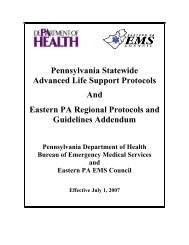
PROTOCOLS PART 2 work copy - Eastern EMS Council
PROTOCOLS PART 2 work copy - Eastern EMS Council
PROTOCOLS PART 2 work copy - Eastern EMS Council
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
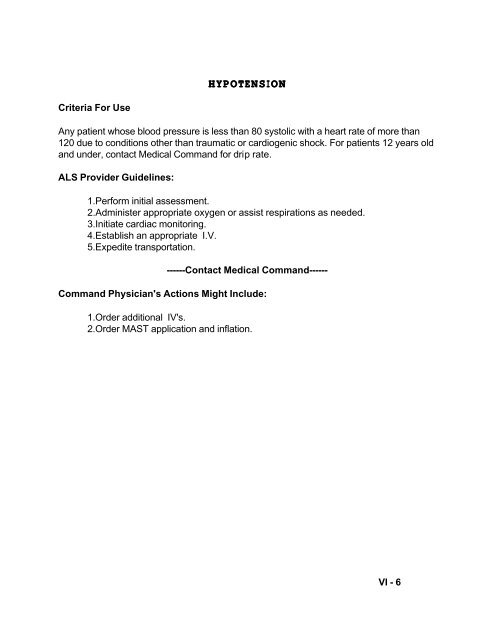
HYPOTENSIONCriteria For UseAny patient whose blood pressure is less than 80 systolic with a heart rate of more than120 due to conditions other than traumatic or cardiogenic shock. For patients 12 years oldand under, contact Medical Command for drip rate.ALS Provider Guidelines:1.Perform initial assessment.2.Administer appropriate oxygen or assist respirations as needed.3.Initiate cardiac monitoring.4.Establish an appropriate I.V.5.Expedite transportation.------Contact Medical Command------Command Physician's Actions Might Include:1.Order additional IV's.2.Order MAST application and inflation.VI - 6
ALS Protocol Assessments and Procedures 7009.02 ALS - AdultPATIENT PRESENTING WITH A GENERAL IMPRESSION OF SERIOUS ILLNESSCriteria:A. A medical or trauma patient who appears to be seriously ill or who presents with anypotentially life threatening symptoms, but does not meet the criteria established for anyother protocols.Exclusion Criteria:System Requirements:A. Size appropriate oxygen delivery equipment and IV materials.Treatment:A. All Patients1. Universal precautions, BSI2. Scene safety3. Perform initial survey, resuscitate as needed.4. Airway managementB. Adult Patient1. Administer appropriate oxygen2. Initiate cardiac monitoring. 13. Initiate an appropriate IV.4. Administer bolus of 500 ml normal saline or lactated ringers if systolic BP 90.4. Contact Medical Command 2Possible Medical Command Orders:A. Promethazine (Phenergan) 12.5 mg if nausea and vomiting occur.B. Alter flow of oxygen.C. Alter fluid therapy.D. Additional ALS procedures as required.Notes: 1 If a 12 lead EKG is performed, a <strong>copy</strong> of the EKG must be presented to theemergency department physician upon arrival at the facility or before departure from thefacility.2The ALS practitioner should continue to monitor the patient’s condition andimmediately initiate the appropriate ALS treatment protocol as the patient’s conditionchanges and contact medical command.Performance Parameters:A. The protocol is applied to appropriate patients.B. Oxygen is applied in every caseVI – 6aApproved DOH 4/04 Page 1 of 1ALS Protocol Assessments and Procedures 8031.02 ALS Adult/Peds
POISONING/OVERDOSECRITERIA:A. Patient whose level of consciousness is altered with confirmed or suspected overdose. 1EXCLUSION CRITERIA:A.SYSTEM REQUIREMENTS:PROCEDURE:A. All Patients:1. Open and maintain open airway.2. Administer Oxygen at 10-15 lpm via non-rebreather mask, assist ventilation ifnecessary.3. Initiate cardiac monitoring. 24. Initiate an appropriate IV.5. Determine blood glucose level if the patient has an altered level of consciousness.6. Administer 25 g of D50 if the glucose level is less than 60. If no IV can beestablished, give 1 mg Glucagon IM.7. If the glucose level is greater than 60 or if there is no improvement after D50,administer Narcan (Naloxone) up to 2.0 mg IV or intranasally via atomizer. 38. If the patient needs to be intubated, 2.0 mg Narcan can be given via theendotracheal tube.9. Contact medical command.Possible Medical Command Orders:A. Additional D50 IVB. If no airway compromise is expected, activated charcoal with sorbitol (without sorbital forpediatric patients) 1 g/kg mixed in easily tolerated fluid (minimum 10 g, maximum 75 g)Note:1 Altered level of consciousness could be a sign of head trauma, CVA or hypoxia. In a child< 12 years of age, administer D25, 0.5 – 1 g/kg if dextrose is indicated.2 If a 12 lead EKG is performed, a <strong>copy</strong> of the EKG must be presented to the emergencydepartment physician upon arrival at the facility or before departure from the facility.3 Anticipate rapid increase in level of consciousness post Narcan administration for narcoticoverdoses. Consider practitioner safety.VI – 7Approved DOH 4/04 Page 1 of 1
ALS Protocol Assessments and Procedures 7007.02 ALS - AdultSEIZURESCriteria:A. A patient with a history of seizures or who is in a seizure stateExclusion Criteria:System Requirements:A. Intranasal administration device if approved by service medical directorTreatment:C. All Patients1. Universal precautions, BSI2. Scene safety3. Perform initial survey, resuscitate as needed.4. Airway managementD. Adult Patient1. Administer appropriate oxygen2. Initiate cardiac monitoring.3. Initiate appropriate IV and determine blood glucose levela. If the patient is not a known seizure patient or if the patient is diabetic and thereading is less than 60, give 25 g D50 IV. If the blood glucose level is less than 60and no IV can be established, administer 1 mg Glucagon IM.b. If unable to initiate IV, give Diazepam (Valium) 0.3-0.5 mg/kg) to a maximum of 10mg rectally. (See Administration of Rectal Medication Specific Protocol Page VII –18)4. If the patient has a known seizure history or has had more than one generalizedseizure and is in a seizure state upon arrival of ALS or has been in a seizure forlonger than 5 minutes, titrate Diazepam (Valium) 1-5 mg, not to exceed 5 mg withoutcontacting medical command5. Be prepared to manage the airway.6. Contact Medical Command.Possible Medical Command Orders:A.. D 50 W IVB.. Administration of Midazolam 1-4 mg, titrated to effect up to dose of 0.1 mg/kg (0.1 ml/kg)slow IVP or IMC. If no IV can be established, may order intranasal or intramuscular midazolam 0.2 mg/kg.Notes:Performance Parameters:A. The protocol is applied to appropriate patients.B. Oxygen is applied in every case.C. Appropriate documents are completed for the administration of controlled substances.VI - 8Approved DOH 4/04 Page 1 of 1
SHOCK - CARDIOGENICCriteria For UsePatient with inadequate perfusion suspected to be cardiac in originALS Provider Guidelines:1. Perform initial survey - resuscitate if needed2. Administer appropriate oxygen3. Initiate cardiac monitoring4. Initiate an appropriate I.V.------Contact Medical Command------Command Physician’s Actions Might Include:1. Order dopamine drip (see specific protocol section)2. Order fluid challengeVI - 9
SYNCOPECriteria For UsePatients who have experienced a total loss of consciousness (fainting) and have recoveredto a conscious stateALS Provider Guidelines:1. Perform initial survey - resuscitate if needed2. Administer appropriate oxygen3. Initiate cardiac monitoring4. Initiate an appropriate I.V.5. Draw blood sugar; determine blood glucose level.6. If patient is hypoglycemic (blood glucose level of 60 or less), administer 12.5 gor 25 cc of D50. If no I.V. can be established, administer 1 mg Glucagon IM.------Contact Medical Command------Command Physician's Actions Might Include:1. Order change in fluid administration (type and rate)2. Order additional D503. If IV access is not available, may order .5 - 1 mg glucagon dissolved in 1 mldiluent administered IM4. If no response within 15 minutes, may order additional administration ofglucagon.NOTE - So-called "near syncope" patients need command physician consultation for ALSskillsRevised 7/95VI - 10
UNCONSCIOUS PATIENT /ALTERED LOCCriteria For UseManagement of a patient unconscious in the A.V.P.U. scale for which the cause is notdeterminedALS Provider Guidelines:1. Perform initial survey - resuscitate as needed2. Administer appropriate oxygen3. Initiate cardiac monitoring4. Initiate an appropriate I.V. - draw blood for glucose determination.5. If patient is hypoglycemic, administer 25 g (50 cc) D50W. If no I.V. can beestablished, and blood glucose level is 60 or less, administer 1 mg GlucagonIM.6. If there is no response after two minutes, administer 2.0 mg Narcan. If no I.V.can be established, give 2 mg Narcan IM.7. If the patient needs to be intubated, 2.0 mg Narcan may be given via theendotracheal tube.------Contact Medical Command------Command Physician's Actions Might Include:1. Order additional glucose2. If I.V. access is not available, may order .5 - 1 mg. glucagon dissolved in 1 mldiluent and administered IM.3. If no response within 15 minutes, may order additional administration ofglucagon.Revised 11/96VI - 11
SECTION VIITRAUMA RELATED PROBL<strong>EMS</strong>
ALS ProtocolCriteria:A. A patient with a moderate or critical burn 1Exclusion Criteria:A. Minor burnsB. Hypotension (systolic BP< 100)System Requirements:Trauma and Environmental 6071.02 ALS - AdultThermal BurnsTreatment:E. All Patients1. Universal precautions, BSI2. Scene safety3. Perform initial survey, resuscitate as needed.4. Make transport decisions.5. Airway managementF. Adult Patient1. Administer appropriate oxygen.2. Treat burns appropriately.3. Initiate cardiac monitoring.4. Initiate an appropriate IV (consider Lactated Ringers) in a proximal site, 500 ml/hr.5. Administer 0.05 mg/kg Morphine Sulfate (Maximum of 5 mg) slow IV, titrated to reliefof pain if systolic BP 110 mm Hg.6. Contact medical command via MedCom immediately.Possible Medical Command Orders:A. IntubationB. Alter transport destination.C. Alter transport mode.D. Alter IV rate.Notes: 1 Moderate burn – full thickness covering 2%-10% of the body (excluding hands, face andneck, feet, genitals); partial thickness covering 15%-30%; superficial covering >50%Critical burn – full or partial thickness burn of the face and neck, hands, feet or genitals;full thickness burns covering >10%; partial thickness covering >30%; burns complicatedby dyspnea, illness or associated trauma; circumferential burns; moderate burns inpediatric and elderly patientsPerformance Parameters:A. The protocol is applied to appropriate patients.B. Oxygen is applied in every caseC. Appropriate documents are completed for the administration of morphine sulfate.D. All cases with use of Morphine Sulfate under standing orders must be reviewed by theservice medical director.E. Patient care reports for all uses of Morphine Sulfate under standing orders must be sent tothe <strong>EMS</strong> <strong>Council</strong> office within 24 hours of the call.Approved DOH 4/04 Page 1 of 1SHOCK - TRAUMATIC/HYPOVOLEMIC
Criteria For UsePatient involved in a traumatic episode with hypovolemia caused by suspected or evidentblood loss resulting in inadequate perfusion.ALS Provider Guidelines:1. Perform initial survey - resuscitate if needed2. Administer appropriate oxygen3. Make decision concerning hospital destination and method of transport as soonas possible4. Without delaying transport, establish at least one I.V. wide open5. MAST are rarely used but may be considered for:a. Long bone extremity splinting 20-25 mm Hgb. Pelvic fractures 20-25 mm Hg------Contact Medical Command------Command Physician's Actions Might Include:1. Alter destination or method of transfer2. Alter fluid administration3. Alter MAST usageRevised 11/96VII -2
TRAUMA - MECHANISM OF INJURYCriteria For UsePatient involved in a traumatic episode with vital signs within the normal range (Step I -Trauma Guidelines) but meets the criteria of (Step II - Anatomy/Mechanism of Injuryrequiring Trauma Center destination)ALS Provider Guidelines:1. Perform initial survey - resuscitate if needed2. Administer appropriate oxygen3. Make decision concerning hospital destination (trauma center) and method oftransport as soon as possible4. Without delaying transport or while arranging aeromedical transport as per#3, establish one appropriate I.V. run at 200 cc/hr.5. MAST are rarely used but may be considered for:a. Long bone extremity splinting 20-25 mm Hgb. Pelvic fractures 20-25 mm Hg------Contact Medical Command------Command Physician=s Actions Might Include:1. Alter destination or method of transfer2. Alter fluid administration3. Alter MAST usageRevised 11/9111/96VII - 3
ALS Protocol Pain Management 2003.02 ALS-AdultPAIN MANAGEMENTInclusion Criteria:A. A patient in significant pain due to a suspected long bone fracture or limb deformity.Exclusion Criteria:A. Major trauma to the head, chest, abdomen or pelvisB. Alcohol intoxicationC. Drug intoxicationD. COPDE. Hypotension (systolic < 100 mm Hg)F. Respiratory compromise.G. Allergy to MorphineH. Abdominal pain due to trauma or medical conditionSystem Requirements:Treatment:A. Adult Patient1. Universal precautions; BSI2. Scene Safety3. Patient/Airway Assessment4. Administer oxygen.5. Treat injuries appropriately.6. Attach pulse oximetry.7. Initiate cardiac monitoring.8. Initiate appropriate IV.9. Administer 0.05 mg/kg (Maximum of 5 mg) Morphine Sulfate IV, titrated to painrelief if systolic BP 110.10. Contact medical command via MedCom immediately.Possible Medical Command Orders:A. Additional Morphine Sulfate 2-5 mg/dose IV.B. Narcan if respiratory complications appear.Notes:A. All uses of Morphine Sulfate under standing orders must be reviewed by the ALSService Medical Director.B. Patient care reports for all uses of Morphine Sulfate under standing orders must be sentto the <strong>EMS</strong> <strong>Council</strong> Office within 24 hours of the call.____________________________________________________________________________Performance Parameters:A. Pulse oximeter used to monitor adequate oxygenation of patient.B. Use of Morphine Sulfate appropriately documented.Approved DOH 4/04 Page 1 of 1
ALS Protocol Trauma & Environmental 6025.02 ALS - AdultTension PneumothoraxCriteria:A. A patient with chest trauma, who has absent breath sounds in one or both lungs uponventilation, who is hemodynamically unstable with a systolic blood pressure of 90 orless and has an altered level of consciousness.Exclusion Criteria:A. A patient with absent breath sounds due to medical reasons.B. Pulse ox reading greater than 90.System Requirements:A. 14 or 16 gauge 2” angiocathTreatment:A. All Patients1. Universal precautions, BSI2. Scene safety3. Perform initial survey - resuscitate if needed4. Intubate as needed and assist ventilations.5. Make decision concerning hospital destination and mode of transport assoon as possible.6. Check for the following conditions:A. Chest traumaB. Absent breath sounds in one or both lungs upon ventilationC. Change in mental statusD. Hemodynamically unstable with a systolic BP of 90 or less7. Perform needle thoracostomy to the affected side. If both lungs are affected,perform bilateral needle thoracostomies. (Insert the needle at a ninety-degreeangle to the skin in the 2nd intercostal space, mid-clavicular line just above the3rd rib.)8. Do not delay transport. Establish an appropriate I.V. enroute.9. Call medical command via MedCom immediately.Possible Medical Command Orders:1. Alter destination or method of transfer2. Alter fluid administration3. Repeat needle thoracostomy.Note: If the patient is unconscious due to a medical problem, follow the appropriatemedical protocol.Performance Parameters:A. The protocol is applied to appropriate patients.B. Each case must be reviewed by the service medical director, and a <strong>copy</strong> of the patientcare report must be sent to the <strong>EMS</strong> <strong>Council</strong>.
Approved DOH 4/04 Page 1 of 1
MASS CASUALTY TREATMENTCriteria for UseIn the event of a mass casualty incident, ALS providers on scene may need to remain onscene to render ALS treatment or take charge of the <strong>EMS</strong> aspects of the incident. If theALS provider elects to initiate patient care, he/she:ALS Provider Guidelines:1. Must assure that <strong>EMS</strong> Command, Triage Officer, Treatment Officer andTransport Officer positions are assigned.2. Perform initial survey - resuscitate if needed and if resources allow.3. Administer appropriate oxygen4. Establish at least one I.V., if needed.5. Inform the EMT attending the patient during transport about how to monitorand operate the I.V. line.NOTE:NOTE 2:This is to be used when the patient requires I.V. administration only! If furtherALS treatment is required, an ALS provider must attend the patient enrouteto the hospital.Regional Disaster Operating Guidelines must be utilized for handling theincident.Added 7/00VII - 5
SECTION VIIISPECIFIC <strong>PROTOCOLS</strong>This section contains protocols that are:1. Generic in nature2. Specific skill oriented protocols
AIRWAYAn adequate airway is mandatory on all patients at all times.Priorities Are As Follows:1. Establishment – (maintain clinical in-line stabilization for trauma patients)a. Head tilt - chin lift for non-trauma patientsb. Jaw thrust for trauma patientsc. Relieve obstruction if necessary1) Heimlich2) Laryngoscope - Magill Forceps2.Maintenancea. Self maintained - alert, awake patientb. Nasopharyngeal airwayc. Oropharyngeal airwayd. Oral endotracheal intubatione. Bag Valve Mask or Autoventf. Nasal endotracheal intubationg. CombiTube®h. Needle cricothyroidotomy (via medical command only)VIII - 1
ALS Protocol Assessments and Procedures 2025.02 Adult-ALSContinuous Positive Airway Pressure (CPAP) 1 UsageCriteria:A. Chief complaint of shortness of breathB. History of CHFC. Physical findings of bibasilar or diffuse ralesD. and at least two (2) of the following:1. retractions or accessory muscle use2. respiratory rate greater than 253. pulse ox reading of less than 95Exclusion Criteria:A. Respiratory or cardiac arrestB. Systolic BP less than 90C. Unresponsive to verbal stimuliD. Inability to maintain airway patencyE. Major traumaF. Signs or symptoms of infection or aspirationG PneumothoraxH. Uncontrolled vomitingI. Unstable facial fracture or facial burnsJ. Patient unable to tolerate maskSystems Requirements:A. Portable static flow generatorB. Appropriate maskTreatment:A. Initiate oxygen via non-rebreather mask.B. Administer nitroglycerin and lasix as per “Dyspnea– Pulmonary Edema” protocol.C. Set up device per manufacturer’s directions.D. Set pressure at 5 - 10 cm H 2 O of pressure if device is not preset.E. Explain procedure to patient.F. Connect flow generator as per manufacturer’s instructions.G. Begin transport if not already enroute.H. Continuously monitor pulse ox to maintain 95 or greater.I. Continuously monitor patient to ensure effectiveness of the CPAP device. 2J. Contact Medical Command. 3,4,5Notes1 BiPAP may be utilized if the ALS Service Medical Director approves and completedtraining consistent with regional guidelines.2 In case of life threatening complications:1. Stop treatment2. Offer reassurance3. Follow appropriate protocol3 . Radio report to the hospital MUST contain notification that CPAP is being utilized.4 . Medical Command Physician might order intermittent treatment or specific duration oftreatment.5. Medical Command must be consulted before use of CPAP in cases of near drowning.Performance Parameters:A. Charting must include date and time of treatment; pulse ox readings; vital signs every 5minutes; effects and/or adverse reactions.Approved DOH 4/04 Page 1 of 1
ENDOTRACHEAL INTUBATIONAdministration of medications via ET is appropriate when IV or IO access is delayed.Medications which may be administered via ET are:OxygenLidocaineEpinephrineAtropineNarcanMedications should be administered twice the dosage as for IV.Nasotracheal IntubationIndications: for hypoventilation and airway protection in the patient with depressed mentalstatus. It can be used where endotracheal intubation is contraindicated due to C-spineinjuries. The patient must be breathing.Contraindications: not for patients who are too combative to allow the procedure, not forpatients who are not breathing; not for patients where significant resistance is metduring insertion attempt.Precautions: the endotracheal balloon must be tested and functioning; lungsounds must be auscultated post intubation; the C-spine must be protected if injury issuspected.Complications: epistaxis, esophageal intubation, right mainstem bronchusintubationConfirm correct placement of endotracheal tube by use of end tidal CO 2 detectiondevice.Revised 02/01VIII - 2
Esophageal Tracheal Combination TubeAirway ManagementAchieving and maintaining a patent airway is a top priority. Airway maneuvers must berapidly and accurately accomplished when needed. The use of the combination tube isan additional ALS adjunct to assure that proper airway patency is achieved whenendotracheal intubation attempts fail. The combination tube is for use in theunconscious patient only.Priorities1. Standard endotracheal intubation should be attempted three times prior toconsideration of using the combination tube, unless position or condition of thepatient preclude attempts.2. Indications for use of the combination tube:a. Unsuccessful endotracheal intubation after three attempts.b. Apneic patient with absent gag reflex.c. Limited access to the patient=s head precluding standard endotrachealintubation.d. The patient=s position or condition prohibits endotracheal intubation.Cautions1. Patients over 5' 6" in height must have the CombiTube7.2. Patients between 4' and 5' 6" in height must have the CombiTubeSA7Contraindications1. Do not use any CombiTube7.if the patient is less than 4' tall.2. The patient has an intact gag reflex and/or is conscious.3. There is known esophageal disease.4. The patient has ingested a caustic substance.5. The patient has a tracheostomy/laryngectomy.Sequence:1. Assure adequate ventilation of the patient with high flow oxygen/BVM.2. Check the combination tube (ETC) balloons for leaks.3. Lift the patient=s mandible and tongue with non-dominate hand.4. Insert the ETC gently with dominant hand following the natural curve of thepharynx. DO NOT use cricoid pressure during insertion. Stop insertion ifresistance is met. Insert the tube until the teeth or alveolar ridge rests betweenthe black lines on the tube.VIII - 2a
5. Inflate the blue tube balloon (#1) with 100 cc air using the syringe provided by themanufacturer.6. Inflate the white tube balloon with 10-15 cc air using the small syringe provided bymanufacturer.7. Ventilate through the blue tube. Listen over the stomach to confirm absence ofsound, then listen over all lung fields to confirm presence of sound. Continueventilating via the blue tube if these parameters are met.8. If gastric sounds are heard or no lung sounds are heard, ventilate through the cleartube (#2) and listen for sounds over the stomach and all lung fields. If no gastricsounds are heard and breath sounds are heard over all lung fields, continueventilating using the clear tube (#2).9. If resistance is met during insertion or if unable to hear lung sounds and no soundover the stomach despite ventilation through both tubes, discontinue attempt, deflateany inflated balloon(s) and remove the tube. Continue ventilation via BVM with highflow O2.Quality Assurance Parameters1. All ALS providers must attend an educational session detailing the properprocedure for the use of the combination tube. Written evaluation of understandingwill require 80% score to pass. Practical skill demonstration will also be required inorder for the ALS provider to be approved by their respective service medicaldirectors for field use of the combination tube for airway control.2. Re-evaluation will be required once every year with the same pass parametersas the initial training.VIII - 2b
BREATHINGAdequate oxygenation of all patients is mandatory. This is assured throughmaintenance of adequate rate and depth of ventilations with adequate concentration ofoxygen.Priorities1.Conscious, alert patient may need only supplemental oxygen concentration ininspired air.Supplemental oxygen administration is defined as:a. Lo-flow -nasal cannula 2-6 L/min with O2 concentration of 24-40%b. Hi-flow -face mask 10-12 L/min with O2 concentration 40-60%-partial or non-rebreather mask 12-15 L/min with O2 concentration60-90%2.Non-breathing patienta. Mouth to maskb. Mouth to mask - supplemental O2c. Bag-valve mask - supplemental O2d. Demand valve (not for Pediatric patients)e. Autovent3.Inadequate rate or depth of ventilationa. Supplement with baggingb. Check complianceNeedle thoracostomy for tension pneumothoraxVIII - 3
CIRCULATIONPerfusion through adequate circulation is necessary to preserve vital organs and thefollowing procedures should be initiated when indicated.Priorities Are As Follows:1. No pulse (no circulation)C.P.R.2. Inadequate (BP 80 with signs of shock)a. Pneumatic Anti-shock Garment Exceptions (Do Not Inflate)1) Cardiogenic shock2) Respiratory shock - may inflate extremities only3) Penetrating wounds of chest4) Penetrating wounds of abdomen with potential of diaphragmatic injuryb. Intravenous therapyAppropriate I.V.3. Potentially inadequate (progressive hypovolemia)two I.V.'s one or both wide open until perfusion is adequate - then titrate asneededVIII - 4
INTRAVENOUS THERAPYIn the prehospital management of the acutely ill or injured patient, there areessentially two reasons to establish an intravenous infusion:1. To administer medications2. To administer fluidsThe following I.V. fluids are approved for use in the <strong>Eastern</strong> PA Region:1. 5% Dextrose in Water (D5W)a. Used when pulmonary edema is suspectedb. Used when mixing most prehospital medication dripsNote: Use the appropriate administration set2. 1/4 normal saline or D5 .25 NSS or bothMay be used for non-trauma pediatric patients under the age of 8Note: May use a minidrip administration set with a buritrol3. Lactated RingersUsed for trauma patients, hemorrhage and/or shockNote: Use a macrodrip administration set4. Normal Saline (0.9 NaCl)a. Used for medical illness other than pulmonary edemab. May be used as a substitute for Lactated Ringers when LR is not availableUse care when setting the drip rate to KVO. Too much fluid mayhave a deleterious effect on medical patients.NOTE: After three (3) unsuccessful attempts to establish an I.V. therapy, medicalcommand must be contacted before further attempts may be made.Revised 7/9511/963/99VIII - 5
FLUID THERAPY USING PRE-EXISTING CENTRAL VENOUS ACCESSDEVICES and PERIPHERAL VENOUS INTERMITTENT INJECTABLEDEVICESUtilized for fluid / medication therapy when no peripheral access is possible. These long-term devices arefound in patients who require frequent IV medication administration over an extended period and / or havedocumented inaccessible peripheral veins.Pre-requisites:1. A patient who is in need of IV therapy or medication.2. Two attempts have been made to access other sites.3. Peripheral venous intermittent injectable device, such as a Hickman catheter or other indwelling centralline, exists.4. In cardiac arrest, these lines may all be used prior to new IV attempts.Indications:Any situation where fluid replacement or the potential need for IV medications existsContraindications:Evidence of swelling, redness, extravasation of fluid around the existing device site.This protocol will address the individual devices separately as their management variesfrom device to device.I. Heparin locks / Capped IV catheters: These may be used without prior IV attempts.A. Peripheral IV access devices with caps that allow intermittent administration of medications withoutcontinuous IV flow.B. Equipment:1. Gloves2. Appropriate IV solution / tubing3. Alcohol swab4. 4 - 20 ga. needles5. 2 - 1O cc syringes (empty)6. 10cc syringe filled with NSS7. TapeC. Sequence:1. No need to obtain medical command approval prior to this procedure.2. Prepare IV solution and flush tubing in the normal manner.3. Swab injectable cap with alcohol swab.4. Puncture injectable cap with 2Oga. needle attached to 10 cc NSS syringe.VIII - 5a
5. Withdraw slightly and observe for blood aspiration. (You may not see any)If the situation requires a blood specimen to be obtained:a. Puncture first with empty 10 cc syringe / needle and withdraw 10 cc blood anddiscard.b. Puncture with second empty 10 cc syringe / needle and withdraw 7 -10 cc of blood(this is your specimen).c. Inject blood into appropriate collection tube.d. Puncture cap with 10cc NSS syringe / needle and continue with #6 below.e. If unable to obtain blood for sample, discontinue attempt andcontinue with # 6 below.6. Slowly inject NSS and observe for resistance, swelling, or pain around the site. If any ofthe above occur STOP FLUSH. discontinue procedure and search for a new site.7. Remove syringe and needle, attach 2Oga. needle to end of IV tubing and puncture capwith that needle.8. Open IV flow clamp and observe for flow.9. Secure needle to cap via tape and adjust flow to prescribed rate, secure tubing withtape.- OR -7. Remove syringe, remove cap (if removable type) while holding digital pressure proximalto insertion site to prevent blood leakage during removal of cap.If situation requires a blood specimen to be obtained, follow steps under # 5 above with thedifference of using syringes without needles and maintaining digital pressure proximal toinsertion site any time a syringe is disconnected.8. Attach end of IV tubing to IV catheter I Heparin lock tubing port.9. Open flow clamp and observe for flow.10. Secure tubing in normal manner and adjust flow to prescribed rate.II. Implanted port (Port-A-Cath)A. Rigid metal device with central core (septum) of self-sealing plastic material with attachedcatheter extending into central venous system. Usually found in upper chest. Implanted underthe skin and must be palpated to determine landmarks.B. Equipment:1. 3 Betadine swabs2. Unsterile gloves3. Appropriate size 2Oga. non-coring needle (AGripper@) with attached extension tubing.3/4", 1", 1 1/4" lengths are most common. If patient or significant other are unable toindicate the proper needle length, use 1". It's better to use too long a needle and have itsticking out of the skin than to use too short and not have it reach the port chamber.VIII-5b
4. 1 - 10 cc syringe containing 8 -9cc NSS.5. 2 - 10 cc syringes, empty.6. Large (at least 4" x 4") clear, occlusive dressing (Tegaderm, Bioclusive, etc.).7. Appropriate IV solution / tubing.8. TapeC. Sequence:1. Attempt to find adequate peripheral site for new IV.2. Contact medical command if unable to establish IV after two attempts or if patient refuses toallow peripheral attempts. Advise physician of same and the presence of a Port-A-Cath andrequest permission to access the port.3. Provide a secure setting to attempt the accessing of the port (i.e.. in the home, in theambulance before transport, in the stationary ambulance).4. Place patient supine.5. Locates / identifies device septum by palpating perimeter edges of port.6. Don gloves.7 Cleanse skin over device using Betadine or alcohol swabs in a spiral motion from center ofdevice outward, repeat x 2.8. Attach 10 cc NSS syringe to extension tubing on "Gripper" needle and flush tubing andneedle until all air expelled.9. Remove protective cover from "Gripper@ needle.10. Close clamp on "Gripper@ needle tubing.11. With one hand identify septum of port by palpating perimeter edges using two fingers orfinger and thumb.12. Maintaining fingers on both sides of septum and providing gentle tension away from the center,slowly, but firmly insert AGripper@ needle through skin and septum perpendicular to the device untilthe needle is felt to strike the bottom of the port chamber.DO NOT WIGGLE NEEDLE OR FORCE NEEDLE BEYOND POINT OF STRIKING BOTTOM!!!13. Open clamp on AGripper@ tubing.14. Verify position by aspirating blood with NSS syringe.If pre-hospital blood specimen is required:a. Using empty 10 cc syringe instead of NSS syringe, draw back 10 cc of blood.b. Clamp tubing, remove and discard syringe.c. Attach second empty syringe, open clamp, withdraw 7 - 10 cc blood.d. Clamp tubing remove syringe (this is your specimen to be injected into the appropriate blood collectiotube).e. Attach NSS syringe, open clamp.f. If unable to aspirate blood, discontinue attempt and continue with # 15 below.VIII - 5c
15. Slowly inject NSS and observe for infiltration of fluid into tissue, pain around site.If unable to advance needle or inject NSS without difficulty:a. Verify that tubing clamp is open. If so and difficulty persistsb. Discontinue attempt.c. Notify medical command.16. Close clamp on AGripper@ tubing.17. Disconnect syringe and connect I.V. tubing.18. Open clamp on AGripper@ tubing.19. Start IV flow at appropriate rate.20. Remove contoured grip Awings@ from cushioned platform above needle.21. Place transparent adhesive dressing over insertion site and secure tubing around site with tape.22. Verify continued I.V. flow and adjust to prescribed rate.23. Administer prescribed IV meds through IV tubing AY@ site n same manner asperipheral IV=s.24. Include in documentation the size f AGripper@ needle used. and verification of placement (i.e.blood return on aspiration, ease of injecting NSS, etc.)III. PICC LinesA. Peripherally Inserted Central Catheters usually found in the antecubital areas. Relatively smallbore long catheters used for long term medication administration.B. Equipment/Sequence:Essentially the same as with Heparin Locks/capped IV catheters with the following conditions:a. Attempt to find adequate peripheral access site x 2 first.b. Notify medical command to obtain permission to access the PICC line, unless the patient isin cardiac arrest. In cardiac arrest cases, the site may be used under standing orders.c. Due to relatively small lumen, faster flow rates will not be attainable and it may becomenecessary to apply some pressure on the IV bag to overcome friction loss and achieve a flow.Use of a pressure infusor at relatively low pressure (no more than 100 mm Hg) is appropriate.IV. A-V accesses for hemodyalysis:A. Include dialysis catheters usually found in the neck or groin and A-V (arterio-venous) grafts usuallyfound in the arms. These area reserved only for the administration of hemodialysis. Patency of thegraft site can be determined by auscultating over the graft and hearing pulsating bruit or feeling apulsating thrill.B. Acceptable:1. In cardiac arrest2. By medical commandVIII - 5d
C. If a patient is at a dialysis center and experiences a situation requiring <strong>EMS</strong> transport to ahospital and they still have needles / dialysis tubing attached to their access site, theneedles/tubing should be secured with a dressing and the area observed for bleedingduring transport. If bleeding occurs or if the needles become dislodged, direct pressure overthe site must be maintained for at least 15 minutes.D. If a patient is at a dialysis center and requires <strong>EMS</strong> transport to a hospital and the dialysiscenter staff have established an IV flow through the dialysis access, the Paramedic / PHRNshould:Contact medial command while at the center to advise the command physician of anexisting IV via the dialysis access. The command physician will advise the paramedic asto how to proceed.E. Arms with active A-V dialysis accesses should not be used for peripheral IV attempts,phlebotomy, BP assessment or any other procedure that may damage the access site.Patients with access that have occluded and are no longer functional may have that armused for peripheral IV attempts, BP assessment, phlebotomy, etc, providing their nephrologistdoes not plan to use another pert of that same arm for another access. Alwaysask the patient/significant other if there are plans to place additional access grafts and wherethey are planned. It would be best to avoid these areas if at all possible. The area over andaround the old access site should be avoided.V. Long Term Central Venous CathetersA. There are a variety of long-term catheters used for intermittent administration of medicationsand/or fluids. The most common are the Hickman, Groshong, Broviac and Quintoncatheters. They are usually found in the clavicular area and are inserted into the subclavianvein. They may have one or more lumens, the multi-lumen catheters having separate distalaccess tubings/caps for each lumen.B. Equipment:1. Gloves2. 2 - 10cc syringes (empty)3. 1 - 10cc syringe filled with NSS4. Alcohol swab5. 2 - 20ga needles6. Appropriate IV solution/tubing7. TapeC. Sequence:1. Attempt to find an adequate peripheral site X 2 first.2. Contact medical command for permission to access long term central catheter,unless the patient is in cardiac arrest. In cardiac arrest cases, the site can be usedunder standing orders.VIII - 5e
VI. Critical Points3. If multilumen catheter, ascertain the most appropriate lumen for blood draw/IV administration.a. Ask the patient/significant other which line is designated for this.b. If information is not available check the extension tubing near the injection caps.Most manufacturers print where the lumen empties in relation to the catheter. Thereforethe Adistal@ lumen would empty closes to the tip of the catheter. This would be an appropriatelumen to use.4. Follow the procedure described above for accessing Heparin Locks with the followingcondition:a. Using an empty syringe withdraw 10cc blood before injecting anything. The catheter mayhave been filled with Heparin to maintain patency and flushing catheter without withdrawingwould give patient bolus of Heparin.b. If unable to withdraw any blood, do not attempt to inject or initiate a flow. In this casecontact medical command. Make sure to close the clamp on the tubing you are usingbefore disconnecting any syringe or IV tubing to prevent any air from entering line. Thenmake sure clamp is re-opened after re-attaching syringe / tubing and attempting to aspirate,inject or initiate flow.A. Strictest aseptic technique is imperative for manipulating central IV lines due to theincreased potential for infection.B. Medical Command must be contacted for permission prior to any attempt to accessany central line, except in cases of cardiac arrest. In cardiac arrest cases, the site may beused under standing orders.C. Patient should be in a stationary setting (at scene or in stationary ambulance) whencentral lines are being accessed.D. No Paramedic / PHRN will be allowed to access central lines until they are fully inserviced and approved to do so by their respective service medical director.VIII-5f
INSERTION OF A SALINE LOCKIndications:A patient who has stable vital signs, but potentially could require I.V. medications or fluids.This patient does not currently need I.V. fluid therapy or is not in need of medications that couldprecipitate hypotension. This patient may fall under one of the standing orders which calls for anI.V. administration.Contraindications:When the need for I.V. fluids is immediate.Objectives:1. Expedite I.V. access2. Simplify the transfer of patients3. Improve patient comfort and mobility4. Decrease the possibility of an I.V. being pulled accidentally5. Lower the cost of operationsEquipment Needed:1. Alcohol swabs2. Gloves3. Standard I.V. catheter4. Multi-use vial of Normal Saline for injection5. Cap (pigtail).6. 20 ga syringe needle, or needleless injector if applicable..Procedure:1. Establish I.V. access using the appropriate size catheter, in the usual manner.2. Place the cap (pigtail) on the back of the catheter.3. Assemble a syringe (3cc to 5cc) with a 20 gauge needle attached, or needle -less injector, ifapplicable.4. Draw up 3cc of Normal Saline Solution from the multi-does vial.5. Wipe the injection site with alcohol, puncture the rubber cap or access the needleless injectionport and inject 3cc of NSS.NOTE: If using an extension piece, fill that with NSS too.Dispose of sharps appropriately.Added 3/99 VIII -5g
CAROTID SINUS MASSAGEUtilized as the second method of treatment of symptomatic supraventricular tachycardia.(The first method would be the Valsalva Maneuver - having the patient hold his/her breathand bear down)Equipment and patient prerequisitesIndications1. The patient must be on cardiac monitor2. The patient must have I.V. running3. The patient must be receiving 02 therapy1. Paroxysmal supraventricular tachycardia which is symptomatic (produces dyspnea,dizziness or hypotension)2. A patient under 55 years of ageContraindicationsSequence1. A patient with known carotid artery disease2. A known stroke patient3. Absent carotid pulse on one side1. Confirm supraventricular tachycardia unresponsive to Valsalva Maneuver2. Contact medical command physician3. Monitor, 02 and I.V. in place4. Palpate carotid pulses, one side at a time5. Upon the orders of the medical command physician, palpate the carotid artery onone side, near the angle of the jaw, with the patient's head turned to the opposite side6. Obtain rhythm strip before and during massage7. Rub carotid artery near the angle of the jaw with two fingers, vertically back forth whileapplying some pressure, and observing cardiac monitor for 15-20 seconds8. Obtain rhythm strip after massage9. Massage may be repeated in 2-3 minutes, if unsuccessful conversion, on the same oropposite side.10.Do not massage both sides at the same timeVIII - 6
SYNCHRONIZED CARDIOVERSIONUtilized for patients who have EKG documented supraventricular tachycardia not responding toValsalva Maneuver, Carotid Massage, Verapamil or Adenosine and ventricular tachycardia,unstable with pulses and not responding to LidocaineEquipment and Patient PrerequisitesIndicationsSequences1. The patient must be on cardiac monitor2. The patient must have an I.V. running3. The patient must be receiving O2 therapy4. A defibrillator with synchronized cardioversion capability and charged batteries mustbe available.1. Supraventricular tachycardia not responsive to:a. Valsalva Maneuverb. Verapamil/Adenosine2. Ventricular TachycardiaUnstable with pulses1. Document rhythm and clinical finding requiring cardioversion2. Turn defibrillator on3. Turn synchronizer switch on4. Set joule level5. Apply gel to paddles6. Charge defibrillator to level for monophasic or biphasic device.7. Apply paddles with 20-25 pounds of pressure: one R subclavicular area and one overapex of heart8. Assure area of safety by stating "Stand clear"9. Discharge paddles10.Obtain new EKG readingVIII - 7
DEFIBRILLATIONUtilized for patients who have EKG documented evidence of ventricular fibrillation or pulselessventricular tachycardia.Equipment and Patient PrerequisitesIndicationsSequences1. Unconscious patient with absent pulses2. EKG monitoring3. Defibrillator with charged batteries1. Pulseless ventricular tachycardia2. Ventricular fibrillation1. Confirm patient is unresponsive2. Confirm patient apneic and pulseless3. C.P.R. in progress4. Document rhythm requiring defibrillation via EKG monitor or defibrillator paddles5. Turn defibrillator on6. Assure synchronizer switch is off7. Set joule level for monophasic or biphasic device.8. Apply gel to paddles or use defibrillation pads or "hands free" patches9. Charge defibrillator10. If paddles are used apply them with 20-25 pounds of pressure one R subclavicular areaand one over apex of heart11. Assure area of safety. Stop CPR and "stand clear"12.Discharge paddles13.Obtain new EKG readingVIII - 8
EXTERNAL CARDIAC PACINGUtilized for patients who have EKG documented evidence of 2nd or 3rd degree heart block,particularly in symptomatic patients and when ordered by medical command.Equipment and Patient PrerequisitesIndications1. Patient must be on cardiac monitor2. Patient must have I.V. running3. Patient must be receiving O2 therapy4. Operational external pacer availableSecond and third degree blocks, particularly with symptomatic patients and who have nobeneficial effect from atropine therapy.ContraindicationPatient with Pulseless Electrical ActivityRelative ContraindicationSequenceAsystolic patient1. Apply anterior and posterior external pacer monitor padsa Anterior - over apex heartb. Posterior - para sternal infra scapular leftc. Connect output (pacing) cable to pads2. Connect patient to external pacer and turn on power (pacer in standby mode)3. Record EKG rhythm strips before, during, and after the application of external pacer.Also, palpate and record pulse rate. Have a defibrillator readily available.4. Adjust gain and lead selection on cardiac monitor to verify QRS detection.VIII - 9
5. Select demand mode (if necessary) unless directed by medical command physician.6. Set escape rate higher (10-20 ppm) than the patient's intrinsic QRS rate, for a minimumof 60 total complexes per minute. Escape Rate = Intrinsic (pt. complexes + drive rate). Ifno intrinsic QRS rate exists, use 60 ppm.7. Turn on External Pacer start button.8. Start at low mA (current) setting 40-60 mA or 1 (depending on the model) andincrease until evidence of electrical capture is evident on the cardiac monitor (saw tooth orwide QRS). Use only enough mA (current) to achieve capture.9. Once electrical capture is achieved, assess for perfusion using pulse pressure (truemechanical capture), blood pressure, and patient's overall clinical picture.10. If perfusion is not achieved, increase mA by increments of 10 mA, then reassess. Ifthere is still no capture after increase to maximum current, notify medical command.11. Reassess patient and treatment plan.12. If ventricular fibrillation or ventricular tachycardia occurs, TURN PACER OFF or toSTANDBY MODE (depending on model) and proceed with appropriate protocol.VIII - 9a
NEEDLE CRICOTHYROIDOTOMYUtilized for patients who have a compromised airway which cannot be controlled by other methodsas listed on page VIII - 1.Equipment and Patient Prerequisites:1. A patient with compromised airway (see indications below).2. #12 or #14 3" needle angiocath adult. #16 or #18 3" needle angiocath children.3. Oxygen tubing with whistle control (pre packaged)Indications:1. Failed oral and/or nasotracheal intubation.2. Compromised airway from massive oropharyngeal trauma.3. Entrapment with need for airway control or ventilatory support with physical constraintson conventional methods.Contraindications:NoneSequences:1.Confirm need.2. Contact medical command physician for permission.3. Head and neck stabilized.4. Puncture site prepped with alcohol wipe and locally anesthetized whenever possible ifthe patient is not unconscious.5. Perform cricothyroid puncture - catheter is advanced and stylet removed.6. Attach tubing with whistle control from oxygen supply to needle.7. Turn oxygen on and adjust to 15 L/min flow.8. Ratio of inflation to deflation is 1 sec to 4 sec.9. Report result to medical command.10.Constantly monitor oxygen supply, as D cylinder lasts approximately 20 minutes Ecylinder lasts approximately 30 minutes if full when initiating flow11.When unloading patient, oxygen tubing must be changed to portable tank and ventilationcontinued until relieved by physician.Complications:1. Improper placement of needle with no aeration - remove needle and repuncture.2. Kinking of catheter - remove and repuncture3. Bleeding from needle - remove and repuncture4. Plugged needle with secretions - attempt syringe aspirationVIII - 10
NEEDLE THORACOSTOMYUtilized for the decompression of a Tension PneumothoraxDiagnosed by:1. Respiratory distress2. Increased resistance to bagging3. Absent breath sounds4. Hyperresonance to percussion5. Deviated trachea away from tension6. Distended jugular veins7. May have S/S shockEquipment and Patient Prerequisites:1. Patient in supine position.2. Patient has secure airway.3. Patient receiving O2 therapy.4. #14 or #16 needle angiocath.5. Heimlich or flutter valve with adaptable tubing for Heimlich.Sequences:1. Confirm need. (See Protocol 6025.02 Tension Pneumothorax)2. Maintain airway3. Find position for insertion of needle (2nd interspace, mid clavicular line just above3rd rib).4. Insert needle 90-degree angle to skin into pleural space, remove stylet and attachHeimlich valve or flutter valve device.5. I.V., Monitor6. Report result to medical command.Contraindications:NoneComplications:1. Misplacement of needle with no relief of signs or symptoms2. Bleeding from or injury to blood vesselsRevised 11/00VIII - 11
PREHOSPITAL BLOOD DRAWINGIt is not the purpose of prehospital operations to draw blood samples for later testing except wherethere may be a necessity to prove clinical impressions for treatment initiated by ALS providersordered by command physician. The only valid prehospital testing is Chem Strip, glucometer anddrawing of blood for glucose level.No other blood will be drawn for the following reasons:Procedure1. Time consuming2. Additional sticks are being done for blood samples only.3. Legal complications4. Majority not labeled when handed to hospital personnel5. Risk of exposure1. Chem Stripa. To be done by ALS personnel ONLY.b. A glucometer may be used.c. Determination may be made during initial attempt to start an IVd. A finger stick may be done at any time, at the discretion of the ALS provider, when it isfelt that the patient may have experienced a hypoglycemic episode. Even if a venipuncturehas already been performed, a fingerstick may be performed.e. Command must be consulted with the results of the chem strip whenever thisprocedure is performed.2. Blood Sugara. One tube of blood may be drawn for blood determination.b. Clinical record must document blood drawn and tube must contain patient's name andALS provider who drew the blood.c. This blood will be drawn in the initiating of the I.V.d. No additional venipuncture may be performed for blood sample only, unless ordered bythe medical command physician. As above, a finger stick for a chem strip reading may beperformed as a standing order.Revised 7/95VIII - 12
INTRAOSSEOUS THERAPY(IO Infusion)Utilized for I.V. therapy in pediatric patients, 4 years old or less, when intravenous access hasbeen unsuccessful after two or three attempts.Equipment and patient prerequisites1. Patient who is 4 years old or less2. Previous unsuccessful I.V. attempts3. Betadine and alcohol preps4. 10 cc syringe and needle5. Normal saline for irrigation6. 15 - 18 gauge Marrow needles or Cook catheters7. I.V. fluids and administration sets8. Sterile glovesIndications1. Cardiac arrest2. Shock3. Severe dehydration4. Burns5. Trauma - multi-system6. Failed IV attemptsContraindications1. Recently fractured bones at or near site2. Infected burns or cellulitis3. Osteogenesis ImperfectaSequence1. Obtain medical command permission if required.2. Immobilize as needed with leg slightly externally rotated.3. Palpate tibial tuberosity.4. Visualize point 1-2 finger widths (2 cm) below (distal) to tuberosity.5. Prep area thoroughly with betadine and/or alcohol.6. Hold needle with stylet (trocar) in place at right angle to bone (slightly caudad).7. Insert with two movements.a. Penetrate skin and subcutaneous tissue.b. Penetrate periosteum and bone itself with a twisting motion until a "pop" or "give" is felt.8. Withdraw the stylet -the needle will feel firmly fixed to bone.9. Aspirate,(this should occur without resistance) - do not aspirate more than 1 cc of bonemarrow.VIII - 13
10. Inject 5 cc of saline and withdraw a small amount, which may be somewhat uncomfortable ina conscious patient.11.Connect the I.V. administration set to needle.12.Stabilize needle and allow fluids to flow.13.May have to pressurize the I.V. bag to obtain satisfactory flow rate.Revised 11/91
2/01 VIII - 14
ALBUTEROL (PROVENTIL) ADMINISTRATIONIndicationsAlbuterol (proventil) is a relatively selective beta2 adrenergic bronchodilator for the relief of acutebronchospasm due to bronchial asthma, chronic bronchitis and emphysema.Dosage and AdministrationAlbuterol (Poventil) is administered by oral inhalation by nebulizing the drug. The mechanism fornebulization will be a disposable nebulizer connected to an oxygen source.The correct dosage of Albuterol (Proventil) is 0.5 ml (2.5 mg) diluted in 3.0 ml of a diluent solution.Protocol for Administration1. Determine whether the patient is a candidate for Albuterol (Proventil) treatment.Suggested candidates for Albuterol (Proventil) administration in the field are patientswho are:a. wheezing or have other evidence of diffuse small airway expiratory obstruction (prolongedexpiration phase; bilateral diminished air entry) with adequate ventilatory effort;b. Have a specific history of asthma or COPD;c. chronically utilize medications to treat wheezing, i.e.: oral theophylline, B-agonist inhalers(Proventil, Alupent, Metapel) or oral B-agonist (brethine, Alupent).Patients who are not likely to be candidates for Albuterol (Proventil) administrationinclude patients who:a. are chronically managed solely with diuretics, and/or nitroglycerin, and/or digoxin, and/orcalcium channel blocker preparations, and likely to be in congestive heart failure.b. have chest pain suggestive of acute ischemic heart disease, unless relief ofbronchoconstriction seems important as a precipitating/aggravating condition.2. Add Albuterol (Proventil) medication to the nebulizer by placing the dose into the base of thenebulizer.3. Assemble mouthpiece to flex tube and place flex tube into "T" fitting. Place "T" fitting on outlet ofnebulizer and hook to oxygen source.4. Set oxygen source to at least 8 liters/min flow rate.VIII - 15
5. Instruct patient to begin breathing normally through mouthpiece. After 1 to 2 minutes of normalbreathing, instruct patient to inspire deeply and slowly and attempt to hold medication within lungsfor several seconds - then exhale normally through mouthpiece.6. Remind the patient not to breath too rapidly. Interpose a deep inspiration for every 5-10 normalbreaths. Ideally, respirations should be deeper than normal, but also, slower than normal.7. Be sure not to invert the nebulizer or you will lose the medication. As the treatment progresses,shake or knock down the beads of medication from the side of the nebulizer.8. Monitor vital signs throughout treatment.9. Discontinue treatment if pulse is elevated 15% or if significant ectopy (PVC's)Adverse ReactionsThe most frequent adverse reactions to Albuterol (Proventil) include nervousness, tachycardia,tremors and nausea. Less frequent reaction are hypertension, palpitations, vomiting and a badtaste in the mouth.Be aware of reducing the hypoxic drive mechanism in chronic carbon dioxide retainers. Whenthis occurs, it is usually reversible by removal of the nebulizer and provision of ventilatory supportfor the patient.Because Albuterol (Proventil) is a sympathomimetic drug, it should be used with caution inpatients with known hypertension, coronary artery disease, congestive heart failure and diabetes.If excessive tachycardia, ventricular ectopy or chest pain are produced, discontinuetreatment and contact medical command. Use caution with administration for children under 12years of age.VIII - 16
GLUCAGONIndications For Use:Unconsciousness due to suspected hypoglycemia, with no IV access.Precautions:Patients with cardiovascular disease may rarely become hypotensive due to smooth muscleeffects.Patients with known hepatic or renal insufficiency.How Supplied:Supplied as 1 mg (1 USP unit) vials, in powder form to be diluted in normal saline solution orother diluent to produce a concentration of 1 mg/ml.Dosage:Adult:Dissolve 1 mg glucagon in 1 ml NSS for a concentration of 1 mg/1 ml. Administer .5 - 1 mgglucagon solution IM.Pediatric: Using the same concentration, administer 0.025 mg/kg IM.VIII – 17
ADMINISTRATION OF RECTAL MEDICATIONIndications1.Use rectal Valium for active seizure lasting longer than 5 minutes andcurrently seizing, and no I.V. can be established after two attempts.2. Use rectal Valium for multiple seizures with no recovery of consciousnessbetween seizures and currently seizing, and no I.V. can be established aftertwo attempts.3. Whenever a medical command physician orders a specific medicationthat has been approved for regional use to be given rectally, the physicianmust give explicit orders regarding dose and rate of administration.Contraindications1. Respiratory insufficiency2. HypotensionEquipment1. 10 cc syringe2. Lubricant3. 5 ml saline4. Soft suction catheter with thumb port removed.Sequence1. Assure airway patency and administration of appropriate oxygen.2. Use universal precautions.3. Draw the calculated dose of medication and dilute with I.V. solution.4. Attach the suction catheter to the syringe or use a10 cc slip tip syringe or.If an IV catheter is used without the suction catheter, ensure that the needlehas been removed.5. Have an assistant hold the patient=s legs apart or place the patient onhis/her side.6. Lubricate the catheter and insert it into the patient=s rectumapproximately 4-6 cm beyond the anus. The catheter should advanceeasily; do not force it.7. Administer the dose and flush with 5cc saline.8. Withdraw the catheter and hold the buttocks closed for 1-2 minutes toprevent leakage.Precautions1. Respiratory depression2. Hypotension3. Administration in the anus, with inadequate absorption4. Forceful placement of the catheter causing rectal injuryNote: Sodium Bicarbonate may not be given rectallyAdded 7/00VIII - 18
SECTION IXQUALITY ASSESSMENTANDIMPROVEMENT PARAMETERS
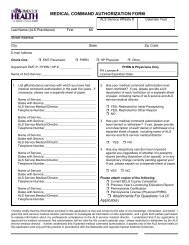
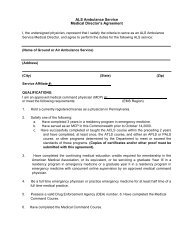
Medical Command AuthorizationandContinuing Education RequirementsTo perform advanced life support skills under the scope of practice of an EMT-paramedic (EMT-P) orprehospital registered nurse (PHRN) in the <strong>Eastern</strong> Pennsylvania Emergency Medical Services regionan individual must obtain and complete the following:1. .Medical command authorization from each of the ALS service medical directors on behalf of theservice the individual intends to function under. (DOH Requirement)2. Completion and/or compliance with the Department of Health's <strong>EMS</strong> continuing educationrequirements. (DOH requirement)3. Any additional education or skill verification approved by the Department of Health and as determinedby the Service Medical Director on an individual basis.Medical Command Authorization: Medical command authorization is the permission given to anEMT-paramedic (EMT-P) or a prehospital registered nurse (PHRN) under Act-82 to perform, onbehalf of an ALS ambulance service, ALS services pursuant to medical command or inaccordance with Department approved regional <strong>EMS</strong> council transfer and medical treatmentprotocols when medical command cannot be secured, is disrupted or is not required pursuant tothe approved regional <strong>EMS</strong> council transfer and medical treatment protocols. Authority to grantmedical command, the prerequisites for initial determination regarding medical commandauthorization and the review of medical command authorization for EMT-paramedics (EMT-P)and prehospital registered nurses (PHRN) in the <strong>Eastern</strong> Pennsylvania Emergency MedicalServices <strong>Council</strong> region are as stated in Act 1994-82 (Act 82) amendments to the EmergencyMedical Service Act 3: P.S. subchapters 6921-6938. The following information is taken directlyfrom Act 1994-82 (Act 82) subchapter 1003.28.Authority to grant medical command - the ALS service medical director has the authority togrant, deny or restrict medical command authorization to an EMT-paramedic (EMT-P) orprehospital registered nurse (PHRN) who seeks to provide <strong>EMS</strong> on behalf of the ALSambulance service. The ALS service medical director shall document the medical commandauthorization decision and how that decision was made. The decision of the ALS servicemedical director shall affect the medical command authorization status of the EMT-P or PHRNfor that ALS ambulance service only. An EMT-P or PHRN who seeks to provide <strong>EMS</strong> on behalfof multiple ALS ambulance services must receive medical command authorization from the ALSservice medical director for each ALS ambulance service.IX - 1
Initial medical command authorization - an individual seeking medical command authorizationmust be:1. Certified by the Pennsylvania Department of Health as an EMT paramedic(EMT-P) or prehospital registered nurse (PHRN).2. Complete an application for medical command authorization on a form prescribed by theDepartment of Health.3. Shall have competently performed each of the services set forth in the individual's applicablescope of practice as documented on the initial skill verification form.Restriction of medical command authorization - if the ALS service medical director determinesthat the individual applying for medical command authorization cannot competently perform theALS services within that individual's scope of practice, the ALS service medical director shalleither deny or restrict the individual's medical command authorization.Review and renewal of medical command authorization - at least annually, and if more frequentlyshould circumstances warrant, the ALS service medical director shall review the medicalcommand authorization status of each EMT paramedic (EMT-P) and prehospital registerednurse (PHRN) providing service on behalf of the ALS ambulance service. The ALS servicemedical director in reviewing the medical command authorization application shall ensure:1. The individual has or is completing the applicable continuing education requirements asstated in Act 1994-82 (Act 82) subchapter 1003.29 on continuing education.2. The individual has demonstrated competence, as verified by the ALS service medicaldirector, in performing each of the skills set forth in the individual=s scope of practice.Upon review of medical command authorization the ALS service medical director may either:1. Renew medical command authorization.2. Renew medical command authorization and require continuing education courses in any fieldthe ALS service medical director deems appropriate.3. Require completion of specified continuing education courses as a prerequisite to renewal ofmedical command authorization.4. Restrict the scope of practice under medical command authorization.5. Withdraw medical command authorizationIX - 2
Appeals of denied or restricted medical command authorization - an individual whose medicalcommand authorization has been denied or restricted by the ALS service medical director mayappeal the decision within 14 days to the regional <strong>EMS</strong> co-medical director(s). The appeal shallbe in writing and shall specify the reasons the individual disagrees with the decision of the ALSservice medical director. The individual shall also have an opportunity to present testimony andother evidence supporting their opinion, cross-examine opposing witnesses and submit oraland written position statements at a hearing conducted by the regional <strong>EMS</strong> co-medicaldirector(s).Appeals to the Department of Health - if either party is dissatisfied with the decision of theregional <strong>EMS</strong> co-medical director(s) with regard to medical command authorization, that partyshall have the right of immediate appeal to the Department. The party appealing shall submit awritten statement to the Department specifying the reasons for the party's objections to theregional <strong>EMS</strong> co-medical director(s)' decision within 14 days of that decision.Scope of appeals - appeals of restriction or denial of medical command authorization shall beconfined to a review and determination of whether, at the time of the assessment conducted bythe ALS service medical director, the individual possessed the competence to perform skills forwhich the individual was denied medical command authorization.Continuing Education Requirements: Pursuant to Act 1994-S2 (Act 82)subchapter 1003.29 amendment to the Emergency Medical Services Act 3: P.S.subchapters 9691-693S, to be eligible to receive and retain medical commandauthorization EMT-paramedics (EMT-P) and prehospital registered nurses (PHRN) shallattend:1. Eighteen (18) hours of education in each calendar year in subjects related to the scopeof practice of an EMT-Paramedic.2. Eighteen (18) hours of education in each calendar year in subjects related to the scopeof practice of a Prehospital Registered Nurse.3. Biennially a cardiopulmonary resuscitation (CPR) course for adult, child andinfant sponsored by the American Heart Association (AHA), American RedCross (ARC) or another CPR course approved by the Department to meet or exceed thestandards of the specified programs.4. At least 9 of the 18 hours of instruction shall be in medical and trauma education.Continuing education credit for instruction - prehospital personnel may also accrue hoursto be credited to the individual=s continuing education requirements equivalent to thenumber of hours the individual is an instructor in a continuing education course offered bya continuing education sponsor, or a course that satisfies requirements for initialcertification or recognition of prehospital personnel conducted by an accredited traininginstitute for prehospital personnel.Revised 7/00IX - 3
Continuing education credit through endorsement - Prehospital personnel who attend coursesoffered by any organization or agency with National or state accreditation to provide continuingeducation may apply to the Department to receive credit for these courses. The individual shallhave the burden of demonstrating to the Department that these courses meet standardsequivalent to those standards imposed by the Department of Health's <strong>EMS</strong> ContinuingEducation Manual.<strong>EMS</strong> provider continuing education record - twice a year EMT-paramedics (EMT-P) andprehospital registered nurses (PHRN) shall receive a record of their continuing education. Theindividual is responsible to present this record to their ALS service medical director to remaineligible for medical command authorization. Medical command authorization may not beextended by an ALS service medical director to any ALS service provider who has not satisfiedthe continuing education requirements stated above.Accrual of continuing education hours and repetitive courses - no EMT-PARAMEDIC (EMT-P)or prehospital registered nurse (PHRN) is eligible to receive credit for the same course morethan once in each calendar year. Credit hours earned in one year may not be carried over intothe subsequent calendar year.Attendance- prehospital personnel must complete all sessions comprising a class as requiredby the continuing education sponsor. Continuing education hours will not be recorded by thecontinuing education sponsor when students:1. Are absent for an entire session (that is not made up).2. Arrive fifteen (15) or more minutes late (that is not made up).3. Are expelled from class for disruptive behavior.4. Leave during a session without permission5. Attend a session or class, but do not participate in the activities.6. Fail to sign the Department approved class roster.7. Fail to satisfactorily complete the continuing education completion form.Accredited continuing education courses - the Department shall maintain a list of approvedcourses that will be updated semi-annually. The <strong>Eastern</strong> Pennsylvania Emergency MedicalServices <strong>Council</strong> shall disseminate the list of approved courses at least twice per year to allcontinuing education sponsors in its jurisdictionIX - 4
Accredited continuing education sponsors - Entities and institutions may be accredited by theDepartment of Health under Act 1994-82 (Act 82), subchapter 1003.30. It is the individual'sresponsibility to be sure the continuing education course and continuing education sponsor areaccredited by the Department of Health.For a definitive reference on continuing education requirements for prehospitalpersonnel see:Pennsylvania Department of Health, Division of <strong>EMS</strong> Systems<strong>EMS</strong> Continuing Education Manual - July 1996IX - 5
Pages 6-13 deleted 4/98IX - 12
MONTHLY REPORT FROM SERVICE MEDICATION INVENTORIESEach month each carrier must complete a Medication Inventory listing all the medicationscarried on each unit, with quantities. This report must be signed by the Service Medical Directoror Pharmacist, as well as a responsible person from the service. This inventory must beretained by the service and available for <strong>EMS</strong> <strong>Council</strong> staff upon request.Services are encouraged to develop an inventory form that suits their standard operatingprocedures. The form should include an inventory for each vehicle, with amounts of eachmedication and fluids carried on the vehicle. The form should include a place for the signaturefor the officer in charge of the inventory and a place for the service medical director=s signature.There should be a place to document the dates for these signatures, as well as a line statingwhat month the inventory was performed.Revised 3/99IX - 14
Page 15 deleted 4/98IX - 15
Protocol for Ambulance RestockingPromulgated By:Applicable To:<strong>Eastern</strong> PA Emergency Medical Services <strong>Council</strong>All Ambulance ServicesDate: April 22, 2002Effective January 3, 2002, The <strong>Eastern</strong> Pennsylvania Emergency Medical Services <strong>Council</strong>promulgates that it shall be the policy of the <strong>Eastern</strong> Pennsylvania Emergency Medical Services<strong>Council</strong> that all Ambulance Services within the <strong>Eastern</strong> Pennsylvania Medical Services Regionshall restock their ambulance according to the <strong>Eastern</strong> Pennsylvania Emergency MedicalServices Region Drug and Non-Reusable Medical Supply Restocking Agreement currently inplace between the Ambulance Services and Hospitals within the <strong>Eastern</strong> Pennsylvania MedicalServices Region. Copies of the <strong>Eastern</strong> Pennsylvania Emergency Medical Services RegionDrug and Non-Reusable Medical Supply Restocking Agreement are available upon request.IX-15a
CONTROLLED SUBSTANCES DOCUMENTATIONControlled substances shall be handled according to the following attached policies and samplelogs.IX - 16
EASTERN PENNSYLVANIA EMERGENCY MEDICAL SERVICES COUNCILPREHOSPITAL OPERATIONSSubjectControlled Substances will be handled according to the following policies utilizing the followingforms.Policies1. Controlled Substances - Squad Responsibility(see Attachment I)2. Controlled Substances - ALS Provider Responsibility(see Attachment II)3. Controlled Substances - Physician Responsibility(see Attachment III)Forms1. Controlled Substances - Inventory Log (see Attachment IV)2. Controlled Substances - Usage Log (see Attachment V)3. Controlled Substances - Ordering Log (see Attachment VI)06/88 IX - 17
EASTERN PENNSYLVANIA EMERGENCY SERVICES COUNCIL PREHOSPITAL OPERATIONCONTROLLED SUBSTANCES - SQUAD RESPONSIBILITYPolicyEach Advanced Life Support Squad shall maintain an Inventory Log and Usage Log for controlledsubstances.Procedures1. At each change of shift the ALS provider will conduct an inventory of the controlledsubstances on the vehicle. If the squad operates more than one unit, a separateControlled Substances Inventory Log will be kept for each vehicle.a. 20 mg. Morphine Sulfate is the maximum supply permitted pervehicle.b. 20 mg. Valium is the maximum supply permitted per vehicle.c. 40 mg. Versed is the maximum supply permitted per vehicle.2. The following information will be recorded on this form:a. Dateb. Timec. Quantity of each controlled substanced. Signature of ALS provider conducting the inventory3. After a controlled substance is ordered and administered, data will be entered on theControlled Substance Usage Log (separate log for each unit).4. The following information will be recorded on this form:a. ALS provider administeringb. Physician orderingc. Patient receivingd. Substance usede. Date usedf. Time usedg. Amount usedh. Amount returned to receiving hospitalI. Witness' signature receiving hospital5. The unused amount will be turned in at the receiving hospital.Revised 1/03 IX -18
6. The amount will be recorded, a new supply obtained and hospital representative signatureobtained.7. These logs will be maintained by the service, available for inspection by the <strong>EMS</strong> <strong>Council</strong> Staff,the Department of Health or other state or federal agencies.8. Any discrepancy of counts or usage of controlled substances shall require immediate verbalnotification of the Co-Medical Directors and written report follow-up. The service must notify thelocal police of any discrepancy.Revised 4/98IX - 19
EASTERN PENNSYLVANIA EMERGENCY SERVICESCOUNCIL PREHOSPITAL OPERATIONSCONTROLLED SUBSTANCES - ALS PROVIDER RESPONSIBILITYPolicyThere shall be a paper trail of all controlled substances administered by ALS Providers withcommand authorization in <strong>Eastern</strong> Pennsylvania <strong>EMS</strong> Region.Procedure1. ALS Providers will establish radio communication with command physician.2. The command physician may order controlled substance by name, dose, and route.3. The ALS provider will administer the drug after confirming order.4. After the ALS provider delivers the patient at the receiving hospital he/she will call (via phone)with the name of patient and time administered.5. The ALS provider will then complete usage log, turning over the unused drug and having thereceiving individual sign usage log verifying receipt and replacement of the drug.6. Usage logs will be maintained by the service as Controlled Substances policy directs and mustbe available for inspection by the <strong>EMS</strong> <strong>Council</strong> Staff, the Department of Health or other state orfederal agencies.Revised 3/99IX - 20
EASTERN PENNSYLVANIA EMERGENCY SERVICES COUNCIL PREHOSPITAL OPERATIONSPolicyCONTROLLED SUBSTANCES - PHYSICIAN RESPONSIBILITYA prescription shall be issued for each order of a controlled substance by the ordering commandphysician.Procedure1. With each order of a controlled substance a prescription will be written with the drugand amount ordered and dated.2. When the ALS provider reaches receiving hospital, he/she will call the command (ordering)physician and supply name of patient.3. The command physician will complete a prescription and a <strong>copy</strong> to the receiving hospitalimmediately.Revised 10/96 IX - 21
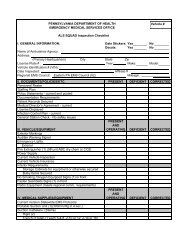
EASTERN PENNSYLVANIA EMERGENCY SERVICES COUNCILPREHOSPITAL OPERATIONSControlled Substance Inventory Log SheetSquad____________________________________Unit_______________Month____________________________________Year_______________DateTimeQuantityMorphine Valium VersedSignature6/88
Revised 1/03IX-22
EASTERN PENNSYLVANIA EMERGENCY SERVICE COUNCILPREHOSPITAL OPERATIONSCONTROLLED SUBSTANCE USAGE LOGSquad__________________________________ Unit_______________Month__________________________________Year______________ALS ProviderAdministeringPhysicianOrderingPatient=sName Substance Date TimeAmountUsedAmountReturnedWitness=SignatureIX - 23
EASTERN PENNSYLVANIA <strong>EMS</strong> SYSTEMPREHOSPITAL TRAUMA TRIAGEDECISION SCHEMETRAUMA PATIENTAssess Vital SignsAndLevel of ConsciousnessUNRESPONSIVE TO VERBAL STIMUATION(on the “AVPU” schema)ORSYSTOLIC B.P. 15% and/or Face or Airwayv Flail chestv Major proximal amputation or degloving injuryMECHANISMOFINJURYEVIDENCEOFHIGHIMPACT- Falls of 20 ft. or more- Crash with Vehicle Deformity of 30” or more- Displacement of front rear Axle- Passenger Compartment intrusion:18” or greater on patient side of vehicle24” or greater on opposite side of vehicle- Ejection of Patient- Rollover- Death of same vehicle occupant- Pedestrian struck at 20 MPH or moreYESNOTRAUMA CENTERQuickest meansof Transportation&Closest TRAUMA CENTERPATIENTS AT INCREASED RISKWHEN TRAUMATIZEDAge < 5 or > 55Known Cardiac or Respiratory DistressIX - 25
YESNOFor Moderate Severity InjuryCONSULT MEDICAL COMMANDYESRe-evaluate withMedical CommandTRAUMA CENTERNOTransport to closestmost – appropriateHospital FacilityGROUNDTRANSPORTATIONA) Direct to Trauma Center if within 20minutes & patient ready to goB) Ground-to-Helicopter rendezvous toexpedite transport of TraumaCenter, when the Ground Unit isenroute toward a Trauma Center &a Helicopter is availableC) If >20 minutes travel time to TraumaCenter, GO TO CLOSEST, MOSTAPPROPRIATE HOSPITALFACILITY for stabilization andtransfer, when helicopter notavailableHELICOPTERClosest Approved HelicopterTo be UtilizedA) Direct to Trauma Center if within30 minutes flight time from sceneB) WHERE BLS OR ALSANTICIPATES DELAYED PATIENTTRANSPORT (e.g. Entrapment;remote location; accumulation ofsnow; hostage situation)C) Rendezvous with Ground Unitenroute to Trauma Center – toexpedite patient transportD) Respond to local ReceivingHospital to transfer patient toTrauma CenterCONSULT MEDICAL COMMAND TO RECEIVE MEDICAL COMMAND&CONFIRM APPROPRIATENESS OF DESTINATION FACILITYMAJOR TRAUMA PATIENT – A patient with severe multi-system or major uni-system injury, theextent of which may be difficult to ascertain, but which has the potential of producing mortality ormajor disability.(As defined by the Pennsylvania Trauma Systems Foundation)NOTE: ALS Unit(s) shall be dispatched to incidents involving known or suspectedmajor trauma patient(s), when available.For further understanding of this decision scheme refer to: PA Dept. of Healthrecommendations and Appendix F to the Hospital Resources Document Field Categorizationof Trauma Patients (Field Triage) by the Committee on Trauma of the American College ofSurgeons, from which the <strong>Eastern</strong> Pennsylvania Emergency Medical Services <strong>Council</strong> hasdeveloped and adopted this regional trauma triage adaptation.IX - 26
QUARTERLY QA & I REPORT FROM FTHESERVICE MEDICAL DIRECTOR1. The service medical director shall submit, on a quarterly basis, a qualitative report tothe <strong>Eastern</strong> PA <strong>EMS</strong> <strong>Council</strong>. This report shall contain a number of indicators whichwill survey various aspects of the squad’s operation. These indicators may changefrom year to year, especially if a specific indicator shows excellent compliance.2. The following indicators, (as of the date of this revision), shall be reviewed andreported:A. Number of ALS cases in the quarter - patients that fit the ALS criteria.B. Enroute time greater than 3 minutes - the time it takes for the ALS unit to goenroute to the call after it was dispatched.C. Response time greater than 20 minutes - the time it takes to travel to the sceneafter going enroute.D. On scene greater than 20 minutes - The number of instances where an ALScrew was on scene with a medical patient for greater than 20 minutes. Patientsin cardiac arrest or with a recent onset of CVA shall be excluded fromthis filter.E. Deviation from protocol - the number of cases that deviated from StandingOrder Protocols or a medical command physician=s orders. This does NOTinclude cases where medical command was sought prior to the initiation of ALStreatment.F. Command not contacted - any ALS case where command was not establishedvia the UHF radio system either because of a mechanical or technical problem,or the proximity to the hospital was < 3 minutes.G. EKG, IV, etc., warranted but not utilized - any ALS case where the patient=scondition warranted a specific treatment, but such treatment was not utilized.NOTE: For the indicators noted in B, C, D, E, F, and G, the first column in thereport is the total number of cases for that indicator. The percentage for thesecond column is calculated by dividing the number of cases in the indicatorby the number of total cases in the quarter. The third column is the number ofcases that were not justified.H. On scene > 20 minutes with cardiac arrest - any cardiac arrest case where anALS crew was on scene fro greater than 20 minutes.I. On scene > 20 minutes with recent onset CVA - any ALS case where the ALScrew remained on scene for greater than 20 minutes with a patient that hadsuffered a CVA within the hour prior to the crews arrival.Revised 1/00IX-27
J. On scene > 10 minutes with non-entrapped trauma - any ALS case where anon-entrapped patient fits into the Trauma Triage Guidelines and the crewwas on scene > 10 minutes. NOTE: When a trapped patient is extricatedfrom the wreckage or confined space, that time is to be recorded on theALS trip report.K. 1 st defibrillation > 4 minutes from patient contact - any ALS case where ittook > 4 minutes for the first defibrillation to take place after the ALSprovider has made contact.L. Chest pain diminished with ALS intervention - any ALS case where chestpain diminished as a result of ALS interventions.NOTE: For the indicators noted in H, I, J, K, and L, the first column in thereport is for the total number of cases for that indicator. The secondcolumn is the number of cases that exceeded the indicator, or in the caseof the chest pain indicator, the number of instances where treatmentimproved the condition. The percentage for the third column is calculatedby dividing the number of cases that improved or exceeded the indicatorby the number of cases in the indicator. The fourth column is the numberof cases that exceeded the indicator and were not justified.3. The quarterly report documents that the QA & I indicators were reviewed for allcases. It is understood that there might often be valid reasons for havingexceeded the indicators listed. However, if an indicator was exceeded, anexplanation MUST be documented by the author of the patient trip sheet.Explanations can be documented in the space provided on the report form, (asfound on page IX - 28 of the ALS Protocols manual), or in a narrative format on aseparate sheet of paper.4. The report shall be signed by the Service Medical Director, indicating that 100% ofthe service=s ALS cases have been reviewed for completeness and quality ofcare, in accordance with the Regional Quality Assessment and Improvementguidelines. The individual preparing the report shall also print his / her namebelow the service medical directors signature. Reports shall be submitted to the<strong>EMS</strong> <strong>Council</strong> by the last day of the month following the end of the quarter.Revised 1/00IX - 27aForm - 2 - 1989
EASTERN PENNSYLVANIA EMERGENCY MEDICAL L SERVICES COUNCILQUARTERLY QA & I REPORTName of Service________________________________________________This report covers theNumber of ALS cases in the quarterquarter of the yearDate report sent _______________Parameter # of cases % of total # not justifiedEnroute time greater than 3 minutesResponse time greater than 20 minutesOn scene greater than 20 minutesDeviation from protocolCommand not contactedEKG, IV, etc., warranted but not utilizedParameter# of casesinparameter# thatimprovedorexceededparameter% thatimprovedor total #of casesinparameter# casesnotjustified(ifapplicable)On scene > 20 minutes with cardiac arrestOn scene > 20 minutes with recent onset CVAOn scene > 10 minutes with non-entrappedtrauma1 st defibrillation > 4 minutes from patientcontactChest pain diminished with ALS interventionCases that are not justified can be explained in the space provided or in a narrative format on aseparate sheet. Explanations for cases not justified MUST be submitted with the report. Thisreport shall be submitted to the <strong>EMS</strong> <strong>Council</strong> by the last day of the month following the quarter.E.g., the 1 st quarter report is due in the <strong>EMS</strong> <strong>Council</strong> office by April 30.I have reviewed the Quarterly QA & I Report and have / will take steps to correct inadequacies.Signature of Service Medical DirectorDatePrinted Name of Peron Preparing Report____________________________________Revised 4/98 IX - 281/00
SECTION XRESOURCES
A & PabdABC=sACFACLSAEDAF or A-Fib.AIDSakaALSamAMAamb.AMIampamtantart.ARDSasaASCVDASHDATLSATAVAAOX4adminAxBCLSBLSBMBPBVMBBBBBSBSBSAc o_cccCacadCABGCAOX4cath.ABBREVIATIONSanatomy and physiologyabdomenairway, breathing, circulationantecubitaladvanced cardiac life supportautomatic external defibrillatoratrial fibrillationacquired immune deficiency syndromealso known asadvanced life supportbefore noonagainst medical adviceambulanceacute myocardial infarctionampuleamountanteriorarteryadult respiratory distress syndromeaspirinarteriosclerotic cardiovascular diseaseartersclerotic heart diseaseadvanced trauma life supportatrial tachycardiaatrio-ventricularalert and oriented to person, place, time and eventadministrationassessmentbasic cardiac life supportbasic life supportbowel movementblood pressurebag valve maskbundle branch blockbi-lateral breath soundsbreath soundsbody surface areacentegradewithcubic centimetercancer, carcinomacoronary artery diseasecoronary artery by-pass graftconscious, alert oriented to person, place, time and event
catheterX - 1CBCC/C or CCCHFCIDcmcmcCNSCOCO 2COPDCOLDcont.c/oCPRCVACSFCL -CPCSMDispDOADOBD/CD 5 WD 50DefibDPTDTDXED/ER<strong>EMS</strong>EKG/ECGEEGEMTEMT-PEENTEOAETAe.g.EMDETOHETText.ENTFHX or FHFRfxfreq.complete blood countchief complaintcongestive heart failurecervical immobilization devicecentimetercontact medical commandcentral nervous systemcarbon monoxidecarbon dioxidechronic obstructive pulmonary diseasechronic obstructive lung diseasecontinuedcomplains ofcardiopulmonary resuscitationcerebrovascular accident (stroke)cerebrospinal fluidchloridechest paincorotid sinus massagedispatcheddead on arrivaldate of birthdiscontinue5% dextrose in water50% dextrose in waterdefribillatediptheria, pertosis, and tetanus vaccinedelirium tremensdiagnosisemergency departmentemergency medical serviceselectrocardiogramelectroencephalogramemergency medical technicianemergency medical technician - paramediceyes, ears, nose and throatesophageal obturator airwayestimated time of arrivalfor exampleemergency medical dispatchethanol (alcohol)endotracheal tubeextremity
ear, nose, throatfamily historyfirst responderfracturefrequentlyFBOFDF oGm., ggr.GIGravidagtt.GUGynGSWHEENTH & PHPIhth or hr.HxIMIVieICICPinf.IPPBIVPIOJVDjkgKVOK+lacLlLPMlb.LBBLLQLOCL & DX - 2LRLLLLLQLULLUQmaxforeign body obstructionfire departmentfarenheitgramgraingastrointestinalnumber of pregnanciesdropsgenitourinarygynecologygun shot woundhead, eyes, ears, nose, throathistory & physicalhistory of present illnessheighthourhistoryintramuscularintravenousthat isintracardiacintercranial pressureinferiorintermittent positive pressure breathingIV pushintraosseousjugular vein distentionjoulekilogramkeep vein open - an IV ratePotassiumlacerationLeft
literliters per minutepoundleft bundle branch blockleft lower quadrant of theabdomenlevel of consciousnesslabor and deliverylactated ringersleft lower lobe (lung)lower left quadrant of theabdomenleft upper lobe (lung)left upper quadrant of theabdomenmaximumX - 3MASTMCLmedsmg, mgmmg/kgMIminMICUMVANa+N/AN 2 Onitro or NTGNKANSRNVDNaClNADNaHCO 3NCNG tubeNSS or NSN/VO 2OBODO.D.O.S.oz_pPACPATpalppcnPDPCO 2PEPEAPEEPPedPJCPMHptPERLPIDpmMedical antishock trousersmidclavicular line, modified chest leadmedicationsmilligrammilligrams per kilogrammyocardial infarctionminimummobile intensive care unitmotor vehicle accidentsodiumnot applicablenitrous oxidenitroglycerineno known allergiesnormal sinus rhythmneck vein distentionsodium chloride
no apparent distresssodium bicarbonatenasal cannulanasogastric tubenormal saline solutionnausea and vomitingoxygenobstetricaloverdoseright eyeleft eyeounceafterpremature atrial contractionparoxysmal atrial tachycardiapalpationpenicillinpolice departmentpartial pressure of carbondioxide, a measurement of thegas dissolved in a fluid, such asbloodphysical exampulseless electrical activitypositive end-expiatorypressure, used to keep thealveoli from collapsing duringexpirationpediatricpremature junctional contractionpast medical historypatientpupils equal and reactive tolightpelvic inflammatory diseaseafternoonX - 4
PMPNDpO 2post.PPMPRNpsiPVCP-waveP/W/DqQRSQRS complexqtRRBBBRDSRhRHDRLRLLRLQRMLR/OROMRSRRULRUQRx_s2 oSCBASCUBASIDSSLS.O.B.SOPSS#STS-TStatSTDSC,SQ,Sub.QSVTsym. Or Sxpost mortemparoxysmal nocturnal dyspneapartial pressure of oxygen, a measurement of the gas dissolvedin a fluid such as bloodposteriorparts per millionadministered as neededpounds per square inch of pressurepremature ventricular contractionfirst positive deflection in an EKG corresponding to sinus nodepolarizationpale, warm, dryeveryquick response unitlarge vertical spike in the EKG which represents ventriculardepolarizationquartrightright bundle branch blockrespiratory distress syndrome(rhesus); blood fctorrheumatic heart diseaseringers lactateright lower lobe (lung)right lower quadrant of the abdomenright middle lobe (lung)rule outrange of motionregular sinus rhythmright upper lobe (lung)right upper quadrant of the abdomentreatmentwithoutsecond degreeself contained breathing apparatusself contained underwater breathing apparatussudden infant death syndromesublingualshortness of breathstandard operating proceduressocial security numbersinus tachycardiaportion of the EKG which follows the QRS compleximmediatelysexually transmitted diseasesubcutaneoussupraventricular tachycardiasymptoms(s) X - 5
TBTKOT-wavetempTIATKtabtbspTPRtspTxunconsuneqUHFVFVHFVSVTVDvolWNLwt.WBCy/o; y.o.tuberculosisto keep open - an IV drip ratelast part of the normal EKG cycle, indicatingrepolorization of the ventricletemperaturetransient ischemic attacktourniquettablettablespoontemperature, pulse, respirationsteaspoontransportunconsciousunequalultra high frequency (radio)ventricular fibrillationvery high frequency (radio)vital signsventricular tachycardiaveneral diseasevolumewithin normal limitsweightwhite blood countyears oldX - 6
LRleftRight› Increased or elevatedflDecreased or depressedMaleFemale- , ˘ Negative, none+ Positive, plus= EqualX2; X3 Times 2 or 3, etc./ Per> Greater than< Less thanChange@ApproximatelyNot equalLeading to? Questionable, question(s)MedicationsAdenAlbutAminAtropBenedBicarbBretCaCl 2D 25D 50DopamEpiLidoMSNTGVerapAdenosineAlbuterolAminophyllineAtropineBenedrylBicarbBretyliumCalcium Chloride25% Destrose50% DextroseDopamineEpinephrineLidocaineMorphine SulfateNiroglycerinVerapamilX - 7
AIR AMBULANCESI. General Criteria Before Requesting An Air AmbulanceA. Would the amount of time needed to transport a patient by ground to an appropriatefacility pose a threat to the patient's survival and recovery?B. Would weather, road conditions, or other factors affecting the use of ground transportseriously delay the patients access to ALS care?C. Does the available ambulance service have the critical skills or equipment needed tocare for the patient during transport?II. General Medical CriteriaA. Unresponsive to verbal stimuliB. Systolic blood pressure < 90C. Respiratory rate of < 10 or > 29D. Penetrating injury to the chest abdomen, head, neck or groin (except forobviously superficial wounds)E. Two or more proximal long bone fracturesF. Combination with burns of greater than or equal to 15% and/or face or airway.G. Flail chestH. Major amputation or degloving injuryI. Crushed or fractured pelvisJ. Multiple systems traumaK. Mechanism of injury (after careful assessment of injuries)1. Falls of 20 feet or more2. Vehicle with deformity of 30" or more3. Displacement of front or rear axle4. Passenger compartment intrusion:a. 18" on patient side of patientb. 24" on opposite side of patient5. Ejection of patient6. Rollover7. Death of same vehicle occupant8. Pedestrian struck at 20 MPH or more.III. Requesting Air Ambulances To An Accident Scene:A. Contact the appropriate communication center. The following information will berequested:1. exact location2. number of patients3. any entrapment4. frequency to communicate from ground to air5. location of nearby landing site in relation to the incidentB. After dispatching the helicopter team, the communication technician may call forfurther information in order to update the flight crew and assist them in locating theincident.X - 8
IV. Cancellation of Air AmbulancesAn ALS provider may cancel an Air Ambulance before it has become airborne only under thefollowing circumstances:A. Has performed a complete assessment of the patientB. Has assessed the mechanism of injuryC. Has evaluated other factors such as road conditions, entrapment, etc.D. Has determined that aeromedical transport is not warranted.If the helicopter is already airborne, the ALS provider who is on the scene and has evaluatedthe situation as above must contact medical command at the trauma center. The medicalcommand physician may choose to cancel the helicopter.V. Landing Site Preparation:A. Vacant lots, athletic fields, parking lots, cleared highways and fields are adequate sites.The site should be at least 60' X 60', preferably 100' x 100'. The site shouldbe cleared of and be as level as possible.B. The landing site must be free of overhead obstructions, such as poles and power lines.All nearby obstructions should be reported to the pilot before landing is attempted.Remember: power lines are difficult to see at night.C. Mark the corners of the landing site with flares. Auxiliary lighting may be used until thePilot locates the scene. Once the site has been located, make sure that all bright lightshave been turned off. Never shine bright lights at the aircraft.VI. Helicopter SafetyA. Never go near the tail rotors. Approach only from the front of the aircraft.B. Remain clear of the helicopter at all times unless accompanied by a flight crew memberor the rotors have stopped completely.C. Do not bring vehicles within 50 feet of the aircraft.D. Transfer patients from the ambulance to the helicopter under the supervision of theflight crew.VII. Air Ambulance Service's InformationAir Ambulance Service Emergency Number Business NumberGeisinger Life Flight 800-852-7828 570-271-6666Hershey LifeLion 800-225-4837 717-531-7777University MedEvac 800-322-9599 610-402-8666PennStar 800-543-7827 610-231-3735Guthrie One 800-535-0911 570-882-4915Sky FlightCare 800-552-6666 215-383-8512Revised 11/964/99 X - 97/00
Purpose:Staff Notification Procedure for Major IncidentsThe following procedure shall be implemented by <strong>Eastern</strong> PA <strong>EMS</strong> provider(s)and Public Safety Answering Points (PSAP). The purpose of this procedure is to alert the<strong>Council</strong> staff of major incidents that can impact <strong>EMS</strong> provider(s), medical facilities, andthe overall health and safety of the citizens and visitors of this six county region.In many cases this notification will be for information purposes only, however itmay necessitate an immediate response from the <strong>Council</strong> staff.Notifications will assist the <strong>Council</strong> staff in providing information to the PADepartment of Health, Emergency Medical Services Office for their assistance andutilization.Situations to Notify the <strong>EMS</strong> <strong>Council</strong>1.) Hazardous Material Responses:Hazardous material incident involving associated fatalities or an evacuation of 25people or greater from a public building such as: hospitals, nursing homes, officecomplexes or residential areas, schools or institutions, and transportationincidents.2.) Air Medical Response:Any situation where three (3) or more air ambulance services are dispatchedto an incident.3.) Mass Casualty Incident:Any situation where ten (10) or more people are injured.4.) Multiple Fatalities:Any situation where three (3) or more deaths have occurred at an incident.5.) Ambulance Accidents:Any ambulance accident that results in an injury or death to ambulance crewmembers, patients or other parties involved in the accident.6.) Line of Duty Death:Any line of duty death of an emergency service provider(s).7.) Fires:Fires of three (3) alarms or greater.8.) Public Health Alerts:Possible outbreak of disease or epidemic, for example: West Nile Virus, foodpoisoning, tuberculosis etc…X-9a
9.) High Risk Evacuation:Evacuations involving twenty five (25) people or greater, that pose a significanthealth and safety risk, for example: nursing homes, hospitals, elderly high riseresidences.10.) Severe Weather Incident:Any type of severe weather condition that causes loss of life, extensive propertydamage or major road closure for extensive periods of time. This may include:flooding, flash flooding, heavy snow / blizzards, hurricanes, ice storms, severethunderstorms, high winds, tornados.11.) Terrorism / Weapons of Mass Destruction Events:A terrorist or weapons of mass destruction event that causes the evacuation ofany facility or institution or other area.12.) Other:<strong>EMS</strong> provider(s) or a PSAP(s) may notify <strong>Eastern</strong> PA staff of unusual events thatmay be occurring in their jurisdiction that they feel warrants <strong>EMS</strong> <strong>Council</strong> staffnotification or intervention.Procedure:1. Regional <strong>EMS</strong> provider(s) will notify their respective PSAP(s) as to the scopeof their particular incident.2. The local PSAP(s) will notify <strong>Eastern</strong> PA MedCom of the situation for any ofthe above noted incidents. The PSAP(s) will relay the details of the event (e.g.type of situation, number of deceased and injured, location of event etc…).3. <strong>Eastern</strong> PA MedCom will notify the appropriate <strong>Council</strong> staff.4. The on-call <strong>Council</strong> staff member may call the local PSAP(s) for additionalinformation concerning the event or to discuss the event with the on scene<strong>EMS</strong> provider(s).5. When the incident is terminated, the local PSAP(s) will notify <strong>Eastern</strong> PAMedCom who will then notify the appropriate <strong>Council</strong> staff member.April 2001X – 9b
MEDICATION ADMINISTRATION CHARTSBRETYLIUM ADMINISTRATIONBolus ---- 5 mg/kg (350-500 mg as initial doseIf V-fib is persistent, the dose can be increased to 10mg/kg and repeated as necessary.Drip ---- Use microdrip (60 gtt) setAdd 500 mg to 250 cc D5W - 2 mg/mlInfusion ---- 1-2 mg/min1 mg/min 30 gtts/min2 mg/min 60 gtts/minWhile onset of action for bretyllium in ventricular fibrillation seems to be within a fewminutes, in ventricular tachycardia it may be delayed.Contraindicated in the treatment of ventricular tachydysrhythmias caused by digitalistoxicity.DOPAMINE ADMINISTRATIONDrip --- Use microdrip (60 gtt) set1 amp (200 mg) in 250 D5W200 mcg/min – 15 gtts/min400 mcg/min – 30 gtts/min600 mcg/min – 45 gtts/min800 mcg/min – 60 gtts/minBolus ---Drip ---LIDOCAINE ADMINISTRATION1.5 mg/kg (up to a maximum of 225 mg) IV push or endotracheallyUse a macrodrip (10, 15, 20 gtt) set - for a concentration of 250 mg/250cc10 gtts/cc set 15 gtts/cc set 20 gtts/cc set1 mg/min = 10 gtts/min 15 gtts/min 20 gtts/min2 mg/min = 20 gtts/min 30 gtts/min 40 gtts/min3 mg/min = 30 gtts/min 45 gtts/min 60 gtts/min4 mg/min = 40 gtts/min 60 gtts/min 80 gtts/minRevised 7/004/04 X - 10
EXPLANATION OF MEDICATIONS AUTHORIZED FOR EASTERN PA EMT-PARAMEDICUSE CHARTSThe following charts contain medications that may be carried on ALS vehicles andadministered by ALS providers. The third column also indicates what the ALS provider mayadminister if medical command cannot be contacted or if medical command is interrupted.Some of these medications are listed as being for use only by orders of medical command.Other medications give the dosages that may be administered in the event that medicalcommand is not available and the patient has a life-threatening condition.Added 4/99X - 11a
MEDICATIONS AUTHORIZED FOR EASTERN PA EMT-PARAMEDIC USEAdenosine 6 mg/2 ml vials Use large vein; 6 mg. Rapid I.V. push. If not resolved, 12 mg rapidpush, followed by a saline flush immediately.Albuterol (Proventil) 2.5 mg in single dose vials 2.5 mg diluted given oral inhalation by nebulizerAspirin 80-81 mg tablets 325 mg orallyAtropine Sulfate1 mg/ml5 or 10 cc pre-filled syringeFirst dose 0.5 to 1.0 mg IV push. Repeat doses at direction of medicalcommand. May be given via endotracheal tube.Benedryl(Diphenhydramine HCl)50 mg/ml 25 mg IV or 25 mg deep IM injection if unable to establish IV.Contraindicated for asthmatics, acute glaucoma and pregnant patients.Bretylium Tosylate(Bretylol)Calcium Chloride(10%)10 ml ampule500 mg1 gram in 10 ml (100 mg/ml)10 ml pre-filled syringeIV push; Initial bolus 5 mg/kg IV bolus for V-Fib refractory to lidocaine.Follow-up doses: 10 mg/kg - may be repeated.IV Drip: 500 mg in 250 D5W (2 mg/ml)Infusion: 1-2 mg/min Use a microdrip (60 gtt/cc) set1 mg/min = 30 gtt min2 mg/min = 60 gtt min5 ml (5-7 mg/kg) SLOW IV push for hyperkalemia, hypocalcemia orcalcium channel block toxicity.May be repeated every 10 min.50 % Dextrose 25 gram in 50 ml pre-filledsyringe(500 mg/ml)25-50 ml as IV bolus in comatose patients. (Repeat x 1 if necessary.Revised 4/98 X - 127/0012/034/04
MEDICATIONS AUTHORIZED FOR EASTERN PA EMT- PARAMEDIC USEDiazepam (Valium) 10 mg in 2 ml pre-filled syringe (5 mg/ml) 2-5 mg SLOW IV push. In status epilepticus. Do notdilute. May give up to 10 mg.Dopamine (Intropin)200 mg (40 mg/ml) in 5 ml pre-filledsyringe200 mg in 250 D5W (800 mcg/cc)Start at 5 mcg/minInfusion Use a microdrip (60 gtt/cc) set200 mcg/min - 15 gtts/min400 mcg/min - 30 gtts/min600 mcg/min - 45 gtts/min800 mcg/min - 60 gtts/minEpinephrine 1:1,000 1 mg/ml ampule or tubex 0.3 to 0.5 mg SC in anaphylactic shock. (Or 0.01 ml/kgup to a maximum of 0.5 mg)If ALS provider must follow protocol, may repeatepinephrine 1:1,000 0.3-0.5 one timeEpinephrine 1:10,000 10 ml (0.1 mg/ml) pre-filled syringe 1.0 mg (10 ml) bolus in cardiac arrest - IV push2.0 mg (20 ml) bolus-endotracheal tubeRepeat 1 mg every 3-5 minutes. MCP may orderescalating or high dose.Furosemide (Lasix)20 mg (10 mg/ml) in 2 ml pre-filled syringe40 mg (10 mg/ml) in 4 ml pre-filled syringe100 mg (10 mg/ml) in 10 ml multidose vial40-100 mg IV push for acute pulmonary edema oredema secondary to congestive heart failure.Or 0.5 - 1 mg/kg slow IV pushGlucagon 1 mg (unit) with 1 ml diluent solution 1 mg IM for hypoglycemia when IV access is notavailableIntropin (Dopamine)Revised 12/03200 mg (40 mg/ml) in 5 ml pre-filledsyringe200 mg in 250 D5W (800 mcg/cc)Start at 5 mcg/minInfusion Use a microdrip (60 gtt/cc) set200 mcg/min - 15 gtts/min400 mcg/min - 30 gtts/min600 mcg/min - 45 gtts/min800 mcg/min - 60 gtts/minX-13
MEDICATIONS AUTHORIZED AFOR EASTERN PA EMT- PARAMEDIC USELidocaineMidazolamMorphine SulfateNaloxoneNitroglycerin100 mg in 10 ml pre-filled syringe.10 mg/ml5 mg/ml vials1mg/ml vials1-6 gr/ml10 mg/ml in a 1 ml tubex0.4 mg in 1 ml ampule.Also comes in multi-dose vials0.4 mg tablet (1/150 gr)Metered dose spray (0.4mg) 200dosesFirst Dose: 1.5 mg/kg bolus IV push or via endotrachealtube.Infusion For a concentration of 250 mg in 250 cc of D5W10 gtts/cc set 15 gtts/cc set 20 gtts/cc set1 mg/min = 10 gtts/min 5 gtts/min 20 gtts/mi2 mg/min = 20 gtts/min 30 gtts/min 40 gtts/min3mg/min = 30 gtts/min 45 gtts/min 60 gtts/min4 mg/min = 40 gtts/min 60 gtts/min 80 gtts/minAdults – 1-4 mg titrated to effect, up to dose of 0.1 mg/kgDilute Tubex (1mg in 9 ml D5W or NSS.) Titrate dose.2.0 mg IV push. May be given via endotracheal tube.1 tablet sublingually q 5 minutes up to 3.Spray as directed on container, usually 0.4 mg SL.Sodium Bicarbonate 44.6 or 50 mEq in 50 ml 1 ampule in unwitnessed arrest (not a first line drug)2 amp (25 mEq or 25 cc) may be repeated q 3-5 min.Verapamil(Isoptin, Calan)2 mg in 2 ml (1 mg/ml) ampule First dose: 5 mg SLOW IV push: repeat dose of 5 mg IV if nochange.ONLY TO BE USED UNDER DIRECT MEDICALCOMMAND.Revised 7/004/04 X - 14