Attachment 2 Medco Balance Inquiry Payer Sheet January 2010 To ...
Attachment 2 Medco Balance Inquiry Payer Sheet January 2010 To ...
Attachment 2 Medco Balance Inquiry Payer Sheet January 2010 To ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
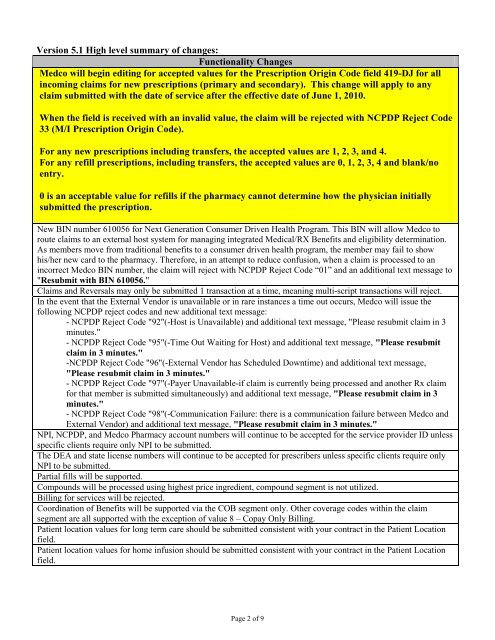
Version 5.1 High level summary of changes:Functionality Changes<strong>Medco</strong> will begin editing for accepted values for the Prescription Origin Code field 419-DJ for allincoming claims for new prescriptions (primary and secondary). This change will apply to anyclaim submitted with the date of service after the effective date of June 1, <strong>2010</strong>.When the field is received with an invalid value, the claim will be rejected with NCPDP Reject Code33 (M/I Prescription Origin Code).For any new prescriptions including transfers, the accepted values are 1, 2, 3, and 4.For any refill prescriptions, including transfers, the accepted values are 0, 1, 2, 3, 4 and blank/noentry.0 is an acceptable value for refills if the pharmacy cannot determine how the physician initiallysubmitted the prescription.New BIN number 610056 for Next Generation Consumer Driven Health Program. This BIN will allow <strong>Medco</strong> toroute claims to an external host system for managing integrated Medical/RX Benefits and eligibility determination.As members move from traditional benefits to a consumer driven health program, the member may fail to showhis/her new card to the pharmacy. Therefore, in an attempt to reduce confusion, when a claim is processed to anincorrect <strong>Medco</strong> BIN number, the claim will reject with NCPDP Reject Code “01” and an additional text message to"Resubmit with BIN 610056."Claims and Reversals may only be submitted 1 transaction at a time, meaning multi-script transactions will reject.In the event that the External Vendor is unavailable or in rare instances a time out occurs, <strong>Medco</strong> will issue thefollowing NCPDP reject codes and new additional text message:- NCPDP Reject Code "92"(-Host is Unavailable) and additional text message, "Please resubmit claim in 3minutes."- NCPDP Reject Code "95"(-Time Out Waiting for Host) and additional text message, "Please resubmitclaim in 3 minutes."-NCPDP Reject Code "96"(-External Vendor has Scheduled Downtime) and additional text message,"Please resubmit claim in 3 minutes."- NCPDP Reject Code "97"(-<strong>Payer</strong> Unavailable-if claim is currently being processed and another Rx claimfor that member is submitted simultaneously) and additional text message, "Please resubmit claim in 3minutes."- NCPDP Reject Code "98"(-Communication Failure: there is a communication failure between <strong>Medco</strong> andExternal Vendor) and additional text message, "Please resubmit claim in 3 minutes."NPI, NCPDP, and <strong>Medco</strong> Pharmacy account numbers will continue to be accepted for the service provider ID unlessspecific clients require only NPI to be submitted.The DEA and state license numbers will continue to be accepted for prescribers unless specific clients require onlyNPI to be submitted.Partial fills will be supported.Compounds will be processed using highest price ingredient, compound segment is not utilized.Billing for services will be rejected.Coordination of Benefits will be supported via the COB segment only. Other coverage codes within the claimsegment are all supported with the exception of value 8 – Copay Only Billing.Patient location values for long term care should be submitted consistent with your contract in the Patient Locationfield.Patient location values for home infusion should be submitted consistent with your contract in the Patient Locationfield.Page 2 of 9