Mary Cornelia Bradley Society - University of Wisconsin Hospital ...
Mary Cornelia Bradley Society - University of Wisconsin Hospital ...
Mary Cornelia Bradley Society - University of Wisconsin Hospital ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
4<br />
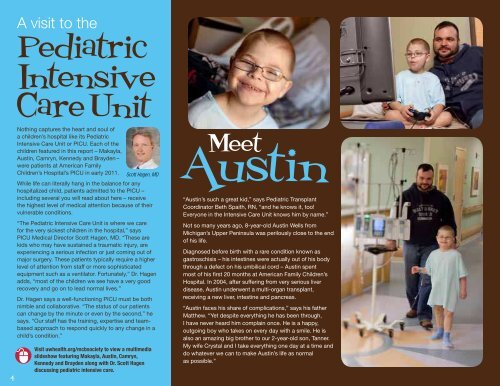
A visit to the<br />
Pediatric<br />
Intensive<br />
CareUnit<br />
Nothing captures the heart and soul <strong>of</strong><br />
a children’s hospital like its Pediatric<br />
Intensive Care Unit or PICU. Each <strong>of</strong> the<br />
children featured in this report – Makayla,<br />
Austin, Camryn, Kennedy and Brayden –<br />
were patients at American Family<br />
Children’s <strong>Hospital</strong>’s PICU in early 2011.<br />
Scott Hagen, MD<br />
While life can literally hang in the balance for any<br />
hospitalized child, patients admitted to the PICU –<br />
including several you will read about here – receive<br />
the highest level <strong>of</strong> medical attention because <strong>of</strong> their<br />
vulnerable conditions.<br />
“The Pediatric Intensive Care Unit is where we care<br />
for the very sickest children in the hospital,” says<br />
PICU Medical Director Scott Hagen, MD. “These are<br />
kids who may have sustained a traumatic injury, are<br />
experiencing a serious infection or just coming out <strong>of</strong><br />
major surgery. These patients typically require a higher<br />
level <strong>of</strong> attention from staff or more sophisticated<br />
equipment such as a ventilator. Fortunately,” Dr. Hagen<br />
adds, “most <strong>of</strong> the children we see have a very good<br />
recovery and go on to lead normal lives.”<br />
Dr. Hagen says a well-functioning PICU must be both<br />
nimble and collaborative. “The status <strong>of</strong> our patients<br />
can change by the minute or even by the second,” he<br />
says. “Our staff has the training, expertise and teambased<br />
approach to respond quickly to any change in a<br />
child’s condition.”<br />
Visit uwhealth.org/mcbsociety to view a multimedia<br />
slideshow featuring Makayla, Austin, Camryn,<br />
Kennedy and Brayden along with Dr. Scott Hagen<br />
discussing pediatric intensive care.<br />
Austin<br />
Meet<br />
“Austin’s such a great kid,” says Pediatric Transplant<br />
Coordinator Beth Spaith, RN, “and he knows it, too!<br />
Everyone in the Intensive Care Unit knows him by name.”<br />
Not so many years ago, 8-year-old Austin Wells from<br />
Michigan’s Upper Peninsula was perilously close to the end<br />
<strong>of</strong> his life.<br />
Diagnosed before birth with a rare condition known as<br />
gastroschisis – his intestines were actually out <strong>of</strong> his body<br />
through a defect on his umbilical cord – Austin spent<br />
most <strong>of</strong> his first 20 months at American Family Children’s<br />
<strong>Hospital</strong>. In 2004, after suffering from very serious liver<br />
disease, Austin underwent a multi-organ transplant,<br />
receiving a new liver, intestine and pancreas.<br />
“Austin faces his share <strong>of</strong> complications,” says his father<br />
Matthew. “Yet despite everything he has been through,<br />
I have never heard him complain once. He is a happy,<br />
outgoing boy who takes on every day with a smile. He is<br />
also an amazing big brother to our 2-year-old son, Tanner.<br />
My wife Crystal and I take everything one day at a time and<br />
do whatever we can to make Austin’s life as normal<br />
as possible.”<br />
Meet<br />
Camryn<br />
Sitting in a large recliner in her room<br />
at American Family Children’s <strong>Hospital</strong>,<br />
12-year-old Camryn Porter <strong>of</strong> Reedsburg, <strong>Wisconsin</strong>,<br />
looks up at her parents, Jen Engebretson and Alex Porter.<br />
Camryn’s voice is s<strong>of</strong>t, but the words capture a harsh truth.<br />
“I was this close to going up to heaven,” she says, holding<br />
her thumb and forefinger a half-inch apart.<br />
Indeed, she was. Just days after Christmas 2010, a<br />
perfectly healthy Camryn suddenly became acutely ill with<br />
no apparent cause. Her abdomen began swelling with<br />
fluid as she went into a coma-like state for several weeks,<br />
unable to breathe, speak or eat on her own.<br />
After weeks <strong>of</strong> undergoing nearly every medical test<br />
imaginable, Camryn was finally diagnosed with a rare<br />
streptococcal infection in her abdomen that triggered<br />
septic shock syndrome – resulting in a near total<br />
shutdown <strong>of</strong> her body’s vital organs.<br />
“Camryn’s body underwent countless chemical reactions,<br />
causing infection-fighting cells to also attack her kidneys,<br />
lungs and digestive system,” says UW Health Pediatric<br />
Critical Care Nurse Practitioner Lynne Sears, RN, MS.<br />
“About six weeks in the hospital went by before her fever<br />
subsided and we knew she would come around.”<br />
Scott Hagen, MD, Medical Director <strong>of</strong> the Pediatric<br />
Intensive Care Unit, says Camryn’s recovery illustrates<br />
the team-based approach at American Family Children’s<br />
<strong>Hospital</strong>.<br />
“Throughout her 10 weeks in the hospital, Camryn was<br />
cared for by pediatric specialists from cardiology, general<br />
surgery, pulmonology, endocrinology, infectious disease,<br />
critical care and health psychology,” Dr. Hagen says. “It<br />
took many great minds working together to get this girl<br />
back to health.”<br />
5