Diagnostics and medical and Surgical Treatments
Diagnostics and medical and Surgical Treatments
Diagnostics and medical and Surgical Treatments
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
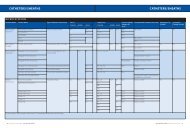
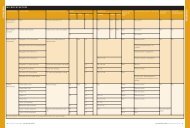
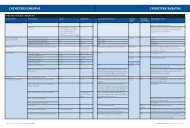
The Road to RecertificationSection Editor: Diana V. Do, MDCompetencies in Glaucoma:<strong>Diagnostics</strong> <strong>and</strong> Medical<strong>and</strong> <strong>Surgical</strong> <strong>Treatments</strong>By Michael Pokabla, DO, MS, <strong>and</strong> Larissa Camejo, MDAs part of the Road to Recertification article series in NewRetina MD, Michael Pokabla, MD, <strong>and</strong> Larissa Camejo,MD, provide an overview of some of the glaucoma topicsthat retina specialists may want to review in more detailfor maintenance of certification. As with every article in thisseries, their overview is not meant to take the place of a comprehensivereview course; rather, its purpose is to highlight somekey areas within the glaucoma subspecialty <strong>and</strong> to encouragea more thorough review prior to taking the Demonstration ofOphthalmic Cognitive Knowledge examination.—Diana V. Do, MD<strong>Diagnostics</strong> <strong>and</strong> Medical<strong>Treatments</strong> for GlaucomaBy Michael Pokabla, DO, MSWhen a patient is being evaluated for glaucoma,I first take a visual field, using the HumphreyVisual Field Analyzer (Carl Zeiss Meditec), whichis a static automated visual field test, or theHumphrey Matrix Perimeter (Carl Zeiss Meditec), whichuses frequency-doubling technology. I also use opticalcoherence tomography (OCT) to image the retinal nervefiber layer. Both of these tests provide a baseline with whichI am able to monitor for progression.Additionally, I measure central corneal thickness with cornealpachymetry to determine whether the patient has anexcessively thin cornea, which can lead to underestimationof intraocular pressure (IOP). I then use Ishihara color platesto help evaluate for optic nerve damage.I will then perform a full pupillary exam <strong>and</strong> a traditionalevaluation of the anterior chamber, paying attention toexternal <strong>and</strong> internal structures in the anterior chamber forclues that may provide a picture of any possible preexistingdisease processes.After I have performed these diagnostic tests, I useGoldman applanation tonometry to measure the patient’sIOP. For patients who cannot physically undergo Goldmanapplanation tonometry, I use a tonopen.After taking the patient’s IOP, I use gonioscopy to examinethe trabecular meshwork to see if there is an obstructioninhibiting aqueous outflow that may be affecting the IOP.I traditionally use the Zeiss indirect goniolens (Carl ZeissMeditec). A goniolens employs prisms in the place of mirrors,allowing visualization of the 4 quadrants of the eye.I then dilate the patient’s eyes <strong>and</strong> use indirect ophthalmoscopyto perform a full evaluation of the optic nerve,which is of prime importance in glaucoma. I evaluate the cupto-discratio, paying special attention to the thickness <strong>and</strong>thinness of the superior <strong>and</strong> inferior neuroretinal rim. Thecolor of the optic nerve, its size, <strong>and</strong> the presence of any hemorrhagesare noted, as well as whether the nerve is excessivelytilted, or whether peripapillary atrophy is present, all of whichare potential indicators of glaucomatous disease.Finally, I perform a full evaluation of the retina looking atthe macula, blood vessels, <strong>and</strong> periphery.Medical <strong>Treatments</strong> for GlaucomaProstagl<strong>and</strong>in analogues (PGAs) are commonly used asfirst-line therapy for glaucoma. Numerous studies validatePGAs for the ability to effectively reduce IOP by enhancingscleral outflow. The most common side effects includechanges in iris color, eyelash growth, <strong>and</strong> darkening of thepigment of the skin around the eye. PGAs are contraindicatedfor patients who have existing macular edema.There are several PGAs currently available, includingbimatoprost (Lumigan, Allergan), latanoprost (Xalatan,Pfizer), tafluprost (Zioptan, Merck), travoprost (Travatan Z,Alcon), <strong>and</strong> generic latanoprost.Alpha adrenergic agonists, carbonic anhydrase inhibitors(CAIs), <strong>and</strong> beta blockers all reduce IOP by inhibiting theproduction of aqueous humor or increasing outflow ofaqueous. Side effects that are associated with this class ofmedication include ocular allergy, dry mouth, drowsiness,<strong>and</strong> increased blood pressure. Alpha adrenergic antagonistsare contraindicated for young children <strong>and</strong> patientswho are taking monoamine oxidase inhibitors.The available alpha adrenergic antagonists include brimonidine(Alphagan, Allergan), apraclonidine, <strong>and</strong> dipivefrin.CAIs can be given in eye drop, oral, or intravenous (IV) form.These drugs work well with PGAs. Side effects of CAI eye8 New Retina MD • Summer 2013
The Road to RecertificationCryotherapy has become less common as it affects surroundingtissue, whereas a laser concentrates its energy more directly.CPC is generally reserved for patients who have peripheralrefractory glaucoma that is unresponsive to therapy who arenot c<strong>and</strong>idates for incisional surgery. It is also indicated forpatients with neovascular glaucoma, high IOP, pain, or lowvisual potential.The technique for CPC using a diode laser is to position theG probe at the limbus, ensuring that the footplate is contactingthe ocular surface. Generally, 8 burns per quadrant areplaced, treating 360º or less. The initial power should be setlow <strong>and</strong> increased in increments of approximately 200 mWuntil there is an audible “pop,” indicating that tissue underneathis being affected. The power should be lowered by200 mW to the threshold level to complete the treatment.The time exposure is usually between 2 <strong>and</strong> 4 seconds.Patient counseling is very important with CPC; althoughuncommon, the laser can cause conjunctival burns, painrelated to inflammation, <strong>and</strong> loss of vision. CPC also oftenneeds to be repeated 2 or 3 times to be effective, so patientsshould be made aware of this.Incisional ProceduresTrabeculectomy. When performing a trabeculectomy, somesurgeons prefer to use a retrobulbar block or a peribulbarblock, while others may choose to use a topical anesthesia withsubconjunctival lidocaine. A 6-0 vicryl suture is passed throughthe superior limbal cornea, <strong>and</strong> the eye is infraducted. A conjunctivalperitomy is created superiorly, <strong>and</strong> a conjunctival flapis made at the limbal or fornix base. I prefer to create a conjunctivalperitomy at the fornix base, <strong>and</strong> then dissect all thesub-Tenon <strong>and</strong> super pocket, making a half-thickness scleralflap that is trapezoidal. The flap is then dissected all the way tothe limbus. An antifibrotic agent, such as 5-fluorouracil or mitomycinC (my preference at 0.2 mg to 0.4 mg for 2 minutes), isthen applied, delivering it with a sponge over the sclera or subconjunctivally.After irrigating the antifibrotic agents, I create atemporal paracentesis in the peripheral cornea. I penetrate thehinge of the scleral flap with a Kelly punch <strong>and</strong> then perform aniridectomy. The scleral flap is closed using 2 10-0 nylon suturesat the sides or corners, after which the conjunctival flap isclosed, either in a winged manner or with a running suture.Aqueous shunt surgery. The different types of shunts includevalved or nonvalved <strong>and</strong> the new mini-shunt. Examples of avalved shunt are the Ahmed (New World Medical) <strong>and</strong> theKrupin (Hood Laboratories) shunts. Examples of a nonvalvedshunt include the Baerveldt (Abbott Medical Optics) <strong>and</strong> theMoltenos (IOP Ophthalmics).The technique for implantation of all is these is similar—aretrobulbar or peribulbar block can be used, but sub-Tenonirrigation of a retrobulbar block with a curved 19-gauge cannulainserted subconjunctivally can also be used. The valvesare inserted superotemporally using a superior corneal limbalsuture. The eye is infraducted, <strong>and</strong> a conjunctival peritomybroader than what is employed for trabeculectomy is used tocover the entire temporal quadrant. The area is dissected, <strong>and</strong>the tube is implanted.We usually isolate the superior rectus <strong>and</strong> the lateral rectusmuscle, <strong>and</strong> we implant the tube with the wings underneaththe rectus muscle to avoid hypotony. Using a 23-gauge needle,the tube is inserted through the sclera bevel up. The tube istied at its base with a 7-0 vicryl suture <strong>and</strong> is threaded up intothe anterior chamber. It can also be implanted in the sulcus forpatients who are pseudophakic or through a pars plana incisionfor patients who have undergone vitrectomy.In more severe cases of glaucoma, 2 or 3 shunts areimplanted.New Procedures <strong>and</strong> TechnologyIn the past, glaucoma specialists’ surgical options werelimited to filtering procedures, such as trabeculectomy <strong>and</strong>shunt implantation, but we now have options that includenonpenetrating <strong>and</strong> microinvasive procedures.The ExPress mini-shunt (Alcon) is a device that isimplanted in a microinvasive procedure similar to trabeculectomy.Instead of penetrating into the anterior chamber,a 26-gauge needle is used, <strong>and</strong> the ExPress mini-shunt isinserted at the level of the posterior border.Another newer technology for microinvasive glaucomasurgery is the Trabectome (NeoMedix), which bypasses the trabecularmeshwork to enhance the natural outflow of the aqueoushumor by eliminating the tissue of most resistance, thetrabecular meshwork, <strong>and</strong> the inner wall of Schlemm canal. TheTrabectome uses an electrocautery tip for 90º to 180º throughdirect visualization of the angle through a small corneal incision.The iStent (Glaukos) was also recently approved by theUS Food <strong>and</strong> Drug Administration. The iStent is injectedinto the eye <strong>and</strong> positioned in the trabecular meshwork toenhance the outflow using the natural pathway, similar tothe Trabectome, but without destructing tissue.Canaloplasty (iScience) is a nonpenetrating procedure thatcreates a low-lying bleb or none at all. This procedure is morecomplex than the aforementioned newer procedures as itinvolves creating a scleral flap, dissecting into Schlemm canal,<strong>and</strong> threading a catheter with an illuminated tip 360º followedby a prolene suture. The suture ties into Schlemm canal <strong>and</strong>dilates it without breaking into Descemet membrane.Combined Cataract <strong>and</strong> Glaucoma SurgeryCombined procedures continue to be a topic of controversyregarding when such a procedure should be performed. Apatient who has a visually significant cataract <strong>and</strong> uncontrolledglaucoma with either progression or high risk for progressiondespite <strong>medical</strong> treatment <strong>and</strong> laser trabeculoplasty would be agood c<strong>and</strong>idate for a combined surgery.Separating these procedures, however, has advantagesin that the level of inflammation from surgery is lowered.Performing a cataract surgery first <strong>and</strong> allowing the eye to10 New Retina MD • Summer 2013