Novel Applications in Cardiovascular Disease - LifeWave
Novel Applications in Cardiovascular Disease - LifeWave
Novel Applications in Cardiovascular Disease - LifeWave
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
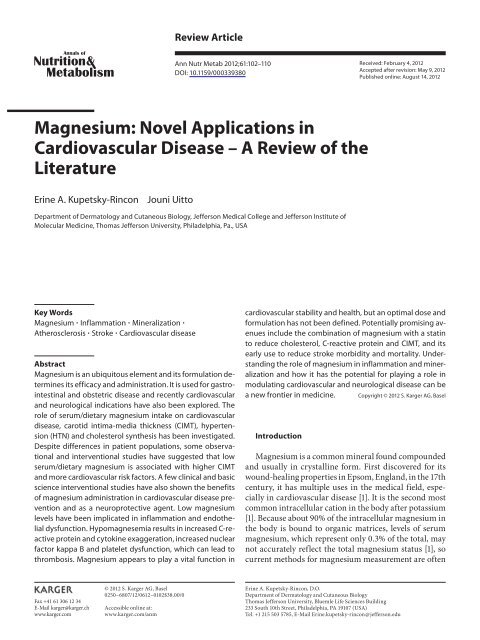
Review ArticleAnn Nutr Metab 2012;61:102–110DOI: 10.1159/000339380Received: February 4, 2012Accepted after revision: May 9, 2012Published onl<strong>in</strong>e: August 14, 2012Magnesium: <strong>Novel</strong> <strong>Applications</strong> <strong>in</strong><strong>Cardiovascular</strong> <strong>Disease</strong> – A Review of theLiteratureEr<strong>in</strong>e A. Kupetsky-R<strong>in</strong>conJouni UittoDepartment of Dermatology and Cutaneous Biology, Jefferson Medical College and Jefferson Institute ofMolecular Medic<strong>in</strong>e, Thomas Jefferson University, Philadelphia, Pa. , USAKey WordsMagnesium Inflammation M<strong>in</strong>eralization Atherosclerosis Stroke <strong>Cardiovascular</strong> diseaseAbstractMagnesium is an ubiquitous element and its formulation determ<strong>in</strong>esits efficacy and adm<strong>in</strong>istration. It is used for gastro<strong>in</strong>test<strong>in</strong>aland obstetric disease and recently cardiovascularand neurological <strong>in</strong>dications have also been explored. Therole of serum/dietary magnesium <strong>in</strong>take on cardiovasculardisease, carotid <strong>in</strong>tima-media thickness (CIMT), hypertension(HTN) and cholesterol synthesis has been <strong>in</strong>vestigated.Despite differences <strong>in</strong> patient populations, some observationaland <strong>in</strong>terventional studies have suggested that lowserum/dietary magnesium is associated with higher CIMTand more cardiovascular risk factors. A few cl<strong>in</strong>ical and basicscience <strong>in</strong>terventional studies have also shown the benefitsof magnesium adm<strong>in</strong>istration <strong>in</strong> cardiovascular disease preventionand as a neuroprotective agent. Low magnesiumlevels have been implicated <strong>in</strong> <strong>in</strong>flammation and endothelialdysfunction. Hypomagnesemia results <strong>in</strong> <strong>in</strong>creased C-reactiveprote<strong>in</strong> and cytok<strong>in</strong>e exaggeration, <strong>in</strong>creased nuclearfactor kappa B and platelet dysfunction, which can lead tothrombosis. Magnesium appears to play a vital function <strong>in</strong>cardiovascular stability and health, but an optimal dose andformulation has not been def<strong>in</strong>ed. Potentially promis<strong>in</strong>g avenues<strong>in</strong>clude the comb<strong>in</strong>ation of magnesium with a stat<strong>in</strong>to reduce cholesterol, C-reactive prote<strong>in</strong> and CIMT, and itsearly use to reduce stroke morbidity and mortality. Understand<strong>in</strong>gthe role of magnesium <strong>in</strong> <strong>in</strong>flammation and m<strong>in</strong>eralizationand how it has the potential for play<strong>in</strong>g a role <strong>in</strong>modulat<strong>in</strong>g cardiovascular and neurological disease can bea new frontier <strong>in</strong> medic<strong>in</strong>e. Copyright © 2012 S. Karger AG, BaselIntroductionMagnesium is a common m<strong>in</strong>eral found compoundedand usually <strong>in</strong> crystall<strong>in</strong>e form. First discovered for itswound-heal<strong>in</strong>g properties <strong>in</strong> Epsom, England, <strong>in</strong> the 17thcentury, it has multiple uses <strong>in</strong> the medical field, especially<strong>in</strong> cardiovascular disease [1] . It is the second mostcommon <strong>in</strong>tracellular cation <strong>in</strong> the body after potassium[1] . Because about 90% of the <strong>in</strong>tracellular magnesium <strong>in</strong>the body is bound to organic matrices, levels of serummagnesium, which represent only 0.3% of the total, maynot accurately reflect the total magnesium status [1] , socurrent methods for magnesium measurement are oftenFax +41 61 306 12 34E-Mail karger@karger.chwww.karger.com© 2012 S. Karger AG, Basel0250–6807/12/0612–0102$38.00/0Accessible onl<strong>in</strong>e at:www.karger.com/anmEr<strong>in</strong>e A. Kupetsky-R<strong>in</strong>con, D.O.Department of Dermatology and Cutaneous BiologyThomas Jefferson University, Bluemle Life Sciences Build<strong>in</strong>g233 South 10th Street, Philadelphia, PA 19107 (USA)Tel. +1 215 503 5785, E-Mail Er<strong>in</strong>e.kupetsky-r<strong>in</strong>con @ jefferson.edu
imprecise. Serum magnesium levels are further divided<strong>in</strong>to ionized, prote<strong>in</strong>-bound and anion-complexed (i.e.magnesium citrate and phosphate) [1] . Convention andpracticality are applied to obta<strong>in</strong> the total magnesiumvalue. Other modalities have been attempted, but arecontroversial. In the blood, erythrocytes conta<strong>in</strong> moremagnesium than serum [2] and studies have shown that<strong>in</strong>tracellular (erythrocyte) magnesium could potentiallybe useful [3–5] . On the frontier of radiological advances,<strong>in</strong>tracellular ionized magnesium <strong>in</strong> body tissues can bemeasured non<strong>in</strong>vasively with nuclear magnetic resonance,but the practicality of this modality for blood measurementmay be questionable due to cost [2, 6] .This review will discuss the most common applicationsof magnesium, its efficacy <strong>in</strong> terms of bioavailabilityand the potential mechanisms of action <strong>in</strong> the cardiovascularsystem. Trial data will demonstrate how magnesiumhas been used to prevent atrial fibrillation,hypertension (HTN), <strong>in</strong>flammation, carotid <strong>in</strong>tima-mediathickness (CIMT) and atherosclerosis, stroke andcoronary heart disease.Magnesium Compounds and EfficacyGenerally, magnesium supplements are found <strong>in</strong> lowquantities <strong>in</strong> multivitam<strong>in</strong>s and over-the-counter laxativepreparations, like magnesium hydroxide or Milk ofMagnesia, or as prescriptions for various other <strong>in</strong>dications.Magnesium oxide and magnesium gluconate, forexample, are orally adm<strong>in</strong>istered and are generally usedto treat mild hypomagnesemia. Magnesium sulfate(MgSO 4 ) is given <strong>in</strong>travenously or <strong>in</strong>tramuscularly and isusually used <strong>in</strong> obstetrics as a tocolytic or <strong>in</strong> the criticallyill sett<strong>in</strong>g to treat severe hypomagnesaemia, whilemagnesium citrate is often used for acute constipation.Patients with renal impairment should be cautious whentak<strong>in</strong>g excessive magnesium supplements and basel<strong>in</strong>ecreat<strong>in</strong><strong>in</strong>e should be assessed. Serum magnesium canalso <strong>in</strong>crease, especially <strong>in</strong> cases of <strong>in</strong>gestion of doses 1 50mEq/day (4.8–7.2 mg/dl), which is rare because of thekidney’s ability to respond to ma<strong>in</strong>ta<strong>in</strong> homeostasis [7] .For practical purposes and for those not critically ill, oralsupplementation is recommended with magnesium oxide,magnesium lactate or magnesium hydroxide [8] .Magnesium L-lactate and L-aspartate are the oralmagnesium compounds that have the greatest bioavailability,are the most water-soluble and have the greatestserum and plasma concentrations [8] . Magnesium can bemade more water-soluble by chelat<strong>in</strong>g it with salicylate,as <strong>in</strong> magnesium salicylate, or with am<strong>in</strong>o acids, such asmagnesium malate, or magnesium diglyc<strong>in</strong>ate [8] . Thelatter two compounds may be beneficial for those patientswith <strong>in</strong>test<strong>in</strong>al resection or complications s<strong>in</strong>ce they havelow gastro<strong>in</strong>test<strong>in</strong>al distress and diarrhea [8, 9] . A studyto determ<strong>in</strong>e the bioavailability of magnesium <strong>in</strong> the ratrevealed that citrate, lactate, aspartate and most organicsalts were more bioavailable than <strong>in</strong>organic salts. Gluconate,however, was the most bioavailable [10] . The authorsof the study concluded that as pH <strong>in</strong>creases, the solubilityand <strong>in</strong>test<strong>in</strong>al bioavailability decrease [10] . The ma<strong>in</strong> sitesfor magnesium absorption <strong>in</strong> both humans and rats arethe ileum and cecum, respectively. As they generally havea higher pH than the proximal <strong>in</strong>test<strong>in</strong>e, organic magnesium-saltexposure may lower the pH, generat<strong>in</strong>g a highersolubility [10] .Magnesium and <strong>Cardiovascular</strong> <strong>Applications</strong>Tables 1–3 summarize the animal and human trialswith magnesium discussed <strong>in</strong> this review.In the scope of us<strong>in</strong>g magnesium <strong>in</strong> cardiovascularmedic<strong>in</strong>e, the data are mostly based on basic science andprecl<strong>in</strong>ical rodent studies with occasional human observationsand some controlled studies.Mechanisms of ActionIn vascular medic<strong>in</strong>e, magnesium <strong>in</strong>duces vascularsmooth-muscle cell relaxation by act<strong>in</strong>g as a mild physiologicalcalcium blocker; <strong>in</strong>creased extracellular magnesiumdecreases <strong>in</strong>tracellular calcium [11, 12] and reducesangiotens<strong>in</strong>-<strong>in</strong>duced aldosterone synthesis, which canlower blood pressure (BP) [12, 13] . It reduces triglyceridesand <strong>in</strong>creases high-density lipoprote<strong>in</strong> (HDL) through<strong>in</strong>creased lipoprote<strong>in</strong> lipase activity, which catabolizestriglyceride lipoprote<strong>in</strong>s and produces HDL [12] . Magnesiumalso <strong>in</strong>hibits HMGCoA reductase, the rate-limit<strong>in</strong>genzyme for cholesterol synthesis, like stat<strong>in</strong> drugs, it isnecessary for lecith<strong>in</strong> cholesterol acyl transferase activity[14] and thus lowers low-density lipoprote<strong>in</strong> (LDL) triglyceridesand raises HDL levels [15] .A possible explanation for the beneficial effects ofmagnesium is based on observations <strong>in</strong> magnesium-deficientanimals. The studies by Mazur et al. [11] demonstratedthat <strong>in</strong> the hypomagnesemic state, the immunesystem of these animals was more likely to have pro<strong>in</strong>flammatory,exaggerated responses marked by elevations<strong>in</strong> C-reactive prote<strong>in</strong>, leukocyte and macrophage activation,nuclear factor kappa B, cytok<strong>in</strong>es and platelet ag-Magnesium <strong>in</strong> <strong>Cardiovascular</strong> <strong>Disease</strong> Ann Nutr Metab 2012;61:102–110 103
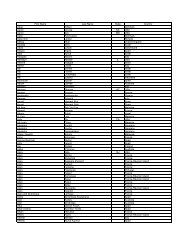
Table 1. S ummary of magnesium basic science and cl<strong>in</strong>ical studiesStudy typeOrganism/patientcharacteristicsDesign Intervention or plan ResultsBasic scienceMazur et al.[11]Basic scienceMar<strong>in</strong>ov et al.[41]Cl<strong>in</strong>icalRe<strong>in</strong>hart et al.[16]Cl<strong>in</strong>icalKawano et al.[17]Cl<strong>in</strong>icalRosanoff [19]Rats <strong>in</strong>terventional blood and organs harvested and analyzedafter 1 week on a severely magnesiumdeficientdietmale rats <strong>in</strong>terventional 30 or 90 mg/kg MgSO 4 or vehicle was<strong>in</strong>jected <strong>in</strong>to the carotid arteries of therats. Middle cerebral artery was occluded,then reperfused after 1.5 or 2 hpatients with elective, isolated1st time coronary artery bypassgraft<strong>in</strong>gJapanese patients who wereeither untreated or already onantihypertensive medicationpatients on antihypertensivetherapy who had stage 1uncomplicated HTN vs. thosepatients who had stage 1 HTNbut who rema<strong>in</strong>ed untreated orwere off their antihypertensivetherapy for at least 4 weeks vs.normotensive patients (systolicBP
Table 2. Summary of magnesium cl<strong>in</strong>ical studiesStudy type Patient characteristics Design Intervention or plan ResultsCl<strong>in</strong>icalSong et al. [20]Cl<strong>in</strong>icalMa et al. [21]female US healthprofessionals ≥45 yearsold <strong>in</strong> the Women’sHealth study, who<strong>in</strong>itially reported normalBPpostmenopausal, 50- to79-year-old womenenrolled <strong>in</strong> the Women’sHealth Initiativeobservational studylargeprospectivecohortfemales participated <strong>in</strong> the study(n = 28,349). Magnesium <strong>in</strong>take wasestimated via the semi-quantitativefood-frequency questionnaire <strong>in</strong> 1993 andmean follow-up was for 9.8 years. Patientsequally divided <strong>in</strong>to qu<strong>in</strong>tiles ofmagnesium <strong>in</strong>take: 256 mg/day (low) to400 mg/day (high)cross-sectional data from women enrolled (n = 1,958)exam<strong>in</strong>ed high-sensitivity C-reactiveprote<strong>in</strong> , IL-6 and TNF- receptor 2 andfood-frequency questionnaire to estimatefiber <strong>in</strong>take for the past 3 monthsBasic science normal rabbits <strong>in</strong>terventional low- or high-magnesium diet with orAltura et al. [23] without a 1 or 2% cholesterol chowBasic scienceLi et al. [28]Kupetsky-R<strong>in</strong>conet al. [29]Cl<strong>in</strong>icalTurgut et al. [32]Cl<strong>in</strong>icalMa et al. [33]after adjustment for confounderswomen <strong>in</strong> the highest qu<strong>in</strong>tile had adecreased HTN risk (p < 0.0001) vs.those <strong>in</strong> the lowest qu<strong>in</strong>tiledecreased IL-6 and TNF- receptor 2were observed and were correlated withan <strong>in</strong>creased <strong>in</strong>take of total fiber andsoluble fiber, which are high <strong>in</strong>magnesiumthe lower the magnesium and thehigher the cholesterol, the greater theatherosclerotic plaque thickness <strong>in</strong> theaortaAbcc6 –/– mice <strong>in</strong>terventional 5-fold magnesium oxide added to diet CIMT decreased 26%. Preventedconnective tissue m<strong>in</strong>eralization <strong>in</strong>Abcc6 –/– micehemodialysis patientsARIC: males/females,blacks/whites, 45–64years olds<strong>in</strong>terventional,RCTtreatment group (n = 32) was given98.6 mg elemental magnesium every otherday for 2 months and control group(n = 12) was given calcium acetate for2 monthscross-sectional blood was drawn from subjects (n =14,982) and analyzed for serummagnesium, cholesterol, glucose and<strong>in</strong>sul<strong>in</strong>. Dietary magnesium <strong>in</strong>take wasqueried by questionnaire. BMI and CIMTmeasurements calculatedmagnesium treatment arm showed astatistically significant drop <strong>in</strong> CIMTover 2 months to 0.70 mm 8 0.2 (p =0.001)low serum/dietary magnesium may berelated to etiologies of cardiovasculardisease, HTN, diabetes andatherosclerosis (elevated CIMT)mended, it is prudent to treat presurgical hypomagnesemia<strong>in</strong> these patients who are predisposed to postoperativeatrial fibrillation [16] .HypertensionSignificant reductions <strong>in</strong> systolic and diastolic BPshave been shown <strong>in</strong> studies where magnesium oxide wasconsumed <strong>in</strong> quantities of 400 mg twice daily [17] ; however,a review of the literature suggests that BP may bereduced further when comb<strong>in</strong>ed with a potassium andlow-sodium <strong>in</strong>take [13] . Another comprehensive analyticalreview also showed that oral magnesium improvedthe BP-lower<strong>in</strong>g effect of the antihypertensive medicationsof patients who were diagnosed with stage 1 HTN,which is def<strong>in</strong>ed by a systolic BP of 140–159 mm Hg or adiastolic BP of 90–99 mm Hg. This effect was <strong>in</strong>creasedwhen the dose was doubled from 230 to 460 mg daily, suggest<strong>in</strong>gthat magnesium supplements above the recommendeddaily allowance [18] may be necessary to significantlylower high BP <strong>in</strong> these patients [19] . F<strong>in</strong>ally, a largeprospective Women’s Health study, composed of femaleUS health professionals aged 6 45 years without previousmyocardial <strong>in</strong>farction, stroke, transient ischemic attackor cancer, who <strong>in</strong>itially reported normal BP (systolic BP! 140 mm Hg, diastolic BP ! 90 mm Hg and no history ofHTN or antihypertensive medication) <strong>in</strong>cluded a semiquantitativefood-frequency questionnaire for daily magnesium<strong>in</strong>take [20] . After a mean follow-up of 9.8 yearsand adjust<strong>in</strong>g for confounders, the authors concludedthat women <strong>in</strong> the highest qu<strong>in</strong>tile (an <strong>in</strong>take of 400 mg/day of magnesium) had a decreased HTN risk (p ! 0.0001)versus those <strong>in</strong> the lowest qu<strong>in</strong>tile (approx. 200 mg/day ofmagnesium) [20] .Magnesium <strong>in</strong> <strong>Cardiovascular</strong> <strong>Disease</strong> Ann Nutr Metab 2012;61:102–110 105
Table 3. S ummary of magnesium cl<strong>in</strong>ical studiesStudy type Patient characteristics Design Intervention or plan ResultsCl<strong>in</strong>icalLiao et al.[39]Cl<strong>in</strong>icalLarsson et al.[40]Cl<strong>in</strong>icalMuir et al.[46]Cl<strong>in</strong>icalSaver et al.[47]Cl<strong>in</strong>icalAbbott et al.[48]ARIC 2: males/females, blacks/whites, 45–64 years oldliterature search on Pubmedand EMBASE for ‘magnesium<strong>in</strong>take’ and ‘stroke’IMAGES: >18 years old,ischemic stroke symptoms ≥1 h,patients could have receivedtissue plasm<strong>in</strong>ogen activatorand bra<strong>in</strong> CT/MRI must havebeen done with<strong>in</strong> 7 days of trialentryFAST-MAG: 45–95 years old,ambulance transported, strokewith<strong>in</strong> ≥15 m<strong>in</strong> of symptoms,≤12 h of treatmentHonolulu Heart Program: men,45–68 years old, of Japaneseancestry liv<strong>in</strong>g <strong>in</strong> Oahu, historyfrom 1965–1968 followed forthe development ofcardiovascular diseaseprospective blood was drawn from subjects (n =13,992) and analyzed for serummagnesium, cholesterol and glucose.Dietary magnesium <strong>in</strong>take was queriedby questionnaire. BMI and BPcalculatedmeta-analysisof prospectivestudiesmulticenter,double-bl<strong>in</strong>ded,placebocontrolled,parallel-groupRCTopen-label,phase-II,feasibility,nonrandomizedcl<strong>in</strong>ical trialobservational7 studies <strong>in</strong>cluded; results (n = 241,348)divided by magnesium <strong>in</strong>take (highest =about 500 mg/day) compared withlowest = about 250 mg/day), and strokerisk factors, years of follow-up, andnumber of casespatients (n = 2,386) randomized toreceive MgSO 4 or normal sal<strong>in</strong>e withmedian treatment time of 7 h ofcl<strong>in</strong>ically diagnosed strokeall enrolled patients (n = 20) received2.5 mg MgSO 4 <strong>in</strong> the field, over 10 m<strong>in</strong>,followed by 1.5 mg, then 16 mg over 24h. Stroke scale performed at hospitalarrival, 24 h, 48 h, 4 days and 90 days.Other assessments donepatients (n = 7,172) divided by qu<strong>in</strong>tilesof magnesium <strong>in</strong>take (low = 50 mg/day,high = 1,138 mg/day) and by <strong>in</strong>cidenceof coronary heart disease (def<strong>in</strong>ed byfatal coronary event and nonfatalmyocardial <strong>in</strong>farction). Coronary heartdisease risk factors were alsoconsidered. Up to 30 years of follow-updata available on each patient<strong>in</strong> women, low serum magnesium wasstrongly related to coronary heart disease,dietary magnesium was weakly associatedto coronary heart disease <strong>in</strong> menafter adjustments for confounders, an<strong>in</strong>crease <strong>in</strong>crement of 100 mg ofmagnesium/day was associated with an 8%decreased risk of total stroke and a 9%decreased risk of ischemic strokeno reduction <strong>in</strong> morbidity or mortality at90 days. The OR for death, the primaryoutcome, was 1.22 <strong>in</strong>dicat<strong>in</strong>g no protectiveeffect of MgSO 4 for ischemic stroke, withCIs cross<strong>in</strong>g the null value, <strong>in</strong>dicat<strong>in</strong>gnonsignificance42% of the patients with
posed to high phosphate to promote vascular calcificationand then <strong>in</strong>cubated <strong>in</strong> either the presence or absenceof magnesium chloride, the presence of magnesium decreasedvascular calcification [25] . While calcium, phosphateand cytok<strong>in</strong>es can promote m<strong>in</strong>eralization or calcification,magnesium is considered an <strong>in</strong>hibitor of vascularcalcification [26, 27] .A study <strong>in</strong> 1990 <strong>in</strong> normal rabbits fed either a low- orhigh-magnesium diet with or without a 1 or 2% cholesterolchow revealed that the lower the magnesium and thehigher the cholesterol, the greater the atheroscleroticplaque thickness <strong>in</strong> the aorta [23] . The aortas were onlym<strong>in</strong>imally thickened <strong>in</strong> the cohort treated with highmagnesium and high cholesterol [23] . These results suggestthat the high dietary magnesium prevented the atheroscleroticplaque formation [1] .The <strong>in</strong>fluence of magnesium on m<strong>in</strong>eralization wasrecently tested <strong>in</strong> a mouse model with an autosomal recessiveectopic m<strong>in</strong>eraliz<strong>in</strong>g disorder, pseudoxanthomaelasticum (PXE), a condition marked with vascular depositsof calcium phosphate [28, 29] . This disease manifestscl<strong>in</strong>ically with HTN, <strong>in</strong>termittent claudication,myocardial <strong>in</strong>farction, stroke, loss of visual acuity, bl<strong>in</strong>dnessand elevated CIMT (a biomarker for atherosclerosis)[30] . This disease has features similar to atherosclerosisand Monckeberg-type arteriosclerosis, or medial stiffen<strong>in</strong>gof the arteries [31] . In humans, there is no effectivetreatment and no validated biomarker for PXE. When aknock-out mouse model for this disease ( Abcc6 –/– ), whichalso shows elevated CIMT, was adm<strong>in</strong>istered with a 5-foldexcess of magnesium oxide <strong>in</strong> its standard rodent chowfor 2 months, the CIMT was significantly reduced by 26%(p = 0.02) [29] . Magnesium, calcium, vitam<strong>in</strong> D and parathyroidhormone levels <strong>in</strong> the blood were normal. Therewas, however, a 10-fold <strong>in</strong>crease <strong>in</strong> calcium and a 77%decrease of phosphorus <strong>in</strong> the ur<strong>in</strong>e of a similar cohort ofmice [28] . Histological exam<strong>in</strong>ation revealed preventionof calcium phosphate deposition <strong>in</strong> the vascular connectivetissues <strong>in</strong> these mice.Because of the success <strong>in</strong> mouse studies, pharmaceutical<strong>in</strong>terventions with dietary magnesium are already be<strong>in</strong>gcontemplated for the treatment of PXE patients. Inaddition, magnesium is already <strong>in</strong> vitam<strong>in</strong> supplements,but the dose that may be safe and cardioprotective andproduce antim<strong>in</strong>eraliz<strong>in</strong>g effects is unknown becauseRCTs are lack<strong>in</strong>g. Results from these studies on PXE, an<strong>in</strong>heritable disorder, may have widespread application <strong>in</strong>cardiovascular medic<strong>in</strong>e and disease prevention as wellas <strong>in</strong> other m<strong>in</strong>eraliz<strong>in</strong>g disorders and nutrition <strong>in</strong> general.Turgut et al. [32] demonstrated that magnesium citratereduces CIMT <strong>in</strong> hemodialysis patients (n = 47). The dosewas 98.6 mg elemental magnesium (8.275 mEq) everyother day for 2 months. Both the treated and the controlgroups of HD patients received calcium acetate as a phosphateb<strong>in</strong>der and a magnesium washout period of 3months prior to the start of the RCT. Both groups of hemodialysispatients had a similar basel<strong>in</strong>e CIMT (0.96mm), but only the magnesium treatment arm showed astatistically significant drop <strong>in</strong> CIMT over 2 months to0.70 mm 8 0.2, (p value = 0.001) [32] . Further translationaland cl<strong>in</strong>ical work is needed to def<strong>in</strong>e the potentialof magnesium and the mechanism of its action <strong>in</strong> reduc<strong>in</strong>gCIMT, not only <strong>in</strong> atherosclerosis but also <strong>in</strong> otherm<strong>in</strong>eraliz<strong>in</strong>g disorders, such as PXE.The Atherosclerosis Risk <strong>in</strong> Communities (ARIC)study, which looked at magnesium dietary <strong>in</strong>take <strong>in</strong> menand women aged 45–64 years, concluded that low dietarymagnesium <strong>in</strong>take and low serum magnesium levels contributedto atherosclerosis development and a meanCIMT <strong>in</strong>crease [33] ; for each 0.1 mmol/l decrease <strong>in</strong> serummagnesium, the CIMT <strong>in</strong>creased 0.0059 mm <strong>in</strong>women who were not on diuretics. This result was significant(p = 0.003) [33] and rema<strong>in</strong>ed so, despite the useof diuretics which can confound results by <strong>in</strong>creas<strong>in</strong>g theur<strong>in</strong>ary excretion of magnesium (0.0124 mm, p = 0.004)[33] . This result was not significant <strong>in</strong> men. Accord<strong>in</strong>g tothe <strong>Cardiovascular</strong> Health Study and NOMAS, normalCIMT ranges vary from 0.7 to 0.9 mm <strong>in</strong> 45- to 75-yearolds[34] and the progression of CIMT – depend<strong>in</strong>g onrisk factors – can range from 0.01 8 0.05 mm/year [35] .If low-serum magnesium can potentially cause a significant<strong>in</strong>crease <strong>in</strong> CIMT <strong>in</strong> women <strong>in</strong> this age range (similarto the pathological progression of CIMT), the risk ofstroke <strong>in</strong>cidence <strong>in</strong>creases as the CIMT rate of change<strong>in</strong>creases [35] , result<strong>in</strong>g <strong>in</strong> <strong>in</strong>creased cardiovascular morbidityand mortality [36–38] .Gender differences with magnesium have also beenfound <strong>in</strong> a second ARIC study <strong>in</strong> 1998, which revealedthat after adjust<strong>in</strong>g for cardiovascular confounders, lowserummagnesium is an <strong>in</strong>dependent predictor of the <strong>in</strong>cidenceof coronary heart disease <strong>in</strong> women (adjustedrelative risk: 1.32 vs. 0.69 <strong>in</strong> men) [39] . Low dietary magnesium,however, was weakly associated with <strong>in</strong>cidentcoronary heart disease <strong>in</strong> men <strong>in</strong> this study [39] . MoreRCT <strong>in</strong>vestigations are needed to determ<strong>in</strong>e the impactof serum magnesium levels and dietary magnesium onatherosclerosis, CIMT and coronary heart disease, especially<strong>in</strong> women.Magnesium <strong>in</strong> <strong>Cardiovascular</strong> <strong>Disease</strong> Ann Nutr Metab 2012;61:102–110 107
St rok eA recent prospective meta-analysis, <strong>in</strong> which the authorsconducted a Pubmed and EMBASE literature reviewfor ‘magnesium <strong>in</strong>take’ and ‘stroke’, identified 7studies published from 1998 to 2011 (241,348 participants<strong>in</strong> total) and found that these stroke patients were on amedian dose of 250 (low)–500 mg (high) of magnesiumper day [40] . After adjustment for stroke risk factors, theconsumption of magnesium at an <strong>in</strong>crement of 100 mg/day, as determ<strong>in</strong>ed by food questionnaires <strong>in</strong> these studies,was <strong>in</strong>versely associated with ischemic stroke [40] .Similar positive results have also been seen <strong>in</strong> basic sciencestudies. Intracarotid adm<strong>in</strong>istration of 3 differentdoses of MgSO 4 <strong>in</strong> rats followed by middle cerebral-arteryocclusion, a model for cerebral ischemia and thenreperfusion, demonstrated neuronal protection or less<strong>in</strong>farct with the higher MgSO 4 dose (p ! 0.001) [41] . Intra-arterialor <strong>in</strong>travenous MgSO 4 may have mechanismsof action <strong>in</strong> the bra<strong>in</strong> that <strong>in</strong>volve <strong>in</strong>hibition of the presynapticrelease of excitatory neurotransmitters, noncompetitiveblock of the N-methyl-D-aspartate receptors,presynaptically potentiate adenos<strong>in</strong>e, block calciumchannels, relax vascular smooth muscle (caus<strong>in</strong>g vasodilationthat <strong>in</strong>creases cerebral blood flow) or antagonizeendothel<strong>in</strong>-1 (a vasoconstrictor) [42] .Although there have been other successful animalstroke or bra<strong>in</strong> <strong>in</strong>jury models with MgSO 4 [43–45] , itsuse for neuroprotection <strong>in</strong> human trials has yielded lessclear results. In the Intravenous Magnesium Efficacy <strong>in</strong>Stroke (IMAGES) trial, a placebo-controlled, doublebl<strong>in</strong>ded,parallel-group, multi-center RCT, where MgSO 4was adm<strong>in</strong>istered to patients with a median time of 7 hto treat cl<strong>in</strong>ically diagnosed ischemic stroke, there wasno reduction <strong>in</strong> morbidity or mortality at 90 days [46] . Itwas postulated that perhaps the reason why translat<strong>in</strong>gthe treatment to humans was not successful was becausethe drug had to be delivered <strong>in</strong> a shorter time span fromthe onset of stroke symptoms because ‘time lost is bra<strong>in</strong>lost’, or that delay of treatment results <strong>in</strong> neuronal death.Design challenges faced by <strong>in</strong>vestigators – to delivertimely care to stroke patients <strong>in</strong> a shorter time-w<strong>in</strong>dow,rapidly identify potential subjects, provide <strong>in</strong>formedconsent, enroll them and assess the degree of stroke severity– led to the Field Adm<strong>in</strong>istration of Stroke Therapy-Magnesium(FAST-MAG) be<strong>in</strong>g <strong>in</strong>itiated [42] . Thefirst FAST-MAG, which was a safety and feasibility nonrandomizedtrial, enrolled 20 patients (80% ischemicand 20% hemorrhagic strokes) and <strong>in</strong>itiated the <strong>in</strong>fusionof MgSO 4 at 100–120 m<strong>in</strong> after diagnosis [47] . At 90days, 42% of the patients with ! 2 h <strong>in</strong>farcts had early recovery,and 69% of all patients and 75% of those patientswith ! 2 h <strong>in</strong>farct achieved good overall global functionaloutcome [47] . There were no serious adverse events[47] . FAST-MAG RCT phase III, which is still ongo<strong>in</strong>g,allows the subject to be rapidly assessed, screened, provideconsent, enrolled and receive the study drug (a bl<strong>in</strong>dstudy kit) <strong>in</strong> under 2 h (while still <strong>in</strong> the ambulance) [42] .Thus far, it has enrolled 73% of patients with ischemicstroke and 24% with hemorrhagic stroke. The trial is impressive<strong>in</strong> that a neuroprotective agent is be<strong>in</strong>g delivered<strong>in</strong> the field <strong>in</strong> the shortest time possible (aka ‘the goldenhour’) prior to patients arriv<strong>in</strong>g at the hospital and receiv<strong>in</strong>gtissue plasm<strong>in</strong>ogen activator (if they are a candidate);this early <strong>in</strong>tervention has the potential to save asmuch bra<strong>in</strong> tissue as possible [42] .Coronary Heart <strong>Disease</strong>The 2003 study <strong>in</strong> Honolulu [48] , which analyzed thefuture risk of coronary heart disease and magnesium <strong>in</strong>takebased on dietary recall, concluded that a higher daily<strong>in</strong>take of magnesium was associated with a lower <strong>in</strong>cidenceof coronary heart disease. Although observationalstudies are helpful at establish<strong>in</strong>g associations, largescale<strong>in</strong>terventional trials or RCTs are required to evaluatethe safety, efficacy and dose ranges of magnesium <strong>in</strong>order to verify a cause and effect hypothesis (e.g. thatmagnesium treats stage 1 HTN). In addition, comparativestudies are needed to determ<strong>in</strong>e how this supplementequates with other drugs currently <strong>in</strong> use for cardiovascular<strong>in</strong>dications.Magnesium – Future <strong>Applications</strong>Because of magnesium’s anti-<strong>in</strong>flammatory, stat<strong>in</strong>likeand anti-m<strong>in</strong>eraliz<strong>in</strong>g effects, a role for it is emerg<strong>in</strong>g<strong>in</strong> cardiovascular and neurological medic<strong>in</strong>e. As <strong>in</strong>dicatedabove, patients with the m<strong>in</strong>eraliz<strong>in</strong>g disorder,PXE, are be<strong>in</strong>g treated with magnesium due to its success<strong>in</strong> animal studies. The actual efficacy of magnesium supplements<strong>in</strong> offsett<strong>in</strong>g the complications of coronaryheart disease, CIMT, HTN, stroke or cardiovascular diseaseis currently unknown, and the optimal dose has notbeen established. As a consequence, larger RCTs areneeded.Because stat<strong>in</strong> drugs have already been approved forlower<strong>in</strong>g cholesterol <strong>in</strong> humans and there are data to supportthe notion that magnesium reduces C-reactive prote<strong>in</strong>levels and also <strong>in</strong>hibits HMG-CoA reductase, <strong>in</strong>directly(like the stat<strong>in</strong>s) [12] , the potential for comb<strong>in</strong><strong>in</strong>g108Ann Nutr Metab 2012;61:102–110Kupetsky-R<strong>in</strong>con/Uitto
magnesium with a stat<strong>in</strong> for a more potent cholesterollower<strong>in</strong>geffect may be worth <strong>in</strong>vestigat<strong>in</strong>g. Magnesium-ATP complex is required for the deactivation or phosphorylationof HMG-CoA reductase, and <strong>in</strong> states of hypomagnesemia,the balance between active and <strong>in</strong>activeforms of HMG-CoA reductase shifts, favor<strong>in</strong>g a hypercholesterolemicstate [15] . S<strong>in</strong>ce magnesium is requiredfor lecith<strong>in</strong> cholesterol transferase, which lowers LDL andtriglycerides and raises HDL, its function to possibly enhanceor to a lesser degree mimic the effect of a stat<strong>in</strong>drug is still to be elucidated [15] . Moreover, the use ofstat<strong>in</strong>s has been proven to reduce CIMT <strong>in</strong> humans [49–51] ; thus, a magnesium-stat<strong>in</strong> comb<strong>in</strong>ation for reducedCIMT might be more efficacious and may reduce morbidityand mortality to a larger extent than a stat<strong>in</strong> only.The future application of magnesium supplementationfor neuroprotective and cardiovascular health for potentiallyreduc<strong>in</strong>g cholesterol, BP, atherosclerosis and CIMTis a much-needed area of study.ConclusionsThe potential impact of magnesium <strong>in</strong> cardiovascularand neurological health, the abundance and low cost of thesupplement, the relatively low side effect profile and thepaucity of <strong>in</strong>formation <strong>in</strong> the literature about this commonm<strong>in</strong>eral suggest that more studies should be conductedto determ<strong>in</strong>e its safety and efficacy. The majority ofhuman trials with magnesium thus far have not been <strong>in</strong>terventional,but based on food questionnaires which maynot be accurate and are subject to a recall bias. Furtherwork is also needed to determ<strong>in</strong>e the mechanism of actionby which magnesium modulates the m<strong>in</strong>eralization and<strong>in</strong>flammation of the cardiovascular and nervous systems.AcknowledgmentsWe would like to thank Dr. Walter K. Kraft, MD, Departmentof Pharmacology and Experimental Therapeutics, Thomas JeffersonUniversity, Philadelphia, Pa. for helpful comments. Ourwork was supported by NIH grants T32 GM008562 (E.A.K.-R.)and R01AR28450 (J.U.).References1 Fawcett WJ, Haxby EJ, Male DA: Magnesium:physiology and pharmacology. Br JAnaesth 1999; 83: 302–320.2 Arnaud MJ: Update on the assessment ofmagnesium status. Br J Nutr 2008; 99(suppl3):S24–S36.3 Simsek E, Karabay M, Kocabay K: Assessmentof magnesium status <strong>in</strong> newly diagnoseddiabetic children: measurement oferythrocyte magnesium level and magnesiumtolerance test<strong>in</strong>g. Turk J Pediatr 2005;47: 132–137.4 Malon A, Brockmann C, Fijalkowska-Morawska J, Rob P, Maj-Zurawska M: Ionizedmagnesium <strong>in</strong> erythrocytes – the bestmagnesium parameter to observe hypo- orhypermagnesemia. Cl<strong>in</strong> Chim Acta 2004;349: 67–73.5 Emelyanov A, Fedoseev G, Barnes PJ: Reduced<strong>in</strong>tracellular magnesium concentrations<strong>in</strong> asthmatic patients. Eur Respir J1999; 13: 38–40.6 Andrade CS, Otaduy MC, Valente KD, MaiaDF, Park EJ, Valerio RM, Tsunemi MH, LeiteCC: Phosphorus magnetic resonance spectroscopy<strong>in</strong> malformations of cortical development.Epilepsia 2011; 52: 2276–2284.7 Moe SM: Disorders <strong>in</strong>volv<strong>in</strong>g calcium, phosphorus,and magnesium. Prim Care 2008; 35:215–237.8 Ranade VV, Somberg JC: Bioavailability andpharmacok<strong>in</strong>etics of magnesium after adm<strong>in</strong>istrationof magnesium salts to humans.Am J Ther 2001; 8: 345–357.9 Schuette SA, Lashner BA, Janghorbani M:Bioavailability of magnesium diglyc<strong>in</strong>ate vsmagnesium oxide <strong>in</strong> patients with ileal resection.J Parenter Enteral Nutr 1994; 18:430–435.10 Coudray C, Rambeau M, Feillet-Coudray C,Gueux E, Tressol JC, Mazur A, RayssiguierY: Study of magnesium bioavailability fromten organic and <strong>in</strong>organic Mg salts <strong>in</strong> Mgdepletedrats us<strong>in</strong>g a stable isotope approach.Magnes Res 2005; 18: 215–223.11 Mazur A, Maier JA, Rock E, Gueux E,Nowacki W, Rayssiguier Y: Magnesium andthe <strong>in</strong>flammatory response: potential physiopathologicalimplications. Arch BiochemBiophys 2007; 458: 48–56.12 Bo S, Pisu E: Role of dietary magnesium <strong>in</strong>cardiovascular disease prevention, <strong>in</strong>sul<strong>in</strong>sensitivity and diabetes. Curr Op<strong>in</strong> Lipidol2008; 19: 50–56.13 Houston M: The role of magnesium <strong>in</strong> hypertensionand cardiovascular disease. JCl<strong>in</strong> Hypertens (Greenwich) 2011; 13: 843–847.14 Rayssiguier Y: Magnesium, lipids and vasculardiseases. Experimental evidence <strong>in</strong> animalmodels. Magnesium 1986; 5: 182–190.15 Rosanoff A, Seelig MS: Comparison ofmechanism and functional effects of magnesiumand stat<strong>in</strong> pharmaceuticals. J Am CollNutr 2004; 23: 501S–505S.16 Re<strong>in</strong>hart K, Baker WL, Siv ML: Beyond theguidel<strong>in</strong>es: new and novel agents for the preventionof atrial fibrillation after cardiothoracicsurgery. J Cardiovasc Pharmacol Ther2011; 16: 5–13.17 Kawano Y, Matsuoka H, Takishita S, OmaeT: Effects of magnesium supplementation <strong>in</strong>hypertensive patients: assessment by office,home, and ambulatory blood pressures. Hypertension1998; 32: 260–265.18 Stand<strong>in</strong>g Committee on the Scientific Evaluationof Dietary Reference Intakes FaNB, Instituteof Medic<strong>in</strong>e Dietary Reference Intakesfor Calcium, Phosphorus, Magnesium,Vitam<strong>in</strong> D and Fluoride. Wash<strong>in</strong>gton, NationalAcademy Press, 1997.19 Rosanoff A: Magnesium supplements mayenhance the effect of antihypertensive medications<strong>in</strong> stage 1 hypertensive subjects.Magnes Res 2010; 23: 27–40.20 Song Y, Sesso HD, Manson JE, Cook NR, Bur<strong>in</strong>gJE, Liu S: Dietary magnesium <strong>in</strong>take andrisk of <strong>in</strong>cident hypertension among middleagedand older US women <strong>in</strong> a 10-year follow-upstudy. Am J Cardiol 2006; 98: 1616–1621.Magnesium <strong>in</strong> <strong>Cardiovascular</strong> <strong>Disease</strong> Ann Nutr Metab 2012;61:102–110 109
21 Ma Y, Hebert JR, Li W, Bertone-Johnson ER,Olendzki B, Pagoto SL, T<strong>in</strong>ker L, Rosal MC,Ockene IS, Ockene JK, Griffith JA, Liu S: Associationbetween dietary fiber and markersof systemic <strong>in</strong>flammation <strong>in</strong> the Women’sHealth Initiative observational study. Nutrition2008; 24: 941–949.22 Galland L: Diet and <strong>in</strong>flammation. NutrCl<strong>in</strong> Pract 2010; 25: 634–640.23 Altura BT, Brust M, Bloom S, Barbour RL,Stempak JG, Altura BM: Magnesium dietary<strong>in</strong>take modulates blood lipid levels and atherogenesis.Proc Natl Acad Sci USA 1990; 87:1840–1844.24 Maier JA: Endothelial cells and magnesium:implications <strong>in</strong> atherosclerosis. Cl<strong>in</strong> Sci(Lond) 2012; 122: 397–407.25 Salem S, Bruck H, Bahlmann FH, Peter M,Passlick-Deetjen J, Kretschmer A, Steppan S,Volsek M, Kribben A, Nierhaus M, JankowskiV, Zidek W, Jankowski J: Relationship betweenmagnesium and cl<strong>in</strong>ical biomarkerson <strong>in</strong>hibition of vascular calcification. Am JNephrol 2012; 35: 31–39.26 Sage A, T<strong>in</strong>tut Y, Garf<strong>in</strong>kel A, Demer L:Systems biology of vascular calcification.Trends Cardiovasc Med 2009; 19: 118–123.27 Luft FC: Vascular calcification and magnesium.J Mol Med (Berl) 2010; 88: 437–439.28 Li Q, Larusso J, Grand-Pierre AE, Uitto J:Magnesium carbonate-conta<strong>in</strong><strong>in</strong>g phosphateb<strong>in</strong>der prevents connective tissue m<strong>in</strong>eralization<strong>in</strong> Abcc6(–/–) mice-potential fortreatment of pseudoxanthoma elasticum.Cl<strong>in</strong> Transl Sci 2009; 2: 398–404.29 Kupetsky-R<strong>in</strong>con EA, Li Q, Uitto J: Magnesiumreduces carotid <strong>in</strong>tima-media thickness<strong>in</strong> a mouse model of pseudoxanthomaelasticum: a novel treatment biomarker. Cl<strong>in</strong>Transl Sci 2012; 5: 259–264.30 Kobolos G AH, Prohaszka Z, Tordai A, VaradiA, Aranyl T: The R1141X loss-of-functionmutation of the ABCC6 gene is a strong geneticrisk factor for coronary artery disease.Genet Test Mol Biomarkers 2010; 14: 75–78.31 Germa<strong>in</strong> DP, Boutouyrie P, Laloux B, LaurentS: Arterial remodel<strong>in</strong>g and stiffness <strong>in</strong> patientswith pseudoxanthoma elasticum. ArteriosclerThromb Vasc Biol 2003; 23: 836–841.32 Turgut F, Kanbay M, Met<strong>in</strong> MR, Uz E, AkcayA, Covic A: Magnesium supplementationhelps to improve carotid <strong>in</strong>tima-mediathickness <strong>in</strong> patients on hemodialysis. IntUrol Nephrol 2008; 40: 1075–1082.33 Ma J, Folsom AR, Melnick SL, Eckfeldt JH,Sharrett AR, Nabulsi AA, Hutch<strong>in</strong>son RG,Metcalf PA: Associations of serum and dietarymagnesium with cardiovascular disease,hypertension, diabetes, <strong>in</strong>sul<strong>in</strong>, and carotidarterial wall thickness: the ARIC study.J Cl<strong>in</strong> Epidemiol 1995; 48: 927–940.34 Walker MD, Fleischer J, Rundek T, McMahonDJ, Homma S, Sacco R, Silverberg SJ: Carotidvascular abnormalities <strong>in</strong> primary hyperparathyroidism.J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab2009; 94: 3849–3856.35 Polak JF, Penc<strong>in</strong>a MJ, O’Leary DH,D’Agost<strong>in</strong>o RB: Common carotid artery <strong>in</strong>tima-mediathickness progression as a predictorof stroke <strong>in</strong> multi-ethnic study of atherosclerosis.Stroke 2011; 42: 3017–3021.36 Simon A, Megnien JL, Chironi G: The valueof carotid <strong>in</strong>tima-media thickness for predict<strong>in</strong>gcardiovascular risk. ArteriosclerThromb Vasc Biol 2010; 30: 182–185.37 O’Leary DH, Bots ML: Imag<strong>in</strong>g of atherosclerosis:carotid <strong>in</strong>tima-media thickness.Eur Heart J 2010; 31: 1682–1689.38 Yamagishi T, Kato M, Koiwa Y, Omata K,Hasegawa H, Kanai H: Evaluation of plaquestabilization by fluvastat<strong>in</strong> with carotid <strong>in</strong>tima-medialelasticity measured by a transcutaneousultrasonic-based tissue characterizationsystem. J Atheroscler Thromb 2009;16: 662–673.39 Liao F, Folsom AR, Brancati FL: Is low magnesiumconcentration a risk factor for coronaryheart disease? The Atherosclerosis Risk<strong>in</strong> Communities (ARIC) study. Am Heart J1998; 136: 480–490.40 Larsson SC, Ors<strong>in</strong>i N, Wolk A: Dietary magnesium<strong>in</strong>take and risk of stroke: a metaanalysisof prospective studies. Am J Cl<strong>in</strong>Nutr 2012; 95: 362–366.41 Mar<strong>in</strong>ov MB, Harbaugh KS, Hoopes PJ, PikusHJ, Harbaugh RE: Neuroprotective effectsof preischemia <strong>in</strong>tra-arterial magnesiumsulfate <strong>in</strong> reversible focal cerebral ischemia.J Neurosurg 1996; 85: 117–124.42 Saver JL: Target<strong>in</strong>g the bra<strong>in</strong>: Neuroprotectionand neurorestoration <strong>in</strong> ischemic stroke.Pharmacotherapy 2010; 30: 62S–69S.43 Izumi Y, Roussel S, P<strong>in</strong>ard E, Seylaz J: Reductionof <strong>in</strong>farct volume by magnesium aftermiddle cerebral artery occlusion <strong>in</strong> rats. JCereb Blood Flow Metab 1991; 11: 1025–1030.44 Kass IS, Cottrell JE, Chambers G: Magnesiumand cobalt, not nimodip<strong>in</strong>e, protectneurons aga<strong>in</strong>st anoxic damage <strong>in</strong> the rathippocampal slice. Anesthesiology 1988; 69:710–715.45 McIntosh TK, V<strong>in</strong>k R, Yamakami I, FadenAI: Magnesium protects aga<strong>in</strong>st neurologicaldeficit after bra<strong>in</strong> <strong>in</strong>jury. Bra<strong>in</strong> Res 1989;482: 252–260.46 Muir KW, Lees KR, Ford I, Davis S: Magnesiumfor acute stroke (<strong>in</strong>travenous magnesiumefficacy <strong>in</strong> stroke trial): randomisedcontrolled trial. Lancet 2004; 363: 439–445.47 Saver JL, Kidwell C, Eckste<strong>in</strong> M, Starkman S:Prehospital neuroprotective therapy foracute stroke: results of the field adm<strong>in</strong>istrationof stroke therapy-magnesium (FAST-MAG) pilot trial. Stroke 2004; 35:e106–108.48 Abbott RD, Ando F, Masaki KH, Tung KH,Rodriguez BL, Petrovitch H, Yano K, CurbJD: Dietary magnesium <strong>in</strong>take and the futurerisk of coronary heart disease (the HonoluluHeart Program). Am J Cardiol 2003;92: 665–669.49 Peters SA, den Ruijter HM, Bots ML: Attenuationof rate of change <strong>in</strong> carotid <strong>in</strong>tima-mediathickness by lipid-modify<strong>in</strong>g drugs: impacton cl<strong>in</strong>ical outcomes. Am J CardiovascDrugs 2011; 11: 253–263.50 Sivapalaratnam S, van Loendersloot LL,Hutten BA, Kastele<strong>in</strong> JJ, Trip MD, de GrootE: Long-term LDL-C lower<strong>in</strong>g <strong>in</strong> heterozygousfamilial hypercholesterolemia normalizescarotid <strong>in</strong>tima-media thickness. Atherosclerosis2010; 212: 571–574.51 Riccioni G, Vitulano N, Manc<strong>in</strong>i B, ZanasiA, D’Orazio N: One-year treatment with rosuvastat<strong>in</strong>reduces <strong>in</strong>tima-media thickness<strong>in</strong> 45 hypercholesterolemic subjects withasymptomatic carotid artery disease. Pharmacology2010; 85: 63–67.110Ann Nutr Metab 2012;61:102–110Kupetsky-R<strong>in</strong>con/Uitto