Safeguarding Children Record Keeping Standards - Halton and St ...
Safeguarding Children Record Keeping Standards - Halton and St ...
Safeguarding Children Record Keeping Standards - Halton and St ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
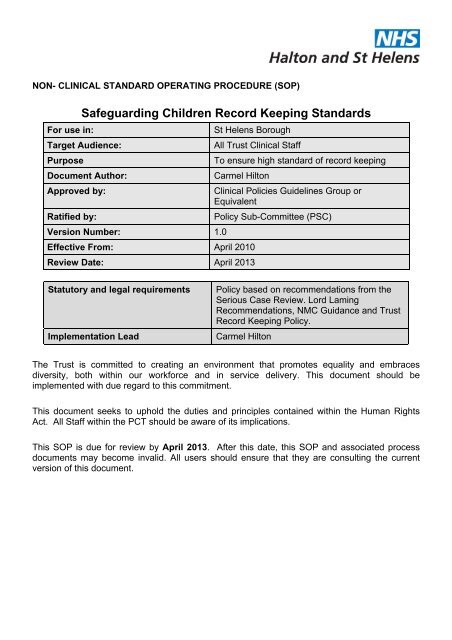
NON- CLINICAL STANDARD OPERATING PROCEDURE (SOP)<strong>Safeguarding</strong> <strong>Children</strong> <strong>Record</strong> <strong>Keeping</strong> <strong><strong>St</strong><strong>and</strong>ards</strong>For use in:<strong>St</strong> Helens BoroughTarget Audience:All Trust Clinical <strong>St</strong>affPurposeTo ensure high st<strong>and</strong>ard of record keepingDocument Author:Carmel HiltonApproved by:Clinical Policies Guidelines Group orEquivalentRatified by:Policy Sub-Committee (PSC)Version Number: 1.0Effective From: April 2010Review Date: April 2013<strong>St</strong>atutory <strong>and</strong> legal requirementsImplementation LeadPolicy based on recommendations from theSerious Case Review. Lord LamingRecommendations, NMC Guidance <strong>and</strong> Trust<strong>Record</strong> <strong>Keeping</strong> Policy.Carmel HiltonThe Trust is committed to creating an environment that promotes equality <strong>and</strong> embracesdiversity, both within our workforce <strong>and</strong> in service delivery. This document should beimplemented with due regard to this commitment.This document seeks to uphold the duties <strong>and</strong> principles contained within the Human RightsAct. All <strong>St</strong>aff within the PCT should be aware of its implications.This SOP is due for review by April 2013. After this date, this SOP <strong>and</strong> associated processdocuments may become invalid. All users should ensure that they are consulting the currentversion of this document.
Key individuals involved in developing the document (Internal <strong>St</strong>aff Only)Name(s)DesignationCarmel HiltonAndrea DerbyshireHayley McCullochSharon KellyNamed Nurse <strong>Safeguarding</strong> <strong>Children</strong> (<strong>St</strong>Helens)<strong>Safeguarding</strong> <strong>Children</strong> Specialist Nurse(<strong>St</strong> Helens)<strong>Safeguarding</strong> <strong>Children</strong> Specialist Nurse(<strong>St</strong> Helens)<strong>Safeguarding</strong> <strong>Children</strong> Specialist Nurse(<strong>St</strong> Helens)Distributed to the following for approvals <strong>and</strong> commentsCommittee(s)Members of the Policy Sub Committee (PSC)Members of the Clinical Policies GuidelinesGroup (CPG)Individual(s)DesignationAnn DunneRos ConnollyJulie BanatLesley BrownlowDesignated Nurse <strong>Safeguarding</strong> <strong>Children</strong>(<strong>St</strong> Helens)AD Child <strong>and</strong> FamilyLead Nurse Health VisitingLead Nurse School NursingRevision History <strong>and</strong> Version ControlRevisionDateReason for Change Version No. By Who Version No.April 2010 First Draft 0.1 Carmel HiltonMay 2010 Draft Approved 0.1 PSC/GAC 1.0Page 2 of 12
Table of ContentsBackground <strong>and</strong> Triggers to the Guidance...................................................................................4Objectives ....................................................................................................................................5Scope...........................................................................................................................................5Duties <strong>and</strong> Responsibilities ..........................................................................................................5General Principles .....................................................................................................................5Best Practice Guidance.............................................................................................................5Identification ..............................................................................................................................6Filing..........................................................................................................................................6Documentation ..........................................................................................................................7Transfer .....................................................................................................................................8Audit ..........................................................................................................................................8Significant Events Form Template.............................................................................................8Key Points for Team Leaders / Family Health Coordinator .......................................................9<strong>Record</strong>s <strong>and</strong> Legal Issues Exercise ........................................................................................10Appendix 1 .................................................................................................................................11Page 3 of 12
This guidance must be read in conjunction with the Clinical <strong>Record</strong> <strong>Keeping</strong> Policy.BACKGROUND AND TRIGGERS TO THE GUIDANCE<strong>Record</strong> keeping is an essential part of good nursing practice <strong>and</strong> is considered by many as abasic tool to help in caring for patients.Good record keeping helps to protect the welfare of patients by promoting high st<strong>and</strong>ards ofclinical care, allowing better communication between members of the whole health care team,giving an accurate account of treatment, <strong>and</strong> allowing the ability to detect problems at an earlystage.Good record keeping is an indication of a skilled <strong>and</strong> safe practitioner, <strong>and</strong> just as true is thefact that careless or incomplete record keeping often reveals wider problems with an individual’spractice. There is also a benchmark on record keeping contained in the Essence of Caredocument – the government’ tool to improve the quality of nursing care.Poor record keeping <strong>and</strong> communication are key factors in a large number of complaintsreceived each year by the NHS complaints department <strong>and</strong> the Nursing <strong>and</strong> Midwifery Council(NMC) in respect of nursing practice. They have also highlighted in every Serious Case Reviewconducted within the <strong>St</strong> Helens Borough, this follows a national trend.The key failings regarding record keeping nationally are: Illegible, ambiguous, unsigned <strong>and</strong> undated entries. Too scanty or meaningless statements which providing little or no evidence of what carehas been offered or delivered Key actions or decisions <strong>and</strong>/or evidence on which they are based (e.g assessment) arenot evidenced<strong>Record</strong>s can be called as evidence for: Family Court ProceedingsCriminal Proceedings: Coroners Court NMC re Fitness to Practice Committee Trust investigation panels NHS Professionals Disciplinary InvestigationsPoor records indicate poor practice – if it is not written down then legally there will be anassumption that it has not been done. Poor record keeping can result in a practitioner beingaccused of professional negligence if records are illegible, inadequate or incomplete. Goodrecords provide evidence of good care <strong>and</strong> can be vital in upholding or refuting a complaint –they are our protection <strong>and</strong> contribute to keeping practitioners as well as service users, safe.Page 4 of 12
All documentation by employees of NHS <strong>Halton</strong> <strong>and</strong> <strong>St</strong> Helens in relation to safeguardingchildren must be on NHS <strong>Halton</strong> <strong>and</strong> <strong>St</strong> Helens record cards. Every page must contain thechild’s name <strong>and</strong> date of birth.Written confirmation of any referrals to other agencies should be sent within 48 hours <strong>and</strong> acopy kept in the child health record.Details of any discussions about children should be recorded <strong>and</strong> at the end of the discussioneach professional involved should ensure the others underst<strong>and</strong>ing of the content of thediscussion <strong>and</strong> any actions or responsibilities agreed.The details of consent for treatment, examination, investigation, <strong>and</strong> referral whereappropriate should always be recorded.The rationale for all decision making in relation to case management must be fullydocumented. This must include evidence that interventions <strong>and</strong> actions are outcomesfocussed <strong>and</strong> grounded in robust assessments of need.The dates of any safeguarding meetings notified / attended must be documented on thechild’s record on the significant events form <strong>and</strong> details including - where relevant - thecategory of child protection plan <strong>and</strong> the date of commencement <strong>and</strong> discontinuationdocumented in the main body of the records.IdentificationAll records should clearly identify children subject to a Child in Need Plan, <strong>Safeguarding</strong> plan orwho are looked after by the Local Authority.All children who are subject to a:Child in Need plan should have their records placed in a blue coloured folder.<strong>Safeguarding</strong> plan should be placed in a red coloured folderLooked After <strong>Children</strong> proceedings should be placed in a yellow coloured folderThe files should be removed as soon as the child is no longer subject to a Child in Need Plan,<strong>Safeguarding</strong> Plan or Looked After by the Local Authority.FilingAll of the above records should be stored in a lockable ‘targeted / specialist need’ drawerseparately from ‘universal need’ case files / records. A tracer card must be appropriatelyplaced in the ‘generic’ caseload file.Page 6 of 12
Additionally, the records for any other child deemed to be in need of targeted / specialistservices should be filed within the appropriate section of the ‘targeted / specialist need’drawer <strong>and</strong> a tracer card appropriately placed in the ‘generic’ caseload file.Supplementary safeguarding information e.g. minutes from meetings, safeguardingsupervision records, reports etc., should be signed <strong>and</strong> dated by the practitioner to indicatethat the information has been read, tagged together in chronological order <strong>and</strong> filed at theback of the child’s record. (For health visitors <strong>and</strong> school nurses – this is the child healthrecord, not the clinic card).Medical reports received from Alder Hey Rainbow Centre should be treated in the samemanner. They should also be entered on the child’s significant events form <strong>and</strong> the practitionermust enter a rational in the main body of the child’s records clearly identifying their plan forintervention (or not) with the child <strong>and</strong> their family.All other supplementary information such as health or medical reports, attendancenotifications, liaison slips, correspondence etc should similarly signed, dated <strong>and</strong> taggedtogether in chronological order <strong>and</strong> filed at the back of the child’s record (before thesafeguarding information).Additional Points for Health Visitors / School Nurses / Lead Health PractitionersIt is essential that children subject to a Child in Need Plan, <strong>Safeguarding</strong> Plan or whoare Looked After by the Local Authority have an identified accountable case manager atall times who is clearly named on the relevant records.In cases of long-term sick leave or vacant caseloads, the relevant team manager mustensure that appropriate decisions are made as a matter of urgency , to allocate the relevantcases <strong>and</strong> notify the <strong>Safeguarding</strong> Office/ <strong>Safeguarding</strong> <strong>Children</strong>’s Specialist Nurse, key worker,the GP <strong>and</strong> all other agencies involved as necessary.DocumentationThe records of children subject to Child in Need Plan, <strong>Safeguarding</strong> Plan or who are lookedafter must include the following:A4 Centile ChartCompleted Significant events formSupervision <strong>Record</strong>sCAF if completedHealth assessmentsWhere there is any concern of a safeguarding nature or any situation within the child’s familyor environment that evidence shows is likely to impact detrimentally on the child’s health orPage 7 of 12
well-being, this should be documented in the main body of the record <strong>and</strong> entered on thesignificant events form to act as a trigger which alerts the reader to a concern.The dates of all Child in Need, child protection conferences, reviews <strong>and</strong> core groups, <strong>Children</strong>Looked After reviews <strong>and</strong> other safeguarding meetings must be recorded on the significantevents form, including - where relevant - the category of child protection plan <strong>and</strong> the date ofcommencement <strong>and</strong> discontinuation.All child health records must include full details of all siblings both older <strong>and</strong> younger (i.e.name, date of birth, school <strong>and</strong> place of residence/ carer if different). The health visitorconducting the primary visit is responsible for ensuring that the details of all oldersiblings are recorded on the new child’s records <strong>and</strong> that details of the new child arerecorded on the records of all older siblings. When new babies are born into families wheresome / all of the older siblings have gone to school, the health visitor must ensure that allthe school nurses for the older siblings are provided with details of the new child. Theschool nurse(s) will be responsible for ensuring that this information is recorded in theappropriate records <strong>and</strong> that any relevant ‘historical’ information contained within the records isnotified to the health visitor. (Please see appendix for notification form).TransferRefer to the <strong>Safeguarding</strong> <strong>Children</strong> Transfer of <strong>Record</strong>s SOPAuditAudit is a component of the risk management process, the aim of which is the promotion ofquality. An audit trail should be able to enable all records entries to be traceable to a namedindividual at a given date / time <strong>and</strong> that all alterations can be similarly traced. Also – that it canbe seen what has or has not been done <strong>and</strong> why. (The same principles also apply toelectronic records.)A specific audit of health visitor <strong>and</strong> school nurse records for children subject to childprotection plans <strong>and</strong> / or looked after will be conducted annually.Significant Events Form TemplateA significant events form provides an immediately ‘visible’ chronological overview of events<strong>and</strong> concerns.This can be beneficial in a number of ways: when bulky records transfer to or are made available to another practitioner, itenables an ‘overview’ it assists with <strong>and</strong> facilitates the preparation of reports for meetings <strong>and</strong>statements of evidencePage 8 of 12
it enables the practitioner to maintain an ‘at a glance’chronological picture which can inform decisions as to when certain thresholds ofconcern are reachedThe types of information that should be recorded on a significant events form are:Hospital / walk-in centre / clinic admissions / attendancesBirth of a new siblingSignificant incident involving parent or carer (e.g. DV, mental health episode,substance misuse episode, hospital admissionBereavementChild protection / safeguarding incidentSignificant meeting e.g. multi-agency / child in need / conference / review / core group/ LAC review etcChanges of details e.g. health practitioner, G.P., address, school, carer, new adult inhousehold, placement etc.Referral to or from another practitioner / service / agency etcTransfer of records / reason.CAF initiation(This list gives suggestions only – it is not exhaustive by any means)The information recorded on a significant e v e n t s f or m should be brief – its purpose aswell as providing an overview, is to act as a trigger to indicate more detailed informationwithin the records <strong>and</strong> where it can be located.Key Points for Team Leaders / Family Health CoordinatorTeam Leaders/ Family Health Coordinators have accountability for their team members <strong>and</strong>have a responsibility to:Identify <strong>and</strong> address poor professional practiceEnsure appropriate <strong>and</strong> adequate mentoring / preceptorship for all new teammembersEnsure all team members have had appropriate trainingInclude record keeping responsibilities in job descriptions, post outlines <strong>and</strong>annual appraisalsUndertake or assist the undertaking of regular records audits.Page 9 of 12
<strong>Record</strong>s <strong>and</strong> Legal Issues ExerciseChoose the records of a child that you have seen in the past month. Based on whatyou have written in the records, ask yourself the following questions:If the family becomes unhappy with my practice <strong>and</strong> decides to take the case tocourt, am I legally vulnerable on any account?How confident in my record keeping am I, if a child protection case requires acourt hearing <strong>and</strong> I am asked to submit a court report?How confident in my record keeping am I if a case becomes a serious case review?How confident do I feel about senior managers, NHS Trust, Local Authoritysolicitors <strong>and</strong> the Courts seeing my records?How vulnerable would I be if a child’s family <strong>and</strong> their solicitors see my records?If I feel vulnerable about my record keeping – why? If I have to defend my practice on the basis of my record keeping, will I be able to doso? Why or why not?Page 10 of 12
APPENDIX 1Click here to download the formHealth Visitor Request for Historical Family InformationThe named family below have recently had a new birth. Please update your records accordingly. In orderto ensure that we have all the relevant information regarding the family circumstances please could youfill in the questions below?HV Name …………………… Base……………………Contact Number………………….Date of Request………………………………………………Family Surname (please list all alias’)………………………………………………………Name of <strong>Children</strong> Date of Birth School Attending…………………… …………….. ………………………………………………….………………….. ………….. ……………………………………………………………………….. ……………………………………………………………………….Address……………………………………………………………………………………….Mother/carers Name………………………………………………………………………..Father/Partner’s Name…………………………………………………………………….Is there any reference in the records to: (please tick)The Child(ren) ever having been on Child Protection Plan?YES** NOThe Child(ren) ever been Looked After either by Local Authority or by Family orFriend ?Any concerns regarding potential risk to professionals visiting the family home ?Any concerns regarding any individuals living in or visiting the family home?Is there any relevant information within the main body of the child’s record?Is there any relevant supplementary documentation (e.g minutes, reports etc)?Page 11 of 12
Are there any concerns regarding the child(ren) currently?Do you feel it would benefit the health visitor to read the records?** If yes answered to any of the above, the health visitor must arrange to read the records <strong>and</strong>summarise any relevant information on the new child’s record. Alternatively, copies of relevantinformation can be taken <strong>and</strong> placed within the record of the new childPage 12 of 12