Wakefield & Kirklees Guidelines for Managing Stable COPD in ...
Wakefield & Kirklees Guidelines for Managing Stable COPD in ...
Wakefield & Kirklees Guidelines for Managing Stable COPD in ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
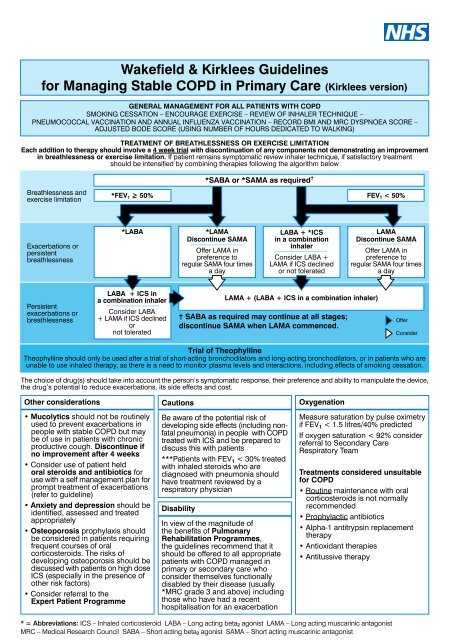
<strong>Wakefield</strong> & <strong>Kirklees</strong> <strong>Guidel<strong>in</strong>es</strong><strong>for</strong> <strong>Manag<strong>in</strong>g</strong> <strong>Stable</strong> <strong>COPD</strong> <strong>in</strong> Primary Care (<strong>Kirklees</strong> version)GENERAL MANAGEMENT FOR ALL PATIENTS WITH <strong>COPD</strong>SMOKING CESSATION – ENCOURAGE EXERCISE – REVIEW OF INHALER TECHNIQUE –PNEUMOCOCCAL VACCINATION AND ANNUAL INFLUENZA VACCINATION – RECORD BMI AND MRC DYSPNOEA SCORE –ADJUSTED BODE SCORE (USING NUMBER OF HOURS DEDICATED TO WALKING)TREATMENT OF BREATHLESSNESS OR EXERCISE LIMITATIONEach addition to therapy should <strong>in</strong>volve a 4 week trial with discont<strong>in</strong>uation of any components not demonstrat<strong>in</strong>g an improvement<strong>in</strong> breathlessness or exercise limitation. If patient rema<strong>in</strong>s symptomatic review <strong>in</strong>haler technique, if satisfactory treatmentshould be <strong>in</strong>tensified by comb<strong>in</strong><strong>in</strong>g therapies follow<strong>in</strong>g the algorithm belowBreathlessness andexercise limitation*SABA or *SAMA as required =*FEV 1 > 50% FEV 1 < 50%Exacerbations orpersistentbreathlessness*LABA*LAMADiscont<strong>in</strong>ue SAMAOffer LAMA <strong>in</strong>preference toregular SAMA four timesa dayLABA + *ICS<strong>in</strong> a comb<strong>in</strong>ation<strong>in</strong>halerConsider LABA +LAMA if ICS decl<strong>in</strong>edor not toleratedLAMADiscont<strong>in</strong>ue SAMAOffer LAMA <strong>in</strong>preference toregular SAMA four timesa dayPersistentexacerbations orbreathlessnessLABA + ICS <strong>in</strong>a comb<strong>in</strong>ation <strong>in</strong>halerConsider LABA+ LAMA if ICS decl<strong>in</strong>edornot toleratedLAMA + (LABA + ICS <strong>in</strong> a comb<strong>in</strong>ation <strong>in</strong>haler)= SABA as required may cont<strong>in</strong>ue at all stages;discont<strong>in</strong>ue SAMA when LAMA commenced.OfferConsiderTrial of Theophyll<strong>in</strong>eTheophyll<strong>in</strong>e should only be used after a trial of short-act<strong>in</strong>g bronchodilators and long-act<strong>in</strong>g bronchodilators, or <strong>in</strong> patients who areunable to use <strong>in</strong>haled therapy, as there is a need to monitor plasma levels and <strong>in</strong>teractions, <strong>in</strong>clud<strong>in</strong>g effects of smok<strong>in</strong>g cessation.The choice of drug(s) should take <strong>in</strong>to account the person’s symptomatic response, their preference and ability to manipulate the device,the drug’s potential to reduce exacerbations, its side effects and cost.Other considerations• Mucolytics should not be rout<strong>in</strong>elyused to prevent exacerbations <strong>in</strong>people with stable <strong>COPD</strong> but maybe of use <strong>in</strong> patients with chronicproductive cough. Discont<strong>in</strong>ue ifno improvement after 4 weeks• Consider use of patient heldoral steroids and antibiotics <strong>for</strong>use with a self management plan <strong>for</strong>prompt treatment of exacerbations(refer to guidel<strong>in</strong>e)• Anxiety and depression should beidentified, assessed and treatedappropriately• Osteoporosis prophylaxis shouldbe considered <strong>in</strong> patients requir<strong>in</strong>gfrequent courses of oralcorticosteroids. The risks ofdevelop<strong>in</strong>g osteoporosis should bediscussed with patients on high doseICS (especially <strong>in</strong> the presence ofother risk factors)• Consider referral to theExpert Patient ProgrammeCautionsBe aware of the potential risk ofdevelop<strong>in</strong>g side effects (<strong>in</strong>clud<strong>in</strong>g nonfatalpneumonia) <strong>in</strong> people with <strong>COPD</strong>treated with ICS and be prepared todiscuss this with patients***Patients with FEV 1 < 30% treatedwith <strong>in</strong>haled steroids who arediagnosed with pneumonia shouldhave treatment reviewed by arespiratory physicianDisabilityIn view of the magnitude ofthe benefits of PulmonaryRehabilitation Programmes,the guidel<strong>in</strong>es recommend that itshould be offered to all appropriatepatients with <strong>COPD</strong> managed <strong>in</strong>primary or secondary care whoconsider themselves functionallydisabled by their disease (usually*MRC grade 3 and above) <strong>in</strong>clud<strong>in</strong>gthose who have had a recenthospitalisation <strong>for</strong> an exacerbationOxygenationMeasure saturation by pulse oximetryif FEV 1 < 1.5 litres/40% predictedIf oxygen saturation < 92% considerreferral to Secondary CareRespiratory TeamTreatments considered unsuitable<strong>for</strong> <strong>COPD</strong>• Rout<strong>in</strong>e ma<strong>in</strong>tenance with oralcorticosteroids is not normallyrecommended• Prophylactic antibiotics• Alpha-1 antitryps<strong>in</strong> replacementtherapy• Antioxidant therapies• Antitussive therapy* = Abbreviations: ICS – Inhaled corticosteroid LABA – Long act<strong>in</strong>g beta 2 agonist LAMA – Long act<strong>in</strong>g muscar<strong>in</strong>ic antagonistMRC – Medical Research Council SABA – Short act<strong>in</strong>g beta 2 agonist SAMA – Short act<strong>in</strong>g muscar<strong>in</strong>ic antagonist
<strong>Wakefield</strong> & <strong>Kirklees</strong> <strong>Guidel<strong>in</strong>es</strong> <strong>for</strong> <strong>Manag<strong>in</strong>g</strong> <strong>Stable</strong> <strong>COPD</strong> <strong>in</strong> Primary Care (<strong>Kirklees</strong> version)Review <strong>in</strong> Primary Care: Mild/Moderate/ Severe Airflow Obstruction Very Severe Airflow ObstructionFrequencyAT LEAST ANNUALAT LEAST TWICE PER YEARMeasurements to make• FEV 1 and *FVC measurement• Record *BMI• MRC Dyspnoea score• FEV 1 and FVC measurement• Record BMI• MRC Dyspnoea score• *SpO 2Cl<strong>in</strong>ical assessment* = AbbreviationsBMI – Body Mass IndexFEV1 – Forced Expiratory Volume <strong>in</strong> 1 SecondFVC – Forced Vital CapacityMRC – Medical Research CouncilSpO2 – Saturation of Peripheral Oxygen• Smok<strong>in</strong>g status and desire to quit• Adequacy of symptom control- Breathlessness- Exercise tolerance- Estimated exacerbation frequency• Presence of complications• Effects of each drug treatment• Inhaler technique• Need <strong>for</strong> referral to specialist and therapy services• Need <strong>for</strong> pulmonary rehabilitation• Consider referral to Expert Patient Programme• Self management advice• Measure saturation by pulse oximetryif FEV 1 < 1.5 litres/40% predictedTo assess the impact of <strong>COPD</strong> on the patient’s wellbe<strong>in</strong>gand daily life, consider the use of the <strong>COPD</strong> AssessmentTest copies to download available on l<strong>in</strong>e athttp://www.catestonl<strong>in</strong>e.org• Smok<strong>in</strong>g status and desire to quit• Adequacy of symptom control- Breathlessness- Exercise tolerance- Estimated exacerbation frequency• Presence of cor pulmonale• Need <strong>for</strong> long term oxygen therapy• Patients nutritional state• Presence of depression• Effects of each drug treatment• Inhaler technique• Need <strong>for</strong> social services and occupational therapy unit• Need <strong>for</strong> referral to specialist and therapy services• Need <strong>for</strong> pulmonary rehabilitation• Presence of complications• Consider referral to Expert Patient Programme• Self management advice• Consider palliative care requirementsTo assess the impact of <strong>COPD</strong> on the patient’s wellbe<strong>in</strong>gand daily life, consider the use of the <strong>COPD</strong> AssessmentTest copies to download available on l<strong>in</strong>e athttp://www.catestonl<strong>in</strong>e.org(on pulse oximetry) For video demonstrations of correct <strong>in</strong>haler technique: http://www.medic<strong>in</strong>es.org.uk/guides/pages/how-to-use-your-<strong>in</strong>haler-videosPublished: November 2010Review: Nov 2013 (unless cl<strong>in</strong>ical evidence changes)Enquiries to: Sandy Smith NHS <strong>Kirklees</strong> 01414 464244References:Chronic Obstructive Pulmonary Disease, National cl<strong>in</strong>ical guidance <strong>for</strong>management of Chronic Obstructive Pulmonary Disease <strong>in</strong> adults <strong>in</strong>primary and secondary care, updated June 2010, NICE*** MHRA Drug Safety Update October 2007 Issue 3Group responsible <strong>for</strong> development:NHS <strong>Wakefield</strong> District Respiratory Partnership GroupDeveloped <strong>in</strong> collaboration with:Mid Yorkshire NHS Hospitals Trust and NHS <strong>Kirklees</strong>