Reading materials for conscious sedation - Yale-New Haven Hospital
Reading materials for conscious sedation - Yale-New Haven Hospital
Reading materials for conscious sedation - Yale-New Haven Hospital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
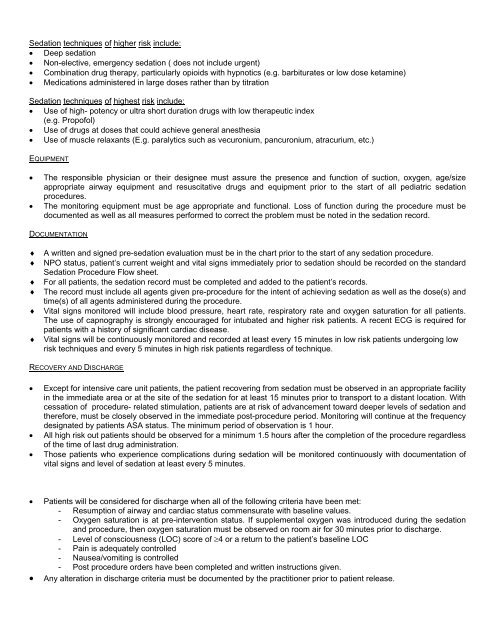
Sedation techniques of higher risk include:• Deep <strong>sedation</strong>• Non-elective, emergency <strong>sedation</strong> ( does not include urgent)• Combination drug therapy, particularly opioids with hypnotics (e.g. barbiturates or low dose ketamine)• Medications administered in large doses rather than by titrationSedation techniques of highest risk include:• Use of high- potency or ultra short duration drugs with low therapeutic index(e.g. Propofol)• Use of drugs at doses that could achieve general anesthesia• Use of muscle relaxants (E.g. paralytics such as vecuronium, pancuronium, atracurium, etc.)EQUIPMENT• The responsible physician or their designee must assure the presence and function of suction, oxygen, age/sizeappropriate airway equipment and resuscitative drugs and equipment prior to the start of all pediatric <strong>sedation</strong>procedures.• The monitoring equipment must be age appropriate and functional. Loss of function during the procedure must bedocumented as well as all measures per<strong>for</strong>med to correct the problem must be noted in the <strong>sedation</strong> record.DOCUMENTATION♦ A written and signed pre-<strong>sedation</strong> evaluation must be in the chart prior to the start of any <strong>sedation</strong> procedure.♦ NPO status, patient’s current weight and vital signs immediately prior to <strong>sedation</strong> should be recorded on the standardSedation Procedure Flow sheet.♦ For all patients, the <strong>sedation</strong> record must be completed and added to the patient’s records.♦ The record must include all agents given pre-procedure <strong>for</strong> the intent of achieving <strong>sedation</strong> as well as the dose(s) andtime(s) of all agents administered during the procedure.♦ Vital signs monitored will include blood pressure, heart rate, respiratory rate and oxygen saturation <strong>for</strong> all patients.The use of capnography is strongly encouraged <strong>for</strong> intubated and higher risk patients. A recent ECG is required <strong>for</strong>patients with a history of significant cardiac disease.♦ Vital signs will be continuously monitored and recorded at least every 15 minutes in low risk patients undergoing lowrisk techniques and every 5 minutes in high risk patients regardless of technique.RECOVERY AND DISCHARGE• Except <strong>for</strong> intensive care unit patients, the patient recovering from <strong>sedation</strong> must be observed in an appropriate facilityin the immediate area or at the site of the <strong>sedation</strong> <strong>for</strong> at least 15 minutes prior to transport to a distant location. Withcessation of procedure- related stimulation, patients are at risk of advancement toward deeper levels of <strong>sedation</strong> andthere<strong>for</strong>e, must be closely observed in the immediate post-procedure period. Monitoring will continue at the frequencydesignated by patients ASA status. The minimum period of observation is 1 hour.• All high risk out patients should be observed <strong>for</strong> a minimum 1.5 hours after the completion of the procedure regardlessof the time of last drug administration.• Those patients who experience complications during <strong>sedation</strong> will be monitored continuously with documentation ofvital signs and level of <strong>sedation</strong> at least every 5 minutes.• Patients will be considered <strong>for</strong> discharge when all of the following criteria have been met:- Resumption of airway and cardiac status commensurate with baseline values.- Oxygen saturation is at pre-intervention status. If supplemental oxygen was introduced during the <strong>sedation</strong>and procedure, then oxygen saturation must be observed on room air <strong>for</strong> 30 minutes prior to discharge.- Level of <strong>conscious</strong>ness (LOC) score of ≥4 or a return to the patient’s baseline LOC- Pain is adequately controlled- Nausea/vomiting is controlled- Post procedure orders have been completed and written instructions given.• Any alteration in discharge criteria must be documented by the practitioner prior to patient release.


![Annual Report Donor Listings [pdf] - Yale-New Haven Hospital](https://img.yumpu.com/49673575/1/190x245/annual-report-donor-listings-pdf-yale-new-haven-hospital.jpg?quality=85)