Neurodevelopment May Be Entirely Normal in Children Born to ...
Neurodevelopment May Be Entirely Normal in Children Born to ...
Neurodevelopment May Be Entirely Normal in Children Born to ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
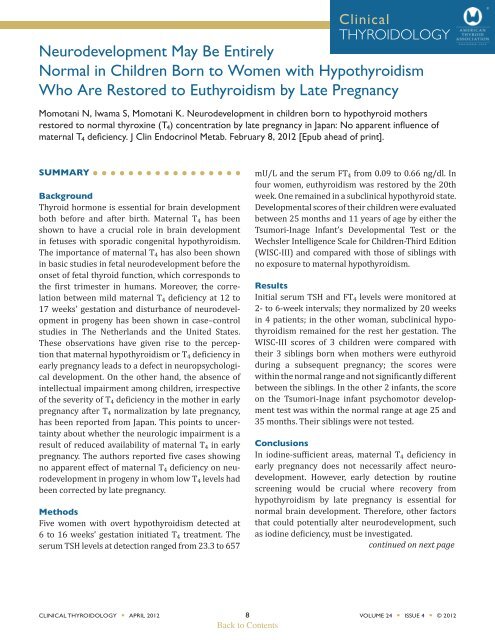
Cl<strong>in</strong>icalTHYROIDOLOGY<strong>Neurodevelopment</strong> <strong>May</strong> <strong>Be</strong> <strong>Entirely</strong><strong>Normal</strong> <strong>in</strong> <strong>Children</strong> <strong>Born</strong> <strong>to</strong> Women with HypothyroidismWho Are Res<strong>to</strong>red <strong>to</strong> Euthyroidism by Late PregnancyMomotani N, Iwama S, Momotani K. <strong>Neurodevelopment</strong> <strong>in</strong> children born <strong>to</strong> hypothyroid mothersres<strong>to</strong>red <strong>to</strong> normal thyrox<strong>in</strong>e (T 4 ) concentration by late pregnancy <strong>in</strong> Japan: No apparent <strong>in</strong>fluence ofmaternal T 4 deficiency. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab. February 8, 2012 [Epub ahead of pr<strong>in</strong>t].SUMMARYBackgroundThyroid hormone is essential for bra<strong>in</strong> developmentboth before and after birth. Maternal T 4 has beenshown <strong>to</strong> have a crucial role <strong>in</strong> bra<strong>in</strong> development<strong>in</strong> fetuses with sporadic congenital hypothyroidism.The importance of maternal T 4 has also been shown<strong>in</strong> basic studies <strong>in</strong> fetal neurodevelopment before theonset of fetal thyroid function, which corresponds <strong>to</strong>the first trimester <strong>in</strong> humans. Moreover, the correlationbetween mild maternal T 4 deficiency at 12 <strong>to</strong>17 weeks’ gestation and disturbance of neurodevelopment<strong>in</strong> progeny has been shown <strong>in</strong> case–controlstudies <strong>in</strong> The Netherlands and the United States.These observations have given rise <strong>to</strong> the perceptionthat maternal hypothyroidism or T 4 deficiency <strong>in</strong>early pregnancy leads <strong>to</strong> a defect <strong>in</strong> neuropsychologicaldevelopment. On the other hand, the absence of<strong>in</strong>tellectual impairment among children, irrespectiveof the severity of T 4 deficiency <strong>in</strong> the mother <strong>in</strong> earlypregnancy after T 4 normalization by late pregnancy,has been reported from Japan. This po<strong>in</strong>ts <strong>to</strong> uncerta<strong>in</strong>tyabout whether the neurologic impairment is aresult of reduced availability of maternal T 4 <strong>in</strong> earlypregnancy. The authors reported five cases show<strong>in</strong>gno apparent effect of maternal T 4 deficiency on neurodevelopment<strong>in</strong> progeny <strong>in</strong> whom low T 4 levels hadbeen corrected by late pregnancy.MethodsFive women with overt hypothyroidism detected at6 <strong>to</strong> 16 weeks’ gestation <strong>in</strong>itiated T 4 treatment. Theserum TSH levels at detection ranged from 23.3 <strong>to</strong> 657mU/L and the serum FT 4 from 0.09 <strong>to</strong> 0.66 ng/dl. Infour women, euthyroidism was res<strong>to</strong>red by the 20thweek. One rema<strong>in</strong>ed <strong>in</strong> a subcl<strong>in</strong>ical hypothyroid state.Developmental scores of their children were evaluatedbetween 25 months and 11 years of age by either theTsumori-Inage Infant’s Developmental Test or theWechsler Intelligence Scale for <strong>Children</strong>-Third Edition(WISC-III) and compared with those of sibl<strong>in</strong>gs withno exposure <strong>to</strong> maternal hypothyroidism.ResultsInitial serum TSH and FT 4 levels were moni<strong>to</strong>red at2- <strong>to</strong> 6-week <strong>in</strong>tervals; they normalized by 20 weeks<strong>in</strong> 4 patients; <strong>in</strong> the other woman, subcl<strong>in</strong>ical hypothyroidismrema<strong>in</strong>ed for the rest her gestation. TheWISC-III scores of 3 children were compared withtheir 3 sibl<strong>in</strong>gs born when mothers were euthyroiddur<strong>in</strong>g a subsequent pregnancy; the scores werewith<strong>in</strong> the normal range and not significantly differentbetween the sibl<strong>in</strong>gs. In the other 2 <strong>in</strong>fants, the scoreon the Tsumori-Inage <strong>in</strong>fant psychomo<strong>to</strong>r developmenttest was with<strong>in</strong> the normal range at age 25 and35 months. Their sibl<strong>in</strong>gs were not tested.ConclusionsIn iod<strong>in</strong>e-sufficient areas, maternal T 4 deficiency <strong>in</strong>early pregnancy does not necessarily affect neurodevelopment.However, early detection by rout<strong>in</strong>escreen<strong>in</strong>g would be crucial where recovery fromhypothyroidism by late pregnancy is essential fornormal bra<strong>in</strong> development. Therefore, other fac<strong>to</strong>rsthat could potentially alter neurodevelopment, suchas iod<strong>in</strong>e deficiency, must be <strong>in</strong>vestigated.cont<strong>in</strong>ued on next pageCLINICAL THYROIDOLOGY • APRIL 2012 8 VOLUME 24 • ISSUE 4 • © 2012Back <strong>to</strong> Contents
<strong>Neurodevelopment</strong> <strong>May</strong> <strong>Be</strong> <strong>Entirely</strong> <strong>Normal</strong> <strong>in</strong> <strong>Children</strong><strong>Born</strong> <strong>to</strong> Women with Hypothyroidism Who AreRes<strong>to</strong>red <strong>to</strong> Euthyroidism by Late PregnancyMomotani N, et al.ANALYSIS AND COMMENTARYIn this study, IQ and DQ (development quotient) scores<strong>in</strong>dicated no apparent neurodevelopmental deficit<strong>in</strong> children whose mothers had overt hypothyroidismdur<strong>in</strong>g the first trimester of pregnancy and wereres<strong>to</strong>red <strong>to</strong> normal serum T 4 levels by late pregnancy.Haddow et al. (1) reported lower IQs <strong>in</strong> children ofuntreated pregnant women with hypothyroidism. Atabout the same time, Pop et al. (2) described impairedpsychomo<strong>to</strong>r development <strong>in</strong> <strong>in</strong>fants of women withhypothyrox<strong>in</strong>emia who had serum TSH levels with<strong>in</strong>the reference range. In the Pop study, children ofwomen with hypothyrox<strong>in</strong>emia with FT 4 levels belowthe 5th percentile (11 mothers) and below the 10thpercentile (22 mothers) at 12 weeks’ gestation wereevaluated at 10 months of age us<strong>in</strong>g the Bailey Psychomo<strong>to</strong>rDevelopment Index scale; they had significantlylower scores as compared with children ofmothers with higher FT 4 values. S<strong>in</strong>ce this study wascarried out <strong>in</strong> an area with iod<strong>in</strong>e sufficiency, therewas no clear cause <strong>to</strong> expla<strong>in</strong> isolated cases of hypothyrox<strong>in</strong>emia.It is well known that <strong>in</strong> areas of chroniciod<strong>in</strong>e deficiency, serum iod<strong>in</strong>e and T 4 are low, witha correspond<strong>in</strong>g <strong>in</strong>crease <strong>in</strong> T3 production (3). Otherstudies from areas of iod<strong>in</strong>e deficiency describe deleteriousneurocognitive defects <strong>in</strong> offspr<strong>in</strong>g of womenwith hypothyrox<strong>in</strong>emia (4). In Japan <strong>in</strong> 1994, Liu etal. (5) studied IQs of eight children born of womenwith severe hypothyroidism (mean [±SD] serum TSH,116±59 µU/ml; FT 4 ,
<strong>Neurodevelopment</strong> <strong>May</strong> <strong>Be</strong> <strong>Entirely</strong> <strong>Normal</strong> <strong>in</strong> <strong>Children</strong><strong>Born</strong> <strong>to</strong> Women with Hypothyroidism Who AreRes<strong>to</strong>red <strong>to</strong> Euthyroidism by Late PregnancyMomotani N, et al.3. Pharoah PO, Law<strong>to</strong>n NF, Ellis SM et al. The roleof triiodothyron<strong>in</strong>e (T 3 ) <strong>in</strong> the ma<strong>in</strong>tenance ofeuthyroidism <strong>in</strong> endemic goitre. Cl<strong>in</strong> Endocr<strong>in</strong>ol(Oxf) 1973;2:193-9.4. Henrichs J, Bongers-Schokk<strong>in</strong>g JJ, Schenck JJ, et al.Maternal thyroid function dur<strong>in</strong>g early pregnancyand cognitive function<strong>in</strong>g <strong>in</strong> early childhood:the generation R study. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab2010;95:4227-34. Epub June 9, 2010.5. Liu H, Momotani N, Noh JY, Ishikawa N, TakebeK, I<strong>to</strong> K. Maternal hypothyroidism dur<strong>in</strong>g earlypregnancy and <strong>in</strong>tellectual development of theprogeny. Arch Intern Med 1994;154:7857.6. Pop VJ, Brouwers EP, Vader HL, Vulsma T, vanBaar AL, de Vijlder JJ. Maternal hypothyrox<strong>in</strong>emiadur<strong>in</strong>g early pregnancy and subsequent childdevelopment: a 3-year follow-up study. Cl<strong>in</strong>Endocr<strong>in</strong>ol (Oxf) 2003;59:282-8.7. Ori<strong>to</strong> Y, Oku H, Kubota S, et al. Thyroid function<strong>in</strong> early pregnancy <strong>in</strong> Japanese healthy women:relation <strong>to</strong> ur<strong>in</strong>ary iod<strong>in</strong>e excretion, emesis, andfetal and child development J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 2009;94:1683-8. Epub March 3, 2009.8. <strong>Be</strong>lfort MB, Pearce EN, Braverman LE, He X, BrowRS. Low iod<strong>in</strong>e content <strong>in</strong> the diets of hospitalizedpreterm <strong>in</strong>fants. J C<strong>in</strong> Endocr<strong>in</strong>ol Metab. February15, 2012 [Epub ahead of pr<strong>in</strong>t].9. Moleti M, Lo Presti VP, Campolo MC, et al.Iod<strong>in</strong>e prophylaxis us<strong>in</strong>g iodized salt and riskof maternal thyroid failure <strong>in</strong> conditions ofmild iod<strong>in</strong>e deficiency. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab2008;93:2616–21. Epub April 15, 2008.www.thyroid.orgWe <strong>in</strong>vite you <strong>to</strong> jo<strong>in</strong> the ATA!Are You Intrigued by the Study of the Thyroid? You <strong>Be</strong>long <strong>in</strong> the ATA!• ATA members are leaders <strong>in</strong> thyroidology who promote excellence and<strong>in</strong>novation <strong>in</strong> cl<strong>in</strong>ical care, research, education, and public policy.• Jo<strong>in</strong> us as we advance our understand<strong>in</strong>g of the causes and improve the cl<strong>in</strong>icalmanagement of thyroid diseases <strong>in</strong> this era of rapid pace biomedical discovery.• A close-knit, collegial group of physicians and scientists, the ATA is dedicated<strong>to</strong> the reseach and treatment of thyroid diseases. ATA's rich his<strong>to</strong>ry dates back <strong>to</strong>1923 and its members are respected worldwide as leaders <strong>in</strong> thyroidology.• The ATA encourages you <strong>to</strong> apply for membership. We want you <strong>to</strong> experience thewealth of knowledge and enjoy the benefits of be<strong>in</strong>g active <strong>in</strong> this highly specializedand regarded society. The ATA looks forward <strong>to</strong> hav<strong>in</strong>g you as a member!CLINICAL THYROIDOLOGY • APRIL 2012 10 VOLUME 24 • ISSUE 4 • © 2012Back <strong>to</strong> Contents