Immunocytochemistry - UK NEQAS for Immunocytochemistry ...
Immunocytochemistry - UK NEQAS for Immunocytochemistry ...
Immunocytochemistry - UK NEQAS for Immunocytochemistry ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
In This Issue:<br />
Volume 3 Issue 4<br />
123 EDITORIAL<br />
<strong>UK</strong> <strong>NEQAS</strong><br />
124 INTER-LAB SURVEY OF<br />
TECHNICAL VARIATIONS<br />
IN PROSTATIC IMMUNO-<br />
HISTOCHEMISTRY: B A S A L<br />
CELL MARKERS<br />
(Murali Varma et al)<br />
128 REPORT OF RESULT S<br />
F ROM THE <strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
QUESTIONNAIRE<br />
(Roger Martin et al)<br />
135 I N T RODUCTION TO<br />
RUN 65 REVIEWS<br />
136 GENERAL PATHOLOGY<br />
MODULE<br />
(Pan Cytokeratin,Thyroglobulin)<br />
142 BREAST HORMONAL<br />
R E C E P TOR MODULE<br />
(Oestrogen receptors (ER))<br />
147 BREAST HER-2<br />
MODULE<br />
(HER-2)<br />
151 LYMPHOMA MODULE<br />
(CD3 & bcl-2)<br />
158 NEURO PATHOLOGY<br />
MODULE<br />
(Synaptophysin and Cytokeratin)<br />
163 C Y TOLOGY MODULE<br />
(Melanoma markers, Cytokeratins)<br />
168 THE ALIMENTA RY T R AC T<br />
(PILOT) MODULE<br />
(CD117)<br />
172 INSTRUCTIONS<br />
FOR AUTHORS<br />
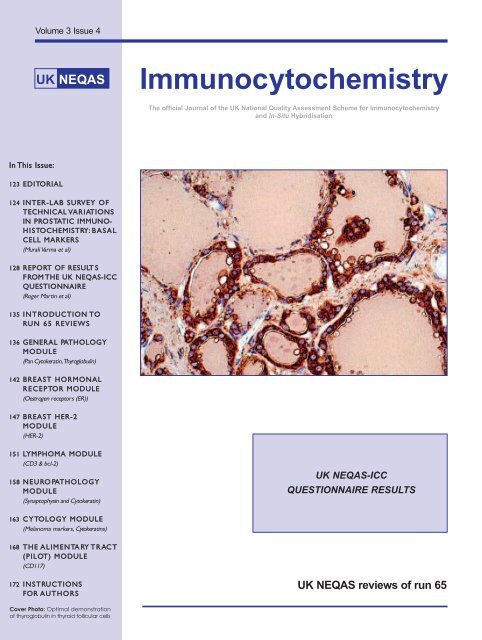
Cover Photo: Optimal demonstration<br />
of thyroglobulin in thyroid follicular cells<br />
<strong>Immunocytochemistry</strong><br />
The official Journal of the <strong>UK</strong> National Quality Assessment Scheme <strong>for</strong> <strong>Immunocytochemistry</strong><br />
and In-Situ Hybridisation<br />
<strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
QUESTIONNAIRE RESULTS<br />
<strong>UK</strong> <strong>NEQAS</strong> reviews of run 65
General In<strong>for</strong>mation<br />
The Journal is open to the publication of original<br />
papers and review articles on <strong>Immunocytochemistry</strong>.<br />
All articles, papers and letters should be submitted to:<br />
Mr. Andrew Dodson. Editor-in-Chief,<br />
<strong>Immunocytochemistry</strong>,<br />
Royal Liverpool University Hospital, Liverpool. L69 3GA.<br />
E-mail: dodson@liv.ac.uk<br />
For further in<strong>for</strong>mation of the <strong>UK</strong> <strong>NEQAS</strong>-ICC scheme,<br />
immunocytochemistry EQA enquiries, including slide<br />
returns, or to request further copies of this journal<br />
please contact:<br />
Dr Merdol Ibrahim, Scheme Manager.<br />
<strong>UK</strong> <strong>NEQAS</strong>-ICC Office.<br />
Suite 3/22 Hamilton House, Mabledon Place,<br />
London. WC1H 9BB.<br />
United Kingdom.<br />
Tel: (44) 207 554 8679 E-mail: merdol.ibrahim@ucl.ac.uk<br />
<strong>Immunocytochemistry</strong> — General In<strong>for</strong>mation<br />
<strong>Immunocytochemistry</strong> is the recognised publication of the <strong>UK</strong> National External Quality Assessment Scheme <strong>for</strong><br />
<strong>Immunocytochemistry</strong> and In-Situ Hybridisation (<strong>UK</strong> <strong>NEQAS</strong>- ICC). It is published quarterly and has a current distribution of<br />
over 1,800 to medical, technical and research staff working within the scientific area of <strong>Immunocytochemistry</strong>.<br />
121<br />
For in<strong>for</strong>mation on Training issues, Meetings, Courses,<br />
please contact:<br />
Mr Keith Miller. <strong>UK</strong> <strong>NEQAS</strong>-ICC Histopathology,<br />
21 University Street, University College London,<br />
London, WC1E 6JJ. United Kingdom.<br />
Tel: (44) 207 679 6048 E-mail: k.miller@ucl.ac.uk<br />
For advertising opportunities please contact:<br />
KT Advertising: Tel: (44) 709 230 6006<br />
E-mail: info@KT-Group.co.uk<br />
<strong>UK</strong> <strong>NEQAS</strong>-ICC wish to thank all advertisers and sponsors<br />
<strong>for</strong> their support, but point out that any product or service<br />
advertised in this Journal does not necessarily denote<br />
an endorsement by <strong>UK</strong> <strong>NEQAS</strong>.<br />
<strong>UK</strong> <strong>NEQAS</strong>-ICC reserves the right to refuse any article<br />
or advertisement without question.<br />
JOURNAL EDITOR ORGANISER MANAGER<br />
Mr A Dodson Mr K Miller Dr M Ibrahim<br />
ASSESSORS<br />
Dr S Al-Sam, Essex, <strong>UK</strong> Dr E Anderson, Manchester, <strong>UK</strong> Dr N Anderson, Belfast, <strong>UK</strong><br />
Dr M Arends, Cambridge, <strong>UK</strong> Dr M Ashton-Key, Southampton, <strong>UK</strong> Dr A Balaton, Bievres, France<br />
Dr D Barnes, London, <strong>UK</strong> Ms S Barnett, London, <strong>UK</strong> Dr E Baslev, Herlev, Denmark<br />
Mr D Blythe, Leeds, <strong>UK</strong> Dr L Bobrow, Cambridge, <strong>UK</strong> Dr J Bulmer, Newcastle, <strong>UK</strong><br />
Dr J Cabecadas, Lisbon, Portugal Mr KK Chan, Cambridge, <strong>UK</strong> Dr C D'Arrigo, London, <strong>UK</strong><br />
Mr A Dodson, Liverpool, <strong>UK</strong> Mr D Fish, Reading, <strong>UK</strong> Mrs. S Forrest, Liverpool, <strong>UK</strong><br />
Ms J Freeman, London, <strong>UK</strong> Dr C Gillett, London, Mr J Gregory, Birmingham, <strong>UK</strong><br />
Ms J Gorst, Bucks, <strong>UK</strong> Prof. A Hanby, Leeds, <strong>UK</strong> Ms L Happerfield, Cambridge, <strong>UK</strong><br />
Dr R Hunt, Stockport, <strong>UK</strong> Dr M Ibrahim, London, <strong>UK</strong> Mr P Jackson, Leeds, <strong>UK</strong><br />
Prof. B Jasani, Cardiff, <strong>UK</strong> Ms S Jordan, London, <strong>UK</strong> Prof. E Kaye, Dublin, Ireland<br />
Mrs I Kirbis, Ljubljana, Slovenia Dr G King, Aberdeen, <strong>UK</strong> Dr T Krenacs, Szeged, Hungary<br />
Dr JM MacKenzie, Aberdeen, <strong>UK</strong> Mr. C. Marsh, Newcastle, <strong>UK</strong> Dr P Maxwell, Belfast, <strong>UK</strong><br />
Mr K McAllister, Dublin, Ireland Mrs J McGloin, London, <strong>UK</strong> Dr S McQuaid, Belfast, <strong>UK</strong><br />
Mr B Mepham, Southampton, <strong>UK</strong> Mr K Miller, London, <strong>UK</strong> Ms J Moorhead, London, <strong>UK</strong><br />
Ms P Munson, London, <strong>UK</strong> Dr M Myskow, New Zealand Mr S Nielsen, Aalborg, Denmark<br />
Dr G Orchard, London, <strong>UK</strong> Dr S Pinder, Cambridge, <strong>UK</strong> Mrs F Rae, Edinburgh, <strong>UK</strong><br />
Dr B Rasmussen, Roskilde, Denmark Dr A Riley, Stirling, <strong>UK</strong> Mr J Ronan, Nottingham, <strong>UK</strong><br />
Dr V Save, Cambridge, <strong>UK</strong> Dr F Schmitt, Porto, Portugal Ms D Steele, London, <strong>UK</strong><br />
Dr M Thom, London, <strong>UK</strong> Mrs B Totty, Cambridge, <strong>UK</strong> Mrs. R Van Wijk, Cape Town, South Africa<br />
Dr M Vyberg, Aalborg, Denmark Mrs J Williams, Portsmouth, <strong>UK</strong> Mrs S Wise, London, <strong>UK</strong><br />
Dr C Wong, Hong Kong Ms S Wozniak, Cardiff, <strong>UK</strong><br />
Office Staff Technical Data Input Steering committee Chairman<br />
Mrs AL Rhodes Mr D Fish (Techniques in Cellular Pathology)<br />
Mrs M Perez Mrs Barbara Totty<br />
Accounts Publishing Manager Typesetting<br />
Ms S Slaymark Mr R Martin Medical In<strong>for</strong>matics Unit, University of Ox<strong>for</strong>d<br />
Published by The KT Group © 2005 <strong>UK</strong> <strong>NEQAS</strong>-ICC /KTG/MIU/2000/09-05
Run 65 Editorial<br />
123<br />
<strong>Immunocytochemistry</strong> — Editorial<br />
Articles <strong>for</strong> <strong>Immunocytochemistry</strong> Journal are like buses (or good English cricketers), you wait <strong>for</strong><br />
ages then two or three come along at once. I am in the happy position of having more articles to<br />
publish than can reasonably be accommodated in one issue of the journal. This issue brings you a<br />
paper from Varma et al concerning prostate immunohistochemistry, and a report from Martin,<br />
Dodson and Ibrahim on the results of the <strong>UK</strong> <strong>NEQAS</strong>-ICC user satisfaction survey; you will have to<br />
wait until the Run 66 issue comes out to see what didn’t make the ‘cut’.<br />
August 2005<br />
Andy Dodson<br />
Department of Pathology<br />
Royal Liverpool University Hospital<br />
For the most up to date<br />
in<strong>for</strong>mation check out<br />
The <strong>UK</strong> <strong>NEQAS</strong>-ICC website<br />
at:<br />
wwwwwwwwwwww....uuuukkkknnnneeeeqqqqaaaassssiiiicccccccc....uuuuccccllll....aaaacccc....uuuukkkk
<strong>Immunocytochemistry</strong><br />
<strong>Immunocytochemistry</strong> 2005; 3: 124 – 127<br />
© <strong>UK</strong> <strong>NEQAS</strong> <strong>for</strong> <strong>Immunocytochemistry</strong>, 2005<br />
Report<br />
Inter-laboratory survey of technical variations in prostatic<br />
immunohistochemistry: basal cell markers<br />
Murali Varma 1<br />
, Daniel M Berney 2<br />
, Bharat Jasani 1<br />
, Anthony Rhodes 3<br />
1. University Hospital of Wales, Cardiff, <strong>UK</strong>; 2. St Bartholomew’s Hospital, London, <strong>UK</strong>; 3. University of the West of England, Bristol, <strong>UK</strong><br />
Correspondence to: Dr M Varma, Department of Histopathology, University Hospital of Wales, Heath Park, Cardiff CF14 4XN Wales, <strong>UK</strong><br />
Tel: +44-2920745316; Fax: +44-2920742701; E-mail: Murali.Varma@cardiffandvale.wales.nhs.uk<br />
Summary<br />
Aims: A survey of the extent of variation in the use of basal cell markers in prostate immunohistochemistry.<br />
Methods: A questionnaire was sent to all laboratories registered with the United Kingdom National<br />
External Quality Assurance Scheme <strong>for</strong> <strong>Immunocytochemistry</strong> enquiring about the immunohistochemical<br />
methods routinely used <strong>for</strong> the diagnosis of prostate cancer.<br />
Results: Responses were received from 220 (68%) of laboratories. Basal cell marker immunohistochemistry<br />
was per<strong>for</strong>med by 115 (87%) of 133 responding <strong>UK</strong> laboratories. Most (60%) of these laboratories used a<br />
single basal cell marker. The most commonly used markers were high-molecular weight cytokeratin antibody<br />
34βE12 (77%), cytokeratin 5/6 (42%) and LP34 (26%). The more recently described basal cell marker, p63<br />
was available in only 4% of laboratories. All the basal cell markers were consistently used after pre-treatment,<br />
with heat induced epitope retrieval the most commonly used method used by <strong>UK</strong> laboratories <strong>for</strong> all the<br />
markers.<br />
Conclusions: There is considerable variation in the choice of basal cell markers used by <strong>UK</strong> laboratories<br />
to distinguish benign prostate glands from prostate cancer, with most centres using only a single marker.<br />
Since none of these markers react with all benign glands, use of a combination of basal cell markers is<br />
suggested to help resolve this important differential diagnosis.<br />
© <strong>UK</strong> <strong>NEQAS</strong> <strong>for</strong> <strong>Immunocytochemistry</strong>, 2005<br />
INTRODUCTION<br />
The absence of basal cells in malignant glands as<br />
opposed to their ubiquitous presence in benign<br />
prostate glands, a finding first described by Totten et al in<br />
1953, is a well-established criterion <strong>for</strong> diagnosis of<br />
prostate cancer 1 . However, it is often not possible to reliably<br />
distinguish basal cells from stromal fibroblasts on routine<br />
histology and so immunostaining with basal cell markers<br />
is widely used as an aid to diagnosis in morphologically<br />
difficult cases.<br />
A variety of basal cell markers are available, but there<br />
is little in<strong>for</strong>mation on the range and rate of use of these<br />
antibodies.<br />
All the commonly used basal cell markers are monoclonal<br />
antibodies that generally require pre-treatment when<br />
124<br />
used in paraffin embedded material. Predigestion<br />
using enzymes such as proteases and pronases as<br />
well as heat induced epitope retrieval (HIER) using<br />
microwaving or steam are commonly used pre-treatment<br />
methods.<br />
It is recognised that the pre-treatment method may<br />
impact the sensitivity and specificity of immunostaining<br />
but the frequency of use of different pre-treatment<br />
methods with each basal cell marker in routine diagnostic<br />
practice is unknown.<br />
We there<strong>for</strong>e conducted a postal survey of immunohistochemical<br />
methods used in the diagnosis of prostate<br />
cancer in laboratories registered with the United<br />
Kingdom National External Quality Assurance Scheme<br />
<strong>for</strong> <strong>Immunocytochemistry</strong> (<strong>UK</strong> <strong>NEQAS</strong>-ICC).
METHODS<br />
• A short questionnaire was circulated to all laboratories<br />
subscribing to the <strong>UK</strong> <strong>NEQAS</strong>-ICC scheme in 2003<br />
(Figure 1). The use of the recently developed, promising<br />
positive marker <strong>for</strong> prostate cancer, alpha-methylacyl-<br />
CoA racemase (AMACR) 2 was not studied as it had<br />
been commercially available only <strong>for</strong> a few months<br />
at the time of the survey.<br />
• In order to maximise the response rate, the questionnaire<br />
along with a stamped and addressed envelope<br />
was circulated with the EQA slides in two successive<br />
runs of the scheme. Duplicated responses were<br />
identified and excluded.<br />
• From the replies received, the frequency of use of<br />
various basal cell markers and the pre-treatment<br />
methods used <strong>for</strong> them were determined.<br />
• The survey findings related to prostate specific antigen<br />
and prostate specific acid phosphatase immunohistochemistry<br />
have been discussed in a separate report 3 .<br />
Figure 1. Questionnaire circulated to all subscribers to the <strong>UK</strong><br />
<strong>NEQAS</strong>-ICC Scheme.<br />
RESULTS<br />
The questionnaire was circulated to 394 laboratories,<br />
323 of which were known to subscribe to the prostate<br />
cancer immunohistochemistry EQA module. Of the<br />
latter 323 centres, 196 represented <strong>UK</strong> laboratories.<br />
125<br />
<strong>Immunocytochemistry</strong><br />
After excluding duplicates, 220 (68%) replies were<br />
received; 133 from the <strong>UK</strong> and 87 from outside the <strong>UK</strong><br />
(13 from The Republic of Ireland, 58 from continental<br />
Europe and 16 from elsewhere). The response rate <strong>for</strong><br />
<strong>UK</strong> laboratories was there<strong>for</strong>e calculated to be 68%<br />
(133/196).<br />
Since virtually all <strong>UK</strong> laboratories practicing diagnostic<br />
prostate immunohistochemistry are known to participate<br />
in the <strong>UK</strong> <strong>NEQAS</strong>-ICC scheme, the response received<br />
from them can be considered to be representative. The<br />
situation regarding <strong>UK</strong> <strong>NEQAS</strong>-ICC participation by<br />
laboratories outside the <strong>UK</strong> is not known so the responses<br />
from these non-<strong>UK</strong> laboratories may not be representative<br />
of the practice in these countries. These data were<br />
there<strong>for</strong>e considered separately from those from <strong>UK</strong><br />
laboratories.<br />
Table 1. Number of basal cell markers used in each laboratory.<br />
Table 2. Choice of basal cell marker (percentage figures are<br />
percentage of laboratories that used basal cell markers).<br />
The frequency of use of various basal cell markers is<br />
summarised in Tables 1 and 2. Over half the responding<br />
laboratories used only a single basal cell marker, with<br />
high-molecular weight cytokeratin antibody clone<br />
34βE12 being the most widely used.<br />
The pre-treatment methods used <strong>for</strong> the basal cell<br />
markers are summarised in Tables 3 and 4. All the basal<br />
cell markers used were of the monoclonal antibody<br />
type and were used after pre-treatment, with HIER<br />
being the most commonly applied method.
<strong>Immunocytochemistry</strong><br />
Table 3. Pre-treatment methods used <strong>for</strong> basal cell markers in <strong>UK</strong> Laboratories (percentage figures are percentage of laboratories<br />
that used that particular basal cell marker).<br />
Table 4. Pre-treatment methods used <strong>for</strong> basal cell markers in Non-<strong>UK</strong> Laboratories (percentage figures are percentage of<br />
laboratories that used that particular basal cell marker).<br />
DISCUSSION<br />
Immunohistochemistry using markers specific <strong>for</strong> basal<br />
cells of the prostate gland is widely used as an adjunct<br />
to the diagnosis of prostate cancer 4 . In our survey, 87%<br />
of laboratories in which prostate marker immunohistochemistry<br />
was available used at least one basal cell<br />
marker. It is possible that some of the respondents that<br />
did not use basal cell markers used PSA and/or PSAP only<br />
to establish the prostatic origin of metastasis and were<br />
presumably not concerned with the primary diagnosis<br />
of prostate cancer.<br />
A number of prostatic basal cell markers are currently<br />
available. In the <strong>UK</strong>, the most widely used basal cell<br />
marker appears to be the high-molecular weight cytokeratin<br />
antibody clone 34βE12 (77%). Cytokeratin 5/6 and<br />
LP34 were used by a significant minority of respondents<br />
(41% and 25% respectively) while p63 was routinely<br />
employed by only 4% of centres. The popularity of<br />
34βE12 is probably related to the fact that its utility has<br />
been extensively studied and validated in the literature,<br />
particularly in the USA. In contrast, the infrequently used<br />
p63 has only recently been established as a basal cell<br />
marker.<br />
126<br />
The wide variation in the use of basal cell markers<br />
would reflect the paucity of studies comparing them<br />
and providing guidance regarding their relative usefulness<br />
and efficacy. A few small studies have reported<br />
cytokeratin 5/6 and p63 to be marginally more sensitive<br />
than 34βE12 5,6,7 . Freeman et al found LP34 to be slightly<br />
more sensitive than cytokeratin 5/6 and cytokeratin 14<br />
but the panel of markers studied did not include<br />
34βE12 8 . Moreover, as the authors commented, unlike<br />
other basal cell markers, LP34 generally reacts with the<br />
secretory cells of the prostate gland, albeit less intensely<br />
than basal cells, making interpretation sometimes more<br />
difficult.<br />
Unlike most other immunohistochemical markers, basal<br />
cell markers are used to distinguish benign prostate<br />
glands from prostate cancer and the diagnosis of<br />
malignancy is confirmed by a negative immunoreaction,<br />
so it would be important to make every ef<strong>for</strong>t to maximise<br />
the sensitivity of immunostaining with these markers.<br />
However, it is generally recognised that none of the<br />
basal cell markers are absolutely sensitive as a small<br />
proportion of benign glands are negative with each of
these markers 5,6,9 . Using a combination of basal cell<br />
markers has been shown to increase the sensitivity of<br />
immunostaining 10 . In this context, it is noteworthy that<br />
currently less than half of <strong>UK</strong> laboratories (40%) appear<br />
to use more than one basal cell marker.<br />
The ideal combination of basal cell markers <strong>for</strong> use in<br />
diagnostic immunohistochemistry practice is uncertain.<br />
34βE12, cytokeratin 5/6 and LP34 are similar in that they<br />
are directed against high-molecular weight cytokeratins<br />
and the immunoreactivity is membranous/intracytoplasmic.<br />
In contrast, p63, a homologue of p53, displays<br />
nuclear immunoreactivity. Hence, using one of the<br />
high-molecular weight cytokeratin antibodies in tandem<br />
with p63 as suggested by Zhou et al may be more<br />
advantageous 10 .<br />
The optimal use of basal cell markers may be in<br />
combination with AMACR, which has been reported<br />
to be consistently positive in prostate cancer. The use of<br />
such a panel would help exclude false negative<br />
immunonegativity with basal cell markers due to technical<br />
factors in immunostaining or cautery effect in<br />
transurethral resection specimens. However, AMACR<br />
immunoreactivity should always be interpreted in<br />
conjunction with basal cell immunohistochemistry, as<br />
high-grade PIN often expresses AMACR 11 .<br />
It is recognised that high-molecular weight cytokeratin<br />
antibodies are sensitive to <strong>for</strong>malin fixation and require<br />
pre-treatment when used on paraffin embedded<br />
material 12 . A few studies using monoclonal antibody clone<br />
34βE12 have found high-molecular weight cytokeratin<br />
expression in prostate cancer after the use of heat<br />
pre-treatment but not after enzyme predigestion 12,13,14 .<br />
This immunoreactivity was generally restricted to rare<br />
tumour cells. This potential pitfall in prostate cancer<br />
diagnosis is significant, as most centres in the <strong>UK</strong> appear<br />
to use heat pre-treatment <strong>for</strong> high-molecular weight<br />
cytokeratin antibodies, LP34, 34βE12 and cytokeratin 5/6.<br />
In conclusion, our study confirms that there is a wide<br />
variation in the immunohistochemical methods used to<br />
identify basal cells of the prostate gland. This variation<br />
probably reflects the fact that none of the available<br />
markers have been clearly shown to be better than the<br />
others. In view of the clinical importance of basal cell<br />
immunohistochemistry in confirming the diagnosis of<br />
adenocarcinoma and the lack of a completely sensitive<br />
marker, use of a combination of at least two basal cell<br />
markers is recommended.<br />
127<br />
REFERENCES<br />
<strong>Immunocytochemistry</strong><br />
1. Totten RS, Heineman MW, Hudson PB, et al. Microscopic differential<br />
diagnosis of latent carcinoma of the prostate. Arch Pathol 1953; 55:<br />
131-141<br />
2. Jiang Z, Woda BA, Rock KL, et al. P504S: A new molecular marker <strong>for</strong> the<br />
detection of prostate carcinoma. Am J Surg Pathol 2001; 25: 1397-1404<br />
3. Varma M, Berney DM, Jasani B, Rhodes A. Technical variations in<br />
prostatic immunohistochemistry: need <strong>for</strong> standardisation and stringent<br />
quality assurance in PSA and PSAP immunostaining. J Clin Pathol<br />
2004; 57: 687-690<br />
4. Wojno KJ, Epstein JI. The utility of basal cell-specific anti-cytokeratin<br />
antibody in the diagnosis of prostate cancer. Am J Surg Pathol 1995;<br />
19: 251-260<br />
5. Abrahams NA, Ormsby AH, Brainard J. Validation of cytokeratin 5/6 as<br />
an effective substitute <strong>for</strong> keratin 903 in the differentiation of benign<br />
from malignant glands in prostate needle biopsies. Histopathology<br />
2002; 41: 35-41<br />
6. Shah RB, Zhou M, LeBlanc M, et al. Comparison of the basal cell-specific<br />
markers, 34betaE12 and p63, in the diagnosis of prostate cancer.<br />
Am J Surg Pathol 2002; 26: 1161-1168<br />
7. Weinstein MH, Signoretti S, Loda M. Diagnostic utility of immunohistochemical<br />
staining <strong>for</strong> p63, a sensitive marker of prostatic basal cells.<br />
Mod Pathol 2002; 15: 1302-1308<br />
8. Freeman A, Treunicht K, Munson P, et al. A comparison of basal cell<br />
markers used in the prostate. Histopathology 2002; 40: 492-494 (letter)<br />
9. Varma M, Amin MB, Linden MD and Zarbo RJ. Discriminant staining<br />
pattern of small glandular and preneoplastic lesions of the prostate<br />
using high molecular weight cytokeratin antibody. Mod Pathol 1997;<br />
10: 93A (abstract)<br />
10. Zhou M, Shah R, Shen R, et al. Basal cell cocktail (34betaE12 and p63)<br />
improves the detection of prostate basal cells. Am J Surg Pathol 2003;<br />
27: 365-371<br />
11. Wu CL, Yang XJ, Tretiakova M, et al. Analysis of alpha-methylacyl-CoA<br />
racemase (P504S) expression in high-grade prostatic intraepithelial<br />
neoplasia. Hum Pathol 2004; 35: 1008-1013<br />
12. Varma M, Linden MD, Amin MB. Effect of <strong>for</strong>malin fixation and<br />
epitope retrieval techniques on antibody 34betaE12 immunostaining<br />
of prostatic tissues. Mod Pathol 1999; 12: 472-478<br />
13. Lindemann N, Weidner N. Immunohistochemical profile of prostatic<br />
and urothelial carcinoma: Impact of heat-induced epitope retrieval<br />
and presentation of tumors with intermediate features. Appl<br />
Immunohistochem 1996; 4: 264-275<br />
14. Bennett CJ, Hicks JL, Gage WR, et al. “False positive” immunostaining<br />
of 34BE12 in prostate cancer: Systematic study of the effect of antigen<br />
retrieval conditions using high density tissue microarrays. Mod Pathol<br />
2003; 1: 141A (abstract)
<strong>Immunocytochemistry</strong><br />
<strong>Immunocytochemistry</strong> 2005; 3: 128 – 136<br />
© <strong>UK</strong> <strong>NEQAS</strong> <strong>for</strong> <strong>Immunocytochemistry</strong>, 2005<br />
Article<br />
Report of results from the <strong>UK</strong> <strong>NEQAS</strong>-ICC questionnaire<br />
Roger J Martin 1 , Andrew Dodson 2 , Merdol Ibrahim 3<br />
1: Consult Business Development Ltd. 2: Department of Pathology, Royal Liverpool University Hospital. 3: <strong>UK</strong>-<strong>NEQAS</strong>-ICC<br />
Correspondence to: Dr. Merdol Ibrahim, <strong>UK</strong> <strong>NEQAS</strong>-ICC Office, Suite 3/22 Hamilton House, Mabledon Place, London WC1H 9BB <strong>UK</strong><br />
E-mail: merdol.ibrahim@ucl.ac.uk; Tel: +44(0)207 554 8679; Fax: +44(0)207 554 8685<br />
Summary<br />
In 2004 a questionnaire was circulated to all <strong>UK</strong> <strong>NEQAS</strong>-ICC participants. The aims the survey were: firstly<br />
to assess user-satisfaction with various aspects of the scheme as it is now; and, secondly to encourage<br />
suggestions <strong>for</strong> improvements to the scheme, including new antibodies to be included. Forty-eight<br />
completed questionnaires were returned, representing a response-rate of over 10%. The following report<br />
describes the results in detail.<br />
<strong>UK</strong> <strong>NEQAS</strong>-ICC would like to thank all those participants who took the trouble to fill-in and return their<br />
questionnaires: your feedback is greatly appreciated.<br />
© <strong>UK</strong> <strong>NEQAS</strong> <strong>for</strong> <strong>Immunocytochemistry</strong>, 2005<br />
INTRODUCTION<br />
The <strong>UK</strong> <strong>NEQAS</strong>-ICC Scheme is run primarily <strong>for</strong> the benefit<br />
of its users. It is intended that it should be a tool which<br />
participants can use to help them maintain and<br />
improve the quality of their immunocytochemistry. To<br />
be effective it must serve its users’ needs.<br />
Opportunities <strong>for</strong> the management team at <strong>UK</strong> <strong>NEQAS</strong>-<br />
ICC to hear participants’ views with regard to the service<br />
it provides are relatively limited. It was there<strong>for</strong>e decided<br />
that a more proactive and structured approach was<br />
required, and a short questionnaire was <strong>for</strong>mulated<br />
covering all the major areas of activity. Users were<br />
asked to grade their response to various questions as<br />
Very satisfied, Satisfied, or Dissatisfied, and space was<br />
given <strong>for</strong> those who wished to elaborate on their<br />
responses to do so. In addition, in<strong>for</strong>mation regarding<br />
<strong>UK</strong> <strong>NEQAS</strong>-ICC organised meetings was sought, and<br />
suggestions <strong>for</strong> antibodies not currently covered, which<br />
might be included in future runs were also asked <strong>for</strong>.<br />
THE QUESTIONS<br />
The questionnaire comprised twelve questions. The first<br />
six dealt with various aspects of the assessment process<br />
itself:<br />
128<br />
Question 1. How satisified are you with the way you<br />
receive your EQA samples?<br />
Question 2. How satisfied are you with the time you are<br />
given to stain the samples?<br />
Question 3. How satisfied are you with the procedure<br />
<strong>for</strong> returning the samples?<br />
Question 4. How satisfied are you with the time taken to<br />
receive your results?<br />
Question 5. How satisfied are you with the <strong>for</strong>mat in<br />
which you receive your results?<br />
Question 6. How satisfied are you with the comments<br />
which accompany the results?<br />
The seventh question concerned the <strong>Immunocytochemistry</strong><br />
Journal:<br />
Question 7. How satisfied are you with the <strong>Immunocytochemistry</strong><br />
newsletter?<br />
Question 8 was about enquiries and complaints:<br />
Question 8. Have you ever had cause to contact the<br />
<strong>UK</strong> <strong>NEQAS</strong>-ICC office with a question or complaint?<br />
If yes – how satisfied were you with the way this was<br />
handled?<br />
The final four questions were centred around the area<br />
of meetings:<br />
Question 9. Have you attended a <strong>UK</strong> <strong>NEQAS</strong>-ICC meeting<br />
in the last 12 months?<br />
If yes – how satisfied were you with this meeting?
Question 10. How satisfied are you with the number and<br />
locations of <strong>UK</strong> <strong>NEQAS</strong>-ICC meetings?<br />
Question 11. How satisfied are you with the opportunities<br />
you have to discuss technical or logistical issues at<br />
meetings?<br />
Question 12. Do you intend to attend any <strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
meetings next year?<br />
RESULTS<br />
Question 1. How satisfied are you with the way you<br />
receive your EQA samples?<br />
Very satisfied Satisfied Dissatisfied<br />
24/47 (51%) 21/47 (45%) 2/47 (4%)<br />
One returnee did not answer this question.<br />
Comments received relating to this question:<br />
• ‘Sometimes feel EQA samples stain more weakly than<br />
in-house samples. May have been cut and stored <strong>for</strong><br />
some time’<br />
• ‘I would like to know when the samples will arrive, <strong>for</strong><br />
example by e-mail’<br />
• ‘It would be useful to receive the <strong>for</strong>ms each time by<br />
e-mail’<br />
• ‘Two sections do not allow <strong>for</strong> much experimentation<br />
to give the best possible stain’<br />
• ‘More <strong>UK</strong> <strong>NEQAS</strong> sections could be supplied so staining<br />
could be…optimised’<br />
Question 2. How satisfied are you with the time you are<br />
given to stain the samples?<br />
Very satisfied Satisfied Dissatisfied<br />
21/47 (45%) 23/47 (49%) 3/47 (6%)<br />
129<br />
<strong>Immunocytochemistry</strong><br />
One returnee did not answer this question.<br />
Comments received relating to this question:<br />
• ‘The time period is too short to assess the previous<br />
results, make improvements and stain the next run…’<br />
• ‘The time is sometimes a little short’<br />
• ‘Should always allow a full calendar month’<br />
Question 3. How satisfied are you with the procedure<br />
<strong>for</strong> returning the samples?<br />
Very satisfied Satisfied Dissatisfied<br />
25/48 (52%) 17/48 (35%) 6/48 (13%)<br />
Comments received relating to this question:<br />
• ‘Perhaps paperwork could be simplified/reduced’<br />
• ‘Forms are clumsy and out-of-date…Can they be<br />
streamlined and generally easier/quicker to fill-in?’<br />
• ‘Space too small on <strong>for</strong>ms. We wish we could fill-out<br />
the <strong>for</strong>m through the internet’<br />
• ‘No pre-typed labels <strong>for</strong> addresses return provided’<br />
• ‘It is rather monotonous writing the same in<strong>for</strong>mation<br />
on numerous sheets’
<strong>Immunocytochemistry</strong><br />
Question 4. How satisfied are you with the time taken to<br />
receive your results?<br />
Very satisfied Satisfied Dissatisfied<br />
10/47 (21%) 32/47 (68%) 5/47 (11%)<br />
One returnee did not answer this question.<br />
In total, ten comments were received relating to this<br />
question, all were variations on the following:<br />
• ‘If the results came earlier it would be better, but we<br />
understand that it takes time to review all slides’<br />
Question 5. How satisfied are you with the <strong>for</strong>mat in<br />
which you receive your results?<br />
Very satisfied Satisfied Dissatisfied<br />
23/48 (48%) 22/48 (46%) 3/48 (6%)<br />
No comments were received relating to this question.<br />
Question 6. How satisfied are you with the comments<br />
which accompany the results?<br />
Very satisfied Satisfied Dissatisfied<br />
9/46 (20%) 25/46 (54%) 12/46 (26%)<br />
130<br />
Two returnees did not answer this question.<br />
This question attracted the most comments of any in the<br />
survey, with a total of seventeen. The range is covered<br />
in the following examples:<br />
• ‘Could have more depth in comments’<br />
• ‘Breakdown of where exactly marks have been<br />
deducted and why’<br />
• ‘Could not the marking be out-of-10, with one overall<br />
set of comments?’<br />
• ‘If there are bad results, please give in<strong>for</strong>mation<br />
about the reasons if you can…fixation, antibody<br />
dilution etc’<br />
• ‘Inconsistency between marker’<br />
• ‘They don’t always help improve staining – not<br />
specific enough’<br />
• ‘More detail in comments section. Photograph of top<br />
scoring section to accompany results’<br />
• ‘An average result <strong>for</strong> all members of the scheme<br />
included with results’<br />
Question 7. How satisfied are you with the <strong>Immunocytochemistry</strong><br />
newsletter?<br />
Very satisfied Satisfied Dissatisfied<br />
26/48 (54%) 22/48 (46%) 0/48 (0%)<br />
Comments received relating to this question:<br />
• ‘Trends in detection methods which are giving the<br />
best results. Can we standardise, should we try – stats<br />
may be of help’
• ‘More in<strong>for</strong>mation on meetings’<br />
• ‘A mean of each stain from all participants would be<br />
helpful with the graphs <strong>for</strong> statistical interpretation<br />
purposes’<br />
Question 8. Have you ever had cause to contact the<br />
<strong>UK</strong> <strong>NEQAS</strong>-ICC office with a question or complaint?<br />
31/48 (65%) of returnees had contacted the <strong>UK</strong> <strong>NEQAS</strong>-<br />
ICC office, 17/48 (35%) had not.<br />
Question 8 (follow-up question). If yes – how satisfied<br />
were you with the way this was handled?<br />
Very satisfied Satisfied Dissatisfied<br />
16/30 (53%) 12/30 (40%) 2/30 (7%)<br />
Of the 31 returnees to whom this question applied, one<br />
did not answer.<br />
One comment was received relating to this question:<br />
• ‘Two times. The first time we got no answer. In the<br />
other case we got a satisfactory answer’<br />
Question 9. Have you attended a <strong>UK</strong> <strong>NEQAS</strong>-ICC meeting<br />
in the last 12 months?<br />
15/48 (31%) of returnees had attended a meeting, 33/48<br />
(69%) had not.<br />
Question 9 (follow-up question). If yes – how satisfied<br />
were you with this meeting?<br />
Very satisfied Satisfied Dissatisfied<br />
8/15 (53%) 7/15 (47%) 0/15 (0%)<br />
131<br />
<strong>Immunocytochemistry</strong><br />
The graphical representation of these results:<br />
Question 10. How satisfied are you with the number and<br />
locations of <strong>UK</strong> <strong>NEQAS</strong>-ICC meetings?<br />
Very satisfied Satisfied Dissatisfied<br />
3/33 (9%) 22/33 (67%) 8/33 (24%)<br />
Fifteen returnees did not answer this question.<br />
Comments relating to questions 10 – 12 have been<br />
grouped together at the end of this section.<br />
Question 11. How satisfied are you with the opportunities<br />
you have to discuss technical or logistical issues at<br />
meetings?<br />
Very satisfied Satisfied Dissatisfied<br />
2/24 (8%) 17/24 (71%) 5/24 (21%)<br />
Twenty-four returnees did not answer this question.<br />
The graphical representation of these results is shown at<br />
top of next page.
<strong>Immunocytochemistry</strong><br />
Question 12. Do you intend to attend any <strong>UK</strong> <strong>NEQAS</strong>-<br />
ICC meetings next year?<br />
41/45 (91%) of returnees were planning on attending a<br />
meeting, 4/45 (9%) were not.<br />
132<br />
Three returnees did not answer this question.<br />
Comments relating to meetings:<br />
• ‘It would be nice to have the occasional meeting in<br />
other parts of the country, and not just in London’<br />
• ‘For overseas participants it is difficult to attend<br />
meetings. A summary of the main topics discussed…would<br />
help’<br />
• ‘Perhaps devote a session to questions and answers<br />
<strong>for</strong> each module’<br />
• ‘Dublin is too far away with no provision <strong>for</strong> attending<br />
1 of the 3 days, which makes it too expensive and<br />
too time consuming’<br />
• ‘More focus on the technical parts’<br />
• ‘Come to Northern England’<br />
Results Summary Chart. Numerical values were assigned to the responses as follows: Very satisfied = +1, Satisfied = 0,<br />
Dissatisfied = −1. A user satisfaction index was calculated <strong>for</strong> each question by multiplying the assigned values by the<br />
proportions in each category, and summing the resulting figures. The results are depicted in the chart above. A value of<br />
+1 would indicate that 100% of returnees are very satisfied, while a value of −1 would mean that 100% were dissatisfied.
SUGGESTIONS FOR NEW ANTIBODIES TO BE<br />
INCLUDED<br />
A number of suggestions <strong>for</strong> new antibodies that might be<br />
looked at were received. These were mainly applicable<br />
to the General Module or to the Lymphoma Module (the<br />
most frequently requested are listed below).<br />
General Module: Cytokeratins 7 and 20, Thyroid<br />
Transcription Factor-1, AMACR (P504S), p63.<br />
Lymphoma Module: bcl6, CD5, CD10, CD21, CD23.<br />
There were also a number of requests <strong>for</strong> CD117 (c-KIT)<br />
to be included (since this survey was conducted <strong>UK</strong><br />
<strong>NEQAS</strong>-ICC has announced the launch of the<br />
Alimentary Tract Module which looks at this antigen).<br />
DISCUSSION<br />
This survey has been of great value, and while much of<br />
the feedback it has provided has been very positive it<br />
has also served to highlighted a number of areas<br />
where improvements can be made. The <strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
management team have made, and are continuing to<br />
make changes to a number of operational aspects to<br />
address these; a number of which are discussed below.<br />
BETTER COMMUNICATION AND FEEDBACK<br />
The Scheme is moving towards e-mail to communicate<br />
in a more efficient and time saving manner with all<br />
participants. A recent example has been notifications<br />
with respect to <strong>UK</strong> <strong>NEQAS</strong>-ICC workshops, which have<br />
been sent out electronically. It is intended that e-mail<br />
notifications will be implemented <strong>for</strong> all aspects of <strong>UK</strong><br />
<strong>NEQAS</strong>-ICC activities, and <strong>for</strong> this reason all participants<br />
who have not already done so, are urged to submit<br />
their current e-mail address. E-Mail addresses may be<br />
sent to the <strong>UK</strong> <strong>NEQAS</strong>-ICC office using either of<br />
the following addresses: rmkdalr@ucl.ac.uk or<br />
m.perez@ucl.ac.uk<br />
During each assessment there are approximately 5000<br />
slides that are assessed in a three-to-four week period.<br />
This means that there are a great deal of scores and<br />
comments to be collated and sent-out, however, it is<br />
still very important to get the results to all participants as<br />
soon as possible. In a move to speed-up this operation<br />
assessors now log their scores directly into laptops<br />
(previously paper score sheets were used, with scores<br />
being transferred later to a central database). In<br />
addition to improvements in speed, this also allows<br />
assessors the opportunity to type in an individual comment<br />
if the prefigured ones are not appropriate <strong>for</strong> any given<br />
slide. This is something which could not be accommodated<br />
by the paper-based system, and it is hoped that<br />
it will be of considerable benefit.<br />
133<br />
<strong>Immunocytochemistry</strong><br />
EDUCATIONAL REMIT OF THE SCHEME<br />
The Scheme aims to educate and help all participants.<br />
In particular it aims to help participants to improve and<br />
adapt their protocols where it is felt that improvements<br />
can be made. ‘Best Methods’ have been published in<br />
the <strong>Immunocytochemistry</strong> Journal <strong>for</strong> every antibody<br />
used in the Scheme. This resource should be extremely<br />
valuable <strong>for</strong> participants wishing to make changes to<br />
their own methods when they prove sub-optimal.<br />
It is gratifying to see that the <strong>Immunocytochemistry</strong><br />
Journal per<strong>for</strong>med well, with this aspect of the<br />
Scheme’s activities achieving the highest satisfaction<br />
rating of any in the survey. Even so, the management<br />
team at <strong>UK</strong> <strong>NEQAS</strong>-ICC are not resting on their laurels<br />
with respect to the Journal. It is intended that improvements<br />
to layout will be made in the next few months,<br />
with individual Module reports having a more logical<br />
and consistent layout.<br />
Discussions are currently underway concerning additional<br />
statistical analysis that can be undertaken on the data<br />
produced at each Run, which we hope will be of further<br />
benefit to participants.<br />
TIME ALLOWED FOR SLIDE STAINING<br />
It is felt that a turnaround of about three weeks to stain<br />
the <strong>UK</strong> <strong>NEQAS</strong>-ICC and in-house control slides is adequate.<br />
We believe that the <strong>UK</strong> <strong>NEQAS</strong>-ICC samples should fit in<br />
with the normal days run <strong>for</strong> any particular laboratory.<br />
With regard to the question of only two slides being<br />
provided per antibody request, it should be noted that<br />
any increase in the number of slides would have an<br />
enormous effect on workload <strong>for</strong> the laboratory providing<br />
this material, and very probably a considerable cost<br />
implication. It is not envisaged that this will be changed<br />
<strong>for</strong> these reasons, however, if any participant does<br />
require further slides to test out their protocols these<br />
can normally be provided on an ad hoc basis upon<br />
request.<br />
IMPROVED WEB-BASED COMMUNICATION<br />
With respect to procedure <strong>for</strong> returning samples; a move<br />
towards an internet-based <strong>for</strong>m submission procedure is<br />
currently underway. Forms will be adapted to make<br />
their completion easier and participants will be able to<br />
submit via the website. At present an interim procedure<br />
has been put in place, whereby participants may<br />
download and then e-mail the data sheets. This facility<br />
can be accessed from the website:<br />
www.ukneqasicc.ucl.ac.uk/runXXdatasheets<br />
(just replace the ‘XX’ with the Run number).
<strong>Immunocytochemistry</strong><br />
Behind the scenes the website is also undergoing a<br />
trans<strong>for</strong>mation and we hope that soon all participants<br />
will be able to access results, view more images, and<br />
download and submit new versions of datasheets.<br />
Furthermore a user-group and messaging system will be<br />
put in place to allow participants to communicate with<br />
one another. A special acknowledgment should be<br />
made to Rifat Hamoudi who has been working<br />
extremely hard to put this in place.<br />
MEETING / WORKSHOPS / DISCUSSIONS<br />
The view that <strong>UK</strong> <strong>NEQAS</strong>-ICC meetings should occur<br />
around the <strong>UK</strong> and not only in London, which was<br />
expressed by a number of participants in their survey<br />
responses has been noted. In 2005, workshops and<br />
lectures have taken place in London, Wolverhampton<br />
and Northumbria, it is hoped that this means that <strong>UK</strong><br />
<strong>NEQAS</strong>-ICC has ‘come to Northern England’!<br />
The next major conference will be in Dublin (July 2006).<br />
This city was found to offer both exemplary conference<br />
facilities and excellent social opportunities when the <strong>UK</strong><br />
<strong>NEQAS</strong>-ICC conference was previously held there. The<br />
conference organisers will be looking into having further<br />
technical sessions during this, and future meetings.<br />
It is also envisaged that the setting-up of a user-group<br />
and messaging system on the website will allow individuals<br />
participants to resolve issues by a system of self-help in<br />
a way that meetings or the <strong>Immunocytochemistry</strong><br />
Journal may not be able to do.<br />
CONCLUSION<br />
<strong>UK</strong> <strong>NEQAS</strong>-ICC would like to once again thank those<br />
participants who responded to the survey. It is hoped<br />
that they will agree with us that this has been a most<br />
worthwhile exercise. If any participant has additional<br />
comments on this survey, or indeed any aspect of the<br />
Scheme the team at <strong>UK</strong> <strong>NEQAS</strong>-ICC headquarters<br />
would be delighted to hear from them.<br />
134
<strong>UK</strong> <strong>NEQAS</strong>-ICC REVIEWS OF RUN 65<br />
INTRODUCTION<br />
135<br />
<strong>Immunocytochemistry</strong> — Introduction to Reviews<br />
The <strong>UK</strong> National External Quality Assessment Scheme <strong>for</strong> <strong>Immunocytochemistry</strong> (<strong>UK</strong> <strong>NEQAS</strong>-ICC) assessments takes place<br />
at approximately three-monthly intervals, throughout the fiscal year. Currently laboratories are able to participate in up<br />
to 6 different modules, depending on their service commitments and specialised areas of interest. These modules are as<br />
follows:<br />
1. The general pathology module; catering <strong>for</strong> routine markers used by the majority of pathology departments<br />
offering a routine immunocytochemistry service.<br />
2. The breast hormonal receptor module; catering <strong>for</strong> laboratories routinely demonstrating oestrogen and<br />
progesterone receptors on paraffin processed tissues.<br />
3. The breast HER-2 module; catering <strong>for</strong> laboratories routinely testing <strong>for</strong> HER-2 on paraffin processed tissues.<br />
4. The lymphoma module; catering <strong>for</strong> the markers used by laboratories with a specialised interest in lymphoid<br />
pathology.<br />
5. The neuropathology module; catering <strong>for</strong> the markers common to most neuropathology departments.<br />
6. The cytology module; catering <strong>for</strong> markers commonly requested on cytological preparations.<br />
7. Alimentary tract pathology (pilot) module; catering <strong>for</strong> laboratories specialising in this area or pathology.<br />
What happens at assessment?<br />
At each assessment, laboratories are sent <strong>for</strong>malin fixed and paraffin processed sections (alcohol fixed cytospins <strong>for</strong><br />
the cytology scheme) along with instruction sheets <strong>for</strong> the schemes to which they have subscribed. They are requested<br />
to demonstrate two different antigens (one <strong>for</strong> each of the breast schemes) on the slides provided and return the<br />
best <strong>for</strong> each antigen <strong>for</strong> assessment along with their usual In House control slide stained with the same marker(s).<br />
For most of the modules, one of the antigens requested is repeated from one assessment to the next <strong>for</strong> a period of<br />
twelve months, and serves as a ‘gold standard’. This allows participants to implement recommended changes if<br />
their quality of immunostaining is found to be sub-standard and to test out their improved technique at the next<br />
assessment. They are also requested to complete a short questionnaire giving brief details of the antibody and<br />
method they have employed. The slides bearing each participant’s unique code number (to ensure anonymity) are<br />
then marked by an expert panel consisting of senior biomedical or clinical scientists and usually one consultant<br />
histopathologist.<br />
Interpretation of the scores achieved at assessment<br />
Each of the four assessors awards a mark from 1 to 5 using the guidelines issued <strong>for</strong> each antigen. The marks are then<br />
added together to give a score out of 20. An acceptable level of staining attracts marks greater than 12/20. A<br />
borderline mark in the range 10/20 – 12/20 indicates that whilst some in<strong>for</strong>mation can be obtained from the slide,<br />
the staining is sub-optimal. Lastly, a score of less than 10/20 is given <strong>for</strong> poor immunocytochemistry that has failed to<br />
clearly demonstrate the required components.<br />
Journal contents<br />
The following pages summarises the results of Assessment Run 62 and provide; guidelines as to how the assessors<br />
marked the immunostaining, brief reviews <strong>for</strong> each antigen assessed, colour photomicrographs where appropriate,<br />
best methods, distribution of results and tabulation of technical data.<br />
Best methods<br />
Included with the reviews are examples of methods employed by participants who achieved some of the best<br />
immuno-staining at this assessment. We have selected techniques, which employ primary antibodies used by the<br />
majority of participants. Examples of the quality of staining that was achieved using these methods are shown in the<br />
colour plates.<br />
Technical data<br />
All the basic technical data collated from this assessment is in tabulated <strong>for</strong>m in order to be economic with the space<br />
available. This is restricted to the sections provided by <strong>UK</strong> <strong>NEQAS</strong>-ICC i.e. the standard material.
<strong>Immunocytochemistry</strong> — General Pathology<br />
The General Pathology Module<br />
Julie Williams<br />
Antigens assessed: Pan Cytokeratin*, Thyroglobulin<br />
*The small number of laboratories not stocking an<br />
antibody to pan-cytokeratin were requested to carry-out<br />
staining <strong>for</strong> high-molecular weight cytokeratins with, <strong>for</strong><br />
example LP34, and <strong>for</strong> low-molecular weight cytokeratins<br />
with, <strong>for</strong> example CAM5.2, on two separate sections.<br />
Tissue sections circulated: composite block of tonsil and<br />
gut (pan-cytokeratin), thyroid (thyroglobulin).<br />
Number of participating laboratories: 396 (pancytokeratin),<br />
330 (thyroglobulin)<br />
General guidelines used in the assessment of slides:<br />
SCORE STAINING PATTERN<br />
0 No returns.<br />
1 Little or no staining of the antigen in question.<br />
2 Very weak demonstration of cells expected to<br />
stain or many of these cells were not demonstrated.<br />
3 Weak demonstration of cells expected to stain.<br />
4 Good demonstration of all cells expected to stain.<br />
5 Excellent demonstration of all cells expected to<br />
stain, with little or no background.<br />
NB. These are only very general guidelines and marks were<br />
deducted <strong>for</strong> such things as poor localisation of staining or diffuse<br />
staining, inappropriate staining of certain cell types, excessive<br />
background staining, excessive counter-stain, uneven staining<br />
or other factors which made interpretation difficult.<br />
The four individual scores <strong>for</strong> each slide were added together<br />
to give a mark out of 20.<br />
Pan-Cytokeratin<br />
Features of optimal immunostaining (Plates 1 & 2)<br />
• Intense cytoplasmic staining of the complete epithelial<br />
layer in both the tonsil and gut. There should be no<br />
staining of lymphocytes although occasional staining<br />
of plasma cells by some cytokeratin antibodies has<br />
been reported (Wotherspoon et al).<br />
• The tissue morphology should be relatively<br />
untouched by retrieval.<br />
Features of sub-optimal immunostaining (Plates 3 & 4)<br />
• Generalised weak or incomplete staining of epithelium.<br />
• Excessive proteolysis of supporting connective tissue<br />
resulting in poor morphology.<br />
• Inappropriate staining of some cells (lymphocytes)<br />
or cell components (nuclei), usually the result of<br />
excessive heat-induced epitope retrieval (HIER).<br />
• Excessive background staining of connective tissue<br />
and lymphocytes.<br />
136<br />
Recommended antigen retrieval system <strong>for</strong><br />
Pan-Cytokeratin<br />
According to data provided by the manufacturers,<br />
both proteolytic enzyme digestion and HIER are suitable<br />
<strong>for</strong> most clones. With proteolytic digestion it is important<br />
to ensure that the digestion time is tailored to the length<br />
of fixation. It is the experience gained from assessment<br />
of slides submitted to this scheme that the use of<br />
enzymes such as freshly prepared 0.1% chymotrypsin in<br />
0.1% calcium chloride (pH adjusted to 7.8) at 37 o C is<br />
very effective <strong>for</strong> pan-cytokeratin staining. Good results<br />
were obtained by participants using both proteolytic<br />
enzyme digestion and HIER (see Table 3).<br />
A significant improvement in per<strong>for</strong>mance<br />
There was a significant improvement in the scoring <strong>for</strong><br />
pan-cytokeratin in this run compared to the last three<br />
runs (Runs 62-64). At this run 73% of participants<br />
achieved a score of >12/20 on the <strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
sections, this compares to only 49% on the previous<br />
one. The main cause of low marks was again the<br />
incomplete staining of the epithelium in both tonsil and<br />
gut, which is clearly demonstrated in Plates 3 and 4.<br />
Participants should be aware that, in order to obtain a<br />
pass mark with pan cytokeratin the full depth of epithelium<br />
must be stained. Scoring on the laboratories own tissue<br />
was again very good as 92% achieved a score of<br />
>12/20. There does not appear to be any obvious reason<br />
<strong>for</strong> the improvement in the scores on the <strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
sections this time except that laboratories may have<br />
taken the advise to adjust their retrieval times to suit the<br />
fixation of the <strong>UK</strong> <strong>NEQAS</strong>-ICC sections. Please note that<br />
participants had marks deducted <strong>for</strong> using non-pan<br />
cytokeratin antibodies such as CAM 5.2 and highmolecular<br />
weight cytokeratins, unless they were used in<br />
conjunction with other cytokeratins as stipulated on the<br />
datasheet.<br />
Notes on cytokeratins and their antibodies<br />
Cytokeratins belong to a group of proteins known as<br />
intermediate filaments that constitute the cytoskeletal<br />
structure in all epithelial cells. It is very important when<br />
making your choice of antibody to choose a marker<br />
which will demonstrate a wide range of cytokeratins<br />
such as the clones AE1/AE3 or MNF116 (the two main<br />
clones used by participants). Both from personal experience<br />
and from published studies (Goddard et al),<br />
AE1/AE3 is a better overall cytokeratin marker than<br />
MNF116 as it is made up of a cocktail of more high and<br />
low molecular weight cytokeratins: AE1 – Cytokeratins<br />
10, 13, 14, 15, 16 & 19; and AE3 – Cytokeratins 1, 2, 3, 4,<br />
5, 6, 7 & 8. In contrast, MNF116 demonstrates<br />
Cytokeratins 5, 6, 8, 17 and probably 19. From the <strong>UK</strong>
<strong>NEQAS</strong>-ICC results the proportion of participants<br />
achieving acceptable staining was the same <strong>for</strong> both<br />
of the main clones.<br />
Thyroglobulin<br />
Main features of optimal results with thyroglobulin<br />
(Plate 5)<br />
• Intense staining of thyroid follicular cells or thyrocytes,<br />
with some staining of the colloid.<br />
Main features of sub-optimal results with thyroglobulin<br />
(Plates 6 & 7)<br />
• Weak staining or no staining of the thyroid follicular<br />
cells or thyrocytes, regardless of the fact that colloid<br />
staining was present in some of these sections.<br />
• Presence of ‘corkscrew’ artifact, probably<br />
caused by over pre-treatment.<br />
Choice of antibody and recommended antigen<br />
retrieval <strong>for</strong> thyroglobulin<br />
Of the two most common thyroglobulin antibodies used<br />
by participants (see Table 2) the polyclonal antibody<br />
with no antigen retrieval gave the best overall staining.<br />
The main monoclonal antibody used scored lower (30%<br />
scored >12/20) than the polyclonal (68% scored >12/20).<br />
A study by De Micco et al suggested that some monoclonal<br />
thyroglobulin clones did not stain as well as the<br />
polyclonal antibodies especially in thyroid tumours.<br />
Notes on thyroglobulin<br />
Thyroglobulin is a large glycoprotein possessing different<br />
molecular <strong>for</strong>ms depending on its metabolic rate i.e.<br />
native, intracellular etc. which is found predominately in<br />
its 660 kD <strong>for</strong>m. Thyroglobulin is synthesied by thyrocytes<br />
and transported to the apical surface where it is secreted<br />
into the lumen of thyroid follicles and stored as a major<br />
Plate 1. Optimal staining of pan-cytokeratin in tonsil (<strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
section). Please note complete depth of epithelium is stained. This<br />
slide scored 20/20.<br />
137<br />
<strong>Immunocytochemistry</strong> — General Pathology<br />
component of colloid. Antibodies to thyroglobulin react<br />
with normal, hyperplastic and neoplastic thyroid tissue<br />
and are most useful <strong>for</strong> the identification of papillary and<br />
follicular thyroid carcinomas. They are also commonly<br />
used to identify metastatic tumours from the thyroid. It<br />
has been reported that the level of staining depends on<br />
the degree of differentiation. Generally more poorly<br />
differentiated tumours contain less thyrogobulin than<br />
well differentiated (DeLellis and Shin). Antibodies to<br />
thyroglobulin do not react with epithelial cells of the<br />
lung, breast, gastrointestinal tract or kidney, nor with the<br />
carcinomas of these organs. It must be noted that<br />
thyroglobulin may diffuse in to other cells in the tissue<br />
including tumour cells of medullary and anaplastic<br />
carcinomas (LiVolsi) and sinus histiocytes in lymph nodes<br />
producing false positive results (Venkatraman et al).<br />
REFERENCES<br />
1. Wotherspoon AC, Norton AJ, Isaacson PG. Immunoreactive<br />
cytokeratins in plasmacytomas. Histopathology 1989; 14(2): 141-50.<br />
2. Goddard MJ, Wilson B, Grant JW. Comparison of commercially<br />
available cytokeratin antibodies in normal and neoplastic adult<br />
epithelial and non-epithelial tissues. J Clin Pathol 1991; 44: 660-<br />
663<br />
3. De Micco C, et al. Thyroglobulin in Medullary Thyroid Carcinomas.<br />
Human Pathology 1993; 24 (3): 256-262.<br />
4. DeLellis RA & Shin S J. Diagnostic Immunohistochemistry of<br />
Endocrine Tumours. In Diagnostic Immunohistochemistry. Dabbs D.<br />
(ed). Churchill Livingstone, Philadelphia 2002 ; 215.<br />
5. LiVolsi VA. Surgical Pathology of the Thyroid. Volume 22 in the Series<br />
Major Problems in Pathology. J.L. Bennington (ed). W.B. Saunders<br />
Company, Philadelphia 1990; 392.<br />
6. Venkatraman V, Maxwell P, McCluggage WG. Thyroglobulin<br />
immunoreactivity in lymph node histiocytes: a potential diagnostic<br />
pitfall. J Clin Pathol 2001; 54: 314-316<br />
Plate 2 . Optimal demonstration of pan-cytokeratin in section of<br />
gut (<strong>UK</strong> <strong>NEQAS</strong>-ICC section). Please note that all epithelial cells<br />
are stained to the full depths of the crypts. This slide scored 20/20.
<strong>Immunocytochemistry</strong> — General Pathology<br />
Plate 3. Poor demonstration of pan-cytokeratin in sections of tonsil<br />
(<strong>UK</strong> <strong>NEQAS</strong>-ICC section). Please note that the complete depth of<br />
epithelium is not staining, this should be compared to the optimal<br />
staining in Plate 1. This slide scored 8/20.<br />
Plate 5. Optimal staining of thyroglobulin (<strong>UK</strong> <strong>NEQAS</strong>-ICC section)<br />
as demonstrated by strong staining of the follicular cells and some<br />
staining in the colloid in the normal thyroid. This slide scored 20/20.<br />
Plate 7. ‘Corkscrew’ artifact, commonly seen in a number of the<br />
thyroid sections and probably caused by excessive pre-treatment.<br />
138<br />
Plate 4. Weak demonstration of pan cytokeratin in sections of gut<br />
(<strong>UK</strong> <strong>NEQAS</strong>-ICC section). Please note that the complete depth<br />
of epithelium within the crypts is not staining, this should be<br />
compared to the optimal staining in Plate 2. This slide scored 8/20.<br />
Plate 6. Poor demonstration of thyroglobulin (<strong>UK</strong> <strong>NEQAS</strong>-ICC section).<br />
Please note strong staining in the colloid only. It is important to note<br />
that <strong>for</strong> an acceptable score follicular cells should also be stained as<br />
in Plate 5.
frequency of returns<br />
Distribution of scores<br />
139<br />
<strong>Immunocytochemistry</strong> — General Pathology<br />
Fig 1. Run 65A Cytokeratin (<strong>UK</strong> <strong>NEQAS</strong>-ICC sections) Fig 2. Run 65B Cytokeratin (In House sections)<br />
frequency of returns<br />
Run 65A Cytokeratin on <strong>UK</strong> <strong>NEQAS</strong> Sections<br />
Summary<br />
Scores >12/20 287(73%)<br />
Scores 10-12/20 69(17%)<br />
Scores 12/20 148(45%)<br />
Scores 10-12/20 69(21%)<br />
Scores 12/20 381(92%)<br />
Scores 10-12/20 24(6%)<br />
Scores 12/20 165(48%)<br />
Scores 10-12/20 83(24%)<br />
Scores
<strong>Immunocytochemistry</strong> — General Pathology<br />
Pan-Cytokeratin<br />
Participant scored 19/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) and 19/20<br />
(In House slide) using this method.<br />
Method: Ventana iView DAB Kit<br />
Automation: Ventana NexES system<br />
Buffer and pH: Ventana buffer<br />
Blockade Type: Ventana blockade system<br />
Antigen Retrieval: Ventana Protease I <strong>for</strong> 20 minutes<br />
Primary Antibody: DakoCytomation M0821 (Clone MNF116)<br />
dilution 1:75 <strong>for</strong> 30 minutes at 37 o C<br />
Chromogen: Ventana DAB <strong>for</strong> 8 minutes<br />
140<br />
Thyroglobulin<br />
Participant scored 20/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) and 16/20<br />
(In House slide) using this method.<br />
Method: Vector Elite<br />
Automation: LabVision Autostainer<br />
Buffer and pH: PBS<br />
Blockade Type: Hydrogen peroxide and serum blocks<br />
Antigen Retrieval: None<br />
Primary Antibody: DakoCytomation A0251 dilution 1:2000<br />
<strong>for</strong> 40 minutes at room temperature<br />
Chromogen: DakoCytomation K3466 DAB, <strong>for</strong> 10<br />
minutes<br />
MAIN TECHNICAL PARAMETERS EMPLOYED BY PARTICIPANTS IN THE GENERAL PATHOLOGY MODULE<br />
The following tables record the number of participants (N) using each system. The percentage (%) refers to the<br />
proportion of these participants achieving acceptable staining (a score >12/20). For example, 15 participants<br />
used A. Menarini MU071 (clones AE1/AE3) of whom 73% achieved acceptable staining.<br />
Table 1. Primary antibody Cytokeratin markers [CK]<br />
Antibody Details N (%)<br />
A. Menarini MU071UC (clone AE1/AE3) 15 73<br />
Becton Dickinson 349205 (Clone CAM 5..2) 4 25<br />
Boehinger Mannheim 1124 (Clone AE1/AE3) 1 100<br />
Chemicon MAB 3412 (Clone AE1/36+2B11) 2 100<br />
DakoCytomation M0821 (Clone MNF116) 171 79<br />
DakoCytomation M3515 (Clone AE1/AE3) 102 74<br />
DakoCytomation M0630 HMWCK (Clone 34BE12) 1 100<br />
Home made cocktails 6 67<br />
Immunotech 1918 (Clone KL1) 7 43<br />
Incomplete data 21 81<br />
Novocastra NCL-PAN CK 16 69<br />
Other 12 50<br />
Ventana 250 2595 AE1/AE3 15 73<br />
Zymed 08 1132 (Clone AE1/AE3) 11 64<br />
Table 2. Primary antibody Thyroglobulin<br />
Antibody Details N (%)<br />
Biogenex MU032 UC 4 0<br />
Biomedia 9833 Polyclonal 1 100<br />
Binding Site PH 068 1 100<br />
CMA 113 (Clone 2H11/6E1) 2 50<br />
DakoCytomation M0781 (Clone DAK IG6 ) 119 30<br />
DakoCytomation A0251 139 68<br />
DakoCytomation N1565 3 33<br />
Novocastra NCL-THY 22 91<br />
Neomarkers MS 206 Polyclonal 2 100<br />
ID Labs BP 54p 1 0<br />
Incomplete data 17 41<br />
Immunon 492020 2 100<br />
Other 4 50<br />
Ventana 250-2740 and 760-2671(Clone 2H11/6E1) 6 0<br />
Zymed 18-0134 (Clone 2H11/6E1) 4 0
Table 3. Pre-treatment<br />
Pan-Cytokeratins Thyroglobulin<br />
Pre-treatment N % N %<br />
Biogenex Protease XXIV EK002 5K 22 68 1 0<br />
Biogenex Protease HK056-5K 1 0 1 0<br />
Becton Dickinson Trypsin 215240 1 0 - -<br />
DakoCytomation Pronase 52013 4 50 - -<br />
DakoCytomation Protease K 53020 16 81 1 0<br />
DakoCytomation K2375 5 80 1 0<br />
Difco Trypsin 215230 18 89 8 12<br />
Enzyme digestion + HMAR 17 76 1 0<br />
ICN 150213 Trypsin 20 90 3 0<br />
Incomplete data 9 78 7 14<br />
Microwave Oven (MW) 62 60 56 23<br />
None 2 50 180 67<br />
Other 17 59 1 100<br />
PC in MW 23 87 13 8<br />
Pressure Cooker (PC) 66 82 32 22<br />
Sigma Pepsin P7000 1 0 - -<br />
Sigma C4129 Chymotrypsin 16 88 1 0<br />
Sigma P8038 Protease 8 100 2 0<br />
Sigma T7409 Trypsin 1 0 2 0<br />
Sigma T8128 Trypsin 1 0 - -<br />
Sigma P5147 Protease 7 43 - -<br />
Water bath 95-98oC 13 38 8 25<br />
Ventana Benchmark 9 44 6 16<br />
Ventana Protease 1 45 82 2 0<br />
Table 5. Detection system<br />
Pan-Cytokeratins Thyroglobulin<br />
Type, supplier & product code N (%) N (%)<br />
Biogenex Super Sensitive Multi link/<br />
HRP LP000-UL<br />
12 75 8 50<br />
Biogenex HK 330 9K 1 100 1 0<br />
Biogenex HK 519-06K HRP 1 100 1 0<br />
Biocarta BCA HP 504 US 1 100 - -<br />
Chemicom HP1000 2 100 2 50<br />
DakoCytomation ChemMate K5005 1 0 1 100<br />
DakoCytomation ChemMate K5001 78 72 61 61<br />
Dakocytomation ChemMate<br />
Envision K5007 DAB<br />
54 81 45 56<br />
DakoCytomation Duet St.ABC K0492 7 71 7 28<br />
DakoCytomation Envision Plus systems 27 70 26 50<br />
DakoCytomation K0690 3 33 2 0<br />
DakoCytomation LSAB Kit/HRP K0675 12 33 8 25<br />
DakoCytomation St.ABC/HRP K0377 2 100 2 50<br />
LabVision TS 125 14 64 13 62<br />
Incomplete data 17 59 13 46<br />
Other 15 60 9 44<br />
Power Vision DPVB 999 HRP 1 100 1 100<br />
Vector 7000 series 18 83 18 39<br />
Vector Elite ABC PK 6102 1 100 1 100<br />
Vector Elite ABC PK 6100 9 67 7 14<br />
Vector Elite Universal ABC PK6200 29 90 25 56<br />
Ventana basic system 13 92 12 0<br />
Ventana iVIEW system 60 73 49 29<br />
VisionBiosystem D59404 2 100 2 50<br />
Zymed 87 8143 2 0 2 0<br />
Zymed 85 9043 2 50 2 0<br />
141<br />
<strong>Immunocytochemistry</strong> — General Pathology<br />
Table 4. Chromogen<br />
Pan-Cytokeratins Thyroglobulin<br />
Chromogen & Supplier N (%) N (%)<br />
Biogenex HK-153-5K DAB 19 84 14 36<br />
DakoCytomation Envision Plus kits 20 80 19 58<br />
DakoCytomation K3466 DAB 18 83 15 47<br />
DakoCytomation K3468 DAB 37 54 32 44<br />
DakoCytomation ChemMate<br />
K5001 DAB<br />
77 73 61 62<br />
Dakocytomation ChemMate<br />
K5005 Alk phos<br />
1 0 1 100<br />
Dakocytomation S3000 DAB 3 100 3 100<br />
Dakocytomation ChemMate<br />
Envision K5007 DAB<br />
52 81 44 52<br />
Incomplete data 24 67 19 26<br />
KEM-EN-TEC 4170 DAB 6 83 5 40<br />
LabVision TA 125 HD 9 44 9 44<br />
Other 17 65 10 30<br />
Sigma D5635 DAB 1 100 1 100<br />
Sigma D5637 DAB 7 71 7 100<br />
Sigma D5905 DAB 4 100 4 50<br />
VisionBiosystem Bond x DAB 2 100 2 50<br />
Vector SK4100 DAB 8 63 6 17<br />
Ventana iVIEW DAB 68 79 56 23<br />
Zymed 87 8143 6 50 6 17<br />
Table 6. Automation<br />
Pan-Cytokeratins Thyroglobulin<br />
Instrument & Supplier N (%) N (%)<br />
Biogenex Optimax 23 78 22 36<br />
Biogenex Genon MX 6000i 13 100 10 60<br />
DakoCytomation Autostainer 78 72 71 55<br />
DakoCytomation TechMate 500 33 73 24 58<br />
DakoCytomation TechMate Horizon 6 50 4 75<br />
Incomplete data 4 75 3 33<br />
Leica Histostainer 1 100 - -<br />
LabVision Autostainer 30 77 28 50<br />
None 100 67 78 46<br />
Shandon Cadenza 1 100 1 0<br />
Shandon Sequenza 24 71 17 53<br />
Ventana ES 4 75 4 25<br />
Ventana Benchmark 27 70 21 19<br />
Ventana Gen 11 2 50 2 0<br />
Ventana NexES 36 86 31 26
<strong>Immunocytochemistry</strong> — Breast Hormonal Receptor<br />
The Breast Hormonal Receptor Module<br />
Keith Miller & Merdol Ibrahim<br />
Antigens assessed: Oestrogen receptors (ER).<br />
Tissue sections circulated: Sections from a composite<br />
block comprising three infiltrating ductal carcinomas<br />
(IDC’s) with differing levels of receptor expression (see<br />
Table below).<br />
IHC Staining characteristics of invasive tumour nuclei*<br />
Tumour Approx. % Main Intensity<br />
(A). IDC 90-95 High (see Plate 8)<br />
(B). IDC 50-75 Medium – High (see Plate 9)<br />
(C). IDC 0 Negative (see Plate 10)<br />
* Refers to the staining characteristics observed when the<br />
tumours were immunostained by the organising laboratory<br />
using the Novocastra 6F11 clone.<br />
Instructions at Assessment:<br />
Participants were requested to demonstrate ER on<br />
the slides provided.<br />
Number of participating laboratories: 343<br />
Assessment of staining of In House tumours:<br />
Participants were also requested to stain their own In<br />
House control with ER and submit at least 2 unstained<br />
sections from the same tissue block, thus allowing the<br />
organising laboratory to stain the same case. The subsequent<br />
comparison of the staining achieved by the<br />
participant and organising laboratories on the In House<br />
sections, allowed <strong>for</strong> a more accurate assessment of<br />
the staining quality present.<br />
Introduction<br />
Oestrogen and progesterone receptors are localised in<br />
nuclei of epithelial cells. Nuclei of approximately 7% of<br />
these cells are immunoreactive to current day oestrogen<br />
receptor antibodies in normal resting breast tissue,<br />
with a higher proportion in lobular than in ductal cells<br />
(Petersen et al). When breast carcinoma arises<br />
demonstrating the presence of oestrogen receptors in<br />
the malignant cells, as we all know, is very important as<br />
they provide a target <strong>for</strong> certain therapies, such as<br />
Tamoxifen and, more recently, Anastrazole (Thurlimann<br />
et al). Nearly 66% of breast cancers from premenopausal<br />
women and 75% from post-menopausal<br />
women contain immuno-detectable oestrogen receptors<br />
(Mayor). If however, a particular case is negative, the<br />
inclusion of positive normal glands is important as they<br />
can often give an indication as to reliability of the<br />
immunostain per<strong>for</strong>med on the slide.<br />
142<br />
Guidelines used in the evaluation of oestrogen and<br />
progesterone receptor assays: Four assessors marked the<br />
slides independently; each awarding scores from 1 to 5<br />
using the guidelines shown. The 4 individual scores <strong>for</strong><br />
each slide were added together to give a mark out of 20.<br />
Those sections showing the expected standard of<br />
immunostaining achieved marks in the 13/20 – 20/20 range.<br />
SCORE STAINING PATTERN<br />
0 No slides returned.<br />
1 & 2 Staining of considerably less nuclei than expected<br />
in either, or both of the two positive tumours.<br />
3 Staining of 10% or greater of tumour nuclei in each<br />
of the two positive tumours, though substantially<br />
less than expected to stain, or staining is weaker<br />
than expected.<br />
4 & 5 Demonstration of the proportion of nuclei of<br />
invasive tumours expected to stain, with roughly<br />
the expected staining intensity.<br />
NB. These are only general guidelines and marks were deducted<br />
<strong>for</strong> excessive cytoplasmic staining, excessive background staining,<br />
diffuse nuclear staining, excessive counter-stain, uneven staining<br />
or other factors that made interpretation difficult.<br />
The four individual scores <strong>for</strong> each slide were added<br />
together to give a mark out of 20.<br />
Distribution of scores<br />
frequency of returns<br />
Run 65E Oestrogen Receptors on <strong>UK</strong> <strong>NEQAS</strong> Sections<br />
Summary<br />
Scores >12/20 116 (36%)<br />
Scores 10-12/20 77 (23%)<br />
Scores 12/20 253(78%)<br />
Scores 10-12/20 53(17%)<br />
Scores
Features of optimal immunostaining (See Plates 8, 9 and<br />
10)<br />
• Staining of the expected proportion of invasive<br />
tumour nuclei with the anticipated staining intensity<br />
(see Plates 11, 12, and 13)<br />
• Intense nuclear staining of the appropriate distribution<br />
in normal glands<br />
• Cytoplasmic staining not excessive<br />
• No background staining of connective tissues or<br />
inappropriate localised staining<br />
Features of sub-optimal results (see Plates 11, 12, 13, 14<br />
and 15)<br />
• Relatively weak nuclear staining of the receptor<br />
positive tumours<br />
• Excessive cytoplasmic staining<br />
• Excessive background staining of connective tissue<br />
elements<br />
• Inappropriate staining of some cells e.g. lymphocytes,<br />
fibroblasts<br />
The importance of good fixation!<br />
One of the most important factors often ignored when<br />
dealing with breast tissue, because of pressure from<br />
those looking after the patients, is good fixation. It cannot<br />
be stressed enough that good fixation is vital to preserve<br />
ER protein. Also, good fixation is required to preserve the<br />
degree of morphological detail needed to diagnose<br />
borderline lesions. Small specimens may be fixed whole<br />
but larger ones really need to be examined and<br />
sliced within a few hours of excision to allow optimum<br />
penetration of fixative. One of the added benefits of<br />
well-processed breast tissue is that sectioning is easier<br />
and retention of section on the slides is better, the latter<br />
is especially significant when employing aggressive<br />
heat retrieval methods.<br />
Antigen retrieval<br />
Participants achieving poor results <strong>for</strong> hormonal receptors<br />
should note that inefficient antigen retrieval is frequently<br />
the main factor responsible <strong>for</strong> weak staining and<br />
attention to this has on previous occasions resulted in<br />
significant improvement (Rhodes et al).<br />
<strong>Immunocytochemistry</strong> — Breast Hormonal Receptor<br />
143<br />
Per<strong>for</strong>mance and sections supplied by <strong>UK</strong> <strong>NEQAS</strong>-ICC.<br />
The per<strong>for</strong>mance on <strong>UK</strong> <strong>NEQAS</strong>-ICC sections on this<br />
occasion was very disappointing. Only 36% of participants<br />
achieved a score of more than 12/20. This again is most<br />
likely due to the extended fixation of the tissue. This once<br />
again indicates that there appears to be a problem with<br />
the tissue being fixed <strong>for</strong> longer than necessary.<br />
However, the extended fixation is making more and<br />
more laboratories review their retrieval protocols and this<br />
may provide some benefit when staining their local<br />
cases. The extended fixation has also enabled the<br />
identification of the more efficient retrieval systems.<br />
Participants employing pressure-cooking retrieval<br />
together with citrate buffer at pH6.0 are, <strong>for</strong> the most<br />
part achieving the desired results.<br />
For those concerned with poor per<strong>for</strong>mance please be<br />
assured that per<strong>for</strong>mance on In House sections, which<br />
was very good indeed with 78% scoring more than<br />
12/20, will be taken into account.<br />
REFERENCES<br />
1. Petersen OW, Hoyer PE, van Duers B. Frequency and distribution<br />
of estrogen receptor-positive cells in normal, non-lactating<br />
human breast tissue. Cancer Res 1987; 47: 5748-5751<br />
2. Thurlimann B, Hess D, Koberle D, et al. Anastrozole ('Arimidex')<br />
versus tamoxifen as first-line therapy in postmenopausal<br />
women with advanced breast cancer: results of the doubleblind<br />
cross-over SAKK trial 21/95 — a sub-study of the TARGET<br />
(Tamoxifen or 'Arimidex' Randomized Group Efficacy and<br />
Tolerability) trial. Breast Cancer Res Treat 2004; 85(3): 247-54.<br />
3. Mayor S. News Roundup: <strong>UK</strong> survey finds variation in<br />
oestrogen receptor testing. BMJ 2001; 323: 713<br />
4. Rhodes A, Jasani B, Balaton A, et al. Study of interlaboratory<br />
reliability and reproducibility of estrogen and progesterone<br />
receptor assays in Europe: documentation of poor reliability<br />
and identification of insufficient microwave antigen retrieval<br />
time as a major contributory element of unreliable assays.<br />
Am J Clin Pathol 2001; 115: 44-58
<strong>Immunocytochemistry</strong> — Breast Hormonal Receptor<br />
Plate 8. <strong>UK</strong> <strong>NEQAS</strong>-ICC high expressor section (Section A) optimally<br />
stained. The smaller figure shows an enlarged section from the<br />
main image showing a clean crisp staining of tumour nuclei.<br />
Plate 10. <strong>UK</strong> <strong>NEQAS</strong>-ICC non-expressor section (Section C) optimally<br />
stained. The smaller magnified image shows an example of strong<br />
positivity in the normal glands.<br />
Plate 12. <strong>UK</strong> <strong>NEQAS</strong>-ICC medium - high expressor section (Section<br />
B) sub-optimally stained. The tumour nuclei are virtually negative.<br />
The excess counterstain further masks any ER positivity which may<br />
be present.<br />
144<br />
Plate 9. <strong>UK</strong> <strong>NEQAS</strong>-ICC medium – high expressor section<br />
(Section B) optimally stained. The smaller figure shows closer<br />
detail of antibody localisation.<br />
Plate 11. <strong>UK</strong> <strong>NEQAS</strong>-ICC high expressor section (Section A)<br />
sub-optimally stained. Very poor demonstration of tumour nuclei<br />
with the tumour remaining largely unstained.<br />
Plate 13. In House section. Staining result produced by the<br />
participant indicates low expression of ER.
Plate 14. Section from same In House case as shown in Plate 13.<br />
Staining by the <strong>UK</strong> <strong>NEQAS</strong>-ICC reference laboratory shows staining<br />
in a greater proportion of nuclei, and with a greater intensity than<br />
that produced by the participant.<br />
Plate 16. Section from same In House case as shown in Plate 15.<br />
Staining by the <strong>UK</strong> <strong>NEQAS</strong>-ICC reference laboratory shows that this<br />
tumour is in fact ER positive, a result which the participant has missed<br />
altogether.<br />
BEST METHODS<br />
Oestrogen Receptor<br />
Participant scored 20/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) and<br />
18/20 (In House slide) using this method.<br />
Method: DakoCytomation ChemMate K5001<br />
Automation: None<br />
Buffer and pH: DakoCytomation ChemMate K5001<br />
buffer<br />
Blockade Type: DakoCytomation ChemMate K5001<br />
blocking solution<br />
Antigen Retrieval: Tefal pressure cooker to heat 1600 ml of<br />
Vector unmasking solution pH 6.0, <strong>for</strong><br />
2.5 minutes at full pressure<br />
Primary Antibody: LabVision RM-9101-S dilution 1:100 <strong>for</strong><br />
60 minutes at room temperature<br />
Chromogen: DakoCytomation ChemMate K5001<br />
DAB <strong>for</strong> 5 minutes<br />
<strong>Immunocytochemistry</strong> — Breast Hormonal Receptor<br />
145<br />
Plate 15. In House section. Staining result produced by the participant<br />
indicates that this tumour was negative <strong>for</strong> ER expression.<br />
Oestrogen Receptor<br />
Participant Scored 19/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) and<br />
20/20 (In House slide) using this method.<br />
Method: Neomarkers Ultravision LP TL-012 HDN<br />
Automation: DakoCytomation Autostainer<br />
Buffer and pH: Tris buffered saline pH7.6<br />
Blockade Type: Hydrogen peroxide blockade, serum<br />
Antigen Retrieval: Dakocytomation Water bath GIR109<br />
using 250 ml of citrate buffer pH 6.0 <strong>for</strong> 40<br />
minutes at 98 o C<br />
Primary Antibody: Neomarkers RM-9101-S dilution 1:80 <strong>for</strong><br />
30 minutes at room temperature<br />
Chromogen: DakoCytomation K3468 DAB <strong>for</strong> 5<br />
minutes
<strong>Immunocytochemistry</strong> — Breast Hormonal Receptor<br />
MAIN TECHNICAL PARAMETERS EMPLOYED BY PARTICIPANTS IN THE BREAST PATHOLOGY<br />
HORMONAL RECEPTOR MODULE<br />
The following tables record the number of participants (N) using each system. The percentage (%) refers to the proportion of these<br />
participants achieving acceptable staining (a score >12/20). For example, in the first table 2 participants used A.Menarini MU 272<br />
antibody (clone 1D5) neither of whom achieved acceptable staining.<br />
Table 7. Primary Antibody Oestrogen receptors (ER)<br />
Antibody details N %<br />
A.Menarini MU 272 (Clone 1D5) 2 0<br />
Biocarta CM 093C (Clone 6F11) 1 0<br />
DakoCytomation M7047 ER (clone 1D5) 101 23<br />
Immunotech 1545 (Clone ID5) 1 100<br />
Incomplete data 5 0<br />
LabVision RM 9101-S (Clone SP1) 30 67<br />
Novocastra NCL-ER 6F11 ER (Clone 6F11) 131 42<br />
Other 1 0<br />
Ventana 250-2596 ER (Clone 6F11) 25 40<br />
Zymed 08 1149 (Clone 1D5) 3 33<br />
Table 9. Detection System<br />
Type, Supplier & Product Code N (%)<br />
Biogenex LP000-UL 11 45<br />
Biogenex HK 330 9K 1 0<br />
Chemicom HP 1000 2 50<br />
DakoCytomation ChemMate L.St.Av/HRP K5001 58 38<br />
DakoCytomation ChemMate Envision K5007 DAB 46 35<br />
DakoCytomation Duet St.ABC K0492 7 43<br />
DakoCytomation Envision 14 21<br />
DakoCytomation LSAB Kit/HRP K0675 7 0<br />
DakoCytomation St.ABC/HRP K0377 3 33<br />
Incomplete data 15 26<br />
Others 9 33<br />
LabVision TS 125 HR 13 23<br />
Vector Elite ABC PK6100 7 57<br />
Vector Elite Universal ABC PK6200 23 43<br />
Vector Elite ABC PK7200 14 57<br />
Ventana iView System 51 39<br />
Ventana System 250-2001 8 63<br />
Vision Biosystems D59404 2 0<br />
Zymed 87 8143 1 100<br />
Table 11. Automation<br />
Instrument & Supplier N (%)<br />
Biogenex Optimax 20 20<br />
Biogenex GENON MX i6000 13 38<br />
DakoCytomation Techmate 500 26 46<br />
DakoCytomation Techmate Horizon 4 25<br />
DakoCytomation Autostainer 62 39<br />
Incomplete data 2 50<br />
LabVision Autostainer 23 39<br />
None 72 35<br />
Shandon Sequenza 17 35<br />
Shandon Cadenza 2 0<br />
Ventana Benchmark 23 35<br />
Ventana ES 3 100<br />
Ventana NexES 28 43<br />
Ventana GEN 11 2 0<br />
Vision Biosystems Bond X 3 0<br />
146<br />
Table 8. Pre-treatment<br />
Pre-treatment N (%)<br />
Incomplete data 6 33<br />
Microwave Oven 80 25<br />
Other 1 0<br />
PC inside MW oven 46 48<br />
Pressure Cooker 129 44<br />
Water bath 95-98oC 14 14<br />
Ventana benchmark 24 29<br />
Table 10. Chromogen<br />
Chromogen & Supplier N (%)<br />
Biogenex HK-153-5K DAB 16 38<br />
DakoCytomation K3466 DAB 10 40<br />
DakoCytomation K3468 DAB 31 35<br />
DakoCytomation K5001 DAB 58 38<br />
DakoCytomation K5005 Alk Phos 1 0<br />
DakoCytomation S3000 DAB 1 100<br />
DakoCytomation K5007 DAB 43 37<br />
DakoCytomation Envision 7 43<br />
KEM-EN-TEC -4170 DAB 7 43<br />
Other 12 8<br />
Incomplete data 24 21<br />
LabVision TS 125 HR 8 25<br />
Sigma D5637 DAB 6 33<br />
Sigma D5905 DAB 5 40<br />
Vector SK4100 DAB 5 60<br />
Ventana DAB 55 44<br />
Vision Biosystems DAB 2 0<br />
Zymed kits DAB 4 25
The Breast HER-2 Module<br />
Keith Miller & Merdol Ibrahim<br />
Antigens assessed: HER-2<br />
Number of participating laboratories: 161<br />
Sections circulated: Formalin fixed and paraffin processed<br />
sections from a composite block comprising human breast carcinoma<br />
cell lines; MDA-MB-453, BT-20, MCF-7 and the ovarian<br />
carcinoma cell line SKOV-3. In a previous study, FISH analysis on<br />
these cell lines showed the SKOV-3 and MDA-MB-453 cell lines to<br />
have HER-2/neu gene amplification, whilst the cell lines BT-20<br />
and MCF-7 did not (Rhodes A, et al Ref 1). Briefly, the ratio of<br />
HER-2/neu to chromosome 17 signals were 4.2 and 3 <strong>for</strong> the<br />
SKOV-3 and MDA-MB-453 cell lines and 0.9 and 1.0 <strong>for</strong> the BT-20<br />
and MCF-7 cell lines, respectively. The sections were positioned<br />
on the microscope slide as indicated in Figure 7.<br />
Fig. 7. Position of cell lines on the microscope slide and the most appropriate scores.<br />
E<br />
Run 64E<br />
(A)<br />
SKOV-3 (3+)<br />
(B)<br />
MDA-MB-453 (2+)<br />
(C)<br />
BT-20 (0 or 1+)<br />
(D)<br />
MCF-7 (0)<br />
Assessment of slides: The immunohistochemical results were<br />
evaluated by <strong>UK</strong> <strong>NEQAS</strong>-ICC assessors scoring independently<br />
using the method of evaluation initially devised <strong>for</strong> the Clinical<br />
Trials Assay. The scoring was as follows:<br />
SCORE STAINING PATTERN<br />
0 No staining at all or very slight partial membrane<br />
staining in less than 10% of tumour cells.<br />
1+ Faint barely perceptible membrane staining in more<br />
than 10% of tumour cells; the cells are only stained in<br />
part of their membrane.<br />
2+ Weak to moderate complete membrane staining<br />
observed in more than 10% of tumour cells.<br />
3+ Strong complete membrane staining in more than 10%<br />
of tumour cells.<br />
Features of optimal immunostaining (see Plates 17,<br />
18 and 19)<br />
• Staining of the expected proportion of membranes<br />
in the given cell lines as set up in the assessment<br />
guidelines above<br />
• Cytoplasmic staining is not excessive.<br />
• Counterstain is not excessive<br />
Features of sub-optimal immunostaining (see Plates 20,<br />
21 and 22)<br />
• Damaged cell morphology<br />
• Excessive cytoplasmic staining making membrane<br />
staining difficult to interpret<br />
• Excessive counterstain masking immunostaining of<br />
membrane<br />
147<br />
<strong>Immunocytochemistry</strong> — Breast HER-2<br />
Staining of the MDA-MB-453 cell line<br />
Previous analysis by FISH showed the cell lines SKOV-3<br />
and MDA-MB-453 to have HER-2 gene amplification,<br />
whilst the cell lines BT-20 and MDA-MB-453 did not<br />
(Rhodes A, et al Ref 2). When testing these cell lines and<br />
reviewing the results of over 90 laboratories from last<br />
year, it became apparent that the MDA-MB-453 could<br />
not be reliably immunostained with greater than 2+<br />
staining intensity, without over-staining the BT-20 and<br />
MCF-7 cell lines i.e. these cell lines typically stain 2+ and<br />
1+ respectively, if 3+ staining occurs on the MDA-MB-453<br />
cell line. Consequently, 2+ staining is the most appropriate<br />
result <strong>for</strong> this cell line. This was considered by the<br />
assessment panel to be the ‘safest’ level of sensitivity to<br />
achieve on the MDA-MB-453 cell line, providing that<br />
guidelines are followed which recommend that all 2+<br />
staining on tumours should be regarded as an equivocal<br />
result which require further analysis by FISH (Ellis IO, et al).<br />
An assay sensitivity level that equates to 1+ staining on<br />
the MDA-MB-453 cell line might have better correlation<br />
with FISH results, as many 2+ tumours have been shown<br />
by FISH not to have HER-2 gene amplification (Tubbs RR,<br />
et al). However, by staining this cell line and tumours with<br />
similar amounts of HER-2 expression as 2+ it ensures that<br />
these tumours are further analysed by FISH to identify<br />
those having HER-2 gene amplification and those having<br />
no amplification. This should there<strong>for</strong>e in turn ensure that<br />
patients with 2+ tumours with gene amplification and<br />
patients with 2+ tumours without gene amplification both<br />
receive appropriate therapy.<br />
Choice of antibody and methodology<br />
Once again, as in previous assessments the<br />
DakoCytomation HercepTest kit seems to out per<strong>for</strong>m<br />
most other methods according to the data (see Tables<br />
12 and 14).<br />
However, reports continue to suggest that the<br />
DakoCytomation HercepTest kits vary slightly from<br />
batch to batch with regard to the 1+ staining, and this<br />
was again confirmed at assessment. Nevertheless, the<br />
evidence still points to the HercepTest kit being the most<br />
reliable if immunocytochemistry is the method of choice<br />
<strong>for</strong> determining levels of HER-2 protein expression.<br />
AN IMPORTANT NOTE REGARDING ANTIGEN<br />
RETRIEVAL: Those intending to persevere with their<br />
own in house methods should note the data on<br />
retrieval methods in Table 13. The data on this<br />
occasion are overwhelmingly in favour of water-bath<br />
retrieval, those using the water bath methodology<br />
are significantly more successful than those using<br />
alternative retrieval methods. 10mM citrate buffer<br />
at pH6.0 would appear to be the solution of choice<br />
when retrieving using the water-bath.
<strong>Immunocytochemistry</strong> — Breast HER-2<br />
Poor per<strong>for</strong>mance concerns<br />
The data shown in the Tables indicate that many<br />
laboratories are attempting to use their own specially<br />
devised In House methods <strong>for</strong> HER-2 testing without<br />
success. EQA is only a small snapshot of per<strong>for</strong>mance<br />
and may not always give a true reflection of the quality<br />
of immunocytochemistry being produced by a particular<br />
laboratory. With this in mind and the per<strong>for</strong>mance<br />
issues this assessment run raises, it is recommend that<br />
those laboratories who are struggling to per<strong>for</strong>m to the<br />
standard set by the <strong>UK</strong> <strong>NEQAS</strong>-ICC assessors review<br />
their HER-2 testing. Auditing of results will in most cases<br />
reveal that 25-30% of breast cancer cases should exhibit<br />
over-expression of the HER-2 protein (3+). According to<br />
Nichols et al this should correlate well with HER-2 gene<br />
amplification. If a particular laboratory finds that their<br />
results do not meet these criteria then it is recommended<br />
that some cases be sent to a recognised specialist centre<br />
so that a valid correlation can be made. For those who<br />
are unsure of the type of immunostaining required,<br />
please refer to the images given in this report. As far as In<br />
House staining was concerned, a number of laboratories<br />
Plate 17. Good demonstration of 3+ staining of the <strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
SKOV-3 cell line<br />
Plate 19. Expected faint and/or incomplete membrane (1+) staining<br />
of the <strong>UK</strong> <strong>NEQAS</strong>-ICC BT-20 cell line<br />
148<br />
are submitting samples where the normal glands are<br />
stained. It is recommended that if this occurs, that the<br />
test should either be repeated using a validated<br />
method or, if appropriate, perhaps FISH testing <strong>for</strong> gene<br />
amplification should be considered.<br />
REFERENCES<br />
1. Rhodes A, Jasani B, Couturier J, et al. A <strong>for</strong>malin fixed, paraffin processed cell<br />
line standard <strong>for</strong> quality control of immunohistochemical assay of HER-2neu<br />
expression in breast cancer. Am J Clin Pathol. 2002; 117: 81–89.<br />
2. Ellis IO, Dowsett M, Bartlett J, et al. Recommendations <strong>for</strong> HER2 testing in<br />
the <strong>UK</strong>. J Clin Pathol 2000; 53: 890–892.<br />
3. Tubbs RR, Pettay JD, Roche PC, et al. Discrepancies in clinical laboratory<br />
testing of eligibility <strong>for</strong> trastuzumab therapy: apparent immunohistochemical<br />
false-positives do not get the message. J Clin Oncol 2001; 19: 2714–272<br />
4. Rhodes A, Jasani B, Anderson E, et al. Evaluation of HER-2/neu immunohistochemical<br />
assay sensitivity and scoring on <strong>for</strong>malin fixed and paraffin<br />
processed cell lines and breast carcinomas: A comparative study involving<br />
results from laboratories in 21 countries. Am J Clin Pathol 2002; 118: 408–417<br />
5. Nichols DW, Wolff DJ, Self S, et al. A testing algorithm <strong>for</strong> determination of<br />
HER2 status in patients with breast cancer. Ann Clin Lab Sci. 2002 Winter;<br />
32 (1): 3-11<br />
Plate 18. Optimal demonstration of 2+ staining of the <strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
MDA-MB-453 cell line<br />
Plate 20. Poor demonstration of staining of the <strong>UK</strong> <strong>NEQAS</strong>-ICC SKOV-3<br />
cell line (expected to be 3+). Morphology of cells is disrupted and<br />
membrane localisation of immunostain is poor
Plate 21. Poor demonstration of staining of the <strong>UK</strong> <strong>NEQAS</strong>-ICC MDA-<br />
MB-453 cell line (expected to be 2+). Membrane localisation of<br />
immunostain is poor and haematoxylin counterstain is excessive<br />
Plate 23. Good demonstration of 3+ staining in the SK-BR-3 cell line<br />
from a DakoCytomation control slide<br />
Plate 25. Good demonstration of 1+ staining in the MDA-175 cell<br />
line from a DakoCytomation control slide<br />
149<br />
<strong>Immunocytochemistry</strong> — Breast HER-2<br />
Plate 22. Excessive haematoxylin staining masks any membrane<br />
staining which may be present in the <strong>UK</strong> <strong>NEQAS</strong>-ICC BT-20 (1+) cell<br />
line<br />
Plate 24. SK-BR-3 (3+) cell line from a DakoCytomation control<br />
slide, showing excessive cytoplasmic staining rendering the cell<br />
membranes difficult to interpret<br />
Plate 26. Excessive cytoplasmic staining in the DakoCytomation<br />
MDA-175 (1+) cell line
<strong>Immunocytochemistry</strong> — Breast HER-2<br />
BEST METHODS Both the DakoCytomation HercepTest and Ventana Pathway system are recognised methods of choice to<br />
demonstrate the Her 2 receptor. Those intending to employ these systems should contact the relevant companies <strong>for</strong> the exact<br />
protocol <strong>for</strong> each of the above methods.<br />
The following method was obtained from a participant who achieved the appropriate result on <strong>UK</strong> <strong>NEQAS</strong>-ICC material<br />
without using one of the above-recognised methods. However, it should be borne in mind that although some laboratories<br />
have been successful using microwave and pressure cooker retrieval methods <strong>for</strong> HER-2 immunostaining, <strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
data shows that water-bath retrieval is more reliable.<br />
Her-2<br />
Method: DakoCytomation Labelled St.Av K0675 system<br />
Automation: A. Menarini Optimax plus<br />
Buffer and pH: Optimax buffer<br />
Blockade Type: None stated<br />
Antigen Retrieval: Pressure cooker to heat 2L of 10mM<br />
citrate buffer ph6.0, <strong>for</strong> 5.5 minutes at<br />
full pressure<br />
Primary Antibody: DakoCytomation A0485 polyclonal<br />
dilution 1:1000 <strong>for</strong> 60 minutes<br />
Chromogen: DakoCytomation K3468 <strong>for</strong> 10 minutes<br />
MAIN TECHNICAL PARAMETERS EMPLOYED BY PARTICIPANTS IN THE HER-2 MODULE<br />
The following tables record the number of participants (N) using each system. The percentage (%) refers to the<br />
proportion of these participants achieving appropriate staining. For example, in the first table 50 participants used<br />
DakoCytomation Hercep Test Kit K5204 of whom 56% achieved acceptable staining.<br />
Table 12. Primary antibody (HER-2)<br />
Antibody details N %<br />
A.Menarini MU 1344 UC (Clone CB11) 1 0<br />
Cell Marque CMA 601 (Clone CB11) 1 0<br />
DakoCytomation HerCep Kit K5204 50 56<br />
DakoCytomation HerCep Kit K5205 13 62<br />
DakoCytomation HerCep Kit K5206 9 67<br />
DakoCytomation A0485 c-erbB2 (Polyclonal) 32 19<br />
Neomarkers MS 730 1 0<br />
Novocastra NCL-CB11 (clone CB11) 11 27<br />
Incomplete data 4 25<br />
Immunotech 1591 (clone 3B5) 1 0<br />
Oncogene OP15 (clone 3B5) 1 0<br />
Ventana 760 2694 CB11 (Pathway) 7 14<br />
Zymed 28 003 or 18-107 7 0<br />
Table 14. Detection System<br />
Type, Supplier & Product Code N (%)<br />
Biogenex Super Sentitive Multi link/HRP LP000-UL 3 0<br />
DakoCytomation Hercep test K5204 49 57<br />
DakoCytomation Hercep test K5205 13 62<br />
DakoCytomation Hercep test K5206 9 67<br />
DakoCytomation ChemMate L.St.Av/HRP K5001 10 10<br />
DakoCytomation Duet St.ABC K0492 1 0<br />
DakoCytomation Envision Plus 9 44<br />
DakoCytomation ChemMate Envision K5007 5 40<br />
DakoCytomation LSAB Kit/HRP K0675 3 33<br />
DakoCytomation K5005 1 0<br />
Incomplete data 3 0<br />
Lab Vision TA125ML 5 20<br />
Other 1 0<br />
Power Vision DPVB999 HRP 1 0<br />
Vector Elite Universal ABC PK6200 2 0<br />
Vector PK7200 (ready to use) 3 33<br />
Ventana System 19 5<br />
Zymed 87 8143 1 0<br />
150<br />
Table 13. Pre-treatment<br />
Pre-treatment N (%)<br />
Incomplete data 6 0<br />
Microwave Oven 17 18<br />
None 3 33<br />
Pressure cooker 19 21<br />
Pressure cooker inside microwave oven 4 25<br />
Ventana benchmark 9 0<br />
Water bath 95-98 o C <strong>for</strong> 40 minutes - 80 55<br />
and 20 minutes cooling<br />
Table 15. Automation<br />
Instrument & Supplier N (%)<br />
Biogenex Optimax 1 100<br />
Biogenex Genon i6000 4 0<br />
DakoCytomation TechMate 500 10 30<br />
DakoCytomation Autostainer 19 68<br />
DakoCytomation TechMate Horizon 3 33<br />
LabVision Autostainer 19 68<br />
None 72 43<br />
Shandon Sequenza 7 43<br />
Ventana Benchmark 8 0<br />
Ventana ES 3 0<br />
Ventana NexES 6 0
The Lymphoma Module<br />
Tibor Krenacs<br />
Antigens assessed: CD3 & bcl-2<br />
Tissue section circulated: reactive tonsil (CD3 and bcl-2)<br />
Number of participating laboratories: 205 (CD3),<br />
204 (Bcl-2)<br />
CD3<br />
Introduction<br />
The pentameric CD3 molecule is non-covalently<br />
associated with the dimeric T-cell receptor (TCR) and<br />
both are localised in the T-lymphocyte membrane<br />
(Griesser and Mak). CD3 is thought to mediate signal<br />
transduction though the membrane upon TCR activation.<br />
Distribution of scores<br />
frequency of returns<br />
frequency of returns<br />
Run 65L CD3 on <strong>UK</strong> <strong>NEQAS</strong> Sections<br />
Summary<br />
Scores >12/20 143(69%)<br />
Scores 10-12/20 30(15%)<br />
Scores 12/20 130(64%)<br />
Scores 10-12/20 43(21%)<br />
Scores 12/20 168(82%)<br />
Scores 10-12/20 24(12%)<br />
Scores 12/20 151(74%)<br />
Scores 10-12/20 40(20%)<br />
Scores
<strong>Immunocytochemistry</strong> — Lymphoma<br />
Guidelines used in the assessment CD3 reactions<br />
SCORE STAINING PATTERN<br />
0 No returns.<br />
1 Little or no staining of T-cells<br />
2 Very weak demonstration of T-cells with many of those<br />
expected to stain, not demonstrated<br />
3 Weak demonstration of T- cells with fewer stained than<br />
expected<br />
4 Good demonstration of the vast majority of T-cells<br />
expected to stain, with good localisation of CD3 on the<br />
cytoplasmic membrane.<br />
5 Very intense staining of most of the T-cells expected to<br />
stain, with crisp localisation of CD3 on the cytoplasmic<br />
membrane, crisp morphology and no background<br />
staining<br />
NB. These are only very general guidelines and marks were deducted <strong>for</strong><br />
such things as poor localisation of staining or diffuse staining, inappropriate<br />
staining of certain cell types, excessive background staining, excessive<br />
counter-stain, uneven staining or other factors which made interpretation<br />
difficult.<br />
The four individual scores <strong>for</strong> each slide were added<br />
together to give a mark out of 20.<br />
Features of optimal immunostaining (see Plates 27 and 28)<br />
The following features should be seen in a section of<br />
reactive tonsil well stained <strong>for</strong> CD3:<br />
• Crisp cell membrane staining of T lymphocytes in all<br />
expected compartments (see Introduction above)<br />
• Moderate cytoplasmic staining is a normal feature<br />
but is insufficient without the obvious cell membrane<br />
labelling (please consider that the rim of cytoplasm is<br />
usually narrow)<br />
• Extracellular appearance of the antigen should be<br />
minimal or lacking<br />
Features of sub-optimal immunostaining (see Plates 29,<br />
30, 31 and 32)<br />
Most low scoring slides were marked down because they<br />
displayed:<br />
• Weak, uneven, partially missing or incomplete staining<br />
of T lymphocytes.<br />
• Diffuse or extracellular localisation of the antigen.<br />
• High background or non-specific staining.<br />
Please note:<br />
Most of the sub-optimal features criticised above<br />
were most probably due to insufficient HIER (weak,<br />
uneven staining – see Plates 30), the overuse of HIER<br />
(strong staining with soft margins, and possibly tissue<br />
damage – see Plates 29), the inappropriate dilution<br />
of primary antibody under the conditions used<br />
(high background, non-specific staining – see Plate<br />
31 and 32), or the possible combinations of these<br />
factors.<br />
152<br />
The best indicators of staining quality are single positive<br />
T-cells found e.g. in the germinal centre (see Plate<br />
28). Close apposition of extra-follicular T-cells may<br />
hinder the clear definition of their membranes.<br />
Summary of findings at this CD3 Assessment<br />
In tonsil sections provided by <strong>UK</strong> <strong>NEQAS</strong>-ICC the number<br />
of laboratories passing CD3 staining was lower (69% vs.<br />
75%), while the number of failing laboratories was higher<br />
(16% vs. 11%) than those in Run 64. This was most probably<br />
due to a longer duration of <strong>for</strong>malin fixation of the tonsil<br />
tissues used in Run 65 than those used in Run 64. This notion<br />
is supported by the fact that there was no difference<br />
between the results achieved on the In House sections<br />
across the two runs (80% vs. 82% passes, and the same 6%<br />
failures in both runs).<br />
The results of those using the rabbit polyclonal CD3<br />
antibody (DakoCytomation A0452, 73%) still surpass<br />
those using monoclonal CD3 antibodies (NovoCastra<br />
NCL-CD3-PS1, 66% pass; DakoCytomation M7452, 65 %<br />
pass rate) (see Table 16).<br />
Heat pre-treatment using a pressure cooker either metal or<br />
a microwavable plastic one allowed the highest passing<br />
rates (76 and 78% respectively) (see Table 18). The rank of<br />
detection systems based on the passing rates achieved<br />
by laboratories were ChemMate-PO (Dakocytomation,<br />
86%); Vector Elite Universal (Vector, 86%); EnVision<br />
(DakoCytomation, 80%); and ChemMate Envision<br />
(DakoCytomation, 78%) (see Table 19). Using standardised<br />
DAB chromogen kits (K5001; EnVision DAB; K3466; and<br />
K5007; all from DakoCytomation) allowed higher (80% or<br />
above) pass rates than the home-prepared versions of<br />
developers (see Table 20). Some automated immunostainers<br />
produced clearly better results than manual<br />
immunostaining, allowing 86% (A. Menarini Optimax,<br />
DakoCytomation Autostainer), 81% (DakoCytomation<br />
TechMate 500), 72% (Ventana NexES) and 69 % (Ventana<br />
Benchmark) passing rates versus the 59% achieved with<br />
manual procedures (see Table 21).<br />
Bcl-2<br />
Introduction<br />
The bcl-2 molecule is an oncogene product (oncoprotein)<br />
blocking apoptotic cell death (Hockenberry et al). In<br />
lymphoid tissues bcl-2 is expressed by mantle zone B-cells<br />
and all effector T-cells, while germinal centre B-cells<br />
lack this molecule. bcl-2 immunoreaction results in an<br />
eccentric cytoplasmic signal since it is localised in<br />
the nuclear envelope, endoplasmic reticulum and<br />
mitochondrial membrane in positive cells.<br />
The upregulation of bcl-2 expression in lymphoid nodular<br />
structures is a specific feature of most follicular lymphomas<br />
resulted from of a non-random chromosomal translocation<br />
t(14;18), when the bcl-2 gene is inserted into juxtaposition<br />
to the highly active IgH gene (Ngan et al).
Guidelines used in the assessment of bcl-2 immunostaining<br />
SCORE STAINING PATTERN<br />
0 No returns.<br />
1 Little or no staining of bcl-2 in the cells expected to stain<br />
(see text above)<br />
2 Very weak demonstration of bcl-2 in most cells expected<br />
to stain, or many of these cells were not demonstrated<br />
3 Weak demonstration of most cells expected to stain.<br />
4 Good demonstration of all the cells expected to stain,<br />
with clear signs of eccentric sub-cellular distribution and<br />
a dynamic range of expression levels of bcl-2<br />
5 Very intense staining in most of the relevant cells with<br />
crisp eccentric localisation of bcl-2 in most cells, crisp<br />
morphology and no background staining<br />
NB. These are only very general guidelines and marks were deducted<br />
<strong>for</strong> such things as poor localisation of staining or diffuse staining, inappropriate<br />
staining of certain cell types, excessive background staining, excessive<br />
counter-stain, uneven staining or other factors which made interpretation<br />
difficult.<br />
The four individual scores <strong>for</strong> each slide were added<br />
together to give a mark out of 20.<br />
Features of optimal immunostaining (see Plates 33, 34, 35<br />
and 36)<br />
• Strong cytoplasmic labelling of most lymphocytes<br />
except germinal centre B-cells<br />
• Eccentric ring-like appearance of immunostaining<br />
within individual cells with a wide range of expression<br />
levels in adjacent cells resulting in a dynamic staining<br />
pattern<br />
• Extracellular appearance of the antigen should be<br />
minimal or lacking<br />
Features of sub-optimal immunostaining (see Plates 37,<br />
38 and 39)<br />
• Weak, uneven, partially missing staining of relevant cells.<br />
• High background or non-specific staining of cell types<br />
not expected to stain<br />
Plate 27. CD3 antibody staining T-cells in reactive tonsil (<strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
section). Strong labelling of peri-follicular T-cell region and dispersed intrafollicular<br />
T-lymphocytes (score20/20). All Plates here with the exception of<br />
Plate 29 are of immunostaining reactions using DAB as a chromogen.<br />
153<br />
<strong>Immunocytochemistry</strong> — Lymphoma<br />
Please note: The reasons <strong>for</strong> poor results most probably<br />
were insufficient HIER (weak, missing staining – see Plates<br />
37 and 38), overused/inappropriate HIER and/or the<br />
inappropriate dilution of primary antibody under the<br />
conditions used (non-specific staining – see Plate 39).<br />
The sensitivity of bcl-2 staining is best assessed on the<br />
demonstration of germinal centre T cells (see Plates 34,<br />
35 and 36).<br />
Summary of bcl-2 results from this assessment<br />
Antibody clone 124 (DakoCytomation M0887) is still the<br />
best choice allowing the highest pass rate (68%) when<br />
demonstrating bcl-2 antigen (see Table 17). Concerning<br />
correlations between the results (pass rates) and other<br />
technical details, most of the general notes made at the<br />
summary of CD3 results (see above) are valid here also.<br />
Some exceptions include lower pass rates <strong>for</strong> bcl-2<br />
compared to CD3 detection when using Vector Elite<br />
Universal ABC kit PK6200 (26% vs. 86%, see Table 19),<br />
Ventana iView DAB chromogen-substrate (38% vs. 68%,<br />
see Table 20), Ventana NexES (56% vs. 72%) or Ventana<br />
Benchmark (25% vs. 69%, see Table 21) automated<br />
immunostainers. These discrepancies were most probably<br />
due to using primary antibodies different from clone 124,<br />
which were found less successful (see Table 17). The 100%<br />
passing rates achieved with using A. Menarini Optimax<br />
immunostainer is also worth mentioning, though the<br />
number of participants using this option is relatively low.<br />
REFERENCES<br />
1. Griesser H, Mak TW. The T-cell receptor-structure, function, and clinical<br />
application. Hematol Pathol. 1994; 8: 1-23<br />
2. Hockenberry DM, Zutter M, Hickey W et al. Bcl-2 protein is topographically<br />
restricted in tissues characterised by apoptotic cell<br />
death. Proc Natl Acad Sci (USA) 88:6961-6965.<br />
3. Mason DY, Cordell J, Brown M et al. Detection of T cells in paraffin<br />
wax embedded tissue using antibodies against a peptide<br />
sequence from the CD3 antigen. J Clin Pathol 1989; 42:1194-1200.<br />
4. Ngan B-Y, Chen-Levy Z, Weiss LM et al. Expression in non-Hodgkin’s<br />
lymphoma of the bcl-2 protein is associated with the t(14;18)<br />
chromosomal translocation. New Engl J Med 318:1638-1644.<br />
Plate 28. CD3 antibody staining T-cells in reactive tonsil (<strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
section). Higher power image of the same reaction as that on Plate 27. All<br />
T-cells show clear cell membrane staining within and around the lymphoid<br />
follicle, (score 20/20).
<strong>Immunocytochemistry</strong> — Lymphoma<br />
Plate 29. CD3 staining on reactive tonsil (<strong>UK</strong> <strong>NEQAS</strong>-ICC section). Strong<br />
but slightly diffuse staining of T-cells particularly in the peri-follicular<br />
region. Immunostained using an alkaline phosphatase labelled detection<br />
system and New Fuchsin as chromogen (score 14/20).<br />
Plate 31. CD3 staining on reactive tonsil (<strong>UK</strong> <strong>NEQAS</strong>-ICC section).<br />
Specific T-cell staining accompanied by excessive background<br />
(score 12/20).<br />
Plate 33. bcl-2 antibody staining in an In House section of reactive lymph<br />
node. Low power view shows excellent staining of areas expected to be<br />
positive, e.g. peri-follicular T-cell regions and mantle zone B-cell regions<br />
(score 20/20).<br />
154<br />
Plate 30. CD3 staining on reactive tonsil (<strong>UK</strong> <strong>NEQAS</strong>-ICC section).<br />
Moderate and incomplete staining of T-cells (score 12/20).<br />
Plate 32. CD3 staining on reactive tonsil. Strong non-specific staining in<br />
the germinal centre obscures specific T-cell staining (score 8/20).<br />
Plate 34. bcl-2 staining in reactive tonsil (<strong>UK</strong> <strong>NEQAS</strong>-ICC section).<br />
Peri- and intra-follicular T-cells and mantle B-cells are strongly positive<br />
(score 20/20).
Plate 35. bcl-2 staining in reactive tonsil (<strong>UK</strong> <strong>NEQAS</strong>-ICC section). Higher<br />
power view of the same reaction as on Plate 34 shows eccentric staining<br />
of individual cells and a wide range of bcl-2 expression levels among<br />
positive cells.<br />
Plate 37. bcl-2 staining in reactive tonsil (<strong>UK</strong> <strong>NEQAS</strong>-ICC section). The<br />
same area as that seen in Plates 36 and 38. Moderate but unequivocal<br />
staining in most cells expected to stain (score 14/20).<br />
Plate 39. bcl-2 staining in reactive tonsil (<strong>UK</strong> <strong>NEQAS</strong>-ICC section).<br />
Strong non-specific staining in the nuclei of germinal centre B-cells<br />
obscure bcl-2 reaction (score 8/20).<br />
155<br />
<strong>Immunocytochemistry</strong> — Lymphoma<br />
Plate 36. bcl-2 staining in reactive tonsil (<strong>UK</strong> <strong>NEQAS</strong>-ICC section). The<br />
same area as that seen in Plates 37 and 38. Strong cytoplasmic staining<br />
in all lymphocytes expected to stain including germinal centre T-cells<br />
(score 20/20).<br />
Plate 38. bcl-2 staining in reactive tonsil (<strong>UK</strong> <strong>NEQAS</strong>-ICC section). The same<br />
follicular area as that seen in Plates 36 and 37. Very weak and incomplete<br />
staining of peri-follicular lymphocytes. The germinal centre-T cells, which<br />
are expected to stain with bcl-2 are not demonstrated (score 8/20).
<strong>Immunocytochemistry</strong> — Lymphoma<br />
MAIN TECHNICAL PARAMETERS EMPLOYED BY PARTICIPANTS IN THE LYMPHOMA MODULE<br />
The following tables record the number of participants (N) using each system. The percentage (%) refers to the<br />
proportion of these participants achieving acceptable staining (a score >12/20). For example in the first table,<br />
15 participants used LabVision CD3 code RM-9017 of whom 67% achieved acceptable staining.<br />
Table 16. Primary Antibody (CD3)<br />
Antibody Details N %<br />
DakoCytomation A0452 34 73<br />
DakoCytomation M7254 65 65<br />
DakoCytomation M 7193 2 0<br />
Cell Marque CMC 364 3 67<br />
ID Labs BP517 1 100<br />
Incomplete data 3 100<br />
LabVision RM-9017 15 67<br />
Novocastra NCL-CD3-PS1 68 66<br />
Neomarkers MS 401 (Clone PS1 ) 1 100<br />
Other 2 100<br />
Ventana 790 2921 9 78<br />
Zymed 18 0102 1 100<br />
Table 18. Pre-treatment<br />
CD3 bcl-2<br />
Pre-treatment N % N %<br />
Incomplete data 1 100 1 100<br />
Microwave Oven 61 70 61 61<br />
Other 5 40 5 100<br />
Pressure Cooker 85 76 84 77<br />
Pressure Cooker inside Microwave 18 78 18 78<br />
Water bath 95-98 o C 15 40 14 36<br />
Ventana Benchmark 18 67 18 22<br />
156<br />
Table 17. Primary Antibody (bcl-2)<br />
Antibody Details N %<br />
Biogenex MU 287-UC 4 50<br />
DakoCytomation M0887 173 68<br />
Neomarkers MS 123 PO 1 0<br />
Novocastra NCL-BCL-2 13 46<br />
Incomplete data 5 60<br />
Ventana 760-2693 (Clone P2D11F11) 6 50<br />
Table 19. Detection system<br />
CD3 bcl-2<br />
Type, supplier & product code N % N %<br />
A.Menarini Multi link/HRP LP000-UL 9 67 9 56<br />
Chemicon HP 1000 1 0 1 0<br />
DakoCytomation ChemMate - 42 86 42 88<br />
L.St.Av/HRP K5001<br />
DakoCytomation ChemMate - 27 78 26 81<br />
EnVision K5007 DAB<br />
DakoCytomation Duet St.ABC K0492 3 67 3 100<br />
DakoCytomation Envision 15 80 15 67<br />
DakoCytomation LSAB Kit/HRP K0675 6 17 5 20<br />
DakoCytomation St.ABC/HRP K0377 1 100 1 100<br />
Incomplete data 5 80 5 60<br />
Other 9 56 9 56<br />
LabVision TS 125 HR 6 33 6 33<br />
Power vision DPVB 999 HRP 1 0 1 0<br />
Vector Elite ABC PK6102 1 0 1 100<br />
Vector Elite Universal ABC PK6200 14 86 14 26<br />
Vector Elite ABC PK6100 4 75 4 100<br />
Vector Elite ABC PK7200 RTU kit 10 60 10 50<br />
Ventana basic system 8 63 8 63<br />
Ventana iView system 37 68 37 35<br />
Zymed 87 8143 1 0 1 0<br />
Zymed 85 9043 1 0 1 0
Table 20. Chromogen<br />
CD3 bcl-2<br />
Chromogen & Supplier N % N %<br />
A. Menarini HK 153 5K DAB 12 67 12 58<br />
DakoCytomation K5001 DAB 43 84 43 88<br />
DakoCytomation K3466 DAB 5 80 5 80<br />
DakoCytomation K3468 DAB 23 56 21 56<br />
DakoCytomation S3000 DAB 2 100 2 100<br />
DakoCytomation Envision DAB 11 82 11 82<br />
DakoCytomation ChemMate<br />
EnVision K5007<br />
27 78 27 78<br />
Incomplete data 11 73 11 64<br />
KEM-EN-TEC 4170 DAB 2 50 2 50<br />
LabVision TA 125 HD DAB 4 25 4 25<br />
Other 7 71 7 71<br />
Sigma D5637 DAB 3 33 3 67<br />
Sigma D5905 DAB 2 50 2 50<br />
Vector SK4100 DAB 4 25 4 50<br />
Ventana iView DAB 40 68 40 38<br />
Zymed 00 2020 DAB 3 33 3 0<br />
BEST METHODS<br />
CD3<br />
Participant Scored 20/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) and<br />
20/20 (In house slide) using this method.<br />
Method: DakoCytomation ChemMate kit K5001<br />
Automation: DakoCytomation TechMate 500 plus<br />
Buffer and pH: DakoCytomation ChemMate EnVision<br />
K5001 buffer<br />
Blockade Type: DakoCytomation ChemMate EnVision<br />
K5001 blocking solution<br />
Antigen Retrieval: Pressure cooker to heat 3L of EDTA buffer<br />
pH 8.0 <strong>for</strong> 1.5 minutes at full pressure<br />
Primary Antibody: Novocastra NCL-CD3-PS1 1:100 dilution,<br />
<strong>for</strong> 50 minutes at room temperature<br />
Chromogen: DakoCytomation ChemMate K5001 DAB,<br />
<strong>for</strong> 15 minutes<br />
Bcl-2<br />
Participant scored 19/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) and<br />
20/20 (In House slide) using this method.<br />
Method: DakoCytomation ChemMate kit K5001<br />
Automation: DakoCytomation TechMate 500 plus<br />
Buffer and pH: DakoCytomation ChemMate kit K5001<br />
Blockade Type: DakoCytomation ChemMate kit K5001<br />
Antigen Retrieval: Prestige pressure cooker to heat 3L of<br />
EDTA buffer pH 8.0 at full pressure <strong>for</strong><br />
1.5 minutes<br />
Primary Antibody: DakoCytomation M0887 (clone 124),<br />
dilution 1:300 <strong>for</strong> 50 minutes at room<br />
temperature<br />
Chromogen: DakoCytomation ChemMate kit K5001<br />
DAB, time not stated<br />
157<br />
<strong>Immunocytochemistry</strong> — Lymphoma<br />
Table 21. Automation<br />
CD3 bcl-2<br />
Instrument & Supplier N % N %<br />
A. Menarini Optimax 14 86 14 100<br />
A. Menarini Genon MX i6000 8 88 8 63<br />
Dakocytomation Autostainer 35 86 35 77<br />
Dakocytomation TechMate Horizon 1 100 1 100<br />
Dakocytomation TechMate 500 27 81 27 85<br />
Incomplete data 2 100 2 100<br />
Lab Vision Autostainer 16 56 16 50<br />
None 49 59 48 65<br />
Shandon Sequenza 10 40 9 56<br />
Shandon Cadenza 1 0 1 0<br />
Ventana ES 5 60 5 0<br />
Ventana NexES 18 72 18 56<br />
Ventana Gen11 1 0 1 0<br />
Ventana Benchmark 16 69 16 25<br />
CD3<br />
Participant Scored 20/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) and<br />
17/20 (In house slide) using this method.<br />
Method: Vector Elite Universal kit PK6200<br />
Automation: None<br />
Buffer and pH: Tris buffer pH7.6<br />
Blockade Type: Hydrogen peroxide solution<br />
Antigen Retrieval: Kenwood Pressure Cooker, to heat 1.5L of<br />
DakoCytomation Target Retrieval solution<br />
S3308, pH10.0 <strong>for</strong> 2 minutes at full pressure<br />
Primary Antibody: Novocastra NCL-CD3-PS1 dilution 1:100<br />
<strong>for</strong> 30 minutes at room temperature<br />
Chromogen: DakoCytomation K3466 DAB, pH7.5<br />
<strong>for</strong> 5 minutes<br />
Bcl-2<br />
Participant scored 19/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) and<br />
20/20 (In House slide) using this method.<br />
Method: Vector Elite Universal PK6200<br />
Ventana DAB kit 253-2198<br />
Automation: Ventana NexES<br />
Buffer and pH: Phosphate buffered saline<br />
Blockade Type: Hydrogen peroxide and serum<br />
Antigen Retrieval: Kenwood Pressure cooker, to heat 1.5L of<br />
citrate buffer pH 6.0 <strong>for</strong> 2 minutes at full<br />
pressure<br />
Primary Antibody: DakoCytomation M0887 (clone 124),<br />
dilution 1:40 at 42 o C <strong>for</strong> 30 minutes<br />
Chromogen: DakoCytomation K3466 DAB pH7.5<br />
<strong>for</strong> 5 minutes
<strong>Immunocytochemistry</strong> — Neuropathology<br />
The Neuropathology Module<br />
Kwok Kee Chan<br />
Antigens assessed: Synaptophysin and Cytokeratin<br />
Tissue sections circulated: a block with a medulloblastoma<br />
(synaptophysin); a block with a secondary<br />
carcinoma in brain (cytokeratin)<br />
Number of participating laboratories:<br />
57 (synaptophysin), 56 (cytokeratin)<br />
Distribution of scores<br />
frequency of returns<br />
Figure 12. Run 65G: Synaptophysin (<strong>UK</strong> <strong>NEQAS</strong>-ICC Sections)<br />
frequency of returns<br />
Run 65G Synaptophysin on <strong>UK</strong> <strong>NEQAS</strong> Sections<br />
Summary<br />
Scores > 12/20 48(84%)<br />
Scores 10-12/20 7(12%)<br />
Scores 12/10 42(75%)<br />
Scores 10-12/20 11(20%)<br />
Scores 12/20 56(96%)<br />
Scores 10-12/20 1( 2%)<br />
Scores 12/20 56(100%)<br />
scores scores<br />
Figure 14. Run 65J: Pan-cytokeratin (<strong>UK</strong> <strong>NEQAS</strong>-ICC Sections) Figure 15. Run 65K: Pan-cytokeratin (In House Sections)<br />
frequency of returns
Synaptophysin<br />
In this run, 84% of the participants achieved satisfactory<br />
to good results with the <strong>UK</strong> <strong>NEQAS</strong>-ICC sections. The<br />
demonstration of synaptophysin in medulloblastoma is<br />
often requested <strong>for</strong> the confirmation of the neuronal<br />
origin of the tumour. Moreover, the tumour may appear as<br />
bi-phasic with islands of strongly stained, neurogenically<br />
more matured cells. Synaptophysin is a fixation sensitive<br />
antigen, i.e. prolonged fixation in <strong>for</strong>malin may require a<br />
correspondingly more extraneous antigen retrieval<br />
regime to recover the reactivity of the antigen. As to the<br />
tissue that was used in this run, it was moderately fixed,<br />
so such regimes may not have been required in order to<br />
produce strong positive staining. On the In House sections,<br />
96% of participants achieving an acceptable result.<br />
Features of optimal immunostaining (Plates 40 and 41)<br />
• Medulloblastoma, intense and specific staining in<br />
the perikarya of the tumour cells.<br />
Plate 40. Optimal demonstration of synaptophysin on <strong>UK</strong><br />
<strong>NEQAS</strong>-ICC section of tumour.<br />
Plate 42. Sub-optimal demonstration of synaptophysin on <strong>UK</strong> <strong>NEQAS</strong>-<br />
ICC section of tumour. Staining is very weak (compare with Plate 40).<br />
159<br />
<strong>Immunocytochemistry</strong> — Neuropathology<br />
Features of sub-optimal immunostaining (Plates 42 and 43)<br />
• Very weak staining in the perikarya of the tumour cells.<br />
Cytokeratin<br />
About 75% of the laboratories achieved satisfactory to<br />
good staining on the <strong>UK</strong> <strong>NEQAS</strong>-ICC sections of a<br />
secondary carcinoma in the central nervous system<br />
and 100% on the In House sections. Anti-cytokeratins is<br />
often incorporated into the panel of antibodies <strong>for</strong> the<br />
differential diagnosis of secondary tumours. Hence, a<br />
broad-spectrum cytokeratin antibody is essential <strong>for</strong><br />
such purpose as to ensure successful detection of<br />
carcinoma of various origins.<br />
Features of optimal immunostaining (Plates 44 and 45)<br />
• Clear demonstration of tumour cells in the metastatic<br />
carcinoma.<br />
Features of sub-optimal immunostaining (Plates 46 and 47)<br />
• Very weak staining of the tumour cells.<br />
Plate 41. Higher power view of same section as shown in Plate 40.<br />
Plate 43. Higher power view of same section as shown in Plate 42.
<strong>Immunocytochemistry</strong> — Neuropathology<br />
Plate 44. Optimal demonstration of cytokeratins on <strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
section of tumour.<br />
Plate 46. Poor demonstration of cytokeratins on <strong>UK</strong> <strong>NEQAS</strong>-ICC<br />
section of tumour. Staining is weak and uneven.<br />
Plate 48. Optimal result with cytokeratin on a participant’s In<br />
House control. The full depth of squamous epithelium is well<br />
stained.<br />
160<br />
Plate 45. Higher power view of same section as shown in Plate 42.<br />
Plate 47. Higher power view of same section as shown in Plate 46.<br />
Plate 49. Optimal result with cytokeratin on a participant’s In House<br />
control. The full depth of crypt epithelium is well stained in this gut<br />
section.
BEST METHODS<br />
Synaptophysin<br />
Participant scored 20/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) and<br />
16/20 (In House slide) using this method.<br />
Method: Ventana iView DAB kit<br />
Automation: Ventana NexES<br />
Buffer and pH: Ventana APK was buffer<br />
Blockade Type: Ventana solution<br />
Antigen Retrieval: Water-bath to heat 200 ml of EDTA buffer<br />
pH 8.0 <strong>for</strong> 23 minutes at 98 o C<br />
Primary Antibody: DakoCytomation N1566<br />
pre-diluted antibody <strong>for</strong> 30 minutes<br />
Chromogen: Ventana DAB <strong>for</strong> 8 minutes<br />
Pan-cytokeratin<br />
Participant scored 20/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slides) and<br />
19/20 (In House Sections) using this method.<br />
Method: DakoCytomation Envision K4007 kit<br />
Automation: LabVision Autostainer<br />
Buffer and pH LabVision TBS TA-125-TB buffer with<br />
0.05% Tween-20<br />
Blockade Type: Hydrogen peroxide solution<br />
Antigen Retrieval: Sigma Chymotrypsin C-4129<br />
(concentration not stated), pH7.8 <strong>for</strong><br />
10 minutes at 37 o C<br />
Primary Antibody: DakoCytomation M3515 (clones AE1/AE3)<br />
dilution 1:85 <strong>for</strong> 30 minutes room<br />
temperature<br />
Chromogen: DakoCytomation EnVision DAB K4007<br />
<strong>for</strong> 5 minutes<br />
161<br />
<strong>Immunocytochemistry</strong> — Neuropathology<br />
Synaptophysin<br />
Participant scored 20/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) and<br />
17/20 (In House slide) using this method.<br />
Method: DakoCytomation ChemMate K5001 kit<br />
Automation: DakoCytomation TechMate 500 plus<br />
Buffer and pH: DakoCytomation ChemMate K5001<br />
buffer<br />
Blockade Type: DakoCytomation ChemMate K5001<br />
solution<br />
Antigen Retrieval: Samsung 800W Microwave oven to<br />
heat 400 ml of citrate buffer pH6.0 <strong>for</strong><br />
20 minutes<br />
Primary Antibody: DakoCytomation A0010 polyclonal,<br />
dilution 1:40 <strong>for</strong> 50 minutes at room<br />
temperature<br />
Chromogen: DakoCytomation DAB K5001 <strong>for</strong> 15<br />
minutes at room temperature<br />
Pan-cytokeratin<br />
Participant scored 20/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slides) and<br />
20/20 (In House Sections) using this method.<br />
Method: Vector Elite RTU kit PK7200<br />
Automation: DakoCytomation Autostainer plus<br />
Buffer and pH Tris buffer saline pH 7.6<br />
Blockade Type: 3% Hydrogen peroxide, and horse serum<br />
Antigen Retrieval: Kenwood PC400 Pressure cooker to heat<br />
1.6L of Vector unmasking solution pH 6.0<br />
<strong>for</strong> 4 minutes at full pressure. Then 2<br />
seconds in Sigma Protease (concentra<br />
tion not stated) Type XXIV P5147 at pH 7.4<br />
at room temperature<br />
Primary Antibody: DakoCytomation M0821 (clone MNF116)<br />
dilution 1:100 <strong>for</strong> 30 minutes at room<br />
temperature<br />
Chromogen: A. Menarini HK-153-5K DAB <strong>for</strong> 10 minutes
<strong>Immunocytochemistry</strong> — Neuropathology<br />
MAIN TECHNICAL PARAMETERS EMPLOYED BY PARTICIPANTS IN THE NEUROPATHOLOGY MODULE<br />
The following tables record the number of participants (N) using each system. The percentage (%) refers to the<br />
proportion of these participants achieving acceptable staining (a score >12/20). For example in the 1st table, 20<br />
participants used DakoCytomation Synaptophysin (code A0100), 70% of whom achieved acceptable staining.<br />
Table 22. Primary Antibody. [Synaptophysin]<br />
Antibody Details N %<br />
A. Menarini MU 363 1 100<br />
Boehninger 902314 (Clone SY38 ) 1 100<br />
DakoCytomation M0776 (Clone SY38) 19 84<br />
DakoCytomation A0010 20 70<br />
DakoCytomation N1566 1 100<br />
Incomplete data 1 100<br />
Lab Vision RM 9111 SO 2 50<br />
Novocastra NCL-SYNAP 9 100<br />
Other 1 100<br />
Zymed 18-0130 3 100<br />
Table 24. Pre-treatment<br />
SYNAPTOPHYSIN PAN-CK<br />
Pre-treatment N % N %<br />
DakoCytomation Protease K S3020 - - 1 100<br />
Difco Trypsin 215240 - - 6 67<br />
Heat and Enzyme - - 4 100<br />
ICN Trypsin - - 2 50<br />
Incomplete data 1 0 1 100<br />
None 3 67 - -<br />
Microwave Oven 27 89 13 69<br />
Other - - 3 100<br />
Pressure Cooker 15 80 10 70<br />
Pressure Cooker inside Microwave Oven 6 100 2 100<br />
Sigma Pepsin P7000 - - 2 100<br />
Sigma Protease P5147 1 0 1 0<br />
Sigma Protease P8038 - - 1 100<br />
Sigma Chymotrypsin C-4129 - - 3 100<br />
Ventana benchmark 2 100 - -<br />
Ventana Protease 1 - - 7 57<br />
Water bath 98oC <strong>for</strong> 40 minutes 3 67 - -<br />
Table 26. Chromogen<br />
SYNAPTOPHYSIN PAN-CK<br />
Chromogen & Supplier N % N %<br />
Biogenex HK-153-5K DAB 2 50 2 50<br />
DakoCytomation K3468 5 60 5 60<br />
DakoCytomation K5001 DAB 12 100 12 83<br />
DakoCytomation S3000 1 100 1 0<br />
DakoCytomation Envision 4 50 4 75<br />
Dakocytomation K5007<br />
ChemMate Envision<br />
9 100 9 78<br />
Dakocytomation K3219 DAB 1 100 1 100<br />
Merk New Fuchsin 4041 1 100 1 100<br />
Sigma A5754 AEC 1 0 1 0<br />
Sigma D3466 1 100 - -<br />
Sigma D5905 1 100 1 100<br />
Sigma D5635 DAB 1 100 1 100<br />
Sigma D5637 DAB 3 100 3 67<br />
Vision Biosystem DAB 1 100 1 100<br />
Ventana iView DAB 7 100 6 67<br />
Zymed DAB kit 1 100 1 100<br />
Table 25. Detection System<br />
SYNAPTOPHYSIN PAN-CK<br />
Type, Supplier & Product Code N % N %<br />
A.Menarini Multi link/HRP LP000-UL 1 100 1 0<br />
DakoCytomation ChemMate<br />
L.St.Av/HRP K5001<br />
12 100 12 83<br />
DakoCytomation Duet St.ABC K0492 1 100 1 100<br />
DakoCytomation Envision Kits 7 57 7 43<br />
DakoCytomation St.ABC/HRP K0377 1 100 1 100<br />
DakoCytomation K0675 2 50 1 100<br />
DakoCytomation K5007 ChemMate Envision 9 100 9 78<br />
DakoCytomation K0391 1 100 1 100<br />
LabVision TS 125 HRP 1 100 1 100<br />
Incomplete data 2 50 2 100<br />
Vector Elite ABC PK 6100 2 50 2 50<br />
Vector Elite Universal ABC PK6200 5 80 5 60<br />
Vector PK7200 RTU 4 50 4 100<br />
Ventana basic system 4 100 4 75<br />
Ventana iView System 3 100 2 50<br />
Vision Biosystem D59404 1 100 1 100<br />
Zymed 85 9043 1 0 1 100<br />
Zymed 87 8143 1 100 1 100<br />
Table 27. Automation<br />
SYNAPTOPHYSIN PAN-CK<br />
Instrument & Supplier N % N %<br />
162<br />
Table 23. Primary antibody. [Cytokeratin]<br />
Antibody Details N %<br />
Becton Dickinson 349205 (CAM 5.2)* 4 100<br />
DakoCytomation M0821 (Clone MNF116 ) 25 80<br />
DakoCytomation M3515 (Clone AE1/AE3 ) 14 57<br />
DakoCytomation H7118 (Clone 34βE12)* 1 100<br />
Home made cocktails 2 100<br />
Novocastra NCL-AE1/AE3 1 100<br />
Sigma C2562 1 100<br />
Ventana 760 2595 (Clone AE1/AE3 ) 4 25<br />
Zymed 28001 (cocktail) 2 100<br />
Zymed 18-0132 (Clone AE1/AE3) 1 100<br />
*Although CAM5.2 and 34βE12 are not pan-cytokeratin antibodies participants who<br />
used them were not penalized at this assessment.<br />
A. Menarini Optimax 1 100 1 100<br />
DakoCytomation Autostainer 12 83 12 67<br />
DakoCytomation TechMate 500 11 100 11 91<br />
LabVision Autostainer 2 50 2 100<br />
Incomplete data 2 50 2 100<br />
None 19 79 18 61<br />
Shandon Sequenza 3 33 3 100<br />
Ventana NexES 3 100 3 100<br />
Ventana Benchmark 2 100 1 0<br />
Ventana ES 2 100 2 50<br />
Vision Biosystem Bond X 1 100 1 100
The Cytology Module<br />
Dr Perry Maxwell<br />
Antigens Assessed: Melanoma Markers. Cytokeratins<br />
Material circulated: cell line from a metastatic<br />
melanoma (melanoma markers), clinical sample from<br />
adenocarcinoma in pleural fluid (cytokeratins)<br />
Number of participating laboratories: 87 (melanoma<br />
markers), 87 (cytokeratins)<br />
Guidelines used in the assessment of slides:<br />
SCORE STAINING PATTERN<br />
0 No returns<br />
1 Little or no staining of the antigen in question.<br />
2 Very weak demonstration of the cells expected to<br />
stain or majority of these cells were not demonstrated.<br />
Inappropriate staining of other cells which<br />
may lead to problems in a diagnostic setting.<br />
3 Weak demonstration of most of the cells expected<br />
to stain.<br />
4 Good demonstration of all the cells expected to<br />
stain<br />
5 Excellent demonstration of all the cells expected<br />
to stain<br />
NB. These are only very general guidelines and marks were deducted <strong>for</strong><br />
such things as poor localisation of staining or diffuse staining, inappropriate<br />
staining of certain cell types, excessive background staining, excessive<br />
counter-stain, uneven staining or other factors which made interpretation<br />
difficult.<br />
Distribution of scores<br />
frequency of returns<br />
frequency of returns<br />
Run 65R Melanoma Markers on <strong>UK</strong> <strong>NEQAS</strong> cytospins<br />
Summary<br />
Scores> 12/20 61(70%)<br />
Scores 10-12/20 18(21%)<br />
Scores 12/20 75(89%)<br />
Scores 10-12/20 9(11%)<br />
Figure 17. Run 65R: Melanoma markers (<strong>UK</strong> <strong>NEQAS</strong>-ICC cytospins) Figure 18. Run 65S: Melanoma markers (In House Slides)<br />
Run 65T Cytokeratin on <strong>UK</strong> <strong>NEQAS</strong> Cytospins<br />
Summary<br />
Scores >12/20 83(96%)<br />
Scores 10-12/20 3( 3%)<br />
Scores 12/20 81(93%)<br />
Scores 10-12/20 5( 6%)<br />
Scores< 10/20 1( 1%)<br />
scores scores<br />
Figure 19. Run 65T: Cytokeratin (<strong>UK</strong> <strong>NEQAS</strong>-ICC cytospins) Figure 20. Run 65U: Cytokeratin (In House Slides)<br />
frequency of returns<br />
frequency of returns
<strong>Immunocytochemistry</strong> — Cytology<br />
Plate 50. Melanoma marker (HMB45) on <strong>UK</strong> <strong>NEQAS</strong>-ICC slide.<br />
Optimal staining.<br />
Plate 52. Sub-optimal staining of melanoma cells in <strong>UK</strong> <strong>NEQAS</strong>-ICC slide.<br />
Melanoma markers<br />
Introduction<br />
There is a role <strong>for</strong> immunocytochemistry in the identification<br />
of metastatic melanoma (Nasiell et al, Nasuti<br />
et al, Filie et al). This role is particularly useful in FNA<br />
preparations of metastatic samples with epithelioid<br />
differentiation (Filie et al) and patients in clinical trials<br />
undergoing immunotherapy (Fetsch et al).<br />
Features of Optimal Staining (Plates 50 and 51)<br />
• Up to 75% of the cells should be positive <strong>for</strong> HMB45<br />
(Plate 50).<br />
• Almost 100% of the cells should be positive <strong>for</strong> S100.<br />
Polarisation of S100 was shown by some participants<br />
(Plate 51).<br />
• The expected cellular location <strong>for</strong> all melanoma<br />
markers is cytoplasmic<br />
• The intensity of the counterstain should be such as to<br />
show nuclei.<br />
164<br />
Plate 51. Melanoma marker (S100) on <strong>UK</strong> <strong>NEQAS</strong>-ICC slide. Optimal<br />
staining, note the polarization of S100 positive reaction.<br />
Plate 53. Pan-cytokeratin on <strong>UK</strong> <strong>NEQAS</strong>-ICC slide. Optimal staining.<br />
Features of Sub-optimal staining (Plate 52)<br />
• Loss of morphology. This was most often seen when<br />
digestion methods were employed using cell conditioning<br />
fluid on automated staining systems,<br />
enzymes or heat mediated antigen retrieval. Any<br />
<strong>for</strong>m of antigen retrieval of alcohol-fixed cytospins<br />
is not usually necessary. If employed, retrieval<br />
should be minimal.<br />
• Poor counterstain quality. Quite often, participants<br />
didn’t seem to employ any counterstain, or if<br />
used, this was too weak to be of use. In cytological<br />
preparations, nuclear morphology can help to<br />
identify cell type.<br />
Note on primary antibodies and pre-treatment methods:<br />
The majority of participants used antibodies to S100 or the<br />
HMB45 clone. One participant used an antibody to<br />
MelanA. Both of the best methods highlighted did not use<br />
any <strong>for</strong>m of pretreatment.
Note on In House controls: Of the 84 participants who submitted<br />
In House controls, only 15 used cytology controls,<br />
including cell blocks. All others used histological sections<br />
of melanoma/skin.<br />
REFERENCES<br />
1. Fetsch PA, Steinberg SM, Riker AI, Marincola FM, Abati A. Melanoma<br />
antigen expression in serial fine-needle aspiration samples in patients<br />
with metastatic malignant melanoma participating in immunotherapy<br />
clinical trials: a preliminary look. Cancer. 2001; 93: 409-14.<br />
2. Filie AC, Simsir A, Fetsch P, Abati A. Melanoma metastatic to the<br />
breast: utility of fine needle aspiration and immunohistochemistry.<br />
Acta Cytol. 2002; 46: 13-8.<br />
3. Nasuti JF, Gupta PK, Baloch ZW. Clinical implications and value of<br />
immunohistochemical staining in the evaluation of lymph node<br />
infarction after fine-needle aspiration. Diagn Cytopathol. 2001; 25: 104-7.<br />
4. Nasiell K, Tani E, Skoog L. Fine needle aspiration cytology and<br />
immunocytochemistry of metastatic melanoma. Cytopathology.<br />
1991; 2: 137-47.<br />
Pan-cytokeratin<br />
Introduction<br />
The use of fine needle aspiration cytology is now<br />
considered a valid and standard method in the<br />
diagnosis of various primary and metastatic tumours.<br />
The use of a pan-cytokeratin marker can be useful in<br />
highlighting epithelial cells in such samples.<br />
Features of Optimal Staining (Plate 53)<br />
• The samples circulated <strong>for</strong> staining were cytospin<br />
preparations from a clinical sample (pleural aspirate)<br />
of adenocarcinoma of the lung. Cytoplasmic staining<br />
of cytokeratin should be seen.<br />
BEST METHODS<br />
Melanoma markers<br />
Participant Scored 19/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) using this<br />
method.<br />
Method: DakoCytomation ChemMate EnVision<br />
kit K5007<br />
Automation: DakoCytomation TechMate 500 plus<br />
Buffer and pH: DakoCytomation ChemMate EnVision<br />
K5007 buffer<br />
Blockade Type: DakoCytomation ChemMate EnVision<br />
K5007 solution<br />
Antigen Retrieval: None<br />
Primary Antibody: DakoCytomation S100 polyclonal Z0311<br />
dilution 1:3000, <strong>for</strong> 60 minutes at room<br />
temperature<br />
Chromogen: DakoCytomation ChemMate EnVision<br />
K5007 DAB <strong>for</strong> 7.5 minutes<br />
165<br />
<strong>Immunocytochemistry</strong> — Cytology<br />
• As this is a clinical sample, there is a population of nonepithelial<br />
cells, which should remain negative.<br />
• In keeping with all cytological preparations, nuclear<br />
morphology can help to identify cell type. The<br />
intensity of the counterstain should be such as to<br />
show nuclei.<br />
Features of Sub-optimal staining<br />
• The major feature of sub-optimal staining was one of<br />
non-specificity. In this clinical sample, background<br />
reactive cells such as polymorphs should be negative.<br />
A poor score was usually attributable to positive<br />
cytoplasmic staining of these reactive cells.<br />
• Often, in those participating laboratories which scored<br />
below an acceptable level, there was also a loss of cell<br />
morphology, particularly of nuclear detail. Loss of<br />
morphology was often seen when the material was<br />
pretreated either by enzyme, cell conditioning fluid or<br />
microwaving. One participant went so far as to both<br />
microwave followed by enzyme digestion.<br />
Pretreatment regimes are not recommended on this<br />
alcohol-fixed material.<br />
• In cytological preparations, the appearance of the<br />
nucleus is important and needs to be seen.<br />
Notes on primary antibodies and automation: The two<br />
clones, most often used were the MNF116 (DakoCytomation)<br />
and the mix of AE1/AE3 (various sources). One laboratory<br />
used CAM5.2, which although not a pan-cytokeratin marker,<br />
was positive in the sample distributed. Twenty-three of the<br />
participating laboratories used some <strong>for</strong>m of automation.<br />
Note on controls: Twenty-five laboratories used cytology<br />
controls, including cell-blocks. All others used histological<br />
sections of appendix, normal colon or normal<br />
colon/colonic adenocarcinoma.<br />
Pan-cytokeratin<br />
Participant Scored 18/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) using this<br />
method.<br />
Method: Ventana iView DAB kit<br />
Automation: Ventana NexES<br />
Buffer and pH: Ventana APK wash buffer<br />
Blockade Type: Ventana blocker solution<br />
Antigen Retrieval: None<br />
Primary Antibody: Biogenex MU-071-UC clones AE1/AE3<br />
dilution 1:200 <strong>for</strong> 30 minutes<br />
Chromogen: Ventana iView DAB <strong>for</strong> 8 minutes
<strong>Immunocytochemistry</strong> — Cytology<br />
Melanoma markers<br />
Participant Scored 18/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) using this<br />
method.<br />
Method: DakoCytomation ChemMate K5001 kit<br />
Automation: DakoCytomation TechMate 500 plus<br />
Buffer and pH: DakoCytomation ChemMate K001 buffer<br />
Blockade Type: DakoCytomation ChemMate K001 solution<br />
Antigen Retrieval: None<br />
Primary Antibody: DakoCytomation HMB45 M0634 dilution<br />
1:5, <strong>for</strong> 60 minutes at room temperature<br />
Chromogen: DakoCytomation ChemMate K5001<br />
DAB <strong>for</strong> 15 minutes<br />
Table 28. Primary Antibody (Melanoma markers)<br />
Antibody Details N %<br />
Biogenex MU 058 UC S100 1 100<br />
DakoCytomation Z0311 S100 40 70<br />
DakoCytomation M0634 (Clone HMB45 ) 34 74<br />
ENZO C34930 HMB45 1 100<br />
Incomplete data 3 100<br />
Other 1 100<br />
Novocastra NCL-HMB45 2 50<br />
Novocastra NCL-Melan A 1 100<br />
Novocastra NCL-S100p 2 0<br />
Ventana 760 2523 S100p 1 0<br />
166<br />
Pan-cytokeratin<br />
Participant Scored 20/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide) using this<br />
method.<br />
Method: DakoCytomation ChemMate K5001 kit<br />
Automation: None<br />
Buffer and pH: DakoCytomation ChemMate K001 buffer<br />
Blockade Type: DakoCytomation ChemMate K001<br />
solution<br />
Antigen Retrieval: None<br />
Primary Antibody: DakoCytomation MNF116 M082 dilution<br />
1:300, <strong>for</strong> 40 minutes at room temperature<br />
Chromogen: DakoCytomation ChemMate K5001<br />
DAB <strong>for</strong> 15 minutes<br />
MAIN TECHNICAL PARAMETERS EMPLOYED BY PARTICIPANTS IN THE CYTOLOGY MODULE<br />
The following tables record the number of participants (N) using each system. The percentage (%) refers to the<br />
proportion of these participants achieving acceptable staining (a score >12/20). For example in the first table,<br />
34 participants used DakoCytomation HMB45 code M0634, of whom 74% achieved acceptable staining.<br />
Table 29. Primary Antibody (pan-cytokeratin)<br />
Antibody Details N %<br />
Biogenex MU071-UC (Clone AE1/AE3) 6 100<br />
Becton Dickinson (CAM 5.2)* 7 100<br />
BMA T1302 1 0<br />
Dakocytomation M0821(Clone MNF116) 35 94<br />
Dakocytomation M 3515 (Clone AE1/AE3) 18 100<br />
Home Made cocktails 2 100<br />
Novocastra NCL-AE1/AE3 3 100<br />
Novocastra NCL-PAN CK 1 100<br />
Incomplete data 3 100<br />
Immunotech 1918 and 1077 (KL1) 3 100<br />
Sigma C2562 (?) 1 0<br />
Ventana 760 2135 (AE1/AE3) 1 100<br />
Zymed 18-0132 (AE1/AE3) 4 100<br />
*Although CAM5.2 is not a pan-cytokeratin antibody participants who used it<br />
were not penalized at this assessment.
Table 30. Pre-treatment<br />
Melanoma PAN CK<br />
Pre-treatment N % N %<br />
DakoCytomation Pronase S2013 1 100 - -<br />
Incomplete data 3 67 1 100<br />
Microwave Oven 8 63 6 100<br />
None 69 75 72 97<br />
Other - - 1 100<br />
Pressure cooker 3 33 2 50<br />
Sigma Chymotrypsin C-4129 - - 1 100<br />
Sigma Protease P8038 - - 1 100<br />
Ventana benchmark CC1 1 0 - -<br />
Ventana Protease 1 - - 2 100<br />
Water bath at 98 o C <strong>for</strong> 40 minutes 1 0 - -<br />
Table 32. Chromogen<br />
Melanoma PAN CK<br />
Chromogen & Supplier N % N %<br />
Biogenex HK 1535K 4 50 4 100<br />
DakoCytomation Envision 5 80 5 100<br />
DakoCytomation K3466 DAB 2 0 2 100<br />
DakoCytomation K5007 10 90 10 70<br />
DakoCytomation K3464 AEC 1 100 1 100<br />
DakoCytomation K3461 AEC 1 0 1 100<br />
DakoCytomation K5001 23 83 23 100<br />
DakoCytomation K5005 4 75 4 100<br />
Incomplete data 2 50 2 100<br />
Lab Vision DAB 3 67 3 67<br />
Other 7 71 7 100<br />
Sigma D5637 DAB 2 50 2 100<br />
Sigma K3468 DAB 6 83 6 100<br />
Ventana Fast red 1 100 1 100<br />
Ventana iView DAB 15 53 15 100<br />
167<br />
<strong>Immunocytochemistry</strong> — Cytology<br />
Table 31. Detection System<br />
Melanoma PAN CK<br />
Type, Supplier & Product Code N % N %<br />
Biogenex Super Sensitive Multi link/<br />
HRP LP000-UL<br />
2 50 2 100<br />
Chemicon HP 1000 1 0 1 100<br />
DakoCytomation ChemMate L.St.Av/<br />
HRP K5001<br />
24 83 24 100<br />
DakoCytomation ChemMate<br />
Envision K5007<br />
11 82 11 73<br />
DakoCytomation ChemMate L.St.Av/<br />
ALP K5005<br />
4 50 4 100<br />
DakoCytomation Duet St.ABC K0492 5 80 5 100<br />
DakoCytomation Envision 7 71 7 100<br />
DakoCytomation LSAB Kit/HRP K0675 3 67 3 100<br />
DakoCytomation K0690 1 0 1 100<br />
Incomplete data 1 100 1 100<br />
LabVision TS 125 HR 2 50 2 100<br />
Other 1 100 1 100<br />
Vector Elite Universal ABC PK6200 4 100 4 100<br />
Vector PK 7200 RTU 2 50 2 100<br />
Vector PK 6100 1 0 1 100<br />
Ventana Basic system 4 0 4 100<br />
Ventana Alk Phos system 3 67 3 67<br />
Ventana iView system 10 70 10 100<br />
Table 33. Automation<br />
Melanoma PAN CK<br />
Instrument & Supplier N % N %<br />
Biogenex Optimax 7 86 7 100<br />
Biogenex Genon MX i6000 2 50 2 100<br />
DakoCytomation Horizon 1 100 1 100<br />
DakoCytomation TechMate 500 13 92 13 92<br />
DakoCytomation Autostainer 17 65 17 94<br />
Incomplete data 1 0 1 100<br />
LabVision Autostainer 5 80 5 100<br />
None 23 78 23 96<br />
Shandon Sequenza 1 0 1 100<br />
Ventana ES 2 0 2 100<br />
Ventana NexES 7 71 7 100<br />
Ventana Benchmark 6 50 6 83<br />
Ventana Gen 11 1 0 1 100
<strong>Immunocytochemistry</strong> — Alimentary Tract<br />
The Alimentary Tract (Pilot) Module<br />
Merdol Ibrahim<br />
Antigens assessed: CD117 (c-KIT)<br />
Material circulated: A composite block comprising of a<br />
Gastro Intestinal Stromal Tumour (GIST) and appendix.<br />
Number of participating laboratories: 50<br />
Guidelines used in the assessment of slides:<br />
SCORE STAINING PATTERN<br />
0 No returns<br />
1 Little or no staining of the GIST or cells of Cajal<br />
2 Very weak demonstration of the GIST or cells<br />
of Cajal<br />
3 Weak demonstration of the GIST or cells of Cajal<br />
4 Good demonstration of the GIST or cells of Cajal<br />
5 Excellent demonstration of the GIST or cells of<br />
Cajal<br />
NB. These are only very general guidelines and marks were deducted <strong>for</strong> such<br />
things as poor localisation of staining or diffuse staining, inappropriate staining<br />
of certain cell types, excessive background staining, excessive counter-stain,<br />
uneven staining or other factors which made interpretation difficult.<br />
Distribution of scores<br />
frequency of returns<br />
Run 65V Cd117 without retrieval on <strong>UK</strong> <strong>NEQAS</strong> Sections<br />
Summary<br />
Scores >12/20 25 (81%)<br />
Scores 10-12/20 4 (13%)<br />
Scores 12/20 34 (78%)<br />
Scores 10-12/20 5 (11%)<br />
Scores 12/20 22 (67%)<br />
Scores 10-12/20 3 (9%)<br />
Scores 12/20 36 (80%)<br />
Scores 10-12/20 7 (16 %)<br />
Scores
Plate 54. Strong staining of mast cells in section of appendix from<br />
<strong>UK</strong> <strong>NEQAS</strong>-ICC section of appendix, however there is also some<br />
background staining present which is particularly noticeable within<br />
crypt epithelial cells.<br />
Plate 56. GIST from the <strong>UK</strong> <strong>NEQAS</strong>-ICC section showing intense and<br />
even staining.<br />
Plate 58. Good demonstration of a GIST from a participant’s In<br />
House section (HIER had been used).<br />
169<br />
<strong>Immunocytochemistry</strong> — Alimentary Tract<br />
Plate 55. Interstitial cell of Cajal, from <strong>UK</strong> <strong>NEQAS</strong>-ICC section,<br />
demonstrating intense staining.<br />
Plate 57. Poor demonstration of mast cells on <strong>UK</strong> <strong>NEQAS</strong>-ICC section,<br />
showing excessive background and non-specific staining.<br />
Plate 59. Poor demonstration of same GIST as that shown in Plate<br />
58. In this case HIER had not been used.
<strong>Immunocytochemistry</strong> — Alimentary Tract<br />
BEST METHODS<br />
CD117<br />
Participant Scored 20/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide), and<br />
20/20 (In House slide) using this method.<br />
Method: DakoCytomation ChemMate K5001<br />
Automation: DakoCytomation TechMate 500 plus<br />
Buffer and pH: DakoCytomation ChemMate K5001<br />
buffer<br />
Blockade Type: DakoCytomation ChemMate K5001<br />
blocking solution<br />
Antigen Retrieval: Pressure cooker to heat 2L citrate<br />
buffer pH6.0 <strong>for</strong> 3 minutes at full<br />
pressure<br />
Primary Antibody: DakoCytomation A4502 polyclonal<br />
c-KIT (dilution and incubation time<br />
were not stated)<br />
Chromogen: DakoCytomation ChemMate K5001<br />
DAB <strong>for</strong> 10 minutes<br />
170<br />
CD117<br />
Participant Scored 20/20 (<strong>UK</strong> <strong>NEQAS</strong>-ICC slide), and<br />
20/20 (In House slide) using this method.<br />
Method: Ventana Benchmark DAB kit<br />
Automation: Ventana Benchmark system<br />
Buffer and pH: Ventana buffer<br />
Blockade Type: Ventana blockade system<br />
Antigen Retrieval: Ventana Cell Conditioning I solution<br />
Primary Antibody: DakoCytomation A4502 polyclonal<br />
Dilution 1:100 <strong>for</strong> 32 minutes at 37 o C<br />
Chromogen: Ventana DAB <strong>for</strong> 8 minutes<br />
MAIN TECHNICAL PARAMETERS EMPLOYED BY PARTICIPANTS IN THE ALIMENTARY TRACT<br />
(PILOT) MODULE<br />
The following tables record the number of participants (N) using each system. The percentage (%) refers to the<br />
proportion of these participants achieving acceptable staining (a score >12/20). For example in the first table,<br />
30 participants used DakoCytomation Polyclonal antibody A4502 of whom 80% achieved acceptable staining using<br />
an antigen retrieval system.<br />
Table 34. Primary Antibody (CD117)<br />
With retrieval Without retrieval<br />
Antibody details N % N %<br />
DakoCytomation A4502 polyclonal 30 80 38 92<br />
Incomplete data 0 0 2 100<br />
NeoMarker RB 1518 0 0 1 0<br />
NeoMarker RB 9038 0 0 1 0<br />
Novocastra NCLCD117 0 0 1 100<br />
Ventana 790 2939 0 0 1 100<br />
Table 35. Pre-treatment<br />
With retrieval Without retrieval<br />
Pre-treatment N % N %<br />
Incomplete data 2 50 - -<br />
Microwave Oven 13 77 n.a. n.a.<br />
Pressure Cooker in Microwave Oven 2 100 n.a. n.a.<br />
Pressure Cooker 10 90 n.a. n.a.<br />
Ventana Benchmark 2 100 n.a. n.a.<br />
Water bath 95-98 o C 1 0 n.a. n.a.<br />
None n.a. n.a. 44 89<br />
n.a. = not applicable
Table 36. Detection System With retrieval Without retrieval<br />
Type, supplier and product code N % N %<br />
DakoCytomation ChemMate K5005 1 100 1 100<br />
DakoCytomation ChemMate K5001 8 88 13 85<br />
DakoCytomation ChemMate – 6 83 8 88<br />
Envision K5007 DAB<br />
Dakocytomation Duet St.ABC K0492 1 0 1 100<br />
DakoCytomation Envision Plus systems 3 67 6 100<br />
DakoCytomation St.ABC/HRP K0377 1 0 1 100<br />
Incomplete data 2 100 2 100<br />
Power Vision DPVB 999 HRP 1 0 0 0<br />
Vision Biosystem D59404 1 100 1 100<br />
Vector Elite ABC PK 6100 1 100 1 100<br />
Vector Elite Universal ABC PK6200 1 100 1 100<br />
Ventana iVIEW system 4 100 7 88<br />
171<br />
Table 37. Chromogen<br />
With retrieval Without retrieval<br />
Chromogen and Supplier N % N %<br />
DakoCytomation Envision Plus kits 3 33 5 100<br />
DakoCytomation K3468 DAB 3 67 3 100<br />
DakoCytomation ChemMate - 8 88 13 85<br />
K5001 DAB<br />
DakoCytomation ChemMate - 1 100 1 100<br />
K5005 Alk phos<br />
DakoCytomation S3000 DAB 1 100 1 100<br />
DakoCytomation ChemMate - 5 80 7 86<br />
Envision K5007 DAB<br />
Table 38. Automation<br />
With retrieval Without retrieval<br />
Instrument and Supplier N % N %<br />
Biogenex Optimax 1 100 2 50<br />
Biogenex Genon MX 6000i 1 100 2 100<br />
DakoCytomation Autostainer 9 67 11 82<br />
DakoCytomation TechMate 500 9 78 15 73<br />
LabVision Autostainer 2 50 1 0<br />
None 4 100 6 100<br />
Ventana Benchmark 3 100 4 75<br />
Vision Biosystem 1 100 1 100<br />
<strong>Immunocytochemistry</strong> — Alimentary Tract<br />
Incomplete data 2 100 2 100<br />
Other 3 67 3 100<br />
Vision Biosystem Bond-x DAB 1 100 1 100<br />
Ventana iVIEW DAB 3 100 6 83
<strong>Immunocytochemistry</strong><br />
Instructions <strong>for</strong> Authors<br />
AIMS<br />
The journal will concentrate on the use of modern<br />
immunocytochemical techniques in prognostic and<br />
diagnostic clinical settings, and clinical research.<br />
Methodological and application based papers will be<br />
equally welcomed. Articles may be:<br />
• Research Reports<br />
• Technical Articles<br />
• Technical Reviews<br />
• Applications Reviews<br />
• Quality Assurance Articles<br />
The main objective of the journal is the timely dissemination<br />
of in<strong>for</strong>mation relevant and valuable to the practitioners<br />
and users of immunocytochemistry.<br />
SUBMISSION OF MANUSCRIPTS<br />
All material submitted <strong>for</strong> publication should be sent to<br />
the Editor-in-Chief:<br />
Mr. Andrew R Dodson<br />
Editor-in Chief<br />
<strong>Immunocytochemistry</strong><br />
Royal Liverpool University Hospital<br />
Liverpool L69 3GA, <strong>UK</strong><br />
Include a covering letter that gives contact details:<br />
name, address, telephone, and e-mail.<br />
Manuscripts should be submitted in English, in duplicate<br />
on A4 paper. All copy must be typed double-spaced<br />
on one side of the paper only. Photographs should be<br />
submitted separately in duplicate as glossy prints. Line<br />
drawings other illustrations, and tables should be<br />
submitted separately in duplicate as one item per<br />
page. Clearly indicate the identity of each item on its<br />
reverse. Indicate within the text where these non-text<br />
items are intended to be placed.<br />
Electronic versions of all items submitted should<br />
accompany the paper ones.<br />
Acceptable <strong>for</strong>mats <strong>for</strong> text are MSWord <strong>for</strong> Windows,<br />
Rich Text Format, and Adobe Acrobat PDF. Photographs<br />
should be submitted as high-resolution JPEG or TIFF files.<br />
In exceptional circumstance high-quality transparencies<br />
will be accepted in place of digital copies. The journal<br />
recognises the utility and importance of colour photomicrographs<br />
to illustrate staining results, and will<br />
make no page charges to authors <strong>for</strong> their inclusion.<br />
<strong>Immunocytochemistry</strong><br />
172<br />
FORMAT<br />
Title: Full title<br />
Authors: Full names of all authors, given in the order<br />
they should appear in the published article; indicate<br />
which is the contact author and insure that full contact<br />
details are given <strong>for</strong> this person.<br />
Summary: A synopsis of the papers contents, brief and<br />
factual, to indicate the full scope of the paper. Avoid<br />
phrases such as ‘…will be discussed’. Length should be<br />
50 to 150 words.<br />
Main body: Full word count (including title, summary,<br />
main body and references) should not exceed 2,000<br />
words. Structure methodological papers in a standard<br />
<strong>for</strong>mat: Introduction, Materials and Methods, Results,<br />
Discussion, Conclusions (Conclusions section is optional).<br />
References: Numbered consecutively as they appear<br />
in the text. Use the following style:<br />
1. Shi SR, Key ME, Kalra KL. Antigen retrieval in <strong>for</strong>malinfixed<br />
paraffin embedded tissues: an enhancement<br />
method <strong>for</strong> immunohistochemical staining based on<br />
microwave oven heating of sections. J Histochem<br />
Cytochem 1991; 39: 741–748<br />
2. Ellis IO. <strong>Immunocytochemistry</strong> in breast pathology. In<br />
Theory and Practice of Histological Techniques (5 th<br />
edn). Bancroft JD, Gamble M (eds). Churchill<br />
Livingstone, London 2002; 499–516<br />
3. Shepherd P, Dean C (eds). Monoclonal antibodies: a<br />
practical approach. Ox<strong>for</strong>d University Press, Ox<strong>for</strong>d;<br />
2000<br />
4. http://www.histopath.ucl.ac.uk/neqas/frame.html<br />
For multiple author references, cite only the first three<br />
authors, followed by et al.<br />
Journal names should be abbreviated using the Index<br />
Medicus standard <strong>for</strong>mat.<br />
Copyright<br />
<strong>UK</strong> <strong>NEQAS</strong>-ICC <strong>for</strong> <strong>Immunocytochemistry</strong> (<strong>UK</strong> <strong>NEQAS</strong>-<br />
ICC) holds the Copyright on all material it publishes in<br />
<strong>Immunocytochemistry</strong>. Author(s) will be required to sign<br />
a Copyright Transfer Agreement prior to publication.<br />
Honorarium<br />
<strong>UK</strong> <strong>NEQAS</strong>-ICC <strong>for</strong> <strong>Immunocytochemistry</strong> will pay an<br />
honorarium to the value of £100 (less tax deducted at<br />
source <strong>for</strong> <strong>UK</strong> residents). This will be made payable to<br />
the lead (first named) author, unless specific written<br />
instructions to the contrary are received at the time of<br />
submission of the paper.