Hydration Management - South Carolina Department of Disabilities ...
Hydration Management - South Carolina Department of Disabilities ...
Hydration Management - South Carolina Department of Disabilities ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Hydration</strong> <strong>Management</strong>56. Fluid intake and output monitoring should be initiated by nursing staff or the primary careprescriber when indicated.a. Fluid intake and urinary output should be recorded on Intake/Output sheet or inthe individual’s record.b. Color, and specific gravity <strong>of</strong> urine should be monitored and recorded using thesecond voiding <strong>of</strong> the morning. Additional specimens may be tested throughout theday.c. The usual range for specific gravity <strong>of</strong> urine is 1.015 – 1.025.d. A specific gravity value greater than or equal to 1.020 implies an underhydratedstate and requires further monitoring. 1e. The upper limit <strong>of</strong> normal for specific gravity is 1.030.7. Oral intake may need to be adjusted during illness and diagnostic testing.8. Unexplained weight gain, pedal edema, neck vein distention or shortness <strong>of</strong> breath maybe an indication <strong>of</strong> overhydration.a. Signs and symptoms <strong>of</strong> overhydration should be reported to the nurse.b. The individual’s condition should be carefully monitored and documented in theindividual’s record.c. Weight as well as Intake and Output should be evaluated on a daily basis anddocumented in the individual’s record.d. The primary care prescriber should be notified <strong>of</strong> the change in status.e. At the discretion <strong>of</strong> the primary care prescriber, fluids may be temporarilyrestricted.GENERAL GUIDELINES1. Everyone should be encouraged to consume adequate amounts <strong>of</strong> fluid each day. Thisincludes all liquids (e.g., ice cream, soup, gelatin, juice, and water) taken by mouth andliquids administered through tube feedings and parenterally. (See Table 2: RecommendedDaily Fluid Intake by Weight.)2. Extra fluid should be provided in hot weather.3. Water should be available at all locations where people reside, work, or participate inrecreational activities.4. New admissions should be weighed weekly for the first 4 weeks to establish a baseline.This includes admissions from other institutions, from the community, or from otherresidential units. Based on history or clinical findings, the nurse, dietitian, or primary careprescriber may determine that a person needs to be weighed more frequently.5. Baseline weights will be documented in the Vital Sign section <strong>of</strong> the Major ProblemsList.6. Any clinical symptoms <strong>of</strong> dehydration should be reported immediately by direct carestaff to nursing staff.a. Direct care staff should receive training to recognize the signs and symptoms <strong>of</strong>dehydration.b. If dehydration is suspected, the nurse will screen urine using a chemical reagentstrip dipped in urine and report the findings to the primary care prescriber. (ACLIA waiver is required from DHEC to conduct laboratory tests usingchemical reagent strips. See References for DHEC mailing address.)c. The primary care prescriber should assess the person’s over-all health status anddetermine the medical plan <strong>of</strong> care.SCDDSN 2006 Revision
<strong>Hydration</strong> <strong>Management</strong>6d. If weight fluctuates by five percent (5%) or more within any given month, theweight should be rechecked for accuracy and the procedures for monitoring weightinitiated. (See Guideline for Dysphagia and Associated Disorders)7. The degree <strong>of</strong> dehydration is classified as mild, marked, severe, or fatal on the basis <strong>of</strong> thepercentage <strong>of</strong> body weight loss. (See Table 3: Degrees <strong>of</strong> Dehydration.)a. If mild dehydration is noted, the following steps may be taken:i. Increase oral fluid intake, if possible. Fluids may be given by a feedingtube, if in place.ii. If there is vomiting, small frequent quantities <strong>of</strong> clear liquids may be giveninitiallyb. If marked or severe dehydration is noted, administration <strong>of</strong> IV fluids may benecessary and the person should be transferred to an acute care facility.8. If someone is acutely ill, and is being transferred to an acute care facility, refer to theGuidelines for Acute Illness and Referral to and Discharge from Acute CareFacilities.9. Every effort should be made to determine the etiology <strong>of</strong> the dehydration. Contributorsmay include:a. Airfluidized beds 4b. Medications 1i. diureticsii. psychotropic (antipsychotics, antidepressants, and anxiolytics)iii. laxativesiv. steroidsv. medications that alter the state <strong>of</strong> consciousnessvi. more than 4 medications10. People may be referred to the Nutritional <strong>Management</strong> Committee at the Regional Centerfor evaluation, diagnosis, and formulation <strong>of</strong> a treatment plan. (See Guideline forDysphagia and Associated Disorders.)11. People who have been dehydrated should be monitored on a regular basis by nursing andprimary care prescriber to assure fluid and weight are restored and maintained.Outcome Factors <strong>of</strong> Successful <strong>Hydration</strong> <strong>Management</strong> Programs1. <strong>Hydration</strong> levels are maintained at appropriate levels.2. The number and severity <strong>of</strong> infections, especially urinary tract infections, decreases.3. The incidence <strong>of</strong> constipation decreases.4. Staff have increased awareness and skill in detecting early signs <strong>of</strong> dehydration.5. Early intervention strategies are implemented to prevent serious complications.6. The necessary parameters are measured and documented to assist in diagnosis andtreatment.7. Monitoring and management <strong>of</strong> dehydration is done in an effective and expeditiousmanner.8. Adequate documentation is found in the individual’s record until the situation isresolved.9. Medical and nursing documentation is clear, concise, and comprehensive.SCDDSN 2006 Revision
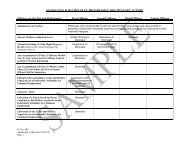
<strong>Hydration</strong> <strong>Management</strong>7Table 1. Relative Strength <strong>of</strong> Different Signs <strong>of</strong> <strong>Hydration</strong> Status in Elderly 1,2Parameter Physical Sign Assessment IndicesDehydration 1,2 Overhydration 2Vital Signs Rapid Pulse ++Orthostatic hypotension +/-Weight Acute increase +++Acute decrease +++Oral mucous membranes Dry, pale, decrease saliva +++Tongue Longitudinal furrows +++Dry +++Skin Turgor Decreased -Eyes Sunken ++Axillary sweat Decreased +Speech Difficulties +++Confusion Acute onset ++Upper body control Muscle weakness ++++Lower extremities Pitting edema ++++Neck veins Distended in supine position +++Note: (+)= some relationship; (++++)= strong relationship; (- )= no relationshipSCDDSN 2006 Revision
<strong>Hydration</strong> <strong>Management</strong>8Table 2. Recommended Daily Fluid Intake by WeightBody WeightKgBody WeightPoundsRecommended TotalFluid Intake per day (mL)Recommended Fluid Intakefrom Liquids per day (mL)10 22.0 1000 75012 26.4 1100 82514 30.8 1200 90016 35.2 1300 97518 39.6 1400 105020 44.0 1500 112522 48.4 1530 114824 52.8 1560 117026 57.2 1590 119328 61.6 1620 121530 66.0 1650 123832 70.4 1680 126034 74.8 1710 128336 79.2 1740 130538 83.6 1770 132840 88.0 1800 135042 92.4 1830 137344 96.8 1860 139546 101.2 1890 141848 105.6 1920 144050 110.0 1950 146352 114.4 1980 148554 118.8 2010 150856 123.2 2040 153058 127.6 2070 155360 132.0 2100 157562 136.4 2130 159864 140.8 2160 162066 145.2 2190 164368 149.6 2220 166570 154.0 2250 168872 158.4 2280 171074 162.8 2310 173376 167.2 2340 1755For each additional 2 Kg body weight (approximately 4.5 pounds) add 30 mL total fluid intake<strong>of</strong> which 22 mL should be from liquids.SCDDSN 2006 Revision
Table 3. Degrees <strong>of</strong> Dehydration 5<strong>Hydration</strong> <strong>Management</strong>9Degree <strong>of</strong> % <strong>of</strong> weight loss SymptomsDehydrationMild 2% ThirstMarked 5% Marked ThirstDry mucous membranesDryness and wrinkling <strong>of</strong> skin – poor skin turgorLow-grade temperature elevationTachycardiaRespirations 28 or greaterDecrease (10-15 mm Hg) in systolic blood pressure instanding positionSlowing <strong>of</strong> venous fillingUrinary output < 25ml/hr (oliguria)Concentrated urineIncreased specific gravity (>1.030)Elevated HctElevated HgbElevated BUNAcid – base equilibrium toward greater acidityBody weight lossSevere 8% Symptoms <strong>of</strong> marked dehydration plus:Flushed skinSystolic blood pressure drop (60 mm Hg or below)Behavioral changes (restlessness, irritability,disorientation, delirium)Fatal22–30% <strong>of</strong> totalbody water losscan prove fatalAnuriaComa leading to deathReferences1. Mentes, J.C. & Iowa Veterans Affairs Nursing Research Consortium (2004, February).<strong>Hydration</strong> <strong>Management</strong> Evidenced-Based Guideline. The University <strong>of</strong> IowaGerontological Nursing Interventions Research Center, Research Translation andDissemination Core. Iowa City, IA: University <strong>of</strong> Iowa.2. Mentes, J.C. & Iowa Veterans Affairs Nursing Research Consortium (1998, September).<strong>Hydration</strong> <strong>Management</strong> Research-Based Protocol. The University <strong>of</strong> Iowa GerontologicalNursing Interventions Research Center, Research Dissemination Core. Iowa City, IA:University <strong>of</strong> Iowa.3. Chidester, J. & Spangler, A. (1997). Fluid intake in the institutionalized elderly. Journal <strong>of</strong>the American Dietetic Association, 97, 23-28.4. Campbell, S.M. (1998). Inquire here. Support Line, 20(1), 17.SCDDSN 2006 Revision
<strong>Hydration</strong> <strong>Management</strong>105. Kee, J.L, & Paulanka, B. J. (2000). Fluids and Electrolytes with Clinical Applications: AProgrammed Approach. (6 th Ed.). Albany, NY: Delmar.To obtain information about the CLIA waiver please contact:<strong>South</strong> <strong>Carolina</strong> <strong>Department</strong> <strong>of</strong> Health and Environmental Control (DHEC)Bureau <strong>of</strong> Certification/CLIA2600 Bull StreetColumbia, SC 29201Phone: 803-545-4291SCDDSN 2006 Revision