Chemoradiation-Induced Cell Loss in Human Submandibular Glands
Chemoradiation-Induced Cell Loss in Human Submandibular Glands
Chemoradiation-Induced Cell Loss in Human Submandibular Glands
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
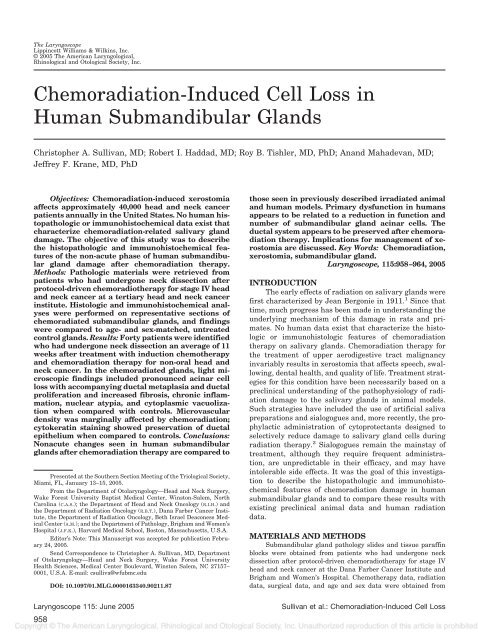
The LaryngoscopeLipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s, Inc.© 2005 The American Laryngological,Rh<strong>in</strong>ological and Otological Society, Inc.<strong>Chemoradiation</strong>-<strong>Induced</strong> <strong>Cell</strong> <strong>Loss</strong> <strong>in</strong><strong>Human</strong> <strong>Submandibular</strong> <strong>Glands</strong>Christopher A. Sullivan, MD; Robert I. Haddad, MD; Roy B. Tishler, MD, PhD; Anand Mahadevan, MD;Jeffrey F. Krane, MD, PhDObjectives: <strong>Chemoradiation</strong>-<strong>in</strong>duced xerostomiaaffects approximately 40,000 head and neck cancerpatients annually <strong>in</strong> the United States. No human histopathologicor immunohistochemical data exist thatcharacterize chemoradiation-related salivary glanddamage. The objective of this study was to describethe histopathologic and immunohistochemical featuresof the non-acute phase of human submandibulargland damage after chemoradiation therapy.Methods: Pathologic materials were retrieved frompatients who had undergone neck dissection afterprotocol-driven chemoradiotherapy for stage IV headand neck cancer at a tertiary head and neck cancer<strong>in</strong>stitute. Histologic and immunohistochemical analyseswere performed on representative sections ofchemoradiated submandibular glands, and f<strong>in</strong>d<strong>in</strong>gswere compared to age- and sex-matched, untreatedcontrol glands. Results: Forty patients were identifiedwho had undergone neck dissection an average of 11weeks after treatment with <strong>in</strong>duction chemotherapyand chemoradiation therapy for non-oral head andneck cancer. In the chemoradiated glands, light microscopicf<strong>in</strong>d<strong>in</strong>gs <strong>in</strong>cluded pronounced ac<strong>in</strong>ar cellloss with accompany<strong>in</strong>g ductal metaplasia and ductalproliferation and <strong>in</strong>creased fibrosis, chronic <strong>in</strong>flammation,nuclear atypia, and cytoplasmic vacuolizationwhen compared with controls. Microvasculardensity was marg<strong>in</strong>ally affected by chemoradiation;cytokerat<strong>in</strong> sta<strong>in</strong><strong>in</strong>g showed preservation of ductalepithelium when compared to controls. Conclusions:Nonacute changes seen <strong>in</strong> human submandibularglands after chemoradiation therapy are compared toPresented at the Southern Section Meet<strong>in</strong>g of the Triological Society,Miami, FL, January 13–15, 2005.From the Department of Otolaryngology—Head and Neck Surgery,Wake Forest University Baptist Medical Center, W<strong>in</strong>ston-Salem, NorthCarol<strong>in</strong>a (C.A.S.); the Department of Head and Neck Oncology (R.I.H.) andthe Department of Radiation Oncology (R.B.T.), Dana Farber Cancer Institute,the Department of Radiation Oncology, Beth Israel Deaconess MedicalCenter (A.M.); and the Department of Pathology, Brigham and Women’sHospital (J.F.K.), Harvard Medical School, Boston, Massachusetts, U.S.A.Editor’s Note: This Manuscript was accepted for publication February24, 2005.Send Correspondence to Christopher A. Sullivan, MD, Departmentof Otolaryngology—Head and Neck Surgery, Wake Forest UniversityHealth Sciences, Medical Center Boulevard, W<strong>in</strong>ston Salem, NC 27157–0001, U.S.A. E-mail: csulliva@wfubmc.eduDOI: 10.1097/01.MLG.0000163340.90211.87Laryngoscope 115: June 2005958those seen <strong>in</strong> previously described irradiated animaland human models. Primary dysfunction <strong>in</strong> humansappears to be related to a reduction <strong>in</strong> function andnumber of submandibular gland ac<strong>in</strong>ar cells. Theductal system appears to be preserved after chemoradiationtherapy. Implications for management of xerostomiaare discussed. Key Words: <strong>Chemoradiation</strong>,xerostomia, submandibular gland.Laryngoscope, 115:958–964, 2005INTRODUCTIONThe early effects of radiation on salivary glands werefirst characterized by Jean Bergonie <strong>in</strong> 1911. 1 S<strong>in</strong>ce thattime, much progress has been made <strong>in</strong> understand<strong>in</strong>g theunderly<strong>in</strong>g mechanism of this damage <strong>in</strong> rats and primates.No human data exist that characterize the histologicor immunohistologic features of chemoradiationtherapy on salivary glands. <strong>Chemoradiation</strong> therapy forthe treatment of upper aerodigestive tract malignancy<strong>in</strong>variably results <strong>in</strong> xerostomia that affects speech, swallow<strong>in</strong>g,dental health, and quality of life. Treatment strategiesfor this condition have been necessarily based on aprecl<strong>in</strong>ical understand<strong>in</strong>g of the pathophysiology of radiationdamage to the salivary glands <strong>in</strong> animal models.Such strategies have <strong>in</strong>cluded the use of artificial salivapreparations and sialogogues and, more recently, the prophylacticadm<strong>in</strong>istration of cytoprotectants designed toselectively reduce damage to salivary gland cells dur<strong>in</strong>gradiation therapy. 2 Sialogogues rema<strong>in</strong> the ma<strong>in</strong>stay oftreatment, although they require frequent adm<strong>in</strong>istration,are unpredictable <strong>in</strong> their efficacy, and may have<strong>in</strong>tolerable side effects. It was the goal of this <strong>in</strong>vestigationto describe the histopathologic and immunohistochemicalfeatures of chemoradiation damage <strong>in</strong> humansubmandibular glands and to compare these results withexist<strong>in</strong>g precl<strong>in</strong>ical animal data and human radiationdata.MATERIALS AND METHODS<strong>Submandibular</strong> gland pathology slides and tissue paraff<strong>in</strong>blocks were obta<strong>in</strong>ed from patients who had undergone neckdissection after protocol-driven chemoradiotherapy for stage IVhead and neck cancer at the Dana Farber Cancer Institute andBrigham and Women’s Hospital. Chemotherapy data, radiationdata, surgical data, and age and sex data were obta<strong>in</strong>ed fromSullivan et al.: <strong>Chemoradiation</strong>-<strong>Induced</strong> <strong>Cell</strong> <strong>Loss</strong>
TABLE I.Age, Sex, Primary Type and Site, Tumor Stage, Induction Chemotherapy, and <strong>Chemoradiation</strong> Data for CRT-SMG Group.Age (y) Sex Primary Type/Site StageInductionChemotherapyConcomitantChemotherapyRadiation(cGy/fractionation)58 M SCCA/Tonsil T3N2bM0 TPF 3 CP 7000/SFX71 M SCCA/Tonsil T4N2cM0 TPF 3 CP 7000/SFX57 M SCCA/BOT T3N3M0 TPF 3 CP 7000/SFX61 M SCCA/Tonsil T4N2cM0 TPF 3 CP 7000/SFX58 M SCCA/Tonsil T2N2bM0 PF 3 CP 7000/SFX63 M SCCA/Tonsil T3N2cM0 PF 3 CP 7000/SFX52 M SCCA/Tonsil T2N3M0 PF 1 T 7230/AFX-CB60 M SCCA/UNK TXN3M0 PF 3 T 7200/AFX-CB57 M SCCA/Tonsil T4N2bM0 PF 3 T 7200/AFX-CB59 F SCCA/Larynx T4N3M0 TPF 3 CP 7000/SFXAFX-CB twice-daily radiation <strong>in</strong> last 2 weeks of therapy; BOT tongue base; CP carboplat<strong>in</strong>um, F 5-fluorouracil; P cisplat<strong>in</strong>um; SFX once-dailyradiation; T taxotere; UNK unknown primary.cl<strong>in</strong>ical records. Radiation doses to the submandibular glandswere calculated from orig<strong>in</strong>al radiation plann<strong>in</strong>g port films andtreatment summary data. Control subjects (C) were then selectedfrom a group of non-irradiated, non-chemotherapy-treated patientswho had undergone neck dissection for the treatment oforal cancer. These patients were then age- and sex-matched tothe chemoradiotherapy group (CRT), creat<strong>in</strong>g control submandibulargland (C-SMG) and chemoradiation-treated submandibulargland (CRT-SMG) groups for comparison.Immunohistochemistry was performed us<strong>in</strong>g the EnvisionPlus/Horseradish Peroxidase system (DakoCytomation Corp.,Carp<strong>in</strong>teria, CA), and mouse monoclonal antibodies to cytokerat<strong>in</strong>s(clone MNF116; 1:700, DakoCytomation), Ki-67 (cloneMIB-1; 1:200, DakoCytomation), CD31 (clone JC70A; 1:40, Dako-Cytomation), and P63 (clone 4A4; 1:400, LabVision Corp., Fremont,CA). Briefly, paraff<strong>in</strong>-embedded sections were <strong>in</strong>cubated <strong>in</strong>hydrogen peroxidase and absolute alcohol for 30 m<strong>in</strong>utes to blockendogenous peroxidase activity. Heat-<strong>in</strong>duced antigen retrievalwas performed <strong>in</strong> a citrate buffer (pH 6.0) prior to <strong>in</strong>cubationwith the P63 and Ki-67 antibodies us<strong>in</strong>g microwave pretreatmentand pressure cooker pretreatment, respectively. Antigen retrievalwas performed by protease digestion for the cytokerat<strong>in</strong> (10 m<strong>in</strong>digestion) and CD31 (20 m<strong>in</strong> digestion) antibodies. Tissue sectionswere subsequently <strong>in</strong>cubated with a primary antibody for 40to 60 m<strong>in</strong>utes at 25°C. After TBS r<strong>in</strong>ses, the tissue was <strong>in</strong>cubatedTABLE II.Age, Sex, Primary Type, Primary Site and Stag<strong>in</strong>g Information forControl Group (C-SMG).Age Sex Primary Type/Site Stage58 M SCCA/Tongue T1N0M072 M CIS/Buccal T1N0M057 M SCCA/Tongue T2N1M060 M SCCA/Tongue T2N1M058 M SCCA/Tongue T1N0M063 M SCCA/Tongue T3N1M052 M SCCA/Tongue T3N1M060 M SCCA/Tongue T2N1M057 M SCCA/Tongue T2N1M059 F SCCA/Tongue T3N1M0CIS carc<strong>in</strong>oma <strong>in</strong> situ; SCCA squamous cell carc<strong>in</strong>oma.us<strong>in</strong>g the Envision Plus secondary antimouse antibody for 30m<strong>in</strong>utes, followed by diam<strong>in</strong>obenzid<strong>in</strong>e for 10 m<strong>in</strong>utes. Appropriatepositive and negative controls (us<strong>in</strong>g normal mouse serum)were sta<strong>in</strong>ed <strong>in</strong> parallel. Ki-67 and P63 antibodies were evaluatedfor nuclear sta<strong>in</strong><strong>in</strong>g, and CD31 and cytokerat<strong>in</strong> antibodies wereassessed for cytoplasmic immunoreactivity.Hematoxyl<strong>in</strong> and eos<strong>in</strong>–sta<strong>in</strong>ed sections were analyzedqualitatively and quantitatively for changes <strong>in</strong> the ratio of serousto muc<strong>in</strong>ous cells (S:M), degree of <strong>in</strong>flammation (CI), fibrosis (F)and ga<strong>in</strong> or loss of ac<strong>in</strong>ar cells (A), <strong>in</strong>tercalated duct cells (ICD),striated duct cells (SD), excretory duct cells (ED), and adiposecells (Ad) <strong>in</strong> the CRT-SMG and the C-SMG groups. Quantitativeestimates of the percentage of epithelial cells sta<strong>in</strong><strong>in</strong>g for cytokerat<strong>in</strong>sand P63 were performed; cell proliferation <strong>in</strong>dices (Ki-67) and microvessel density (CD31) were averaged from counts offive random high-power fields (field size 0.173 mm 2 ; 400 X) <strong>in</strong>CRT-SMG and C-SMG tissue. The data from the C-SMG andCRT-SMG groups were then compared to each other and to historicaldata <strong>in</strong> animal and human studies. All patient data acquisitionwas overseen by the Brigham and Women’s InstitutionalReview Board and was HIPPA compliant.TABLE III.Summary of Procedures Used to Obta<strong>in</strong> <strong>Submandibular</strong> Tissue,Number of Days between Completion of <strong>Chemoradiation</strong> Therapyand Histopathologic Analysis of <strong>Submandibular</strong> <strong>Glands</strong>, andRadiation Dose to the <strong>Submandibular</strong> <strong>Glands</strong>.Procedure Days Out from CRT XRT Dose to SMG (cGy)R MRND 77 7000R MRND 66 7000L RND 72 5600L RND 87 7000R RND 43 5670L RND 107 5580L MRND 123 7200R RND 74 7200R MRND 66 5000L MRND 42 5580CRT chemoradiation therapy; L left; MRND modified radicalneck dissection; R right; RND radical neck dissection; SMG submandibulargland; XRT radiation therapy.Laryngoscope 115: June 2005Sullivan et al.: <strong>Chemoradiation</strong>-<strong>Induced</strong> <strong>Cell</strong> <strong>Loss</strong>959
TABLE IV.Control <strong>Submandibular</strong> Gland Immunosta<strong>in</strong><strong>in</strong>g and Histologic Data.Cytokerat<strong>in</strong> (%) Ki-67 (cells/HPF) P63 (%) CD31 (vessels/HPF) S:M F CI30 4 10 36 95:5 0 075 2 15 31 90:10 30 2 10 19 80:20 0 015 1 10 25 75:25 0 20 1 10 32 100:0 0 030 2 10 30 80:20 0 060 4 10 34 60:40 0 045 20 25 46 60:40 020 5 12 32 80:20 0 20 6 10 30 90:10 0 0CD31 number of vessels per high-power field sta<strong>in</strong><strong>in</strong>g for CD31; CI chronic <strong>in</strong>flammation, scale of 0 to ; Cytokerat<strong>in</strong> % of epithelial cells sta<strong>in</strong><strong>in</strong>gfor cytokerat<strong>in</strong>; F fibrosis, scale of 0 to ; Ki-67 number of cells per high power field sta<strong>in</strong><strong>in</strong>g for Ki-67; P63 % of cells sta<strong>in</strong><strong>in</strong>g for P63; S:M ratioof serous to muc<strong>in</strong>ous cells.RESULTSForty patients were identified who had undergoneprotocol-driven <strong>in</strong>duction chemotherapy followed by chemoradiationtherapy for stage IV non-oral squamous cellcarc<strong>in</strong>oma. From this group, 11 patients were identifiedwhose radiation port films were available for review. Atotal of 12 submandibular glands from 11 patients wereidentified for histopathologic and immunohistochemicalanalysis. Of these, 10 were able to be age- and sexmatchedto control subjects. Age, sex, primary tumor site,TNM stage, chemotherapy, and radiation data are summarized<strong>in</strong> Table I and Table II. There were n<strong>in</strong>e male andone female subjects. Average age was 60 years. All patientshad stage IV disease of the tongue base, tonsil, orlarynx. Patients received cisplat<strong>in</strong>, 5-fluorouracil, andtaxotere (TPF) or cisplat<strong>in</strong> and 5-fluorouracil (PF)–basedchemotherapy. <strong>Submandibular</strong> gland specimens were distributedequally between left and right sides. Radiationdoses to the submandibular glands varied between 5000cGy and 7200 cGy with an average dose of 6283 cGy. Thetime from the end of chemoradiation therapy to removal ofthe study glands (CRT-SMG) dur<strong>in</strong>g neck dissectionranged between 42 and 123 days, with a median of 73 days(10 wk) and an average of 76 days (11 wk) (Table III).The C-SMG group specimens showed normalappear<strong>in</strong>gsubmandibular tissue <strong>in</strong> all cases (Table IV,Fig. 1) In the CRT-SMG group histopathologic f<strong>in</strong>d<strong>in</strong>gs<strong>in</strong>cluded severe loss of both serous and muc<strong>in</strong>ous ac<strong>in</strong>arcells and secretory granules. There was moderate to severechronic <strong>in</strong>flammation and fibrosis <strong>in</strong> all CRT-SMGspecimens. (Fig. 2, Table V). In CRT-SMG specimens,cytokerat<strong>in</strong> (PAN-K) immunosta<strong>in</strong><strong>in</strong>g of epithelial cellswas <strong>in</strong>creased by a factor of 2.2 correspond<strong>in</strong>g to themorphological appearance of ac<strong>in</strong>ar cell loss with accompany<strong>in</strong>gductal cell metaplasia and ductal proliferation.<strong>Cell</strong> proliferation as assessed by Ki-67 immunosta<strong>in</strong><strong>in</strong>gwas <strong>in</strong>creased by a factor of 3.6. P63 sta<strong>in</strong><strong>in</strong>g was <strong>in</strong>creasedby a factor of 2.9 and endothelial cell (CD31)sta<strong>in</strong><strong>in</strong>g was <strong>in</strong>creased by a factor of 1.4. (Table V, VI;Figs. 3, 4, 5, 6).Fig. 1. Representative, normal human submandibular gland fromthe C-SMG group. Note the abundant serous ac<strong>in</strong>i with zymogengranules, normal muc<strong>in</strong>ous ac<strong>in</strong>ar cells, and ductal elements.Fig. 2. Chemoradiated submandibular gland. Note severe loss ofserous and muc<strong>in</strong>ous ac<strong>in</strong>ar cells, ductal metaplasia and proliferation,periductal fibrosis, and lymphoplasmacytic <strong>in</strong>filtration.Laryngoscope 115: June 2005960Sullivan et al.: <strong>Chemoradiation</strong>-<strong>Induced</strong> <strong>Cell</strong> <strong>Loss</strong>
TABLE V.<strong>Chemoradiation</strong>-Treated <strong>Submandibular</strong> Gland Immunosta<strong>in</strong><strong>in</strong>g and Histologic Data.Cytokerat<strong>in</strong> (%) Ki-67 (cells/HPF) P63 (%) CD31 (vessels/HPF) S:M F CI100 19 50 51 0:0 90 19 25 26 S:0 90 10 30 0 0:0 , AI100 4 50 22 0:0 70 35 40 43 0:100 95 14 40 22 10:90 60 21 30 42 S:0 70 18 25 46 0:100 100 20 25 46 S:0 100 19 30 43 0:0 , AIAI focal acute <strong>in</strong>flammation; CD31 number of vessels per high-power field sta<strong>in</strong><strong>in</strong>g for CD31; CI chronic <strong>in</strong>flammation, scale of 0 to ;Cytokerat<strong>in</strong> % of epithelial cells sta<strong>in</strong><strong>in</strong>g for cytokerat<strong>in</strong>; F fibrosis, scale of 0 to ; Ki-67 number of epithelial cells per high-power field sta<strong>in</strong><strong>in</strong>g for MIB-1;P63 % of cells sta<strong>in</strong><strong>in</strong>g for P63; S:0 rare serous cells; S:M ratio of serous to muc<strong>in</strong>ous cells.DISCUSSIONThe exist<strong>in</strong>g experimental data on salivary gland radiosensitivityand the theoretical mechanism by which salivarytissue damage occurs dur<strong>in</strong>g head and neck radiationare well described <strong>in</strong> animal and primate models. It is generallyagreed that radiation causes lipid peroxidation that iscatalyzed by heavy metal ions present <strong>in</strong> the granules ofserous cells. This process leads to membrane disruption andrelease of cellular enzymes, which then cause autolysis andcell death. It is hypothesized that this damage may also<strong>in</strong>clude reproductive death of ac<strong>in</strong>ar progenitor cells. 3–5 Inhumans, the major salivary glands typically lie with<strong>in</strong> thehead and neck radiation fields, and the amount of glandulardamage is believed to be dependent on radiation dose, fractionation,latency of treatment, the premorbid functionalstate of the glands, and the ratio of serous to muc<strong>in</strong>ous cellswith<strong>in</strong> an <strong>in</strong>dividual gland. 5 Cl<strong>in</strong>ical studies have shownboth qualitative and quantitative changes <strong>in</strong> the saliva ofpatients undergo<strong>in</strong>g head and neck radiation, but data onthe accompany<strong>in</strong>g histopathologic changes is lack<strong>in</strong>g. 6,7Data on chemoradiation-<strong>in</strong>duced histopathologic changes <strong>in</strong>either human or animal models is nonexistent. We chose toacquire submandibular tissue from patients who had previouslyundergone protocol-driven treatment because this populationwas essentially homogeneous relative to primary sitetreated and was easily accessible through our protocol database,and because retrospective data acquisition would notrequire any alteration of the cancer treatment plan. Werecognize that prospective data collection could allow forbetter control of variables such as primary site treated, thetim<strong>in</strong>g of concomitant chemotherapy, the agents used, thedose and tim<strong>in</strong>g of radiation and control of the time periodbetween the last dose of radiation and the removal of submandibulargland specimens. It is conceivable that patientscould be enrolled <strong>in</strong> a protocol that would require neck dissectionat a def<strong>in</strong>ed number of weeks after chemoradiationtherapy; however, patients show different rates of heal<strong>in</strong>gand variable nutritional statuses after chemoradiotherapyand not all patients will be ready to undergo surgery at thetime def<strong>in</strong>ed by such a protocol. The logistics of patienttravel and operat<strong>in</strong>g room schedul<strong>in</strong>g would make protocolmanagement problematic and could potentially impact cancertreatment outcome unfavorably. It was our objective toidentify histopathologic and immunohistochemical changesthat are seen after chemoradiation therapy for non-oral cancersof the head and neck, to compare these f<strong>in</strong>d<strong>in</strong>g to thoseseen <strong>in</strong> radiation-<strong>in</strong>duced models, and to discuss the impactof these f<strong>in</strong>d<strong>in</strong>gs on exist<strong>in</strong>g and potential treatment optionsfor xerostomia.Only one human study exists that classifies thehistopathologic and immunohistochemical changes tothe salivary glands after therapeutic radiation for headand neck cancer. 4 In this study, radiation damage wasanalyzed us<strong>in</strong>g quantitative estimates of the degree ofTABLE VI.Average Values for Quantitative Estimates of Immunosta<strong>in</strong><strong>in</strong>g Patterns and Histopathologic F<strong>in</strong>d<strong>in</strong>gs <strong>in</strong> Control vs. Chemoradiated<strong>Submandibular</strong> <strong>Glands</strong>.*Cytokerat<strong>in</strong> (%) Ki-67 (cells/HPF) P63 (%) CD31 (vessels/HPF) S:M F CIC-SMG 40 5 12 30 81:19 CRT-SMG 88 18 35 42 1:1 RIF 2.2 3.6 2.9 1.4 — — —*Note high relative <strong>in</strong>crease factor (RIF) across all immunosta<strong>in</strong>ed specimens <strong>in</strong> the chemoradiation treated group.CD31 number of vessels per high-power field sta<strong>in</strong><strong>in</strong>g for CD31; CI chronic <strong>in</strong>flammation, scale of 0 to ; CRT-SMG chemoradiation-treatedsubmandibular gland group; C-SMG control submandibular gland group; F fibrosis; Ki-67 number of epithelial cells per high-power field sta<strong>in</strong><strong>in</strong>g for Ki-67;PAN-K % of epithelial cells sta<strong>in</strong><strong>in</strong>g for cytokerat<strong>in</strong>; P63 % of cells sta<strong>in</strong><strong>in</strong>g for P63; RIF relative <strong>in</strong>crease factor of immunosta<strong>in</strong>ed cells; S:M ratio of serousto muc<strong>in</strong>ous cells.Laryngoscope 115: June 2005Sullivan et al.: <strong>Chemoradiation</strong>-<strong>Induced</strong> <strong>Cell</strong> <strong>Loss</strong>961
Fig. 3. Cytokerat<strong>in</strong> immunosta<strong>in</strong><strong>in</strong>g of CRT-SMG (A) and C-SMG(B). Note <strong>in</strong>tense cytokerat<strong>in</strong> sta<strong>in</strong><strong>in</strong>g of the treated gland with arelative decrease <strong>in</strong> ac<strong>in</strong>ar tissue when compared to the controlspecimen.Fig. 4. Ki-67 proliferation immunosta<strong>in</strong><strong>in</strong>g of CRT-SMG (A) andC-SMG (B). Note the relative <strong>in</strong>crease <strong>in</strong> Ki-67 sta<strong>in</strong><strong>in</strong>g cells <strong>in</strong> theCRT-treated specimen.cellular and tissue damage; the degree of damage wasthen classified by severity <strong>in</strong>to three stages. These datadid not <strong>in</strong>clude the radiation doses or latency of radiationtherapy. Our histopathologic data correlate wellwith this stag<strong>in</strong>g system and <strong>in</strong> all cases would be bestdescribed as stage III (most severe), the chief features ofwhicharehigh-gradeparenchymalreductionwithlymphocytic<strong>in</strong>filtrate, ductal proliferation, periductal fibrosis,andvascularsclerosis.Withtheadditionofweeklychemotherapyto radiation doses between 5000 cGy and 7200cGy, we observed severe and equal loss of both serousand muc<strong>in</strong>ous ac<strong>in</strong>ar cells and near complete loss ofsecretory granules between 42 and 123 days posttreatment.These f<strong>in</strong>d<strong>in</strong>g are contrasted to rodent andprimate data <strong>in</strong> which zymogen granule–laden serousac<strong>in</strong>ar cells are considered to be more sensitive to radiationthan muc<strong>in</strong>ous cells and ductal structures. 3,8 Ourdata showed consistent severe loss of both cell types across awide range of radiation doses with complete reversal of theserous to muc<strong>in</strong>ous cell ratio, suggest<strong>in</strong>g that the addition ofchemotherapy may have led to <strong>in</strong>creased ac<strong>in</strong>ar cell loss ofboth types when compared with radiation alone. This likelyLaryngoscope 115: June 2005962reflects the known tissue sensitiz<strong>in</strong>g effect of chemotherapythat is characterized by greater cell loss <strong>in</strong> general dur<strong>in</strong>gradiation therapy.Immunohistochemical markers for cytokerat<strong>in</strong>, P63,Ki-67, and CD31 were employed <strong>in</strong> this study to analyzecellular changes <strong>in</strong> a semiquantitative manner. Cytokerat<strong>in</strong>is an <strong>in</strong>termediate filament prote<strong>in</strong> that makes up acritical component of <strong>in</strong>tracellular mechanical support forepithelial cells. Increased cytokerat<strong>in</strong> expression <strong>in</strong> ratsubmandibular cells that have received greater than 40Gy correlated with morphologic changes that were believedto represent irreversible damage to the salivaryglands 4 to 6 months after radiation. 9 In our CRT-SMGspecimens, cytokerat<strong>in</strong> sta<strong>in</strong><strong>in</strong>g was <strong>in</strong>creased by a factorof 2.2 over control specimens and was seen primarily <strong>in</strong>association with ductal epithelium. Morphologically, thesef<strong>in</strong>d<strong>in</strong>gs corresponded to a loss of ac<strong>in</strong>ar cells with accompany<strong>in</strong>gductal proliferation. These alterations would beassociated with a potentially irreversible ac<strong>in</strong>ar cell lossand decreased function of the gland.The <strong>in</strong>creased cytokerat<strong>in</strong> sta<strong>in</strong><strong>in</strong>g seen <strong>in</strong> CRT-SMGspecimens was accompanied by <strong>in</strong>creased sta<strong>in</strong><strong>in</strong>g for Ki-Sullivan et al.: <strong>Chemoradiation</strong>-<strong>Induced</strong> <strong>Cell</strong> <strong>Loss</strong>
Fig. 5. P63 immunosta<strong>in</strong><strong>in</strong>g of CRT-SMG (A) and C-SMG (B). Notethe <strong>in</strong>crease <strong>in</strong> P63-positive cells <strong>in</strong> the CRT-treated gland.Fig. 6. CD31 immunosta<strong>in</strong><strong>in</strong>g of CRT-SMG (A) and C-SMG (B). Noteslightly more extensive sta<strong>in</strong><strong>in</strong>g of endothelial-l<strong>in</strong>ed lum<strong>in</strong>al structures<strong>in</strong> CRT-treated specimens.Laryngoscope 115: June 200567. Ki-67 is a proliferation-associated antigen that hasbeen used as a marker for sites of cellular proliferation <strong>in</strong>numerous tissues, <strong>in</strong>clud<strong>in</strong>g salivary gland. 10 Topographiclocalization and quantification of Ki-67 associatedcellular proliferation <strong>in</strong> normal human salivary glandshas demonstrated basel<strong>in</strong>e proliferative activity <strong>in</strong> basal,<strong>in</strong>tercalated, and ac<strong>in</strong>ar cells and lower proliferative rates<strong>in</strong> myoepithelial and oxyphilic cells. The exact mechanismof physiologic ductal regeneration and metaplasia has notbeen established, but regeneration from an uncommittedstem cell population has long been favored. 11 Based onthese data, Ki-67 sta<strong>in</strong><strong>in</strong>g <strong>in</strong> our study may representeither normal or pathologic attempts by all or some celltypes to regenerate normal epithelium from undamagedprogenitor cells after chemoradiation therapy.It is possible that a certa<strong>in</strong> number of progenitor cellsrema<strong>in</strong> after radiation or chemoradiation therapy. P63has been shown to sta<strong>in</strong> a population of progenitor stemcells <strong>in</strong> squamous epithelium and has been shown to be amarker of myoepithelial differentiation <strong>in</strong> salivary glandand breast tissue. 12–14The comb<strong>in</strong>ed Ki-67 and P63 immunosta<strong>in</strong><strong>in</strong>g results<strong>in</strong> our study may suggest both myoepithelial and progenitorcell attempts at regeneration and proliferation. Furtherstudy <strong>in</strong> human and animal models is needed to provethis concept.It is ac<strong>in</strong>ar cell loss and subsequent failure to regenerateac<strong>in</strong>ar structures after radiation or chemoradiationtherapy that ultimately results <strong>in</strong> the cl<strong>in</strong>ical condition ofxerostomia. The additional loss of blood flow to the fibrotic,end-stage gland further limits the stimulated flowof saliva from any rema<strong>in</strong><strong>in</strong>g ac<strong>in</strong>i. Precl<strong>in</strong>ical and cl<strong>in</strong>icalstrategies for prevent<strong>in</strong>g xerostomia have been designedto limit cell loss and have used agents that degranulateserous cells, stimulate progenitor cell growth, chelateheavy metals, or scavenge free radicals. Modulated radiationstrategies have attempted to shield the salivaryglands from radiation and thus prevent cell loss. 4 Thedata presented <strong>in</strong> our study show preservation of theductal system after chemoradiation therapy and thereforea novel approach to xerostomia could be to regenerateac<strong>in</strong>ar cells rather than risk undertreat<strong>in</strong>g disease to preserveac<strong>in</strong>ar cells. The CD31 immunosta<strong>in</strong><strong>in</strong>g data <strong>in</strong> ourstudy showed that endothelial cell sta<strong>in</strong><strong>in</strong>g was actuallymodestly <strong>in</strong>creased after therapy, suggest<strong>in</strong>g that theremay be adequate vascularity <strong>in</strong> the salivary bed to supportSullivan et al.: <strong>Chemoradiation</strong>-<strong>Induced</strong> <strong>Cell</strong> <strong>Loss</strong>963