Hypospadias Clinical Pathway - Sydney Children's Hospital
Hypospadias Clinical Pathway - Sydney Children's Hospital
Hypospadias Clinical Pathway - Sydney Children's Hospital
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
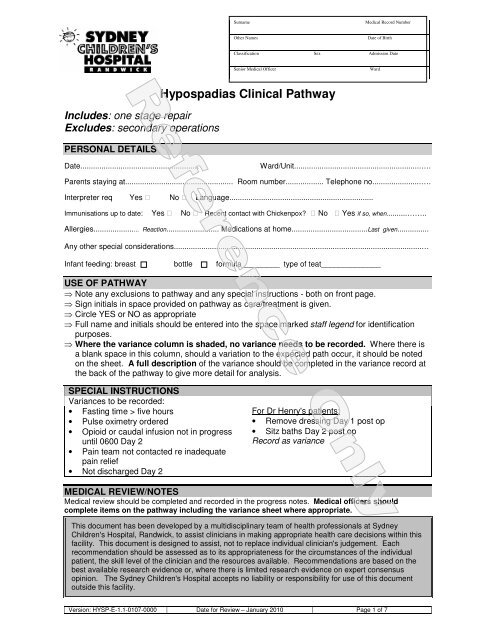
SurnameMedical Record NumberOther NamesDate of BirthClassification Sex Admission DateSenior Medical OfficerWardIncludes: one stage repairExcludes: secondary operationsPERSONAL DETAILS<strong>Hypospadias</strong> <strong>Clinical</strong> <strong>Pathway</strong>Date........................................................Ward/Unit............................................................….Parents staying at................................................... Room number.................. Telephone no.......................….Interpreter req Yes No Language....................................................................Immunisations up to date: Yes No Recent contact with Chickenpox? No Yes if so, when..........……..Allergies...................... Reaction......................... Medications at home....................................Last given...............Any other special considerations.....................................................................................................................…Infant feeding: breast bottle formula_________ type of teat______________USE OF PATHWAY⇒ Note any exclusions to pathway and any special instructions - both on front page.⇒ Sign initials in space provided on pathway as care/treatment is given.⇒ Circle YES or NO as appropriate⇒ Full name and initials should be entered into the space marked staff legend for identificationpurposes.⇒ Where the variance column is shaded, no variance needs to be recorded. Where there isa blank space in this column, should a variation to the expected path occur, it should be notedon the sheet. A full description of the variance should be completed in the variance record atthe back of the pathway to give more detail for analysis.SPECIAL INSTRUCTIONSVariances to be recorded:• Fasting time > five hours• Pulse oximetry ordered• Opioid or caudal infusion not in progressuntil 0600 Day 2• Pain team not contacted re inadequatepain relief• Not discharged Day 2For Dr Henry's patients:• Remove dressing Day 1 post op• Sitz baths Day 2 post opRecord as varianceMEDICAL REVIEW/NOTESMedical review should be completed and recorded in the progress notes. Medical officers shouldcomplete items on the pathway including the variance sheet where appropriate.This document has been developed by a multidisciplinary team of health professionals at <strong>Sydney</strong><strong>Children's</strong> <strong>Hospital</strong>, Randwick, to assist clinicians in making appropriate health care decisions within thisfacility. This document is designed to assist, not to replace individual clinician's judgement. Eachrecommendation should be assessed as to its appropriateness for the circumstances of the individualpatient, the skill level of the clinician and the resources available. Recommendations are based on thebest available research evidence or, where there is limited research evidence on expert consensusopinion. The <strong>Sydney</strong> <strong>Children's</strong> <strong>Hospital</strong> accepts no liability or responsibility for use of this documentoutside this facility.Version: HYSP-E-1.1-0107-0000 Date for Review – January 2010 Page 1 of 7
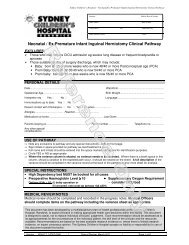
SurnameMedical Record NumberOther NamesDate of BirthClassification Sex Admission DateSenior Medical OfficerWardEXPECTED OUTCOMES♦ Child will not be required to fast for more than 5 hours♦ Opioid or caudal infusion will be in progress until 0600 hours Day 2 for pain relief♦ Analgesia will be effective, and if not effective, pain team/anaesthetist will be contacted♦ Continuous oximetry will be insitu until Day 1 unless ordered by MO thereafter♦ Child will be discharged by Day 2 post opPre admission: Medical questionnaire checked by Anaesthetic registrarParents have contacted Ambulatory care for fasting timeYES/NOYES/NODay of Admission/OperationDate..............................AdmissionWard..................……...E/L/N = nursing shiftsFasted from …………..… Time to theatre…………….(record fasting time of > 5 hours as variance)TPRWeightAnaesthetic review, pre-operative paracetamol chartedCheck consentOrientation to ward/hospitalUnderstanding of admission/processDischarge information/arrangements discussedMO = medical officer V = varianceE L N MO VPost Op in RecoveryInterventions E L MO VContinuous pulse oximetryDocument TPR 1/2 hrly in RecoveryReport to Medical officer prior to transfer to ward if pulse isconsistently >140/min; temp > 38ºC, hypotensionCheck wound for bleedingReport to Medical officer immediately if moderate bleeding orairway impairmentCaudal block given YES / NO (please circle)Drug used (please circle):CLONIDINE FENTANYL ROPIVICAINEOpioid or caudal infusion as ordered by anaesthetist(Record as variance If no opioid or caudal infusion)Intra-operative paracetamol documentedOral analgesia charted prior to leaving recoveryStaff Legendplease print name Initials please print name Initials please print name InitialsVersion: HYSP-E-1.1-0107-0000 Date for Review – January 2010 Page 2 of 7
Date..............................SurnameOther NamesMedical Record NumberDate of BirthWard............................Classification Sex Admission DateSenior Medical OfficerWardPost op in WardOrientation to wardReviewed by Medical OfficerFluid/NutritionMaintain fluid balance chartEnsure urethral stent draining freelyDiet as toleratedObservationsPulse & Respiratory rate hourlyTemp 4 hourlyCheck IV therapy hourly until ceasedContinuous OximetryChange oximetry probe position 4/24(Record as variance if continuous oximetry is not insitu)If analgesia not effective, pain team contacted for furthermanagement YES/NO(Record NO as a variance)HygieneMaintain hygiene- sponge bath onlyMedicationsParacetamol(for pain)max 60mg/kg/day6monthsAs per DURC Guideline 20.8Check if intra-operative dosage givenCaudal infusion / Opioid infusionWound CareObserve for bleeding from woundCheck position of urethral stentCheck glans for colour and circulationActivityBedrestDischarge PlanningDiscuss post discharge arrangements with parentE/L/N = nursing shifts MO = medical officer V = varianceE L N MO VStaff Legendplease print name Initials please print name Initials please print name InitialsThis clinical pathway forms an integral part of the medical recordbut does not replace progress notes. Supplementary informationon a patient’s progress can be obtained from the progress notes.Version: HYSP-E-1.1-0107-0000 Date for Review – January 2010 Page 3 of 7
Date..............................SurnameOther NamesMedical Record NumberDate of BirthWard............................Classification Sex Admission DateSenior Medical OfficerWardDay 1 Post Op in WardE/L/N = nursing shifts MO = medical officer V = varianceInterventions E L N MO VMedical ReviewReviewed by Medical OfficerFluid/NutritionMaintain fluid balance chartEnsure urethral stent draining freelyDiet as desiredObservationsPulse, Respiratory rate and Temp 4 hourlyCheck IV therapy hourly until ceasedContinuous Oximetry as ordered by MO YES/NOChange probe position 4/24(record YES as variance)HygieneMaintain hygiene-sponge bath onlyMedicationsParacetamol max 60mg/kg/day6monthsAs per DURC Guideline 20.8Opioid infusion / caudal infusionWound care with each nappy changeObserve for bleeding from woundCheck position of urethral stentObserve glans for colour and circulationCaudal insertion point visible (if applicable)Removal of finger(outer) dressings- opsite to remain intact)For Dr Henry's patients: remove dressing(Record as variance)Discharge PlanningParental education re care of urethral stentDiscuss post discharge arrangements with parentStaff Legendplease print name Initials please print name Initials please print name InitialsVersion: HYSP-E-1.1-0107-0000 Date for Review – January 2010 Page 4 of 7
SurnameMedical Record NumberDate..............................Other NamesDate of BirthWard............................Classification Sex Admission DateSenior Medical OfficerWardDay 2 post-opE/L/N = nursing shifts MO = medical officer V = varianceE L N MO VMedical ReviewReviewed by Medical OfficerFluid/NutritionMaintain fluid balance chartEnsure urethral stent draining freelyDiet as desiredObservationsObserve woundTemperature, Pulse & Respiratory rate 4 hourlyHygieneSponge onlyFor Dr Henry's patients: Sitz baths(Record as variance)MedicationsOpioid infusion /caudal infusion ceased 0600hrsContinue Paracetamol max 60mg/kg/day6monthsAs per DURC Guidelines 20.8Wound Care with each nappy changeObserve for bleeding from woundCheck position of urethral stentObserve glans for colour and circulationActivityNormal activityDischarge PlanningParent/discharge information given, care of wounddressing and urethral stentDischarge CriteriaProceed to discharge section for discharge criteria,complete the discharge section if patient is for dischargeDischargeDischarge CriteriaDischarge summaryObservations within normal limitsNo bleedingUrethral stent remain insituFollow up appointment in clinicExpected discharge Day 2 post opDATE OF DISCHARGE:………………. TIME:…………….If discharged prior to or after Day 2 , record as varianceRN MO VStaff Legendplease print name Initials please print name Initials please print name InitialsThis pathway was developed by Hypospadius Working GroupDate for review: January 2010Version: HYSP-E-1.1-0107-0000 Date for Review – January 2010 Page 5 of 7
SCH <strong>Clinical</strong> Standards and Practice Manual Hypospadius Working GroupSection 19: <strong>Clinical</strong> <strong>Pathway</strong>s and Guidelines Effective Date: August 2004When you have collected variance in one of the shaded boxes on the pathway,Complete a full explanation of that variance here. Give enough detail so that a full analysisof the variance can be completed. Coding for variance will be completed at data entry.An explanation of codes can be obtained from the <strong>Clinical</strong> <strong>Pathway</strong>s & Guidelines Coordinator.Variance Record SheetSurname Medical Record NumberOther Names Date of BirthClassification Sex Admission DateSenior Medical Officer WardDateEg.01/01/00TimeType of variance Description of Variance Occurrence Code Signature(Include what happened, why it happened and what wasdone about it)Eg. 2400 Eg. Medication not given according to schedule Eg.Patient refused to swallow medication because of the blue colour.Eg. XXMedication altered, dose missed while new prescription filled,improved compliance when changed to colourless liquidFasting time greater than 5 hoursOpioid or caudal infusion not in progress onadmission to recoveryOpioid/caudal infusion not insitu day 1Removal of dressing Day 1 post opOpioid/ caudal not ceased 0600 day 2Sitz baths Day 2 post opAnaesthetist not contacted re analgesia notappropriateContinuous oximetry not insitu post op in wardPlease note: further variance can be found on page 7Version: HYSP-E-1.1-0107-0000 Date for Review – January 2010 Page 6 of 7
SCH <strong>Clinical</strong> Standards and Practice Manual Hypospadius Working GroupSection 19: <strong>Clinical</strong> <strong>Pathway</strong>s and Guidelines Effective Date: August 2004Date Time Type of variance Description of Variance Occurrence(Include what happened, why it happened and what wasdone about it)Continuous oximetry ordered Day 1 post opNot discharged Day 2Day of discharge……………..Other: please stateCodeSignatureVersion: HYSP-E-1.1-0107-0000 Date for Review – January 2010 Page 7 of 7