Spring 2010: Sleep Disturbance & G-Tube Feeding - CdLS
Spring 2010: Sleep Disturbance & G-Tube Feeding - CdLS
Spring 2010: Sleep Disturbance & G-Tube Feeding - CdLS
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
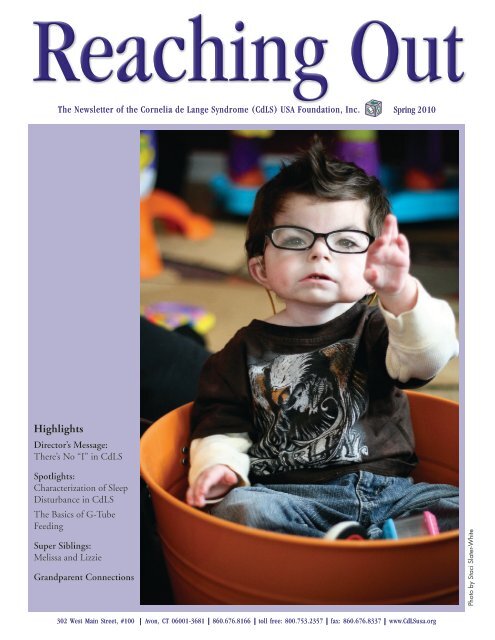
Reaching OutThe Newsletter of the Cornelia de Lange Syndrome (<strong>CdLS</strong>) USA Foundation, Inc.<strong>Spring</strong> <strong>2010</strong>HighlightsDirector’s Message:There’s No “I” in <strong>CdLS</strong>Spotlights:Characterization of <strong>Sleep</strong><strong>Disturbance</strong> in <strong>CdLS</strong>The Basics of G-<strong>Tube</strong><strong>Feeding</strong>Super Siblings:Melissa and LizzieGrandparent ConnectionsPhoto by Staci Slater-White302 West Main Street, #100 Avon, CT 06001-3681 860.676.8166 toll free: 800.753.2357 fax: 860.676.8337 www.<strong>CdLS</strong>usa.org
Di r e c t o r’s MessageThere’s no “I” in <strong>CdLS</strong>Despite society’s emphasis on individuality, teamwork is abig part of how we get things done at the <strong>CdLS</strong> Foundation.Teamwork isn’t just important, it’s essential to our success.With collaborations among staff and volunteers, we canaccomplish more than each person can on his or her own.This work benefits Foundation staff, families, people with<strong>CdLS</strong>, and professionals.Our fall 2009 wine-tasting benefit, Vines, Wines andMeaningful Times, is one example of teamwork. The ideacame up during a volunteer Development Committeemeeting. Staff ran with the concept, put it into practice,developed guidelines, and raised $8,000.Another example is the workshop Collaboration forContinuing Care, taking place at the National Family Conference next month. The idea for this program was born duringmy visit with the mother of a young adult with <strong>CdLS</strong>. She shared her frustration regarding obstacles and lack of resourcesfor transitioning her child into adulthood. Her story inspired the Foundation to create an Ad Hoc Transition Committee,which then helped develop a questionnaire to survey parents about their experiences. The results of that survey will helpguide the workshop and the Foundation’s vision for this program.In an effort to continue capitalizing on this type of synergy, I’m kicking off a Northeast Thank You Tour this summer. Thepurpose of these trips is two-fold: 1) to thank families and volunteers for their teamwork, dedication and commitment toour mission and 2) to talk about their needs, ideas and hopes for the Foundation’s future.The Thank You Tour will travel to upstate New York, the New York City-metro area, southern New Jersey/Philadelphiaregion, and Boston. If you live in these areas and are interested in hosting a visit, please let me know. I’ll bring the coffeeand dessert.I look forward to collecting ideas and adding more members to the “team” as I journey through the Northeast.Sincerely,Liana Garcia-Fresher, R.D., M.S.Executive Directordirector@<strong>CdLS</strong>usa.org5Closer Look: In Pursuitof <strong>Sleep</strong>6 The Basics of G-<strong>Tube</strong> <strong>Feeding</strong>Closer Look: G-<strong>Tube</strong>s—A Tale of Two Children8911In This Issue4 Characterization of <strong>Sleep</strong>8 Professional Outreach Program<strong>Disturbance</strong> in <strong>CdLS</strong>7New <strong>CdLS</strong> Articles Available forBilingual and Spanish-DominateReadersSuper Siblings: Melissa and LizzieUpcoming Events91112Grandparent ConnectionsMailbagCommittee Corner: The Roadto Transition14 DonationsReaching Out2www.<strong>CdLS</strong>usa.org
Co m i n g to a Di ag n o s i sBy Antonie Kline, M.D., <strong>CdLS</strong> Foundation Medical DirectorWe are happy to announce a nationwide mailingthat educates medical professionals about <strong>CdLS</strong>and encourages them to request a free <strong>CdLS</strong>Diagnostic Criteria Checklist note pad.The diagnostic criteria for <strong>CdLS</strong> was devised tohelp both families and professionals with the oftendifficult dilemma of determining whether or notan individual could have <strong>CdLS</strong>. If a mutation ina gene related to <strong>CdLS</strong> is present, that would besufficient for a diagnosis. Without a confirmedgene change, we rely on facial features plus elements of growth, development,behavior, and medical involvement to confirm a clinical diagnosis of <strong>CdLS</strong>.From the professional point of view, consideration of <strong>CdLS</strong> is often not broughtup by a geneticist, but by a gastroenterologist, a developmentalist, a neurologist,or another specialist. All of these specialists (usually pediatric) may know theirparticular field’s findings in <strong>CdLS</strong>, but may not know the overall picture. By usingspecific diagnostic criteria, medical professionals can use additional knowledgeoutside their field to help determine diagnosis.Specialists can also contact members of the Foundation’s Clinical Advisory Boardto ask if their suspicions are correct. A clinical geneticist, like myself, often receivesqueries about correct diagnoses, with photos and descriptions; the diagnosticcriteria will only help with this process. (Of course, they have to know about<strong>CdLS</strong> before doing that, and this national program will help raise consciousness ofthe syndrome.)From the family point of view, there may have been an extensive search for thecorrect diagnosis, over months or years, resulting in many laboratory studies,X-rays, and emotional ups and downs. Definitive diagnosis is important becausespecific medical and educational recommendations can be made, and there areexperts available to address the multitude of specialized issues in <strong>CdLS</strong>. Thereis also a “home” for families—the <strong>CdLS</strong> Foundation—from which extensiveknowledge can be gained and connections with other families made.With support and correct diagnosis, potential bumps in the road can be bettermaneuvered over or even avoided.Our MissionThe Cornelia de Lange Syndrome Foundation is a family supportorganization that exists to ensure early and accurate diagnosis of<strong>CdLS</strong>, promote research into the causes and manifestations of thesyndrome, and help people with a diagnosis of <strong>CdLS</strong>, and others withsimilar characteristics, make informed decisions throughout their lives.<strong>CdLS</strong> FoundationCornelia de Lange Syndrome Foundation, Inc.Reaching Out, Providing Help, Giving HopeReaching OutPublished Since 1977(ISSN 1097-3052)Cornelia de Lange SyndromeFoundation, Inc.Incorporated December 1981302 West Main Street, #100Avon, CT 06001800.753.2357, 860.676.8166fax: 860.676.8337email: info@<strong>CdLS</strong>usa.orgwww.<strong>CdLS</strong>usa.orgBoard of DirectorsPresident.. . . . . . . . . . . . . David Fowler, MAVi c e President .. . . . . . . . . . Dave Viland, MNVi c e President .. . . . . Glenn Dixon, Esq., NCTr e a s u r e r .. . . . . . . . . . . . Paul Patitucci, PADi r e c t o r s. . . . Eileen Ahearn,Ph.D, M.D., WI. . . . . . . . . . . . . . . . . . . . . Garth Black, PA. . . . . . . . . . . . . . Robert Boneberg, Esq., NJ. . . . . . . . . . . Kari Cunningham-Rosvik, WA. . . . . . . . . . . . . . .Dale Dorsett, Ph.D., MO. . . . . . . . . . . . . . Elizabeth Fouts,Ph.D., NH. . . . . . . . . . . . . . . . . . . . David Harvey, GA. . . . . . . . . . . . . . . . . . . Penny Ketchem, PA. . . . . . . . . . . . . . . . . . . Marc Needlman, ILPROFESSIONAL STAFFEXECUTIVE DIRECTORLiana Garcia-Fresher, R.D., M.SMEDICAL DIRECTORAntonie Kline, M.D.ASSISTANT EXECUTIVE DIRECTORMarie Concklin MalloyFAMILY SERVICE MANAGERDeirdre Summa, M.S.W.FAMILY SERVICE COORDINATORSLynn P. Audette, M.S.W.Janette Peracchio, M.Ed.INFORMATION COORDINATORBarbara KoontzEVENTS COORDINATORGail SpeersCOMMUNICATIONS COORDINATORAlexi DaleneFINANCE MANAGERKelly BrownAll information contained herein is for the reader’spersonal interest. Articles on treatments, medications,or procedures, etc. are not guides for selftreatment.Questions should be discussed with yourdoctor or other appropriate professionals.1-800-753-23573 Sp r i n g <strong>2010</strong>
Ch a r ac t e r i z at i o n o f <strong>Sleep</strong>Di s t u r b a n c e in <strong>CdLS</strong>By <strong>CdLS</strong> Foundation Clinical Advisory Board MemberStacey Ishman, M.D., Johns Hopkins Hospital, and RoseStavinoha, M.D. Johns Hopkins HospitalCommon sleep problemsamong individuals with<strong>CdLS</strong> consist mainly ofinsomnia (trouble goingto sleep or staying asleep)and sleepiness. It appearsthat sleep apnea may alsooccur more commonly in<strong>CdLS</strong> than in the generalpopulation. Each of these Dr. Ishmancan make for long nights for parents and leave childrentired and grumpy during the day.Since there is a known occurrence of behavioral problemsin individuals with <strong>CdLS</strong>, a small number of studieslooked at the relationship between behavior and sleep totry to uncover a link. This provided conflicting results asto why sleep disturbances occur, however studies suggestthat 12 to 72 percent of individuals with <strong>CdLS</strong> havetrouble going to sleep and staying asleep.The articles published on sleep primarily studied thegeneral occurrence of sleep difficulties among peoplewith <strong>CdLS</strong>. The first by Berney et al. surveyed thefamilies/caregivers of 49 children and adults with <strong>CdLS</strong>with mild versus severe intellectual disability (ID).They screened for irregular sleep patterns, insomnia,interrupted sleep and excessive daytime sleepiness. Outof those individuals, 55 percent demonstrated at leastone symptom. Patients with mild ID were less likely tohave sleep disturbance than those with severe ID. Thesecond study by Hall et al. compared sleep disturbancein 54 children with <strong>CdLS</strong> and 46 children with IDbut without <strong>CdLS</strong>. <strong>Sleep</strong> disturbance was found in 55percent of the children in both groups and they foundthat sleep disturbance was not associated with selfinjuriousbehavior. A third study by Basille et al foundsleep disorders in only 12 percent of 56 children with<strong>CdLS</strong>.More recently, a study by Kline et al. of 18 adults and 46children with <strong>CdLS</strong> noted that 51 percent had difficultyfalling asleep; 65 percent had frequent night-timeReaching Out4awakening; 30 percent had consecutive days withoutsleep; and 24 percent had frequent daytime napping. Theonset of sleep disturbance in most occurred as infants ortoddlers. Nearly 40 percent also noted an increase in theseverity of sleep disturbance with increasing age. Unlikeprevious studies, a strong association was seen betweensleep disturbance and self-injurious behavior (63 percent)as well as gastroesophageal reflux. About half of therespondents listed medications taken for sleep includingmelatonin, eszopiclone (Lunesta®), zolpidem (Ambien®),chloral hydrate, and temazepam.Obstructive sleep apnea (OSA) is a conditioncharacterized by snoring, witnessed pauses in breathingand night-time gasping and choking. Children with OSAoften have problems with daytime focus and attention,increased behavioral problems including hyperactivity,and decreased school performance. Adults are more likelyto experience daytime sleepiness, morning headaches andmoodiness. However, some patients present only withpoor sleep quality or restless sleep. Treatment in childrenoften starts with tonsillectomy and adenoidectomy,while adults are usually treated with a breathing machineduring sleep called CPAP (continuous positive airwaypressure). Weight loss can be critical. In those withpersistent OSA or who cannot tolerate CPAP, dentaldevices and further surgical options are considered.<strong>Sleep</strong> study evaluation is the primary method fordiagnosis of OSA and has been successfully carried outin children with Down and Angelman syndromes. Thisdemonstrates that it is a useful tool in the evaluation ofsleep disturbances in patients with ID. However, therehave been no studies reporting sleep study results or thefrequency of snoring or OSA in individuals with <strong>CdLS</strong>.To better characterize the nature and extent ofsleep problems, we are using three validated sleepquestionnaires to evaluate snoring, symptoms suggestiveof OSA and sleepiness in children and adults with<strong>CdLS</strong>. Our results suggest that people with <strong>CdLS</strong> havean increased rate of possible OSA (35-36 percent) andsleepiness (25-35 percent). However, additional studiesare needed with larger sample sizes and confirmationwith sleep studies.For problems with falling or staying asleep, behavioraltherapy with consistent bedtime routines, minimizingbright light before bedtime and regular sleep schedulesare important. For those in whom this is ineffective, sleepstudies and sleep logs are often used to better characterizecontinued on page 15www.<strong>CdLS</strong>usa.org
A Closer Lo o k: In Pu r s u i t o f <strong>Sleep</strong>For individuals with <strong>CdLS</strong>, the road to restful sleep canbe long and challenging, not only for them but theirfamilies too. It’s not uncommon for a child with <strong>CdLS</strong>to have difficulty with sleep, leaving everyone exhausted.Below, two families share their children’s sleep issues:AidenThree-year-old Aiden spent the firstfive-and-a-half months of his life inthe Neonatal Intensive Care Unit(NICU). Due in part to his smallsize at birth, Aiden experiencedsleep apnea, causing his heart toslow down considerably or stop,thereby preventing him frombreathing. His doctors placed himon a pulse oximeter and an apneamonitor to alert them if his heartAidendropped. Aiden’s sleep apnea didnot affect his mood or even wake him up from sleep; thisis what compelled his doctors to keep him in the NICUfor an extended period of time.It was a stressful time for Aiden’s mother Stacy and herfamily. Not only did Stacy miss Aiden, she was left feeling“very distance from him, depressed at times and in shockover the whole situation.” She couldn’t always be at thehospital with him since she had a two-year-old daughterat home to care for.“It was difficult,” says Stacy. “But the hospital staff wasphenomenal. They were able to communicate with the<strong>CdLS</strong> Foundation directly on how to best help Aiden.”Today, Aiden is no longer dependent on the apnea monitorand only uses a pulse oximeter as needed. With time,he outgrew sleep apnea and now is able to sleep soundlythrough the night. Overall, he is a very happy little boy,sitting up on his own and scooting around on his behindto reach for things.BrendenFor Brenden and his family, sleep never comes easily. Sincehis birth in 1997, he has faced several difficulties that haveprevented him from having a restful night.Like Aiden, Brenden was diagnosed with sleep apneashortly after birth. He was placed on oxygen, an apneamonitor and a pulse oximeter. He was also diagnosed withsevere reflux, which interrupted his breathing and restrictedthe amount of nourishment he was able to take in.“He didn’t have the capabilityto suck, swallow and breathe atthe same time,” says Brenden’smom Teresa. “This led him toturn blue and stop breathingaltogether.” Three weeks afterhis birth, his doctors placeda Jejunostomy tube ( J-tube)that helped him receive muchneeded nutrients, reducedaspiration and as a resultimproved his breathing.( J-tubes are inserted into theBrendenJejunum—situated below thestomach—lowering the risk of aspiration with feedings.)Brenden has never slept well, and without medication it’snearly impossible to get him to rest. A typical night forBrenden starts around 10:30 p.m. when he receives threedifferent medications to help him settle down. Most of thetime, he is able to sleep through the night, and he has nightattendants ensure he is okay. His sleep apnea only occursoccasionally and there is no longer a need for monitors.It’s is not easy having a child who has difficulty sleeping,but Brenden’s family stays focused on the positives. Teresabelieves she is “lucky enough to have people around herthat are continually helping Brenden during the day andat night. It’s a very nice feeling to know that someone isalways watching him.”Brenden with his family1-800-753-23575 Sp r i n g <strong>2010</strong>
Th e Ba s i c s o f G-Tu b e Fe e d i n gBy <strong>CdLS</strong> Foundation Clinical Advisory Board MemberCarol Potter, M.D., Pediatric Gastroenterologist,Nationwide Children’s Hospital, Columbus, OHA gastrostomy tube, or G-tube, is a small tube insertedthrough the abdomen skin into the stomach. Liquidnutrition and medications can pass through the tube intothe stomach, and air or fluids can be vented out of thestomach. G-tubes are very common for children and adultswith special needs. Below, are answers to some commonquestions about G-tubes.When should I consider a feeding tube for my child?<strong>Feeding</strong> tubes should be considered in children whostruggle to safely take in enough nutrition to grow well.This may include children who aspirate (get breast milkor formula into their lungs while drinking), have issueswith oral eating (swallowing, coughing or gagging whileeating, or lack the desire to eat) and/or who tire out beforethey take in enough nutrition. Sometimes children can getenough nutrition by mouth, but it takes so long that theydon’t have time or energy left for therapies that help themgain other developmental skills.Can my child still eat orally with a G-tube?Yes—if approved by your child’s doctor—having a G-tubedoes not prevent oral feeding. In fact, having a G-tube mayimprove oral feeding by allowing feedings to be a qualityand safe interaction for the child, without the struggles ofhaving to swallow every last bit of formula or medicine.How are G-tubes put in?G-tubes are pulled through the skin of the abdomen into thestomach. A PEG tube (percutaneousendoscopic gastrostomy tube) is acommon type of G-tube. A scope isplaced though the mouth, down intothe stomach to help pull the tube intothe stomach from the exterior. The tubecan be placed in a few minutes witheither general anesthesia or sedation.They are usually placed by pediatricgastroenterologists or pediatricsurgeons. Pediatric interventionalradiologists can also place PEG tubes. The tubes they placeare slightly different and are placed with guidance of X-rayrather than a scope.G-tubes can also be put in surgically. This may be done ifReaching Out6the child’s anatomy does not allow safe placement of a tubeor if the child is already having an operation.Insertion of G-tubes for complex infants and children, likethose with <strong>CdLS</strong>, should be done in an institution withpediatric surgeons, gastroenterologists, or interventionalradiologists, as well as an anesthesiologist personallyexperienced with complicated pediatric airways orabnormal jaws. This usually means a children’s hospital.Your child’s doctor can help determine what approach isbest for your child.What is the recovery time after G-tube placement?Children who receive PEG tubes usually start their feedingthe next day and are back to their pre-procedure feedingregime in two to three days. G-tubes placed with surgerymay have a slightly longer recovery time, related to howextensive their procedure was. Most children will startfeedings in a day or two.What size child can have a G-tube?The size of the child depends on the expertise of theinstitution where the procedure is being done. At myhospital, we routinely put PEG tubes into babies at about4.4 pounds. Babies can have surgical G-tubes placed atabout the same weight.When can my child’s G-tube be removed and is this donesurgically?Determining removal of a child’s G-tube should be done byyour doctor. Some signals that a child can have it removedis if the child does not have aspiration issues, can feed andreceive medications orally and can be properly hydratedwithout use of the tube. I usually recommend that G-tubesbe left in place until they have not been needed for severalmonths. This makes it less likely that they will have to beput back in.If a G-tube has only been in for several weeks/months, thehole will often heal quickly after the tube is removed andsurgery will not be needed. More often, a minor surgicalprocedure is needed to close the opening after a G-tube isremoved. This is usually an outpatient procedure.www.<strong>CdLS</strong>usa.org
A Closer Lo o k: G-t u b e s— A Ta l e o f Tw o Ch i l d r e nFor children with <strong>CdLS</strong>, eating by mouth can be a challengeor not possible, and many rely on getting their nutritionvia a tube, either inserted into their abdomen (a gastricfeeding tube—more commonly called a G-tube) or nose(a nasogastric feeding tube, or NG-tube).Some children are tube fed for a short period of time, whileothers need tube feeding their entire lives. Here are twofamilies’ stories:BenBen received an NG-tubeshortly after birth due toaspiration and inability tosuck. When he was five monthsold and big enough for surgery,a G-tube replaced the NGtube.A Nissen fundoplication Ben(a procedure in which the upper part of the stomach iswrapped around the esophagus to prevent gastric reflux)was performed at the same time the G-tube was placed. “Westruggled with the idea of surgery, but he was so miserablefrom the reflux,” says mom Karen.Following surgery, Ben’s vomiting stopped, and after amonth on G-tube feeds, he started gaining weight. “Wenever looked back,” says Karen. “It was the best thingwe could have done for Ben.” At age four, Ben is now 27pounds, which is about the 90th percentile for boys his ageon the <strong>CdLS</strong> growth chart.The G-tube was the best option saysKaren because it’s easy to put backin if it comes out (Ben has pulled thetube out a few times—he wears overallsduring the day and has it wrapped inace bandages at night to prevent himfrom pulling on it) and she doesn’tworry about aspiration or aspirationpneumonia, caused by fluid gettingBeninto the lungs. Ben vomited a lot onthe NG-tube, so aspiration was always a fear.The negatives, she says, is that it’s difficult to know whento size up the tube, it’s inconvenient to lug around thefeeding pump and supplies, and it’s expensive. While herhealth insurance covers the costs, she once saw the bill, andit exceeded $1,000 for one month.The ultimate goal is to have Ben eat orally during the dayand supplement with tube feedings at night. However, Benisn’t that interested in food, says Karen. Since he was one,Karen and her husband Mark have tried spoon feeding, tono avail. “There’s no medical reason he can’t eat,” says Karen,“it’s a behavioral issue.”Karen does have hope that Ben will make the transition.When her husband made homemade broccoli soup recently,Ben seemed interested. “It’s a work in progress,” she says.BreezeFor some children with <strong>CdLS</strong>, tubefeeding is not long-term. That was thecase with Breeze, who had a G-tubefor 15 months, starting from the timeshe was six months old.“Breeze never sucked, had animmature swallow and awful reflux,”recalls mom Margaret. “She nevertook to bottle or breastfeeding.”Breeze started with a NG-tube likeBen, as the doctors wouldn’t place a BreezeG-tube until she reached eight pounds. Margaret says theNG-tube was a nightmare because Breeze ripped it out afterevery feeding, leaving Margaret to snake the tube throughher nose every two hours to feed her.Once the G-tube was placed, it was, according to Margaret,“a lifesaver.” Breeze gained weight and her reflux wascontrolled. The G-tube helped in other areas as well. Withthe NG-tube, physical and occupational therapy wereproblematic because the therapists couldn’t move Breezearound too much. The G-tube changed that.At 17 months old—and after Margaret brought home“every type of drinking device on the market”—Breezebegan using a sippy cup. Margaret hit the jackpot with theTake and Toss cup, a valve-less cup that doesn’t requiresucking.Once she started drinking, Breeze moved on to baby foodand Pediasure. Those gave her enough nutrition and thetube came out when she was 21 months old.continued on page 151-800-753-23577 Sp r i n g <strong>2010</strong>
Professional Ou t r e a c h Pr o g r a mThanks to funding from the Centers for Disease Controland the American Legion Child Welfare Foundation, Inc.,more than 60,000 postcards will be mailed to medicalprofessionals across the country this summer. In addition toeducating recipients—which include NICUand OB nurses, nurse practitioners andpediatricians—about <strong>CdLS</strong>, the postcardsprovide details on our new <strong>CdLS</strong> DiagnosticCriteria Checklist note pad, provided free toanyone in the medical field who requests it.New <strong>CdLS</strong> Articles Ava i l a b l ef o r Bi l i n g ua l a n d Spa n i s h-Do m i n a t e ReadersIn a move that takes the commitment to the Hispaniccommunity to the next level, the <strong>CdLS</strong> Foundationis proud to announce new Spanish language articlesconcerning <strong>CdLS</strong>. Articles range from basic knowledgeabout <strong>CdLS</strong> to specialized articles on aging, ENT care,behavioral challenges, and our new Treatment Guidelines.Stay tuned for more Spanish language articles availablelater this year including the updated version of Facing theChallenges.To access these articles, go to www.<strong>CdLS</strong>usa.org and clickon Be Informed, or call 800-753-2357 to request a specificarticle or publication to be mailed to you.Nu e v o s Ar t í c u l o s So b r e <strong>CdLS</strong>En Es pa ñ o lComo forma de mostrar su dedicación a la comunidadHispana, la Fundación <strong>CdLS</strong> está orgullosa de anunciarque están disponibles al público numerosos artículossobre el síndrome Cornelia de Lange. Los artículos tratande temas tan variados como información básica de <strong>CdLS</strong>a artículos especializados en envejecimiento, cuidadosotorrinolaringológicos, desafíos de comportamiento ylas nuevas pautas de tratamiento. En breve se esperanlas traducciones de varios artículos más disponibles esteaño, además de la nueva edición de Enfrentándose a losDesafíos.¿Cómo tener acceso a estos artículos? Váyase awww.<strong>CdLS</strong>usa.org o llame a 1-800-753-2357 para pedirque un artículo o publicación específico se le mande.1. Aflicción Gastrointestinal —Malrotación, Vólvulo, ObstrucciónIntestinal, PancreatitisPor Carol Potter, M.D.2. El Síndrome <strong>CdLS</strong> Y La FisioterapiaPor Amy Metrena, M.S.P.T.3. Salud de oído, nariz y garganta depacientes con <strong>CdLS</strong>Por Robert Thayer Sataloff, M.D.,D.M.A.4. Informacion Genetica sobre <strong>CdLS</strong>5. Manejo De Ansiedad Y AgresiónPor Eileen P. Ahearn, M.D., Ph.D.6. Individuos Mayores Con <strong>CdLS</strong>Por Antonie Kline, M.D.7. Pautas sobre manejo y tratamientopara el síndrome Cornelia de LangePor Antonie Kline, M.D.8. Los desafíos del cuidado dentalPor Richard Mungo, D.D.S.9. La Educación Especial En LosEstados UnidosPor Mary T. Morse, Ph.D.10. La anestesia para las personas con<strong>CdLS</strong>Por Aaron Zuckerberg, M.D.11. Datos sobre <strong>CdLS</strong> y sobre laFundacion <strong>CdLS</strong>Reaching Out8www.<strong>CdLS</strong>usa.org
Su p e r Si b l i n g s: Melissa a n d Li z z i eWhile many siblings of people with <strong>CdLS</strong> would go the extramile for their brother or sister, Melissa went 26.2 miles.Melissa was a 2009 member of Team <strong>CdLS</strong>, running theChicago Marathon in honor of her sister, Lizzie. She wasjoined by older sister, Janine, who talked Melissa into themarathon after signing up herself.“I have been running since grade school but never ran fartherthan two miles, so it was crazy to think about running26.2,” says Melissa. “I was so nervous and worried abouthow much it would hurt.” She says that the encouragingemails from fellow Team <strong>CdLS</strong> members helped her makeit to Chicago and, ultimately, to the finish line.Melissa, Janine andLizzie’s sneakers“It was one of the best experiencesof my life. I can’t even tell you howgreat it was to be running and hearingpeople cheer you on all the wayto the end.” Among those cheeringfrom the sidelines were her biggestfans: her parents and sister Lizzie,bundled up watching Janine andMelissa finish the race.Melissa—one of five children—was five years old whenLizzie was born in 1991. “I can’t really remember thinkingshe was different or even being protective of her, she wasjust another sister to me,” says Melissa.“I truly believe that we lived a very normal family life.My parents are two of the most amazing people I know.Lizzie with her sisters: Becca, Janine and MelissaNotonly did they raise five children, including one withspecial needs, they were very involved with everything thatwe did in and out of school.”And although Melissa didn’t treat Lizzie much differentlythan she did her other siblings, she says having a sister withspecial needs helped shape who she is today. “We have meta lot of amazing people because of her, and I think she hasopened my eyes to be more accepting of everyone.”“Running the marathon is just my way of saying thankyou for being the best baby sister we have. Without her wewould not be the people we are today.”Cheer Melissa on this October as she runs the ChicagoMarathon once again with Team <strong>CdLS</strong>.WELCOME NEW FAMILIESColoradoThelma and Benand daughter Fabiola,born March 24, 2007FloridaAngela and Samand son Vinny,born July 8, 2001IndianaKristen and daughter Emma,born February 25, <strong>2010</strong>KentuckyVicki andgranddaughter Brianna,born September 25, 2000MassachusettsChandra and Jamesand daughter Amerah,born December 24, 2009New YorkMarsha and Garyand daughter Maria,born May 3, 2006OhioAmanda and son Dominic,born February 19, <strong>2010</strong>OklahomaCharles and son Charles,born October 21, 2009PennsylvaniaKim and Frankand son Alexander,born April 15, 2000TennesseeDeanna and son Nikolaus,born October 21, 1997TexasJulie and Randyand daughter Savannah,born October 2, 2008Alicia and Bibianoand son Isaac,born February 18, 2009WashingtonDawn and Daveand son Alexander,born December 5, 20061-800-753-23579 Sp r i n g <strong>2010</strong>
Help Sta r t t h e Rac e to t h eFinish Li n eWith your help, Team <strong>CdLS</strong> celebratesa m i l e stone in c omm i tm ent anddetermination by raising more than a halfmillion dollars for individuals with <strong>CdLS</strong>.From California to Pennsylvania, teamshave been forming to go the distancefor people with <strong>CdLS</strong>. Last year alone,running events raised more than $111,000to support services the Foundation provides to families.As the momentum of running for a cause quickens its paceamong the Foundation’s friends and families (and even afew strangers!) so does awareness about the syndrome. Inearly May, Team <strong>CdLS</strong> shirts were spotted throughoutPhiladelphia at the Broad Street Run, noted as the fastest10-mile course in the country. Runners were inspired byPhiladephia Team <strong>CdLS</strong> Ambassador Connor—whose dadorganized the team and ran the race himself.Also, the <strong>CdLS</strong> Foundation is pleased to announce itsacceptance again as an associated charity for the Bank ofAmerica Chicago Marathon on October 10. Althoughregistration is closed for the race, entries are still availableexclusively through the Foundation.Take the challenge and join Team <strong>CdLS</strong> today—either inChicago or as part of a race in your area. Experience thesatisfaction of making a difference in the lives of individualswith <strong>CdLS</strong> and those that care for them.If you would like to form your own Team <strong>CdLS</strong>, contactGail at events@<strong>CdLS</strong>usa.org or 800-753-2357 for moreinformation.Rid t h e Clutter,Ma k e a DifferenceWh e r e Wildflowers Gr o wTh e r e is Ho p e<strong>2010</strong> CalendarLast year, Yard Sale Across Americaevents were organized nationwideto benefit the <strong>CdLS</strong> Foundation,raising more than $10,000 to support programs and servicesfor families.This year, you can rid yourself (and your friends and familymembers, too) of clutter by hosting your own yard sale tobenefit the Foundation. The official event date is Saturday,June 5, but any time this summer will do.Ready to Tag the Day for <strong>CdLS</strong>? Contact Gail at 800-753-2357or events@<strong>CdLS</strong>usa.org for your Yard Sale AcrossAmerica kit.Imagine a garden of wildflowers— blue, pink and yellowpetals, representing the hope the <strong>CdLS</strong> Foundationprovides children with <strong>CdLS</strong>. You can help spread thathope by asking your friends and family to plant their ownwildflower garden this spring.Request your free Cornelia’s Garden kit by contacting Gailat 800-753-2357 or events@<strong>CdLS</strong>usa.org.May 22Northeast RegionFamily GatheringCentreville, MDMay 24New England Golf TournamentIpswich Country ClubIpswich, MAJune 6Yard Sale Across AmericaJune 12Motorcycle ride for <strong>CdLS</strong>Minneapolis/St. Paul, MNJune 12Hoof it 4 HunterTwo-mile Benefit WalkSeabrook, NHJune 24-27<strong>CdLS</strong> Foundation NationalFamily ConferenceDallas, TXJuly 10Lapel Village Fair<strong>CdLS</strong> Benefit 5KLapel, INAugust 7Southwest RegionFamily GatheringAurora, COSeptember 18“The Lizzy” <strong>CdLS</strong> Golf CharityTournmentGibsonia, PASeptember 25Midwest RegionFamily GatheringMinneapolis, MNOctober 10Team <strong>CdLS</strong> Chicago MarathonChicago, ILOctober 17Team <strong>CdLS</strong>- DukeCity MarathonAlbuquerque, NMReaching Out10www.<strong>CdLS</strong>usa.org
Gr a n d pa r e n t Co n n e c t i o n sRight now we are going on trial and error looking for amedicine that will stop the aggression but all and all she isvery happy. You can see it in her smile.PatriciaGrandmother to JasmineIllinois– Ja s m i n e –This is Jasmine. She is 18 years old.She lives with her grandma andhas all her life; grandma has hadguardianship since Jasmine wasthree months old. She ( Jasmine)now attends the Illinois Center forAutism.She gets out of school at 2:30 pmand is at home by 3:30 pm. Jasmineloves music and pretends to talk on her cell phone, andwhile she doesn’t speak, she understands everything beingsaid. When she was born the doctor said she would neverwalk, talk, laugh, or cry. She can do all those things buttalk.–Delaney –We are the grandparent’s of Delaney,who will soon be 16 years old. Sheis truly our angel and we love takingcare of her. She goes to a school fordisabled children, riding the busevery day. She doesn’t walk or talkbut sure communicates in her ownway! She weighs about 25 lbs. andis still fed through the G-tube.We have been involved with theFoundation since shortly after she was born and really enjoyreading Reaching Out when it comes.Arnold and SallyGrandparents of DelaneyNevadaSend your Grandparent Connectionssubmissions to communications@<strong>CdLS</strong>usa.org or <strong>CdLS</strong> Foundation Attn:Alexi, 302 West Main Street, #100, Avon,CT 06001.Billy FrazierJuly 26, 1954 – March 12, <strong>2010</strong>Son of Mary Lou and Clark Frazier5372 CR-26Rawson, OH 45881Jessica Elizabeth MurphyJuly 30, 1994 – March 22, <strong>2010</strong>Granddaughter of Roberta MurphyP.O. Box 784Orleans, MA 02653Our Deepest SympathyDavid Reilly SperaJune 26, 1991 – March 28, <strong>2010</strong>Son of Joanne and Joe SperaMorton, PAFaith RiederOctober 22, 1995 – March 28, <strong>2010</strong>Daughter of Darleen and Stanley Rieder111 Gabrielle LaneDestrehan, LA 70047-3025Aaron Daniel KramerFebruary 28, 1992- April 2, <strong>2010</strong>Son of Brenda and Steven Kramer807 West Creek LaneMiddletown, DE 197091-800-753-235711 Sp r i n g <strong>2010</strong> 2009
MAILBAG– Rya n –Did you ever hear thesaying that hearing impairedpersons can “feelthe music” from vibration?Well, I witnessedit first hand with my son,Ryan. Ryan has Corneliade Lange Syndrome andcelebrated his twentyfourthbirthday on September 11th. At birth, we were toldthat Ryan would probably not live to be a teenager. Ryanhas many health-related issues including being hearingimpaired,fed through a G-tube, and now has a permanentcolostomy bag.This year started out with Ryan being hospitalized fortwisted bowel. This resulted in emergency surgery anda colostomy bag. Numerous children with <strong>CdLS</strong> haveencountered twisted bowel in their twenties. Many donot survive this painful experience. Ryan did survive andcontinues to inspire us.Ryan has lived at a Connecticut Institute of the Blind (CIB)Group Home in Hebron for the past two years. We feelblessed that Ryan is there; he loves his new home, his housemates and all of the staff. Once a month, the house matesparticipate in music therapy and look forward to listeningto the guitar and using the maraca and drums. During thesesessions, Ryan started putting his hand on the guitar to “feelthe music” and would evenpush his wheelchair forwardto reach the guitar. Manystaff members kept tellingme that I should see Ryan’sactions towards the guitar.Ryan turning twenty-four was a large milestone and Iwanted to really celebrate it this year. Usually, we have pizzaand cake but since Ryan doesn’t eat by mouth, I decided dosomething really special and hire someone to play the guitarto see exactly what Ryan does. I asked one of my bosses, Billif he knew anyone that plays the acoustic guitar. Bill saidhe had one and would check with his brother, Jeff if theywere available for Ryan’s party. Next thing I know, a groupof band mates are going to play for Ryan.I truly believe after witnessing Ryan, that he could “feel themusic”. Ryan may not have heard the music from his ears,but he definitely felt it in his hands. He put his little handson the guitar and hardly took them off ! It brought tearsto my eyes seeing the happiness Ryan was experiencing. Itwas the best birthday party that I’ve witnessed in Ryan’stwenty-four years!Shari & Maury, Ryan’s parentsConnecticut– Olivia –Hi my name is Olivia .I was born on December25th, 2007. I was born sixweeks premature and with asyndrome called Cornelia deLange Syndrome. One out ofabout 10,000 births are bornwith this syndrome and I wasthe chosen one. I was born3 pounds, 7 ounces and wasborn without my lower arms. Iwill have delays in starting to walk and talk and doing thingsthe average baby does. But I will never give up trying. I amvery small still, I am almost 2 years old and weigh 12 poundsand 8 ounces. I am small but mighty. I have four wonderfultherapists and they help me a lot. Sometimes they makeme do things I don’t really want to do but I know it is formy own good. They are making me stronger, and teachingme to do things I need to do . I love them. I will also bementally delayed. People with this syndrome range frommild to profoundly mentally retarded and doctors tell myGrandma that they think I am on the mild side. I will learnand I will play and I will grow. Not maybe like everyoneelse. But I will be like me. I am a little girl that anyone whomeets falls in love with. A little girl that gave her family anew meaning on life. Someone that will make you smileevery time you look at her little face. I will be different, butI will be me. A little girl with the heart of gold and a faceyou will never forget.Sandra, Olivia’s AuntIllinoisReaching Out12www.<strong>CdLS</strong>usa.org
Co m m i t t e e Co r n e rThe Ad Hoc Transition Committee guides the Foundationin providing much needed support and services to familiesas their children with <strong>CdLS</strong> reach adulthood. Below is astory about committee member, Diana Ramsey’s personalexperience on the road to transition.The Road to TransitionBy Diana Ramsey, <strong>CdLS</strong> Foundation Ad Hoc TransitionCommittee memberMy daughter Megan is 31 years old and has been livingaway from home since she was 19. The transition processwas smooth but not without effort once the decision wasmade to place Megan in a home away from home.Megan with her mother Diana, sister Alyson and nephewsCooper and TuckerI was at my wits end. Multiple, full-blown tantrums each day,enormous daily transition problems, (couldn’t get her intothe tub, then couldn’t get her out, etc.) refusal to participatein her school day, little progress in career options, and ageneral sadness on her part that I believe started when shesaw her older sister Alyson become independent and veryactive away from home.There were times when Alyson would leave with friendsand Megan would hold on to the car door to prevent themfrom backing out of the driveway. She’d then chase the cardown the street and collapse into a puddle of tears right inthe middle of the road. Megan wasn’t sleeping well, andwe were all exhausted working hard to help her be all shecould be.A friend first suggested having Megan live away from home.I was appalled. Give up on Megan? “Send” her away? AdmitI was overwhelmed? Oh, no – not this super-mom. Then theheart-to-heart talks started, and I realized every oppositionI held for Megan living in a supported community wasabout ME! Yes, the endlessly patient, I love my daughterand I am her best chance, and don’t you tell me I can’t dothis, me. Oops. Okay then, time for a change of focus. Thequestion became: What is best for Megan?That’s when I realized that Megan’s social, emotionaland productivity needs had to be met outside our fourwalls. I can’t give Megan employment to make her feelaccomplished and part of a larger world. I can’t be her peer,but I can be a mom who looks after her needs, in the biggestsense of the word. We are a close-knit family and we adoreMegan. But I have to say that once Megan adjusted to livingaway, we could all take a deep breath and know that all ourpaths were heading in the right direction.Our children grow up and move out. Some boomerang,some take a while, but the nature of things is that we areeach to find our place in the world. Megan is no differentin that regard. She is doing beautifully at her communityin Pennsylvania. She comes home frequently, we call andshe even takes trips to visit relatives who live out-of-stateand I don’t go along. I miss Megan the way I miss Alyson.Being a mom has been such a blessing for me, but they havetheir lives. I will always be their mom, but I don’t have tobe the one to cook every meal, share every giggle or wipeaway every tear. They are surrounded by people who lovethem, and that is their job now. I am still a central part oftheir lives—just not every day.I said the road to transition was easy for us. The first timeit was. Megan has moved twice since that first placementand those next two times were complicated and stressfuland that’s why the <strong>CdLS</strong> Foundation wants to help. We areall in this together. If your child is at home, just keep an eyeon what’s possible and hear those folks who are seeing yoursituation from the outside looking in. We love our kids inall their complexity and we want to do it all. I have cometo know that there are homes away from home that comepretty darn close, and I see my adult daughter with <strong>CdLS</strong>thriving away from home as a happy, productive, loving,and capable young lady. What a gift.Interested in learning more abouttransitioning your child into adulthood?At the <strong>CdLS</strong> National Family Conference inDallas, TX, the workshop Collaboration forContinuing Care is dedicated to transition issues.Contact Liana at director@<strong>CdLS</strong>usa.org or 800-753-2357 to learn more about this workshop.1-800-753-235713 Sp r i n g <strong>2010</strong>
Characteristics of <strong>Sleep</strong> <strong>Disturbance</strong>s in <strong>CdLS</strong>continued from page 4sleep patterns and breathing. Weighted blankets mayhelp those with <strong>CdLS</strong> and autistic features. Medicationsfor insomnia may also be used including melatonin,clonidine, zolpidem (Ambien®) and zaleplon (Sonata®).It is important to note, however, that most medicationsprescribed for insomnia are not FDA approved forchildren.In conclusion, sleep disordered breathing, insomnia andsleepiness appear to be common in <strong>CdLS</strong>. As previousstudies have shown, it is unclear if sleep disturbancecorrelates to behavioral and learning issues in thispopulation. Further in-depth studies will help us learnmore about this and should serve to improve quality oflife for both those with <strong>CdLS</strong> and their families.1. Basile E, Villa L, Selicorni A, Molteni M. The behavioral phenotype ofCornelia de Lange Syndrome: a study of 56 individuals. J Intellect DisabilRes. 2007 Sept;51:671-681.2. Berney T, Ireland M, Burn J. Behavioral phenotype of Cornelia de LangeSyndrome. Arch Dis Child 1999 Oct;81(4):333-336.3. Hall SS, Arron K, Sloneem J, Oliver C. Health and sleep problems inCornelia de Lange Syndrome: a case control study. J Intellect Disabil Res.2008 Mar;52:458-468.4. Kline A. Clinical delineation of sleep disturbance in Cornelia de LangeSyndrome. American Society of Human Genetics, Annual meeting, Oct2007.Closer Look: G-<strong>Tube</strong>s— A Tale of Two Childrencontinued from page 7Four years later, Breeze, now six, continues on Pediasure andonly eats pureed foods, but she remains tube free.Margaret’s advice to other parents is to “keep trying andthen try some more. I tried every cup on the market andfound the cheapest, most available ones worked best.” Shealso believes that controlling reflux, which Breeze takesmedication for, was a big part of being able to eliminatethe G-tube.Common Types of <strong>Feeding</strong> <strong>Tube</strong>sAll tubes can be used to give feedings or medications. Thereare cases in which a special tube is needed to drain air orliquid, as well as a tube that provides the child their feedingsinto the small intestine rather than the stomach.A gastric feeding tube, or G-tube, is a tube inserted througha small incision in the abdomen into the stomach. Inaddition to feeding, the tube can be used to “vent” thechild’s stomach of air.A nasogastric feeding tube, or NG-tube, is passed throughthe nostril, down the esophagus and into the stomach.A jejunostomy tube, or J-tube, is inserted into the smallbowel called the jejunum, bypassing the stomach.A nasojejunal tube, or NJ-tube, is passed through thenostril and guided (by X-ray) into the jejunum.Yes, I want to make a difference in the lives of children with <strong>CdLS</strong>!Enclosed is my tax-deductible gift of: Other $ $500 $250 $100 $50 $35 Use my gift to help children with <strong>CdLS</strong> I have included the <strong>CdLS</strong> Foundation inmy will or trust.Charge my gift to: VISA MC AMEXCard #: ___________________________________Expiration: ________ Security Code: ___________Print name on card: __________________________Signature: __________________________________Email address(es): ___________________________Donate online at www.<strong>CdLS</strong>usa.org.One hundred percent of your contribution is tax deductible.1-800-753-235715 Sp r i n g <strong>2010</strong>
Cornelia de Lange Syndrome Foundation, Inc.302 West Main Street, #100Avon, Connecticut, USA 06001Return Service RequestedNON-PROFITU.S. POSTAGEPAIDHARTFORD, CTPERMIT NO. 751• Memory sticks• Printer ink cartridges• Digital camera (minimum 10 mega pixels)• Phone cards for volunteers• Postage stamps• Cards for staff travelWishlist• Pro-bono experts in grant writing, graphic designand photography• Airine tickets to get staff to conferenceTen $1,000 pledges for the 21•stCenturyConference Fund<strong>CdLS</strong> Family Gatherings are happening allthroughout the year, providing a fun and informalway for families to meet others like themselves toshare resources, information and support. Meetwith Foundation staff and specialists in variousfields during the five <strong>CdLS</strong> Foundation sponsoredgatherings throughout the country.Interested in hosting your own <strong>CdLS</strong> familygathering? The Foundation can help you through theprocess by providing you with some tips on how toget started, names of released families in your area aswell as providing resources to plan your event.Contact familysupport@<strong>CdLS</strong>usa.org or 800-753-2357 to start planning your own gathering.Fa m i ly Gat h e r i n g s