PDF 32 KB / 2 pages - Promoting Excellence in End-of-Life Care
PDF 32 KB / 2 pages - Promoting Excellence in End-of-Life Care
PDF 32 KB / 2 pages - Promoting Excellence in End-of-Life Care
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
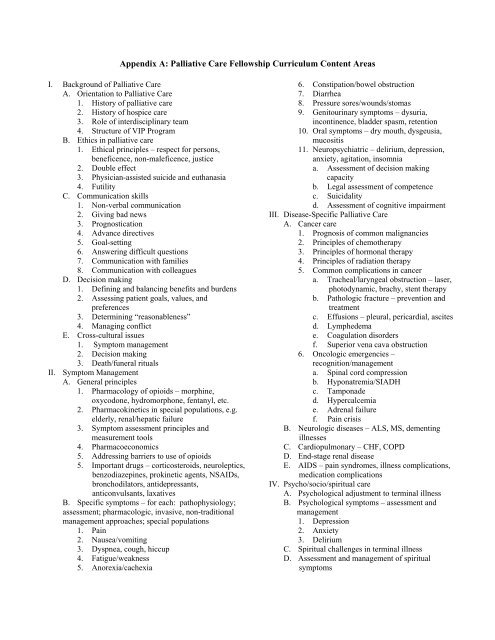
Appendix A: Palliative <strong>Care</strong> Fellowship Curriculum Content AreasI. Background <strong>of</strong> Palliative <strong>Care</strong>A. Orientation to Palliative <strong>Care</strong>1. History <strong>of</strong> palliative care2. History <strong>of</strong> hospice care3. Role <strong>of</strong> <strong>in</strong>terdiscipl<strong>in</strong>ary team4. Structure <strong>of</strong> VIP ProgramB. Ethics <strong>in</strong> palliative care1. Ethical pr<strong>in</strong>ciples – respect for persons,beneficence, non-maleficence, justice2. Double effect3. Physician-assisted suicide and euthanasia4. FutilityC. Communication skills1. Non-verbal communication2. Giv<strong>in</strong>g bad news3. Prognostication4. Advance directives5. Goal-sett<strong>in</strong>g6. Answer<strong>in</strong>g difficult questions7. Communication with families8. Communication with colleaguesD. Decision mak<strong>in</strong>g1. Def<strong>in</strong><strong>in</strong>g and balanc<strong>in</strong>g benefits and burdens2. Assess<strong>in</strong>g patient goals, values, andpreferences3. Determ<strong>in</strong><strong>in</strong>g “reasonableness”4. Manag<strong>in</strong>g conflictE. Cross-cultural issues1. Symptom management2. Decision mak<strong>in</strong>g3. Death/funeral ritualsII. Symptom ManagementA. General pr<strong>in</strong>ciples1. Pharmacology <strong>of</strong> opioids – morph<strong>in</strong>e,oxycodone, hydromorphone, fentanyl, etc.2. Pharmacok<strong>in</strong>etics <strong>in</strong> special populations, e.g.elderly, renal/hepatic failure3. Symptom assessment pr<strong>in</strong>ciples andmeasurement tools4. Pharmacoeconomics5. Address<strong>in</strong>g barriers to use <strong>of</strong> opioids5. Important drugs – corticosteroids, neuroleptics,benzodiazep<strong>in</strong>es, prok<strong>in</strong>etic agents, NSAIDs,bronchodilators, antidepressants,anticonvulsants, laxativesB. Specific symptoms – for each: pathophysiology;assessment; pharmacologic, <strong>in</strong>vasive, non-traditionalmanagement approaches; special populations1. Pa<strong>in</strong>2. Nausea/vomit<strong>in</strong>g3. Dyspnea, cough, hiccup4. Fatigue/weakness5. Anorexia/cachexia6. Constipation/bowel obstruction7. Diarrhea8. Pressure sores/wounds/stomas9. Genitour<strong>in</strong>ary symptoms – dysuria,<strong>in</strong>cont<strong>in</strong>ence, bladder spasm, retention10. Oral symptoms – dry mouth, dysgeusia,mucositis11. Neuropsychiatric – delirium, depression,anxiety, agitation, <strong>in</strong>somniaa. Assessment <strong>of</strong> decision mak<strong>in</strong>gcapacityb. Legal assessment <strong>of</strong> competencec. Suicidalityd. Assessment <strong>of</strong> cognitive impairmentIII. Disease-Specific Palliative <strong>Care</strong>A. Cancer care1. Prognosis <strong>of</strong> common malignancies2. Pr<strong>in</strong>ciples <strong>of</strong> chemotherapy3. Pr<strong>in</strong>ciples <strong>of</strong> hormonal therapy4. Pr<strong>in</strong>ciples <strong>of</strong> radiation therapy5. Common complications <strong>in</strong> cancera. Tracheal/laryngeal obstruction – laser,photodynamic, brachy, stent therapyb. Pathologic fracture – prevention andtreatmentc. Effusions – pleural, pericardial, ascitesd. Lymphedemae. Coagulation disordersf. Superior vena cava obstruction6. Oncologic emergencies –recognition/managementa. Sp<strong>in</strong>al cord compressionb. Hyponatremia/SIADHc. Tamponaded. Hypercalcemiae. Adrenal failuref. Pa<strong>in</strong> crisisB. Neurologic diseases – ALS, MS, dement<strong>in</strong>gillnessesC. Cardiopulmonary – CHF, COPDD. <strong>End</strong>-stage renal diseaseE. AIDS – pa<strong>in</strong> syndromes, illness complications,medication complicationsIV. Psycho/socio/spiritual careA. Psychological adjustment to term<strong>in</strong>al illnessB. Psychological symptoms – assessment andmanagement1. Depression2. Anxiety3. DeliriumC. Spiritual challenges <strong>in</strong> term<strong>in</strong>al illnessD. Assessment and management <strong>of</strong> spiritualsymptoms
Appendix A (cont.): Palliative <strong>Care</strong> Fellowship Curriculum Content AreasE. Spiritual management <strong>of</strong> physical symptomsF. Family dynamics <strong>in</strong> life threaten<strong>in</strong>g illnessG. Conduct<strong>in</strong>g family conferencesH. Role <strong>of</strong> complementary therapies – music therapy, art therapy,hypnosis, etc.V. Last Hours <strong>of</strong> <strong>Life</strong>A. Term<strong>in</strong>al restlessnessB. Death rattleC. Term<strong>in</strong>al sedationD. Withdrawal <strong>of</strong> life-susta<strong>in</strong><strong>in</strong>g treatment –ventilator, dialysis, nutrition/hydrationVI. BereavementA. Normal and pathologic grief responses – patientand familyB. Predict<strong>in</strong>g pathologic grief responseC. Manag<strong>in</strong>g pathologic grief responseD. Interpr<strong>of</strong>essional bereavement careE. Management <strong>of</strong> pr<strong>of</strong>essional grief reactionsF. Community services for grief supportVII. Cultural/Religious Traditions <strong>in</strong> <strong>End</strong>-<strong>of</strong>-<strong>Life</strong> <strong>Care</strong>A. Christian – Catholic, Protestant (traditional,fundamentalist, African-American)B. Jewish – Orthodox, Conservative, ReformC. Eastern religions – Buddhist, H<strong>in</strong>du, Taoist, otherD. MuslimVIII. Discharge Plann<strong>in</strong>gA. Cost issues1. Medications2. Palliative care services – home care, hospice, prosthetics3. F<strong>in</strong>anc<strong>in</strong>g <strong>of</strong> services – VA, Medicare, Medical/Medicare,managed care, etc.4. Cost-efficiency <strong>of</strong> <strong>in</strong>patient/outpatient/home services5. Appropriate use <strong>of</strong> expensive treatment modalities – cost-benefit<strong>in</strong> term<strong>in</strong>al careB. Home care/hospice1. Legal requirements for home care/hospice2. Role <strong>of</strong> <strong>in</strong>patient hospice/extended care facility3. Management <strong>of</strong> patients <strong>in</strong> home care sett<strong>in</strong>gs4. Pr<strong>of</strong>essional <strong>in</strong>teractions with home care/hospice teamIX. Pediatric Palliative Medic<strong>in</strong>e