrating Tablets [package inserts]. Whitehouse Station, NJ:Merck & Co, Inc.; June 2006.16. Relpax ® [package insert]. New York, NY: Pfizer, Inc.; April 2006.17. Zomig ® , Zomig-ZMT ® Tablets and Orally Disintegrating Tablets, Zomig ® Nasal Spray [package inserts].Wilmington, DE: AstraZeneca; 2005-2006.18. Jhee SS, Shiovtz T, Crawford AW, Cutler NR. Pharmacokinetics and pharmacodynamics of the triptanantimigraine agents: a comparative review. Clin Pharmacokinet. 2001;40(3)189-205,19. Wickersham RM, Novak KK, managing eds. Drug Facts and Comparisons. St. Louis, MO: Wolters KluwerHealth, Inc.; 2004-2006.20. Tatro DS, ed. Drug Interaction Facts. St. Louis, MO: Wolters Kluwer Health, Inc.; 2006.21. Almotriptan, eletriptan, frovatriptan, naratriptan, rizatriptan, sumatriptan, zolmitriptan: drug information. In:Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.22. Cabarrocas X, Esbri R, Peris F, Ferrer P. Long-term efficacy and safety of oral almotriptan: interim analysis ofa 1-year open study. Headache. 2001;41:57-62.23. Diener HC, Gendolla A, Gerbert I, Beneke M. Almotriptan in migraine patients who respond poorly to oralsumatriptan: a double-blind, randomized trial. Headache. 2005;45:874-882.24. Pascual J, Falk R, Docekal R, Prusinski A, Jelencsik J, Cabarrocas X, Segarra X, et al. Tolerability and efficacyof almotriptan in the long-term treatment of migraine. Eur Neurol. 2001;45:206-13.25. Dowson AJ, Massiou H, Lainez JM, Cabarrocas X. Almotriptan is an effective and well-tolerated treatment formigraine pain: results of a randomized, double-blind, placebo-controlled clinical trial. Cephalagia.2002;22(6):453-461.26. Dahlof CG, Tfelt-Hansen P, Massiou H, Fazekas A. Dose finding, placebo-controlled study of oral almotriptanin the acute treatment of migraine. Neurology. 2001;57(10):1811-1817.27. Dahlof C, Pascual J, Dodick DW, Dowson AJ. Efficacy, speed of action and tolerability of almotriptan in theacute treatment of migraine: pooled individual patient data from four randomized, double-blind, placebocontrolledclinical trials. Cephalagia. 2006;26:400-408.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.58
28. Colman SS, Brod MI, Krishnamurthy A, Rowland CR, Jirgens KJ, Gomez-Mancilla B. Treatment satisfaction,functional status, and health related quality of life of migrating patients treated with almotriptan or sumatriptan.Clin Ther. 2001;23(1):127-145.29. Spierings EL, Gomez-Mancilla B, Grosz DE, Rowland CR, Whaley FS, Jirgens KJ. Oral almotriptan vs. oralsumatriptan in the abortive treatment of migraine: a double-blind, randomized, parallel-group, optimum-dosecomparison. Arch Neurol. 2001;58(6):944-950.30. Olesen J, Diener HC, Schoenen J, Hettiarachchi J. No effect of eletriptan administration during the aura phaseof migraine. Eur J Neurol. 2004;11:671-677.31. Farkkila M, Olesen J, Daholf C, Stovner LJ, ter Bruggen JP, Rasmussen S, Muirhead N, Sikes C. Eletriptan forthe treatment of migraine in patients with previous poor response or tolerance to sumatriptan. Cephalagia.2003;23:463-471.32. Garcia-Ramos G, MacGregor EA, Hilliard B, Bordini CA, Leston J, Hettiarachchi J. Comparative efficacy ofeletriptan vs. naratriptan in the acute treatment of migraine. Cephalalgia. 2003; 23:869–876.33. Sheftell F, Ryan R, Pitman V. Efficacy, safety, and tolerability of oral eletriptan for treatment of acute migraine:a multicenter, double-blind, placebo-controlled study conducted in the United States. Headache. 2003;43:202-213.34. Diener HC, Jansen JP, Reches A, Pascual J, Pitei D, Steiner TJ. Efficacy, tolerability and safety of oraleletriptan and ergotamine plus caffeine (Cafergot ® ) in the treatment of migraine: A multicentre, randomized,double-blind, placebo-controlled comparison. Eur Neurol. 2002;47:99-107.35. Steiner TJ, Diener HC, MacGregor EA, Schoenen J, Muirhead N, Sikes CR. Comparative efficacy of eletriptanand zolmitriptan in the acute treatment of migraine. Cephalalgia. 2003; 23:942-952.36. Goadsby PJ, Ferrari MD, Olesen J, Stovner LJ, Senard JM, Jackson JC, and Poole PH. Eletriptan in acutemigraine: a double blind, placebo-controlled comparison to sumatriptan. Neurology. 2000;54(1):156-161.37. Mandema JW, Cox E, and Alderman J. Therapeutic benefit of eletriptan compared to sumatriptan for the acuterelief of migraine pain—results of a model-based meta-analysis that accounts for encapsulation.Cephalalgia.2005;25:715-725.38. Mathew NT, Schoenen J, Winner P, Muirhead N, and Sikes CR. Comparative efficacy of eletriptan 40 mgversus sumatriptan 100 mg. Headache. 2003;43:214-222.39. Schoenen J, Pascual J, Rasmussen S, Sun W, Sikes C, Hettiarachchi J. Patient preference for eletriptan 80 mgversus subcutaneous sumatriptan 6 mg: results of a crossover study in patients who have recently usedsubcutaneous sumatriptan. Eur J Neurol. 2005;25:108-117.40. Sandrini G, Farkkila M, Burgess G, Forster E, and Haughie S. Eletriptan vs. sumatriptan a double-blind,placebo-controlled, multiple migraine attack study. Neurol. 2002;59:1210–1217.41. Ryan R. Geraud G, Goldstein J, Cady R, Keywood C. <strong>Clinical</strong> efficacy of frovatriptan: placebo-controlledstudies. Headache. 2002;(42 Suppl 2):S84-92.42. Cady R, Elkind A, Goldstein J, Keywood C. Randomized, placebo-controlled comparison of early use offrovatriptan in a migraine attack versus dosing after the headache has become moderate or severe. Curr MedRes Opin. 2004;20:1465-1472.43. Stark S, Spierings EL, McNeal S, Putnam GP, Bolden-Watson CP, O'Quinn S. Naratriptan efficacy inmigraineurs who respond poorly to oral sumatriptan. Headache. 2000;40:513-520.44. Klassen A, Elkind A, Asgharnejad M, Webster C, Laurenza A. Naratriptan is effective and well tolerated in theacute treatment of migraine: results of a double-blind, placebo-controlled, parallel-group study. Headache.1997;37:640-645.45. Gobel H, Winter P, Boswell D, et al. Comparison of naratriptan and sumatriptan in recurrence-prone migrainepatients. Clin Ther. 2000;22(8):981-989.46. Ashcroft DM, Millson D. Naratriptan for the treatment of acute migraine: meta-analysis of randomisedcontrolled trials. Pharmacoepidemiol Drug Saf. 2004;13(2):73-82.47. Mathew NT, Kailasam J, Meadors L. Early treatment of migraine with rizatriptan: a placebo-controlled study.Headache. 2004;44:669-673.48. Ferrari MD, Loder E, McCarroll KA, Lines CR. Meta-analysis of rizatriptan efficacy in randomized controlledclinical trials. Cephalalgia. 2001; 21:129-136.49. Oldman, AD. Smith, LA. McQuay, HJ. Moore, RA. Rizatriptan for acute migraine. Cochrane Pain, Palliativeand Supportive Care Group Cochrane Database of Systematic <strong>Review</strong>s. 4, 2006.50. Kolodny A, Polis A, Battisti WP, Johnson-Pratt L, Skobieranda F. Comparison of rizatriptan 5 mg and 10 mgtablets and sumatriptan 25 mg and 50 mg tablets. Cephalagia. 2004;24:540-546.51. Láinez MJA, Evers S, Kinge E, Allais G, Allen C, Rao NA, Massaad R, Lis K. Preference for rizatriptan 10-mgwafer vs. eletriptan 40-mg tablet for acute treatment of migraine. Cephalalgia. 2006; 26:246–256.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.59
52. Adelman JU, Lipton RB, Ferrari MD, Diener HC, McCarrol KA, Vandormael K, Lines CR. Comparison ofrizatriptan and other triptans on stringent measures of efficacy. Neurology. 2001;57:1377-1383.53. Bomhof M, Paz J, Legg N, Allen C, Vandermael K, Patel K, and the Rizatriptan-Naratriptan Study Group.Comparison of rizatriptan 10 mg vs. naratriptan 2.5 in migraine. Euro Neurol. 1999;42:173-179.54. Lipton RB, Pascual J, Goadsby PJ, Massiou H, McCarroll KA, Vandormael K, Jiang K, Lines CR. Effect ofrizatriptan and other triptans on the nausea symptom of migraine: a post hoc analysis. Headache.2001;41(8):754-763.55. Cady RK, Wendt JK, Kirchner JR, Sargent JD, Rothrock JF, Skaggs H Jr. Treatment of acute migraine withsubcutaneous sumatriptan. JAMA. 1991;265(21):2831-2835.56. Treatment of migraine attacks with sumatriptan. The Subcutaneous Sumatriptan International Study Group.New England Journal of Medicine. 1991;325(5):316-321.57. Self-treatment of acute migraine with subcutaneous sumatriptan using an auto-injector device. SumatriptanAuto-Injector Study Group. Eur Neurol. 1991;31:323-331.58. Cutler N, Mushet GR, Davis R, Clements B, Whitcher L. Oral sumatriptan for the acute treatment of migraine:evaluation of three dosage strengths. Neurology. 1995;45(suppl 7):S5-9.59. Salonen R, Ashford E, Dahlöf C, et al. Intranasal sumatriptan for the acute treatment of migraine. J Neurol.1994;241:463-469.60. Winner P, Landy S, Richardson M, Ames M. Early intervention in migraine with sumatriptan tablets 50 mgverses 100 mg: a pooled analysis of data from six clinical trials. Clin Ther. 2005;27:1785-1794.61. Gershovich OE, Billups SJ, Delate T, et al. Assessment of clinical, service, and cost outcomes of a conversionprogram of sumatriptan to rizatriptan ODT in primary care patients with migraine headaches. J Manag CarePharm. 2006;12:246-253.62. Loder E, Brandes JL, Silberstein S, et al. Preference comparison of rizatriptan ODT 10-mg and sumatriptan 50-mg tablet in migraine. Headache 2001;41(8):745-753.63. McCrory, DC. Gray, RN. Oral sumatriptan for acute migraine. Cochrane Database of Systematic <strong>Review</strong>s. 4,2006.64. Cady RK, Sheftell F, Lipton RB, Quinn S, Jones M, Putnam G, Crisp A, Metz A, NcNeal S. Effect of earlyintervention with sumatriptan on migraine pain: Retrospective analyses of data from 3 clinical trials. Clin Ther.2000;22:1035-1048.65. Geraud G, Olsen J, Pfaffenrath V, Tfelt-Hansen P, Zupping R, Diener HC, Sweet R. Comparison of the efficacyof zolmitriptan and sumatriptan: issues in migraine trial design. Cephalagia. 2000; 20:30-38.66. Diener H, Gendolla A. Part IV: Effects of zolmitriptan orally disintegrating tablet on migraine symptoms andability to perform normal activities: a post-marketing surveillance study in Germany. Curr Med Res Opin.2005;21 Suppl 3:S18-S24.67. Spierings ELH, Rapoport AM, Dodick DW, et al. Acute treatment of migraine with zolmitriptan 5 mg orallydisintegrating tablet. CNS Drugs. 2004;18:1133-1141.68. Loder EW, Dowson AJ, Spierings ELH. Part II: <strong>Clinical</strong> efficacy and tolerability of zolmitriptan orallydisintegrating tablet in the acute treatment of migraine. Curr Med Res Opin. 2005;21 Suppl 3:S8-S12.69. Dowson AJ, Almqvist P. Part III: The convenience of, and patient preference for, zolmitriptan orallydisintegrating tablet. Curr Med Res Opin. 2005;21 Suppl 3:S13-S17.70. Charlesworth BR, Dowson AJ, Purdy A, Becker WJ, Boes-Hansen S, Farkkila M. Speed of onset and efficacyof zolmitriptan nasal spray in the acute treatment of migraine: a randomised, double-blind, placebo-controlled,dose-ranging study versus zolmitriptan tablet. CNS Drugs. 2003;17:653-667.71. Dowson AJ, Charlesworth BR, Prudy A, Becker WJ, Boes-Hansen S, Farkkila M. Tolerability and consistencyof effect of zolmitriptan nasal spray in a long-term migraine treatment trial. CNS Drugs. 2003;17:839-851.72. Ferrari MD, Goadsby PJ, Roon KI, Lipton RB. Triptans (serotonin, 5-HT1B/1D agonists) in migraine: detailedresults and methods of a meta-analysis of 53 trials. Cephalagia.2002;22:633-658.73. Allais G, Acuto G, Cabarrocas X, Esbri R, Benedetto G, Bussone G. Efficacy and tolerability of almotriptanversus zolmitriptan for the acute treatment of menstrual migraine. Neurol Sci. 2006; 27:S193-197.74. Silberstein SD, Elkind AH, Schreiber C, Keywood C. A randomized trial of frovatriptan for the intermittentprevention of menstrual migraine. Neurology. 2004;63:261-269.75. Siow HC, Pozo-Rosich P and Silberstein SD. Frovatriptan for the treatment of cluster headaches. Cephalagia.2004;24:1045-1048.76. Gobel H, Linder V, Heinze A, Ribbat M, Deushl G. Acute therapy for cluster headache with sumatriptan:Findings of a one-year long-term study. Neurology. 1998;51(3):908-911.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.60
77. Ekbom K, Monstad I, Prusinski A, Cole JA, Pilgrim AJ, Noronha D. Subcutaneous sumatriptan in the acutetreatment of cluster headache: a dose comparison study. The Sumatriptan Cluster Headache Study Group. ActaNeurol Scand. 1993;88(1):63-69.78. Elkind AH, Satin LZ, Nila A, Keywood C. Frovatriptan use in migraineurs with or at high risk of coronaryartery disease. Headache. 2004;44:403-410.79. Fleishaker JC, MeEnroe JD, Azie NE, Francom SF, Carel BJ. Cardiovascular effect of almotriptan in treatedhypertensive patients. Clin Pharmacol Ther. 2002;71;169-175.80. Lipton RB, Stewart WF, Diamond S et al. Prevalence and burden of migraine in the United States: data from theAmerican Migraine Study II. Headache. 2001;41:646-657.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.61
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane AntibacterialsAHFS Class 840404February 7, 2007I. OverviewInfections of the skin and soft tissues are among the most common infections seen in both community andhospital settings. 1 The skin and mucous membrane antibacterials include single agents and combinationproducts for the treatment and/or prevention of various superficial skin infections, bacterial vaginosis, andimpetigo. 2, 3-11 The agents that the American Hospital Formulary Service (AHFS) have placed in this classinclude clindamycin, gentamicin, metronidazole, mupirocin, neomycin, bacitracin, and polymyxin B. Inaddition, hydrocortisone has been added to some of the combination products. Many of these topicalagents have been a part of treatment regimens for years.Bacterial vaginosis is estimated to be responsible for 22%-50% of all vaginal infections, followed bycandidiasis (17%-39%) and trichomoniasis (4%-35%). 12 As many as 72% of women suffering fromvaginitis may remain undiagnosed. 3,5 Untreated vaginitis is associated with numerous health risks, such aspelvic inflammatory disease, cervicitis, postoperative infection, preterm delivery, postpartum endometritis,posthysterectomy infections, intrauterine infections, and other sexually transmitted infections. 3,5Considering the potential risks, it is important to recognize the symptoms of vaginal infection and to treatthe underlying causes without undue delay.Impetigo is a superficial vesiculopustular skin infection primarily caused by Staphylococcus aureus. 3-11 Inchildren, the impetigo infection caused by Beta Hemolytic Streptococci can be associated withpoststreptococcal glomerulonephritis. Mild impetigo, characterized by a limited number of lesions, istreated with topical antibiotics, while systemic antibiotic therapy is reserved for severe disease.Caution must be exercised with the use of topical antibacterial agents, due to the risk of antibioticresistance. 2 To avoid this problem, topical antibiotics that are not available in systemic dosage forms arepreferable. Consequently, topical aminoglycosides, erythromycin, clindamycin, and metronidazole shouldbe used conservatively.Mupirocin (pseudomonic acid) is a natural product produced by Pseudomonas fluorescens. 6 Mupirocin isactive against gram-positive cocci, and its use is directed against S. aureus, both methicillin-susceptible andmethicillin-resistant strains. Low-level resistance has been observed after prolonged use, but localconcentrations achieved with topical application are well above the minimum inhibitory concentration(MIC). High-level resistance results in complete loss of activity. Strains with high-level resistance havecaused nosocomial (hospital) outbreaks of staphylococcal infection and colonization. Mupirocin isindicated for topical treatment of minor skin infections, such as impetigo. Topical application over largeinfected areas, such as decubitus ulcers or open surgical wounds, has been identified as an important factorleading to emergence of mupirocin-resistant strains and is not recommended. Mupirocin is also indicatedfor intranasal application for elimination of methicillin-resistant S. aureus carriage by patients or healthcare workers.The skin and mucous membrane antibacterial agents that are included in this review are listed in Table 1.This review encompasses all (topical) dosage forms and strengths. Products solely indicated for thetreatment of acne and/or rosacea are considered cosmetics, and are not covered by Alabama Medicaid;hence, these products are not included in this review. Most of the agents within this class are availablegenerically in at least one dosage form, and combination products containing bacitracin and polymyxin B,with or without neomycin, are available over-the-counter.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.62
Table 1. Skin and Mucous Membrane Antibacterials Included in this <strong>Review</strong>Generic Name(s) Formulation(s) Example BrandName(s)Current PDLAgent(s)clindamycinvaginal cream, vaginal Cleocin ® *,clindamycinsuppositoryClindesse ®gentamicin cream, ointment Garamycin† gentamicinmetronidazole vaginal gel Metrogel-Vaginal ® *,Vandazole ®metronidazole,Metrogel-Vaginal ®mupirocin ointment Bactroban ® * mupirocinCentany ® *mupirocin calcium cream, nasal ointment Bactroban nonebacitracin andpolymyxin B‡ointment, packet,powderPolysporin ® * bacitracin andpolymyxin Bbacitracin, neomycin,and polymyxin B‡ointment, packet Neosporin ® * bacitracin, neomycin,and polymyxin Bbacitracin, neomycin, ointment Cortisporin ® nonepolymyxin B, andhydrocortisoneneomycin andpolymyxin BirrigationNeosporin G.U.Irrigant ® *neomycin andpolymyxin Bneomycin, polymyxinB, and hydrocortisonecream Cortisporin ® none*Generic is available in at least one dosage form or strength.†Brand is no longer available.‡Over-the-counter product is available in at least one dosage form or strength.Humans are natural hosts for many microorganisms that colonize the skin as normal flora. 1,2 Table 2outlines the predominant microorganisms of normal skin. Staphylococcus aureus and Streptococcuspyogenes are infrequent resident flora, but they account for a wide variety of bacterial pyodermas. Exposedareas of the body, such as the face and neck, generally have the highest bacterial density and hereStaphylococcus epidermidis is the most common organism.Table 2. Predominant Microorganisms of Normal Skin 1BacteriaGram-positiveCoagulase-negative staphylococciMicrococci (Micrococcus luteus)Corynebacterium species (diphtheroids)Propionibacterium speciesGram-negativeActinetobacter speciesFungiMalassezia speciesCandida speciesCommon bacterial infections of the skin are classified as primary or secondary. 1 Primary infections usuallyinvolve previously healthy skin and are typically caused by a single pathogen. Secondary infections occurin areas of previously damaged skin and are frequently polymicrobic (Table 3).Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.63
Table 3. Bacterial Classification of Important Skin and Soft Tissue Infections 1Type of InfectionMicroorganismsPrimaryErysipelasGroup A streptococciImpetigoStaphylococcus aureus, group A streptococciLymphangitis Group A streptococci, occasionally S. aureusCellulitisNecrotizing fasciitisType 1Type 2SecondaryDiabetic footinfectionsPressure soresBite woundsAnimalHumanBurn woundsGroup A streptococci, S. aureus, occasionally other gram-positive cocci, gramnegativebacilli, and/or anaerobesAnaerobes (Bacteroides spp., Peptostreptococcus spp.) and facultative bacteria(streptococci, Enterobacteriaceae)Group A streptococciS. aureus, streptococci, Enterobacteriaceae, Bacteroides spp.,Peptostreptococcus spp., Pseudomonas aeruginosaS. aureus, streptococci, Enterobacteriaceae, Bacteroides spp.,Peptostreptococcus spp., Pseudomonas aeruginosaPasteurella multocida, S. aureus, streptococci, Bacteroides spp.Eikenella corrodens, S. aureus, streptococci, Corynebacterium spp.,Bacteroides spp., Peptostreptococcus spp.Pseudomonas aeruginosa, Enterobacteriaceae, S. aureus, streptococciII.Evidence-Based Medicine and Current Treatment GuidelinesCurrent treatment guidelines that incorporate the skin and mucous membrane antibacterials are summarizedin Table 4.Table 4. Treatment Guidelines Using the Skin and Mucous Membrane Antibacterials<strong>Clinical</strong> GuidelineRecommendation(s)The American College of Obstetriciansand Gynecologists (ACOG) PracticeBulletin: <strong>Clinical</strong> ManagementGuidelines for Obstetrician-Gynecologists: Vaginitis 12 ••Nonpregnant women with bacterial vaginosis can betreated with vaginal clindamycin, oral clindamycin,vaginal metronidazole, or oral metronidazole products.Disulfiram reactions may occur with both oral and topicalmetronidazole.Centers for Disease Control andPrevention (CDC) Morbidity andMortality Weekly Report(MMWR):Sexually TransmittedDiseases Treatment Guidelines, 2006 13 • Bacterial vaginosis in nonpregnant persons: CDCguidelines recommend the use of either metronidazole gel0.75% (one 5-g applicator per day, intravaginally) for 5days, clindamycin cream 2% (one 5-g applicatorintravaginally) for 7 days every evening, ormetronidazole 500 mg twice daily for 7 days.• The oral and vaginal metronidazole regimens are equallyefficacious. The 2 g single dose metronidazole therapy isno longer recommended.• Two alternative regimens are clindamycin ovules, 100mg intravaginally at bedtime for 3 days or clindamycin300 mg capsules twice daily for 7 days.• Clindamycin vaginal cream and ovules are comparable inefficacy.• Bacterial vaginosis in pregnant persons: CDC guidelinesrecommend the use of either metronidazole 500 mg twicedaily, 250 mg three times daily, or clindamycin 300 mgtwice daily for 7 days. According to some specialists,systemic therapy is preferred in treating pregnant patientswith bacterial vaginosis.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.64
<strong>Clinical</strong> GuidelineRecommendation(s)British Association for Sexual Healthand HIV, <strong>Clinical</strong> Effectiveness Group:National Guideline for theManagement of Bacterial Vaginosis(2006) 14 ••The guideline recommends the use of oral metronidazolegiven as either a single 2 g dose or as 400-500 mg twicedaily for 5-7 days.Alternative regimens include: intravaginal metronidazolegel (0.75%) once daily for 5 days, clindamycin cream(2%) once daily for 7 days, clindamycin 300 mg twicedaily for 7 days, or tinidazole 2 g single dose.• Intravaginal products are preferred in lactating women.Infectious Diseases Society of America(IDSA): Practice Guidelines for theDiagnosis and Management of Skinand Soft-Tissue Infections 15 • Impetigo: penicillinase-resistant penicillins or firstgenerationcephalosporins are the preferred therapy.Topical therapy with mupirocin is equivalent to oralsystemic antimicrobials and may be used when lesions arelimited in number.• Furuncles/carbuncles: antibacterial agents are thepreferred method of controlling recurrent furunculosis.Mupirocin ointment applied twice daily in the anteriornares for the first 5 days each month reduces recurrenceby 50%. Few systemic antibiotics attain adequate levels inthe nasal secretions to achieve prolonged elimination ofstaphylococci.• Therapy for the typical case of erysipelas or cellulitisshould include an antibiotic active against streptococci.Agency for Health Care Policy andResearch (AHCPR) Pressure Ulcer<strong>Clinical</strong> Practice Guidelines: ManagingBacterial Colonization and Infection 16 ••A 2-week trial of topical antibiotics should be consideredfor nonhealing clean pressure ulcers.Topical antiseptics should not be used to reduce bacteriain wound tissue.• Systemic antibiotics are not required for pressure ulcerswith clinical signs of local infection.• Systemic antibiotic therapy is required for patients withbacteremia, sepsis, advancing cellulitis, or osteomyelitis.International Society for PeritonealDialysis (ISPD) Guideline: PeritonealDialysis-Related Infections: 2005Update 17 ••Prevention of catheter infections (and thus peritonitis) isthe primary goal of exit-site care.One of the following three strategies is recommended:oDaily application of mupirocin cream/ointment to theskin around the exit site, in response to a positiveexit-site culture for S. aureuso Intranasal mupirocin twice daily for 5–7 days eachmonth, once the patient is identified as a nasal carriero Exit-site gentamicin cream daily• Mupirocin ointment should be avoided in patients withpolyurethane catheters and mupirocin cream should besubstituted.American Diabetes Association:Consensus Development Conferenceon Diabetic Foot Wound Care 18 • Current evidence does not support the use of antibiotictherapy for patients with clinically uninfected lesions.• Oral antibiotic therapy is recommended for patients withmild to moderate infections. Commonly used oral agentsinclude cephalexin, clindamycin, andamoxicillin/clavulanate.• Topical antibiotics have not been well studied in patientswith diabetic foot infections.• Antiseptic agents and various astringents are cytotoxic tothe tissue and are not recommended.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.65
III.IndicationsFood and Drug Administration (FDA)-approved indications for the skin and mucous membrane antibacterials are noted in Table 5.Table 5. FDA-Approved Indications for the Skin and Mucous Membrane Antibacterials 3-11,20-30Drug(s) Treatmentof PrimaryandSecondarySkinInfectionsTreatment ofSecondarily InfectedTraumatic SkinLesions due toSusceptible Strainsof S. Aureus And S.Treatmentof BacterialVaginosisTopicalTreatmentof Impetigodue to S.Aureus andS. PyogenesPyogenesClindamycin a(pregnancycategory B*)Gentamicin aMetronidazole a(pregnancycategory B)Mupirocin a(ointment)Mupirocin calcium a(cream)Bacitracin andpolymyxin BBacitracin, neomycin,and polymyxin BBacitracin, neomycin,polymyxin B, andhydrocortisoneNeomycin andpolymyxin BNeomycin, polymyxin B,and hydrocortisoneEradication ofNasalColonizationwith MRSA inAdult Patientsand HealthCare Workersa(nasal)First Aid toHelp Reducethe Risk ofSkin Infectionin MinorCuts, Scrapes,and BurnsaaTreatment ofCorticosteroid-ResponsiveDermatoseswith SecondaryInfectionaBladderIrrigation,Adjuncta a*Non-pregnant women only (Clindesse®); non-pregnant women, pregnant women during the second and third trimesters (Cleocin®); but note that CDC guidelines recommend against use late in pregnancy.MRSA= methicillin-resistant Staphylococcus aureusaIV.PharmacokineticsPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.66
The pharmacokinetic parameters for the skin and mucous membrane antibacterials are summarized in Table 6.Table 6. Pharmacokinetic Parameters of the Skin and Mucous Membrane Antibacterials 3-11,20-30Drug(s)Onset(hours)Duration(hours)Time to Peak(hours)Absorption(%)Active Metabolites Half-Life(hours)Protein Binding(%)Clindamycin No data No data 1-3 10 Yes1.5-5.3 60-95Clindamycinsulfoxide,N-dimethylclindamycinGentamicin* No data 6-12 No data 5 No 1.5-4 0-30Metronidazole No data No data 8-12 0.75-71 Yes6-14
V. Drug InteractionsDrug interactions reported in association with vaginal products are presented in Table 7. A literature searchindicates that there are no significant drug interactions with other skin and mucous membrane antibacterialagents discussed in this review. 3-11,20-31Table 7. Significant Drug-Drug Interactions Reported With the Skin and Mucous MembraneAntibacterialsDrug(s)Significance InteractionMechanismLevelClindamycin 2 Nondepolarizingmuscle relaxantsClindamycin may potentiate theaction of nondepolarizing musclerelaxants, possibly contributing torespiratory depression.Metronidazole 1 Disulfiram Concurrent use may result in acutepsychosis or a confusional state.Metronidazole vaginal gel shouldnot be used within 2 weeks ofdisulfiram.Metronidazole 1 Ethanol Disulfiram-like reaction may occurwith concurrent metronidazole andethanol use.Metronidazole 2 Anticoagulants Metronidazole may potentiate theanticoagulant effect of warfarin,resulting in prolongation of theprothrombin time and an increasedrisk of bleeding.Significance Level 1=major severitySignificance Level 2=moderate severityPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.68
VI.Adverse Drug EventsThe most common adverse drug events reported with the skin and mucous membrane antibacterials are noted in Table 8.Table 8. Adverse Drug Events (%) Reported with the Skin and Mucous Membrane Antibacterials 3-11,20-30AdverseEvent(s)Clindamycin Gentamycin Metronidazole Mupirocin BacitracinandPolymyxinBBacitracin,Neomycin,andPolymyxinBBacitracin,Neomycin,Polymyxin B,andHydrocortisoneNeomycinandPolymyxinBNeomycin,Polymyxin B,andHydrocortisoneCentral Nervous SystemAtaxia - a - - - - - - -Dizziness - a 2 a - - - - -Depression - - a - - - - - -Fatigue - - a - - - - - -Headache 1-10 a 5-9 1.7-3.6 - - - - -Neurotoxicity - a - - - - - - -DermatologicalBurning >10 - a 1.5-3.6 1-10 - - a aCellulites - - - a - - - - -Contact- - - a a a a a adermatitisDermatitis a - - a - - - - -Dryness 12 - a a - - - - -Edema - a - a - a - - -Erythema - 1-10 a a 1-10 a - a aFailure to heal - - - - - a - - -Folliculitis 1-10 - - - - - - - -Irritation - a a - - a a - -Oiliness >10 - - - - - - - -Pain - - - 1.5 - - - - aPeeling of skin >10 - - - - - - - -Pruritis >10 1-10 a 1-2.4 1-10 a a - aRash a 1-10 a a 1-10 - a a aStinging - - - 1.5 - - - - aSwelling - - - a 1-10 a - - aUrticaria - - - - - - - a aPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.69
AdverseEvent(s)Clindamycin Gentamycin Metronidazole Mupirocin BacitracinandPolymyxinBBacitracin,Neomycin,andPolymyxinBBacitracin,Neomycin,Polymyxin B,andHydrocortisoneNeomycinandPolymyxinBNeomycin,Polymyxin B,andHydrocortisoneGastrointestinalAbdominal pain 1-10 - - - - - - - -Bloating - - a - - - - - -Constipation 1 - - - - - - - -Cramping - - a - - - - - -Decreased- - 1 - - - - - -appetiteDiarrhea 1-10 - 1 - - - - - -Dyspepsia a - - - - - - - -Gas - - a - - - - - -Nausea 1-10 - 4 a - - - - -Taste- - 2 0.8 - - - - -perversionVomiting 1-10 - 4 - - - - - -GenitourinaryBladderirritation- - - - - - - a -Dark urine - - a - - - - - -Pelvic- - 3 - - - - - -discomfortNephrotoxicity - a - - - - - a -Urinary tract1 - - - - - - - -infectionVaginal burning - - a - - - - - -Vaginal1 - 12 - - - - - -dischargeVaginal- - 9 - - - - - -irritationVaginosis,14 a 10 - - - - - -fungalVaginal pain 1.9 a - - - - - - -Vulvovaginalpruritis3.3 a - - - - - - -Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.70
AdverseEvent(s)HematologicBlooddyscrasiasMusculoskeletalClindamycin Gentamycin Metronidazole Mupirocin BacitracinandPolymyxinBBacitracin,Neomycin,andPolymyxinBBacitracin,Neomycin,Polymyxin B,andHydrocortisoneNeomycinandPolymyxinBNeomycin,Polymyxin B,andHydrocortisonea a 1.7 a - - - - -Back pain 1.6 - - - - - - - -Neuromuscular a - - - - - - a -blockadeGait instability - a - - - - - - -RespiratoryApnea - - - - - - a - -Cough - - - a - - - - -Dyspnea - a - - - - - - -Nasopharyngitis 1 - - 0.5-4 - - - - -Respiratory- - - 5 - - - - -tract infectionRhinitis - - - 1-6 - - - - -MiscellaneousAllergy 1-10 a - - 1-10 a - - aAlopecia - a - - - - - - -Ototoxicity - a - - - - - a aPhotosensitivity - a - - - - - - -SecondaryinfectionSensitization toneomycin- - - - - - a - a- - - - - - - - aPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.71
VII.Dosing and AdministrationThe usual dosing regimens for the skin and mucous membrane antibacterials are summarized in Table 9.Table 9. Usual Dosing for the Skin and Mucous Membrane Antibacterials 3-11,20-30Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityClindamycin Vaginal suppository:insert once daily, preferablyat bedtime, for 3 consecutivedaysSafety and efficacy inchildren have not beenestablishedVaginal suppository:100 mgVaginal cream: 2%Vaginal cream:Cleocin ® : insert oneapplicatorful intravaginallyonce daily, preferably atbedtime, for 3-7 consecutivedays in nonpregnant womenGentamicinMetronidazoleMupirocinMupirocin calciumBacitracin andpolymyxin BClindesse ® : insert oneapplicatorful intravaginallyonceCream: apply to the affectedarea 3-4 times dailyOintment: apply to theaffected area 3-4 times dailyInsert one applicatorful onceor 2 times daily for 5 daysOintment: apply to theaffected area 3 times dailyCream: apply to the affectedarea 3 times daily for 10 daysNasal ointment: apply onehalfof the ointment from thesingle-use tube into eachnostril 2 times daily for 5daysOintment, powder: apply tothe affected area 1-4 timesdailyCream: apply to theaffected area 3-4 timesdailyOintment: apply to theaffected area 3-4 timesdailySafety and efficacy inchildren have not beenestablishedOintment: apply to theaffected area 3 timesdaily, re-evaluate areasnot showing a responsewithin 3-5 daysCream: apply to theaffected area 3 times dailyfor 10 daysNasal ointment: 12 yearsof age or older: applyone-half of the ointmentfrom the single-use tubeshould into each nostriltwice daily for 5 daysOintment, powder: applyto the affected area 1-4times dailyCream: 0.1%Ointment: 0.1%Vaginal gel 0.75%Ointment: 2%Cream: 2%Nasal ointment: 2%Ointment:bacitracin 500 U/gand polymyxin B10,000 U/gPowder:bacitracin 500 U/gand polymyxin B10,000 U/g72Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityApply to the affected area 1-3 Apply to the affected areatimes daily1-3 times dailyBacitracin,neomycin, andpolymyxin BBacitracin,neomycin,polymyxin B, andhydrocortisoneNeomycin andpolymyxin BNeomycin,polymyxin B, andhydrocortisoneApply to the affected area 2-4times dailyBladder irrigation: 1 mLirrigant added to 1 L of salinesolution, 1 L of irrigant dailyfor up to 10 daysApply to the affected area 1-4times dailyApply to the affected area2-4 times dailyBladder irrigation: 1 mLirrigant added to 1 L ofsaline solution, 1 L ofirrigant daily for up to 10days2 years of age or older:apply to the affected area1-4 times dailyOintment:Bacitracin 400 U/g,neomycin 3.5 mg/g,polymyxin B 5000U/gOintment 1.0%:bacitracin 400 U/g,neomycin 3.5 mg/g,polymyxin B 5000U/g, andhydrocortisone 10mg/gSolution, irrigant:neomycin 40 mg,polymyxin B sulfate200,000 units/mL:1mL, 20 mLCream 0.5%:neomycin 3.5 mg/g,polymyxin B 10,000units/g, andhydrocortisone 5mg/gPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.73
VIII. Effectiveness<strong>Clinical</strong> studies evaluating the safety and efficacy of the skin and mucous membrane antibacterials are summarized in Table 10.Table 10. Comparative <strong>Clinical</strong> Trials Using the Skin and Mucous Membrane AntibacterialsStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsVaginal ProductsFaro et al. 32Clindamycin phosphate2%, formulated in 5 g ofsustained-release vaginalcream, for a total of 100mg (Clindesse ® ), oneintravaginal dosevs.RCT, MC, SB, PG,ACPatients were nonpregnantwomen, 18years of age or older,with bacterialvaginosis (BV)infectionsN=54030 daysPrimary:Investigator cure,clinical cure,therapeutic cureSecondary:Not reportedResultsPrimary:There were no statistically significant differences found in the cure ratesbetween the Clindesse ® and the Cleocin ® treatment groups. The P valuesfor investigator cure, clinical cure, and therapeutic cure were 0.702,0.945, and 0.572, respectively.Secondary:Not reportedclindamycin phosphate2%, formulated in 5 gconventional vaginalcream (Cleocin ® ),applied once a dayMcCormack et al. 33Clindamycin phosphate2% vaginal cream, 5 gapplied intravaginally atbedtimeandplacebo, 5 g appliedintravaginally in themorningvs.RCT, DB, MCPatients werenonpregnantnonlactating women,aged 16 years andolder, withsymptomaticbacterial vaginosisN=1597 days, withfollow-upvisits at days5-10 and 25-39Primary:<strong>Clinical</strong> cure orimprovementSecondary:Not reportedPrimary:<strong>Clinical</strong> cure or improvement was seen in 69.6% (55/79) of patients inthe clindamycin treatment group compared to 41.8% (33/79) of patientsin the triple sulfonamide group (P
StudyandDrug Regimentriple sulfonamidevaginal cream, 5 gapplied intravaginally inthe morning and atbedtimeStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsclindamycin and sulfonamide were 44.2% and 46.4%, respectively(P=0.11).The Gram stain evaluation showed fewer stains consistent with bacterialvaginosis for the clindamycin group as compared to the sulfonamidegroup, at both post-treatment evaluations (P0.5).There was no significant difference between the proportion of patients inthe metronidazole treatment group who rated their vaginal infection ascured (79.6%) vs. the proportion of patients randomized to clindamycintherapy who considered themselves cured (78.3%); P value not reported.There was no difference in the number of patients reporting symptoms ofvaginitis and cervicitis at either the first or second follow-up visit (Pvalue not reported).Treatment-related adverse effects were more frequent in themetronidazole group (16.3%), compared to the clindamycin treatmentgroup (10.3%), but this difference was not statistically significant(P=0.104).Austin et al. 35Clindamycin vaginalRCT, DB, ACPremenopausal, non-N=11990 daysPrimary:Overall clinicaloutcome,Secondary:Not reportedPrimary:The clinical response rate did not differ between the two treatmentgroups. At 7-12 days, cure rates were 79% and 88% for metronidazole75Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimenovules QD for 3 daysvs.metronidazole vaginalgel QD for 5 daysStudy DesignandDemographicspregnant women>18 years of agediagnosed withbacterial vaginosis;patients wereexcluded if theywere pregnant,breastfeeding,menstruating, werecurrently receivingbacterial therapy, orhad an intrauterinedeviceSample Sizeand StudyDurationEnd PointsmicrobiologicresponseSecondary:Not reportedResultsand clindamycin, respectively (P=0.3). At 35-45 days, cure rates were62% and 55%, respectively (P=0.5). The rates were 58% and 55%,respectively, at days 70-90 after therapy (P=0.8).While both therapies resulted in decreased colonization by Gardnerellavaginalis and Mycoplasma hominis (P
StudyandDrug RegimenBID for 7 daysFischbach et al. 37Clindamycin phosphatevaginal cream 2%, 5 gintravaginally at bedtimefor 7 days, in addition totwo placebo capsulesBID for 7 daysvs.Study DesignandDemographicsRCT, DB, AC, MCPremenopausal, nonpregnantwomen>18 years of agediagnosed withbacterial vaginosisSample Sizeand StudyDurationN=40739 daysEnd PointsPrimary:Cure rate, posttreatmentvulvovaginalcandidiasisSecondary:Not reportedResultsPrimary:There was no significant difference in cure rate for oral metronidazole(78%) and clindamycin vaginal cream (83%) (P value not reported).The incidence of drug-related adverse effects was similar in both groups,approximately 12% (P value not reported).There was no significant difference in the rates of post-treatmentvulvovaginal candidiasis associated with oral metronidazole (4.7%), andclindamycin vaginal cream (8.5%) (P value not reported).metronidazole 500 mg(two 250 mg capsules)BID for 7 days, inaddition to placebovaginal cream, 5 gintravaginally at bedtimefor 7 daysArredondo et al. 38Metronidazole 500 mgcapsules BID for 7 daysin addition to placebocreamvs.clindamycin vaginalcream 2%, 5 g BID for 7days in addition toplacebo capsulesRCT, DB, MCWomen withsymptomaticbacterial vaginosisN=18450 daysPrimary:Total healing rate,relapse rate, failurerate, adverseeventsSecondary:Not reportedSecondary:Not reportedPrimary:Improvement in total healing was 87% for clindamycin and 79% formetronidazole (P>0.22).While 7% of patients randomized to the metronidazole group developedrelapse of the disease following treatment, none of the patients receivingtopical clindamycin experienced a relapse (P value not reported).While clindamycin had a failure rate of 3%, 15% of patients in themetronidazole group failed treatment (P value not reported).Both drugs were well tolerated, with the most serious side effect,generalized rash, reported by a patient on metronidazole therapy.Andres et al. 39 RCT, DB, PC, PRO N=60 Primary:Cure rate,Secondary:Not reportedPrimary:There was no statistically significant difference between thePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.77
StudyandDrug RegimenMetronidazole 500 mgcapsules BID for 7 daysin addition to placebocreamvs.clindamycin vaginalcream 2%, 5 g BID for 7days in addition toplacebo capsulesSchmitt et al. 40Metronidazole 500 mgcapsules BID for 7 daysin addition to placebocreamvs.clindamycin vaginalcream 2% 5 g QD for 7days in addition toplacebo capsulesStudy DesignandDemographicsNon-pregnantwomen 18 to
StudyandDrug RegimenHiguera et al. 41Metronidazole 500 mgcapsules BID for 7 daysin addition to placebocreamvs.clindamycin vaginalcream 2% 5 g QD for 7days in addition toplacebo capsulesStudy DesignandDemographicsperiodic diarrhea, orcurrent genitalherpes virusinfectionRCT, DB, PCNonpregnant women16 to ≤60 years ofage diagnosed withbacterial vaginosis;patients wereexcluded if theywere pregnant,breastfeeding,menstruating,received bacterialtherapy within theprevious 2 weeks,had history ofantibiotic-associatedcolitis or frequentperiodic diarrhea,current genitalherpes virusinfection, positivecultures of Neisseriagonorrhoeae,Candida albicans,Trichomonasvaginalis, orChlamydia, centralnervous disease, orblood dyscrasiasSample Sizeand StudyDurationN=8250 daysEnd PointsPrimary:Cure rate,improvement,clinical failure rate,relapse rateSecondary:microbiologicalcure rate, vaginalfluid description,patient’s efficacyevaluation, adverseeffectsResultsThere was no statistically significant difference in side effects amongpatients randomized to receive either of the two study drugs (P value notreported).Secondary:Not reportedPrimary:There was no statistically significant difference between themetronidazole (82%) and clindamycin (86%) study groups at the 1-weekfollow-up visit in terms of patients who have either improved or werecured post-treatment (P value not reported).There was no statistically significant difference in cure rate between themetronidazole (88%) and the clindamycin (90%) groups at the 4-weekfollow-up visit (P value not reported).There was no statistically significant difference in failure rate betweenthe metronidazole (17.9%) and clindamycin (14.3%) treatment groups atthe 1-week and 4-week follow-up visits (P value not reported).Secondary:There was no statistically significant difference in microbiological curerate between the metronidazole (82%) and the clindamycin (86%) groupsat the first follow-up visit (P value not reported).There was no statistically significant difference in patient self-reportedcure rate between the metronidazole (82%) and clindamycin (86%)groups (P value not reported).There was a significantly higher percentage of patients in theclindamycin group (10%) with a gram stain compatible with bacterialvaginosis at the second follow-up visit compared with the metronidazolegroup (4%) (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsNasal ProductsPerl et al. 42Mupirocin calcium nasalointment 2%, applied toeach anterior nostril BIDfor up to 5 days prior tooperative procedurevs.placebo ointment,applied to each anteriornostril BID for up to 5days prior to operativeprocedureMody et al. 43Mupirocin calcium nasalointment 2%, applied toeach anterior nostril BIDfor up to 2 weeksvs.placebo ointment,applied to each anteriorRCT, DB, PCAdult patientsundergoing elective,nonemergency,cardiothoracic,general, oncologic,gynecologic, orneurologic surgicalprocedure, no S.aureus infectionwithin 1 month ofstudy onset, no nasalor facial bonedisruption; patientswho were onlyhaving permanentcatheters insertedwere excluded fromthe studyRCT, DB, PCResidents ofVeterans Affairs(VA) andcommunity longtermfacilities, withS. aureuscolonization, asassessed by 2consecutive culturesN=3,86430 daysN=1276 monthsPrimary:Nosocomial S.aureus infection,nasal carriage of S.aureusSecondary:Not reportedPrimary:Nosocomial S.aureus infection,nasal carriage of S.aureusSecondary:Not reportedThere was no statistically significant difference in the incidence of sideeffects between the metronidazole group (22%) and clindamycin (15%)group (P value not reported).Primary:The rates of S. aureus infection at surgical sites among patients receivingmupirocin ointment (2.3%) and placebo (2.4%) were similar (P value notreported).Among patients colonized with S. aureus, the risk for developing anosocomial S. aureus infection at any site was significantly lower inpatients receiving mupirocin ointment (4%) as compared to the placebogroup (7.7%) (odds ratio [OR], 0.49; 95% confidence interval (CI), 0.25-0.92; P=0.02).Nasal carriage was eliminated in 83.4% of patients randomized tomupirocin ointment as compared to 27.4% of patients receiving placebotherapy (P=0.001).Patients receiving 6 or more doses of mupirocin exhibited a greater rateof S. aureus elimination (93.3%) compared to patients getting 3-5 dosesof mupirocin ointment (81.3) (P value not reported).Secondary:Not reportedPrimary:Over the entire study duration, the hazard rate of colonization was 4.12times higher for the placebo group vs. mupirocin group (95% CI, 2.68-6.31; P
StudyandDrug Regimennostril BID for up to 2weeksWertheim et al. 44Mupirocin calcium nasalointment 2%, applied toeach anterior nostril BIDfor 5 daysvs.placebo ointment,applied to each anteriornostril BID for 5 daysHarbarth et al. 45Mupirocin calcium nasalointment 2%, applied toeach anterior nostril BIDfor 5 daysvs.Study DesignandDemographicsperformed 18years old with S..aureus colonization,hospitalized in nonsurgicaldepartments, notexpected to bedischarged within 1day of study onset;patients wereexcluded if they hada nasal tube, recentor current mupirocintherapy, or anycurrent S. aureusinfectionRCT, DB, PC,Patients >16 yearsold with methicillinresistant S. aureus(MRSA)colonization,admitted to theSample Sizeand StudyDurationN=1,6022 weeksN=9830 daysEnd PointsPrimary:Incidence ofnosocomial S.aureus infectionSecondary:Time tonosocomial S.aureus infection,duration ofhospitalization, inhospitalmortalityPrimary:Incidence ofoverall MRSAcarriageeradicationSecondary:Nasal MRSAcolonization (P
StudyandDrug Regimenplacebo ointment,applied to each anteriornostril BID for 5 daysSoto et al. 46Mupirocin calcium nasalointment 2%, one-half of1 g tube applied to eachnostril BID for 5 daysvs.bacitracin ointment, 0.5cm applied to eachnostril TID for 5 daysStudy DesignandDemographicsuniversity hospitalsof Geneva; patientsexcluded if pregnant,active treatment forstaphylococcalinfection, trachealMRSA colonizationor tracheotomy tubecolonized withMRSA, or externalosteosynthesismaterial colonizedwith MRSAHealthcare workerscolonized with S.aureusSample Sizeand StudyDurationN=3530 daysEnd Pointscarriageeradication, MRSAinfection rate,development ofmupirocinresistancePrimary:Rate of S. aureuseradication at 72-96 hours, and 30days post topicalantibioticadministrationSecondary:Not reportedResultsgroup (23%) (RR, 0.57; 95% CI, 0.31-1.04; P=0.06).There was no statistically significant difference in the incidence ofMRSA infections between the two groups (1.48 vs. 2.82 infections per1,000 patient days, respectively; RR, 0.52; 95% CI, 0.14-2.02; P=0.53).There was an association between low-level mupirocin resistance atstudy entry and subsequent treatment failure in both study groups(P=0.003). High-level mupirocin resistance was not identified in thestudy groups.Primary:Nasal carriage was eradicated in 44% of patients randomized tobacitracin ointment as compared to 94% of patients receiving mupirocintherapy, as assessed 72-96 hours after administration of the topicalantibiotic (P
StudyandDrug Regimensystemic antimicrobialagentsvs.placeboStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsNot reported MRSA infections between the mupirocin and placebo groups (RR, 0.47;95% CI, 0.13-1.70; P value not reported).In the study comparing topical mupirocin and fusidic acid, nasaldiscomfort was reported by patients in both study groups (P value notreported).A topical and systemic combination therapy is not more efficaciouscompared to topical antibiotic monotherapy (P value not reported).Three of the evaluated trials reported resistance of the MRSA strains tothe antibacterial agents (P value not reported).Topical Products: Catheter-Related InfectionsBernardini et al. 48 RCT, DB, MCMupirocin calcium 2%topical cream, applied tothe catheter exit site QDvs.gentamicin sulfate 0.1%topical cream, applied tothe catheter exit site QDPatients >18 years ofage on peritonealdialysis; patientswere excluded ifthey had catheterinfection orperitonitis within 30days of study onsetN=13312 monthsPrimary:P. aeruginosa andS. aureus catheterinfection ratesSecondary:Gram-negative andgram-positiveperitonitis, overallcatheter infection,peritonitis rate,causativeorganism, catheterremoval, time tofirst catheterinfectionSecondary:Not reportedPrimary:There was a statistically significant difference in P. aeruginosa catheterinfection rate between the gentamicin and mupirocin treatment groups(0.0/year vs. 0.11/year, respectively; P
StudyandDrug RegimenStudy DesignandDemographicsTopical Products: Infection ProphylaxisD’Amico et al. 49 RCT, MATopical antibacterialregimens (e.g.,polymyxin, tobramycin,amphotericin, nystatin,neomycin, gentamycin,vancomycin)vs.topical antibacterial inaddition to systemicantibacterial regimensvs.systemic antibacterialregimens (e.g.,cefotaxime, ceftriaxone,ciprofloxacin,ceftazidime)vs.All randomizedcontrolled trialsevaluating the effectof antibioticprophylaxis on theprevention ofrespiratory tractinfections and deathsin critically ill adultpatients in intensivecare unit (ICU);studies based onspecific pre-selectedpatient types (e.g.,patients undergoingelective esophagealresection, cardiac orgastric surgery, livertransplantation,suffering from acuteliver failure) wereexcludedSample Sizeand StudyDurationN=3,36116 trialsEnd PointsPrimary:Prevention ofrespiratory tractinfection, overallmortalitySecondary:Not reportedResults(0.09/year with mupirocin vs. 0.15/year with gentamicin; P=0.45).Primary:The prevalence of respiratory tract infections was 16% among patientsreceiving prophylaxis with a combination of topical and systemicantibacterial regimen compared to 36% in the control group (OR, 0.35;95% CI, 0.29-0.41; P value not reported).The prevalence of respiratory tract infections was 18% among patientsreceiving prophylaxis with a topical antibacterial regimen compared to28% in the control group (OR, 0.56; 95% CI, 0.46-0.68; P value notreported).There was a 24% mortality rate among patients receiving prophylaxiswith a combination of topical and systemic antibacterial regimencompared to 30% in the control group (OR, 0.80; 95% CI, 0.69-0.93; Pvalue not reported).There was no difference in mortality between patients receivingprophylaxis with topical antibacterial regimen and placebo (26% in bothgroups; OR, 1.01; 95% CI, 0.84-1.22; P value not reported).Secondary:Not reportedplaceboTopical Products: Miscellaneous Skin InfectionsRist et al. 50RCT, DB, DD, MC,PGMupirocin calciumtopical cream 2% TID,in addition to oralplacebo QID for 10 daysvs.Patients >8 yearsold, weighing >40kg, with secondaryeczema infectionscored as >8, on theN=15910 daysPrimary:<strong>Clinical</strong> responseat the end oftherapySecondary:Bacteriologicalresponse, adversePrimary:There was no statistically significant difference in clinical responseamong the two treatment groups (P=0.29).Secondary:Bacteriological success, defined in terms of bacterial eradication, wasstatistically higher in the mupirocin group (50%) compared to thecephalexin group (28%) (P=0.005).84Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimencephalexin 250 mg QID,in addition to creamplacebo TID for 10 daysGoldfarb et al. 51Mupirocin topicalointment 2% TID for 8daysvs.erythromycinethylsuccinate 40mg/kg/day QID for 8daysDagan et al. 52Mupirocin topicalointment 2% TIDadministered in additionto a placebo suspensionfor 7 daysvs.erythromycinethylsuccinatesuspension 50mg/kg/day, up tomaximum daily dose of750 mg daily, in additionto placebo ointment,administered TID for 7daysStudy DesignandDemographicstotal skin infectionrating scale (SIRS)RCT, ACSample Sizeand StudyDurationN=62Children >3 months 15 daysof age, withimpetigo; patientswere excluded ifthey had cellulitis,extensive skininvolvement, or tookantibiotic therapywithin 24 hours ofstudy onsetRCT, DB, ACN=102Children
StudyandDrug RegimenTopical antibioticregimens (e.g.,bacitracin, neomycin,gentamycin cream)vs.topical antisepticregimensvs.systemic antibacterialregimensvs.Study DesignandDemographicsPatients withbullous, nonbullous,primary andsecondary impetigoSample Size End Pointsand StudyDuration57 trials symptomsSecondary:Not reportedResultsimprovement compared to placebo (OR, 6.49; 95% CI, 3.93-10.73; Pvalue not reported).None of the evaluated topical antibiotics had any efficacy advantage overone another (P value not reported).A pooled analysis of 10 studies comparing mupirocin with oralerythromycin found mupirocin to be associated with significantly bettercure rates and overall improvement (OR, 1.76; 95% CI, 1.05-2.97; Pvalue not reported).However, there were no significant differences in clinical responsebetween mupirocin, dicloxacillin, cephalexin, or ampicillin.Two small studies found bacitracin to be equivalent to erythromycin andpenicillin (P value not reported).placeboA pooled analysis of two studies found topical antibiotics to be moreeffective in treating impetigo, compared to disinfectant agents (RR, 1.84;95% CI, 1.03-3.29; P value not reported).Combination Topical ProductsLok et al. 54RCT, DB, MCBacitracin (500 U/g),gramicidin (0.25 mg/g),and polymyxin B(10,000 U/g) ointment(Polysporin ® : notegramicidin is no longerin this formulation),applied to the centralvenous catheter at theend of each dialysissession for 2 weeks andPatients >18 years ofage with end-stagerenal diseaserequiringhemodialysis, usinga permanent cuffedcatheter in theinternal jugular veinas their primarysource of vascularaccess; patients wereN=1696 monthsPrimary:Incidence ofinfection,bacteremia,mortality,hospitalization,catheter removaldue to infectionsSecondary:Not reportedSecondary:Not reportedPrimary:A smaller proportion of patients in the active group compared to placeboexperienced an infection during the study duration (12% vs. 34%;P=0.0013). It was calculated that treating 5 patients with the Polysporin ®ointment would prevent one infection (95% CI, 3-11).The proportion of patients experiencing a bacteremia was significantlyhigher in the placebo group compared to the active group (24% vs. 10%;P=0.02). It was calculated that treating 7 patients with the Polysporin ®ointment would prevent one case of bacteremia (95% CI, 4-33).There were 13 deaths in the placebo group compared to 3 deaths in thePolysporin® group within the study period (P=0.0041). It was calculated86Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimenthen with each dressingchangevs.placebo ointment,applied to the centralvenous catheter at theend of each dialysissession for 2 weeks andthen with each dressingchangeHood et al. 55Mupirocin topicalointment, applied to thewound TIDvs.neomycin sulfate/bacitracin/polymyxin Bsulfate ointment (Tao ® ),applied to the woundTIDDire et al. 56Bacitracin zinc, appliedto the wound TIDvs.Study DesignandDemographicsexcluded if they hadacute renal failure,antibiotic use within7 days, or knownallergy to studydrugsRCT, ACEmergencydepartment (ED)patients withuncomplicated softtissue wound 24hours or less beforestudy enrollment;patients wereexcluded if they hadan underlyingfracture, antibioticuse in the previous 7days, puncturewounds, knownallergy to studydrugs, presentwound infectionRCT, DB, PC, PROPatients withuncomplicated softtissue woundadmitted to theSample Sizeand StudyDurationN=997 daysEnd PointsPrimary:Presence ofinfection 7 daysafter study onsetSecondary:Not reportedN=426 Primary:Infection rateSecondary:Not reportedResultsthat treating 8 patients with the Polysporin® ointment would prevent onedeath (95% CI, 5-27).More patients in the placebo group compared to the active treatmentgroup required hospitalization (24% vs. 7%; P=0.0041).More patients in the placebo group compared to the active treatmentgroup required catheter removal due to infections (27% vs. 10%;P=0.0071).Secondary:Not reportedPrimary:There was no statistically significant difference in wound infectionincidence between the mupirocin and the triple antibiotic ointment studygroups (4% vs. 0%, respectively; P value not reported).Secondary:Not reportedPrimary:The wound infection rates for the treatment groups were 5.5% in thebacitracin group, 4.5% in the Tao ® group, 12.1% in the silversulfadiazine group, and 17.6% in the placebo group (P=0.0034).Secondary:87Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimenbacitracin, neomycinsulfate, and polymyxin Bointment (Tao ® ), appliedto the wound TIDvs.silver sulfadiazine,applied to the woundTIDvs.petrolatum, applied tothe wound TIDLeyden et al. 57Bacitracin, neomycinsulfate, and polymyxin B“triple-antibiotic”ointment (Neosporin ® ),applied to the woundBIDvs.Study DesignandDemographicsemergencydepartment (ED)within 12 hours ofinjury; patients wereexcluded if they hadpuncture wounds,allergy to studymedications, historyof immunocompromise,historyof antibiotic usewithin 7 days,underlying fracture,or pregnancyRCT, OL, ACHealthy volunteers,with inducedintradermal blisterwoundscontaminated with S.aureusSample Sizeand StudyDurationN=4822 daysEnd PointsPrimary:Healing rate,overall ranking ofclinical appearanceand the healingrate of wounds,infection rate, S.aureus count after2 applications ofeach test agentNot reportedResultsPrimary:Contaminated blister wounds treated with the triple antibiotic and thePolysporin ® ointments healed significantly faster (mean 9.2 and 8.8 days,respectively) compared to patients treated with benzalkonium chloridespray (14.2 days), merbromin (13.1 days), or those receiving noantibacterial treatment (13.3 days) (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsvs.thimerosal, applied to thewound BIDSecondary:Not reportedvs.hydrogen peroxide 3%,applied to the woundBIDvs.tincture of iodine,applied to the woundBIDvs.camphor and phenol,applied to the woundBIDvs.merbromin, applied tothe wound BIDvs.wound protectant,applied to the woundBIDvs.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.89
StudyandDrug Regimenno treatmentBerger et al. 58Bacitracin, neomycin,and polymyxin B “tripleantibiotic”ointment(Neosporin ® ), applied tothe wound BIDvs.bacitracin andpolymyxin B “doubleantibiotic”ointment(Polysporin ® ), applied tothe wound BIDvs.nonocclusive gauzedressingStudy DesignandDemographicsRCT, AC, PGHealthy volunteers>18 years of age,with dermabrasionwounds on the upperback, producedunder anesthesiaSample Sizeand StudyDurationN=7014 daysEnd PointsPrimary:Pigmentarycomposite score(PCS), texturalcomposite score(TCS)Secondary:Overall ranking ofpigmentarychanges, overallranking of texturalchanges,percentage area ofthe test siteexhibiting scarringResultsPrimary:The triple-antibiotic ointment treatment group had a statisticallysignificant lower PCS (2.6) at 90 days after study onset, compared to thegroup receiving gauze alone (4.2) (P
Additional EvidenceDose SimplificationA search of Medline and Ovid did not reveal data pertinent to this topic.Stable TherapyA search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician VisitsA search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 11. Relative Cost of the Skin and Mucous Membrane AntibacterialsGeneric Name(s) Formulation(s) Example Brand Name(s) BrandCostGenericCostclindamycinvaginal cream, vaginal Cleocin ® *, Clindesse ® * $$$ $$suppositorygentamicin cream, ointment Garamycin† N/A $metronidazole vaginal gel Metrogel-Vaginal ® *,$$$ $$$Vandazole ®mupirocin ointment Bactroban ® *, Centany ® $$-$$$ $$mupirocin calcium cream, nasal ointment Bactroban ® $$$ N/Abacitracin and polymyxin B‡ ointment, packet, powder Polysporin ® * $ $bacitracin, neomycin, and ointment, packet Neosporin ® * $ $polymyxin B‡bacitracin, neomycin, ointment Cortisporin ® $$$ N/Apolymyxin B, andhydrocortisoneneomycin and polymyxin B irrigation Neosporin G.U. Irrigant ® * $$$ $neomycin, polymyxin B, andhydrocortisonecream Cortisporin ® $$ N/A*Generic is available in at least one dosage form or strength.†Brand is no longer available.‡Over the counter product is available in at least one dosage form or strength.N/A = not available.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.91
X. ConclusionsThe skin and mucous membrane antibacterials are approved for the treatment or prevention of varioussuperficial skin infections and bacterial vaginitis. Most of the single entity and combination products areavailable generically in at least one dosage form. The general effectiveness of these agents has beendemonstrated through clinical trials.Because of the complications associated with bacterial vaginosis, all symptomatic women (particularlypregnant women) should be treated. The treatment options include oral or vaginal preparations ofmetronidazole and clindamycin, except in pregnant women, who should not receive intravaginalclindamycin secondary to an association with premature deliveries. 2 Metronidazole and clindamycin areavailable generically in both oral and vaginal dosage forms. Topical products are not more effective thansystemic (oral) agents for this condition; however, they may be preferable due to the reduced potential forsystemic side effects. Although clindamycin use may be associated with in vitro antimicrobial resistance,this has not been shown to affect its in vivo efficacy; thus all of these regimens have been shown to becomparable in terms of efficacy and safety. 33-41 A disulfiram-like reaction has occurred in at least onepatient who ingested alcohol while receiving intravaginal metronidazole. 20,27 Consequently patients shouldbe counseled to avoid alcohol during metronidazole vaginal gel therapy. Additionally, intravaginalclindamycin should be used with caution in patients receiving neuromuscular blocking agents (e.g., ether,pancuronium). 27Topical antibacterials have demonstrated effectiveness in the treatment of S. aureus and methicillinresistantS. aureus (MRSA). A meta-analysis has shown that topical antibacterial therapy favorablycompares to a combination of topical and systemic antibacterial therapy in treating MRSA infections. 47A distinction must be drawn between infection prophylaxis and treatment, as several placebo-controlledclinical trials have shown mupirocin calcium to be ineffective in preventing either S. aureus or MRSAinfections in hospitalized patients. 42-47 In addition, prophylactic mupirocin therapy did not decrease thelength of hospital stay or have an impact on survival. However, mupirocin was effective in eradicating S.aureus nasal carriage in patients already colonized with this pathogen. Furthermore, one study comparingmupirocin and bacitracin topical ointments found the former to be significantly more efficacious inachieving nasal S. aureus eradication. 46 Larger head-to-head studies are needed to access potentialadvantages of mupirocin over the other topical antibacterial agents.Several studies have been conducted comparing different therapeutic options in this population. Regardingthe use of the combination antibacterials in wound care, two studies of patients hospitalized foruncomplicated soft-tissue wound management have found that topical combination antibacterial productsare comparable to single agents in terms of infection prevention. 12,13,56 The “triple-antibiotic” ointment(bacitracin, neomycin, and polymyxin B) did not show an advantage in efficacy over mupirocinmonotherapy. 55 Another study found a small benefit with the use of triple antibiotic compared to bacitracinmonotherapy. 56 In this study, the wound infection rates for the bacitracin and the triple-antibiotic treatmentgroups were 5.5% and 4.5%, respectively. Both therapies were significantly more effective in controllinginfection rate compared to silver sulfadiazine and placebo. In addition, two small studies in healthyvolunteers with administered wounds, (wounds purposely inflicted to evaluate the effect of the study drug)indicate that while there is no statistically significant difference between the triple-antibiotic and thedouble-antibiotic ointments in terms of wound healing rate, both are more efficacious compared to notreatment or treatment with antiseptic products (P< 0.05). 58,59 Combination products containing bacitracinand polymyxin B with and without neomycin, are available over-the-counter. Topical antibacterial agentsshould not be used for the treatment of deep or puncture wounds, animal bites, or serious burns. In addition,they should not be used for the treatment of large surface areas.For the treatment of impetigo, a meta-analysis of relevant studies has found all of the evaluated topicalantibacterials to be comparable in efficacy. 53 Mupirocin was associated with greater response and curerates compared to systemic erythromycin but comparable to other evaluated systemic antibiotics. Bacitracinwas comparable to erythromycin and penicillin. According to the IDSA guideline, penicillinase-resistantpenicillins or first-generation cephalosporins are the preferred therapies for impetigo. 15 Topical therapyPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.92
with mupirocin is equivalent to oral systemic antimicrobials and may be used when lesions are limited innumber.The pharmacokinetics of the skin and mucous membrane antibacterials are similar. 3-11,19-26 Their systemicabsorption is minimal and consequently their side effects are generally limited to local effects. The mostcommonly reported adverse events with the topical antibacterials are allergic contact dermatitis andhypersensitivity type reactions. Due to limited absorption, there is little concern for drug interactions.Therefore, all brand products within the class reviewed are comparable to each other, to the generics andover-the-counter products in this class and offer no significant clinical advantage over other alternatives ingeneral use.XI.RecommendationsNo brand skin and mucous membrane antibacterial is recommended for preferred status. AlabamaMedicaid should accept cost proposals from manufacturers to determine cost effective products andpossibly designate one or more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.93
References1. Pendland SL, Fish DN, Danziger LH. Skin and soft tissue infections. In: DiPiro JT, Talbert RL, Yee GC, et al,eds. Pharmacotherapy: A Pathophysiological Approach. 6 th ed. New York, NY: McGraw-Hill;2005:1977-1995.2. Stulberg DL, Penrod MA, Blatny RA. Common bacterial infections. Am Fam Phys 2002;66(1):119-124.3. Clindamycin: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.4. Gentamicin: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.5. Metronidazole: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.6. Mupirocin: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.7. Bacitracin polymyxin B: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.8. Bacitracin neomycin polymyxin B: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate;2006.9. Bacitracin neomycin polymyxin B hydrocortisone: drug information. In: Rose BD, ed. UpToDate. Waltham,MA: UpToDate; 2006.10. Neomycin polymyxin B: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.11. Neomycin polymyxin B hydrocortisone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA:UpToDate; 2006.12. ACOG Committee on Practice Bulletins—Gynecology. ACOG practice bulletin: <strong>Clinical</strong> managementguidelines for obstetrician-gynecologists, Number 72, May 2006: Vaginitis. Obstet Gynecol 2006;107(5):1195-1206.13. Centers for Disease Control and Prevention (CDC): Sexually Transmitted Diseases Treatment Guidelines.MMWR Recomm Rep 2006;55(RR-11):1-94 Available at: http://www.cdc.gov/std/treatment/default.htm.Accessed November, 2006.14. British Association for Sexual Health and HIV:<strong>Clinical</strong> Effectiveness Group. National Guideline For TheManagement Of Bacterial Vaginosis (2006). Available at:http://www.bashh.org/guidelines/2006/bv_final_0706.pdf, Assessed November 2006.15. Stevens DL, Bisno AL, Chambers HF, Everett ED, Dellinger P, Goldstein EJ, Gorbach SL, Hirschmann JV,Kaplan EL, Montoya JG, Wade JC; Infectious Diseases Society of America. Practice guidelines for thediagnosis and management of skin and soft-tissue infections. Clin Infect Dis. 2005;41:1373-1406.16. Bergstrom N, Bennett MA, Carlson CE, et al. <strong>Clinical</strong> Practice Guideline Number 15: Treatment of PressureUlcers. Rockville, Md: US Dept of Health and Human Services, Public Health Service, Agency for Health CarePolicy and Research; 1994. AHCPR publication 95-0652.17. International Society for Peritoneal Dialysis (ISPD). Peritoneal dialysis-related infections: recommendations:2005 update. Peritoneal Dialysis International 2005;25:107–131.18. Consensus Development Conference on Diabetic Foot Wound Care: 7-8 April 1999, Boston, Massachusetts.American Diabetes Association. Diabetes Care. 1999 Aug;22(8):1354-1360.19. Wickersham RM, Novak KK, managing eds. Drug Facts and Comparisons. St. Louis, Mo: Wolters KluwerHealth, Inc.; 2006.20. Micromedex ® Healthcare Series, (electronic version). Thomson Micromedex, Greenwood Village, Colorado,USA. Available at: http://www.thomsonhc.com. Accessed October, 2006.21. Cleocin [package insert]. Kalamazoo, MI: Pharmacia & Upjohn; August 2001.22. Clindesse ® [package insert]. St.Louis, MO: Ther-Rx Corporation; November 2004.23. Bactroban Nasal ® [package insert]. Research Triangle Park, NC: GlaxoSmithKline; July 2004.24. Bactroban Cream ® [package insert]. Research Triangle Park, NC: GlaxoSmithKline; September 2004.25. Bactroban Ointment ® [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2001.26. Neosporin G.U.Irrigant Sterile ® [package insert]. Greenville, NC: DSM Pharmaceuticals, Inc.; May 2003.27. MetroGel-Vaginal ® [package insert]. Northridge, CA: 3M Pharmaceuticals; 1997.28. Vandazole [package insert]. Minneapolis, MN: Upsher-Smith Laboratories; May 2005.29. Cortisporin ® Cream [package insert]. Bristol, TN: Monarch Pharmaceuticals, November 2003.30. Cortisporin ® Ointment [package insert]. Bristol, TN: Monarch Pharmaceuticals, September 2003.31. Tatro DS, ed. Drug Interaction Facts. St. Louis, MO: Wolters Kluwer Health, Inc.; 2006.32. Faro S, Skokos CK. The efficacy and safety of a single dose of Clindesse TM vaginal cream versus a seven-doseregimen of Cleocin® vaginal cream in patients with bacterial vaginosis. Infect Dis Obstet Gynecol.2005;13:155-160.33. McCormack WM, Covino JM, Thomason JL, et al. Comparison of clindamycin phosphate vaginal cream withtriple sulfonamide vaginal cream in the treatment of bacterial vaginosis. Sex Transm Dis. 2001;28:569-575.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.94
34. Paavonen J, Mangioni C, Martin M, et al. Vaginal clindamycin and oral metronidazole for bacterial vaginosis: arandomized trial. Obstet Gynecol 2000;96:256-260.35. Austin MN, Beigi RH, Meyn LA, et al. Microbiologic response to treatment of bacterial vaginosis with topicalclindamycin or metronidazole. J Clin Microbiol 2005;43(9):4492-4497.36. Ferris DG, Litaker MS, Woodward L, et al. Treatment of bacterial vaginosis: a comparison of oralmetronidazole, metronidazole vaginal gel, and clindamycin vaginal cream. J Fam Pract 1995;41(5):443-449.37. Fischbach F, Peterson EE, Weissenbacher ER, et al. Efficacy of clindamycin vaginal cream versus oralmetronidazole in the treatment of bacterial vaginosis. Obstet Gynecol 1993;82(3):405-410.38. Arredondo JL, Higuera F, Narcio L, et al. Clindamycin vaginal cream versus oral metronidazole in thetreatment of bacterial vaginosis. Arch AIDS Res. 1992;6(3):183-195.39. Andres FJ, Parker R, Hosein I, et al. Clindamycin vaginal cream versus oral metronidazole in the treatment ofbacterial vaginosis: a prospective double-blind clinical trial. South Med J 1992;85(11):1077-1080.40. Schmitt C, Sobel JD, Meriwether C. Bacterial vaginosis: treatment with clindamycin cream versus oralmetronidazole. Obstet Gynecol 1992;79:1020-1023.41. Higuera F, Hidalgo H, Sanches CJ, et al. Bacterial vaginosis: a comparative, double-blind study of clindamycinvaginal cream versus oral metronidazole. Curr Therap Res 1993;54:98-110.42. Perl TM, Cullen JJ, Wenzel RP, et al. Intranasal mupirocin to prevent postoperative Staphylococcus aureusinfections. N Engl J Med 2002; 346(24):1871-1877.43. Mody L, Kauffman CA, McNeil SA, et al. Mupirocin-based decolonization of Staphylococcus aureus carriers inresidents of 2 long-term care facilities: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis.2003;37:1467-1474.44. Wertheim HFL, Vos M, Ott A, et al. Mupirocin prophylaxis against Staphylococcus aureus infections innonsurgical patients. Ann Intern Med 2003; 140:419-425.45. Harbarth S, Dharan S, Liassine N, et al. Randomized-controlled, double-blind trial to evaluate the efficacy ofmupirocin for eradicating carriage of methicillin-resistant Staphylococcus aureus Antimicrob AgentsChemother 1999;43(6):1412-1416.46. Soto N, Vaghjimal A, Stahl-Avicolli A, et al. Bacitracin versus mupirocin for Staphylococcus aureus nasalcolonization. Infect Control Hosp Epidemiol 1999;20:351-353.47. Loeb M, Main C, Walker-Dilks C, Eady A. Antimicrobial drugs for treating methicillin-resistantStaphylococcus aureus colonization. Cochrane Database of Systematic <strong>Review</strong>s 2003, Issue 4. Art. No.:CD003340. DOI: 10.1002/14651858.CD003340.48. Bernardini J, Bender F, Florio T, et al. Randomized, double-blind trial of antibiotic exit site cream forprevention of exit site infection in peritoneal dialysis for patients. J Am Soc Nephrol 2005;16:539-545.49. D’Amico R, Pifferi S, Leonetti C, et al. Effectiveness of antibiotic prophylaxis in critically ill adult patients:systemic review of randomized controlled trials. BMJ 1998;316:1275-1285.50. Rist T, Parish LC, Capin LR, et al. A comparison of the efficacy and safety of mupirocin cream and cephalexinin the treatment of secondary infected eczema. Clin Exp Dermatol 2002;27:14-20.51. Goldfarb J, Crenshaw D, O’Horo J, et al. Randomized clinical trial of topical mupirocin versus oralerythromycin for impetigo. Antimicrob Agents Chemother 1988:32(12):1780-1783.52. Dagan R, Bar-David Y. Double-blind study comparing erythromycin and mupirocin for treatment of impetigoin children: implications of a high prevalence of erythromycin-resistant Staphylococcus aureus strains.Antimicrob Agents Chemother 1992;36(2):287-290.53. Koning S, Verhagen AP, van Suijlekom-Smit LWA, Morris A, Butler CC, van der Wouden JC. Interventionsfor impetigo. Cochrane Database of Systematic <strong>Review</strong>s 2003, Issue 2. Art. No.: CD003261. DOI:10.1002/14651858.CD003261.pub2.54. Lok CE, Stanley KE, Hux JE, et al. Hemodialysis infection prevention with polysporin ointment. J Am SocNephrol 2003 Jan;14(1):169-79.55. Hood R, Shermock KM, Emerman C. A prospective, randomized pilot evaluation of topical triple antibioticversus mupirocin for the prevention of uncomplicated soft tissue wound infection. Am J Emerg Med 2004;22:1-3.56. Dire DJ, Coppola M, Dwyer DA, et al. Prospective evaluation of topical antibiotics for preventing infections inuncomplicated soft-tissue wounds repaired in the ED. Acad Emerg Med 1995 Jan;2(1):4-10.57. Leyden JL, Bartelt NM. Comparison of topical antibiotic ointments, a wound protectant, and antiseptics for thetreatment of human blister wounds contaminated with Staphyloccocus aureus. J Fam Pract 1987;24(6):601-604.58. Berger RS, Pappert AS, Van Zile PS, et al. A newly formulated topical triple-antibiotic ointment minimizesscarring. Cutis 2000; 65:401-404.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.95
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane AntiviralsAHFS Class 840406February 7, 2007I. OverviewBoth acyclovir and penciclovir are synthetic nucleoside analogs derived from guanine. These agents areactive against various Herpesviridae including herpes simplex virus types 1 and 2 (HSV-1 and HSV-2). 1The two most common cutaneous manifestations of the herpes simplex virus infection are orolabial andgenital herpes. Orolabial herpes, which presents most commonly as cold sores, is the most prevalent formof mucocutaneous herpes infection, with 35%-60% of Caucasians in the United States showing serologicevidence of having been infected by HSV-1. 2 The incidence varies among regions and countries dependingon hygiene and socioeconomic conditions, with the highest incidence of first infection occurring between 6months and 3 years of age. 3Genital herpes, although one of the most common viral sexually transmitted diseases (STD) in the world,has shown a decrease over the past few years. Between the periods 1988-1994 and 1999-2000, the overallprevalence of HSV-2, the most common cause of genital herpes, declined 17%, from 21.3% of males andfemales infected with the virus to 17.6%. The prevalence in men declined most dramatically, from 17.3%to 11.2%, for a 35% decrease. 4 Most people infected with HSV-2 have not been diagnosed. Many suchpersons have mild or unrecognized infections but shed virus intermittently in the genital tract. Afterresolution of primary infection, the virus persists in the nerve roots of the sacral plexus, causing recurrent(often less severe) outbreaks.Before the introduction of acyclovir as an antiviral drug in the early 1980s, cutaneous HSV infection wasmanaged with drying agents and other local care. Today, treatment options include multiple oral,intravenous, and topical antiviral agents. Oral treatments are effective in reducing symptoms, whileintravenous administration may be required in immunocompromised patients and those with severedisseminated infection. 2 Topical antivirals reduce the duration of viral shedding and the length of timebefore all lesions become crusted, but this treatment is much less effective than oral or intravenoustherapies. No antiviral agent currently available will eradicate HSV, and thus treatment is aimed atmanaging rather than curing the disease.Table 1 lists the skin and mucous membrane antivirals included in this review. There are no genericalternatives available for the topical antiviral agents. This review encompasses all (topical) dosage formsand strengths.Table 1. Skin and Mucous Membrane Antivirals Included in this <strong>Review</strong>Generic Formulation(s) Example Brand Name(s) Current PDL Agent(s)Name(s)acyclovir cream, ointment Zovirax ® Zovirax ®penciclovir cream Denavir ® noneNo generic products are available in this class.II.Evidence-Based Medicine and Current Treatment GuidelinesThe following are summaries from national and international guidelines on the treatment of herpes andherpes lesions.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.96
Table 2. Treatment Guidelines Using the Skin and Mucous Membrane Antivirals<strong>Clinical</strong> GuidelineRecommendation(s)Centers for Disease Control andPrevention (CDC) Morbidity andMortality Weekly Report(MMWR): Sexually TransmittedDiseases Treatment Guidelines,2006 5 ••The use of systemic antivirals including valacyclovir,acyclovir, and famciclovir is encouraged for the treatmentof primary and recurrent genital herpes.Systemic antiviral drugs partially control the symptomsand signs of herpes infection when used to treat firstclinical episodes and recurrent episodes, or when used asdaily suppressive therapy.• For recurrent and suppressive therapy, oral valacyclovir,acyclovir, and famciclovir are recommended.• Topical therapy with antiviral drugs offers minimalclinical benefit, and their use is not recommended.The World Health Organization(WHO): Guidelines for theManagement of SexuallyTransmitted Infections 2003 6 • Treatment of herpes simplex virus can be expected toreduce the formation of new lesions, the duration of pain,the time required for healing and viral shedding.• Daily suppressive therapy reduces the frequency ofgenital herpes recurrences by more than 75% amongpatients who have frequent recurrences (6 or morerecurrences per year).• Suppressive treatment with acyclovir reduces, but doesnot eliminate asymptomatic viral shedding.• For recurrent and suppressive therapy oral valacyclovir,acyclovir, and famciclovir are recommended• Topical therapy with acyclovir produces only minimalshortening of the duration of symptomatic episodes and isnot recommended.• In pregnancy, oral acyclovir is recommended.American College ofObstetricians and Gynecologists:ACOG Practice Bulletin:<strong>Clinical</strong> ManagementGuidelines for Obstetrician-Gynecologists. GynecologicHerpes Simplex VirusInfections 7 •••Acyclovir, valacyclovir, and famciclovir are antiviraldrugs approved for treatment of genital herpes.Comparative trials of these medications suggest theyhave compatible clinical efficacy and result incomparable decrease in viral shedding.Treatment should be offered for first episode, even if theyappear to be mild initially.• Treatment decreases lesions, viral shedding, andsymptoms but does not effect the long-term naturalhistory of infection.• Oral therapy is recommended, except in severe cases inwhich a woman is unable to tolerate oral intake or hasprominent neurologic involvement.• Intravenous acyclovir should be used for severe cases.• Topical antiviral medication is not effective therapy anddoes not add to the benefit of the oral medication; its useis discouraged.III.IndicationsFood and Drug Administration (FDA)-approved indications for the skin and mucous membrane antiviralsare noted in Table 3.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.97
Table 3. FDA-Approved Indications for the Skin and Mucous Membrane Antivirals 8-10Drug(s)Management ofInitial HerpesGenitalisTreatment ofRecurrent HerpesLabialisManagement of Non-Life-ThreateningMucocutaneous Herpes Simplex VirusInfections in ImmunocompromisedPatientsAcyclovir creamaAcyclovir ointment aPenciclovir creamaaIV.PharmacokineticsThe pharmacokinetic parameters for the skin and mucous membrane antivirals are summarized in Table 4.Table 4. Pharmacokinetic Parameters of the Skin and Mucous Membrane Antivirals 8-10Drug (s) Systemic Absorption Distribution Excretion (Renal)Acyclovir cream Minimal Not determined 0.04% of daily doseAcyclovir ointment Minimal Not determined
Adverse Event(s) Acyclovir Cream Acyclovir Ointment Penciclovir CreamUrticaria - -OtheraDecreased therapeutic response - - aOral/pharyngeal edema - - aPain - - aParosmia - - aTaste perversion - -
VIII. Effectiveness<strong>Clinical</strong> studies evaluating the safety and efficacy of the skin and mucous membrane antivirals are summarized in Table 7.Table 7. Comparative <strong>Clinical</strong> Trials Using the Skin and Mucous Membrane AntiviralsStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsHerpes GenitalisLuby et al. 12Acyclovir 5% ointment,applied after anoccurrence of aprodrome; 6 times a dayat 3 hour intervalsvs.placebo, applied afteran occurrence of aprodrome; 6 times a dayat 3 hour intervalsReichman et al. 13Acyclovir 5% ointmentapplied 6 times a day at3 hour intervalsvs.placebo applied 6 timesa day at 3 hour intervalsRCT, MC, PCMale and femalepatients with recurrentgenital herpes whoexperienced a prodromemore than 75% of thetime before occurrenceof actual lesionsRCT, DB, PCMale and femalepatients with cultureprovenrecurrent herpessimplex genitalis;patients entered studywithin 48 hours of theonset of lesionsN=3095 daysN=885 daysPrimary:Duration of viralexcretionSecondary:Duration ofulceration/crustingof genital lesions,healing time oflesions, andduration of painand itchingPrimary:Duration of virusshedding, time tocrusting of lesions,time required forlesions to heal,time to cessation ofpainSecondary:Not reportedResultsPrimary:In female patients, the duration of viral excretion was less in theacyclovir group compared to placebo (1.1 days vs. 2 days;P=0.04). In male patients, there was no difference between theacyclovir and placebo groups (1.8 days; No P value reported).Secondary:There was no difference between placebo and acyclovir inulceration and/or crusting time for male patients who had genitallesions present at the initial clinic visit (2.2 days).The mean duration of pain and itching in males treated withacyclovir compared to placebo was 3.7 days and 3.8 days,respectively. The mean duration of pain and itching in femalestreated with acyclovir compared to placebo was 5.4 days and 4.4days, respectively (no P values were reported for males orfemales).Primary:The duration of virus shedding from lesions present at time ofstudy entry was significantly reduced for men who receivedacyclovir compared to placebo (2 days vs. 3.2 days; P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsCorey et al. 14Acyclovir 5% ointmentapplied 4 or 6 times adayvs.placebo applied 4 or 6times a dayRCT, DB, PCPatients with initial orrecurrent episodes ofgenital herpesN=18021 daysPrimary:Mean duration ofviral sheddingfrom genitallesions, meanduration of localpain or itching,mean time tohealing of lesionsSecondary:Not reportedSecondary:Not reportedPrimary:Among acyclovir recipients with first episodes of genital herpes,the mean duration of viral shedding from genital lesions (2.0 daysvs. 4.6 days), mean duration of local pain or itching (3.6 days vs.6.7 days), and the mean time to healing of lesions (11.2 days vs.15.8 days) were less than placebo (P
StudyandDrug Regimentimes a day for 7 daysin combination withacyclovir 200 mgtablets taken 4 times adayStudy DesignandDemographicspresented within 6 daysof onset of symptoms offirst episode genitalherpesSample Sizeand StudyDurationEnd Pointstime to healing oflesionsSecondary:Not reportedResultsvs. 1.7 days, P value not reported). The mean duration of viralshedding for women in the acyclovir cream group compared toplacebo was also not statistically significant (external lesions: 2.6days vs. 2.8 days, P value not reported; cervix: 1.7 days vs. 1.8days, P value not reported).vs.placebo appliedtopically 5 times a dayfor 7 days incombination withacyclovir 200 mgtablets taken 4 times adayThe duration of symptoms of pain, dysuria, and discharge showedno statistical significance between treatment groups (P value notreported).There was a decrease in the duration of itching with acyclovircream compared to placebo (1.2 days vs. 2.2 days; P=0.08).The mean duration of time to healing of lesions was notsignificantly different (P value not reported).Chen et al. 17Penciclovir 1% creamapplied topically 5times a dayvs.acyclovir 3% creamapplied topically 5times a dayRCT, DB, MC, PGPatients aged 18-65years with clinicaldiagnosis of genitalherpes, treatmentinitiated within 24 hoursof onset of the first signof lesionsN=2057 daysPrimary:Time to healing,resolution of allsymptoms, absenceof blisters,cessation of newblisters, crusting,and loss of crustSecondary:Not reportedSecondary:Not reportedPrimary:A decrease in crusting time was noted in patients with primaryfirst episodes of genital herpes with penciclovir compared toacyclovir (2.0 days vs. 3.0 days; P=0.03).The acyclovir group compared to the penciclovir group had alonger time to healing, absence of blisters, cessation of newblisters, and loss of crust. None of these differences were found tobe statistically significant.A comparison of clinical efficacy in terms of cure rate at day 7indicated that there was no difference between penciclovir andacyclovir treatment (86/104 vs. 80/101; P=0.53).Herpes LabialisSpruance et al. 18 RCT, DB, PC, MC N=1,385 Primary:Clinician-assessedSecondary:Not reportedPrimary:The mean clinician-assessed duration of herpes labialis episodePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.102
StudyandDrug RegimenAcyclovir 5% creaminitiated within 1 hourof first sign ofsymptoms and applied 5times dailyvs.placebo cream initiatedwithin 1 hour of firstsign of symptoms andapplied 5 times a dailyStudy DesignandDemographicsTwo identical studiesconducted in 45 centersin the United StatesHealthy adult patients 18years of age and olderwith a clinical history ofrecurrent herpes labialis(at least 3 episodes inthe past year)Sample Size End Pointsand StudyDuration4 days duration of herpeslabialis episodeSecondary:Patient-assessedduration of pain,proportion ofpatients developingclassical lesions(ulcers, vesicles,and crust)Resultswas significantly shorter for the patients treated with acyclovir(ACV) cream versus patients treated with placebo cream in eachof the two clinical trials (study 1: P=0.007; study 2: P=0.006).In study 1, the mean duration of herpes labialis episodes forpatients with a known duration was 4.3 days in the ACV groupcompared to 4.8 days for the placebo group (P=0.010). In study 2,the durations of herpes labialis episodes for patients with a knownduration was 4.6 days in the ACV group compared to 5.2 days forthe placebo group (P=0.007).Secondary:The mean patient-assessed duration of pain was significantlyshorter for patients in the ACV group compared to placebo in bothstudies (study 1: P=0.017; study 2: P=0.014).Gibson et al. 19Acyclovir 5% cream,applied 4 times a dayvs.placebo applied 4 timesa dayRCT, DB, PCPatients aged 16 yearsand older with 6 or morerecurrences of herpeslabialis per yearN=2332 weeks (16weeks ofacyclovirapplicationand 16 weeksof placebo)Primary:Number ofrecurrent sores,number of dayswith sores present,and number ofdays withsigns/symptoms ofdisease presentSecondary:Not reportedIn study 1, the mean duration of pain was 2.9 days for patients inthe ACV group compared to 3.2 days in the placebo group(P=0.024). In study 2, the mean duration of pain was 3.1 days forpatients in the ACV group compared to 3.5 days for patients in theplacebo group (P=0.027).Primary:There was a significant difference in favor of the acyclovir groupin mean number of doctor-confirmed recurrent sores (0.5 vs. 1.1,P
StudyandDrug RegimenRaborn et al. 20Acyclovir 5% creamapplied topically 4times a day at 4 hourintervalsvs.placebo appliedtopically 4 times a dayat 4 hour intervalsStudy DesignandDemographicsRCT, DB, MC, PCPatients 18 years orolder who hadexperienced more thanthree episodes of suninducedherpes labialiswithin the past year, firstapplication was to beapplied twelve hoursbefore intensive sunexposureSample Sizeand StudyDurationN=1918 daysEnd PointsPrimary:Number of lesionsformed duringtreatment, numberof lesions formedduring follow-upSecondary:Not reportedResultsPrimary:The difference in the number of patients who had lesions formduring treatment was not statistically significant in the acyclovirgroup compared to placebo (15/91 vs. 23/90; P=0.20).During the four day follow-up period, a smaller percentage ofpatients with lesion formation were found in the acyclovir groupcompared to the placebo group (21% vs. 40%; P
StudyandDrug Regimenplacebo, appliedtopically 4 times a dayfor 5 daysStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsSecondary:Not reportedonset.ResultsThe acyclovir group had a mean number of episodes per month of0.38 compared with 0.45 in the placebo group (P=0.22).Raborn et al. 23Penciclovir 1% creaminitiated within 1 hourof first sign ofsymptoms and applied 6times on day 1 thenevery two hours whileawakevs.placebo initiated within1 hour of first sign ofsymptoms and applied 6times on day 1 thenevery two hours whileawakeRCT, DB, PC, MC, PG,PROMale and femalepatients 18 years of ageand older, with a historyof recurrent herpessimplex labialis, whohad 3 or more episodesper year that typicallymanifested as classicallesionsN=4,5734 daysPrimary:Healing ofclassical lesionsSecondary:Resolution oflesion pain andduration of viralsheddingSecondary:Not reportedPrimary:Lesion healing occurred significantly faster in the penciclovirgroup (4.9 days) than in the placebo group (5.5 days; P=0.0001).The percentage of cases healed by day 6 was significantly greaterin the penciclovir group (70%) than in the placebo group (59%;P=0.001).The percentage of cases healed by day 8 was significantly greaterin the penciclovir group (85%) than in the placebo group (78%) asdetermined by the investigator (P=0.012). A similar finding wasreported by the patient at day 8 with the penciclovir group at 84%and the placebo group at 76% (P=0.002).Secondary:Resolution of lesion pain (days) was significantly differentbetween the penciclovir group and the placebo group (3.5 days vs.4.2 days; P=0.0001).There was a significant difference in healing in favor ofpenciclovir over placebo for early (P=0.001), late (P=0.0001) andvesicle (P=0.0115) stages.Boon et al. 24Penciclovir 1% creaminitiated within 1 hourRCT, DB, PC, PGPatients between theages of 18 and 81 yearsN=5414 daysPrimary:Clinician-recordedtime to lesionhealing andLoss of lesion pain also showed a significant difference in favor ofthe penciclovir group relative to the placebo group for early(P=0.0004), late (P=0.0001) and vesicle (P=0.0023) stages.Primary:Penciclovir was significantly more effective than placebo indecreasing the time to lesion healing (P
StudyandDrug Regimenof first sign ofsymptoms and appliedevery two hours whileawakevs.placebo initiated within1 hour of first sign ofsymptoms and appliedevery two hours whileawakeSpruance et al. 25Penciclovir 1% creamapplied every two hourswhile awakevs.placebo applied everytwo hours while awakeStudy DesignandDemographicswith a history of suninducedherpes labialis,at least 3 recurrences ayearRCT, DB, PC, PG, PRO,MCHealthy patients with ahistory of frequentepisodes of herpeslabialis, treatment wasself initiated by thepatient within 1 hour ofthe first sign orsymptoms of recurrenceSample Sizeand StudyDurationN=1,5734 daysEnd PointsseveritySecondary:Patient-recordedtime of healing andseverity of pain aswell as other lesionsymptomsPrimary:Lesion healing,proportion ofpatients who losttheir lesions bydays 6-8Secondary:Time to loss oflesion painResultslesions demonstrated a reduction of 2 days in median healing timecompared to the placebo group (P
StudyandDrug RegimenFemiano et al. 26Penciclovir 1% creamapplied every two hourswhile awake at onset ofprodrome phase or atappearance of vesiclesvs.acyclovir 5% creamapplied every two hourswhile awake at onset ofprodrome phase or atappearance of vesiclesLin et al. 27Penciclovir 1% creamapplied up to 5 times adayvs.acyclovir 3% creamapplied up to 5 times adayStudy DesignandDemographicsRCTIndividuals ranging from12 to 47 years who had ahistory of frequentepisodes of recurrentherpes labialis (at least 5each year)RCT, DB, MC, PGPatients 18-65 years ofage with clinicaldiagnosis of herpessimplex facialis/labialisSample Sizeand StudyDurationN=404 daysN=2487 daysEnd PointsPrimary:Clinicians’judgment of theappearance ofvesiculation tocrusting andpatients’experience of painSecondary:Not reportedPrimary:Time to healing,resolution of allsymptoms, absenceof blisters,cessation of newblisters, crustingand loss of crustSecondary:Not reportedResultsPrimary:In the prodromal acyclovir group, labial lesions reached a crustingstage by 6 days, with pain ceasing at day 5. In the prodromalpenciclovir group, both phases were reached earlier; the crustingphase was reached and pain ceased by day 4, a difference that wassignificant (P=0.002041).In the disease therapy (appearance of vesicles) group, theacyclovir patients’ clinical evolution and symptomology weresimilar to those seen in the absence of any therapy. Thepenciclovir patients, however, benefited from a reduction of 30%in the time to lesional crusting and a 20% reduction of theduration of pain compared to baseline and acyclovir (P
StudyandDrug RegimenAcyclovir 5% ointmentapplied topically 6times a dayvs.placebo appliedtopically 6 times a dayStudy DesignandDemographicsImmunocompromisedpatients with diagnosedherpes simplex virusregardless of typeSample Size End Pointsand StudyDuration28 days resolution of pain,total lesion healingSecondary:Not reportedResultsclearance of virus (P=0.0006), resolution of pain (P=0.004), andtotal healing (P=0.038). Median differences between groupsaveraged 6 days for each of these parameters.Secondary:Not reportedStudy abbreviations: AC=active-controlled, CI=confidence interval, DB=double-blind, DD=double-dummy, ES=extension study, HR=hazard ratio, MA=meta-analysis, MC=multicenter, OL=open-label,OR=odds ration, OS=observational study, PC=placebo-controlled, PG=parallel-group, PM=post marketing, PRO=prospective, RCT=randomized controlled trial, RETRO=retrospective, RR=rate ratio,SB=single-blind, TB=triple-blind, XO=crossoverPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.108
Additional EvidenceDose Simplification:A search of Medline and Ovid did not reveal data pertinent to this topic.Stable Therapy:A search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician Visits:A search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 8. Relative Cost of the Skin and Mucous Membrane AntiviralsGeneric Name(s) Formulation(s) Example BrandName(s)BrandCostGenericCostacyclovir cream, ointment Zovirax ® $$$ N/Apenciclovir cream Denavir ® $$ N/ANo generic products are available in this class.N/A=not availableX. ConclusionsAcyclovir and penciclovir are approved for the treatment of oral and/or genital herpes simplex infectionsand have been shown to be efficacious when compared to placebo. 8-10,12-24 These agents have been shownto be safe with no significant drug interactions and limited adverse events. 8-11 Most national andinternational guidelines on the treatment of herpes simplex infections, including those published by theCenters for Disease Control and Prevention, report that the topical antiviral agents offer minimal clinicalbenefit and should not be recommended over other options in general use, such as the oral agents. 5-7However, no studies have been conducted that directly compare oral and topical formulations for thetreatment of genital or orolabial herpes. There are no generic formulations of the topical antivirals, but ageneric formulation of an oral antiviral is available.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.109
Studies comparing the efficacy of these agents for the treatment of oral and/or genital herpes simplex havebeen conducted. Chen et al. demonstrated that there was no significant difference between the penciclovirand acyclovir treatment groups in genital herpes cure rate. 17 In a comparison trial in the treatment ofherpes labialis, penciclovir cream resulted in a quicker time to crusting and cessation of pain compared toacyclovir, however there was no significant difference in time to healing. 26 Lin et al also comparedpenciclovir and acyclovir in the treatment of herpes labialis, and found that there was no significantdifference in clinical cure rates and time to healing. 27Therefore, since the skin and mucous membrane antivirals offer minimal clinical benefit, are notrecommended over other options in general use, such as oral agents, by national and internationalguidelines, it is advisable that these agents be managed through the existing medical justification portion ofthe prior-authorization process.XI.RecommendationsNo brand skin and mucous membrane antiviral is recommended for preferred status. Alabama Medicaidshould accept cost proposals from manufacturers to determine cost effective products and possiblydesignate one or more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.110
References1. McEvoy GK, ed. AHFS Drug Information 2006: Antivirals 8:18, Nucleosides and Nucleotides 8:18.32[monograph on the Internet]. Bethesda, MD: American Society of Health-System Pharmacists. Available at:http://online.statref.com/Document/Document.aspx?DocID=183&StartDoc=183&EndDoc=191&FxID=1&offset=7. Accessed September, 2006.2. Emmert DH. Treatment of common cutaneous herpes simplex virus infections. Am Fam Phy 2000;61(6):1697-1706, 1708.. Available at: www.aafp.org . Accessed September, 2006.3. Simon, M. Who gets herpes? The University of Maryland Medical Center, Medical Reference, PatientEducation. Available at:http://www.umm.edu/patiented/articles/who_gets_herpes_simplex_virus_000052_4.htm. Accessed September,2006.4. Xu F, Sternberg MR, Kottiri BJ, et al. Trends in herpes simplex virus type 1 and type 2 seroprevalence in theUnited States. JAMA. 2006;296:964-973.5. Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2006.MMWR 2006;55(No. RR-11):1-100. Available at: http://www.cdc.gov/std/treatment/default.htm. AccessedSeptember, 2006.6. The World Health Organization (WHO): Guidelines for the management of sexually transmitted infections,revised version – 2003. Available at: http://www.who.int/reproductivehealth/publications/rhr_01_10_mngt_stis/index.html.Accessed September, 2006.7. American College of Obstetricians and Gynecologists. ACOG practice bulletin: clinical management guidelinesfor obstetrician-gynecologists. Gynecologic herpes simplex virus infections. Obstet Gynecol.2004;104(5):1111-1117.8. Zovirax ® Cream [package insert]. Bridgewater, NJ: GlaxoSmithKline; January 2004.9. Zovirax ® Ointment [package insert]. Bridgewater, NJ: GlaxoSmithKline; January 2004.10. Denavir ® [package insert]. Parsippany, NJ: Novartis; October 2003. Raborn WG, Martel AY.11. Tatro DS, ed. Drug Interaction Facts. St. Louis, Mo: Wolters Kluwer Health, Inc.; 2006.12. Luby JP, Gnann JW Jr, Alexander WJ, et al. A collaborative study of patient-initiated treatment of recurrentgenital herpes with topical acyclovir or placebo. J Infect Dis. 1984;150:1-6.13. Reichman RC, Badger GJ, Guinan ME, et al. Topically administered acyclovir in the treatment of recurrentherpes simplex genitalis: a controlled trial. J Infect Dis. 1983;147(2):336-340.14. Corey L, Benedetti JK, Critchlow CW, et al. Double-blind controlled trial of topical acyclovir in genital herpessimplex virus infections. Am J Med. 1982;73(1A):326-334.15. Kinghorn GR, Turner EB, Barton IG, et al. Efficacy of topical acyclovir cream in first and recurrent episodes ofgenital herpes. Antiviral Res. 1983;3:291-301.16. Kinghorn GR, Abeywickreme I, Jeavons M, et al. Efficacy of combined treatment with oral and topicalacyclovir in first episode genital herpes. Genitourin Med. 1986;186-188.17. Chen XS, Han GZ, Guo ZP, et al. A comparison of topical application of penciclovir 1% cream with acyclovir3% cream for treatment of genital herpes: a randomized, double-blind, multicenter trial. Int J STD AIDS.2000;11:568-573.18. Spruance SL, Nett R, Marbury T, et al. Acyclovir cream for treatment of herpes simplex labialis: results of tworandomized, double-blind, vehicle-controlled, multicenter clinical trials. Antimicrob Agents Chemother.2002;46(7):2238-2243.19. Gibson JR, Klaber MR, Harvey SG, et al. Prophylaxis against herpes labialis with acyclovir cream—a placebocontrolledstudy. Dermatologica. 1986;172:104-107.20. Raborn GW, Martel AY, Grace MG, et al. Herpes labialis in skiers: randomized clinical trial of acyclovir creamversus placebo. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:641-645.21. Shaw M, King M, Best JM, et al. Failure of acyclovir cream in treatment of recurrent herpes labialis. Br Med J.1985;291:7-9.22. Spruance SL, Crumpacker CS, Schnipper LE, et al. Early, patient-initiated treatment of herpes labialis withtopical 10% acyclovir. Antimicrob Agents Chemotherapy. 1984;25:553-555.23. Raborn GW, Martel AY, Lassonde M, et al, for the Worldwide Topical Penciclovir Collaborative Study Group.Effective treatment of herpes simplex labialis with penciclovir combined results of two trials. J Am Dent Assoc.2002;133:303-309.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.111
24. Boon R, Goodman JJ, Martinez J, et al. Penciclovir cream for the treatment of sunlight-induced herpes simplexlabialis: a randomized, double-blind, placebo-controlled trial. Clin Ther. 2000;22(1):76-90.25. Spruance SL, Rea TL, Thoming C, et al. Penciclovir cream for the treatment of herpes simplex labialis. Arandomized, multicenter, double-blind, placebo-controlled trial. JAMA. 1997;277(17):1374-9.26. Femiano F, Gombos F, Scully C, et al. Recurrent herpes labialis: efficacy of topical therapy with penciclovircompared with acyclovir (aciclovir). Oral Dis. 2001;7:31-33.27. Lin L, Chen XS, Cui PG, et al. Topical application of penciclovir cream for the treatment of herpes simplexfacialis/labialis: a randomized, double blind, multicenter, acyclovir-controlled trial. J Dermatolog Treat.2002;13:67-72.28. Whitley RJ, Levin M, Barton N, et al. Infections caused by herpes simplex virus in the immunocompromisedhost: natural history and topical acyclovir therapy. J Infect Dis. 1984;150(3):323-329.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.112
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane AntifungalsSingle Entity AgentsAHFS Class 840408February 7, 2007I. OverviewThe skin and mucous membrane antifungals are available in multiple dosage forms and are indicated for anumber of fungal infections and related conditions. In general, these agents are Food and DrugAdministration (FDA)-approved for the treatment and/or prophylaxis of the following conditions:cutaneous candidiasis (including onychomycosis and diaper rash), oropharyngeal candidiasis, vulvovaginalcandidiasis, seborrheic dermatitis or dandruff, tinea corporis, tinea cruris, tinea pedis, and tineaversicolor. 1,2 The antifungals may be further classified into the following categories based upon theirchemical structures: allylamines (naftifine, terbinafine), azoles (butoconazole, clotrimazole, econazole,ketoconazole, miconazole, oxiconazole, sertaconazole, sulconazole, terconazole, tioconazole),benzylamines (butenafine), hydroxypyridones (ciclopirox), polyenes (amphotericin B, nystatin),thiocarbamates (tolnaftate), and miscellaneous (undecylenic acid). 1,2 Ciclopirox, clotrimazole, econazole,ketoconazole, nystatin and terconazole are available generically in numerous dosage forms. Clotrimazole,miconazole, terbinafine, tioconazole and tolnaftate are available over-the-counter in at least one dosageform.Classified as fungicidals or fungistatics, most of these skin and mucous membrane antifungals share similarmechanisms of action. They primarily block the enzyme responsible for breaking down sterol precursors,thereby inhibiting the formation of key cell membrane components (e.g., ergosterol) of the fungus. Thisaction compromises the integrity of the cell membrane leading to growth inhibition and/or cell death. 1,2Mycological and clinical cure is often achieved with topical therapy alone.The single entity skin and mucous antifungals that are included in this review are listed in Table 1. Thisreview encompasses all (topical) dosage forms and strengths.Table 1. Single Entity Skin and Mucous Membrane Antifungals Included in this <strong>Review</strong>GenericName(s)Formulation(s) Example Brand Name(s) Current PDLAgent(s)butenafine cream Mentax ® nonebutoconazole vaginal cream Gynazole-1 ® noneciclopirox cream, gel, Loprox ® *, Penlac ®ciclopiroxshampoo, solution,suspensionclotrimazole‡ cream, solution, Clotrim Antifungal ® *, Cruex ® *, Desenex ® *, clotrimazoletroche, vaginalcream, vaginaltabletFemcare ® *, Gyne-Lotrimin ® *, Mycelex ® *econazole cream Spectazole ® * econazoleketoconazole cream, gel, Nizoral ® *, Xolegel ®ketoconazolemiconazole‡shampoocream, vaginalcombinationpackage, vaginalcream, vaginalBaza Antifungal ® *, Carrington Antifungal ® *,Micaderm ® *, Micatin ® *, Micro-Guard ® *,Mitrazol ® *Monistat 1 Combo Pack ® , Monistat3 ® *, Monistat 7 ® *, Monistat-Derm ® *, NeosporinPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.113miconazole
GenericName(s)Formulation(s) Example Brand Name(s) Current PDLAgent(s)suppository AF ® *naftifine cream, gel Naftin ® nonenystatin cream, ointment, Mycostatin ® *nystatinpowder, vaginaltabletoxiconazole cream, lotion Oxistat ® nonesertaconazole cream Ertaczo ® nonesulconazole cream, solution Exelderm ® noneterbinafine‡ cream, spray Lamisil ® , Lamisil AT ® noneterconazole vaginal cream, Terazol 3 ® *, Terazol 7 ® *terconazolevaginal suppositorytioconazole‡ vaginal ointment Monistat 1 ® *, Vagistat-1 ® * tioconazoletolnaftate‡ cream Tinactin ® *† tolnaftate*Generic is available in at least one dosage form or strength.†Brand is no longer available.‡Over-the-counter product is available in at least one dosage form or strength.II.Evidence-Based Medicine and Current Treatment GuidelinesCurrent national and international treatment guidelines that incorporate the single entity skin and mucousmembrane antifungals are summarized in Table 2.Table 2. Treatment Guidelines Using the Single Entity Skin and Mucous Membrane Antifungals<strong>Clinical</strong> GuidelineRecommendation(s)Infectious Diseases Society ofAmerica (IDSA): PracticeGuidelines for the Diagnosisand Management of Skin andSoft-Tissue Infections 4 ••Immunocompromised patients are more susceptible toopportunistic fungal infections.Noninvasive fungal infections may be treated with skin careand a topical antifungal agent; alternatively, a short coursesystemic azole antifungal agent may be used.• Oral and intravenous (IV) agents (e.g., amphotericin B,voriconazole, caspofungin, fluconazole, and itraconazole) areinitiated empirically in immunocompromised patientspresenting with neutropenia; these agents may be used to treatinvasive fungal infections.• Note: oral amphotericin B is no longer commerciallyavailableAmerican Academy ofDermatology (AAD),Guidelines/Outcomes Committee:Guidelines of Care forSuperficial Mycotic Infectionsof the Skin: Tinea Corporis,Tinea Cruris, Tinea Faciei,Tinea Manuum, and TineaPedis 5 ••Topical antifungal agents are used in the treatment ofnoninflammatory tinea corporis, tinea cruris, tinea faciei, tineamanuum, and tinea pedis; systemic oral agents are used forother tinea conditions.Examples of topical antifungal agents include azoles (e.g.,clotrimazole, econazole, ketoconazole, miconazole,oxiconazole, and sulconazole), allylamines (e.g., naftifine andterbinafine), ciclopirox, miscellaneous agents (e.g., benzoicacid, tolnaftate, haloprogin, drying agents, powders, andsalicylic acid), and combination topical corticosteroidantifungal mixtures.• Examples of systemic antifungal agents include griseofulvin,American Academy ofDermatology (AAD),Guidelines/Outcomes Committee:ketoconazole, terbinafine, itraconazole, and fluconazole.• Topical antifungal agents are used in treatment of mild casesof tinea versicolor.• Systemic antifungal agents are used in the treatment of tineaPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.114
<strong>Clinical</strong> GuidelineGuidelines of Care forSuperficial Mycotic Infectionsof the Skin: Pityriasis (Tinea)Versicolor 6Infectious Diseases Society ofAmerica (IDSA): Guidelines forthe Treatment of Candidiasis 7Recommendation(s)versicolor in patients who have failed topical therapy, haverecurrent infections, or have extensive skin involvement.Concurrent therapy with topical antifungal agents isacceptable.• Examples of topical antifungal agents include azoles (e.g.,clotrimazole, econazole, ketoconazole, miconazole,oxiconazole, and sulconazole), ciclopirox, and miscellaneousagents (e.g., selenium sulfide, zinc pyrithione, sulfur, salicylicacid, propylene glycol, and benzoyl peroxide).• Examples of systemic antifungal agents include ketoconazole,itraconazole, and fluconazole.Candida Onychomycosis• Topical agents are not effective against cases ofonychomycosis caused by Candida species; both oralitraconazole and terbinafine are effective.Candidal Skin Infection• Topical azoles and polyenes are effective.Cutaneous Neonatal Candidiasis• Topical agents may be used for primary cutaneous disease inhealthy, normal-birth-weight, full-term infants.Genital Candidiasis• Examples of agents include over-the-counter (OTC)clotrimazole, OTC butoconazole, OTC miconazole, OTCtioconazole, OTC terconazole, nystatin, fluconazole, andboric acid.• For uncomplicated vaginitis, topical agents are effective whenused for 1 to 7 days; short-course oral therapy may be used.• For complicated vaginitis, topical agents should beadministered daily for greater than 7 days; alternatively, two150-mg doses of fluconazole given 72 hours apart may beused.• For recurrent vaginitis, a 2-week therapy of either oral ortopical azole should be initiated followed by 6 months of oneof the following agents: fluconazole 150 mg every week,ketoconazole 100 mg/day, itraconazole 100 mg every otherday, or daily treatment with a topical azole.• Boric acid 600 mg administered intravaginally for 14 days isalso effective.Oropharyngeal Candidiasis• Initial treatment options include topical azoles (clotrimazoletroches), oral azoles (fluconazole, itraconazole, ketoconazole),and oral polyenes (nystatin suspension).• Treatment options for refractory or recurrent infectionsinclude oral azoles suspensions (fluconazole, itraconazole,ketoconazole), or IV amphotericin B (for refractory cases).• Begin treatment with clotrimazole 10mg troches five timesdaily or nystatin 200,000 U to 400,000 U five times daily orfluconazole 100mg/day; therapy should be continued for 7 to14 days after clinical improvement.• Alternative agents include oral itraconazole, IV amphotericinPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.115
<strong>Clinical</strong> GuidelineRecommendation(s)or IV caspofungin.• In refractory cases, the following agents have demonstratedefficacy: fluconazole solution, itraconazole capsules(chewed), itraconazole solution, IV amphotericin B (last line).German Dermatological Society, • Acute vaginosis may be treated with a systemic (e.g., azoles)Society for Gynecology and • Patients who fail topical treatment should use boric acid (600Obstetrics: Guideline formg daily for 14 days) or systemic agents, such as itraconazoleVulvovaginal Candidosis 8 or fluconazole (up to 750 mg daily) depending on the speciesthe German Speakingor topical agent (e.g., polyenes, azoles, or ciclopirox).Mycological Society and the • Vulvar inflammation should be treated with an antifungalWorking Group for Infections and cream or ointment applied to affected area(s) once to twiceInfectimmunology of the German daily.of microorganism.• Chronic recurrent C. Albicans vaginitis should be treated with150 mg to 300 mg oral fluconazole weekly followed by amaintenance regimen of tapering fluconazole 150 mg every 2to 4 weeks.• Mycological cure rate for an acute C. Albicans infection usinga topical agent is 75% to 80%. Although therapeutic successis similar among agents, patient compliance is better with oralagents.Association of GenitourinaryMedicine and the Medical Societyfor the Study of Venereal Disease<strong>Clinical</strong> Effectiveness Group:National Guideline for theManagement of VulvovaginalCandidiasis 9 ••Mycological cure rate for acute vulvovaginal candidiasis innonpregnant women with topical and oral azole treatmentoptions is 80% to 95%; nystatin gives a 70% to 90% cure rate.Chronic recurrent candidosis are treated with inductiontherapy followed by a 6-month maintenance regimen.Grampian Evidence-Based • There is no difference in efficacy between oral and intravaginallyTreatment of Vulvovaginal • Intravaginally administered agents are associated with onlyCandidiasis (VVC) 10 local adverse effects while oral fluconazole has the most sideCommunity Pharmacy Guidelinesadministered antifungal agents.Group: Evidence-BasedGuidelines for Non-prescription• External-use-only antifungal cream should not be used asmonotherapy in vulvovaginal candidiasis.effects.• Clotrimazole may be used in lactating patients under medicalsupervision; avoid fluconazole and econazole.• Patients who are experiencing >2 episodes of vulvovaginalcandidiasis in 6 months should seek medical attention.• Patients with vulvovaginal candidiasis who are pregnantshould seek medical attention.Department of Health and HumanServices, Centers for DiseaseControl and Prevention (CDC):Treatment Guidelines forDiseases Characterized byVaginal Discharge 11Uncomplicated vulvovaginal candidiasis• Topical antifungal therapies used for 1 to 3 days arecorrelated with efficacy rates ranging from 80% to 90%.• Topical azole antifungal agents are more effective comparedto nystatin.• Examples of agents include butoconazole, clotrimazole,miconazole, nystatin, tioconazole, terconazole, andfluconazole.• Over-the-counter products are only recommended for patientswith a history of a previously diagnosed case of vulvovaginalcandidiasis.• Patients who are pregnant or immunocompromised should usePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.116
<strong>Clinical</strong> GuidelineRecommendation(s)at least 7 to 14 days of antifungal therapies; only antifungaltopical agents should be used in pregnancy.Complicated vulvovaginal candidiasis (> 4 episodes/year)• To promote remission, topical antifungal agents used for 7 to14 days, or two fluconazole 150 mg tablets given 72 hoursapart, should be used.• For maintenance, a 6-month therapy of an antifungal agentgiven once daily to once monthly, depending on the agent,should be used; examples include clotrimazole, ketoconazole,fluconazole, and itraconazole.Severe vulvovaginal candidiasis• Topical antifungal agents used for 7 to 14 days or twofluconazole 150 mg tablets given 72 hours apart should beused.Non-C. albicans vulvovaginal candidiasis• First-line therapy is a 7- to 14-day treatment course using anonfluconazole azole antifungal.• Boric acid 600 mg in a gelatin capsule once daily for 2 weeksis used in recurrent cases.• If the patient fails boric acid therapy, nystatin 100,000 unitsvaginal suppositories may be used.European Branch of the• Topical antifungal therapies used for 1 to 3 days areWorld Health Organization: • Examples of topical agents include clotrimazole andEuropean Guideline for the miconazole. The guideline mentions that a large number ofManagement of Vaginalother topical preparations exist without listing these agents.Discharge 12 • Examples of oral agents include fluconazole and itraconazole.International Union againstcorrelated with efficacy rates ranging from 80% to 90%.Sexually Transmitted Infectionand the European Office of the• There is no difference in efficacy between oral and intravaginallyadministered antifungal agents.• For recurring candidiasis, an initial induction therapy of oralfluconazole or topical clotrimazole followed by a 6-monthmaintenance therapy should be initiated.British Association ofDermatologists: Guidelines forTreatment of Onychomycosis 13 • Onychomycosis may be caused by fungi includingdermatophytes, nondermatophytes molds and yeast (Candidaspecies).• Fingernail infection cure rates range between 80% to 90%;toenail cure rates range between 70% to 80%.• Topical agents are not as efficacious as systemic therapy; oralterbinafine is more efficacious compared to oral itraconazole.• Combination therapy of topical and systemic antifungalagents leads to improved clinical and mycological cure rates.• Examples of topical agents include azoles, allylamines,polyenes, or a combination agent with an antifungal,antiseptic or keratolytic (e.g., benzoic acid).• Examples of oral agents include griseofulvin, terbinafine, anditraconazole; fluconazole and ketoconazole are not approvedfor use in onychomycosis.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.117
III.IndicationsFDA-approved indications for the single entity skin and mucous membrane antifungals are noted in Tables3 and 4.Table 3. FDA-Approved Indications for the Single Entity Skin and Mucous Membrane Antifungals—TineaInfections 1,2,14-39Drug(s)DermatophytosesTinea corporis Tinea cruris Tinea pedis Tinea versicolorButenafine (cream) a a a aButoconazole- - - -(vaginal cream)Ciclopirox(cream)a a a aCiclopirox (gel) a - a -Ciclopirox (shampoo) - - - -Ciclopirox (solution) - - - -Ciclopirox (suspension) a a a aClotrimazole (cream, solution) a a a aClotrimazole (troche) - - - -Clotrimazole (vaginal cream,vaginal suppository)- - - -Econazole (cream) a a a aKetoconazole (cream) a a a aKetoconazole (gel) - - - -Ketoconazole (shampoo) - - - aMiconazole (cream) a a a -Miconazole (vaginal suppository) - - - -Naftifine (cream, gel) a a a -Nystatin (cream, ointment, powder) - - - -Oxiconazole (cream) a a a aOxiconazole (lotion) a a a -Sertaconazole (cream) - - a -Sulconazole (cream) a a a aSulconazole (solution) a a a -Terbinafine (cream, spray) a a a -Terconazole (vaginal cream,vaginal suppository)- - - -Tioconazole (vaginal ointment) - - - -Tolnaftate a a a aPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.118
Table 4. FDA-Approved Indications for the Single Entity Skin and Mucous Membrane Antifungals—Candidiasis/Seborrheic Dermatitis 1,2,14-39Drug(s)CutaneousCandidiasisOropharyngealCandidiasisVulvovaginalCandidiasisSeborrheicDermatitis/DandruffButenafine (cream) - - - -Butoconazole ( vaginal cream) - - a -Ciclopirox (cream) - - - -Ciclopirox (gel) - - - aCiclopirox (shampoo) - - - aCiclopirox (solution) a‡ - - -Ciclopirox (suspension) a - - -Clotrimazole (cream, solution) a - - -Clotrimazole (troche) - a§ - -Clotrimazole (vaginal cream,vaginal suppository)- - a† -Econazole (cream) a - - -Ketoconazole (cream) a - - aKetoconazole (gel) - - - a- - - aKetoconazole(shampoo)Miconazole (cream) - - - -Miconazole (vaginal suppository) - - a† -Naftifine (cream, gel) - - - -Nystatin (cream, ointment, powder) a* - - -Oxiconazole (cream) - - - -Oxiconazole (lotion) - - - -Sertaconazole (cream) - - - -Sulconazole (cream, solution) a - - -Terbinafine (cream, spray) - - - -Terconazole (vaginal cream,vaginal suppository)- - a -Tioconazole (vaginal ointment) - - a -Tolnaftate - - - -* Includes candidal diaper dermatitis† Uncomplicated and complicated/recurrent‡ FDA approved for treatment of onychomycosis§ FDA approved for treatment and prophylactic usePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.119
IV.PharmacokineticsThe pharmacokinetic parameters for the single entity skin and mucous membrane antifungals aresummarized in Table 5.Table 5. Pharmacokinetic Parameters of the Single Entity Skin and Mucous Membrane Antifungals 1,2,14-39Drug(s)Systemic Distribution Excretion MetaboliteAbsorption(Renal)Butenafine (cream) Minimal PenetratesthroughtransepidermalandMinimalYes(Hydroxylation atterminal t-butyl sidechain)*transfollicularroutesButoconazole1.7% of dose No data 2.7% of dose No(vaginal cream)Ciclopirox (cream) 0.8%-1.6% of dose 94%-98%protein boundCiclopirox (gel) No data 94%-98%protein boundCiclopirox (shampoo) With continuous 29 94%-98%days of treatment, protein boundaverage serumconcentration was10.3 ng/mL–13.2ng/mLCiclopirox (solution)
Drug(s)Systemic Distribution Excretion MetaboliteAbsorption(Renal)Naftifine (cream) ~6% after a single No data 64% of dose NoapplicationNaftifine (gel)
VI.Adverse Drug EventsThe most common adverse drug events reported with the single entity skin and mucous membrane antifungals are noted in Table 6. Topical antifungalagents are not typically associated with systemic adverse effects. Imidazole-derivative azole antifungals may be associated with unpredictable crosssensitivityamong agents within this particular class.Table 6. Adverse Drug Events (%) Reported with the Single Entity Skin and Mucous Membrane Antifungals 1,2,14-39Adverse Event(s)Central Nervous SystemDizziness - - - - -
Adverse Event(s)Scalp pustules - - - - - 1 - - - - 5 - >10 - 1-10 - 1-10 1-10 - - aStevens-Johnson syndrome - - - - - - - - a - - - - - - -Tenderness - - - - - - - - - - 1-10 - - - - -Toxic epidermal necrolysis - - - - - - - - - - - - - - - -Vesiculation - - - - - - - - - - a - - - - -GastrointestinalAbdominal cramping - a - - - - a* - - - - - - 1-10 - -Abdominal pain - a - - - - - - - - - - - - a -Pelvic pain - a - - - - - - - - - - - - - -GenitourinaryDysmenorrhea - - - - - - - - - - - - - 1-10 - -Itching - a - - - - - - - - - - - - - -Penile discomfort* - - -
VII.Dosing and AdministrationThe usual dosing regimens for the single entity skin and mucous membrane antifungals are summarized inTable 7. The duration of therapy for a particular agent is dependent on the specific indication for which itis being used.Table 7. Usual Dosing for the Single Entity Skin and Mucous Membrane Antifungals 1,2,14-39Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityButenafine Interdigital tinea pedis:Cream: apply to affected area(s)twice daily for 7 days or once dailyfor 4 weeksFor children >12 years old: Cream: 1%ButoconazoleCiclopiroxTinea versicolor, tinea corporis,tinea pedis, tinea cruris:Cream: apply to affected area(s)once daily for 2 weeksVulvovaginal candidiasis:Cream: insert 1 applicatorfulvaginally once daily at bedtime for1 (Gynazole-1 ® ) or 3 (Femstate ® -3) consecutive daysCutaneous candidiasis:Suspension: gently massage intoaffected skin area(s) twice daily for4 weeksOnychomycosis:Solution: apply to affected nailplate(s) once dailySeborrheic dermatitis,Gel: gently massage into affectedskin area(s) twice daily for 4 weeksShampoo: initial, wet hair andapply 1 to 2 teaspoonsful to scalpfor 3 minutes then rinse;maintenance, repeat twice weeklyfor 4 weeks with a minimum of 3days between applicationsTinea cruris, tinea versicolor:Cream, suspension: gently massageinto affected skin area(s) twicedaily for 2 weeksTinea corporis, tinea pedis:Cream, gel, suspension: gentlymassage into affected skin area(s)twice daily for 4 weeksTinea corporis, tinea cruris,tinea versicolor: Cream:apply to affected area(s)once daily for 2 weeksTinea pedis:Cream: apply to affectedarea(s) twice daily for 7days or once daily for 4weeksSafety and efficacy inchildren have not beenestablishedFor children >16 years old:Seborrheic dermatitis:Gel: gently massage intoaffected skin area(s) twicedaily for 4 weeksShampoo: initial, wet hairand apply 1 to 2teaspoonsful to scalp for 3minutes then rinse;maintenance, repeat twiceweekly for 4 weeks with aminimum of 3 days betweenapplicationsTinea cruris, tineaversicolor:Cream, suspension: gentlymassage into affected skinarea(s) twice daily for 2weeksTinea corporis, tinea pedis:Cream, gel, suspension:gently massage into affectedskin area(s) twice daily for 4weeksVaginal cream:2%Cream: 0.77%*Gel: 0.77%Shampoo: 1%Solution: 8%Suspension:0.77%Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.124
Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityClotrimazole Cutaneous candidiasis:Cream, solution (Rx dosageforms): apply to affected area(s)twice daily for 4 weeksFor children >3 years old: Cream: 1%Solution: 1%Oropharyngeal candidiasis:Troche: initial treatment, dissolve1 troche in mouth five times dailyfor 2 weeks; maintenance(prophylaxis), dissolve 1 troche inmouth three times dailyTinea corporis, tinea pedis:Cream, solution (OTC dosageforms): apply to affected area(s)twice daily for 4 weeksTinea cruris:Cream, solution (OTC dosageforms): apply to affected area(s)twice daily for 2 weeksTinea versicolor:Cream, solution (Rx dosageforms): apply to affected area(s)twice daily for 4 weeksVulvovaginal candidiasis:Vaginal cream (1%): initial, insert1 applicatorful vaginally atbedtime for 7 to 14 daysVaginal cream (2%): insert 1applicatorful vaginally at bedtimefor 3 daysVaginal suppository (200 mg):insert 1 suppository vaginally atbedtime for 3 daysOropharyngeal candidiasis:Troche: dissolve 1 troche inmouth five times daily for 2weeksFor children >2 years old:Tinea corporis, tinea cruris,tinea pedis, tinea versicolor:Cream, solution (OTCdosage forms): apply toaffected area(s) twice dailyfor 2 to 4 weeksTroche: 10 mgVaginal cream:1%, 2%Vaginalsuppository:100 mg, 200 mg,500 mgEconazoleVaginal suppository (500 mg):insert 1 suppository vaginally atbedtime for 1 dayCutaneous candidiasis:Cream: apply to affected area(s)twice daily for 2 weeksSafety and efficacy inchildren have not beenestablishedCream: 1%Tinea corporis, tinea cruris, tineaversicolor:Cream: apply to affected area(s)once daily for 2 weeksTinea pedis:Cream: apply to affected area(s)once daily for 1 month125Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityKetoconazole Dandruff:Shampoo: initial, shampoo twiceweekly for 4 weeks with 3 daysbetween each application;maintenance, shampoointermittently as neededFor children > 12 years old:Dandruff:Shampoo (1%): shampootwice weekly for 4 weekswith 3 days between eachapplicationCream: 2%Shampoo:1%,2%Seborrheic dermatitis:Cream: apply to affected area(s)twice daily for 4 weeksGel: apply to affected area(s) oncedaily for 2 weeksTinea corporis, tinea cruris, tineaversicolor, cutaneous candidiasis:Cream: apply to affected area(s)once daily for 2 weeksMiconazoleNaftifineTinea pedis,Cream: apply to affected area(s)once daily for 6 weeksTinea corporis, tinea cruris (OTCand Rx dosage forms):Cream: apply to affected area(s)twice daily for 2 weeksTinea pedis (OTC and Rx dosageforms):Cream: apply to affected area(s)twice daily for 4 weeksPowder: spray or sprinkle overaffected area(s) twice daily for 4weeksVulvovaginal candidiasis: Vaginalsuppository (100 mg): insert 1suppository vaginally at bedtimefor 7 daysVaginal suppository (200 mg):insert 1 suppository vaginally atbedtime for 3 daysVaginal suppository (1200 mg):insert 1 suppository vaginally atbedtime for 1 dayTinea corporis, tinea cruris, tineapedis:Cream: apply to affected area(s)once daily for 4 weeksFor children > 2 years old:Tinea corporis, tinea cruris,tinea pedis (OTC and Rxdosage forms):Cream: apply to affectedarea(s) twice dailyFor children > 12 years old:Vulvovaginal candidiasis:Vaginal suppository (100mg): insert 1 suppositoryvaginally at bedtime for 7daysVaginal suppository (200mg): insert 1 suppositoryvaginally at bedtime for 3daysVaginal suppository (1200mg): insert 1 suppositoryvaginally at bedtime for 1daySafety and efficacy inchildren have not beenestablishedCream: 2%, 4%Powder: 2%Vaginalsuppository: 100mg, 200 mg,1200 mgCream: 1%Gel: 1%Gel: apply to affected area(s) twicedaily for 4 weeks126Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityNystatinCutaneous candidiasis:Cream, ointment, powder: apply toaffected area(s) two to three timesdaily until healing is completeCutaneous candidiasis:Cream, ointment, powder:apply to affected area(s) twoto three times daily untilCream:100,000 units/gOintment:healing is complete 100,000 units/gOxiconazoleSertaconazoleSulconazoleVulvovaginal candidiasis:Vaginal suppository: insert 1suppository vaginally once dailyfor 2 weeksTinea corporis, tinea cruris:Cream, lotion: apply to affectedarea(s) twice daily for 2 weeksTinea pedis:Cream, lotion: apply to affectedarea(s) twice daily for 4 weeksTinea versicolor:Cream: apply to affected area(s)once daily for 2 weeksTinea pedis:Cream: apply to affected area(s)twice daily for 4 weeksCutaneous candidiasis:Cream, solution: apply to affectedarea once or twice daily for 3 to 4weeksTinea corporis, tinea cruris, tineaversicolor:Cream, solution: apply to affectedarea(s) once or twice daily for atleast 3 weeksTinea corporis, tinea cruris:Cream, lotion: apply toaffected area(s) twice dailyfor 2 weekstinea pedis:Cream, lotion: apply toaffected area(s) twice dailyfor 4 weeksTinea versicolor:Cream: apply to affectedarea(s) once daily for 2weeksFor children > 12 years old:Tinea pedis:Cream: apply to affectedarea(s) twice daily for 4weeksSafety and efficacy inchildren have not beenestablishedPowder:100,000 units/gVaginalsuppository:100,000 unitsCream: 1%Lotion: 1%Cream: 2%Cream: 1%Solution: 1%TerbinafineTinea pedis:Cream: apply to affected area(s)twice daily for 4 weeksTinea corporis, tinea cruris, tineapedis:Cream, spray: apply to affectedarea(s) once or twice daily;maximum, apply up to 4 weeksFor children > 12 years old:Tinea corporis, tinea cruris:Cream: apply to affectedarea(s) once daily for 1weekCream: 1%Spray: 1%127Tinea pedis:Cream: apply to affectedarea(s) twice daily for 1Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityweekTerconazole Vulvovaginal candidiasis:Vaginal cream (0.4%): insert 1applicatorful at bedtime for 7 daysSafety and efficacy inchildren have not beenestablishedVaginal cream:0.4%, 0.8%Vaginal cream (0.8%): insert 1applicatorful at bedtime for 3 daysVaginalsuppository: 80mgTioconazoleTolnaftateVaginal suppository: insert 1suppository vaginally at bedtimefor 3 daysVulvovaginal candidiasis:Vaginal ointment: insert 1applicatorful vaginally once atbedtimeTinea corporis, tinea cruris, tineapedis, tinea versicolor:Cream, spray: treatment, apply toaffected area(s) twice daily for 2 to3 weeksSafety and efficacy inchildren have not beenestablishedFor children >2 years old:Tinea corporis, tinea cruris,tinea pedis, tinea versicolor:Cream, spray: treatment,apply to affected area(s)twice daily for 2 to 3 weeksVaginalointment:6.5%Cream: 1%Spray: 1%*Ciclopirox is formulated as ciclopirox olaminePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.128
VIII. Effectiveness<strong>Clinical</strong> studies evaluating the safety and efficacy of the single entity skin and mucous membrane antifungals are summarized in Table 8.Table 8. Comparative <strong>Clinical</strong> Trials Using the Single Entity Skin and Mucous Membrane AntifungalsStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsCandidiasis (Cutaneous)Gupta et al. 40Ciclopirox nail lacquer8% topical solutionapplied to affectedfingernail(s) andtoenail(s) QDvs.2 DB, MC, PC, PGPatients aged 18 to 70years old with mild tomoderate toenailonychomycosis causedby dermatophytesN=56048 weeksPrimary:Mycological curerate, treatmentsuccess, treatmentcure, negativecultureSecondary:Adverse effectsResultsPrimary:In study A, there was significant improvement in mycologicalcure in patients treated with ciclopirox compared to patientsreceiving the vehicle throughout the 48-week treatment period(29% vs. 11%, respectively; P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsthe 48-week treatment period (8.5% vs. 0%, respectively;P=0.001).Secondary:In study A, adverse effects associated with ciclopirox compared tovehicle were mainly localized site reactions including erythema(4% vs. 1%, respectively); tingling sensation, pain or intermittentburning (3% vs. 2%, respectively) and changes in nail shape orcolor (2% vs. 1%, respectively), P values not reported.Gupta et al. 40Ciclopirox nail lacquertopical solutiontherapiesvs.topical solution vehicletherapiesBagatell et al. 41Ciclopirox 1% creamapplied to affectedMARandomized trials,mostly OL and MC,conducted in Europe,Asia, North America,and South America withpatients with extensivefinger and/or toe nailinvolvement ofonychomycosis causedby dermatophytes ornondermatophytes (e.g.,Candida species)2 DB, MC, PG, RCTPatients aged 12 to 75years old with stable orN=2,0756 months13 trialsN=24028 daysPrimary:Mycological cure,clinical cure,clinical responsefor ciclopiroxtherapiesSecondary:Adverse effectsPrimary:Mycological cure,clinical cureIn study B, adverse effects associated with ciclopirox compared tovehicle were mainly localized site reactions including erythema(10% vs. 2%, respectively); tingling sensation, pain or intermittentburning (0% vs. 1%, respectively) and changes in nail shape orcolor (3% vs. 3%, respectively), P values not reported.Primary:Mycological cure rates ranged from 46.7% to 85.7%, clinical cureranged from 0% to 56.9%, and clinical response ranged from36.7% to 86% when ciclopirox was used according to dosingregimens ranging from once daily to twice weekly. The lowestreportedclinical cure and response rates were associated with thetwice-weekly regimens. The highest reported clinical cure andresponse rates were associated with the once-daily regimens. Pvalues not reported in the MA.Average relapse rate was 20.7% at up to 6 months of treatment. Pvalues not reported in the MA.Secondary:Minimal local side effects were associated with ciclopiroxtherapy. Reported side effects included nail changes, burning,stinging, erythema, pain, and skin reactions. P values not reportedin the MA.Primary:In the first week of therapy for study A, statistically significantdifferences favoring the active drug were observed in patientstreated with ciclopirox compared to placebo in terms of clinical130Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimenarea(s) BIDvs.clotrimazole 1% creamapplied to affectedarea(s) BIDvs.Study DesignandDemographicsexacerbating skinlesions that wereclinically andmycologically diagnosedas cutaneous candidiasisSample Sizeand StudyDurationEnd PointsSecondary:Adverse eventsResultsand mycological cures (90% vs. 50%, respectively; P
vs.StudyandDrug RegimenWhitfield’s Ointment ®(3% salicyclic acid, 6%benzoic acid) applied toaffected area(s) of skinBIDTanenbaum et al. 43Miconazole 2% creamapplied to affectedarea(s) on skin BIDvs.sulconazole 1% creamapplied to affectedarea(s) on skin QDvs.sulconazole 1% creamapplied to affectedarea(s) on skin BIDvs.Study DesignandDemographics2 DB, PG, RCTPatients with cutaneouscandidiasisSample Sizeand StudyDurationN=963 weeksEnd PointsPrimary:Mycological curerate, signs ofinflammation(erythema, scaling,pustules,maceration,vesiculation,fissuring), itching,clinician ratedoverall clinicalstatusSecondary:Adverse effectsResultstreated with clotrimazole or Whitfield’s ointment; P value notreported.Relative to patients with Candida infections, there was nostatistically significant difference in efficacy between patientstreated with clotrimazole or nystatin; P value not reported.Secondary:Not reportedPrimary:At the end of 3 weeks in study A, 100% of patients treated withsulconazole and 10% of patients who received the vehicle hadnegative results on the potassium hydroxide test; 100% of patientstreated with sulconazole and 0% of patients who received thevehicle had negative cultures (P values not reported). At the endof 3 weeks in study B, 100% of patients receiving sulconazole andmiconazole were negative on the potassium hydroxide test; 80%and 92% of sulconazole and miconazole patients, respectively,had negative cultures.At the end of 3 weeks in study A, 100% of patients treated withsulconazole and 26% of patients who received the vehicle werefree of signs of inflammation; 89% and 21% of sulconazole andvehicle patients, respectively, were free of itching (P values notreported). At the end of 3 weeks in study B, 100% and 92% ofsulconazole and miconazole patients, respectively, were free ofsigns of inflammation; 89% and 83% of sulconazole andmiconazole patients, respectively, were free of itching.cream vehicle applied toaffected area(s) BIDIn study A, participantsreceived eithersulconazole or vehiclegiven BID. In study B,participants receivedSecondary:One patient receiving the vehicle experienced itching. Erythemaand/or pruritus was reported by 6 patients treated with sulconazoleand 3 patients treated with miconazole (P values not reported).132Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimeneither sulconazole givenQD or miconazolegiven BID.Candidiasis (Oropharyngeal)Kirkpatrick et al. 44 DB, RCTClotrimazole 10 mgbuccal troche dissolve 1troche five times dailyvs.Study DesignandDemographicsPatients with chronicoral candidiasis for atleast 6 months with poorresponse to nystatin orgentian violetSample Sizeand StudyDurationN=202 weeksEnd PointsPrimary:<strong>Clinical</strong> response,mycologicalresponseSecondary:Adverse eventsResultsPrimary:<strong>Clinical</strong> and laboratory results were negative in more patientstreated with clotrimazole compared to patients receiving placebo(6 vs. 1, respectively; P
StudyandDrug RegimenCandidiasis (Vulvovaginal)Drogemueller et al. 46Butoconazole 2% creaminsert 1 applicatorful (6mL) intravaginally QDvs.Study DesignandDemographicsDB, MC, PG, RCTPatients with confirmedvulvovaginal candidiasisSample Sizeand StudyDurationN=2533 daysEnd PointsPrimary:<strong>Clinical</strong> cure,microbiologic cureSecondary:Adverse effectsResultsPrimary:At 8 days post treatment, 95% and 91% of patients treated withbutoconazole and clotrimazole, respectively, achievedmicrobiologic cure. At 30 days post treatment, 80% and 74% ofpatients treated with butoconazole and clotrimazole, respectively,were infection-free. The difference in microbiologic cure betweenthe two treatments was not statistically significant.clotrimazole 100 mgvaginal tablet insert 2tablets intravaginallyQDAt 8 days post treatment, 77% and 75% of patients treated withbutoconazole and clotrimazole, respectively, achieved clinicalcure. At 30 days post treatment, 82% and 74% of patients treatedwith butoconazole and clotrimazole, respectively, achievedclinical cure. The difference in clinical cure between the twotreatments was not statistically significant.Eighty-two percent and 72% of patients treated with butoconazoleand clotrimazole, respectively, had a complete absence of candidalsigns and symptoms.Hajman 47Butoconazole 2%vaginal cream insert 1applicatorfulintravaginally QHS (for3 days)vs.clotrimazole 1% vaginalcream insert 1applicatorfulintravaginally QHS (forPG, RCT, SBFemale patients aged 19to 63 years old withlaboratory confirmedvulvovaginal candidiasisN=633 to 6 daysPrimary:<strong>Clinical</strong> cure,microbiologicalcure, therapeuticcure (combinesclinical andmicrobiologicalcure)Secondary:Adverse eventsSecondary:Patients treated with either butoconazole or clotrimazole reportedincreased local vulvar/vaginal irritation and burning.Primary:The difference between the clinical response of patients treatedwith butoconazole at the initial vs. final visit was statisticallysignificant and indicated improvement in signs and symptoms ofvulvovaginal candidosis, such as vaginal discharge, itching,burning, erythema, and swelling (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Points6 days) clinical cure. At this time, 93.3% and 77.4% of patients treatedwith butoconazole and clotrimazole, respectively, achievedmicrobiological cure (e.g.,, negative cultures). Likewise, 82.1%and 72.4% of patients treated with butoconazole and clotrimazole,respectively, achieved therapeutic cure (P values not reported).ResultsAt one month after treatment, 86.7% and 96.4% of patients treatedwith butoconazole and clotrimazole, respectively, achievedclinical cure. At this time, 76.7% and 67.7% of patients treatedwith butoconazole and clotrimazole, respectively, achievedmicrobiological cure (e.g., negative cultures). Likewise, 66.7%and 64.5% of patients treated with butoconazole and clotrimazole,respectively, achieved therapeutic cure (P values not reported).There was no statistically significant difference between treatmentgroups in terms of clinical, microbiological, and therapeutic curerates.Brown et al. 48Butoconazole 2%vaginal cream insert 1applicatorfulintravaginally atbedtime (for 1 day)MC, PG, RCTFemale, nonpregnantpatients with confirmedvulvovaginal candidiasisN=2051 to 7 daysPrimary<strong>Clinical</strong> cure,microbiologicalcureSecondary:Adverse eventsSecondary:No adverse events were reported.Primary:For butoconazole-treated patients, symptoms declined aftertreatment from 20% to 1% from day 1 to day 7 since treatmentinitiation. At 8 to 10 days post treatment, 92% and 87% of patientimproved clinically and had negative cultures, respectively. At 30days post treatment, 88% and 74% of patients improved clinicallyand had negative cultures, respectively.vs.miconazole 2% vaginalcream insert 1applicatorfulintravaginally atbedtime (for 7 days)For the miconazole-treated patients, symptoms declined aftertreatment from 23% to 19% after the first dose. At 8 to 10 dayspost treatment, 92% and 87% of patient improved clinically andhad negative cultures, respectively. At 30 days post treatment,86% and 77% pf patients improved clinically and had negativecultures, respectively.All parameters between butoconazole and miconazole therapieswere not statistically different with the exception of the difference135Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsin the rapidity of severe symptom relief after the first dose ofbutoconazole compared to miconazole (P=0.01).Kaufman et al. 49Butoconazole 2%vaginal cream insert 1applicatorful (5 g)intravaginally QHS (for3 days)vs.miconazole 2% vaginalcream insert 1applicatorfulintravaginally QHS (for7 days)MC, PG, RCTFemale patients aged 18to 61 years old who arenonpregnant andconfirmed forvulvovaginal candidiasisN=2253 to 7 daysPrimary:Microbiologicalcure, clinical cureSecondary:Adverse eventsSecondary:No systemic events were reported. Vulvovaginal irritation (e.g.,burning, itching) was reported.Primary:At days 8 to 10 post treatment, 88% and 91% of patients treatedwith butoconazole and miconazole, respectively, were Candidafree (P=0.888); 80% and 82% of patients treated withbutoconazole and miconazole, respectively, were clinically cured(P=0.541).At 30 days post treatment, 73% and 69% of patients treated withbutoconazole and miconazole, respectively, were Candida free(P=2.14); 78% and 80%, of patients treated with butoconazole andmiconazole, respectively, were clinically cured (P=0.996); 59%and 52% of patients treated with butoconazole and miconazoleexperienced therapeutic cure.All parameters between butoconazole and miconazole therapieswere not statistically different.Higton 50Clotrimazole 100 mgvaginal tablet insert 1intravaginally QHSvs.nystatin 100,000 unitvaginal suppositoryinsert 2 intravaginallyPG, RCTObstetrical andgynecological patientswith mycologicallyconfirmed vaginalcandidiasisN=506 daysPrimary:Relapse rate,overall cure rateSecondary:Adverse eventSecondary:Minimal side effects were reported from both butoconazole- andmiconazole-treated patients including vaginal irritation.Primary:After 6 days of therapy, initial cure rates were 96% and 76% forpatients treated with clotrimazole and nystatin, respectively.After 4 weeks post treatment, infection relapse rates were 12.5%and 42% for patients treated with clotrimazole and nystatin,respectively. At this time, overall cure rates were higher forpatients treated with clotrimazole compared to patients treatedwith nystatin (84% vs. 58%; difference was not statisticallysignificant).136Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenQHSStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsBoth clotrimazole and nystatin reduced symptoms at 5 days posttreatment (P
StudyandDrug Regimenusing an applicator, 1vaginal tabletintravaginally QAMand QPM (for 15 days)Cohen 53Clotrimazole 10%vaginal cream 5 g QDfor one dosevs.clotrimazole 2% vaginalcream 5 g BID for 3daysFluery et al. 54Clotrimazole 100 mgvaginal tablet insert 2tablets intravaginallyQD (for 3 days)vs.Study DesignandDemographicsOS, PROPatients aged 16 yearsand older who presentedclinical signs andsymptoms of acutevaginal candidiasis(female) or candidalbalanitis (male) in thepast 3 monthsDB, PG, MC, RCTPatients aged 17 to 51years old with clinicallyand mycologicallyconfirmed vulvovaginalcandidiasisSample Sizeand StudyDurationN=1111 to 3 daysN=1031 to 3 daysEnd PointsSecondary:Adverse eventsPrimary:CulturesSecondary:Adverse effectsPrimary:<strong>Clinical</strong> cure,mycological cureSecondary:Adverse eventsResultsSecondary:Patients treated with nystatin reported adverse events, such ascondyloma acuminata of the labia, severe burning and vulvaredema, and pelvic pain. Patients treated with miconazole reportedadverse events, such as mild headache, vaginal burning, andmoderate irritation.Primary:At 1 week after treatment, the 1-dose treatment and 3-daytreatment demonstrated equal efficacy shown by negative culturesin vulvovaginal candidiasis at day 7 (90.9% vs. 96.4%; P valuenot reported) and day 35 (84% vs. 81%; P value not reported)Secondary:No adverse events were reported for either agent in femalepatients. Of the male patients, 45% reported signs and symptomsof balanitis.Primary:Baseline characteristics for the patients were similar except thatthe patients treated with clotrimazole 500 mg were older than theother treatment group (P=0.05).Between 5 to 10 days post treatment, 90% and 89% of patientstreated with clotrimazole 500 mg and clotrimazole 200 mg,respectively, achieved both clinical and mycological cure.clotrimazole 500 mgvaginal tablet insert 1tablet intravaginally QD(for 1 day)At 27 days post treatment, 75% and 72% of patients treated withclotrimazole 500 mg and clotrimazole 200 mg, respectively,achieved treatment success.There was no statistically significant difference in efficacybetween either treatment group in all study parameters.Secondary:One patient taking clotrimazole 200 mg reported moderate edemaof the vulva.138Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenLebherz et al. 55Clotrimazole 100 mgvaginal tablet insert 2tablets intravaginallyQD (for 3 days)vs.Study DesignandDemographicsDB, PG, RCTPatients aged 19 to 71years old withmycologically andclinically activevulvovaginal candidiasisSample Sizeand StudyDurationN=1011 to 3 daysEnd PointsPrimary:Mycological cure,clinical cureSecondary:Adverse eventsResultsPrimary:Between 5 to 10 days post treatment, 77% and 89% of patientstreated with single-dose and three-day regimens of clotrimazole,respectively, achieved mycological and clinical cure.At 27 days post treatment, 65% and 74% of patients treated withsingle-dose and three-day regimens of clotrimazole, respectively,achieved mycological and clinical cure.clotrimazole 500 mgvaginal tablet insert 1tablet intravaginally QD(for 1 day)Thomason et al. 56Miconazole 100 mgvaginal suppositoriesinsert 1 intravaginallyQHSvs.DB, RCTNonpregnant patientswith at least one clinicalvulvovaginal sign orsymptom and cultureconfirmedvulvovaginalcandidiasisN=297 daysPrimary:Microbiologiccure, clinical cure,therapeutic cureSecondary:Adverse eventsThere was no statistically significant difference in efficacybetween either treatment group in all study parameters.Secondary:Two patients treated with either the one- or three-day therapy ofclotrimazole reported a vulvar lesion. One patient treated with 3-day therapy of clotrimazole complained of a perianal rash.Primary:At 8-10 days, 100% of patients (N=5) treated with terconazoleachieved clinical, microbiologic, and therapeutic cure. At thattime, 100%, 89%, and 89% of patients treated with miconazoleachieved clinical, microbiologic, and therapeutic cure,respectively. At that time, 44%, 33%, 33% of patients receivingplacebo achieved clinical, microbiologic, and therapeutic cure,respectively.terconazole 80 mgvaginal suppositoriesinsert 1 intravaginallyQHS (for 3 days), thensuppository vehicleinsert 1 intravaginally(for 4 days)vs.Terconazole and miconazole treatment groups showed statisticallysignificant improvements in clinical, microbiologic, andtherapeutic cure compared to placebo (P
StudyandDrug RegimenQHSJacobson et al. 57Butoconazole 1%vaginal cream insert 1applicatorful (5 g) QDvs.butoconazole 2%vaginal cream insert 1applicatorful (5 g) QDvs.miconazole 2% vaginalcream insert 1applicatorful (5 g) QDCorson et al. 58Miconazole 2% creaminsert 1 applicatorful (5g) intravaginally QDvs.terconazole 0.4% creaminsert 1 applicatorful (5g) intravaginally QDvs.terconazole 0.8% creaminsert 1 applicatorful (5Study DesignandDemographicsDB, MC, PG, RCTPatients aged 13 to 39years old with confirmedvulvovaginal candidiasisby clinical signs andsymptoms of vaginalyeast infection (e.g.,swelling, redness,itching, burning, and/orcharacteristic discharge)or presence of Candidaalbicans confirmed bypotassium hydroxide testand cultureDB, MC, RCTNonpregnant, femalepatients aged 17 to 61years old with signs andsymptoms ofvulvovaginalcandidiasis,microbiologicallyconfirmedvulvovaginalcandidiasis, and eitherhistory of beingpostmenopausal for 2years or using aneffective means ofcontraceptionSample Sizeand StudyDurationN=1306 daysN=5747 daysEnd PointsPrimary:Microbiologicalcure, clinical cure,relapse rateSecondary:Adverse effectsPrimary:<strong>Clinical</strong> response,microbiologicalresponse,therapeutic cure,relapseSecondary:Adverse eventsResultsPrimary:On day 8, 98%, 91%, and 83% of patients treated withbutoconazole 2%, butoconazole 1%, and miconazole 2%,respectively, achieved negative fungal cultures. Likewise, 78%,75%, and 68% of patients treated with butoconazole 2%,butoconazole 1%, and miconazole 2%, respectively, achievedclinical cure at this visit.After 30 days from the end of treatment, 82%, 80% and 68% ofpatients treated with butoconazole 2%, butoconazole 1%, andmiconazole 2%, respectively, maintained negative fungal cultures;therefore, relapse rate was low. Likewise, 73%, 67%, and 66% ofpatients treated with butoconazole 2%, butoconazole 1%, andmiconazole 2%, respectively, maintained clinical cure at this visit.The differences between cure rates of the three treatment groupswere not statistically significant.Secondary:Two patients in each treatment group reported side effects (i.e.,headache, vaginal burning, leakage of cream, and bleeding).Primary:Relative to demographics, the use of contraceptives appears tohave a negative effect on cure rate across all treatment groups;patients not on contraceptives achieved a higher cure rate(P=0.01).Between 8 to 10 days post treatment (visit 1), the microbiologiccure rates for terconazole 0.4%, terconazole 0.8%, and miconazole2% were 91.1%, 86.9%, and 83.6%, respectively; clinical curerates were 95.5%, 93.4%, and 91.6%, respectively; the therapeuticcure rates were 87.9%, 83,8%, and 81.3%, respectively. Themicrobiologic cure rates of patients treated with terconazole 0.4%were higher than that of patients treated with miconazole 2%(91.1% vs. 83.6%, P=0.02). There was no statistically significantdifference for other comparisons.140Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsg) intravaginally QD After 7 days of treatment, patients treated with terconazole 0.4%,terconazole 0.8%, and miconazole 2% had complete symptomrelief rates of 83.3%, 77.0%, and 79.5%, respectively. There wasno statistically significant difference between treatment groups.ResultsAfter 7 days of treatment, patients treated with terconazole 0.4%,terconazole 0.8%, and miconazole 2% had combined clinical andmicrobiological cure rates of 87.9%, 83.8%, and 81.3%,respectively. There was no statistically significant differencebetween treatment groups.Between 30 to 35 days post treatment (visit 2), there were nostatistically significant differences in microbiologic, clinical, ortherapeutic cure rates in the treatment groups.Hirsch 59Clotrimazole 200 mgtablets (for 3 days)vs.MAPatients with confirmedvulvovaginal candidiasisin mostly DB, MC, PC,RCT trials, pregnantN=1,8001 to 7 days16 trialsPrimary:<strong>Clinical</strong> cure rateSecondary:Adverse effectsSecondary:There was no statistically significant difference in the number ofpatients who reported adverse effects in the terconazole 0.4%,terconazole 0.8%, and miconazole 2% treatment groups (61.1%,62.2%, 57.2%), respectively. Adverse reactions most commonlyreported involved the central nervous system or genitalreproductivesystem. Although no P values were provided,investigators claim that patients treated with terconazole 0.4% hadsignificantly less side effects associated with the genitalreproductivesystem compared to the other groups, that patientstreated with the lower strength of terconazole had significantlylower rates of pruritus and metrorrhagia, that patients treated withmiconazole experienced more vulvovaginal symptoms andrhinorrhea compared to both terconazole groups, that patientstreated with terconazole 0.4% experienced more pyrexiacompared to the other groups.Primary:According to the meta-analysis, the most effective regimens ofterconazole were the 80 mg suppository for 3 days, 240 mgsuppositories for 1 day, and the 0.4% cream for 7 days. The 240mg suppository for 1 day was more effective than the 80 mgsuppository for 3 days, which may have been due to a better141Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimenclotrimazole 1% creaminsert 1 applicatorful (5g) intravaginally QHS(for 7 days)vs.econazole 150 mgsuppositories* (for 3days); dosing notspecifiedStudy DesignandDemographicspatients were included inmost of the trialsSample Sizeand StudyDurationEnd PointsResultscompliance. The clinical efficacies of the 0.4% and 0.8% creamfor 7 days were comparable.At 4 weeks from the start of treatment, 92% patients receivingterconazole 80 mg suppositories achieved clinical cure; 88% forterconazole 240 mg suppository for 1 day, 94% for terconazole0.8% cream for 5 days, 90% for terconazole 0.4% cream for 7days.After 4 weeks, mycological cure rates with terconazole 0.2%cream were similar to miconazole 2% cream but less compared toterconazole 0.4% cream.vs.miconazole 2% creaminsert 1 applicatorful (5g) intravaginally QHS(for 7 days)vs.terconazole (40 mg, 80mg, 240 mg) vaginalsuppositories, (0.2%,0.4%, 0.8%) cream, orother formulationsAfter 4 weeks, mycological cure rates were 100% and 80% forterconazole 0.4% cream and clotrimazole 1% cream, respectively,for nonpregnant patients. After 4 weeks, mycological cure rateswere 92% and 89% for terconazole 0.4% cream and clotrimazole1% cream, respectively, for pregnant patients.After 4 weeks, mycological cure rates were similar betweenterconazole 80 mg suppositories and econazole 150 mgsuppositories for pregnant and nonpregnant patients.After 4 weeks, mycological cure rates were similar betweenterconazole 80 mg and 240 mg suppositories and clotrimazole 240mg tablets.Note: Statistical significance was not addressed in the studyresults; P values were not reported.Secondary:Vaginal burning was reported by 2%, 2%, and 1% of patientstaking terconazole 80 mg vaginal suppositories, terconazole 0.4 %vaginal cream, and terconazole 0.8% vaginal cream, respectively.Regimens comprised of terconazole 240 mg vaginal suppositorywere well tolerated.142Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenBrown et al. 60Butoconazole 1%vaginal cream (for 3days), then creamvehicle (for 3 days)vs.Study DesignandDemographicsDB, MC, PG, RCTPatients aged 17 to 67years old with confirmedvulvovaginal candidiasisSample Sizeand StudyDurationN=5803 to 6 daysEnd PointsPrimary:Microbiologicalcure, clinical cure,therapeutic cureSecondary:Adverse eventsResultsPrimary:<strong>Clinical</strong> and microbiological cure rates were greater in allbutoconazole- and miconazole-treated patients compared toplacebo (P
StudyandDrug RegimenYoung et al. 61Clotrimazole (specificagent and dosing notreported)vs.econazole* (specificagent and dosing notreported)vs.hydrargaphen* (specificagent and dosing notreported)vs.miconazole (specificagent and dosing notreported)Study DesignandDemographicsMA (all RCTs)Pregnant patientsreceiving any topicaltreatment for vaginalcandidiasisSample Sizeand StudyDurationSample sizenot reported10 trialsEnd PointsPrimary:Secondary:Not reportedResultsPrimary:According to data from 5 trials, patients treated with topicalazoles achieved greater cure compared to patients treated withnystatin (odds ratio 0.21, 95% CI 0.06 to 0.29).According to data from 1 trial, there was no statisticallysignificant difference between patients treated with nystatincompared to hydrargaphen* (odds ratio 0.14, 95% CI 0.05 to1.84).According to data from trials with clotrimazole, the followingresults were reported: (1) clotrimazole is more effective thanplacebo (odds ratio 0.14, 95% CI 0.06 to 0.31), (2) clotrimazoletreatment was similar regardless of single or multiple (i.e., 3 to 4days) dosing, (3) clotrimazole treatment for 7 days was moreefficacious compared to treatment for 4 days (odds ratio 11.7,95% CI 4.21 to 29.15), (4) clotrimazole treatment was similarregardless of 7-day or 14-day treatment duration (odds ration 0.41,95% CI 0.16 to 1.05), (5) clotrimazole and terconazole had similarefficacy (odds ratio 1.41, 95% CI 0.28 to 7.10).Secondary:Not reportedvs.nystatin (specific agentand dosing not reported)vs.terconazole (specificagent and dosing notreported)vs.144Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimenplacebo (specific agentand dosing not reported)Thomason 62Miconazole 2% vaginalcream (for 7 days;dosing regimen notspecified)vs.miconazole 100 mgvaginal suppositories(for 7 days; dosingregimen not specified)Study DesignandDemographicsMA (DB, PG, RCT; AC,PC, or both)Patients greater than 18years old, nonpregnant,with signs andsymptoms ofvulvovaginal candidiasis(i.e., itching, burning,irritation, erythema,edema, excoriation) andconfirmed vulvovaginalcandidiasisSample Sizeand StudyDurationN=1,2593 to 7 daysNumber oftrials notreportedEnd PointsPrimary:<strong>Clinical</strong> cure rate,mycological curerate, relapse rateSecondary:Adverse eventsResultsPrimary:Terconazole cream and suppository formulations were moreefficacious compared to placebo (P
StudyandDrug Regimenregimens not specified)Study DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsvs.cream vehicle (for 7days; dosing regimennot specified)vs.suppository vehicle (for7 days; dosing regimennot specified)Seborrheic Dermatitis / DandruffAly at el. 63DB, MC, PC, RCTCiclopirox 0.77% gelapplied to affectedarea(s) BIDvs.gel vehicle applied toaffected area(s) BIDPatients aged 19 to 85years old withmoderate, stable orexacerbating,inflammatory seborrheicdermatitis of the scalpN=17828 daysPrimary:<strong>Clinical</strong> evaluation,efficacy evaluationSecondary:Adverse eventsPrimary:At days 22, 29, and at the study endpoint (final visit, up to day33), patients treated with ciclopirox achieved >75% improvementin global evaluation scores compared to those treated with thevehicle (P=0.01).At days 15 (P=0.01), days 22 (P=0.001), 29 (P=0.001), and at thestudy endpoint (P=0.001), total patient signs and symptom scoreswere higher in patients treated with ciclopirox compared tovehicle.Twenty-nine percent of patients treated with ciclopirox rated themedication as cosmetically acceptable (P values not reported).Vardy et al. 64Ciclopirox 1% shampooapplied for 5 minutes,then rinse twice weeklyDB, PC, PRO, RCTPatients aged 15 yearsand older with mild tomoderate seborrheicdermatitis of the scalpN=824 weeksPrimary:Symptom scores,clinical cure,clinicalassessmentsSecondary:A burning sensation was reported in 13% and 9% in ciclopiroxand vehicle-treated patients, respectively (P values not reported).Primary:At the end of 4 weeks of treatment, 93% and 41% of patientstreated with ciclopirox and placebo, respectively, hadimprovement or clearing of infections (P
vs.StudyandDrug Regimenshampoo vehicleapplied for 5 minutes,then rinse twice weeklyStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsSecondary:Not reportedResultsAt the 2-week checkup, 4-week checkup, and at 2 weeks posttreatment, there was greater improvement in overall symptomsscores in patients treated with ciclopirox compared to patientstreated with placebo (P=0.022, P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsvs.gel vehicle wash hairtwice weekly bymassaging in gel for 3-5minutes prior to rinsingwith warm waterElewski et al. 67Ketoconazole 2% gelapplied QDvs.gel vehicle applied QDPC, PRO, RCTPatients aged 13 to 91years old with moderateto severe seborrheicdermatitis (baselinesigns and symptomsscored greater than 2 forerythema and scalingand greater than 1 forpruritus; investigator’sglobal assessment scoreof 3 or greater)N=45914 daysPrimary:Successfultreatment at day 28Secondary:Change frombaseline in signsand symptomsscores forerythema, scaling,and pruritus at day14, adverse eventsSecondary:Adverse events were mostly cosmetic in nature. One patient whoreceived placebo reported hair loss, and one patient treated withketoconazole reported dry hair.Primary:At day 28, successful treatment was reported in more patientstreated with ketoconazole compared to placebo (27.2% v 13.9%,respectively; P=0.0005). With the intent-to-treat analysis,ketoconazole treatment shower greater efficacy compared toplacebo (P=0.0014).Secondary:Scaling was reduced by ketoconazole as compared to placebo (-1.55 vs. -1.31, respectively; P=0.0022). Mean overall symptomseverity was reduced by ketoconazole and placebo (53% vs. 39%,respectively; P value not reported). With the intent-to-treatanalysis, ketoconazole treatment was associated with a loweroverall mean score compared to placebo at day 7 (2.92 vs.. 3.32,respectively; P=0.048) and at day 28 (2.76 vs. 3.56, respectively;P
StudyandDrug RegimenJohnson ® ’s BabyShampoo for 4 weeks,then wash hair QD withshampoo vehicle for 4weeksvs.Study DesignandDemographicsSample Sizeand StudyDurationEnd Pointsof scalp itchingand scaling(ranging from noneto worse ever)Secondary:Not reportedResultsPatients treated with ketoconazole 2% shampoo experienced astatistically significant improvement in scalp itching (P
StudyandDrug RegimenTinea InfectionsWu et al. 70Ciclopirox 1% creamapplied to affectedarea(s) BID to TIDOL, OSStudy DesignandDemographicsPatients living intemperate climates withculture ormicroscopicallyconfirmedonychomycosis and/ortinea pedisSample Sizeand StudyDurationN=493 to 24 monthsEnd PointsPrimary:<strong>Clinical</strong> cure,mycological cureSecondary:Adverse effectsResultsPrimary:For onychomycosis, 14% and 36% of patients (N=42) treated withciclopirox were cured and showed improvement, respectively.Cure was influenced by the degree of nail plate affected; moderateinvolvement correlated to a better cure rate (P values notreported).For tinea pedis, 42% and 45% of patients (N=33) treated withciclopirox were cured and showed improvement, respectively (Pvalues not reported).Kagawa et al. 71Terbinafine 1% creamapplied to affectedarea(s) BIDNo comparatorMCPatients with tinea pedis,tinea corporis, tineacruris, interdigital andintertriginouscandidiasis andpityriasisN=6144 weeks fortinea pedis; 2weeks forother tineainfectionsPrimary:Mycologicalefficacy,improvement ofclinical signs andsymptoms (e.g.,erythema, scaling,itching, papuleformations,vesiculation,erosion,maceration)Secondary:Paronychia was reported as a side effect, possibly due to excessiveapplication of the agent.Primary:Mycological efficacy was demonstrated in 74% of 218 patientstreated for tinea pedis and 93% of 85 patients treated for Candidaintertrigo. Approximately 78% to 94% of patients found thetreatment acceptable (P values not reported).Secondary:Adverse reactions, such as acute irritant contact dermatitis andpruritus, were reported in 1% of patients treated with terbinafine.These reactions were reversible upon discontinuing treatment andinitiating corticosteroid or imidazole treatment (P values notreported).Reyes et al. 72Butenafine 1% cream invehicle applied to tineapedis lesions QDvs.DB, MC, PC, RCTPatients with interdigitaltinea pedis rated with aminimum erythemascore of 2 and aminimum score of 2 forN=1054 weeksSecondaryAdverse effectsPrimary:Mycological cure,investigator globalassessment ofclinical response,patient’sassessment ofPrimary:Patients who received butenafine were more likely to experiencemycological cure at 4 weeks compared to the vehicle (91% vs..63%, respectively; P
StudyandDrug Regimencream vehicle applied totinea pedis lesions QDStudy DesignandDemographicseither pruritus or scalingSample Sizeand StudyDurationEnd Pointschange, effectivetreatmentSecondary:Adverse effectsResultsAccording to the investigator global response, patients receivingbutenafine had significantly better clinical response to comparedto the vehicle at 4 (P=0.03) and 8 weeks (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Points(P75% clinical improvement (P=0.05). This statistically significantdifference in treatment success between ciclopirox and vehiclewas observed at days 26, 43 and at the study endpoint (final visit,up to day 50) (P=0.05).Secondary:At the end of the study, 40% and 4% of the patients treated withciclopirox and vehicle, respectively, had complete clinical cure.This statistically significant difference in clinical cure betweenciclopirox and vehicle was observed at days 26, 43 and at thestudy endpoint (P=0.05).At the end of the study, 66% and 16% of patients treated withciclopirox and vehicle, respectively, had either cleared orexcellent improvement relative to the infection (P=0.05).At 2 weeks post treatment, 85% and 16% of patients treated withciclopirox and vehicle, respectively, were mycologically cured(P=0.05).152Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenMandy et al. 75Miconazole 2% creamapplied to affectedarea(s) of skin sparinglyBIDvs.cream vehicle applied toaffected area(s) of skinsparingly BIDJordon at el. 76Naftifine 1% creamapplied to affectedarea(s) of skin QDvs.cream vehicle applied toaffected area(s) of skinQDVan Esso et al. 77Sertaconazole 2%cream applied toaffected area(s) on skinQDStudy DesignandDemographicsDB, RCTMale patients between17 and 39 years of agewith confirmeddermatophyte infections(primarily tinea cruris,but inclusive of tineacorporis and tinea pedis)DB, RCTPatients aged 14 to 67years old with confirmedtinea cruris or tineacorporisMC, OLPatients aged 2 to 16years old with eithertinea corporis, tineacruris, or tinea pedisSample Sizeand StudyDurationN=624 weeksN=704 weeksN=162 weeksEnd PointsPrimary:<strong>Clinical</strong> evaluation,symptomaticevaluationSecondary:Adverse eventsPrimary:Mycological cure,clinical cureSecondary:Adverse eventsPrimary:Symptoms(erythema,desquamation,vesicles, pruritus),clinical cureResultsAt the end of the treatment, 46% and 24% of patients treated withciclopirox and vehicle, respectively, described treatment ascosmetically acceptable (P values not reported).Primary:After 4 weeks of therapy, 93.3% of patients treated withmiconazole and 18.8% of patients receiving the placebo creamexperienced resolution of infection; P values not reported.After 4 weeks of therapy, 6.7% of patients treated withmiconazole tested positive on the potassium hydroxide test and10% of patients tested positive upon culturing. After 4 weeks oftherapy, 66% of patients receiving placebo tested positive on thepotassium hydroxide test and 72% of patients tested positive uponculturing (P values not reported).Secondary:No adverse events were reported.Primary:After 2 weeks, 79% and 31% of patients treated with naftifine andplacebo, respectively, achieved mycological cure (P
vs.StudyandDrug Regimencream vehicle applied toaffected area(s) on skinQDVillars et al. 78Terbinafine 1% creamapplied to affectedarea(s) as directedvs.cream vehicle applied toaffected area(s) asdirectedStudy DesignandDemographics(primarily tineacorporis)MAPatients with tineainfections (i.e., tineacorporis, tinea pedis,cutaneous candidiasis,onychomycosis,pityriasis versicolor)Sample Sizeand StudyDurationN=1,258Duration notreported27 trialsEnd PointsSecondary:Adverse effectsPrimary:Complete cure,mycological cure,clinical signs andsymptoms forterbinafine 1%cream therapiesSecondary:Adverse effects forterbinafine 1%cream therapiesResultscure after 4 weeks since start of treatment; 31% achieved cure atweek 1 and 75% achieved cure at week 2.Secondary:No local or systemic adverse effects were observed.Primary:In the topical treatment of dermatomycoses, terbinafinedemonstrated clinical efficacy between 70% and 90%; relative totinea versicolor, topical terbinafine showed a cure rate of 70% to80%. No P values reported.Secondary:In 2.2% of patients receiving topical terbinafine 1% creamexperienced adverse effects such as burning, itching, and rednessof the site of application.Kamalam et al. 79Clotrimazole (dosingregimen not reported)vs.econazole (dosingregimen not reported)DB, OSPatients aged 45 days to36 years old withconfirmed tineainfectionsN=453 to 60 daysPrimary:<strong>Clinical</strong> cure,microscopicallynegative resultsSecondary:Adverse eventsPrimary:At 6 weeks post treatment, 98% (43 of 44) and 2% (1 of 44) of allpatients achieved complete or partial cure, respectively, regardlessof treatment with either clotrimazole or econazole (P values notreported). The 1 patient with the partial cure achieved clinicalcure but not microscopic cure. The use of "total cure rate" maynot best demonstrate the 1 case with the partial cure.For econazole-treated patients, clinical cure was observed inapproximately 14 days (range: 5-29 days) and microscopicallynegative results were seen in 1 to 2 weeks. At 6 weeks posttreatment, all cases were cured (P values not reported).For clotrimazole-treated patients, clinical cure was observed inapproximately 16.5 days (range: 3-44 days) and microscopicallynegative results were seen in 1 to 6 weeks. At 6 weeks post154Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultstreatment, there was 1 case not cured (P values not reported).Lassus et al. 80Clotrimazole 1% creamapplied to affectedarea(s) on skin BIDvs.sulconazole 1% creamapplied to affectedarea(s) on skin BIDRajan et al. 81Clotrimazole 1% creamapplied to affectedarea(s) of skin BIDvs.sulconazole 1% creamapplied to affectedarea(s) of skin QAMand cream vehicleapplied to affectedarea(s) QHSDB, PGPatients withmicrobiologicallyconfirmeddermatomycosis(primarily tinea pedis)DB, PG, RCTPatients (mean age 41years) with clinicallyproven cutaneouscandidiasis (interdigitalor intertriginouscandidiasis or perleche)N=404 weeksN=413 weeksPrimary:<strong>Clinical</strong> signs andsymptoms(erythema, itching,scaling ,maceration,fissuring,vesiculation),overall clinicalimprovement,cosmeticacceptabilitySecondary:Adverse eventsPrimary:Efficacyparameters (fungalculture/microscopicpreparation,physician’sassessment ofoverallimprovement)Secondary:Adverse eventsSecondary:No adverse effects were reported. There was 1 report of arecurrence after 2 weeks of stopping therapy (P values notreported).Primary:Patients with signs and symptoms of scaling and erythemaresponded better to sulconazole than clotrimazole at weeks 2(P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsTham 82Clotrimazole 1%solution applied toaffected area(s) on skinBIDvs.sulconazole 1% solutionapplied to affectedarea(s) on skin QAMand lotion vehicleapplied to affectedarea(s) QHSStudy design notreportedPatients aged 14 to 62years old withmicroscopicallyconfirmed pityriasisversicolorN=843 weeksPrimary:<strong>Clinical</strong>assessment(itching, scaling,erythema),investigatorassessment, patientassessment,negativemicroscopySecondary:Adverse effectsSecondary:Five patients treated with sulconazole reported adverse effects,which included itching of various degrees of severity. No adverseeffects were reported by patients treated with clotrimazole.Primary:Reduced rates of itching, scaling, and erythema did not differbetween treatment groups at weeks 2 and 3 (P>0.05). Potassiumhydroxide results did not differ (P>0.05) between patients treatedwith sulconazole or clotrimazole at weeks 2 (67% vs. 72%,respectively) and 3 (76% vs. 93%, respectively).Investigator assessed clinical efficacy was 63% and 65% inpatients treated with sulconazole and clotrimazole, respectively(P=0.8911).Overall evaluation by the patients was similar (P=0.2197).After 6 weeks post treatment, negative microscopy wasmaintained by 79% and 92% of patients taking sulconazole andclotrimazole, respectively. This difference was not statisticallysignificant.Patel et al. 83Clotrimazole 1% creamapplied to affectedarea(s) of skin BID for4 weeksvs.DB, MC, PG, PRO,RCTPatients with clinicallydiagnosed andmycologicallyconfirmed interdigitaltinea pedisN=1044 weeksPrimary:Mycological cureSecondary:Effectivetreatment,complete cure,perceived efficacy,Secondary:Five patients who were treated with sulconazole reported adverseeffects which included mild itching and burning. Eight patientswho were treated with clotrimazole reported adverse effects suchas severe itching, biting sensation, stickiness of product, and skinpeeling.Primary:Patients randomized to the terbinafine treatment group had ahistory of infection that was longer than that of patients treatedwith clotrimazole (P=0.04).After 1 week of treatment, 84.6% and 55.8% of patients treatedwith terbinafine and clotrimazole, respectively, were culturenegative (P=0.001). Patients treated with terbinafine achieved156Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimenterbinafine 1% creamapplied to affectedarea(s) of skin BID (for1 week), then creamvehicle applied toaffected area(s) BID(for 3 weeks)Petres et al. 84Econazole 1% creamapplied to affectedarea(s) of skin BIDvs.sulconazole 1% creamapplied to affectedarea(s) of skin BIDStudy DesignandDemographicsDB, PG, RCTPatients with culture andmicroscopy confirmeddermatophytoses(primarily tinea pedis)Sample Sizeand StudyDurationN=384 weeksEnd Pointsrelapse rate,adverse eventsPrimary:Microbiologicalcure, clinical cure(itching, erythema,scaling, fissuring,maceration,vesiculation,pustulation),overall clinicalimprovement,relapse, cosmeticacceptabilitySecondary:Adverse effectsResultsmycological cure more rapidly than patients treated withclotrimazole resulting potentially in improved compliance withterbinafine therapy. Relative to mycological cure, there was nostatistically significant difference between study groups at weeks4, 8, and 12 weeks.Secondary:In terms of study parameters such as effective treatment andcomplete cure, there was a statistically insignificant trend favoringterbinafine compared to clotrimazole. Throughout the study, bothpatients and investigators evaluated the treatments as very good togood in 75% to 80% of cases. Relapse rate was 15% and 19% inpatients treated with terbinafine and clotrimazole, respectively; Pvalues not reported. Most commonly reported adverse effectsincluded burning, hypersensitivity, stinging, and exacerbation ofpruritus.Primary:By week 2, every patient achieved microbiological cure with theexception of one patient treated with sulconazole. By week 4, allpatients achieved microbiological cure (P values not reported).Both treatment groups responded well to treatment leading tosignificant reductions in itching, scaling, and erythema. However,by week 4, 2 and 3 patients treated with sulconazole andeconazole, respectively, were still mildly symptomatic. There wasno statistically significant difference between treatment groups interms of overall clinical improvement. The diagnosis of tineapedis in 80% of the study participants did not influence the studyresults (P values not reported).At week 10, all patients treated with sulconazole remainedsymptom- and microbiologically-free of infection, whereas 3patients treated with econazole experienced clinical relapses (Pvalues not reported).Relative to cosmetic acceptability, 90% and 79% of patientstreated with sulconazole and econazole, respectively, rated the157Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsacceptability as excellent. There was no statistically significantdifference in cosmetic acceptability.Grigoriu et al. 85Econazole 1% creamapplied to affectedarea(s) of skin BIDvs.tioconazole 1% creamapplied to affectedarea(s) of skin BIDDB, RCTPatients (average agewas 30 years old) withconfirmed fungal skininfection or erythrasmaN=61average of38 to 40 daysPrimary:<strong>Clinical</strong> response,mycologicalresponse,combined clinicaland mycologicalcureSecondary:One patient treated with econazole reported an allergic reaction.One patient treated with sulconazole reported a case of eczema.Primary:There was one case of nonantifungal infection in each studygroup.In 28 days or less, 46.7% and 41.7% of patients treated withtioconazole and econazole, respectively, achieved symptomaticimprovement. After 14 days of treatment, 23 and 25 patientstreated with tioconazole and econazole, respectively, were cured.Combined clinical and mycological cure was achieved in 93.1%and 93.5% of patients treated with tioconazole and econazole,respectively (P values not reported).There was no statistically significant difference in rate ofimprovement, mycologically or clinically, between the twotreatment groups. Overall response rate was 90% observed in bothtreatment groups (P values not reported).Bonifaz et al. 86Ketoconazole 2% creamapplied to affectedarea(s) QD (for 14days)vs.terbinafine 1%emulsion gel applied toOL, PG, PRO, RCTPatients aged 12 to 79years old with clinicallyand mycologicallyconfirmed tinea corporisand tinea crurisN=657 to 14 daysPrimary:Mycological cure,clinical cureSecondary:Reported adverse event included mild intermittent pruritus, whichwas identified in a patient treated with econazole.Primary:<strong>Clinical</strong> cure was not statistically significant between the twotreatment groups (P=0.088).At the end of the study, mycological cure was achieved in 94%and 69% of patients treated with terbinafine and ketoconazole,respectively (P=0.027); combined clinical and mycological overallcure was achieved in 72% and 31% of patients treated withterbinafine and ketoconazole, respectively (P=0.002).Of note, the demographic data revealed an unequal distribution of158Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimenaffected area(s) of skinQD (for 7 days)Study DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultspatients in terms of gender (P=0.015); the ketoconazole studygroup had more male patients compared to the terbinafine studygroup.Tanenbaum et al. 87Miconazole 2% creamapplied to affectedarea(s) of skin BIDvs.sulconazole 1% creamapplied to affectedarea(s) of skin BIDTanenbaum et al. 88Miconazole 2% creamapplied to affectedarea(s) BIDvs.sulconazole 1% creamapplied to affectedarea(s) BIDDB, MC, PG, RCTPatients with confirmedtinea versicolorDB, PG, RCTPatients aged 18 to 65years old with cutaneousdermatomycosis (tineapedis and tineacruris/corporis)N=1813 weeksN=963 weeks(tinea cruris/corporis);4 weeks(tinea pedis)Primary:<strong>Clinical</strong> cure,mycological cureSecondary:Adverse eventsPrimary:Mycological cure,clinical cure,relapse rateSecondary:Adverse eventsSecondary:One patient treated with terbinafine and 3 patients treated withketoconazole reported dermatitis-like side effects. Terbinafinewas better tolerated than ketoconazole (P=0.003)Primary:At the end of the study, 93% and 87% of patients treated withsulconazole and miconazole were mycologically cured(P=0.6198). At this time, clinical cure was achieved in 89% and82% of patients treated with sulconazole and miconazole(P=0.2431).Secondary:Patients treated with miconazole reported stinging, itching,dermatitis, or irritation. Patients treated with sulconazole reporteditching, stinging/burning, dryness/scaling, and fissure/cracking.Primary:At the end of 4 weeks in patients treated for tinea pedis, 100% ofpatients treated with sulconazole and 67% of patients treated withmiconazole were mycologically cured (P values not reported).After the end of 3 weeks in patients treated for tineacruris/corporis, 91% of patients treated with sulconazole and100% of patients treated with miconazole were mycologicallycured (P values not reported).At the end of 3 weeks, 91% and 100% of patients treated withsulconazole and miconazole, respectively, reported significant orcomplete clearing of symptoms (P values not reported).Relapse rates were reported as 16% and 35% in patients treatedwith sulconazole and miconazole, respectively (P values notreported).159Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenVander Ploeg et al. 89Miconazole 2% creamapplied to affectedarea(s) on skin BIDvs.tioconazole 1% creamapplied to affectedarea(s) on skin BIDFredriksson 90Miconazole 2% creamapplied to affectedarea(s) BIDvs.tioconazole 1% creamapplied to affectedarea(s) BIDStudy DesignandDemographicsStudy design notreportedPatients aged 18 to 72years old withmycologically proveninfection with one of thefollowing fungi:Trichophyton sp,Microsporum sp,Epidermophyton sp,Candida sp, andPityrosporum orbiculareSB, PGPatients withmicroscopically andculture-confirmed fungalskin infectionsSample Sizeand StudyDurationN=774 weeksN=6014 days(tineapityriasis);28 days(dermatophyteand yeastinfections)End PointsPrimary:Mycological cure,clinical cure,relapse ratesSecondary:Adverse effectsPrimary:<strong>Clinical</strong> cure,mycological cureSecondary:Adverse eventsResultsSecondary:Two patients treated with miconazole reported severe irritantdermatitis. One patient treated with sulconazole experiencesmoderate-to-severe itching.Primary:After 4 weeks of treatment, 91.4% and 85.3% of patients takingtioconazole and miconazole, respectively, achieved both clinicaland mycological cures.After 4 weeks from the end of the treatment period, 93.5% and89.3% of patients taking tioconazole and miconazole remainedcured.There was no statistically significant difference between clinicalor mycological cure rates between tioconazole and miconazoletherapies.Secondary:Four patients treated with tioconazole reported side effects (e.g.,burning) and one patient treated with miconazole reported sideeffects (e.g., papular rash on the chest)Primary:At the end of the treatment, 77% and 63% of patients treated withtioconazole and miconazole, respectively, were both clinically andmycologically cured. Relative to the most common infection (byTrichophyton rubrum), tioconazole and miconazole cured 80%and 38%, respectively. The difference was not statisticallysignificant (P value not reported).Approximately 6 weeks later, patients treated with tioconazole andmiconazole remained infection-free at rates of 87% and 95%,respectively (P value not reported).Ramelet et al. 91 DB, MC, RCT N=138 Primary:Mycological cure,Secondary:No adverse events were recorded during the study.Primary:At the conclusion of the study, 69 and 70 patients treated withPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.160
StudyandDrug RegimenOxiconazole creamapplied to affectedarea(s) of skin QAMand placebo applied toaffected area(s) of skinQPMvs.oxiconazole creamapplied to affectedarea(s) of skin QAMand QPMBogaert et al. 92Ciclopirox 1% creamapplied to affectedarea(s) on skin BIDvs.clotrimazole 1% creamapplied to affectedarea(s) on skin BIDvs.cream vehicle applied toaffected area(s) on skinBIDStudy DesignandDemographicsPatients aged 8 to 80years old with one ormore clinically andmycologicallyconfirmeddermatomycoses (tineapedis, tinea cruris, tineacorporis) or erythrasma2 DB, MC, PG, RCTPatients with tineacorporis or tinea crurisSample Size End Pointsand StudyDuration7 to 60 days clinical cureN=22928 weeksSecondary:Adverse eventsPrimary:<strong>Clinical</strong> evaluation(scores rangingfrom 1=none to 4-severe), assessmentof treatmentresponseSecondary:Safety, toleranceResultsoxiconazole once daily and twice daily, respectively, achievedcure (P values not reported).The cure rates were 92% and 93.3% for patients treated withoxiconazole once daily and twice daily, respectively; nostatistically significant difference found between treatment groups(P values not reported).Secondary:Adverse effects were negligible. Three patients reported adverseevents which included irritation with erythema and pruritus nearthe infected area and burning sensations.Primary:In study A, patients treated with ciclopirox demonstratedstatistically significant improvement in clinical and mycologicalcure rate compared to the patients receiving the vehicle at 6 weeks(61% vs. 15%; P
StudyandDrug Regimenciclopirox 1 % creamBID or clotrimazole 1% cream BID.Fuerst et al. 93Tolnaftate 1% creamapplied to affectedarea(s) of skin QAMand QPMvs.undecylenic acid 5%ointment applied toaffected area(s) of skinQAM and QPMvs.vehicle (dosage formnot reported) applied toaffected area(s) of skinQAM and QPMStudy DesignandDemographicsDB, PG, PROMale patients withsymptomatic andclinically evident tineapedisSample Sizeand StudyDurationN=1034 weeksEnd PointsPrimary:<strong>Clinical</strong> cure,mycological cureSecondary:Not reportedResultsPrimary:At 2 weeks, 34.2%, 28.1%, and 15.2% of patients treated withundecylenic acid, tolnaftate, and placebo, respectively hadnegative potassium hydroxide test results.At 4 weeks, 65.8%, 46.9%, and 30.3% of patients treated withundecylenic acid, tolnaftate, and placebo, respectively hadnegative potassium hydroxide test results. At this time, 84.2%,80.7%, and 26.9% of patients treated with these agents,respectively, achieved negative cultures.At 6 weeks, 65.6%, 59.2%, and 41.9% of patients treated withundecylenic acid, tolnaftate, and placebo, respectively, hadnegative potassium hydroxide test results. At this time, 68.7%,66.6%, and 25.0% of patients treated with these agents,respectively, achieved negative cultures.Relative to negative potassium hydroxide results, undecylenic wasmore efficacious than placebo at weeks 2 (P=0.05), 4 (P0.05). Both tolnaftate and undecylenic acid werenot significantly different from each other in terms of negativecultures (P>0.05). Tolnaftate and undecylenic acid were notstatistically different from each other in terms of negative culturesor potassium hydroxide tests (P>0.05).Patients treated with undecylenic acid and tolnaftate improvedmore rapidly compared to placebo in regards to symptoms oferythema, scaling, fissuring, vesiculation, and itching/burning (Pvalues not reported).Secondary:Not reported162Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenAblon et al. 94Naftifine gel applied toaffected area(s) of skinQDvs.oxiconazole lotionapplied to affectedarea(s) of skin QDvs.terbinafine creamapplied to affectedarea(s) of skin QDStudy DesignandDemographicsDB, PRO, RCTMale patients aged 25 to80 years old withmicroscopically andculture-confirmed tineapedisSample Sizeand StudyDurationN=902 weeksEnd PointsPrimary:<strong>Clinical</strong> cure,mycological cureSecondary:Not reportedResultsPrimary:At 10 weeks, clinical cure rates for terbinafine, naftifine, andoxiconazole were 83.3%, 75%, 32.1%, respectively. At this time,mycological cure rates were 80.6%, 75%, 26.9%, respectively.In a comparison between terbinafine and naftifine treated patients,the difference in clinical and mycological cure was not statisticallysignificant at weeks 2-6, 6-10, or 2-10 (P>0.05).In a comparison between terbinafine and oxiconazole treatedpatients, the difference in clinical and mycological cure was notstatistically significant at weeks 2-6 but the difference wasstatistically significant for clinical and mycological cure at weeks6-10 (P=0.000186, P=0.0000984, respectively) and weeks 2-10(P=0.0000507, P=0.00000585, respectively) favoring terbinafine.In a comparison between naftifine and oxiconazole treatedpatients, the difference in clinical and mycological cure was notstatistically significant at weeks 2-6 but the difference wasstatistically significant for clinical and mycological cure at weeks6-10 (P=0.00808, P=0.00234, respectively) and weeks 2-10(P=0.00808, P=0.000890, respectively) favoring naftifine.Tschen et al. 95Tolnaftate creamapplied to affectedarea(s) of skin on feetBIDvs..undecylenic acidointment applied toaffected area(s) of skinDB, PC, PG, RCTPatients aged 18 to 62years old with clinicallyand mycologicallyproven tinea pedisN=904 weeksPrimary:Mycological cure,clinical cureSecondary:Adverse eventsSecondary:Not reportedPrimary:At four weeks of treatment, patients treated with undecylenic acidhad a greater improvement compared to placebo (P
StudyandDrug Regimenon feet BIDStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsvs.ointment vehicleapplied to affectedarea(s) of skin on feetBIDGupta et al. 96Ciclopirox 0.77% gelapplied to affectedarea(s) QDvs.ciclopirox 0.77% gelapplied to affectedarea(s) BIDvs.gel vehicle applied toaffected area(s) BIDDB, PC, PRO, RCTPatients aged 18 to 70years old with moderateinterdigital tinea pedisand secondary bacterialinfectionN=1008 weeksPrimary:Global clinicalevaluation score,subject clinicalevaluation score,clinical cure,mycological cure,complete cure;clinical evaluationscores range from1 excellent to 7worseSecondary:Adverse effectsPrimary:There was no statistically significant difference in improvedevaluation scores between once daily or twice daily applicationsof ciclopirox (P value not reported). However, both once andtwice daily ciclopirox treatment groups showed significantimprovement in evaluation scores compared to the vehicle at week8 (2.06 vs. 6.17, P=0.0003 and 2.41 vs. 6.17, P=0.0036,respectively).There was no statistically significant difference in improvedmycological cure rates between once daily or twice dailyapplications of ciclopirox; P values not reported. However bothonce and twice daily ciclopirox treatment groups showedsignificant improvement in mycological cure rate compared to thevehicle at week 8 (82.8% vs. 43.8%, P=0.013 and 80.8% vs.43.8%, P=0.007, respectively).There was a significant difference in complete cure rate betweentwice-daily ciclopirox and the vehicle (50.0% vs. 12.5%,respectively, P=0.014). Other comparisons were not statisticallysignificant.Pariser et al. 97 DB, MC, PC, PG, RCT N=332 Primary:Mycological cure,Secondary:The most common reported adverse effects were local sitereactions of burning or itching. There was no statisticallysignificant difference in the incidence of adverse effects betweentreatment groups; P value not reported.Primary:At the end of the study, 67% and 31% of patients treated withPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.164
StudyandDrug RegimenOxiconazole 1% lotionapplied to affectedarea(s) BIDvs.lotion vehicle applied toaffected area(s) of skinQAM, then oxiconazole1% lotion applied toaffected area(s) QPMStudy DesignandDemographicsPatients aged 12 to 82years old with confirmedtinea pedisSample Size End Pointsand StudyDuration6 weeks clinical cure,overall cure (i.e.,combinedmycological andclinical cure),global responsescoreSecondary:Adverse eventsResultsoxiconazole and placebo, respectively, experienced mycologicalcure (P values not reported).At the end of the study, >80% and 50% of patients treated withoxiconazole and placebo, respectively, experienced good toexcellent improvement in clinical signs and symptoms of tineapedis as well as global response (P values not reported).A statistically significant improvement was observed in patientstreated with oxiconazole compared to placebo relative to overallcure (P values not reported).vs..lotion vehicle applied toaffected area(s) BIDTanenbaum et al. 98Clotrimazole creamapplied to affectedarea(s) of skin BIDvs.sulconazole 1% creamapplied to affectedarea(s) of skin QAM,then cream vehicleapplied to affectedarea(s) of skin QPMvs.sulconazole 1% creamapplied to affectedarea(s) of skin BID2 DB, PG, RCTMale patient with tineacruris/tinea corporisN=1173 weeksPrimary:Microbiologicalcure, cultureconversion, overallclinical evaluationSecondary:Adverse eventsSecondary:Adverse effects reported were similar across study groups.Commonly reported adverse events included burning, stinging,dyshidrotic eczema, pain, scaling on dorsum of feet, and tingling.Primary:In study A, there was no statistically significant differencebetween treatment groups throughout the study relative tomicrobiological cure or culture conversion (P values not reported).In study B, there was a statistically significant improvement inculture conversion and microbiological cure for patients treatedwith sulconazole compared to vehicle at week 2 (P=0.0001) andweek 3 (P=0.0001).By week 3, 100% of patients treated with either clotrimazole orsulconazole achieved complete or partial clearing comparedto 30% of patients receiving placebo; there was no statisticaldifference between active treatment groups, (P value notreported). In study B, patients treated with sulconazole had astatistically significant improvement in overall clinical evaluationcompared to placebo (P=0.0001).Secondary:In study A, 4 patients receiving clotrimazole cream reportedmoderate to severe side effects, including erosive primary165Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
vs.StudyandDrug Regimencream vehicle applied toaffected area(s) of skinBIDStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsirritation, fissuring, and erythema. In study B, 6 patients receivingthe vehicle experienced primary irritant reactions (erosions,burning).In study A, participantsreceived eithersulconazole appliedQAM with creamvehicle QPM orclotrimazole appliedBID. In study B,participants receivedeither sulconazoleapplied BID or a creamvehicle applied BID.Sivayathorn et al. 99Clotrimazole 1% creamapplied to affectedarea(s) of skin TIDvs.DB, RCTPatients aged 2 to 72years old withsuperficialdermatophytosesN=1012 weeksPrimary:<strong>Clinical</strong> response,mycological cureSecondary:Adverse eventsPrimary:Satisfactory clinical response was reported in 50%, 73.68%,77.78%, 81.48% of patients treated with Whitfield’s Ointment ® ,tolnaftate, clotrimazole, and miconazole, respectively.Mycological cure was reported in 21.42%, 63.16%, 59.26%, and77.78% of patients treated with Whitfield’s Ointment ® , tolnaftate,clotrimazole, and miconazole, respectively.miconazole 2% creamapplied to affectedarea(s) of skin TIDvs.tolnaftate 2% creamapplied to affectedarea(s) of skin TIDAlthough miconazole demonstrated the highest clinical andmycological cure rate, there was no statistically significantdifference between clotrimazole, miconazole, and tolnaftatetreatment groups (P>0.05). Clotrimazole, miconazole, andtolnaftate therapies were more efficacious compared toWhitfield’s Ointment ® (P
StudyandDrug RegimenWhitfield’s Ointment ®(3% salicyclic acid, 6%benzoic acid) applied toaffected area(s) of skinTIDAly et al. 100Ciclopirox 1% creamapplied to affectedarea(s) on skin BIDvs.ciclopirox 1% lotionapplied to affectedarea(s) on skin BIDStudy DesignandDemographicsDB, MC, PG, RCTPatients with clinicallyand mycologicallyconfirmed plantar,interdigital, or vesiculartinea pedisSample Sizeand StudyDurationN=13428 daysEnd PointsPrimary:<strong>Clinical</strong> cure,mycological cureSecondary:Adverse eventsResultsPrimary:On day 29, patients treated with ciclopirox lotion experiencedgreater mycological response compared to patients receiving theplacebo (P
StudyandDrug Regimenand dosing not reported)vs.ciclopirox(specific agent anddosing not reported)vs.tolnaftate (specificagent and dosing notreported)vs.Study DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsAccording to a meta-analysis of 12 trials comparing azoles (i.e.,bifonazole*, clotrimazole, miconazole) to allylamines (i.e.,naftifine, terbinafine) given QD or BID for >4 weeks, the pooledrisk for failure to cure was 0.88 (95% CI, 0.78 to 0.99) with studyresults favoring the allylamines. It is important to note that therewas a statistically significance difference in (1) the clinicalefficacy of the azoles and duration of use and (2) relative riskestimates reported by English and foreign language papers. Nodifference was detected between individual azoles andallylamines.According to a meta-analysis of 3 trials comparing tolnaftate tovehicle, the pooled risk for failure to cure was 0.46 (95%confidence interval 0.17 to 1.22). Data showed that tolnaftate wasnot as effective as haloprogen or clotrimazole.undecenoic acid†(specific agent anddosing not reported)According to a meta-analysis of 4 trials comparing undecenoicacid to vehicle or active control, the pooled risk for failure to curewas 0.28 (95% confidence interval 0.11 to 0.74).vs.tea tree oil (specificagent and dosing notreported)vs.placebo vehicles(specific dosing notreported)Crawford et al. 102Allylamines (specificagents and dosing notreported; includesamorolfine 0.5%MA (all RCTs)Patients withmycologically diagnosedfungal infections of theskin and nails of the footSample sizenot reported72 trialsPrimary:Pooled relativerisks of failure tocure for topicalantifungal agentsIn nail trials, ciclopirox was shown to be statistically better thanvehicle (0.14, 0.06 to 0.32) and better than, though notsignificantly, clotrimazole (0.89, 0.72 to 1.10). Study data waslimited.Relative to trials of fungal nail infections, a larger trial showedclotrimazole solution and tea tree oil both achieving a cure rate of10% after 6 months. P value not reported.Secondary:Not reportedPrimary:Among the placebo-controlled trials, the pooled relative risks offailure to cure for skin infections were as follows for the topicalantifungal agents: allylamines 0.30 (95% CI 0.23 to 0.37), azoles0.53 (95% CI 0.42 to 0.68), undecenoic acid 0.28 (0.11 to 0.74),and tolnaftate 0.46 (0.17 to 1.22).168Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimencream*)vs.azoles (specific agentsand dosing not reported;includes bifonazole 1%cream*, neticonazolecream*)vs.Study DesignandDemographicsSample Sizeand StudyDurationEnd PointsSecondary:Not reportedResultsRelative to 11 meta-analysis trials comparing allylamines andazoles, the pooled relative risks of failure to cure for skininfections was 0.88 (0.78 to 0.99) in favor of allylamines; of note,there appears to be language bias in the reported results, where the7 English language studies favored allylamines and the 4 foreignlanguage studies reported no statistical difference.Secondary:Not reportedgriseofulvin topicalagent* (specific agentand dosing not reported)vs.haloprogen*(specific agent anddosing not reported)vs.tea tree oil (specificagent and dosing notreported)vs.tolnaftate (specificagent and dosing notreported; includestolciclate solution*)vs.169Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsundecenoic acid†(specific agent anddosing not reported)vs.placebo vehicles(specific dosing notreported)Drug regimen abbreviations: QD=once daily, BID=twice daily, TID=three times daily, QID=four times daily, QAM=every morning, QHS=at bedtime, QPM=every eveningStudy abbreviations: AC=active-controlled, CI=confidence interval, DB=double-blind, MA=meta-analysis, MC=multicenter, OL=open-label, OS=observational study, PC=placebo-controlled, PG=parallelgroup,PRO=prospective, RCT=randomized controlled trial, SB=single blinded, XO=crossover*Agent not available in the United States†Undecenoic acid= undecylenic acid.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.170
Additional EvidenceDose SimplificationFor uncomplicated vaginitis, topical agents are effective when used for 1 to 7 days. 7-9 The Centers forDisease Control and Prevention (CDC) report efficacy rates of 80% to 90% for 1- to 3-day therapy withtopical antifungal agents 11 A number of clinical trials demonstrated similar efficacy between differentantifungal agents used for vulvovaginal candidiasis despite different FDA-approved durations of therapies(e.g., 1-day vs.. 7-day). 46-62 In a meta-analysis, investigators concluded that the increased efficacy ofterconazole 240 mg vaginal suppository (for 1 dose) in vulvovaginal candidiasis, as compared toterconazole 80 mg vaginal suppository (for 3 days), was likely due to an increased compliance rateassociated with the shorter duration of therapy. 58 For onychomycosis, once-daily ciclopirox treatmentregimens were more effective than twice-daily regimens in clinical cure and response rates. 40 The availabledata suggests that the agent requiring the shortest duration of therapy, without compromising efficacy,should be initiated in cases of uncomplicated vulvovaginal candidiasis and noninvasive fungal infections.Stable TherapyAn evidence-based medicine literature search did not reveal data pertinent to this topic.Impact on Physician VisitsIn 1990, clotrimazole became the first product available OTC for the treatment of uncomplicated candidalvaginitis; a number of Rx-to-OTC switches for vaginal antifungal agents occurred between January 1991 toDecember 1991 103 In evaluating National Ambulatory Medical Care Survey and Bureau of Census data,Lipsky et al. identified a 15% reduction in physician’s office visits for vaginitis care between 1990 and1994 (P11 years old) and in the number of physician visits for vaginitis (0.66 per 100 patients) during the oneyearperiod after the OTC availability of vaginal products. 104IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.171
Table 9. Relative Cost of the Single Entity Skin and Mucous Membrane AntifungalsGeneric Name(s) Formulation(s) Example Brand Name(s) BrandCostGenericCostbutenafine cream Mentax ® $$$ N/Abutoconazole vaginal cream Gynazole-1 ® $$ N/Aciclopiroxcream, gel,shampoo, solution,suspensionLoprox ® *, Penlac ® $$$-$$$$$$$clotrimazole‡cream, solution,troche, vaginalcream, vaginaltabletClotrim Antifungal ® *,Cruex ® *, Desenex ® *,Femcare ® *, Gyne-Lotrimin ® *,Mycelex ® *$-$$$ $econazole cream Spectazole ® * $$ $$ketoconazole cream, gel, Nizoral ® *, Xolegel ® $$ $shampoomiconazole‡ cream, vaginalcombo package,vaginal cream,vaginalsuppository$ $Baza Antifungal ® *,Carrington Antifungal ® *,Micaderm ® *, Micatin ® *,Micro-Guard ® *, Mitrazol ® *,Monistat 1 Combo Pack ® ,Monistat 3 ® *, Monistat 7 ® *,Monistat-Derm ® *, NeosporinAF ® *naftifine cream, gel Naftin ® $$$ N/ANystatincream, ointment,powder, vaginaltabletMycostatin ® * $ $oxiconazole cream, lotion Oxistat ® $$$ N/Asertaconazole cream Ertaczo ® $$$ N/Asulconazole cream, solution Exelderm ® $ N/Aterbinafine‡ cream, spray Lamisil ® , Lamisil AT ® $ N/Aterconazole vaginal cream, Terazol 3 ® *, Terazol 7 ® * $$-$$$ $$vaginalsuppositorytioconazole‡ vaginal ointment Monistat 1 ® *, Vagistat-1 ® * $ $tolnaftate‡ cream Tinactin ® *† N/A $*Generic is available in at least one dosage form or strength.†Brand is no longer available.‡Over-the-counter product is available in at least one dosage form or strength.N/A=not availableX. ConclusionsThe skin and mucous membrane antifungals are FDA approved for the management of various fungalinfections, such as cutaneous candidiasis , oropharyngeal candidiasis, vulvovaginal candidiasis, seborrheicdermatitis, tinea corporis, tinea cruris, tinea pedis, and tinea versicolor. 1,2 The topical antifungal agentscurrently available belong to one of the following drug classes: allylamines, azoles, benzylamine,hydroxypyridones, polyenes, thiocarbamates, and miscellaneous agents (e.g., undecylenic acid). 1,2Ciclopirox, clotrimazole, econazole, ketoconazole, nystatin and terconazole are available generically in atleast one dosage form. The benzylamine (butenafine) is the only antifungal subclass where there is not ageneric formulation. Several antifungal formulations are available over-the-counter and are used tomanage fungal infections including tinea infections, vulvovaginal candidiasis, and onychomycosis. 3 Dataregarding the safety and efficacy in children varies among the products.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.172
National and international consensus guidelines which discuss the management of fungal infections focusprimarily on superficial mycotic infections. Several guidelines list topical antifungal agents or subclasses,and generally do not give preference to one agent versus another. 4-9,11-13 According to these guidelines,mycological and clinical cure of noninvasive fungal infections are often achieved with topical therapyalone. 4-9,11-13 Evidence-based recommendations for the management of fungal infections as presentedwithin the limited guidelines and published literature are discussed below.For candidal onychomycosis, oral antifungal agents are more effective than the skin and mucous membraneantifungals. 7,13 Ciclopirox is the only agent from this class that is FDA approved for candidalonychomycosis. Based on a comprehensive review of the published literature, ciclopirox topical 8%solution demonstrated a statistically significant improvement over placebo in both clinical and mycologicalcure after 28 days to 48 weeks of therapy (P
egardless of dosage formulation: econazole vs. clotrimazole, clotrimazole vs. terbinafine, ciclopirox QDvs. ciclopirox BID. 79,81,83,93,95,96 In a parallel group study, both naftifine and terbinafine were associatedwith a better improvement in clinical and mycological cure when directly compared to oxiconazole(P
References1. McEvoy GK, ed. [2006]. AHFS Drug Information: Skin and Mucous Membrane Agents 84:00: Antifungals84.04.08, [monograph on the Internet]. Bethesda, MD: American Society of Health-System Pharmacists.Available at:http://online.statref.com/Document/Document.aspx?FxId=1&StartDoc=1099&EndDoc=1100&Level=4&Offset=38&State=False&SessionId=7A5C72TJCRQOBHCL [2006 Sept 21].2. Micromedex® Healthcare Series, (electronic version). Thomson Micromedex, Greenwood Village, CO, USA.Available at: http://www.thomsonhc.com. Accessed October 15, 2006.3. Orange Book [database on the Internet]. U.S. Department of Health and Human Services / Food and DrugAdministration / Center for Drug Evaluation and Research. c2006 [cited 2006 Oct 27]. Available at:http://www.fda.gov/cder/ob/default.htm.4. Stevens DL, Bisno AL, Chambers HF, Everett ED, Dellinger P, Goldstein EJ, Gorbach SL, Hirschmann JV,Kaplan EL, Montoya JG, Wade JC; Infectious Diseases Society of America. Practice guidelines for thediagnosis and management of skin and soft-tissue infections. Clin Infect Dis. 2005;41:1373-1406.5. Drake LA, Dinehart SM, Farmer ER, et al. Guidelines of care for superficial mycotic infections of the skin:tinea corporis, tinea cruris, tinea faciei, tinea manuum, and tinea pedis. Guidelines/Outcomes Committee.American Academy of Dermatology. J Am Acad Dermatol. 1996;34(2):282-286.6. Drake LA, Dinehart SM, Farmer ER, et al. Guidelines of care for superficial mycotic infections of the skin:pityriasis (tinea) versicolor. Guidelines/Outcomes Committee. American Academy of Dermatology. J Am AcadDermatol. 1996;34(2):287-289.7. Pappas PG, Rex JH, Sobel JD, et al. Guidelines for treatment of candidiasis. Infectious Diseases Society ofAmerica. Clin Infect Dis. 2004;38:161-189.8. Mendling W, Seebacher C. Guideline vulvovaginal candidosis. Guideline of the German DermatologicalSociety, the German Speaking Mycological Society and the Working Group for Infections andInfectimmunology of the German Society for Gynecology and Obstetrics. Mycoses. 2003;46:365-369.9. Association of Genitourinary Medicine and the Medical Society for the Study of Venereal Diseases <strong>Clinical</strong>Effectiveness Group. National guideline for the management of vulvovaginal candidiasis. Sex Transm Inf.1999;75(Suppl 1):S19-S20.10. Watson MC, Bond CM. Evidence-based guidelines for non-prescription treatment of vulvovaginal candidiasis.Grampian Evidence Based Community Pharmacy Guidelines Group. Pharm World Sci. 2003;25(4):129-134.11. Department of Health and Human Services. Centers for Disease Control and Prevention. Diseases characterizedby vaginal discharge. Sexually treated diseases treatment guidelines. MMWR. 2002;51(RR-6):42-48.12. Sherread J. European guideline for the management of vaginal discharge. European Branch of the InternationalUnion against Sexually Transmitted Infection and the European Office of the World Health Organization. Int JSTD AIDS. 2001;12(Suppl 3):73-77.13. Roberts DT, Taylor WD, Boyle J. Guidelines for treatment of onychomycosis. British Association ofDermatologists. Br J Dermatol. 2003;148:402-410.14. Amphotericin B: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.15. Mentax ® [package insert]. San Antonio, TX: Bertek Pharmaceuticals; June 2001.16. Mentax-TC ® [package insert]. San Antonio, TX: Bertek Pharmaceuticals; October 2002.17. Gynazole-1 ® [package insert]. St. Louis, MO: KV Pharmaceutical Co; August 2003.18. Loprox ® [package insert]. Scottsdale, AZ: Medicis Pharmaceutical Corp.; February 2003.19. Loprox ® [package insert]. Scottsdale, AZ: Medicis Pharmaceutical Corp.; May 2002.20. Ciclopirox olamine: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.21. Clotrimazole: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.22. Econazole [package insert]. Melville, NY: E. Fougera & Co.: November 2002.23. Econazole: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.24. Ketoconazole [package insert]. Sellersville, PA: Teva Pharmaceuticals: August 1999.25. Xolegel ® [package insert]. Princeton, NJ: Barrier Therapeutics, Inc.; July 2006.26. Miconazole: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.27. Naftifine: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.28. Nystatin: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.29. Oxistat ® [package insert]. Pittsburgh, PA: GlaxoSmithKline Comsumer HealthCare LP: January 2004.30. Ertaczo ® [package insert]. Research Triangle Park, NC: Bertek Pharmaceutical, Inc; December 2003.31. Exelderm ® [package insert]. Buffalo, NY: Westwood-Squibb Pharmaceuticals, Inc.; May 2003.32. Lamisil ® DermGel [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corp; February 2004.175Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
33. Lamisil ® Solution [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corp; March 2003.34. Terbinafine: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.35. Terazol ® [package insert]. Raritan, NJ: Ortho McNeil Pharmaceutical, Inc.; March 2001.36. Tioconazole: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.37. Tolnaftate: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.38. Undecylenic acid: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.39. Wickersham RM, Novak KK, managing eds. Drug Facts and Comparisons. St. Louis, MO; Wolters KluwerHealth, Inc.; 2006.40. Gupta AK, Fleckman P, Baran R, et al. Ciclopirox nail lacquer solution 8% in the treatment of toenailonychomycosis. J Am Acad Dermatol. 2000;43:S70-S80.41. Bagatell FK, Bogaert H, Cullen S, et al. Evaluation of a new antifungal cream ciclopirox olamine 1% in thetreatment of cutaneous candidiasis. Clin Therap. 1985;8(1):41-48.42. Clayton YM, Connor BL. Comparison of clotrimazole cream, Whitfield’s ointment and nystatin ointment forthe topical treatment of ringworm infections, pityriasis versicolor, erythrasma and candidiasis. Brit J Dermatol.1973;89:297-303.43. Tanenbaum L, Anderson C, Rosenberg, et al. A new treatment for cutaneous candidiasis: sulconazole nitratecream 1%. Int J Dermatol. 1983;22(5):318-320.44. Kirkpatrick CH, Alling DW. Treatment of chronic oral candidiasis with clotrimazole troches: a controlledclinical trial. NEJM. 1978;299(22):1202-1203.45. Owens NJ, Nightingale CH, Schweizer RT, et al. Prophylaxis of oral candidiasis with clotrimazole troches.Arch Intern Med. 1984;144:290-293.46. Droegemueller W, Adamson DG, Brown D, et al. Three-day treatment with butoconazole nitrate forvulvovaginal candidiasis. Obstet Gynecol. 1984;64(4):530-534.47. Hajman AJ. Vulvovaginal candidosis: comparison of 3-day treatment with 2% butoconazole nitrate cream and6-day treatment with 1% clotrimazole cream. J Int Med Research. 1988;16:367-375.48. Brown D, Henzl MR, Kaufman RH, et al. Butoconazole nitrate 2% for vulvovaginal candidiasis: new singledosevaginal cream formulation vs., seven-day treatment with miconazole nitrate. J Reprod Med. 1999;44:933-938.49. Kaufman RH, Henzl MR, Brown D, et al. Comparison of three-day butoconazole treatment with seven-daymiconazole treatment for vulvovaginal candidiasis. J Reprod Med. 1989;34(July):479-483.50. Higton BK. A trial of clotrimazole and nystatin in vaginal candidiasis. Postgrad Med J. 1974;7:95-97.51. Stein GE, Gurwith D, Mummaw N, et al. Single-dose tioconazole compared with 3-day clotrimazole treatmentin vulvovaginal candidiasis. Antimicrobial Agents Chemo. 1986;29(6):969-971.52. Davis JE, Frudenfeld JH, Goddard JL. Comparative evaluation of Monistat and Mycostatin in the treatment ofvulvovaginal candidiasis. Obstet Gynecol. 1974;44(3):403-406.53. Cohen L. Treatment of vaginal candidosis using clotrimazole vaginal cream: single dose versus 3-day therapy.Curr Med Res Opin. 1985;9:520-523.54. Fluery F, Hughes D, Floyd R. Therapeutic results obtained in vaginal mycoses after single-dose treatment with500 mg clotrimazole vaginal tablets. Am J Obstet Gynecol. 1985;152:968-970.55. Lebherz T, Guess E, Wolfson N. Efficacy of single- versus multiple-dose clotrimazole therapy in themanagement of vulvovaginal candidiasis. Am J Obstet Gynecol. 1985;152(7):965-968.56. Thomason JL, Gelbart SH, Kellett AV, et al. Terconazole for the treatment of vulvovaginal candidiasis. JReproduc Med. 1990;35(11):992-994.57. Jacobson JB, Hajman AJ, Wiese J, et al. A new vaginal antifungal agent. Acta Obstet Gynecol Scand.1985;64:241-244.58. Corson SL, Kapikian RR, Nehring R. Terconazole and miconazole cream for treating vulvovaginal candidiasis:a comparison. J Reproduc Med. 1991;36(8):561-567.59. Hirsch HA. <strong>Clinical</strong> evaluation of terconazole. J Reproduc Med. 1989;34(8):593-596.60. Brown D, Henzl, Lepage ME, et al. Butoconazole vaginal cream in the treatment of vulvovaginal candidiasis:comparison with miconazole nitrate and placebo. J Reprod Med. 1986;31(11):1045-1048.61. Young GL, Jewell D. Topical treatment of vaginal candidiasis (thrush) in pregnancy. Cochrane Database ofSyst Rev. 2001;4: CD000225.62. Thomason JL. <strong>Clinical</strong> evaluation of terconazole. J Reproduc Med. 1989;3(8):597-60163. Aly R, Katz HI, Kempers SE, et al. Ciclopirox for seborrheic dermatitis of the scalp. Int J Dermatol.2003;42(Suppl 1):19-22.64. Vardy DA, Zvulunov A, Tchetov T, et al. A double-blind, placebo-controlled trial of a ciclopirox olamine 1%shampoo for the treatment of scalp seborrheic dermatitis. J Dermatol. 2000;11:73-77.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.176
65. Green, CA, Farr PM, Shuster S. Treatment of seborrheic dermatitis with ketoconazole: II. Response toseborrheic dermatitis of the face, scalp and trunk to topical ketoconazole. Brit J Dermatol. 1987;116:217-221.66. Cauwenbergh G, Doncker PD, Schrooten R, et al. Treatment of dandruff with a 2% ketoconazole scalp gel: adouble-blind placebo-controlled study. Int J Dermatol. 1986;25(8):541-542.67. Elewski B, Ling MR, Phillips TJ. Efficacy and safety of a new once-daily topical ketoconazole 2% gel in thetreatment of seborrheic dermatitis: phase III trial. J Drugs Dermatol. 2006;5(7):646-650.68. Carr MM, Pryce DM, Ive FA. Treatment of seborrheic dermatitis with ketoconazole: I. response of seborrheicdermatitis of the scalp to topical ketoconazole. Brit J Dermatol. 1987;116:213-216.69. Franchimont CP, Pierard GE, Arrese JE, et al. Effect of ketoconazole 1% and 2% shampoos in severe dandruffand seborrheic dermatitis: clinical, squamometric and mycological assessments. Dermatol. 2001;202:171-176.70. Wu YC, Chuan MT, Lu YC. Efficacy of ciclopiroxolamine 1% cream in onychomycosis and tinea pedis.Mycoses. 1991;34:93-95.71. Kagawa S. <strong>Clinical</strong> efficacy of terbinafine in 629 Japanese patients with dermatomycosis. 1989;14:114-115.72. Reyes BA, Beutner KR, Cullen S, et al. Butenafine, a fungicidal benzylamine derivative, used once daily for thetreatment of interdigital tinea pedis. Int J Dermatol. 1997;37:433-453.73. Tschen E, Elewski B, Gorsulowsky, et al. Treatment of interdigital tinea pedis with a 4-week once- dailyregimen of butenafine hydrochloride 1 % cream. J Am Acad Dermatol. 1997;36:S9-S14.74. Aly R, Fisher G, Katz, et al. Ciclopirox gel in the treatment of patients with interdigital tinea pedis. Int JDermatol. 2003;42(Suppl 1): 29-35.75. Mandy SJ, Garrott TC, Miconazole treatment for severe dermatophytoses. JAMA. 1974;230(1):72-75.76. Jordan RE, Rapini RP, Rex IH, et al. Once-daily naftifine cream 1 % in the treatment of tinea cruris and tineacorporis. Int J Dermatol. 1990;29(6):441-442.77. Van Esso D, Fajo G, Losada I, et al. Sertaconazole in the treatment of pediatric patients with cutaneousdermatophyte infections. Clin Therap. 1995;17(2):264-269.78. Villars V, Jones TC. <strong>Clinical</strong> efficacy and tolerability of terbinafine (lamisil)- a new topical and systemicfungicidal drug for the treatment of dermatomycoses. Clin Experimental Dermatol. 1989;14:124-127.79. Kamalam A, Thambiah AS. Clotrimazole and econazole in dermatophytoses (a double blind study). Mykosen.1980;23(12):707-710.80. Lassus A, Forstrom S, Salo O. A double-blind comparison of sulconazole nitrate 1 % cream with clotrimazole 1% cream in the treatment of dermatophytoses. Brit J Dermatol. 1983;108:195-198.81. Rajan VS, Thirumoorthy T. Treatment of cutaneous candidiasis: a double blind parallel group comparison ofsulconazole nitrate 1% cream and clotrimazole 1% cream. Australas J Dermatol. 1983;24:33-3682. Tham SN. Treatment of pityriasis versicolor: comparison of sulconazole nitrate 1% solution and clotrimazole1% solution. Australas J Dermatol. 1987;28:123-125.83. Patel A, Brookman SD, Bullen MU, et al. Topical treatment of interdigital tinea pedis: terbinafine comparedwith clotrimazole. Austral J Dermatol. 1999;40:197-200.84. Petres HV, Kunze J, Muller RPA. Double-blind parallel study comparing sulconazole with econazole in thetreatment of dermatophytoses. Mykosen. 1984;27(12):592,595-598.85. Grigoriu D, Grigoriu A. Double-blind comparison of the efficacy, toleration, and safety of tioconazole base 1%and econazole nitrate 1% cream in the treatment of patients with fungal infections of the skin or erythrasma.Dermatologica. 1983;166(Suppl 1):8-13.86. Bonifaz A, Saul A. Comparative study between terbinafine 1% emulsion-gel versus ketoconazole 2% cream intinea cruris and tinea corporis. Eur J Dermatol. 2000;10:107-109.87. Tanenbaum L, Anderson C, Rosenberg MJ. 1% sulconazole cream v 2% miconazole cream in the treatment oftinea versicolor: a double blind, multicenter study. Arch Dermatol. 1984;120:216-219.88. Tanenbaum L, Anderson C, Rosenberg MJ. Sulconazole nitrate 1.0 percent cream: a comparison withmiconazole in the treatment of tinea pedis and tinea cruris/corporis. Cutis. 1982;30:105-107,115, 118.89. Vander Ploeg DE, De Villez RL. A new topical antifungal drug. Int J Dermatol. 1984;23(10):681-683.90. Fredriksson T. Treatment of dermatomycoses with topical tioconazole and miconazole. Dermatologica.1983;166(Suppl 1)14-19.91. Ramelet AA, Walker-Nasir E. One daily application of oxiconazole cream is sufficient for treatingdermatomycoses. Dermatologica. 1987;175:293-295.92. Bogaert H, Cordero C, Ollague W, et al. Multicentre double-blind trial of ciclopirox olamine cream 1% in thetreatment of tinea corporis and tinea cruris. J Int Med Res. 1986;14:210-216.93. Fuerst JF, Cox GF, Weaver SM, et al. Comparison between undecylenic acid and tolnaftate in the treatment oftinea pedis. Cutis. 1980;25:544-547.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.177
94. Ablon G, Rosen T, Spedale J. Comparative efficacy of naftifine, oxiconazole, and terbinafine in short-termtreatment of tinea pedis. Int J Dermatol. 1996;35(8):591-593.95. Tschen EH, Becker LE, Ulrich JA, et al. Comparison of over-the-counter agents for tinea pedis. Cutis.1979;23:696-69896. Gupta AK, Skinner AR, Cooper EA. Evaluation of the efficacy of ciclopirox 0.77% gel in the treatment of tineapedis interdigitalis (dermaphytosis complex) in a randomized, double-blind placebo-controlled trial. Int JDermatol. 2005;44:590-593.97. Pariser DM, Pariser RJ. Oxiconazole nitrate lotion, 1 percent: an effective treatment for tinea pedis. Cutis.1994;54:43-44.98. Tanenbaum L, Taplin D, Lavelle C, et al. Sulconazole nitrate cream 1 percent for treating tinea cruris andcorporis. Cutis. 1989;44:344-347.99. Sivayathorn A, Piamphongsant. Topical antimycotic agents for the treatment of superficial dermatophytoses inThailand – a double-blind study. Mykosen. 1978;22(1):21-24.100. Aly R, Bagatell FK, Dittmar W, et al. Ciclopirox olamine lotion 1%: bioequivalence to ciclopirox olaminecream 1 % and clinical efficacy in tinea pedis. Clin Therap. 1989;11(3):290-303.101. Hart R, Bell-Syer SE, Crawford F, et al. Systematic review of topical treatments for fungal infections of the skinand nails of the feet. BMJ. 1999;319:79-82.102. Crawford F, Hart R, Bell-Syer S, et al. Topical treatments for fungal infections of the skin and nails of the foot.Cochrane Database Syst Rev. 2006;3.103. Lipsky MS, Waters T, Sharp L, et al. Impact of vaginal antifungal products on utilization of health careservices: evidence from physician visits. J Am Board of Fam Pract. 2000;13(3):178-182.104. Gurwitz JH, McLaughlin TJ, Fish LS. The effect of an Rx-to-OTC switch on medication prescribing patternsand utilization of physician services: the case of vaginal antifungal products. Health Serv Res. 1995;30(5):672-685.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.178
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane AntifungalsCombination ProductsAHFS Class 840408February 7, 2007I. OverviewThe agents discussed within this review are identified by the American Hospital Formulary Service ascombination skin and mucous membrane antifungals. 1 These combination products are available byprescription only and some of them are available generically (clotrimazole/betamethasone dipropionate,nystatin/triamcinolone, and sodium thiosulfate/salicylic acid). 2,3 These combination products are Food andDrug Administration (FDA)-approved for the treatment of fungal infections (e.g., cutaneous candidiasis,tinea corporis, tinea cruris, tinea pedis, tinea versicolor), dermatitis, eczema, mild cervicitis or postpartum1,2, 4-20healing.The combination of benzoic acid and salicylic acid is indicated for inflammatory conditions, such asdermatitis, and has an unknown mechanism of action. 4 In animal studies, this combination of agentsimproved wound healing through re-epithelialization. 4 As single entities, they work as follows: benzoicacid has antifungal and antibacterial properties, and salicylic acid exerts keratolytic effects that suppressfungal growth. 2,4,5 In combination, these active ingredients are used in the treatment of fungal skininfections. 2,5The combination product containing clotrimazole and betamethasone dipropionate is approved for commontinea infections (i.e., corporis, cruris, pedis). 6 This combination product was designed to provide antifungalactivity via clotrimazole in addition to corticosteroidal activity via bethamethasone. 6-8 By inhibiting 14-αdemethylationof lanosterol, clotrimazole increases methylsterol levels and decreases ergosterol formation,leading to fungal cell death or growth inhibition due to compromised cell integrity. 7 By controlling hostinflammation in tinea infections, betamethasone dipropionate indirectly increases tinea infection cure rate. 8A similar antifungal/corticosteroid combination product, miconazole and hydrocortisone, is also approvedfor use in the treatment of fungal infections (i.e., cutaneous candidiasis, tinea corporis, tinea pedis). 9,10Approved for cutaneous candidiasis, the nystatin and triamcinolone acetonide combination product alsoconsists of an antifungal and a corticosteroid component, respectively. 13 Nystatin provides antifungalactivity by binding to sterols and preventing proper cell membrane formation; triamcinolone acetonideprovides corticosteroidal activity. 13-15 Another combination product consists of two antifungal agents:sodium thiosulfate and salicylic acid. 19,20 This combination product is approved for the treatment of tineaversicolor. 19The combination agent containing miconazole and zinc oxide is specifically approved as an adjunct agentfor treatment of diaper dermatitis. 9,11,12 As a skin protectant and mild astringent with weak antisepticproperties, zinc oxide promotes healing in cutaneous candidiasis while miconazole provides mycologicalcure of the fungal infection. 9,11,12The amino acid cervical cream which contains sodium propionate, urea, inositol (excipient according toUSP), and amino acids combination no. 14 is approved for mild cervicitis and postpartum healing. 16,18 Theamino acid combination (i.e., methionine and cystine) is necessary in wound healing. Inositol promotestissue growth and urea works by removing dead or damaged tissues. 19 Sodium propionate provides abacteriostatic effect. 19 Other ingredients in the amino acid cervical cream are listed as inactiveingredients. 19The combination skin and mucous membrane antifungals that are included in this review are listed in Table1. This review encompasses all (topical) dosage forms and strengths.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.179
Table 1. Combination Skin and Mucous Membrane Antifungals Included in this <strong>Review</strong>Generic Name(s) Formulation(s) Example Brand Current PDL Agent(s)Name(s)amino acids (methionine/cystine), inositol, sodiumpropionate, and ureavaginal cream N/A amino acids(methionine/cystine),inositol, sodiumpropionate, and ureabenzoic acid and salicylic acid ointment Bensal HP ® noneclotrimazole and betamethasonedipropionatecream, lotion Lotrisone ® * clotrimazole andbetamethasonedipropionatemiconazole and hydrocortisone combination Fungoid & HC ® nonepackagemiconazole and zinc oxide ointment Vusion ® nonenystatin and triamcinolone cream, Mycolog II†* nystatin andsodium thiosulfate and salicylicacid*Generic is available in at least one dosage form or strength.†Brand is no longer available.N/A=not availableointmenttriamcinolonelotion N/A sodium thiosulfate andsalicylic acidII.Evidence-Based Medicine and Current Treatment GuidelinesCurrent national and international treatment guidelines that would incorporate the combination skin andmucous membrane antifungals are summarized in Table 2.Table 2. Treatment Guidelines Using the Combination Skin and Mucous Membrane Antifungals<strong>Clinical</strong> GuidelineRecommendation(s)Infectious Diseases Society ofAmerica (IDSA): PracticeGuidelines for the Diagnosisand Management of Skin andSoft-Tissue Infections 21 ••Immunocompromised patients are more susceptible toopportunistic fungal infections.Noninvasive fungal infections may be treated with skincare and a topical antifungal agent; alternatively, a shortcourse systemic azole antifungal agent may be used.• Oral and intravenous (IV) agents (e.g., amphotericin B,voriconazole, caspofungin, fluconazole, and itraconazole)are initiated empirically in immunocompromised patientspresenting with neutropenia; these agents may be used totreat invasive fungal infections.• Specific combination products were not addressed withinthe guidelines.American Academy ofDermatology (AAD),Guidelines/Outcomes Committee:Guidelines of Care forSuperficial Mycotic Infectionsof the Skin: Tinea Corporis,Tinea Cruris, Tinea Faciei,Tinea Manuum, and TineaPedis 22 ••Topical antifungal agents are used in the treatment ofnoninflammatory tinea corporis, tinea cruris, tinea faciei,tinea manuum, and tinea pedis; systemic oral agents areused for other tinea conditions.Examples of topical antifungal agents include azoles(e.g., clotrimazole, econazole, ketoconazole, miconazole,oxiconazole, and sulconazole), allylamines (e.g., naftifineand terbinafine), ciclopirox, miscellaneous agents (e.g.,benzoic acid, tolnaftate, haloprogin, drying agents,powders, and salicylic acid), and combination topicalcorticosteroid antifungal mixtures.• Examples of systemic antifungal agents includegriseofulvin, ketoconazole, terbinafine, itraconazole, andfluconazole.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.180
<strong>Clinical</strong> GuidelineRecommendation(s)• Specific combination products were not addressed withinthe guidelines; however, salicylic acid products, benzoicacid products (e.g., Whitfield’s Ointment ® ), andcombination topical corticosteroid antifungal mixtureswere identified as potential treatment options fornoninflammatory tinea infections.American Academy ofDermatology (AAD),Guidelines/Outcomes Committee:Guidelines of Care forSuperficial Mycotic Infectionsof the Skin: Pityriasis (Tinea)Versicolor 23 ••Topical antifungal agents are used in treatment of mildcases of tinea versicolor.Systemic antifungal agents are used in the treatment oftinea versicolor in patient who have failed topicaltherapy, have recurrent infections, or have extensive skininvolvement. Concurrent therapy with topical antifungalagents is acceptable.• Examples of topical antifungal agents include azoles(e.g., clotrimazole, econazole, ketoconazole, miconazole,oxiconazole, and sulconazole), ciclopirox, andmiscellaneous agents (e.g., selenium sulfide, zincpyrithione, sulfur, salicylic acid, propylene glycol, andbenzoyl peroxide).• Examples of systemic antifungal agents includeketoconazole, itraconazole, and fluconazole.• Specific combination products were not addressed withinthe guidelines; however, a combination productcontaining salicylic acid was identified as a potentialInfectious Diseases Society ofAmerica (IDSA): Guidelines forthe Treatment of Candidiasis 24treatment option for tinea versicolor.Candidal skin infection• Topical azoles and polyenes are effective.Cutaneous neonatal candidiasis• Topical agents may be used for primary cutaneousdisease in healthy, normal-birth-weight, term infants.• Specific combination products were not addressed withinthe guidelines.Primary Care Dermatology • Recommendations for prevention include avoidance ofof Atopic Eczema 25 • Emollients should be applied three to four times daily onSociety and the Britishexacerbating factors and maintenance of well-hydratedAssociation of Dermatologists: skin.Guidelines for the Management • Early treatment of infections is recommended.moist skin up to 600 g/week for adults and 250 g/weekfor children. Use of combined emollient andcorticosteroid should meet the ratio of 10:1.• Topical corticosteroids should be used a few days foracute eczema and up to 4 to 6 weeks for chronic eczema.More potent corticosteroids are indicated in eczema ofthe hands and feet.• Immunomodulatory agents may be initiated if a patient isintolerant to corticosteroids, or has failed corticosteroidtherapy.• Sedating systemic antihistamines are more effective thannonsedating ones for relief of pruritus.• Short courses of corticosteroid-antibiotic combinationsare effective in clinical practice, but published evidencebasedliterature on their efficacy is lacking.• Specific combination products were not addressed withinthe guidelines.181Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
<strong>Clinical</strong> GuidelineRecommendation(s)European Task Force on AtopicDermatitis: Position Paper onDiagnosis and Treatment ofAtopic Dermatitis 26 ••Emollients should be applied at least twice daily up to150-200 g/week for children and 500 g/week for adults.Topical corticosteroids are first-line anti-inflammatorytreatment to be given two to three times weekly up to 15g/month for infants, up to 30 g/month for children, up to60-90 g/month for adults.• Topical calcineurin inhibitors should be initiated if apatient is intolerant or has failed corticosteroid therapy;tacrolimus 0.1% is equipotent to a corticosteroid withintermediate activity and is more potent thanpimecrolimus 1.0%.• Systemic anti-inflammatory agents are reserved for lastlineuse, when intolerance to all topical treatment hasbeen exhausted.• Sedating systemic antihistamines are more effective thannonsedating ones for relief of pruritus.• There is no conclusive clinical data supporting the use ofanti-infectious agents in the absence of clinical signs ofinfection in atopic dermatitis.• Specific combination products were not addressed withinthe guidelines.European Academy ofAllergology and <strong>Clinical</strong>Immunology/American Academyof Allergy, Asthma andImmunology/PRACTALLConsensus Group: Diagnosis andTreatment of Atopic Dermatitisin Children and Adults 27 •••Topical antiseptics may be used in emollients to reduceskin colonization of Staphylococcus aureus and skinsymptoms.A combination antimicrobial and topical corticosteroid ismore effective than topical corticosteroid monotherapy.All other guideline statements are similar to thosepresented by the European Task Force on AtopicDermatitis. 26American Academy ofDermatology (AAD),Guidelines/Outcomes Task Force:Guidelines of Care for AtopicDermatitis 28 ••Tar may be effective but its use is limited by compliancedue to cosmetic issues.Topical doxepin may be effective in reducing pruritus butits use is limited by side effects of sedation and contactallergies.• All other guideline statements are similar to thosepresented by the European Task Force on AtopicDermatitis. 26III.IndicationsFDA-approved indications for the combination skin and mucous membrane antifungals are noted in Table3.Table 3. FDA-Approved Indications for the Combination Skin and Mucous Membrane Antifungals 1,2,4-20Drug(s) CutaneousCandidiasisTineacorporisTineacrurisTineapedisTineaversicolorDermatitis/EczemaAmino acids(methionine/cystine), inositol,sodium propionate,and ureaBenzoic acid and a*Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.182Mild Cervicitis/PostpartumHealinga
Drug(s)salicylic acidClotrimazole andbetamethasonedipropionateMiconazole andhydrocortisoneMiconazole andzinc oxideNystatin andtriamcinoloneSodium thiosulfateand salicylic acidCutaneousCandidiasisTineacorporisTineacrurisTineapedisa a aTineaversicolorDermatitis/Eczemaa a a aa†a*FDA approved for the treatment of nonspecific dermatitis/eczema/ fungal infections, insect bites, and burns†FDA approved as an adjunctive agent in the treatment of diaper dermatitisaMild Cervicitis/PostpartumHealingIV.PharmacokineticsThe pharmacokinetic parameters for the combination skin and mucous membrane antifungals aresummarized in Table 4.Table 4. Pharmacokinetic Parameters of the Combination Skin and Mucous Membrane Antifungals 1,2,4-20Drug(s) Systemic Distribution ExcretionMetaboliteAbsorption(kidney)Benzoic acid Not appreciablyabsorbedNo data Yes Benzoylglucuronic acid*,hippuric acid*Betamethasone 12%-14% 64% protein bound
V. Drug InteractionsDue to limited systemic absorption when these combination skin and mucous membrane antifungals areadministered topically, no drug interactions are likely to occur and none are documented with thesecombination skin and mucous membrane antifungals. Of note, the oral, single entity formulations of theseantifungal agents may have a more extensive drug interaction profile due to increased systemic absorption.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.184
VI.Adverse Drug EventsThe most common adverse drug events reported with the individual agents in the combination skin and mucous membrane antifungals are noted in Table 5.Topical agents are typically not associated with systemic adverse effects. Of note, the oral formulations of the following antifungal agents have differentsafety profiles than those presented below. Azole antifungals may be associated with unpredictable cross-sensitivity within this particular class.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.185SodiumThiosulfateTable 5. Adverse Drug Events (%) Reported with the Combination Skin and Mucous Membrane Antifungals 1,2,4-20Adverse Event(s) BenzoicAcidBetamethasoneClotrimazoleHydrocortisoneMiconazole Nystatin SalicylicAcidTriamcinoloneDermatologicalAcne - a - - - - - - a -Burning - a - - a - a - a -Dermatitis - a - - a a - a a -Dry skin - a - 2 - - - - a -Eczema - - - 12.5 - - - - - -Erythema - a - - - - - - - -Folliculitis - a - - - - - - a -Hypertrichosis - a - - - - - - a -Hypopigmentation - - - - - - - - a -Irritation a a a - - - a a a 1-10Maceration - - - - a - - - a -Miliaria - a - - - - - - a -Oral mucosa atrophy - - - - - - - - a -Peeling - - - - - - a - - -Pigmentary changes - - - - - - - - - -Perioral dermatitis - - - - - - - - a -Pruritis - a a 6 - - - - a -Rash - - - - - - - - - -Scaling - - - - - - a - - -Sensitization - - - - - - - - - aSkin atrophy - a - - - - - - a -Skin infection (secondary) - - - - - - - - a -Stinging - - - 2 - - - - - -Stevens-Johnson syndrome - - - - - a - - - -Striae - a - - - - - - a -Urticaria a - - - - - - - - -Vesiculation - a - - - - - - - -*No data on adverse effects found for the product containing sodium propionate, cystine, inositol, methionine, and urea.a Percent not specified.- Not reported.Zincoxide
VII.Dosing and AdministrationThe usual dosing regimens for the combination skin and mucous membrane antifungals are summarized inTable 6. The duration of therapy for a particular agent is dependent on the specific indication for which itis being used.Table 6. Usual Dosing for the Combination Skin and Mucous Membrane Antifungals 1,2,4-20Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityAmino acids(methionine/cystine),inositol, sodiumpropionate, and ureaCervicitis:Cream: insert 1applicatorful at bedtime fortwo weeksSafety and efficacy inchildren have not beenestablished.Cream:8.34%/0.83%/0.35%/0.83%Postpartum healing:Benzoic acid andsalicylic acidClotrimazole andbetamethasonedipropionateCream: insert 1applicatorful at bedtime forfour weeksDermatitis/eczema:Ointment: initial, apply toaffected area(s) of skintwice dailyTinea corporis, tinea cruris:Cream, lotion: initial, applyto affected area(s) of skintwice daily for one to twoweeks; maximum, 45g/week.Safety and efficacy inchildren have not beenestablished.Safety and efficacy inpatients less than 17 yearsof age have not beenestablished.Ointment: 6%/3%Cream: 1%/0.05%Lotion: 1%/0.05%Tinea pedis:Miconazole andhydrocortisoneMiconazole and zincoxideCream, lotion: initial, applyto affected area(s) of skintwice daily for two to fourweeks; maximum, 45g/weekCutaneous candidiasis, tineacorporis, tinea pedis:Cream: apply to affectedarea(s) twice dailyDiaper dermatitis:Ointment: apply to affectedarea(s) of skin at eachdiaper change for sevendaysSafety and efficacy inchildren have not beenestablished.For infants aged 4 weeksand older:Diaper dermatitis:Ointment: apply toaffected area(s) of skin ateach diaper change for 7daysCream: 2%/0.5%Ointment:0.25%/15%/81.35%186Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityCutaneous candidiasis: Cutaneous candidiasis: Cream:100,000 U/g, 0.1%Nystatin andtriamcinoloneSodium thiosulfateand salicylic acidCream, ointment: apply toaffected area(s) of skintwice daily up to 25 daysTinea versicolor:Lotion: apply to affectedarea(s) of skin twice dailyCream, ointment: apply toaffected area(s) of skinonce to twice daily up to25 daysSafety and efficacy inchildren have not beenestablished.Ointment:100,000 U/g, 1%Lotion: 25%/1%Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.187
VIII. Effectiveness<strong>Clinical</strong> studies evaluating the safety and efficacy of the combination skin and mucous membrane antifungals are summarized in Table 7.Table 7. Comparative <strong>Clinical</strong> Trials Using the Combination Skin and Mucous Membrane AntifungalsStudyandDrug RegimenStudy DesignandDemographicsEnd PointsCandidiasis (Cutaneous)Beveridge et al. 29Nystatin cream applied toaffected area(s) of skin onright/left armvs.nystatin/triamcinoloneacetonide combinationcream applied to affectedarea(s) of skin on the otherarmDermatitis/EczemaHarcup et al. 30Miconazole 2%/hydrocortisone 1%combination ointmentapplied to affected area(s) ofskin QAM and QPMDB, MC, PG,RCTPatients aged 6months to 71years withconfirmedbilateral Candidallesions of theflexuresOS, MCPatients aged 35to 74 years oldwith eczematouslesions with orwithout bacterialsuperinfectionSampleSizeand StudyDurationN=3114 daysN=7314 to 28daysPrimary:Eradication ofCandida, clinicalprogress oflesions, patientpreference foragent, physicianpreference foragentSecondary:Adverse eventsPrimary:Investigatorassessments(severity ofsymptoms, globalevaluation ofresponse), patientassessments(daily symptomscores,acceptability)ResultsPrimary:There was little difference between clinical (12/31 [38.7%] vs. 14/31[45%], respectively) and mycological cure (27/31 [87.1%] vs. 26/31[83.8%], respectively) between nystatin and nystatin/triamcinolonetherapies; P value not reported.There was no statistically significant difference in the preference foreither treatment in terms of the patient’s or physician’s perspective(P>0.05).Secondary:Two patients treated with the creams reported burning and stinging.One patient treated with nystatin monotherapy complained of burningand one patient reported pustules.Primary:Investigator-based symptom scores showed a statistically significantimprovement (P
StudyandDrug RegimenConcannon et al. 31Miconazole 0.25% in zincoxide/petrolatum baseapplied to rash at eachdiaper change and afterinfant’s bathvs.zinc oxide/petrolatum baseapplied to rash at eachdiaper change and afterinfant’s bathStudy DesignandDemographicsDB, PC, PG,RCTPatients aged 2 to13 months withacute diaperdermatitisSampleSizeand StudyDurationN=1887 daysEnd PointsPrimary:Number of rashsites, mean totalrash scoreSecondary:Adverse eventsResultsPrimary:On days 5 and 7, patients treated with miconazole/zincoxide/petrolatum had fewer rash sites and lower mean total rash scoresthan patient receiving zinc oxide/petrolatum alone (P
StudyandDrug Regimenoxide/petrolatum ointmentapplied to rash at eachdiaper change and afterinfant’s bathvs.zinc oxide/petrolatumointment applied to rash ateach diaper change and afterinfant’s bathStudy DesignandDemographicsPatients withdiaper dermatitiscomplicated bycandidiasis with aseverity score of3 or higherSampleSizeand StudyDurationEnd Pointscure, overall rateof cure, diaperdermatitis indexscoreSecondary:Adverse eventsResultsoxide/petrolatum (38% vs. 11%, respectively; P
StudyandDrug RegimenStudy DesignandDemographicsSampleSizeand StudyDurationEnd PointsResultsvs.miconazole2%/hydrocortisone 1%combination solutionapplied to whole scalp QPMfor (3 weeks, or up to 6weeks until cured); thenapplied prophylactically toscalp twice monthly (for 3months)Tinea InfectionsClayton et al. 34Clotrimazole 1% creamapplied to affected area(s) ofskin BIDvs.nystatin 100,000 U/gointment applied to affectedarea(s) of skin BIDvs.Whitfield’s Ointment ® (3%salicylic acid, 6% benzoicacid) applied to affectedarea(s) of skin BIDWortzel 35Betamethasone dipropionateapplied to affected area(s) ofDB, AC, RCTPatients aged 13to 63 years oldwith eitherconfirmed tineacorporis, tineapityriasis,erythrasma, orCandidainfectionsDB, MC, RCTPatients withconfirmed tineaN=1034 weeksN=452 weeksPrimary:<strong>Clinical</strong> cure,mycological cureSecondary:Not reportedPrimary:<strong>Clinical</strong> cure,microbiologicalcurePrimary:Relative to patients with confirmed tinea corporis, there was nostatistically significant difference in efficacy in patients treated withclotrimazole or Whitfield’s Ointment ® ; P value not reported.Relative to patients with confirmed tinea pityriasis, there was nostatistically significant difference in efficacy in patients treated withclotrimazole or Whitfield’s ointment; P value not reported.Relative to patients with confirmed erythrasma, there was nostatistically significant difference in efficacy in patients treated withclotrimazole or Whitfield’s ointment; P value not reported.Relative to patients with Candida infections, there was no statisticallysignificant difference in efficacy in patients treated with clotrimazole ornystatin; P value not reported.Secondary:Not reportedPrimary:At the end of 2 weeks, 80%, 20% and 13% of patients treated with thecombination product, clotrimazole only, and betamethasone only,respectively, achieved either complete cure or excellent response to191Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimenskin QAM and QPMvs.clotrimazole applied toaffected area(s) of skinQAM and QPMvs.betamethasonedipropionate/clotrimazole (strengthunspecified) combinationapplied to affected area(s)of skin QAM and QPMKatz et al. 36Betamethasone dipropionate0.05% cream applied toaffected area(s) of skin BIDvs.clotrimazole 1% creamapplied to affected area(s) ofskin BIDvs.betamethasone dipropionate0.05%/clotrimazole 1%combination cream appliedto affected area(s) of skinStudy DesignandDemographicscrurisDB, MC, PG,RCTPatients with amicroscopicallyconfirmedclinical diagnosisof moderate tosevere tinea crurisor tinea corporisSampleSizeand StudyDurationN=3312 weeksEnd PointsSecondary:Adverse eventsPrimary:Total signs andsymptomsseverityscore/clinicalresponse ratings,mycologicfindingsSecondary:Adverse eventstherapy.ResultsAt the end of 2 weeks, 87%, 100% and 46% of patients treated with thecombination product, clotrimazole only, and betamethasone only,respectively, had negative culture.Two weeks after treatment, 93%, 100% and 40% of patients treatedwith the combination product, clotrimazole only, and betamethasoneonly, respectively, achieved either complete cure or excellent responseto therapy.Relative to overall clinical rating of the treatment, the combinationproduct was better than clotrimazole (P=0.013) and betamethasone(P=0.001); clotrimazole was better than betamethasone (P=0.001).Secondary:One patient treated with betamethasone reported severe burning andtingling.Primary:Patients treated with clotrimazole had higher total signs and symptomsscores at baseline (P
BIDStudyandDrug RegimenStudy DesignandDemographicsSampleSizeand StudyDurationEnd PointsResultsAccording to mycologic responses (e.g., negative cultures), thecombination product and clotrimazole were more effective thanbetamethasone dipropionate (63% vs. 51% vs. 32%, respectively;P
Additional EvidenceDose SimplificationAn evidence-based medicine literature search did not reveal data pertinent to this topic.Stable TherapyAn evidence-based medicine literature search did not reveal data pertinent to this topic.Impact on Physician VisitsAn evidence-based medicine literature search did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 8. Relative Cost of the Combination Skin and Mucous Membrane AntifungalsGeneric Name(s) Formulation(s) Example Brand Brand Generic CostName(s) Costamino acidsvaginal cream N/A N/A $(methionine/cystine),inositol, sodium propionate,and ureabenzoic acid and salicylic ointment Bensal HP ® $$$ N/Aacidclotrimazole andcream, lotion Lotrisone ® * $$$ $$betamethasone dipropionatemiconazole andcombination Fungoid & HC ® $$ N/Ahydrocortisonepackagemiconazole and zinc oxide ointment Vusion ® $$$ N/Anystatin and triamcinolone cream, ointment Mycolog II†* N/A $sodium thiosulfate andsalicylic acidlotion N/A N/A $*Generic is available in at least one dosage form or strength.†Brand is no longer available.N/A=not availablePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.194
X. ConclusionsThe combination skin and mucous membrane antifungal agents are approved by the FDA for a number of1,2, 4-20indications, including fungal infections, dermatitis, and mild cervicitis. Clotrimazole/betamethasonedipropionate, nystatin/triamcinolone, and sodium thiosulfate/salicylic acid are available generically ascreams, lotions and/or ointments. There are no over-the-counter products in this class.The national and international consensus treatment guidelines recognize the importance of topicalantifungal agents for the initial treatment of noninvasive fungal infections. 21-24 While the azole derivativesare the antifungals discussed most often; benzoic acid, salicylic acid, and combination corticosteroid andantifungal agents are briefly mentioned as other treatment options. 21-24 For the management of atopic andgeneral dermatitis, topical corticosteroids are indicated for initial therapy if the affected area(s) does notinclude the hands and feet. 25-28 One guideline reports that a corticosteroid/antibiotic combination product iseffective for the treatment of atopic dermatitis, but mentioned there was a lack of data demonstrating thatthese products were more efficacious than the single entity agents. 25 Overall, the consensus treatmentguidelines do not discuss specific combination agents; therefore, the guidelines do not give preference toone product versus another. 21-28Based on a comprehensive literature search, there are a limited number of available clinical trials whichevaluated the safety, and efficacy of the combination skin and mucous membrane antifungals. Productscontaining an antifungal agent and a corticosteroid were the most widely studied. No clinical studies werefound that evaluated the safety and effectiveness of sodium propionate/urea/inositol/amino acid 14 orsodium thiosulfate/salicylic acid. Some of the ingredients in the older combination products were FDAapproved without undergoing rigorous clinical trials to establish their safety and efficacy. Two studiesdemonstrated greater clinical cure of diaper dermatitis in patients treated with miconazole in zincoxide/petrolatum ointment compared to patients treated with zinc oxide/petrolatum ointment alone. 31,32Studies comparing the efficacy of a combination antifungal/corticosteroid product to the individualcomponents have produced mixed results. Worzel noted that betamethasone dipropionate/clotrimazole ledto greater improvement in clinical and microbiological cure of tinea cruris than either monotherapy withbetamethasone dipropionate or clotrimazole. 35 Katz et al. reported that the combination product ofbetamethasone dipropionate/clotrimazole led to greater improvement in total signs and symptom scorescompared to its single entities in patients with tinea corporis or tinea cruris. 36 In both of these studies, thecombination product and the antifungal component were more effective than the single entity corticosteroidwith regards to clinical and/or mycologic response. Compared to baseline, the combination product ofmiconazole/hydrocortisone was effective for the treatment of eczematous lesions; however, there was nocomparator in this study. 30 On the contrary, several studies did not demonstrate that the combinationantifungal/corticosteroid product was more efficacious than the antifungal component alone. 29,30 Oneadditional study reported no statistically significant difference between benzoic acid/salicylic acid andclotrimazole in treating various tinea infections. 34 No studies were found that compared one combinationskin and mucous membrane antifungal agent to another.Adverse effects for these agents are primarily dermatological, with the corticosteroid component associatedwith relatively more side effects. 1,2,4-20 Due to limited systemic absorption associated with topicalapplication of the combination antifungal agents, there are no significant differences in their1,2, 4-20pharmacokinetic profiles and potential drug interactions. The dosing and administration of theseagents are dependent upon the condition being treated and the patient population, with dosing frequencyranging from one to four times daily. 1,2,4-20Therefore, all brand products within the class reviewed are comparable to each other and to the genericsand over-the-counter products in this class and offer no significant clinical advantage over otheralternatives in general use.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.195
XI.RecommendationsNo brand combination skin and mucous membrane antifungal is recommended for preferred status.Alabama Medicaid should accept cost proposals from manufacturers to determine cost effective productsand possibly designate one or more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.196
References1. McEvoy GK, ed. [2006]. AHFS Drug Information: Skin and Mucous Membrane Agents 84:00: Antifungals84.04.08, [monograph on the Internet]. Bethesda, MD: American Society of Health-System Pharmacists.Available at:http://online.statref.com/Document/Document.aspx?FxId=1&StartDoc=1099&EndDoc=1100&Level=4&Offset=38&State=False&SessionId=7A5C72TJCRQOBHCL [2006 Sept 21].2. Micromedex® Healthcare Series, (electronic version). Thomson Micromedex, Greenwood Village, CO, USA.Available at: http://www.thomsonhc.com. Accessed October 15, 2006.3. Orange Book [database on the Internet]. U.S. Department of Health and Human Services / Food and DrugAdministration / Center for Drug Evaluation and Research. c2006 [cited 2006 Oct 27]. Available from:http://www.fda.gov/cder/ob/default.htm.4. Bensal HP® [package insert]. Bellefonte, PA: AciesHealth, Inc.: February 2006.5. Salicylic acid: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.6. Lotrisone® Cream, USP Lotrisone® Lotion [package insert]. Kenilworth, NJ: Schering Corporation/KeyPharmaceuticals: March 2003.7. Clotrimazole: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.8. Betamethasone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.9. Miconazole: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.10. Hydrocortisone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.11. Vusion® [package insert]. Princeton, NJ: Barrier Therapeutics, Inc.: February 2006.12. Zinc oxide: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.13. Nystatin and triamcinolone acetonide cream USP Nystatin and triamcinolone acetonide ointment USP[package insert]. Bramalea, Ontario, Canada: TARO Pharmaceuticals, Inc.: March 1994.14. Nystatin: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.15. Triamcinolone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.16. Amino Acid Cervical ® Cream [monograph in the Internet]. Scottsdale, AZ: Hope Pharmaceuticals: 1998-2005[cited 2006 Nov 8]. Available from: http://www.hopepharm.com/amino/index.htm17. Urea: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.18. Inositol: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.19. Versiclear® Lotion [monograph in the Internet]. Scottsdale, AZ: Hope Pharmaceuticals: 1998-2005 [cited2006 Nov 8]. Available from: http://www.hopepharm.com/versiclear/prescribe.html.20. Sodium thiosulfate: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.21. Stevens DL, Bisno AL, Chambers HF, Everett ED, Dellinger P, Goldstein EJ, Gorbach SL, Hirschmann JV,Kaplan EL, Montoya JG, Wade JC; Infectious Diseases Society of America. Practice guidelines for thediagnosis and management of skin and soft-tissue infections. Clin Infect Dis. 2005;41:1373-1406.22. Drake LA, Dinehart SM, Farmer ER, et al. Guidelines of care for superficial mycotic infections of the skin:tinea corporis, tinea cruris, tinea faciei, tinea manuum, and tinea pedis. Guidelines/Outcomes Committee.American Academy of Dermatology. J Am Acad Dermatol. 1996;34(2):282-286.23. Drake LA, Dinehart SM, Farmer ER, et al. Guidelines of care for superficial mycotic infections of the skin:pityriasis (tinea) versicolor. Guidelines/Outcomes Committee. American Academy of Dermatology. J AmAcad Dermatol. 1996;34(2):287-289.24. Pappas PG, Rex JH, Sobel JD, et al. Guidelines for treatment of candidiasis. Infectious Diseases Society ofAmerica. Clin Infect Dis. 2004;38:161-189.25. Primary Care Dermatology Society & British Association of Dermatologists. Guidelines for the managementof atopic eczema. Available from: www.eGuidelines.co.uk. Accessed October 10, 2006.26. Darsow U, Lubbe J, Taieb A, et al. Position paper on diagnosis and treatment of atopic dermatitis. EuropeanTask Force on Atopic Dermatitis. JEADV. 2005;19:286-295.27. Akdis CA, Akdis M, Bieber T, et al. Diagnosis and treatment of atopic dermatitis in children and adults:European Academy of Allergology and <strong>Clinical</strong> Immunology/American Academy of Allergy, Asthma andImmunology/PRACTALL Consensus Report. J Allergy Clin Immunol. 2006;118:152-169.28. Hanifin JM, Cooper KD, Ho VC, et al. Guidelines of care for atopic dermatitis. J Am Acad of Dermatol.2004;50:391-404.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.197
29. Beveridge GW, Fairburn E, Finn OA, et al. A comparison of nystatin cream with nystatin/triamcinoloneacetonide combination cream in the treatment of Candidal inflammation of the flexures. Curr Med Res Opin.1977;4:584-587.30. Harcup JW, Tooley PJH. An open clinical trial with 2% miconazole plus 1% hydrocortisone ointment in thetreatment of eczematous lesions. Pharmatherap. 1987;5:145-151.31. Concannon P, Gisoldi E, Phillips S, et al. Diaper dermatitis: a therapeutic dilemma. Results of a double-blindplacebo controlled trial of miconazole nitrate 0.25%. Pediatr Dermatol. 2001;18(2):149-155.32. Spraker MK, Gisoldi EM, Siegfried EC, et al. Topical miconazole nitrate ointment in the treatment of diaperdermatitis complicated by candidiasis. Cutis. 2006;77(2):113-120.33. Faergermann J. Seborrhoeic dermatitis and Pityrosporum orbiculare: treatment of seborrhoeic dermatitis of thescalp with miconazole-hydrocortisone (Daktacort), miconazole and hydrocortisone. Brit J Dermatol.1986;114:695-700.34. Clayton YM, Connor BL. Comparison of clotrimazole cream, Whitfield’s ointment and Nystatin ointment forthe topical treatment of ringworm infections, pityriasis versicolor, erythrasma and candidiasis. Brit J Dermatol.1973;89:297-303.35. Wortzel MH. A double-blind study comparing the superiority of a combination antifungal(clotrimazole)/steroidal (betamethasone dipropionate) product. Cutis. 1982;30:258-261.36. Katz HI, Bard JB, Cole GW, et al. SCH 370 (Clotrimazole-betamethasone dipropionate) cream in patients withtinea cruris or tinea corporis. Cutis. 1984;34:183-186,188.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.198
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane Scabicides andPediculicidesAHFS Class 840412February 7, 2007I. OverviewPediculosis and scabies are caused by ectoparasites. Pediculi or lice, which are obligate human parasites,can cause infestations either on the head (by the parasite Pediculus humanus capitis), body (by Pediculushumanus corporis), or the pubic region (by Phthirus pubis). Another skin infection known as scabies iscaused by the parasitic mite Sarcoptes scabiei. While these skin conditions are associated with lowmorbidity, they are common causes of skin rash and pruritus, and are occurring with increasing frequency. 1,2This review includes both prescription and OTC topical agents for scabies and lice treatment. Thescabicides and pediculicides that are included in this review are detailed in Table 1. This reviewencompasses all (topical) dosage forms and strengths. Lindane, permethrin, and piperonyl butoxide andpyrethrins products are available as generics.Although some data suggest a growing resistance to permethrin in the United States, all reviewed resourcesstill recommend it as first-line antiparasitic therapy for treatment of both scabies and lice infections. 3Lindane, while still widely used, is considered second-line therapy due to its toxicity risks. 4Table 1. Skin and Mucous Membrane Scabicides and Pediculicides Included in this <strong>Review</strong>Generic Name(s) Formulation(s) Example BrandName(s)Current PDLAgent(s)crotamiton cream, lotion Eurax ® Eurax®lindanelotion, shampoo N/A lindane(gamma-hexachlorocyclohexane)malathion lotion Ovide ® nonepermethrin‡ cream, lotion Acticin ® *, permethrinElimite ® *piperonyl butoxide and pyrethrins‡ shampoo, solution Licide ® * piperonylbutoxide andpyrethrins*Generic is available in at least one dosage form or strength.‡Over-the-counter product is available in at least one dosage form or strength.N/A=not availableII.Evidence-Based Medicine and Current Treatment GuidelinesCurrent treatment guidelines that incorporate the skin and mucous membrane scabicides and pediculicidesare summarized in Table 2.Table 2. Treatment Guidelines Using the Skin and Mucous Membrane Scabicides and Pediculicides<strong>Clinical</strong> GuidelineRecommendation(s)Centers for Disease Control andPrevention (CDC) Morbidity andPediculosis pubis (pubic lice infestation)Recommended regimens are:Mortality Weekly Report(MMWR): Sexually Transmitted• permethrin 1% cream rinse applied to affected areas andwashed off after 10 minutes ORPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.199
<strong>Clinical</strong> GuidelineRecommendation(s)Diseases Treatment Guidelines,2006 5 • piperonyl butoxide and pyrethrins applied to the affectedarea and washed off after 10 minutes.Alternative regimens are:• malathion 0.5% lotion applied for 8-12 hours and washedoff OR• ivermectin 250 mcg/kg orally repeated in 2 weeks.ScabiesRecommended regimens are:• permethrin 5% cream applied to all areas of the bodyfrom the neck down and washed off after 8-14 hours OR• ivermectin 200 mcg/kg orally, repeated in 2 weeks.Alternative regimens are:• lindane 1% lotion (1 oz) or cream (30 g) applied in a thinlayer to all areas of the body from the neck down andthoroughly washed off after 8 hours.American Academy of Pediatrics:2002 Head Lice Guidelines 6 • Permethrin 1% is currently the recommended treatmentfor head lice, with retreatment in 7 to 10 days if live liceare seen. Instructions on proper use of products shouldbe carefully relayed. Safety and efficacy should be takeninto account when recommending any product fortreatment of head lice infestation.• None of the currently available pediculicides are 100%ovicidal and resistance has been reported with lindane,pyrethrins, and permethrin. Treatment failure does notequate with resistance, and most instances of such failurerepresent either misdiagnosis/misidentification ornoncompliance with the treatment regimen.III.IndicationsThe Food and Drug Administration (FDA)-approved indications for the skin and mucous membranescabicides and pediculicides are noted in Table 3.Table 3. FDA-Approved Indications for the Skin and Mucous Membrane Scabicides andPediculicides 7-11Drug(s) Scabies Head Lice Head and PubicLiceHead, Body,and Pubic Licecrotamitonalindane a* amalathionapermethrin a apiperonyl butoxide andpyrethrinsa*Lindane is reserved for patients who cannot tolerate or have failed other approved therapies.IV.PharmacokineticsThe pharmacokinetic parameters for the skin and mucous membrane scabicides and pediculicides aresummarized in Table 4.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.200
Table 4. Pharmacokinetic Parameters of the Skin and Mucous Membrane Scabicides andPediculicides 1,7-11Drugs(s)Peak Concentration(hours)Absorption(%)Serum Half-Life(hours)crotamiton 24 No data No datalindane 6 10 18malathion No data 8 No datapermethrin No data 2 No datapiperonyl butoxide and pyrethrins 0.5 No data No dataV. Drug InteractionsThere are no significant drug interactions with the skin and mucous membrane scabicides andpediculicides. 1,12-16 However, note that lindane should be used with caution with any drug that is known tolower the seizure threshold. These include antipsychotics, antidepressants, theophylline, cyclosporine,mycophenolate, tacrolimus, penicillins, imipenem, fluoroquinolones, chloroquine, isoniazid, meperidine,radiographic contrast media, centrally active anticholinesterases, and methocarbamol. 13VI.Adverse Drug EventsThe most common adverse drug events reported with the skin and mucous membrane scabicides andpediculicides are noted in Table 5.Table 5. Adverse Drug Events (%) Reported with the Skin and Mucous Membrane Scabicides andPediculicides 12-16Adverse Event(s) Crotamiton Lindane Malathion* Permethrin Piperonyl Butoxideand PyrethrinsCentral Nervous SystemAtaxia - a - - -Dizziness - a - - -Headache - a - - -Pain - a - - -Seizures - a - - -DermatologicalAlopecia - a - - -Dermatitis a a - - -Erythema - - - 1-10 -Irritation of skin a - a - aand scalpMild transient- a - 1-10 aburning/stingingNumbness - - - 1-10 -Pruritus a a - 1-10 aRash a - - 1-10 -Urticaria - a - - -GastrointestinalNausea - a - - -Vomiting - a - - -OtherAplastic anemia - a - - -Cardiacarrhythmia- a - - -Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.201
Adverse Event(s) Crotamiton Lindane Malathion* Permethrin Piperonyl Butoxideand PyrethrinsConjunctivitis (if - - a - -eye contact)Edema - - - 1-10 -Hematuria - a - - -Hepatitis - a - - -Paresthesia - a - - -Pulmonary edema - a - - -* Malathion is an insecticide/pesticide. Inadvertent transmucosal will manifest as excessive cholinergic activity (e.g., increasedsweating, salivary and gastric secretion, gastric and uterine motility, and bradycardia). Additionally, malathion contains flammablealcohol and should not be exposed to an open flame or electric heat, including hair dryers and electric curlers.aFrequency not defined (includes postmarketing and case reports)- Event not reportedThe FDA issued a Public Health Advisory regarding lindane in March 2003. 4 A new boxed warning wasadded to the product labeling for all forms of lindane. Table 6 details this information.Table 6. 2003 FDA Warnings Added to Lindane Product Labeling 17Lindane lotion 1% Lindane shampoo 1%WarningsLindane lotion should only beused in patients who cannottolerate or have failed first-linetreatment with safer medicationsfor the treatment of scabies. for the treatment of lice.Neurologic ToxicityContraindicationsProper UseSeizures and deaths have beenreported following lindane lotionuse with repeat or prolongedapplication, but also in rare casesfollowing a single applicationused according to directions.Lindane lotion should be usedwith caution for infants, children,the elderly, and individuals withother skin conditions (e.g., atopicdermatitis, psoriasis) and in thosewho weigh
VII.Dosing and AdministrationThe usual dosing regimens for the skin and mucous membrane scabicides and pediculicides aresummarized in Table 7.Table 7. Usual Dosing for the Skin and Mucous Membrane Scabicides and Pediculicides 7-11Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityCrotamiton Prior to application, patientsshould bathe or shower.Shake the lotion well beforeusing. Thereafter, a thin layerof the cream or lotion shouldbe thoroughly massaged intoall skin surfaces from the chindown to the toes including allskin folds and creases.Crotamiton is left on the skinand a second application isadvisable 24 hours later. Thepatient should take acleansing bath 24 to 48 hoursafter the last application toremove any remaining drug.Patients can be retreated after7 days if live mites appear orif no clinical improvement isobserved.Prior to application, patientsshould bathe or shower.Shake the lotion well beforeusing. Thereafter, a thin layerof the cream or lotion shouldbe thoroughly massaged intoall skin surfaces from the chindown to the toes including allskin folds and creases.Crotamiton is left on the skinand a second application isadvisable 24 hours later. Thepatient should take acleansing bath 24 to 48 hoursafter the last application toremove any remaining drug.Patients can be retreated after7 days if live mites appear orif no clinical improvement isobserved.Cream: 10%Lotion: 10%LindaneLiceApply a sufficient quantity ofshampoo onto clean, dry hair;generally 1 ounce issufficient, no more than 2ounces should be used. Workthe shampoo into hairthoroughly and allow toremain on hair for 4 minutes.Add small quantities of waterand massage until a goodlather forms. Rinsethoroughly and towel drybriskly. Nits should beremoved using a nit comb ortweezers. Retreatment is notrecommended. It is notknown how soon after lindaneDue to potential lindanetoxicity, crotamiton is a drugof choice for young childrenand pregnant or lactatingwomen in the treatment ofscabies. However, crotamitonis not approved by the FDAfor the treatment of scabies inpediatric patients.The use of lindane should beavoided in infants and youngchildren due to a higherincidence of adverse reactionsin this age group. Clinicianspostulate that young childrenare predisposed to toxicitybecause their surface area tovolume ratio is larger thanadults; however, there havebeen no studies todemonstrate that childrenabsorb more than adults.Older children weighinggreater than 50 kilograms(110 pounds) may be treatedthe same as adults.Lotion: 1%Shampoo: 1%203Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Drug(s) Usual Adult Dose Usual Pediatric Dose Availabilityadministration that a seconddose can safety bereadministered.MalathionPermethrinScabiesOne ounce of lindane lotion isgenerally sufficient to treatthe average adult. Do not usemore that 2 ounces for largeradults. The lotion should beapplied thinly and rubbed inthoroughly. Avoid applyinglindane to open cuts. Thelotion should be left on for 8to 12 hours and removed bythorough washing.Retreatment is notrecommended. It is notknown how soon after lindaneadministration that a seconddose can safety bereadministered.Apply lotion on dry hair in anamount just sufficient tothoroughly wet the hair andscalp. Allow hair to drynaturally, do not use anelectric heat source, and allowhair to remain uncovered.After 8 to 12 hours, the hairshould be shampooed. Rinseand use a fine-toothed (nit)comb to remove dead lice andeggs. If lice are still presentafter 7-9 days, repeat with asecond application of lotion.LiceInitial: A sufficient volume(25 to 50 ml) applied tosaturate the hair and scalp. Asecond application may beindicated if live lice arepresent 7 days or more after204Apply lotion on dry hair in anamount just sufficient tothoroughly wet the hair andscalp. Allow hair to drynaturally, do not use anelectric heat source, and allowhair to remain uncovered.After 8 to 12 hours, the hairshould be shampooed. Rinseand use a fine-toothed (nit)comb to remove dead lice andeggs. If lice are still presentafter 7-9 days, repeat with asecond application of lotion.Application in pediatricpatients should occur onlyunder direct adultsupervision, and iscontraindicated in neonates.Safety and efficacy ofmalathion 0.5% lotion inchildren younger than 6 yearsof age have not beenestablished via wellcontrolledtrials.LiceInitial: A sufficient volume(25 to 50 ml) applied tosaturate the hair and scalpA second application may beindicated if live lice arepresent 7 days or more afterLotion: 0.5%Cream: 5%Lotion: 1%Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Drug(s) Usual Adult Dose Usual Pediatric Dose Availabilitythe initial application. the initial application.ScabiesInitial: 30 g is usuallysufficient for an average adultto provide for a single head totoe application. Repeat dose14 days later if demonstrableliving mites.ScabiesInitial: 30 g is usuallysufficient for an average adultto provide for a single head totoe application. Repeat dose14 days later if demonstrableliving mites.Piperonylbutoxide andpyrethrinsIf topical solution, shake wellbefore use. The undilutedliquid should be applied todry hair and scalp or to anyinfested area until entirelywet. The liquid should not beused on the eyelashes oreyebrows.This should be used inchildren 2 months or older.Safety and efficacy inchildren have not beenestablished.Shampoo:4-0.33%Solution:4-0.33%Shampoo should be applied tothe affected area until all hairis thoroughly wet and allowedto stand for no longer than 10minutes. Then, the areashould be washed with warmwater and shampoo or soap.A fine-toothed comb, usuallysupplied with the product,should be used to removedead lice and ova. Thetreatment should be repeatedin 7 to 10 days to assureeradication of unhatched nits.Two consecutive applicationsshould not be administeredwithin 24 hours.Special Dosing ConsiderationsCrotamiton: it is not known whether crotamiton can cause fetal harm when administered to pregnantwomen or affect reproduction capacity. The safety and efficacy of crotamiton has not been established inchildren.Lindane: pregnancy category B and is not recommended by the CDC for use in pregnancy or nursingwomen. Lindane is contraindicated in premature neonates due to an increase in skin permeability. TheCDC currently recommends that alternative treatments be used in infants and children younger than 2 yearsof age.Malathion: safety and efficacy of malathion 0.5% lotion in children younger than 6 years of age have notbeen established via well-controlled trials. Topical products should not be applied to the scalp of infantsand neonates and is contraindicated. Additionally, malathion lotion that is commercially available in theU.S. is flammable and everyone should be warned to stay away from lighted cigarettes, open flames, andelectric heat sources while their hair is wet with the lotion. Malathion should be used or handled duringPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.205
pregnancy only when clearly needed. There have been no adequate controlled studies on pregnant womenat this time.Permethrin: pregnancy category B. Safety and efficacy of permethrin 1% cream rinse and 5% cream inchildren younger than 2 months of age have not been established. However, the drug has been usedeffectively without unusual adverse effects in this age group.Piperonyl butoxide and pyrethrins: pregnancy category C.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.206
VIII. Effectiveness<strong>Clinical</strong> studies evaluating the safety and efficacy of the skin and mucous membrane scabicides and pediculicides are summarized in Table 8.Table 8. Comparative <strong>Clinical</strong> Trials Using the Skin and Mucous Membrane Scabicides and PediculicidesStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsScabiesHaustein et al. 18Lindane (1% and0.3%)vs.permethrin (5% and2.5%)vs.Open, not blinded114 adults and 80children with scabiesN=1943 weeksPrimary:EfficacySecondary:Side effectsResultsPrimary:Efficacy: lindane 92% (treatment failures in three adults and twochildren), permethrin 100%, benzyl benzoate 100%.Lindane was shown to be less effective (P
StudyandDrug RegimenLindane cream 1%vs.permethrin cream 5%Taplin et al. 21Lindane lotion 1%vs.permethrin cream 5%Taplin et al. 22Permethrin cream 5%vs.crotamiton cream 10%Study DesignandDemographicsPatients with scabiesolder than 5 years of ageRCTPatients withmicroscopicallyconfirmed scabiesDB, RCTTreatment of scabies inchildren 2 months to 5years of ageSample Sizeand StudyDuration2 weeksN=231 monthN=471 monthEnd PointsSecondary:Not reportedPrimary:EfficacySecondary:Not reportedPrimary:EfficacySecondary:Not reportedResultswhereas lindane was effective only in 48.8% of patients (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultscrotamiton 10%Chouela et al. 24Lindane solution 1%vs.ivermectin, oral dose,150-200 mcg/kg ofbody weightRCT, PRO, DB, DD, PGPatients with scabies thatwere outpatients,hospitalized patients, andthose referred to thehospital from nursinghomes and asylumsN=531 monthPrimary:<strong>Clinical</strong>healingSecondary:AdverseeffectsPrimary:Of 53 patients, 43 (81%) completed the study, 19 in the group treatedwith ivermectin and 24 in the group treated with lindane. At day 15, 14patients (74%; 95% CI, 48.8%-90.8%) in the group receiving ivermectinshowed healing of their scabies and 13 patients (54%; 95% CI, 32.8%-74.4%) in the group treated with lindane were healed. At 29 days, bothtreatments resulted in statistically equivalent therapeutic efficacy.Eighteen patients (95%; 95% CI, 74.0%-99.9%) were healed withivermectin and 23 patients (96%; 95% CI, 78.9%, 99.9%) were healedwith lindane (P
StudyandDrug RegimenHead, Body, or Pubic LiceBrandenberg et al. 27Lindane shampoo 1%vs.permethrin cream rinse1%Taplin et al. 28Permethrin cremerinse 1%vs.lindane shampoo 1%vs.placeboBowerman et al. 29Lindane shampoovs.permethrin creme rinse1%RCTStudy DesignandDemographicsPatients with the headlouse Pediculus humanusvar capitis (head lice)Of 573 patients enrolledat eight centers, 559 wereassessable for toleranceand 508 for efficacy.DB, RCTPatients with Pediculushumanus var capitis (headlice)RCTPatients with head lice inthe Nezahualcoyotlcommunity of Mexicocity representing 296family groupsSample Sizeand StudyDurationN=5732 weeksN=932 weeksN=10402 weeksEnd PointsPrimary:EfficacySecondary:TolerancePrimary:EfficacySecondary:SafetyPrimary:EfficacySecondary:AdverseeffectsResultsPrimary:Of the 257 patients treated with 1% permethrin cream rinse, 99% werelice free at 14 days; of the 251 patients treated with 1% lindane shampoo,85% were lice free at 14 days (P
StudyandDrug RegimenKalter et al. 30Lindane shampoo 1%vs.RCTStudy DesignandDemographicsMen with the diagnosis ofpediculosis pubisSample Sizeand StudyDurationN=5310 daysEnd PointsPrimary:EfficacySecondary:TolerabilityResultsPrimary:In the lindane group, 10 (40%) of 25 subjects were infested at the finalassessment. In the permethrin group, 12 (43%) of 28 subjects wereinfested at the final assessment. The difference was not statisticallysignificant. Lindane was 60% effective and permethrin was 57%.permethrin cremerinse 1%Carson et al. 31Permethrin 1%vs.pyrethrins combinedwith piperonylbutoxideRCTPatients with Pediculushumanus var capitis (headlice)N=582 weeksPrimary:EfficacySecondary:TolerabilitySecondary:Both treatments were well tolerated, with one mild adverse reaction ineach group.Primary:Seven days after the initial visit, permethrin was determined to besignificantly better than pyrethrins with piperonyl butoxide foreradicating the lice infestation. Of the 27 subjects receiving permethrin,26 were lice free vs. 14 of the 31 piperonyl butoxide and pyrethrintreatedsubjects (P0.01) in thetreatments (27 of 27 permethrin-treated vs. 29 of 31 pyrethrins withpiperonyl butoxide-treated subjects were lice free).DiNapoli et al. 32Permethrin crèmerinse 1%vs.RandomizedPatients with Pediculosiscapitis (head liceinfestation)N=4352 weeksPrimary:EfficacySecondary:AdverseeffectsSecondary:Both treatments were well tolerated, and no subject experienced adversereactions.Primary:Seven days after the treatment, 98% of the permethrin-treated and 85%of the pyrethrins combined with piperonyl butoxide-treated patients werefree of lice. At 14 days, prior to nit removal, 96% of the permethrintreatedand 62% of the pyrethrins combined with piperonyl butoxidetreatedpatients were still lice free.pyrethrins combinedwith piperonylbutoxideSecondary:Seventeen (7%) permethrin-treated and 32 (16%) pyrethrins combinedwith piperonyl butoxide-treated patients were reported to have adverseexperiences.211Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenRoberts et al. 33Malathion lotionvs.wet combing with afine-toothed combMeinking et al. 34Malathion lotion 0.5%vs.permethrin crème rinse1%Hipolito et al. 35Permethrin crèmerinse 1%vs.trimethoprim andsulfamethoxazolevs.permethrin crème rinse1% plus trimethoprimand sulfamethoxazoleRCTStudy DesignandDemographicsSchoolchildren (aged 3 to14 years) in two countiesin Wales, UKObserver-blindedPatients with head liceRCTChildren with head liceranging in age from 2 to13 yearsSample Sizeand StudyDurationN=812 weeksN=6615 daysN=1151 monthEnd PointsPrimary:EfficacySecondary:Not reportedPrimary:EfficacySecondary:Not reportedPrimary:EfficacySecondary:AdverseeffectsResultsPrimary:74 children completed the study and 72 were included in the analysis.The cure rate was 38% (12 of 32) for wet combing and 78% (31 of 40)for malathion. Children assigned wet combing were 2.8 (95% CI 1.5-5.2)times more likely than those assigned malathion to have lice at the end oftreatment (P=0.0006).Secondary:Not reportedPrimary:A 20-minute application of malathion was significantly morepediculicidal and ovicidal (98%) compared to permethrin at day 15(P
Additional EvidenceDose SimplificationLittle peer-reviewed data was found in a literature search of Medline/Pubmed and Ovid on adherence withdifferent treatments for pediculosis and scabies. Some dermatologists suggest most treatment failures arenot a result of poor compliance, but due to growing resistance to insecticides. 36Stable TherapyA search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician VisitsA search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 9. Relative Cost of the Skin and Mucous Membrane Scabicides and PediculicidesGeneric Name(s) Formulation(s) Example Brand Name(s) BrandCostGenericCostcrotamiton cream, lotion Eurax ® $ N/Alindane lotion, shampoo N/A N/A $$$$malathion lotion Ovide ® $$$$ N/Apermethrin‡ cream, lotion Acticin ® *, Elimite ® * $$ $piperonyl butoxideand pyrethrins‡shampoo,solution*Generic is available in at least one dosage form or strength.‡Over-the-counter product is available in at least one dosage form or strength.N/A=not availableLicide ® * $ $X. ConclusionsA number of effective skin and mucous membrane scabicides and pediculicides are available. Permethrinproducts are recommended as first-line therapy for treatment of scabies and lice. The permethrin productsreviewed here, as well as their generic equivalents, are available over-the-counter (OTC) and are coveredPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.213
y Alabama Medicaid. Lindane, a well-known older agent, has been relegated to second-line therapy dueto risk of toxicity. Other available agents offer alternative options should a resistant case occur.A comparison of the overall success rates of skin and mucous membrane scabicides, as detailed in Table 8,shows 89%-100% success with permethrin, 65%-92% with lindane, and 60%-88% with crotamiton.Permethrin is recommended as first-line therapy and lindane as second-line in the CDC guidelines. 5Crotamiton also has a role as an antipruritic for those with scabies. 5 All patients treated for scabies shouldexpect the rash and itching to continue for about 2 weeks after treatment. 2Overall, the comparative success rates of skin and mucous membrane pediculicides are 57%-99% withpermethrin, 60%-88% with lindane, 45%-95% with piperonyl butoxide and pyrethrins, and 78% withmalathion. Combing or ‘bug-busting’ was only 38% successful in a comparison to malathion (78%), andshould not be considered a first-line therapy for treatment of head lice. The CDC recommends permethrinor the combination of piperonyl butoxide and pyrethrins as equivalent therapies for pediculosis pubis. 5 Bothof these products are available generically and OTC. The American Academy of Pediatrics recommendspermethrin for head lice. 6Reasons for treatment failures for either skin and mucous membrane scabicides and pediculicidesinclude misdiagnosis, noncompliance, failure to follow instructions correctly, not enough pediculicideapplied, reinfestation, and resistance. If resistance is suspected, retreatment should be with a differentchemical entity than initially used. 2Therefore, all brand products within the class reviewed are comparable to each other and to the genericsand over-the-counter products in this class and offer no significant clinical advantage over otheralternatives in general use. Lindane possesses an extensive adverse reaction profile and should not be usedas a first-line agent.XI.RecommendationsNo brand skin and mucous membrane scabicide and pediculicide is recommended for preferred status.Alabama Medicaid should accept cost proposals from manufacturers to determine cost effective productsand possibly designate one or more preferred brands.At this time, no brand lindane product is available; however, if one becomes available, it should not beplaced in preferred status regardless of cost.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.214
References1. Roos TC, Alam M, Roos S, Merk HF, Bickers DR. Pharmacotherapy of ectoparasitic infections. Drugs.2001;61:1067-1088.2. Wendel K, Rompalo A. Scabies and pediculosis pubis: an update of treatment regimens and general review.Clin Infect Dis. 2002;35(Suppl 2):S146-151.3. Pollack RJ, Kiszewski A, Armstrong P, et al. Differential permethrin susceptibility of head lice sampled in theUnited States and Borneo. Arch Pediatr Adolesc Med. 1999;153:969-973.4. Food and Drug Administration. FDA Issues Health Advisory Regarding Labeling Changes for LindaneProducts. FDA Talk Paper, March 28, 2003. Available at:http://www.fda.gov/bbs/topics/ANSWERS/2003/ANS01205.html. Accessed October 27, 2006.5. Centers for Disease Control and Prevention. Ectoparasitic infections. In: Centers for Disease Control andPrevention. Sexually Transmitted Diseases Treatment Guidelines, 2006. MMWR 2006;55(No. RR-11):1-100.Available at: http://www.cdc.gov/std/treatment/2006/ectoparasitic.htm. Accessed October 27, 2006.6. Frankowski B, Weiner L. Head lice. Pediatrics 2002:110(3);638-643. Available at:http://aappolicy.aappublications.org/cgi/content/full/pediatrics;110/3/638.7. Crotamiton. In: Micromedex ® Healthcare Series, (electronic version). Thomson Micromedex, GreenwoodVillage, CO, USA. Available at: http://www.thomsonhc.com. Accessed October 27, 2006.8. Lindane. In: Micromedex ® Healthcare Series, (electronic version). Thomson Micromedex, Greenwood Village,CO, USA. Available at: http://www.thomsonhc.com. Accessed October 27, 2006.9. Malathion. In: Micromedex ® Healthcare Series, (electronic version). Thomson Micromedex, GreenwoodVillage, CO, USA. Available at: http://www.thomsonhc.com. Accessed October 27, 2006.10. Permethrin. In: Micromedex ® Healthcare Series, (electronic version). Thomson Micromedex, GreenwoodVillage, CO, USA. Available at: http://www.thomsonhc.com. Accessed October 27, 2006.11. Pyrethrins/Piperonyl. In: Micromedex ® Healthcare Series, (electronic version). Thomson Micromedex,Greenwood Village, CO, USA. Available at: http://www.thomsonhc.com. Accessed October 27, 2006.12. Crotamiton: Drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.13. Lindane: Drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.14. Malathion: Drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.15. Permethrin: Drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.16. Pyrethrins: Drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.17. Food and Drug Administration (FDA), Center for Drug Evaluation and Research. Drug information: lindaneshampoo and lindane lotion. Available at: http://www.fda.gov/cder/drug/infopage/lindane/default.htm.Accessed October 27, 2006.18. Haustein UF, Hlawa B. Treatment of scabies with permethrin versus lindane and benzyl benzoate. Acta DermVenereol. 1989;69:348-351.19. Schultz MW, Gomez M, Hansen RC, et al. Comparative study of 5% permethrin cream and 1% lindane lotionfor the treatment of scabies. Arch Dermatol. 1990;126:167-170.20. Zargari O, Golchai J, Dehpour AR, et al. Comparison of the efficacy of topical 1% lindane vs. 5% permethrin inscabies: A randomized, double-blind study. Indian J Dermatol Venereol Leprol. 2006;72;33-36.21. Taplin D, Meinking TL, Porcelain SL, Castilero PM, Chen JA. Permethrin 5% dermal cream: a new treatmentfor scabies. J Am Acad Dermatol. 1986;15:995-1001.22. Taplin D, Meinking TL, Chen JA., Sanchez R. Comparison of crotamiton 10% cream (Eurax) and permethrin5% cream (Elimite) for the treatment of scabies in children. Pediatr Dermatol. 1990; 7:67-73.23. Amer M, el-Garib I. Permethrin versus crotamiton and lindane in the treatment of scabies. Int J Dermatol.1992;31:357-358.24. Chouela EN, Abeldano AM, Pellerano G, et al. Equivalent therapeutic efficacy and safety of ivermectin andlindane in the treatment of human scabies. Arch Dermatol. 1999;135:651-655.25. Madan V, Jaskiran K, Gupta U, Gupta DK. Oral ivermectin in scabies patients: a comparison with 1% topicallindane lotion. J Dermatol. 2001;28:481-484.26. Usha V, Gopalakrishnan Nair TV. A comparative study of oral ivermectin and topical permethrin cream in thetreatment of scabies. J Am Acad Dermatol. 2000; 42(2 Pt 1):236-240.27. Brandenburg K, Deinard AS, DiNapoli J, Englender SJ, Orthoefer J, Wagner D.1% permethrin cream rinse vs.1% lindane shampoo in treating pediculosis capitis. Am J Dis Child. 1986; 140:894-896.28. Taplin D, Meinking TL, Castillero PM, Sanchez R. Permethrin 1% creme rinse for the treatment of Pediculushumanus var capitis infestation. Pediatr Dermatol. 1986;3:344-348.29. Bowerman JG, Gomez MP, Austin RD, Wold DE. Comparative study of permethrin 1% creme rinse andPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.215
lindane shampoo for the treatment of head lice. Pediatr Infect Dis J. 1987;6:252-255.30. Kalter DC, Sperber J, Rosen T, Matarasso S. Treatment of pediculosis pubis. <strong>Clinical</strong> comparison of efficacyand tolerance of 1% lindane shampoo vs. 1% permethrin creme rinse. Arch Dermatol. 1987;123:1315-1319.31. Carson DS, Tribble PW, Weart CW. Pyrethrins combined with piperonyl butoxide (RID) vs. 1% permethrin(NIX) in the treatment of head lice. Am J Dis Child. 1988;142:768-769.32. DiNapoli JB, Austin RD, Englender SJ, Gomez MP, Barrett JF. Eradication of head lice with a single treatment.Am J Public Health. 1988;78:978-980.33. Roberts RJ, Casey D, Morgan DA, Petrovic M. Comparison of wet combing with malathion for treatment ofhead lice in the UK: a pragmatic randomized controlled trial. Lancet. 2000;356:540-544.34. Hipolito RB, Mallorca FG, Zuniga-Macaraig ZO, Apolinario PC, Wheeler-Sherman J. Head lice infestation:single drug versus combination therapy with one percent permethrin and trimethoprim/sulfamethoxazole.Pediatrics. 2001;107:E30.35. Meinking T, Vicaria M, Eyerdam DH, et al. Efficacy of a reduced application time of ovide lotion (malathion)compared to nix crème rinse (1% permethrin) for the treatment of head lice. Pediatric Dermatology. 2004;21(6);670-674.36. Downs AM. Managing head lice in an era of increasing resistance to insecticides. Am J Clin Dermatol.2003;5(3):169-77.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.216
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane Local Anti-infectives,MiscellaneousSingle Entity AgentsAHFS Class 840492February 7, 2007I. OverviewMiscellaneous local anti-infectives are indicated for a variety of uses, depending on the specific product.The agents reviewed in this review can be used for antiseptic cleansing, burn treatment, vaginal infectionsand wound care.Burn patients are predisposed to infection due to a loss of the protective barrier function of the skin, whichleads to the entry of microorganisms and induces systemic immunosuppression. 1,2 Complicationssecondary to infections are the major cause of morbidity and mortality in patients with severe burns.Closure and healing of the wound are the major goals of burn wound management. Standard therapy forburn victims includes excision of burned tissue, debridement of necrotic tissue, as well as grafting of skinor skin substitutes. Topical anti-infective agents are utilized for decreasing the bacterial burden of burnwounds, thus minimizing the incidence of infection. 1,2 The introduction of these agents to clinical practicesince the 1960s has led to a decrease of approximately 50% in the burn-wound mortality rate. 3 Streptococciand Staphylococci are the main organisms involved in burn wound infections. Pseudomonas and fungi areincreasingly found to cause burn infections due to the growing use of wide-spectrum antibiotics. 1,2The three most commonly used topical anti-infectives in burn management are silver sulfadiazine,mafenide acetate and silver nitrate. All three agents have a broad spectrum of activity. 1 The initial agenttypically used is silver sulfadiazine. In addition to its broad spectrum of activity (including Pseudomonas),mafenide acetate has the ability to penetrate eschars. However, its side-effect profile limits the use ofmafenide acetate as first-line therapy. 3 Silver nitrate solution delivered in occlusive dressings may be aneffective option for patients with an allergy to sulfonamides or those who develop hypersensitivity to oneof the other agents. 2 However, silver nitrate may be used only for prevention of infection and is noteffective in treating wound infections because it does not penetrate the eschar due to precipitation uponcontact with the exudates.Single entity skin and mucous membrane local anti-infectives, miscellaneous included in this review arelisted in Table 1. This review encompasses all (topical) dosage forms and strengths. Silver nitrate andsilver sulfadiazine are available in generic formulations.Table 1. Single Entity Skin and Mucous Membrane Local Anti-infectives, Miscellaneous Included inthis <strong>Review</strong>Generic Name(s) Formulation(s) Example Brand Name(s) Current PDL Agent(s)formaldehyde solution, spray Formalyde-10 ® , Lazerformalyde ® nonehexachlorophene liquid Phisohex ® nonemafenide acetate cream, packet Sulfamylon ® nonesilver nitrate solution N/A silver nitratesilver sulfadiazine cream Silvadene ® *, SSD ® *, SSD AF ® SSD ® *, SSD AF ® *,silver sulfadiazinesulfanilamide vaginal cream AVC ® none*Generic is available in at least one dosage form or strength.N/A=not availablePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.217
II.Evidence-Based Medicine and Current Treatment GuidelinesThe following are summaries from national guidelines that incorporate the use of the single entity skin andmucous membrane local anti-infectives, miscellaneous.Table 2. Treatment Guidelines Using the Single Entity Skin and Mucous Membrane Local Antiinfectives,Miscellaneous<strong>Clinical</strong> GuidelineRecommendation(s)Agency for Health Care Policyand Research (AHCPR; now theAgency for Healthcare Researchand Quality[AHRQ]) : Treatmentof Pressure Ulcers 4 ••A 2-week trial of topical antibiotics should be consideredfor nonhealing clean pressure ulcers.The antibiotic should be effective against gram-negative,gram-positive, and anaerobic organisms (silversulfadiazine).• Topical antiseptics should not be used to reduce bacteriain wound tissue.American Diabetes Association:Consensus DevelopmentConference in Diabetic FootWound Care 5 ••Current evidence does not support the use of antibiotictherapy for patients with clinically uninfected lesions.Oral antibiotic therapy is recommended for patients withmild to moderate infections. Commonly used oral agentsinclude cephalexin, clindamycin, andamoxicillin/clavulanate.• Topical antibiotics have not been well studied in patientswith diabetic foot infections.• Antiseptic agents and various astringents are cytotoxic tothe tissue and are not recommended.Healthcare Infection ControlPractices Advisory Committee(HICPAC), Hand-Hygiene TaskForce: Guideline for HandHygiene in Healthcare Settings 6 ••Guideline strongly recommends the use of alcohol-basedhand rubs for hand antiseptics in healthcare workers.Alcohol-based hand rubs are more effective at reducingbacteria on hands, cause less irritation, require less time,and more accessible compared to soap and water.• Alcohols, chlorhexidine, iodophors, and other antisepticagents have poor activity against spores.Centers for Disease Control andPrevention (CDC) Morbidity andMortality Weekly Report(MMWR): Sexually TransmittedDiseases Treatment Guidelines,2006 7 • No reference to sulfanilamide as a potential agent for thetreatment of vaginal candidiasis.Harrison’s Principles of InternalMedicine. 16 th ed: Chapter 109A.Infectious Complications ofBites and Burns, 2005 1 • As antibiotics more effective against Pseudomonas havebecome available, fungi (particularly Candida albicans,Aspergillus spp., and the agents of mucormycosis) haveemerged as increasingly important pathogens in burnwoundpatients.• The frequency of infection parallels the extent andseverity of burn injury.• The ultimate goal of burn-wound management is closureand healing of the wound.• Silver sulfadiazine cream, mafenide acetate cream, andsilver nitrate are broadly active against many bacteria andagainst some fungi and are useful before bacterialcolonization is established.• Silver sulfadiazine is often used initially, but its valuecan be limited by bacterial resistance, mafenide acetatehas broader activity.• When superficial fungal infection occurs, nystatin may bePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.218
<strong>Clinical</strong> GuidelineRecommendation(s)mixed with silver sulfadiazine or mafenide acetate astopical therapy.• In general, prophylactic systemic antibiotics have no rolein the management of burn wounds and can in fact lead tocolonization with resistant microorganisms.III.IndicationsFood and Drug Administration (FDA)-approved indications for the single entity skin and mucousmembrane local anti-infectives, miscellaneous are noted in Table 3.Table 3. FDA-Approved Indications for the Single Entity Skin and Mucous Membrane Local Anti-infectives,Miscellaneous 8-14Indication Formaldehyde Hexachlorophene MafenideAcetateFoot antiperspirantWart treatmentBacteriostatic skincleanserTreatment ofvulvovaginitis causedby Candida albicansAdjunct therapy in thetreatment of secondandthird-degree burnsAdjunct therapy in theprevention of burnwound infectionsWound care, forreduction of exuberantgranulations*Cream only†Solution onlyaaaSilverNitrateSilverSulfadiazinea* aa† a aaSulfanil-amideaIV.PharmacokineticsThe pharmacokinetic parameters for the single entity skin and mucous membrane local anti-infectives,miscellaneous are summarized in Table 4.Table 4. Pharmacokinetic Parameters of the Single Entity Skin and Mucous Membrane Local Antiinfectives,Miscellaneous 8-14Drug(s) Time toPeak(hours)Absorption(%)Active Metabolites Half-Life(hours)ProteinBinding(%)Formaldehyde No data No data No data No data No dataHexachlorophene No data 3 No data 6.1-44.2 No dataMafenide acetate 2-4 No data No No data No dataSilver nitrate No data Minimal No data No data No dataSilver sulfadiazine 72-264 No data No data 10 No dataSulfanilamide No data No data No data No data No dataPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.219
V. Drug InteractionsA literature search indicates that there are no significant drug interactions with the single entity skin and mucous membrane local anti-infectives,miscellaneous. 8-15VI.Adverse Drug EventsThe most common adverse drug events reported with the single entity skin and mucous membrane local anti-infectives, miscellaneous are noted in Table 5.Table 5. Adverse Drug Events (%) Reported with the Single Entity Skin and Mucous Membrane Local Anti-infectives, Miscellaneous 8-14Adverse Event(s) Formaldehyde Hexachlorophene Mafenide Silver Nitrate Silver Sulfadiazine SulfanilamideAcetateCentral Nervous System (CNS)CNS injury - a - - - -Convulsion a - - - - -Delirium - a - - - -Diplopia - a - - - -Dizziness a - - - - -Irritability -
Adverse Event(s) Formaldehyde Hexachlorophene Mafenide Silver Nitrate Silver Sulfadiazine SulfanilamideAcetateEndocrine/MetabolicHyperchloremia - - a - - -Hyponatremia - - - a - -Metabolic acidosis a - a - - -GastrointestinalDiarrhea a - a - - aNausea a - - - - -Ulceration a - - - - -Vomiting a a - - - -GenitourinaryAnuria a - - - - -Hematuria a - - - - -Interstitial nephritis - - - - a -Renal dysfunction a - - - - -Tubular necrosis a - - - - -HematologicAgranulocytosis - - - - a aAplastic anemia - - - - a -Bleeding - - a - -Bone marrow- - a - - -suppressionCirculatory failure a - - - - -Hemolytic anemia a - a - a -Leukopenia - - - - a -Methemoglobinemia - - a a - -Porphyria - - a - - -RespiratoryBronchitis a - - - - -Cough a - - - - -Dysphagia a - - - - -Dyspnea - - a - - -Hyperventilation - - a - - -Pneumonia a - - - - -Pulmonary edema a - - - - -Respiratory failure a - - - - -Tachypnea - - a - - -Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.221
Adverse Event(s) Formaldehyde Hexachlorophene Mafenide Silver Nitrate Silver Sulfadiazine SulfanilamideAcetateMiscellaneousAnaphylaxis - - - - a -Hypersensitivity - - a - - aPhotosensitivity -
VII.Dosing and AdministrationThe usual dosing regimens for the single entity skin and mucous membrane local anti-infectives,miscellaneous are summarized in Table 6.Table 6. Usual Dosing for the Single Entity Skin and Mucous Membrane Local Anti-infectives,Miscellaneous 8-14Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityFormaldehydeHexachloropheneMafenide acetateApply once daily toaffected areaApply 5 mL cleanser andwater to area to becleansed; lather and rinseunder running waterApply to the affected area1-2 times dailySilver nitrate Apply a cotton applicatordipped in solution on theaffected area 1-3 times aweek for 2-3 weeksSilver sulfadiazine Apply to the affected area1-2 times dailySulfanilamide One applicatorful (about 6g) intravaginally 1-2 timesdailyApply once daily toaffected areaApply 5 mL cleanser andwater to area to becleansed; lather and rinseunder running waterApply to the affected area1-2 times dailyApply a cotton applicatordipped in solution on theaffected area 1-3 times aweek for 2-3 weeksApply to the affected area1-2 times dailySafety and efficacy havenot been established inchildrenSolution: 10%Spray: 10%Liquid: 3%Cream: 8.5%Powder: 50 g packet to prepare5% topical solutionSolution; 0.05%Cream: 1%Cream: 15%Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.223
VIII. Effectiveness<strong>Clinical</strong> studies evaluating the safety and efficacy of the single entity skin and mucous membrane local anti-infectives, miscellaneous are summarized inTable 7.Table 7. Comparative <strong>Clinical</strong> Trials Using the Single Entity Skin and Mucous Membrane Local Anti-infectives, MiscellaneousStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsBarret et al. 16Silver sulfadiazine (SSD) 1%,applied BID followingsuperficial debridementvs.Biobrane ® (bilaminartemporary skin substitute),applied BID to all openwounds, following superficialdebridementRCT, ACPatients
StudyandDrug Regimensilver sulfadiazine, applied tothe wound TIDStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsvs.petrolatum, applied to thewound TIDBodey et al. 18Hexachlorophene 3%vs.P-300 ® (bar soap containingtribromosalan and triclosan)RCT, ACPatients with acuteleukemia hospitalized inisolation unitsN=26
Kucan et al. 20StudyandDrug RegimenMafenide acetate 5% topicalsolutionPROStudy DesignandDemographicsPatients with burn woundsrequiring topicalantibacterial therapy;patients were excluded ifthey had a sulfonamideallergy or superficialpartial-thickness burnwoundsSample Sizeand StudyDurationN = 6697 yearsEnd PointsPrimary:Burn woundbiopsy, infection,sepsis, adverseeffectsSecondary:Not reportedResultsNot reportedPrimary:Eighteen percent of the patients receiving mafenide acetate5% topical solution had at least one positive burn woundbiopsy (no P values reported).Forty-two patients exhibited systemic signs of sepsis.Use of mafenide acetate 5% topical solution was notassociated with acid-base disturbances.Discontinuation of therapy because of the patient’s pain wasnecessary in less than 1% of patients.DuBouchet et al. 21Clotrimazole vaginal tablet 100mg, 2 tablets QD for 7 daysvs.AVC ® suppository (1.05 g ofsulfanilamide, 14 mg ofaminacrine hydrochloride, 140mg of allantoin) BID for 7 daysvs.metronidazole 2 g QD for 1 dayNote: AVC suppositories are nolonger available.)RCT, AC, OL, MCWomen >18 years of agediagnosed withsymptomatictrichomoniasis, diagnosisconfirmed by motiletrichomonad visualization insaline wet mounts ofvaginal secretion, positiveculture symptom score of>4; patients were excludedif they had metronidazolehypersensitivity, werepregnant, or had beentreated for vaginaltrichomoniasis within 4weeks preceding studyN=1686 weeksPrimary:T. vaginalisculture, symptomrelief, adverseeventsSecondary:Not reportedSecondary:Not reportedPrimary:There were significantly fewer patients in the oralmetronidazole group with a positive T .vaginalis culture aftertreatment compared to the patients randomized to receivetopical regimens (P
Additional EvidenceDose SimplificationA search of Medline and Ovid did not reveal data pertinent to this topic.Stable TherapyA search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician VisitsA search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 8. Relative Cost of the Single Entity Skin and Mucous Membrane Local Anti-infectives,MiscellaneousGeneric Name(s) Formulation(s) Example Brand Name(s) BrandCostGenericCostformaldehyde solution, spray Formalyde-10 ® ,$$-$$$ N/ALazerformalyde ®hexachlorophene liquid Phisohex ® $$ N/Amafenide acetate cream, packet Sulfamylon ® $$$$ N/Asilver nitrate solution N/A N/A $$silver sulfadiazine cream Silvadene ® *, SSD ® *, SSD $-$$ $AF ® *sulfanilamide vaginal cream AVC ® $$$ N/A*Generic is available in at least one dosage form or strength.N/A=not availablePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.227
X. ConclusionsThe miscellaneous local anti-infectives have been shown to be effective for a variety of conditions. Atthis time, there are generic formulations available for silver sulfadiazine cream. Recent research data islacking on most of the reviewed single entity local anti-infectives because of the age of the agents. Theagents in this class are either part of standard treatment (e.g., burn therapy) or not typically used in generalpractice (e.g., formaldehyde, sulfanilamide).Several small-scale studies have evaluated the role of various anti-infective agents (silver sulfadiazine,hexachlorophene, silver nitrate, and mafenide acetate) in the treatment of burn patients, finding them to beuseful in wound management. 10-14Formaldehyde solution is a bactericidal disinfectant that hardens the epidermis, rendering it tough andwhitish. International Agency for Research on Cancer (IARC) has concluded that formaldehyde is a humancarcinogen. In addition, according to the FDA and the American Academy of Pediatrics Committee onFetus and Newborn, hexachlorophene is not recommended to be used for total body bathing of infants dueto risk of toxicity. 9There is insufficient data to support that one brand single entity skin and mucous membrane miscellaneouslocal anti-infective is safer or more efficacious than another. Therefore, all brand products within the classreviewed are comparable to each other and to the generics and over-the-counter products in this class andoffer no significant clinical advantage over other alternatives in general use.XI.RecommendationsNo brand single entity skin and mucous membrane miscellaneous local anti-infective is recommended forpreferred status. Alabama Medicaid should accept cost proposals from manufacturers to determine costeffective products and possibly designate one or more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.228
References1. Madoff LC. Infectious complications of bites and burns. In: Braunwald E, Harrison TR, eds. Harrison’sPrinciples of Internal Medicine. 16 th ed. New York, McGraw-Hill, 2005.2. Mozingo DW, Cioffi WG, Pruitt BA. Burns. In: Bongard FS, Sue DY, eds. Current Critical Care Diagnosis &Treatment. 2 nd ed. New York: McGraw-Hill; 2003.3. Vu H, McCoy LF, Carino E, et al. Burn wound infection susceptibilities to topical agents: the Nathan’s AgarWell Diffusion Technique. P&T 2002;27(8):390-396.4. Bergstrom N, Bennett MA, Carlson CE, et al. <strong>Clinical</strong> Practice Guideline Number 15: Treatment of PressureUlcers. Rockville, Md: US Dept of Health and Human Services, Public Health Service, Agency for Health CarePolicy and Research; 1994. AHCPR publication 95-0652. Available at:http://www.ahrq.gov/clinic/cpgonline.htm. Accessed December 28, 2006.5. Consensus Development Conference on Diabetic Foot Wound Care: 7-8 April 1999,Boston, Massachusetts.American Diabetes Association. Diabetes Care. 1999 Aug;22(8):1354-1360.6. Healthcare infection control practices advisory committee (HICPAC), Hand-hygiene task force: Guideline forhand hygiene in healthcare settings. J Am Coll Surg 2004;198(1):121-7.7. Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2006.MMWR 2006;55(No. RR-11):1-100. Available at: http://www.cdc.gov/std/treatment/default.htm. AccessedNovember, 2006.8. Wickersham RM, Novak KK, managing eds. Drug Facts and Comparisons. St. Louis, MO: Wolters KluwerHealth, Inc.; 2006.9. Formaldehyde: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006. AccessedOctober, 2006.10. Hexachlorophene: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006. AccessedOctober, 2006.11. Mafenide acetate: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006. AccessedOctober, 2006.12. Silver nitrate: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006. AccessedOctober, 2006.13. Silver sulfadiazine: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006. AccessedOctober, 2006.14. Micromedex® Healthcare Series, (electronic version). Thomson Micromedex, Greenwood Village, CO, USA.Available at: http://www.thomsonhc.com. Accessed October, 2006.15. Tatro DS, ed. Drug Interaction Facts. St. Louis, MO: Wolters Kluwer Health, Inc.; 2006.16. Barret JP, Dziewulski P, Ramzy PI, et al. Biobrane versus 1% silver sulfadiazine in second-degree pediatricburns. Plast Reconstr Surg 2000;105(1):62-65.17. Dire DJ, Coppola M, Dwyer DA, et al. Prospective evaluation of topical antibiotics for preventing infections inuncomplicated soft-tissue wounds repaired in the ED. Acad Emerg Med 1995 Jan;2(1):4-10.18. Bodey GP, Edersole R, Hong H. Randomized trial of a hexachlorophene preparation and P-300 bacteriostaticsoaps. J Invest Dermatol 1976;67(4):532-537.19. Heinle EC, Dougherty WR, Garner WL, et al. The use of 5% mafenide acetate solution in the postgrafttreatment of necrotizing fasciitis. J Burn Care Rehabil 2001;22:35-40.20. Kucan JO, Smoot EC. Five percent mafenide acetate solution in the treatment of thermal injuries. J Burn CareRehabil 1993;14:158-163.21. DuBouchet L, Spence MR, Rein MF, et al. Multicenter comparison of clotrimazole vaginal tablets, oralmetronidazole, and vaginal suppositories containing sulfanilamide, aminacrine hydrochloride, and allantoin inthe treatment of symptomatic trichomoniasis. Sex Transm Dis 1997;24(3):156-160.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.229
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane Local Anti-infectives,MiscellaneousCombination ProductsAHFS Class 840492February 7, 2007I. OverviewThe combination skin and mucous membrane local anti-infectives, miscellaneous include products containacetic acid and oxyquinoline, with or without ricinoleic acid. These products are indicated as adjunctivetherapy in cases where restoration and maintenance of vaginal acidity is desirable, such as in bacterialvaginosis (BV). BV is the most common cause of vaginitis in women of childbearing age, and accounts for22%-50% of all forms of vaginitis in the United States. 1,2 BV is a polymicrobial infection, precipitated by areduction of hydrogen peroxide producing lactobacilli, an increase in vaginal pH, and an overgrowth ofanaerobic organisms. The combination of acetic acid and oxyquinoline, with or without ricinoleic acid, isused as adjunctive therapy to restore and maintain vaginal acidity.The combination skin and mucous membrane local anti-infectives, miscellaneous that are included in thisreview are listed in Table 1. This review encompasses all (topical) dosage forms and strengths. Productssolely indicated for the treatment of acne and/or rosacea are not covered by Alabama Medicaid; hence,these products are not included in this review.Table 1. Combination Skin and Mucous Membrane Local Anti-infectives, Miscellaneous Included inthis <strong>Review</strong>Generic Name(s) Formulation(s) Example Brand Name(s) Current PDLAgent(s)acetic acid and oxyquinoline vaginal jelly Relagard ® * acetic acid andoxyquinolineacetic acid, oxyquinoline, andricinoleic acid*Generic is available in at least one dosage form or strength.†Brand is no longer available.N/A=not availablevaginal jelly Aci-Jel ® *† acetic acid,oxyquinoline,and ricinoleicacidII.Evidence-Based Medicine and Current Treatment GuidelinesCurrent treatment guidelines that incorporate the combination skin and mucous membrane local antiinfectives,miscellaneous are summarized in Table 2.Table 2. Treatment Guidelines Using the Combination Skin and Mucous Membrane Local Antiinfectives,Miscellaneous<strong>Clinical</strong> GuidelineRecommendation(s)American College ofObstetricians and Gynecologists(ACOG): <strong>Clinical</strong> ManagementGuidelines for Obstetrician-Gynecologists 1 ••Nonpregnant women with bacterial vaginosis can be treated witheither vaginal clindamycin, oral clindamycin, vaginal metronidazole,or oral metronidazole products.All of the above regimens are comparable in terms of efficacy andsafety.• The combination miscellaneous local anti-infectives were notmentioned in these recommendations.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.230
<strong>Clinical</strong> GuidelineRecommendation(s)Centers for Disease Control and • Bacterial vaginosis in nonpregnant persons: CDC guidelinesPrevention (CDC) ) Morbidityand Mortality Weekly Report(MMWR): Sexually TransmittedDiseases Treatment Guidelines,2006 2 •recommend the use of either metronidazole gel 0.75% (one 5-gapplicator per day, intravaginally) for 5 days, clindamycin cream 2%(one 5-g applicator intravaginally) for 7 days every evening, ormetronidazole 500 mg capsules twice daily for 7 days.The oral and vaginal metronidazole regimens are equally efficacious.The 2 g single dose metronidazole therapy is no longerrecommended.• Two alternative regimens are clindamycin ovules, 100 mgintravaginally at bedtime for 3 days or clindamycin 300 mg capsulestwice daily for 7 days.• Clindamycin vaginal cream and ovules are comparable in efficacy.• Bacterial vaginosis in pregnant persons: CDC guidelines recommendthe use of either metronidazole 500 mg twice daily, 250 mg threetimes daily, or clindamycin 300 mg twice daily for 7 days.According to some specialists, systemic therapy is preferred intreating pregnant patients with bacterial vaginosis.• The combination miscellaneous local anti-infectives were notmentioned in these recommendations.British Association for SexualHealth and HIV, <strong>Clinical</strong>Effectiveness Group: NationalGuideline for the Managementof Bacterial Vaginosis (2006) 3 ••The guideline recommends the use of metronidazole oral capsulesgiven as either a single 2 g dose or as 400-500 mg twice daily for 5-7days.Alternative regimens include: intravaginal metronidazole gel(0.75%) once daily for 5 days, clindamycin cream (2%) once dailyfor 7 days, clindamycin 300 mg twice daily for 7 days, or tinidazole2 g single dose.• While all of the regimens have similar efficacy, oral metronidazoleis less expensive compared with the topical products.• Intravaginal products are preferred in lactating women.• The combination miscellaneous local anti-infectives were notmentioned in these recommendations.III.IndicationsFood and Drug Administration (FDA)-approved indications for the combination skin and mucousmembrane local anti-infectives, miscellaneous are noted in Table 3.Table 3. FDA-Approved Indications for the Combination Skin and Mucous Membrane Local Antiinfectives,Miscellaneous 4,5,6AgentRestoration and Maintenance of Vaginal Acidity;AdjunctAcetic acid and oxyquinolineaAcetic acid, oxyquinoline, and ricinoleic acidaIV.PharmacokineticsA literature search failed to retrieve pharmacokinetic data for the combination skin and mucous membranelocal anti-infectives, miscellaneous.V. Drug InteractionsA literature search indicates that there are no significant drug interactions with the combination skin andmucous membrane local anti-infectives, miscellaneous. 4-7Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.231
VI.Adverse Drug EventsSince only a small percentage of the drug is absorbed, most adverse drug events occur at the site ofapplication. The most common adverse drug events reported with the combination skin and mucousmembrane local anti-infectives, miscellaneous are noted in Table 4.Table 4. Adverse Drug Events (%) Reported with the Combination Skin and Mucous MembraneLocal Anti-infectives, Miscellaneous 4,5, 6Adverse Event(s) Acetic Acid and Oxyquinoline Acetic Acid, Oxyquinoline,and Ricinoleic AcidDermatologicalBurning a aStinging a aaPercent not specified-Event not reportedVII.Dosing and AdministrationThe usual dosing regimens for the combination skin and mucous membrane local anti-infectives,miscellaneous are summarized in Table 5.Table 5. Usual Dosing for the Combination Skin and Mucous Membrane Local Anti-infectives,Miscellaneous 4,5,6Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityAcetic acid andoxyquinolineAcetic acid,oxyquinoline, andricinoleic acidVIII. EffectivenessOne applicatorful, administeredintravaginally, morning and evening;duration of treatment may bedetermined by the patient’s responseto therapyOne applicatorful, administeredintravaginally, morning and evening;duration of treatment may bedetermined by the patient’s responseto therapySafety and efficacy inchildren have notbeen establishedSafety and efficacy inchildren have notbeen establishedVaginal jelly:acetic acid 0.9%,oxyquinoline sulfate0.025%Vaginal jelly:glacial acetic acid0.921%, oxyquinolinesulfate 0.025%,ricinoleic acid 0.7%A thorough literature search failed to retrieve any clinical studies evaluating the safety and effectiveness ofthe combination skin and mucous membrane local anti-infectives, miscellaneous.Additional EvidenceDose SimplificationA search of Medline and Ovid did not reveal data pertinent to this topic.Stable TherapyA search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician VisitsA search of Medline and Ovid did not reveal data pertinent to this topic.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.232
IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 6. Relative Cost of the Combination Skin and Mucous Membrane Local Anti-infectives,MiscellaneousGeneric Name(s) Formulation(s) Example BrandName(s)BrandCostGenericCostacetic acid and oxyquinoline vaginal jelly Relagard ® * $ $acetic acid, oxyquinol, andricinoleic acidvaginal jelly Aci-Jel ® *† N/A $*Generic is available in at least one dosage form or strength.†Brand is no longer available.N/A=not availableX. ConclusionsAcetic acid and oxyquinoline, with or without ricinoleic acid, are used as adjunctive therapy in conditionswhere restoration and maintenance of vaginal acidity is desirable (e.g., bacterial vaginosis). 4,5,6 Systemicabsorption of either product is minimal. Consequently, there are no significant drug interactions with thecombination skin and mucous membrane local anti-infectives, miscellaneous and the only reported adverseevents are burning and stinging at the site of application. There are no clinical studies comparing theseagents to each other or to other anti-infective agents, such as clindamycin or metronidazole for thetreatment of bacterial vaginosis. The current treatment guidelines for bacterial vaginosis do not includethese products in their recommendations. Both of the combination skin and mucous membrane local antiinfectives,miscellaneous discussed in this review are available in a generic formulation.Therefore, all brand products within the class reviewed are comparable to each other and to the genericsand over-the-counter products in this class, and offer no significant clinical advantage over otheralternatives in general use.XI.RecommendationsNo brand combination skin and mucous membrane miscellaneous local anti-infective is recommended forpreferred status. Alabama Medicaid should accept cost proposals from manufacturers to determine costeffective products and possibly designate one or more preferred brands.233Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
References1. ACOG Committee on Practice Bulletins—Gynecology. ACOG practice bulletin: clinical managementguidelines for obstetrician-gynecologists, Number 72, May 2006: Vaginitis. Obstet Gynecol 2006;107(5):1195-1206.2. Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2006.MMWR 2006;55(No. RR-11):1-100. Available at: http://www.cdc.gov/std/treatment/default.htm. AccessedDecember, 2006.3. British Association for Sexual Health and HIV: <strong>Clinical</strong> Effectiveness Group. National Guideline For TheManagement Of Bacterial Vaginosis (2006). Available at:http://www.bashh.org/guidelines/2006/bv_final_0706.pdf. Accessed December, 2006.4. Fem pH ® [drug information]. Available at: http://www.pharmics.com/femph.htm. Assessed December, 2006.5. Acid Jelly ® [drug information]. Available at: http://www.hopepharm.com/acidjelly/prescribe.html. AssessedDecember, 2006.6. Acidic Vaginal ® [drug information]. Available at: www.Pharmacyhealth.net. Accessed December, 2006.7. Tatro DS, ed. Drug Interaction Facts. St. Louis, MO: Wolters Kluwer Health, Inc.; 2006.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.234
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane Anti-inflammatory AgentsSingle Entity AgentsAHFS Class 840600February 7, 2007I. OverviewMillions of people are affected annually with skin diseases that cause marked discomfort, significantmorbidity, and rarely death. A major quality-of-life issue is raised by the prevalence of common chronicinflammatory skin diseases such as atopic dermatitis (AD) and psoriasis, which give rise to significantpsychosocial morbidity and negative health effects. Topical corticosteroids are utilized for symptomaticrelief and treatment of both acute and chronic inflammatory dermatoses. While systemic corticosteroidsare typically more effective in most dermatologic inflammatory conditions, they are typically reserved formore widespread and advanced conditions. 1 Topical treatment is preferred in most cases with limited orlocalized involvement, and to help minimize systemic adverse effects. The mechanism of action of thecorticosteroids is complex and not completely understood. After entering the cell through passivediffusion, they are able to bind to specific receptors. The steroid compounds possess various bindingaffinities to the large number of receptors in almost every tissue (there are between 5,000 and 100,000receptors per cell) and therefore elicit a wide variety of biologic effects. 2 Corticosteroids play an importantand routine role in various dermatologic conditions because of their anti-inflammatory andimmunosuppressive effects, as well as their ability to suppress mitotic activity and cause localizedvasoconstriction.Since the introduction of hydrocortisone in the early 1950s, treatment with topical corticosteroids has beenwidely utilized. The primary vasoconstrictor assay is the method commonly used to classify the potency oftopical steroids, and provides a way to differentiate the drugs in this class that generally correlates withclinical efficacy. 3 The hydrocortisone molecule and its analogues have been modified via halogenation,methylation, acetylation, esterification, and/or double-band induction to increase the therapeutic effects andminimize side effects. 4 The efficacy and adverse effect profiles of these agents are highly dependent on avariety of factors including steroid type, the vehicle used, application method, nature and extent of the skindisease, and specific patient factors, such as age and site of the disease. Currently there is at least one agentin each potency group available generically and hydrocortisone is available in various formulations overthe-counter.Topical corticosteroids are generally most effective in the treatment of acute or chronic dermatoses, such asseborrheic or atopic dermatitis, localized neurodermatitis, anogenital pruritus, psoriasis, and theinflammatory phase of xerosis. 1 They are also effective in the late phase of allergic contact dermatitis orirritant dermatitis, but systemic corticosteroids are most often utilized to relieve the acute manifestations ofthese conditions. 1The single entity skin and mucous membrane anti-inflammatory agents that are included in this review arelisted in Table 1. This review encompasses all (topical) dosage forms and strengths. In accordance withPreferred Drug List (PDL) Legislation, this review does not include information on Verdeso (desonide0.05% foam) because it has not been on the market for at least 6 months. This medication will be reviewedat a future time.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.235
Table 1. Single Entity Skin and Mucous Membrane Anti-inflammatory Agents Included in this<strong>Review</strong>Generic Name(s) Formulation(s) Example Brand Name(s) Current PDLAgent(s)alclometasone cream, Aclovate ® *alclometasoneointmentamcinonidecream, lotion, Cyclocort ® *amcinonidebetamethasonedipropionatebetamethasonedipropionate andpropylene glycolbetamethasonevalerateclobetasolointmentaerosol, cream,gel, lotion,ointmentcream, lotion,ointmentAlphatrex ® *, Diprosone ® *Diprolene ® *, Diprolene AF ® *Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.236betamethasonedipropionatebetamethasonedipropionate andpropylene glycolbetamethasonevalerateclobetasolcream, foam, Beta-Val ® *, Luxiq ®lotion, ointmentcream, foam, Clobex ® , Cormax ® *, Embeline ® *,gel, lotion, Embeline E ® *, Olux ® , Temovate ® *,ointment, Temovate E ® *, Temovate Emollient ® *shampoo,solution, sprayclocortolone cream Cloderm ® nonedesonidecream, lotion, Desowen ® *, Tridesilon ® *desonideointmentdesoximetasone cream, gel, Topicort ® *, Topicort LP ® *desoximetasoneointmentdiflorasonecream, Apexicon ® *, Apexicon E ® *, Psorcon E ® * diflorasoneointmentfluocinolonecream, oil, Capex Shampoo ® , Derma-Smoothe/FS ® , Capexointment, Synalar ® *Shampoo ® ,shampoo,DermasolutionSmoothe/FS ® ,fluocinonideflurandrenolidefluticasonehalcinonidehalobetasolhydrocortisone‡hydrocortisoneacetate‡cream, gel,ointment,solutioncream, lotion,ointment, tapecream, lotion,ointmentcream,ointment,solutioncream,ointmentcream, enema,gel, lotion,ointment,solution, spraycream, foam,lotion,Lidex ® *, Lidex-E ® *, Vanos ®Cordran ® , Cordran SP ®Cutivate ® *Halog ®Ultravate ® *Anusol-HC ® *, Aquanil HC ® *, Beta HC ® *,Cetacort ® *, Colocort ® *, Cortaid ® *,Cortizone-10 ® *, Dermolate Anti-Itch ® *,Dr. Smith's Anti-Itch ® *, Hytone ® *,Hydrocortisone ® , Instacort-10 ® *,Nutracort ® *, Preparation H ® *,Proctocort ® *, Proctocream-HC ® *, RecortPlus ® *, Sarnol-HC ® *, Summer's Eve ® *,Texacort ® *Cortaid ® *, Cortifoam ® , Medi-Cortisone ® *fluocinolonefluocinonidenonefluticasonenonehalobetasolhydrocortisonehydrocortisoneacetate
Generic Name(s) Formulation(s) Example Brand Name(s) Current PDLAgent(s)ointment,packet, rectalsuppositoryhydrocortisonebutyratehydrocortisoneprobutatehydrocortisonevaleratemometasoneprednicarbatetriamcinolonetriamcinoloneacetonide and sodiumlauryl sulfatecream,ointment,solutionLocoid ® *, Locoid Lipocream ®cream Pandel ® nonehydrocortisonebutyratecream,ointmentWestcort ® *hydrocortisonevaleratecream, Elocon ® *mometasoneointment, lotioncream, Dermatop ® *prednicarbateointmentaerosol, cream, Aristocort ® *, Aristocort HP ® *, Kenalog ® * triamcinolonelotion,ointment, pastecream Aristocort A ® none*Generic is available in at least one dosage form or strength.‡Over-the-counter product is available in at least one dosage form or strength.Table 2. Relative Potency Ratings of the Single Entity Skin and Mucous Membrane AntiinflammatoryAgents 1,3,5,6Group*Generic Name Strength Formulation(s)(I=highest potency;VII = lowest potency)Ibetamethasone dipropionate 0.05% cream, lotion, ointmentand propylene glycolI clobetasol 0.05% cream, foam, gel, lotion,ointment, shampoo, solution,sprayI fluocinonide 0.1% creamI flurandrenolide 4 mcg/cm 2 tapeI halobetasol 0.05% cream, ointmentII amcinonide 0.1% lotion, ointmentII betamethasone dipropionate 0.05% ointmentII betamethasone dipropionate 0.1% aerosolII desoximetasone 0.05% gelII desoximetasone 0.25% ointmentII diflorasone 0.05% ointmentII fluocinonide 0.05% cream, gel, ointment, solutionII halcinonide 0.1% ointmentIII amcinonide 0.1% creamIII betamethasone dipropionate 0.05% cream, gelIII betamethasone valerate 0.1% ointmentIII desoximetasone 0.25% creamIII diflorasone 0.05% creamIII fluticasone 0.005% ointmentIII halcinonide 0.1% cream, solutionPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.237
Group*Generic Name Strength Formulation(s)(I=highest potency;VII = lowest potency)III mometasone 0.1% ointmentIII triamcinolone 0.5% cream, ointmentIIItriamcinolone acetonide and 0.5% creamsodium lauryl sulfateIV betamethasone valerate 0.12% foamIV desoximetasone 0.05% creamIV fluocinolone 0.025% ointmentIV flurandrenolide 0.05% ointmentIV fluticasone 0.05% cream, lotionIV hydrocortisone valerate 0.2% ointmentIV mometasone 0.1% cream, lotionIV prednicarbate 0.1% ointmentIV triamcinolone 0.1% ointmentV betamethasone dipropionate 0.05% lotionV betamethasone valerate 0.1% cream, lotionV clocortolone 0.1% creamV fluocinolone 0.025% creamV flurandrenolide 0.05% cream, lotionV hydrocortisone butyrate 0.1% cream, ointment, solutionV hydrocortisone valerate 0.2% creamV hydrocortisone probutate 0.1% creamV prednicarbate 0.1% creamV triamcinolone (Kenalog ® ) 0.1% cream, lotion, pasteVI alclometasone 0.05% cream, ointmentVI desonide 0.05% cream, lotion, ointmentVI fluocinolone 0.01% cream, oil, shampoo, solutionVI triamcinolone 0.025% aerosol, cream, lotion,ointmentVI triamcinolone (Aristocort ® ) 0.1% creamVItriamcinolone acetonide and 0.025% creamsodium lauryl sulfateVItriamcinolone acetonide andsodium lauryl sulfate0.1% creamVIIhydrocortisone,hydrocortisone acetate (all)all strengths*Potency ratings are given following the Stoughton-Cornell classification of topical glucocorticoid potency.cream, enema, foam, gel,lotion, ointment, packet,rectal suppository, solution,sprayII.Evidence-Based Medicine and Current Treatment GuidelinesCurrent treatment guidelines that incorporate the single entity skin and mucous membrane antiinflammatoryagents are summarized in Table 3.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.238
Table 3. Treatment Guidelines Using the Single Entity Skin and Mucous Membrane AntiinflammatoryAgents<strong>Clinical</strong> GuidelineRecommendation(s)American Academy of• The strength and vehicle of a topical corticosteroid selectedDermatology (AAD): Guidelinesof Care for the Use of TopicalGlucocorticosteroids 4 •depends on the nature, location, and extent of the skinlesions, the patient’s age, and duration of therapy.Ointments are generally the most effective vehicle fortreating thick, fissured, lichenified skin lesions. Theocclusive nature of the vehicle enhances corticosteroidpenetration. However, some patients may considerointments aesthetically undesirable.• Creams are generally the vehicle of choice for acute andsubacute dermatoses. They may be used on moist areas ofthe skin and in intertriginous areas and are generallyaesthetically acceptable to patients. Cream vehicles may bedrying, and patients may benefit from applying moisturizersin addition to the corticosteroid cream.• Solutions, gels, and sprays are generally the vehicles mostaesthetically pleasing for use on the scalp. They are alsouseful when a non-oil-based vehicle is desirable. Frequentlycontaining alcohol and propylene glycol, these particularvehicles may cause irritation or burning if applied to acutedermatoses, erosions, or fissures.• Usage of the lowest potency corticosteroid that is effective isrecommended, especially in children and infants and for theface and intertriginous areas.• Corticosteroids of low- to medium-strength are preferredwhen large areas of the body are to be treated, to helpminimize systemic absorption.• Short-term use of more potent agents is occasionallyrequired; however, these agents should rarely be used in thediaper area of infants and avoided whenever possible.• The duration of use of very-high-strength topical agentsshould not exceed 3 weeks.• Intermittent therapy may be preferred to long-termcontinuous therapy to help minimize side effects.American Academy of• Topical corticosteroids are the standard of care to whichDermatology (AAD)/AmericanAcademy of DermatologyAssociation: Guidelines of Carefor Atopic Dermatitis 7 ••other treatments are compared.Cutaneous complications such as striae, atrophy, andtelangiectasia limit the extensive use of these agents.Altering the local environment by hydration and/orocclusion, as well as by varying the vehicle, can impact theabsorption and effects of the topical corticosteroid used.• Tachyphylaxis is a clinical concern, but there is noexperimental documentation.Joint Task Force on PracticeParameters in Collaboration with• Topical corticosteroids, applied to areas of eczema, areeffective treatment for atopic dermatitis.the American College of Allergy,Asthma and Immunology(ACAAI), the AmericanAcademy of Allergy, Asthma,• Low-potency agents are recommended for maintenancetherapy, whereas intermediate- and high-potency agentsshould be used for clinical exacerbations and should beapplied over short periods of time.and Immunology (AAAAI), and • Potent fluorinated agents should be avoided on the face,the Joint Council of Allergy,eyelids, genitalia, intertriginous areas, and in infants.Asthma and Immunology • Low-potency agents are generally recommended for areas(JCAAI): Disease Management with increased potential for transepidermal penetration,of Atopic Dermatitis: Anincluding mucous membranes, genitalia, eyelids, face, and239Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
<strong>Clinical</strong> GuidelineRecommendation(s)Updated Practice Parameter 8 intertriginous areas.• Intermediate-potency agents can be used for longer periodsof time than high-potency agents to treat chronic conditionsinvolving the trunk and extremities.• High-potency agents should only be used for short periods oftime (up to 3 weeks) for clinical exacerbations.• Ultrahigh-potency agents should only be used for very shortperiods of time (up to several days) and limited to lichenifiedareas.Primary Care Dermatology • Recommendations for prevention include avoidance ofthe Management of Atopic • Emollients should be applied three to four times daily onEczema 9 moist skin up to 600 g/week for adults and 250 g/week forSociety & British Association of exacerbating factors and maintenance of well-hydrated skin.Dermatologists: Guidelines for • Early treatment of infections is recommended.children. Use of combined emollient and corticosteroidshould meet the ratio of 10:1.• Topical corticosteroids should be used a few days for acuteeczema and up to 4 to 6 weeks for chronic eczema. Morepotent corticosteroids are indicated in eczema of the handsand feet.• Immunomodulatory agents may be initiated if a patient isintolerant to corticosteroids, or has failed corticosteroidtherapy.• Sedating systemic antihistamines are more effective thannonsedating ones for relief of pruritus.• Short courses of corticosteroid-antibiotic combinations areeffective in clinical practice, but published evidence-basedliterature on their efficacy is lacking.• Specific combination products were not addressed within theguidelines.American Academy of FamilyPhysicians (AAFP): Treatmentof Psoriasis: An Algorithm-Based Approach for PrimaryCare Physicians 10 ••Topical therapy is the mainstay of treatment for localizeddisease.Treatment options include anthralin, calcipotriene, coal tarproducts, corticosteroids, and tazarotene. Use of emollientsshould be encouraged, but they should be used selectivelybecause many products (e.g., those containing lactic acid oralpha-hydroxy acids) can be irritating to inflamed or brokenskin.• While topical corticosteroids are the mainstay of treatmentfor psoriasis, coal tar and anthralin are effective treatmentoptions.• Coal tar is effective when it is combined with topicalcorticosteroids. Coal tar shampoo can be used incombination with a corticosteroid scalp solution for thetreatment of psoriasis on the scalp.• If good control of psoriasis is not achieved with topicalcorticosteroids, alone or in combination with calcipotriene orcoal tar, consideration should be given to the addition ofanthralin or tazarotene therapy.British Association ofDermatologists: PsoriasisGuideline 2006 11 • Therapy depends on the affected sites, and the extent andseverity of psoriasis, in addition to the patient’s age, sex,occupation, personality, and general health.• Emollients are recommended to soften scaling and reduceirritation.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.240
<strong>Clinical</strong> GuidelineRecommendation(s)• Topical corticosteroids are effective, cosmeticallyacceptable, and safe if used appropriately. There is a widerange of strengths available from mild to potent. Tolerancemay develop, as well as rebound exacerbations upondiscontinuation. Topical corticosteroids should be rotatedwith nonsteroidal treatments. Potent corticosteroids shouldnot be used for more than 7 days consecutively.• Tar and topical corticosteroids have a synergistic effect, andsome dermatologists adopt a regimen of a moderately potenttopical corticosteroid by day, with coal tar at night, for easeof patient use.The AmericanGastroenterological Association:Technical <strong>Review</strong> on theDiagnosis and Treatment ofHemorrhoids 12 ••Universal recommendations include adding fiber to the dietand avoiding straining at defecation.Over-the-counter topical agents are recommended despitethe lack of supportive data regarding their efficacy.• Topical analgesics are useful for symptom relief of pain anditching.• Corticosteroid creams may decrease local inflammation butlong-term use of high potency steroids should be avoided.• There is no data to show that corticosteroids reducehemorrhoidal swelling, bleeding, or protrusion.• Topical nitroglycerin may relieve pain associated withhemorrhoids by decreasing anal tone.• Flavonoids may be of benefit since they may increasevenous tone, lymphatic drainage, capillary resistance, andmay normalize capillary permeability.• Nonoperative treatment, such as banding and sclerotherapy,and operative procedures such as hemorrhoidectomy may beuseful in patients with more severe hemorrhoids and in thosenot responding to other treatments.American Society of Colon andRectal Surgeons:Practice Parameters for theManagement of Hemorrhoids 13 ••Medical treatment includes warm sitz baths, dietarycorrection, stool modifiers, and topical creams.Long-term use of topical steroids should be avoided.• Rubber band ligation, hemorrhoidectomy, and otherprocedures are reserved for patients who fail moreconservative therapy.American Society of Colon andRectal Surgeons:Practice Parameters for theManagement of Hemorrhoids,2005 Update 14 ••Dietary management, including adequate fiber and fluidintake, is the primary management recommendation.Office treatment (including rubber band ligation,sclerotherapy, cryotherapy, etc.) and surgical interventionare reserved for patients with more severe hemorrhoids orthose not responding to more conservative therapy.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.241
III.IndicationsFood and Drug Administration (FDA)-approved indications for the single entity skin and mucousmembrane anti-inflammatory agents are noted in Table 4.Table 4. FDA-Approved Indications for the Single Entity Skin and Mucous Membrane Anti-inflammatoryAgents 14-33Drug(s) Dermatosesof the AnalRegionDermatosesof the ScalpInflammatoryand PruriticDermatosesOralInflammatoryor UlcerativePlaquePsoriasisSelf-Medication(OTC)Lesions FromTraumaAlclometasoneaAmcinonideaBetamethasoneadipropionateBetamethasoneadipropionate andpropylene glycolBetamethasoneavalerateClobetasol a a aClocortoloneaDesonideaDesoximetasoneaDiflorasoneaFluocinoloneaFluocinonideaFlurandrenolideaFluticasoneaHalcinonideaHalobetasolaHydrocortisone* a aHydrocortisonea a aaacetate*(paste)HydrocortisoneabutyrateHydrocortisoneaprobutateHydrocortisoneavalerateMometasoneaPrednicarbateaTriamcinoloneaaacetonide(paste)Triamcinoloneaacetonide and sodiumlauryl sulfate*Hydrocortisone and hydrocortisone acetate nonprescription preparations are used for the temporary relief of minor skin irritations, itching, andrashes caused by eczema, dermatitis, insect bites, poison ivy, poison oak, poison sumac, soaps, detergents, cosmetics, or jewelry. They can alsobe used for the temporary relief of itchy anal and/or genital areas, and for temporary relief of itching and minor scalp irritation caused by scalpdermatitis. Hydrocortisone acetate, probutate, butyrate, and valerate esters can also be used for dermatoses of the anogenital area.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.242
IV.PharmacokineticsThe pharmacokinetic parameters for the single entity skin and mucous membrane anti-inflammatory agentsare summarized in Table 5.Table 5. Pharmacokinetic Parameters of the Single Entity Skin and Mucous Membrane AntiinflammatoryAgents 14-34Drug (s) Systemic Absorption Distribution Excretion (Renal)Alclometasone 3% No data No dataAmcinonide No data No data No dataBetamethasoneVariable No data No datadipropionateBetamethasoneVariable No data No datadipropionate andpropylene glycolBetamethasoneVariable No data No datavalerateClobetasol No data No data No dataClocortolone Variable No data Urine and fecesDesonide Variable No data No dataDesoximetasone Variable Variable Urine and fecesDiflorasone ~ 1% No data No dataFluocinolone Variable No data Urine and fecesFluocinonide1 (thick stratum corneum) No dataUrine and fecesto 36% (thin stratumcorneum)Flurandrenolide Variable No data Urine and fecesFluticasone No data 0.02% No dataHalcinonide Variable No data UrineHalobetasol ~ 6% No data UrineHydrocortisone Rapid No data UrineHydrocortisone acetate Rapid No data UrineHydrocortisoneRapid No data UrinebutyrateHydrocortisoneRapid No data UrineprobutateHydrocortisoneRapid No data UrinevalerateMometasone 0.1% No data No dataPrednicarbate No data No data No dataTriamcinoloneVariable No data Urine and fecesacetonideTriamcinoloneacetonide and sodiumlauryl sulfateVariable No data Urine and fecesV. Drug InteractionsDue to limited systemic absorption when the single entity skin and mucous membrane anti-inflammatoryagents are administered topically, no drug interactions are likely to occur and none are documented withthese agents. More caution should be used in those patients using topical corticosteroids on large areas ofthe body, for prolonged periods of time, with an occlusive dressing, and/or in infants and children or whenpotent agents are used. Significant drug interactions with the skin and mucous membrane antiinflammatoryagents are not documented within the literature. 14-34Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.243
VI.Adverse Drug EventsSince the single entity skin and mucous membrane anti-inflammatory agents are administered topically and only a small percentage of drug is absorbed,most adverse drug events occur at the site of application. The most common adverse drug events reported with the single entity skin and mucous membraneanti-inflammatory agents are noted in Table 6.Table 6. Adverse Drug Events (%) Reported with the Single Entity Skin and Mucous Membrane Anti-inflammatory Agents 14-33Adverse Event(s)Central Nervous SystemAlclometasoneAmcinonideBetamethasone*Clocort-aloneAnxiety - - - - - - - 0-2 - - - - - - - - - -Asthenia - - - - - - - 0-2 - - - - - - - - - -Blurred vision - - - - - - - - - - - a - - - - - -Dizziness - - - - - - - 0-4 - - - - - - - - - -Headache - - - - - - - 0-7 - - - 2 - - - - - -Hypo-kinesia - - - - - - - 0-2 - - - - - - - - - -Migraine - - - - - - - 0-2 - - - - - - - - - -- - a - - - - - - a - - - - - - - -Reversible hypothalmicpituitaryadrenalaxissuppressionDermatologicalAcne - - - - - - - 0-4 - a - - a a - - - -Acniforma a a a
Adverse Event(s)AlclometasoneAmcinonideBetamethasone*Clocort-aloneatopic dermatitisExfoliation - - - - - - - 4-24 - - - - - - - - - -Fissuring - - - a - - - - - - - - - - - - - -Folliculitis a a a a - a 0.8 - a a a
Adverse Event(s)AlclometasoneAmcinonideBetamethasone*Clocort-aloneThinness - - - - - - - - - - - - - - - a a -Urticaria - - - - - - - - - - - a - a - - a -Endocrine and MetabolicHyperglycemia - - a - - 2 - - - a - a - - - - - -HematologicLeucopenia - - - - - - - - - - - a - - - - - -Thrombocytopeni - - - - - - - - - - - a - - - - - -aMusculoskeletalArthralgia - - - - - - - 0-2 - - - - - - - - - -Myalgia - - - - - - - 0-3 - - - - - - - - - -OtherCushing’sSyndromeaPercent not specified- Event not reported*All agents containing betamethasone.†All agents containing hydrocortisone.‡All agents containing triamcinolone.Fluocin-oloneFluocin-onide- - a a - - - - - a - a a - - - - -HalobetasolMomet-asoneClobetasolDesonideDesoximetasoneDiflorasoneFlurandrenolideFluticasoneHalcinonideHydrocortisone†PrednicarbateTriamcinolone‡Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.246
VII.Dosing and AdministrationThe usual dosing regimens for the single entity skin and mucous membrane anti-inflammatory agents aresummarized in Table 7.Table 7. Usual Dosing for the Single Entity Skin and Mucous Membrane Anti-inflammatoryAgents 14-33Drug(s) Usual Adult Dose Usual Pediatric Dose* AvailabilityAlclometasoneApply a thin film to theaffected area of the skintwo or three times dailyApply a thin film to theaffected area of the skintwo or three times dailyCream: 0.05%Ointment: 0.05%AmcinonideBetamethasonedipropionateBetamethasonedipropionate andpropylene glycolBetamethasonevalerateClobetasolApply to the affected areatwo to three times daily,lotion may be appliedtopically two times a dayCream, gel, and ointment:Apply 1-2 times dailyLotion:Apply a few drops 2 timesdailyCream and ointment:Apply 1-2 times dailyLotion:Apply a few drops 1-2times dailyCream and ointment:Apply 1-2 times dailyFoam and lotion:Apply 2 times daily in themorning and at nightCream, gel, lotion, andointment:Apply a thin layer to theaffected skin area 2 timesdaily for up to 2 weeksFoam and solution:Apply to scalp 2 timesdaily for up to 2 weeksShampoo:Apply thin film to dryscalp once daily, leave inSafety and efficacy inchildren have not beenestablishedChildren 13 years of ageand older:Cream and ointment:Apply 1-2 times dailyLotion:Apply a few drops 2 timesdailyChildren 13 years of ageand older:Cream, gel, and ointment:Apply 1-2 times dailyLotion:Apply a few drops 1-2times dailyChildren 13 years of ageand older:Cream and ointment:Apply 1-2 times dailyFoam and lotion:Apply 2 times daily in themorning and at nightChildren 12 years of ageand older:Cream, gel, lotion, andointment:Apply a thin layer to theaffected skin area 2 timesdaily for up to 2 weeksFoam and solution:Apply to scalp 2 timesdaily for up to 2 weeksCream: 0.1%Lotion: 0.1%Ointment: 0.1%Aerosol: 0.1%Cream: 0.05%Gel: 0.05%Lotion: 0.05%Ointment: 0.05%Cream: 0.05%Lotion: 0.05%Ointment: 0.05%Cream: 0.1%Foam: 0.12%Lotion: 0.1%Ointment: 0.1%Cream: 0.05%Foam: 0.05%Gel: 0.05%Lotion: 0.05%Ointment: 0.05%Shampoo: 0.05%Solution: 0.05%Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.247
Drug(s) Usual Adult Dose Usual Pediatric Dose* Availabilityplace for 15 minutes, addwater, lather, and rinseSpray: 0.05%ClocortoloneDesonideSpray:Spray directly ontoaffected area 2 times dailyand gently rub into skinfor up to 4 weeksApply sparingly andgently to affected areas 1-4 times dailyApply sparingly 2-4 timesdailyShampoo:Apply thin film to dryscalp once daily, leave inplace for 15 minutes, addwater, lather, and rinseSpray:Spray directly ontoaffected area 2 times dailyand gently rub into skinfor up to 4 weeksSafety and efficacy inchildren have not beenestablishedApply sparingly 2-4 timesper dayCream: 0.1%Cream: 0.05%Lotion: 0.05%DesoximetasoneApply a thin film toaffected area 2 times dailyApply a thin film toaffected area 2 times dailyOintment: 0.05%Cream: 0.05%, 0.25%Gel: 0.05%DiflorasoneCream:Apply sparingly toaffected area 2-4 timesper daySafety and efficacy inchildren have not beenestablishedOintment: 0.25%Cream: 0.05%Ointment: 0.05%FluocinoloneOintment:Apply sparingly toaffected area 1-3 timesdailyCream, ointment, andsolution:Apply a thin layer toaffected areas 2-4 timesper dayCream, ointment, andsolution:Apply a thin layer toaffected areas 2-4 timesper dayCream: 0.01%, 0.025%Oil: 0.01%Ointment: 0.025%Derma-Smoothe/FS®:Apply thin film toaffected area 3 times dailyDerma-Smoothe/FS®:Apply to moistened skin 2times dailyShampoo: 0.01%Solution: 0.01%FluocinonideShampoo (Capex ® ):Apply no more than 1ounce to scalp 1 timedaily, lather, keep onscalp for 5 minutes, andrinse thoroughly0.5% strength:Apply a thin layer toaffected area 2-4 timesdaily0.1% strength:Apply a thin layer 1-2Shampoo (Capex ® ):Apply no more than 1ounce to scalp 1 timedaily, lather, keep onscalp for 5 minutes, andrinse thoroughly0.5% strength:Apply a thin layer toaffected area 2-4 timesdaily0.1% strength:Apply a thin layer 1-2248Cream: 0.05%, 0.1%Gel: 0.05%Ointment: 0.05%Solution: 0.05%Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Drug(s) Usual Adult Dose Usual Pediatric Dose* Availabilitytimes dailytimes dailyFlurandrenolide Cream, lotion, ointment:Apply sparingly 2-3 timesdailyCream, lotion, ointment:Apply sparingly 1-2 timesdailyCream: 0.025%, 0.05%Lotion: 0.05%FluticasoneTape:Apply once daily (may bechanged every 12 hours tominimized adverseeffects)Atopic dermatitis:Apply sparingly toaffected area 1-2 timesdailyCorticosteroid-responsivedermatoses:Apply sparingly toaffected area 2 times dailyTape:Apply once daily (may bechanged every 12 hours tominimized adverseeffects)Atopic dermatitis inchildren 3 months of ageor older:Cream: apply sparingly toaffected area 1-2 timesdailyAtopic dermatitis inchildren 1 year of age orolder:Lotion: apply sparingly toaffected area 1 time dailyOintment: 0.025%,0.05%Tape: 4 mcg/cm 2Cream: 0.05%Lotion: 0.05%Ointment: 0.005%HalcinonideApply sparingly 1-3 timesdaily, occlusive dressingmay be usedCorticosteroid-responsivedermatoses in children 3months of age or older:Cream: apply sparingly toaffected area 2 times dailyApply sparingly 1-3 timesdaily, occlusive dressingmay be usedCream: 0.1%Ointment: 0.1%Halobetasol Apply sparingly to skin 2times daily, rub in gentlyand completelyHydrocortisone Apply to affected area 2-4times dailyEnema:Use 10-100 mg 1-2 timesdaily for 2-3 weeksChildren 12 years of ageand older:Apply sparingly to skin 2times daily, rub in gentlyand completelyApply to affected area 2-4times dailyEnema:Safety and efficacy inchildren have not beenestablishedSolution: 0.1%Cream: 0.05%Ointment: 0.05%Cream: 0.05%, 0.5%,1%, 2.5%Enema: 100 mg/60 mlGel: 1%, 10%Lotion: 0.25%, 0.5%,1%, 2.5%Ointment: 0.5%, 1%,2.5%Solution: 2.5%HydrocortisoneacetateApply to affected area 2-4 Apply to affected area 2-4times dailytimes daily249Spray: 1%Cream: 0.5%, 1%, 2.5%Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Drug(s) Usual Adult Dose Usual Pediatric Dose* AvailabilityFoam: 10%Lotion: 0.5%, 1%, 2.5%Ointment: 1%HydrocortisonebutyrateApply to affected area 2-3times dailyApply to the affected areaonce dailyRectal suppository: 25mg, 30 mgCream: 0.1%Ointment: 0.1%HydrocortisoneprobutateHydrocortisonevalerateMometasoneApply to affected area 1-2times dailyApply to affected area 2-3times dailyCream and ointment:Apply a thin film toaffected area of the skinonce dailyLotion:Apply a few drops toaffected area once dailySafety and efficacy inchildren have not beenestablishedSafety and efficacy inchildren have not beenestablishedChildren 2 years of ageand older (cream andointment): Apply a thinfilm to affected area ofthe skin once dailyChildren 12 years of ageand older (lotion):Apply a few drops toaffected area once dailySolution: 0.1%Cream: 0.1%Cream: 0.2%Ointment: 0.2%Cream:0.1%Lotion: 0.1%Ointment: 0.1%PrednicarbateTriamcinoloneacetonideTriamcinoloneacetonide andsodium laurylsulfateApply a thin film toaffected area 2 times dailyAerosol:Apply to affected area 3-4times dailyCream, lotion, andointment:Apply a thin film 2-4times dailyPaste:Press a small dab (1/4inch) to the lesion until athin film develops up to 4times dailyApply a thin film 2-4times dailySafety and efficacy inchildren have not beenestablishedAerosol:Apply to affected area 3-4times dailyCream, lotion, andointment:Apply a thin film 2-4times daily (0.1% or 0.5%formulations should beapplied 2-3 times daily)Paste:Press a small dab (1/4inch) to the lesion until athin film develops up to 4times dailyApply a thin film 2-4times daily (0.1% or 0.5%formulations should beapplied 2-3 times daily)Cream: 0.1%Ointment: 0.1%Aerosol: 0.2 mg/2second sprayCream: 0.025%, 0.1%,0.5%Lotion: 0.025%, 0.1%Ointment: 0.025%,0.1%, 0.5%Paste: 0.1%Cream: 0.025%, 0.1%,0.5%*Administration of topical corticosteroids to children should be limited to the least amount compatible with an effective therapeuticregimen.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.250
VIII. Effectiveness<strong>Clinical</strong> studies evaluating the safety and efficacy of the single entity skin and mucous membrane anti-inflammatory agents are summarized in Table 8.Table 8. Comparative <strong>Clinical</strong> Trials Using the Single Entity Skin and Mucous Membrane Anti-inflammatory AgentsStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsPsoriasisHuntley et al. 35Amcinonide 0.1%ointment, applied twicedailyvs.betamethasonedipropionate 0.05%ointment, applied twicedailyRCT, DB, PGPatients with moderateto severe psoriasisN=312 weeksPrimary:Evaluation ofpapules/plaques,erythema, scales,itching, burning,and painSecondary:Patient-evaluatedcosmetic efficacyPrimary:At the week 1 evaluation point, an overall investigator rating ofeither “excellent” or “good” was made for 14/16 patients in theamcinonide group compared to 8/15 patients in the betamethasonegroup (P
StudyandDrug Regimenfluocinonide 0.05%ointment, applied threetimes dailyEngel 37Amcinonide 0.1%ointment applied twicedailyvs.fluocinonide 0.05%ointment applied 3times a dayMillikan et al. 38Amcinonide 0.1%ointment, appliedtopically twice a dayvs.halcinonide 0.1%ointment, appliedtopically twice a dayStudy DesignandDemographicsRCT, DB, PGPatients with psoriasisDB, PGPatients aged 18-75years with psoriasisSample Sizeand StudyDurationN=503 weeksN=322 weeksEnd Pointsimprovement oflesionsSecondary:Patient-evaluatedcosmeticacceptabilityPrimary:Total score basedon (a) severity ofsigns: crusting,erythema,papules/plaques,scales, pustules (b)severity ofsymptoms: itching,burning, painSecondary:Not reportedPrimary:Patient- andinvestigatormeasured:itching,burning, pain,erythema, papulesor plaques andscalesSecondary:Patients completeda cosmeticacceptabilityquestionnaireResultsErythema, papules/plaques, and scaling were completely resolvedin 5%, 20%, and 35% of patients in the amcinonide group,compared to 5%, 11%, and 21% of patients in the fluocinonidegroup, respectively (P≤0.01).Secondary:No significant difference was reported between the two treatmentgroups (P value not reported).Primary:There were no significant differences found between the twotreatment groups in improvements in signs and symptoms, andtotal score between the two treatment groups (P value notreported).Overall improvement of psoriasis at endpoint was noted ascleared, excellent, or good in 22/26 (85%) amcinonide patientsand 18/24 (75%) flucinonide patients, respectively (P value notreported).Secondary:Not reportedPrimary:Evaluation at day 7 showed greater efficacy in the primaryendpoints in the amcinonide treatment group compared to thehalcinonide group (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsday 14 evaluation in 37% of the amcinonide group compared to8% of the halcinonide group, respectively (P value not reported).Katz et al. 39Betamethasonedipropionate 0.05%lotion, applied twice adayvs.clobetasol propionate0.05% solution, appliedtwice a dayRCT, MC, SB, PGPatients 18 years of ageand older with at least20% scalp-surfaceinvolvement ofmoderate-to-severe scalppsoriasis that had beenstable or worsening formore than 1 week priorto enrollmentN=1932 weeksPrimary:Scaling,induration,erythema, pruritus,complied into atotal sign andsymptom scoreSecondary:Not reportedSecondary:Results of questionnaire were not reportedPrimary:At day 4, the mean percent improvement for the betamethasonegroup was 39.1% compared to 31.8% in the clobetasol group,respectively (P=0.010).The percent improvement was greater in the betamethasone groupat day 8, with a 66.0% improvement compared to a 57%improvement for the clobetasol group, respectively (P≤0.005).Evaluations at day 15 showed an 82.8% improvement in thesign/symptom score for the betamethasone group compared to74.9% improvement in the clobetasol group, respectively(P≤0.015).Erythema was the only individual sign that was significantlydifferent between the two treatment groups at 14 days (P=0.023).The mean sign/symptom score was 1.5 in the betamethasonegroup compared to 2.3 in the clobetasol group, respectively(P≤0.009).Jacobson et al. 40Betamethasonedipropionate 0.05%ointment, applied twicedailyvs.MC, DBPatients with moderateto-severepsoriasisN=1302 weeksPrimary:Treatmentpreference,assessment ofefficacy of oneside compared tothe other(erythema, scaling,skin thickening),Secondary:Not reportedPrimary:At the end of the two-week treatment period, 41% of investigatorspreferred the response obtained from clobetasol compared to the8% of investigators who favored the response from betamethasone(P≤0.001).Overall magnitude of response (or at least a 75% reduction inerythema, scaling, and skin thickening) was greater on theclobetasol side (27 patients [22%]) compared to betamethasone (3253Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimenclobetasol propionate0.05% ointment,applied twice dailyBetamethasone wasapplied to one side andclobetasol to the otherShupack et al. 41Betamethasonedipropionate 0.05%ointmentvs.diflorasone diacetate0.05% ointmentBarsky 42Betamethasone 0.025%gel, applied 3 times adayvs.fluocinonide 0.05% gel,applied 3 times a dayBetamethasone wasapplied to one side andfluocinonide to theotherStudy DesignandDemographicsRCT, DB, PGPatients aged 18 yearsand older who have hadmoderate-severe plaquetypepsoriasis for at least6 monthsRCT, DB, MCPatients older than 2years with psoriasisSample Sizeand StudyDurationN=442 weeksN=2633 weeksEnd Pointsoverall magnitudeof responseSecondary:Not reportedPrimary:Erythema, scaling,induration,investigator’sevaluationSecondary:Patient satisfactionPrimary:Physicianevaluation oftherapeuticresponseSecondary:Physician andpatient preference(2-definitepreference forfluocinonide, 1-slight preference,0- no preference, -2 definitepreference forpatients [2 %]; P
StudyandDrug RegimenPacifico et al. 43Betamethasone valerate0.12% cream, appliedonce dailyvs.betamethasone valerate(BMV) 0.1% tape,applied once dailyBMV cream wasapplied to one side andBMV tape was appliedto the otherBergstrom et al. 44Clobetasol propionate0.05% foam, applied tothe skin and scalpvs.clobetasol cream0.05%, applied to theskinandclobetasol 0.05%solution, applied to thescalpStudy DesignandDemographicsRCT, PRO, SBPatients with mild tomoderate psoriasisRCT, SB,Patients with psoriasisSample Sizeand StudyDurationN=4230 daysN=3214 daysEnd Pointsbetamethasone, -1slight preferencePrimary:Psoriasis Area andSeverity Index(PASI) scores;hydration based oncutaneous trophismevaluationSecondary:Patient quality-oflifequestionnairePrimary:Patient quality oflife (QOL);effectiveness, usersatisfaction;severity based onthe psoriasis areaand severity index(PASI) and selfadministeredPASI(SAPASI)Secondary:Not reportedResultsPrimary:Lesions treated with BMV tape had a greater reduction in thePASI score compared to the BMV cream with a mean percentagereduction of 59.3% and 38.4%, respectively (P
StudyandDrug RegimenJegasothy 45Clobetasol propionate0.05% ointment,applied twice a dayvs.diflorasone diacetate0.05% ointment,applied twice a dayClobetasol was appliedto one side anddiflorasone the otherWillis et al. 46Desoximetasone 0.05%gel, applied twice dailyvs.fluocinonide 0.05% gel,applied twice dailyZachariae 47Desoximetasone 0.25%,applied twice dailyvs.hydrocortisone butyrate0.1%, applied twicedailyStudy DesignandDemographicsRCT, DBPatients with mild tosevere psoriasisRCT, DB, MC, PGPatients with scalppsoriasisRCT, DBPatients with psoriasisSample Sizeand StudyDurationN=602 weeksN=1232 weeksN=272 weeksEnd PointsPrimary:Physician andpatient preferencesSecondary:Assessment of signand symptomseverityPrimary:Mean sign andsymptom scorebased on severityof erythema,scaling, thickening,and pruritusSecondary:Patient cosmeticacceptabilityPrimary:Erythema,induration, scaling,pruritus,pustulationSecondary:Patient preferenceResultsPrimary:At two weeks post treatment 75% of physicians and 68% ofpatients favored clobetasol treatment compared to 9% ofphysicians and 11% of patients who favored diflorasone,respectively (P
StudyandDrug RegimenDesoximetasone wasapplied to one side andhydrocortisone to theotherAnonymous 48Desoximetasone 0.25%ointment, applied twicea dayvs.fluocinonide 0.05%ointment, applied twicea dayKruger et al. 49Flurandrenolide tape, 4mg/cm 2 applied tolesions on one side ofthe body once daily forup to 16 hoursvs.diflorasone diacetate0.05% ointment,applied contralaterallyStudy DesignandDemographicsRCT, MC, SB, PGPatients 3 years of ageand older with stable orexacerbating psoriasisRCT, SBPatients 18 years of ageand older with stable,bilaterally symmetricplaque psoriasis with upto 10% of body surfacearea involvedSample Sizeand StudyDurationN=12114 daysN=304 weeksEnd PointsPrimary:Assessment of signand symptomseverity scores(based on pruritus,erythema, scaling,and thickening),clinicalimprovementSecondary:Patients’evaluation ofcosmetic attributesPrimary:Lesions wereevaluated forerythema, scaling,and induration, allmeasured on a 0-3scale (0=none,3=severe); the sumof these scores(ESI), wasevaluated by theinvestigator atbaseline, week 2,Results13 patients preferred desoximetasone, and 3 patients preferredhydrocortisone (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointstwice daily and week 4Secondary:Not reportedResultsthe diflorasone ointment group decreased by 53% (P
vs.StudyandDrug Regimenclobetasol propionatecream, applied twicedailyLowe et al. 52Clobetasol propionatelotion, applied twicedailyvs.clobetasol propionateemollient cream,applied twice dailyvs.clobetasol lotionvehicle, applied twicedailyMedansky et al. 53Mometasone furoate0.1% ointment orcream, applied oncedailyvs.fluocinolone acetonide0.025% ointment orcream, applied 3 timesdailyStudy DesignandDemographicsRCT, MC, SB, PC, PGPatients with moderateto severe plaque-typepsoriasisRCT, SB, PG, MCPatients with chronicmoderate to severepsoriasis vulgaris thathad been stable orworsening for more thana week were enrolled in1 of the 4 studiesSample Sizeand StudyDurationN=1924 weeksN=76421daysEnd PointsPrimary:Erythema, plaqueelevation, scaling,DermatologicalSum Score (DSS),pruritus, globalimprovementglobal severitySecondary:Not reportedPrimary:Evaluation ofindividual diseasesigns in the targetareas and changein disease signscore; change inoverall diseasestatusSecondary:Not reportedResultspenetration time (P=0.043), drying quickly (P=0.002), feelinggreasy (P
andStudyandDrug Regimenmometasone furoate0.1% ointment orcream, applied oncedailyvs.Study DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsThe mometasone cream group had a slight increase in percentageimprovement compared to the triamcinolone cream group, but theresults were not statistically significant (54% vs. 51%; P value notreported).A moderate improvement was found in the mometasone groupcompared to a slight improvement in the fluocinolone andtriamcinolone group (P
StudyandDrug RegimenStudy DesignandDemographics20% of their bodysurfaceSample Sizeand StudyDurationEnd PointsSecondary:Not reportedResultswith a mean score value of 1.9 on day 8, 1.5 on day 15, and 1.1 onday 22 (P value not reported).Total sign and symptom score improved by 85% at endpoint (Pvalue not reported).Cosmetic acceptability was rated as excellent by 71% of thepatients’ parents or guardians (P value not reported).Sears et al. 56Hydrocortisonebuteprate 0.1% cream,applied once dailyvs.placebo cream, appliedonce dailyRCT, DB, MC, PCPatients with atopicdermatitisN=16814 daysPrimary:Severity ofdermatitis signsbased on the meanlesion score for:infiltration,scaling, erythema,lichenification,vesicles, papules,excoriation,pruritusSecondary:overallimprovement;overall treatmentefficacy; cosmeticacceptabilitySecondary:Not reportedPrimary:At day 3 evaluations, there was a decrease of 3.10 in the meanlesion score for the hydrocortisone group compared to a decreaseof 1.71 for the placebo group (P=0.0027). The mean reductions inmean lesion score at day 7 evaluations for the hydrocortisonegroup compared to placebo were 4.65 and 2.93, respectively(P=0.0061). At endpoint (day 14), the mean decrease was 6.38 forthe hydrocortisone group and 3.39 for placebo (P=0.0001).Secondary:On day 3, the investigators gave a rating of cleared, excellent, orgood, in terms of overall improvement, to a total of 36/98 patientsin the hydrocortisone group, compared to 6/58 patients in theplacebo group (P=0.0004). The same ratings were given to 65/103hydrocortisone patients and 17/60 in the placebo group on day 7(P=0.0001); and, at endpoint, there were 72/93 in thehydrocortisone group compared to 19/54 in the placebo groupassessed as cleared, excellent, or good (P=0.0001).Investigator assessment of treatment efficacy at endpoint wasnoted as excellent or good for 69% (N=73) of the hydrocortisonepatients compared to 26% (N=16) in the placebo group. Patientassessment had 69% (N=73) in the hydrocortisone groupcompared to 32% (N=20) of placebo patients (P
StudyandDrug RegimenLassus 57Alclometasonedipropionate 0.05%cream, applied twicedailyvs.Study DesignandDemographicsRCT, DB, PGChildren with stable orworsening atopicdermatitisSample Sizeand StudyDurationN=432 weeksEnd PointsPrimary:Erythema,induration,pruritus, physicianglobal evaluationSecondary:Not reportedResultsacceptability was the response to “pleasant feeling on the skin”, inwhich hydrocortisone was favored (P=0.02).Primary:Average percent reduction in disease signs was greater for theclobetasol group (86%) compared to the alclometasone group(85%), respectively (P>0.10).Physicians deemed 9/22 patients in the alclometasone groupcleared compared to 10/21 patients in the clobetasol group(P>0.10).clobetasol butyrate0.05% cream, appliedtwice dailyKuokkanen et al. 58Alclometasonedipropionate 0.05%ointment, applied twicedailyvs.hydrocortisone 1%ointment, applied twicedailyBickers. 59Amcinonide 0.1%cream, applied twicedailyvs.halcinonide 0.1%cream, applied twicedailyRCT, DBChildren with eczemaAlclometasone wasapplied to one side, andhydrocortisone to theotherRCT, DB, PGPatients aged 17-84years with acute orsubacute eczematousdermatitisN=343 weeksN=332 weeksPrimary:Potential forinduction ofcutaneous atrophy;severity oferythema,induration,pruritus; globalevaluationSecondary:Not reportedPrimary:Itching, burning,pain, erythema,edema,excoriation,vesiculation,crusting, scaling,lichenification,plaques,pigmentationchanges, secondarySecondary:Not reportedPrimary:At endpoint, the percent improvement in sign and symptomseverity seen in the alclometasone and hydrocortisone treatmentsides were 88% and 86%, respectively (P value not reported).Secondary:Not reportedPrimary:The amcinonide group had a greater improvement in edemacompared to the halcinonide group at endpoint (P=0.04). All otherprimary endpoints were not significantly different between thetwo treatment groups (0.25≤P≤0.82).Secondary:No significant difference in cosmetic acceptability was seenbetween the two treatment groups (P=0.92).262Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsskin infection,fissuringResultsGuenther et al. 60Amcinonide 0.1%cream, applied twicedailyvs.halcinonide 0.1%cream, applied twicedailyWolkerstorfer et al. 61Clobetasone butyrate(CB) 0.05% cream,applied twice a dayvs.fluticasone propionate(FP) 0.05% cream,DB, PGPatients aged 16 to 71years with eczematousdermatitis for at leastone year with slowexacerbation of diseaseRCT, DBChildren aged 3 to 8with moderately activeatopic dermatitisN=292 weeksN=214 weeksSecondary:CosmeticacceptabilityquestionnairePrimary:Erythema, scaling,lichenification,plaques, fissuring,oozing, crusting,excoriation,pigmentationchanges, itchingand burning and/orpainSecondary:Investigator’soverall evaluation,patient’s overallevaluation, andpatient’sacceptabilityevaluationPrimary:Modified Scoringof AtopicDermatitis system(SCORAD)Secondary:Not reportedPrimary:All signs and symptoms, and the total score, yielded statisticallysignificant improvements in both treatment groups at both weeks 1and 2, with the exception of pigmentation changes at week 1(P=0.10 to 0.001).Halcinonide-treated patients had significantly greaterimprovements in fissuring at week 1; however, there was noapparent difference at week 2.At week 2, the amcinonide group had much greater improvementin burning/pain, and this was repeated in the evaluation of thenumber of patients experiencing complete burning/pain relief (all11 amcinonide patients reported complete relief vs. 4 of 7halcinonide patients). There were no major differences amongother signs and symptoms between the groups at week 2.Secondary:No significant difference was reported between the two treatmentgroups.Primary:There were no statistically significant differences between the FPand the CB treatment groups in SCORAD improvements (P=0.8).Secondary:Not reported263Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimenapplied once dailyJorizzo et al. 62Desonide 0.05%ointment, applied twicedailyvs.hydrocortisone 1%ointment, applied twicedailyStudy DesignandDemographicsRCT, MC, SB, PGChildren no older than12 years of age withmild to moderate atopicdermatitisSample Sizeand StudyDurationN=1115 weeks (witha 6 monthextension for36 of thepatients)End PointsPrimary:Globalimprovement,erythema,lichenification,excoriations,oozing or crusting,pruritus, indurationSecondary:Not reported.ResultsPrimary:The investigator’s global assessment favored desonide overhydrocortisone. In the desonide group, 69% of patients showedclearing or marked improvement, compared to 41% of patients inthe hydrocortisonegroup (P=0.003).There was a greater improvement in erythema, excoriations,oozing/crusting, and pruritus in the desonide group compared tothe hydrocortisone group with improvements of 52.7% and 33.9%for erythema, 76.4% and 57.1% for excoriations, 78.2% and60.7% for oozing/crusting, and 58.2% and 39.3% for pruritus,respectively (P
StudyandDrug RegimenDelescluse et al. 64Fluticasone propionate0.005% ointment,applied twice dailyvs.betamethasonedipropionate 0.05%oinement, applied twicedailyPei et al. 65Mometasone furoate0.1% ointment, appliedonce dailyvs.fluticasone 0.005%ointment, applied oncedailyOne treatment groupapplied medicationwithout wet wrapdressings (Group I[fluticasone] and II[mometasone]); theother had 2 weekswithout wet wrapdressings followed by 2weeks of medicationapplication under a wetwrap (Group III[fluticasone] and IVStudy DesignandDemographicsRCT, DB, PG, MCPatients with moderateto-severeeczemaRCT, SBPatients with refractoryatopic dermatitisSample Sizeand StudyDurationN=924 weeksN=274 weeksEnd PointsPrimary:Physicianassessment ofclinical response,sign and symptomseverity, patientassessment oftreatmentSecondary:Not reportedPrimary:Disease extent andseveritySecondary:Not reportedResultsPrimary:Improvement was seen in sign and symptom severity in bothtreatment groups at 2 and 4 weeks (P value not reported).There was no statistically significant difference in efficacyvariables between fluticasone and betamethasone (P value notreported).Secondary:Not reportedPrimary:The difference in efficacy between the mometasone andfluticasone treatments was not statistically significant in terms ofthe extent of disease score (P=0.846) and the severity score(P=0.068).There was improvement in disease severity score for both studymedications when all patients were not using any wet wrapdressing (P=0.043).Patients who used wet wrap dressings in weeks 2-4 of treatmenthad a greater improvement in disease severity compared to thosewho did not use wet wraps. Groups II, III, and IV had statisticallysignificant improvements in disease severity score during week 3with P values of 0.043, 0.008, and 0.011, respectively (P=0.116for Group I).During week 4, only the patients who received wet wrapscontinued to have statistically significant improvement in theirdisease severity score. The P value for groups III and IV were0.018, and 0.050, respectively (P=0.091 for Group I and P=0.078for group II).The extent of disease did not change significantly between groupIII and IV, with P values of 0.028 and 0.025, respectively (only265Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimen[mometasone])Study DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultspatients who were using wet wrap dressings completed the studywith less extensive disease).Lebwohl 66Mometasone furoate0.1% cream, appliedonce dailyvs.hydrocortisone valerate0.2% cream, appliedtwice dailyRCT, MCPediatric patients aged2-12 years with atopicdermatitis who hadfailed a topicalhydrocortisonepreparationN=2193 weeksPrimary:Total sign andsymptom score(based on severityof erythema,induration/lichenification,scaling/crusting,exudation,excoriation, andpruritus), physicianassessment ofglobal clinicalresponseSecondary:Not reportedPrimary:The mean percentage improvement in total sign/symptom scorewas greater for the mometasone group (87.2%) compared to thehydrocortisone group (78.6%) (P=0.011).Based on the physician’s assessment of global clinical response,mometasone was found to be more efficacious thanhydrocortisone (P=0.003).Secondary:Not reportedAshton et al. 67Desoxymethasone0.25% cream, appliedtwice dailyDB, PG, MCPatients aged 2 yearsand older with eczemaN=963 weeksSecondary:Not reportedPrimary:Erythema/redness,scaling, itching,extent of areaaffectedPrimary:Based on final clinician assessment scores, the difference inerythema was most significant between the desoxymethasone0.25% and hydrocortisone (P=0.006; mean P value for alltreatments was P
StudyandDrug Regimen0.1% cream, appliedtwice dailyStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsbetamethasone (mean=1.6) compared to hydrocortisone(mean=3.2; P=0.02).vs.hydrocortisone 1%,cream applied twicedailyThe differences in mean change from baseline betweendesoxymethasone 0.25% (4.3) and betamethasone (2.5) wassignificant (P=0.047). The difference between desoxymethasone0.25% when compared to hydrocortisone at week 3 was alsosignificant (P=0.001).The mean scores for scaling were 0.8 for desoxymethasone0.25%, 1.5 for desoxymethasone 0.05%, 0.8 for betamethasone,and 3.0 for hydrocortisone (P=0.01).The patient mean scores for extent of affected area were 1.5 fordesoxymethasone 0.25%, 2.6 for desoxymethasone 0.05%, 2.0 forbetamethasone, and 3.8 for hydrocortisone (P=0.08).The patient mean scores for itching were 1.2 for desoxymethasone0.25%, 2.5 for desoxymethasone 0.05%, 1.9 for betamethasone,and 4.1 for hydrocortisone (P=0.014).There was no significant difference in patient mean scores forredness between the treatment groups (P=0.13).Fowler et al. 68Hydrocortisone butyrate(HB) 0.1% cream,appliedvs.fluticasone propionate(FP) 0.05% creamRCT, DB, MC, PGPatients aged 18-65 withmoderate handdermatitis or atopicdermatitisHB was applied to oneside and either FP, PC,or MF was applied to theotherN=892 weeksPrimary:Investigator andsubject ratings ofsigns andsymptoms:erythema,cracking/fissuring,scaling, papules/vessiclesSecondary:Secondary:Not reportedPrimary:Based on the investigators’ observations, the rate of improvementof cracking/fissuring was greater in the HB (43%) groupcompared to the PC (21%) group (P
orStudyandDrug Regimenprednicarbate (PC)0.1% creamormometasone furoate(MF) 0.1% creamRoth et al. 69Study DesignandDemographicsRCT, DBSample Sizeand StudyDurationN=68End PointsResults of cosmeticacceptabilityquestionnairePrimary:not reported).ResultsIn terms of resolution from baseline, all treatment groups showedimprovement (P0.06).Secondary:Not reportedPrimary:Hydrocortisone valerate(HCV) 0.2% cream,applied 3 times a dayvs.hydrocortisone (HC)0.1% cream, applied 3times a dayorPatients aged 2-75 yearswith chronic atopicdermatitis4 weeks(HCvs. placebowas 2 weeks)HCV vs. HC:Pruritus, erythema,scaling,excoriation,lichenification,overall judgmentof responseHCV vs. BMV:Overallimprovement scoreHCV vs. HC:Overall response was in favor of the HCV group compared to theHC group, with 11 patients showing a better response compared to3 patients, respectively (P
StudyandDrug RegimenPrednicarbate 0.25%creamorprednicarbatecorresponding vehiclecreamvs.Study DesignandDemographicsPatients with atopiceczemaPrednicarbate or itsvehicle cream wereapplied to one forearmand betamethasone orclobetasol was appliedto the otherSample Sizeand StudyDuration6 weeksEnd PointsSecondary:Not reportedResultsthickness greater than either prednicarbate or its vehicle (P valuenot reported).The decrease in skin thickness was greater with betamethasonecompared to clobetasol, but this was statistically insignificant (Pvalue not reported).Also, the decrease in skin thickness was greater withprednicarbate compared to its vehicle, but this was statisticallyinsignificant (P value not reported).betamethasone-17-valerate 0.1% creamSecondary:Not reportedorclobetasol-17-propionate 0.05% creamMultiple DermatosesRocha et al. 71Amcinonide 0.1%cream, applied twice adayvs.betamethasone valerate0.1% cream, appliedtwice a dayDBPatients with atopicdermatitis, contactdermatitis, and eczemaN=603 weeksPrimary:Investigatorassessment ofclinical response,patient assessmentof clinical responseSecondary:CosmeticacceptabilityPrimary:Amcinonide and betamethasone treatment groups demonstratedimprovement in objective and subjective parameters over thecourse of 3 weeks.Investigator’s overall ratings of efficacy was comparable for the 2treatment groups (P=0.38).All 30 amcinonide patients rated its efficacy as excellentcompared to 27/30 betamethasone patients (the remaining 3 gave arating of good; P=0.24).Rosenberg 72Amcinonide 0.1%RCT, DB, PGPatients withN=352 weeksPrimary:Mean overallimprovementSecondary:No significant difference was found between treatment groups(0.42≤P≤1.00).Primary:Both treatment groups demonstrated a decrease in pruritus,lichenification, erythema, crust, scaling, papules, and excoriation269Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimencream, applied twice adayvs.betamethasone valerate0.1% cream, appliedtwice a dayStudy DesignandDemographicseczematous dermatitis,including contactdermatitis, atopicdermatitis, nummulareczema, seborrheicdermatitis, and eczemaSample Sizeand StudyDurationEnd Pointsrating of diseasestatus andsymptomsSecondary:Not reported(P value not reported).ResultsThe amcinonide treatment group had a greater improvementcompared to the betamethasone group in pruritus, lichenification,erythema, crust, scaling, and excoriation. The betamethasonetreatment group had a greater improvement compared to theamcinonide group in papules. None of these differences werefound to be statistically significant (P value not reported).Mean percent improvement was greater for the amcinonide groupcompared to the betamethasone group (P
StudyandDrug Regimenwater-miscible base,applied once dailyStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsinfiltration andremission ofchronicinflammationAcute dermatosesat the exacerbationstage (eczema,contact dermatitis,neurodermatitis):relief of acuteinflammation,pruritusSecondary:Not reportedvalue not reported).ResultsEczema:6/8 patients had a greater improvement when using halcinonidetreatment compared to treatment with betamethasone (P value notreported).Contact dermatitis:Halcinonide was shown to be more effective when compared tobetamethasone in the 10 patients with contact dermatitis (P valuenot reported).Atopic dermatitis:There was no significant difference found between the twotreatment groups (P value not reported).Neurodermatitis:There was no significant difference between the two treatmentgroups (P value not reported).Bluefarb 75Betamethasone valerate0.1% creamvs.desonide 0.05% creamRCT, DBPatients withdermatologicalconditions, includingatopic eczema, contactdermatitis, lichensimplex, nummulareczema, psoriasis,seborrheic dermatitisN=1174 weeksPrimary:Pruritus, erythema,induration, scaling;global responseSecondary:Not reportedSecondary:Not reportedPrimary:Dermatitides:Desonide cleared a greater percent of dermatitides (70.4%)compared to betamethasone, (56.5%) (P value not reported).Eczematous conditions:There was a greater rate of clearance for the betamethasone group(62.5%) compared to the desonide group (45.5%) (P value notreported).Psoriasis:A greater percentage of patients had their psoriasis rated as eitherclear or excellent in the desonide group (48%) compared to thebetamethasone group (35%) (P value not reported).271Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsVollum et al. 76Betamethasone valerate0.1% ointmentvs.RCT, DBPatients with lesions ofbilateral eczema orpsoriasisN=38 Primary:Improvement inlesions on one sideof the patient’sface compared tothe otherSecondary:Not reportedPrimary:There were 10 clinicians who chose betamethasone valerate, 0 thatpreferred halcinonide, and 5 that found no difference (P
StudyandDrug Regimencream, applied threetimes dailyStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsNot reportedResultsEight-six percent of patients in the clobetasol group had eitherexcellent or good improvement in their psoriasis compared to 61%in the fluocinonide group, respectively (P
StudyandDrug RegimenDesonide 0.05% cream,applied twice dailyvs.fluocinonide 0.05%cream, applied twicedailyKelly et al. 81Mometasone furoate(MF) 0.1% cream,applied once dailyvs.betamethasonedipropionate (BD)0.05% cream, appliedtwice dailyStudy DesignandDemographicsPatients withdermatologic disorders,including eczema,seborrheic dermatitis,contact dermatitis, andlichen simplexRCT, SB, MC, PGPatients 15 years of ageand older with a varietyof dermatoses, includingpsoriasis, atopicdermatitis, and eczemaSample Size End Pointsand StudyDuration2 weeks pruritus, palpableindurationN=6712 weeksSecondary:Physician’s scoringof improvementPrimary:Erythema,induration, scaling,crusting, pruritus,excoriation, painSecondary:Mean plasmacortisol levelsResultsscaling compared to the fluocinonide group in week 1 (P0.25 or more).Secondary:There was no significant difference in the overall physicianevaluation between treatment groups at week 1 or endpoint(P>0.20 and P>0.60, respectively).Primary:There were 15/33 patients in the MF group who left the studyprior to day 85 due to the fact that their lesions were cleared. Thiscorresponds to 18/32 patients in the BD patients.The difference in mean sign and symptom scores at end point wasnot statistically significant between the 2 treatment groups (MFmean=3.0; BD mean=2.5; P=0.68).The mean percent improvement was not statistically significant;there was a 74.4% improvement for the MF group and an 80.1%improvement in the BD side (P=0.51).Secondary:The only instance in which the mean plasma cortisol levelsbetween the 2 groups reached statistical significance was at day 8.The change in mean plasma cortisol level for the MF group at day8 was 6.1, and for the BD group the change was -86.0 (P=0.02).Study abbreviations: DB=double-blind, MC=multicenter, PC=placebo-controlled, PG=parallel-group, PRO=prospective, RCT=randomized controlled trial, SB=single-blind,Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.274
Additional EvidenceDose Simplification:A search of Medline and Ovid did not reveal data pertinent to this topic.Stable Therapy:A search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician Visits:A search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 9. Relative Cost of the Single Entity Skin and Mucous Membrane Anti-inflammatory AgentsGeneric Name(s) Formulation(s) Example Brand Name(s) Brand GenericCost Costalclometasone cream, ointment Aclovate ® * $ $amcinonidecream, lotion, Cyclocort ® * $-$$ $$ointmentbetamethasone dipropionate aerosol, cream, Alphatrex ® *, Diprosone ® * $ $gel, lotion,ointmentbetamethasone dipropionate cream, lotion, Diprolene ® *, Diprolene $$$ $$and propylene glycol ointment AF ® *betamethasone valerate cream, foam, Beta-Val ® *, Luxiq ® $-$$$$ $lotion, ointmentclobetasolcream, foam, Clobex ® , Cormax ® *, $-$$$$$ $$gel, lotion, Embeline ® *, Embeline E ® *,ointment, Olux ® , Temovate ® *,shampoo, Temovate E ® *, Temovatesolution, spray Emollient ® *clocortolone cream Cloderm ® $$$ N/Adesonide cream, lotion, Desowen ® *, Tridesilon ® * $$-$$$ $275Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Generic Name(s) Formulation(s) Example Brand Name(s) BrandCostGenericCostointmentdesoximetasonecream, gel, Topicort ® *, Topicort LP ® * $$-$$$ $ointmentdiflorasone cream, ointment Apexicon ® *, Apexicon E ® *, $$$ $$$Psorcon E ® *fluocinolonecream, oil,ointment,shampoo,solutionCapex Shampoo ® , Derma-Smoothe/FS ® , Synalar ® *$-$$$$ $fluocinonidecream, gel,ointment,solutionLidex ® *, Lidex-E ® *, $$$-$$$$ $Vanos ®flurandrenolidecream, lotion, Cordran ® , Cordran SP ® $-$$$ N/Aointment, tapefluticasonecream, lotion, Cutivate ® * $$$ $$ointmenthalcinonidecream, ointment, Halog ® $-$$ N/Asolutionhalobetasol cream, ointment Ultravate ® * $$$ $$$hydrocortisone‡cream, enema,gel, lotion,ointment,solution, spray$-$$$ $hydrocortisone acetate‡cream, foam,lotion, ointment,packet, rectalsuppositorycream, ointment,solutionAnusol-HC ® *, AquanilHC ® *, Beta HC ® *,Cetacort ® *, Colocort ® *,Cortaid ® *, Cortizone-10 ® *,Dermolate Anti-Itch ® *, Dr.Smith's Anti-Itch ®,Hytone ® *,Hydrocortisone ® *,Instacort-10 ® *, Nutracort ® *,Preparation H ® *,Proctocort ® *, Proctocream-HC ® *, Recort Plus ® *,Sarnol-HC ® *, Summer'sEve ® *, Texacort ® *Cortaid ® , Cortifoam ® ,Medi-Cortisone ® *$-$$$$$ $$$-$$$ $$hydrocortisone butyrateLocoid ® *, LocoidLipocream ®hydrocortisone probutate cream Pandel ® $$$ N/Ahydrocortisone valerate cream, ointment Westcort ® * $$ $mometasonecream, ointment, Elocon ® * $$ $$solutionprednicarbate cream, ointment Dermatop ® * $$$ $$triamcinoloneaerosol, cream, Aristocort ® *, Aristocort $$ $lotion, ointment,pasteHP ® *, Kenalog ® *triamcinolone acetonide and cream Aristocort A ® $ N/Asodium laurel sulfate*Generic is available in at least one dosage form or strength.‡Over the counter product is available in at least one dosage form or strength.N/A = not available.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.276
X. ConclusionsSkin and mucous membrane anti-inflammatory agents are utilized for symptomatic relief and treatment ofboth acute and chronic inflammatory dermatoses. Systemic corticosteroids are typically more effective inmost dermatologic inflammatory conditions, but are generally reserved for more wide-spread and advancedconditions. 1 Topical treatment is preferred in most cases with limited or localized involvement, and to helpminimize systemic adverse effects.National and international guidelines state that topical corticosteroids are the standard of care to whichother treatments are compared for localized disease. While guidelines state that topical corticosteroids areeffective, cosmetically acceptable, and safe if used appropriately, they do not differentiate one agent overanother. These same guidelines state that the strength and vehicle of a topical corticosteroid selecteddepends on the nature, location, and extent of the skin lesions, the patient’s age, and duration of therapy. 3-13The efficacy and adverse effect profiles depend on a variety of factors including: steroid type, the vehicleused, application method, nature and extent of the skin disease, and specific patient factors such as age andsite of the disease. <strong>Clinical</strong> studies evaluating skin and mucous membrane anti-inflammatory agents, withsimilar factors in the treatment of psoriasis, atopic dermatitis, or individuals with multiple dermatosesconcluded with varying results. These results demonstrated that there is no one agent more efficacious thanthe others when factors are considered comparable. 35-42,46-49,54-63,72-81 Studies have also been conductedevaluating the different dosage forms of the skin and mucous membrane anti-inflammatory agents to eachother. These studies have not been able to demonstrate consistently that a specific dosage form (i.e., lotionor cream) is more efficacious than another. 43-44,51-52,63,67,73The topical anti-inflammatory agents offer varying potency groups for the treatment of many dermatologicconditions. Generic alternatives are available in each potency group. In addition, over-the-counterformulations are available for hydrocortisone in various formulations, such as creams and ointments. Thereare no significant clinical advantages of one brand skin and mucous membrane anti-inflammatory agentover another in this class, with regards to drug interactions, adverse events, and clinical effectiveness.Therefore, all brand products within the class reviewed are comparable to each other and to the genericsand over-the-counter products in this class and offer no significant clinical advantage over the otheralternatives in general use.XI.RecommendationsNo brand single entity skin and mucous membrane anti-inflammatory agent is recommended for preferredstatus. Alabama Medicaid should accept cost proposals from manufacturers to determine cost effectiveproducts and possibly designate one or more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.277
References1. McEvoy GK, ed. [2006]. AHFS Drug Information: Skin and Mucous Membrane Agents 84:00: AntiinflammatoryAgents 84:06, [monograph on the internet]. Bethesda, MD: American Society of Health-SystemPharmacists. Available at http://online.statref.com/document.aspx?fxid=1&docid=1190 [2006 Nov 25].2. Gums JG, Tovar JM. Adrenal Gland Disorders. In: Dipiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy:A Pathophysiologic Approach. 6 th ed. New York, NY: McGraw-Hill Companies, Inc.; 2005:1391-1406.3. Habif TM. <strong>Clinical</strong> Dermatology: A Color Guide to Diagnosis And Therapy [monograph on the internet].Edinburgh: Mosby, 2004 [cited 2006 Nov 30]. Available at http://home.mdconsult.com/das/book/64517804-2/view/1195.4. Drake LA, Dinehart SM, Farmer ER et al. Guidelines of care for the use of topical glucocorticosteroids. J AmAcad Dermatol. 1996, 35:615-19.5. West DP, West LE, Scuderi L, Micali G. Psoriasis. In: Dipiro JT, Talbert RL, Yee GC, et al, eds.Pharmacotherapy: A Pathophysiologic Approach. 6 th ed. New York, NY: McGraw-Hill Companies, Inc.;2005:1769-1783.6. Goldstein BG, Goldstein AO. General principles of dermatologic therapy and topical corticosteroid use. In:Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.7. Hanifin JM, Cooper KD, Ho VC et al. Guidelines of care for atopic dermatitis. J Am Acad Dermatol.2004;50:391-404. Available at: http://www.aad.org/professionals/guidelines.8. Leung DY, Nicklas RA, Li JT, et al. Disease management of atopic dermatitis: an updated practice parameter.Ann Allergy Asthma Immunol. 2004;93:S1-S21. Available at: http://www.jcaai.org/pp/ad_toc.asp.9. Primary Care Dermatology Society & British Association of Dermatologists. Guidelines for the management ofatopic eczema. Available from: www.eGuidelines.co.uk. Accessed October 10, 2006.10. Pardasani AG, Feldman SR, Clark AR. Treatment of psoriasis: an algorithm-based approach for primary carephysicians. Am Fam Physician 2000;61:725-733,736.11. British Association of Dermatologists. Psoriasis Guidelines 2006. Available at:http://www.bad.org.uk/healthcare/guidelines/psoriasis.asp. Accessed October 4, 2006.12. American Gastroenterological Association. Technical review on the diagnosis and treatment of hemorrhoids.Gastroenterology. 2004;126:1463-1473.13. American Society of Colon and Rectal Surgeons. Practice Parameters for the treatment of hemorrhoids.Available at: www.fascrs.org/displaycommon.cfm?an=1subarticlenbr=145. Accessed October 31, 2006.14. Castaldo P, Ellis C, Gregorcyk S et al. Practice parameters for the management of hemorrhoids. Dis ColonRectum. 2005;48(2):189-194.15. Aclometasone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.16. Amcinonide: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.17. Betamethasone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.18. Clobetasol: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.19. Clocortolone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.20. Desonide: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.21. Desoximetasone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.22. Diflorasone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.23. Fluocinolone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.24. Fluocinonide: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.25. Flurandrenolide: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.26. Fluticasone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.27. Halcinonide: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.28. Halobetasol: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.29. Hydrocortisone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.30. Mometasone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.31. Prednicarbate: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.32. Triamcinolone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.33. Micromedex ® Healthcare Series, (electronic version). Thomson Micromedex, Greenwood Village, CO, USA.Available at: http://www.thomsonhc.com. Accessed November 26, 2006.34. Tatro DS, ed. Drug Interaction Facts. St. Louis, MO: Wolters Kluwer Health, Inc.; 2006.35. Huntley AC, Isseroff R. Amcinonide vs. betamethasone dipropionate ointments in the treatment of psoriasis.Cutis. 1985 May;35(5):489-492.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.278
36. Cornell RC. Comparison of amcinonide ointment 0.1 percent twice daily and fluocinonide ointment 0.05percent three times daily in the treatment of psoriasis. Cutis. 1983 May;31(5):566-569.37. Engel MF. Treatment of psoriasis with amcinonide 0.1 percent and fluocinonide 0.05 percent ointments. Acomparative double-blind study. Cutis. 1982 Jun;29(6):646-650.38. Millikan LE, Mroczkowski TF. A comparative study of amcinonide and halcinonide 0.1% ointments in thetreatment of psoriasis. Int J Dermatol. 1986 Oct;25(8):542.39. Katz HI, Lindholm JS, Weiss JS, Shavin JS, Morman M, Bressinck R, Cornell R, Pariser DM, Pariser RJ, WengW, et al. Efficacy and safety of twice-daily augmented betamethasone dipropionate lotion versus clobetasolpropionate solution in patients with moderate-to-severe scalp psoriasis. Clin Ther. 1995 May-Jun;17(3):390-401.40. Jacobson C, Cornell RC, Savin RC. A comparison of clobetasol propionate 0.05 percent ointment and anoptimized betamethasone dipropionate 0.05 percent ointment in the treatment of psoriasis. Cutis. 1986Mar;37(3):213-214, 216, 218-220.41. Shupack JL, Jondreau L, Kenny C, Stiller MJ. Diflorasone diacetate ointment 0.05% versus betamethasonedipropionate ointment 0.05% in moderate-severe plaque-type psoriasis. Dermatology. 1993;186(2):129-132.42. Barsky S. Multicenter trial analysis. Fluocinonide and betamethasone gel in psoriasis. Arch Dermatol. 1976Dec;112(12):1729-1733.43. Pacifico A, Daidone R, Peris K. A new formulation of an occlusive dressing containing betamethasone valerate0.1% in the treatment of mild to moderate psoriasis. J Eur Acad Dermatol Venereol. 2006 Feb;20(2):153-157.44. Bergstrom KG, Arambula K, Kimball AB. Medication formulation affects quality of life: a randomized singleblindstudy of clobetasol propionate foam 0.05% compared with a combined program of clobetasol cream0.05% and solution 0.05% for the treatment of psoriasis. Cutis. 2003;72:407-411.45. Jegasothy BV. Clobetasol propionate ointment 0.05% versus diflorasone diacetate ointment 0.05% in moderateto severe psoriasis. Int J Dermatol. 1990 Dec;29(10):729-730.46. Willis I, Cornell RC, Penneys NS, Zaias N. Multicenter study comparing 0.05% gel formulations ofdesoximetasone and fluocinonide in patients with scalp psoriasis. Clin Ther. 1986;8(3):275-282.47. Zachariae H. Comparison of desoximetasone and hydrocortisone butyrate in psoriasis. Acta Derm Venereol.1976;56(4):309-310.48. Anonymous. Comparative study of desoximetasone ointment 0.25% versus fluocinonide ointment 0.05% inpatients with psoriasis. Clin Ther. 1985;8(1):118-125.49. Kuokkanen K, Sillantaka I. Alclometasone dipropionate 0.05% vs. hydrocortisone 1.0%: potential to inducecutaneous atrophy in children. Clin Ther. 1987;9:223-231.50. Swinehart JM, Barkoff JR, Dvorkin D, Fisher G, Peets E. Mometasone furoate lotion once daily versustriamcinolone acetonide lotion twice daily in psoriasis. Int J Dermatol. 1989 Dec;28(10):680-681.51. Decroix J, Pres H, Tsankov N, Poncet M, Arsonnaud S. Clobetasol propionate lotion in the treatment ofmoderate to severe plaque-type psoriasis. Cutis. 2004 Sep;74(3):201-206.52. Lowe N, Feldman SR, Sherer D, Weiss J, Shavin JS, Lin YL, Foley V, Soto P. Clobetasol propionate lotion, anefficient and safe alternative to clobetasol propionate emollient cream in subjects with moderate to severeplaque-type psoriasis. J Dermatolog Treat. 2005 Aug;16(3):158-164.53. Medansky RS, Bressinck R, Cole GW, Deeken JH, Ellis CN, Guin JD, Herndon JH, Lasser AE, Leibsohn E,Menter MA, et al. Mometasone furoate ointment and cream 0.1 percent in treatment of psoriasis: comparisonwith ointment and cream formulations of fluocinolone acetonide 0.025 percent and triamcinolone acetonide 0.1percent. Cutis. 1988 Nov;42(5):480-485.54. Friedlander SF, Herbert AA, Allen DB. Safety of fluticasone propionate cream 0.05% for the treatment ofsevere and extensive atopic dermatitis in children as young as 3 months. J Am Acad Dermatol. 2002;46:387-393.55. Moshang T. Prednicarbate emollient cream 0.1% in pediatric patients with atopic dermatitis. Cutis. 2001;68:63-69.56. Sears HW, Bailer JW, Yeadon A. Efficacy and safety of hydrocortisone buteprate 0.1% cream in patients withatopic dermatitis. Clin Ther. 1997;19:710-719.57. Lassus A. Alclometasone dipropionate cream 0.05% versus clobetasone butyrate cream 0.05%. A controlledclinical comparison in the treatment of atopic dermatitis in children. Int J Dermatol. 1984 Oct;23(8):565-566.58. Krueger GG, O’Reilly MA, Weidner M, et al. Comparative efficacy of once-daily flurandrenolide tape versustwice-daily diflorasone diacetate ointment in the treatment of psoriasis. J Am Acad Dermatol. 1998;38:186-190.59. Bickers DR. A comparative study of amcinonide and halcinonide in the treatment of eczematous dermatitis.Cutis. 1984 Aug;34(2):190-194.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.279
60. Guenther L, Solomon AR, Voorhees JJ. A controlled comparison of amcinonide cream 0.1 percent andhalcinonide cream 0.1 percent in the treatment of eczematous dermatitis. Cutis. 1981 Oct;28(4):461-462, 464,467.61. Wolkerstorfer A, Strobos MA, Glazenburg EJ, Mulder PG, Oranje AP. Fluticasone propionate 0.05% creamonce daily versus clobetasone butyrate 0.05% cream twice daily in children with atopic dermatitis. J Am AcadDermatol. 1998 Aug;39(2 Pt 1):226-231.62. Jorizzo J, Levy M, Lucky A, Shavin J, Goldberg G, Dunlap F, Hinds A, Strelka L, Baker M, Tuley M, et al.Multicenter trial for long-term safety and efficacy comparison of 0.05% desonide and 1% hydrocortisoneointments in the treatment of atopic dermatitis in pediatric patients. J Am Acad Dermatol. 1995 Jul;33(1):74-77.63. Lucky AW, Grote GD, Williams JL, et al. Effect of desonide ointment, 0.05%, on the hypothalamic-pituitaryadrenalaxis of children with atopic dermatitis. Cutis. 1997;59:151-153.64. Delescluse J, van der Endt JD. A comparison of the safety, tolerability, and efficacy of fluticasone propionateointment, 0.005%, and betamethasone-17,21-dipropionate ointment, 0.05%, in the treatment of eczema. Cutis.1996;57(2 Suppl):32-38.65. Pei AY, Chan HH, Ho KM. The effectiveness of wet wrap dressings using 0.1% mometasone furoate and0.005% fluticasone propionate ointments in the treatment of moderate to severe atopic dermatitis in children.Pediatr Dermatol. 2001 Jul-Aug;18(4):343-348.66. Lebwohl M. A comparison of once-daily application of mometasone furoate 0.1% cream compared with twicedailyhydrocortisone valerate 0.2% cream in pediatric atopic dermatitis patients who failed to respond tohydrocortisone: mometasone furoate study group. Int J Dermatol. 1999 Aug;38(8):604-606.67. Ashton RE, Catterall M, Morley N, Fairris G, Joseph DN. A double-blind comparison of 0.25% and 0.05%desoxymethasone, 0.1% betamethasone valerate and 1% hydrocortisone creams in the treatment of eczema. JInt Med Res. 1987 May-Jun;15(3):160-166.68. Fowler JF, Fransway AF, Jackson M, et al. Hydrocortisone butyrate 0.1% cream in the treatment of chronicdermatitis. Cutis. 2005;75:125-131.69. Roth HL, Brown EP. Hydrocortisone valerate. Double-blind comparison with two other topical steroids. Cutis.1978 May;21(5):695-698.70. Korting HC, Vieluf D, Kerscher M. 0.25% Prednicarbate cream and the corresponding vehicle induce less skinatrophy than 0.1% betamethasone-17-valerate cream and 0.05% clobetasol-17-propionate cream. Eur JPharmacol. 1992;42:159-161.71. Rocha GL, Quinete SS, Dantas FE, Faria T. A double-blind comparative study between amcinonide andbetamethasone valerate in the treatment of eczematoid conditions. Curr Ther Res Clin Exp. 1976May;19(5):538-549.72. Rosenberg EW. Management of eczematous dermatitis with amcinonide or betamethasone valerate. A doubleblindcomparative study. Cutis. 1979 Dec;24(6):642-645.73. Rhodes EL, Scott LV. Diprosone (betamethasone dipropionate) cream 0.05%. A review and interim report of acomparative multi-centre study versus betamethasone valerate 0.1%. Br J Clin Pract. 1983 Apr;37(4):130-132.74. Levy A. Comparison of 0.1% halcinonide with 0.05% betamethasone dipropionate in the treatment of acute andchronic dermatoses. Curr Med Res Opin. 1977-1978;5(4):328-332.75. Bluefarb SM. <strong>Clinical</strong> comparison of desonide cream with betamethasone valerate cream. A double-blindrandomized study. Int J Dermatol. 1972 Apr-Jun;11(2):73-76.76. Vollum DI, Sparkes CG. Influence of the base on the results of clinical trials with topical corticosteroids.Dermatologica. 1979;158(4):293-298.77. Wishart JM, Lee IS. Mometasone versus betamethasone creams: a trial in dermatoses. N Z Med J. 1993 May26;106(956):203-205.78. Jegasothy B, Jacobson C, Levine N, Millikan L, Olsen E, Pinnell S, Cole G, Weinstein G, Porter M. Clobetasolpropionate versus fluocinonide creams in psoriasis and eczema. Int J Dermatol. 1985 Sep;24(7):461-465.79. Bleeker J. Double-blind comparison between two new topical corticosteroids, halcinonide 0.1% and clobetasolpropionate cream 0.05%. Curr Med Res Opin. 1975;3(4):225-228.80. Barsky S. <strong>Clinical</strong> comparison of desonide cream with fluocinonide cream in steroid-responsive dermatologicdisorders. Cutis. 1976 Dec;18(6):826-830.81. Kelly JW, Cains GD, Rallings M, Gilmore SJ. Safety and efficacy of mometasone furoate cream in thetreatment of steroid responsive dermatoses. Australas J Dermatol. 1991;32(2):85-91.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.280
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane Anti-inflammatory AgentsCombination ProductsAHFS Class 840600February 7, 2007I. OverviewThe class of combination skin and mucous membrane anti-inflammatory agents consists of combinations ofa corticosteroid with one or more other agents. Topical corticosteroids are utilized for symptomatic reliefand treatment of both acute and chronic inflammatory dermatoses. Systemic corticosteroids are generallymore effective in most dermatologic inflammatory conditions, but are typically reserved for morewidespread and advanced conditions. 1 Topical treatment is preferred in most cases with limited or localizedinvolvement, and these topical medications help to minimize systemic adverse effects.Topical corticosteroids are generally most effective in the treatment of acute or chronic dermatoses such asseborrheic or atopic dermatitis, localized neurodermatitis, anogenital pruritus, psoriasis, and theinflammatory phase of xerosis. 1 They are also effective in the late phase of allergic contact dermatitis orirritant dermatitis, but systemic corticosteroids are most often utilized to relieve the acute manifestations ofthese conditions. 1 Topical corticosteroid agents have routinely been used in the treatment of hemorrhoidsdue to their ability to decrease local inflammation. Over-the-counter topical agents are recommendeddespite the lack of supportive data regarding their efficacy. 2Topical corticosteroids have been combined with other agents for various reasons. The added agent may beused to help minimize adverse events associated with the application of topical corticosteroids (e.g.,hydrocortisone and aloe vera) or may work in conjunction with the topical corticosteroid (e.g.,hydrocortisone acetate and pramoxine). Several formulations are available generically. Some of thecombination products are also available over-the-counter, and all are used for relief of the inflammatoryand pruritic manifestations of corticosteroid-responsive dermatoses.Table 1 lists the combination skin and mucous membrane anti-inflammatory agents included in this review.This review encompasses all (topical) dosage forms and strengths.Table 1. Combination Skin and Mucous Membrane Anti-inflammatory Agents Included in this<strong>Review</strong>Generic Name(s) Formulation(s) Example Brand Current PDL Agent(s)Name(s)hydrocortisone and aloe vera‡ cream,ointmentN/Ahydrocortisone and aloeverahydrocortisone acetate and aloe vera‡ cream, gel,ointmentCortaid W withAloe ® *, Nuzon ®hydrocortisone acetateand aloe verahydrocortisone, mineral oil and whitepetrolatum‡ointment N/A hydrocortisone, mineraloil and whitepetrolatumhydrocortisone acetate and pramoxine rectal foam, Analpram-HC ® , nonerectal lotion Proctofoam-HC ®hydrocortisone acetate and urea cream Carmol HC ® * hydrocortisone acetateand urea*Generic is available in at least one dosage form or strength.‡Over-the-counter product is available in at least one dosage form or strength.N/A = not available.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.281
II.Evidence-Based Medicine and Current Treatment GuidelinesCurrent treatment guidelines that incorporate the combination skin and mucous membrane antiinflammatoryagents are summarized in Table 2.Table 2. Treatment Guidelines Using the Combination Skin and Mucous Membrane AntiinflammatoryAgents<strong>Clinical</strong> GuidelineRecommendation(s)American Academy of Dermatology (AAD): Guidelines ofCare for the Use of Topical Glucocorticosteroids 3 • Combination products are notaddressed.American Academy of Dermatology (AAD), <strong>Clinical</strong>Guidelines Task Force:Guidelines of Care for Atopic Dermatitis 4 • Combination products are notaddressed.Joint Task Force on Practice Parameters in collaborationwith the American College of Allergy, Asthma andImmunology (ACAAI), the American Academy of Allergy,Asthma, and Immunology (AAAAI), and the Joint Councilof Allergy, Asthma and Immunology (JCAAI): DiseaseManagement of Atopic Dermatitis: An Updated PracticeParameter 5 • Combination products are notaddressed.American Academy of Family Physicians (AAFP):Treatment of Psoriasis: An Algorithm-Based Approachfor Primary Care Physicians 6 • Combination products are notaddressed.British Association of Dermatologists: Psoriasis Guideline2006 7 • Combination products are notaddressed.The American Gastroenterological Association:Technical <strong>Review</strong> on the Diagnosis and Treatment ofHemorrhoids 2 • Combination products are notaddressed.American Society of Colon and Rectal Surgeons:Practice Parameters for the Management ofHemorrhoids 8 • Combination products are notaddressed.American Society of Colon and Rectal Surgeons:Practice Parameters for the Management ofHemorrhoids, 2005 Update 9 • Combination products are notaddressed.III.IndicationsFood and Drug Administration (FDA)-approved indications for the combination skin and mucousmembrane anti-inflammatory agents are noted in Table 3.Table 3. FDA-Approved Indications for the Combination Skin and Mucous Membrane AntiinflammatoryAgents 10-14Drug(s)Hydrocortisone and aloe veraHydrocortisone acetate andaloe veraHydrocortisone, mineral oiland white petrolatumHydrocortisone acetate andpramoxineRelief of the Inflammatory andPruritic Manifestations ofCorticosteroid-ResponsiveDermatosesPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.aaa282Relief of the Inflammatory andPruritic Manifestations ofCorticosteroid-ResponsiveDermatoses of the Anal Regiona
Drug(s)Hydrocortisone acetate andureaRelief of the Inflammatory andPruritic Manifestations ofCorticosteroid-ResponsiveDermatosesaRelief of the Inflammatory andPruritic Manifestations ofCorticosteroid-ResponsiveDermatoses of the Anal RegionIV.PharmacokineticsThe pharmacokinetic parameters for the combination skin and mucous membrane anti-inflammatory agentsare summarized in Table 4.Table 4. Pharmacokinetic Parameters of the Combination Skin and Mucous Membrane AntiinflammatoryAgents 10-14Drug (s)SystemicAbsorptionDistribution Excretion(Renal)Hydrocortisone and aloe vera Rapid No data UrineHydrocortisone acetate and aloe vera Rapid No data UrineHydrocortisone, mineral oil and whiteRapid No data UrinepetrolatumHydrocortisone acetate and pramoxine Rapid No data UrineHydrocortisone acetate and urea No data No data No dataV. Drug InteractionsDue to limited systemic absorption when the combination skin and mucous membrane anti-inflammatoryagents are administered topically, no significant drug interactions are likely to occur, and none aredocumented with these agents. 10-15VI.Adverse Drug EventsAdverse events with the combination skin and mucous membrane anti-inflammatory agents are rare. Sinceonly a small percentage of drug is absorbed, most adverse events occur at the site of application. The mostcommon adverse events reported with the combination skin and mucous membrane anti-inflammatoryagents are noted in Table 5.Table 5. Adverse Drug Events (%) Reported with the Combination Skin and Mucous Membrane AntiinflammatoryAgents 10-14Adverse Event(s)Hydrocortisoneand AloeVeraHydrocortisoneAcetate andAloe VeraHydrocortisone,Mineral Oil andWhite PetrolatumHydrocortisoneAcetate andPramoxinePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.HydrocortisoneAcetate andUreaDermatologicAcneiform eruptions a a a a aAllergic contactdermatitisa a a a aBurning - - a a aDryness a a a a aFolliculitis a a a a aHypertrichosis - - a a aHypopigmentation a a a a aIrritation a a a a a283
Adverse Event(s)Hydrocortisoneand AloeVeraHydrocortisoneAcetate andAloe VeraHydrocortisone,Mineral Oil andWhite PetrolatumHydrocortisoneAcetate andPramoxineHydrocortisoneAcetate andUreaItching a a a a aMaceration of the skin a a a a aMiliaria a a a a aPerioral dermatitis a a a a aSecondary infection - - a a aSkin atrophy a a a a aStriae - - a a aaPercent not specified- Event not reportedVII.Dosing and AdministrationThe usual dosing regimens for the combination skin and mucous membrane anti-inflammatory agents aresummarized in Table 6.Table 6. Usual Dosing for the Combination Skin and Mucous Membrane Anti-inflammatoryAgents 10-14Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityHydrocortisone andaloe veraApply to the affected areaas a thin film 2-4 timesdaily depending on theseverity of the condition.Administration of topicalcorticosteroids to childrenshould be limited to the leastamount compatible with aneffective therapeutic regimen.Cream: 0.5%, 1%Ointment: 1%Hydrocortisoneacetate and aloe veraHydrocortisone,mineral oil andwhite petrolatumHydrocortisoneacetate andpramoxineApply to the affected areaas a thin film 2-4 timesdaily depending on theseverity of the condition.Apply to the affected areaas a thin film 2-4 timesdaily depending on theseverity of the condition.Apply to affected area 3-4times daily.For perianal use, transfera small quantity to atissue and rub in gently.Administration of topicalcorticosteroids to childrenshould be limited to the leastamount compatible with aneffective therapeutic regimen.Administration of topicalcorticosteroids to childrenshould be limited to the leastamount compatible with aneffective therapeutic regimen.Administration of topicalcorticosteroids to childrenshould be limited to the leastamount compatible with aneffective therapeutic regimen.Cream: 0.5%Gel: 2%Ointment: 0.5%Ointment: 1%Cream: 1%-1%Foam: 1%-1%Lotion: 2.5%-1%Hydrocortisoneacetate and ureaFor anal administration,use the applicatorsupplied.Apply to the affected areaas a thin film 2-4 timesdaily depending on theseverity of the condition.Administration of topicalcorticosteroids to childrenshould be limited to the leastamount compatible with aneffective therapeutic regimen.Cream: 1%-10%284Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
VIII. Effectiveness<strong>Clinical</strong> studies evaluating the safety and efficacy of the combination skin and mucous membrane anti-inflammatory agents are summarized in Table 7.Table 7. Comparative <strong>Clinical</strong> Trials Using the Combination Skin and Mucous Membrane Anti-inflammatory AgentsStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsGreer et al. 16Hydrocortisone 1%and pramoxine 1% in awater-misciblemucoadhesive foambase, applied fourtimes dailyvs.simple aqueous foamas placebo, appliedfour times dailyWilliamson 17Hydrocortisone 1%and urea 10% creamapplied twice daily tolesions on the left sideof the bodyvs.betamethasonevalerate 0.1% appliedtwice daily to lesionson the right side of thebodyRCT, DB, PCFemale patientsentering thepostnatal wardcomplaining ofepisiotomy painSB, RCTMales andfemales over theage of 12 yearswith bilateral,approximatelysymmetrical,lesions of dryexogenouseczema of thelimbs or trunkN=405 daysN=323 weeksPrimary:Edema, erythema, pain, impairmentof mobility, and analgesicrequirements graded by the treatingphysicians on a scale of 1 to 4 (thehigher the score, the greater theseverity of the symptoms)Secondary:Healing and overall subjectiveresponse to treatment at day 5Primary:Assessment of eczema severity basedon a scale of 0-7 (0.0-2.5, mild; 2.5-5.5 moderate; and 5.5-7.0 severe)and the severity of erythema,dryness/scaling, papules, itching, andexcoriation using a 0-4 scale (0,none; 1, mild; 2, moderate; 3, severe;and 4, very severe)Secondary:Patient self-assessment questionnaireindicating preference and degree ofacceptance of the two topicalpreparationsStudy abbreviations: DB=double-blind, PC=placebo-controlled, RCT=randomized controlled trial, SB=single-blindResultsPrimary:No significant difference was found between mean totaldaily scores on days 1 or 3, but a significant differenceexisted in favor of placebo on day 5.Secondary:Subjective response to treatment showed no differencebetween groups (P>0.1) although healing was better withplacebo (P
Additional EvidenceDose Simplification:A search of Medline and Ovid did not reveal data pertinent to this topic.Stable Therapy:A search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician Visits:A search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 8. Relative Cost of the Combination Skin and Mucous Membrane Anti-inflammatory AgentsGeneric Name(s) Formulation(s) Example BrandName(s)BrandCostGenericCosthydrocortisone and aloe cream, ointment N/A N/A $vera‡hydrocortisone acetate and cream, gel, Cortaid W with Aloe ® *, $$ $aloe vera‡ointment Nuzon ®hydrocortisone, mineral oil ointment N/A N/A $and white petrolatum‡hydrocortisone acetate and rectal foam, Analpram-HC ® ,$$$ N/Apramoxinerectal lotion Proctofoam-HC ®hydrocortisone acetate andureacream Carmol HC ® * $$$$ $$$*Generic is available in at least one dosage form or strength.‡Over-the-counter product is available in at least one dosage form or strength.N/A = not available.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.286
X. ConclusionsThe combination skin and mucous membrane anti-inflammatory agents are FDA approved for the relief ofthe inflammatory and pruritic manifestations of corticosteroid-responsive dermatoses. Several of theproducts are available generically, and some are available over-the-counter. These combination productsare similar in many ways, including their adverse events which stem primarily from the hydrocortisonecomponent of each product.Current national and international guidelines do not address the combination skin and mucous membraneanti-inflammatory agents, and there are limited clinical studies evaluating their use. Greer et aldemonstrated that combination skin and mucous membrane anti-inflammatory agents were comparable toplacebo, while Williamson demonstrated that these agents were similar to topical corticosteroidmonotherapy. 16-17 Specifically, for the treatment of hemorrhoids, current treatment guidelines do notrecommend the routine use of these topical products due to the lack of data evaluating efficacy and safety,though their use is widespread. 1-9 With a lack of published data supporting their use, any evidence-basedclinical role that can be assigned to these agents is strictly limited. 1-9There is insufficient data to support that one brand skin and mucous membrane anti-inflammatory agent issafer or more efficacious than another. Therefore, all brand products within the class reviewed arecomparable to each other and to the generics and over-the-counter products in this class and offer nosignificant clinical advantage over other alternatives in general use.XI.RecommendationsNo brand combination skin and mucous membrane anti-inflammatory agent is recommended for preferredstatus. Alabama Medicaid should accept cost proposals from manufacturers to determine cost effectiveproducts and possibly designate one or more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.287
References1. McEvoy GK, ed. [2006]. AHFS Drug Information: Skin and Mucous Membrane Agents 84:00: AntiinflammatoryAgents 84:06, [monograph on the internet]. Bethesda, MD: American Society of Health-SystemPharmacists. Available at http://online.statref.com/document.aspx?fxid=1&docid=1190 [2006 Nov 25].2. American Gastroenterological Association. Technical review on the diagnosis and treatment of hemorrhoids.Gastroenterology. 2004;126:1463-1473.3. Drake LA, Dinehart SM, Farmer ER, et al. Guidelines of care for the use of topical glucocorticosteroids. J AmAcad Dermatol. 1996,35:615-619.4. Hanifin JM, Cooper KD, Ho VC, et al. Guidelines of care for atopic dermatitis. J Am Acad Dermatol.2004;50:391-404.5. Leung DY, Nicklas RA, Li JT, et al. Disease management of atopic dermatitis: an updated practice parameter.Ann Allergy Asthma Immunol. 2004;93:S1-S21.6. Pardasani AG, Feldman SR, Clark AR. Treatment of psoriasis: an algorithm-based approach for primary carephysicians. Am Fam Physician 2000;61:725-733,736.7. British Association of Dermatologists. Psoriasis Guidelines 2006. Available fromhttp://www.bad.org.uk/healthcare/guidelines/psoriasis.asp. Accessed October 4, 2006.8. American Society of Colon and Rectal Surgeons. Practice parameters for the treatment of hemorrhoids.Available at: www.fascrs.org/displaycommon.cfm?an=1&subarticlenbr=145. Accessed October 31, 2006.9. Castaldo P, Ellis C, Gregorcyk S, et al. Practice parameters for the management of hemorrhoids. Dis ColonRectum. 2005;48(2):189-194.10. Proctosol-HC ® [package insert]. Jacksonville, FL: Ranbaxy Laboratories; March 2005.11. Proctofoam HC ® [package insert]. Milwaukee, WI: Schwarz Pharma; August 2004.12. Carmol HC ® [package insert]. Fairfield, NJ: Doak Dermatologics; No date.13. Marion, DW. Hydrocortisone: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.14. Micromedex ® Healthcare Series, (electronic version). Thomson Micromedex, Greenwood Village, CO, USA.Available at: http://www.thomsonhc.com. Accessed November 26, 2006.15. Tatro DS, ed. Drug Interaction Facts. St. Louis, MO: Wolters Kluwer Health, Inc.; 2006.16. Greer IA, Cameron AD. Topical pramoxine and hydrocortisone foam versus placebo in relief of post partumepisiotomy symptoms and wound healing. Scott Med J. 1984;29(2):104-106.17. Williamson DM. Comparison of a modified hydrocortisone/urea cream and betamethasone valerate cream inthe treatment of dry eczema. J Int Med Res. 1987;15(2):99-105.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.288
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane Antipruritics and LocalAnestheticsSingle Entity AgentsAHFS Class 840800February 7, 2007I. OverviewThe single entity skin and mucous membrane antipruritics and local anesthetics include medications for avariety of indications. They are often used to alleviate itching and pain caused by insect bites, minor burns,sunburns, atopic dermatitis, hemorrhoids, or eczema, and some may be used to provide an anesthetic effectduring minor surgical procedures and diagnostic tests. Topical antipruritics are recommended for shorttermuse, usually less than 8 days in duration and data regarding efficacy is somewhat limited. Thelidocaine 5% patch is approved for relief of pain due to post-herpetic neuralgia and is the only topicalanesthetic in the class to carry this indication. The variety of products, dosage forms, and indications makehead-to-head comparisons of agents in this class difficult.Some of the older products in this class are available over-the-counter and limited data is availableevaluating the efficacy of these products for their approved indications. Products that are available overthe-counterinclude dibucaine ointment, benzocaine gel, and lidocaine cream and solution.The single entity skin and mucous membrane antipruritics and local anesthetics that are included in thisreview are listed in Table 1. This review encompasses all (topical) dosage forms and strengths.Table 1. Single Entity Skin and Mucous Membrane Antipruritics and Local Anesthetics Included inthis <strong>Review</strong>Generic Name(s) Formulation(s) Example Brand Name(s) CurrentPDLAgent(s)benzocaine‡ gel Americaine ® nonedibucaine‡ ointment N/A dibucainedichlorotetrafluoroethane (CFC-114) aerosol Gebauer's 114 ® nonedoxepin cream Prudoxin ® , Zonalon ® Prudoxin ®ethyl chloride spray Ethyl chloride ® * ethylchloridelidocaine‡cream, lotion,ointment,solution,transdermalpatchEla-Max ® , Lidamantle ® *,Lidoderm ® , Pre-AttachedLTA Kit ®lidocainepramoxine rectal foam Proctofoam ® nonetetracaine solution Pontocaine ® none*Generic is available in at least one dosage form or strength.‡Over-the-counter product is available in at least one dosage form or strength.N/A=not availableII.Evidence-Based Medicine and Current Treatment GuidelinesCurrent treatment guidelines that incorporate the single entity skin and mucous membrane antipruritics andlocal anesthetics are summarized in Table 2.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.289
Table 2. Treatment Guidelines Using the Single Entity Skin and Mucous Membrane Antipruriticsand Local Anesthetics<strong>Clinical</strong> GuidelineRecommendation(s)American Academy of• Topical corticosteroids are the standard of care to whichDermatology (AAD), <strong>Clinical</strong>Guidelines Task Force:Guidelines of Care for AtopicDermatitis 1 ••other treatments are compared.Cutaneous adverse effects (striae, skin atrophy, andtelangiectasia) limit the use of topical corticosteroids.Data regarding the optimal strength, concentration,duration, and frequency of application is lacking.• Noncutaneous adverse effects associated with long-termuse of topical corticosteroids are not well documented.• Emollients are a standard of care and may be useful formaintenance therapy. They may also be steroid sparing.• Calcineurin inhibitors (tacrolimus and pimecrolimus)have demonstrated efficacy in reducing the severity andextent of symptoms in adults and children. The longtermsafety of these agents (therapy for longer than 1year) is unknown, including the potential forimmunosuppression and malignancy.• Coal tar has been used in the treatment of atopicdermatitis though cosmetic tolerability may be a barrierto compliance and effective therapy.• Oral antihistamines have limited usefulness because thereis limited evidence to support their efficacy in relievingitch or urticaria associated with atopic dermatitis.• Topical doxepin may be used short term to controlpruritis.Primary Care Dermatology • Patients should be educated to avoid exacerbating factors.Guidelines for the Management • Topical corticosteroids provide short-term relief of acuteof Atopic Eczema 2 flares and potency should be matched to disease severity.Association and the BritishAssociation of Dermatologists:• Patients should be educated about the proper use ofemollients.• Very potent corticosteroids may be used rarely inresistant severe disease.• Immunomodulators are an alternative to corticosteroidsand should only be used if the patient is intolerant to orhas failed conventional corticosteroid therapy.European Academy ofDermatology and Venereology:Position Paper on Diagnosis andTreatment of Atopic Dermatitis 3 • Management of atopic dermatitis requires efficient shorttermtherapy to control disease exacerbations which doesnot affect long-term therapy aimed at stabilization andflare prevention.• Hydration of skin should be maintained with emollients.• Allergen avoidance should be practiced.• Topical corticosteroids are a first-line anti-inflammatorytherapy. Application 2-3 times monthly with emollientsshould suffice in mild disease.• Tapering the dose of topical corticosteroids is importantto avoid withdrawal rebound.• Topical calcineurin inhibitors have demonstrated efficacyagainst placebo in clinical trials for short-term and longtermuse.• Topical antihistamines have no benefit aside from theircooling vehicles.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.290
<strong>Clinical</strong> GuidelineRecommendation(s)The American• Universal recommendations include adding fiber to theGastroenterological Association:Technical <strong>Review</strong> on theDiagnosis and Treatment ofHemorrhoids 4 ••diet and avoiding straining at defecation.Over-the-counter topical agents are recommended despitethe lack of supportive data regarding their efficacy.Topical analgesics are useful for symptomatic relief ofpain and itching.• Corticosteroid creams may decrease local inflammationbut long-term use of high potency corticosteroids shouldbe avoided.• There is no data to show that corticosteroids reducehemorrhoidal swelling, bleeding, or protrusion.• Topical nitroglycerin may relieve pain associated withhemorrhoids by decreasing anal tone.• Flavonoids may be of benefit since they may increasevenous tone, lymphatic drainage, capillary resistance, andmay normalize capillary permeability.• Nonoperative treatment such as banding andsclerotherapy, and operative procedures such ashemorrhoidectomy, may be useful in patients with moresevere hemorrhoids and in those not responding to othertreatments.American Society of Colon and • Medical treatment includes warm sitz baths, dietaryRectal Surgeons:Practice Parameters for theManagement of Hemorrhoids 5 ••correction, stool modifiers, and topical creams.Long-term use of topical steroids should be avoided.Rubber band ligation, hemorrhoidectomy, and otherprocedures are reserved for patients who fail moreconservative therapy.American Society of Colon andRectal Surgeons:Practice Parameters for theManagement of Hemorrhoids,2005 Update 6 ••Dietary management including adequate fiber and fluidintake is the primary management recommendation.Office treatment (including rubber band ligation,sclerotherapy, cryotherapy, etc.) and surgical interventionare reserved for patients with more severe hemorrhoids orthose not responding to more conservative therapy.American Academy ofNeurology:Treatment of PostherpeticNeuralgia: An Evidence-BasedReport of the Quality StandardsSubcommittee 7 ••Based on class I evidence, topical lidocaine patches areeffective in reducing the pain of postherpetic neuralgia.Tricyclic antidepressants, gabapentin, pregabalin,opioids, and topical lidocaine patches are effective andshould be used in the treatment of postherpetic neuralgia.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.291
III.IndicationsFood and Drug Administration (FDA)-approved indications for the single entity skin and mucous membrane antipruritics and local anesthetics are notedin Table 3.Table 3. FDA-Approved Indications for the Single Entity Skin and Mucous Membrane Antipruritics and Local Anesthetics 8-15Drug(s) Benzocaine Dibucaine Dichloro-Doxepin Ethyl Lidocaine Pramoxine Tetracainetetrafluoro-ethaneChlorideRelief of pain associated with minor burns,sunburn, insect bites, and pruritic dermatosis aRelief of pain and itching due tohemorrhoids and minor burns aShort-term (
IV.PharmacokineticsThe pharmacokinetic parameters for the single entity skin and mucous membrane antipruritics and localanesthetics are summarized in Table 4.Table 4. Pharmacokinetic Parameters of the Single Entity Skin and Mucous Membrane Antipruriticsand Local Anesthetics 8-16Drugs(s)OnsetDurationAbsorption(hours)(hours)Benzocaine Not reported Not reported PoorDibucaine 15 minutes 2-4 hours PoorDichlorotetrafluoroethane Not reported Not reported Not reportedDoxepin 1.32 hours Not reported Plasma levels rangefrom undetectable tothose achieved afteroral administrationEthyl chloride Not reported Not reported Not reportedLidocaine Not reported Not reported 1-5%(Lidoderm®)Pramoxine 2-5 minutes Several days Not reportedTetracaine 5-10 minutes 30 minutes Not reportedV. Drug InteractionsSignificant drug interactions with the single entity skin and mucous membrane antipruritis and localanesthetics are summarized in Table 5.Table 5. Significant Drug-Drug Interactions with the Single Entity Skin and Mucous MembraneAntipruritics and Local Anesthetics 16Drug(s) SignificanceLevelInteractionMechanismDoxepin 1 Monoamine oxidaseinhibitors (MAOIs)Altered catecholamine uptake andmetabolism may occur whendoxepin and MAOIs are takenconcurrently. This may result inhyperpyrexia, convulsions, anddeath.Doxepin 2 Cimetidine Concurrent administration ofdoxepin and cimetidine may causefluctuations, specifically elevations,in serum doxepin concentrations.Elevated serum doxepinconcentrations may result inanticholinergic side effects.Significance Level 1=major severitySignificance Level 2=moderate severityPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.293
VI.Adverse Drug EventsThe most common adverse drug events reported with the single entity skin and mucous membrane antipruritics and local anesthetics are noted in Table 6.Table 6. Adverse Drug Events (%) Reported with the Single Entity Skin and Mucous Membrane Antipruritics and Local Anesthetics 8-15Adverse Event(s) Benzocaine Dibucaine Dichlorotetrafluoro-Doxepin Ethyl Lidocaine Pramoxine TetracaineethaneChlorideCardiovascularArrhythmia - - - - - a - -Arterial spasms - - - - - a - -Asystole - - - - - a - -Bradycardia - - - - - a - -Cardiovascular- - - - - a - -collapseDefibrillator- - - - - a - -thresholdincreasesHeart block - - - - - a - -Hypotension - - - - - a - -Shock - - - - - a - -Sinus node- - - - - a - -suppressionVascular- - - - - a - -insufficiencyCentral Nervous System (CNS)Agitation - - - - - a - -Anxiety - - -
Adverse Event(s) Benzocaine Dibucaine DichlorotetrafluoroethaneDoxepinPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.295EthylChlorideLidocaine Pramoxine TetracainechangesEuphoria - - - - - a - -Hallucinations - - - - - a - -Headache - - - - - a - -Hyperesthesia - - - - - a - -Hypoesthesia - - - - - a - -Lethargy - - - - - a - -Lightheadedness - - - - - a - -Nervousness - - - - - a - -Paresthesia - - - - - a - -Psychosis - - - - - a - -Seizure - - - - - a - -Slurred speech - - - - - a - -Somnolence - - - - - a - -Unconsciousness - - - - - a - -DermatologicalBlisters - - - - - a - -Bruising - - - - - a - -Burning a 1-10 - 23 - a a -Contact dermatitis a 1-10 - - - a a -Depigmentation - - - - - a - -Edema of the skin - - - - - a - -Erythema a - - - - - - -Exfoliation - - - - - a - -Itching - - - - - a - -Papules - - - - - a - -Petechia - - - - - a - -Pruritis a - - - - a - -Rash a - - - - a - -Skin irritation - - - - - a - -Skin pigment - - - - 1-10 - - -alterationSkin reaction - - - - - a - -Stinging a - - 23 - - a -
DoxepinPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.296EthylChlorideLidocaine Pramoxine TetracaineAdverse Event(s) Benzocaine Dibucaine DichlorotetrafluoroethaneTenderness a - - - - - a -Thrombophlebitis - - - - - a - -Urticaria a - - - - a a -Vesicles - - - - - a - -Endocrine and MetabolicEdema a - - 1 - a a -GastrointestinalMetallic taste - - - - - a - -Nausea - - - - - a - -Taste alteration - - - 2 - - - -Vomiting - - - - - a - -Xerostomia - - - 10 - - - -GenitourinaryUrethritis - - - - - - - -Laboratory Test AbnormalitiesMethemo-a - - - - a a -globinemiaMusculoskeletalTremor - - - - - a - -Twitching - - - - - a - -Weakness - - - - - a - -RespiratoryAdult respiratory - - - - - a - -distress syndrome(ARDS)Bronchospasm - - - - - a - -Dyspnea - - - - - a - -Laryngospasm - - - - - a - -Respiratory arrest - - - - - a - -Respiratory- - - - - a - -depressionOtherAllergic reaction - - - - - a - -Anaphylactoid- - - - - a - -reaction
Adverse Event(s) Benzocaine Dibucaine DichlorotetrafluoroethaneDoxepinEthylChlorideLidocaine Pramoxine TetracaineAngioedema 1-10 - - - - a a -Blurred vision - - - - - a - -Convulsions - - - - - a - -Diplopia - - - - - a - -Flushing - - - - - a - -Hypersensitivity a - - - - - - -Mucousmembraneirritation- - - - 1-10 - - -Pain exacerbation - - - - - a - -Sensitivity to- - - - - a - -temperatureextremesTinnitus - - - - - a - -Tongue numbness - - -
VII.Dosing and AdministrationThe usual dosing regimens for the single entity skin and mucous membrane antipruritics and localanesthetics are summarized in Table 7.Table 7. Usual Dosing for the Single Entity Skin and Mucous Membrane Antipruritics and LocalAnesthetics 8-15Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityBenzocaine Apply to the affected area 3-4times per dayDibucaine Apply to the affected area asdirected. Use no more than 30 gfor adults in a 24-hour periodDichlorotetrafluoroethaneDose varies with useDoxepin Apply a thin film to affected area 4times per day with at least 3-4hours between applications. Donot use for more than 8 daysApply to the affected area 3-4times per day (children >2 yearsof age)Apply to the affected area asdirected, use no more than 7.5 gfor children in a 24-hour periodSafety and efficacy in childrenhave not been establishedSafety and efficacy in childrenhave not been establishedEthyl chloride Dose varies with use Safety and efficacy in childrenhave not been establishedLidocaine Cream:Cream:Apply to the affected area 2-3 Apply to the affected area 2-3times per day as neededtimes per day as needed(LidaMantle ® )(Lidamantle ® )Gel 20%Ointment 1%SprayCream 5%SprayCream 3%,4%, 5%Lotion 3%Apply ¼” thick layer to area, leaveon until adequate anesthetic affect,wash off before beginningprocedure (L-M-X 4 ® )*Apply to clean, dry area or insertrectally up to 6 times per day (L-M-X 5 ® )*Ointment, solution:Apply to affected area
VIII. Effectiveness<strong>Clinical</strong> studies evaluating the safety and efficacy of the single entity skin and mucous membrane antipruritics and local anesthetics are summarized in Table8.Table 8. Comparative <strong>Clinical</strong> Trials Using the Single Entity Skin and Mucous Membrane Antipruritics and Local AnestheticsStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsDrake and Millikan. 17Doxepin 5% cream BIDat the baseline visit andthen QID for a total of 7daysvs.placebo cream BID atthe baseline visit andthen QID for a total of 7daysRCT, DB, PCPatients 12-65 years ofage diagnosed withlichen simplexchronicus, nummulareczema, or contactdermatitis experiencingmoderate to severepruritis on a daily basisfor at least 1 weekN=3097 daysPrimary:Pruritis severityrating scale,Physician’s GlobalEvaluation forPruritis Relief(PGE-PR),patient’sassessment ofPruritis Relief on aVisual AnalogueScale (VAS-PR)Secondary:Not reportedPrimary:Significantly more patients in the doxepin group experiencedpruritis relief in the first 24 hours compared to placebo patients inall forms of eczema included in the study (P
StudyandDrug RegimenRamsook et al. 18Ethyl chloride sprayvs.isopropyl alcohol sprayDavies and Molloy 19Ethyl chloride sprayapplied to the site of thevenipuncture no morethan 45 seconds prior toprocedurevs.tetracaine cream(Ametop ® , not availablein the U.S.) applied tosite of the venipuncture,covered with andocclusive dressing, andleft in place for 30-45minutesKokinsky et al.. 20Lidocaine 10% aerosolvs.Study DesignandDemographicsRCT, PC, DBPatients 3-18 years ofage who presented to theemergency department(ED) requiringintravenous (IV)cannulation for fluids ormedicationadministration, orvenipuncture fordiagnostic testsXOPatients with a mean ageof 8.6 years beingadmitted formeasurement ofglomerular filtration rate(GFR) which involved aseries of 3 venipuncturesin a 4 hour period (thefirst 2 venipuncturesconstituted the crossoverand children couldchoose their owntreatment for the thirdvenipuncture)RCT, PC, DBPediatric patients 9months to 11 years oldundergoing unilateralSample Sizeand StudyDurationN=2221 dayN=771 dayN=4412 hoursEnd PointsPrimary:Results of theFaces Pain Scale(used for patients3-10 years of age)and the NumericPain Score (usedfor patients 10-18years of age)Secondary:Not reportedPrimary:Children’s selfreportedpainmeasured by theWong-Baker facesscaleSecondary:Not reportedPrimary:Pain scoresassessed by nurseor patient(depending on age)ResultsPrimary:Pain scores reported by the patients did not differ between groups(P value not reported).There was no statistically significant difference in pain scoresbetween groups when stratified for age (12 years, P values not reported).Significantly more procedures in the ethyl chloride group wererated as difficult compared to the isopropyl alcohol group(P
StudyandDrug Regimenplacebo aerosolvs.control groupMinassian et al. 21Lidocaine ointment 5%applied up to every 4hoursvs.placebo ointmentapplied up to every 4hoursStudy DesignandDemographicsinguinal hernia repairRCT, DB, PCFemale patients 21-23years of age with anepisiotomy or a first,second, third, or fourthdegree perineallaceration during theirperipartum periodSample Sizeand StudyDurationN=2002 daysEnd Pointsupon arrival to therecovery room, 1,4, and 12 hourspostoperatively,and reaction scoresafter gentlepalpation of thewound by thenurseSecondary:Plasmaconcentrations oflidocainePrimary:Amount of painrelief obtained(measured byamount ofointment used andtotal number ofpain pills taken bythe patient)Secondary:Results of a painquestionnaireadministered onthe first and secondday postpartumResultsThere were no significant differences between the lidocaine groupand the placebo group or the lidocaine and the control groups 1, 4,or 12 hours postoperatively.At 1 hour postoperatively, reaction scores to palpation were lowerin the lidocaine group compared to the placebo and control groups(P
StudyandDrug RegimenCorkill et al. 22Lidocaine 2% gelapplied up to every 4hoursvs.placebo gel applied upto every 4 hoursLuhmann et al. 23Lidocaine 5% cream(ELA-Max ® ) coveredwith an occlusivedressing 30 minutesbefore intravenous (IV)insertionvs.buffered lidocainesubcutaneously (SQ) 5minutes before IVinsertionStudy DesignandDemographicsRCT, DB, PCFemale patients who hada normal delivery of ahealthy baby andsustained a first orsecond degree perinealtearRCT, SBPatients 4-17 years ofage requiring peripheralIV (PIV) insertionSample Sizeand StudyDurationN=1492 daysN=691 dayEnd PointsPrimary:Perineal pain at 24hours post-delivery[measured on the101-pointNumerical RatingScale (NRS-101)]Secondary:Perineal pain 48hours postdelivery,theconsumption ofadditionalanalgesia, maternalsatisfactionPrimary:Visual analoguescales (VAS)ranging from 1-10(higher scoresindicate greaterpain, anxiety,satisfaction, ortechnicaldifficulty)completed pre- andpost-IV insertionby patients,parents, andblinded observerResultsfrom the pain questionnaire between the lidocaine group and theplacebo group (P=0.36).Primary:There were no significant differences between the lidocaine andplacebo groups at 24 hours according to the NRS-101 (P=0.5).Secondary:At 48 hours, the lidocaine group reported significantly less paincompared to the placebo group according to the NRS-101(P=0.023).There was no significant difference observed in the amount ofadditional analgesia used between the 2 groups (P
StudyandDrug RegimenGaler et al. 24Lidocaine 5% patch for12 hours daily (up to 4patches could beapplied at once)vs.placebo patch for 12hours daily (up to 4patches could beapplied at once)Meir et al. 25Lidocaine 5% patchapplied for 12 hoursdaily (up to 4 patchescould be applied atonce)vs.placebo applied for 12hours daily (up to 4patches could beapplied at once)Study DesignandDemographicsRCT, PC, XOPatients 62-96 years ofage with post-herpeticneuralgia (PHN) alreadyenrolled in the openlabelprotocol and usinglidocaine patches on aregular basis for at least1 monthRCT, PRO, DB, PC, XOPatients 21 years of ageand older suffering fromchronic painfulperipheral focalneuropathic syndromesthat were superficial andlocalized to a limitedskin zoneSample Sizeand StudyDurationN=3328 daysN=5828 daysEnd PointsPrimary:Time to exit thestudy [(patientsexited the studywhen their verbalpain relief ratingdecreased by 2 ormore categories forany 2 consecutivedays whencompared to prestudyopen-labelpain report (6-itemscale from0=worse to5=complete relief)]Secondary:Not reportedPrimary:Ongoing painintensity (duringthe first 8 hours,every 2 hours afterpatch applicationon day 1, and 1hour after dailyremoval of thepatch) allodynia,quality ofneuropathicsymptoms, andquality of sleepSecondary:Not reportedResultsPrimary:The median time to exit was >14 days in the lidocaine groupcompared with 3.8 days in the placebo group (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsAdjusted AUC values show better allodynia relief compared withplacebo during the first 8 hours (P=0.023) and for the remainderof the treatment period (P=0.03).There was a significant reduction in neuropathic symptoms in thelidocaine group compared to baseline (P=0.032), but nosignificant differences were observed between the lidocaine andplacebo groups at any time.No significant differences were observed between the lidocaineand placebo groups in quality of sleep.Devers and Galer 26Lidocaine 5% patchapplied for 12 hoursdaily (up to 3 patchescould be applied atonce)all patients receivedactive treatmentGaler et al. 28Lidocaine 5% patchvs.placebo patchOLPatients 23-85 years ofage diagnosed withperipheral neuropathicpainRCT, DB, PC, PGAdult patients diagnosedwith post-herpeticneuralgia (PHN)involving the torso areafor at least 1 month andin whom allodynia wasobserved on physicalexaminationN=1612 weeksN=1503 weeksPrimary:Degree of painrelief using averbal scale of0=worse to5=complete reliefSecondary:Not reportedPrimary:Change frombaseline to week 3in NeuropathicPain Scale (NPS)and 4 subitems ofthis scale: NPScomposite score,NPS totaldescriptor score(sum of scores of 8descriptor subitemsSecondary:Not reportedPrimary:Thirteen patients (81%) reported either “moderate relief”, “a lot ofrelief”, or “complete relief” from the lidocaine patch. Of these 13patients, all noted a reduction in brush-evoked mechanicalallodynia.All patients who responded to medication continued to experiencerelief throughout the duration of the study.Secondary:Not reportedPrimary:The reduction in pain scores for all four composite endpoints wasconsistently larger in the lidocaine patch group compared to theplacebo group (P=0.043, P=0.042, P=0.022, and P=0.013respectively).Secondary:Not reported304Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsother than“intensity” and“unpleasant”), NPSnonallodynic score(sum of scores ofall 8 subitemsother than “skinsensitivity” or“surface pain”),and NPS 4 Score(sum of the scoresof the 4 descriptors“sharp,” “hot,”“dull,” and “deep”)ResultsKatz et al. 28Lidocaine 5% patchapplied for 12 hoursdaily (up to 3 patchescould be applied atonce)all patients receivedactive treatmentOLPatients 20-99 years ofage diagnosed with postherpeticneuralgia(PHN)N=33228 daysSecondary:Not reportedPrimary:Changes in painintensity, paininterference inquality of life(QOL), pain relief,and patient andphysician globalassessmentsSecondary:Not reportedPrimary:Mean scores for all measures of pain intensity were significantlylower than baseline scores at all evaluations (P=0.0001).At the end of the study 40% of patients experienced a >50%reduction in average daily pain intensity.Mean pain interference with QOL scores were significantly lowercompared to baseline at all evaluations (P=0.0001).The majority of patients responded to lidocaine treatment withinthe first week.There was a significant improvement from baseline in pain reliefat all evaluations (P=0.0001). Overall, 58% of patients reportedmoderate to complete pain relief at day 28.The results of the physician global assessments and patient globalassessments were similar. Approximately 60% of patients werejudged to have complete improvement or moderate (“a lot of”)305Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsimprovement at day 28, slight improvement was reported inapproximately 15% of patients, and no change was reported in20% of patients.Yosipovitch andMaibach 29Pramoxine 1% lotionvs.vehicle lotionRCT, DB, PC, XOHealthy patients 34-52years of ageN=152 proceduredays (at least 3days apart)Primary:Itch magnitude anddurationSecondary:Not reportedSecondary:Not reportedPrimary:Pramoxine significantly shortened the duration of itch frombaseline (P=0.03).Pramoxine significantly decreased the itch magnitude (P
StudyandDrug RegimenintranasallyStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsall patients were giveneach product over thecourse of 3 sessions(separated by at least 48hours) and sensationthreshold and painperception weremeasured with theSemmes-WeinsteinmonofilamentDrug regimen abbreviations: BID=twice daily, QID=four times dailyStudy abbreviations: DB=double-blind, MC=multicenter, OL=open-label, PC=placebo-controlled, PG=parallel-group, PRO=prospective, RCT=randomized controlled trial, SB=single blind, XO=crossoverPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.307
Additional EvidenceDose SimplificationA search of Medline and Ovid did not reveal data pertinent to this topic.Stable TherapyA search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician VisitsA search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 9. Relative Cost of the Single Entity Skin and Mucous Membrane Antipruritics and LocalAnestheticsGeneric Name(s) Formulation(s) Example Brand Name(s) BrandCostGenericCostbenzocaine‡ gel Americaine ® $ N/Adibucaine‡ ointment N/A N/A $dichlorotetrafluoroethaneaerosol Gebauer's 114 ® $ N/A(CFC-114)doxepin cream Prudoxin ® , Zonalon ® $$-$$$ N/Aethyl chloride spray Ethyl chloride ® * $ $lidocaine‡cream, lotion,ointment, solution,transdermal patchEla-Max ® , Lidamantle ® *,Lidoderm ® , Pre-Attached LTA Kit ® $$$-$$$$$pramoxine rectal foam Proctofoam ® $$ N/Atetracaine solution Pontocaine ® $ N/A*Generic is available in at least one dosage form or strength.‡Over-the-counter product is available in at least one dosage form or strength.N/A=not available$Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.308
X. ConclusionsThe variety of products, dosage forms, and indications present in the single entity skin and mucousmembrane antipruritics and local anesthetics class of medications makes direct, head-to-head comparisonsof these agents difficult. Therefore, the results of available studies and current guidelines are discussedbelow for each agent.Benzocaine is available over-the-counter for the relief of minor burns, sunburns, insect bites and pruriticdermatoses. No controlled trials exist which adequately assess the efficacy of the single agent benzocainegel in the treatment of any of the above indications. Dibucaine ointment, also available over-the-counter, isindicated for the relief of pain and itching associated with hemorrhoids and minor burns. Again, no clinicaltrials adequately evaluate the efficacy of this product for these indications. Current clinical guidelines forthe treatment of hemorrhoids recommend the use of over-the-counter topical agents despite the lack ofsupportive data regarding their efficacy. 4-5 The guidelines do not differentiate between the types of topicalproducts recommended or the active ingredients.Doxepin cream is indicated for short-term (
with post-herpetic neuralgia, but do not indicate that topical lidocaine patches are recommended over oraltherapies. There are no head-to-head trials evaluating lidocaine 5% patches against the oral medicationsthat are also indicated for the treatment of pain associated with post-herpetic neuralgia. Benefits of topicallidocaine patches compared to the oral medications used for the pain associated with post-herpeticneuralgia would include the relative absence of clinically significant drug-drug interactions. Topicallidocaine patches are generally well tolerated and adverse effects are related to the degree of systemicabsorption. The most common adverse effects include application site reactions such as burning,dermatitis, and erythema. Allergic reactions are rare and may include bronchospasm, angioedema, pruritis,urticaria, and shock. Causality has not been established for other adverse effects, such as confusion,dizziness, metallic taste, blurred vision, bradycardia, and hypotension, which have been reported in postmarketingsurveillance.Pramoxine (Proctofoam ® ) is indicated for the relief of pain and itching associated with anogenital pruritisand irritation. Currently, no adequate, controlled trials exist evaluating the efficacy of this agent in therelief of itching, pain, and irritation caused by hemorrhoids. Current clinical guidelines for the treatment ofhemorrhoids recommend the use of over-the-counter topical agents despite the lack of supportive dataregarding their efficacy. 4-5 The guidelines do not differentiate the types of creams recommended or theactive ingredients.Tetracaine solution is indicated for use in the nose and throat as an anesthetic for diagnostic procedures.Noorily et al. evaluated the efficacy of a tetracaine and oxymetazoline solution compared to lidocaine andoxymetazoline or cocaine in healthy patients. Sensation threshold and pain perception were measured withthe Semmes-Weinstein monofilament and results indicated that sensation threshold was significantlyincreased in the tetracaine and oxymetazoline group compared to the other treatment groups at 10 and 70minutes after administration. 29 No other adequate controlled trials were available evaluating the efficacy oftetracaine as an anesthetic for diagnostic procedures.There is insufficient data to support that one brand single entity skin and mucous membrane antipruritic orlocal anesthetic is safer or more efficacious than another. Therefore, all brand products within the classreviewed are comparable to each other and to the generics and over-the-counter products in this class andoffer no significant clinical advantage over other alternatives in general use.XI.RecommendationsNo brand single entity skin and mucous membrane antipruritic or local anesthetic is recommended forpreferred status. Alabama Medicaid should accept cost proposals from manufacturers to determine costeffective products and possibly designate one or more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.310
References1. Hanifin J, Cooper K, Ho V, et al. Guidelines of care for atopic dermatitis. J Am Acad Dermatol.2004;50(3):391-404.2. Primary Care and Dermatology Society and the British Society of Dermatologists. Guidelines for themanagement of atopic eczema. http://www.eGuidelines.co.uk. Accessed October 10, 2006.3. Darsow U, Lubbe J, Taieb A, et al. Position paper on diagnosis and treatment of atopic dermatitis. J Eur AcadDermatol Venereol. 2005;19:286-295.4. American Gastroenterological Association. Technical review on the diagnosis and treatment of hemorrhoids.Gastroenterology. 2004;126:1463-1473.5. American Society of Colon and Rectal Surgeons. Practice Parameters for the treatment of hemorrhoids.www.fascrs.org/displaycommon.cfm?an=1&subarticlenbr=145. Accessed on October 31, 2006.6. Castaldo P, Ellis C, Gregorcyk S, et al. Practice parameters for the management of hemorrhoids. Dis ColonRectum. 2005;48(2):189-194.7. Dubinsky R, Kabbani H, El-Chami Z, Boutwell C, Ali H, et al. Practice parameter: treatment of postherpeticneuralgia: an evidence-based report of the quality standards subcommittee of the American Academy ofNeurology. Neurology. 2004;63:959-965.8. Benzocaine: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.9. Dibucaine: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.10. Doxepin: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.11. Ethyl chloride: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.12. Ethyl chloride and dichlorotetrafluoroethane: drug information. In: Rose BD, ed. UpToDate. Waltham, MA:UpToDate; 2006.13. Lidocaine: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.14. Pramoxine: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.15. Tetracaine: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.16. Micromedex® Healthcare Series, (electronic version). Thompson Micromedex, Greenwood Village, CO, USA.Available at: http://www.thomsonhc.com. Accessed October 28, 2006.17. Drake L, Millikan L. The antipruritic effect of 5% doxepin cream in patients with eczematous dermatitis. ArchDermatol. 1995;131:1403-1408.18. Ramsook C, Kozinetz C, Moro-Sutherland D. Efficacy of ethyl chloride as a local anesthetic for venipunctureand intravenous cannula insertion in a pediatric emergency department. Pediatric Emergency Care.2001;17(5):341-343.19. Davies E, Molloy A. Comparison of ethyl chloride spray with topical anaesthetic in children experiencingvenipuncture. Pediatric Nursing. 2006;18(3):39-43.20. Kokinsky E, Cassuto J, Sinclair R, Rubensson A, Nilsson K, Larsson L. Topical wound anesthesia in children—a temporary postoperative pain relief. Acta Anaesthesiol Scand. 1999;43:225-229.21. Minassian V, Jazayeri A, Prien S, Timmons R, Stumbo K. Randomized trial of lidocaine ointment versusplacebo for the treatment of postpartum perineal pain. Obstetrics and Gynecology. 2002;100(6):1239-1243.22. Corkill A, Lavender T, Walkinshaw S, Alfirevic Z. Reducing postnatal pain from perineal tears by usinglignocaine gel: a double-blind randomized trial. Birth. 2001;28(1):22-27.23. Luhmann J, Hurt S, Shootman M, Kennedy R. A comparison of buffered lidocaine versus ELA-Max beforeperipheral intravenous catheter insertions in children. Pediatrics. 2004;113(3):217-220.24. Galer B, Rowbotham M, Perander J, Friedman E. Topical lidocaine patch relieves postherpetic neuralgia moreeffectively than a vehicle topical patch: results of an enriched enrollment study. Pain. 1999;80:533-538.25. Meier T, Wasner G, Faust M et al. Efficacy of lidocaine patch 5% in the treatment of focal peripheralneuropathic pain syndromes: a randomized, double-blind, placebo-controlled study. Pain. 2003;106:151-158.26. Devers A, Galer B. Topical lidocaine patch relieves a variety of neuropathic pain conditions: and open-labelstudy. Clin J Pain. 2000;16(3):205-208.27. Galer B, Jensen M, Ma T, Davies P, Rowbotham M. The lidocaine patch 5% effectively treats all neuropathicpain qualities: results of a randomized, double-blind, vehicle-controlled, 3-week efficacy study with use of theneuropathic pain scale. Clin J Pain. 2002;18(5):297-301.28. Katz N, Gammaitoni A, Davis M, et al. Lidocaine patch 5% reduces pain intensity and interference with qualityof life in patients with postherpetic neuralgia: an effectiveness trial. Pain Medicine. 2002;3(4):324-332.29. Yosipovitch G, Maibach H. Effect of topical pramoxine on experimentally induced pruritis in humans. J AmAcad Dermatol. 1997;37(2):278-280.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.311
30. Noorily A, Noorily S, Otto R. Cocaine, lidocaine, and tetracaine: which is best for topical nasal anesthesia?Anesth Analg. 1995;81-724-727.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.312
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane Antipruritics and LocalAnestheticsCombination ProductsAHFS Class 840800February 7, 2007I. OverviewThe combination products that fall within the American Hospital Formulary Service (AHFS) class 840800contain at least one ingredient intended for antipruritic or local anesthetic use. Topical antipruritic agentsare used to treat symptoms of itch caused by insect bites and stings, rashes, some allergic reactions,eczema, and other dermatologic conditions. There is some debate about the usefulness of these products incontrolling itch, and current treatment guidelines for various skin conditions addressing their use in thiscapacity differ somewhat in their recommendations.Local anesthetics are indicated for providing analgesia before minor dermatologic procedures includingvenous access, shave biopsies, and cannulation, among other procedures. The combination localanesthetics in this review are available in different dosage forms and routes of delivery including patches,creams, rectal products, and an iontophoresis system. They also differ in the amount of time they arerequired to be left on the skin prior to procedures, and this, in addition to dosage form, may be a factorwhen choosing a product for a particular patient. The efficacy of each product compared to placebo, andclinical trials comparing these products to each other or to other agents, are discussed in this review.Consensus guidelines for the use of topical local anesthetics are lacking, so decision-making regarding theuse of these agents should be based on patient-specific criteria in addition to the available data on generaland comparative efficacy. Currently the combination lidocaine and prilocaine is available generically. Thecombination lidocaine and hydrocortisone acetate is also available generically.The combination antipruritics and local anesthetics that are included in this review are listed in Table 1.This review encompasses all (topical) dosage forms and strengths.Table 1. Combination Skin and Mucous Membrane Antipruritics and Local Anesthetics Included inthis <strong>Review</strong>Generic Name(s) Formulation(s) Example Brand Name(s) Current PDLAgent(s)ethyl chloride anddichlorotetrafluoroethane(CFC-114)aerosol Fluro-Ethyl ® nonelidocaine and epinephrine transdermal patch Lidosite ® nonelidocaine and hydrocortisone cream, lotion, Anamantle HC ® *, Anamantleacetaterectal cream, rectal HC Forte ® *, Lidamantle HC ® *,lidocaine andhydrocortisoneacetatekitlidocaine and prilocaine cream, kit EMLA ® * lidocaine andprilocainelidocaine and tetracaine transdermal patch Synera ® nonelidocaine, aloe vera, andhydrocortisone acetatelidocaine, aloe vera, collagen,and vitamin E*Generic is available in at least one dosage form or strength.rectal gel, rectal kit Anamantle HC ® , Rectagel HC ® nonegel Regenecare ® nonePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.313
II.Evidence-Based Medicine and Current Treatment GuidelinesCurrent treatment guidelines that incorporate the combination skin and mucous membrane antipruritics andlocal anesthetics are summarized in Table 2.Table 2. Treatment Guidelines Using the Combination Skin and Mucous Membrane Antipruriticsand Local Anesthetics<strong>Clinical</strong> GuidelineRecommendation(s)The American Gastroenterological • Universal recommendations include adding fiber to the dietAssociation:Technical <strong>Review</strong> on theDiagnosis and Treatment ofHemorrhoids 1 ••and avoiding straining at defecation.Over-the-counter topical agents are recommended despitethe lack of supportive data regarding their efficacy.Topical analgesics are useful for symptomatic relief of painand itching.• Corticosteroid creams may decrease local inflammation butlong-term use of high potency corticosteroids should beavoided.• There is no data to show that corticosteroids reducehemorrhoidal swelling, bleeding, or protrusion.• Topical nitroglycerin may relieve pain associated withhemorrhoids by decreasing anal tone.• Flavonoids may be of benefit since they may increasevenous tone, lymphatic drainage, capillary resistance, andmay normalize capillary permeability.• Nonoperative treatment such as banding and sclerotherapyand operative procedures such as hemorrhoidectomy maybe useful in patients with more severe hemorrhoids and inthose not responding to other treatments.American Society of Colon and • Medical treatment includes warm sitz baths, dietaryRectal Surgeons:Practice Parameters for theManagement of Hemorrhoids 2 ••correction, stool modifiers, and topical creams.Long-term use of topical steroids should be avoided.Rubber band ligation, hemorrhoidectomy, and otherprocedures are reserved for patients who fail moreconservative therapy.American Society of Colon andRectal Surgeons:Practice Parameters for theManagement of Hemorrhoids,2005 Update 3 ••Dietary management including adequate fiber and fluidintake is the primary management recommendation.Office treatment (including rubber band ligation,sclerotherapy, cryotherapy.) and surgical intervention isreserved for patients with more severe hemorrhoids or thosenot responding to more conservative therapy.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.314
III.IndicationsThe Food and Drug Administration (FDA)-approved indications for the combination skin and mucous membrane antipruritics and local anesthetics are notedin Table 3.Table 3. FDA-Approved Indications for the Combination Skin and Mucous Membrane Antipruritics and Local Anesthetics 5-9Indication(s)Ethyl chlorideandDichlorotetrafluoroethaneLidocaine andEpinephrineLidocaine andHydrocortisoneAcetateLidocaineandPrilocaineLidocaineandTetracaineaIntended to control pain associated withminor surgical procedures, dermabrasion,injections, and minor sports injuriesLocal anesthesia for superficialdermatological proceduresAnti-inflammatory and anesthetic for skindisordersAnti-inflammatory and anesthetic for thetreatment of hemorrhoids, anal fissures,pruritis ani, and similar conditionsProviding local analgesia on intact skin aaaLidocaine, AloeVera, andHydrocortisoneAcetatea aLidocaine,Aloe Vera,Collagen, andVitamin EPretreatment on genital mucosalmembranes for superficial minor surgeryaPretreatment for infiltration anesthesia aProviding local analgesia on intact skinfor superficial venous access andsuperficial dermatological procedures likeexcision, electrodessication, and shavebiopsyManagement and pain control of pressureulcers, superficial wounds and scrapes,and first and second degree burnsReducing rash and itch caused byepidermal growth factor receptors andreducing problems with hand and footsyndromeaaa315Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
IV.PharmacokineticsThe pharmacokinetic parameters for the combination skin and mucous membrane antipruritics and localanesthetics are listed in Table 4.Table 4. Pharmacokinetic Parameters of the Combination Skin and Mucous MembraneAntipruritics and Local Anesthetics 5-9Drugs Absorption Onset DurationEthyl chloride andNot reported Not reported Not reporteddichlorotetrafluoroethaneLidocaine and epinephrine Minimal 5 minutes 2 hours(dose and procedureLidocaine andhydrocortisone acetatedependent)Variable Not reported Not reportedLidocaine and prilocaine Variable 1 hour(5-10 minutesgenital application)1-2 hours post-removal(15-20 minutes genitalapplication)Lidocaine and tetracaine Variable 30 minutes Dose and proceduredependentLidocaine, aloe vera, andhydrocortisone acetateLidocaine, aloe vera,collagen, and vitamin EVariable Not reported Not reportedNot reported 3-10 minutes Not reportedV. Drug InteractionsSignificant drug interactions reported with the combination skin and mucous membrane antipruritics andlocal anesthetics are summarized in Table 5.Table 5. Significant Drug-Drug Interactions with the Combination Skin and Mucous MembraneAntipruritics and Local Anesthetics 5-9Drug(s) SignificanceLevelInteractionMechanismLidocaine andprilocaine2 Agents that are associatedwith methemoglobinemia*The use of lidocaine andprilocaine has been rarelyassociated withmethemoglobinemia, and coadministrationof medicationsalso known to cause druginducedmethemoglobinemiashould be avoided in childrenunder 12 months of age.Significance Level 1=major severitySignificance Level 2=moderate severity*sulfonamides, acetaminophen, acetanilide, aniline dyes, benzocaine, chloroquine, dapsone, naphthalene, nitrates, nitrofurantoin,nitroglycerine, nitroprusside, pamaquine, para-aminosalicylic acid, phenacetin, phenobarbital, phenytoin, primaquine, quininePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.316
VI.Adverse Drug EventsAdverse drug events reported with the combination skin and mucous membrane antipruritics and local anesthetics are listed in Table 6.Table 6. Adverse Drug Events (%) Reported with the Combination Skin and Mucous Membrane Antipruritics and Local Anesthetics 5-9Adverse Event(s) Ethyl chlorideandDichlorotetrafluoroethaneLidocaineandEpinephrineLidocaine andHydrocortisoneAcetateLidocaine and Prilocaine LidocaineandTetracaineLidocaine,Aloe Vera, andHydrocortisoneAcetateCardiovascularBradycardia - - - a - - -Cardiovascular arrest - - - a - - -Cardiovascular collapse - - - a - - -Hypotension - - - a - - -Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.317Lidocaine,Aloe Vera,Collagen,andVitamin ECentral Nervous System (CNS)CNS excitation - - - a- - -(with systemic absorption)CNS depression - - - a- - -(with systemic absorption)Dizziness - - - -
Adverse Event(s)Ethyl chlorideandDichlorotetrafluoroethaneLidocaineandEpinephrineLidocaine andHydrocortisoneAcetateLidocaine and PrilocaineLidocaineandTetracaineLidocaine,Aloe Vera, andHydrocortisoneAcetateFrostbite a - - - - - -Hematoma -
VII.Dosing and AdministrationThe usual dosing schedules for the combination skin and mucous membrane antipruritics and localanesthetics are summarized in Table 7.Table 7. Usual Dosing for the Combination Skin and Mucous Membrane Antipruritics and LocalAnesthetics 5-9Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityEthyl chloride anddichlorotetrafluoroethaneLidocaine andepinephrineLidocaine andhydrocortisone acetateInvert the container over thetreatment area, press gently onthe side of the spray valve,allowing the liquid to emergeas a fine mist sprayPlace 1 transdermal patch overthe area requiring analgesia,attach patch to iontophoreticcontroller and leave on for 10minutes; perform procedurewithin 10-20 minutes of patchremoval and do not useanother patch for at least 30minutesTopical:Apply to affected area 2-3times per daySafety and efficacy in childrenhave not been establishedChildren 5 years and older:Place 1 transdermal patch overthe area requiring analgesia,attach patch to iontophoreticcontroller and leave on for 10minutes; perform procedurewithin 10-20 minutes of patchremoval and do not useanother patch for at least 30minutesSafety and efficacy in childrenhave not been establishedAerosolTransdermal patch:10%-0.1%Cream: 0.5%-3%Lotion: 0.5%-3%Lidocaine andprilocaineRectal:Use 1 applicatorful 2 timesdailyMinor dermal procedures*:Apply 2.5 g (1/2 of the 5 gtube) over 20-25 cm 2 of skinsurface for at least 1 hour andcover with an occlusivedressingMajor dermal procedures†:Apply 2 g per 10 cm 2 of skinand leave on for at least 2hours and cover with anocclusive dressingAs applied to adult malegenital skin:Apply a thick layer (1 g /10cm 2 ) to skin for 15 minutesand perform procedureimmediately followingremoval of the cream andcover with an occlusivedressingAs applied to adult female0 to 3 months of age or 5kg:Apply 2 g up to 20 cm 2 of skinfor 4 hours and cover with anocclusive dressing1-6 years of age and >10 kg:Apply 10 g up to 100 cm 2 ofskin for 4 hours and coverwith an occlusive dressing7-12 years of age and >20 kg:Apply 20 g up to 200 cm 2 ofskin for 4 hours and coverwith an occlusive dressingDo not use in neonates
Lidocaine andtetracaineDrug(s) Usual Adult Dose Usual Pediatric Dose Availabilitygenitalmucous membranes:Apply a thick layer (5-10 g) tomucous membranes for 5-10minutes and performprocedure immediatelyfollowing removal of thecream (occlusion is notnecessary)who are being treated withother agents associated withmethemoglobinemiaVenipuncture orintravenous cannulation:Apply to intact skin for 20-30minutesVenipuncture orintravenous cannulation:Apply to intact skin for 20-30minutesPatch: 70 mg – 70 mgLidocaine, aloe vera,and hydrocortisoneacetateLidocaine, aloe vera,collagen, and vitaminE*Venipuncture or intravenous cannulation†Split thickness skin graft harvestingSuperficial dermatologicalprocedures:Apply to intact skin for 30minutesTopical:Apply to affected area 2-3times per dayRectal:Use 1 applicatorful 2 timesdailyApply ⅛ inch to wound orrash 3 times daily and coverwith dressingSuperficial dermatologicalprocedures:Apply to intact skin for 30minutesSafety and efficacy in childrenhave not been establishedApply ⅛ inch to wound orrash 3 times daily and coverwith dressing (maximum doseshould not exceed 4.5 mg/kgof lidocaine [a 6-inch dosecontains 65 mg of lidocaine])Rectal gel: 0.55%-2.8%Rectal kit: 2.5%-3%Gel: 2%320Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
VIII. Effectiveness<strong>Clinical</strong> trials evaluating the safety and efficacy of the combination skin and mucous membrane antipruritics and local anesthetics are summarized in Table8.Table 8. Comparative <strong>Clinical</strong> Trials Using the Combination Skin and Mucous Membrane Antipruritics and Local AnestheticsStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsZempsky et al. 10Lidocaine and epinephrine patchdelivered via iontophoresisvs.placebo patch and iontophoresissystemRCT, PRO, MC, DB,PCAdult patients 18years of age andolder presenting fornon-urgentvenipuncture orvenous cannulationPediatric patients 5-17 years of agepresenting for nonurgentvenipunctureor venouscannulationN=279(adults)N=272(children)1 dayPrimary:Pain perceived aftervenipuncture orvenous cannulationas measured usingthe Visual AnalogueScale (VAS) foradults and children12-17 years of age orthe Facial AffectiveScale (FAS) foryounger childrenSecondary:Success rate ofvenipuncture orvenous cannulation,adverse effectsPrimary:The VAS scores for adults and children 12-17 years of age wassignificantly lower in the lidocaine and epinephrine groupcompared to the placebo group (P
StudyandDrug Regimenhand of the patient with aplacebo version of the otherproduct and vice versaZempsky and Parkinson 12Lidocaine and epinephrine patchdelivered via iontophoresisvs.placebo (saline)Study DesignandDemographicsPRO, MC, RCT, DB,PCChildren 4-16 yearsof age presenting forminor dermatologicproceduresSample Sizeand StudyDurationN=601 dayEnd PointsPrimary:Oucher Pain ScalescoresSecondary:Not reportedResultsPrimary:In the lidocaine and epinephrine group, 94% reported feelingno pain from the pinprick and required no supplementalanesthesia compared to 7% in the placebo group (P
StudyandDrug Regimenwith salinevs.placebo cream applied over awide area of skin on the hand 60minutes prior to cannulation andinduction of anesthesia withpropofol mixed with salineStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsSecondary:Not reportedResultsand prilocaine group compared to the placebo group (P valuenot reported).Significantly greater pain frequency was seen in the lidocaineand prilocaine group compared to the lidocaine and propofolmixed injection group (P=0.002).Secondary:Not reportedvs.placebo cream applied over awide area of skin on the hand 60minutes prior to cannulation andinduction of anesthesia withpropofol mixed with lidocaineKoh et al. 15Lidocaine and prilocaine cream(EMLA ® ) applied to the skin for60 minutesvs.lidocaine 4% cream (ELA-Max ® ) applied to the skin for 30minutesKuvaki et al. 16Lidocaine and prilocaine creamapplied to the outer half of theinferior orbital margin at least 45minutes prior to retrobulbarinjectionRCT, DBPatients 8-17 years ofage having anintravenous (IV)insertion prior tosurgeryRCT, DBPatients presentingfor day case cataractsurgery under localanesthesiaN=601 dayN=1031 dayPrimary:Pain scores accordingto the VisualAnalogue Scale(VAS), difficulty ofplacing the IVaccording to theinvestigatorSecondary:Not reportedPrimary:Subjective painintensity on a 10-point scale (0=nopain, 10=intolerablepain)Secondary:Primary:There was no significant difference in pain ratings accordingto the VAS between the 2 groups (P=0.87).There was no significant difference in the investigator ratingsof difficulty of the procedure between the 2 groups (P=0.73).There was significantly more blanching in the lidocaine andprilocaine group compared to the lidocaine group (P=0.04).Secondary:Not reportedPrimary:There were no significant differences in pain scores reportedbetween the 2 groups (P=0.67).Secondary:Not reported323Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
vs.StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsNot reportedResultslidocaine 5% ointment applied tothe outer half of the inferiororbital margin at least 45 minutesprior to retrobulbar injectionDutta et al. 17Lidocaine and prilocaine creamapplied to the skin 1 hour prior tocannulationvs.piroxicam gel applied to the skin1 hour prior to cannulation(piroxicam gel is notcommercially available)RCT, DB, DB, PROHealthy patients 20-60 years of ageN=1048 hoursPrimary:Pain scores accordingto the VisualAnalogue Scale(VAS) oncannulation, duringcannulaadvancement, and atregular intervals over48 hours aftercannula removal,local skin condition(blanching, erythema,induration, edema)Primary:Pain scores were significantly higher in the piroxicam groupcompared to the lidocaine and prilocaine group on cannulationand during cannula advancement (P
StudyandDrug Regimenplacebo patch applied 30 minutesprior to procedureStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointseffectiveness of thepatch, the need forrescue medication,investigator ratingsof patients’ painintensity, investigatorratings of adequacyof the anesthetic,independentobserver’s score ofhis perception of thepatients’ painintensity using aprocedure painassessment scaleSecondary:Not reportedResultsundergoing excision, electrodessication, keloid injection,cryotherapy, and skin tag removal (P
Sethna et al. 20StudyandDrug RegimenLidocaine and tetracaine patchapplied for 20 minutes prior tothe procedurevs.placebo patch applied for 20minutes prior to the procedureStudy DesignandDemographicsRCT, PRO, DB, PCPatients 3-17 yearsold requiringintravenous (IV)access or bloodsamplingSample Sizeand StudyDurationN=641 dayEnd Pointsassessment of thedegree of anesthesiaprovided on a 4-pointscale (0=no pain,3=severe pain),investigator’sassessment ofwhether the patchprovided adequateanesthesia, anindependentobserver’sassessment of thedegree of anesthesiaprovided by the patchusing the same 4-point scalePrimary:Pain intensityaccording to theOucher Pain Scale,investigator andindependent observerassessments of thedegree of analgesiaprovided on a 4-pointscaleSecondary:Not reportedSecondary:Not reportedStudy abbreviations: DB=double-blind, MC=multicenter, PC=placebo-controlled, PRO=prospective, RCT=randomized controlled trialResultsThere were no significant differences between groups in theinvestigator’s assessments of patient pain or impression ofwhether or not the local anesthetic provided adequateanesthesia (P=0.461 and P=0.838, respectively).Primary:Significantly lower pain scores were reported in patients in thelidocaine and tetracaine group compared to the placebo group(P
Additional EvidenceDose SimplificationA search of Medline and Ovid did not reveal any data pertinent to this topic.Stable TherapyA search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician VisitsA search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 9. Relative Cost of the Combination Skin and Mucous Membrane Antipruritics and LocalAnestheticsGeneric Name(s) Formulation(s) Example BrandName(s)BrandCostGenericCostethyl chloride and dichlorotetrafluoroethaneaerosol Fluro-Ethyl ® $ N/A(CFC-114)lidocaine and epinephrine transdermal patch Lidosite ® $$ N/Alidocaine andcream, lotion, rectal Anamantle HC ® *, $$$-$$$$ $hydrocortisone acetate cream, rectal kit Anamantle HC Forte ® *,Lidamantle HC ® *lidocaine and prilocaine cream, kit Emla ® * $$ $$lidocaine and tetracaine transdermal patch Synera ® $$ N/Alidocaine, aloe vera, and rectal gel, rectal kit Anamantle HC ® , Rectagel $ N/Ahydrocortisone acetateHC ®lidocaine, aloe vera, gel Regenecare ® $ N/Acollagen, and vitamin E*Generic is available in at least one dosage form or strength.N/A=not availablePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.327
X. ConclusionsThe combination skin and mucous membrane antipruritics and local anesthetic products represented in thisreview are indicated for a variety of uses, including providing anesthesia for minor dermatologicalprocedures and the treatment of various conditions such as rashes, hemorrhoids, and superficial woundsand scrapes.The lidocaine and epinephrine patch (LidoSite ® ) was approved in 2004 for use as an anesthetic for minordermatological procedures. It is part of a system including the LidoSite ® Controller which deliverslidocaine and epinephrine via iontophoresis. Placebo-controlled trials demonstrate efficacy of the system,while comparative trials with lidocaine and prilocaine cream (EMLA ® ) and lidocaine injection show nosignificant differences in pain scores. 10-13 Current data does not show a clinically significant advantage ofthe LidoSite ® system over other products with the same indications.Lidocaine and hydrocortisone acetate cream and lotion are available generically and are indicated for therelief of pain and inflammation in various skin disorders, hemorrhoids, anal fissures, pruritis ani, andsimilar disorders. There are no controlled trials which are adequate to evaluate the efficacy of thiscombination for these indications. Current clinical guidelines addressing the treatment of hemorrhoidsrecommend the use of topical products for symptomatic relief despite the lack of supportive data. 1-3Lidocaine and prilocaine cream (EMLA ® ) is available generically and is indicated for use as an anestheticon intact skin and genital mucosal membranes prior to superficial dermatological procedures. Comparativetrials with injectable lidocaine, lidocaine cream 4%, and lidocaine ointment 5% vs. lidocaine and prilocainecream demonstrate no significant differences in pain scores in patients undergoing various dermatologicalprocedures between treatment groups. 14-16The lidocaine and tetracaine patch (Synera ® ) is indicated for use as an anesthetic on intact skin prior tominor dermatological procedures and venous access. Placebo-controlled trials demonstrate significantlybetter pain relief when using lidocaine and tetracaine patches compared to placebo patches, though onestudy by Schecter et al. showed no significant differences in pain scores in elderly patients undergoingprocedures on the arm/shoulder, chest/abdomen, back, hip/leg, and penis, and those undergoing shavebiopsies. 18-21 There was also no significant difference in the percentage of patients reporting adequate painrelief and no significant difference in those reporting that they would be willing to use the patch again priorto similar procedures. Currently, there are no published clinical trials that evaluate the efficacy of thelidocaine and tetracaine patches head-to-head with EMLA ® , ELA-Max ® (L.M.X.®) , or iontophoresis.A combination product containing lidocaine, aloe vera, collagen, and vitamin E gel (Regenecare ® ) isindicated for the management and pain control of pressure ulcers, superficial wounds and scrapes, and firstand second degree burns, in addition to reducing rash and itch caused by epidermal growth factor receptorsand reducing problems with hand and foot syndrome. There are no published placebo-controlled orcomparative trials evaluating the efficacy of this product for the above indications.There is insufficient data to support that one brand combination skin and mucous membrane antipruritic orlocal anesthetic is safer or more efficacious than another. Therefore, all brand products within the classreviewed are comparable to each other and to the generics and over-the-counter products in this class andoffer no significant clinical advantage over other alternatives in general use.XI.RecommendationsNo brand combination skin and mucous membrane antipruritic or local anesthetic is recommended forpreferred status. Alabama Medicaid should accept cost proposals from manufacturers to determine costeffective products and possibly designate one or more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.328
References1. American Gastroenterological Association. Technical review on the diagnosis and treatment of hemorrhoids.Gastroenterology. 2004;126:1463-1473.2. American Society of Colon and Rectal Surgeons. Practice Parameters for the treatment of hemorrhoids.www.fascrs.org/displaycommon.cfm?an=1&subarticlenbr=145. Accessed on October 31, 2006.3. Castaldo P, Ellis C, Gregorcyk S et al. Practice parameters for the management of hemorrhoids. Dis ColonRectum. 2005;48(2):189-194.4. Stevens DL, Bisno AL, Chambers HF, Everett ED, Dellinger P, Goldstein EJ, Gorbach SL, Hirschmann JV,Kaplan EL, Montoya JG, Wade JC; Infectious Diseases Society of America. Practice guidelines for thediagnosis and management of skin and soft-tissue infections. Clin Infect Dis. 2005;41:1373-1406.5. Marion, DW. Lidocaine and epinephrine: drug information. In: Rose BD, ed. UpToDate. Waltham, MA:UpToDate; 2006.6. Marion, DW. Lidocaine and epinephrine: drug information. In: Rose BD, ed. UpToDate. Waltham, MA:UpToDate; 2006.7. EMLA ® [package insert]. Wilmington, DE: AstraZeneca LP;May 2005.8. Synera ® [package insert]. Chadds Ford, PA: Endo Pharmaceuticals, Inc.; January 2006.9. MPM Regenecare ® [product information]. Irving, TX: MPM Medical, Inc.; 2006.10. Zempsky W, Sullivan J, Paulson D, Hoath S. Evaluation of a low-dose lidocaine iontophoresis system fortopical anesthesia in adults and children: a randomized, controlled trial. Clin Therap. 2004;26(7):1110-1119.11. Moppett I, Szypula K, Yoeman P. Comparison of EMLA and lidocaine iontophoresis for cannulation analgesia.Eur J Anaesthesiol. 2004;21:210-213.12. Zempaky W, Parkinson T. Lidocaine iontophoresis for topical anesthesia before dermatologic procedures inchildren: a randomized controlled trial. Pediatric Dermatology. 2003;20(4):364-368.13. Sherwin J, Awad I, Sadler P, Liddle A, Rowbotham D. Analgesia during radial artery cannulation: comparisonof the effects of lidocaine applied by local injection or iontophoresis. Anaesthesia. 2003;58:471-479.14. McCluskey A, Currer B, Sayeed I. The efficacy of 5% lidocaine-prilocaine (EMLA) cream on pain duringintravenous injection of propofol. Anesth Analg. 2003;97:713-714.15. Koh J, Harrison D, Myers R et al. A randomized, double-blind comparison study of EMLA ® and ELA-Max ®for topical anesthesia in children undergoing intravenous insertion. Pediatric Anesthesia. 2004;14:977-982.16. Kuvaki B, Gokmen N, Gunenc F et al. EMLA ® does not permit pain-free retrobulbar injection. ActaAnaesthesiol Scand. 2003;47:739-741.17. Dutta A, Puri G, Wig J. Piroxicam gel, compared to EMLA cream is associated with less pain after venouscannulation in volunteers. Can J Anesth. 2003;50(8):775-778.18. Berman B, Flores J, Pariser D et al. Self-warming lidocaine/tetracaine patch effectively and safely induces localanesthesia during minor dermatologic procedures. Dermatol Surg. 2005;31:135-138.19. Schecter A, Pariser D, Pariser R et al. Randomized, double-blind, placebo-controlled study evaluating thelidocaine/tetracaine patch for induction of local anesthesia prior to minor dermatologic procedures in geriatricpatients. Dermatol Surg. 2005;31:287-291.20. Sethna N, Verghese S, Hannallah R et al. A randomized controlled trial to evaluate S-Caine Patch TM forreducing pain associated with vascular access in children. Anesthesiology. 2005;102:403-408.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.329
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane AstringentsAHFS Class 841200February 7, 2007I. OverviewAstringents are products that cause dehydration, tightening of the skin, shrinking of tissues and contractionof skin pores. Astringents include topical prescription drugs used for the treatment of hyperhidrosis, whichis excessive sweating in amounts greater than physiologically needed for thermoregulation. 1 Hyperhidrosisis usually a chronic idiopathic condition.Idiopathic (primary) hyperhidrosis, also called focal hyperhidrosis, usually affect the axillae, palms, and/orsoles. The prevalence of primary hyperhidrosis in the United States (US) is estimated to be 2.8%. One-sixthof these individuals or 0.5% of the US population is estimated to suffer from sweating that is intolerable orinterferes with daily activities. 2With idiopathic hyperhidrosis, onset of symptoms typically presents in childhood or adolescence, and thecondition persists throughout adult life. 3 Idiopathic hyperhidrosis is not a psychological disorder orautonomic dysfunction. Episodes of excessive sweating usually occur at least once a week and do not occurduring periods of sleep. Diagnosis is based on a patient’s history and upon visible signs of sweating.Treatment options include topical therapy, medications, iontophoresis, botulinum toxin, and surgery.Generalized sweating is indicative of an etiology other than idiopathic hyperhidrosis. 3,4 Generalized orsecondary hyperhidrosis is likely to be due to medications or a systemic illness. Unlike primaryhyperhidrosis, episodes of excessive sweating occur during sleep with secondary hyperhidrosis.In addition to being used for the treatment of hyperhidrosis, astringents are also available in a non-legendproduct for wound healing. Balsam of Peru and castor oil are the active ingredients found in this over-thecounterproduct which has limited scientific information.The skin and mucous membrane astringents that are included in this review are listed in Table 1. Thisreview encompasses all (topical) dosage forms and strengths.Table 1. Skin and Mucous Membrane Astringents Included in this <strong>Review</strong>Generic Formulation(s) Example Brand Name(s) Current PDL Agent(s)Name(s)aluminum solution Drysol ® *, Drysol Dab-O-Matic ® *, Xerac aluminum chloridechlorideAC ®balsam of Peruand castor oil†aerosol N/A balsam of Peru andcastor oil*Generic is available in at least one dosage form or strength.†Brand is no longer available.N/A=not availableII.Evidence-Based Medicine and Current Treatment GuidelinesTreatment options for hyperhidrosis include topical therapy, iontophoresis, botulinum toxin, systemicmedications, and surgery. 2-8 Current treatment guidelines that incorporate the skin and mucous membraneastringents are summarized in Table 2.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.330
Table 2. Treatment Guidelines Using the Skin and Mucous Membrane Astringents<strong>Clinical</strong> GuidelineRecommendation(s)European Journal ofFor the treatment of axillary hyperhidrosis:Dermatology: CurrentTherapeutic Strategies for• Topical application of aluminum chloride is the methodof choice.Hyperhidrosis 5• Botulinum toxin is an alternative.• Surgery should be considered only after conservativemethods have failed.• Systemic anticholinergic medications can be tried, but theadverse effects profile may limit their use.For the treatment of palmoplantar hyperhidrosis:• Tap water iontophoresis is the method of choice.• Botulinum toxin is an alternative.• Surgery should be considered only in well-justified casessince it is highly invasive.• Systemic anticholinergic medications can be tried, but theadverse effects profile may limit their use.Mayo Clinic: Hyperhidrosis:Evolving Therapies for a Well-Established Phenomenon 2 • Treatment of choice for axillary hyperhidrosis isantiperspirants, such as 20% aluminum chloridehexahydrate.• Iontophoresis is available for palmoplantar and axillaryhyperhidrosis.• If topical aluminum chloride fails, botulinum toxin can betried.• Systemic anticholinergics are seldom used because ofadverse effects, such as sedation, dry mouth, andconstipation.American Academy of Family • Treatment of palmoplantar hyperhidrosis is a challengePhysicians: PalmoplantarHyperhidrosis: A TherapeuticChallenge 6 •and therapy should be individualized based on the degreeof functional impairment.The most effective topical treatment is 20% aluminumchloride.• Topical aluminum chloride and iontophoresis are simpleand safe, but their uses are limited by short-lived orinsufficient results.• Anticholinergic drugs are not usually used because of theside effects.• Botulinum toxin is an option in treatment-resistant cases,but effects are limited to a few months.• Surgery should be reserved for the most severe cases andshould only be considered after all other therapeuticoptions have been exhausted.Canadian Medical Association: • Topical aluminum chloride can be used as first-lineFocal Hyperhidrosis: Diagnosisand Management 7 •treatment of axillary and palmar hyperhidrosis.Iontophoresis can be used as second-line treatment ofpalmar and plantar hyperhidrosis.• Botulinum toxin is considered the most effectivetreatment, but is painful.• Surgery is an option for severe cases in which othertreatments have failed.The Royal Colleges of Surgeonsof Edinburgh and Ireland:Current Treatments forAxillary Hyperhidrosis 8 ••First-line treatment is topical aluminum chloride, whichis effective in the majority of cases.Systemic anticholinergics and iontophoresis areconsidered alternative treatments and have significantPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.331
<strong>Clinical</strong> GuidelineRecommendation(s)disadvantages.• Surgical sympathectomy is regarded as the gold standardin definitive treatment of axillary hyperhidrosis.However, risks of adverse consequences have to beconsidered.• Botulinum toxin is considered to be a highly effectiveand minimally-invasive treatment with few side effects.Botulinum toxin is recommended as the treatment ofchoice in isolated axillary hyperhidrosis and should beconsidered in patients who have failed topical agents.Aluminum chloride in ethanol (Drysol ® ) and aluminum tetrachloride (Xerac AC ® ) are examples ofprescription strength antiperspirants that may control mild to moderate symptoms. Over-the-counterantiperspirants are only successful with very mild symptoms of sweating. Antiperspirants work byphysically blocking the opening of the sweat gland or causing atrophy of the secretory cells. Skin irritationmay occur with the use of strong antiperspirants and therefore may limit their use. 2-8Iontophoresis is a process in which ionized substances are introduced into intact skin by a direct current totemporarily block sweat glands. 2-8 Limited data have shown iontophoresis to be effective in 85 percent ofpatients with palmar or plantar hyperhidrosis. Treatments can take between 10 to 30 minutes and thefrequency of treatments for maintenance of anhidrosis can vary between three times a week to every twoweeks.Botulinum toxin can temporarily reduce sweat production by blocking the release of neuronal acetylcholineat the presynaptic junction of both neuromuscular and cholinergic autonomic neurons. 2-8 The effects can benoticed within a day or two and last 6-10 months. Commonly reported adverse events include pain atinjection site (that may be alleviated with a topical anesthetic prior to injection), and temporary weakness inthe muscles of the thenar eminence that lasted an average of three weeks.Systemic medication such as beta-blockers or benzodiazepines may be helpful in cases of hyperhidrosisthat is made worse with emotional stimuli. 2-8 Although anticholinergic agents are sometimes used, data tosupport its use is lacking and they are often associated with side effects, such as dry mouth, blurred vision,or urinary retention.In severe cases, surgery to remove the sweat glands of the axillae may be performed. 2-8 However,permanent scarring and restricted arm movement may occur. Surgery to interrupt the upper thoracicsympathetic chain or endoscopic transthoracic sympathectomies (ETS) may also be performed, but areoften associated with side effects.III.IndicationsFood and Drug Administration (FDA)-approved indications for the skin and mucous membrane astringentsare summarized in Table 3. 9Table 3. FDA-Approved Indications for the Skin and Mucous Membrane AstringentsDrug(s)HyperhidrosisAluminum chlorideaPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.332
IV.PharmacokineticsThe pharmacokinetic parameters for the skin and mucous membrane astringents are summarized in Table 4.Table 4. Pharmacokinetic Parameters of the Skin and Mucous Membrane Astringents 9,10Drug (s) Systemic Absorption Distribution Excretion (Renal)Aluminum chloride Minimal Not determined Not determinedV. Drug InteractionsNo significant drug interactions with skin and mucous membrane astringents have been reported due to thetopical route of administration and the relatively low systemic bioavailability. 9,10VI.Adverse Drug EventsAdverse events with the skin and mucous membrane astringents are rare. 9,10 Since only a small percentageof drug is absorbed, most adverse events occur at the site of application. The most common adverse eventsreported with the skin and mucous membrane astringents are noted in Table 5.Table 5. Adverse Drug Events (%) Reported with the Skin and Mucous Membrane Astringents 9,10Adverse Event(s)Aluminum chlorideDermatologicalBurningaItchingaPrickling sensationaStingingaaPercent not specifiedVII.Dosing and AdministrationThe usual dosing regimens for the skin and mucous membrane astringents are summarized in Table 6. 9,10Table 6. Usual Dosing for Skin and Mucous Membrane AstringentsUsual PediatricDrug(s) Usual Adult DoseDoseAluminumchlorideApply to affected areaonce daily, only atbedtime. Onceexcessive sweating iscontrolled, apply onceor twice weekly asneeded.Apply to affectedarea once daily, onlyat bedtime. Onceexcessive sweating iscontrolled, applyonce or twice weeklyas needed.AvailabilitySolution: 6.25% aluminum chloride,20% aluminum chlorideTo minimize skin irritation, preparation should be applied to dry skin at bedtime and washed off in themorning before the sweat glands are fully active. 9,10 Irritated skin can be treated with topicalcorticosteroids, such as 2.5% hydrocortisone cream. For maximum effect, the treated area can be coveredwith plastic wrap and held in place by a snug-fitting T-shirt, mitten, or sock, but adhesive tape should notbe used for this purpose.Skin and mucous membrane astringents should not be applied to broken, irritated, or recently shavedskin. 9,10 Regular daytime antiperspirants or deodorants should not be used concurrently with skin andmucous membrane astringents.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.333
VIII. EffectivenessNo comparative clinical trials or brand vs. generic studies are available. <strong>Clinical</strong> studies evaluating the safety and efficacy of skin and mucous membraneastringents are summarized in Table 7.Table 7. Comparative <strong>Clinical</strong> Trials Using the Skin and Mucous Membrane AstringentsStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsScholes et al. 1120% aluminum chloridehexahydrate in absolutealcohol , applied nightlyMC, non-controlledPatients 14-51 years ofage with axillaryhyperhidrosis for 2-25yearsN=6515 monthsPrimary:Symptomatic reliefSecondary:Adverse effectsResultsPrimary:Sixty four patients or 98% achieved complete control of axillarysweating with periodic use of the solution.Secondary:Irritation of the axillary skin was reported in 45% of the patients,of which all but one patient achieved relief with 1%hydrocortisone cream.Rayner et al. 1220% aluminumchloride, applied onalternate nightsvs.placeboDB, PC, XOPatients 18-41 years ofage with axillaryhyperhidrosisN=366 monthsStudy abbreviations: DB=double-blind, MC=multicenter, PC=placebo-controlled, XO=crossoverPrimary:Symptomaticrelief, avoidance ofsurgerySecondary:Adverse effectsOne patient discontinued treatment due to intolerable irritation.Primary:After 2 weeks, 24 patients had achieved considerable relief, 6patients showed no improvement, 2 patients obtained relief withplacebo, and 4 patients obtained relief with both solutions.After 6 months of treatment, 68% opted for surgery.Secondary:Significant local reaction was seen in 55% of the patients.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.334
Additional EvidenceDose SimplificationA search of Medline and Ovid did not reveal data pertinent to this topic.Stable TherapyA search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician VisitsA search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 8. Relative Cost of the Skin and Mucous Membrane AstringentsGeneric Name(s) Formulation(s) Example Brand Name(s) BrandCostGenericCost$ $aluminum chloride solution Drysol ® *, Drysol Dab-O-Matic ® *, Xerac AC ®balsam of Peru and aerosol N/A N/A $castor oil*Generic is available in at least one dosage form or strength.N/A=not availableX. ConclusionsAluminum chloride products are considered first-line agents for the treatment of hyperhidrosis. 2,5-8Aluminum chloride is the simplest and safest method that has been shown to provide symptomatic relieffrom hyperhidrosis in most patients. 11 Iontophoresis, botulinum toxin, and surgery in severe cases areconsidered alternative treatments if topical application of aluminum chloride does not provide adequaterelief.There are no comparative clinical trials or brand vs. generic trials of the aluminum chloride products.Currently, aluminum chloride solution and balsam of Peru and castor oil are available generically.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.335
Therefore, all brand products within the class reviewed are comparable to each other and to the genericsand over-the-counter products in this class and offer no significant clinical advantage over otheralternatives in general use.XI.RecommendationsNo brand skin and mucous membrane astringent is recommended for preferred status. Alabama Medicaidshould accept cost proposals from manufacturers to determine cost effective products and possiblydesignate one or more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.336
References1. Stolman LP. Treatment of hyperhidrosis. Dermatol Clin. 1998;16(4):863-869.2. Eisenach JH, Atkinson JLD, Fealey RD. Hyperhidrosis: evolving therapies for a well-established phenomenon.Mayo Clin Proc. 2005;80(5):657-666.3. Smith CC. Idiopathic hyperhidrosis. In: Rose, BD, ed. UpToDate. Waltham, Mass: UpToDate, 2006.4. Stolman LP. Treatment of hyperhidrosis. J Drugs Dermatol. 2003;2(5):521-527.5. Togel B, Greve B, Raulin C. Current therapeutic strategies for hyperhidrosis: a review. Eur J Dermatol.2002;12:219-223.6. Thomas I, Brown J, Vafaie J, et al. Palmoplantar hyperhidrosis: a therapeutic challenge. Am Fam Physician.2004;69:1117-1120.7. Haider A, Solish N. Focal hyperhidrosis: diagnosis and management. CMAJ. 2005;172(1):69-75.8. Fitzgerald E, Feeley TM, Tierney S. Current treatments for axillary hyperhidrosis. Surg J R Coll Surg EdinbIrel. 2004;2(6):311-314.9. Wickersham RM, Novak KK, managing eds. Drug Facts and Comparisons. St. Louis, Mo: Wolters KluwerHealth, Inc.; 2006.10. Micromedex® Healthcare Series, (electronic version). Thomson Micromedex, Greenwood Village, CO, USA.Available at: http://www.thomsonhc.com. Accessed October, 2006.11. Scholes KT, Crow KD, Ellis JP, et al. Axillary hyperhidrosis treated with alcoholic solution of aluminumchloride hexahydrate. BMJ. 1978;2:84-85.12. Rayner CRW, Ritchie ID, Stark GP. Axillary hyperhidrosis, 20% aluminum chloride hexahydrate, and surgery.BMJ. 1980;280(6224):1168.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.337
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane Keratolytic AgentsAHFS Class 842800February 7, 2007I. OverviewKeratolytic agents induce sloughing of cornified epithelium. 1 Keratolytics cause peeling of the skin bysoftening and destroying the stratum corneum by increasing endogenous hydration. This in turn causes thecornified epithelium of the skin to swell, soften, and then desquamate. 1,2In normal skin with more than 10% hydration, the stratum corneum is a “wall” composed of stacked layersof comeocytes held together by a lipid-based intercellular matrix that serves as a tough yet flexibleprotective barrier against excessive water loss. 2 When the water content is less than 10%, disruption in thestratum corneum can occur, leading to scaling, cracking, and irritation, and resulting in skin disorders, suchas xerosis, ichthyosis, and psoriasis.Xerosis, or excessive dryness of the skin, is characterized by redness, dry scaling, and fissures. 2 Xerosisoccurs when there are abnormalities in the structure of the stratum corneum due to keratinization,proliferation, surface lipids, water metabolism, pH changes, and sebum. Ichthyosis is a hyperkeratotic skindisorder, characterized by dry and scaly skin that resembles the scales of a fish. 2,3 Psoriasis is associatedwith well-defined plaques bearing adherent, silvery scales. 1,4-5The skin and mucous membrane keratolytic agents that are included in this review are listed in Table 1.This review encompasses all (topical) dosage forms and strengths. Products solely indicated for thetreatment of acne and/or rosacea are considered cosmetics, and are not covered by Alabama Medicaid;hence, these products are not included in this review.Table 1. Skin and Mucous Membrane Keratolytic Agents Included in this <strong>Review</strong>GenericName(s)Formulation(s) Example Brand Name(s) CurrentPDLAgent(s)salicylic acid‡ cream, lotion, Salex ® *, Salex Shampoo ®salicylicurea‡shampoocream,emulsion,foam, gel,lotion,ointment,solution,suspension,toweletteCarmol 40 ® *, Kerafoam ® , Keralac ® *, Kerol Redi-Cloths ® , Umecta ® , Vanamide ® **Generic is available in at least one dosage form or strength.‡Over-the-counter product is available in at least one dosage form or strength.acidureaII.Evidence-Based Medicine and Current Treatment GuidelinesCurrent treatment guidelines that incorporate the skin and mucous membrane keratolytic agents aresummarized in Table 2.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.338
Table 2. Treatment Guidelines Using the Skin and Mucous Membrane Keratolytic Agents<strong>Clinical</strong> GuidelineRecommendation(s)Finnish Medical SocietyDuodecim: Psoriasis 4 • Treatment for psoriasis depends on the subtype, extent,severity, site of lesions, and patient’s preferences.• Topical treatment choices include vitamin D derivatives,emollients containing 5% salicylic acid to enhance theexfoliating effect, corticosteroids, coal tar preparations,dithranol, and tazarotene.• Other treatment options include phototherapy, acitretin,methotrexate, cyclosporin, sulfasalazine, and biologicals,such as alefacept, efalizumab, etanercept, and infliximab.International Journal of• Initial therapy for stable plaque psoriasis is often topicalDermatology: The Role ofSalicylic Acid in the Treatmentof Psoriasis 5 •agents, such as corticosteroids, coal tar, calcipotriene,tazarotene, salicylic acid, and emollients.For the treatment of psoriasis, salicylic acid should onlybe used in combination with other agents, such ascorticosteroids, to enhance penetration.• Phototherapy and systemic therapy may be employed inpatients who do not respond to topical therapy or havewidespread psoriasis.Finnish Medical SocietyDuodecim: SeborrhoeicDermatitis 6 • Treatment of seborrheic dermatitis includes removing thethick scales, decreasing the amount of sebum, decreasingfungal growth, and alleviating symptoms with topicalagents, such as corticosteroids, moisturizing emollient,and ketoconazole shampoo. Thick scales can be softenedwith a cream that contains salicylic acid and sulfur or bywetting and washing.British Association ofDermatologists: Guidelines forthe Management of CutaneousWarts 7 ••No treatment has a very high success rate. The average is60-70% clearance in three months.The treatment options depend on the type and site of thewart.• It is a valid option to leave warts untreated.• For warts on the face, salicylic acid (cream), cryotherapy,curettage plus light, and cautery can be used.• Salicylic acid paint, glutaraldehyde, and formaldehydecan be used for warts on the hands and feet.• For warts on the body and filiform warts, salicylic acid isnot a treatment option.III.IndicationsFood and Drug Administration (FDA)-approved indications for the skin and mucous membrane keratolyticagents are noted in Table 3.Table 3. FDA-Approved Indications for the Skin and Mucous Membrane Keratolytic Agents 8-18Indication Salicylic Acid UreaDebridement and promotion of normal healing ofhyperkeratotic surface lesionsaaHyperkeratotic conditions such as dry, rough skin,dermatitis, psoriasis, xerosis, ichthyosis, eczema,aakeratosis, keratoderma, corns, callusesDamaged, ingrown, and devitalized nailsaPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.339
IV.PharmacokineticsThe pharmacokinetic parameters for the skin and mucous membrane keratolytic agentsare summarized in Table 4.Table 4. Pharmacokinetic Parameters of the Skin and Mucous Membrane Keratolytic Agents 8-18Drug(s) Bioavailability(%)Volumeof DistributionProteinBinding(%)Site ofMetabolismSalicylic acid 60%absorbedNo data 50%-80%bound toalbuminNo dataMetabolites Excretion SerumHalf-Life(hours)Salicyluric acid(52%),salicylateglucuronides(42%),free salicylicacid (6%)95% isexcretedwithin 24hours intothe extracellularspaceNo dataUrea No data No data No data No data No data No data No dataV. Drug InteractionsDrug interactions with skin and mucous membrane keratolytic agents are limited due to the topical route ofadministration and the relatively low systemic bioavailability. 19-21 There are no significant drug interactionsreported with topical urea. Significant drug interactions have been reported with oral salicylicadministration. However, these drug interactions are unlikely to occur with topical administration unlessexcessive amounts are applied to diseased skin under occlusion. No cases of drug interactions have beenlinked to topical salicylate acid (Salex ® ) to date. 18VI.Adverse Drug EventsSystemic adverse drug events are unlikely with the skin and mucous membrane keratolytic agents, since thesystemic bioavailability is extremely low. 19-21 The most common adverse drug events reported with the skinand mucous membrane keratolytic agents are noted in Table 5.Table 5. Adverse Drug Events (%) Reported with the Skin and Mucous Membrane KeratolyticAgents 8-18Adverse Event(s) Salicylic acid UreaDermatologicalBurning - aErythema a -Irritation - aItching - aScaling a -Stinging - aVII.Dosing and AdministrationThe dosage and administration for the skin and mucous membrane keratolytic agents are summarized inTable 6.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.340
Table 6. Usual Dosing for the Skin and Mucous Membrane Keratolytic Agents 8-18Usual PediatricDrug(s) Usual Adult DoseDoseAvailabilitySalicylic acid Apply to affectedarea at night afterwashing; cover theIn children > 2 yearsof age: apply toaffected area at nightCream: 6%Lotion: 6%area; and washmedication off in themorning.after washing; coverthe area; and washmedication off in themorning.Urea Cream, emulsion, gel,lotion, ointmentsuspension: Apply toaffected area one tothree times a day asdirected; rub in untilcompletely absorbed;cover as needed.Apply to affectedarea one to threetimes a day; rub inuntil completelyabsorbed; cover asneeded.Cream: 40%, 50%Emulsion: 40%FoamGel: 40%, 50%Foam: Twice per day,or as directed by aphysician direct awayfrom the patient anddepress the actuatorfor 3 to 5 seconds oruntil foam begins todispense, rub in toaffected area untilcompletely absorbed.Towellette: Gentlyapply to affected skintwice per day, or asdirected by aphysician; use thesmooth side to helpmoistureize andevenly spreadsolutionover affectedarea.Lotion: 35%, 40%, 50%Ointment: 50%Suspension with applicator: 40%,50%Topical suspension: 40%Towelette: 42%Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.341
VIII. EffectivenessLimited comparative clinical trials of the skin and mucous membrane keratolytic agents are available. <strong>Clinical</strong> studies evaluating the safety and efficacy ofthe skin and mucous membrane keratolytic agents are summarized in Table 7.Table 7. Comparative <strong>Clinical</strong> Trials Using the Skin and Mucous Membrane Keratolytic AgentsStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsAdemola et al. 22Topical urea cream 40%(Carmol 40 ® ),frequency not specifiedvs.ammonium lactatetopical lotion 12% (Lac-Hydrin 12% ® ),frequency not specifiedRCT, DBPatients with moderateto severe xerosisN=2528 daysPrimary:Water loss fromthe skin surface,skin capacitance,skin desquamation,skin roughness,subject selfassessment of skin,and investigatorevaluationSecondary:Not reportedResultsPrimary:Significant improvements in skin roughness and fissure reduction,thickness, and dryness were observed with 40% urea creamcompared with 12% ammonium lactate lotion (no P valuereported).<strong>Clinical</strong> observation ratings by patients and investigators werebetter with urea cream compared with ammonium lactate lotion(no P value reported).Secondary:Not reportedDrug regimen abbreviations: QD=once daily, BID=twice daily, TID=three times daily, QID=four times dailyStudy abbreviations: AC=active-controlled, CI=confidence interval, DB=double-blind, DD=double-dummy, ES=extension study, HR=hazard ratio, MA=meta-analysis, MC=multicenter, OL=open-label,OS=observational study, PC=placebo-controlled, PG=parallel-group, PM=post marketing, PRO=prospective, RCT=randomized controlled trial, RETRO=retrospective, TB=triple-blind, XO=crossoverPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.342
Additional EvidenceDose SimplificationA search of Medline and Ovid did not reveal data pertinent to this topic.Stable TherapyA search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician VisitsA search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 8. Relative Cost of the Skin and Mucous Membrane Keratolytic AgentsGenericName(s)Formulation(s) Example Brand Name(s) BrandCostGenericCostsalicylic acid‡ cream, lotion, Salex ® *, Salex Shampoo ® $$$-$$$$ $$shampoourea‡cream, emulsion,foam, gel, lotion,ointment,solution,suspension,toweletteCarmol 40 ® *, Kerafoam ® ,Keralac ® *, Kerol Redi-Cloths ® , Umecta ® ,Vanamide ® *$$$-$$$$ $$*Generic is available in at least one dosage form or strength.‡Over-the-counter product is available in at least one dosage form or strength.X. ConclusionsKeratolytic agents, such as topical salicylic acid and urea, are effective and safe therapies for skinconditions such as seborrheic dermatitis, psoriasis, warts, corns, and calluses. These agents can be usedalone or in combination with other topical therapies, including corticosteroids. These topical agents arePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.343
generally well tolerated, with side effects limited to local skin reactions. No significant drug interactionshave been reported.Urea is available in different formulations (cream, emulsion, gel, lotion, ointment, solution, andsuspension), while the salicylic acid included in this review is available as a cream or lotion. No studieshave been conducted to demonstrate differences in efficacy or safety due to the different formulations.There are limited comparative clinical trials and no brand vs. generic trials of the skin and mucousmembrane keratolytic agents. Currently, salicylic acid and urea products are available generically.Therefore, all brand products within the class reviewed are comparable to each other and to the genericsand over-the-counter products in this class and offer no significant clinical advantage over otheralternatives in general use.XI.RecommendationsNo brand skin and mucous membrane keratolytic agent is recommended for preferred status. AlabamaMedicaid should accept cost proposals from manufacturers to determine cost effective products andpossibly designate one or more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.344
References1. McEvoy GK, ed. American Hospital Formulary Services, AHFS Drug Information. Bethesda, Md: AmericanSociety of Health-System Pharmacists; 2006.2. Bikowski J. Hyperkeratosis of the heels: treatment with salicylic acid in a novel delivery system. Skinmed.2004;3(6):350-351.3. Grekin JL, Basler RSW. New treatments for ichthyosis. Cutis. 1980;25:432-434.4. Finnish Medical Society Duodecim. Psoriasis. In: EBM Guidelines. Evidence-Based Medicine. Helsinki,Finland: Duodecim Medical Publications Ltd.; 2005.5. Lebwohl M. The role of salicylic acid in the treatment of psoriasis. Int J Dermatol. 1999;38:16-24.6. Finnish Medical Society Duodecim. Seborrhoeic dermatitis. In: EBM Guidelines. Evidence-Based Medicine.Helsinki, Finland: Duodecim Medical Publications Ltd.; 2004.7. Sterling JC, Handfield-Jones S, Hudson PM. Guidelines for the management of cutaneous warts. Br J Dermatol.2001;144(1):4-11.8. Salex ® [package insert]. DPT Laboratories. San Antonio, TX; not dated.9. Umecta ® [package insert]. JSJ Pharmaceuticals. Doylestown, PA; November 2005.10. U-Kera E TM [package insert]. Taro Pharmaceuticals, Inc. Hawthorne, NY; January 2006.11. Keralac ® Ointment [package insert]. Doak Dermatologics. Fairfield, NJ; July 2005.12. Keralac ® Nailstik [package insert]. Doak Dermatologics. Fairfield, NJ; October 2005.13. Keralac ® Lotion [package insert]. Doak Dermatologics. Fairfield, NJ; not dated.14. Keralac ® Cream [package insert]. Doak Dermatologics. Fairfield, NJ; not dated.15. Keralac ® Nail Gel [package insert]. Doak Dermatologics. Fairfield, NJ; not dated.16. Cervovel ® [package insert]. Hawthorn Pharmaceuticals, Inc. Madison, MS; not dated.17. Carmol ® 40 [package insert]. Doak Dermatologics. Fairfield, NJ; not dated.18. Abramovits W, Gupta AK. Salex (6% salicylic acid cream). Skinmed. 2004;3(5):272-273.19. Taylor JR, KM Halprin. Percutaneous absorption of salicylic acid [abstract]. Arch Dermatol. 1975;111(6):740.20. Gip L, Hamfelt A. Percutaneous absorption of betamethasone-17, 21-dipropionate and salicylic acid during thetreatment of psoriasis and eczema [abstract]. J Int Med Res. 1976;4(2):106.21. Birmingham BK, Greene DS, Rhodes CT. Systemic absorption of topical salicylic acid. Int J Dermatol.1979;18(3):228-231.22. Ademola J, Frazier C, Kim SJ, et al. <strong>Clinical</strong> evaluation of 40% urea and 12% ammonium lactate in thetreatment of xerosis [abstract]. Am J Clin Dermatol. 2002;3(3):217.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.345
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane Keratoplastic AgentsAHFS Class 843200February 7, 2007I. OverviewTopical coal tar and anthralin preparations are classified as keratoplastic agents. Topical coal tar has avariety of uses including treatment of psoriasis, seborrheic dermatitis, atopic dermatitis, and dandruff. Coaltar is available in several dosage forms including creams, lotions, oils, and shampoos. Coal tar is alsoavailable in combination with lanolin.The use of coal tar was first described by Dr. William Goeckerman in 1925, when it was combined withultraviolet light for the treatment of psoriasis. 1 It is a viscous liquid mixture of hydrocarbons that is distilledfrom coal in coking ovens. Medicinal use of coal tar likely stemmed from studies of the drug and itscarcinogenic properties. Researchers studied coal tar in these trials by applying it to the skin of mice,subsequently noticing improvements in the skin conditions of mice with psoriasis. It is thought to suppressepidermal deoxyribonucleic acid, (DNA) synthesis. 1Anthralin, also known as dithralin or dithranol, is a topical product also used to treat psoriasis, in particular,plaque psoriasis. Presently, anthralin is available in a cream dosage form. 2 It has been demonstrated toinhibit cell growth and restore cell differentiation. 2 Anthralin has been available since 1916, buttraditionally has not been used as a first-line agent because of its staining and irritant properties.Anthralin is available generically and coal tar is available over-the-counter and generically.The skin and mucous membrane keratoplastic agents that are included in this review are listed in Table 1.This review encompasses all (topical) dosage forms and strengths.Table 1. Skin and Mucous Membrane Keratoplastic Agents Included in this <strong>Review</strong>GenericName(s)Formulation(s) Example Brand Name(s) Current PDLAgent(s)anthralin cream Psoriatec ® * anthralincoal tar‡ cream, gel, Denorex ® , Denorex Extra Strength ® , DHS Tar ® *, coal tarlotion, oil,solution,shampooDoak Tar ® *, Fototar ® *, Ionil T ® *, Ionil T Plus ® *,Oxipor VHC ® , Pentrax ® , Polytar ® *, Psorigel ® ,Reme-T ® , Therapeutic Gel ® *, Theraplex T ® , X-Seb T Plus ® , Zetar ® *coal tar andlanolin‡solution Balnetar ® none*Generic is available in at least one dosage form or strength‡Over-the-counter product is available in at least one dosage form or strength.II.Evidence-Based Medicine and Current Treatment GuidelinesCurrent treatment guidelines that incorporate the skin and mucous membrane keratoplastic agents aresummarized in Table 2.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.346
Table 2. Treatment Guidelines Using the Skin and Mucous Membrane Keratoplastic Agents<strong>Clinical</strong> GuidelineRecommendation(s)American Academy of FamilyPhysicians (AAFP): Treatmentof Psoriasis: An Algorithm-Based Approach for PrimaryCare Physicians 1 ••Topical therapy is the mainstay of treatment for localizeddisease.Treatment options include anthralin, calcipotriene, coal tarproducts, corticosteroids, and tazarotene. Use of emollientsshould be encouraged, but they should be used selectivelybecause many (e.g., products containing lactic acid or alphahydroxyacids) can be irritating to inflamed or broken skin.• While topical corticosteroids are the mainstay of treatmentfor psoriasis, coal tar and anthralin are effective treatmentoptions.• Coal tar is most effective when it is used in combinationwith other agents, especially ultraviolet B light.• Coal tar is effective when it is combined with topicalcorticosteroids. Coal tar shampoo can be used incombination with a corticosteroid scalp solution for thetreatment of psoriasis on the scalp.• Because coal tar is messy and malodorous and can stainclothing, nighttime application is recommended.• If good control of psoriasis is not achieved with topicalcorticosteroids, alone or in combination with calcipotriene orcoal tar, consideration should be given to the addition ofanthralin or tazarotene therapy.• Anthralin is a second-line agent because of its irritating andstaining properties.• The concentration and duration of contact with eachtreatment is gradually increased, up to a maximum of 30minutes per application. Anthralin can also be combinedwith ultraviolet phototherapy• Combination products are not addressed.British Association ofDermatologists: PsoriasisGuidelines 2006 3 • Therapy depends on the affected sites, and the extent andseverity of psoriasis, in addition to the patient’s age, sex,occupation, personality, and general health.• Emollients are recommended to soften scaling and reduceirritation.• Topical corticosteroids are effective, cosmeticallyacceptable, and safe if used appropriately. There is a widerange of strengths available from mild to potent. Tolerancemay develop, as well as rebound exacerbations upondiscontinuation. Topical corticosteroids should be rotatedwith nonsteroidal treatments. Potent corticosteroids shouldnot be used for more than 7 days consecutively.• Coal tar-based creams in strengths between 1% and 5% havebeen proven efficacious in inducing remission in patientswith psoriasis, but are limited by adverse effects and patientpreference. Questions exist about the potentialcarcinogenicity of coal tar products, but no evidence exists tofirmly link them with cancers.• Tar and topical corticosteroids have a synergistic effect, andsome dermatologists adopt a regimen of a moderately potenttopical corticosteroid by day, with coal tar at night, for easeof patient use.• A vitamin D analogue, such as calcipotriene, may be used. Itis more convenient than coal tar products and does notproduce the side effects associated with topicalPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.347
corticosteroids. Irritant reactions are common. This hasbecome one of the first-line treatments for psoriasis andefficacy is comparable to potent corticosteroid treatment.• A vitamin A analogue (tazarotene) may be used and issuitable for moderate plaque psoriasis, affecting up to 10%of skin areas. Local irritation is common.• Anthralin has been used in the treatment of stable plaquepsoriasis and remains an effective topical remedy, withoutlong term local, systemic or teratogenic effects, but is limitedby adverse effects and patient preference.• Normally treatment is started at a lower concentration ofanthralin, and gradually increased as tolerated, but decreasedif burning occurs. Response can be gauged by palpating theplaque. Once lesions are palpably flat, anthralin should bediscontinued.• Combination products are not addressed.III.IndicationsFood and Drug Administration (FDA)-approved indications for the skin and mucous membranekeratoplastic agents are noted in Table 3.Table 3. FDA-Approved Indications for the Skin and Mucous Membrane Keratoplastic Agents 4-6Drug(s) Treatment of psoriasis Topically treatment for controlling dandruff,(quiescent or chronic) seborrheic dermatitis, or psoriasisAnthralinaCoal taraCoal tar and lanolinaIV.PharmacokineticsThe pharmacokinetic parameters for the skin and mucous membrane keratoplastic agents are summarizedin Table 4.Table 4. Pharmacokinetic Parameters of the Skin and Mucous Membrane Keratoplastic Agents 4-6Drug (s) Systemic Absorption Distribution Excretion (Renal)Anthralin Poor systemicabsorption, excellentepidermal absorptionNot determined The primary mode ofelimination is by washingoffCoal tar Minimal Not determined Not determinedCoal tar andlanolinMinimal Not determined Not determinedPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.348
V. Drug InteractionsDue to limited systemic absorption when anthralin and coal tar are administered topically, no druginteractions are likely to occur and none are documented with these skin and mucous membranekeratoplastic agents. 4-7VI.Adverse Drug EventsAdverse events with the skin and mucous membrane keratoplastic agents are common and result in theseagents being used as a second line agent. 1-3 Since only a small percentage of drug is believed to beabsorbed, most adverse events occur at the site of application. The most common adverse events reportedwith the skin and mucous membrane keratoplastic agents are noted in Table 5.Table 5. Adverse Drug Events (%) Reported with the Skin and Mucous Membrane KeratoplasticAgents 4-6Adverse Event(s) Anthralin Coal tar Coal tar and LanolinDermatologicalContact allergic reactions a - -Contact dermatitis - a aErythema a - -Folliculitis - a aHeat sensations a a aHerpes lesions - a aInflammation a - -Irritation a a aKeratocystomatosis - a aNecrosis a - -Pain a - -Photosensitivity - a aPsoriasis - a aPustular rash a - -Redness a - -Skin ulcerations - a aStatus varicosus - a aSwelling a - -Temporary discoloration of skin,hair, and fingernailsa - -Verruca vulgaris - a aWorsening of disease - a aOtherBacterial infection - a aCarcinogen effect-a(highconcentrations)a(high concentrations)Hypersensitivity reaction a a aNeutrophilia a - -Renal irritation a - -a Percent not specified- Event not reportedPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.349
VII.Dosing and AdministrationThe usual dosing regimens for the skin and mucous membrane keratoplastic agents are summarized inTable 6.Table 6. Usual Dosing for the Skin and Mucous Membrane Keratoplastic Agents 4-6Drug(s) Usual Adult Dose Usual PediatricDoseAnthralinPsoriasis:Skin: apply once a day to psoriaticlesions for 5-10 minutes using thelowest strength possible for at least 1week; contact time may increase up to20-30 minutes as toleratedSafety and efficacyin children havenot beenestablished.AvailabilityCream: 0.1%,0.25%, 0.5%,1%Coal tarandcoal tar andlanolinScalp: comb hair to remove scalardebris; wet and part hair; rub creaminto lesions; avoid spreading creamonto the forehead; remove by washingor showeringDandruff:Rub shampoo onto wet hair and scalp,massage into skin, rinse, and repeat;leave on skin for 5 minutes and rinsethoroughly; apply 2 times a week forthe first 2 weeks then once weekly or asneededSeborrheic dermatitis:Skin: apply to the affected area 1-4times daily; decrease frequency to 2-3times a week once the condition hasbeen controlledSoap: use on affected areas instead ofregular soap; work into a lather usingwarm water; massage into skin; rinseBath: add approximately 60-90 mL of5% - 20% solution or 15 mL - 25 mL of30% lotion to bath water; soak 5-20minutes; pat dry; use once daily for 3daysPsoriasis:Scalp application: tar oil bath or coaltar solution may be painted sparingly tothe lesions 3-12 hours before eachshampooSafety and efficacyin children havenot beenestablished.Cream: 0.5%,2%Emulsion: 1%,1.5%, 7.5%Gel:5%, 7.5%Liquid:1%, 1.2%, 9%,30%, 40%Lotion:1%, 2%, 5%,25%Oil: 2%, 2.5%Ointment: 1%,2%Shampoo:0.5%, 1%,1.1%, 2%,2.5%, 2.9%,3%, 4%, 4.3%,5%, 7%, 10%,12.5%, 15%Body application: apply at bedtime; ifthick scales are present, use productwith salicylic acid and apply severaltimes during the daySoap: 0.5%Solution: 0.5%,20%, 30%350Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
VIII. Effectiveness<strong>Clinical</strong> studies evaluating the safety and efficacy of the skin and mucous membrane keratoplastic agents are summarized in Table 7.Table 7. Comparative <strong>Clinical</strong> Trials Using the Skin and Mucous Membrane Keratoplastic AgentsStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsPsoriasisLangner et al. 8Coal tar gel, applieddaily for 6 days andcoal tar shampoo,applied twice a weekduring remissionvs.non-tar shampoo,applied twice a weekduring remissionSmith et al. 9Coal tar 1% lotion withesterified essential fattyacids (Exorex ® ), appliedtwice dailyvs.coal tar 1% lotion,applied twice dailyOne side received coaltar with fatty acidRCTPatients aged 7-70 yearswith scalp psoriasisRCT, DBPatients aged 18 yearsand older with mild tomoderate chronic plaquepsoriasisN=1127 daysN=208 weeksPrimary:Extent of lesions,severity of lesionsSecondary:Response ofpatients who failedother treatments;duration ofremission phasePrimary:Efficacy evaluationbased on score oferythema,induration, anddesquaminationSecondary:Psoriasis Area andSeverity Index(PASI); cosmeticacceptabilityPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.351ResultsPrimary:Complete clearing or marked improvement was seen in 83% ofpatients in the treatment group (P value not reported).Secondary:Among the 35 patients that were unresponsive to other treatments29 (82.8%) showed significant improvement (P value notreported).The duration of the remission phase was longer in patients whoused coal tar shampoo compared to non-tar shampoo.The median time to relapse among patients using non-tar shampoowas 3.22 months compared to 8.37 months for those using coal tarshampoo (P=0.003).Primary:No significant difference was found between the two treatmentgroups in the primary endpoints (P=0.52).Secondary:No significant difference was found between the two treatmentgroups in the secondary endpoints (P value not reported).
StudyandDrug Regimencomponent and theother side received coaltar without fatty acidcomponentGoodfield et al. 10Coal tar 1% lotion,applied 3 times a dayvs.coal tar 5% lotion,applied 3 times a dayChristensen et al. 11Dithranol 0.1% or0.25% cream(Amitase ® ), applied atbedtimevs.dithranol 0.1% or0.25% (Micanol ® )cream, applied atbedtimeAmitase ® is notcurrently available inthe Unites StatesStudy DesignandDemographicsRCT, DB, MC, PGPatients aged 16 yearsand older with chronicmild to moderate plaquepsoriasisRCT, SB, PG, MCPatients with plaquepsoriasisSample Sizeand StudyDurationN=32412 weeksN=726 weeksEnd PointsPrimary:Total Sign Score(TSS), or the sumof erythema,induration andscaling (range of 0-12); PASISecondary:Investigator andpatient assessedeffect ofmedication; patientcosmeticacceptabilityevaluationPrimary:Lesion indurationand scaling wasdetermined basedon the CompositeSign SeverityScore (CSSS)Secondary:Cosmetic variablesResultsPrimary:There was a greater percentage change in the TSS at week 12compared to baseline in the coal tar 1% group (5.6 to 3.2) whencompared to the coal tar 5% group (5.5 to 3.2; P=0.02).The percentage decrease in mean PASI at week 12 compared tobaseline was greater in the coal tar 1% group (6.8 to 4.4)compared to the coal tar 5% group (6.7 to 5.2; P=0.06).Secondary:A greater number of patients in the coal tar 1% group (38%)showed an improvement in clearance of their psoriasis comparedto the to the coal tar 5% group (27%). No P value reported.Primary:The CSSS reduction rate was similar for the Amitase ® groupcompared to the Micanol ® group. The only point that reachedstatistical significance was the greater CSSS reduction in theAmitase ® group (24%) compared to the Micanol ® group (19%) atweek 1 evaluations (P
StudyandDrug RegimenYoung. 12Dithranol 0.1% creamvs.dithranol 0.1% pasteDithranol cream wasapplied to one side anddithranol paste to theotherFredrikson. 13Dithranol cream 0.1%,applied once dailyvs.dithranol cream 0.25%,applied once dailyvs.Study DesignandDemographicsRCTPatients with psoriasisRCTPatients aged 18 yearsand older with psoriasisSample Sizeand StudyDurationN=152 weeksN=604 weeksEnd PointsPrimary:Sum of the scaling,erythema, andinduration scoresSecondary:Not reportedPrimary:Induration,redness, scaling,pruritus; evaluationof clinical effect oftreatmentSecondary:Cosmetic variablesResultsPrimary:The difference between the paste and the cream was notstatistically significant (P value not reported). Two patients foundthe paste to be more effective, five patients found the cream to bemore effective, and the remaining eight patients found thetreatments to be the same (P value not reported).Irritation was caused by the dithranol paste in seven patients, andthe remaining eight had no irritation on either treatment side(P=0.02). The paste also caused staining in thirteen patients, whiletwo did not have staining on either side (P value not reported).Secondary:Not reportedPrimary:There was no difference in efficacy between the dithranol cream0.25% and the dithranol ointment 0.25%. However, both werefound to be more effective when compared to the dithranol cream0.1% (P
StudyandDrug Regimendithranol 1%, 2%, and3% ointment, overnighttherapyStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsSecondary:Over the course of the study, overnight therapy caused morestaining than short contact therapy (P
StudyandDrug Regimenplacebo bath daily;dithranol 0.5% wasapplied dailyIncreasing strengths ofdithranol and dailyUVB radiation were useHarrington. 17Dithranol 0.11%, coaltar 1%, salicylic acid1.6% (Psorin ® ), appliedtwice dailyvs.RCTStudy DesignandDemographicsPatients with moderateplaque psoriasisSample Sizeand StudyDurationN=236 weeksEnd PointsPrimary:Scaling, erythemaSecondary:Patient daily recordResultsregimens and 10 disliked the combined therapy because it tooklonger to perform.The nursing staff members were not in favor of the combinedtherapy as it “entailed extra work”.Secondary:Not reportedPrimary:Psorin ® was more efficacious when compared to Alphosyl ® inimproving erythema, scaling, and overall improvement inpsoriasis (P
StudyandDrug Regimencoal tar 6% solution andsalicylic acid 2%pomade, applied oncedaily following a 17.5%cetrimide shampooDandruffPierard-Franchimont etal. 19Coal tar 0.5% shampoo,applied 3 times a weekStudy DesignandDemographicsRCT, DBPatients with moderateto marked dandruffSample Sizeand StudyDurationN=604 weeksEnd PointsPrimary:Scaliness of thescalp, Malasseziaspp. count, severityof dandruffResultserythema were all less for the dithranol group compared to thecoal tar group; but, pruritus occurred more often in the dithranolgroup compared to the coal tar group (P value not reported).Secondary:Not reportedPrimary:Both treatment groups were found to be effective at reducing thedandruff severity based on clinical scoring (P
Additional EvidenceDose Simplification:A search of Medline and Ovid did not reveal data pertinent to this topic.Stable Therapy:A search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician Visits:A search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 8. Relative Cost of the Skin and Mucous Membrane Keratoplastic AgentsGenericName(s)Formulation(s) Example Brand Name(s) BrandCostGenericCostanthralin cream Psoriatec ® * $$$$ $$coal tar‡ cream, gel, lotion, Denorex ® , Denorex Extra$ $oil, solution,shampooStrength ® , DHS Tar ® *, DoakTar ® *, Fototar ® *, Ionil T ® *,Ionil T Plus ® *, Oxipor VHC ® ,Pentrax ® , Polytar ® *,Psorigel ® , Reme-T ® ,Therapeutic Gel ® *, TheraplexT ® , X-Seb T Plus ® , Zetar ® *coal tar and solution Balnetar ® $ N/Alanolin‡*Generic is available in at least one dosage form or strength.‡Over-the-counter product is available in at least one dosage form or strength.N/A=not availablePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.357
X. ConclusionsTopical coal tar and anthralin preparations are classified as keratoplastic agents. Topical coal tar has avariety of uses including treatment of psoriasis, seborrheic dermatitis, and dandruff, while anthralin’sapproval is solely for quiescent or chronic psoriasis. 4-6 Coal tar is available in a variety of topicalformulations. Anthralin is available generically and coal tar is available over-the-counter and generically.One available formulation of coal tar is a combination with lanolin, an emollient. Guidelines state that anemollient can be used to soften scaling and reduce irritation. There is no specific mention of thiscombination product, which is available over-the-counter and generically.For the treatment of psoriasis, topical therapy is the mainstay of treatment for localized disease.Treatment options include anthralin, calcipotriene, coal tar products, corticosteroids, and tazarotene. Whiletopical corticosteroids are the mainstay of treatment for psoriasis, coal tar and anthralin are effectivetreatment options. If good control of psoriasis is not achieved with topical corticosteroids, alone or incombination with calcipotriene or coal tar, consideration should be given to the addition of anthralin ortazarotene therapy. 1-6 Coal tar is most effective when it is used in combination with other agents, especiallyultraviolet B light. Because coal tar is messy and malodorous and can stain clothing, nighttime applicationis recommended. Anthralin is considered a second-line agent because of its irritating and stainingproperties. When using anthralin the concentration and duration of contact with each treatment is graduallyincreased, up to a maximum of 30 minutes per application. Anthralin can also be combined with ultravioletphototherapy. 1-6The effectiveness of coal tar preparations in the treatment of psoriasis, dandruff and seborrheic dermatitishas been demonstrated in few well-controlled studies. Newer coal tar agents have been further modified orrefined to be more esthetically acceptable to patients. However, there currently are no published data thatshow that these modified or refined preparations of coal tar are more effective or better tolerated.Head-to-head trials comparing the skin and mucous membrane keratoplastics, coal tar, anthralin, and thecoal tar and lanolin combination are limited. The only study identified compared these two agents was inthe treatment of scalp psoriasis and no difference was found between the two treatment groups. 18 Theseagents may be used in combination with one another or with other antipsoriatics and phototherapy. 8,16-19These agents do have staining properties, and anthralin causes significant skin irritation. 4-6Therefore, all brand products within the class reviewed are comparable to each other and to the genericsand over-the-counter products in this class and offer no significant clinical advantage over otheralternatives in general use.XI.RecommendationsNo brand skin and mucous membrane keratoplastic agent is recommended for preferred status. AlabamaMedicaid should accept cost proposals from manufacturers to determine cost effective products andpossibly designate one or more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.358
References1. Pardasani AG, Feldman SR, Clark AR. Treatment of psoriasis: an algorithm-based approach for primary carephysicians. Am Fam Physician 2000;61:725-733,736.2. Federman DG, Froelich CW, Kirsner RS. Topical psoriasis therapy. Am Fam Physician 1999;59:957-62, 964.3. British Association of Dermatologists. Psoriasis Guidelines 2006. Available at:http://www.bad.org.uk/healthcare/guidelines/psoriasis.asp. Accessed October 4, 2006.4. Anthralin: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.5. Coal tar: drug information. In: Rose BD, ed. UpToDate. Waltham, MA: UpToDate; 2006.6. Micromedex ® Healthcare Series, (electronic version). Thomson Micromedex, Greenwood Village, CO, USA.Available at: http://www.thomsonhc.com. Accessed November 1, 2006.7. Tatro DS, ed. Drug Interaction Facts. St. Louis, Mo: Wolters Kluwer Health, Inc.; 2006.8. Langner A, Wolska A, Hebborn P. Treatment of psoriasis of the scalp with coal tar gel and shampoopreparations. Cutis. 1983;32:290-296.9. Smith CH, Jackson K, Chinn S, et al. A double-blind, randomized, controlled clinical trial to assess the efficacyof a new coal tar preparation (Exorex) in the treatment of chronic, plaque type psoriasis. Clin Exp Dermatol2000;25:580-583.10. Goodfield M, Kownacki S, Berth-Jones J. Double-blind, randomized, multicentre, parallel group studycomparing a 1% coal tar preparation (Exorex) with a 5% coal tar preparation (Alphosyl) in chronic plaquepsoriasis. J Dermatolog Treat. 2004;15:14-22.11. Christensen OB, Enstrom Y, Juhlin L, et al. A novel formulation in the over night treatment of psoriasis athome. Acta Derm Venereol. 1992:71:25-27.12. Young E. Treatment of psoriasis with dithranol cream compared with dithranol paste. Dermatologica.1986;173:285-287.13. Fredriksson T. A comparative study of dithranol cream, 0.25% and 0.1%, and dithranol ointment 0.25% in thetreatment of psoriasis. Pharmatherapeutica. 1983;3:496-498.14. Jones SK, Campbell WC, Mackie RM. Out-patient treatment of psoriasis: short contact and overnight dithranoltherapy compared. Br J Dermatol. 1985;113:331-337.15. Downey DJ, Finlay AY. Combined short contact crude tar and dithranol therapy for psoriasis. Clin ExpDermatol. 1986;11:498-501.16. Duhra P, Ryatt KS. Lack of additive effect of coal tar combined with dithranol for psoriasis. Clin Exp Dermatol.1988;13:72-73.17. Harrington CI. Low concentration dithranol and coal tar (Psorin) in psoriasis: a comparison with alcoholic coaltar extract and allantoin (Alphosyl).Br J Clin Pract. 1989;43:27-29.18. Wright S, Mann RJ. Comparison of a cream containing 0.1% dithranol in a 17% urea base (Psoradrate ® ) withcoal tar pomade in the treatment of scalp psoriasis. Clin Exp Dermatol. 1985;10:375-378.19. Pierard-Franchimont C, Pierard GE, Vroome V, et al. Comparative anti-dandruff efficacy between a tar and anon-tar shampoo. Dermatology. 2000;200:181-184.20. Davies, D.B., Boorman, G.C., Shuttleworth, D. Comparative efficacy of shampoos containing coal tar (4.0%w/w; Tarmed(TM)), coal tar (4.0% w/w) plus ciclopirox olamine (1.0% w/w; Tarmed(TM) AF) andketoconazole (2.0% w/w; Nizoral(TM)) for the treatment of dandruff/seborrhoeic dermatitis. J DermatologTreat. 1999;10(3):177-183.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.359
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane Agents, MiscellaneousSingle Entity AgentsAHFS Class 849200February 7, 2007I. OverviewThe skin and mucous membrane agents, miscellaneous included in AHFS Class 849200 represent a varietyof different products indicated to treat numerous skin conditions. Indications include actinic keratoses,Kaposi’s Sarcoma, atopic dermatitis, psoriasis, basal cell carcinoma, cutaneous T-cell lymphoma, andgenital warts. The wide variety of products, as well as the variety of indications, makes direct comparisonsdifficult. It is important to analyze current treatment guidelines, in addition to available evidence-basedmedicine when making therapeutic decisions. The single entity skin and mucous membrane agents,miscellaneous included in this review are listed in Table 1. This review encompasses all (topical) dosageforms and strengths.Table 1. Single Entity Skin and Mucous Membrane Agents, Miscellaneous Included in this <strong>Review</strong>Generic Name(s) Formulation(s) Example Brand Name(s) Current PDLAgent(s)acemannan suspension Salicept ® nonealitretinoin gel Panretin ® nonebecaplermin gel Regranex ® nonebexarotene gel Targretin ® nonecalcipotriene cream, ointment, Dovonex ®nonesolutionchloroxine shampoo Capitrol ® Capitrol ®collagenase ointment Santyl ® nonediclofenac gel Solaraze ® nonefluorouraciladhesive bandage, Carac ® , Efudex ® *,fluorouracilcream, solution Fluoroplex ®imiquimod packet Aldara ® nonepimecrolimus cream Elidel ® nonepodofilox gel, solution Condylox ® * podofiloxpodophyllum solution Podocon-25 ® nonetacrolimus ointment Protopic ® nonetazarotene cream, gel Tazorac ® none*Generic is available in at least one dosage form or strength.II.Evidence-Based Medicine and Current Treatment GuidelinesCurrent treatment guidelines that incorporate the single entity skin and mucous membrane agents,miscellaneous are summarized in Table 2.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.360
Table 2. Treatment Guidelines Using the Single Entity Skin and Mucous Membrane Agents,Miscellaneous<strong>Clinical</strong> GuidelineRecommendation(s)Infectious Diseases Society of • Proper care for patient with diabetic foot infectionsAmerica (ISDA):Diagnosis and Treatment ofDiabetic Foot Infections 1 •should include off-loading of pressure, wound cleansingand debridement, and appropriate antibiotic treatment.Sharp debridement with scalpel, scissors, or tissuenippers is preferable to the use of topical debridingagents.American Diabetes Association:Consensus DevelopmentConference on Diabetic FootWound Care 2 • Six approaches to the treatment of diabetic ulcers aresupported by clinical trials or well-established principlesof wound healing and include off-loading, debridement,dressings, management of infection, vascularreconstruction, and amputation.• Sharp debridement at frequent intervals has been shownto heal neuropathic wounds more rapidly.• Little data exists to support enzymatic debridement oversharp debridement.• Recombinant platelet derived growth factor (e.g.,becaplermin) has shown modest benefit when used withoff-loading, debridement, and treatment of infection butshould not be a substitute for appropriate wound care.Infectious Diseases Society of • Surgical debridement is recommended when needed.Skin and Soft-Tissue Infections 3America (ISDA):Practice Guidelines for theDiagnosis and Management of• Enzymatic debridement is not mentioned in theseguidelines.American Academy ofDermatology (AAD), Task Forceon Actinic Keratoses:Guidelines of Care for ActinicKeratoses 4 ••Actinic keratoses are the most common pre-malignantlesions.They may develop into squamous cell carcinomas.• Medical treatments may include topical 5-fluorouracil,masoprocol cream, or trichloroacetic acid (typicallyreserved for patients with extensive actinic keratoses).• Cryosurgery, curettage, electrosurgery, excision,dermabrasion, and laser surgery represent other options,depending on the extent and severity of the lesions.• Evolving strategies include α-hydroxy acids, topicalretinoids, systemic retinoids, and interferon.• This guideline was published prior to the Food and DrugAdministration (FDA) approval of imiquimod cream anddiclofenac gel for actinic keratoses.Centers for Disease Control and • Primary goal of treatment of visible genital warts isDiseases Treatment Guidelines, • Treatment should be guided by patient preference, cost,2006 5Prevention (CDC) Morbidity and removal of the warts.Mortality Weekly Report(MMWR):Sexually Transmitted• Currently available therapies may reduce infectivity butprobably do not eliminate infectivity.resources available, and the experience of the health careprovider.• No evidence exists to identify one treatment as moreefficacious than another and no treatment is ideal for allpatients with genital warts.• Treatment selection may be based on wart size andnumber, anatomic site of wart, wart morphology,convenience factors, and adverse effects of treatment.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.361
<strong>Clinical</strong> GuidelineRecommendation(s)• Treatment modalities should be changed if a patient hasnot experienced substantial improvement within 3 monthsof therapy.• Patient-applied treatments include podofilox 0.5% geland imiquimod cream. The patient can apply eitherproduct for the duration of therapy; however, an initialapplication may be performed by a health care providerto demonstrate proper technique.• Provider-administered treatments include cryotherapy,podophyllin resin, trichloroacetic acid, bichloroaceticacid, and surgery.• Alternative treatments include intralesional interferontherapy (though this is not recommended as initialtherapy) and laser surgery.American Academy ofDermatology (AAD), <strong>Clinical</strong>Guidelines Task Force:Guidelines of Care for AtopicDermatitis 6 ••Topical corticosteroids are the standard of care to whichother treatments are compared.Cutaneous adverse effects (striae, skin atrophy, andtelangiectasia) limit the use of topical corticosteroids.• Data regarding the optimal strength, concentration,duration, and frequency of application is lacking.• Noncutaneous adverse effects associated with long termuse of topical corticosteroids are not well documented.• Emollients are a standard of care and may be useful formaintenance therapy. They may also be steroid-sparing.• Calcineurin inhibitors (tacrolimus and pimecrolimus)have demonstrated efficacy in reducing the severity andextent of symptoms in adults and children. The longtermsafety of these agents (therapy for longer than 1year) is unknown, including the potential forimmunosuppression and malignancy.• Coal tar has been used in the treatment of atopicdermatitis though cosmetic tolerability may be a barrierto compliance and effective therapy.• Oral antihistamines have limited usefulness. There islimited evidence to support the efficacy of these agents incontrolling itch or urticaria associated with atopicdermatitis.• Topical doxepin may be used short term to controlpruritis.Primary Care Dermatology • Patients should be educated to avoid exacerbating factors.Guidelines for the Management • Topical corticosteroids provide short-term relief of acuteof Atopic Eczema 7Association of Dermatologists:Society and the British•emollients.Patients should be educated about the proper use offlares and potency should be matched to disease severity.• Very potent corticosteroids may be used on rareoccasions in resistant severe disease.• Immunomodulators are an alternative to corticosteroidsand should only be used if the patient is intolerant to orhas failed conventional corticosteroid therapy.European Academy ofDermatology and Venereology:Position Paper on Diagnosis andTreatment of Atopic Dermatitis 8 • Management of atopic dermatitis (AD) requires efficientshort-term therapy to control disease exacerbations, butthis must be managed carefully so that it does notnegatively affect long-term therapy aimed at stabilizationPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.362
<strong>Clinical</strong> GuidelineRecommendation(s)and flare prevention.• Hydration of skin should be maintained with emollients.• Allergen avoidance should be practiced.• Topical corticosteroids are a first-line anti-inflammatorytherapy. Application 2-3 times monthly with emollientsshould suffice in mild disease.• Tapering the dose of topical corticosteroids is importantto avoid withdrawal rebound.• Topical calcineurin inhibitors have demonstrated efficacyagainst placebo in clinical trials for short-term and longtermuse.• Tacrolimus 0.1% ointment is similar to an intermediatelypotent topical corticosteroid and an intermediately potenttopical corticosteroid is more active than pimecrolimus1% cream.• Safety has been demonstrated in clinical trials and themost common adverse effect is transient burning orwarmth at the application site.• The topical calcineurin inhibitors do not induce skinatrophy like corticosteroids, which favors their use ondelicate skin areas like the eyelids, perioral skin, genitalareas, inguinal fold, and for topical long-termmanagement.• <strong>Clinical</strong> and pre-clinical data do not indicate an increasedrisk for photocarcinogenicity, though ultraviolet (UV)protection is advised.• The efficacy of long-term monotherapy with tacrolimusointment has been shown in children over the age of 2and adults.American Academy of FamilyPhysicians (AAFP): Treatmentof Psoriasis: An Algorithm-Based Approach for PrimaryCare Physicians 9 ••Topical therapy is the mainstay of treatment for localizeddisease.Treatment options include corticosteroids, calcipotriene,coal tar products, tazarotene, and anthralin. Use ofemollients should be encouraged, but they should be usedselectively because many products (e.g., those containinglactic acid or α-hydroxy acids) can be irritating toinflamed or broken skin.• While topical corticosteroids are the mainstay oftreatment for psoriasis, coal tar and anthralin are effectivetreatment options.• Calcipotriene may be used as monotherapy but is usuallyused in combination with topical corticosteroids formaximum benefits.• Calcipotriene may be used with corticosteroids untillesions are flat, and then used as monotherapy with a“pulse” of corticosteroids on weekends only.• Tazarotene once daily has been shown to be as effectiveas twice daily fluocinonide cream 0.05%.• Tazarotene may be used as monotherapy but maximumbenefits are seen when it is combined with topicalcorticosteroids. It is pregnancy category X and shouldbe avoided in women of childbearing age.• Systemic therapy, including methotrexate, may bebeneficial in patients with refractory lesions.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.363
<strong>Clinical</strong> GuidelineRecommendation(s)British Association ofDermatologists:Psoriasis Guidelines 2006 10 • Therapy depends on the affected sites, the extent, and theseverity of psoriasis, in addition to the patient’s age, sex,occupation, personality, and general health.• Emollients are recommended to soften scaling and reduceirritation.• Coal tar based creams of between 1% and 5% have beenproven efficacious in inducing remission in patients withpsoriasis, but are limited by adverse effects and patientpreference. Questions exist about the potentialcarcinogenicity of coal tar products but no evidenceexists to firmly link them with cancers.• Topical corticosteroids are effective, cosmeticallyacceptable, and safe if used appropriately. There is awide range of strengths available from mild to potent.Tolerance may develop, as well as rebound exacerbationsupon discontinuation. Topical corticosteroids should berotated with nonsteroidal treatments. Potent steroidsshould not be used for more than 7 days consecutively.• A vitamin D analogue such as calcipotriene may be used.It is more convenient than tar products and does notproduce the side effects associated with topical steroids.Irritant reactions are common. This has become one ofthe first-line treatments for psoriasis and efficacy iscomparable to potent corticosteroid treatment.• Combination betamethasone and calcipotriene may beused, though data on long-term relapse rates is unknownat this point.• A vitamin A analogue (tazarotene) may be used and issuitable for moderate plaque psoriasis affecting up to10% of skin area. Local irritation is common.• Methotrexate may be considered in patients that havegreater than 10% of body surface area affected and inthose with extensive chronic plaque psoriasis, and inpatient who have failed topical therapy. Patients takingmethotrexate should be monitored closely forhematological abnormalities, renal function, and liverfunction.Joint British Association ofDermatologists and UnitedKingdom (U.K.) CutaneousLymphoma Group:Guidelines for the Managementof Primary Cutaneous T-CellLymphomas 11 ••The disease is classified and staged according to theWorld Health Organization (WHO) classification oflymphoma. Early disease, in which topical therapy isappropriate, corresponds to stages IA, IB, and IIA*.Therapeutic options include topical therapy, radiotherapy,immunotherapy, chemotherapy, monoclonal antibodytherapy, retinoids, and photopheresis.• Topical therapy, superficial radiotherapy, andphototherapy are appropriate for patients with early stagedisease (stage 1A-IIA) and the specific therapy should bebased on extent of disease and plaque thickness.• Psoralen ultraviolet A (PUVA) and α-interferon therapycan be effective for patients with resistant early-stagedisease (stage IB-IIA). Later stages will require systemictherapy.• Topical therapies include emollients, corticosteroids, andbexarotene; the antineoplastic agents mechlorethaminePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.364
<strong>Clinical</strong> GuidelineRecommendation(s)and carmustine are also used topically for this condition.• Topical bexarotene is typically reserved for patients withstage I mycosis fungoides (CTCL) not responding to orintolerant to other topical therapies.National Comprehensive CancerNetwork (NCCN) <strong>Clinical</strong>Practice Guidelines in Oncology:Basal Cell and Squamous CellSkin Cancers 12 ••Primary goals of treatment are cure of the tumor andmaximal preservation of function and cosmesis.Surgery offers the most effective and efficient means toachieve a cure, though radiation may be chosen as aprimary treatment based on maintaining function,cosmesis, and considering patient preference.• Low-risk basal cell carcinoma in situ may be treatedtopically with 5-fluorouracil, imiquimod, andphototherapy when surgery or radiation iscontraindicated. Cure rates may be lower with thesetreatments compared to surgery or radiation.• Actinic keratoses should be treated aggressively andtreatment options include cryosurgery, topical 5-fluorouracil, imiquimod, phototherapy, and curettage andelectrodessication.British Association ofDermatologists:Guidelines for the Managementof Basal Cell Carcinoma 13 ••Topical therapy with 5-fluorouracil is recommended forlow-risk, extrafacial basal cell carcinoma.Topical 5-fluorouracil can not be expected to eradicateinvasive disease or disease with follicular involvement.• Topical 5-fluorouracil can be useful in the treatment ofmultiple superficial basal cell carcinomas on the trunkand lower extremities.• This guideline was published before the approval ofimiquimod for the treatment of superficial basal cellcarcinoma.* Stage IA: T1 N0 (patches or plaques < 10% body surface area, no palpable nodes)Stage IB: T2 N0 (patches or plaques > 10% body surface area, no palpable nodes)Stage IIA: T1/2 N1 (patches or plaques < 10% or > 10% of body surface area, palpable nodes without histological involvement)Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.365
III.IndicationsFood and Drug Administration (FDA)-approved indications for the single entity skin and mucous membrane agents, miscellaneous are noted in Table 3.Table 3. FDA-Approved Indications for the Single Entity Skin and Mucous Membrane Agents, Miscellaneous 14-29IndicationStomatitis aKaposi’sSarcomaDiabeticulcers oflower limbsand feetwhich extendinto subcutaneoustissue andbeyond andhave adequateblood flowRefractorycutaneousT-celllymphoma(stage 1A and1B) intolerantto othertherapiesPlaquepsoriasisDandruff andseborrheicdermatitis ofthe scalpDebridementof necrotictissue indermal ulcersand severeburnsaaaDiclofenacsodiumPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.366AcemannanAlitretinoinBecaplerminBexaroteneCalcipotrieneChloroxineCollagenaseFluorouracilImiquimodPimecrolimusPodofiloxPodophyllumresina aaaTacrolimusTazarotene
IndicationActinickeratosisSuperficialbasal cellcarcinomaExternalgenital andperianal wartsDiclofenacsodiuma a aaEfudex ®5% onlyaAcemannanAlitretinoinBecaplerminBexaroteneCalcipotrieneChloroxineCollagenaseFluorouracilImiquimodPimecrolimusPodofiloxPodophyllumresina a aTo beadministeredonlyby aphysiciana aAtopicdermatitisAcne vulgaris aTacrolimusTazarotenePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.367
IV.PharmacokineticsThe pharmacokinetic parameters for the single entity skin and mucous membrane agents, miscellaneous aresummarized in Table 4.Table 4. Pharmacokinetic Parameters of the Single Entity Skin and Mucous Membrane Agents,Miscellaneous 14-29Drugs(s) Systemic Absorption Distribution Excretion (Renal) ActiveMetabolitesAcemannan No data No data No data No dataAlitretinoin Minimal No data No data No dataBecaplermin Minimal No data No data No dataBexarotene Minimal No data Minimal YesCalcipotriene 5-6% (ointment) No data No No1%(scalp solution)Chloroxine No data No data No data No dataCollagenase No data No data No data No dataDiclofenac 10% No data No data No dataFluorouracil No data (Carac ® )5.98% (Efudex ® )No data Minimal 0.055% (Carac ® )0.24% (Efudex ® )Imiquimod Minimal No data 0.11% (males) No data2.41% (females)Pimecrolimus Minimal No data No NoPodofilox Minimal No data No data No dataPodophyllumNo data No data No data No dataresinTacrolimus Minimal No data No data No dataTazarotene
VI.Adverse Drug EventsThe most common adverse drug events reported with the single entity skin and mucous membrane agents, miscellaneous are noted in Table 6.Table 6. Adverse Drug Events (%) Reported with the Single Entity Skin and Mucous Membrane Agents, Miscellaneous 14-29Adverse Event(s)Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.369DiclofenacsodiumCardiovascularAngina pectoris - - - - - - - - - - - - - >1 -Arrhythmias - - - - - - - - - a - - - >1 -Atrial fibrillation - - - - - - - - - 1.4 - - - - -Capillary leak- - - - - - - - - a - - - - -syndromeCardiac failure - - - - - - - - - a - - - - -Cardiomyopathy - - - - - - - - - a - - - - -Chest pain - - - - - - - 1-2 - 0.5 - - - - -Hypertension - - - - - - - 1-2 - 1.4- - - - >1 -2.7Ischemia - - - - - - - - - a - - - - -Myocardial- - - - - - - - - a - - - - -infarctionPalpitations - - - - - - - - - a - - - >1 -Pulmonary edema - - - - - - - - - a - - - - -Syncope - - - - - - - - - a - - - - -Tachycardia - - - - - - - - - a - - - - -Central Nervous SystemAgitation - - - - - - - - - a - - - - -Anxiety - - - - - - - - - 1.1 - - - >1 -Asthenia - - - 6 - - - 2 - - - - - 1-3 -Cerebrovascular - - - - - - - - - a - - - >1 -accidentConvulsions - - - - - - - - - a - - - - -Depression - - - - - - - - - a - - - >1 -Dizziness - - - - - - - - - 1.1- - 1 -1.4Emotional upset - - - - - - - - a - - - - - -Headache - - - 14 - - - 7 - 4-7.6 14-25 - - 5-20 -Hyperesthesia - - - - - - - 3 - - - - - 3-7 -AcemannanAlitretinoinBecaplerminBexaroteneCalcipotrieneChloroxineCollagenaseFluorouracilImiquimodPimecrolimusPodofiloxPodophyllumresinTacrolimusTazarotene
Adverse Event(s)Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.370DiclofenacsodiumHypokinesia - - - - - - - 2 - - - - - - -Insomnia - - - - - - - - a a - 1 -Multiple sclerosis - - - - - - - - - a - - - - -aggravationNeuritis - - - - - - - - - - - - - >1 -Paresis - - - - - - - - - a - - - - -Paresthesia - 3-22 - 6 - - - 8-20 - - - - a >1 -Polyneuritis - - - - - - - - - - - - a - -Suicide - - - - - - - - - a - - - - -Vertigo - - - - - - - - - - - - - >1 -DermatologicalAcne - - - - - - - 1 - - - - - 1-7 -Alopecia - - - - - - - 1-2 a 1.4 - - - >1 -Basal cell carcinoma - - - - - - - - - 2.3 - - - - -Benign skin- - - - - - - - - - - - - 1-3 -neoplasmBleeding at target - - - - - - - - - 2.2- - 1 -Contact dermatitis - - - 8-14 - - - 2-33 a - - - - 1-4 1-10Cracking - 8 - - - - - - - - - - - - -Crusting - 8 - - - - - - a 8-79 - - - - -Dermatitis - 25-77 - - - - - - - 1.4 - - - - -Desquamation - 3-9 - - - - - - - - - - - - 1-30Drainage - 8 - - - - - - - - - - - - -Dry skin - - - - 1-10 - - - - - - - - 1-7 1-10Eczema - - - - - - - - - 1.9 - - - - -Eczema herpeticum - - - - - - - - - - 0.8 - - 1-3 -Erosion - - - - - - - - 24.7-63.5Erythema - 25-77 - - 1-10 - - - 89.4-96.5AcemannanAlitretinoinBecaplerminBexaroteneCalcipotrieneChloroxineCollagenaseFluorouracilImiquimodPimecrolimusPodofiloxPodophyllumresinTacrolimusTazarotene1-54 - 67 - - -4-97 - - - 9-28 10-30
Adverse Event(s)Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.371DiclofenacsodiumErythematous rash - - 2 - - - - - - - - - - - -Eschar - 8 - - - - - - - - - - - - -Excoriation - 8 - - - - - - - 1-26 - - - - -Exfoliation - - - - - - - 6-24 - - - - - - -Exfoliative- 3-9 - 6 - - - - - a - - - 1-3 -dermatitisFlaking - 3-9 - - - - - - - 1-93 - - - - -Fissure - 8 - - - - - - - - - - - - 1-10Folliculitis - - - -
Adverse Event(s)Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.372DiclofenacsodiumSkin atrophy - - - - 1 -Skin disorder - - - - - - - - - 0.5- - - - 1-4 -2.8Skin hardening - - - - - - - - - - - - - - -Skin inflammation - - - - - - - - - - - - - - 1-10Skin nodule - - - - - - - - - - - - - - -Skin ulcer - - - - - - - 1-2 a 3-34 - 1 -Telangiectasia - - - - - - - - a - - - - - -Tinea cruris - - - - - - - - - >1 - - - - -Varicella zoster - - - - - - - - - - - - 1-5 -Verruca - - - - - - - - - 0.5 - - - - -Vesicles - - - - - - - - - 2-29 - 1 -functionDysmenorrhea - - - - - - - - - - - - - 2-4 -Edema - 3-8 - 10 - - - 3-4 14.1-60 7-71 - - - >1 -Gout - - - - - - - - - 1.1 - - - - -Hyperglycemia - - - - - - - 1 - - - - - >1 -Hyperlipidemia - - - 10 - - - 1 - 1.8 - - - - -Hypoglycemia - - - - - - - - - - - - - >1 -Peripheral edema - - - 6 - - - - - - - - - 1-4 -AcemannanAlitretinoinBecaplerminBexaroteneCalcipotrieneChloroxineCollagenaseFluorouracilImiquimodPimecrolimusPodofiloxPodophyllumresinTacrolimusTazarotene
Adverse Event(s)Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.373DiclofenacsodiumThyroiditis - - - - - - - - - a - - - - -GastrointestinalAbdominal pain - - - - - - - 1-2 - 0.5 - - - 1-5 -Anorexia - - - - - - - - - - - - - >1 -Constipation - - - - - - - - - - - - - >1 -Diarrhea - - - - - - - 2 - 0.5- 8 - - 3-6 -2.8Dyspepsia - - - - - - - 2-3 - 1.6- - - - 1-4 -2.8Gastritis - - - - - - - - - - - - - >1 -Gastroenteritis - - - - - - - - - - 7 - - 2-4 -Gastroesophageal - - - - - - - - - 1.4 - - - - -refluxMedicinal taste - - - - - - - - a - - - - - -Nausea - - - - - - - - - 1.1- - - - 1-3 -1.4Paralytic ileus - - - - - - - - - - - - a - -Stomatitis - - - - - - - a - - - - - -Vomiting - - - - - - - - - 1.4 9
Adverse Event(s)Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.374DiclofenacsodiumPlatelet count- - - - - - - - - a - - - - -decreasesRBC decreases - - - - - - - - - a - - - - -Thrombocytopenia - - - - - - - - a - - - a - -Toxic granulation - - - - - - - - a - - - - - -Laboratory Test AbnormalitiesBilirubinemia - - - - - - - - - - - - - >1 -CreatinineelevationsCreatininephosphokinaseelevationsAcemannanAlitretinoinBecaplerminBexaroteneCalcipotrieneChloroxineCollagenaseFluorouracilImiquimodPimecrolimusPodofiloxPodophyllumresin- - - - - - - 2 - - - - - >1 -- - - - - - - 4 - - - - - - -SGOT elevations - - - - - - - 3 - - - - - >1 -SGPT elevations - - - - - - - 2 - - - - - >1 -MusculoskeletalArthralgia - - - - - - - 2 - 0.9 - - - >1 -Arthritis - - - - - - - - - 0.9 - - - >1 -Arthrosis - - - - - - - 2 - - - - - - -Myalgia - - - - - - - 2-3 - 1-1.4 - - - 1-3 -Osteomyelitis - - a - - - - - - - - - - - -Skeletal pain - - - - - - - - - 0.5- - - - - -1.6RespiratoryAsthma - - - - - - - 2 - - - - - 4-16 -Bronchitis - - - - - - - - - 0.9 - - 2-6 -Cough - - - 6 - - - - - 1.6- 15-16 - - 1-18 -2.8Dyspnea - - - - - - - 2 - a - - - >1 -Hypoxia - - - - - - - - - - - - - >1 -Laryngitis - - - - - - - - - - - - - >1 -Lung disorder - - - - - - - - - - - - - >1 -Nasal irritation - - - - - - - - a - - - - - -Nasopharyngitis - - - - - - - - - - 15-26 - - - -Pharyngitis - - - 6 - - - 2 - 1.1- 8 - - 3-10 -1.9Pneumonia - - - - - - - 2 - - - - 1-2 -TacrolimusTazarotene
Adverse Event(s)Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.375DiclofenacsodiumPulmonary- - - - - - - - - 0.5 - - - - -congestionPulmonary infection - - - - - - - - - - - - - - -Rhinitis - - - - - - - 2 - 2.7- 13 - - 2-6 -3.3Rhinorrhea - - - - - - - - - - 4 - - - -Sinusitis - - - - - - - 2 1.6-4.7 2.2- - - - 2-7 -7.4Upper respiratory - - - - - - - - - 3.2- 21-24 - - - -infection15.3Wheezing - - - - - - - - - - 4 - - - -OtherAbrasion - - - - - - - - - 3.3 - - - - -Accidental injury - - - - - - - 4 - - - - - 3-12 -Alcohol intolerance - - - - - - - - - - - - - 3-7 -Allergic reaction - - - - - - - 1 1.2-2.3 - - - - 4-15 -Allergy aggravated - - - - - - - - - 1.1 - - - - -Anaphylactoid - - - - - - - - - - - - - >1 -reactionAngioedema - - - - - - - - - a - - - >1 -Back pain - - - - - - - 2-4 - 1.4- - - - 1-3 -3.8Birth defect - - - - - - - - - - - - - - -Breast pain - - - - - - - - - - - - >1 -Burning - 34 - - 10-15 - - - 60-83.5 1.9-26 - 64-78- 26-5810-30Chafing - - - - - - - - - - - 1 -Chills - - - - - - - - - - - - - >1 -Coma - - - - - - - - - - - - a - -Common cold - - - - - - - - 2.4-4.7 - - - - - -Conjunctival- - - - - - - - a - - - - - -reactionConjunctivitis - - - - - - - 2-4 - 0.5 - - - 1-4 -Corneal reaction - - - - - - - - a - - - - - -Cyst - - - - - - - - - - - - - 1-3 -AcemannanAlitretinoinBecaplerminBexaroteneCalcipotrieneChloroxineCollagenaseFluorouracilImiquimodPimecrolimusPodofiloxPodophyllumresinTacrolimusTazarotene
Adverse Event(s)Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.376DiclofenacsodiumDeath - - - - - - - - - - - - a - -Dehydration - - - - - - - - - - - - - >1 -Ear pain - - - - - - - - - - - - - >1 -Ecchymosis - - - - - - - - - - - - - >1 -Epistaxis - - - - - - - - - - - - - >1 -Eye infection - - - - - - - - - - - - - - -Eye irritation - - - - - - - - 3.4-7.1 - - - - - -Eye pain - - - - - - - 2 - - - - - >1 -Facial edema - - - - - - - - - - - - - 1-3 -Fatigue - - - - - - - - - 1.4- - - - - -2.2Fever - - - - - - - - - 1.4- 13-32 - a 1-21 -1.6Flu symptoms - - - - - - - - - 1.9-3 - - - 22- -35Flu syndrome - - - - - - - 1-10 - - - - - - -Fungal infection - - - - - - - - - 1.1 - - - - -Furunculosis - - - - - - - - - - - - - >1 -Hernia - - - - - - - - - 1.9 - - - >1 -Hypersensitivity - - - - - - a - - - 8 - - - -Infection - - a 18 - - - 4 - 0.5- - - - 1-14 -1.1Inflammation - 3-8 - - - - - - - - - 63- - - -71Inflicted injury - - - - - - - - - 1.6- - - - - -8.8Influenza - - - - - - - - - - 13 - - - -Lack of effect - - - - - - - - - - - - - 1-10 -Lacrimation - - - - - - - - a - - - - - -Malaise - - - - - - - - - - - - - >1 -Malodor - - - - - - - - - - - 1 -Otitis media - - - - - - - - - - 4 - - 1-12 10-30Pain - 34 - 30 - - - 2-26 30.6- 1.4-8 - 50- - 1-4 -AcemannanAlitretinoinBecaplerminBexaroteneCalcipotrieneChloroxineCollagenaseFluorouracilImiquimodPimecrolimusPodofiloxPodophyllumresinTacrolimusTazarotene
Adverse Event(s)Diclofenacsodium61.2 72Periodontal abscess - - - - - - - - - - - - - 1-3 -Peripheral vascular - - - - - - - - - - - - - >1 -disorderPost-operative pain - - - - - - - - - 1.4 - - - - -Rigors - - - - - - - - - 1.4 - - - - -Sensitivity reaction - - - - - - - - - - - - - - -Swelling - 3-8 - - - - - - a - - - - - -Taste perversion - - - - - - - - - - - - - >1 -Tooth disorder - - - - - - - - - - - - - >1 -Unintended- - - - - - - - - - - - - >1 -pregnancyUrticaria - - - - - - - - a - - - - 1-5 -Vasodilatation - - - - - - - - - - - - - >1 -Viral infection - - - - - - - - - 1.4 7 - - - -RBC=red blood cells, SGOT=serum glutamic-oxaloacetic transaminase, SGPT=serum glutamate pyruvate transaminase, WBC=white blood cellsa Percent not specified- Event not reportedAcemannanAlitretinoinBecaplerminBexaroteneCalcipotrieneChloroxineCollagenaseFluorouracilImiquimodPimecrolimusPodofiloxPodophyllumresinTacrolimusTazarotenePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.377
On February 15, 2005, the FDA Pediatric Advisory Committee convened to evaluate the potential cancerrisk of pediatric patients being treated for atopic dermatitis with topical immunosuppressants. At thismeeting, carcinogenicity studies in 3 animal species were reviewed along with post-marketing reports ofcancer-related adverse events associated with the use of these medications.As of December 2004, the FDA received 19 reports of cancer-related adverse events linked with Protopic ®use (3 cases in pediatric patients
carcinogenic and that there is a need for long-term cohort studies in patients using topical calcineurininhibitors to further evaluate any potential photocarcinogenicity. 36VII.Dosing and AdministrationThe usual dosing regimens for the single entity skin and mucous membrane agents, miscellaneous aresummarized in Table 7.Table 7. Usual Dosing for the Single Entity Skin and Mucous Membrane Agents, Miscellaneous 14-29Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityAcemannan Not reported Not reported Freeze-driedpowder forreconstitutionAlitretinoinBecaplerminApply generous coating tolesions 2 times daily; mayincrease to 3-4 times dailyas toleratedApply an even coating oncedaily to ulcer, cover with asaline dressing for 12 hoursthen remove dressing andrinse woundThe amount of gel useddepends on the size of theulcer:15 g tube: length (at longestpoint) x width (at widestpoint) x 0.6Safety and efficacy in childrenhave not been establishedSafety and efficacy in childrenhave not been establishedGel: 01%Gel: 0.1%BexaroteneCalcipotriene2 g tube: length (at longestpoint) x width (at longestpoint) x 1.3Apply to lesions every otherday for 1 week, thenincrease as tolerated to oncedaily for 1 week, then 2times daily for 1 week, then3 times daily for 1 week,then 4 times dailyApply a thin layer toaffected area 1-2 times perday and rub in completelySafety and efficacy in childrenhave not been establishedSafety and efficacy in childrenhave not been establishedGel: 1%Cream: 0.005%Ointment:0.005%ChloroxineUse twice weekly, massageinto wet scalp, avoid contactwith eyes, lather shouldremain on the scalp forapproximately 3 minutes,then rinsed; applicationshould be repeated and thescalp rinsed thoroughlySafety and efficacy in childrenhave not been establishedSolution:0.005%Shampoo 2%Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.379
Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityCollagenase Apply directly to wound orto gauze pad affixed to theSafety and efficacy in childrenhave not been establishedOintment: 250units/gwound once daily or morefrequently if dressingbecomes soiledDiclofenac Apply to lesions 2 times Safety and efficacy in children Gel: 3%Fluorouracildaily for 60-90 daysActinic keratosis:Carac ® : apply a thin layer tolesions once daily for up to 4weeksEfudex ® : apply to lesions 2times daily for 2-4 weeksFluoroplex ® : apply tolesions 2 times daily for 2-6weekshave not been establishedSafety and efficacy in childrenhave not been establishedCream: 0.5%,1%, 5%Solution: 2%ImiquimodSuperficial basal cellcarcinoma:Efudex ® 5%: apply tolesions 2 times daily for 3-6weeksActinic keratosis: apply tolesions 2 times per week for16 weeks, apply to acontiguous area of 25 cm 2 ,continue therapy for 16weeksSafety and efficacy in childrenunder the age of 12 have notbeen establishedCream: 5%External genital warts: applyto warts 3 times per week atbedtime and leave on for 6-10 hours, continue therapyfor a maximum of 16 weeksPimecrolimusPodofiloxPodophyllumresinSuperficial basal cellcarcinoma: apply to biopsyconfirmed area 5 times perweek at bedtime and leaveon for 8 hours, continuetherapy for 6 weeksApply a thin layer to theaffected skin and rub incompletely 2 times dailyApply to wart tissue 2 timesdaily (morning and evening)for 3 consecutive days thendo not use for 4 consecutivedays, may repeat up to 4times until no visible warttissue remainsApply sparingly to lesionwith applicator and allow itto dry, limit contact time to1-4 hours, rinse off with380Children > 2 years of age:apply a thin layer to theaffected skin and rub incompletely 2 times dailySafety and efficacy in childrenhave not been establishedSafety and efficacy in childrenhave not been establishedCream: 1%Gel: 0.5%Solution: 0.5%Solution: 25%Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Drug(s) Usual Adult Dose Usual Pediatric Dose Availabilitysoap and waterTacrolimus Apply a thin layer of 0.03%or 0.1% ointment to theaffected skin and rub incompletely 2 times dailyuntil clearing occurs, andcontinue for 1 additionalweekChildren > 2 years of age:apply a thin layer of the 0.03%ointment to the affected skinand rub in completely 2 timesdaily until clearing occurs, andcontinue for 1 additional weekOintment:0.03%, 0.1%TazarotenePsoriasis: apply a thin layerof 0.05% gel to coverlesions only once daily inthe evening, apply to nomore than 20% of bodysurface area, strength maybe increased to 0.1% gel astoleratedSafety and efficacy in childrenunder the age of 12 have notbeen establishedGel: 0.05%,0.1%Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.381
VIII. Effectiveness<strong>Clinical</strong> studies evaluating the safety and efficacy of the single entity miscellaneous mucous membrane agents are summarized in Table 8.Table 8. Comparative <strong>Clinical</strong> Trials Using the Single Entity Miscellaneous Skin and Mucus Membrane AgentsStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsActinic KeratosisNelson et al. 37Diclofenac 3% gelBIDall patients receivedopen-label activetreatmentMC, OLPatients 48-100 years of agewith a diagnosis of 5 ormore actinic keratosis (AK)lesions contained in 1-3blocks (5 cm 2 ) on theforehead, central face, orscalp)N=7690 days with30 dayfollow-upperiodPrimary:Investigators’ globalimprovement index(IGII) at each postbaselinevisit, targetlesion number score(TLNS), andcumulative lesionnumber score(CLNS)Secondary:Not reportedSecondary:Not reportedWolf et al. 38 RCT, DB, PC N=118 Primary: Primary:ResultsPrimary:Diclofenac gel demonstrated a decrease in the TLNS as early as30 days after treatment initiation and the decrease was greatestat 90 and 120 days post-treatment. Baseline TLNS was 8.4lesions, decreasing to 6.1 on day 30, 3.2 on day 60, 1.4 on day90, and 0.8 on day 120.The percentage of patients with >75% lesion clearance was 78%at day 90 and 85% at day 120.The percentage of patients with 100% lesion clearance was 41%at day 90 and 58% at day 120.Diclofenac gel demonstrated a decrease in the CLNS of 78%from baseline at day 90 and 83% from baseline at day 120.The percentage of patients with >75% lesion clearance was 69%at day 90 and 72% at day 120.The percentage of patients with 100% lesion clearance was 32%at day 90 and 45% at day 120.The IGII indicated that AK lesions were significantly improvedin 45% of patients and completely improved in 27% of patientsat day 90. At day 120, 42% were considered significantlyimproved and 42% were considered completely improved.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.382
StudyandDrug RegimenDiclofenac 3% gelBIDvs.placebo vehicle(hyaluronan gel) BIDStudy DesignandDemographicsPatients 18 years of age orolder with a diagnosis ofactinic keratosis (AK) withlesions contained in 1 to 35-cm 2 blocks in one or moreselected major body areas(forehead, central face,scalp, arms, and hands)Sample Sizeand StudyDuration90 daysEnd Points(1) Proportion ofpatients at follow-upwith no lesions asrated by target lesionnumber score(TNLS) andcumulative lesionnumber score(CLNS) (both equalto 0, “no lesions”);(2) proportion ofpatients rated as“completelyimproved”, withvalues equal to 4 onthe investigatorglobal improvementindex (IGII) and thepatient globalimprovement index(PGII)ResultsThe proportion of patients with TLNS=0 was 50% of patients inthe diclofenac group compared to 20% in the vehicle group(P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsratings), absolutereductions frombaseline in AK lesioncounts andproportionalreductionsResultssignificantly improved in the fluorouracil group compared to theplacebo group at weeks 1, 2, and 4 (P6 AK lesions (minimum of3 on each side of treatmentarea); the 0.5% cream wasapplied to one side of thestudied area (face or baldscalp) and the 5% cream tothe other for the duration ofthe study; the severity of theAK lesions was equallymatched on either sideN=218 weeksSecondary:Not reportedPrimary:Reduction in numberof AK lesionscompared to baseline,total clearance of AKlesions at the end ofthe 4-week posttreatmentperiod,tolerability, patientpreferencequestionnaireSecondary:Not reportedPrimary:There was a reduction in lesion count of 8.8 in the patientsreceiving the 0.5% cream and 6.1 in patients receiving the 5%cream (P=0.006 and P=0.054 respectively compared tobaseline). The difference between groups was also significant(P=0.044).The mean absolute change in baseline in the number of AKlesions by treatment side showed that the 0.5% cream had amean decrease of 8.2 lesions on the left side of the face and 9.5on the right side of the face compared to the 5% cream whichhad a mean decrease of 6.3 lesions on the left side of the faceand 6.0 on the right side (significance of this finding notdiscussed).The percentage change in the number of AK lesions aftertreatment was 67% for the 0.5% cream and 47% for the 5%cream (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsThe severity of facial irritation was rated as mild in 19% ofpatients treated with the 0.5% cream and 14.3% of patients inthe 5% group, moderate in 33.3% in the 0.5% group and 28.6%in the 5% group, and severe in 47.6% of patients in the 0.5%group and 57.1% in the 5% group (P values not reported).On the patient preference questionnaire, 85% of patientspreferred the 0.5% cream and 15% of patients preferred the 5%cream (P=0.003).Eight patients felt their skin looked better after treatment withthe 0.5% cream and 1 patient felt their skin looked better aftertreatment with the 5% cream, 5 people felt that the 0.5% cream“did a better job” compared to 2 people who felt the 5% cream“did a better job”, and 5 patients preferred the physicalproperties of the 0.5% cream compared to 0 patients preferringthe 5% cream (P values not reported).Significantly more patients expressed a willingness to re-treatwith the 0.5% cream if necessary (P=0.031).Jorizzo et al. 41Fluorouracil 0.5%cream QD for 7 daysvs.vehicle cream QD for7 dayspatients with residuallesions after the 4-week follow-up periodreceived cryosurgeryRCT, MC, DB, PCPatients 18 years of age orolder with 5 or more visibleor palpable actinic keratosis(AK) lesions on the faceN=14412 monthPrimary:Reduction (bothabsolute andpercentage) in AKlesions at the 4-weekfollow-up visit, theproportion of patientswith completeclearance of AKlesions at the 4-weekfollow-up visit beforecryosurgery, theoccurrence rate at the6-month follow-upSecondary:Not reportedPrimary:At 4 weeks, patients in the fluorouracil group had significantlyfewer lesions compared to the patients in the vehicle group (4.3and 9.1 respectively, P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsvisit, and theclearance rate the 6-month follow-up visitResultsreceived both fluorouracil and cryosurgery were clear of AKlesions compared to 7.7% in the vehicle and cryosurgery group(P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsperiod.ResultsStockfleth et al. 43Imiquimod 5% creamQD 3 times/week for12 weeksvs.vehicle cream 3times/week for 12weeksRCT, DB, PCN=36Patients 45-85 years of age 12 weeks ofdiagnosed with actinic treatmentkeratoses (AK) in aand 1 yeartreatment area that did not of follow-upexceed 20 cm 2Primary:Lesion clearancerates at the end oftreatment and at 14weeks, recurrence ofAK lesions inpatients treated withimiquimod at 1 yearpost-treatmentSecondary:Not reportedComplete clearance rates increased as the severity of erythema,edema, erosion/ulceration, weeping/exudate, andscabbing/crusting increased (P
StudyandDrug Regimenthis study contains theresults of follow-updata at 2 years in theprevious StockflethstudyLee at al. 45Imiquimod 5% creamQD 2 or 3 times/weekfor 16 weeksvs.vehicle cream QD 2 or3 times/week for 16weeksthis study followedpatients who hadshowed completeclearance of actinickeratosis (AK) lesionsat 8 weeks posttreatmentin four phaseIII studies, and invitedthem back for a 1-timeevaluation at 12-18months post-originaltreatmentKorman et al. 46Imiquimod 5% creamQD 3 times/week for16 weeksvs.OSStudy DesignandDemographicsPatients 45-86 years of agewith AK who demonstratedcomplete clearance of AKlesions at 8 weeks posttreatmentin 4 phase IIIclinical trials of imiquimodvs. vehicle creamMAPatients 18 years of age andolder diagnosed with actinickeratosis (AK) having 4-8AK lesions with acontiguous 25 cm 2treatment area on the face orSample Sizeand StudyDurationN=1461 time visit12-18monthspost-originaltreatmentN=49216 weeks oftreatmentand 8 weeksof posttreatmentfollow-upEnd PointsPrimary:AK recurrence rateSecondary:Not reportedPrimary:Complete clearancerate (proportion ofpatients at the 8-weekpost-treatmentfollow-up with noclinically visible AKlesions in theSecondary:Not reportedResultsPrimary:The recurrence rate of AK lesions was lower in patients whohad previously received imiquimod 3 times/week (24.7%)compared to those who had received it 2 times/week (42.6%).Patients with fair skin had a higher recurrence of AK lesionscompared to patients with Fitzpatrick type III-V skin (in the 3times/week group: 29% vs. 14%, and in the 2 times/week group:50% vs. 33%).The recurrence rate of AK lesions in the vehicle-treated patientswas 46.7%.Statistical comparisons between groups were not reported.Secondary:Not reportedPrimary:Complete clearance was observed in 48.3% of patients in theimiquimod group and 7.2% of patients in the vehicle group(P
StudyandDrug Regimenvehicle cream QD 3times/week for 16weeksAtopic DermatitisKapp et al. 47Pimecrolimus 1%cream BID at first signof flare until completeclearance of signs andsymptomsvs.vehicle cream BID atfirst sign of flare untilcomplete clearance ofsigns and symptomspatients in both groupswere permitted use ofmoderately potentcorticosteroids to helpStudy DesignandDemographicsbalding scalpRCT, DB, PC, PG, MCInfants 3-23 months of agewith a clinical diagnosis ofatopic dermatitis (AD)Sample Sizeand StudyDurationN=25112 monthsEnd Pointstreatment area)Secondary:Partial clearance rate(proportion ofpatients at the 8-weekpost-treatmentfollow-up with 75%reduction in thenumber of baselineAK lesions in thetreatment area),median percentage ofreduction of baselineAK lesions at the 8-week post-treatmentvisitPrimary:Incidence of flares ofAD at 6 monthsSecondary:Investigator’s GlobalAssessment (IGA)score, Eczema Areaand Severity Index(EASI), andcaregiver’sassessments ofpruritis and overalllevel of diseasecontrol (pruritis wasassessed by thecaregiver for 24hours prior to studyvisits and ranked on a(P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointstreat flares scale of 0 [none] to 3[severe], and wereasked to assess thelevel of control overthe preceding 7 dayson a 4-point scale.The IGA score,pruritis assessment,and caregiverassessments weredichotomized intotreatment success[score of 0 or 1] ortreatment failure [allother scores]).Resultscorticosteroid during the study period, compared to 34.8% inthe vehicle group and the proportion of study days on acorticosteroid was 3.2% in the pimecrolimus group compared to6.2% in the vehicle group (P values not reported).Secondary:An IGA score of 0 or 1 (clear or almost clear) was achieved in44.6% of patients in the pimecrolimus group compared to 8.7%in the vehicle group (P
StudyandDrug RegimenPapp et al. 48Pimecrolimus 1%cream BID at first signof flare until completeclearance of signs andsymptomsall patients receivedactive treatmentpatients werepermitted use ofmoderately potentcorticosteroids to helptreat flaresStudy DesignandDemographicsSample Sizeand StudyDurationOL, ESN=91Infants 3-23 months of age 12 monthswith a clinical diagnosis ofatopic dermatitis (AD)This was an extension of thestudy by Kapp et al, above 66End PointsPrimary:Proportion of patientswith no flares,treatment successrates (proportion ofpatients with clear oralmost clear skin asindicated by anInvestigator’s GlobalAssessment [IGA] of0 or 1), Eczema Areaand Severity Index[EASI], percentageof total body surfacearea (TBSA) affectedby AD, course ofdisease (proportionof disease-free dayswithout the use ofany medication),adverse effectsSecondary:Not reportedResultsmonth 6 (P0.058).Primary:The median number of days of pimecrolimus use during the 12months of the present study was 99, and 27.5% of these patientsrequired corticosteroids during this time.Seventy-six patients used pimecrolimus for 2 years (originalstudy by Kapp et al, and present study combined) and there wasa progressive reduction in the mean proportion of pimecrolimustreatment days from 73.7% during the first 3 months of thesecond year to 42.3% during the last 3 months of the secondyear.The proportion of patients in this study who did not use topicalcorticosteroids during the first year was 71.1% and thisincreased to 72.4% during the second year. Overall, 57.9% ofpatients in the pimecrolimus group did not use corticosteroids atall during the 2 years.The percentage of patients experiencing no flares during thesecond year was 76.9% and 8.8% had only a single flare. Inpatients on pimecrolimus for 2 years, the proportionexperiencing no flares increased from 77.6% during the firstyear to 85.5% during the second year.The proportion of patients who were clear or almost clear ofsigns of AD increased from 36.3% at the beginning of thesecond year to 71.4% at the end of the second year.The mean EASI score decreased from 5.8 to 2.9 and the meanpercentage of TBSA affected by AD decreased from 11.3% to6.6%.At the beginning of the first, double-blind year, 75% of patientstreated with pimecrolimus for 2 years had moderate or severedisease. At the end of the second year, the percentage of391Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultspatients with minimal residual activity or were clear of signs ofAD was 69.7%. Only 13.2% had an IGA of >2. In this samegroup of patients, an improvement in EASI scores was alreadyevident at 3 months and persisted for the remaining 21months.The mean percentage of TBSA affected by AD decreased from28.4% at the beginning of the first year to 7.3% at the end of thesecond year.The proportion of disease-free days increased from 30% duringthe first 6 months of the second year to 50.9% during the last 2months.The majority of adverse effects reported were conditionscommonly seen in childhood such as nasopharyngitis, pyrexia,cough, diarrhea, ear infection, bronchitis, rhinitis, vomiting, andgastroenteritis.There were no reports of application site reactions.Staab et al. 49Pimecrolimus 1%cream BID for 4weeksvs.placebo cream BID for4 weeksPhase I: 4 weeks oftreatmentPhase II: 12 weekopen-label extensionRCT, DB, PC, PG, MCPatients 3-23 months of agediagnosed with atopiceczema (1) affecting somepart of face (2) affecting>5% of body surface area(BSA), and (3) having abaseline InvestigatorsGlobal Assessment (IGA)score of mild severity orgreaterN=1964 weeks(Phase Idata only)Primary:(1) Parents’ qualityof life in 5 domains:psychosomatic wellbeing,effects onsocial life,confidence inmedical treatment,emotional coping,and acceptance ofdisease, as measuredby the quality-of-life(QoL) questionnairefor Parents ofChildren with AtopicSecondary:Not reportedPrimary:Significant improvements were seen in all domains of thePQoL-AD in favor of pimecrolimus (P
StudyandDrug RegimenPhase II:4 week follow-upStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsDermatitis (PQoL-AD); (2) pruritis andsleep loss, using theSeverity Scoring ofAtopic Dermatitis(SCOR-AD); (3)severity of disease,using InvestigatorsGlobal Assessment(IGA); (4) degree ofdisease control,measured by theEczema Area andSeverity Index(EASI)Resultsobserved in 53.5% of patients in the pimecrolimus group at day29 compared to 10.6% of patients in the placebo group(P1 point comparedwith baseline within48 and/or 72 hours,percentage ofpatients with apruritis responsePrimary:There was a significant improvement in pruritis (>1 point) in thepimecrolimus group compared to the vehicle group over the 7day treatment period (P=0.001).The median time to pruritis improvement (>1 point) was 2 daysin the pimecrolimus group compared with 4 days in the vehiclegroup (P values not reported).Secondary:Improvements in pruritis scores (>1 point) were seen by day 2(within 48 hours) in 56% if pimecrolimus patients compared to34% of patients in the vehicle group (P=0.003). By day 3(within 72 hours), 72% of pimecrolimus patients reportedimprovements in pruritis severity compared with 45% of vehiclepatients (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointswithin 4,5,6, and 7days of treatment, thepercentage ofpatients with apruritis severity scoreof 0 (absent) or 1(mild) for treatmentdays 2,3,4,5,6, and 7regardless of baselinescores, and thepercentage ofpatients with an IGAscore improvementof >1 point at studycompletion (end ofthe DB phase)compared withbaselineResultsgroup who showed improvement by day 7 (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsWarmth/stinging/burning was reported in 20% of thepimecrolimus patients compared to 17% in the tacrolimuspatients though this difference was not statistically significant(P=0.931).The duration of ASRs tended to be shorter in the pimecrolimusgroup compared to the tacrolimus group (P value not reported).None of the patients in the pimecrolimus group whoexperienced erythema/irritation reported that it lasted longerthan 30 minutes, compared to 85% of patients in the tacrolimusgroup who reported that this ASR lasted between 30 minutesand 12 hours (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsproduct (P=0.06).ResultsThe overall incidence of adverse effects was similar between thetreatment groups: 86% of patients in the pimecrolimus groupreported adverse effects compared to 845 in the tacrolimusgroup (P value not reported).There was no significant difference in IGA scores ofclear/almost clear between treatment groups at any visit, thoughboth increased compared to baseline values (P>0.05).On day 22, significantly more patients in the tacrolimus groupreported absent or mild pruritis compared to the pimecrolimusgroup (P=0.042), though differences on all other days were notsignificant.On day 43, there were no significant differences betweentreatment groups in the proportion of patients achieving IGA orpruritis scores of 0 or 1 (P=0.493).IGA response rates were slightly higher in the tacrolimus groupcompared to the pimecrolimus group from day 8-43, thoughthese differences were not statistically significant (except forday 22 as mentioned above).More than 60% of patients in both groups reported absent ormild pruritis.Ashcroft et al. 52Pimecrolimus 1%creamMAChildren, adolescents, andadults diagnosed with atopicdermatitisN=68971 week to 12monthsPrimary:For pimecrolimus:proportion of patientsrated by theinvestigator as clearThe change from baseline in body surface area (BSA) affectedby AD was similar in both treatment groups, thoughpimecrolimus tended to have a greater effect on the head andneck compared to tacrolimus which tended to have a greatereffect on the legs.Primary:For pimecrolimus:In five trials evaluating pimecrolimus vs. vehicle, pimecrolimuswas significantly more effective than vehicle at 3 weeks(P
vs.StudyandDrug Regimentacrolimusvs.vehiclevs.topical corticosteroidsStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsor almost clearFor tacrolimus:proportion of patientsachieving at least90% improvementfrom baselineSecondary:Patients’ globalassessments offeeling better ormuch better,proportion of patientswith flares of atopicdermatitis,improvements inquality of life,tolerability assessedby overall rates ofwithdrawal,withdrawal due toadverse effects,proportion of patientswith burning of theskin and skininfectionsResultsthis efficacy at 6 weeks (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsproportion of patients clear or achieving excellent improvement(P=0.006), but that the 0.1% strength did not differ from vehicle(P=0.13) at 3 weeks. When evaluating patients’ assessments ofimprovement as better or much better, both strengths provedsignificantly better than vehicle. Three other trials reported thesame outcomes as described above after 12 weeks and foundboth strengths to be significantly more effective than vehicle(P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Points(P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsquality of life to be improved in patients taking pimecrolimuscompared to placebo, and 3 trials showed increases in quality oflife in patients taking tacrolimus 0.03%and 0.1% compared toplacebo (P values not reported).Tacrolimus 0.1% was found to have a significantly greaterimprovement on quality of life in adults compared to the 0.03%strength, but no significant differences were found in infantsand children (P values not reported).Reitamo et al. 53Tacrolimus 0.1%ointment BID toaffected areas untilclear and then for 7more daysvs.RCT, DB, MC, CSPatients 18 years of age andolder with a diagnosis ofatopic dermatitis with aseverity grading ofmoderate to severeN=9726 monthsPrimary:Response rate atmonth 3 (proportionof patients with atleast 60%improvement inmodified EczemaArea and SeverityIndex [mEASI])No quality of life assessments were found comparingpimecrolimus and tacrolimus to topical corticosteroids (P valuesnot reported).Primary:At month 3, 72.6% of patients in the tacrolimus groupresponded to treatment compared to 52.3% of patients in thecorticosteroid group (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsaffected body surfacearea (BSA), patient’sassessment of itchand quality of sleep,and the number ofdays on treatment asa percentage of daysin the studyResultsin the tacrolimus group compared to the corticosteroid group(P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointspercent of BSAaffected, patient’sassessment of itch,and safety endpoints(overall incidences ofall adverse eventsand individualincidence rates ofapplication siteadverse events)ResultsIn all patients with moderate disease, the percentage reductionin EASI score at week 6 was significantly higher in thetacrolimus group compared to the pimecrolimus group(P=0.003).In patients with head and neck involvement, the percentagereduction in EASI score at week 6 was greater in the tacrolimusgroup compared with the pimecrolimus group (57% and 42%respectively, P=0.01).Secondary:IGADA scores were significantly better at 6 weeks fortacrolimus compared to pimecrolimus in the adult patient group,in the children with moderate to very severe disease, and in thecombined analysis (all P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsIn both pediatric studies, there were no significant differencesobserved in adverse effects between tacrolimus andpimecrolimus groups (P values not reported).In the adult study, application site burning occurred morefrequently in the tacrolimus group compared to thepimecrolimus group (P=0.02) early in treatment, but by week 1there were no significant differences observed between thegroups (P value not reported).Basal Cell CarcinomaRomagosa et al. 55Fluorouracil 5% creamin a phosphatidylcholine carrier BID for4 weeksvs.RCT, DBPatients with biopsy-provenmoderate thickness BCCsN=13(17 BCCs)4 weekstreatmentand followupat week16Primary:Cure rateSecondary:Not reportedIn the pediatric study of patients with mild AD, significantlymore patients withdrew from the study due to an adverse effectin the pimecrolimus group compared to the tacrolimus group(P=0.002).Primary:The cure rate in the phosphatidyl choline group was 90% andthe cure rate in the regular fluorouracil group was 57% (Pvalues not reported, investigators reported no statisticallysignificant difference in outcomes detected between groups).Secondary:Not reportedfluorouracil 5% cream(as Efudex ® ) BID for 4weeksMarks et al. 56Imiquimod 5% creamapplied 5 times/weekvs.imiquimod 5% creamapplied 7 times/weekOSPatients with histologicallyconfirmed superficial basalcell carcinoma (sBCC) ontheir trunk, limbs, or neckN=67(208tumors)18 weeksPrimary:Presence of residualtumor upon clinicaland histologicalevaluation 12 weeksafter treatment,tolerability oftreatmentSecondary:Primary:Histological clearance occurred in 161 tumors (77%). In the 5times/week group, 100% of patients had clearance of at least 1tumor compared with 93% in the 7 times/week regimen (Pvalue not reported).Tumors cleared in 47% of patients in the 5 times/week regimenand in 58% of patients in the 7 times/week regimen (P value notreported).403Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsNot reportedResultsIn the 5 times/week regimen, 89% of patients had 50% or moreof their tumors clear compared with 84% in the 7 times/weekregimen (P value not reported).Local skin reactions were common but well tolerated and therewas a correlation to the intensity of local inflammatoryreactions and the histological clearance of tumors (statistics notreported).Gollnick et al. 57Imiquimod 5% cream5 times/week onconsecutive days for 6weeksall patients receivedactive treatmentPeris et al. 58Imiquimod 5% creamQD 3 times/week for12 weeksOL, OSPatients 21-89 years of agewith at least 1 histologicallyconfirmed superficial basalcell carcinoma (sBCC) onthe limbs, trunk, neck, orhead with a minimum areaof 0.5 cm 2 and a maximumdiameter of 2.0 cm with amaximum tumor depth of
StudyandDrug Regimenall patients receivedactive treatmentStudy DesignandDemographicswhere surgery is not anoption or if treatment otherthan surgery was requestedSample Sizeand StudyDurationnodular)12 weektreatmentwith 12monthfollow-upEnd Pointstreatmentobservational periodEfficacy rates:1=complete response,disappearance ofBCC, 2=partialresponse,>40%
StudyandDrug RegimenGeisse et al. 59Imiquimod 5% creamQD 5 times/weekvs.vehicle cream QD 5times/weekvs.imiquimod 5% creamQD 7 times/weekvs.vehicle cream QD 5times/weekStudy DesignandDemographicsMC, RCT, DB, PC, DRPatients 18 years of age orolder with a primary,histologically confirmedsuperficial basal cellcarcinoma (sBCC) at least0.5 cm 2 with a maximumdiameter of 2 cm, located onthe limbs, trunk (anogenitalarea excluded), neck, orhead with no signs ofaggressive growth patternsSample Sizeand StudyDurationN=7246 weeks oftreatmentwith 12week posttreatmentfollow-upperiodEnd PointsPrimary:Complete compositeclearance rate, i.e.,proportion of patientsat 12 weeks posttreatmentwho wereconsidered completeresponders, definedas those with (1) noclinical orhistological evidenceof BCC at target siteor (2) with clinicalevidence but nohistological evidenceof BCC, and wherethe false-positiveclinical assessmentwas explained by thehistological findingsSecondary:Adverse effectsResultsPrimary:The composite clearance rates for the 5 times/week and 7times/week imiquimod groups were 75% (95% CI: 68%-81%)and 73% (95% CI: 66%-79%) respectively.Clearance rates based on histological data only for the 5times/week and 7 times/week groups were 82% (95% CI: 76%-87%) and 79% (95% CI: 73%-85%) respectively.Composite and histological clearance rates for the vehiclegroups were 2%-3%. The differences between both activegroups and their corresponding vehicle groups for compositeand histological clearance rates were statistically significant(P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsApplication site reactions possibly or probably related totreatment occurred in 29% of patients in the imiquimod 5times/week group, and in 43% of the 7 times/week group,compared to 2.8% and 6.6% of patients in the respective vehiclegroups.Less than 10% of patients experienced a severe adverse effectLocal skin reactions (LSR) were more intense in the activetreatment groups compared to the vehicle groups. LSRs weremost intense at 3 weeks and fell back to at or below baseline byweek 12.LSRs had significantly higher severity ratings in the imiquimodgroups compared to their respective vehicle groups (P
StudyandDrug RegimenCutaneous T-Cell LymphomaHeald et al. 61MC, OLBexarotene 1% gelQD, BID, TID, QID,escalated as toleratedall patients receivedactive treatmentStudy DesignandDemographicsPatients 18 years of age andolder diagnosed withcutaneous T-cell lymphoma(CTCL) staged as IA, IB, orIIA according to the tumornodes metastasis stagingsystem for malignanttumors (TNM), andrefractory or intolerant to,or have reached the 6-monthor greater response plateauon at least 2 prior therapiesfrom the following:psoralen ultraviolet A(PUVA), ultraviolet B(UVB), electron beamradiation therapy (EBT),photopheresis, interferon,systemic cytotoxicchemotherapy, topicalmechlorethamine, or topicalcarmustineSample Sizeand StudyDurationN=5016 weekswith anoption tocontinuetreatmentEnd PointsPrimary:Physicians GlobalAssessment of<strong>Clinical</strong> Condition(PGA), or CompositeAssessment of IndexLesion DiseaseSeverity (CA)For PGA: Completeclinical response(CCR) required100% improvementof cutaneous diseaseand partial response(PR) required >50%improvement. Bothhad to be confirmedby at least 2consecutiveobservations within 4weeks.For CA:Five index lesionswere chosen andassessed based onscaling, erythema,plaque elevation,hypopigmentation,and hyperpigmentation.Thesum of all grades forall clinical signs forall index lesions atbaseline was dividedResultsPrimary:CCR or PR was observed in 44% of patients according to thePGA and in 46% of patients according to the CA.Responses were observed in 64% of patients with Stage IAdisease and 50% of patients with Stage IB disease. Patientswith Stages IIA disease did not respond to therapy.Secondary:The percentage of BSA involvement decreased from a baselinevalue of 9% to 6.6% at week 16 and 4.5% at week 44.Index lesion erythema, plaque elevation, scaling, pruritis,hypopigmentation or hyperpigmentation all improved during thestudy (no specific percentages given).There was a decrease in the aggregate of index lesions by 9.7%at week 24 and 70% at week 40.The earliest time to response was recorded at 28 days and thelatest was recorded at 504 days.The time to relapse (duration of response) was recorded at 214.5days in 26% of responding patients.The time to disease progression ranged from 1 day to 87 days.When asked to compare general CTCL status at baseline and atweek 16, 75% of patients reported that they were moderately ormuch improved, and 705 of patients at week 16 weremoderately or very satisfied with treatment.408Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsinto the sum gradesfor all comparableclinical signs for thesame index lesions ateach subsequentpost-baseline visit.This generated a CAratio. A CA ratio of1.0indicated aworsening of disease.CCR was defined asa CA of 0 and a PRwas defined as a CAof
StudyandDrug RegimenGenital WartsArican et al. 62Imiquimod 5% cream3 times/week for 12weekvs.placeboStudy DesignandDemographicsRTC, DB, PCPatients 18 years of age andolder with a diagnosis ofexternal anogenital wartsSample Sizeand StudyDurationN=4512 weektreatment, 6monthfollow-upEnd Pointssurface area responseto treatment, time toresponse (defined asfirst observationwhen a patient hasimproved by 50% orgreater), duration ofresponse, and time todisease progression,responses to thepatient Quality ofLife QuestionnairePrimary:Clearance ofanogenital wartsSecondary:Not reportedResultsPrimary:After treatment, 69.7% of patients in the treatment group (all ofthe female patients and 54.5% of the male patients) hadcomplete clearance of the warts, 9 patients had 50%-90%clearance, and 1 patient had
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsDuring the follow-up period, 13% developed recurrent diseaseand were treated with CO 2 vaporization (17 patients were lost tofollow-up during this time).Moresi et al. 64Imiquimod 5% creamvs.podofilox 0.05% gelRETROInfants and young childrendiagnosed with anogenitalwartsN=254 monthsPrimary:Clearing of lesions,adverse effects, andrecurrence of lesionswith estimated lengthof wart-free periodSecondary:Not reportedSecondary:Not reportedPrimary:Seventeen patients were treated with podofilox and of those,parents of 15 patients reported resolution of lesions with norecurrence for periods ranging from 4 months to 2 years.Adverse reactions reported in the podofilox group includedburning (most common), pain, redness, erosions, and edema.Eight patients were treated with imiquimod and of those,parents of 6 patients reported clearing of lesions whichremained clear 6-12 months after therapy ended.Tyring et al. 65Podofilox 0.5% gelBID for 3 consecutivedays followed by 4days with no treatmentvs.placebo gel BID for 3consecutive daysfollowed by 4 dayswith no treatmentminimum of 2 and aRCT, DB, MC, PCPatients 18 years of age andolder who wereimmunocompetent and hadat least 2 distinct externalanogenital wartsN=3268 weeks oftreatmentand 8 weekposttreatmentfollow-upPrimary:Total disappearanceof treated warts(treatment success)Secondary:Number of warts,wart surface area,individual wartassessment scores,physician assessmentof overall response(based on total areaof treated wartsremaining andAdverse reactions reported in the imiquimod group includeditching, redness, and irritation. Half of the patients reported fewor no side effects.Primary:Podofilox gel was significantly better than placebo at clearinganogenital and external genital warts after 4 and 8 weeks oftreatment (P
StudyandDrug Regimenmaximum of 8treatment cyclesStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsoverall severity ofdisease signscompared tobaseline), patientdiscontinuation dueto insufficientresponse, andrecurrence rate oftreated wartsResultsThe change on percentage of baseline wart area showed asignificant effect of podofilox gel at 4 and 8 weeks in theexternal and anogenital wart populations (P=0.001) and at 8weeks in patients with perianal warts (P=0.03).At 4 weeks, 41.5% of baseline number of anogenital wartstreated with podofilox remained, compared with 89.5% of wartsremaining in the vehicle group (P=0.001). At 8 weeks, 35.9%of baseline anogenital warts treated with podofilox remainedcompared to 88.4% of warts in the vehicle group (P=0.001).Physician assessment of improvement was significantly better at4 weeks in the podofilox group compared to the vehicle group(73.8% of patients had either moderate or marked improvementor complete clearance compared to 15.1% in the vehicle group,P=0.001). This trend continued at week 8 (81.1% of patients inthe podofilox group compared to 17.2% in the vehicle group,P=0.001).Overall, 61.1% of patients in the vehicle group discontinuedtherapy due to insufficient response compared with 8.6% ofpatients in the podofilox group (P=0.002). At week 4, 37% inthe vehicle group and 1.5% in the podofilox group haddiscontinued due to insufficient response (P value not reported).After treatment was completed, 30.9% of patients in thepodofilox group had recurrence of at least 1 wart within 12week, most occurring within the first 4 weeks. Theinvestigators were not able to compare this to the vehicle groupsince only 4 patients in this group had their warts clearcompletely during treatment.Greenberg et al. 66Podofilox 0.5%RCT, DB, PC, PGWomen 18 years of age andN=7210 weeksPrimary:Percentage of wartsthat were completelyData for individual wart assessment scores is not reported.Primary:There was a significant difference in the percentage of wartscleared in the podofilox groups compared to the vehicle group412Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug Regimensolution BID for 3days then 4 days offvs.podofilox 0.5% creamBID for 3 days then 4days offvs.placebo solution orcream BID for 3 daysthen 4 days offminimum of 2treatment cycles, couldbe extended to 4cycles if patients didnot respond to the first2Baker et al. 67Podofilox 0.5%solution BID for 3days then 4 days offfor minimum of 2treatment cycles andmaximum of 4treatment cyclesall patients receivedactive treatmentStudy DesignandDemographicsolder with a clinicaldiagnosis of exophyticvulvar condylomaSample Sizeand StudyDurationOLN=37Women 18-46 years of age 10 weekswith a diagnosis of externalanogenital warts involvingan area of less than 10 cm 2End Pointshealed at anytimeduring the study,investigators’ overallassessment oftreatment responseSecondary:Not reportedPrimary:Patients’ subjectiveresponse to treatment(pain, burning, anditching), physicians’objective evaluationof the area(inflammation,erosion, other), andthe number of wartsSecondary:Not reportedResultsat every week of the study (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsdecreased during treatment, as did physicians’ objective reportsof inflammation and erosion.Other objective observations by investigators occurred duringthe first 3 visits and included edema, odor, skin slough,tenderness, and stinging and no patients described these assevere. Over 80% of patients had none of these additionalobjective observations.Beutner et al. 68Podofilox 0.5%solution BID for 3days then 4 days offvs.placebo solution BIDfor 3 days then 4 daysoffminimum of 2treatment cycles andmaximum of 4treatment cyclesRCT, DB, PC, MCMen 18 years of age andolder with a diagnosis ofgenital wartsN=10916 weeksPrimary:Change in wartcount, change in wartarea, and number andpercentage ofpatients completelyclearedSecondary:Not reportedSecondary:Not reportedPrimary:At the end of the active treatment phase (week 4), 73.6% ofwarts in the podofilox group were cleared compared to 8.3% inthe placebo group and the total wart area was reduced by 82.3%in the podofilox group compared to 4.2% in the placebo groupon weeks 1-6 (P=0.0001 for each). Comparisons could not bemade at weeks 12 and 16 because there were no patients left inthe placebo group.At week 6, 82% of warts in the podofilox group had completelycleared and of these, 34% had some evidence of recurrencecompared to 13% of warts in the placebo group achievingcomplete clearance with 1 wart having evidence of recurrence(P value not reported).Overall, 44.6% of podofilox patients were completely clear atsome point in the study compared to 0 patients in the placebogroup (P
StudyandDrug RegimenKaposi’s SarcomaWalmsley et al. 69Alitretinoin 0.1% gelTID for the first 2weeks followed byQID for the remainderof the studyvs.placebo vehicleStudy DesignandDemographicsSample Sizeand StudyDurationRCT, DB, PC, MCN=268Patients 18 years of age and 12 weeksolder, positive diagnosis ofKaposi’s Sarcoma (KS)proven by biopsy, positivefor antibodies againsthuman immunodeficiencyvirus (HIV), minimum of 6accessible cutaneous KSlesions including at least 3raised lesions, each lesionpresent for 30 days orhaving a diameter of at least10 mm, Karnofskyperformance score of >60,bilirubin 700 cells/mm 3 , andplatelet count of >50,000cells/m 3End PointsPrimary:Patient’s cutaneousKS tumor responserate as evaluated bythe group of 6 indexlesions, responseswere categorized as aclinical completeresponse (CCR)defined as a decreasein lesion area to zero,partial response area(PRA) defined asdecrease in lesionarea by >50% frombaseline without aconcurrent increasein lesion height,partial responseheight (PRH) definedas completeflattening of a lesionthat was raised atbaseline without anincrease in lesionarea by >25% frombaseline, progressivedisease (PD) definedas an increase inlesion area by >25%from baseline orincrease in lesionheight from flat atbaseline to raised, orstable disease (SD)defined as a lesionResultsPrimary:CCR was observed in a significantly higher percentage ofpatients treated with alitretinoin 0.1% gel (35%) compared toplacebo vehicle (18%) (P=0.002). This statistically significantdifference was maintained when the results were adjusted forbaseline CD4+ counts and the number of raised lesions atbaseline (P=0.00185).The incidence of PD as a best response was lower in thealitretinoin group compared to the placebo vehicle group (Pvalue not reported).Reponses were analyzed based on age, race, aggregate area ofindex lesions, and Karnofsky performance scores and theresponse rate in the alitretinoin group remained significantlyhigher compared to the placebo vehicle (P=0.002, 0.002,0.0015, and 0.003 respectively).One hundred and eighty four patients received open labelalitretinoin treatment following the 12 week blinded phase and49% of these patients met the criteria for response and of thesepatients, 2 achieved complete response.Time to first response was significantly faster in the alitretinoingroup compared to the placebo vehicle group (P=0.0001).Overall response rates (CCR plus PR) was significantly higherin the alitretinoin group (28%) compared with the placebovehicle group (13%) (P=0.001).Treatment with placebo vehicle was associated with less lesionpain compared to treatment with alitretinoin (P=0.007).Secondary:Not reported415Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsthat did not meetevaluation criteria forCCR, PRA, PRH, orPDResultsBodsworth et al. 70Alitretinoin 0.1% gelBIDvs.vehicle gel BIDRCT, DB, PCPatients diagnosed withacquired immunodeficiencysyndrome (AIDS)- relatedKaposi’s Sarcoma (KS)N=13412 weeksSecondary:Not reportedPrimary:Cutaneous KS tumorresponse rateaccording to theAIDS <strong>Clinical</strong> TrialsGroup (ACTG)objective criteriaSecondary:Not reportedPrimary:The overall patient response was 37% in the alitretinoin groupcompared to 7% in the vehicle group (P=0.00003).The significant difference in response rates was sustained evenwhen potential confounding factors were taken into accountincluding age, Eastern Co-operative Oncology Group (ECOG)status, CD4+ cell count, history of opportunistic infection,aggregate area of indicator lesions, number of raised indicatorlesions, prior therapy for KS, and number of drugs used inconcomitant antiretroviral therapy (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsthis therapy toprevious therapiesSecondary:Not reportedResultsor good, 91.7% rated the treatment to be very well or welltolerated, and 95.8% rated the cosmetic acceptance to be verygood or good.Investigators rated calcipotriol solution to be more effectivethan past treatments in 45.1% of patients.Safety was rated as improved by 32.4% of patients compared topast treatments.Application of the product was rated easier by 36.8% ofpatients.Calcipotriol was rated cosmetically more acceptable thanprevious treatments by 45.1% of patients.There were no major differences between investigator andpatient global assessments (P value not reported).Reygagne et al. 72Calcipotriol 0.005%solution BIDvs.clobetasol 0.05%shampoo QDRCT, MC, SB, PGN=151Patients 12 years of age or 4 weeksolder with moderate tosevere scalp psoriasishaving a global severityscore (GSS) of at least 3 andan affected area of at least 2cm 2Primary:Global severity score(GSS) and the totalseverity score (TSS).The GSS is assessedon scale ranging from0 (none) to 5 (verysevere). The TSS isthe sum of the scoresof erythema,desquamation, andplaque thickening allassessed on a scoreof 0 (none) to 3(severe).Secondary:Not reportedPrimary:Clobetasol propionate was shown to be significantly moreefficacious compared to calcipotriol in TSS measures (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsVeronikis et al. 73Calcipotriene BIDvs.coal tar emulsion 1%BIDSB, CSPatients 18-75 years of agewith plaque-type psoriasisN=2012-125 daysSecondary:Pruritis, surface areaof scalp affected bypsoriasisPrimary:Erythema, scaling,and plaque thicknesswere evaluated usinga 4-point scale (0=nolesion, 2=mild,4=moderate,6=severe)Primary:The scores for erythema, scaling, and plaque thicknesssignificantly decreased in both the calcipotriene group and thecoal tar group (P50%reduction in ESI score) in 60% of patients on the calcipotriolside compared to 23.3% of patients on the coal tar side(P505reduction in ESI score) in 73.3% of patients on the calcipotriolside compared to 33.3% of patients on the coal tar side(P75% reductionin ESI score) in 26.6% of patients on the calcipotriol sidecompared to 0% of patients on the coal tar side (P value notreported).At 12 weeks, there was a marked improvement (>75% reductionin ESI score) in 53.3% of patients on the calcipotriol sidecompared to 33.3% of patients on the coal tar side (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResults86.7% of patients for both calcipotriol and coal tar (P value notreported).The median time for attaining a >50% reduction in ESI scorefor calcipotriol was 6.1+1.9 weeks and 9.6+1.8 weeks for coaltar (P0.05).There was no significant difference between the physician andpatient assessments of degree of improvement at any timeduring the study. There was a preference for calcipotriolointment for visual presentability, lack of staining, and cosmeticelegance compared to coal tar (P value not reported).Tosti et al. 75Calcipotriol 50 mcg/gointment BIDvs.betamethasone 64mg/g ointment andsalicylic acid 0.03 g/gointment BIDRCT, DBPatients 18 years of age andolder with a diagnosis ofnail bed psoriasis withsevere subungualhyperkeratosis (>1 mm forfingernails, >2.5 mm fortoenails)N=583 monthswith anoptionaladditional 2months oftreatmentforrespondersPrimary:Nail thicknessexpressed inmillimeters using amicrometer caliper,patient assessment ofacceptability oftreatment using 5-point scale (0=nil,1=poor, 2=fair,3=good, 4=excellent)Secondary:Not reportedSecondary:Not reportedPrimary:For fingernail psoriasis, subungual hyperkeratosis was reducedby 26.5% in the calcipotriol group and by 30.4% in thebetamethasone and salicylic acid group after 3 months and thedifference between groups was not significant (P value notreported). Eight patients in the calcipotriol group and 10patients in the betamethasone and salicylic acid group wereconsidered responders (>50% reduction in subungualhyperkeratosis in at least one nail).At 5 months, responders showed a 49.2% reduction inhyperkeratosis in the calcipotriol group and 51.7% reduction inthe betamethasone and salicylic acid group (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsthe differences between groups were not significant (P value notreported). Seven patients in the calcipotriol group wereconsidered responders and 12 in the betamethasone and salicylicacid group (>50% reduction in subungual hyperkeratosis in atleast one nail).At 5 months, there was a further reduction in hyperkeratosis inthe calcipotriol group (40.7%) and in the betamethasone andsalicylic acid group (51.9%) from baseline (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsSkin infiltration on the trunk disappeared in 30.0% ofcalcipotriol and betamethasone and salicylic acid patients, skininfiltration on the arms disappeared in 55.0% of calcipotriolpatients and 56.2% of betamethasone and salicylic acid patients,and infiltration on the legs disappeared in 42.5% of calcipotriolpatients and 36.3% of betamethasone and salicylic acid patients.These differences were significant compared to baseline(P
StudyandDrug RegimenSingh et al. 77Calcipotriene 0.005%ointment BID onweeks 2 and 4 andaugmentedbetamethasone 0.05%cream QD on weeks 1and 3 (experimentalgroup)vs.augmentedbetamethasone 0.05%cream QD for 4 weeks(control group)De Jong et al. 78Calcipotriol 50 mcg/gointment BID plusmethotrexate (MTX)vs.placebo vehicle plusMTXPhase I:Cessation of MTX andtreatment initiation ofblinded topicaltreatment with eithercalcipotriol or placeboStudy DesignandDemographicsRCT, SB, PGPatients 20-50 years of agewith stable plaque psoriasisfor more than 1 monthsdurationRCT, PC, MC, DB, PGPatients 18 years of age andolder with chronic plaquepsoriasis who had beentreated with MTX with orwithout topical treatmentduring the last 6 months andwhose psoriasis had beenstable for at least 3 monthsSample Sizeand StudyDurationN=524 weeksN=9854 weeksEnd PointsPrimary:Proportion of patientshaving at least 90%reduction in baselinePASI scores at theend of the 4 weekstudy periodSecondary:PASI scores on aweekly basis,percentage reductionin PASI scores after2 and 4 weeks oftreatment, proportionof patients withmarked improvementor who are almostcompletely cleared atthe end of treatmentPhase I:Relapse-free interval[relapse measured bythe modifiedpsoriasis severityscore (MPSS)]Phase II:MTX-sparing effectof calcipotriol(measured by thedose of MTXneeded)Phase III:Maintenance of thetarget MPSS onResultsPrimary:In the control group, 18.5% of patients had a 90% or greaterreduction in baseline PASI scores after 4 weeks of therapycompared with 68% of patients in the experimental group(P
StudyandDrug Regimenvehicle for total of 30weeks or until relapseoccursPhase II:MTX titration phasewith open MTXtreatment andcontinuation ofblinded topical therapyfor 18 weeks or untiltarget MPSS reachedStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointstopical treatment plusthe MTX dose usedat the end of phase II(measured by theoccurrence ofrelapse)ResultsMTX, 6.5 mg/week, than the vehicle group, who required 9.9mg/week of MTX (P=0.002).Investigator assessments of efficacy in the intent-to-treatpopulation showed a non-significant trend in favor ofcalcipotriol (P=0.068).Phase III:Follow-up phase forpatients reaching thetarget MPSS for amaximum of 6 weeksTorras et al. 79Calcipotriol cream 50mcg/g BID pluspsoralen plusultraviolet A (PUVA)3 times/weekvs.vehicle cream BIDplus PUVA 3times/weekRCT, MC, PC, PGPatients 18 years of age orolder with skin type II or IIIand a diagnosis of extensivepsoriasis vulgaris covering20-50% of body surfacearea (BSA), and who werescheduled to receive PUVAtherapy on the trunk and thelimbsPhase I:Two week washout periodduring which patientsreceived an emollient only,or a shorter wash out ifpatients had received noprevious treatment and didN=12012 weeksPrimary:Psoriasis area andseverity index (PASI)scores, overall patientassessment of skinlesions, and the totalUVA dosage neededSecondary:Not reportedPrimary:Statistically significant decreases in PASI scores were observedform week 2 to week 10 with the decrease being greater in thecalcipotriol group (P
StudyandDrug RegimenTzung et al. 80Tazarotene 0.1% gelQHS plus petrolatumQAMvs.calcipotriol 0.005%ointment BIDStudy DesignandDemographicsnot need the full 2 weeksPhase II:Patients received eithercalcipotriol 50 mcg/g orvehicle BID for at least 10weeksPhase III:Within 1 week ofrandomization, patientsreceived PUVA therapy 3times per week in additionto topical therapy(methopsoralen wasadministered 2 hours priorto UVA treatment)RETRO, IB, CSPatients 12-80 years of agewith a diagnosis of psoriasisand a total of 50 targetlesion pairsSample Sizeand StudyDurationN=1912 weeks oftreatmentand 4 weeksof posttreatmentevaluationEnd PointsPrimary:Severity scores forscaling, plaqueelevation, erythema,overall lesionseverity, and patientself-reported efficacySecondary:Not reportedResultswas rated moderately improved or totally cleared in 79.3% ofpatients in the calcipotriol group compared to 60% of patients inthe vehicle group (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsdifference was not significant (P>0.46).Guenther et al. 81Tazarotene 0.1% gelQHS plus mometasone0.1% cream QAMvs.calcipotriene 0.005%BIDMC, IB, PGAdult patients with chronic,stable plaque psoriasisaffecting 5%-20% of totalbody surface areaN=1208 weeks oftreatmentwith 12week posttreatmentfollow-upphasePrimary:Physician-ratedmeasures of efficacyincluding globalimprovement, plaqueelevation, scaling,erythema, andpercentage of bodysurface areainvolvement; patientratedassessmentsincluding efficacy ofstudy treatmentcompared withprevious therapies,comfort of treatedskin, outlook forlong-term control,and overallimpression oftreatmentSecondary:Not reportedPrimary:Physician-rated assessments:After 2 weeks of treatment, the percentage of patients achievingmarked improvement (>75% global improvement) wassignificantly higher in the tazarotene and corticosteroid groupcompared to the calcipotriene group (45% and 25%respectively, P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsgroup compared to the calcipotriene group at week 4 oftreatment and at the end of treatment (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsNo significant between-group differences were observed in thepercentage of patients who rated their outlook for long-termcontrol as very promising or extremely promising at the end ofthe 12 week post-treatment phase (P values not reported).Overall impression of treatment favored the tazarotene pluscorticosteroid regimen compared to the calcipotriene regimen(P value not reported), however the percentages of patients whorated their impression of therapy as favorable or highlyfavorable did not differ between groups, except at the 12-weekpost-treatment visit (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsclobetasol side. Adverse effects in the tazarotene pluscalcipotriene side were mild and did not result in alteration ofthe treatment schedule for any patient.Schiener et al. 83Tazarotene 0.05% gelQD plus total bodynarrowband ultravioletB (UVB) irradiationQD 4 times per weekIB, CSPatients with widespreadsymmetrical psoriasisN=10Minimumduration of4 weeksPrimary:Psoriasis Area andSeverity Index(PASI)Secondary:Not reportedSecondary:Not reportedPrimary:PASI scores decreased on both treatment sides and there was nosignificant difference between treatment regimens (P value notreported).Complete clearance of the skin was observed after a median of19 treatment sessions for both treatment regimens.vs.calcipotriene 0.005%ointment QD plus totalbody narrowbandultraviolet B (UVB)irradiation QD 4 timesper weekSecondary:Not reportedboth treatments wereused in each patient onopposite sides of thebodyWound CareWieman et al. 84Becaplermin gel 30mcg or 100 mcgvs.good ulcer careMAPatients 19 years of age andolder, type I or II diabeteswith at least 1 but no morethan 3 lower extremitydiabetic neuropathic ulcersthat extended into thesubcutaneous tissue orN=92220 weeks oruntilcompleteulcerhealing wasachievedPrimary:Incidence ofcomplete woundhealing defined asulcers withoutdraining and with nodressing requiredSecondary:Primary:In Study 1, the incidence of complete healing was significantlyhigher in the becaplermin group compared to the placebo group(P=0.02).In study 2, the incidence of complete healing was 50% in thebecaplermin 100 mcg group, 36% in the becaplermin 30 mcggroup, and 35% in the placebo group and was only significantwhen comparing the 100 mcg group to placebo (P=0.01).428Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
vs.StudyandDrug Regimenplacebo gelin study 1 patientsreceived placebo orbecaplermin 30 mcggel, in study 2 patientsreceived becaplermin30 mcg, 100 mcg, orplacebo, in study 3patients receivedbecaplermin 100 mcg,placebo, or good ulcercare (undefined), andin study 4 patientsreceived becaplermin30 mcg or 100 mcgEmbil et al. 85Becaplermin 100 mcgQDall patients receivedactive treatmentStudy DesignandDemographicsbeyond (stages III and IV asdefined in the InternationalAssociation of EnterostomalTherapy guide to chronicwound staging)OL, MCPatients 18 years of age andolder with type I or IIdiabetes, having at least 1but no more than 2 fullthickness (stage III or IV asdefined by the NationalPressure Ulcer AdvisoryPanel staging system)neuropathic ulcers of thelower extremitiesSample Sizeand StudyDurationN=13420 weeks oruntilcompletewoundhealingEnd PointsTime to completehealing (study 2only)Primary:Percentage ofpatients achievingcomplete woundclosure within the 20week treatmentperiodSecondary:Time to achievecomplete closure,percentage reductionin ulcer area at eachvisit, and rate oftarget ulcerrecurrence during the6-month periodfollowing healingResultsIn study 3, the incidence of complete healing was 44% in thebecaplermin 100 mcg group, 36% in the placebo group, and22% in the good ulcer care group. This study was designed tocompare good ulcer care to placebo vehicle and included asmall group of patients receiving becaplermin 100 mcg (N=34).The becaplermin group was not powered for statisticalcomparison.In study 4, the incidence of complete healing was 36% in thebecaplermin group and 32% in the placebo group and was notstatistically significant (P value not reported).Secondary:In study 2, the time needed to achieve complete healing wasapproximately 85 days.Primary:Complete healing was achieved in 57.5% of patients.Secondary:Complete closure was achieved in a mean of 63 days in thosepatients achieving complete healing.The percentage of patients achieving >50% reduction in ulcerarea at week 8 achieved a complete closure at the study end,compared to 13% of patients whose ulcer decreased by
StudyandDrug RegimenAlvarez et al. 86Collagenase ointmentQD until completedebridement or 4weeksvs.papain-urea ointmentQD until completedebridement or 4weeksStudy DesignandDemographicsRCT, PRO, PG, MC, OLNursing home residentswith a diagnosis of pressureulcer(s)Sample Sizeand StudyDurationN=282 weeks tostabilize thewound, thenanevaluationperiod of4 weeksEnd PointsPrimary:Nonviable, necrotictissue reductionassessed weekly,amount of nonviabletissue, degree ofwound granulation,and overall woundresponse all assessedweeklySecondary:Not reportedResultsPrimary:The papain-urea ointment was significantly more effective inreducing the amount of non-viable, necrotic tissue at eachevaluation compared to the collagenase ointment (P
Additional EvidenceDose SimplificationA literature search of Medline and Ovid did not reveal data pertinent to this topic.Stable TherapyA literature search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician VisitsA literature search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 9. Relative Cost of the Single Entity Skin and Mucous Membrane Agents, MiscellaneousGeneric Name(s) Formulation(s) Example Brand Brand Cost GenericName(s)Costacemannan suspension Salicept ® $ N/Aalitretinoin gel Panretin ® $$$$$ N/Abecaplermin gel Regranex ® $$$$$ N/Abexarotene gel Targretin ® $$$$$ N/Acalcipotrienecream, ointment, Dovonex ® $$$$ N/Asolutionchloroxine shampoo Capitrol ® $ N/Acollagenase ointment Santyl ® $$$$ N/Adiclofenac gel Solaraze ® $$$$ N/Afluorouraciladhesive bandage, Carac ® , Efudex ® *, $$$$ $$cream, solution Fluoroplex ®imiquimod packet Aldara ® $$$$ N/Apimecrolimus cream Elidel ® $$$$ N/Apodofilox gel, solution Condylox ® * $$$$ $$$podophyllum resin solution Podocon-25 ® $$$ N/Atacrolimus ointment Protopic ® $$$$ N/A431Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
Generic Name(s) Formulation(s) Example BrandName(s)Brand Cost GenericCosttazarotene cream, gel Tazorac ® $$$$ N/A*Generic is available in at least one dosage form or strength.N/A=not availableX. ConclusionsThe single entity miscellaneous skin and mucous membrane agents are a diverse group of products withmany different indications. Important considerations for their potential designation as preferred agents aresummarized below, grouped by indication. It is important to keep in mind that the medications within thisclass that share the same indications often have different mechanisms of action, or are recommended foruse in different circumstances. For that reason, a direct comparison between similarly-indicated productsmay not always give a complete picture of their effectiveness profiles.Actinic keratosisThree agents in this review are FDA approved for the treatment of actinic keratosis (AK): diclofenac,fluorouracil, and imiquimod. They are available as diclofenac sodium gel (Solaraze ® ), fluorouracil cream(0.5%, 1%, and 5%), fluorouracil solution (2% and 5%), and imiquimod 5% cream. Trials of diclofenacgel in the treatment of actinic keratosis showed approximately 41-50% of patients attaining 100% lesionclearance after treatment. In these diclofenac trials, lesion clearance measurement was based on targetlesion number score (TLNS) and cumulative lesion number score (CLNS), not on direct lesion counts. 37-38For fluorouracil there are relatively few clinical trials comparing its different dosage forms as this is anolder product and clinical trial data is lacking. Newer strengths and formulations of fluorouracil like the0.5% cream (Carac ® ) were included in several efficacy studies in patients with actinic keratoses, wherethey were compared to both placebo and the 5% cream commercially available as Efudex ® . These studiesshow comparable efficacy between the 5% cream and the 0.5% cream in reducing the number andpercentage of AK lesions compared to baseline values, though some of them suggest better tolerability ofthe 0.5% formulation. The study by Loven et al did not show a significant difference between the twoformulations, with total clearance of AK lesions occurring at the same rate (43%) in a group of patientswho used both formulations simultaneously, the 0.5% cream on one side of the face and the 5% cream onthe other side. A higher proportion of patients preferred the 0.5% cream (85% vs. 15%). 40 This study alsoobserved no significant difference in the incidence of burning, erosion, pruritis, pain, or edema between thetwo treatments, though a lower cumulative proportion of patients reported these symptoms in the 0.5%group and a significantly greater portion of patients expressed a willingness to re-treat with the 0.5% cream(P=0.031). 40 Another study by Jorizzo et al. showed that 30% of patients who were treated withfluorouracil 0.5% cream and cryosurgery (for lesions remaining after a 4-week follow-up period aftertreatment with fluorouracil) were clear of AK lesions six months after initial treatment. 39Another drug used to treat actinic keratosis is imiquimod. Lebwohl et al demonstrated a complete AKlesion clearance rate of 45.1% of patients treated with imiquimod 5% cream and Korman et al.demonstrated a complete AK lesion clearance rate of 48.3%. 42,46 These percentages are comparable to thecomplete clearance rate of 43% observed in the previously-discussed trial by Loven. 40 Recurrence rates ofAK lesions in patients treated with imiquimod and followed for 1-2 years were also reported in clinicaltrials and ranged from approximately 10-25% according to trials conducted by Stockfleth and Lee. 43-45It is difficult to make direct comparisons of these agents for the treatment of actinic keratosis based on thelack of head-to-head trials for this indication. While clearance rates reported in the trials by Loven,Lebwohl, and Korman appear to be comparable, it is difficult to directly compare the efficacy of theseagents since patient populations and treatment durations differed between the studies. Overall, therapeuticdecisions in the treatment of actinic keratosis should be based on clinical guidelines, adverse effects, andtolerability of each agent.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.432
Atopic dermatitisThe two topical calcineurin inhibitors, pimecrolimus and tacrolimus that are FDA-approved for thetreatment of atopic dermatitis are discussed in this review. They are available as pimecrolimus 1% cream(Elidel ® ) and tacrolimus 0.03% and 0.1% ointment (Protopic ® ). Current guidelines for the treatment ofatopic dermatitis recommend the use of topical corticosteroids as first line treatment and recommend theuse of topical pimecrolimus or tacrolimus in those patients intolerant or unresponsive to corticosteroids orin whom corticosteroids are contraindicated. 6-8 Recent concerns regarding the long-term safety of theseagents have been addressed in the guidelines and position papers outlined in this review. As of December2004, the FDA received 19 reports of cancer-related adverse events linked with Protopic ® use (3 cases inpediatric patients
United Kingdom (U.K.) Cutaneous Lymphoma Group, topical bexarotene is typically reserved for patientswith stage I mycosis fungoides (CTCL) not responding to or intolerant to other topical therapies. 11 It hasbeen shown to be effective in an open label trial evaluating its use in patients who have failed othertherapies. 61 Currently, it is not used as a first-line agent.Genital wartsFour products reviewed in this class are FDA approved for the treatment of external genital warts; theseinclude imiquimod 5% cream, podofilox 0.5% gel and solution, and podophyllum resin. It is important tonote that no clinical trials evaluating the use of podophyllum resin in the treatment of genital warts werefound and product labeling limits the use of this product to application by a health-care provider. This isnot a patient-administered treatment. Imiquimod is currently a brand-name product marketed as Aldara ® ,while podofilox is available generically as a solution and as a brand name product in the gel formulation.One study that is represented in this review evaluated the head-to-head effectiveness of the cream and gelformulations of these products in infants and young children with anogenital warts. This study did notdemonstrate better efficacy of one product compared to the other. Of the 17 patients treated withpodofilox, parents of 15 of the patients reported clearance of the warts, with no recurrence, for periodsranging from 4 months to 2 years. Of the 8 patients treated with imiquimod, parents of 6 of the patientsreported clearing of lesions with no recurrence in 6-12 months. 64 In other vehicle-controlled or open-labeltrials presented in this review, imiquimod demonstrated total clearance rates of 69.7%-71%. 62-63 One ofthese studies, by Arican et al., evaluated both male and female patients. Of the female patients, 100%reported total wart clearance after treatment. 62A study by Tyring et al evaluating total wart clearance in patients treated with podofilox gel versus vehiclegel showed complete clearance in 38.4% of patients after 4 weeks of therapy, and in 44.6% of patients after8 weeks of therapy. 65 No difference was observed between male and female patients with respect tocomplete clearance rates. While these percentages are not as high as those previously discussed in theimiquimod trials, this study had a much larger sample size (n=326). Other secondary endpoints includingwart count, wart surface area, wart assessment scores, and patient and physician assessment of treatmentwere evaluated and showed significant advantages of podofilox over placebo. 65With limited head to head studies of podofilox and imiquimod for genital wart treatment, and with thevariability in primary outcomes in placebo-controlled trials, it is difficult to conclude that one product ismore efficacious than the other, though both show efficacy compared to placebo. Current treatmentguidelines do not identify one product as more efficacious than the other and state that there is not onespecific treatment appropriate for all patients. 5Kaposi’s SarcomaThere is one product included in this review that is used for the treatment of cutaneous lesions associatedwith Kaposi’s Sarcoma (KS). Alitretinoin has been proven to be effective in treating Kaposi’s Sarcoma inplacebo-controlled trials. 69-70 Alitretinoin is used for the treatment of cutaneous lesions only and should notbe used when systemic anti-KS therapy is required (i.e., >10 new KS lesions in the past month,symptomatic lymphedema, symptomatic pulmonary KS, or symptomatic visceral involvement). 14PsoriasisFor the treatment of psoriasis, there are two FDA-approved agents evaluated in this review, calcipotriene(Dovonex ® ) and tazarotene (Tazorac ® ). Several head-to-head studies evaluating the efficacy ofcalcipotriene and tazarotene are represented in this review. Overall, no significant differences were80-81, 83observed between the two medications. Current treatment guidelines recommend the use of theseproducts in patients with psoriasis either as monotherapy or in combination with topical corticosteroids;however, topical corticosteroids remain the primary therapeutic option in this disease state. These agentsare typically reserved for patients intolerant to or unresponsive to topical corticosteroids, or for whomtopical corticosteroids are contraindicated. 9,10Wound treatmentTwo products included in this review have various applications in the treatment of wounds. Collagenase isindicated for enzymatic debridement, but there are few studies available evaluating its use. One study byPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.434
Alvarez et al. compared the efficacy of collagenase and papain-urea in patients with pressure ulcers. Thepapain-urea ointment was significantly more effective in reducing the amount of non-viable, necrotic tissueat each evaluation compared to the collagenase ointment and generally enhanced the level of granulationand epithelialization, though the degree of epithelialization did not correlate to a reduction in wound areaand significant conclusions can not be made as a result of this study. 86 Current treatment guidelinesrecommend surgical (sharp) debridement over enzymatic debridement according to the literatureavailable. 1-3Becaplermin is a recombinant human platelet derived growth factor indicated for the treatment of lowerextremity diabetic neuropathic ulcers that extend into the subcutaneous tissue or beyond and have anadequate blood supply. It has shown benefits in clinical trials in enhancing the incidence of completewound healing compared to placebo or good ulcer care alone. A study by Wieman et al. described theresults of 4 clinical trials of becaplermin and demonstrated a significantly higher incidence of completehealing in the patients receiving becaplermin 30 mcg and/or 100 mcg gel in two studies (note- only the 100mcg gel is commercially available). 84 The other two studies either showed no significant differencebetween active treatment group and placebo or good ulcer care or were not powered to detect a differencebetween becaplermin and standard care. 84 A study by Embil et al. showed that complete healing of ulcerswas achieved in 57.5% of patients receiving becaplermin 100 mcg gel. 85 All patients in this study receivedactive treatment. Current treatment guidelines from the American Diabetes Association ConsensusDevelopment Conference on Diabetic Foot Wound Care states that recombinant platelet derived growthfactor has shown modest benefit when used with off-loading, debridement, and treatment of infection butshould not be a substitute for appropriate wound care. 2 Other treatment guidelines do not address the use ofthis agent. 1,3At this time, there is not a role for single entity miscellaneous skin and mucous membrane agents in generaluse. Because these agents have narrow indications with limited usage, they should be available for specialneeds/circumstances that require medical justification through the prior authorization process. Afterclinical circumstances are explored, proper medical justification will provide patient access to these agents.There is insufficient data to support that one brand single entity miscellaneous skin and mucous membraneagent is safer or more efficacious than another. Therefore, all brand products within the class reviewed arecomparable to each other and to the generics and over-the-counter products in this class and offer nosignificant clinical advantage over other alternatives in general use.XI.RecommendationsNo brand single entity miscellaneous skin and mucous membrane agent is recommended for preferredstatus. Alabama Medicaid should accept cost proposals from manufacturers to determine cost effectiveproducts and possibly designate one or more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.435
References1. Lipsky B, Berendt A, Deery H, et al. Diagnosis and treatment of diabetic foot infections. Clin Infect Dis..2004;39:885-910.2. Consensus Development Conference on Diabetic Foot Wound Care: 7-8 April 1999,Boston, Massachusetts.American Diabetes Association. Diabetes Care. 1999 Aug;22(8):1354-1360.3. Stevens DL, Bisno AL, Chambers HF, Everett ED, Dellinger P, Goldstein EJ, Gorbach SL, Hirschmann JV,Kaplan EL, Montoya JG, Wade JC; Infectious Diseases Society of America. Practice guidelines for thediagnosis and management of skin and soft-tissue infections. Clin Infect Dis. 2005;41:1373-1406.4. Drake LA, Ceilley RI, Cornelison RL, et al. Guidelines of care for actinic keratoses. J Am Acad Dermatol.1995;32(1):95-98.5. Centers for Disease Control and Prevention. Genital warts. In: Centers for Disease Control and Prevention.Sexually Transmitted Diseases Treatment Guidelines, 2006. MMWR 2006;55(No. RR-11):1-100. Available at:http://www.cdc.gov/std/treatment/2006/genital-warts.htm. Accessed October 10, 2006.6. Hanifin J, Cooper K, Ho V, et al. Guidelines of care for atopic dermatitis. J Am Acad Dermatol.2004;50(3):391-404.7. Primary Care Dermatology Society and the British Association of Dermatologists. Guidelines for themanagement of atopic eczema. Available at: http://www.pcds.org.uk/pdf/PCDSBAD-Eczema.pdf AccessedOctober 10, 2006.8. Darsow U, Lubbe J, Taieb A, et al. Position paper on diagnosis and treatment of atopic dermatitis. J Eur AcadDermatol Venereol. 2005;19:286-295.9. Pardasani A, Feldman S, Clark A. Treatment of psoriasis: an algorithm-based approach for primary carephysicians. Am Fam Physician. 2000;61(3):725-740.10. British Association of Dermatologists. Psoriasis Guideline 2006.http://www.bad.org.uk/healthcare/guidelines/psoriasis.asp. Accessed October 10, 2006.11. Whittaker S, Marsden J, Spittle M, Jones R. Joint British Association of Dermatologists and U.K. CutaneousLymphoma Group guidelines for the management of primary cutaneous T-cell lymphomas. Br J Dermatol.2003;149(6):1095-1107.12. National Comprehensive Cancer Network (NCCN) Guidelines. Available athttp://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf. Accessed September 26, 2006.13. Telfer N, Clover G, Bowers P. Guidelines for the management of basal cell carcinoma. Br J Dermatol.1999;141:415-423.14. Panretin ® [package insert]. San Diego, CA: Ligand Pharmaceuticals, Inc.; 1999.15. Regranex ® [package insert]. Raritan, NJ: Ortho-McNeil Pharmaceutical, Inc.; May 2005.16. Targretin ® [package insert]. San Diego, CA: Ligand Pharmaceutical, Inc; 1999.17. Dovonex ® [package insert]. Rockaway, NJ: Warner Chilcott, Inc.; Jan 2006.18. Santyl ® [package insert]. Columbus, OH: Abbott Laboratories Inc.; July 2003.19. Solaraze TM [package insert]. Fairfield, NJ: Bradley Pharmaceuticals, Inc.; 2000.20. Carac ® [package insert]. Berwyn, PA: Dermik Laboratories, Inc.; December 2003.21. Efudex ® [package insert]. Costa Mesa, CA: Valeant Pharmaceuticals; September 2005.22. Fuoroplex ® [package insert]. Irvine, CA: Allergan, Inc.; 2003.23. Lazerformaldehyde ® [package insert]. Farmingdale, NY: Pedinol Pharmaceuticals; 2003.24. Aldara ® [package insert]. St. Paul, MN: 3M Pharmaceuticals; August 2005.25. Elidel ® [package insert]. East Hanover, NJ: Novartis; July 2004.26. Podofilox ® [package insert]. Corona, CA: Watson Laboratories; January 2003.27. Podocon-25 ® [package insert]. Minneapolis, MN: Paddock Laboratories; 2005.28. Protopic ® [package insert]. Deerfield, IL: Astellas Pharma; April 2005.29. Tazorac ® [package insert]. Irvine, CA: Allergan, Inc.; January 2004.30. Tatro DS, ed. Drug Interaction Facts. St. Louis, Mo: Wolters Kluwer Health, Inc.; 2006.31. FDA Alert for Healthcare Professionals: Tacrolimus (marketed as Protopic) Available from:www.fda.gov/CDER/Drug/Inforsheets/HCP/ProtopicHCP/PDF Accessed on 03/17/0532. FDA Alert for Healthcare Professionals: Pimecrolimus (marketed as Elidel) Available from:www.fda.gov/CDER/Drug/Inforsheets/HCP/ElidelHCP/PDF Accessed on 03/17/0533. FDA Public Health Advisory; Elidel (pimecrolimus) Cream and Protopic (tacrolimus) Ointment. Availablefrom: www.fda.gov/CDER/Drug/advisory/elidel_protopic.htm Accessed on 03/14/05Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.436
34. FDA News: FDA Approves Updated Labeling with Boxed Warning and Medication Guide for Two EczemaDrugs, Elidel and Protopic. Available from: http://www.fda.gov/bbs/topics/news/2006/NEW01299.htmlAccessed on: 07/12/0635. Fonacier L, Spergel J, Charlesworth E, et al. Report of the topical calcineurin inhibitor task force of theAmerican college of allergy, asthma, and immunology and the American academy of allergy, asthma, andimmunology. J Allergy Clin Immunol. 2005;115(6):1249-1253.36. Ring J, Barker J, Behrendt H, et al. <strong>Review</strong> of the potential photo-carcinogenicity of topical calcineurininhibitors: position statement of the European dermatology forum. J Eur Acad Dermatol Venereol.2005;19:663-671.37. Nelson C, Rigel D, Smith S, Swanson N, Wolf J. Phase IV, open-label assessment of the treatment of actinickeratosis with a 3.0% diclofenac sodium topical gel (Solaraze TM ). J Drugs Dermatol. 2004;3(4):401-407.38. Wolf J, Taylor R, Tschen E, Kang S. Topical 3.0% diclofenac in 2.5% hyaluronan gel in the treatment of actinickeratoses. Int J Dermatol. 2001;40:709-713.39. Jorizzo J, Stewart D, Bucko A, et al. Randomized trial evaluating a new 0.5% fluorouracil formulationdemonstrates efficacy after 1-, 2-, or 4-week treatment in patients with actinic keratosis. Cutis. 2002;70:335-339.40. Loven K, Stein L, Furst K, Levy S. Evaluation of the efficacy and tolerability of 0.5% fluorouracil cream and5% fluorouracil cream applied to each side of the face in patients with actinic keratosis. Clin Ther.2002;24(6):990-1000.41. Jorizzo J, Weiss J, Furst K, VandePil C, Levy S. Effect of a 1-week treatment with 0.5% topical fluorouracil onoccurrence of actinic keratosis after cryosurgery: a randomized, vehicle-controlled clinical trial. Arch Dermatol.2004;140:813-816.42. Lebwohl M, Dinehart S, Whiting D, et al. Imiquimod 5% cream for the treatment of actinic keratosis: resultsfrom two phase III, randomized, double-blind, parallel group, vehicle-controlled trials. J Am Acad Dermatol.2004;50(5):714-721.43. Stockfleth E, Meyer T, Benninghoff B, et al. A randomized, double-blind, vehicle-controlled study to assess 5%imiquimod cream for the treatment of multiple actinic keratoses. Arch Dermatol. 2002;138:1498-1502.44. Stockfleth E, Christophers E, Benninghoff B, Sterry W. Low incidence of new actinic keratoses after topical 5%imiquimod cream treatment: a long-term follow-up study. Arch Dermatol. 2004;140:1542.45. Lee P, Harwell W, Loven K, et al. Long-term clinical outcomes following treatment of actinic keratosis withimiquimod 5% cream. Dermatol Surg. 2005;31(6):659-663.46. Korman N, May R, Ling M, et al. Dosing with 5% imiquimod cream 3 times per week for the treatment ofactinic keratosis: results of two phase 3, randomized, double-blind, parallel-group, vehicle-controlled trials.Arch Dermatol. 2005;141:467-473.47. Kapp A, Papp K, Bingham A, et al. Long-term management of atopic dermatitis in infants with topicalpimecrolimus, a non-steroid anti-inflammatory drug. J Allerg Clin Immunol. 2002;110(2):277-284.48. Papp K, Werfel T, Folster-Holst R, Ortonne J, et al. Long-term control of atopic dermatitis with pimecrolimuscream 1% in infants and young children: a two-year study. J Am Acad Dermatol. 2005;52(2):240-246.49. Staab D, Kaufman S, Brautigam M. Treatment of infants with atopic eczema with pimecrolimus cream 1%improves parents’ quality of life: a multicenter, randomized trial. Pediatr Allergy Immunol. 2005;16:527-533.50. Kaufman R, Bieber T, Helgesen A, et al. Onset of pruritis relief with pimecrolimus cream 1% in adult patientswith atopic dermatitis: a randomized trial. Allergy. 2006;61:375-381.51. Kempers S, Boguniewicz M, Carter E, et al. A randomized investigator-blinded study comparing pimecrolimuscream 1% with tacrolimus ointment 0.03% in the treatment of pediatric patients with moderate atopicdermatitis. J Am Acad Dermatol. 2004;51(4):515-525.52. Ashcroft D, Dimmock P, Garside R, Stein K, Williams H. Efficacy and tolerability of topical pimecrolimus andtacrolimus in the treatment of atopic dermatitis: a meta-analysis of randomized controlled trials. BMJ.2005;330(7490):516-524.53. Reitamo S, Ortonne J, Sand C, et al. A multicentre, randomized, double-blind, controlled study of long-termtreatment with 0.1% tacrolimus ointment in adults with moderate to severe atopic dermatitis. Br J Dermatol.2005;152:1282-1289.54. Paller A, Lebwohl M, Fleischer A, et al. Tacrolimus ointment is more effective than pimecrolimus cream with asimilar safety profile in the treatment of atopic dermatitis: results from 3 randomized, comparative studies. JAm Acad Dermatol. 2005;52(5):810-822.55. Romagosa R, Saap L, Givens M, et al. A pilot study to evaluate the treatment of basal cell carcinoma with 5-fluorouracil using phosphatidyl choline as a transepidermal carrier. Dermatol Surg. 2000;26(4):338-340.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.437
56. Marks R, Owens M, Walters S. Efficacy and safety of 5% imiquimod cream in treating patients with multiplesuperficial basal cell carcinomas. Arch Dermatol. 2004;140:1284-1285.57. Gollnick H, Barona C, Frank R, et al. Recurrence rate of superficial basal cell carcinoma following successfultreatment with imiquimod 5% cream: interim 2-year results from an ongoing 5-year follow-up study in Europe.Eur J Dermatol. 2005;15(5):374-381.58. Peris K, Campione E, Micantonio T, et al. Imiquimod treatment of superficial and nodular basal cell carcinoma:12-week open-label trial. Dermatol Surg. 2005:31(3):318-323.59. Geisse J, Caro I, Lindholm J, et al. Imiquimod 5% cream for the treatment of superficial basal cell carcinoma:results from two phase III, randomized, vehicle-controlled studies. J Am Acad Dermatol. 2004;50(5):722-733.60. Schulze H, Cribier B, Requena L, et al. Imiquimod 5% cream for the treatment of superficial basal cellcarcinoma: results from a randomized vehicle-controlled phase III study in Europe. Br J Dermatol.2005;152:939-947.61. Heald P, Mehlmauer M, Martin A, et al. Topical bexarotene therapy for patients with refractory or persistentearly-stage cutaneous T-cell lymphoma: results of the phase III clinical trial. J Am Acad Dermatol.2003;49(5):801-815.62. Arican O, Guneri F, Bilgic K, Karaoglu A. Topical imiquimod 5% cream in external anogenital warts: arandomized, double-blind, placebo-controlled study. J Dermatol. 2004;31(8):627-631.63. Haidopolous D, Diakomanolis E, Rodolakis A, et al. Safety and efficacy of locally applied imiquimod cream5% for the treatment of condylomata acuminate of the vulva. Arch Gynecol Obstet. 2004;270:240-243.64. Moresi J, Herbert C, Cohen B. Treatment of anogenital warts in children with topical 0.05% podofilox gel and5% imiquimod cream. Pediatric Dermatol. 2001;18(5):448-452.65. Tyring S, Edwards L, Cherry L, et al. Safety and efficacy of 0.5% podofilox gel in the treatment of anogenitalwarts. Arch Dermatol. 1998;134(1):33-38.66. Greenberg M, Rutledge L, Reid R, et al. A double-blind, randomized trial of 0.5% podofilox and placebo for thetreatment of genital warts in women. Obstet Gynecol. 1991;77(5):735-739.67. Baker D, Douglas J, Buntin D, et al. Topical podofilox for the treatment of condylomata acuminate in women.Obstet Gynecol. 1990;76(4):656-659.68. Beutner K, Conant M, Friedman-Kien A, et al. Patient-applied podofilox for treatment of genital warts. Lancet.1989;1(8642):831-834.69. Walmsley S, Northfelt D, Melosky B, et al. Treatment of AIDS-related Kaposi’s Sarcoma with topicalalitretinoin (9-cis-retinoic acid) gel. J Acquir Immune Defic Syndr. 1999;22(3):235-253.70. Bodsworth N, Bloch M, Bower M, et al. Phase III vehicle-controlled, multi-centered study of topical alitretinoingel 0.1% in cutaneous AIDS-related Kaposi ’s sarcoma. Am J Clin Dermatol. 2001;2(2):77-78.71. Thaci D, Daiber W, Boehncke W, et al. Calcipotriol solution for the treatment of scalp psoriasis: evaluation ofefficacy, safety, and acceptance in 3,396 patients. Dermatology. 2001;203:153-156.72. Reygagne P, Mrowietz U, Decroix J, et al. Clobetasol propionate shampoo 0.05% and calcipotriol solution0.005%: a randomized comparison of efficacy and safety in subjects with scalp psoriasis. J DermatologicTreatment. 2005;16:31-36.73. Veronikis I, Malabanan A, Holick M. Comparison of calcipotriene (Dovonex) with a coal tar emulsion (Exorex)in treating psoriasis in adults: a pilot study. Arch Dermatol. 1999;135(4):474-475.74. Sharma V, Kaur I, Kumar B, et al. Calcipotriol versus coal tar: a prospective randomized study in stable plaquepsoriasis. Int J Dermatol. 2003;42:834-838.75. Tosti A, Piraccini B, Cameli N, et al. Calcipotriol ointment in nail psoriasis: a controlled double-blindcomparison with betamethasone dipropionate and salicylic acid. Br J Dermatol. 1998;139:655-659.76. Crosti C, Finzi A, Mian E, Scarpa C, et al. Calcipotriol in psoriasis vulgaris: a controlled trial comparingbetamethasone dipropionate and salicylic acid. Int J Dermatol. 1997;36:537-541.77. Singh S, Reddy D, Pandey S. Topical therapy for psoriasis with the use of augmented betamethasone andcalcipotriene on alternate weeks. J Am Acad Dermatol. 2000;43(1):61-65.78. De Jong E, Mork N, Seijger M, et al. The combination of calcipotriol and methotrexate compared withmethotrexate and vehicle in psoriasis: results of a multicentre placebo-controlled randomized trial. Br JDermatol. 2003;148:318-325.79. Torras H, Aliaga A, Lopez-Estebaranz J, et al. A combination therapy of calcipotriol cream and PUVA reducesthe UVA dose and improves the response of psoriasis vulgaris. J Dermatol Treat. 2004;15:98-103.80. Tzung T, Wu J, Hsu N, Chen Y, Ger L. Comparison of tazarotene 0.1% gel plus petrolatum once daily versuscalcipotriol 0.005% ointment twice daily in the treatment of plaque psoriasis. Acta Derm Venereol.2005;85:236-239.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.438
81. Guenther L, Poulin Y, Pariser D. A comparison of tazarotene 0.1% gel once daily plus mometasone furoate0.1% cream once daily versus calcipotriene 0.005% ointment twice daily in the treatment of plaque psoriasis.2000;22(10):1225-1238.82. Bowman P, Maloney J, Koo J. Combination of calcipotriene (Dovonex) ointment and tazarotene (Tazorac) gelversus clobetasol ointment in the treatment of plaque psoriasis: a pilot study. J Am Acad Dermatol.2002;46(6):907-913.83. Schiener R, Behrens-Williams S, Pillekamp H, et al. Calcipotriol vs. tazarotene as combination therapy withnarrowband ultraviolet B (311 nm): efficacy in patients with severe psoriasis. Br J Dermatol. 2000;143:1275-1278.84. Wieman T, et al. <strong>Clinical</strong> efficacy of becaplermin (rhPDGF-BB) gel. Am J Surg. 1998;176(2A):74S-79S.85. Embil J, Papp K, Sibbald G, et al. Recombinant human platelet-derived growth factor-BB (becaplermin) forhealing chronic lower extremity diabetic ulcers: an open-label clinical evaluation of efficacy. Wound RepairRegen. 2000;8(3):162-168.86. Alvarez O, Fernandez-Obregon A, Rogers R, et al. A prospective, randomized, comparative study ofcollagenase and papain-urea for pressure ulcer debridement. Wounds. 2002;14(8):293-301.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.439
Alabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacotherapy <strong>Review</strong> of Skin and Mucous Membrane Agents, MiscellaneousCombination ProductsAHFS Class 849200February 7, 2007I. OverviewThe American Hospital Formulary Service (AHFS) class 849200 includes products with a range ofdifferent indications. The combination skin and mucous membrane agents, miscellaneous that are includedin this review are listed in Table 1. This review encompasses all (topical) dosage forms and strengths.Table 1. Combination Skin and Mucous Membrane Agents, Miscellaneous Included in this <strong>Review</strong>Generic Name(s) Formulation(s) Example BrandName(s)Current PDLAgent(s)allantoin, hyaluronic acid, mannan gel RadiaplexRX ® nonepolysaccharides, and vitamin Ealoe vera, maltodextrin, mannan mouthwash OraMagicRx ® nonepolysaccharides, and potassium sorbatebalsam of Peru, castor oil, and trypsin gel Optase ® nonecalcipotriene and betamethasone ointment Taclonex ® nonedipropionatechlorophyllin, papain, and ureaaerosol,ointment, sprayGladase-C ® *,Panafil ® *chlorophyllin,papain, and ureamucositis and stomatitis combo 1 (oral oral wafer Mucotrol ® nonegel wafer)papain and ureaaerosol, Accuzyme ® *, papain and ureaointment, spray Gladase ® *potassium phosphatespray Constant Clens ® none(monobasic/dibasic), sodium phosphate(monobasic/dibasic), urea, and zinc‡shark liver oil and live yeast cell extract rectal cream N/A shark liver oil andlive yeast cellextractshark liver oil, phenylephrine, glycerin,and white petrolatum‡rectal cream Preparation H ® * shark liver oil,phenylephrine,glycerin, andshark liver oil, phenylephrine, mineraloil, and white petrolatum‡*Generic is available in at least one dosage form or strength.‡Over-the-counter product is available in at least one dosage form or strength.N/A = not available.white petrolatumrectal ointment Preparation H ® * shark liver oil,phenylephrine,mineral oil, andwhite petrolatumII.Evidence-Based Medicine and Current Treatment GuidelinesCurrent treatment guidelines that incorporate the combination skin and mucous membrane agents,miscellaneous are summarized in Table 2.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.440
Table 2. Treatment Guidelines Using the Combination Skin and Mucous Membrane Agents,Miscellaneous<strong>Clinical</strong> GuidelineRecommendation(s)The American Gastroenterological • Universal recommendations include adding fiber to the dietAssociation:Technical <strong>Review</strong> on theDiagnosis and Treatment ofHemorrhoids 1 ••and avoiding straining at defecation.Over-the-counter topical agents are recommended despitethe lack of supportive data regarding their efficacy.Topical analgesics are useful for symptom relief of pain anditching.• Corticosteroid creams may decrease local inflammation butlong-term use of high potency steroids should be avoided.• There is no data to show that corticosteroids reducehemorrhoidal swelling, bleeding, or protrusion.• Topical nitroglycerin may relieve pain associated withhemorrhoids by decreasing anal tone.• Flavonoids may be of benefit since they may increasevenous tone, lymphatic drainage, capillary resistance, andmay normalize capillary permeability.• Nonoperative treatment, such as banding and sclerotherapy,and operative procedures such as hemorrhoidectomy maybe useful in patients with more severe hemorrhoids and inthose not responding to other treatments.American Society of Colon andRectal Surgeons:Practice Parameters for theManagement of Hemorrhoids 2 ••Medical treatment includes warm sitz baths, dietarycorrection, stool modifiers, and topical creams.Long-term use of topical steroids should be avoided.• Rubber band ligation, hemorrhoidectomy, and otherprocedures are reserved for patients who fail moreconservative therapy.American Society of Colon andRectal Surgeons:Practice Parameters for theManagement of Hemorrhoids,2005 Update 3 ••Dietary management, including adequate fiber and fluidintake, is the primary management recommendation.Office treatment (including rubber band ligation,sclerotherapy, cryotherapy, etc.) and surgical intervention isreserved for patients with more severe hemorrhoids or thosenot responding to more conservative therapy.Multinational Association ofSupportive Care in Cancer(MASCC) and the InternationalSociety of Oral Oncology (ISOO):<strong>Clinical</strong> Practice Guidelines forthe Prevention and Treatment ofCancer Therapy-Induced Oraland Gastrointestinal Mucositis 4 ••Good oral care is important to maintain mucosal health andprevent soft-tissue infections.Patient-controlled analgesia (PCA) with morphine isrecommended as the treatment of choice in patients withoral mucositis pain undergoing hematopoietic stem celltransplantation (HSCT).• Topical preparations comprised of ingredients likelidocaine, benzocaine, milk of magnesia, diphenhydramine,kaolin, pectin, and chlorhexidine are in widespread use,though they are not recommended due to lack of sufficientevidence of efficacy.Multinational Association ofSupportive Care in Cancer(MASCC) and the InternationalSociety of Oral Oncology (ISOO):Summary of Evidence-Based<strong>Clinical</strong> Practice Guidelines forCare of Patients with Oral andGastrointestinal Mucositis (2005Update) 5 •••Patient-controlled analgesia (PCA) with morphine is thetreatment of choice in patients with oral mucositis painundergoing hematopoietic stem cell transplantation(HSCT).Sucralfate and antimicrobial lozenges are not recommendedfor the prevention of radiation-induced oral mucositis.Benzydamine is recommended for the prevention ofradiation-induced mucositis in patients with head and neckcancer receiving moderate-dose radiation.• Acyclovir and chlorhexidine are not recommended toPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.441
<strong>Clinical</strong> GuidelineRecommendation(s)prevent or treat oral mucositis.• Keratinocyte Growth Factor-1 (palifermin) is recommendedfor the prevention of oral mucositis at a dose of 60mcg/kg/day for 3 days prior to conditioning treatment andfor 3 days post-transplant in patients undergoing autologousstem cell transplantation.Infectious Diseases Society of • Proper care for patient with diabetic foot infections shouldDiabetic Foot Infections 6 • Sharp debridement with scalpel, scissors, or tissue nippersAmerica (ISDA):Diagnosis and Treatment ofinclude off-loading of pressure, wound cleansing anddebridement, and appropriate antibiotic treatment.is preferable to the use of topical debriding agents.American Diabetes Association:Consensus DevelopmentConference on Diabetic FootWound Care 7 • Six approaches to the treatment of diabetic ulcers that aresupported by clinical trials or are well-establishedprinciples of wound healing include off-loading,debridement, dressings, management of infection, vascularreconstruction, and amputation.• Sharp debridement at frequent intervals has been shown toheal neuropathic wounds more rapidly.• Little data exists to support enzymatic debridement oversharp debridement.• Recombinant platelet derived growth factor has shownmodest benefit when used with off-loading, debridement,and treatment of infection but should not be a substitute forappropriate wound care.Infectious Diseases Society of • Surgical debridement is recommended when needed.Skin and Soft-Tissue Infections 8America (ISDA):Practice Guidelines for theDiagnosis and Management of• Enzymatic debridement is not mentioned in theseguidelines.American Academy of FamilyPhysicians (AAFP): Treatment ofPsoriasis: An Algorithm-BasedApproach for Primary CarePhysicians 9 ••Topical therapy is the mainstay of treatment for localizeddisease.Treatment options include corticosteroids, calcipotriene,coal tar products, tazarotene, and anthralin, Use ofemollients should be encouraged, but they should be usedselectively because many (e.g., products containing lacticacid or α-hydroxy acids) can be irritating to inflamed orbroken skin.• While topical corticosteroids are the mainstay of treatmentfor psoriasis, coal tar and anthralin are effective treatmentoptions.• Calcipotriene may be used as monotherapy but is usuallyused in combination with topical corticosteroids formaximum benefits.• Calcipotriene may be used with corticosteroids until lesionsare flat, and then used as monotherapy with a “pulse” ofcorticosteroids on weekends only.• Tazarotene once daily has been shown to be as effective astwice daily fluocinonide cream 0.05%.• Tazarotene may be used as monotherapy but maximumbenefits are seen when it is combined with topicalcorticosteroids. It is pregnancy category X and should beavoided in women of childbearing age.British Association of• Therapy depends on the affected sites, the extent, and thePsoriasis Guidelines 2006 10 occupation, personality, and general health.Dermatologists:severity of psoriasis, in addition to the patient’s age, sex,442Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
<strong>Clinical</strong> GuidelineRecommendation(s)• Emollients are recommended to soften scaling and reduceirritation.• Coal tar based creams of between 1% and 5% have beenproven effective in inducing remission in patients withpsoriasis, but are limited by adverse effects and patientpreference. Questions exist about the potentialcarcinogenicity of coal tar products but no evidence existsto firmly link them with cancers.• Topical corticosteroids are effective, cosmeticallyacceptable, and safe if used appropriately. There is a widerange of strengths available from mild to potent. Tolerancemay develop, as well as rebound exacerbations upondiscontinuation. Topical corticosteroids should be rotatedwith nonsteroidal treatments. Potent corticosteroids shouldnot be used for more than 7 consecutive days.• A vitamin D analogue, such as calcipotriene, may be used.It is more convenient than coal tar products and does notproduce the side effects associated with topicalcorticosteroids. Irritant reactions are common. This hasbecome one of the first-line treatments for psoriasis andefficacy is comparable to potent corticosteroid treatment.• Combination betamethasone and calcipotriene may be used,though data on long-term relapse rates is unknown at thispoint.• A vitamin A analogue (tazarotene) may be used and issuitable for moderate plaque psoriasis affecting up to 10%of skin area. Local irritation is common.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.443
III.IndicationsFood and Drug Administration (FDA)-approved indications for the combination skin and mucous membrane agents, miscellaneous are noted in Table 3.Table 3. FDA-Approved Indications for the Combination Skin and Mucous Membrane Agents, Miscellaneous 11-20Indication(s)Management of radiationdermatitis, partial and fullthickness wounds, 1 st and 2 nddegree burns, cuts, andabrasions`Allantoin,HyaluronicAcid, MannanPoly-Saccharides,and Vitamin EaAloe Vera,Maltodextrin,MannanPoly-Saccharides,andPotassiumSorbateBalsam ofPeru,CastorOil, andTrypsinCalcipotrieneand Beta-MethasoneDipropionateChloro-Phyllin,Papain, andUreaMucositis andStomatitisCombo 1 (OralGel Wafer)PapainandUreaSharkLiverOil andLiveYeastCellExtractShark LiverOil, Phenyl-Ephrine,Glycerin,and WhitePetrolatumShark LiverOil, Phenyl-Ephrine,Mineral Oil,and WhitePetrolatumOral mucositis, stomatitis, orallesions, aphthous ulcers, cancersores, tissue injury caused by illfitting dentures, gum diseaseTreatment of varicose ulcers,dehiscent wounds, decubitalulcers, sunburn, and debridementof escharPsoriasis vulgaris aAcute and chronic lesions suchas varicose, diabetic, anddecubitus ulcers, burns, postoperativewounds, pilonidal cystwounds, carbuncles, andmiscellaneous woundsaaaPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.444
Indication(s)Relief of pain, soothing of orallesions such as oral mucositis,stomatitis, irritation due to oralsurgery, and traumatic ulcerscaused by braces or ill fittingdentures or diseaseAllantoin,HyaluronicAcid, MannanPoly-Saccharides,and Vitamin EAloe Vera,Maltodextrin,MannanPoly-Saccharides,andPotassiumSorbateBalsam ofPeru,CastorOil, andTrypsinCalcipotrieneand Beta-MethasoneDipropionateChloro-Phyllin,Papain, andUreaMucositis andStomatitisCombo 1 (OralGel Wafer)aPapainandUreaSharkLiverOil andLiveYeastCellExtractShark LiverOil, Phenyl-Ephrine,Glycerin,and WhitePetrolatumShark LiverOil, Phenyl-Ephrine,Mineral Oil,and WhitePetrolatumDebridement of necrotic tissueand liquefaction of slough inacute and chronic lesions likepressure ulcers, varicose anddiabetic ulcers, burns, postoperativewounds, pilonidalcysts, carbuncles, andmiscellaneous woundsaTo shrink swelling of irritatedhemorrhoidal tissue and providerelief of burning, itching, anddiscomfort from hemorrhoidsTo provide relief of burning,itching, and discomfort fromhemorrhoids, shrinkhemorrhoidal tissue, providecoating for relief from anorectaldiscomforts, protect anorectalsurface to make bowelmovements less painfula aaPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.445
IV.PharmacokineticsA literature search failed to retrieve pharmacokinetic data for the combination skin and mucous membraneagents, miscellaneous.V. Drug InteractionsA literature search indicates that there are no significant drug interactions with the combination skin andmucous membrane agents, miscellaneous.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.446
VI.Adverse Drug EventsThe most common adverse events reported with the combination skin and mucous membrane agents, miscellaneous are noted in Table 4.Table 4. Adverse Drug Events (%) Reported with the Combination Skin and Mucous Membrane Agents, Miscellaneous 11-20Adverse Event(s)Allantoin,HyaluronicAcid, MannanPoly-Saccharides,and Vitamin EAloe Vera,Maltodextrin,Mannan Poly-Saccharides, andPotassiumSorbateBalsam ofPeru,Castor Oil,and TrypsinCalcipotrieneand Beta-MethasoneDipropionatePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.447Chloro-Phyllin,Papain,and UreaMucositisandStomatitisCombo 1(Oral GelWafer)PapainandUreaShark LiverOil and LiveYeast CellExtractShark LiverOil, Phenyl-Ephrine,Glycerin, andWhitePetrolatumCentral Nervous SystemHeadache - - - 2.8 - - - - - -DermatologicalApplication sitepruritis- - - 0.5 - - - - - -Burning sensation - - - 0.2-1.4 a - a - - -Ecchymosis - - - 1 - - - - - -Erythema - - - 0.4-1 - - - - - -Folliculitis - - -
Adverse Event(s)Allantoin,HyaluronicAcid, MannanPoly-Saccharides,and Vitamin EAloe Vera,Maltodextrin,Mannan Poly-Saccharides, andPotassiumSorbateBalsam ofPeru,Castor Oil,and TrypsinCalcipotrieneand Beta-MethasoneDipropionateChloro-Phyllin,Papain,and UreaMucositisandStomatitisCombo 1(Oral GelWafer)PapainandUreaShark LiverOil and LiveYeast CellExtractShark LiverOil, Phenyl-Ephrine,Glycerin, andWhitePetrolatumOtherInfluenza - - - 0.9 - - - - - -Pain - - - 0.3 - - - - - -a Percent not specified- Event not reportedShark LiverOil, Phenyl-Ephrine,Mineral Oil,and WhitePetrolatumPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.448
VII.Dosing and AdministrationThe usual dosing schedules for the combination skin and mucous membrane agents, miscellaneousare summarized in Table 5.Table 5. Usual Dosing for the Combination Skin and Mucous Membrane Agents, Miscellaneous 11-20Drug(s) Usual Adult Dose Usual Pediatric Dose AvailabilityAllantoin, hyaluronicacid, mannanpolysaccharides, andvitamin EApply to affected area afterradiation treatment 3 times perday or as neededSafety and efficacy inchildren have not beenestablishedGelAloe vera,maltodextrin, mannanpolysaccharides, andpotassium sorbateBalsam of Peru,castor oil, and trypsinMove 1 tablespoon around themouth for 1 minute 4 timesper day or as neededMay be swallowedGel and ointment:Apply a thin film a minimumof 2 times per day or asneededMay use a dressing or woundmay be left openSpray:Hold bottle approximately 12inches from the affected area,coat wound rapidly with spray2 times per day or as neededSafety and efficacy inchildren have not beenestablishedSafety and efficacy inchildren have not beenestablishedMouthwash(dry powder forreconstitution)GelOintmentSprayCalcipotriene andbetamethasonedipropionateMay use a dressing or woundmay be left openApply an adequate layer toaffected area and rub in gentlyand completely once daily forup to 4 weeksSafety and efficacy inchildren have not beenestablishedOintmentMaximum: do not exceed 100g of ointment in 1 weekChlorophyllin,papain, and ureaDo not treat more than 30% ofbody surface area and do notapply to the face, axillae, orgroinAerosol and Spray:Completely cover the woundwith the spray (wound shouldnot be visible under the spray)and apply appropriate dressing1-2 times per daySafety and efficacy inchildren have not beenestablishedAerosolOintmentSprayOintment:Apply to wound 1-2 times perday and cover withappropriate dressingMucositis and Allow 1 tablet to slowly Safety and efficacy in WaferPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.449
Drug(s) Usual Adult Dose Usual Pediatric Dose Availabilitydissolve in the mouth 3 times children have not beenper day, avoid eating or establisheddrinking for at least 1 hourafter usestomatitis combo 1(oral gel wafer)Papain and ureaAerosol and Spray:Completely cover the woundwith the spray (wound shouldnot be visible under the spray)and apply appropriate dressing2 times per daySafety and efficacy inchildren have not beenestablishedAerosolOintmentSprayShark liver oil andlive yeast cell extractShark liver oil,phenylephrine,glycerin, andwhite petrolatumShark liver oil,phenylephrine,mineral oil, andwhite petrolatumOintment:Apply to wound 2 times perday and cover withappropriate dressingApply to affected area 4 timesper day, especially at night, inthe morning, or after eachbowel movementApply to affected area 4 timesper day, especially at night, inthe morning, or after eachbowel movementApply to affected area 4 timesper day, especially at night, inthe morning, or after eachbowel movementSafety and efficacy inchildren have not beenestablishedSafety and efficacy inchildren have not beenestablishedSafety and efficacy inchildren have not beenestablishedCreamCreamOintment450Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
VIII. Effectiveness<strong>Clinical</strong> trials evaluating the safety and efficacy of the combination skin and mucous membrane agents, miscellaneous are summarized in Table 6.Table 6. Comparative <strong>Clinical</strong> Trials Using the Combination Skin and Mucous Membrane Agents, MiscellaneousStudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsGray et al. 21Balsam of Peru, castor oil,trypsin ointment (BCT-O) BIDvs.balsam of Peru, castor oil,trypsin spray (BCT-S) BIDvs.salineone study group compared BCT-O and BCT-S directly, while asecond arm compared BCT-Oand saline and a third armcompared BCT-S and saline,patients served as their owncontrolsRCT, SBPatients 65 yearsof age and older,otherwise healthyLasers were usedto create partialthickness woundson the right andleft thighN=609 daysPrimary:<strong>Clinical</strong> gradefor erythema,scabbing, oredema on a scaleof 0 (none) to 10(severe) andclinical grade forhealing on ascale of 0 (nohealing) to 10(completehealing)Secondary:Not reportedResultsPrimary:BCT-O vs. BCT-SErythema was significantly lower on day 3 in the BCT-O groupcompared to the BCT-S group and continued to be significantlylower until the end of the study (P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsThere was a significantly lower degree of erythema in patients inthe BCT-S group compared to saline only at day 1 (P
Guenther et al. 24StudyandDrug RegimenCalcipotriene plusbetamethasone ointment QD inthe evening and vehicle ointmentQD in the morningvs.Study DesignandDemographicsa >60 year oldgroup for the metaanalysisRCT, MC, PRO,DB, PC, PGPatients 18-86years of age with adiagnosis ofpsoriasis vulgarisinvolving at leastSample Sizeand StudyDurationN=8284 weeksEnd Points(assessed in 3 ofthe 4 studies),Investigator’sGlobalAssessment ofDisease Severity(IGA) from“absence ofdisease” to “verysevere disease”,patients wereconsideredcontrolled if theyhad either absentor very milddisease (assessedin 2 studies),patients’assessment oftreatmentresponse on ascale of “worse”to ‘clearance” (inall 4 studies),treatmentsuccess definedas “markedimprovement” or“clearance”Primary:Percentagechange in PASIfrom baseline toweek 4Secondary:PercentageResultsand a 40.75 reduction in patients >60.In the 2 studies assessing Investigator’s Global Assessment ofDisease Severity, 52.1% of patients 60had controlled disease after up to 4 weeks of treatment.A total of 59% of patients 60 judgedthemselves as having attained treatment success.A similar portion of patients 60 experienced lesional orperilesional adverse reactions during the study.No P values were reported in this meta-analysis.Primary:The difference in PASI from baseline to week 4 in the combinationtreatment groups of once and twice daily was not significant (5.4%,P=0.052).The once-daily combined-medication group had a significantlyreduced PASI compared to the calcipotriol group (68.6% vs.58.8%, P
StudyandDrug Regimencalcipotriene plus betamethasoneointment BIDvs.calcipotriene ointment BIDvs.vehicle ointment BIDStudy DesignandDemographics10% of one ormore body regionsSample Sizeand StudyDurationEnd Pointschange inthickness scoreof a targetpsoriatic lesionfrom baseline toeach treatmentvisit, speed ofresponseassessed bychange in PASIfrom baseline toweek 2,investigator’soverallassessment oftreatmentefficacy, adverseeffectsP
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsA significantly lower proportion of patients experienced adverseeffects in both combination groups compared to the calcipotrienegroup (P0.1), though a significant difference was noted in favor of thecombination groups when compared to the vehicle group(P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultscompared to the calcipotriene group (P
vs.StudyandDrug Regimenvehicle ointment QD (V)Study DesignandDemographicsSample Sizeand StudyDurationEnd Pointsdisease)Secondary:Not reportedResults216, 137, and 15 respectively, P
Kragbale et al. 30StudyandDrug RegimenCalcipotriene plusbetamethasone ointment QD for8 weeks followed bycalcipotriene ointment QD for 4weeks (Group 1)vs.calcipotriene plus betamethasoneointment QD for 4 weeksfollowed by 8 weeks ofcalcipotriene ointment QD onweekdays and calcipotriene plusbetamethasone ointment QD onweekends (Group 2)vs.calcipotriene ointment BID for12 weeks (Group 3)Study DesignandDemographicsRCT, PRO, DB,PGPatients 18 yearsof age and olderwith a diagnosis ofpsoriasisSample Sizeand StudyDurationN=97112 weeksEnd Pointsimprovement orclearance), andpatients withcontrolleddisease (absentor very milddisease)according toIGA and PASIPrimary:Mean percentchange in PASIfrom baseline toweek 8,proportion ofpatients withabsent or verymild diseaseaccording to theIGA at the endof 8 weeksSecondary:Mean percentchange in PASIfrom baseline toeach visit and at12 weeks,proportion ofpatients withabsent/very milddiseaseaccording toIGA severity atResultsAmong patients with severe disease at baseline, 54.2% of patientsachieved treatment success after 4 weeks according to patient’sassessments, 60.9% in patients with moderate disease, and 61.2%in patients with mild disease.According to PASI-defined baseline disease severity, 38.7% ofpatients had controlled disease after 4 weeks, 52.9% in patientswith moderate disease, and 66.1% in patients with mild disease.According to IGA-defined baseline disease severity, 44.1% ofpatients had controlled disease after 4 weeks, 53.0% in patientswith moderate disease, and 69.3% in patients with mild disease.Primary:There was a significant reduction in the mean percent change inPASI from baseline to week 8 in group 1 compared to groups 2 and3 (73.3%, 68.2%, and 64.1% respectively, P
Naidu et al. 31StudyandDrug RegimenMF 5232 (Mucotrol ® ) TID afterfood for 7-10 daysvs.placebo TID after food for 7-10daysStudy DesignandDemographicsRCT, DB, PC,PRO, PGPatients 18-65years of age withhistopathologicalconfirmation ofhead and neckcancers anddiagnosed withoral mucositis perWorld HealthOrganization(WHO) criteriaSample Sizeand StudyDurationN=3010 daysEnd Pointseach visit and at12 weeksPrimary:Improvements inthe WHOgrading scale fororal mucositis,the RadiationTherapyOncology Group(RTOG) OralMucositisGrading System,and theObjectiveScoring Systemfor evaluation ofulceration anderythemaSecondary:Not reportedResultsPrimary:There was a significant reduction in mean WHO mucositis scoresin the MF 5232 group from baseline (P=0.007), but no significantchange in the placebo group from baseline (P value not reported).There was a significant reduction in the RTOG scores in the MF5232 group from baseline (P=0.031,) but no significant change inthe placebo group from baseline (P value not reported).There was a significant reduction in mean objective scores forulceration and erythema in the MF 5232 group from baseline(P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd Pointsassessed weeklySecondary:Not reportedResultstissue did not predict a significantly different rate of reduction inthe wound area.No significant conclusions can be made as a result of this study.Secondary:Not reportedDrug regimen abbreviations: QD=once daily, BID=twice daily, TID=three times dailyStudy abbreviations: DB=double-blind, MA=meta-analysis, MC=multicenter, OL=open-label, PC=placebo-controlled, PG=parallel-group, PRO=prospective, RCT=randomized controlled trial, SB=singleblindMiscellaneous abbreviations: IGA=investigator’s global assessment of disease severity, PASI=Psoriasis Area and Severity Index, PGA=patient’s global assessmentPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.460
Additional EvidenceDose SimplificationA search of Medline and Ovid did not reveal data pertinent to this topic.Stable TherapyA search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician VisitsA search of Medline and Ovid did not reveal data pertinent to this topic.IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. Todifferentiate the average cost per prescription from one product to another, a specific number of‘$’ signs from one to five is assigned to each medication. Assignment of relative cost values isbased upon current Alabama Medicaid prescription claims history and the average cost perprescription as paid at the retail pharmacy level. For branded products with little or no recentutilization data, the average cost per prescription is calculated by the average wholesale price(AWP) and the standard daily dosing per product labeling. For generic products with little or norecent utilization data, the average cost per prescription is calculated by the Alabama Medicaidmaximum allowable cost (MAC) and the standard daily dosage per product labeling. Please notethat the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 7. Relative Cost of the Combination Skin and Mucous Membrane Agents,MiscellaneousGeneric Name(s) Formulation(s) Example BrandName(s)BrandCostGenericCostallantoin, hyaluronic acid, gel RadiaplexRX ® $ N/Amannan polysaccharides,and vitamin Ealoe vera, maltodextrin, mouthwash OraMagicRx $ N/Amannan polysaccharides,and potassium sorbatebalsam of Peru, castor oil, gel Optase ® $-$$$ N/Aand trypsincalcipotriene andointment Taclonex ® $$$$$ N/Abetamethasone dipropionatechlorophyllin, papain, and aerosol, Gladase-C ® *,$$-$$$ $$ureaointment, spray Panafil ® *mucositis & stomatitiscombo 1 (oral gel wafer)wafer Mucotrol ® $$$ N/APrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.461
Generic Name(s) Formulation(s) Example BrandName(s)BrandCostGenericCostpapain and ureaaerosol, Accuzyme ® *,$$-$$$ $$ointment, spray Gladase*potassium phosphate spray Constant Clens ®(monobasic/dibasic),sodium phosphate(monobasic/dibasic), urea,and zinc and zinc‡shark liver oil and live yeast cream N/A N/A $cell extractshark liver oil,rectal cream Preparation H ® * $$ N/Aphenylephrine, glycerin, andwhite petrolatum‡shark liver oil,phenylephrine, mineral oil,and white petrolatum‡rectal ointment Preparation H ® * $$ N/A*Generic is available in at least one dosage form or strength.‡Over-the-counter product is available in at least one dosage form or strength.N/A = not available.X. ConclusionsThe combination miscellaneous skin and mucous membrane agents represent a diverse class ofmedications used for a variety of different indications. Important considerations based onavailable clinical trials are discussed below.There were no clinical studies available evaluating the efficacy and safety of the combination ofaloe vera, maltodextrin, mannan polysaccharides, and potassium sorbate (OraMagicRx ® ) in thetreatment of oral mucositis, stomatitis, aphthous ulcers, and sores. Therefore, it is difficult tomake recommendations regarding this product. Current guidelines for the treatment of severe oralmucositis recommend the use of morphine for patient-controlled analgesia (PCA), and paliferminfor prevention. 4,5 Likewise, there is no data regarding the efficacy and safety of combinationrectal products containing shark liver oil, live yeast cell extract, phenylephrine, glycerin, mineraloil, and white petrolatum for the treatment of hemorrhoids. Current guidelines for the treatment ofhemorrhoids do not recommend the routine use of these topical products due to the lack of dataevaluating efficacy and safety, though their use is widespread. 1-4A few small clinical trials support the use of the combination of balsam of Peru, castor oil, andtrypsin in the treatment of various ulcers and wounds, and as a debriding agent. 21,22 One studyshowed that the ointment dosage form was more effective than both the spray form and saline forthe treatment of man-made wounds in otherwise healthy adults, while an open-label study with nocontrol group demonstrated healing of split-thickness skin grafts within 11 days. 21,22 There are nohead-to-head studies evaluating the use of this combination compared to other debriding agents.There are also no studies comparing this combination to other agents in this class used for thetreatment of ulcers and wounds.One study showed greater efficacy of the combination of papain and urea compared to collagenasein the treatment of pressure ulcers in decreasing the amount of necrotic tissue at each evaluationpoint, though no clinically significant conclusions were reached as a result of this study. 32 Nostudies were found evaluating the efficacy of the combination of chlorophyllin, papain, and urea.One small study evaluated the efficacy of Mucotrol ® oral gel wafer in the treatment of oralmucositis in patients with head and neck cancers. The study found Mucotrol ® was significantlymore effective than placebo in reducing mucositis scores, ulceration and erythema. 31 There are noPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.462
studies comparing this product to OraMagicRx ® . Current guidelines for the treatment of mucositisdo not reference the use of this device. 4,5The combination of calcipotriene and betamethasone (Taclonex ® ) is indicated for the treatment ofpsoriasis. There are several studies evaluating the efficacy of this drug in the treatment ofpsoriasis compared to placebo vehicle and to each individual component. Overall, results indicatethat the combination product was more effective in reducing psoriasis area and severity index(PASI) scores, and that it also increased the percentage of patients with clear or almost cleardisease compared to either agent alone or placebo. 23-30 However, no data was found evaluating theuse of the combination product versus a combined use of its two ingredients on the same efficacyparameters. There are also no studies evaluating the impact of this medication on patientcompliance or physician visits. Current guidelines for the treatment of psoriasis state that topicalcorticosteroids are used as first-line agents, though calcipotriene, tazarotene, anthralin and coal tarare other therapeutic options. 9,10 A combination of calcipotriene and betamethasone isrecommended as an option by the British Association of Dermatologists, but long-term relapserates are unknown at this time. 9There is insufficient data to support that one brand combination miscellaneous skin and mucousmembrane agent is safer or more efficacious than another. Therefore, all brand products withinthe class reviewed are comparable to each other and to the generics and over-the-counter productsin this class and offer no significant clinical advantage over other alternatives in general use.XI.RecommendationsNo brand combination miscellaneous skin and mucous membrane agent is recommended forpreferred status. Alabama Medicaid should accept cost proposals from manufacturers to determinecost effective products and possibly designate one or more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.463
References1. American Gastroenterological Association. Technical review on the diagnosis and treatment ofhemorrhoids. Gastroenterology. 2004;126:1463-1473.2. American Society of Colon and Rectal Surgeons. Practice Parameters for the treatment ofhemorrhoids. Available at: www.fascrs.org/displaycommon.cfm?an=1&subarticlenbr=145. AccessedOctober 31, 2006.3. Castaldo P, Ellis C, Gregorcyk S, et al. Practice parameters for the management of hemorrhoids. DisColon Rectum. 2005;48(2):189-194.4. Rubenstein E, Peterson D, Schubert M, et al. <strong>Clinical</strong> practice guidelines for the prevention andtreatment of cancer therapy-induced oral and gastrointestinal mucositis. Cancer. 2004Suppl;100(9):2026-2046.5. MASCC/ISOO. Summary of evidence-based clinical practice guidelines for care of patients with oraland gastrointestinal mucositis (2005 update). Available at:http://www.mascc.org/media/Resource_centers/Guidelines_mucositis.pdf. Accessed October 31,2006.6. Lipsky B, Berendt A, Deery H, et al. Diagnosis and treatment of diabetic foot infections. Clin InfectDis. 2004;39:885-910.7. Consensus Development Conference on Diabetic Foot Wound Care: 7-8 April 1999,Boston,Massachusetts. American Diabetes Association. Diabetes Care. 1999 Aug;22(8):1354-1360.8. Stevens DL, Bisno AL, Chambers HF, Everett ED, Dellinger P, Goldstein EJ, Gorbach SL,Hirschmann JV, Kaplan EL, Montoya JG, Wade JC; Infectious Diseases Society of America. Practiceguidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis.2005;41:1373-1406.9. Pardasani A, Feldman S, Clark A. Treatment of psoriasis: an algorithm-based approach for primarycare physicians. Am Fam Physician. 2000;61(3):725-740.10. British Association of Dermatologists. Psoriasis Guideline 2006. Available at:http://www.bad.org.uk/healthcare/guidelines/psoriasis.asp. Accessed October 10, 2006.11. RadiaPlexRX ® Gel [package insert]. Irving, TX: MPM Medical, Inc.; 2005.12. OraMagicRx ® [package insert]. Irving, TX: MPM Medical, Inc.; 2005.13. Xenaderm ® [package insert]. San Antonio, TX: Healthpoint, Ltd.14. Taclonex ® [package insert]. Rockaway, NJ: Warner Chilcott; January 2006.15. Ziox 405 ® [package insert]. Carlstdt, NJ: Stratus Pharmaceuticals, Inc.; November 2005.16. Mucotrol ® [package insert]. Eatontown, NJ: Cura Pharmaceutical Co., Inc.; 2005.17. Accuzyme ® [package insert]. Fort Worth, TX: Healthpoint Ltd.; 2005.18. Hem-prep Cream ® [package insert]. Madison, NJ: Whitehall Laboratories; 2005.19. Formulation-R ® [package insert]. South Plainfield, NJ: G&W Laboratories; 2005.20. Preparation-H ® [package insert]. Madison, NJ: Wyeth Consumer Healthcare; 2005.21. Gray M, Jones D. The effect of different formulations of equivalent active ingredients on theperformance of two topical wound treatment products. Ostomy Wound Manage. 2004;50(3):34-44.22. Carson S, Wiggins C, Overall K, Hebert J. Using a castor oil-balsam of Peru-trypsin ointment to assistin the healing of skin graft donor sites. Ostomy Wound Manage. 2003;49(6):60-64.23. Parslew R, Traulsen J. Efficacy and local safety of a calcipotriol/betamethasone dipropionate ointmentin elderly patients with psoriasis vulgaris. Eur J Dermatol. 2005;15(1):37-39.24. Guenther L, Cambazard F, van de Kerkhof P, et al. Efficacy and safety of a new combination ofcalcipotriol and betamethasone dipropionate (once or twice daily) compared to calcipotriol (twicedaily) in the treatment of psoriasis vulgaris: a randomized, double-blind, vehicle-controlled clinicaltrial. Br J Dermatol. 2002;147:316-323.25. van de Kerkhof P. The impact of a two-compound product containing calcipotriol and betamethasonedipropionate (Daivobet ® /Dovobet ® ) on the quality of life in patients with psoriasis vulgaris: arandomized controlled trial. Br J Dermatol. 2004;151:663-668.26. Douglas W, Poulin Y, Decroix J, et al. A new calcipotriol/betamethasone formulation with rapid onsetof action was superior to monotherapy with betamethasone dipropionate or calcipotriol in psoriasisvulgaris. Acta Derm Venereol. 2002;82:131-135.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.464
27. Kaufman R, Bibby A, Bissonnette R, et al. A new calcipotriol/betamethasone dipropionate formulation(Daivobet TM ) is an effective once-daily treatment for psoriasis vulgaris. Dermatology. 2002;205:389-393.28. Papp K, Guenther L, Boyden B, et al. Early onset of action and efficacy of a combination ofcalcipotriene and betamethasone dipropionate in the treatment of psoriasis. J Am Acad Dermatol.2003;48(1):48-54.29. van de Kerkhof P, Wasel N, Kragballe K, Cambazard F, Murray S. A two-compound productcontaining calcipotriol and betamethasone dipropionate provides rapid, effective treatment of psoriasisvulgaris regardless of baseline disease severity. Dermatology. 2005;210:294-299.30. Kragballe K, Noerrelund K, Lui H, et al. Efficacy of once-daily treatment regimens withcalcipotriol/betamethasone dipropionate ointment and calcipotriol ointment in psoriasis vulgaris.2004;150:1167-1173.31. Naidu M, Ramana V, Ratnam V, et al. A randomized, double-blind, parallel, placebo-controlled studyto evaluate the efficacy of MF 5232 (Mucotrol TM ), a concentrated oral gel wafer, in the treatment ofmucositis. Drugs R D. 2005;6(5):291-298.32. Alvarez O, Fernandez-Obregon A, Rogers R, et al. A prospective, randomized, comparative study ofcollagenase and papain-urea for pressure ulcer debridement. Wounds. 2002;14(8):293-301.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.465
I. OverviewAlabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingNew Drug Pharmacotherapy <strong>Review</strong>—Levemir ® (insulin detemir)Insulins, AHFS Class 682008February 07, 2007Insulin is used as replacement therapy in patients with diabetes, replacing deficient endogenousinsulin and temporarily restoring the ability of the body to properly utilize carbohydrates, fats, andproteins. Insulin is secreted by the beta cells in the pancreas and lowers blood glucose byfacilitating peripheral glucose uptake into cells and by inhibiting gluconeogenesis in the liver. Inaddition to its glycemic effects, insulin has anabolic properties, enhancing protein synthesis,inhibiting lipolysis in adipocytes and inhibiting proteolysis. 1-3Insulin detemir is a new long-acting basal insulin analogue approved by the Food and DrugAdministration (FDA) for the treatment of diabetes in adult patients requiring basal insulin for thecontrol of hyperglycemia. Insulin detemir differs from human insulin through the addition of afatty acid chain to the amino acid B29. The addition of the fatty acid chain increases the insulin’saffinity to albumin and contributes to the pharmacokinetic properties of insulin detemir. Insulindetemir has a slow rate of systemic absorption and a duration of action of up to 24 hours.Though several insulin products are available over-the-counter (OTC), insulin detemir is availableby prescription only. Please note that OTC insulin preparations are currently listed on the AlabamaMedicaid Preferred Drug List (PDL). Currently, the only prescription insulin formulation availableon the Alabama Medicaid PDL is insulin lispro (Humalog ® ).Table 1 lists all insulin detemir formulations included in this review. This review encompasses alldosage forms and strengths. Within this review, only clinical trials investigating the safety andefficacy of insulin detemir will be summarized. Reference data from unpublished trials and datapresented as abstracts or posters for insulin detemir were not evaluated and are not included in thisreview. The insulins therapeutic class was previously reviewed in August 2006 and the completereview is available in the Appendix.Table 1. Insulin Detemir Products Included in this <strong>Review</strong> 1-4Generic Name Formulation(s) Example Brand Name(s) Current PDLStatusinsulin detemir injection Levemir ® noneNo generic products are available for insulin detemir.II.Evidence-Based Medicine and Current Treatment GuidelinesTable 2 summarizes the current treatment guidelines for insulin therapy in the management ofdiabetes mellitus.Table 2. Treatment Guidelines Using the Insulins 5-11<strong>Clinical</strong> GuidelineRecommendation(s)American Diabetes Association Treatment Algorithm(ADA)/European Association forthe Study of Diabetes:Step 1: Lifestyle Intervention and MetforminManagement of Hyperglycemiain Type 2 Diabetes: AConsensus Algorithm for the• Lifestyle intervention consisting of weight loss and increasedlevels of activity should be initiated as the first step in treatingnew-onset type 2 diabetes.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.466
<strong>Clinical</strong> GuidelineRecommendation(s)Initiation and Adjustment ofTherapy 5 • Metformin should be initiated with lifestyle intervention asthe initial pharmacologic therapy in the absence of specificcontraindications, when lifestyle intervention fails to achieveor maintain metabolic goals.Step 2: Additional Medications• If lifestyle intervention and maximally tolerated doses ofmetformin fail to achieve glycemic goals, another medicationshould be added within 2-3 months of therapy initiation orwhenever glycosylated hemoglobin (HbA1c) goal is notachieved.• Second-line therapies may include a thiazolidinedione, asulfonylurea, or insulin.• Consideration of insulin as the second-line therapy should begiven when HbA1c >8.5%, or with symptomatichyperglycemia.Step 3: Further Adjustments• If lifestyle intervention, metformin, and a second medicationfail to achieve glycemic goals, insulin therapy should beinitiated or intensified.• If HbA1c is 250 mg/dL; random glucose levelsconsistently >300 mg/dL; HbA1c>10%; presence ofketonuria; or as symptomatic diabetes with polyuria,polydipsia, and weight loss), insulin therapy in combinationwith lifestyle intervention therapy is the treatment of choice.• After symptoms are relieved, oral agents may be added andtherapy with insulin may possibly be withdrawn.• Type 1 diabetes: therapy will include intensive insulin therapywhich may require multiple insulin injections or use of aninsulin pump for optimal management.• Type 2 diabetes: proper nutrition, exercise and education arePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.467
<strong>Clinical</strong> GuidelineMellitus 6American College ofEndocrinologists (ACE)/AACEDiabetes RecommendationsImplementation Conference:Road Map for the Preventionand Treatment of Type 2Diabetes 7International Diabetes Federation(IDF) <strong>Clinical</strong> Guidelines TaskForce: Global Guideline forType 2 Diabetes 8Institute for <strong>Clinical</strong> SystemsImprovement (ICSI): HealthcareGuideline: Management ofType 2 Diabetes Mellitus 9National Institute for <strong>Clinical</strong>Excellence (NICE): <strong>Clinical</strong>Guidelines for Type 2 Diabetes 10National Institute for <strong>Clinical</strong>Excellence (NICE): Type 1Recommendation(s)the cornerstones of therapy. Therapy utilizing oralmedications and/or insulin regimens should be individualizedto maximize the likelihood of attaining near-normal bloodglucose while minimizing adverse reactions. The method usedto attain normal blood glucose levels is less important thanactually achieving normal blood glucose levels.Patients Naïve to Therapy:• In patients with HbA1c 6%-7%, rapid-acting insulin analogsare recommended for special situations.• In patients with HbA1c 7%-8%, rapid-acting insulin analogsor premixed insulin analogs are recommended for specialsituations.• In patients with HbA1c 8%-10%, combine therapies toaddress fasting plasma and postprandial glucose. Rapidactinginsulin analogs, premixed insulin analogs or NPHinsulin are among the treatment options.• Initiate insulin in patients with an HbA1c of >10%, utilizingeither (1) a rapid-acting insulin analog with NPH or glargine,or (2) premixed insulin analogs.Treated Patients:• In patients with HbA1c of 6.5%-8.5% on monotherapy,combination therapy may be initiated utilizing basal orpremixed insulin analogs.• Rapid-acting insulin analogs can be added to any therapeuticintervention at any time to address persistent postprandialhyperglycemia in patients with HbA1c of 6.5%-8.5%.• In patients with HbA1c of 6.5%-8.5% on combinationtherapy, maximize insulin therapy by adding basal insulin iffasting plasma glucose (FPG) is elevated, adding bolus insulinif postprandial glucose (PPG) is elevated, and if both FPG andPPG are elevated, adding either basal-bolus insulin orpremixed insulin analogs.• In patients with HbA1c of >8.5%, initiate insulin basal-bolustherapy utilizing a rapid-acting insulin with a long-actinginsulin or premixed insulin analogs.Begin insulin therapy when optimized oral glucose-loweringagents and lifestyle interventions are unable to maintain bloodglucose at target levels. Insulin regimens may include thefollowing:• Basal insulin once daily or,• Twice daily premixed (biphasic) insulin with higher HbA1cor,• Multiple daily injections (mealtime and basal insulin) inpatients that are not controlled on other insulin regimens.If glycemic goals are not achieved on oral agents, begin insulinregimen either as monotherapy or as an adjunct to oral therapy.Insulin programs should be individualized based on treatmentgoals, lifestyle and self-monitored blood glucose results.Insulin therapy may be offered to patients with inadequate bloodglucose control on optimized oral glucose-lowering agents.Children and Young People:Insulin regimens should be individualized for each patient. ThreePrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.468
<strong>Clinical</strong> GuidelineDiabetes: Diagnosis andManagement of Type 1 Diabetesin Children, Young People andAdults 11Recommendation(s)basic regimens that can be considered include:• One to three injections per day utilizing short-acting insulin orrapid-acting insulin mixed with intermediate-acting insulin.• Multiple daily injections utilizing short-acting insulin orrapid-acting insulin before meals and ≥1 separate injection ofan intermediate-acting insulin or long-acting insulin.• Continuous subcutaneous insulin infusion utilizing aprogrammable insulin pump.Adults:Insulin regimens should be individualized for each patient andinsulin choice should permit optimal well-being. Two basicregimens that can be considered include:• Multiple daily injection regimen–must be used in conjunctionwith appropriate education, self-monitoring, and dietarymanagement.• Twice-daily injection regimen–consider use in patients whohave learning disabilities, find adherence to lunch timeinjections difficult, and those that prefer fewer injections.III.IndicationsInsulin detemir is indicated for once-daily or twice-daily subcutaneous injection for the treatmentof adult and pediatric type 1 diabetic patients or adult patients with type 2 diabetes who require abasal insulin for the control of hyperglycemia.IV.PharmacokineticsTable 3 summarizes the pharmacokinetic properties of insulin detemir. Insulin detemir is classifiedby the American Hospital Formulary Service (AHFS) as a long-acting insulin.Table 3. Pharmacokinetic Parameters of Insulin Detemir 1-4InsulinPreparationType Half-Life(hours)Onset(hours)Peak(hours)Duration(hours)CompatibleWhen MixedInsulin detemir Long-acting 5-7 3-4 6-8 5.7-23.2 NoneV. Drug InteractionsTable 4 includes the clinically significant drug interactions associated with insulin products.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.469
Table 4. Significant Drug-Drug Interactions for the Insulins 12DrugSignificance Interaction MechanismLevelInsulin 2 β-Adrenergicblocking agents (βblockers),nonselectiveβ-blockers may blunt the sympatheticmediated response to hypoglycemiaand may mask hypoglycemicsymptoms. Discontinue nonselectiveβ-blocker therapy or switch to a β-blocker with selective activity ifpossible. Monitor for signs ofhypoglycemia if coadministration isnecessary.Insulin 1 Ethanol Ethanol may enhance the release ofinsulin following a glucose load andinhibit gluconeogenesis, increasing theglucose-lowering action of insulin. Ifethanol is to be ingested, it should bedone in moderation and taken with ameal in order to minimize the risk ofthis interaction.Insulin 2 Fenfluramine Fenfluramine may potentiate thehypoglycemic effects of insulin.Monitor blood glucose concentrationsand adjust the dose of insulin asneeded to avoid hypoglycemia.Insulin 2 Monoamine oxidaseinhibitors (MAOI)MAOI may potentiate thehypoglycemic effects of insulin bystimulating insulin secretion andinhibiting gluconeogenesis. Monitorblood glucose concentrations andadjust the dose of insulin as needed.Insulin 2 Salicylates Salicylates increase basal insulinsecretion and acute insulin response toa glucose load. The hypoglycemiceffects of insulin may be potentiated.Monitor blood glucose concentrationsand adjust the dose of insulin asneeded.Significance Level 1=major severitySignificance Level 2=moderate severityVI.Adverse Drug Events<strong>Clinical</strong> studies comparing insulin detemir with short-acting insulins did not demonstrate adifference in frequency of adverse events. 1 Adverse reactions commonly associated with insulintherapy are listed below.Hypoglycemia 1-3Hypoglycemia is the most common adverse event reported with insulin therapy. Because of thedifferences in onset and duration of action, the timing of hypoglycemia can vary betweenformulations. Hypoglycemia risk may be increased when patients receive excessive insulin doses,reduce their caloric intake, increase physical activity, during illnesses or when receivingmedications that increase the hypoglycemic effects of insulin (see Table 4).Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.470
Injection Site Reactions 1-3Redness, swelling and itching at the injection site may result if the injection is not done properly,if the skin is sensitive to cleansing solution or if the patient is allergic to insulin or components ofthe insulin formulation.Hypersensitivity 1-3Generalized insulin allergies are rare but may present as a skin rash over the body, shortness ofbreath, fast pulse, sweating, a drop in blood pressure, bronchospasm, shock, anaphylaxis orangioedema.ContraindicationsInsulin detemir is contraindicated in patients who are hypersensitive to insulin detemir or anycomponent in Levemir ® .VII.Dosing and AdministrationLike other insulin formulations, appropriate dosing of insulin detemir is dependent on theindividual patient’s glycemic response to diet and exercise. Table 5 includes the dosing,administration and availability information for insulin detemir.According to the manufacturer, insulin detemir should normally be used in once-daily or twicedailydosing regimens. If a once-daily regimen is used, the dose should be administered at theevening meal or at bedtime. If a twice-daily regimen is used, the evening dose can be administeredat the evening meal, at bedtime or 12 hours after the morning dose.Per the manufacturer, insulin detemir is not to be used in insulin infusion pumps nor should it bediluted or mixed with any other insulin preparation.Table 5. Usual Dosing for Insulin Detemir 1-3Drug Usual Adult Dose Usual Pediatric Dose AvailabilityInsulin detemir Dose and frequency areindividualized per patientneeds.Cartridges (100 U/mL):3 mLType 1 diabetes: doseand frequency areindividualized per patientneeds.Type 2 diabetes: safetyand efficacy in childrenhave not beenestablished.Vial (100 U/mL):10 mLPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.471
VIII. EffectivenessTable 6. Outcomes Evidence for Insulin DetemirStudyStudy DesignandandDrug RegimenDemographicsType 1 DiabetesRussell-Jones et al. 13 RCT, OL, MC, PGInsulin detemir BIDin addition tomealtime insulinaspartvs.NPH BID in additionto mealtime insulinaspartBasal insulin doseswere adjusted toachieve fasting bloodglucose (FBG) of 4.0-7.0 mmol/L (72-126mg/dL) andpostprandial (90minutes after a meal)blood glucose of 12 years with an HbA1c ≤12%on a basal-bolus insulin regimenfor ≥2 months; baseline HbA1cwas 8.35% for participants inboth groupsPatients were excluded if theywere pregnant or breastfeeding,had a total daily basal insulinrequirement of >100 IU, hadproliferative retinopathy,impaired hepatic or renalfunction, severe cardiacproblems, uncontrolledhypertension, or recurrent majorhypoglycemic episodesSample Sizeand StudyDurationN=7476 monthsEnd PointsPrimary:Effect on HbA1c,fasting plasmaglucose (FPG), 9-point self-monitoredblood glucose(SMBG), 24-hourcontinuous bloodglucose profiles,frequency ofhypoglycemia, weightgain, and adverseeventsSecondary:Not reportedResultsPrimary:Mean HbA1c value decreased 0.06% with insulindetemir while HbA1c increased 0.06% with NPH. Thedifference was not significant (P=0.083).Difference in FPG was significantly lower with insulindetemir compared to NPH (-1.16 mmol/L; P=0.001).Nine-point SMBG profiles demonstrated significantlylower glucose values before breakfast with insulindetemir when compared to NPH (values not reported;P
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsDe Leeuw et al. 14Insulin detemir BIDin addition tomealtime insulinaspartvs.NPH BID in additionto mealtime insulinaspartBasal insulin doseswere adjusted toachieve FBG of 4.0-7.0 mmol/L (72-126mg/dL) andpostprandial (90minutes after a meal)blood glucose of
vs.StudyandDrug RegimenNPH BID in additionto mealtime insulinaspartBasal insulin doseswere adjusted toachieve FBG of 4.0-7.0 mmol/L (72-126mg/dL) andpostprandial (90minutes after a meal)blood glucose of 100 IU; had abody mass index (BMI) of >35kg/m 2 ; had proliferativeretinopathy; impaired hepatic orrenal function; severe cardiacproblems; uncontrolledhypertension; recurrent majorhypoglycemic episodes; or hadan allergy to insulinRCT, OL, MC, PGAdult type 1 diabetic patients ona basal-bolus insulin regimen for≥2 months; baseline HbA1c was8.01% for participants takinginsulin detemir QAM and atdinner, 8.13% for those takinginsulin detemir QAM and atbedtime, and 8.08% for thoserandomized into the NPH groupPatients were excluded if theywere pregnant or breastfeeding;had a significant medicaldisorder (not specified); had ahistory of recurrent majorSample Sizeand StudyDurationN=40016 weeksEnd PointsSecondary:Not reportedPrimary:Effect on HbA1c andFPGSecondary:Variability in fastingSMBG, 10-pointSMBG, 24-hourglucose profile,frequency ofhypoglycemia, andweight gainResultsThere was significantly less day-to-day fluctuation offasting SMBG profiles with insulin detemir whencompared to NPH (P
StudyandDrug Regimenbedtime in addition tomealtime insulinaspartStudy DesignandDemographicshypoglycemic or hypoglycemiaunawareness; or were onmedications that interfered withglucose metabolismSample Sizeand StudyDurationEnd PointsResultssignificantly lower with either insulin detemir treatmentscompared to NPH (P
StudyandDrug RegimenStudy DesignandDemographicsproblems; uncontrolledhypertension; recurrent majorhypoglycemic episodes; historyof alcohol or narcotic abuse; orhad an allergy to insulinSample Sizeand StudyDurationEnd Points(+0.07 kg; P
StudyandDrug RegimenHome et al. 19Insulin detemir Q12hours in addition tomealtime insulinaspartvs.insulin detemir QAMand bedtime inaddition to mealtimeinsulin aspartvs.NPH QAM andbedtime in addition tomealtime insulinaspartBasal insulin doseswere adjusted toachieve FBG of 4.0-7.0 mmol/L (72-126mg/dL) andpostprandial bloodglucose of 2 months; baseline HbA1c was8.55% for participants takinginsulin detemir Q12 hours,8.74% for those taking insulindetemir QAM and at bedtime,and 8.52% for those randomizedinto the NPH groupPatients were excluded if theywere pregnant or breastfeeding;had a history of proliferativeretinopathy; recurrenthypoglycemia, impaired renal orhepatic function; or were onmedications that interfered withglucose metabolismSample Sizeand StudyDurationN=40816 weeksEnd PointsPrimary:Effect on HbA1c andFPGSecondary:Fasting SMBG, 10-point SMBG,frequency ofhypoglycemia, andweight gainResultsNot reportedPrimary:After 16 weeks, there was no significant difference inHbA1c between all treatment groups (P=0.082). Insulindetemir dosed Q12 hours reduced HbA1c 0.85%. Whendosed QAM and at bedtime, HbA1c was reduced 0.82%.NPH reduced HbA1c 0.65%. When the insulin detemirgroups were combined, the reduction of HbA1c wassignificantly greater compared to NPH (-0.18%;P=0.027).FPG differences were significant with insulin detemirdosed Q12 hours (-1.5 mmol/L; P=0.004) and insulindetemir dosed QAM and bedtime (-2.3 mmol/L;P0.05).Secondary:Within-person between-day variation in fasting SMBGwas significantly lower with either insulin detemirtreatments compared to NPH (P0.05).Overall risk of hypoglycemia was significantly lowerwith insulin detemir dosed Q12 hours (25%; P=0.046)and dosed QAM and at bedtime (32%; P=0.002)compared to NPH. There was no significant difference inrisk of nocturnal hypoglycemia between insulin detemirdosed Q12 hours and NPH; however, when dosed QAM477Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenStudy DesignandDemographicsSample Sizeand StudyDurationEnd PointsResultsand at bedtime, insulin detemir had a significantly lowerrisk (53%; P4 months; baseline HbA1c was7.9% for participants receivinginsulin detemir first and 7.9% forthose receiving NPH firstPatients were excluded if theywere pregnant or breastfeeding;had a history of significantmedical disorders; recurrenthypoglycemia; or had an allergyto insulinRCT, OL, MC, PGAdult type 2 diabetic patients onan insulin regimen for >2months; baseline HbA1c was7.9% for participants takingN=13032 weeksN=50526 weeksPrimary:Incidence of selfrecordedhypoglycemiaSecondary:Incidence of severehypoglycemicepisodes, effect onHbA1c and selfmonitoredplasmaglucose (SMPG)Primary:Effect on HbA1cSecondary:FPG, fasting SMBG,9-point SMBG,Mean weight change saw a significant decrease withinsulin detemir dosed Q12 hours (-0.8 kg; P=0.006) andinsulin detemir dosed QAM and bedtime (-0.6 kg;P=0.040) when compared to NPH. There was nosignificant difference in weight change between theinsulin detemir groups (P>0.05).Primary:The relative risk of hypoglycemia was 18% lower withinsulin detemir compared to NPH (P=0.001). Therelative risk of nocturnal hypoglycemia was 50% lowerwith insulin detemir compared to NPH (P
StudyandDrug RegimenNPH QD-BIDBasal insulin doseswere adjusted toachieve an FBG of4.0-7.0 mmol/L (72-126 mg/dL) andpostprandial bloodglucose of 100 units; or wereon medications that interferedwith glucose metabolismSample Sizeand StudyDurationEnd Pointsfrequency ofhypoglycemia, andweight gainResultsSecondary:After 26 weeks, there was no significant difference inmean FPG reductions between insulin detemir (-0.5mmol/L) and NPH (-0.6 mmol/L; P>0.05).There was significantly less day-to-day fluctuation offasting SMBG profiles with insulin detemir whencompared to NPH (P=0.021).There were no significant differences in mean 9-pointSMBG profiles between the 2 treatment groups(P=0.58).There was no significant difference in the overall risk ofhypoglycemia between insulin detemir compared toNPH (P=0.48).Hermanson et al. 22Insulin detemir BIDin addition to thepatient’s current oralantidiabetic regimenvs.NPH BID in additionto the patient’s currentoral antidiabeticregimenRCT, OL, MC, PGAdult type 2 diabetic patientswith no history of insulin use;baseline HbA1c was 8.61% forparticipants taking insulindetemir and 8.51% for thoserandomized into the NPH groupPatients were excluded if theywere pregnant or breastfeeding;receiving thiazolidinediones; hada history of proliferativeN=47626 weeksPrimary:Effect on HbA1cSecondary:FPG, proportion ofparticipants achievingHbA1c ≤7.0%,proportion ofparticipants achievingHbA1c ≤7.0%withouthypoglycemia, 10-point SMBG,After 26 weeks, body weight change from baseline wassignificantly lower with insulin detemir (1.0 kg)compared to NPH (1.8 kg; P=0. 017).Primary:After 26 weeks, HbA1c reductions with the insulindetemir group (-1.8%; P=0.004) did not differsignificantly from reductions observed with NPH (-1.9%; P=not significant).Secondary:After 26 weeks, the difference in mean FPG reductionsbetween insulin detemir and NPH was not significant(0.32 mmol/L; P>0.05).The proportion of patients achieving an HbA1c of≤7.0% was 70% in those taking insulin detemir and 74%479Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.
StudyandDrug RegimenBasal insulin doseswere adjusted toachieve prebreakfastFBG of 6.0 mmol/L(108 mg/dL).Study DesignandDemographicsretinopathy, recurrenthypoglycemia, or impaired renalor hepatic function; hadsecondary diabetes; or were onmedications that interfered withglucose metabolismSample Sizeand StudyDurationEnd Pointsfrequency ofhypoglycemia, andweight gainResultswith those taking NPH. The difference betweentreatment groups was not significant.The proportion of patients achieving an HbA1c of≤7.0% without hypoglycemia was significantly higher inthose taking insulin detemir (26%) compared to thosetaking NPH (16%; P=0.008).There was significantly less day-to-day fluctuation offasting SMBG profiles with insulin detemir whencompared to NPH (P=0.021).There were no significant differences in mean 10-pointSMBG profiles between the 2 treatment groups(P=0.19).There was a 47% lower risk of overall hypoglycemiawith insulin detemir compared to NPH (P
Additional EvidenceDose SimplificationA search of Medline and Ovid did not reveal data pertinent to this topic.Stable TherapyA search of Medline and Ovid did not reveal data pertinent to this topic.Impact on Physician VisitsA search of Medline and Ovid did not reveal data pertinent to this topicPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.481
IX.CostA “relative cost index” is provided below as a comparison of the average cost per prescription formedications within this American Hospital Formulary Service (AHFS) drug class. To differentiate theaverage cost per prescription from one product to another, a specific number of ‘$’ signs from one to five isassigned to each medication. Assignment of relative cost values is based upon current Alabama Medicaidprescription claims history and the average cost per prescription as paid at the retail pharmacy level. Forbranded products with little or no recent utilization data, the average cost per prescription is calculated bythe average wholesale price (AWP) and the standard daily dosing per product labeling. For genericproducts with little or no recent utilization data, the average cost per prescription is calculated by theAlabama Medicaid maximum allowable cost (MAC) and the standard daily dosage per product labeling.Please note that the relative cost index does not factor in additional cost offsets available to the AlabamaMedicaid program via pharmaceutical manufacturer rebating.The relative cost index scale for this class is as follows:Relative Cost Index Scale$ $0-$30 per Rx$$ $31-$50 per Rx$$$ $51-$100 per Rx$$$$ $101-$200 per Rx$$$$$ Over $200 per RxRx=prescriptionTable 7. Relative Cost of Insulin DetemirGeneric Name(s) Formulation(s) Example BrandName(s)Brand CostGenericCostinsulin detemir injection Levemir ® $$$ N/ANo generic products are available for insulin detemir.N/A=not availableX. ConclusionsInsulin detemir is a long-acting basal insulin preparation that has been demonstrated to be an effective aidto glycemic control in type 1 and type 2 diabetics. Insulin detemir can be dosed once or twice daily,depending on the glycemic needs of the patient and is most similar to insulin glargine (Lantus ® ) in terms ofduration of action. It is available by prescription only. As with insulin glargine, diluting or mixing insulindetemir with other insulin preparations is not recommended.A majority of the clinical trials that have been published were conducted in type 1 diabetics, and directlycompared insulin detemir to NPH insulin in combination with a bolus insulin. Overall, these trials did notproduce consistent results when comparing the levels of glycemic control achieved with these two insulins.In the majority of the trials, insulin detemir was found to be comparable to NPH insulin in HbA1creduction 13-16,18-20 and in FPG reductions. 14,15,17,18 One clinical trial comparing insulin detemir incombination with insulin aspart (Novolog ® ) found significantly lower HbA1c than with NPH insulin. Itshould be noted that in this trial, NPH insulin was not used in conjunction with insulin aspart, but ratherwith regular human insulin. 17 In this same study, FPG results were comparable between the two treatmentgroups. Another trial compared two dosing regimens of insulin detemir, and found comparable HbA1creductions to NPH when the regimens were compared individually; however, when the insulin detemirgroups were combined, the HbA1c reductions were significantly greater. 19 This trial also demonstratedsignificant reductions in FPG with insulin detemir compared to NPH.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.482
Two published trials conducted in type 2 diabetics were available for review. As monotherapy, insulindetemir was found to be comparable in HbA1c and mean FPG reductions to NPH insulin. 21 When used inconjunction with oral antidiabetic agents, insulin detemir was again found to be comparable to NPH insulinin HbA1c and mean FPG reductions. 22Overall risk of hypoglycemia was reported to be lower with insulin detemir in five trials 15,17,19,20,22 butcomparable to NPH insulin in five trials. 13,14,16,18,21 There was a significantly lower risk of nocturnalhypoglycemia with insulin detemir in the majority of the trials. 13,14,15,17,19,20,22 The majority of the trialsreported comparable rates of other adverse reactions between treatment groups; however, all clinical trialsreported statistically significant less weight gain with insulin detemir compared to NPH insulin. Althoughstatistically significant this difference of approximately 2 lb is of questionable clinical significance13-19, 21-22especially in light of comparable HbA1c results.Comparative data regarding insulin detemir has not demonstrated distinct, clinically significant differencesregarding glycemic control or safety. In addition, national guidelines state that in the treatment in type 2diabetes second-line therapies may include a thiazolidinedione, a sulfonylurea, or insulin thus making ainsulin detemir a second line agent.Therefore, all brand products within the class reviewed are comparable to each other and to the genericsand over-the-counter products in this class and offer no significant clinical advantage over otheralternatives in general use.XI.RecommendationsNo brand insulin detemir (Levemir ® ) is recommended for preferred status. Alabama Medicaid shouldaccept cost proposals from manufacturers to determine cost effective products and possibly designate oneor more preferred brands.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.483
References1. Levemir ® [package insert]. Kansas City, MO: Aventis Pharmaceuticals Inc.; November 2005.2. Micromedex® Healthcare Series, (electronic version). Thomson Micromedex, Greenwood Village, CO, USA.Available at: http://www.thomsonhc.com. Accessed December 4, 2006.3. Wickersham RM, Novak KK, managing eds. Drug Facts and Comparisons. St. Louis, Mo: Wolters KluwerHealth, Inc.; 2006.4. McEvoy GK, ed. [2006]. AHFS Drug Information: Antidiabetic Agents 68:20, Insulins 68:20.08 [monographon the Internet]. Bethesda, MD: American Society of Health-System Pharmacists. Available athttp://online.statref.com/document.aspx?fxid=1&docid=1190 [2006 Dec 4].5. Nathan DM, Buse JB, Davidson MB, Heine RJ, et al. Management of hyperglycemia in type 2 diabetes: aconsensus algorithm for the initiation and adjustment of therapy: a consensus statement from the AmericanDiabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2006; 29(8):1963-1972.6. American Association of <strong>Clinical</strong> Endocrinologists (AACE). Medical guidelines for the management ofdiabetes mellitus: the AACE system of intensive diabetes self-management–2002 update. Endocr Pract. 2002;8(Suppl.1):40-82.7. American College of Endocrinologists (ACE)/American Association of <strong>Clinical</strong> Endocrinologists (AACE),Diabetes Recommendations Implementation Conference: Road Map for the Prevention and Treatment of Type2 Diabetes. Available at: www.aace.com/meetings/consensus/odimplementation/roadmap.pdf. Accessed July12, 2006.8. International Diabetes Federation (IDF) <strong>Clinical</strong> Guidelines Task Force. Global Guideline for Type 2 Diabetes.Available at: http://www.idf.org/webdata/docs/IDF%20GGT2D.pdf. Accessed February 2, 2006.9. Institute for <strong>Clinical</strong> Systems Improvement. Healthcare Guideline-Management of Type 2 Diabetes Mellitus-Tenth Edition. Available at: http://www.icsi.org/knowledge/detail.asp?catID=29&itemID=182. AccessedFebruary 2, 2006.10. National Institute for <strong>Clinical</strong> Excellence (NICE). Type 2 Diabetes—Management of Blood Glucose. Availableat: http://www.nice.org.uk/pdf/NICE_full_blood_glucose.pdf. Accessed February 2, 2006.11. National Institute for <strong>Clinical</strong> Excellence (NICE). Type 1 Diabetes in Children, Young People and Adults:NICE Guideline. Available at: http://www.nice.org.uk/pdf/CG015NICEguideline.pdf. Accessed February 2,2006.12. Tatro DS, ed. Drug Interaction Facts. St. Louis, Mo: Wolters Kluwer Health, Inc.; 2006.13. Russell-Jones D, Simpson R, Hylleberg B, Draeger E, Bolinder J. Effects of QD insulin detemir or neutralprotamine Hagedorn on blood glucose control in patients with type I diabetes mellitus using a basal-bolusregimen. Clin Ther. 2004; 26(5):724-736.14. De Leeuw I, Vague P, Selam JL, Skeie S, Lang H, Draeger E, Elte JW. Insulin detemir used in basal-bolustherapy in people with type 1 diabetes is associated with a lower risk of nocturnal hypoglycaemia and lessweight gain over 12 months in comparison to NPH insulin. Diabetes Obes Metab. 2005; 7(1):73-82.15. Vague P, Selam JL, Skeie S, De Leeuw I, Elte JW, Haahr H, Kristensen A, Draeger E. Insulin detemir isassociated with more predictable glycemic control and reduced risk of hypoglycemia than NPH insulin inpatients with type 1 diabetes on a basal-bolus regimen with premeal insulin aspart. Diabetes Care. 2003;26(3):590-596.16. Pieber TR, Draeger E, Kristensen A, Grill V. Comparison of three multiple injection regimens for Type 1diabetes: morning plus dinner or bedtime administration of insulin detemir vs. morning plus bedtime NPHinsulin. Diabet Med. 2005; 22(7):850-857.17. Hermansen K, Fontaine P, Kukolja KK, Peterkova V, Leth G, Gall MA. Insulin analogues (insulin detemir andinsulin aspart) versus traditional human insulins (NPH insulin and regular human insulin) in basal-bolus therapyfor patients with type 1 diabetes. Diabetologia. 2004; 47(4):622-629.18. Standl E, Lang H, Roberts A. The 12-month efficacy and safety of insulin detemir and NPH insulin in basalbolustherapy for the treatment of type 1 diabetes. Diabetes Technol Ther. 2004; 6(5):579-588.19. Home P, Bartley P, Russell-Jones D, Hanaire-Broutin H, et al. Insulin detemir offers improved glycemiccontrol compared with NPH insulin in people with type 1 diabetes: a randomized clinical trial. Diabetes Care.2004; 27(5):1081-1087.20. Kolendorf K, Ross GP, Pavlic-Renar I, Perriello G, et al. Insulin detemir lowers the risk of hypoglycemia andprovides more consistent plasma glucose levels compared with NPH insulin in Type 1 diabetes. Diabet Med.2006;23(7):729-35.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.484
21. Haak T, Tiengo A, Draeger E, Suntum M, Waldhausl W. Lower within-subject variability of fasting bloodglucose and reduced weight gain with insulin detemir compared to NPH insulin in patients with type 2 diabetes.Diabetes Obes Metab. 2005; 7(1):56-64.22. Hermansen K, Davies M, Derezinski T, Martinez Ravn G, Clauson P, Home P. A 26-week, randomized,parallel, treat-to-target trial comparing insulin detemir with NPH insulin as add-on therapy to oral glucoseloweringdrugs in insulin-naive people with type 2 diabetes. Diabetes Care. 2006; 29(6):1269-1274.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.485
AppendixAlabama Medicaid AgencyPharmacy and Therapeutics Committee MeetingPharmacologic Management of Diabetes MellitusFebruary 7, 2007I. OverviewDiabetes mellitus is a collection of diseases of abnormal carbohydrates metabolism that results in highblood sugars. It is associated with impairment in insulin secretion, along with varying degrees of resistanceto the action of insulin in the peripheral tissue. The disorder can be classified as either type 1 (insulindependent) or type 2 (non-insulin dependent) diabetes. Other less common forms of diabetes are gestationaldiabetes, drug-induced diabetes, and immune-mediated diabetes. Diagnosis of diabetes type 1 or 2 is basedon pathogenesis and clinical presentation, rather than age of onset. Ninety percent of diabetics have type 2disease, which can be associated with physical inactivity and other lifestyle characteristics. 1 In type 2diabetes, plasma insulin concentrations may be decreased, increased or normal. Glucose-stimulatedsecretion of endogenous insulin is frequently reduced, and decreased peripheral sensitivity to insulin isalmost always associated with glucose intolerance. Obesity may be a confounder as overlapping insulinresistance with β-cell dysfunction may result in diabetes. In comparison, type 1 diabetes results fromautoimmune destruction of the pancreatic β-cell. Type 1 diabetes responds to insulin replacement therapyto restore deficient levels of endogenous insulin and temporarily restore the ability of the body to properlyutilize carbohydrates, fats, and proteins.Nearly 16 million Americans (7% of the population) have diabetes, and there is likely one personundiagnosed for every two persons currently diagnosed with the disease. 1 In 2002, antidiabeticmedications accounted for 208 prescriptions per 1,000 national Medicaid members. 2 Uncontrolled diabetesresults in microvascular, macrovascular and neuropathic complications. This disease is the leading causeof blindness in adults and is the leading contributor to the development of end-stage renal disease.Additional metabolic abnormalities commonly seen in diabetic patients include obesity, hypertension,hyperlipidemia, and impaired fibrinolysis. Epidemiologic data indicate that the incidence of obesity inchildren with type 2 diabetes is increasing such that 8-45% of children with newly diagnosed diabetes havenonimmune-mediated diabetes mellitus. 2Although type 1diabetes is likely initiated by the exposure of a genetically susceptible individual to anenvironmental agent, type 2 diabetes is a heterogenous disorder with multiple risk factors. 3Risk factors for the development of type 2 diabetes include: 4• Family history (parents or siblings with diabetes)• Overweight (Body Mass Index [BMI] ≥25 kg/m 2 )• Habitual physical inactivity• Age ≥45 years• Race/ethnicity (Native Americans, Hispanic Americans, Asian Americans, African Americans andPacific Islanders)• Previously identified impaired glucose tolerance or impaired fasting glucose• Hypertension (≥ 140/90 mm Hg)• High-density lipoprotein (HDL) cholesterol ≤35 mg/dL and/or a triglyceride level ≥250 mg/dL• History of gestational diabetes or delivery of a baby >9 pounds• Polycystic ovary disease• History of vascular diseaseProper treatment, both pharmacological and non-pharmacological with lifestyle modifications, can reducecardiovascular mortality, reduce mortality from other diabetic complications, and help diabetic patients livehealthier, longer lives.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.486
II.Evidence-Based Medicine and Current Treatment GuidelinesUnited Kingdom Prospective Diabetes Study (UKPDS)The UKPDS diabetes initiative, started in 1977, was a multicenter, randomized, controlled interventiontrial, comparing treatment with conventional diet-based blood glucose control therapy to intensivepharmacotherapy with a sulfonylurea, insulin, or metformin. The primary goal of the study was todetermine if glycemic control in type 2 diabetes prevents diabetic complications and their associatedmorbidity and mortality. The study included various subsets, looking at blood pressure control and efficacyof combination pharmacotherapy treatments. Results from the trial were published in 1998 and involved3,867 newly diagnosed type 2 diabetic patients. 4 The study provided definitive evidence for the benefit ofintensive management of blood glucose level and blood pressure in patients with type 2 diabetes. 5Full results of the five-year post-study monitoring period have not yet been published. Preliminary datareported in August 2003 at the International Diabetes Federation Scientific Meeting in Paris included thefollowing results: 6• Only a quarter of patients had achieved the target glycosylated hemoglobin (HbA1c) level of
Study Sample Resultschange in mean body weight and significant reduction in mean fastingplasma insulin concentration (P
Table 2. Current Treatment Guidelines for Diabetes MellitusWorld Health Organization (WHO): Diagnosis Criteria 15Diabetes• Fasting plasma glucose levels ≥126 mg/dL (≥ 7.0 mmol/L) or fasting whole blood glucoselevels ≥110 mg/dL (≥ 6.1 mmol/L)• 2-hour post glucose load ≥200 mg/dL (≥ 11.1 mmol/L) for plasma or capillary whole bloodImpaired Glucose Tolerance (IGT)• Plasma glucose 2-hour post glucose load ≥140 mg/dL (≥ 7.8 mmol/L)Impaired Fasting Glucose (IFG)• Plasma fasting blood glucose (FBG) of 110–125 mg/dL (6.1-6.9 mmol/L)American Diabetes Association (ADA): Standards of Medical Care in Diabetes 16ClassificationUnder the ADA position statement, diabetes is differentiated into 4 clinical classes:Type 1 diabetes–results from β-cell destruction, usually leading to absolute insulin deficiencyType 2 diabetes–results from a progressive defect in insulin secretion coupled with insulinresistanceOther–specific types of diabetes due to other causes, which may include• Genetic defects in β-cell function• Genetic defects in insulin action• Diseases of the exocrine pancreas• Drug or chemical induced• Gestational diabetes mellitus (GDM)–diagnosed during pregnancyIn addition to the above classifications, impaired fasting glucose (IFG) or impaired glucosetolerance (IGT) has been officially termed pre-diabetes. Both IFG and IGT are risk factors fordiabetes and cardiovascular disease and are defined below:• Impaired fasting glucose – fasting blood glucose (FBG) of 100–125 mg/dL• Impaired glucose tolerance – 2-hour plasma glucose of 140–199 mg/dL during an oralglucose tolerance test (OGTT)Screening Recommendations• Individuals ≥45 years old, particularly if BMI ≥25 kg/m 2• Adult individuals 9 pounds or have been diagnosed with GDM– Are hypertensive (≥140/90 mm Hg)– Have a HDL cholesterol level 250 mg/dLPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.489
– Have polycystic ovary syndrome (PCOS)– Had IGT or IFG on previous testing– Have other clinical conditions associated with insulin resistance (e.g., PCOS oracanthosis nigricans)– Have a history of vascular disease• High-risk, asymptomatic, undiagnosed patients within the health care setting• Overweight children (BMI >85 th percentile for age and sex, weight for height >85 th percentileor >120% of ideal weight for height) with 2 or more of the following:– Family history of type 2 diabetes in first or second degree relative– Are members of a high-risk ethnic population (e.g., African American, Latino,Native American, Asian American, Pacific Islander)– Have other clinical conditions associated with insulin resistance (e.g., PCOS oracanthosis nigricans)– Maternal history of diabetes or GDM• Pregnant women with clinical characteristic consistent with a high risk for GDM including:– Marked obesity– Personal history of GDM– Glycosuria– A strong family history of diabetes• Women with GDM 6-12 weeks post partumScreening should be repeated every 3 years for adults and every 2 years for children.Diagnosis• Symptoms of diabetes plus casual plasma glucose concentration ≥200 mg/dL. Symptoms ofdiabetes include polyuria, polydipsia and unexplained weight loss. Casual is defined as anytime of day without regard to time since last meal.OR• Fasting plasma glucose (FPG) ≥126 mg/dL. Fasting is defined as no caloric intake for >8hours.OR• 2-hour plasma glucose ≥200 mg/dL during an oral glucose tolerance test (OGTT) as describedby the WHO, utilizing an equivalent of 75 g anhydrous glucose dissolved in water.Repeat testing on a separate day may be required in the absence of unequivocal hyperglycemia.Glycemic goals• HbA1c:
Prevention/Delay of Type 2 Diabetes• Drug therapy should not be routinely used to prevent diabetes until more information isknown about its cost effectiveness.American Diabetes Association (ADA) / European Association for the Study of Diabetes:Management of Hyperglycemia in Type 2 Diabetes: A Consensus Algorithm for the Initiation andAdjustment of Therapy 17Glycemic Goals• The primary goal of therapy is achieving and maintaining glucose levels as close to thenondiabetic range as possible.• HbA1c should be lowered to as close to the nondiabetic range as possible or, at a minimum,decreasing the HbA1c8.5%, orwith symptomatic hyperglycemia.Step 3: Further Adjustments• If lifestyle intervention, metformin, and a second medication fail to achieve glycemic goals,insulin therapy should be initiated or intensified.• If HbA1c is
treatment algorithm due to their generally lower overall glucose-lowering effectiveness andlimited clinical data. However, these agents may be appropriate in selected patients.Specific Medications Combinations• When more than one combination is used, the synergy of particular combinations and otherinteractions should be considered.• Insulin in combination with metformin or in combination with a thiazolidinedione isparticularly effective in lowering HbA1c.• The combination of a thiazolidinedione and metformin has modest additive effects inlowering HbA1c.Special Considerations/Patients• In severely uncontrolled diabetes (defined as fasting plasma glucose levels > 250 mg/dL;random glucose levels consistently > 300 mg/dL; HbA1c>10%; presence of ketouria; or assymptomatic diabetes with polyuria, polydipsia, and weight loss) insulin therapy incombination with lifestyle intervention therapy is the treatment of choice.• After symptoms are relieved, oral agents may be added and therapy with insulin may possiblybe withdrawn.American Association of <strong>Clinical</strong> Endocrinologists (AACE): Medical Guidelines for the Managementof Diabetes Mellitus 18• A diabetes health-care team, ideally consisting of a diabetes-trained nurse, dietitian skilled indiabetes education, and as needed, a pharmacist, psychologist and exercise physiologist led bya clinical endocrinologist or other physician who has expertise/experience in overseeing thisintegrated system of care should be utilized in an effort to achieve normal or near-normalblood glucose levels.• Intensive therapy, consisting of a comprehensive program that includes frequent selfmonitoringof blood glucose levels and sophisticated regimens for maintaining near-normal,blood glucose levels should be initiated for type 1 and type 2 diabetics.• Type 1 therapy–Therapy will include intensive insulin therapy which may require multipleinsulin injections or use of an insulin pump for optimal management• Type 2 therapy–Proper nutrition, exercise and education are the cornerstone of therapy.Therapy utilizing oral medications and/or insulin regimens should be individualized tomaximize the likelihood of attaining near-normal blood glucose while minimizing adversereactions. The method used to attain normal blood glucose levels is less important thanactually achieving normal blood glucose levels. The decision to use a specific regimen shouldbe made by the leader of the diabetes care team.• Successful implementation of this system is dependent on active patient participation, acommitted health-care team and adherence to scheduled interactions between the patient andthe team.International Diabetes Federation (IDF) <strong>Clinical</strong> Guidelines Task Force: Global Guideline for Type 2Diabetes 19Diagnosis• Diagnosis should be based on the 1999 WHO criteria.• An OGTT should be performed in high risk individuals with a fasting plasma glucose of 100-126 mg/dL.• If a random plasma glucose test result is 100-200 mg/dL, repeat test with an OGTT or fastingtest.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.492
TreatmentLifestyle managementNutrition therapy and physical activity training should be incorporated in diabetes selfmanagementprograms.Oral therapy• Metformin should be considered 1 st line therapy unless contraindicated.• Sulfonylurea should be considered when metformin fails or as 1 st line therapy in nonoverweightpatients.• Peroxisome proliferator-activated receptor (PPAR) -γ agonists may be added tometformin as an alternative to a sulfonylurea, added to a sulfonylurea when metformin iscontraindicated or in addition to metformin/sulfonylurea combination therapy.• α-glucosidase inhibitors may be considered as a further option.InsulinBegin when optimized oral glucose-lowering agents and lifestyle interventions are unable tomaintain blood glucose at target levels and may include the following regimens:• Basal insulin once daily or,• Twice daily premixed (biphasic) insulin with higher HbA1c or,• Multiple daily injections (mealtime and basal insulin) in patients that are not controlledon other insulin regimensGlucose control levels• HbA1c:
Lifestyle interventions• Weight loss and physical activity should be encouraged in overweight (BMI> 25 kg/m 2 )and obese patientsMetformin• Considered 1 st line treatment choice in overweight patients (BMI> 25 kg/m 2 ) notcontrolled through lifestyle interventions• Considered 1 st line choice in non-overweight patientsInsulin secretagogues• Considered 1 st line treatment choice in non-overweight patients• Considered 1 st line treatment choice when metformin is not tolerated or contraindicated• Consider use in combination with metformin in overweight patients when glucose controlis unsatisfactoryPPAR -γ agonists• Considered as combination therapy in patients unable to take metformin and insulinsecretagogue combination therapy or when HbA1c control is unsatisfactory withmetformin and insulin secretagogue combinationα-Glucosidase inhibitors• Considered as an alternative agent for patients unable to use other oral glucose-loweringagentsInsulin• May be offered to patients with inadequate blood glucose control on optimized oralglucose-lowering agentsMonitoring glycemic control• HbA1c: 6.5–7.5% based on the risk for microvascular and macrovascular complications.HbA1c should be tested every 3-6 monthsNational Institute for <strong>Clinical</strong> Excellence (NICE): Type 1 Diabetes: Diagnosis and Management ofType 1 Diabetes in Children, Young People and Adults 22Children and Young PeopleDiagnosis• Diagnosis is based on criteria specified in the 1999 WHO report on the diagnosis andclassification of diabetes mellitus.TreatmentInsulin regimens should be individualized for each patient. Three basic regimens that can beconsidered include:• One to three injections per day utilizing short-acting insulin or rapid-acting insulin mixedwith intermediate-acting insulin• Multiple daily injections utilizing short-acting insulin or rapid-acting insulin before mealsand ≥1 separate injection of an intermediate-acting insulin or long-acting insulin• Continuous subcutaneous insulin infusion utilizing a programmable insulin pumpMonitoring glycemic control• HbA1c:
Adults• Postprandial blood glucose should be
9%-10% Combine therapies utilizing metformin, thiazolidinedione, sulfonylurea, insulinglargine, rapid-acting insulin analogs, premixed insulin analogs, NPH, or otherapproved combinations to address fasting plasma and postprandial glucose levelsTreated PatientsInitial HbA1c Current Therapy Intervention6%-6.5% Monotherapy or combinationtherapy• Continue current therapy if ACEglycemic goals are met• Adjust therapy as needed to meet ACEFPG and PPG goals6.5%-8.5% Monotherapy with meglitinide,sulfonylurea, α-glucosidaseinhibitor, metformin,thiazolidinedione, premixedinsulin analogs or basal insulin6.5%-8.5% Combination therapy withmeglitinide, sulfonylurea, α-glucosidase inhibitor,metformin, thiazolidinedione,exenatide, premixed insulinanalogs, rapid-acting insulinanalogs or basal insulin>8.5% Monotherapy or combinationtherapyInitiate combination therapy:• Metformin plus sulfonylurea ormeglitinide• Metformin plus thiazolidinedione or α-glucosidase inhibitor• Thiazolidinedione plus sulfonylurea• Incretin mimetic (exenatide) plusmetformin and/or sulfonylurea• Basal or premixed insulin analogs• Other approved interventionRapid-acting insulin analogs may be added toany intervention at any time to addresspersistent postprandial hyperglycemiaMaximize combination therapyMaximize insulin therapy• Add basal insulin if FPG is elevated• Add bolus insulin if PPG is elevated• If both FPG and PPG are elevated, addeither basal-bolus insulin or premixedinsulin analogs• Add exenatide to patients on metforminand/or sulfonylureaInitiate basal-bolus insulin therapy• Long-acting plus rapid-acting insulin• Premixed insulin analogsPharmacologic Prevention of Type 2 DiabetesFood and Drug Administration (FDA) ApprovedNon-FDA ApprovedOrlistatMetforminThiazolidinedioneα-glucosidase inhibitorPrepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.496
References:1. Oki JC, Isley WL. Diabetes Mellitus. In: Pharmacotherapy. A Pathophysiologic Approach, 5 th ed. Dipiro JT,Talbert RL, Yee GC, et al, eds. New York: McGraw-Hill; 2002: 1335-1358.2. Novartis Pharmacy Benefit Report. Facts and Figures. 2003 Edition. East Hanover, NJ: NovartisPharmaceuticals, 2003.3. McEvoy GK, ed. American Hospital Formulary Services, AHFS Drug Information. Bethesda, MD: AmericanSociety of Health-System Pharmacists; 2006.4. American Diabetes Association. Screening for Type 2 Diabetes. Diabetes Care. 2004 27:S11-145. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulfonylureas or insulincompared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33).Lancet. 1998;352:837-853.6. Davis TME and Colagiuri S. The continuing legacy of the United Kingdom Prospective Diabetes Study. MJA.2004;180(3):104-105.7. The Writing Team For The Diabetes Control And Complications Trial / Epidemiology Of DiabetesInterventions And Complications Research Group. Effect of intensive therapy on the microvascularcomplications of type 1 diabetes mellitus. JAMA. 2002;287(19):2563-2569.8. UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin oncomplications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352:854-865.9. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular andmicrovascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317:703-713.10. United Kingdom Prospective Diabetes Study Group. United Kingdom Prospective Diabetes Study (UKPDS)13: relative efficacy of randomly allocated diet, sulfonylurea, insulin, or metformin in patients with newlydiagnosed non-insulin dependent diabetes followed for three years. BMJ. 1995;310:83-88.11. United Kingdom Prospective Diabetes Study Group. United Kingdom Prospective Diabetes Study (UKPDS)24: A 6-year, randomized, controlled trial comparing sulfonylurea, insulin, and metformin therapy in patientswith newly diagnosed type 2 diabetes that could not be controlled with diet therapy. Ann Intern Med. 1988;128(3):165-175.12. United Kingdom Prospective Diabetes Study Group. United Kingdom Prospective Diabetes Study (UKPDS)28: A randomized trial of efficacy of early addition of metformin in sulfonylurea-treated type 2 diabetics.Diabetes Care. 1998;21(1):87-92.13. Turner RC, Cull CA, Frighi A, et al, from the United Kingdom Prospective Diabetes Study Group. UnitedKingdom Prospective Diabetes Study (UKPDS) 49: Glycemic control with diet, sulfonylurea, metformin, orinsulin in patients with type 2 diabetes mellitus. Progressive requirement for multiple therapies. JAMA.1998;281(21):2005-12.14. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes onthe development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl JMed. 1993;329(14):977-986.15. World Health Organization. Definition, Diagnosis and Classification of Diabetes Mellitus and itsComplications. Part 1: Diagnosis and Classification of Diabetes Mellitus. Availableat:http://whqlibdoc.who.int/hq/1999/WHO_NCD_NCS_99.2.pdf. Accessed February 2, 2006.16. American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2006 29:S43-48.17. Nathan DM, Buse JB, Davidson MB, Heine RJ, et al. Management of hyperglycemia in type 2 diabetes: aconsensus algorithm for the initiation and adjustment of therapy: a consensus statement from the AmericanDiabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2006;29(8):1963-1972.18. American Association of <strong>Clinical</strong> Endocrinologists (AACE). Medical Guidelines for the Management ofDiabetes Mellitus: The AACE System of Intensive Diabetes Self-Management–2002 Update. Endocr Pract.2002;8(Suppl.1):40-82.19. The International Diabetes Federation (IDF) <strong>Clinical</strong> Guidelines Task Force. Global Guideline for Type 2Diabetes. Brussels: International Diabetes Federation, 2005. Available at:http://www.idf.org/webdata/docs/IDF%20GGT2D.pdf. Accessed February 2, 2006.20. Institute for <strong>Clinical</strong> Systems Improvement. Healthcare Guideline: Management of Type 2 Diabetes Mellitus.10th Ed. Available at: http://www.icsi.org/knowledge/detail.asp?catID=29&itemID=182. Accessed February 2,2006.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.497
21. National Institute for <strong>Clinical</strong> Excellence (NICE). <strong>Clinical</strong> Guidelines for Type 2 Diabetes: Management ofBlood Glucose.. Available at: http://www.nice.org.uk/pdf/NICE_full_blood_glucose.pdf. Accessed February 2,2006.22. National Institute for <strong>Clinical</strong> Excellence (NICE). Type 1 Diabetes: Diagnosis and Management of Type 1Diabetes in Children, Young People and Adults. Available at:http://www.nice.org.uk/pdf/CG015NICEguideline.pdf. Accessed February 2, 2006.23. American College of Endocrinologists (ACE)/American Association of <strong>Clinical</strong> Endocrinologists (AACE)Diabetes Recommendations Implementation Conference: Road Map for the Prevention and Treatment of Type2 Diabetes. Available from: www.aace.com/meetings/consensus/odimplementation/roadmap.pdf. Accessed July12, 2006.Prepared by University of Massachusetts Medical School <strong>Clinical</strong> Pharmacy Services for MedMetrics Health Partners, Inc.498