election notice form for Connecticut mini-COBRA - ConnectiCare
election notice form for Connecticut mini-COBRA - ConnectiCare
election notice form for Connecticut mini-COBRA - ConnectiCare
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
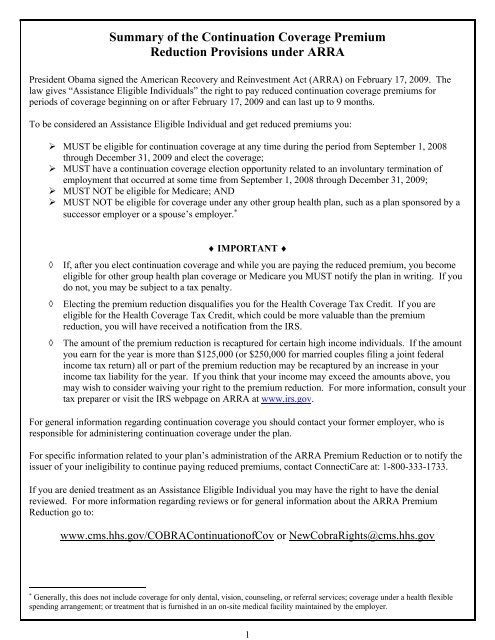
5In considering whether to elect continuation coverage, you should take into account that a failure to continueyour group health coverage will affect your future rights under state and federal law. First, you can lose theright to avoid having preexisting condition exclusions applied to you by other group health plans if you have a150-day gap in health coverage, and <strong>election</strong> of continuation coverage may help prevent such a gap. Second,you will lose the guaranteed right to purchase individual health coverage that does not impose a preexistingcondition exclusion if you do not elect continuation coverage <strong>for</strong> the maximum time available to you. Finally,you should take into account that you have special enrollment rights under federal law. You have the right torequest special enrollment in another group health plan <strong>for</strong> which you are otherwise eligible (such as a plansponsored by your spouse’s employer) within 30 days after your group health coverage ends because of thequalifying event listed above. You will also have the same special enrollment right at the end of continuationcoverage if you get continuation coverage <strong>for</strong> the maximum time available to you.How much does continuation coverage cost?Generally, each qualified beneficiary may be required to pay the entire cost of continuation coverage. Theamount a qualified beneficiary may be required to pay may not exceed 102 percent (or, in the case of anextension of continuation coverage due to a disability, 150 percent) of the cost to the group health plan(including both employer and employee contributions) <strong>for</strong> coverage of a similarly situated plan participant orbeneficiary who is not receiving continuation coverage. The required payment <strong>for</strong> each continuation coverageperiod <strong>for</strong> each option is described in this <strong>notice</strong>.The American Recovery and Reinvestment Act of 2009 (ARRA) reduces the continuation coverage premium insome cases. The premium reduction is available to certain individuals who experience a qualifying event that isan involuntary termination of employment during the period beginning with September 1, 2008 and ending withDecember 31, 2009. If you qualify <strong>for</strong> the premium reduction, you need only pay 35 percent of the continuationcoverage premium otherwise due to the issuer. This premium reduction is available <strong>for</strong> up to nine months. Ifyour continuation coverage lasts <strong>for</strong> more than nine months, you will have to pay the full amount to continueyour continuation coverage. See the attached “Summary of the Continuation Coverage Premium ReductionProvisions under ARRA” <strong>for</strong> more details, restrictions, and obligations as well as the <strong><strong>for</strong>m</strong> necessary toestablish eligibility.The Trade Act of 2002 created a tax credit <strong>for</strong> certain individuals who become eligible <strong>for</strong> trade adjustmentassistance and <strong>for</strong> certain retired employees who are receiving pension payments from the Pension BenefitGuaranty Corporation (PBGC). Under the tax provisions, eligible individuals can either take a tax credit or getadvance payment of 65% of premiums paid <strong>for</strong> qualified health insurance, including continuation coverage.ARRA made several amendments to these provisions, including an increase in the amount of the credit to 80%of premiums <strong>for</strong> coverage be<strong>for</strong>e January 1, 2011 and temporary extensions of the maximum period ofcontinuation coverage <strong>for</strong> PBGC recipients (covered employees who have a non<strong>for</strong>feitable right to a benefit anyportion of which is to be paid by the PBGC) and TAA-eligible individuals. Contact your <strong><strong>for</strong>m</strong>er employer ifyou think you might be eligible <strong>for</strong> the TAA program.If you have questions about these provisions, you may call the Health Coverage Tax Credit Customer ContactCenter toll-free at 1-866-628-4282. TTD/TTY callers may call toll-free at 1-866-626-4282. More in<strong><strong>for</strong>m</strong>ationabout the Trade Act is also available at www.doleta.gov/tradeact.
6When and how must payment <strong>for</strong> continuation coverage be made?Please ask your <strong><strong>for</strong>m</strong>er employer to complete the in<strong><strong>for</strong>m</strong>ation on this page.First payment <strong>for</strong> continuation coverageIf you elect continuation coverage, you do not have to send any payment with the Election Form. However, youmust make your first payment <strong>for</strong> continuation coverage not later than 45 days after the date of your <strong>election</strong>.(This is the date the Election Notice is post-marked, if mailed.) If you do not make your first payment <strong>for</strong>continuation coverage in full not later than 45 days after the date of your <strong>election</strong>, you will lose all continuationcoverage rights under the Plan. You are responsible <strong>for</strong> making sure that the amount of your first payment iscorrect. You may contact your <strong><strong>for</strong>m</strong>er employer or <strong>ConnectiCare</strong> to confirm the correct amount of your firstpayment or to discuss payment issues related to the ARRA premium reduction.Monthly payments <strong>for</strong> continuation coverageAfter you make your first payment <strong>for</strong> continuation coverage, you will be required to make monthly payments.The amount due <strong>for</strong> each month <strong>for</strong> each qualified beneficiary is shown in this <strong>notice</strong> (Section 1B). Under thePlan, each of these monthly payments <strong>for</strong> continuation coverage is due on the first day of the month. If youmake a monthly payment on or be<strong>for</strong>e the first day of the month to which it applies, your coverage under thePlan will continue <strong>for</strong> that month without any break.Grace periods <strong>for</strong> monthly paymentsAlthough monthly payments are due on the dates shown above, you will be given a grace period of 30 daysafter the first day of the month to make each monthly payment. Your continuation coverage will be provided <strong>for</strong>each month as long as payment <strong>for</strong> that month is made be<strong>for</strong>e the end of the grace period <strong>for</strong> that payment.However, if you pay a monthly payment later than the first day of the month to which it applies, but be<strong>for</strong>e theend of the grace period <strong>for</strong> the month, your coverage under the Plan may be suspended as of the first day of themonth and then retroactively reinstated (going back to the first day of the month) when the monthly payment isreceived. This means that any claim you submit <strong>for</strong> benefits while your coverage is suspended may be deniedand may have to be resubmitted once your coverage is reinstated.If you fail to make a monthly payment be<strong>for</strong>e the end of the grace period <strong>for</strong> that month, you will lose all rightsto continuation coverage under the Plan.Your first payment and all monthly periodic payments <strong>for</strong> continuation coverage should be sent to your <strong><strong>for</strong>m</strong>eremployer at:___________________________________________________________________________________________________________________________________________________________________________________________________________________________Your <strong><strong>for</strong>m</strong>er employer will complete Section 1B. If you have questions or want to confirm the correct amountof your first payment, you can contact <strong>ConnectiCare</strong>’s billing Department at 1-800-333-1733.
7For more in<strong><strong>for</strong>m</strong>ationThis <strong>notice</strong> does not fully describe continuation coverage or other rights with respect to your coverage. Morein<strong><strong>for</strong>m</strong>ation about continuation coverage or other rights under the Plan is available in your group healthinsurance certificate or from your <strong><strong>for</strong>m</strong>er employer.If you have any questions concerning the in<strong><strong>for</strong>m</strong>ation in this <strong>notice</strong> or your rights to coverage you shouldcontact your <strong><strong>for</strong>m</strong>er employer. Please ask your <strong><strong>for</strong>m</strong>er employer to put their contact in<strong><strong>for</strong>m</strong>ation here:Continuation Coverage Ad<strong>mini</strong>strator: _______________________________________________________Address: _______________________________________________________________________________Telephone Number: ______________________________________________________________________For more in<strong><strong>for</strong>m</strong>ation about your rights under state law, contact the <strong>Connecticut</strong> Insurance Department,Division of Consumer Affairs at 1-800-203-3447.Keep Your Plan In<strong><strong>for</strong>m</strong>ed of Address ChangesIn order to protect your and your family’s rights, you should keep your <strong><strong>for</strong>m</strong>er employer and <strong>ConnectiCare</strong>in<strong><strong>for</strong>m</strong>ed of any changes in your address and the addresses of family members. You should also keep a copy,<strong>for</strong> your records, of any <strong>notice</strong>s you send to your <strong><strong>for</strong>m</strong>er employer and <strong>ConnectiCare</strong>.
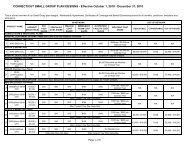
8Section 1B – Bring to <strong><strong>for</strong>m</strong>er employer who will be able to fill in the rate and coverage termapplicable to youIf elected, continuation coverage will begin on ____________________ and can last until ______________.You may elect any of the following options <strong>for</strong> medical coverage under <strong>Connecticut</strong> Continuation coverage: Medical - $ __________ per monthOption AIf you qualify as an “Assistance Eligible Individual”the rate is $ ______________ per month <strong>for</strong> up to9 months.Rate quoted is <strong>for</strong>: Employee$_____________ full premium (A) Employee + Spouse$(-)___________ employer contribution (if any) (B) Employee + 1$(=)___________ subsidy eligible premium (C) Employee + Child(ren) $(-) ___________subsidy premium (65% of C) Family $(=)___________ your monthly premium (35%)---------------------------------------------------------------------------------------------------------------------------------------Section 1CYou do not have to send any payment with the Election Form. Important additional in<strong><strong>for</strong>m</strong>ation about payment<strong>for</strong> continuation coverage is included in the pages following the Election Form.If you have any questions about this <strong>notice</strong> or your rights to continuation coverage, you should contact your<strong><strong>for</strong>m</strong>er employer. Please ask your <strong><strong>for</strong>m</strong>er employer to put their contact in<strong><strong>for</strong>m</strong>ation here:Name of Continuation Coverage Ad<strong>mini</strong>strator: (<strong><strong>for</strong>m</strong>er employer) ___________________________________Address; __________________________________________________________________________________Telephone #: _______________________________________________________________________________
9Section 2A – If you do not have continuation coverage now, use this <strong><strong>for</strong>m</strong> to enrollContinuation Coverage Election FormInstructions: To elect continuation coverage, complete this Election Form and give it to your <strong><strong>for</strong>m</strong>eremployer. You have 60 days after the date of this <strong>notice</strong> to decide whether you want to electcontinuation coverage. Please ask your <strong><strong>for</strong>m</strong>er employer to put their contact in<strong><strong>for</strong>m</strong>ation here:Send completed Election Form to: (<strong><strong>for</strong>m</strong>er employer) _________________________________________Address:________________________________________________________________________________________________This Election Form must be completed and returned to your <strong><strong>for</strong>m</strong>er employer no later than 6/17/09. Ifmailed, it must be post-marked no later than 6/17/09 (60 days from the date of Election Notice.)If you do not submit a completed Election Form by the due date shown above, you will lose your rightto elect continuation coverage. If you reject continuation coverage be<strong>for</strong>e the due date, you may changeyour mind as long as you furnish a completed Election Form be<strong>for</strong>e the due date. However, if youchange your mind after first rejecting continuation coverage, your continuation coverage will begin onthe date you furnish the completed Election Form.I (We) elect continuation coverage in the _____________________________ (the Plan) as indicatedbelow:<strong><strong>for</strong>m</strong>er employer’s group medical planName(First and Last Name)Relationshipto EmployeeSocial SecurityNumberDate ofBirthElectingMedicalYes NoYes NoYes NoYes No_____________________________________Signature______________________________________Print Name__________________________________________________________________________________________________________________Print Address (home mailing address)_____________________________Date_____________________________Relationship to individual(s) listed above______________________________Telephone number
10Section 3A – Request <strong>for</strong> treatment as an assistance eligible individualTo apply <strong>for</strong> ARRA Premium Reduction, complete this <strong><strong>for</strong>m</strong> and return it to your <strong><strong>for</strong>m</strong>er employer along with yourElection Form, (Section 2A if applicable.)You may also send this <strong><strong>for</strong>m</strong> in separately. If you choose to do so, send the completed “Request <strong>for</strong> Treatmentas an Assistance Eligible Individual” to: your <strong><strong>for</strong>m</strong>er employer. Please ask your <strong><strong>for</strong>m</strong>er employer to put theircontact in<strong><strong>for</strong>m</strong>ation below.You may also want to read the important in<strong><strong>for</strong>m</strong>ation about your rights included in the “Summary of theContinuation Coverage Premium Reduction Provisions Under ARRA.”Employer Name:_________________________________________________PERSONAL INFORMATIONName and mailing address of employee (list any dependents on the back ofthis <strong><strong>for</strong>m</strong>)Employer Mailing Address________________________________________________________________________________________________________Telephone numberE-mail address (optional)To qualify, you must be able to check ‘Yes’ <strong>for</strong> all statements.1. The loss of employment was involuntary. Yes No2. The loss of employment occurred at some point on or after September 1, 2008 and on or be<strong>for</strong>e December 31, 2009. Yes No3. I elected (or am electing) continuation coverage. Yes No4. I am NOT eligible <strong>for</strong> other group health plan coverage (or I was not eligible <strong>for</strong> other group health plan coverage Yes Noduring the period <strong>for</strong> which I am claiming a reduced premium).5. I am NOT eligible <strong>for</strong> Medicare (or I was not eligible <strong>for</strong> Medicare during the period <strong>for</strong> which I am claiming a reduced Yes Nopremium).I make an <strong>election</strong> to exercise my right to the ARRA Premium Reduction. To the best of my knowledge and belief all of the answers I haveprovided on this <strong><strong>for</strong>m</strong> are true and correct.Signature__________________________________________________ Date _________________________________________Type or print name__________________________________________ Relationship to employee _________________________Section 3B – Covered dependentsDEPENDENT INFORMATION (Parent or guardian should sign <strong>for</strong> minor children.)Name Date of Birth Relationship to Employee SSN (or other identifier)a. _________________________________________________________________________1. I elected (or am electing) continuation coverage. Yes No2. I am NOT eligible <strong>for</strong> other group health plan coverage. Yes No3. I am NOT eligible <strong>for</strong> Medicare. Yes NoI make an <strong>election</strong> to exercise my right to the ARRA Premium Reduction. To the best of my knowledge and belief all of the answers Ihave provided on this <strong><strong>for</strong>m</strong> are true and correct.Signature __________________________________________________ Date ______________________________________Type or print name__________________________________________ Relationship to employee _________________________
11Name Date of Birth Relationship to Employee SSN (or other identifier)b. _________________________________________________________________________1. I elected (or am electing) continuation coverage. Yes No2. I am NOT eligible <strong>for</strong> other group health plan coverage. Yes No3. I am NOT eligible <strong>for</strong> Medicare. Yes NoI make an <strong>election</strong> to exercise my right to the ARRA Premium Reduction. To the best of my knowledge and belief all of the answers Ihave provided on this <strong><strong>for</strong>m</strong> are true and correct.Signature __________________________________________________ Date ______________________________________Type or print name__________________________________________ Relationship to employee _________________________Name Date of Birth Relationship to Employee SSN (or other identifier)c. _________________________________________________________________________1. I elected (or am electing) continuation coverage. Yes No2. I am NOT eligible <strong>for</strong> other group health plan coverage. Yes No3. I am NOT eligible <strong>for</strong> Medicare. Yes NoI make an <strong>election</strong> to exercise my right to the ARRA Premium Reduction. To the best of my knowledge and belief all of the answers Ihave provided on this <strong><strong>for</strong>m</strong> are true and correct.Signature __________________________________________________ Date ______________________________________Type or print name __________________________________________ Relationship to employee _________________________(If you need space to list additional dependents please make a copy of this page and submit with this <strong><strong>for</strong>m</strong>.)---------------------------------------------------------------------------------------------------------------------------------------Section 3CFORMER EMPLOYER MUST COMPLETEThis application is: Approved Denied Approved <strong>for</strong> some/denied <strong>for</strong> others (explain in #4 below)Specify reason below and then return a copy of this <strong><strong>for</strong>m</strong> to the applicant. If this application is approved, send the original ofthis <strong><strong>for</strong>m</strong> to <strong>ConnectiCare</strong>, Attn: enrollment, at 175 Scott Swamp Road, Farmington, CT 06032REASON FOR DENIAL OF TREATMENT AS AN ASSISTANCE ELIGIBLE INDIVIDUAL1. Loss of employment was voluntary. 2. The involuntary loss did not occur between September 1, 2008 and December 31, 2009. 3. Individual did not elect continuation coverage. 4. Other (please explain here)5. Employer is contributing $ _____________ to coverageThe employer has 19 or fewer employees and is subject to the state continuation laws (“<strong>mini</strong>”-<strong>COBRA</strong>) rather than federal <strong>COBRA</strong> law.Signature of person at employer responsible <strong>for</strong> continuation coverage ad<strong>mini</strong>stration <strong>for</strong> the Planx ______________________________________________________________ Date _________________________________________Type or print name ______________________________________________________________________________________________Telephone number _______________________________________________E-mail address _________________________________
13Participant NotificationThis <strong><strong>for</strong>m</strong> is designed <strong>for</strong> <strong>ConnectiCare</strong> to distribute to qualified beneficiaries who are paying reduced premiumspursuant to ARRA so they can notify <strong>ConnectiCare</strong> if they become eligible <strong>for</strong> other group health plan coverage orMedicare.Use this <strong><strong>for</strong>m</strong> to notify <strong>ConnectiCare</strong> that you are eligible <strong>for</strong> other group health plan coverageor Medicare.<strong>ConnectiCare</strong>175 Scott Swamp Road, Farmington, CT 06032Attn: EnrollmentPERSONAL INFORMATIONName and mailing addressTelephone numberE-mail address (optional)PREMIUM REDUCTION INELIGIBILITY INFORMATION – Check oneI am eligible <strong>for</strong> coverage under another group health plan.If any dependents are also eligible, include their names below.Insert date you became eligible______________________ I am eligible <strong>for</strong> Medicare.Insert date you became eligible______________________ IMPORTANTIf you fail to notify <strong>ConnectiCare</strong> of becoming eligible <strong>for</strong> other group health plan coverage or Medicare ANDcontinue to pay reduced continuation coverage premiums you could be subject to a fine of 110% of the amount ofthe premium reduction.Eligibility is determined regardless of whether you take or decline the other coverage.However, eligibility <strong>for</strong> coverage does not include any time spent in a waiting period.To the best of my knowledge and belief all of the answers I have provided on this <strong><strong>for</strong>m</strong> are true and correct.Signature __________________________________________________ Date ____________________________Type or print name_______________________________________________________________________________If you are eligible <strong>for</strong> coverage under another group health plan and that plan covers dependents you must also list theirnames here:____________________________________________________________________________________________________________________________________________________________________