Reading materials for conscious sedation - Yale-New Haven Hospital
Reading materials for conscious sedation - Yale-New Haven Hospital
Reading materials for conscious sedation - Yale-New Haven Hospital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
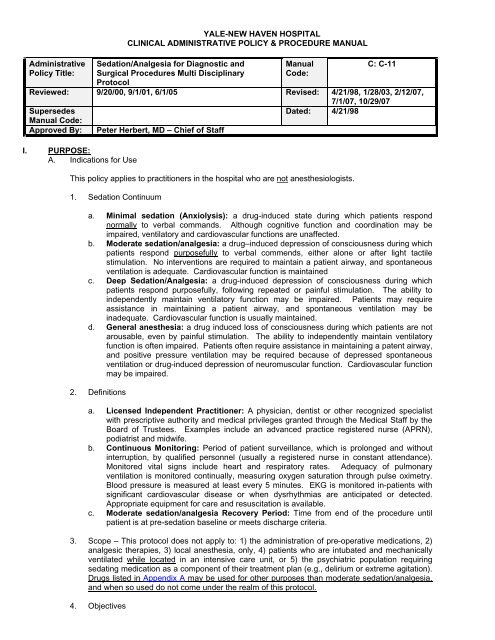
AdministrativePolicy Title:YALE-NEW HAVEN HOSPITALCLINICAL ADMINISTRATIVE POLICY & PROCEDURE MANUALSedation/Analgesia <strong>for</strong> Diagnostic andSurgical Procedures Multi DisciplinaryProtocolManualCode:C: C-11Reviewed: 9/20/00, 9/1/01, 6/1/05 Revised: 4/21/98, 1/28/03, 2/12/07,7/1/07, 10/29/07SupersedesDated: 4/21/98Manual Code:Approved By: Peter Herbert, MD – Chief of StaffI. PURPOSE:A. Indications <strong>for</strong> UseThis policy applies to practitioners in the hospital who are not anesthesiologists.1. Sedation Continuuma. Minimal <strong>sedation</strong> (Anxiolysis): a drug-induced state during which patients respondnormally to verbal commands. Although cognitive function and coordination may beimpaired, ventilatory and cardiovascular functions are unaffected.b. Moderate <strong>sedation</strong>/analgesia: a drug–induced depression of <strong>conscious</strong>ness during whichpatients respond purposefully to verbal commends, either alone or after light tactilestimulation. No interventions are required to maintain a patient airway, and spontaneousventilation is adequate. Cardiovascular function is maintainedc. Deep Sedation/Analgesia: a drug-induced depression of <strong>conscious</strong>ness during whichpatients respond purposefully, following repeated or painful stimulation. The ability toindependently maintain ventilatory function may be impaired. Patients may requireassistance in maintaining a patient airway, and spontaneous ventilation may beinadequate. Cardiovascular function is usually maintained.d. General anesthesia: a drug induced loss of <strong>conscious</strong>ness during which patients are notarousable, even by painful stimulation. The ability to independently maintain ventilatoryfunction is often impaired. Patients often require assistance in maintaining a patent airway,and positive pressure ventilation may be required because of depressed spontaneousventilation or drug-induced depression of neuromuscular function. Cardiovascular functionmay be impaired.2. Definitionsa. Licensed Independent Practitioner: A physician, dentist or other recognized specialistwith prescriptive authority and medical privileges granted through the Medical Staff by theBoard of Trustees. Examples include an advanced practice registered nurse (APRN),podiatrist and midwife.b. Continuous Monitoring: Period of patient surveillance, which is prolonged and withoutinterruption, by qualified personnel (usually a registered nurse in constant attendance).Monitored vital signs include heart and respiratory rates. Adequacy of pulmonaryventilation is monitored continually, measuring oxygen saturation through pulse oximetry.Blood pressure is measured at least every 5 minutes. EKG is monitored in-patients withsignificant cardiovascular disease or when dysrhythmias are anticipated or detected.Appropriate equipment <strong>for</strong> care and resuscitation is available.c. Moderate <strong>sedation</strong>/analgesia Recovery Period: Time from end of the procedure untilpatient is at pre-<strong>sedation</strong> baseline or meets discharge criteria.3. Scope – This protocol does not apply to: 1) the administration of pre-operative medications, 2)analgesic therapies, 3) local anesthesia, only, 4) patients who are intubated and mechanicallyventilated while located in an intensive care unit, or 5) the psychiatric population requiringsedating medication as a component of their treatment plan (e.g., delirium or extreme agitation).Drugs listed in Appendix A may be used <strong>for</strong> other purposes than moderate <strong>sedation</strong>/analgesia,and when so used do not come under the realm of this protocol.4. Objectives
A. It is the goal of the certification process to ensure that those seeking <strong>sedation</strong> privileges arebeing thoroughly assessed and are able to provide to all patients the same standard of patientcare; whether undergoing a diagnostic, surgical, or therapeutic procedure. All individualsresponsible <strong>for</strong> ordering, administering and monitoring of patients receiving <strong>sedation</strong> will berequired to demonstrate competency prior to their privileges being granted or renewed. Thispolicy applies only when <strong>sedation</strong> and analgesia are provided during diagnostic, surgical, orinterventional/therapeutic procedures. It does not apply to clinicians managing painintervention, alcohol withdrawal, or the control of psychiatric disorders (agitation/anxiety). It isnot a policy directed <strong>for</strong> the <strong>sedation</strong> of patients on ventilators or <strong>for</strong> patients administered onlylocal anesthetics.B. The JCAHO has noted that “because <strong>sedation</strong> – to – anesthesia is a continuum, it is not alwayspossible to predict how an individual patient receiving medication with the intent to achievemoderate to deep <strong>sedation</strong> will respond. There<strong>for</strong>e, qualified individuals are trained inprofessional standards and techniques.” In order to be compliant with the stated standards andtechniques, the credentialling process will incorporate required knowledge of these measures.C. All members and affiliates of the Medical Staff with prescriptive authority under Connecticutstature may apply <strong>for</strong> moderate <strong>sedation</strong> privileges. Individual services may allow Housestafffrom the PGY 3 year and above to be credentialled in moderate <strong>sedation</strong>, after fulfillingmandated requirements, and when administered under the general, but not direct supervision ofan Attending Physician.D. Respiratory compromise is the main potential primary complication of moderate <strong>sedation</strong>, andas such, individuals responsible <strong>for</strong> the administration of moderate <strong>sedation</strong> are responsible <strong>for</strong>monitoring, detecting and treating patients who may experience such compromise. Thoseindividuals completing the certification process and being granted privileges <strong>for</strong> moderate<strong>sedation</strong> and analgesia will be required to:1. Submit recent (within four years) Basic Life Support (BLS) or more advanced life supportcertification, or demonstrate acceptable airway management skills.2. Be able to recognize and safely manage anticipated complications associated with themoderate <strong>sedation</strong> and analgesia process.3. Be capable of establishing a patent airway in order to assure adequate oxygenation andventilation.4. Understand and support the process of identifying any and all untoward events anddocument the occurrence and outcome on the appropriate Adverse Events Form. Adverseand sentinel events are to be reported to the Quality Assurance Subcommittee of the <strong>Yale</strong><strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong> (YNHH), Sedation Analgesia Council and/or directed to the Chief ofStaff within a timely fashion.E. Those individuals seeking moderate <strong>sedation</strong> and analgesia privileges must complete theprocess implemented by the YNHH Sedation Analgesia Council. This consists of verifiedunderstanding of basic knowledge concerning administration of moderate <strong>sedation</strong>/analgesia,as well as demonstrated airway management skills. The process parallels the two-yearrecredentialling cycle mandated by the Medical Staff. Individuals being granted privileges <strong>for</strong>moderate <strong>sedation</strong> and analgesia are required to have knowledge or show competency in theitems described below:1. Assure that sufficient numbers of qualified personnel are present during procedures usingmoderate <strong>sedation</strong> and analgesia in order to:a. Appropriately evaluate the patient prior to beginning the procedure using moderate<strong>sedation</strong> and analgesia.b. Provide safe and effective moderate <strong>sedation</strong> and analgesia.c. Safely per<strong>for</strong>m the intended procedure.d. Appropriately monitor the patient (e.g., level of <strong>conscious</strong>ness, and hemodynamics)e. Ensure a safe recovery and discharge of the patient.2. Administer pharmacological agents to predictably achieve desired levels of <strong>sedation</strong>.3. Understand the pharmacology and appropriate utilization of specific antagonists wheneveropioid analgesics or benzodiazepines are being administered <strong>for</strong> <strong>sedation</strong> and analgesia.Monitor patients carefully in order to maintain them at the desired level of <strong>sedation</strong>.Methods and techniques required to rescue those patients who unavoidably orunintentionally progress into a deeper than desired level of <strong>sedation</strong> or analgesia.Manage a compromised airway and to provide adequate oxygenation and ventilation.
If credentialed to provide deep <strong>sedation</strong>, is competent to manage an unstablecardiovascular system as well as a compromised airway and inadequate oxygenation andventilation.Ensure that emergency equipment is immediately accessible in every location wheremoderate or deep <strong>sedation</strong> is to be administered.Order appropriate post-procedural recovery care with nursing monitoring.Adequately and completely document the patient’s response to <strong>sedation</strong> and analgesia inthe patient’s medical record.Support data collection <strong>for</strong> patients having complications of moderate <strong>sedation</strong>, in order toidentify opportunities to improve care.In order to accomplish these basic goals and to be granted moderate <strong>sedation</strong> and analgesiacertification, individuals must:Be familiar with the expected and known possible adverse effects of selected drugs(sedative hypnotics and opioids).Acknowledge that <strong>sedation</strong> is a continuum and that the more alert patient mayunpredictably progress to deeper levels of <strong>sedation</strong>.Be aware of drug administration techniques that have a higher likelihood of resulting inover <strong>sedation</strong> (example: rapid injection, co-drug administration, etc.).
THE YNHH GUIDELINES FOR SEDATION AND ANALGESIA WILL BE BROADLY DIVIDED INTO A TWO (2) TIEREDSYSTEM OF CERTIFICATION AS DESCRIBED BELOWTIER 1 – Privileges <strong>for</strong> Moderate Sedation/Analgesia:Those individuals who qualify <strong>for</strong> Tier 1 certification and wish to be granted privileges <strong>for</strong> administration ofmoderate <strong>sedation</strong> and analgesia during identified procedures must be compliant with the followingdescribed standards:1. Must submit recent BLS or more advanced certification (completed within the past four years) ormust satisfactorily demonstrate airway management skills.2. Show a working knowledge of the drug time to onset and duration of clinical effect <strong>for</strong> those agentssuggested <strong>for</strong> use in TIER 1 which are indicated as follows:a. benzodiazepines (example: midazolam, diazepam, etc)b. opioids (example: fentanyl, morphine sulfate, meperidine, etc.)c. barbiturates (example: pentobarbital)d. reversal agents/antagonists of the above identified drugs (example: naloxone, flumazenil)e. Chloral hydrateNote: Dentists and Oral Surgeons holding a current State of Connecticut Conscious Sedation Permitor Conscious Sedation and Anesthesia Permit fulfill the above criteria and are granted Tier 1privileges without additional examination.TIER 2 – PRIVILEGES FOR DEEP SEDATION AND ANALGESIAThose individuals who qualify <strong>for</strong> Tier 2 certification <strong>for</strong> administration of deep <strong>sedation</strong> and analgesiaduring identified procedures must be compliant with the following described standards:1. Must be an attending physician of either the Department of Anesthesiology, Department of SurgerySection of Emergency Medicine, or is an attending physician with regular and ongoing responsibilitiesas an intensive care unit attending. Appropriate certification in Advanced Cardiac Life Support(ACLS), Advanced Trauma Life Support (ATLS), Pediatric Advanced Life Support (PALS), or theNeonatal Resuscitation Program (NRP) is encouraged. Other Attending physicians currently certifiedin any of the above advanced life support programs, and meeting the following two criteria, may beconsidered to Tier 2 privileges with the approval of the Sedation Analgesia Council.a. Show knowledge and ability to safely and appropriately administer those medications includedin TIER 1 above.b. Show knowledge and ability to safely and appropriately administer those medications in TIER 2which are as follows:1) ketamine2) etomidate3) propofolAt least one member of the team providing moderate <strong>sedation</strong> and analgesia will be required to have acurrent <strong>sedation</strong> and analgesia certification (TIER 1 or TIER 2) during the administration of <strong>sedation</strong> andanalgesia <strong>for</strong> any described procedure.NOTE: General anesthesia is to be delivered only by an anesthesiologist.I have read (and understand) the <strong>conscious</strong> <strong>sedation</strong> guidelines and agree to comply with same:__________________________________________Signature_____/_____/_____Date__________________________________________Printed NameRETURN TO MEDICAL STAFF OFFICE – 1060 CB
APPENDICESAppendix A ……………………………………………………………………………….Moderate Sedation/AnalgesiaAgentsAppendix B ……………………………………………………………………………….JCAHO StandardsAppendix C ………………………………………………………………………………..ASA ClassificationAppendix D ………………………………………………………………………………..NPO GuidelinesAppendix E ………………………………………………………………………………..Emergency EquipmentChecklistAppendix F ………………………………………………………………………………..Pediatric EquipmentChecklistAppendix G ……………………………………………………………………………….Quality Improvement Forms(Adult and Pediatric)Appendix H ………………………………………………………………………………..The Sedation/AnalgesiaProcedure Flow sheetAppendix I …………………………………………………………………………………Consent FormAppendix J …………………………………………………………………………………Criteria <strong>for</strong> ClinicalPrivilegesSUPPLEMENTSThe Pediatric Sedation Supplement <strong>for</strong> <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> Children’s <strong>Hospital</strong>
APPENDIX AP R E F E R R E D A G E N T SU N R E S T R I C T E D S E D A T I O N A G E N T STypical Pediatric dose Typical Adult dose ConsiderationsAgent Route Onset(min)Midazolam(Versed®)Fentanyl(Sublimaze®)Duration(hr)IV 1-5 0.5-1.5PO 10-15PR 10-30IntranasalIVTransmucosa5-30l3-5 0.5-1.06mo-5yo pt: 0.05-0.1 mg/kg/dose, max 1mg; may repeat q3-5min to max total doseof lesser of 0.6 mg/kg or 6 mg6-12yo pt: 0.025-0.05 mg/kg/dose, max 2.5mg; may repeat q3-5min to total dose oflesser of 0.4 mg/kg or 10 mg.1-2 6mo-40 kg pt: 5 mcg/kg.Dose rarely to exceed 400 mcg.0.5-2.5mg/dosemay repeat q3-5 min, total doserarely to exceed 10mg.Not routinely given to adultsNot routinely given to adultsNot routinely given to adults25-50 mcg/dose; may repeat q1-2min. Patients not responding to a 50mcg dose may receive 100 mcgrepeat doses. Total dose >200 mcgrarely needed <strong>for</strong> short procedures;patients undergoing prolongedprocedures (i.e. >45 min) mayrequire up to 400 mcg total dose.Not routinely given to adultsPREFERRED BENZODIAZEPINEReversible with flumazenil.Administer slowly over at least 2minutes to avoid respiratorydepression or apnea.Use smaller doses in debilitated,chronically ill, elderly, or patients withdecreased pulmonary or cardiovascularreserve.Patients with chronic benzodiazepineor alcohol use may require higherdoses.Respiratory depression ispotentiated when combined with anarcotic.PREFERRED OPIATEReversible with naloxone.Use smaller doses in debilitated,chronically ill, elderly, or patients withdecreased pulmonary/cardiovascularreserve.Respiratory depression ispotentiated when combined with abenzodiazepine.Administer slowly over 3-5 minutesto avoid chest wall rigidity.
Flumazenil(Romazicon®)Naloxone(Narcan®)IV 1-3 1-4 20kg: 0.2 mg over at least 15 seconds, mayrepeat after 45 seconds. Additional doses of0.2 mg may be given at 60 second intervals..Maximum cumulative dose 0.05 mg/kg or 1mg whichever is less.IV2-3 0.33-4 10mcg/kg over 30 seconds toreverse <strong>sedation</strong>.May repeat every 2-3 minutes.Larger doses may be required totreat overdose.0.2 mg over at least 15 seconds, mayrepeat in 45 seconds.Additional subsequent doses of 0.2mg may be given at 60 secondintervals. Total dose requiredgenerally not >1mg.20-40 mcg over 30 seconds toreverse <strong>sedation</strong>.May repeat every 2-3 minutes.Larger doses may be required to treatoverdose.REVERSAL AGENT FORBENZODIAZEPINESThe duration of action of flumazenil may be lessthan that of the benzodiazepine. Symptoms mayreappear requiring additional doses of flumazenil.Contraindicated in patients on chronicbenzodiazepines or tricyclic antidepressants (i.e.amitriptyline) in whom intubation is preferred toreversal with this agentUse caution in patients with seizure history.REVERSAL AGENT FOROPIATESMay be administered IM or SC if IVroute unavailable, but onset of effect isslower (i.e. 15 minutes). The durationof action of naloxone may be less thanthat of the opiate. Symptoms mayreappear requiring additional doses ofnaloxone.
UNRESTRICTED SEDATION AGENTSTypical Pediatric dose Typical Adult dose ConsiderationsA L T E R N A T I V E A G E N T SAgent Route Onset(min)Chloralhydrate(Noctec®)Diazepam(Valium®)Meperidine(Demerol®)PO 10-20Duration(hr)4-8 50-75 mg/kg, may repeatafter 30 min if <strong>sedation</strong>inadequate.TOTAL DOSE NOT TOEXCEED 120mg/kg or 1GRAM IN INFANTS and2 GRAMS IN CHILDRENIV 1-3 2-6 0.05-0.1mg/kg/dose, mayrepeat q30 min. Total dosegenerally not >5mgPR 10-30N/A 0.2-0.3mg/kgIV 5 2-4 Not used in pediatricpatientsMorphine IV 5 2-4 0.05-0.1mg/kg/dosemay repeat q10 minNot routinely given to adults For Children over 48 weeks postconceptional age to 3yrs of age and under 30 lbs.No at-home prescribing or administration be<strong>for</strong>earrival to institution <strong>for</strong> procedure.If <strong>sedation</strong> inadequate after 2 nd dose, then mustreschedule <strong>for</strong> future date. Caution! Effects arelong lasting! Consider alternative agent <strong>for</strong> futureprocedure.2-10mg/dose, may repeat q30min.Total dose generally not >30mgNot routinely given to adults25-150mg/dosemay repeat q5 min, rarely toexceed total dose of 300mgRecommended <strong>for</strong> one-timeintra-procedural use only2.5-10mg/dose, may repeatq10 min Total dose requiredgenerally not > 15mgMIDAZOLAM IS PREFERRED BENZODIAZEPINEDiazepam lasts longer than midazolam.Reversible with flumazenil.Administer slowly (i.e. over at least 2-3 min) toavoid respiratory depression/apnea. Re-<strong>sedation</strong>may occur at 6-8 hours due to enterohepaticrecirculation and <strong>for</strong>mation of active metabolite.Respiratory depression is potentiated whencombined with a narcotic.Reversible with naloxone. Contraindicated inpatients receiving MAOI (phenelzine,tranylcypromine, selegeline) within 14 days.Avoid in patients with renal failure or seizurehistory. Administer slowly (i.e. 10mg/min).Respiratory depression is potentiated whencombined with a benzodiazepine.Reversible with naloxone. Administer slowly toavoid respiratory depression or apnea. Use smallerdoses in debilitated, chronically ill, elderly, orpatients with decreased pulmonary or cardiovascularreserve. Respiratory depression ispotentiated when combined with abenzodiazepine.
Pentobarbital(Nembutal®)IV 1 0.25 1-2mg/kg/dose, may Not routinely given to adultsrepeat q5-10 min. Totaldose generally not toexceed lesser of 6mg/kg or150mgPO 15-601-4 2-6mg/kg, max 100mgmay repeat q5-10 minNot routinely given to adultsIM 10- 1-415NO reversal agent available. Administer slowlyover 2-5 minutes to avoid respiratory depression orapnea. Not considered first line agent due to slowonset and long duration of action (especiallyIM/PO route).
R E S T R I C T E D A G E N T SRESTRICTED TO TIER II CREDENTIALED PHYSICIANSNOTE: MDs MUST BE CONTINUOUSLY AT BEDSIDE DURING DRUG ADMINISTRATION!Duration Typical Pediatric dose Typical Adult dose ConsiderationsAgent Route Onset(min)Etomidate(Amidate®)Propofol(Diprivan®)Ketamine(Ketalar®)IV
APPENDIX BJCAHO Standards <strong>for</strong> Sedation and Anesthesia CareAs Evidenced ByTx2 Pre-<strong>sedation</strong> of pre-anesthesia assessment Individualized plan of care, safe administration of<strong>sedation</strong> or anesthesia and interpretation of patientmonitoring.Tx2.1 Moderate or deep <strong>sedation</strong> and anesthesia care isplanned.Tx2.2 Sedation or anesthesia options and risks arediscussed<strong>Hospital</strong> policies, guidelines, standards and medicalrecords (including the flow sheet).In<strong>for</strong>med consent policies and medical records (includingthe flow sheets)Tx2.3 The patient’s physiological status is monitored. Intra-procedure patient monitoring protocols, medicalrecords including special procedures’ room record(including the flow sheet).Tx2.4 Patient’s post-procedural status is assessed onadmission to andBe<strong>for</strong>e discharge from the post-<strong>sedation</strong> or postanesthesiaRecovery area.Tx2.41 Patients are discharged by a qualified, licensedindependentPractitioner or according to approved criteria.<strong>Hospital</strong> polices, guidelines, standards and medicalrecords (including the flow sheet).Standardized criterion <strong>for</strong> discharge including,responsible adult to accompany patient and charteddocumentation as to the findings from the patients’physiological status and outcome of anesthesia.
APPENDIX CAmerican Society of Anesthesiologists ClassificationClassification of Physical StatusASA ClassificationMedical Description of PatientIIIIIIIVVVIA normal healthy patientMild systemic diseaseSevere systemic diseaseSevere systemic disease that is a constant threat to lifeMoribund patient not expected to survive without theoperationPatient declared brain-dead/awaiting organ removal <strong>for</strong>transplantAmerican Society of Anesthesiologists, Manual <strong>for</strong> Anesthesia Department Organization and Management, 1999 Park RidgeIllinois, p. 141
APPENDIX DNPO GuidelinesSUMMARY OF FASTING RECOMMENDATIONS TO REDUCE THE RISK OF PULMONARY ASPIRATION 1Ingested Material Minimum Fasting Period 2Clear liquids 32 hoursBreast milk4 hoursInfant <strong>for</strong>mula6 hoursNon-human milk 46 hoursLight meal 56 hours1 These recommendations apply to healthy patients who are undergoing elective procedures. They are not intended <strong>for</strong>women in labor. Following the guidelines does not guarantee that a complete gastric emptying has occurred.2 The fasting periods noted above apply to all ages.3 Examples of clear liquids include water, fruit juices without pulp, carbonated beverages, clear tea and black coffee.4 Since non-human milk is similar to solids in gastric emptying time, the amount ingested must be considered whendetermining as appropriate fasting time.5 A light meal typically consists of toast and clear liquids. Meals that include fried or fatty foods or meat may prolonggastric emptying time. Both the amount and type of foods ingested must be considered when determining an appropriatefasting period.American Society of Anesthesiologists: 520 North-Northwest Highway, Park Ridge, Illinois 60068-2573.©1999American Society of Anesthesiologists. All rights reserved.
APPENDIX EExample of Emergency Equipment <strong>for</strong> Sedation and Analgesia♦♦♦♦♦ Intravenous equipment• Gloves• Tourniquets• Alcohol swabs• Sterile gauze pads• Intravenous catheters [24- or 22- G]• Intravenous tubing• Intravenous fluid• Three-way stopcocks• Assorted needles <strong>for</strong> drug aspiration, intramuscular injection [interosseous bone marrow needle]• Appropriately sized syringes• TapeBasic airway management equipment• Source of compressed oxygen tank (tank with regulator or pipeline supply with flow meter)• Source of suction• Suction catheters [pediatric suction catheters]• Yankauer- type suction• Face masks (age and size appropriate)• Self-inflating breathing bag-valve set [pediatric]• Oral and nasal airways [infant and child sized airways]• LubricantAdvanced airway management equipment (<strong>for</strong> practitioners with intubation skills)• Laryngoscope handle (checked <strong>for</strong> function)• Laryngoscope blades[ include pediatric]• Endotracheal tubes• Cuffed:6.0, 7.0, or 8.0 mm ID [Uncuffed; 2.5,3.0,3.5, 4.0, 4.5, 5.0, 5.5, or 6.0 mm ID]• Stylet (appropriately size <strong>for</strong> selected endotracheal tubes)Pharmacological antagonists• Naloxone• FlumazenilEmergency medications• Epinephrine• Ephedrine• Atropine• Lidocaine• Glucose, 50% [10% or 25% <strong>for</strong> pediatrics]• Diphenhydramine• Hydrocortisone, methylprednisolone, or dexamethasone• Diazepam or midazolam• Ammonia spirits
APPENDIX FPediatric Sedation Equipment♦♦♦♦♦♦♦♦♦♦♦♦♦♦Ambu bag: Self- inflating with reservoirJackson-Reese Anesthesia bag <strong>for</strong> neonates and small infantsTonsil tip ( Yankauer) suctionSuction catheter and glove set: 6 French, 8 French, 10 FrenchClear face masks: Neonatal, infant, child, small adultGreen oxygen tubingPortable suction if wall suction not availableOral airways: neonatal, infant, childEndotracheal tubesFunctioning laryngoscope and size-appropriate bladesInfusion pump(s)Intravenous tubing: [60 drop micro-drip set]Hand boards <strong>for</strong> securing IVsTapeThis list is appropriate <strong>for</strong> the pediatric subspecialties that provide <strong>sedation</strong> <strong>for</strong> infants and young children atsatellite locations. If any subspecialty anticipates the need to provide <strong>sedation</strong> <strong>for</strong> older children or adolescents,then the standard list of Appendix E should be reviewed in addition to the review of pediatric <strong>sedation</strong>equipment.
UNIT NO.NAME:ADDRESS:DOB:VISIT NO.APPENDIX G(If handwritten, record name, unit no., and DOB)DATE: _______SEX: ___AGE: ____WT:________________DIAGNOSIS:Ordering LIP: _______________PROCEDURE: _____________________________________Medication(s) Used & Dose:Midazolam IV ________mg. Flumazenil _______Fentanyl IV________ mcg.Nalaxone ________Meperidine IV ________mg.Propofol ________ mg.Other _______________________Sedation Events: (Complete only if adverse event occurs)Sedation: Failed (Proc. Cancelled)Inadequate (Pt. Complained of discom<strong>for</strong>t)Over-<strong>sedation</strong> (Proc. delayed due to <strong>sedation</strong>)Prolonged (Proc. Delayed due to <strong>sedation</strong>)Airway:Airway management required (oral, naso-pharyngeal, jawsupport/chin lift, BVM, intubation)circle or specify:_____________________________Difficult airway managementRespiratory:Oxygen Saturation < 5% below baselineWheezing Stridor AspirationResp. Arrest BronchospasmRecovery Events: (Complete only if event is <strong>sedation</strong> related)Airway:Airway management required (oral, naso-pharyngeal, jawsupport/chin lift, BVM, intubation)circle or specify:_____________________________Difficult airway managementRespiratory:Oxygen Saturation < 90% on Room Air (or baseline FIO 2 )Wheezing Stridor AspirationResp. Arrest BronchospasmComments:_____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________Signature: ______________________________________________Printed Name: ___________________________________<strong>Yale</strong> <strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong>Adult Sedation Quality Improvement FormProcedure completed, no reportable occurrences (All ED andfloor <strong>sedation</strong>s must be reported)Reportable occurrence, see <strong>for</strong>mProcedure completed, unexpected admission or elevation incare related to <strong>sedation</strong>: Admission Transfer to ICUPROCEDURE LOCATION: _________________________SEDATION RN: ___________________________________RECOVERY RN: __________________________________Exam:CTUpper EndoscopyMRIColonoscopyNuc. MedPEGCardiac Cath/PTCA ERCPBronchoscopy .Interventional (specify)____________________Other (specify)____________________Area of Body:Head/Neck Spine Thorax Abdomen ExtremityCardiovascular:Bradycardia (140 and 30% above baseline)Arrhythmia specify: ____________________________Hypotension (< 90 syst. and 10% below baseline)Hypertension (> 170 syst., 105 diast., and 10% above baseline)Cardiac ArrestMedication:Medication error specify: _____________________Adverse reaction specify: _____________________Other:Equipment failure Unplanned admissionSeizure Vomiting Corneal AbrasionOther specify: ___________________________________Cardiovascular:Bradycardia (140 and 30% above baseline)Arrhythmia specify: ____________________________Hypotension (< 90 syst. and 10% below baseline)Hypertension (> 170 syst., 105 diast., and 10% above baseline)Cardiac ArrestOther:Equipment failure Unplanned admissionSeizure Vomiting Corneal AbrasionOther specify: ________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________(RN or Sedation Practitioner may complete)
UNIT NO. APPENDIX GNAME:ADDRESS:DOB:VISIT NO.(If handwritten, record name, unit no., DOB, and visit no.)<strong>Yale</strong> <strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong>Pediatric SedationQuality Improvement FormDATE SEX AGE WT____DIAGNOSISPROCEDUREMedication(s) Used & Dose:Midazolam IV ________mg/kgFentanyl IV________ mcg/kgMidazolam PO ________mg/kgChloral Hydrate PO ________mg/kgPentobarbital IV ________ mg/kgPentobarbital PO ________ mg/kgOther _______________________Flumazenil ____________Nalaxone ______________PROCEDURE LOCATIONSEDATION PRACTITIONERRECOVERY RNExam:CTMRIInterventionalNuc. Med.Other (specify)___________________Area of Body:Head/NeckSpineThoraxAbdomenExtremitySedation Events:Sedation: Desired EffectInadequate Over<strong>sedation</strong>Prolonged FailedAirway:Airway management required (oral, naso-pharn., jawsupport/chin lift, BVM, intubation)specify:____________________________________Difficult airway managementRespiratory:Oxygen Saturation < 93% on Room Airresolved on own pt. stimulatedpt. Repositioned oxygen admin.Wheezing Stridor AspirationResp. Arrest BronchospasmRecovery EventsAirway:Airway management required (oral, naso-pharn., jawsupport/chin lift, BVM, intubation)specify:____________________________________Difficult airway managementRespiratory:Oxygen Saturation < 93% on Room Airresolved on own pt. Stimulatedpt. Repositioned oxygen admin.Wheezing Stridor AspirationResp. Arrest BronchospasmDelayed Events:(24hr F/U)Prolonged Drowsiness 24hrsVomiting 24hrsHyperactivity 24hrsIrritability 24hrsOther 24hrsspecify: __________________________________Pt/Family Contacted Yes No MessageCardiovascular:Bradycardia (150 age 2-8y, >125 age >8y)Arrythmia specify: ____________________________Hypotension
APPENDIX H
APPENDIX I – CONSENT FORMYALE-NEW HAVEN HOSPITALPERMISSION FOR OPERATION,SPECIAL PROCEDUREOR TREATMENTF-1696 …. This <strong>for</strong>m can be ordered through the hospital <strong>for</strong>mulary
APPENDIX JYALE NEW HAVEN HOSPITALCRITERIA FOR CLINICAL PRIVILEGES: MODERATE SEDATION/ ANALGESIASedation Analgesia Council <strong>for</strong> 2001-2002Attending physicians and other licensed independent practitioners desiring to obtain privileges to administermoderate <strong>sedation</strong>/analgesia must comply with the following:1) Read, understand and comply with the guidelines <strong>for</strong> administering moderate <strong>sedation</strong>/analgesia as outlined in theSedation/Analgesia Protocol.2) Possess an adequate knowledge, as evidenced by successful completion of testing <strong>materials</strong>, of the clinicalpharmacological aspects of all medications included in the moderate <strong>sedation</strong>/analgesia guidelines (drug dosingrecommendations as per Appendix A - adult, Appendix B - pediatric)3) Possess knowledge and expertise in airway management skills. For Tier 1 (standard) privileges, has completedappropriate basic/advanced life support training within four years, or has completed YNHH-sponsored airwaymanagement training. For Tier 2 (advanced) privileges, has appropriate expertise defined by appointment inAnesthesia, Section of Emergency Medicine, or is an experienced Intensivist routinely practicing in an ICUenvironment.4) All sedating practitioners utilizing moderate <strong>sedation</strong>/analgesia must comply with all criteria relevant to monitoring,levels of care, medication administration and standards of care as defined in the Sedation/Analgesia Protocol.I have read (and understand) the <strong>sedation</strong>/analgesia guidelines and agree to comply with same:_______________________________________________________________________________SignatureDate____________________________________________Printed NameRETURN TO DEPT. OF PHYSICIAN SERVICES - GB 107
SUPPLEMENTSpecial Considerations <strong>for</strong> Sedation of Pediatric PatientsPURPOSETo maximize the safety and com<strong>for</strong>t of children undergoing diagnostic and therapeutic procedures as outpatientsor inpatients.To provide guidelines that ensure consistent standards of care regardless of location or admission status.To provide tools <strong>for</strong> assessment of and recovery from <strong>sedation</strong> during and after the planned procedure.SCOPEThis policy applies to all patients at the <strong>Yale</strong> <strong>New</strong> <strong>Haven</strong> Children’s <strong>Hospital</strong> who receive anxiolytic, analgesic or hypnoticdrugs (see Appendix A) in an attempt to obtain moderate or deep <strong>sedation</strong> analgesia <strong>for</strong> diagnostic, invasive, or surgicalprocedures on the wards, emergency departments, clinics, radiological suites and other remote locations. This policy doesnot apply to the administration of analgesic, sedative, or hypnotic drugs <strong>for</strong> other indications or to patients residing in theintensive care units who are already continuously monitored and are medicated with sedatives, analgesics, and/or musclerelaxants. Note: patients who are transferred to the intensive care units <strong>for</strong> a procedure with moderate <strong>sedation</strong> are notexempted from this policy.DEFINITIONS• Minimal <strong>sedation</strong>, moderate <strong>sedation</strong>, deep <strong>sedation</strong> and general anesthesia are descriptions of arbitrary points on acontinuum of pharmacologically altered <strong>conscious</strong>ness in which progressive loss of protective reflexes producesprogressive increase in physiologic change and potential risk to the patient.• Please see the Definitions section found in the main text of the YNHH Multidisciplinary Guidelines <strong>for</strong> definitions ofeach of the above-described states of <strong>conscious</strong>ness.• Procedures: Therapeutic and diagnostic maneuvers involving puncture or incision of the skin, insertion of aninstrument or <strong>for</strong>eign body or removal of a device or <strong>for</strong>eign body.• Post-conceptional age is defined to include the gestational age plus the postnatal age and is described in terms ofweeks.• Postmenstrual age is the same as post-conceptional age.• Premature- an infant born be<strong>for</strong>e 37 weeks gestation.• Neonatal – relating to the period immediately following birth and continuing through the first 28 days of life.
•Level of Consciousness Score0 = Unresponsive 3 = Drowsy, but will open eyes when name is calledseveral times1 = Responds to pain 4 = Drowsy, but easily aroused (Responds byopening eyes when name is called)2 = Drowsy, but hard to arouse, needs tactile stimuli 5 = Alert, awake and oriented x 3Developmental Milestones– The natural progression in physical and psychological maturation3 months - Holds head up, reaches <strong>for</strong> familiar objects6 months- Sits unsupported, recognizes a stranger9 months- Crawls, uses pincer grasp12 months- Walks alone, says, “mama” and “dada”, mimics vocal sounds18 months- Runs, scribbles, constructs 2- block towers, points to body parts2 years- Walks up/down steps, uses two- word sentences, builds 6- block towers3 years- Pedals tricycle, uses three-word sentences4 years- Hops, knows colors, copies square5 years- Skips, copies triangle, prints first name, asks word definitions
POLICYAll moderate and deep <strong>sedation</strong> shall be directed by a <strong>sedation</strong> practitioner. A <strong>sedation</strong> practitioner is a licensed physician/ dentist, or licensed independent practitioner, who has delineated clinical privileges to administer procedural <strong>sedation</strong> andwho must be immediately available throughout the procedure and initial recovery period. The responsible practitionermust be present during recovery and must evaluate and document the discharge assessment.The person per<strong>for</strong>ming the procedure must not be the person monitoring the patient.The appropriate use of topical anesthetic creams, iontopheresis of local anesthetics, swaddling, pacifiers, distractiontechniques and other com<strong>for</strong>t measures are encouraged and should be introduced in a timely fashion. These com<strong>for</strong>tmeasures are adjuncts and should not be used as a substitute <strong>for</strong> <strong>sedation</strong> techniques.SEDATION PRACTITIONER REQUIREMENTS AND RESPONSIBILITIESThe practitioner directing moderate <strong>sedation</strong> must:• Demonstrate airway management skills through BLS or other advanced life support training certification within thepast four years. Airway management skills may also be demonstrated in YNHH sponsored airway managementtraining courses.• Be able to display an acceptable degree of knowledge of the effects of sedatives/analgesics via the recognized YNHHcertification process.• Physicians directing intentional deep <strong>sedation</strong> must have the appropriate credentials to practice intentional deep<strong>sedation</strong>.• Not per<strong>for</strong>m concurrent <strong>sedation</strong> procedures and/or concurrently per<strong>for</strong>m the <strong>sedation</strong> and the procedure.• The scope of practice of the Tier II practitioner includes expertise in airway management and <strong>sedation</strong> pharmacology.Tier II practitioners include anesthesiologists, critical care medicine (i.e. ICU) physicians, emergency medicinephysicians and neonatologists and are exempt from the certification process.Please see the appropriate Tier of certification <strong>for</strong> which you are eligible.Sedation Risk Assessment• A <strong>sedation</strong> risk assessment shall be per<strong>for</strong>med immediately prior to the procedure and must address both patient- andtechnique- specific factors. The child’s psychomotor abilities (i.e., developmental milestones) should be noted. Thisassessment must be documented on the standard Sedation Procedure Flow Sheet.• Patients will be described as low risk (ASA class I- II) or high risk (ASA class III or above)• Techniques will be described as low risk , higher risk or highest risk.• Patients ASA class IV or above must have an anesthesiology or critical care medicine consults prior to the <strong>sedation</strong>procedure. Patients ASA class III may need an anesthesiology or critical care medicine consult prior to the <strong>sedation</strong>procedure.• High risk patients include those of ASA class II or higher OR one who is noted to have:• Inadequate NPO time (see Appendix D)• Significant upper airway obstruction (stridor when awake)• Sleep apnea• Mandibular hypoplasia, craniofacial abnormalities or history of upper airway obstruction, or acute facial or cervicaltrauma• Marked gastrointestinal dysfunction (active vomiting, gastroesophageal reflux associated with history of aspirationpneumonia, current intestinal obstruction)• Perfusion derangements such as hypovolemia, cardiac disease, septicemia• Profound pulmonary disease such as pneumonia, hypoxia of new onset or respiratory failure with hypercarbia orother derangement of gas exchange• Intubated/ paralyzed patients• Full term infants less than four months of age• All pre-term infants who have not reached the age of 60 weeks post- conception (i.e., post- menstrual age)• History of recent <strong>sedation</strong> failure resulting in 1) an adverse event or 2) an escalation of care <strong>for</strong> same procedure• History of documented malignant hyperthermia or neuroleptic syndromeSedation techniques of low risk include:• Anxiolysis achieved with non-pharmacological techniques (e.g. hypnosis)• Moderate <strong>sedation</strong> analgesia with a single agent requiring a single low dose administration
Sedation techniques of higher risk include:• Deep <strong>sedation</strong>• Non-elective, emergency <strong>sedation</strong> ( does not include urgent)• Combination drug therapy, particularly opioids with hypnotics (e.g. barbiturates or low dose ketamine)• Medications administered in large doses rather than by titrationSedation techniques of highest risk include:• Use of high- potency or ultra short duration drugs with low therapeutic index(e.g. Propofol)• Use of drugs at doses that could achieve general anesthesia• Use of muscle relaxants (E.g. paralytics such as vecuronium, pancuronium, atracurium, etc.)EQUIPMENT• The responsible physician or their designee must assure the presence and function of suction, oxygen, age/sizeappropriate airway equipment and resuscitative drugs and equipment prior to the start of all pediatric <strong>sedation</strong>procedures.• The monitoring equipment must be age appropriate and functional. Loss of function during the procedure must bedocumented as well as all measures per<strong>for</strong>med to correct the problem must be noted in the <strong>sedation</strong> record.DOCUMENTATION♦ A written and signed pre-<strong>sedation</strong> evaluation must be in the chart prior to the start of any <strong>sedation</strong> procedure.♦ NPO status, patient’s current weight and vital signs immediately prior to <strong>sedation</strong> should be recorded on the standardSedation Procedure Flow sheet.♦ For all patients, the <strong>sedation</strong> record must be completed and added to the patient’s records.♦ The record must include all agents given pre-procedure <strong>for</strong> the intent of achieving <strong>sedation</strong> as well as the dose(s) andtime(s) of all agents administered during the procedure.♦ Vital signs monitored will include blood pressure, heart rate, respiratory rate and oxygen saturation <strong>for</strong> all patients.The use of capnography is strongly encouraged <strong>for</strong> intubated and higher risk patients. A recent ECG is required <strong>for</strong>patients with a history of significant cardiac disease.♦ Vital signs will be continuously monitored and recorded at least every 15 minutes in low risk patients undergoing lowrisk techniques and every 5 minutes in high risk patients regardless of technique.RECOVERY AND DISCHARGE• Except <strong>for</strong> intensive care unit patients, the patient recovering from <strong>sedation</strong> must be observed in an appropriate facilityin the immediate area or at the site of the <strong>sedation</strong> <strong>for</strong> at least 15 minutes prior to transport to a distant location. Withcessation of procedure- related stimulation, patients are at risk of advancement toward deeper levels of <strong>sedation</strong> andthere<strong>for</strong>e, must be closely observed in the immediate post-procedure period. Monitoring will continue at the frequencydesignated by patients ASA status. The minimum period of observation is 1 hour.• All high risk out patients should be observed <strong>for</strong> a minimum 1.5 hours after the completion of the procedure regardlessof the time of last drug administration.• Those patients who experience complications during <strong>sedation</strong> will be monitored continuously with documentation ofvital signs and level of <strong>sedation</strong> at least every 5 minutes.• Patients will be considered <strong>for</strong> discharge when all of the following criteria have been met:- Resumption of airway and cardiac status commensurate with baseline values.- Oxygen saturation is at pre-intervention status. If supplemental oxygen was introduced during the <strong>sedation</strong>and procedure, then oxygen saturation must be observed on room air <strong>for</strong> 30 minutes prior to discharge.- Level of <strong>conscious</strong>ness (LOC) score of ≥4 or a return to the patient’s baseline LOC- Pain is adequately controlled- Nausea/vomiting is controlled- Post procedure orders have been completed and written instructions given.• Any alteration in discharge criteria must be documented by the practitioner prior to patient release.
Patients who must be considered <strong>for</strong> admission are as follows:Admission is required <strong>for</strong> patients who:- Are <strong>for</strong>mer pre-term infants (< 60 weeks) AND undergo initiation of <strong>sedation</strong> after 5 PM- Remain with a LOC score ≤ 3 <strong>for</strong> more than three hoursHave ongoing vomiting, decreased oxygen saturation < 93 % or below baseline pre-<strong>sedation</strong> saturation, uncontrolled painor signs of cardiovascular instability at the conclusion of the usual observation period.Practitioners who choose to alter the admission criteria must be present at the time of discharge and mustdocument time of discharge, patient status at the time of discharge and rationale <strong>for</strong> deviation from guidelines.QUALITY ASSURANCEAll adverse events that occur during the <strong>sedation</strong> or during the recovery period will be reported on a standardized<strong>for</strong>m and must be signed by the person per<strong>for</strong>ming the <strong>sedation</strong>. The practitioner must be listed on the Adverseand Sentinel Events <strong>for</strong>m.Adverse events include, but are not limited to:- Vomiting during the procedure ( Note: a single episode of emesis post- procedure shall be documented in therecord, but does not require QA/QI reporting)- Suspected Aspiration with changes in auscultation and/or oxygen saturation- Cardiopulmonary compromise requiring mechanical or pharmacological intervention- Abandonment of attempted procedure due to patient status- All cases where a code-7 is called, regardless of outcome- DeathThe Department of Pediatrics will per<strong>for</strong>m regular QA/QI <strong>for</strong> <strong>sedation</strong> at least quarterly with oversight by the Chiefof Staff or their designee. The completion of these <strong>for</strong>ms should be per<strong>for</strong>med in a timely manner and it issuggested to occur at the time of the event.This Supplement is devised in accordance with the American Academy of Pediatrics Policy Statement. Guidelines <strong>for</strong> Monitoringand Management of Pediatric Patients During and After Sedation <strong>for</strong> Diagnostic and Therapeutic Procedures (RE9252). Pediatrics89(6):1110-1115, 1992. These AAP guidelines are attached to this document.Prepared by the <strong>Yale</strong> <strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong> Sedation Analgesia CouncilSubcommittee <strong>for</strong> Pediatric SedationBrenda C. McClain, M.D.,ChairpersonClif<strong>for</strong>d Bogue, M.D.Luke Probst, BS, PharmPina Violano, RN, CNEKaren Santucci, M.D. Submitted December 5, 2001


![Annual Report Donor Listings [pdf] - Yale-New Haven Hospital](https://img.yumpu.com/49673575/1/190x245/annual-report-donor-listings-pdf-yale-new-haven-hospital.jpg?quality=85)