Our Side of the Story - VSO
Our Side of the Story - VSO
Our Side of the Story - VSO
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Coalition for Health Promotionand Social Development<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>A policy report on <strong>the</strong> lived experienceand opinions <strong>of</strong> Ugandan health workers
HEPS-Uganda, The Coalition for Health Promotion and Social DevelopmentEstablished in 2000, HEPS-Uganda, <strong>the</strong> Coalition for Health Promotion and Social Development,is a health rights organisation that advocates for increased access to affordable essential medicinesfor poor and vulnerable people in Uganda. HEPS promotes pro-people health policies and carriesout campaigns at local, national and regional levels. It also initiates and conducts research necessaryfor health and human rights advocacy. Since 2007, HEPS-Uganda has actively promoted healthrights within seven local government districts, addressing maternal health and equitable access tohealthcare. Working in some <strong>of</strong> <strong>the</strong> most disadvantaged rural areas <strong>of</strong> Uganda, HEPS has trainedcommunity representatives to spread <strong>the</strong> word about health rights and how to exercise <strong>the</strong>m.It also promotes <strong>the</strong> responsible use <strong>of</strong> healthcare resources and effective ways <strong>of</strong> communicatingwith health workers. For more details, visit: www.heps.or.ug<strong>VSO</strong> Uganda<strong>VSO</strong> Uganda volunteers are currently working in <strong>the</strong> central, western and nor<strong>the</strong>rn regions <strong>of</strong> <strong>the</strong>country, in <strong>the</strong> fields <strong>of</strong> participation and governance, disability, health, education and livelihoods.Poor and disadvantaged people in Uganda are badly affected by preventable diseases. Healthservice provision and access is low, and staff retention is a challenge. <strong>VSO</strong> is supporting <strong>the</strong>Ugandan Government in implementing <strong>the</strong> Health Sector Strategic Plan (HSSP) to improve healthsystems in <strong>the</strong> context <strong>of</strong> a decentralised health delivery system at district level. HSSP focuses onworking with communities and <strong>the</strong> implementation <strong>of</strong> primary and preventive healthcare services,as well as good-quality, accessible clinical services as stipulated in <strong>the</strong> minimum healthcarepackage. It has a particular emphasis on reaching <strong>the</strong> majority <strong>of</strong> <strong>the</strong> population, over 80% <strong>of</strong>whom live in rural areas, where <strong>the</strong> people tend to be poorer than in urban settings. For moredetails, visit: www.vsointernational.org/where-we-work/uganda.asp<strong>VSO</strong> International<strong>VSO</strong> is different from most organisations that fight poverty. Instead <strong>of</strong> sending money or food,we bring people toge<strong>the</strong>r to share skills and knowledge. In doing so, we create lasting change.<strong>Our</strong> volunteers work in whatever fields are necessary to fight <strong>the</strong> forces that keep people inpoverty – from education and health through to helping people learn <strong>the</strong> skills to make a living.We have health programmes in 11 countries, with plans to open fur<strong>the</strong>r health programmes in<strong>the</strong> coming years.From extensive experience supporting health and HIV programmes in developing countries,<strong>VSO</strong> believes that in order for health systems to improve, more health workers must be recruitedand retained. They must be <strong>of</strong> good quality, in <strong>the</strong> right places, well trained and with access to<strong>the</strong> basic equipment and drugs needed. They also need to be well supported – placed in <strong>the</strong>right location, treated fairly and managed well.Through our Valuing Health Workers research and advocacy project, <strong>VSO</strong> identifies <strong>the</strong> issuesthat affect health workers’ ability to deliver quality healthcare. These findings will supportpartners to carry out fur<strong>the</strong>r research and make a significant contribution to improvementsin <strong>the</strong> quality <strong>of</strong> health worker recruitment, training and management. For more details visit:www.vsointernational.org/what-we-do/advocacy
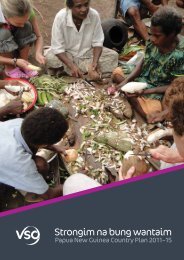
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersAcknowledgementsThe Valuing Health Workers research and advocacy project is <strong>the</strong> initiative <strong>of</strong><strong>VSO</strong> International. This report is based on research in Uganda in partnership withHEPS-Uganda, <strong>the</strong> Coalition for Health Promotion and Social Development, andwith support from <strong>VSO</strong> Uganda. Thanks are due to Rosette Mutambi, executivedirector <strong>of</strong> HEPS-Uganda, Sarah Kyobe, <strong>VSO</strong> Uganda health programme manager,and Stephen Nock, <strong>VSO</strong> International policy and advocacy adviser, for <strong>the</strong>irpractical support and encouragement.Stacey-Anne Penny brought to <strong>the</strong> project her drive to explore and understand<strong>the</strong> lived experience <strong>of</strong> Ugandan nurses and her invaluable contribution asco-researcher up to August 2010. HEPS-Uganda colleagues provided a supportiveand friendly working environment. The following HEPS staff played practical rolesin managing consultative workshops, facilitating access to fieldwork sites andco-convening and transcribing focus group discussions: Prima Kazoora, PhionaKulabako, Aaron Muhinda and Kenneth Mwehonge.This report would not have been possible without <strong>the</strong> willing participation <strong>of</strong>122 health workers across Uganda. Thank you to <strong>the</strong>m for voicing <strong>the</strong> rewardsand challenges <strong>of</strong> <strong>the</strong>ir daily lives. Thank you to local managers for makingstaff available, and to patients for <strong>the</strong>ir forbearance while <strong>the</strong>ir health workersgave time to <strong>the</strong> research. Not least, thanks are due to <strong>the</strong> representatives <strong>of</strong>organisations concerned with health worker and health consumer interests,for <strong>the</strong>ir participation in workshops and interviews.Patricia ThorntonText: Patricia ThorntonField research: Patricia Thornton, Stacey-Anne Penny, Prima Kazoora,Phiona Kulabako, Aaron Muhinda and Kenneth MwehongeEditing: Stephen Nock, Diane Milan, Stephanie Debere and Emily Wooster.Layout: www.revangeldesigns.co.ukPhotography: Cover photo © Mat<strong>the</strong>w Oldfield/Science Photo Library©<strong>VSO</strong> 2012 Unless indicated o<strong>the</strong>rwise, any part <strong>of</strong> this publication may be reproduced withoutpermission for non-pr<strong>of</strong>it and educational purposes on <strong>the</strong> condition that <strong>VSO</strong> is acknowledged.Please send <strong>VSO</strong> a copy <strong>of</strong> any materials in which <strong>VSO</strong> material has been used. For any reproductionwith commercial ends, permission must first be obtained from <strong>VSO</strong>.The views expressed in this report belong to individuals who participated in <strong>the</strong> research and maynot necessarily reflect <strong>the</strong> views <strong>of</strong> HEPS-Uganda, <strong>VSO</strong> Uganda or <strong>VSO</strong> International.ISBN: 978 1903697 3373
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersContentsSummary 61. Introduction 121.1 The <strong>VSO</strong> Valuing Health Workers initiative 121.2 The Valuing Health Workers research in Uganda 121.3 The research approach and participants 141.4 Structure <strong>of</strong> <strong>the</strong> report 142. Healthcare in Uganda: challenges and provision 152.1 Ugandan healthcare challenges 162.2 Formal healthcare provision 192.3 The Ugandan health workforce 213. Research design and methods 253.1 The research stages 253.2 Qualitative research methodology and <strong>the</strong> purposive sampling design 253.3 Data collection 263.4 Data analysis 263.5 The health worker participants 264. The rewards 284.1 Benefiting o<strong>the</strong>rs 284.2 Job satisfaction 284.3 Being recognised, appreciated and valued 294.4 Appreciative and supportive management and colleagues 295. Reasons for becoming a health worker: <strong>the</strong> “right heart” and <strong>the</strong> “wrong heart” 305.1 A passion for <strong>the</strong> patients 305.2 “They join for <strong>the</strong> wrong reasons” 315.3 Recommendations 316. Workload 336.1 The context 336.2 The health worker experience 33Unmanageable workloads 34Too many tasks and responsibilities 34Working day and night 34Over-long shifts and too little time <strong>of</strong>f 34Impacts on health 34Restricted pr<strong>of</strong>essional development 34Failing <strong>the</strong> patients 356.3 Factors contributing to understaffing and work overload 366.4 Recommendations 374
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers7. The facility infrastructure 387.1 The context 387.2 The health worker experience 39Low job satisfaction 39Risks to health workers 39Risks to patients 397.3 Recommendations 408. Equipment and medical supplies 418.1 The context 418.2 The health worker experience 418.3 Recommendations 439. Medicine supplies 449.1 The context 449.2 The health worker experience 449.3 Recommendations 4710. Pay 4810.1 The context 4810.2 The health worker experience 48Money worries 49Failing to meet social expectations 49Disrespect 49Thwarted pr<strong>of</strong>essional ambitions 49Unfair pay 4910.3 Poor pay, turnover and loss to Uganda 5110.4 Recommendations 5211. The way forward 5311.1 Raising <strong>the</strong> voices <strong>of</strong> health workers 5311.2 Changing public perceptions <strong>of</strong> health workers 5511.3 Bridging patient communities and healthcare facilities and staff 5511.4 Summary <strong>of</strong> participants’ recommendations 57Appendix A: Sample details 59Appendix B: Local government structures in Uganda 61References 63Annex: Health worker topic guide 665
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersReasons for becoming a health workerand rewards <strong>of</strong> <strong>the</strong> workThe urge to help, prevent suffering and save lives stood outamong <strong>the</strong> reasons people gave for becoming a health worker.It had been common in rural areas to see people suffer in painand die with no proper medical care. Their training wouldbring to <strong>the</strong> community knowledge to help prevent illnesses,discourage harmful traditional healing practices and save lives.Participants who had been impressed by caring nurses and<strong>the</strong> skills <strong>of</strong> medical staff wanted to give something in return.Interest was stimulated by <strong>the</strong> example <strong>of</strong> family members whoworked in healthcare. Experiencing poor service also prompteda desire to raise healthcare standards.A desire for money was not a driving force. Clinical <strong>of</strong>ficers andmedical doctors told <strong>of</strong> expectations on <strong>the</strong>m as <strong>the</strong> brightestschool students to enter one <strong>of</strong> <strong>the</strong> prestigious pr<strong>of</strong>essions.It was widely believed that new entrants to nursing came with“<strong>the</strong> wrong heart”, resulting in unhappy, disinterested andself-serving recruits, who resorted to bad habits and forgot<strong>the</strong>ir accountability to patients.The benefits to <strong>the</strong> community, to individual patients and to<strong>the</strong>ir own families were <strong>the</strong> biggest sources <strong>of</strong> satisfaction. Jobsatisfaction came from making a difference to patients, doing<strong>the</strong>ir duty <strong>the</strong> best <strong>the</strong>y could, using <strong>the</strong>ir skills and learningthrough work. Health workers valued being appreciated,respected and trusted by patients. Tangible demonstrations <strong>of</strong>appreciation by managers were a huge positive, as were goodteamwork and supportive managers who created opportunitiesfor health workers to raise <strong>the</strong>ir concerns.The impact <strong>of</strong> working conditionsWorkload, workplace infrastructure, medical equipment andsupplies, <strong>the</strong> availability <strong>of</strong> essential medicines and <strong>the</strong> level <strong>of</strong>remuneration affected health workers’ well-being, <strong>the</strong> quality<strong>of</strong> care <strong>the</strong>y could provide and relations with patient communities.It is apparent from health workers’ experiences that workingconditions are <strong>the</strong> root cause <strong>of</strong> <strong>the</strong> attitudes, behaviours andpractices for which health workers have been criticised.WorkloadMinistry <strong>of</strong> Health sources reveal almost half <strong>of</strong> approvedposts at health centres and hospitals are vacant – a shortfall<strong>of</strong> 25,506 staff. There are gross disparities across localgovernment districts, with four districts having less than30% <strong>of</strong> posts filled, while 10 districts filled more than 70%.Unmanageable workloads overwhelmed nurses and made<strong>the</strong>m physically and mentally ill. Too many tasks andresponsibilities led to burn-out. Lack <strong>of</strong> more qualified staffmeant taking on stressful roles beyond <strong>the</strong> scope <strong>of</strong> duty.Participants told <strong>of</strong> working round <strong>the</strong> clock, foregoing mealsand compromising <strong>the</strong>ir health. Overlong shifts and limitedtime <strong>of</strong>f allowed little personal or family time. Feeling <strong>the</strong>ywere failing <strong>the</strong> patients added to health workers’ distress.Hospital nurses torn apart by calls for attention and toomany tasks recognised <strong>the</strong>y could lose <strong>the</strong>ir temper. Midwifebehaviour changed as a result <strong>of</strong> working alone day and night.Long, tiring shifts, when overwhelmed by <strong>the</strong> workload, ledto nurses being short with patients, not interacting with <strong>the</strong>mand conveying disinterest through attitude and expression.7
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersManagers and frontline doctors had seen how hunger madenursing staff bad-tempered and rude to patients. It was saidthat long shifts, toge<strong>the</strong>r with poor pay, led nurses to not turn upfor duty and leave work early. Managers observed that lack <strong>of</strong>opportunity to fulfil <strong>the</strong>ir proper pr<strong>of</strong>essional role demotivatednurses, who <strong>the</strong>n ran out <strong>of</strong> compassion and skip out fromwork. Work overload and staff shortages had impacted oncommunity relations, and participants told <strong>of</strong> aggressiveoutpatients and wrongful accusations <strong>of</strong> neglect <strong>of</strong> duty.Managers explained that financial allocations for salaries stoodin <strong>the</strong> way <strong>of</strong> recruiting more staff and that vacancies persisteddue to bureaucratic procedures. Paradoxically, scarcity <strong>of</strong>staff was a barrier to holding public sector health workers toaccount, as disciplinary procedures might lead to transfer andan even worse workload for remaining staff.InfrastructureAccording to <strong>of</strong>ficial sources, most facilities are in a state <strong>of</strong>disrepair. Many health centres have non-functional operating<strong>the</strong>atres. Only one in four facilities has electricity or a back-upgenerator and only 31% have a year-round water supply.Over half facilities lack transport for patient referral in maternalemergencies and only 6% have technology to communicate.Government sector workers in rural facilities bore <strong>the</strong> brunt<strong>of</strong> infrastructure failures. When <strong>the</strong>atres were unusable,underemployed doctors lost interest and left. Lack <strong>of</strong> electricitycompromised staff and patient safety. At night, patient notescould be not read to ascertain HIV status and deliverieswere carried out by <strong>the</strong> light <strong>of</strong> a mobile phone or a candle.Maternity workers said patients construed <strong>the</strong>ir behaviour asrude or neglectful because <strong>the</strong>y shied away from risk. Lack <strong>of</strong>generator fuel meant operations were completed by torchlight.Nurses feared assault working in unlit wards or crossing darkcompounds, a risk made worse by lockless doors, breaches incompound fences and inadequately equipped or absent guards.A lack <strong>of</strong> water to flush toilets forced staff to return home,fuelling patients’ beliefs <strong>the</strong>y were not at work. Infectioncontrol was near impossible when nursing staff had to beg<strong>the</strong> little water spared by patients’ family attendants to wash<strong>the</strong>ir hands. It was deeply upsetting to know that poor patientswould die because <strong>the</strong> facility had no means <strong>of</strong> transporting<strong>the</strong>m to a hospital that could give <strong>the</strong> treatment <strong>the</strong>y needed.Making transport available to bring patients to <strong>the</strong> facility,supported by easy mobile phone access to staff, was said tobenefit community relations.Equipment and medical suppliesThe Ministry <strong>of</strong> Health acknowledges a shortage <strong>of</strong> basicequipment in health facilities and that only 40% <strong>of</strong> equipmentin place is in good condition. An independent survey revealsa gross lack <strong>of</strong> equipment for <strong>the</strong> diagnosis and treatment<strong>of</strong> malaria, and that six in 10 facilities surveyed were notequipped to measure haemoglobin.Health workers praised well-equipped facilities and imaginativemanagement that solved temporary supply problems byborrowing from o<strong>the</strong>r facilities. Elsewhere, working withinadequate equipment was a huge challenge. There waswidespread frustration at not being able to work effectively.Failing <strong>the</strong>ir patients greatly distressed nurses and doctors,who saw patients die because <strong>of</strong> lack <strong>of</strong> supplies and missingor poorly maintained diagnostic equipment. In <strong>the</strong> governmentsector, doctors and nurses told <strong>of</strong> interruptions in supplies <strong>of</strong>oxygen and blood; missing needles giving sets and sutures,and minimal urine testing kits and family planning supplies.Rural midwives in government facilities told <strong>of</strong> struggling withno delivery kit, cord clamp, sucker, gauze or cotton wool andjust one pair <strong>of</strong> scissors. The regulatory prohibition on askingpatients to buy medical supplies was a huge frustration whichchallenged <strong>the</strong>ir ethical duty to do <strong>the</strong>ir best for <strong>the</strong>ir patients.Managers recognised that doctors lose morale when unable tooperate, and that being unable to apply knowledge was verydemotivating. It was said that nurses forgot what <strong>the</strong>y hadbeen taught and as a result some did not work, so projecting abad image to <strong>the</strong> community, which in turn made nurses feelnot respected and prompted <strong>the</strong>m to leave. Health workers feltblamed for <strong>the</strong> lack <strong>of</strong> supplies. They noted patients’ attitudeschange if asked to buy <strong>the</strong>ir own, with some carers becomingangry and violent.Availability <strong>of</strong> essential medicinesThe proportion <strong>of</strong> health facilities registering ‘stock-outs’ inessential medicines has consistently been over 60% for <strong>the</strong>last 10 years. Not one <strong>of</strong> 40 essential medicines was availablein every government facility in a sample survey in <strong>the</strong> secondquarter <strong>of</strong> 2010. Only eight were found in each not-for-pr<strong>of</strong>itsector facility surveyed.Participants working outside <strong>the</strong> government sector mostlyconsidered medicine supplies adequate. In <strong>the</strong> governmentsector <strong>the</strong>re was sharp contrast between praise for <strong>the</strong> betterstocked facilities and disgruntlement that essential drugs were8
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersused up in a matter <strong>of</strong> weeks or even days. Complaints centredon undersupply for population demand; shortfalls in supplywhere deliveries did not match orders; erratic deliveries (such asoversupply <strong>of</strong> condoms but no anti-malaria drugs) and irregulardeliveries which did not conform to promised quarterly schedules.Unable to give <strong>the</strong>ir patients <strong>the</strong> drugs <strong>the</strong>y needed, healthworkers became demoralised by <strong>the</strong> futility <strong>of</strong> <strong>the</strong>ir roles,and <strong>the</strong>ir self-esteem suffered when patients lost confidencein <strong>the</strong>m. Health workers grieved for <strong>the</strong>ir patients’ sufferingfrom <strong>the</strong> lack <strong>of</strong> medicines, such as antiretroviral drugs, whichshould be taken on a lifelong basis. Helplessness was hard tobear when <strong>the</strong>y felt forced to tell poor patients to buy <strong>the</strong>irmedication in <strong>the</strong> private market. Health workers struggledwith disappointed patients and <strong>the</strong>ir limited understanding <strong>of</strong>reasons for shortfalls in supplies. They also told <strong>of</strong> angry, bitterpatients who cursed <strong>the</strong>m and refused to listen. They said thatcommunities served by government facilities assumed healthworkers took <strong>the</strong> drugs.There was widespread indignation at accusations <strong>of</strong> stealingnon-existent medications. Health workers resented negativestories in <strong>the</strong> media and felt that local leaders and politiciansmade matters worse when <strong>the</strong>y failed to present <strong>the</strong> truepicture to complaining patients, and even accused healthworkers in front <strong>of</strong> patients. There was hurt and indignationabout top public figures spoiling <strong>the</strong> pr<strong>of</strong>essions’ reputationsby stating publicly that health workers are thieves.PayUgandan nurses’ and doctors’ salaries are <strong>the</strong> lowest in EastAfrica. Monthly starting salaries in public service in 2009-10were 353,887 UGX (Ugandan Shillings) ($US 191) for a registerednurse and 657,490 UGX (($US 354) for a medical <strong>of</strong>ficer. Highcourt judges received 6.8 million UGX (($US 3,664) per month. 1Nursing staff spoke heatedly about <strong>the</strong>ir struggles to surviveon low pay and support <strong>the</strong>ir dependents, see <strong>the</strong>ir childrenthrough education, pay for a ro<strong>of</strong> over <strong>the</strong>ir heads, settleessential bills, afford transport to work and save towards<strong>the</strong> costs <strong>of</strong> fur<strong>the</strong>r training. Financial worries added to <strong>the</strong>stresses caused by impoverished workplaces. Doctors feltsocially embarrassed when <strong>the</strong>y could not contribute largesums <strong>of</strong> money at functions held to raise funds for weddings orfunerals, or meet expectations to help with school fees. It wassaid that patients look down on nurses when <strong>the</strong>y know howlittle <strong>the</strong>y are paid. Participants voiced strong opinions that<strong>the</strong> pay was unfair and undervalued health workers. Nursescomplained that <strong>the</strong>ir salaries did not reflect <strong>the</strong> years <strong>of</strong> study<strong>the</strong>y had put in, and going unrewarded for doing <strong>the</strong> samework as higher grade staff was thought bitterly unfair. Doctorsbeing paid less than secretaries and drivers in some statutoryagencies underscored <strong>the</strong> little value attached to <strong>the</strong> medicalpr<strong>of</strong>ession in Uganda. Salaries were doubly unfair because <strong>the</strong>ydid not reflect <strong>the</strong> long hours many health workers put in.Participants acknowledged that poverty led to bad practices –minimal effort, late arrival at work, venting <strong>of</strong> frustrations onpatients, small-scale pilfering <strong>of</strong> drugs and accepting money<strong>of</strong>fered by patients. It was widely believed that urban healthworkers were forced to work in two or even three jobs to makeends meet, leading to exhaustion and behaviour which patientsperceived as rude.Better pay was not an overriding consideration for workingoutside Uganda. Nurses explained <strong>the</strong>y were looking for anenvironment where <strong>the</strong>ir work would be respected andwhere <strong>the</strong>y could learn about different medical conditions,use equipment <strong>the</strong>y were trained to use, update <strong>the</strong>ir skillsand have <strong>the</strong> chance to advance pr<strong>of</strong>essionally. Doctors spokeabout <strong>the</strong> attraction <strong>of</strong> a better income from work abroad, butopportunities to use proper equipment and enjoy <strong>the</strong> workalso were important.Conclusions and participants’recommendationsHealth workers’ accounts show that working conditions were<strong>the</strong> root causes <strong>of</strong> bad practices and unethical behaviour, andthat health workers bore <strong>the</strong> brunt <strong>of</strong> <strong>the</strong> blame for systemfailures. The research revealed a vicious circle: impoverishedworking environments and low pay affected <strong>the</strong> quality <strong>of</strong>patient care; patients blamed <strong>the</strong> health workers; <strong>the</strong> widercommunity <strong>the</strong>n distrusted health workers and so healthworkers’ distress increased. The situation was made worse bynegative media stories and political leaders’ vocal criticism <strong>of</strong>health workers, which fuelled public distrust, damaged <strong>the</strong>standing <strong>of</strong> <strong>the</strong> pr<strong>of</strong>ession, added to health workers’ distressand raised <strong>the</strong> barriers to access to healthcare.The view <strong>of</strong> civil society organisations and <strong>of</strong> some managers wasthat frontline health workers are not empowered to speak up.The concept <strong>of</strong> ‘voice’ was unfamiliar to many frontline healthworkers in <strong>the</strong> research, and <strong>the</strong> idea that <strong>the</strong>y might speak outand gain support to improve poor working conditions and quality<strong>of</strong> care was new to <strong>the</strong>m. The research identified barriers toindividual health workers voicing <strong>the</strong>ir concerns, and healthworkers’ preferences for advocacy by representative organisations.1. US dollar = 1,856 Ugandan Shillings at 31 March 20109
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersThe findings identified two priorities for action:1. to value health workers for <strong>the</strong>ir contributions to <strong>the</strong> health<strong>of</strong> Ugandans2. to expose <strong>the</strong> poor working conditions that prevent healthworkers from providing good quality healthcare.Four enabling strategies emerged from health workers’accounts and stakeholder advice:1. to improve <strong>the</strong> quality and relevance <strong>of</strong> training2. to raise <strong>the</strong> voices <strong>of</strong> health workers through representation3. to change public perceptions through <strong>the</strong> media4. to build bridges with patient communities.Priorities1. Value health workers for <strong>the</strong>ir contributionsto <strong>the</strong> health <strong>of</strong> UgandansHealth worker terms and conditions <strong>of</strong> service• Review salary scales to determine whe<strong>the</strong>r increases inbasic salaries are possible. Reform government salaryscales to recognise first and postgraduate degrees, in orderto attract degree nurses to public sector jobs and ensure<strong>the</strong>ir education is used to support patient care directly.• Consider <strong>the</strong> establishment <strong>of</strong> a minimum wage and<strong>the</strong> feasibility <strong>of</strong> imposing <strong>the</strong> same salary structurein all sectors (government, not-for-pr<strong>of</strong>it and private).Overtime and responsibility payments• Explore a system for remunerating health workers for overtime.• Consider implementing a responsibility allowance paid whena nurse has sole charge <strong>of</strong> a ward.Small financial motivations• Incentivise staff through small items <strong>of</strong> personal support, suchas food for <strong>the</strong> household, snacks at work, and Christmas andEaster gifts. Contributions towards family burials, medicaloperations and provision <strong>of</strong> cloth for uniforms are well received.• Review current allowances for risk, hardship, housing,transport, responsibility and study, to ensure consistencyand fairness across all facilities.• Use <strong>the</strong> income from local government hospitals’ privatewings to benefit staff, by supplementing salaries or allowances.2. Ensure working conditions enable healthworkers to provide good-quality healthcareHealth worker/patient ratios• Introduce standards for patient/nurse and patient/doctorratios, so that health worker overload is transparent andquantifiable, and managers have information to help reducepressure on overloaded staff.Recruitment blockages• Manage health worker recruitment and deploymentcentrally, to address <strong>the</strong> problem <strong>of</strong> unfilled posts anduneven distribution <strong>of</strong> health workers.Decent staff accommodation• The Government should follow through on its strategy toprovide decent and safe accommodation for health workersat health facilities, especially in remote areas. Civil societyorganisations should continue to monitor implementation<strong>of</strong> this strategy and press for concrete targets.Facility infrastructure• Ensure regular meetings between management anddepartment heads, at which facility-related problemscan be raised and decisions taken on actions needed.• Invest in good <strong>the</strong>atre facilities and <strong>the</strong>ir staffing in a smallnumber <strong>of</strong> level IV health centres, and showcase <strong>the</strong>m asgood practice before embarking on fur<strong>the</strong>r investment.Equipment, medical and medicine supplies• Give much more attention to <strong>the</strong> maintenance and quickrepair <strong>of</strong> medical equipment, including systems for monitoringequipment maintenance and adequate stocks <strong>of</strong> spare parts.• Hold regular formal consultations with frontline workersto enable <strong>the</strong>m to participate in decision-making aboutequipment and supplies, and to improve transparencyin equipment procurement processes.• Encourage international donors to provide large items<strong>of</strong> equipment directly.Enabling strategies1. Improve <strong>the</strong> quality and relevance<strong>of</strong> health worker trainingCareer guidance and early contact• Ensure well-motivated trainees, for example throughmore talks at schools and work experience placements.Training schools’ admission procedures• Reject applicants who seem to be applying for <strong>the</strong> “wrongreasons”, including those allocated to a university coursewhich is not <strong>the</strong>ir first or second choice.Developing and sustaining “<strong>the</strong> right heart” in training schools• Return oversight <strong>of</strong> training to <strong>the</strong> Ministry <strong>of</strong> Health from<strong>the</strong> Ministry <strong>of</strong> Education and Sports.• Reduce nursing and midwifery class-sizes and improvetutor capacity, to ensure <strong>the</strong> right attitudes and practicalunderstanding <strong>of</strong> <strong>the</strong> ethical code are encouragedthroughout pre-qualification training.10
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersHealth and human rights training• Expand existing partnerships between training institutionsand health consumer advocacy organisations. Improvenursing course content to make sure that students takeon board <strong>the</strong> role <strong>of</strong> <strong>the</strong> nurse as a patient’s advocate.De-urbanise health worker training• Increase <strong>the</strong> number <strong>of</strong> training schools and residencyprogrammes in rural areas to produce staff already adaptedto rural environments and connected to <strong>the</strong> local community.• Improve <strong>the</strong> community service element in medical curriculaand increase <strong>the</strong> exposure <strong>of</strong> urban health students to ruralsettings with increased fieldwork.Nurses and Midwives Council registration interviews• The Nurses and Midwives Council should weigh up <strong>the</strong>advantages <strong>of</strong> screening interviews held as a prerequisitefor registration post-qualification against detrimentaleffects on nurse morale.2. Raise <strong>the</strong> voices <strong>of</strong> health workersSharing <strong>of</strong> experience and common approaches• Encourage staff to meet with people from o<strong>the</strong>r healthcarefacilities to discuss solutions to common problems andcommunicate <strong>the</strong>m to sub-district level managers. Thesemanagers could also be encouraged to instigate similar forums.Speaking through pr<strong>of</strong>essional associations, unions andregulatory councils• Channel health worker concerns to <strong>the</strong> Ministry <strong>of</strong> Health,Government or Parliament through bodies that speak for<strong>the</strong>m, such as pr<strong>of</strong>essional organisations and trade unions.• Pr<strong>of</strong>essional associations and unions should do more to bringmembers toge<strong>the</strong>r, for instance at local general meetings,and make greater efforts to visit facilities and talk with healthworkers so that <strong>the</strong> “right voices” can be taken to <strong>the</strong> top.They should compile strong collective arguments to improveconditions in <strong>the</strong> workplace, as well as addressing individualgrievances and traditional welfare issues.• The Health Workforce Advocacy Forum – Uganda (a coalition<strong>of</strong> health pr<strong>of</strong>essional associations, unions and health rightsorganisations) should expand its membership and continue itscampaign for a positive practice environment for health workers.3. Change public perceptions by influencing <strong>the</strong> media• Inform journalists about <strong>the</strong> obstacles to health workerrecruitment and discourage <strong>the</strong>m from writing sensationalistor negative stories in <strong>the</strong> media. Put complaints on locallanguage radio call-in shows into a wider context. Encourage<strong>the</strong> running <strong>of</strong> positive human interest features, such aspr<strong>of</strong>iles <strong>of</strong> individual health workers and <strong>the</strong> work <strong>the</strong>y do.Work with <strong>the</strong> Uganda Health Communication Alliance.• Improve <strong>the</strong> capacity <strong>of</strong> civil society and health workerorganisations to write press releases, hold press conferencesand build relationships with individual reporters and mediahouses, so <strong>the</strong> key campaign messages hit home.4. Build bridges between patient communities,healthcare facilities and staffTransparency on drug availability• Use well-managed public opening <strong>of</strong> medicine deliveries tohelp convince communities that medicines are not in stock,and to counter accusations <strong>of</strong> <strong>the</strong>ft. Call on local notables,police or patients to witness <strong>the</strong> opening <strong>of</strong> boxes. Supportwith paperwork to show what has been ordered and delivered.• Ensure that local leaders are fully informed through regularmeetings about <strong>the</strong> demand for and supply <strong>of</strong> drugs and that<strong>the</strong>y use this information responsibly.Connecting communities and facilities• Use opportunities to talk with people on <strong>the</strong>ir own groundand explain <strong>the</strong> problems health workers face, for instancethrough Village Health Teams, facility-based health workersproviding outreach immunisation services, and talks towomen awaiting prenatal checks.• Promote ‘community dialogue’ meetings bringing toge<strong>the</strong>rservice users, local leaders and health unit managementteams. Increase funds to cover <strong>the</strong>se activities.• Invite top local politicians to spend time in facilities alongsidestaff to see what <strong>the</strong> work is really like.• Civil society organisations should continue <strong>the</strong>ir work tocreate common cause between health workers and patients.11
1. Introduction1.1 The <strong>VSO</strong> Valuing HealthWorkers initiativeWhat is life like working in healthcare ina low-income country? What promptsnurses, midwives and doctors to takeup <strong>the</strong>ir pr<strong>of</strong>essions and what are <strong>the</strong>rewards? What do health workers sayabout <strong>the</strong> barriers <strong>the</strong>y face in providingaccess to healthcare? What in <strong>the</strong>ir viewneeds to change? And how can <strong>the</strong>ir voicesbe heard? <strong>VSO</strong>’s Valuing Health Workersinitiative is listening to <strong>the</strong> experiences <strong>of</strong>health workers and ga<strong>the</strong>ring evidence toadvocate for change.The lived experience and opinions <strong>of</strong> health workersare rarely recorded in <strong>the</strong> many explorations <strong>of</strong>solutions to <strong>the</strong> health worker crisis affecting <strong>the</strong>developing world. Health workers are commonlyseen as ‘human resources’, as a part <strong>of</strong> a healthcaredelivery mechanism to which ‘levers’ may be applied,and not as human beings whose individual actions areinfluenced by <strong>the</strong> societies and conditions in which<strong>the</strong>y live and work. Ra<strong>the</strong>r, performance managementtechniques and incentives to attract and retain staffdominate research and policy.<strong>VSO</strong> International set out to redress this imbalancethrough its Valuing Health Workers research andadvocacy initiative. Recognising that health workers’voices must be heard and acted on to improve accessto healthcare, and so help to achieve <strong>the</strong> MillenniumDevelopment Goals, <strong>VSO</strong> International startedparticipatory research in four countries in Africa andAsia, in partnership with in-country non-governmentalorganisations. <strong>VSO</strong> will support local partners to use<strong>the</strong> research findings to advocate for health workers in<strong>the</strong>ir countries, and will ga<strong>the</strong>r <strong>the</strong> research evidenceto advocate on a global level.1.2 The Valuing Health Workersresearch in UgandaIn Uganda negative images <strong>of</strong> health workers areprojected in <strong>the</strong> media, political speeches, policydocuments, healthcare user research and healthconsumer advocacy work. The overriding messageis that health workers’ attitudes, behaviour andpractices present barriers to accessing healthcare.The Valuing Health Workers research in Ugandaset out to explore with frontline health workersand <strong>the</strong>ir managers <strong>the</strong> conditions underlyingaccusations <strong>of</strong> unethical behaviour and serviceinadequacies. The overall objective was to giveopinion formers and healthcare service usersa realistic picture <strong>of</strong> what life is like as a healthworker in Uganda, so as to increase understandingand modify expectations. Ugandan civil societyorganisations will use <strong>the</strong> findings to help buildmutual understanding and promote harmoniousrelationships between healthcare users andworkers, as well as to advocate for improvedconditions for health workers in Uganda.It has been well-documented through researchand health rights projects that healthcareusers in Uganda experience from health workersbad attitudes, rudeness, inhumane treatment,neglect, discrimination and extortion <strong>of</strong> illegalfees for services. They also face staff absencesand <strong>the</strong> unavailability <strong>of</strong> medicines and o<strong>the</strong>rtreatment supplies. 2 Research has reportedpatient community perceptions that drugs arestolen. 3 The press and radio media have fuellednegative perceptions <strong>of</strong> health workers’ behaviour,branding <strong>the</strong>m as shirkers and thieves. 4 Indeed,<strong>the</strong> media have reported leaders in governmentaccusing health workers <strong>of</strong> stealing medicines.2. See Kiwanuka et al 2008 for a systematic research review3. Kiguli et al 20094. Medicines and Health Service Delivery Monitoring Unit2010 lists 43 press articles in under one year, almost allreporting negatively on health worker behaviour
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersEven Ugandan health policy documents have commentednegatively on health workers’ low productivity, high absencerates, poor attitudes and lack <strong>of</strong> accountability to clientcommunities. Organisations promoting health rights have seendistrust and hostility among communities and some defensivereactions among health facility staff.Health workers in Uganda face harsh working conditions.The Ugandan Ministry <strong>of</strong> Health acknowledges staff shortages,inadequate pay, poor worksites, risk and insecurity in <strong>the</strong>workplace, limited and poor-quality staff accommodation,and harassment; it also recognises that staff endure poorsupervision and leadership and a lack <strong>of</strong> promotion, trainingopportunities and career progression. 5 Facilities and equipmentin states <strong>of</strong> disrepair, and shortages and wastage <strong>of</strong> medicines,have been pervasive problems. 6Yet little attention has been paid to <strong>the</strong> impacts <strong>of</strong> workingconditions on <strong>the</strong> lives <strong>of</strong> healthcare staff, and so on <strong>the</strong> quality<strong>of</strong> services <strong>the</strong>y can provide. Research on or with Ugandanhealth workers has focussed on workforce retention questions,such as migration, intent to migrate and turnover. 7 It hasmeasured job satisfaction and quantified work factors related tointent to stay or leave. 8 A second area <strong>of</strong> research has measuredhealth workers’ informal income generation practices, such asspending working hours engaged in agriculture and operatingprivate clinics, and has quantified absenteeism. 9 10 Certainly,some research reports include <strong>the</strong> voiced experiences <strong>of</strong> healthworkers. 11 But only exceptionally has research started from <strong>the</strong>viewpoint <strong>of</strong> health staff as workers and members <strong>of</strong> familiesand communities, as opposed to <strong>the</strong> viewpoint <strong>of</strong> <strong>the</strong> system. 12Only one study has focussed on <strong>the</strong> distress and emotional toll <strong>of</strong>working with insufficient resources for acceptable levels <strong>of</strong> care. 13The starting assumption <strong>of</strong> <strong>the</strong> Valuing Health Workers researchin Uganda was that health workers are unfairly blamed forattitudes and behaviour caused by <strong>the</strong> system in which <strong>the</strong>y work.Health workers are human beings – men and women with <strong>the</strong>irown worries, working in very challenging circumstances – and<strong>the</strong>y develop ways <strong>of</strong> coping with difficulties, frustrations andbeing under-valued. The research does not condone unethicalor unpr<strong>of</strong>essional behaviour and dereliction <strong>of</strong> duty, but it doesnot brand as ‘quiet corruption’ absences from <strong>the</strong> workplaceand external income-generating activities. 14 Such ‘moralisingfinger-wagging’ 15 , which addresses issues in terms <strong>of</strong> lack <strong>of</strong>motivation, corruption and betrayal <strong>of</strong> pr<strong>of</strong>essional codes <strong>of</strong>conduct, diverts attention from structural conditions and socialand cultural environments. 16The research set out to challenge <strong>the</strong> overwhelmingly negativecommentary on Ugandan health workers. It wanted to hear <strong>the</strong>positive side from health workers <strong>the</strong>mselves: <strong>the</strong>ir passion for<strong>the</strong>ir pr<strong>of</strong>essions, commitment to patients and communities,determination to give <strong>the</strong>ir best and <strong>the</strong> satisfaction gainedfrom contributing what <strong>the</strong>y can.The research was especially concerned to find ways <strong>of</strong>bridging <strong>the</strong> seemingly widening gap between communitiesand healthcare facility staff. Projects on <strong>the</strong> ground in Ugandahave tended to focus on promoting <strong>the</strong> rights <strong>of</strong> healthcareusers and increasing <strong>the</strong> community role in monitoring healthworkers. 17 While less attention has been given to <strong>the</strong> healthworker side, community-based projects have latterly fosteredmutually respectful relationships. 18 Research in Uganda and fiveo<strong>the</strong>r African countries recommended improved understanding<strong>of</strong> <strong>the</strong> roles <strong>of</strong> health workers and encouragement <strong>of</strong> mutualrespect through better communication and interaction. 195. Ministry <strong>of</strong> Health 20066. Ministry <strong>of</strong> Health 2010a; 2010b7. Awases et al 2004; Dambisya 2004; Nguyen et al 2008; Onzubo 2007; O’Neil and Paydos 20088. Ministry <strong>of</strong> Health 2009a; Hagopian et al 20099. McPake et al 1999; McPake et al 200010. Chaudhury et al 2006; UNHCO 201011. Ministry <strong>of</strong> Health 2009a; UNFPA Uganda Country Office 200912. Kyaddondo and Whyte 200313. Harrowing and Mill 2010; Harrowing 201114. World Bank 201015. Van Lerberghe et al 2000 p316. Schwalbach et al 200017. Björkman and Svensson 200718. Muhinda et al 200819. Awases et al 200413
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers1.3 The research approachand participants<strong>VSO</strong> carried out <strong>the</strong> research in Uganda from February 2010 toFebruary 2011 in partnership with HEPS-Uganda, <strong>the</strong> Coalitionfor Health Promotion and Social Development.Using qualitative research methods, <strong>the</strong> researchersencouraged health workers to speak freely in response to openquestions, promising that identities would not be revealed.In all, 122 health workers – medical doctors, clinical <strong>of</strong>ficers,nurses, midwives and nursing assistants (including frontlineworkers, facility managers and local government district health<strong>of</strong>ficers) – participated in small group discussions and individualinterviews at <strong>the</strong>ir workplaces. The facility-based participantswere working at 18 hospitals and health centres in seven localgovernment districts in all regions <strong>of</strong> Uganda and in <strong>the</strong> capitalcity, Kampala. The selection <strong>of</strong> facilities took account <strong>of</strong> region,<strong>the</strong> extent to which <strong>the</strong> district was easy or hard to serve, <strong>the</strong>level <strong>of</strong> hospital and health centre, location (urban or rural) andownership (government, not-for-pr<strong>of</strong>it or private sector). Manyparticipants drew on <strong>the</strong>ir prior experiences from training orworking in different sectors and levels <strong>of</strong> healthcare facility.1.4 Structure <strong>of</strong> <strong>the</strong> reportChapter 2 introduces <strong>the</strong> main challenges to healthcareprovision in Uganda, outlines healthcare provision andpatterns <strong>of</strong> use, and describes <strong>the</strong> health workforce.The research approach is described in Chapter 3, along with anoverview <strong>of</strong> <strong>the</strong> participants (with fur<strong>the</strong>r details in Appendix A).Chapter 4 presents what participants said about <strong>the</strong> rewards<strong>of</strong> being a health worker. Chapter 5 looks at why <strong>the</strong>y becamehealth workers.The chapters that follow address elements <strong>of</strong> <strong>the</strong> main <strong>the</strong>mesthat emerged from <strong>the</strong> participatory research – <strong>the</strong> impacts<strong>of</strong> workload (Chapter 6); <strong>the</strong> infrastructure <strong>of</strong> <strong>the</strong> healthcarefacilities (Chapter 7); <strong>the</strong> availability <strong>of</strong> medical equipment andsupplies (Chapter 8); supplies <strong>of</strong> medicines (Chapter 9); andlevels <strong>of</strong> remuneration (Chapter 10).Each element is followed by <strong>the</strong> relevant recommendationsfor change drawn from health workers’ and stakeholders’contributions. Chapter 11 lists all recommendations underpotential strategies for change.In addition, 24 stakeholders from civil society organisations,trades unions, pr<strong>of</strong>essional associations and regulatory councilscontributed <strong>the</strong>ir perspectives on <strong>the</strong> issues facing healthworkers in Uganda, through workshops and individual interviews.14
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers2. Healthcare in Uganda:challenges and provisionSummaryA major challenge for <strong>the</strong> Ugandan healthcare system is <strong>the</strong>rapidly growing population, with <strong>the</strong> third-highest growth ratein <strong>the</strong> world and a strikingly high birth rate (especially amongteenage women) and a very young pr<strong>of</strong>ile. A fur<strong>the</strong>r challengeis serving <strong>the</strong> exceptionally high proportion <strong>of</strong> <strong>the</strong> populationresiding in rural areas, who have extremely poor access toelectricity and low access to improved water supplies. Althoughdeclining somewhat, maternal, infant and under-five deathrates are still not under control. Malaria is <strong>the</strong> main sicknessand a major cause <strong>of</strong> childhood deaths.Uganda has only one doctor per 10,000 people, and only14 health workers (doctors, nurses and midwives) per 10,000people. This is significantly below <strong>the</strong> level <strong>of</strong> 23 healthworkers per 10,000 people recommended by <strong>the</strong> World HealthOrganisation (WHO). Only four o<strong>the</strong>r countries have poorerprovision <strong>of</strong> hospital beds. Only 16 countries worldwide spendsmaller proportions <strong>of</strong> <strong>the</strong>ir Gross Domestic Product on healththan Uganda. Although <strong>the</strong> Government <strong>of</strong> Uganda is committedunder <strong>the</strong> Ajuba declaration to apportion 15% <strong>of</strong> its budget tohealth, its expenditure on health has never exceeded 10% <strong>of</strong>total public expenditure.Most healthcare in <strong>the</strong> formal system is delivered at healthcentres and at hospitals at national, regional and district levels.One in five local government districts had no hospital whenan <strong>of</strong>ficial inventory <strong>of</strong> <strong>the</strong> (<strong>the</strong>n) 80 districts was drawn up in2010. Each sub-district should have a health centre IV, headedby a medical doctor and providing emergency surgery: five <strong>of</strong><strong>the</strong> 80 districts in <strong>the</strong> inventory had no health centre IV at alland a fur<strong>the</strong>r 23 had one only. The situation is likely to haveworsened with <strong>the</strong> continuing creation <strong>of</strong> districts, to total 112in mid-2010. One in four facilities is classified as a health centreIII and should provide maternity, in-patient and laboratoryservices. Two-thirds <strong>of</strong> health facilities are classed as healthcentre II, intended for preventive services and outpatientcurative care; three in 10 <strong>of</strong> those are in <strong>the</strong> capital city.The Government runs 60% <strong>of</strong> <strong>the</strong> hospitals and health centres.Not-for-pr<strong>of</strong>it organisations, mostly faith-based, run just under20%. Private for-pr<strong>of</strong>it organisations run just over 20% <strong>of</strong> <strong>the</strong><strong>of</strong>ficially-classified healthcare facilities, mainly in urban areas.There are also innumerable unrecognised small private units.Fewer than four in ten Ugandans turn to health centres orhospitals when <strong>the</strong>y fall sick. The rural population uses healthcentres more than urban dwellers, while <strong>the</strong> urban populationuses hospitals more than people in rural areas. The poorer youare in Uganda, <strong>the</strong> more likely you are to go to a governmen<strong>the</strong>alth centre. Children and pregnant women are <strong>the</strong> largestgroups <strong>of</strong> health facility patients. Over one in four Ugandanslives more than five kilometres from <strong>the</strong>ir nearest health facility.Nine in 10 walk or cycle to <strong>the</strong>ir government health centre.The available data on <strong>the</strong> make-up <strong>of</strong> <strong>the</strong> Ugandan healthworkforce shows extreme shortfalls <strong>of</strong> <strong>the</strong> most highly qualifiedoccupational groups, and mal-distribution across <strong>the</strong> country.Although <strong>the</strong> aim is to phase nursing assistants out, Ugandahas relied heavily on <strong>the</strong>m , especially in rural areas. Medicaldoctors and <strong>the</strong> most highly qualified midwives and nursesare concentrated in urban areas, especially in and around<strong>the</strong> capital city. An estimated four in 10 <strong>of</strong> <strong>the</strong> facility-basedworkforce are in <strong>the</strong> government sector, 30% in <strong>the</strong> not-forpr<strong>of</strong>itand 30% in <strong>the</strong> private sector. Medical doctors areconcentrated in <strong>the</strong> private sector although <strong>the</strong>re are high rates<strong>of</strong> dual employment, with medical doctors working in bothprivate and government sectors. Half <strong>the</strong> medical doctors andfour in ten nurses employed in government facilities work in<strong>the</strong> regional and national referral hospitals.15
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers2.1 Ugandan healthcare challengesUganda is one <strong>of</strong> <strong>the</strong> 48 least-developed countries <strong>of</strong> <strong>the</strong> world. 20It stands at 143 out <strong>of</strong> <strong>the</strong> 169 countries in <strong>the</strong> United NationsHuman Development Index, and is classed as a low humandevelopment country. The United Nations DevelopmentProgramme (UNDP) publishes statistics for <strong>the</strong> indicatorsused in <strong>the</strong> Human Development Index. 21 These allowcomparisons between Uganda and o<strong>the</strong>r least-developedcountries, Sub-Saharan Africa and <strong>the</strong> world overall. 22Table 1Estimated population 2010 23Total population: 30.7 millionAged 0-14 years 50.8%Aged 14-64 years 46.1%Aged 65+ years 3.1%Table 2Population growth and birth ratesUganda’s rate <strong>of</strong> population growth (3.2 %) is <strong>the</strong> third-highestin <strong>the</strong> world. It is a very young population with an average age<strong>of</strong> 15.6 years, <strong>the</strong> second-lowest in <strong>the</strong> world. The averagewoman will give birth to 5.9 children if she lives to <strong>the</strong> age<strong>of</strong> 50; only three countries have a higher fertility rate thanUganda. The birth rate among women aged 15 to 19 is alsostriking: 150 per 1000 women, which is considerably higherthan in Sub-Saharan Africa overall and is surpassed in onlytwo countries in <strong>the</strong> world. The contraceptive prevalence rate(23.6%) is on a par with that <strong>of</strong> Sub-Saharan Africa.Infant, under-five and maternal mortalityIn Uganda, 85 <strong>of</strong> every thousand babies born alive are likelyto die before <strong>the</strong>ir first birthday (<strong>the</strong> infant mortality rate) and135 <strong>of</strong> every thousand are likely to die before <strong>the</strong>y are five (<strong>the</strong>under-five mortality rate). These rates are somewhat higherthan for least-developed countries overall and somewhat lowerthan for Sub-Saharan Africa, yet <strong>the</strong>y are close to twice globalrates. Maternal deaths (<strong>the</strong> death <strong>of</strong> women while pregnant orwithin 42 days <strong>of</strong> <strong>the</strong> end <strong>of</strong> pregnancy) are estimated by UNDPto be 550 for every 100,000 live births, a considerably betterratio than across Sub-Saharan Africa, but twice <strong>the</strong> global ratio. 24At 54.1 years, life expectancy stands above that <strong>of</strong> Sub-SaharanAfrica but falls far short <strong>of</strong> <strong>the</strong> 69.3 years in <strong>the</strong> world overall.Population growth and mortality indicators in international context 25UgandaSub-SaharanAfricaLeast-DevelopedCountriesWorldAverage annual population growth (2010-15) (%) 3.2 2.4 2.2 1.1Median age (2010) 15.6 18.6 19.9 29.1Total fertility rate (2010-15) 5.9 3.6 4.1 2.3Number <strong>of</strong> births per 1000 women age 15-19 150.0 122.3 104.5 53.7Contraceptive prevalence rate, any method(% <strong>of</strong> married women ages 15-49)23.7 23.6 29.5 -Infant mortality per 1000 live births (2008) 85 86 82 44Under-five mortality per 1000 live births (2008) 135 144 126 63Maternal mortality ratio per 100,000 live births 550 881 786 273Life expectancy at birth (2010) 54.1 52.7 57.7 69.320. Countries with less than 75 million population, gross national income per capita <strong>of</strong> under $905, high economic vulnerability and combined poor indicators<strong>of</strong> under-five mortality, undernourishment, secondary school enrolment and adult literacy.21. United Nations Human Development Programme 2010, Statistical Annex22. As <strong>the</strong> UNDP has to make sure its data are from comparable time periods, <strong>the</strong> statistics in <strong>the</strong> 2010 Report are not necessarily <strong>the</strong> most up-to-date.The UNDP and national estimates sometimes differ.23. Baryahirwa 201024. According to data collected in <strong>the</strong> Uganda Demographic Health Surveys, <strong>the</strong> maternal mortality ratio declined to 435 in 2005-06 from 505 in 2000-01,but <strong>the</strong> change is not statistically significant (Ministry <strong>of</strong> Finance, Planning and Economic Development 2010).25. United Nations Human Development Programme 2010, Statistical Annex16
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersRural population, access to electricityand to improved waterOnly 13.3% <strong>of</strong> Uganda’s population lives in an urban area;only one country has a lower proportion <strong>of</strong> urban dwellers.This is in striking contrast to Sub-Saharan Africa (37%),least-developed countries (29.1%) and <strong>the</strong> world overall(50.5%). Globally, Uganda has <strong>the</strong> highest proportion <strong>of</strong>inhabitants with no access to electricity, 91.1%. A third <strong>of</strong>its population has no access to improved water; 25 countrieshave worse access than Uganda. Over half <strong>of</strong> <strong>the</strong> population(52%) has no access to improved sanitation, a better ratethan most low human development countries.Availability <strong>of</strong> formal healthcareUganda has one doctor for every 10,000 people. With only14 doctors, nurses and midwives for every 10,000 peopleUganda is one <strong>of</strong> 44 low-income countries that do not meet<strong>the</strong> WHO minimum threshold <strong>of</strong> 23 doctors, nurses andmidwives per 10,000 population necessary to deliveressential maternal and child health services. 26Uganda has four hospital beds per 10,000 people; in only fouro<strong>the</strong>r countries is <strong>the</strong> ratio lower. The proportion <strong>of</strong> womenmaking at least one antenatal visit is high, at 94%, but <strong>the</strong>proportion <strong>of</strong> births attended by skilled health personnel dropsto 42%. The Uganda Millennium Development Goals reportfor 2010 gives <strong>the</strong> following information. 27 An expectantmo<strong>the</strong>r’s first antenatal visit is late in <strong>the</strong> pregnancy, a median<strong>of</strong> 5.5 months. Among <strong>the</strong> poorest fifth <strong>of</strong> <strong>the</strong> population, <strong>the</strong>share <strong>of</strong> births attended by skilled health personnel was29% in 2005-06 compared to 77% among <strong>the</strong> wealthiest fifth.There are also large urban-rural inequalities: 80% <strong>of</strong> deliveriesin urban areas were attended by a doctor, nurse or midwifebut only 37% in rural areas.Table 3Availability <strong>of</strong> formal healthcareMedical doctor per 10,000 people* 1Doctors, nurses and midwives per 10,000** 14Hospital beds per 10,000 people* 4Antenatal coverage <strong>of</strong> at least one visit (%)* 94Births attended by skilled health personnel (%)* 42*UNDP 2010; **WHO 2010Disease in UgandaSickness is normal ra<strong>the</strong>r than exceptional. Over 4 in 10household members surveyed (43%) said <strong>the</strong>y had fallen sickin <strong>the</strong> previous 30 days; malaria or fever is by far <strong>the</strong> mostprevalent illness, reported by over half, followed by respiratoryillnesses which affected 15%. 28 Seventy per cent <strong>of</strong> child deathsare due to disease or malnutrition, with malaria accounting forone third <strong>of</strong> <strong>the</strong>se deaths. 29HIV prevalence fell to 7% in 2007-08 from 27% in 2000-01. 30Yet <strong>the</strong> number <strong>of</strong> people living with HIV in 2010, around1.2 million, was higher than at <strong>the</strong> peak <strong>of</strong> <strong>the</strong> epidemic in<strong>the</strong> 1990s. 31 The WHO ranked Uganda 16th <strong>of</strong> <strong>the</strong> 22 countrieswith a high tuberculosis burden in 2010. Uganda has <strong>the</strong>second highest accident burden. 3226. World Health Organisation 201027. Ministry <strong>of</strong> Finance, Planning and Economic Development 201028. Baryahirwa 201029. Ministry <strong>of</strong> Health 2010a30. Ibid.31. Ministry <strong>of</strong> Finance, Planning and Economic Development 201032. Ministry <strong>of</strong> Health 2010b17
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersPublic expenditure on healthUganda’s public expenditure on health stands at 1.6% <strong>of</strong>Gross National Product (GDP) (in 2008). Only 16 countriesspend smaller proportions <strong>of</strong> GDP on health than Uganda.At 2.3% <strong>of</strong> GDP, Ugandan military expenditure is almost50% more than its health expenditure; only 10 o<strong>the</strong>r lowhuman development countries devote higher proportions<strong>of</strong> GDP to military than to health.Government <strong>of</strong> Uganda health expenditure as a percentage<strong>of</strong> total government expenditure in 2009-10 was estimatedat 9.6%. The proportion is 2.1 points above that <strong>of</strong> 2000-01and just under that <strong>of</strong> <strong>the</strong> peak year <strong>of</strong> 2004-05, and continuesto stand well below <strong>the</strong> Ajuba target 34 and <strong>the</strong> Government’sown target <strong>of</strong> 15% by 2014-15. From Table 5 it may bededuced that <strong>the</strong> Government funded almost 60% <strong>of</strong> heal<strong>the</strong>xpenditure in 2009-10, while donor projects accounted for40%. It should be noted that several development partnerschannel development assistance through <strong>of</strong>f-budget support:government estimates indicate that 77% <strong>of</strong> health projectsupport in 2009-10 was <strong>of</strong>f-budget. 35Table 4Ugandan public expenditure 33Education (% <strong>of</strong> GDP) 3.8%Military (% <strong>of</strong> GDP) 2.3%Health (% <strong>of</strong> GDP) 1.6%Debt service (% <strong>of</strong> GDP) 0.5%Expenditure on health per capita (PPP$) 74Table 5Health financing and expenditure 2000-01 to 2009-10 36 (in billion Uganda shillings)YearGovernment <strong>of</strong>Uganda fundingDonor Projectsand GlobalHealth InitiativesTotalGovernment heal<strong>the</strong>xpenditure as % <strong>of</strong> totalgovernment expenditure2000/01 124.23 114.77 239.00 7.52001/02 169.79 144.07 313.86 8.92002/03 195.96 141.96 337.92 9.42003/04 207.80 175.27 383.07 9.62004/05 219.56 146.74 366.30 9.72005/06 229.86 268.38 498.24 8.92006/07 242.63 139.23 381.86 9.32007/08 277.36 141.12 418.48 9.02008/09 375.46 253.00 628.46 8.32009/10* 435.80 301.80 737.60 9.6*Provisional Budget outturn 2009-1033. United Nations Human Development Programme 2010, Statistical Annex34. In 2001, African Heads <strong>of</strong> State made a commitment to allocate 15% <strong>of</strong> <strong>the</strong>ir annual domestic budgets to health during <strong>the</strong> special summit on AIDS,TB and Malaria held in Abuja, Nigeria. The Abuja commitment was to exclude donor support.35. Ministry <strong>of</strong> Health 2010b table 2.236. Ministry <strong>of</strong> Health 2010b table 2.318
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers2.2 Formal healthcare provisionIn Ugandan policy, <strong>the</strong> healthcare system comprises servicesaccessed at health units (hospitals, health centres, clinics and‘drug shops’ selling medicines) and community services whichrange from home-based care (typically provided by organisationsfunded through overseas aid) to traditional and complementarymedicine practitioners. Approximately 60% <strong>of</strong> Uganda’spopulation seeks care from traditional and complementarymedicine practitioners (herbalists, bone-setters, birth attendants,hydro-<strong>the</strong>rapists, spiritualists and dentists) before and aftervisiting <strong>the</strong> formal sector. 37 It is reported that birth attendantsconstitute 12.3% <strong>of</strong> traditional healers and have organised aregistered association with about 60,000 members. 38Within <strong>the</strong> formal system, healthcare is provided primarilyin hospitals and health centres run by <strong>the</strong> government,not-for-pr<strong>of</strong>it organisations and private pr<strong>of</strong>it-makingorganisations. Not-for-pr<strong>of</strong>it providers, three-quarters <strong>of</strong> whichare under <strong>the</strong> umbrellas <strong>of</strong> <strong>the</strong> Protestant, Catholic, Muslim andOrthodox Medical Bureaux, are well integrated into <strong>the</strong> publichealth system. The government oversees not-for-pr<strong>of</strong>it facilitieswithin its devolved district management system and subsidises<strong>the</strong>m at around 16% in 2008-09, down from 22% in 2007-08. 39The expansion <strong>of</strong> private health providers has been describedby <strong>the</strong> Ministry <strong>of</strong> Health itself as “largely unregulated andchaotic”. 40 There are innumerable unregistered private sectorunits, including drug shops. A count in 2005 in three districtsfound government and not-for-pr<strong>of</strong>it units toge<strong>the</strong>r made up aslittle as 4% <strong>of</strong> all health units. 41The Ministry <strong>of</strong> Health’s recent inventory <strong>of</strong> facilities, drawn upin 2010, lists 4,441 facilities <strong>of</strong>ficially registered as a hospital orhealth centre. 42 Table 6 shows 60% in <strong>the</strong> government sector,18% in <strong>the</strong> not-for-pr<strong>of</strong>it sector and 22% in <strong>the</strong> private sector.The health facility hierarchy:health centres and hospitalsHealth centres and hospitals are structured in tiers in line with<strong>the</strong> local government structure (see Appendix B). The originallowest level <strong>of</strong> health centre (health centre I), equivalent toan aid post, has been phased out. Now <strong>the</strong> Ministry <strong>of</strong> Healthis promoting Village Health Teams. Unpaid local people aretrained to increase health awareness, as well as to treat minorillnesses, and are expected to link communities with healthcentres. In late November 2009, teams had been establishedin three-quarters <strong>of</strong> districts, but only a third <strong>of</strong> districts hadtrained teams in all villages. 43The size <strong>of</strong> population served and <strong>the</strong> services that shouldbe <strong>of</strong>fered by health centres increase from <strong>the</strong> bottomlevel upwards. A health centre II should provide preventive,promotive and outpatient curative health services. TheMinistry <strong>of</strong> Health’s inventory shows over a quarter <strong>of</strong> healthcentre II facilities located in <strong>the</strong> capital, Kampala, with 98.5%<strong>of</strong> those in private hands. Some 95% <strong>of</strong> private health centre IIswere found in four districts, including Kampala. A health centreIII should provide maternity, in-patient and laboratory services,in addition to health centre II-type services.A health centre IV should provide emergency surgery and bloodtransfusion in addition to <strong>the</strong> types <strong>of</strong> services a health centreIII should <strong>of</strong>fer, and should be headed by a medical doctor. In2009-10, less than 25% <strong>of</strong> <strong>the</strong> 119 health centre IVs reportingto <strong>the</strong> Ministry <strong>of</strong> Health provided at least 10 <strong>of</strong> 12 key servicesexpected <strong>of</strong> a health centre IV, and only 57% <strong>of</strong> those had amedical <strong>of</strong>ficer. 44 Five <strong>of</strong> <strong>the</strong> 80 districts in <strong>the</strong> inventory hadno health centre IV at all and a fur<strong>the</strong>r 23 had one only.Table 6Health facilities by level and ownershipHospital Health Centre IV Health Centre III Health Centre II TotalNo. % No. % No. % No. % No. %Government 65 49.6 165 92.7 847 76.0 1572 52.1 2649 59.7Not-for-pr<strong>of</strong>it 57 43.5 12 6.7 241 21.7 486 16.1 796 17.9Private 9 6.9 1 0.6 26 2.3 960 31.8 996 22.4Total 131 100 178 100 1114 100 3018 100 4441 10037. Ministry <strong>of</strong> Health 2010b38. Nabudere et al 201039. Republic <strong>of</strong> Uganda 201040. Ministry <strong>of</strong> Health 2009c p341. Konde-Lule et al 200742. Retrieved at www.unfpa.org/sowmy/resources/en/library.htm Includes 134 facilities under construction or o<strong>the</strong>rwise not functioning43. Ministry <strong>of</strong> Health 2010b44. Ministry <strong>of</strong> Health 2010b Table 5.319
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersThe next tier up is <strong>the</strong> general hospital at district level, to whicha health centre IV should refer patients it cannot serve. TheMinistry <strong>of</strong> Health’s inventory shows that 15 out <strong>of</strong> 80 districtshad no hospital. The problem <strong>of</strong> providing a district-levelhospital has become more acute since <strong>the</strong> number <strong>of</strong> districtsreached 112 in mid-2010. A general hospital is expected torefer patients to <strong>the</strong> nearest <strong>of</strong> <strong>the</strong> 13 government-sectorregional referral hospitals for services not available at generalhospitals. Current policy does not allow not-for-pr<strong>of</strong>it orprivate hospitals to be designated as regional referral hospitals,although in practice some not-for-pr<strong>of</strong>it general hospitals fulfilthat role. The main national referral hospital stands at <strong>the</strong> top <strong>of</strong><strong>the</strong> pyramid and provides specialist services. 45 Patients may, and<strong>of</strong>ten do, by-pass lower levels and go direct a referral hospital.The central government oversees <strong>the</strong> semi-autonomousnational and regional referral hospitals. Since decentralisationin 2006, district health <strong>of</strong>fices oversee general hospitals andhealth centres. Health sub-districts are expected to plan,conduct in-service training, coordinate service delivery andsupervise <strong>the</strong>ir lower-level health units. They are normallyheaded by a medical doctor at a general hospital or anupgraded health centre IV.All local government health centres and hospitals must havea Health Unit Management Committee (HUMC) which shouldoversee <strong>the</strong> running <strong>of</strong> <strong>the</strong> facility. Committee memberscan be selected by <strong>the</strong> District Council, locally elected orappointed because <strong>the</strong>y hold o<strong>the</strong>r positions. They havebeen recommended as vehicles for community participation,46 47but have been reported as not functioning as expected.HUMCs had a chequered reputation in <strong>the</strong> past, believed tobe implicated in disappearance <strong>of</strong> medicines and distrustedby local communities. 48 They rarely met after <strong>the</strong> abolition <strong>of</strong>user fees in government facilities. 49 The Ministry <strong>of</strong> Health,with support from <strong>the</strong> USAID-supported Capacity Programme,has embarked on a training programme for HUMC members inboth government and not-for-pr<strong>of</strong>it facilities. 50Patterns <strong>of</strong> use <strong>of</strong> health facilitiesThe vast majority <strong>of</strong> Ugandans, 93%, seek treatment forsickness. 51 Ugandans turn to private clinics and drug shops forwalk-in healthcare and medication, and favour health centresand hospitals for more serious conditions and in-patient care. 52Well over half (58%) go to drug shops and private clinics, 28%to health centres and nine% to hospitals; considerably higherproportions <strong>of</strong> rural than urban dwellers use health centres,while higher proportions <strong>of</strong> urban dwellers use hospitals. 53The poorer you are in Uganda, <strong>the</strong> more likely you are to go toa government health centre. Almost half <strong>of</strong> <strong>the</strong> poorest tenth<strong>of</strong> <strong>the</strong> population use a government health centre, comparedwith only 12% <strong>of</strong> <strong>the</strong> richest tenth. Moreover, <strong>the</strong> pooresttenth almost doubled <strong>the</strong>ir use over a five-year period, while<strong>the</strong> richest 10% increased use only marginally. 54 In 2010, overone in four Ugandans (28%) lived more than five kilometresfrom <strong>the</strong> nearest health facility. 55 The government has investedin improving physical access to healthcare by building morehealth units. By 2009-10 <strong>the</strong> average distance to a governmen<strong>the</strong>alth centre was 4.6 kilometres, which <strong>the</strong> majority <strong>of</strong> peoplewalk (75%) or cycle (14%). 56Children and pregnant women are <strong>the</strong> largest groups <strong>of</strong> healthfacility patients: 38% are children aged 0-14, with <strong>the</strong> majority(97%) seeking immunisation services; and 38% are womenseeking antenatal and delivery care services. 57 The proportion<strong>of</strong> deliveries in government and not-for-pr<strong>of</strong>it facilities in2009-10 was 33%. 58 In contrast, traditional birth attendantsassisted 23% <strong>of</strong> deliveries, and relatives or o<strong>the</strong>r unskilledhelpers 25% in 2005-06. 5945. The o<strong>the</strong>r national referral hospital is a psychiatric hospital.46. Kapiriri et al 200347. Rutebemberawa et al 200948. Azfar et al n.d49. Burnham et al 200450. Kidder 201051. Uganda Bureau <strong>of</strong> Statistics 200852. Konde-Lule et al 200753. Baryahirwa 201054. Ministry <strong>of</strong> Finance, Planning and Economic Development 201055. Ministry <strong>of</strong> Health 2010b56. Baguma 201057. Uganda Bureau <strong>of</strong> Statistics 200858. Republic <strong>of</strong> Uganda 201059. Uganda Bureau <strong>of</strong> Statistics 200620
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers2.3 The Ugandan health workforceThere are no available up-to-date data on <strong>the</strong> constitution <strong>of</strong><strong>the</strong> Ugandan health workforce. The prime source is <strong>the</strong> 2002Population and Housing Census. 60 The census recorded peoplewho had worked paid or unpaid in a health occupation in <strong>the</strong>previous seven days. Most commentary relies on <strong>the</strong> censusdata. 61 In addition, WHO has produced estimates for 2004 and2005. 62 These cover people working full-time in paid activitiesin organisations whose primary intent is to improve health, aswell as those whose personal actions are primarily intended toimprove health but who work for o<strong>the</strong>r types <strong>of</strong> organisation.Occupations: numbers and densityThis chapter focuses on <strong>the</strong> main occupational groups (Box 1).Box 1The medical doctor hierarchy includes intern (junior house <strong>of</strong>ficer), medical <strong>of</strong>ficer, medical <strong>of</strong>ficer special grade(specialist with a few years’ experience), consultant (specialist with at least five years’ post-specialisation experience)and senior consultant (consultant with many years experience). Appointment as consultant and senior consultantdepends on <strong>the</strong> availability <strong>of</strong> posts. 63The clinical <strong>of</strong>ficer is a distinct cadre in Uganda, termed medical assistant prior to 1996. Clinical <strong>of</strong>ficers undergothree years’ training in specialist schools. Their clinical work has expanded from diagnosis and treatment, includingprescribing, in primary healthcare to cover outpatient treatment and admission in district and regional hospitals.At <strong>the</strong> better-equipped health centres and at district hospitals, <strong>the</strong>y carry out minor surgical procedures. When a healthcentre IV lacks a medical doctor, <strong>the</strong> clinical <strong>of</strong>ficer provides both outpatient and inpatient services, except for major64 65surgery. Clinical <strong>of</strong>ficers are <strong>of</strong>ten responsible for administration as <strong>the</strong> person ‘in charge’ <strong>of</strong> a health centre.Nurses and midwives fall into three groups within <strong>the</strong> Ugandan health system: registered nurses, registered midwivesor those doubly registered as nurse and midwife (that is, with a diploma or degree in nursing); enrolled nurses, enrolledmidwives or those enrolled as both (that is, having completed a certificate programme); and comprehensive nurses, ei<strong>the</strong>rregistered or enrolled. The registered comprehensive nurse and <strong>the</strong> enrolled comprehensive nurse training programmes,started in 1994 and 2003 respectively, were intended to create a multi-purpose nurse with competencies in generalnursing, midwifery, public health, psychiatry, paediatrics and management, and able to provide basic health services inprimary healthcare. Enrolled comprehensive nurse training programmes have replaced <strong>the</strong> traditional enrolled nursing andenrolled midwifery training programmes in all government-owned health training institutions, and have been introducedinto many not-for-pr<strong>of</strong>it training institutes. The future <strong>of</strong> comprehensive nurse training is under review. 66Nursing aides, who have no formal training, have over time upgraded into nursing assistants through short formal courses,though <strong>the</strong> workforce still contains significant numbers <strong>of</strong> untrained nursing aides. The initial strategy was to train nursingaides as a temporary solution until more qualified staff were trained and made available. 67 The current policy is to graduallyphase out <strong>the</strong> nursing assistant/aide position and ban recruitment and formal training, though new training institutionshave continued to emerge. 68 Regulation <strong>of</strong> nursing assistants has been difficult, as <strong>the</strong> Nurses and Midwifery Council doesnot recognise <strong>the</strong> cadre. 6960. Uganda Bureau <strong>of</strong> Statistics 200261. Eg Ministry <strong>of</strong> Health 2006; Uganda Ministry <strong>of</strong> Health and The Capacity Project 2008; Africa Health Workforce Observatory 2009; Ministry <strong>of</strong> Health 2010b;Nabudere et al 201062. World Health Organisation Global Atlas <strong>of</strong> <strong>the</strong> Health Workforce63. East, Central, and Sou<strong>the</strong>rn African Health Community 201064. Banerjee et al 200565. East, Central, and Sou<strong>the</strong>rn African Health Community 201066. UNFPA 201067. Ministry <strong>of</strong> Health 200468. Republic <strong>of</strong> Uganda 201069. East, Central, and Sou<strong>the</strong>rn African Health Community 201021
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersTable 7 shows <strong>the</strong> proportions <strong>of</strong> <strong>the</strong>se occupational groupsin <strong>the</strong> 2002 census. Nurses and midwives made up almosthalf, nursing assistants/aides over one third, and allied healthpr<strong>of</strong>essionals (including clinical <strong>of</strong>ficers) 70 and medical doctorsless than 10% each. The census found 1.2 doctors and 14.5nurses, midwives and nursing assistants per 10,000 people.WHO data for 2005 give a similar picture <strong>of</strong> 1.2 doctors and13.1 nursing and midwifery personnel per 10,000 <strong>of</strong> <strong>the</strong>population. While <strong>the</strong>re are no comprehensive up-to-datedata, it is known that numbers have increased – as has <strong>the</strong>population <strong>of</strong> Uganda. For example, it was reported in 2011that Uganda has 9,701 midwives; however this numberequates to only seven midwives per 1000 live births. 71Geographical distributionUrban/rural imbalance in <strong>the</strong> distribution <strong>of</strong> health workers isa key problem in <strong>the</strong> delivery <strong>of</strong> healthcare. WHO 2004 data inTable 8 show that <strong>the</strong> majority <strong>of</strong> medical doctors (61%) wereurban-based, while <strong>the</strong> great majority <strong>of</strong> nurses, midwives andespecially medical assistants (clinical <strong>of</strong>ficers) were rural-based.Moreover, data from <strong>the</strong> 2002 census show that <strong>the</strong> mosthighly qualified pr<strong>of</strong>essionals were concentrated in <strong>the</strong>region which includes <strong>the</strong> capital, Kampala (Central region).It contained only 27% <strong>of</strong> <strong>the</strong> population but had 64% <strong>of</strong> <strong>the</strong>nursing and midwifery pr<strong>of</strong>essionals (degree holders andspecialist registered nurses) and 71% <strong>of</strong> medical doctors. 72Table 7Number, distribution and density <strong>of</strong> five main occupational groups(2002 Census data)NumberPercentagePer 10,000populationMedical doctors 2,919 6.9 1.2Allied health pr<strong>of</strong>essionals 3,785 9.0 1.6Nursing & midwifery occupations 20,186 48.0 8.3Nursing aides / assistants 15,228 36.1 6.3Total 42,118 100 19.1Population 2002 = 24.4 millionTable 8Urban / rural distribution <strong>of</strong> four main cadres (WHO 2004 data)UrbanRuralTotal No % No %Medical doctors 2,209 1,345 60.9 864 39.1Medical assistants 2,472 247 10.0 2,225 90.0Nurses 14,805 2,613 17.6 12,192 82.4Midwives 4,164 1,047 25.1 3117 74.9Totals 23,650 5,252 22.2 18,398 78.870. Under The Allied Health Pr<strong>of</strong>essionals Act, allied health pr<strong>of</strong>essionals comprise clinical <strong>of</strong>ficers (medical, anaes<strong>the</strong>tic, ophthalmic, psychiatric, orthopaedic);public health dental <strong>of</strong>ficers and dental technologists; laboratory technologists and technicians; dispensers; orthopaedic technicians; physio<strong>the</strong>rapists;occupational <strong>the</strong>rapists; radiographers; health inspectors; health associates; and assistant field <strong>of</strong>ficers for entomology.71. UNFPA 201172. Ministry <strong>of</strong> Health 200622
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersEmployment status and attritionOfficial documents have complained <strong>of</strong> “rampant dualism”. 73In 2002, 30% <strong>of</strong> all medical doctors, dentists, medical specialistsand consultants were privately employed and only one quarter<strong>of</strong> those worked full-time. 74 A survey in 2005 confirmed thatdual employment is common among medical doctors: 54% <strong>of</strong>medical doctors employed in private healthcare facilities alsoworked in <strong>the</strong> government sector. 75 While <strong>the</strong> census found29% <strong>of</strong> nurses privately employed, almost all (95%) wereemployed full-time. 14% <strong>of</strong> medical doctors and <strong>of</strong> nurses andmidwives were self-employed. 76While <strong>the</strong>re are no data on health worker unemployment,<strong>the</strong>re are indications that some nurses and midwives disappearfrom view after qualifying. All practising health workers in <strong>the</strong>country are required to register with <strong>the</strong> relevant pr<strong>of</strong>essionalregulatory council and obtain a licence to practise in Uganda. 77A new human resource information system supported by <strong>the</strong>United States Agency for International Development (USAID)allowed <strong>the</strong> Uganda Nurses and Midwives Council to see howmany nurses and midwives failed to register. The first publishedanalysis showed that 12% <strong>of</strong> <strong>the</strong> 17,297 nurses and midwivespassing final examinations from 1980 to 2004 did not registerwith <strong>the</strong> council. 78 When <strong>the</strong> period <strong>of</strong> analysis was extendedto cover 1970 to 2005, <strong>the</strong> proportion increased slightly to13%. 79 Some qualified students went into employment withoutregistration to avoid paying <strong>the</strong> registration fees. 80 The humanresource information system revealed that 55% <strong>of</strong> registeredmidwives (4,075 midwives) did not obtain a licence to practisefrom <strong>the</strong> Nurses and Midwives Council. 81Table 9Facility-based staff 2004 88 and 2005 89It is widely held that medical doctors and nurses leave Ugandafor employment in o<strong>the</strong>r countries, but comprehensivesupportive data are not available. 82 The Uganda Nurses andMidwives Council verified that 808 nurses left Uganda in2009-10, nearly half for <strong>the</strong> UK. 83 The destinations <strong>of</strong> qualifiedstaff leaving six hospitals in a remote region between 1999and 2004 did not include work in o<strong>the</strong>r countries. 84 Follow-up<strong>of</strong> a cohort <strong>of</strong> graduates <strong>of</strong> one medical school found deaths,most presumed to be AIDS-related, “a bigger brain-drainthan emigration” in <strong>the</strong> 20 years after graduation in 1984. 85Premature death is emerging as one <strong>of</strong> <strong>the</strong> most importantcauses <strong>of</strong> exit from <strong>the</strong> workforce in Sub-Saharan Africa, causingUganda to lose an estimated 2% or so <strong>of</strong> its medical, nursingand midwifery workforce each year. Annually an estimated 26physicians in every 1,000 and 22 nurses and midwives in every1,000 die before <strong>the</strong> age <strong>of</strong> 60 in Uganda, among <strong>the</strong> highestrates in <strong>the</strong> 12 African countries for which data are available. 86The facility-based workforceOf particular interest to this research are health workersemployed in facilities. The Ministry <strong>of</strong> Health has a newhuman resource information system, but <strong>the</strong> publicly availablecomparative data relate to 2004 and 2005. Table 9 showsthat 45% <strong>of</strong> facility-based health workers were in governmentfacilities (excluding district health <strong>of</strong>fice staff) and 23% innot-for-pr<strong>of</strong>it facilities in 2004; and that in 2005, <strong>the</strong> number inprivate for-pr<strong>of</strong>it facilities was estimated at 12,775, representinga 32% share <strong>of</strong> <strong>the</strong> total 39,663 employees. It should not beassumed that almost 40,000 different people worked in facilitiesin 2004 and 2005. The data for <strong>the</strong> for-pr<strong>of</strong>it sector includean estimated 3,228 people employed simultaneously in o<strong>the</strong>rsectors. 87 It is possible that government data include personnelworking also in <strong>the</strong> not-for-pr<strong>of</strong>it sector (it is not permitted tobe employed in more than one government facility).HealthoccupationsO<strong>the</strong>r staff Per cent TotalGovernment (2004) 15,124 2,619 45 17,743Not-for-pr<strong>of</strong>it (2004) 6,102 3,052 23 9,145Private for-pr<strong>of</strong>it (2005) 12,775* 32 12,775Total 39,663*Non-health occupations not recorded separately; includes 3,228 employed simultaneously in o<strong>the</strong>r sectors73. Ministry <strong>of</strong> Health 2009c, p674. Ministry <strong>of</strong> Health 200675. Mandelli et al 200576. Ministry <strong>of</strong> Health 200677. Africa Health Workforce Observatory 200978. Dal Poz et al 2009 Table 5.379. Spero et al 201180. De Vries 200981. Spero and McQuide 201182. Africa Health Workforce Observatory 200983. Senkabirwa 201084. Onzubo 200785. Dambisya 2004 p60186. Dal Poz et al 200987. Mandelli et al 200588. Ministry <strong>of</strong> Health HSSP II Table 189. Mandelli et al 200523
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersMore recent sources state that members <strong>of</strong> three faith-basedmedical bureaux (Catholic, Protestant and Muslim) toge<strong>the</strong>r in2009-10 had slightly over 11,600 health workers, around 30%<strong>of</strong> <strong>the</strong> combined government and not-for-pr<strong>of</strong>it workforce, 90and that government facility staff numbers had reached 23,452in 2009. 91 Despite efforts to clean <strong>the</strong> government payroll andupdate rosters, <strong>the</strong>re are still problems in determining howmany staff in each cadre are on <strong>the</strong> payroll and where <strong>the</strong>y areassigned. 92 In 2010, ‘ghost workers’ were exposed in a number<strong>of</strong> districts and notably at a national referral hospital, andtransferred staff were found to be still receiving salaries at <strong>the</strong>iroriginal place <strong>of</strong> work. 93The most recently available data on occupational breakdownacross sectors are for 2004 and 2005, as shown in Table 10. Ashealth workers, especially medical doctors, have jobs in morethan one sector, <strong>the</strong> numbers include double-counting. It isreported that “more recent tables show that <strong>the</strong>re has beentremendous improvement in health worker staffing levels inUganda since 2004” and that <strong>the</strong> total number <strong>of</strong> medicaldoctors in health facilities is 3,917 (presumably in governmentand not-for-pr<strong>of</strong>it facilities). 94In 2004, almost half <strong>the</strong> medical doctors and over four in 10nurse employees in government facilities worked in <strong>the</strong> twonational referral hospitals and <strong>the</strong> 11 regional referral hospitals,while <strong>the</strong> great majority <strong>of</strong> nursing assistants, clinical <strong>of</strong>ficersand midwives worked in district level facilities (Table 11).Overall, <strong>the</strong>re are severe shortages <strong>of</strong> facility-based health workersin <strong>the</strong> formal sector. Chapter 6 details <strong>the</strong> shortfalls and <strong>the</strong>consequent impact on health workers and access to healthcare.Table 10Occupational groups in government and not-for-pr<strong>of</strong>it facilities(August 2004) 95 and private facilities (estimated 2005) 96Occupation Government Not-for-pr<strong>of</strong>it PrivateMedical doctor 598 305 1,511Clinical <strong>of</strong>ficer 1,585 436 190Midwife 2,129 914 1,377Nurse 4,500 1,915 3,557Nursing assistant/aide 4,463 2,005 1,146Table 11Occupational groups in local government district facilities and nationaland regional referral hospitals, August 2004 97OccupationDistrict facilitiesNational & regionalreferral hospitalsNumber % <strong>of</strong> total Number % <strong>of</strong> totalTotalMedical doctor 308 51.5 290 48.5 598Clinical <strong>of</strong>ficer 1,319 83.2 266 16.8 1,585Midwife 1,635 76.8 494 23.2 2,129Nurse 2,542 56.5 1,958 43.5 4,500Nursing assistant 4,165 93.3 298 6.7 4,46390. Republic <strong>of</strong> Uganda 201091. Matsiko 201092. Ministry <strong>of</strong> Health and The Capacity Project 200893. Medicines and Health Service Delivery Monitoring Unit 201094. Matsiko 2010 p2495. Adapted from Matsiko 2010 Table 3.196. Mandelli et al 2005 Table 997. Adapted from Matsiko 2010 Table 3.124
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers3. Research design and methodsThis chapter first describes <strong>the</strong> three-stage approach to <strong>the</strong> research.Outlines <strong>of</strong> <strong>the</strong> qualitative research methodology and sampling design, datacollection and data analysis follow. The chapter concludes with an overview<strong>of</strong> <strong>the</strong> health worker participants. Fur<strong>the</strong>r details are in Appendix A.3.1 The research stagesThe research was conducted in three main stages: consultationwith local stakeholders on <strong>the</strong> draft protocol to be submittedfor ethical approval 98 ; focus groups and individual interviewswith health facility staff and managers; and stakeholderfeedback on draft findings.In June 2010, <strong>VSO</strong> Uganda and HEPS-Uganda held a researchworkshop with support from <strong>VSO</strong> International. Fourteenrepresentatives <strong>of</strong> organisations concerned with health workerissues in Uganda attended, including healthcare providerorganisations, pr<strong>of</strong>essional associations, regulatory councilsand consumer and health worker advocacy organisations.Participants explored practical challenges in ga<strong>the</strong>ring anddisseminating <strong>the</strong> views <strong>of</strong> health workers. The workshopstarted to build an alliance <strong>of</strong> interested stakeholders to takeforward <strong>the</strong> research findings.Main-stage fieldwork was carried out from late June 2010 toFebruary 2011. From June to August 2010, <strong>the</strong> Valuing HealthWorkers researcher, a <strong>VSO</strong> volunteer, joined forces with asecond <strong>VSO</strong> volunteer who had in February 2010 begun similarresearch with nurses as an independent initiative. The two topicguides were combined, and a small number <strong>of</strong> interviews andfocus groups already conducted in <strong>the</strong> nursing research projectwere amalgamated with <strong>the</strong> Valuing Health Workers data.<strong>VSO</strong> produced a report <strong>of</strong> interim findings to coincide with <strong>the</strong>Global Health Workers Forum in Bangkok in January 2011. 99A roundtable discussion at a <strong>VSO</strong>-led side meeting at <strong>the</strong>Forum followed a presentation <strong>of</strong> selected findings from <strong>the</strong>Valuing Health Workers research in Uganda. Ugandan ando<strong>the</strong>r participants shared <strong>the</strong>ir perspectives on <strong>the</strong> issuespresented and put forward promising solutions. In January andFebruary 2011, interim findings were shared with stakeholdersin Uganda through one-to-one meetings and a stakeholderworkshop organised by HEPS-Uganda. The workshop broughttoge<strong>the</strong>r 16 representatives <strong>of</strong> organisations includingpr<strong>of</strong>essional associations and unions, regulatory councils andhealth and human rights organisations. The workshop servedboth to validate <strong>the</strong> findings and to elicit suggestions forcoverage <strong>of</strong> additional aspects in <strong>the</strong> final report.3.2 Qualitative research methodologyand <strong>the</strong> purposive sampling designQualitative research aims to provide an in-depth understanding<strong>of</strong> <strong>the</strong> social world <strong>of</strong> research participants through learningabout <strong>the</strong>ir social and material circumstances, experiences,perspectives and histories. 100 Qualitative research is not basedon statistically representative samples and so does not producestatistically significant findings. Participants are selectedin a non-random way, according to characteristics <strong>of</strong> mostinterest to <strong>the</strong> particular study. This is known as purposivesampling. The criteria used to select participants are moreimportant than <strong>the</strong> number <strong>of</strong> people taking part. Indeed,qualitative research is <strong>of</strong>ten based on a small number <strong>of</strong> cases.In reporting, qualitative research does not use numbers; anyexperience or perspective has value, regardless <strong>of</strong> how <strong>of</strong>ten orseldom it appears.The research sampled facility-based health workers whoseprime role is treating or caring for patients, and facility-basedmanagers: nursing assistants, nurses, midwives, clinical <strong>of</strong>ficersand medical doctors. The study design thus excluded o<strong>the</strong>rpr<strong>of</strong>essional groups.In achieving <strong>the</strong> health worker sample it was first necessaryto ensure that all regions were included, as although notan administrative grouping, region has social and politicalimportance in Uganda. The strategy was to select one localgovernment district in each <strong>of</strong> <strong>the</strong> Central, West, SouthWest, North, North East and East regions, and also to include<strong>the</strong> capital city. It was felt important to include a range <strong>of</strong>districts in terms <strong>of</strong> how far <strong>the</strong>y were deemed easy or hardto serve. Within each district in <strong>the</strong> sample, one hospital(where one existed) and at least one health centre were tobe selected, covering urban and rural facilities. Among <strong>the</strong>selected facilities, <strong>the</strong> aim was for a spread <strong>of</strong> level <strong>of</strong> hospitaland health centre, and inclusion <strong>of</strong> not-for-pr<strong>of</strong>it and privatefacilities as well as government facilities.98. The study protocol was approved by Makerere University School <strong>of</strong> Public Health Higher Degrees, Research and Ethics Committee and by <strong>the</strong> UgandaNational Council for Science and Technology.99. <strong>VSO</strong> 2011100. Ritchie and Lewis 200325
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers3.3 Data collectionSeven districts in six regions and <strong>the</strong> capital city, Kampala, wereselected, so <strong>the</strong> selected facilities were distributed acrossall regions (Table A.1). The districts ranged from very hard toserve to not hard to serve, according to <strong>the</strong> Ministry <strong>of</strong> Healthcriteria (Table A.3). The 18 facilities in <strong>the</strong> sample comprisedthree referral hospitals, six general hospitals, four health centreIVs and five health centre IIIs. Eleven were government-run,five were run by not-for-pr<strong>of</strong>it organisations and two by privateorganisations (Table A.2).Permission to carry out <strong>the</strong> research was obtained from distric<strong>the</strong>alth <strong>of</strong>ficers in <strong>the</strong> five districts where government facilitieswere included in <strong>the</strong> sample. District health <strong>of</strong>fices assisted inlinking <strong>the</strong> researchers to district-level government facilities.Referral hospitals and not-for-pr<strong>of</strong>it and private sector facilitieswere approached directly.At each facility <strong>the</strong> staff member in charge was asked toarrange for staff to meet with <strong>the</strong> researcher in small groups<strong>of</strong> peers: enrolled nurses or midwives, registered nurses ormidwives, nursing assistants and those in charge <strong>of</strong> wards. Insmaller facilities, mixed groups and individual interviews werenecessary because <strong>of</strong> <strong>the</strong> limited numbers <strong>of</strong> available staff.Medical doctors, clinical <strong>of</strong>ficers and facility managers wereinterviewed individually, apart from one joint interview withtwo managers. Sixteen small group discussions with a total <strong>of</strong>71 participants and 46 one-to-one interviews took place at <strong>the</strong>18 facilities. One health worker declined to take part because<strong>of</strong> a lack <strong>of</strong> staff to cover her absence. The five district health<strong>of</strong>ficers were also interviewed.Group discussions and interviews were carried out in English.Informed consent was gained from all participants. Participantswere encouraged to talk freely in response to a set <strong>of</strong> openquestions. They were assured that <strong>the</strong>y and <strong>the</strong>ir facilitywould not be identifiable in <strong>the</strong> research reports. The topicsdiscussed covered reasons for becoming a health worker;understanding <strong>of</strong> <strong>the</strong> pr<strong>of</strong>essional role; rewards; challenges,<strong>the</strong>ir impact and coping strategies; reasons for negativeattitudes towards health workers; areas for change, and ways<strong>of</strong> increasing <strong>the</strong> voice <strong>of</strong> health workers. The full topic guide isincluded in <strong>the</strong> Appendix. Facility managers and district health<strong>of</strong>ficers were asked additionally about management issues<strong>the</strong>y faced, although frontline workers were not asked directlyabout <strong>the</strong>ir management. Participants also completed a shortbiographical pr<strong>of</strong>orma.3.4 Data analysisDiscussion groups and interviews were audio-recorded andtranscribed with participants’ permission. The analytical processstarted with repeated readings <strong>of</strong> <strong>the</strong> transcripts to identify a<strong>the</strong>matic framework. The textual data were <strong>the</strong>n structured inmatrices with a row for each group or individual and a columnfor each <strong>the</strong>matic area. Mapping and interpretation followedfrom this charting process, to define concepts, find associationsand provide explanations. As already noted, early findings werevalidated by non-governmental stakeholders through individualinterviews and workshops.3.5 The health worker participantsA general hospital was <strong>the</strong> most common workplace forparticipants (53 out <strong>of</strong> 122); 40 participants worked in healthcentres (Figure 1). Government employees numbered 75,not-for-pr<strong>of</strong>it 36 and private sector 11.Figure 1Workplace <strong>of</strong> participants202052453General hospitalReferral hospitalHealth centre IVHealth centre IIIDistrict health <strong>of</strong>fice26
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersThe largest pr<strong>of</strong>essional group was registered nurseand/or midwife, followed by enrolled nurse and/ormidwife and nursing assistant (Figure 2).There was a broad spectrum <strong>of</strong> ages among participants(Figure 4).Figure 2Participants’ pr<strong>of</strong>essional statusFigure 4Age groups <strong>of</strong> participants26152430144Registered nurseand/or midwifeEnrolled nurseand/or midwifeNursing assistantMedical doctorClinical <strong>of</strong>ficerNone24164014120-2930-3940-4950-5960-69O<strong>the</strong>rEleven participants worked solely in administration: fivequalified nurses, five medical doctors and one with ano<strong>the</strong>rmedical-related qualification. A fur<strong>the</strong>r seven participantscombined a role being in-charge <strong>of</strong> a facility with frontlinecare. The remainder were frontline employees, mostworking in nursing or midwifery roles (Figure 3).Figure 3Participants’ roles113 3 46262544NurseMidwifeNursing assistantAdministration onlyMedical doctorMedical doctor in chargeClinical <strong>of</strong>ficer in chargeClinical <strong>of</strong>ficerOf <strong>the</strong> 122 participants, 38 were men. Men were in alloccupational groups except clinical <strong>of</strong>ficer (Figure 5).Figure 5Sex <strong>of</strong> pr<strong>of</strong>essional groups70605040302010063MaleFemale1911145 6 01 2 1Nurses & Nursing Clinical Doctors O<strong>the</strong>r/nonemidwives assistants <strong>of</strong>ficers27
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers4. The RewardsUgandan health workers rarely get <strong>the</strong> chance to speak about <strong>the</strong> positives <strong>of</strong>being a healthcare worker – <strong>the</strong> rewards and satisfactions – and participantswelcomed <strong>the</strong> opportunity <strong>the</strong> research gave <strong>the</strong>m. The main areas <strong>of</strong> satisfactionwere helping o<strong>the</strong>rs, doing a good job and being valued for what <strong>the</strong>y did. Positivepractice environments were by no means commonplace. Some participants wereso discouraged by working conditions that <strong>the</strong>y struggled to find anything else goodto say about being a health worker. For a few <strong>the</strong> only positives were <strong>the</strong> materialbenefits <strong>of</strong> a regular salary and a free house. Later chapters will show how workingenvironments damaged chances for fulfilment and satisfaction at work.4.1 Benefiting o<strong>the</strong>rsParticipants told <strong>of</strong> feeling happy carrying out <strong>the</strong>ir vocation,helping <strong>the</strong>ir people, giving something back, delivering careand comfort, helping those unable to help <strong>the</strong>mselves andsaving lives. Very strikingly, <strong>the</strong> benefits to <strong>the</strong> community, toindividual patients and to families were <strong>the</strong> biggest sources <strong>of</strong>satisfaction even in <strong>the</strong> harshest working environments.Benefiting <strong>the</strong> wider communityHealth workers emphasised <strong>the</strong> rewards <strong>of</strong> sharing <strong>the</strong>irknowledge and skills with communities to counter harmfultraditional beliefs and practices, educate people about ways <strong>of</strong>preventing disease and encourage take-up <strong>of</strong> health services.Seeing more women delivering babies in health units, diseasescontrolled through immunisation programmes, or reducedreliance on harmful traditional remedies brought greatsatisfaction. Health workers were especially pleased wheninvolved in new programmes and able to see <strong>the</strong>ir impacts,such as a nutrition clinic, a mental health unit or prevention<strong>of</strong> mo<strong>the</strong>r-to-child HIV transmission. Satisfaction came frombeing part <strong>of</strong> a health facility that put <strong>the</strong> patients first.Especially in rural areas, health workers were happy to use<strong>the</strong>ir knowledge to help informally outside working hoursand around <strong>the</strong>ir homes. For an <strong>of</strong>f-duty nurse, it was good tosocialise with in-patients, hear <strong>the</strong>ir family problems and have<strong>the</strong> chance to give some health education.Benefiting patientsParticipants highlighted <strong>the</strong> visible results <strong>of</strong> care and treatment.They expressed <strong>the</strong>ir delight at <strong>the</strong> benefits to patients. Nursesand medical doctors spoke about how happy and proud <strong>the</strong>yfelt when a patient who arrived sick, even on <strong>the</strong> edge <strong>of</strong>death, went home recovered: “I love it when someone comesin ill and goes back happy.” Seeing life enhanced was alsohugely rewarding: “Making people happy makes me happy.”Just seeing some improvement in a patient was cheering.Midwives spoke <strong>of</strong> <strong>the</strong> rewards <strong>of</strong> working for <strong>the</strong> welfare <strong>of</strong>two people, “a live mo<strong>the</strong>r and a live baby” – and achievingsomething positive with no mo<strong>the</strong>r or baby lost.Benefiting families“The nurse is <strong>the</strong> most important person in <strong>the</strong> family.”Especially for nurses in rural settings or from rural families it washugely rewarding to be able to deal with family health problems.Knowing how to prevent and treat illness in your immediatefamily, as well as how to protect yourself, was a significantfactor encouraging a commitment to nursing which would lastup to and beyond retirement: “You will be a nurse until you die.”Nurses at some rural health centres pointed to <strong>the</strong> advantagesto <strong>the</strong>ir family and <strong>the</strong>mselves <strong>of</strong> quick access to free treatment.The nurse could use his or her knowledge to treat a relativeand save <strong>the</strong> costs associated with referral to a health centre orhospital. It was said in some facilities that staff and <strong>the</strong>ir familymembers were given free medication.4.2 Job satisfactionLinked to <strong>the</strong> happiness <strong>of</strong> seeing someone recover is <strong>the</strong>satisfaction <strong>of</strong> knowing your own contribution, among medicaldoctors and clinical <strong>of</strong>ficers especially: “I feel happy when I givetreatment to my patients and <strong>the</strong>y get well, I feel so proud, Ifeel very fine” or “I can see <strong>the</strong> difference I have made, that’svery important.” Introducing new treatments and bringing aboutchange in a challenging environment was hugely satisfying:“What o<strong>the</strong>rs thought was so difficult, I have been able to do.”28
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersMaternity workers spoke <strong>of</strong> <strong>the</strong>ir joy when <strong>the</strong>y safelydelivered a healthy baby, “when everyone is smiling”,and <strong>the</strong> satisfaction <strong>of</strong> seeing that baby grow.Having done good nursing work treating a badly-<strong>of</strong>f patient whoimproved and was discharged gave “a kind <strong>of</strong> job satisfactionand encourages me to care for patients a little more.” For nurses,it was good to have done something, no matter how little, tohelp save a life. Achieving successes is not easy in Uganda andan occasional “victory”, such as when a sick child recovers, wassomething to “live for”, that “makes you do what you do”.Participants spoke <strong>of</strong> <strong>the</strong> satisfaction <strong>of</strong> doing a good job when<strong>the</strong>re was enough equipment, o<strong>the</strong>r medical supplies andmedicines to enable proper care: “Most <strong>of</strong> what you need fora patient is available, so your job is not much interfered with”or “You cannot forget your skills”. Elsewhere health workerscommented on <strong>the</strong> satisfaction <strong>of</strong> just being able to play<strong>the</strong>ir part and do <strong>the</strong>ir duty <strong>the</strong> best <strong>the</strong>y could despite manyshortcomings in supplies and equipment and staffing shortfalls.Some spoke <strong>of</strong> pride in working efficiently to treat patients orcaring tenderly where <strong>the</strong>y could.Particularly for younger participants, opportunities to learnthrough work and to experience managing different kinds <strong>of</strong>medical condition were highly valued. While not commonlyreported, opportunities to learn new skills, such as counselling,were valued for <strong>the</strong>ir benefits to patients. In <strong>the</strong> few instanceswhere workplace-based education programmes were in place,participants spoke enthusiastically about how <strong>the</strong>y shared <strong>the</strong>irlearning with o<strong>the</strong>r staff and developed new communication skills.4.3 Being recognised, appreciatedand valuedCommunity recognitionSome nurses in rural settings liked being acknowledged andknown in <strong>the</strong> community: “When you go out you are respected”or “You are famous.” Being a nurse meant being seen as aneducated person; it was gratifying to be called a “small doctor.”Nurses sometimes felt <strong>the</strong>ir training set <strong>the</strong>m apart from o<strong>the</strong>rpeople, conferring a certain prestige, especially when <strong>the</strong>ycould use <strong>the</strong>ir knowledge to help outside <strong>the</strong>ir formal work.Nursing was also valued as a way to meet different types <strong>of</strong>people, get to know many people and make friends.Patients’ appreciation, trust and respectHealth workers valued being liked, appreciated, praised,respected and trusted by patients.It was noted that expressing thanks was not <strong>the</strong> norm in someparts <strong>of</strong> Uganda, and health workers spoke enthusiasticallyabout <strong>the</strong> boost a “thank you” from a patient gave <strong>the</strong>m: “Youfeel very happy after your work when <strong>the</strong>y say thank you.So you keep on, because you are enjoying it.” For some, <strong>the</strong>pleasure <strong>of</strong> helping was enough whe<strong>the</strong>r praised or not: “I feelit inside my heart.” As well as appreciation, recognition <strong>of</strong> <strong>the</strong>irexpertise was important to nurses: “Their confidence in youboosts your own confidence.”Midwives expressed <strong>the</strong>ir delight when a baby was given<strong>the</strong>ir name. Nursing staff and medical doctors emphasisedhow recognised and appreciated <strong>the</strong>y felt when a past patientgreeted and thanked <strong>the</strong>m warmly or showed <strong>of</strong>f “your baby”.Being remembered by patients was seen as a mark <strong>of</strong> trustand a boost to <strong>the</strong> nurse’s own confidence. For some nurses,respect and trust on <strong>the</strong> part <strong>of</strong> patients or caregivers openedup disclosure <strong>of</strong> confidences and opportunities for fur<strong>the</strong>r help.4.4 Appreciative and supportivemanagement and colleaguesAppreciation on <strong>the</strong> part <strong>of</strong> managers was a huge positive,although not widely reported: “When you are recognisedthat you are doing good work, I think that is important, itmotivates”. Simply being told “thank you” was not necessarilyvery satisfying in difficult working conditions. Health workersvalued more tangible demonstrations <strong>of</strong> appreciation, such asopen internet access, Christmas and Easter presents and staffparties. Rare, and especially valued, was facility sponsorship <strong>of</strong>fur<strong>the</strong>r training with a job to return to.Uniquely in <strong>the</strong> study, participants in a local government hospitalpraised management who “appreciate us so much.” They told<strong>of</strong> certificates <strong>of</strong> appreciation, staff parties, presents, financialcontributions to costs <strong>of</strong> burials and operations, help with costs<strong>of</strong> fur<strong>the</strong>r study, days <strong>of</strong>f to recover from illness, interest instaff’s work and responsiveness to problems staff identified.Health workers felt valued by good, supportive managerswho created opportunities for <strong>the</strong>m to raise <strong>the</strong>ir concerns,were always willing to discuss a problem, and sought andimplemented solutions.Nurses spoke <strong>of</strong> <strong>the</strong> satisfaction <strong>of</strong> working cooperativelywith o<strong>the</strong>r staff, having someone to consult if needed, sharingideas and reaching solutions. Teamwork also meant helpingeach o<strong>the</strong>r out, such as an <strong>of</strong>f-duty nurse caring for ano<strong>the</strong>rnurse’s sick child, and willingness to extend hours to cover for anurse’s delayed arrival at work. Where working conditions wereespecially challenging, nurses valued being part <strong>of</strong> a supportnetwork where everyone understood <strong>the</strong> difficulties.29
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers5. Reasons for becoming a health worker:<strong>the</strong> “right heart” and <strong>the</strong> “wrong heart”Participants explained what prompted <strong>the</strong>m to become healthcare pr<strong>of</strong>essionals. The urgeto help, prevent suffering and save lives stood out. The overriding impression from <strong>the</strong>irwords was <strong>of</strong> a heartfelt desire to “make a difference” as a nurse, midwife, clinical <strong>of</strong>ficeror medical doctor, ra<strong>the</strong>r than merely to earn a living. It is a mark <strong>of</strong> <strong>the</strong>ir pr<strong>of</strong>essionalcommitment that almost all participants said <strong>the</strong>y would still choose to be health worker.Participants commented on people joining health pr<strong>of</strong>essions, notably nursing, for<strong>the</strong> “wrong” reasons. This, in <strong>the</strong>ir view, was one explanation for poor attitudes andunethical behaviour, and <strong>the</strong>y put forward suggestions for improving <strong>the</strong> calibre <strong>of</strong>recruits. The recommendations also include views <strong>of</strong> o<strong>the</strong>r stakeholders.5.1 A passion for <strong>the</strong> patientsFor many health workers, <strong>the</strong> strong need to give to o<strong>the</strong>rs wasborn from childhood experiences. It had been common in ruralareas to see close family and members <strong>of</strong> <strong>the</strong> local communitysuffer in pain and die, with no proper medical care. Participantsrecounted how siblings and parents had died from mysteriousillnesses that, <strong>the</strong>y later realised, were caused by preventableepidemics or treatable with modern medicine. Training as anurse, clinician or medical doctor would bring to <strong>the</strong> communityessential knowledge to help prevent illnesses, discourage harmfultraditional healing practices and save lives. “They were reallysuffering, people were dying, <strong>the</strong>re were no doctors, no nurses,nobody to give <strong>the</strong>m an idea about <strong>the</strong>ir health. I wanted tohelp my people.” O<strong>the</strong>rs spoke <strong>of</strong> atrocities in conflict areasand <strong>the</strong> need for medical skills to rebuild communities.Health workers spoke warmly <strong>of</strong> positive experiences when <strong>the</strong>yor family members were in hospital. The gentle and caring touchand <strong>the</strong> healing words <strong>of</strong> nursing staff left a lasting impression.They wanted to be that person, to give in that caring way. Theysaw how nurses stopped pain and wanted to stop o<strong>the</strong>rs’ pain.Growing up, <strong>the</strong>y learnt how <strong>the</strong> skills <strong>of</strong> <strong>the</strong> medical staff hadsaved <strong>the</strong> life <strong>of</strong> someone close to <strong>the</strong>m, or even <strong>the</strong>ir ownlife, and <strong>the</strong>y wanted to give something in return. Some wereencouraged by a grateful parent who remembered midwivesurging that <strong>the</strong> baby become a midwife too.Not all impressions were good. Negative experiences <strong>of</strong>healthcare services lay behind a desire to raise <strong>the</strong> standard<strong>of</strong> medicine in Uganda. Young men and women said <strong>the</strong>y feltcompelled to join <strong>the</strong>ir pr<strong>of</strong>essions because <strong>the</strong>y believedthat pr<strong>of</strong>essional neglect had contributed to <strong>the</strong> deaths <strong>of</strong>a parent, siblings and a newborn baby, or because <strong>the</strong>y hadperceived <strong>the</strong> limitations <strong>of</strong> Ugandan medical expertise for alife-threatening condition. Unsympa<strong>the</strong>tic handling prompteda wish to improve <strong>the</strong> quality <strong>of</strong> nursing, and <strong>the</strong> shouts <strong>of</strong>women abandoned in labour evoked an urge to help.Women spoke <strong>of</strong> wanting to be a nurse from as early as primaryschool stage, never considering any alternative. They saw<strong>the</strong>mselves as naturally kind, a helping sort <strong>of</strong> person, with anurge to relieve suffering: “I just had it in me” or “I had that heart.”Some women found <strong>the</strong>y “developed <strong>the</strong> heart” as young adultswhen <strong>the</strong>y had to nurse a family member. Not-for-pr<strong>of</strong>it sectorparticipants especially cited a desire “to love and serve <strong>the</strong>patients” or “to care for <strong>the</strong> needy”, spoke <strong>of</strong> coming “closer toGod” or explained <strong>the</strong>y had “a call” or were “chosen by God”.Health workers emphasised giving and spoke less about what<strong>the</strong>y had expected to gain from <strong>the</strong>ir pr<strong>of</strong>ession, though <strong>the</strong>prospect <strong>of</strong> knowledge to care for and treat one’s family andoneself was important, especially among lesser qualified womenin rural areas. Nurses’ happiness when a patient recovered wasmentioned, as was <strong>the</strong> respect people gave to a local nurse.The nurse had status as a life-saver, a person <strong>of</strong> importance tocall on in an emergency. Young girls who went on to be nurseshad been greatly attracted by <strong>the</strong> dress and deportment <strong>of</strong>nurses, admiring <strong>the</strong>ir smart, clean uniforms, shoes and gloves,and <strong>the</strong> way <strong>the</strong>y walked, which distinguished <strong>the</strong>m from o<strong>the</strong>rpeople. Among would-be medical doctors <strong>the</strong>re was someadmiration <strong>of</strong> smart white coats and acknowledgement <strong>of</strong> <strong>the</strong>prestige attached to doctors.A desire for money was not a driving force, though earning in asteady job was certainly a better option than “digging” in vegetablegardens and relying on uncertain harvests. In <strong>the</strong> most remoterural area, <strong>the</strong> health facility was <strong>the</strong> only source <strong>of</strong> trainingand employment locally, and so a magnet for school-leavers.30
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersFor most participants, <strong>the</strong> decision to become a healthpr<strong>of</strong>essional was positive and informed. Time spent at hospitalsor health centres – as a patient, relative <strong>of</strong> a patient or just asa curious child allowed to sit with nurses – had shown hownurses worked with patients and helped stimulate an interest.Empathy for patients sometimes developed when “touched”by <strong>the</strong>ir condition.Having a fa<strong>the</strong>r, mo<strong>the</strong>r, sister, bro<strong>the</strong>r or aunt in a nursing ormedical field gave some insight into <strong>the</strong> work, through visiting<strong>the</strong>ir place <strong>of</strong> work, living in staff quarters or listening to <strong>the</strong>iraccounts <strong>of</strong> day-to-day happenings. A close relative’s positiveattitude, humility or empathy for patients attracted youngwomen to nursing. For many <strong>of</strong> those participants, <strong>the</strong> example<strong>of</strong> <strong>the</strong>ir relative was <strong>the</strong> main reason for entering a nursing ormedical pr<strong>of</strong>ession. With little career guidance at school, it wasnatural to do what members <strong>of</strong> <strong>the</strong> family were doing.O<strong>the</strong>rs felt family expectations to take up some kind <strong>of</strong> pr<strong>of</strong>essionand saw health work as more appealing than <strong>the</strong> teaching,secretarial or business occupations suggested – even rebellingagainst fa<strong>the</strong>rs who insisted on a teaching course. Some olderparticipants spoke <strong>of</strong> encouragement from adults at school orfamily friends, such as priests and nuns, to apply for a medicalor nursing course. There were a few instances <strong>of</strong> people fromthat generation recruited to apply for nursing by agents <strong>of</strong><strong>the</strong> Ministry <strong>of</strong> Health, and also <strong>of</strong> following family wishes orsuggestions in complete ignorance <strong>of</strong> what nursing involved.Clinical <strong>of</strong>ficers and medical doctors told <strong>of</strong> expectations on<strong>the</strong>m as <strong>the</strong> brightest school students to enter one <strong>of</strong> <strong>the</strong>prestigious pr<strong>of</strong>essions. If <strong>the</strong>y excelled in science subjects,engineering and medicine were <strong>the</strong> prime alternatives. Thepath towards medicine could be set in early years when topstudents were pushed towards sciences.Where faced with a choice <strong>of</strong> career direction, financial securitywas something younger men had considered, in <strong>the</strong> context <strong>of</strong>many qualified pr<strong>of</strong>essionals chasing too few jobs: “At least youcan always find a job.” But nobody said <strong>the</strong>y joined <strong>the</strong> nursingor medical pr<strong>of</strong>ession purely for that reason. Among doctors,<strong>the</strong> choice <strong>of</strong> medical training against ano<strong>the</strong>r science-basedpr<strong>of</strong>ession was in some cases influenced by <strong>the</strong> prospect <strong>of</strong>pr<strong>of</strong>essional advancement and mobility, self-employment andprivate practice.Not all those who had decided on a career in <strong>the</strong> medical fieldentered via <strong>the</strong> course <strong>of</strong> <strong>the</strong>ir choice. Lacking financial backingfrom <strong>the</strong>ir families, uncertain about getting <strong>the</strong> grades orfailing to gain entry, would-be medical doctors had to settle forclinical <strong>of</strong>ficer training or a nursing course, and aspiring clinical<strong>of</strong>ficers became nurses. It was sometimes hard at first to accepta substitute course, especially when o<strong>the</strong>r people said nursingis for “failures”.5.2 “They join for <strong>the</strong> wrong reasons”There were widespread beliefs among nursing and midwiferypr<strong>of</strong>essionals that poor attitudes and unethical behaviour arelinked to people joining nursing for “<strong>the</strong> wrong reasons”. It wasthought that more recent recruits joined because <strong>the</strong>y hadno o<strong>the</strong>r option, because nursing was a last resort when <strong>the</strong>yfailed to qualify for more prestigious pr<strong>of</strong>essions or becauseparents pushed <strong>the</strong>m into it. Pursuing pay, looking only at <strong>the</strong>job market and even as a route to leaving <strong>the</strong> country wereo<strong>the</strong>r presumed reasons for joining nursing.Older nurse managers had noted “very few nurses come witha sense <strong>of</strong> vocation now”. There was a widespread view thatpeople enter nursing with “<strong>the</strong> wrong heart”. It was believedthat as a result, unhappy, disinterested and self-serving recruitsresort to bad habits, become rude and forget <strong>the</strong>ir ethics andaccountability to patients. There were also some commentsby managers about medical doctors’ questionable attitudes towork when <strong>the</strong>y seemed to lack that “inner drive”.Yet more than one nurse and a medical doctor told how <strong>the</strong>ycame to love <strong>the</strong>ir pr<strong>of</strong>ession only when in practice, and astory was told <strong>of</strong> how a lecturer inspired an enthusiasm fornursing in a student whose sole ambition had been to train asa doctor. Indeed, some <strong>of</strong> <strong>the</strong> loudest voices criticising motivesfor joining belonged to staff who had developed an interest in<strong>the</strong>ir pr<strong>of</strong>ession after <strong>the</strong>y started work.5.3 RecommendationsCareer guidance and early contactThere were suggestions from frontline health workers andmanagers on how <strong>the</strong> decision to join nursing and medicinemight be better informed and pr<strong>of</strong>essionalism thus improved.A strenuous pr<strong>of</strong>ession like nursing was said to need emotionalpreparedness, with career guidance at an early stage “to knowwhat it takes”. It was suggested that more talks at schoolsshould set out to “give <strong>the</strong> real picture”.What emerged strongly from participants’ accounts was <strong>the</strong>impact <strong>of</strong> contact with nurses, midwives and medical workersduring formative years. It was told how staff at a boardingschool regularly took pupils to visit a local hospital, and howinterest in nursing grew out <strong>of</strong> voluntary employment initiallyundertaken reluctantly. Experiences such as <strong>the</strong>se suggestvalue in schools arranging contact between students andhealth facilities, and work experience placements.31
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersTraining schools’ admission proceduresThere were calls for nurse training schools to apply tighteradmission procedures, to make sure applicants have not beenforced into nursing and to probe attitude, so as to screen outthose with no “heart” and <strong>the</strong> “wrong elements” that spoil <strong>the</strong>name <strong>of</strong> “genuine” nurses. Admission interviewers should “study<strong>the</strong> psychology <strong>of</strong> <strong>the</strong> person”, investigate thoroughly and rejectapplicants who seem not to be driven by <strong>the</strong> “right reasons”.There were also calls for reform <strong>of</strong> <strong>the</strong> points-based systemthrough which university applicants can be allocated to a nursingcourse when nursing is not <strong>the</strong>ir first or even second choice.Developing and sustaining “<strong>the</strong> right heart”in training schoolsIt was generally thought that <strong>the</strong> person with <strong>the</strong> “wrongheart” cannot be reformed: “Some personalities are naturallyrude, she can’t change”. On <strong>the</strong> o<strong>the</strong>r hand, <strong>the</strong>re were somebeliefs that <strong>the</strong> “right heart” can be developed and sustainedthrough training.With training now falling under <strong>the</strong> remit <strong>of</strong> <strong>the</strong> Ministry <strong>of</strong>Education and Sports, it was commented that nursing schoolshad become indistinguishable from o<strong>the</strong>r higher educationinstitutions, and had been allowed to multiply regardless <strong>of</strong>standards, notably in <strong>the</strong> private sector. It was said that as aconsequence <strong>of</strong> too many nursing schools with ill-qualifiedtutors, students come out lacking respect for patients andpatient’s confidentiality. Some participants added <strong>the</strong>ir voiceto calls for oversight <strong>of</strong> training to revert to <strong>the</strong> Ministry <strong>of</strong>Health “because <strong>the</strong>y were producing competent peopleand now standards have dropped”; “new nurses are not sointerested in <strong>the</strong> work.”The prospects <strong>of</strong> inculcating <strong>the</strong> right attitudes throughpre-qualification training would be improved if nursingand midwifery class-sizes were reduced and tutor capacityimproved: “Two hundred students in a class when you aresupposed to have 60!” and “If you are a serious tutor, howdo you teach and how do you supervise and follow up 200students in one class?”Nurse participants and stakeholders recommended thattraining schools do more to ensure that nurses not only know<strong>the</strong> <strong>the</strong>ory <strong>of</strong> <strong>the</strong> code <strong>of</strong> ethical conduct, but also understandhow it should be applied in <strong>the</strong> workplace. 101 Nursing coursecontent could be improved to make sure that students take onboard <strong>the</strong> role <strong>of</strong> <strong>the</strong> nurse as <strong>the</strong> patient’s advocate.Health and human rights trainingStakeholders advocated for <strong>the</strong> integration <strong>of</strong> health andhuman rights training into curricula, through expansion <strong>of</strong>existing partnerships between training institutions and healthconsumer advocacy organisations. 102 Civil society organisationshave also advocated for health and human rights training forin-service health workers. 103Improve <strong>the</strong> community service element<strong>of</strong> pre-qualification trainingStakeholders stated that community service curricula in mostmedical pr<strong>of</strong>essional education is not <strong>of</strong> sufficient quantityor quality to prepare students for <strong>the</strong> conditions <strong>the</strong>y facein <strong>the</strong> field, and should be improved. Community-basededucation programmes, which typically run for between fourand eight weeks in each year <strong>of</strong> training, have been foundto create some awareness <strong>of</strong> healthcare communities butimplementation concerns and strategies to improve <strong>the</strong>curricula need to be addressed. 104Nurses and Midwives Council registration interviewsNurses and midwives had mixed opinions on <strong>the</strong> interviews<strong>the</strong> Nurses and Midwives Council held as a prerequisitefor registration. Some found <strong>the</strong>m an unnecessary, timeconsumingand expensive imposition, given that <strong>the</strong>y hadalready graduated from nurse training schools and thatattending interviews took <strong>the</strong>m away from caring for patients.It was explained that when nurses and midwives were notaccepted for registration, <strong>the</strong>y were posted to certain hospitalsfor supervised practice and mentoring, and among nursemanagers <strong>the</strong>re were views that this in itself contributed topoor attitudes, as nurses became tired and fed up with <strong>the</strong>irhard life. For o<strong>the</strong>r managers, <strong>the</strong> interviews were a valid way<strong>of</strong> filtering out those with gaps.A mark <strong>of</strong> <strong>the</strong> commitment <strong>of</strong> health workers in <strong>the</strong> study is <strong>the</strong>belief that <strong>the</strong> desire to care, help and make a difference stayswith a person. On <strong>the</strong> o<strong>the</strong>r hand, managers who had observed<strong>the</strong> working environments and cultures <strong>of</strong> differing workplacesbelieved that good intentions can dissipate. Chapters 6 to 10look at how aspects <strong>of</strong> <strong>the</strong> working environment underminemotivations for being a health worker.101. Codes <strong>of</strong> conduct and ethics require health pr<strong>of</strong>essionals to act in a manner that safeguards and promotes <strong>the</strong> interest <strong>of</strong> individual patients; serves <strong>the</strong>interest <strong>of</strong> society; justifies public trust and confidence; and upholds and enhances <strong>the</strong> good standing and reputation <strong>of</strong> <strong>the</strong> pr<strong>of</strong>essions (HWAF-U 2010).102. See Open Society Initiative for East Africa 2010103. Action Group for Health, Human Rights, and HIV/AIDS 2010104. Kaye et al 201132
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers6. Workload6.1 The contextPublic health facilities are required to adhere to a job structure,set centrally, that limits <strong>the</strong> number and cadres <strong>of</strong> staff thatcan be employed at a facility; this defined establishment <strong>of</strong>employment posts is commonly referred to as <strong>the</strong> ‘norm’.Staffing shortfalls: key factsNationally, 48% <strong>of</strong> posts are vacant, representing a shortfall<strong>of</strong> 25,506 staff; <strong>the</strong> lower <strong>the</strong> level <strong>of</strong> facility, <strong>the</strong> greater<strong>the</strong> shortfall (December 2009). 105Across local government districts, 47% <strong>of</strong> approvedpositions are filled; in only 10 <strong>of</strong> <strong>the</strong> 80 districts aremore than 70% <strong>of</strong> positions filled. 106Percentage <strong>of</strong>posts vacantStaffingshortfallPercentage <strong>of</strong>approved posts filledNumber <strong>of</strong>districtsHealth centre II 64% 7,245Health centre III 54% 8,051Health centre IV 45% 3,396General hospital 38% 2,750Regional referral hospital 30% 1,082Main national referral hospital 10% 22221-30 431-40 2541-50 1551-60 1161-70 1571-80 781-90 290-100 1In 2009-10:• 41% <strong>of</strong> medical doctor positions in 42 general hospitals were not filled – a shortfall <strong>of</strong> 180 doctors• 41% <strong>of</strong> nursing positions in 42 general hospitals were not filled – a shortfall <strong>of</strong> 3,380 nurses107• 64% <strong>of</strong> medical doctor positions at 117 health centre IVs were not filled, a shortfall <strong>of</strong> 154.6.2 The health worker experienceConcerns about understaffing and workload were most markedamong health workers and managers in government facilitiesat all levels. At some not-for-pr<strong>of</strong>it and private facilities <strong>the</strong>concern barely surfaced, while at o<strong>the</strong>rs it was a key issuefor participants. Overload was reported even in well-staffedhospitals within <strong>the</strong> not-for-pr<strong>of</strong>it sector.Not surprisingly, health workers told <strong>of</strong> <strong>the</strong> personalrepercussions <strong>of</strong> understaffing and heavy workloads.But also <strong>the</strong>y spoke passionately about <strong>the</strong> damaging effectson patients and on community perceptions <strong>of</strong> health workers.105. Matsiko 2010 Table 3.2106. Adapted from Oketcho et al 2009 Slide 6107. Ministry <strong>of</strong> Health 2010b Tables 3.35 and 5.433
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersThe impact on health workersUnmanageable workloads“Overwhelmed” was a word widely used by nurses speakingabout unmanageable workloads in many government hospitalsand a not-for-pr<strong>of</strong>it hospital: “How can you manage? It doessomething to you.” Nurses spoke <strong>of</strong> being affected mentally and“destroyed” to <strong>the</strong> extent <strong>of</strong> becoming ill: “One nurse runninga full ward, with patients sleeping on <strong>the</strong> floor as well, <strong>the</strong>overwhelming number can affect <strong>the</strong> nurse psychologically.” Witha nurse <strong>of</strong>f sick, <strong>the</strong> workload became even harder to manage.Too many tasks and responsibilitiesIn government health centres, midwifery and nursing staff said<strong>the</strong>y were stretched to <strong>the</strong> limit by too many tasks: “You haveto run <strong>the</strong> ante-natal clinic, conduct deliveries, carry out postnatal,do <strong>the</strong> ward round, one person. Then you have to runmost <strong>of</strong> <strong>the</strong> young child clinic.” Burn-out resulted: “You have todo <strong>the</strong> counselling, take blood, see <strong>the</strong> patients, prescribe for<strong>the</strong>m and do everything. When you leave at <strong>the</strong> end <strong>of</strong> <strong>the</strong> day,you are burnt down completely.”Among nurses in government hospitals, <strong>the</strong>re were complaintsabout having to take on doctors’ duties: “I don’t know when award round was last done. We review patients, even prescribe.”Non-availability <strong>of</strong> a doctor caused dilemmas for midwives,who feared blame if <strong>the</strong>y undertook a medical procedurebeyond <strong>the</strong>ir scope <strong>of</strong> duty. Health centre nurses believed <strong>the</strong>ydid <strong>the</strong> work <strong>of</strong> a clinical <strong>of</strong>ficer. Government hospital nursingassistants complained about undertaking work which should bedone by nurses.Working in a team had been one <strong>of</strong> <strong>the</strong> attractions <strong>of</strong> nursingas a career choice. It was frustrating and disheartening whencooperation was lacking, such as when a relief worker failed toturn up: “No teamwork at all, and when it is an emergency and<strong>the</strong>y delay, you really feel bad. You know what <strong>the</strong> outcome willbe but you can’t help.”Working day and nightHealth workers in government health centres told <strong>of</strong> workingday and night, <strong>of</strong>ten alone, due to understaffing and staffabsences. It was pointed out that clinical <strong>of</strong>ficers, midwives,nurses and nursing assistants had stayed on duty round <strong>the</strong>clock or even longer, contrary to government rules and codes<strong>of</strong> conduct. They said <strong>the</strong>y kept on in <strong>the</strong> face <strong>of</strong> fatiguebecause <strong>of</strong> <strong>the</strong>ir commitment to helping o<strong>the</strong>rs: “If God werenot calling, you could not do this work 24 hours.”Health centre midwives suffered especially. Midwives in ruralhealth centres told <strong>of</strong> working alone day and night, sleepingwith <strong>the</strong>ir children in disused wards, always on call to deal wi<strong>the</strong>xpectant mo<strong>the</strong>rs <strong>of</strong>ten arriving in late stages <strong>of</strong> labour. Amanager acknowledged that a midwife had worked alone andon call for five months.In a private sector health centre scheduled time <strong>of</strong>f had to beforegone for <strong>the</strong> sake <strong>the</strong> patients: “If a doctor prescribes carefor 24 hours we have to stay, and <strong>the</strong>n work again next day.”Over-long shifts and too little time <strong>of</strong>fAmong not-for-pr<strong>of</strong>it hospital nurses <strong>the</strong>re were complaintsabout being forced into working 12-hour shifts. Taking up <strong>the</strong>option <strong>of</strong> working shorter hours would reduce days <strong>of</strong>f fromtwo to one, a hard choice for nurses with children and homesto look after. Days <strong>of</strong>f duty are important times “to do yourown things” and should be an entitlement. Yet it seemedtaken for granted that nurses and nursing assistants living onsite in staff accommodation would turn out in <strong>the</strong>ir “<strong>of</strong>f” timeto fill staffing gaps in some health centres. Even a not-forpr<strong>of</strong>ithospital with clearly specified conditions <strong>of</strong> service wasreported not to give good time <strong>of</strong>f because <strong>of</strong> understaffing.Impacts on healthAmong nursing staff in government health centres and generalhospitals <strong>the</strong>re were concerns about <strong>the</strong> effects on health <strong>of</strong>foregoing or delaying meals because <strong>of</strong> work pressure. Noteating on schedule was a key concern when suffering fromdiabetes, and eating well was important to maintain immunityagainst infection from patients. Even taking a drink was noteasy “because how would it look when <strong>the</strong>y are in pain?”It was even hard to make a quick toilet visit without beingreprimanded by hospital managers.Restricted pr<strong>of</strong>essional developmentManagers’ concerns included <strong>the</strong> impact on clinical <strong>of</strong>ficers’development when <strong>the</strong>y lacked <strong>the</strong> opportunity to workunder <strong>the</strong> guidance <strong>of</strong> a medical doctor, and <strong>the</strong> pr<strong>of</strong>essionallyisolating consequences for staff with no supporting teamwork:“Nobody to consult when you are stuck, nobody to delegate towhen you are unable.”A nursing assistant had been put in a role that took her awayfrom direct patient care, to fill gaps in <strong>the</strong> pr<strong>of</strong>essional staffcomplement: “I want to learn more from <strong>the</strong> patients but Ihave no choice.”There were views that opportunities for fur<strong>the</strong>r study wereblocked because <strong>the</strong> facility would not be able to recruit areplacement if <strong>the</strong> nurse left.34
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersFailing <strong>the</strong> patientsAmong health centre IV workers <strong>the</strong> lack <strong>of</strong> a medical doctorwas one <strong>of</strong> <strong>the</strong> biggest concerns, more important to <strong>the</strong>mthan frustrations about individual workload and personalconsequences: “I can get demoralised seeing someone dyingin my hands because we are missing a doctor” and “It reallyhurts a lot when a patient is dying and you know what shouldbe done. You even go home depressed.”Health workers who expressed <strong>the</strong>se feelings were adamantthat <strong>the</strong>y kept on turning up for work to stop <strong>the</strong> next person’ssuffering: “If I’m depressed because someone has died andI say I am not going to work <strong>the</strong> next day, <strong>the</strong>n we are goingto lose more.”The impact on attitudes, behaviour and practicesHospital nurses acknowledged that overload damaged quality<strong>of</strong> work: “At <strong>the</strong> end you are very tired and no quality <strong>of</strong> workis done.” Participants employed outside <strong>the</strong> government sectorwere especially outspoken about <strong>the</strong> impact on <strong>the</strong> quality <strong>of</strong>nursing in a large government hospital where <strong>the</strong>y had seenperformance drop and patients’ needs neglected. Personaldistress made things worse, <strong>the</strong>y felt: “Understaffed in a wardfull <strong>of</strong> patients, on top <strong>of</strong> family worries, <strong>the</strong>y find <strong>the</strong>y can’tperform, miss things and cannot provide all <strong>the</strong> services patientsneed.” The nursing role should be much more than taking routineobservations and giving treatment, but it was impossible for anoverworked nurse to find time to talk with patients, uncover<strong>the</strong>ir problems and deal with <strong>the</strong> whole picture. Consequentlytask-oriented nursing was unavoidable and even routine taskswere hard to complete: “With two nurses for 50 patients, youare reduced to trouble-shooting, it’s not nursing.”Hospital nurses “torn apart” by patients calling for attentionfound it hard to make patients understand that <strong>the</strong>y had towait <strong>the</strong>ir turn. They recognised <strong>the</strong>y could lose <strong>the</strong>ir temper insuch stressful situations and forget <strong>the</strong>ir basic good intentions:“You become different.” Medical staff had seen <strong>the</strong> effects <strong>of</strong>tiredness: “The tone <strong>of</strong> voice changes” and “The nurses endup losing it, when <strong>the</strong>y are already frustrated by poor pay.”Managers were generally understanding: “As a human beingyou can get irritated and lose your temper because <strong>of</strong> fatigue”and “What do you expect with only half <strong>the</strong> nurses you shouldhave? They become rude.”Participants working in well-staffed private and not-for-pr<strong>of</strong>ithospitals had seen <strong>the</strong> consequences <strong>of</strong> work overload in <strong>the</strong>government sector. Managers observed that a lack <strong>of</strong> opportunityto fulfil <strong>the</strong>ir proper pr<strong>of</strong>essional role “demotivates” nurses,who <strong>the</strong>n adapt to a culture <strong>of</strong> poor standards <strong>of</strong> care in <strong>the</strong>irwork environment. A “don’t care” attitude resulted: “By <strong>the</strong>time she is 30 she is used up. Already tired due to understaffing,she has run out <strong>of</strong> compassion and <strong>the</strong> patients say she is notcaring.” They said that overwhelmed nurses skip out fromwork, ask to be transferred and “run away” to <strong>the</strong> privatesector, where patients do not complain <strong>the</strong>y are neglected.Midwife behaviour towards patients changed as a result <strong>of</strong>working alone all day and all night, especially with “no peace <strong>of</strong>mind” due to personal and family worries: “So you become toughwith <strong>the</strong> mo<strong>the</strong>r so that she understands and you get a live babyand a live mo<strong>the</strong>r.” Managers were well aware <strong>of</strong> <strong>the</strong> unacceptablylong hours midwives put in and spoke openly about <strong>the</strong> effects<strong>the</strong>y had seen: “As time goes by, because <strong>of</strong> <strong>the</strong> fatigue andperpetual calling, somehow as a human being you tend todeteriorate.” Midwives no longer in <strong>the</strong> government sectorunderstood how overtired midwives were forced to “escape” from24-hour work in health centres to make contact with <strong>the</strong>ir families.Among midwives, perpetual responsibility for <strong>the</strong> lives <strong>of</strong>mo<strong>the</strong>rs and babies was “a burden” and it was hard to staypatient with <strong>the</strong> mo<strong>the</strong>rs.Nurses spoke about <strong>the</strong> knock-on effects on <strong>the</strong>ir patients <strong>of</strong><strong>the</strong>ir having to do too many things at once: “You find you arestressed and are rude to patients unknowingly.” There weresome strong views that workload in some large hospitals wasmade worse by senior staff “malingering” or not pulling <strong>the</strong>irweight. A view from <strong>the</strong> private sector was that frustrated juniornurses in <strong>the</strong> government sector “took it out on <strong>the</strong> patients”.Long tiring, shifts led to nurses overwhelmed by <strong>the</strong> workloadbeing short with patients, not interacting with <strong>the</strong>m andconveying disinterest through attitude and expression.Managers and frontline doctors had seen how hunger madenursing staff bad-tempered and rude to patients. It was saidthat long shifts, toge<strong>the</strong>r with poor pay, made nurses look forways <strong>of</strong> “escaping”: not turning up for duty and leaving workearly. Yet it was also said that even after 12-hour shifts, somenurses went on to o<strong>the</strong>r nursing jobs, just to survive financially,and so developed “bad habits”.The impact on community relationsAggressive or demanding outpatients were a particular concernfor medical doctors and clinical <strong>of</strong>ficers. With so many patientswaiting for attention, it was important to prioritise <strong>the</strong>ir treatment.But patients ei<strong>the</strong>r did not understand <strong>the</strong> triage system orbelieved <strong>the</strong>y deserved priority. Such challenges to pr<strong>of</strong>essionaljudgement were especially hard to handle when aggrievedpatients called on local leaders to intervene on <strong>the</strong>ir behalf.Among midwives working round <strong>the</strong> clock, huge distress wascaused by patients accusing <strong>the</strong>m <strong>of</strong> not working when <strong>the</strong>yhad found a little time to rest. This misperception was said t<strong>of</strong>uel community hostility towards health workers.35
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersHealth centre workers realised that no respite in long shiftsled to community complaints about harsh language: “We work<strong>the</strong> whole day without resting, and in <strong>the</strong> late afternoon weget tired and <strong>the</strong>n we change face.” Staff working set hourshad met some hostility from local people who assumed <strong>the</strong>health centre was closed to outpatients when <strong>the</strong>y saw healthworkers socialising toge<strong>the</strong>r towards <strong>the</strong> end <strong>of</strong> <strong>the</strong> workingday. The staff <strong>the</strong>re pointed out that <strong>the</strong>y worked hard to serveoutpatients quickly and so deserved some rest-time afterpatients had stopped arriving. It was also hard to make waitingpatients understand that health workers were not resting when<strong>the</strong>y sat completing paperwork.Health workers in sole charge <strong>of</strong> patients faced a dilemma:go hungry or leave <strong>the</strong> patients alone? Doing <strong>the</strong> latter wasreported to have brought unfortunate consequences for staffwho were arrested for neglect <strong>of</strong> duty. It was said that <strong>the</strong>arrests were motivated by local political candidates seekingto gain electoral favour through discrediting ruling politicianswith oversight <strong>of</strong> <strong>the</strong> facility. Clinical <strong>of</strong>ficers can be left aloneto cover an entire health centre, running from one departmentto ano<strong>the</strong>r. So it was deeply upsetting when a patient arrived,assumed no staff were available, and called on a local leaderwho <strong>the</strong>n complained to higher authorities.The lack <strong>of</strong> a medical doctor rebounded on o<strong>the</strong>r staff: “When<strong>the</strong> patient dies, <strong>the</strong> community look on you as a bad personwho refused to treat <strong>the</strong> patient.” Lack <strong>of</strong> a midwife or qualifiednurse meant that nursing assistants carried out deliveries. Theyfound it hard to convince patients to put <strong>the</strong>ir trust in <strong>the</strong>m,especially as <strong>the</strong>y <strong>the</strong>mselves recognised <strong>the</strong>y lacked <strong>the</strong> fullrange <strong>of</strong> knowledge to save pregnant women in difficulty.6.3 Factors contributing to understaffingand work overloadIt is important to understand <strong>the</strong> structural causes <strong>of</strong>inadequate staff numbers in government health facilities. Itis not necessarily <strong>the</strong> case that <strong>the</strong>re is a shortage <strong>of</strong> healthworkers available in <strong>the</strong> labour force; some governmentsector managers were aware <strong>of</strong> huge numbers <strong>of</strong> applicantsfor advertised vacancies, while o<strong>the</strong>rs said <strong>the</strong>y had failed torecruit. Among managers at district level, views were expressedthat decentralisation <strong>of</strong> <strong>the</strong> health system was to blame for <strong>the</strong>uneven distribution <strong>of</strong> health workers in local government.Recruitment barriersGovernment sector managers explained that financial allocationsfor salaries stood in <strong>the</strong> way <strong>of</strong> recruiting more staff: <strong>the</strong>re wassimply no money in <strong>the</strong> pot to pay more health workers. Evenif funds were made available to fill authorised posts, vacanciesremained due to bureaucratic procedures and <strong>the</strong> absence <strong>of</strong>a District Service Commission tasked with recruiting healthpersonnel to <strong>the</strong> district.Managers explained why remote and rural facilities found ithard to recruit and retain medical doctors, nurses and midwives.They sympathised with new recruits who turned round and leftfor want <strong>of</strong> something to do in a village: “They post someoneout <strong>the</strong>re in <strong>the</strong> wilderness and <strong>the</strong>y expect <strong>the</strong>m to work!” Withno electricity for TV and internet, people were “not connectedto <strong>the</strong> world”. Poor roads and no public transport at night leftstaff “stuck”. Free staff accommodation was widely believed tomake it easier for nurses and medical doctors to leave behind<strong>the</strong> amenities <strong>of</strong> town life. Poor-quality staff quarters, on <strong>the</strong>o<strong>the</strong>r hand, were a deterrent to taking up and staying in posts.An example was cited <strong>of</strong> rented accommodation <strong>of</strong> so poor astandard that it was not safe to raise a child <strong>the</strong>re, leading toa nurse leaving her post. Health workers living in towns spokealong similar lines, adding that <strong>the</strong> cost <strong>of</strong> food was high inremote areas and educational standards poor.It was remarked that medical doctors dislike working in villagesbecause <strong>of</strong> <strong>the</strong> lack <strong>of</strong> opportunity for learning and careeradvancement. It was also said that medical doctors avoid jobsat district level because local politicians misuse health serviceresources and interfere in treatment decisions.Local management factorsIn <strong>the</strong> local government sector <strong>the</strong> problems <strong>of</strong> overwork andtoo little time <strong>of</strong>f stemmed in part from limited managementcapacity to draw up fair duty rosters. It was noted that poorlyplanned rosters scheduled nurses to work back-to-back day andnight shifts. The view among nurses was that properly organisedtime <strong>of</strong>f would motivate <strong>the</strong>m to work. Concerned healthcentre managers said <strong>the</strong>y recognised <strong>the</strong> need to manage staffhours fairly, but with so few staff that was almost impossible.Government sector managers explained how unexpectedabsences worsened <strong>the</strong> load on nursing staff. When staffdid not turn up for work, and especially when <strong>the</strong>y didnot communicate <strong>the</strong>ir intent, managers struggled to findworkers to fill <strong>the</strong> gaps and patients were left waiting. While<strong>the</strong>re was sympathy among managers for <strong>the</strong> personal andfamily problems that kept staff from work, <strong>the</strong>re were als<strong>of</strong>eelings that <strong>the</strong> reasons <strong>of</strong>fered were not always genuine.In Ugandan culture, it was hard to question whe<strong>the</strong>r familysickness or burials had actually occurred and hard to enforcea requirement to produce sick notes. Sometimes managerssuspected, or even knew, that absent staff were “moonlighting”or pursuing a “side income”, “doing o<strong>the</strong>r things to survive”.Managers and frontline workers commented that staff wholived on site were rarely absent, unless <strong>the</strong>y were sick or arelative had a problem, as <strong>the</strong>y would be ashamed whenpatients came looking for <strong>the</strong>m at home.Participants working in government health centres explainedhow <strong>the</strong>ir hours and workload increased at short noticewhen senior colleagues were called away to workshops andmeetings. They rarely questioned why <strong>the</strong>se activities took36
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workerspriority over clinical and management duties at <strong>the</strong> facility,though <strong>the</strong> attraction <strong>of</strong> attendance allowances was alluded to.Paradoxically, staff scarcity was a barrier to holding publicsector health workers to account for <strong>the</strong>ir absences. “Turninga blind eye” was preferable to starting disciplinary procedureswhich would likely lead to a transfer. It would be “suicide” to losesomeone, as <strong>the</strong> remaining few would be more overburdenedand blame <strong>the</strong> manager. Managers noted wryly that <strong>the</strong>y hadlittle leeway to dictate to medical doctors and midwives inunderstaffed facilities: “They hold you at ransom, <strong>the</strong>y know<strong>the</strong>y have power because <strong>the</strong>y can just go and get worksomewhere else.” A frontline doctor echoed <strong>the</strong> point: “Youwork in a relaxed environment, <strong>the</strong>y don’t want to pressure youtoo much and push you away.” It is reported elsewhere thatUgandan facility managers have no authority to discipline staff. 108Scarcity was similarly a barrier to redistribution <strong>of</strong> staff withina district. While in <strong>the</strong>ory a district health manager could movea nurse or midwife from a better-served health centre to easeunderstaffing at ano<strong>the</strong>r centre in <strong>the</strong> district, in practice <strong>the</strong>manager met resistance: “They won’t go because <strong>the</strong>y know<strong>the</strong>y are marketable.”Task-shiftingIt is clear from workers’ accounts that work overload, stressand poor community relations result from doing work forwhich <strong>the</strong>y were not qualified or trained. Such task-shifting hasbeen found in government healthcare facilities elsewhere inUganda. 109 Managers and frontline workers expressed concernsabout staff working beyond <strong>the</strong>ir scope <strong>of</strong> practice, when anursing assistant acted as a nurse, a nurse as a midwife and amidwife as a medical doctor. This is necessitated by shortagesand absences <strong>of</strong> suitably qualified staff. However, it seems thattask-shifting was also a deliberate strategy to save money byemploying less-qualified staff.6.4 RecommendationsStaff shortages and work overload damage health workers, <strong>the</strong>quality <strong>of</strong> care and community relations. Attitudes and behaviourfor which health workers have been criticised stem fromphysical and mental exhaustion, moral distress and burn-out.Health worker/patient ratiosThere were views that <strong>the</strong> norm was out-dated and failed torecognise <strong>the</strong> changing nature <strong>of</strong> services, such as HIV andAIDS treatment clinics, new cadres coming out <strong>of</strong> trainingschools and local population growth. It was recommendedthat standards for patient/nurse and patient/doctor ratios beintroduced so that health worker overload is transparent andquantifiable. Pressures would reduce if ratios were adheredto: “The nurse can manage if a limit is put on <strong>the</strong> number <strong>of</strong>patients per nurse.”Recruitment blockagesSensationalist media headlines about ‘shortages’ contribute tonegative images <strong>of</strong> health pr<strong>of</strong>essions. Health reporters shouldbe informed about obstacles to recruitment. The district levelrecruitment process is cumbersome and lengthy, entailing anumber <strong>of</strong> steps as responsibility and paperwork pass from oneauthority to ano<strong>the</strong>r. The District Service Commission has a roleat several stages, but meets infrequently because <strong>of</strong> <strong>the</strong> costs <strong>of</strong>convening members and advertising vacancies. 110 Many remotedistricts have no functional District Service Commission and nopersonnel <strong>of</strong>ficers to declare <strong>the</strong> vacant posts for recruitment. 111It was suggested that <strong>the</strong> problem <strong>of</strong> unfilled posts andmal-distribution <strong>of</strong> health workers across local governmentdistricts would reduce if health worker recruitment anddeployment were managed centrally. Health workers explainedthat <strong>the</strong> current system de-motivates potential applicants whohave to seek out and apply for positions.Decent staff accommodationParticipants spoke enthusiastically about <strong>the</strong> benefits <strong>of</strong> goodquality staff accommodation, equipped with electric lightingand a clean water supply, suitable for families. A decent place tolive attracted health workers to remote and rural facilities andmade for a more contented workforce. On-site accommodationwas said to reduce absenteeism. Civil society organisationsadvocating for health workers should hold to <strong>the</strong>ir objective <strong>of</strong>monitoring <strong>the</strong> government’s intention to “provide decent andsafe accommodation for health workers at health facilities,especially in hard-to-reach areas” 112 and press for concrete targets.De-urbanise health worker trainingIt was suggested that more training schools located in ruralareas would produce nurses and midwives already adaptedto rural environments. Managers saw value in attachingnurse training to remote hospitals, both to generate a localworkforce and to bind health workers to <strong>the</strong> community. Civilsociety organisations recommend targeting admission policiesto enrol students with rural backgrounds, exposing studentsto greater rural field work and building schools and residencyprogrammes outside major urban areas. 113108. Mwita et al 2009109. East, Central, and Sou<strong>the</strong>rn African Health Community (ECSA-HC) 2010110. See Ministry <strong>of</strong> Health and The Capacity Project 2008.111. Matsiko 2010112. Ministry <strong>of</strong> Health 2010b p102113. Action Group for Health, Human Rights, and HIV/AIDS 201037
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers7. The facility infrastructureGovernment sector workers in rural hospitals and health centres bore <strong>the</strong> brunt <strong>of</strong>dilapidated conditions: non-functioning operating <strong>the</strong>atres, erratic or non-existentelectric power, unreliable access to clean water, blocked sewers, broken-downtransport and no communication technology. They told <strong>of</strong> damaging effects on jobsatisfaction, risks to <strong>the</strong>mselves and deeply felt harm to patients.7.1 The contextOfficial reports paint a gloomy picture <strong>of</strong> <strong>the</strong> physical state <strong>of</strong>health facilities. While new health centres have been built andsome health centres upgraded with newly constructed <strong>the</strong>atres,outpatient departments and maternity wards, <strong>the</strong> governmentacknowledges that most facilities are in disrepair and thatinadequate allocation <strong>of</strong> funds hampers maintenance andrehabilitation. The government also recognises failures in electricityand water supplies, transport and communications technology.What <strong>of</strong>ficial documents do not show is <strong>the</strong> extent <strong>of</strong> broken ornon-functioning power, water, transport and communications,revealed in an independent survey <strong>of</strong> a sample <strong>of</strong> 41 out <strong>of</strong> 64government health centres in two districts. 120 (Box 2)Data from a survey <strong>of</strong> not-for-pr<strong>of</strong>it sector facilities indicate abetter picture, but <strong>the</strong> survey was biased towards urban facilities.Electricity was most <strong>of</strong>ten reported to be “sometimes available”,although in a few cases it was “never available”. Access to waterwas most commonly described as being generally reliable.About two-thirds <strong>of</strong> facilities reported always having access totelephones. Half <strong>the</strong> sites had reliable email access. In a quarter<strong>of</strong> <strong>the</strong> sites, ambulance or transport services were not available. 121Failing infrastructure: key factsMost facilities are in a state <strong>of</strong> disrepair. Rehabilitation<strong>of</strong> buildings is not carried out regularly. 114Many health centre IVs still lack crucial infrastructureto make <strong>the</strong>m fully functional: 49% [<strong>of</strong> <strong>the</strong> 117 healthcentre IVs providing information] ei<strong>the</strong>r have nooperating <strong>the</strong>atre or have an incomplete ornon-functional <strong>the</strong>atre. 115Only about 24% <strong>of</strong> health facilities have electricity or abackup generator with fuel routinely available duringservice hours. Only 31% have year-round water suppliedin <strong>the</strong> facility by tap or available within 500 metres. 116Only 47% <strong>of</strong> all facilities can transport a patient to areferral site in maternal emergencies. 117 An independentevaluation <strong>of</strong> <strong>the</strong> ambulance service in 13 districts <strong>of</strong>nor<strong>the</strong>rn Uganda found only 8% <strong>of</strong> mo<strong>the</strong>rs reportedusing an ambulance to reach <strong>the</strong> health facility during<strong>the</strong>ir last delivery. 118Only 6% <strong>of</strong> health facilities have information andcommunication technology, mostly comprising mobilephone, radio, TV and, to a smaller extent, computers. 119Box 2: Basic conditions in a random sample<strong>of</strong> government health centres in two districts(November-December 2009)PowerWaterTransportCommunication25% no power source10% functioning electric power30% functioning solar panel25% non-functional solar panel1 <strong>of</strong> 5 generator sets functional10% functioning piped water supply10% non-functional piped supply40% functioning rainwater supply10% functioning ambulance12% non-functional ambulance50% functioning motorcycle20% non-functioning motorcycle0% a landline, functioning<strong>of</strong>ficial cell phone or email10% functioning radio call20% non-functioning radio call114. Ministry <strong>of</strong> Health 2010b115. Republic <strong>of</strong> Uganda 2010116. Ministry <strong>of</strong> Finance, Planning and Economic Development 2010117. Ministry <strong>of</strong> Finance, Planning and Economic Development 2010118. Womakuyu 2010119. Ministry <strong>of</strong> Health 2010b120. HEPS-Uganda 2010, Annex IX121. Schmid et al 2008, Chapter 638
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers7.2 The health worker experienceThe state <strong>of</strong> facilitiesAmong government facility managers and district health<strong>of</strong>ficers <strong>the</strong>re were questions about why more health centreswere being constructed when existing facilities could not workas <strong>the</strong>y should. Facility managers in <strong>the</strong> government sectortold <strong>of</strong> struggling with inadequate budgets to repair or replacedecades-old infrastructure: “The only borehole, you pump for30 minutes and <strong>the</strong>n it stops for two hours”. Pumping wateronly every second day and encouraging rainwater collectionin jerry cans and drums was a partial solution. Elsewhere,<strong>the</strong> best that could be hoped for was being earmarked forrehabilitation – “at least we are in a programme” – or “a goodSamaritan” to help connect to a distant water source. On <strong>the</strong>o<strong>the</strong>r hand, external funding coupled with well-managedin-house technical services allowed a not-for-pr<strong>of</strong>it hospitalmanager to speak with pride <strong>of</strong> rainwater conservation andsolar power systems. There was a marked contrast between ahospital where wards were cleaned three times a day and onewhich had no piped water supply “for years”.The impact on health workers“The condition <strong>of</strong> <strong>the</strong> working environment is one <strong>of</strong> <strong>the</strong> biggestchallenges. So that people can work with a smile, wake up in<strong>the</strong> morning and be happy going to work. You enjoy your workand your pr<strong>of</strong>ession.”Low job satisfactionA key concern was <strong>the</strong> state <strong>of</strong> operating <strong>the</strong>atres at healthcentre IVs. Government sector managers spoke <strong>of</strong> <strong>the</strong>atres thatcould not function because <strong>of</strong> poor design or shoddy construction.They said that when a <strong>the</strong>atre was unusable, or lacked properequipment or anaes<strong>the</strong>tists, underemployed medical doctorslost interest and left. Frontline doctors commented that <strong>the</strong> lack<strong>of</strong> opportunity to practise surgery explained <strong>the</strong> unwillingnessto take up a medical doctor post at a health centre IV.For nurses working with only one paraffin lamp and limited fuel,proper care <strong>of</strong> night-time emergency admissions was impossible:“How can you manage to put in <strong>the</strong> intravenous line with a dimlight?” Sharing one paraffin lamp across three wards was veryhard, yet: “We just have to bear with it for <strong>the</strong> betterment <strong>of</strong>our community.” Nurses working with no good light felt <strong>the</strong>ywere failing <strong>the</strong>ir duty to patients in need <strong>of</strong> scheduled treatmentsduring night hours. Hospital communication systems do notwork without power, and midwives can be left to bear <strong>the</strong>brunt when a doctor cannot be called.Risks to health workersWorking with no power or water, health workers naturallywere worried about <strong>the</strong> huge risks to <strong>the</strong>mselves: “We arerisking our lives.” Maternity workers emphasised <strong>the</strong> risk <strong>of</strong>contamination from infected blood when working in <strong>the</strong> dark.Nurses expressed fear <strong>of</strong> assault working <strong>of</strong>ten alone in unlitwards or crossing dark compounds, a risk increased by locklessdoors, breaches in compound fences and inadequately equippedor absent guards: “We fear to answer <strong>the</strong> door when somebodyknocks for help.” No functioning flush toilet at <strong>the</strong> workplaceforced a dangerous walk home through a snake-infested compound.Risks to patientsMidwives and maternity nurses emphasised <strong>the</strong> risks to womengiving birth at night. Assisting deliveries by <strong>the</strong> light <strong>of</strong> a mobilephone or a candle begged from a patient, <strong>the</strong>y were forced todelay repairing episiotomies until daylight. Unable to read <strong>the</strong>patient’s case notes at night, midwives could not tell if she hadHIV and so reduce <strong>the</strong> risk to <strong>the</strong> baby. Only a donor’s gift <strong>of</strong>lamps relieved months <strong>of</strong> “suffering” delivering in <strong>the</strong> dark.Infection control was near impossible when nursing staff had tobeg <strong>the</strong> little water spared by patients’ attendants to wash <strong>the</strong>irhands, and so try to prevent carrying infections to <strong>the</strong> patients.Participants told how expensive fuel for electricity generatorsran out at crucial moments: “Just yesterday we were doingan operation and we had to complete stitching by torchlight.”Sterilisation was “a huge challenge”. As generator power mustbe conserved, it could not be used routinely for preciousequipment, such as an ultrasound machine which mostly stoodidle despite having a trained operator. Limited generator powerdid not allow refrigerated blood storage and patients couldrarely afford <strong>the</strong> costs <strong>of</strong> travel to <strong>the</strong> referral hospital, to <strong>the</strong>distress <strong>of</strong> health workers: “I feel so sympa<strong>the</strong>tic and sorry.”Transport is essential if <strong>the</strong> referral system is to work as intended,and is crucial when a facility cannot provide <strong>the</strong> intendedservices because <strong>of</strong> lack <strong>of</strong> infrastructure, power, equipment,supplies or qualified staff. Health workers showed pride in<strong>the</strong>ir facility when it had a functioning ambulance to transportreferred patients or could rely on an ambulance sent onrequest from a higher tier facility. On <strong>the</strong> o<strong>the</strong>r hand, workingin a facility with no patient transport was deeply upsettingbecause many patients just could not afford to pay <strong>the</strong>ir owntransport costs: “They say <strong>the</strong>y will go to <strong>the</strong> hospital but <strong>the</strong>ygo home and later you find out that <strong>the</strong>y died.” Health workers’distress was acute when a health centre patient was referreddirect to a distant regional referral hospital. They knew thatpatients were deterred not only by <strong>the</strong> travel costs but also by<strong>the</strong> prospect <strong>of</strong> a strange hospital and an alien language.39
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersCommonly, budgets did not stretch to fuel <strong>the</strong> vehicle forreferrals. It was widely acknowledged that patients were askedto pay towards fuel but that was <strong>of</strong>ten beyond <strong>the</strong> reach <strong>of</strong>people in poor communities. The negative impact on nursesand midwives cannot be exaggerated. They came into nursing tosave lives, to use <strong>the</strong>ir knowledge to benefit <strong>the</strong>ir communities.For <strong>the</strong>m it was very hard and frustrating to stand by unhappyand helpless, knowing that a mo<strong>the</strong>r and baby would diebecause <strong>the</strong> vehicle lacked fuel. Nor was it a good experienceto see patients return to <strong>the</strong> facility “in a terrible condition andvery weak” or with complications because <strong>of</strong> <strong>the</strong> lack <strong>of</strong> fuel forreferral. Health workers also spoke <strong>of</strong> <strong>the</strong>ir frustrations whenmechanical problems were left unattended.A managerial concern in <strong>the</strong> government sector was thateffective referral systems need a means <strong>of</strong> communicationfrom lower- to higher-level facilities. Health workers seemedresigned to using <strong>the</strong>ir personal mobile phones and paying forcalls from <strong>the</strong>ir own pockets to contact referral hospitals.Because <strong>of</strong> <strong>the</strong> constraints on providing transport, it wasunusual to hear <strong>of</strong> a vehicle being used to bring patients to ahealth facility. Staff in a government sector hospital were proudthat it provided an ambulance service to bring in emergencypatients, and noted how relations with <strong>the</strong> communitybenefitted as a result. There was also praise and gratitudeexpressed for a project that supported pregnant women’stransport costs, resulting in more facility-based deliveries.The impact on attitudes, behaviour and practicesHealth workers spoke <strong>of</strong> <strong>the</strong>ir distress over how a lack <strong>of</strong>electric power, water and transport affected <strong>the</strong> quality <strong>of</strong>service. They wanted to do <strong>the</strong>ir best for patients but hadto protect <strong>the</strong>mselves too. They explained how patientperceptions <strong>of</strong> rudeness arose from <strong>the</strong> lack <strong>of</strong> power and water.The fear <strong>of</strong> infection influenced <strong>the</strong>ir approach to patients:“Sometimes we come in with a scared heart” and “Sometimesyou shy away from risk and <strong>the</strong> patient thinks you are rude, butit is <strong>the</strong> working conditions.” 122 They also acknowledged that<strong>the</strong> frustrations <strong>of</strong> working in <strong>the</strong> dark caused impatience anddelays that patients construed as neglect.7.3 RecommendationsFrontline staff seemed resigned to working in poor conditionsand struggled to identify ways <strong>of</strong> improving <strong>the</strong>m, short<strong>of</strong> wholesale rehabilitation that would need unrealisticamounts <strong>of</strong> public expenditure. Recommendations aremostly from managers.The building and rehabilitation programmeA suggestion was to invest in good <strong>the</strong>atre facilities and <strong>the</strong>irstaffing in a small number <strong>of</strong> health centre IVs and showcase<strong>the</strong>m as good practice before embarking on fur<strong>the</strong>r work.Responsiveness to problems identified by staffGovernment sector frontline workers noted facility and districtmanagers who had been slow to respond to requests forimproved lighting. Ano<strong>the</strong>r source tells that a similar requestwas not acted on although a large stock <strong>of</strong> lamps was held in<strong>the</strong> district store. 123 Good practices identified in <strong>the</strong> not-forpr<strong>of</strong>itsector included regular meetings between managementand department heads at which faults were raised for action.Health worker ‘ownership’ <strong>of</strong> <strong>the</strong> facilityIt appears beneficial to get facility staff involved in tacklinginfrastructure problems. For example, staff at a governmenthospital organised rainwater collection.The impact on community relationsIt was said that patients refused to be admitted for treatmentwhen <strong>the</strong> toilets did not work and <strong>the</strong>y were not able toba<strong>the</strong>, thus damaging <strong>the</strong> reputation <strong>of</strong> <strong>the</strong> facility. A lack<strong>of</strong> water to flush toilets forced staff to return home, fuellingpatients’ beliefs <strong>the</strong>y were not at work and running <strong>the</strong> risk<strong>of</strong> <strong>the</strong>ir being blamed by local political leaders for leaving <strong>the</strong>workplace while on duty.122. Similar findings reported by Dieleman et al 2007123. Medicines and Health Service Delivery Monitoring Unit 201040
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers8. Equipment and medical suppliesThis chapter looks at <strong>the</strong> impacts <strong>of</strong> deficits in equipment andassociated medical supplies, and <strong>the</strong> following chapter reports<strong>the</strong> impacts <strong>of</strong> shortages <strong>of</strong> medicines in healthcare facilities.8.1 The contextEquipment failures: key factsThere is a shortage <strong>of</strong> basic equipment in health facilities. Only 40% <strong>of</strong> availableequipment was in good condition and about 17% needed replacement [in 2008-09]. 124A survey in 11 districts showed <strong>the</strong> extent to which health facilities lacked equipmentto diagnose and treat malaria in mid-2009. Of <strong>the</strong> 105 facilities surveyed, 83% were in<strong>the</strong> government sector. The survey found:• No functional microscope in about 50% <strong>of</strong> <strong>the</strong> 35 health centre IIIs and 20% <strong>of</strong> <strong>the</strong>10 hospitals and 12 health centre IVs• No malaria rapid diagnostic tests in 86% <strong>of</strong> <strong>the</strong> 83 health centre IIs and IIIs• No haemoglobin measurement equipment in 61% <strong>of</strong> all facilitiesDuring <strong>the</strong> three months prior to <strong>the</strong> survey, none <strong>of</strong> <strong>the</strong> hospitals and healthcentre IVs had all seven components <strong>of</strong> a basic care package for <strong>the</strong> management <strong>of</strong>severe malaria consistently available. The most common ‘stock-out’ was blood fortransfusion, available in only one facility. Blood transfusion sets were lacking in aroundtwo thirds <strong>of</strong> facilities and over half had no giving sets. 125Evidence suggests that only 5% <strong>of</strong> facilities have a vacuum extractor (used for assistedvaginal delivery) and only 10% have a dilation and curettage kit (needed to remove aretained placenta). 1268.2 The health worker experienceHealth workers praised facilities with good diagnostic equipment,such as x-ray and ultrasound, and with a commitment to awell-equipped establishment: “It’s a good place, that’s whyI have stayed so long.” Elsewhere, working with inadequateequipment was a huge challenge, damaging workers’pr<strong>of</strong>essional fulfilment, <strong>the</strong> quality <strong>of</strong> services and communityrelationships. The difficulties were acute in <strong>the</strong> governmentsector, but also present in parts <strong>of</strong> <strong>the</strong> not-for-pr<strong>of</strong>it sector.The impact on health workersGovernment sector medical doctors and nurses told <strong>of</strong>interruptions to <strong>the</strong> supplies <strong>of</strong> oxygen and blood; missingcanulas, needles, giving sets and sutures; minimal availability<strong>of</strong> urine testing kits and family planning supplies; insufficientdressing packs, and absent or faulty diagnostic equipment.Rural midwives in <strong>the</strong> government sector told how <strong>the</strong>ystruggled to provide a service with no delivery kit, cord clamp,sucker, gauze or cotton wool and just one pair <strong>of</strong> scissors.124. Ministry <strong>of</strong> Health 2010b125. Achan et al 2011126. Ministry <strong>of</strong> Finance, Planning and Economic Development 201041
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersWorking without protective wear – gloves, aprons, gumboots,shoes, masks – was a huge risk, especially for midwivesworking in <strong>the</strong> dark: “You are ba<strong>the</strong>d in blood.” Lacking gloves,midwives even used <strong>the</strong>ir own clo<strong>the</strong>s and plastic bags to grasp<strong>the</strong> baby during delivery. Workers in some rural facilities in <strong>the</strong>government sector provided <strong>the</strong>ir own work clo<strong>the</strong>s as, it wassaid, <strong>the</strong> Ministry <strong>of</strong> Health no longer supplied uniforms.In <strong>the</strong> government sector <strong>the</strong>re was widespread frustration atnot being able to work effectively: “What really hinders my workis lack <strong>of</strong> some equipment” and “The equipment does not allowyou to do what you are supposed to do.” Nurses spoke aboutthwarted pr<strong>of</strong>essional fulfilment. Willing to work and capable <strong>of</strong><strong>of</strong>fering a full service, <strong>the</strong>y felt “handicapped” and “disappointed”.As a result, work was nei<strong>the</strong>r enjoyable nor happy: “If I amprovided with what I am supposed to use, I can enjoy <strong>the</strong> work”and “You can’t really be happy in such conditions, but would behappier with equipment to do your best.”Frontline medical doctors spoke <strong>of</strong> “struggling with <strong>the</strong> minimum”and <strong>of</strong> feeling “deflated” by poorly maintained equipment suchas x-ray machines with blown bulbs or no chemical to print <strong>the</strong>film: “You wake up and have <strong>the</strong> same problem, you go home,you come back and it has not changed.” Doctors wanting <strong>the</strong>satisfaction <strong>of</strong> doing <strong>the</strong>ir best for <strong>the</strong>ir patients spoke <strong>of</strong>frustrations such as a lack <strong>of</strong> diagnostic equipment or facilityfor blood counts. Managers recognised that medical doctors“eventually lose morale” when <strong>the</strong>y are unable to operate on apatient because oxygen or sutures are missing, and that beingunable to apply knowledge was “very demotivating”.Failing <strong>the</strong>ir patients greatly distressed nurses and doctors.Patients died because <strong>of</strong> <strong>the</strong> lack <strong>of</strong> essential supplies: “Wewould have saved that life if we had oxygen. It stresses you.”A lack <strong>of</strong> diagnostic equipment lost lives too: “The patientprobably would have survived if you were able to investigate.”Government sector workers faced a dilemma when <strong>the</strong>facility ran out <strong>of</strong> supplies. User charges were abolished in <strong>the</strong>government sector 127 and health workers told <strong>of</strong> prohibitionson asking patients to go and buy missing items: “It is veryannoying, you go home dissatisfied.” The medical doctor has aduty towards <strong>the</strong> patient’s health: “What do you do? Ask <strong>the</strong>patient to buy or see <strong>the</strong>m get worse?” The o<strong>the</strong>r option was“to be kind” and refer <strong>the</strong> patient to a higher-level facility.Participants spoke against <strong>the</strong> policy: “I don’t feel it wrong toask a patient to buy needles in order to help <strong>the</strong>m,” and it wasclear that patients in some facilities were being asked to buysupplies. It was hard to ask a patient to buy items that shouldhave been provided free <strong>of</strong> charge: “I don’t want to be <strong>the</strong> oneto say go and look for a canula.”Participants in facilities with relatively good supplies welcomedrelief from <strong>the</strong> stresses <strong>of</strong> telling patients to buy <strong>the</strong>ir own.They also spoke <strong>of</strong> pride in a facility that did not force patientsto spend <strong>the</strong>ir little money on intravenous fluids, canulas,gloves, dressings and <strong>the</strong> like. There was praise for imaginativemanagement that solved temporary supply problems byborrowing from o<strong>the</strong>r facilities.The impact on attitudes, behaviour and practicesParticipants working in <strong>the</strong> private and not-for-pr<strong>of</strong>it sectorsspoke frankly about effects <strong>of</strong> shortages <strong>the</strong>y had seenduring <strong>the</strong>ir time in government facilities. They told <strong>of</strong> nursesforgetting what <strong>the</strong>y had been taught in training schools andsome not working as a result, so projecting a bad image to <strong>the</strong>community which in turn made nurses feel not respected andprompted <strong>the</strong>m to leave. Participants in <strong>the</strong> government sectordid not identify <strong>the</strong>se effects. However, <strong>the</strong>re was a suggestionthat nurses were reluctant to come to work and face patientsand <strong>the</strong>ir relatives knowing that essential supplies were lacking:“Staff don’t want to come in and look at a mo<strong>the</strong>r with a dyingchild and no canula to give intravenous fluids.”The impact on community relationsHealth workers felt blamed for <strong>the</strong> lack <strong>of</strong> supplies andresented accusations <strong>of</strong> <strong>the</strong>ft. The patient’s attitude changedwhen asked to buy supplies: “You feel bad when somebodyis not appreciating what you are doing.” Patients’ carers weresometimes angry and violent, such as a husband who hit amidwife when asked to buy gloves.There were fears <strong>of</strong> personal repercussions if <strong>the</strong> rule wasdisregarded and <strong>the</strong> patient was asked to buy supplies: “TheGovernment is going to see you as a bad person.” Staff in onefacility were stressed by <strong>the</strong> arrest <strong>of</strong> a health worker whoasked a patient to buy essential supplies. The view <strong>the</strong>re wasthat local political candidates had set <strong>the</strong> arrest in motion todiscredit <strong>the</strong> incumbent leader.127. User charges were abolished in 2001 in all government facilities except private wings in hospitals.42
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers8.3 RecommendationsThe limitations <strong>of</strong> equipment and medical supplies seemed anintractable problem to many participants. Frontline workers saw<strong>the</strong> supply problem as out <strong>of</strong> <strong>the</strong>ir hands and it was hard for<strong>the</strong>m to come up with recommendations o<strong>the</strong>r than <strong>the</strong> obvious– increase equipment and ensure constant treatment supplies.Encourage international donors to provide largeitems <strong>of</strong> equipment directlyThere was a view that mismanagement and corruption dissipateddevelopment partners’ support to <strong>the</strong> Ugandan health budgetand that donors should provide large items <strong>of</strong> equipmentdirectly. It was felt that it would be counter-productive ifdonors were to donate smaller, more easily removable items.Equipment maintenanceThe view was expressed that more attention needed to begiven to <strong>the</strong> maintenance <strong>of</strong> existing medical equipment. It wasfrustrating to have equipment on site that could not be usedbecause <strong>of</strong> broken or missing small parts. The expense <strong>of</strong> <strong>the</strong>parts was a minor issue. Ra<strong>the</strong>r, <strong>the</strong> problem was said to stemfrom inertia and poor organisation among facility management.Improve frontline health worker voiceand participationFrontline health workers showed limited knowledge <strong>of</strong> how<strong>the</strong> ordering and delivery system is supposed to work andhow financial allocations and priorities are set. Workers in<strong>the</strong> government sector told <strong>of</strong> putting requests to facilitymanagement, but did not understand why <strong>the</strong>ir needs werenot met. Workers in district-level facilities commonly blamed<strong>the</strong> Ministry <strong>of</strong> Health for deficits. Participants at a governmenthospital identified as good practice formal consultations bymanagement to find out what equipment frontline workersneeded, and enabling <strong>the</strong>m to participate in decision-makingabout equipment and supplies. Health workers were free toidentify not only equipment essential for patient treatment butalso items that made <strong>the</strong>ir work easier and more comfortable,such as fans and radios. Transparent decision-making onpriorities and implementation allowed workers to have a voiceand see that <strong>the</strong>ir views had been listened to.43
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers9. Medicine suppliesMedicine shortages and ‘stock-outs’ emerged as one <strong>of</strong> <strong>the</strong> biggest challengesfor government health workers. Unable to give <strong>the</strong>ir patients <strong>the</strong> drugs <strong>the</strong>yneeded, health workers grieved for <strong>the</strong>ir patients’ suffering and becamedemoralised by <strong>the</strong> futility <strong>of</strong> <strong>the</strong>ir roles. They struggled with disappointed orangry patients and <strong>the</strong>ir limited understanding <strong>of</strong> <strong>the</strong> reasons for shortfallsin supplies. They were deeply hurt by accusations <strong>of</strong> stealing drugs, <strong>the</strong> lack<strong>of</strong> trust <strong>the</strong> public had in health facility staff, a seemingly hostile press and bywhat <strong>the</strong>y saw as politically motivated moves to discredit <strong>the</strong>m.9.1 The contextDrug availability failures: key facts“The percentage <strong>of</strong> health facilities registering stock-outs in essential medicines hasconsistently been over 60% for <strong>the</strong> last 10 years.” 128The availability <strong>of</strong> 40 essential medicines in <strong>the</strong> period April-June 2010 was recorded in asample <strong>of</strong> 28 government and 18 not-for-pr<strong>of</strong>it facilities across Uganda. None <strong>of</strong> <strong>the</strong> 40medicines was available in every government facility when surveyed, while eight <strong>of</strong> <strong>the</strong>40 were found in all <strong>of</strong> <strong>the</strong> not-for-pr<strong>of</strong>it facilities. Average availability <strong>of</strong> <strong>the</strong> 40 medicineswas 59% in <strong>the</strong> government facilities, compared with 78% in <strong>the</strong> non-for-pr<strong>of</strong>it facilities. 129An assessment <strong>of</strong> <strong>the</strong> pharmaceutical situation in 36 government and 36 not-for-pr<strong>of</strong>i<strong>the</strong>alth facilities with pharmacies or dispensaries in six districts was carried out in 2008.For <strong>the</strong> listed essential medicines, <strong>the</strong> average ‘stock-out’ days per year were 72.9 ingovernment facilities and 7.6 in not-for-pr<strong>of</strong>it ones. 130Only one in three respondents surveyed in 2008 agreed that <strong>the</strong>ir nearest governmentfacility usually had all <strong>the</strong> medicines <strong>the</strong> household needed. 1319.2 The health worker experienceThe drug supply situationOutside <strong>the</strong> government sector, medicine supplies weregenerally thought adequate to treat most conditions. Asufficient supply brought health workers <strong>the</strong> satisfaction <strong>of</strong>working effectively, as well as pride in an efficient facilitythat logged all movements <strong>of</strong> medicines. The not-for-pr<strong>of</strong>itsector was not immune to shortages, however; in one facility,shortages were said to be due to loss <strong>of</strong> revenue because itgave impoverished patients drugs on credit.In parts <strong>of</strong> <strong>the</strong> government sector <strong>the</strong>re was someacknowledgement that government efforts to improve <strong>the</strong>delivery system <strong>of</strong> <strong>the</strong> central medical store had broughtimprovements in supplies <strong>of</strong> essential medicines. It was alsonoted also that drug supply increased after a governmentstamp on packets was introduced. There was enthusiasmabout how better supplies now benefited patients: “Nowwe have enough drugs, I would not say all drugs, and inpatientsget <strong>the</strong> drugs <strong>the</strong> doctors prescribe.”128. Ministry <strong>of</strong> Finance, Planning and Economic Development 2010129. Uganda Country Working Group 2010130. Ministry <strong>of</strong> Health 2008a131. Ministry <strong>of</strong> Health 2008b44
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersThere was sharp contrast between praise for medicine suppliesin better-stocked facilities and disgruntlement among workerselsewhere. Health workers told <strong>of</strong> some essential drugs usedup in a matter <strong>of</strong> weeks, or even days: “They bring one tin <strong>of</strong>quinine tabs for a whole unit” and “Just five tins <strong>of</strong> panadolwhich <strong>the</strong> department can use up in one day.” Complaintscentred on undersupply for population demand; shortfalls insupply where deliveries did not match orders; erratic deliveries,such as oversupply <strong>of</strong> condoms but no anti-malaria drugs,and irregular deliveries which did not conform to promisedquarterly schedules. It was suggested that shortages weremade worse by patients taking unfair advantage <strong>of</strong> briefperiods <strong>of</strong> plenty but with no testing equipment it was hard torefuse drugs to patients who claimed <strong>the</strong> common complaint <strong>of</strong>malaria. And it had been noted that patients turned up with adifferent patient record book every day <strong>of</strong> <strong>the</strong> week in order tostock up with drugs at home.Government facilities typically could not stretch <strong>the</strong>ir budgetsto purchase drugs in <strong>the</strong> private market, and were forced to sitand wait for <strong>the</strong> next delivery from <strong>the</strong> central medical store.However, one hospital dedicated a quarter <strong>of</strong> its private-wingincome to medicines.The impact on health workers and <strong>the</strong> quality <strong>of</strong> careHealth workers said <strong>the</strong>y felt “disappointed” and that <strong>the</strong> lack<strong>of</strong> drugs “demoralises” <strong>the</strong>m. Job satisfaction suffered when<strong>the</strong>y were unable to give patients <strong>the</strong> drugs <strong>the</strong>y needed.Their presence in <strong>the</strong> workplace sometimes seemed futile:“You are here and <strong>the</strong>re is nothing to give <strong>the</strong> patients. You arejust sitting waiting for <strong>the</strong>m, <strong>the</strong>n tell <strong>the</strong>m to go back as <strong>the</strong>reis no drug.” Helplessness was especially hard to bear whenforced to tell poor patients to buy <strong>the</strong>ir medication in <strong>the</strong> privatemarket: “I hate <strong>the</strong> situation <strong>of</strong> being helpless before <strong>the</strong>patient when <strong>the</strong>y can’t afford to buy drugs” and “You feel youhave not done much for <strong>the</strong> patient when <strong>the</strong>y have to buy.”It seemed like fobbing <strong>of</strong>f <strong>the</strong> patient: “You tell <strong>the</strong>m to buy, but<strong>the</strong> patient is expecting answers.” It was hard to be seen asletting down patients keen to have family planning supplies whocould barely afford <strong>the</strong> transport to <strong>the</strong> facility: “You feel so bad,it seems as if you are deceiving <strong>the</strong>m and <strong>the</strong>y lose confidencein you.” Self-esteem suffered when drugs were not available:“They look at you and think <strong>the</strong> health workers are bad, andyet it is <strong>the</strong> government, not us” or “Their eye looks at <strong>the</strong> nurseand that doesn’t make me able to be <strong>the</strong> nurse I want to be.”The biggest source <strong>of</strong> distress for health workers was <strong>the</strong> impacton <strong>the</strong> patients, and <strong>the</strong>y spoke emotionally about how <strong>the</strong>y feltfor <strong>the</strong>ir patients when no medicines were available for <strong>the</strong>m.In <strong>the</strong> case <strong>of</strong> antiretroviral drugs against HIV, which shouldbe taken for <strong>the</strong> rest <strong>of</strong> a person’s life, it was very hard to seepatients go for up to six months without treatment. Healthworkers cared passionately about <strong>the</strong> consequences for poorpatients: “Few can afford even 2,000 shillings [$1], so day afterday <strong>the</strong>y walk here and wait. Walk 15, 20 km despite <strong>the</strong> pain.” 132They felt <strong>the</strong> pain too when patients became more sick whilewaiting for <strong>the</strong>ir families to raise money to purchase medication.Hospital doctors spoke <strong>of</strong> how <strong>the</strong>y were forced to referadmitted patients who could not afford to buy medicines, orjust keep <strong>the</strong>m in a bed without medication. The quality <strong>of</strong>care also suffered when <strong>the</strong> patient could afford only cheaper,inferior drugs which <strong>the</strong>n failed to improve <strong>the</strong>ir condition,resulting in referral, an option many patients could not afford.The impact on community relations“It puts a lot <strong>of</strong> strain on community relations.” Health workerssaid it was hard to make patients and o<strong>the</strong>r communitymembers understand why drugs were not available at all times.They acknowledged that among people sick and in pain <strong>the</strong>rewas little appetite for words <strong>of</strong> explanation, and that <strong>the</strong>complexities <strong>of</strong> <strong>the</strong> supply system were beyond <strong>the</strong> understanding<strong>of</strong> some people without education. But <strong>the</strong>y also told <strong>of</strong> angry,bitter patients who cursed <strong>the</strong>m and refused to listen.In <strong>the</strong> past, Ugandan healthcare users maintained a beliefthat government health facilities lacked medicines even whenreceipts increased. 133 According to health worker participants,<strong>the</strong>re now appears to be a prevailing belief that health facilitiesare well supplied with medicines: “People say why don’t yougive us drugs?” A particular problem arose when a health facilitychanged ownership from not-for-pr<strong>of</strong>it to government and <strong>the</strong>previously superior supply <strong>of</strong> medicines could not be maintained.Health workers said that communities served by governmentfacilities assumed health workers took <strong>the</strong> drugs: “Patients thinkyou steal” and “Patients call us thieves.” They said that patientsbelieved that health workers took government supplies to stock<strong>the</strong>ir own clinics and drug shops, to which patients were <strong>the</strong>nsent to buy medicines. It was acknowledged that such abuseshad occurred. Indeed, good supplies in one hospital wereattributed to <strong>the</strong> fact that few <strong>of</strong> its nurses ran private clinics anddrug shops. Health workers expressed sorrow about <strong>the</strong> lack<strong>of</strong> trust put in <strong>the</strong>m and <strong>the</strong> effect on community attitudes:“When drugs are not <strong>the</strong>re, <strong>the</strong>y tend to hate nurses.”In contrast, it had been observed that patients’ attitudestowards health workers improved when given supplies <strong>of</strong> drugsto last several days. It was especially upsetting to be directlyaccused <strong>of</strong> <strong>the</strong>ft when a patient demanded a drug that <strong>the</strong>clinician knew was not appropriate for <strong>the</strong> patient’s condition.132. Some 51.5% <strong>of</strong> Ugandans live on less than $1.50 a day (UNDP 2010 Statistical Annex)133. Nabyonga-Orem et al 200845
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersThere was widespread indignation at accusations <strong>of</strong> stealingnonexistent medications: “What are <strong>the</strong>y supposed to bestealing?” or “What kinds <strong>of</strong> drugs can we steal? Paracetamol?Because that’s <strong>the</strong> only drug in <strong>the</strong> hospital!” and “How can<strong>the</strong>y take things that are not <strong>the</strong>re!” Health workers felt thatlocal leaders and politicians made matters worse when <strong>the</strong>yfailed to present <strong>the</strong> true picture to complaining patients, andeven accused health workers in front <strong>of</strong> patients: “It is makingus lose morale for what we are supposed to do.”Health workers resented negative stories in <strong>the</strong> print media,TV and radio, believing that journalists blew up single incidentsunfairly to give an exaggerated picture <strong>of</strong> <strong>the</strong> extent to whichfrontline health workers were guilty <strong>of</strong> pilfering drugs.A stakeholder concurred: “We can’t brand all health workersas thieves just because someone has stolen a tin <strong>of</strong> aspirin.”Stakeholders noted that press stories about health workersstealing drugs had increased with <strong>the</strong> work <strong>of</strong> <strong>the</strong> Medicinesand Health Supplies Delivery Monitoring Unit, an autonomousunit set up in October 2009 within <strong>the</strong> President’s Office. 134While <strong>the</strong>re was support for its efforts to expose poor workingconditions as well as abuses, <strong>the</strong> view was expressed that it wasunhelpful to create a media story around every wrongdoing<strong>the</strong> unit uncovered: “They tried to create publicity instead <strong>of</strong>dealing with <strong>the</strong> real issue <strong>of</strong> what is causing <strong>the</strong> stock-outs.”There was hurt and indignation too about top public figuresspoiling <strong>the</strong> pr<strong>of</strong>essions’ reputations when <strong>the</strong>y stated publiclythat health workers are thieves: “How can any patient valuea doctor, value a nurse, when <strong>the</strong>y say such things about us!”There were beliefs that government conspired to make outthat all health workers were thieves although, in <strong>the</strong> opinion <strong>of</strong>health workers, top managers and not frontline workers were<strong>the</strong> chief culprits. Public accusations by <strong>the</strong> President wereespecially damaging to health workers’ self esteem.“Museveni warns medical workersQuoting a proverb that says ‘a dog which stealspays with its back’, Mr Museveni told a rally […]that <strong>the</strong> same would be done to health workerswho steal drugs from now on.” 135“Politicians stop playing gameson <strong>the</strong> right to healthA story is <strong>of</strong>ten told <strong>of</strong> a politician whodelivered a truck laden with ‘medicines’ to ahealth centre in his constituency. The truckwas reportedly containing all <strong>the</strong> medicinesthat this health centre needed at <strong>the</strong> time. Ina country where getting medicines in publicfacilities is intermittent and health workers arereviled for ‘stealing’ medicines, this politicianwas an angel straight from heaven.Now, long after <strong>the</strong> speeches and pleasantrieshad ended, and <strong>the</strong> MP had gone, it was timeto open <strong>the</strong> boxes. But alas, <strong>the</strong> boxes werefull <strong>of</strong> saline solution. […] There was no waymedics at <strong>the</strong> facility would tell people <strong>the</strong>next day that <strong>the</strong>re was no medicine. To <strong>the</strong>politician he had scored a political goal. But in<strong>the</strong> process, <strong>the</strong> health workers had been putin a tight position.” 136“Patients get angry because <strong>the</strong> politicians tell <strong>the</strong>m drugs areprovided”. Views were expressed that politicians deliberatelymislead <strong>the</strong> public: “Government makes <strong>the</strong>m believe <strong>the</strong>y havesent drugs” and “The public is being hoodwinked!” But for apublic servant it would be “suicide” to contradict political masters.134. The Unit’s first annual report exposed malpractices and “vices” identified through its staff visits to 145 facilities in 45 districts, with an average <strong>of</strong> threefollow-up visits in each district. Initially visits were impromptu, in response to “emergency calls” from <strong>the</strong> public about <strong>the</strong> state <strong>of</strong> healthcare and allegeddrug <strong>the</strong>fts, and routine monitoring visits were introduced later in <strong>the</strong> year.135. Emojong 2010136. Kirunda 201146
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers9.3 RecommendationsTransparency at <strong>the</strong> point <strong>of</strong> delivery“They see <strong>the</strong> boxes coming and if next day you say <strong>the</strong>re areno drugs, <strong>the</strong>y feel like beating you up.” Public opening <strong>of</strong>deliveries was one step that government sector health centreshad taken, with varying degrees <strong>of</strong> success, to try to convincecommunities that medicines were not in stock. For example, tocounter <strong>the</strong> community assumption that a lorry had delivereddrugs, it was important to show that boxes <strong>of</strong>floaded containedcondoms or saline solution. When essential medicines weredelivered, <strong>the</strong>ir quantities were verified openly. Healthworkers told how variously <strong>the</strong> chairperson <strong>of</strong> <strong>the</strong> healthunit management committee, <strong>the</strong> elected chair <strong>of</strong> <strong>the</strong> localcommunity, <strong>the</strong> government internal security <strong>of</strong>ficer, policeand patients witnessed <strong>the</strong> opening <strong>of</strong> boxes. This step mustbe supported by paperwork to show what has been orderedand delivered; government health centre recording <strong>of</strong> orders,deliveries and purchases has been described as “appalling”. 137Drug movements within <strong>the</strong> facilityParticipants within <strong>the</strong> not-for-pr<strong>of</strong>it and private sectorsrecommended recording drug inflows and outflows, althoughit was also said that such time-consuming steps were notnecessary when staff were trusted by management and <strong>the</strong>community. Management staff in a not-for-pr<strong>of</strong>it sector healthcentre welcomed scrutiny by <strong>the</strong> higher level body to which itwas accountable.Local leadersThe local government structure produces a large number <strong>of</strong>committee or council members and leaders at village, parishand sub-county level (see Appendix B). These people, <strong>of</strong>tentermed local politicians or local leaders, can have considerableinfluence over <strong>the</strong>ir local communities. Health centre workerstold <strong>of</strong> dissatisfied patients who called on local leaders tosupport <strong>the</strong>ir demands for drugs. It is <strong>the</strong>refore essentialthat local leaders are fully informed and use informationresponsibly. Staff at one facility reported that “trouble fromlocal politicians” had reduced after a meeting with <strong>the</strong>m.Educate community membersSome health workers said <strong>the</strong>y had tried hard to help patientsto understand <strong>the</strong> ordering and delivery system. O<strong>the</strong>rs hadwearied <strong>of</strong> such attempts or had barely tried: “They only wantdrugs, not your words.” Some simply wrote <strong>of</strong>f local peopleas uneducated, illiterate and incapable <strong>of</strong> understanding – apoint <strong>of</strong> view contested by health consumer organisations in<strong>the</strong> study. It was pointed out that patients were not receptiveto explanations when in pain or angry when asked to buymedicines, though it was acknowledged that opportunitiesfor facility-based information sharing do exist, such as withgroups <strong>of</strong> women waiting for pre-natal checks. The mostpromising solution was to talk with community membersduring outreach visits, such as child immunisation days, thoughsome health workers had limited confidence that <strong>the</strong>y couldsucceed in changing entrenched suspicions. O<strong>the</strong>rs pointedto a lack <strong>of</strong> funding for outreach allowances. There were alsoviews that Village Health Teams might have a bigger role insensitising <strong>the</strong> community to <strong>the</strong> real situation.137. HEPS-Uganda 201047
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers10. PayUgandan health workers’ salaries are low compared with those in o<strong>the</strong>r EastAfrican countries. They are also low compared to <strong>the</strong> market value <strong>of</strong> goodsand services in <strong>the</strong> country. 138 Especially among medical doctors, <strong>the</strong> disparitybetween <strong>the</strong>ir salaries and those <strong>of</strong> o<strong>the</strong>r pr<strong>of</strong>essionals is a huge grievance.There have been calls to raise doctors’ salaries to match those <strong>of</strong> high courtjudges, whose income at 6.8 million shillings (US$ 3,664) was more than eighttimes <strong>the</strong> starting salary <strong>of</strong> a senior medical <strong>of</strong>ficer in 2009-10. 139 Regardless<strong>of</strong> how much <strong>the</strong>y <strong>the</strong>mselves were paid, health workers spoke out about <strong>the</strong>damaging consequences <strong>of</strong> low pay for <strong>the</strong>mselves, patients and <strong>the</strong> pr<strong>of</strong>ession.10.1 The contextSalaries: key factsStarting salaries per month in governmentservice in 2009-10 140,141Senior medical <strong>of</strong>ficer UGX 840,749 (USD 453) 142Medical <strong>of</strong>ficer UGX 657,490 (USD 354)Registered nurse UGX 353,887 (USD 191)Nursing assistant UGX 113,306 (USD 61)Average monthly salary for a seniornurse/midwife in government service 143Uganda USD 341Tanzania USD 630Kenya USD 1,384As local government districts have discretion to top up salaries,<strong>the</strong>se vary among staff <strong>of</strong> <strong>the</strong> same level. The Ministry <strong>of</strong>Health introduced salary top-ups in <strong>the</strong> most hard-to-serveareas, to attract and retain staff. It is reported that top-ups<strong>of</strong> up to 30% for six months attracted pr<strong>of</strong>essionals to <strong>the</strong>seareas. 144 Facilities in <strong>the</strong> not-for-pr<strong>of</strong>it and private sectors set<strong>the</strong>ir own pay levels. It is known that not-for-pr<strong>of</strong>it sectorsalaries are lower than in <strong>the</strong> public sector. 14510.2 The health worker experienceThe frontline workers and managers participating in <strong>the</strong> researchsaid <strong>the</strong>y did not join <strong>the</strong>ir pr<strong>of</strong>essions just for <strong>the</strong> money. Theywanted to use <strong>the</strong>ir training to help o<strong>the</strong>rs, prevent and cureillness and save lives: “I became a nurse not so much becauseI am interested in money, though money is also important. Ifeel it really was a vocation.” In any case, salaries were simplynot attractive enough: “With so little money, nurses must wantto care and help patients, just to keep going.” Money wasnever an overriding factor for job satisfaction, though amongfrontline doctors <strong>the</strong>re were expectations <strong>of</strong> earning enough to“help build yourself up” and feel good about helping people at<strong>the</strong> same time. Yet <strong>the</strong>re were some strongly held views amongparticipants that some <strong>of</strong> <strong>the</strong> recent generation <strong>of</strong> healthworkers entered <strong>the</strong> pr<strong>of</strong>ession with no natural interest for itand became disaffected because salaries were so low.Staff in rural health facilities said that despite long workinghours with little chance to rest, <strong>the</strong>y worked over weekendsand on public holidays for <strong>the</strong> sake <strong>of</strong> <strong>the</strong> patients. They evenvolunteered <strong>the</strong>ir help unpaid on top <strong>of</strong> <strong>the</strong>ir regular work, out<strong>of</strong> commitment to patients’ welfare, for instance in HIV clinics.Low salaries were <strong>of</strong> course a huge and widespread concern,and <strong>the</strong>re were many calls for better financial compensation.But it is very striking that when asked about what had tochange to make things better for <strong>the</strong>m, health workersemphasised improvements in <strong>the</strong> infrastructure that wouldresult in better care and treatment for patients. Frustrationwith equipment and supplies outstripped frustration oversalaries, as found in o<strong>the</strong>r studies. 146138. Matsiko 2010139. Ladu 2010140. Matsiko 2010141. Ministry <strong>of</strong> Public Service http://www.publicservice.go.ug/public/Traditinal%20Salary%20Structure%202010%20-%202011.pdf142. 1 US Dollar = 1,856 Ugandan Shillings at 31 March 2010143. Ministry <strong>of</strong> Health 2010b p37144. Matsiko 2010145. Schmid et al 2008146. Fonn et al 200148
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersThe impact on health workersMoney worriesHealth workers said salaries were not enough for <strong>the</strong> costs <strong>of</strong>ordinary daily living, to allow <strong>the</strong>m to pursue a career or tomeet social expectations. They said that money worries gotin <strong>the</strong> way <strong>of</strong> doing <strong>the</strong>ir best work and even contributed tobad practices. Managers said inadequate pay was one <strong>of</strong> <strong>the</strong>biggest challenges to healthcare delivery.Nursing staff spoke heatedly about <strong>the</strong>ir struggles to surviveon low pay and support <strong>the</strong>ir dependents, see <strong>the</strong>ir childrenthrough education, pay for a ro<strong>of</strong> over <strong>the</strong>ir heads, settleessential bills and afford transport to work. Financial worriesadded to <strong>the</strong> stresses <strong>of</strong> long hours and little rest, <strong>the</strong> burden<strong>of</strong> too many patients, <strong>the</strong> frustrations <strong>of</strong> not enough medicalsupplies or <strong>the</strong> lack <strong>of</strong> appreciation in <strong>the</strong> workplace: “If betterpaid, a nurse will work with patients with love and happinessknowing that rent and bills are paid.”In areas where demand for housing had pushed up rents,health workers found housing costs hard to meet or wereforced to pay high transport costs to reach more affordableaccommodation. Paying US $1.50 or more a day for transportwas very hard to afford on a nursing assistant’s salary.In Uganda income is important not just to meet daily livingcosts. There are extended families to support: participantshad up to 15 children depending on <strong>the</strong>m. One <strong>of</strong> <strong>the</strong>satisfactions <strong>of</strong> earning is being in a position to support <strong>the</strong>study costs <strong>of</strong> a family member. As educated people, healthpr<strong>of</strong>essionals naturally want a good education for <strong>the</strong>irchildren. Public primary and secondary education is free, butschools <strong>of</strong>ten impose fees for lunch, uniforms and buildingdevelopment, and many Ugandans favour <strong>the</strong> private schoolsthat comprise over a quarter <strong>of</strong> <strong>the</strong> secondary educationsector. 147 Worry about school fees pervaded health workers’lives. A participant spoke heatedly about <strong>the</strong> impossibility <strong>of</strong>affording university fees <strong>of</strong> US $900 a semester with threechildren and a monthly salary <strong>of</strong> US $330.Failing to meet social expectationsAs a health pr<strong>of</strong>essional <strong>the</strong>re are also social expectationsto meet. Families, friends and social associates assumeyou are well <strong>of</strong>f, and it was shaming to reveal how little <strong>the</strong>salary actually was. Medical doctors especially felt sociallyembarrassed when <strong>the</strong>y could not afford to contribute largesums <strong>of</strong> money at functions held to raise funds for wedding orfuneral expenses. They also spoke <strong>of</strong> how <strong>the</strong>y were expectedto help with school fees or medical costs: “Society expects somuch from you. It’s impossible to convince people that youdon’t have money when you are a doctor.” The pressurecame from <strong>the</strong> community expecting a nurse or doctor tobe “at a certain level” and seeing <strong>the</strong>m as not responsive tocommunity problems. It was also hard for doctors to face<strong>the</strong> disbelief <strong>of</strong> patients begging <strong>the</strong>m to pay for life-savingtreatment that should have been freely available: “You look in<strong>the</strong>ir eyes and see <strong>the</strong> hurt and <strong>the</strong> disappointment.”Medical doctors and senior nurses spoke <strong>of</strong> unaffordablelifestyle aspirations such as a house that befits <strong>the</strong>ir status.Doctors wanted to be in a position to afford a decent housera<strong>the</strong>r than put up with low-standard government sectoraccommodation on site.Disrespect“In Uganda respect comes with how much you earn.” It wassaid that patients “look down on nurses” when <strong>the</strong>y know howlittle <strong>the</strong>y are paid. Rural nursing assistants who were especiallypoorly paid said this would be a barrier to enlisting <strong>the</strong> localcommunity to advocate for higher salaries: “It’s our secret.”Thwarted pr<strong>of</strong>essional ambitionsA widespread and serious concern was unaffordable fur<strong>the</strong>rtraining: “I have to sponsor my own study yet I am serving<strong>the</strong> nation!” Health workers spoke, <strong>of</strong>ten passionately, aboutthwarted ambitions to improve on skills and knowledge.Nursing assistants wanted to train as enrolled nurses ormidwives, and enrolled nurses and midwives to train asregistered nurses and midwives. Moreover, registerednurses wished to add midwifery to <strong>the</strong>ir qualifications orgo to degree level. Doctors wished to bring <strong>the</strong>ir knowledgeup to date and train as specialists.Unfair payParticipants regularly voiced strong opinions that <strong>the</strong> pay wasunfair and undervalued health workers. Nurses complainedthat <strong>the</strong>ir salaries did not reflect <strong>the</strong> years <strong>of</strong> study <strong>the</strong>y hadput in. They pointed to o<strong>the</strong>r medical jobs that required <strong>the</strong>same length <strong>of</strong> training yet were more highly paid: “Nursingis one <strong>of</strong> <strong>the</strong> lowest paid medical pr<strong>of</strong>essions.” Doctorspointed to <strong>the</strong> much higher salaries <strong>of</strong> o<strong>the</strong>r pr<strong>of</strong>essionals:“We send our children to <strong>the</strong> same schools, buy our food at<strong>the</strong> same markets.” It was dispiriting to see <strong>the</strong>ir universitycontemporaries earning so much more yet working less hard.The fact that medical doctors are paid less than secretaries anddrivers in some statutory agencies underscored <strong>the</strong> little valueattached to <strong>the</strong> medical pr<strong>of</strong>ession in Uganda. There weresome strong feelings, notably among managers and practisingdoctors, that low pay reflected a lack <strong>of</strong> political will atministerial and presidential level to invest in healthcare. Therewas some anger about public spending on political campaigns,<strong>the</strong> military and a presidential jet, and about wastage throughcorruption, while healthcare was grossly underfunded.147. Uganda Bureau <strong>of</strong> Statistics 200849
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersSalaries were doubly unfair because <strong>the</strong>y did not reflect <strong>the</strong>long hours many health workers put in: “You can give yourfamily nei<strong>the</strong>r time nor money.” Nor did salary levels takeaccount <strong>of</strong> <strong>the</strong> risks <strong>of</strong> infection health workers faced. Notbeing rewarded for doing <strong>the</strong> same work as higher-grade staffwas thought bitterly unfair. It sometimes seemed to hospitalnurses that doctors did little while <strong>the</strong>y did all <strong>the</strong> work.Nurses complained that after paying for additional training toupgrade <strong>the</strong>ir skills, <strong>the</strong>y lingered for years on <strong>the</strong>ir previoussalary until promotion was granted.A fur<strong>the</strong>r area <strong>of</strong> perceived unfairness was <strong>the</strong> disparity insalaries <strong>of</strong>fered by <strong>the</strong> government, not-for-pr<strong>of</strong>it and privatesectors. Not-for-pr<strong>of</strong>it sector workers pointed to <strong>the</strong>ir longerhours, and it was commented that unlike some governmen<strong>the</strong>alth workers, <strong>the</strong>y worked <strong>the</strong> hours <strong>the</strong>y were paid for.It was pointed out that not-for-pr<strong>of</strong>it and private facilitieswere free to decide <strong>the</strong>ir own salary levels and acknowledgeseniority in <strong>the</strong>ir own way, resulting in lower pay than ingovernment settings. A particular grievance was <strong>the</strong> absence <strong>of</strong>a senior clinical <strong>of</strong>ficer grade in a not-for-pr<strong>of</strong>it facility. A fur<strong>the</strong>rconcern was that <strong>the</strong> government’s salary enhancement foremployment in hard-to-reach areas seemed not to have beenadopted systematically in <strong>the</strong> not-for-pr<strong>of</strong>it sector.Rarely was it said outright that health workers are exploited,although <strong>the</strong>re were views that unfair advantage is taken <strong>of</strong><strong>the</strong>ir pr<strong>of</strong>essional ethics and dedication to patients: “Nursesare trained to love and serve, and no matter how little we arepaid we have to have that love.” Indeed, among managers <strong>the</strong>rewas some intolerance <strong>of</strong> frontline workers’ complaints aboutlow salaries, and an attitude that commitment to <strong>the</strong> workregardless <strong>of</strong> <strong>the</strong> pay was praiseworthy: “Patients have to get aservice, poorly paid or not.” Yet managers were among <strong>the</strong> mostvocal critics <strong>of</strong> salary levels: “The salary is deplorable!” Overall,participants appeared more resigned than militant about unfairpay, though <strong>the</strong>re was some anger that <strong>the</strong> government cited<strong>the</strong> Hippocratic Oath to prevent doctors from protesting.Impact on attitudes, behaviour and practicesHealth workers and managers were encouraged to say whatin <strong>the</strong>ir view explained behaviour regularly criticised in <strong>the</strong>Ugandan media, including being rude to patients, stealingmedicines and supplies, not turning up or coming late to work,and taking money from patients. Health workers acknowledgedthat <strong>the</strong>se bad practices did happen in some places: “It’spoverty. You get a salary <strong>of</strong> US $200, you pay school fees <strong>of</strong>around US $150, you get stuck. You don’t have transport totake you to work, you don’t have food in <strong>the</strong> house, you don’thave anything, children are crying, your parents need you tokeep <strong>the</strong>m. That’s what drives people to do those things.” But<strong>the</strong>y also argued that <strong>the</strong> media exaggerated <strong>the</strong> scale <strong>of</strong> suchpractices by unfairly generalising a single instance to all healthworkers: “It spoils <strong>the</strong> reputation <strong>of</strong> all nurses, it pains anddiscourages us so much.”One <strong>of</strong> <strong>the</strong> hottest topics in <strong>the</strong> Ugandan media is <strong>the</strong> apparentdisappearance <strong>of</strong> essential medicines and medical suppliesbetween <strong>the</strong> central store and patients in government healthfacilities. Theft on <strong>the</strong> part <strong>of</strong> health workers is only oneexplanation for shortfalls in supplies (see Chapter 9). Participantsacknowledged that <strong>the</strong>ft did occur within some health facilities.In <strong>the</strong>ir view, <strong>the</strong> explanation lay with low pay and moneyworries: “They are not stealing medicines because <strong>the</strong>y are evil– <strong>the</strong>ir income does not satisfy <strong>the</strong>ir needs.” Delays in salarypayment were implicated too: “They steal for survival.”In no way was stealing condoned. Some participants expressedsorrow that patients were deprived <strong>of</strong> already scarce supplies.O<strong>the</strong>rs were bewildered that health workers could put <strong>the</strong>irown interests before those <strong>of</strong> <strong>the</strong> patients. Only rarely didparticipants believe that greed led health workers to steal.Some health workers thought that pilfering <strong>of</strong> medicineshappened only on a small scale, and that drugs were taken forpersonal or family needs and not to sell. But <strong>the</strong>re were alsoviews that helping yourself had become a habit, with reports<strong>of</strong> staff openly justifying selling supplies on <strong>the</strong> grounds that<strong>the</strong> facility did not reward <strong>the</strong>m well enough. Participantswith experience <strong>of</strong> closely managed facilities spoke <strong>of</strong> tighteradministrative practices that helped to safeguard medicines.Workplace cultures which accepted stealing were also noted.The suggested solutions were tighter management to reduceopportunities for abuse, and holding staff to <strong>the</strong>ir codes <strong>of</strong>employment. As found in research elsewhere, peer influence tochange behaviour was seldom proposed. 148Taking money from patients is a sensitive topic which somehealth workers were understandably reluctant to discuss.Soliciting bribes from patients was thought to be rare and wasunacceptable because it would add to patients’ poverty. If itdid occur, it was attributable to low pay: “If paid a satisfactorysalary, I think <strong>the</strong>y would not get money from <strong>the</strong> patients.”There was also a view that worries about surviving onretirement pensions drove health workers to ask for bribes. Itwas observed that in some settings, patients expected to givestaff some inducement to attend to <strong>the</strong>m. 149 Such mistrust washurtful and <strong>of</strong>fensive, and it was suggested that <strong>the</strong> distancebetween workers and patients widened as a result. Participantstold <strong>of</strong> scams whereby patients were robbed <strong>of</strong> <strong>the</strong>ir littlemoney by conmen masquerading as health workers, and <strong>of</strong>angry patients subsequently attacking legitimate staff.148. Ferrinho et al 2004149. Hospital health workers in Tanzania frequently commented in focus groups that un<strong>of</strong>ficial payments were more commonly initiated by users than by workers(Stringhini et al 2009)50
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersHealth workers distinguished accepting “appreciation” fromdemanding money, and some acknowledged a temptation toaccept unsolicited money from patients as compensation forill-paid, exhausting work. It was suggested that some seehealth workers accepting appreciation and wrongly concludethat a bribe has passed hands.It was widely believed that urban health workers were forcedto work in two or even three jobs to make ends meet, withgovernment sector employees working also in private clinics orprivate hospitals. One unfortunate consequence, it was said,was to reinforce patients’ suspicions that health workers stealdrugs from <strong>the</strong>ir workplace to sell in private clinics. Moonlightingwas <strong>of</strong>ten known, or suspected, to explain absences: “Mostpeople, when <strong>the</strong>y don’t turn up for work you find <strong>the</strong>y arerunning a clinic somewhere.” It was said that absenteeismwas not a problem in areas where private treatment or drugswere unaffordable. Exhaustion from doing too many jobs wasthought to cause behaviour patients saw as rude.Rural areas were said to <strong>of</strong>fer many fewer opportunities forside-employment, but <strong>the</strong>re it seemed that health workerswere sometimes forced to take time out to tend crops t<strong>of</strong>eed <strong>the</strong>ir families. It was noted that before decentralisation,rural workers regularly saw to <strong>the</strong>ir vegetable gardens beforeleaving for work, when salaries arrived late or not at all. It wassuggested that this habit continued.There were beliefs that absence from <strong>the</strong> workplace wasencouraged by lump sums given notionally to cover transportand attendance at workshops, and <strong>the</strong>re were grievancesabout perceived unfair selection <strong>of</strong> participants: “They onlywant <strong>the</strong> big people.” The more junior staff valued <strong>the</strong> learningand pr<strong>of</strong>essional contacts that workshops <strong>of</strong>fered.Effort at work was affected by low pay, managers felt. Viewswere expressed that nurses put in minimal effort “because <strong>the</strong>yfeel <strong>the</strong>y are not getting what <strong>the</strong>y are worth.” It was observedthat because nurses are paid so little, “<strong>the</strong>y take out <strong>the</strong>irfrustrations on patients’, arrive late, fail to monitor patients andare unkind to <strong>the</strong>m. It was noted how hard it was to get peopleto work when <strong>the</strong>y lacked <strong>the</strong> basic minimum, and that withno “incentive” <strong>of</strong> a decent wage, it was impossible to retainskilled and interested workers. Occasionally, in managers’ eyes,“low morale” was related to low pay. Low pay was argued tocontribute to doctors’ “questionable attitude to work”. Thingswould change with better pay: “When you are paid highly youare more motivated” and “If <strong>the</strong> pay was more, <strong>the</strong> nurses wouldrespect <strong>the</strong>ir work more and respect <strong>the</strong> job that pays <strong>the</strong>m.”10.3 Poor pay, turnoverand loss to UgandaThe research participants were, <strong>of</strong> course, “stayers” in <strong>the</strong>irpr<strong>of</strong>ession. Career histories showed a fair amount <strong>of</strong> mobilityfrom one health facility to ano<strong>the</strong>r, but only very exceptionallydid a participant speak <strong>of</strong> leaving <strong>the</strong>ir pr<strong>of</strong>ession, and thatwas to earn more.The consensus was that <strong>the</strong> biggest turnover was among medicaldoctors. There were firm beliefs that Ugandan-trained doctorsleft <strong>the</strong> government sector to work for NGOs, prestigiousnot-for-pr<strong>of</strong>it hospitals or <strong>the</strong> private sector. Private sectorwork was tempting, in order to get more money and avoid<strong>the</strong> “frustrations” <strong>of</strong> government hospitals. Managers andpractising doctors told how young doctors “run away” fromhard-to-fill rural posts because <strong>of</strong> poor salaries. As well as lowpay, reasons were believed to include limited opportunity to usepr<strong>of</strong>essional skills in poorly equipped facilities, disinclination tolive far from modern amenities and a lack <strong>of</strong> earning potentialfrom private practice. Yet practising doctors explained that formany young doctors, a year or two gaining experience in a ruralsetting, even in deprived circumstances, was a step towardsacceptance for specialist training. Staying longer meant passing<strong>the</strong> age limit for scholarships. Specialism was <strong>the</strong>n <strong>the</strong> gatewayto private practice and considerably higher earnings. In anycase, district level facilities rarely could support <strong>the</strong> costs <strong>of</strong> aspecialist if <strong>the</strong>y wished to return after training.Participants were asked if <strong>the</strong>y had thought about workingabroad and why. For some nurses <strong>the</strong> possibility was remote:family responsibilities came first, <strong>the</strong> barriers to getting anursing job abroad were just too high, or <strong>the</strong>y had not evenrealised it was allowed. For o<strong>the</strong>rs, nursing abroad was areal aspiration, and <strong>the</strong>re were one or two stories aboutdisappointments. Nurses’ reasons for considering workingoutside Uganda counter <strong>the</strong> widely-held perception that <strong>the</strong>lure <strong>of</strong> money pulls nurses to lucrative jobs in o<strong>the</strong>r countries.Better pay was not an overriding consideration. Nursesexplained <strong>the</strong>y were looking for an environment where “<strong>the</strong>re’srespect for what you do” and where <strong>the</strong>y could learn aboutdifferent medical conditions, use equipment <strong>the</strong>y were trainedto use, update <strong>the</strong>ir skills and have <strong>the</strong> chance to advancepr<strong>of</strong>essionally. Individual advancement was not <strong>the</strong> sole drivingfactor: “I would bring my skills back to share with Ugandannurses” and “I would bring back <strong>the</strong> knowledge to my people.”51
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersAmong participants with medical qualifications <strong>the</strong>re werebeliefs that medical doctors left country in large numbersfor “greener pastures”, as well as claims that few <strong>of</strong> <strong>the</strong>irgraduation contemporaries were still in Uganda, though<strong>the</strong> lack <strong>of</strong> hard facts on <strong>the</strong> extent <strong>of</strong> emigration was alsoacknowledged. The prevailing assumption was that doctorsmoved in pursuit <strong>of</strong> money. When questioned about <strong>the</strong>irown intent, doctors spoke about <strong>the</strong> attraction <strong>of</strong> a betterincome. Yet opportunities to work with proper equipmentand “love what you do” also were important – not simply agood salary. Doctors spoke about <strong>the</strong> possibilities <strong>of</strong> workingin highly regarded, well-resourced hospitals in o<strong>the</strong>r EastAfrican countries or in Sou<strong>the</strong>rn Africa. African countries wereattractive because <strong>the</strong>y are close to home, but <strong>the</strong> USA andEurope were not ruled out. Not all doctors wanted to leave forbetter working conditions, and <strong>the</strong>re were also keen ambitionsto take <strong>the</strong>ir skills to countries even more in need <strong>of</strong> medicaldoctors than Uganda, such as Sudan or Somaliland.10.4 RecommendationsUgandan health workers feel undervalued because salary levelsdo not match <strong>the</strong>ir needs and social expectations. The pay isfelt to be unfair and failing to signify an appropriate return forwhat <strong>the</strong>y put in.Not surprisingly, <strong>the</strong>re were very many calls for increasesin basic salaries. There were concerns about exploitationin private clinics and a suggestion that a minimum wage beintroduced. Ideally, <strong>the</strong> same salary structure should apply inall sectors. Government salary scales should recognise first andpost-graduate degrees. There was considerable frustration thatthis issue was not being resolved and calls for reform in orderto attract degree nurses to public sector jobs and ensure <strong>the</strong>ireducation is used to directly support patient care. A commondemand was to address blockages to promotion.There were also practical recommendations to reward effortand improve motivation.Overtime and responsibility paymentsWhile staff <strong>of</strong>ten willingly worked over-long hours for <strong>the</strong> sake<strong>the</strong> patients, <strong>the</strong>re were views that <strong>the</strong>ir extra hours should notgo unrewarded. No health worker told <strong>of</strong> overtime payments.Financial motivators“We are not motivated, <strong>the</strong>y should give us some motivation,some appreciation.” In Uganda “motivation” <strong>of</strong>ten means extramoney or payments in kind. Being given something signifiesappreciation. Non-financial rewards were no substitute formoney: “Lovely words <strong>of</strong> thank you don’t feed a family!”Free accommodation <strong>of</strong> a good standard, with electricity andwater paid for, was hugely appreciated and said to be a factorin attracting and retaining staff. Even free housing <strong>of</strong> lowerstandard was valued and its absence a cause for resentment,especially among nursing assistants.Free food for <strong>the</strong> household, tea and snacks provided at workand Christmas and Easter gifts were identified as especiallyappropriate ways to value and motivate Ugandan health workers.Staff <strong>of</strong> a government facility spoke enthusiastically about <strong>the</strong>help it gave towards costs <strong>of</strong> family burials and medical operations,as well as <strong>the</strong> provision <strong>of</strong> cloth to make <strong>the</strong>ir own uniforms.Generally in Uganda, allowances on top <strong>of</strong> basic salary arecommon and can contribute quite significantly to <strong>the</strong> overallpay. Small allowances for outreach visits, such as to provideimmunisation services, were much appreciated. There were callsfor allowances for risk, housing, transport, responsibility andstudy. 150 Hardship allowances were suggested to compensatefor living and working in remote locations where it is difficultto access facilities and goods, and where <strong>the</strong> standard <strong>of</strong>accommodation is very poor and lacking in essential utilities.A private sector facility’s monthly award for nurses who methigh standards <strong>of</strong> dress and customer care had a multipleeffect in pushing up standards, boosting income and valuingindividual staff.It was pointed out that local government hospitals are allowedto run private wings and that some use <strong>the</strong> income to benefitstaff. One hospital allocated over half <strong>of</strong> that income toenhance <strong>the</strong> monthly salaries <strong>of</strong> all its staff: “health workersfeel owned and happy.” It was recommended that localgovernment hospital administrations inform staff about <strong>the</strong>irprivate wing income and how it is spent.Staff told <strong>of</strong> <strong>the</strong> stresses <strong>of</strong> working alone and bearing soleresponsibility. A good practice cited from <strong>the</strong> not-for-pr<strong>of</strong>itsector is a responsibility allowance paid when a nurse hassole charge <strong>of</strong> a ward.150. Some health workers reported receiving allowances for risk and transport. There seemed little awareness that a proportion <strong>of</strong> government sector salariesconstitutes a housing allowance.52
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers11. The way forwardWork overload, poor infrastructure and <strong>the</strong> lack <strong>of</strong> medical equipment, suppliesand medicines frustrated and distressed health workers. They felt unrewardedfor <strong>the</strong> work <strong>the</strong>y do and undervalued. Their accounts show that workingconditions were <strong>the</strong> root causes <strong>of</strong> bad practices and unethical behaviour, andthat health workers bore <strong>the</strong> brunt <strong>of</strong> <strong>the</strong> blame for system failures. The researchrevealed a vicious circle: impoverished working environments, along with lowpay, affected <strong>the</strong> quality <strong>of</strong> patient care; patients blamed <strong>the</strong> health workers; <strong>the</strong>wider community <strong>the</strong>n distrusted health workers, and so health workers’ distressincreased. The situation was made worse by negative media stories and politicalleaders’ vocal criticism <strong>of</strong> health workers, which fuelled public distrust, damaged<strong>the</strong> standing <strong>of</strong> <strong>the</strong> health pr<strong>of</strong>ession, added to workers’ distress and, mostimportantly, raised <strong>the</strong> barriers to access to healthcare.11.1 Raising <strong>the</strong> voices <strong>of</strong> health workersThe view <strong>of</strong> civil society organisations, and <strong>of</strong> some managers,was that frontline health workers are not empowered to speakup. Indeed <strong>the</strong> concept <strong>of</strong> ‘voice’ was unfamiliar, and <strong>the</strong> ideathat <strong>the</strong>y might speak out and gain support to improve poorworking conditions and <strong>the</strong> quality <strong>of</strong> care was new to manyfrontline health workers. The research identified barriers toindividual health workers voicing <strong>the</strong>ir concerns, and <strong>the</strong>irpreferences for advocacy by representative organisations.Constraints on speaking upThere were views among frontline workers that responsibilityfor improvements lies with facility managers, districtmanagement or <strong>the</strong> Ministry <strong>of</strong> Health. Stakeholders notedthat where decisions are made with no staff involvement “<strong>the</strong>staff are afraid for <strong>the</strong>ir jobs, <strong>the</strong>y fear to speak up.”Anxiety about repercussions was a barrier to speaking out inpublic. It was explained that “in Uganda, <strong>the</strong>re is a lot <strong>of</strong> fear<strong>of</strong> being pin-pointed if you talk out about your problems.” Theresearchers observed some apprehension over signing <strong>the</strong>irconsent form, although health workers were willing to takepart in <strong>the</strong> research and seemed satisfied with <strong>the</strong> researchers’assurances <strong>of</strong> confidentiality and <strong>the</strong> safe-keeping <strong>of</strong> data. Theunspoken fear, it seems, was that <strong>the</strong>ir participation mightrebound on <strong>the</strong>m.Lack <strong>of</strong> respect from management undermined nurses. Thosewith experience in large urban hospitals told <strong>of</strong> senior nursemanagers and administrators who “sat on”, “barked at”and “belittled” <strong>the</strong>m in front <strong>of</strong> patients. They also spoke <strong>of</strong>doctors who publicly ignored and disparaged <strong>the</strong>ir knowledgeand contributions as “mere nurses”: “I have quite <strong>of</strong>tenheard doctors tell a nurse she is stupid.” Such behaviourcoloured patients’ respect for nursing staff and damaged <strong>the</strong>irreputation in <strong>the</strong> wider community: “They think a nurse barkedat is nothing.” They said management blamed nurses unfairly,failed to investigate problems and made <strong>the</strong>ir lives “miserable”.Suppressed and voiceless in <strong>the</strong> workplace, it is not surprisingthat nurses had little appetite for championing <strong>the</strong>ir pr<strong>of</strong>ession.This report has shown that rural workers in governmentfacilities have faced disappointed, distrustful and sometimesangry patients, interfering and bullying local politicians andpolitically engineered attacks on health workers’ credibility.Hostile environments and impoverished workplaces drainedany will <strong>the</strong>y had to do more than meet patients’ needs <strong>the</strong>best <strong>the</strong>y could.Moreover, health workers had few chances to meet withpeople from o<strong>the</strong>r healthcare facilities to exchange experiencesand build solidarity. Nurses spoke enthusiastically about aforum organised by a health sub-district which discussedsolutions to common problems.The low esteem accorded to health workers was a fur<strong>the</strong>rbarrier. It was said that nurses do not speak out because <strong>of</strong>stigma attached to <strong>the</strong> pr<strong>of</strong>ession: “The moment you stand upand say you are a nurse, people see you as a person who killspatients, <strong>the</strong>y assume you are a bad nurse, a failure.”53
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersSpeaking through pr<strong>of</strong>essional associations,unions and regulatory councilsHealth worker participants favoured channelling concernsto <strong>the</strong> Ministry <strong>of</strong> Health, Government or Parliament throughbodies that spoke for <strong>the</strong>m as, unlike individual health workers,such bodies “know <strong>the</strong> way”. Awareness <strong>of</strong> pr<strong>of</strong>essionalorganisations and trades unions was not widespread and<strong>the</strong>re was some confusion over <strong>the</strong>ir names, how <strong>the</strong>irstatus differed and which body did what.Some health workers felt unions were doing a good job,evidenced by salary increases and <strong>the</strong> successful legal defence<strong>of</strong> individual workers. Health workers saw advantages in <strong>the</strong>protection <strong>of</strong> a union and <strong>the</strong> pursuit <strong>of</strong> individual complaints.A union had <strong>the</strong> advantage over an association <strong>of</strong> registrationwith <strong>the</strong> Ministry <strong>of</strong> Labour and permission to negotiate with<strong>the</strong> government.Male frontline workers spoke most enthusiastically about <strong>the</strong>potential <strong>of</strong> unions as a collective voice, and saw a need forlocal organisation and meetings at district level. They alsoidentified a role for unions to streng<strong>the</strong>n advocacy withinhealth facilities and talk to management on behalf <strong>of</strong> <strong>the</strong>workers: “They need to bring in people from above and helpus at a lower level to improve things.” Women too saw <strong>the</strong>potential strength <strong>of</strong> <strong>the</strong> nurses’ union if all nurses joinedcollectively, paid subscriptions and attended meetings. Therewas some confidence that more involvement in unions wouldget nurses listened to at national level. Supporters <strong>of</strong> <strong>the</strong>nurses’ union acknowledged that nurses were not currentlywell-informed about it.It was suggested that pr<strong>of</strong>essional associations might do moreto bring members toge<strong>the</strong>r, such as convening annual meetingsto discuss challenges facing <strong>the</strong> pr<strong>of</strong>ession. Opportunities toattend pr<strong>of</strong>essional association conferences were few buthighly valued, and <strong>the</strong>re were calls for <strong>the</strong>m to be held locally.However, <strong>the</strong>re were also doubts about <strong>the</strong> value <strong>of</strong> <strong>the</strong>unions and pr<strong>of</strong>essional associations. 151 It was pointed out thatbodies did not do enough to inform <strong>the</strong>ir memberships about<strong>the</strong>ir activities or call <strong>the</strong>m to meetings. A lack <strong>of</strong> feedback,no tangible benefits and no evidence <strong>of</strong> proper financialmanagement, alongside rumours <strong>of</strong> power struggles, weredeterrents to workers spending part <strong>of</strong> <strong>the</strong>ir little salary onsubscriptions to remote associations and unions. There werealso suspicions that those at <strong>the</strong> top <strong>of</strong> <strong>the</strong> organisationshad different agendas from workers on <strong>the</strong> frontline. Theeffectiveness <strong>of</strong> representative bodies was also questioned,given a history <strong>of</strong> government suppression.There were conflicting interpretations and somemisunderstandings <strong>of</strong> <strong>the</strong> remit <strong>of</strong> <strong>the</strong> regulatory councils. 152Some health workers saw <strong>the</strong>ir council as equivalent to aunion, with a role to advocate for <strong>the</strong>ir constituency. O<strong>the</strong>rssaw a “punishing attitude”, and complained that <strong>the</strong> Nursesand Midwives Council was “down on nurses” and investigatedonly serious, high-pr<strong>of</strong>ile cases <strong>of</strong> irregular behaviour. Concernswere voiced that <strong>the</strong> council did little to defend nurses accused<strong>of</strong> stealing medicines and that no action had been takenagainst politicians who “beat up” nurses. The nurses’ councilwas seen as remote from nurses on <strong>the</strong> ground, preoccupiedwith meetings, disinclined to inform members <strong>of</strong> what <strong>the</strong>ydiscussed and not independent enough <strong>of</strong> government.It was suggested that it would be better if representatives <strong>of</strong>pr<strong>of</strong>essional associations, unions and regulatory councils wereless remote from workers on <strong>the</strong> ground. In particular, <strong>the</strong>rewere calls for people “up <strong>the</strong>re” to visit health facilities, talkwith health workers and learn about <strong>the</strong>ir difficulties first hand,so that <strong>the</strong> “right voices” were taken to <strong>the</strong> top.Recommendations among managers were that representativeorganisations compare reports from different places andcompile strong collective arguments to improve conditions in<strong>the</strong> workplace, ra<strong>the</strong>r than simply address individual grievancesand traditional welfare issues.Representatives <strong>of</strong> associations and unions acknowledgedshortcomings and weaknesses. They were understaffed andseverely under-resourced, with poor <strong>of</strong>fice facilities. Theconsensus among stakeholders was that individual associationsand unions were not yet strong voices for health workers andthat working in an alliance would be more effective. It wasrecognised that much would have to be done to align <strong>the</strong>efforts <strong>of</strong> multiple and sometimes competing pr<strong>of</strong>essionalunions and associations.151. A survey for <strong>the</strong> Ugandan Association <strong>of</strong> Nurses and Midwives found only one third <strong>of</strong> members completing a questionnaire rated it as very effective inpromoting nursing (Zuyderduin et al 2009)152. The legal functions <strong>of</strong> <strong>the</strong> Nurses and Midwives Council are to regulate standards and conduct; exercise disciplinary control; approve courses <strong>of</strong> study;supervise and regulate training; grant diplomas or certificates; supervise registration and enrolment; advise and make recommendations to <strong>the</strong> Governmenton matters relating to <strong>the</strong> nursing and midwifery pr<strong>of</strong>essions; and exercise general supervision and control over <strong>the</strong> two pr<strong>of</strong>essions (according to <strong>the</strong> Nursesand Midwives Act 1996).54
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersAn advocacy allianceIn Uganda, countless small civil society organisations work topromote health rights. Dependent on financial support froma patchwork <strong>of</strong> sources (mainly development partners), <strong>the</strong>ygain strength through loose, generally informal coalitions basedon common aims. They are broadly aligned to consumers’interests. Health workers’ interests fall mainly to <strong>the</strong>pr<strong>of</strong>essional organisations. Coalitions rarely bridge <strong>the</strong> two sets<strong>of</strong> interest. The Health Workforce Advocacy Forum-Uganda is acoalition <strong>of</strong> health pr<strong>of</strong>essional associations, unions and healthrights organisations. A membership organisation largely madeup <strong>of</strong> health workers, it has recently campaigned for a positivepractice environment for health workers.The Valuing Health Workers research found consensus thata way forward would be for all civil society organisationsconcerned about limits on access to healthcare to join with <strong>the</strong>Health Workforce Advocacy Forum-Uganda, to support andstreng<strong>the</strong>n its advocacy on behalf <strong>of</strong> health workers.11.2 Changing public perceptions<strong>of</strong> health workersParticipants were hugely affected by <strong>the</strong> persistently negativeportrayal <strong>of</strong> health workers in Uganda: “I feel like I am apr<strong>of</strong>essional being abused.” Members <strong>of</strong> civil society andpr<strong>of</strong>essional organisations identified priority actions to reversethat image through targeting <strong>the</strong> media. Strong views wereexpressed by health workers that <strong>the</strong> public must hear <strong>the</strong>irstory: “We haven’t gone to <strong>the</strong> radio to tell people <strong>the</strong> problemis not us. We should be talking about our side <strong>of</strong> <strong>the</strong> story.”The public must be told <strong>the</strong> real causes: “Papers always blame<strong>the</strong> person, saying nurses are rude. etc, but <strong>the</strong>re’s a needto dig and find what really causes it.” People must see <strong>the</strong>contributions health workers make: “We never show why weshould be valued.”Participants said that reporters working for <strong>the</strong> national mediaare inadequately informed about <strong>the</strong> health worker situationand are overly reliant on <strong>of</strong>ficial briefings for <strong>the</strong>ir information.It is important to increase <strong>the</strong> capacity <strong>of</strong> civil society andhealth worker organisations to write press releases, hold pressconferences and build relationships with individual reportersand media houses, so that <strong>the</strong> key campaign messages hithome. It is similarly important to engage with local reportersand try to moderate <strong>the</strong> tendency to create sensational storiesfrom isolated incidents. The Uganda Health CommunicationAlliance is an important ally.While it was widely understood that <strong>the</strong> media look for badnews, <strong>the</strong>re was scope for positive human interest features,such as pr<strong>of</strong>iles <strong>of</strong> individual health workers and <strong>the</strong> work <strong>the</strong>ydo. It will be important to avoid suspicions <strong>of</strong> favouritism inselection <strong>of</strong> <strong>the</strong> health workers featured.Local language radio is highly popular in Uganda and is avehicle <strong>of</strong>ten used by civil society advocacy organisations.Radio call-in shows attract health users voicing complaintsabout local services: “You hear <strong>the</strong>m on <strong>the</strong> radio, it makesus uncomfortable.” While health workers are restricted inwhat <strong>the</strong>y can say publicly, civil society organisations have <strong>the</strong>opportunity to put complaints in <strong>the</strong> wider context and speakup for health workers.11.3 Bridging patient communities andhealthcare facilities and staffConnecting communities and facilitiesThere seemed, from health workers’ accounts, places whererelationships between patient communities and facilitiesworked well. These were places which ignored status “so <strong>the</strong>ydon’t feel you are greater than <strong>the</strong>m” and welcomed patients“on <strong>the</strong> same level”; where <strong>of</strong>f-duty nurses mixed sociallywith patients; where Village Health Team workers visited <strong>the</strong>facility and had direct phone contact with <strong>the</strong> facility headand o<strong>the</strong>r staff; where people called for an ambulance and itcame; where local people volunteered to clean <strong>the</strong> facility andlook after <strong>the</strong> compound; where facility management listenedto what <strong>the</strong> local community wanted from it, and where <strong>the</strong>community saw <strong>the</strong> facility as <strong>the</strong>ir own.At district level, managers told <strong>of</strong> ongoing efforts to buildor repair bridges with communities. There was a role formembers <strong>of</strong> Village Health Teams (where <strong>the</strong>y were functional)as go-betweens to explain to people in <strong>the</strong>ir own homes <strong>the</strong>problems health workers faced. ‘Outreach’, where facility-basedhealth workers took services such as immunisation to <strong>the</strong>community, was thought a good opportunity to talk with peopleon <strong>the</strong>ir own ground, though limited by a lack <strong>of</strong> transport.There were hopes that “empowered” health unit managementcommittees would “tell <strong>the</strong> community <strong>the</strong> truth”. The aimwas for committee members to explain how facilities work, forexample, how supplies are ordered and staff disciplined, as wellas to encourage people to use <strong>the</strong>ir services. But funds wereshort to cover <strong>the</strong> expenses <strong>of</strong> village health workers, outreachand health unit management committee members.55
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers‘Community dialogue’ meetings were recommended to bringtoge<strong>the</strong>r service users, local leaders and those involved inproviding services: “If <strong>the</strong>re can be community dialogue meetingsin each village, <strong>the</strong>n we can discuss with <strong>the</strong>m <strong>the</strong>ir problems.We tell <strong>the</strong>m what we do, <strong>the</strong>y express <strong>the</strong>ir problems, how wego wrong, I also tell <strong>the</strong>m where <strong>the</strong>y go wrong”. Communitydialogues also meant that district managers learnt communityviews about individual health workers.There were places where <strong>the</strong> distance between communitiesand facilities appeared hard to bridge. Patients arrivedexpecting staff not to help, and health workers came to workfearing that patients would complain. “They don’t respect<strong>the</strong> nurses’ needs, we don’t respect each o<strong>the</strong>r.” Interferingand demanding politicians seemed an intractable problem,but health workers reported favourable effects when a toplocal politician’s family used maternity services at a localgovernment facility. Seeing <strong>the</strong> challenges encouraged <strong>the</strong>politician to understand <strong>the</strong>ir root causes. A more generalrecommendation was to invite politicians to spend time infacilities alongside staff to see what <strong>the</strong> work is really like.Civil society organisations have been working to createcommon cause between health workers and patients. Earlyprojects learnt that empowering community members toexercise <strong>the</strong>ir health rights must go hand in hand with valuinghealth workers. O<strong>the</strong>rwise <strong>the</strong>re is a real risk <strong>of</strong> adversarialrelationships between healthcare workers and users. Indeed,early experiences were that community members, fired upwith new knowledge about violations <strong>of</strong> <strong>the</strong>ir health rights,reprimanded workers <strong>the</strong>y perceived to be rude, while healthworkers complained <strong>of</strong> harassment and threatened to resign.Subsequently, community-based training has enabled healthworkers to talk out about <strong>the</strong> structural problems, with serviceusers coming to appreciate <strong>the</strong> reasons behind health workerbehaviour <strong>the</strong>y object to. Now <strong>the</strong> focus <strong>of</strong> community-basedtraining has moved towards fostering mutual understandingand communication through participatory methods involvinghealth workers and community members toge<strong>the</strong>r. 153Mutual respect and understandingHealth workers understood what life is like for patients,<strong>the</strong>y felt <strong>the</strong> pain that patients feel, and <strong>the</strong>y wanted betterconditions to improve things for patients. It was exceptional tohear that patients empathised with health workers: “Patientsalso feel badly when <strong>the</strong>y see us with no way to help <strong>the</strong>m.They don’t blame us. When you explain <strong>the</strong>y understand.”More commonly, health workers said that patients did notunderstand what life is like for health workers: “They don’tunderstand what we go through, that sometimes nurses arerude due to <strong>the</strong> working conditions.” Patients seemed not torealise that health workers, like any o<strong>the</strong>r people, get tired,need to eat and fall sick. Health workers said <strong>the</strong>y tried “to get<strong>the</strong>m to understand we are human beings.”153. Eg TARSC and HEPS 201156
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers11.4 Summary <strong>of</strong> participants’ recommendationsThe findings identified two priorities for action• Value health workers for <strong>the</strong>ir contributions to <strong>the</strong> health <strong>of</strong> Ugandans.• Expose <strong>the</strong> poor working conditions that prevent health workers from providing good-quality healthcare.Four enabling strategies emerged from health workers’ accounts and stakeholder advice1.2.3.4.Improve <strong>the</strong> quality and relevance <strong>of</strong> training.Raise <strong>the</strong> voices <strong>of</strong> health workers through representation.Change public perceptions through <strong>the</strong> media.Build bridges with patient communities.PrioritiesValue health workers for <strong>the</strong>ir contributionsto <strong>the</strong> health <strong>of</strong> UgandansHealth worker terms and conditions <strong>of</strong> service• Review salary scales to determine whe<strong>the</strong>r increases inbasic salaries are possible. Reform government salaryscales to recognise first and postgraduate degrees, in orderto attract degree nurses to public sector jobs and ensure<strong>the</strong>ir education is used to support patient care directly.• Consider <strong>the</strong> establishment <strong>of</strong> a minimum wage and<strong>the</strong> feasibility <strong>of</strong> imposing <strong>the</strong> same salary structurein all sectors (government, not-for-pr<strong>of</strong>it and private).Overtime and responsibility payments• Explore a system for remunerating health workers for overtime.• Consider implementing a responsibility allowance paid whena nurse has sole charge <strong>of</strong> a ward.Small financial motivations• Incentivise staff through small items <strong>of</strong> personal support, suchas food for <strong>the</strong> household, snacks at work, and Christmas andEaster gifts. Contributions towards family burials, medicaloperations and provision <strong>of</strong> cloth for uniforms are well received.• Review current allowances for risk, hardship, housing,transport, responsibility and study, to ensure consistencyand fairness across all facilities.• Use <strong>the</strong> income from local government hospitals’ privatewings to benefit staff, by supplementing salaries or allowances.Ensure working conditions enable health workers to providegood-quality healthcareHealth worker/patient ratios• Introduce standards for patient/nurse and patient/doctorratios, so that health worker overload is transparent andquantifiable, and managers have information to help reducepressure on overloaded staff.Recruitment blockages• Manage health worker recruitment and deploymentcentrally, to address <strong>the</strong> problem <strong>of</strong> unfilled posts anduneven distribution <strong>of</strong> health workers.Decent staff accommodation• The Government should follow through on its strategy toprovide decent and safe accommodation for health workersat health facilities, especially in remote areas. Civil societyorganisations should continue to monitor implementation<strong>of</strong> this strategy and press for concrete targets.Facility infrastructure• Ensure regular meetings between management anddepartment heads, at which facility-related problemscan be raised and decisions taken on actions needed.• Invest in good <strong>the</strong>atre facilities and <strong>the</strong>ir staffing in a smallnumber <strong>of</strong> health centre IVs, and showcase <strong>the</strong>m as goodpractice before embarking on fur<strong>the</strong>r work.Equipment, medical and medicine supplies• Give much more attention to <strong>the</strong> maintenance and quickrepair <strong>of</strong> medical equipment, including systems for monitoringequipment maintenance and adequate stocks <strong>of</strong> spare parts.• Hold regular formal consultations with frontline workersto enable <strong>the</strong>m to participate in decision-making aboutequipment and supplies, and to improve transparencyin equipment procurement processes.• Encourage international donors to provide large items<strong>of</strong> equipment directly.57
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersEnabling strategies1. Improve <strong>the</strong> quality and relevance <strong>of</strong> health worker trainingCareer guidance and early contact• Ensure well-motivated trainees, for example throughmore talks at schools and work experience placements.Training schools’ admission procedures• Reject applicants who seem to be applying for <strong>the</strong> “wrongreasons”, including those allocated to a university coursewhich is not <strong>the</strong>ir first or second choice.Developing and sustaining “<strong>the</strong> right heart” in training schools• Return oversight <strong>of</strong> training to <strong>the</strong> Ministry <strong>of</strong> Health from<strong>the</strong> Ministry <strong>of</strong> Education and Sports.• Reduce nursing and midwifery class-sizes and improvetutor capacity, to ensure <strong>the</strong> right attitudes and practicalunderstanding <strong>of</strong> <strong>the</strong> ethical code are encouragedthroughout pre-qualification training.Health and human rights training• Expand existing partnerships between training institutionsand health consumer advocacy organisations. Improvenursing course content to make sure that students takeon board <strong>the</strong> role <strong>of</strong> <strong>the</strong> nurse as a patient’s advocate.De-urbanise health worker training• Increase <strong>the</strong> number <strong>of</strong> training schools and residencyprogrammes in rural areas to produce staff already adaptedto rural environments and connected to <strong>the</strong> local community.• Improve <strong>the</strong> community service element in medical curriculaand increase <strong>the</strong> exposure <strong>of</strong> urban health students to ruralsettings with increased fieldwork.Nurses and Midwives Council registration interviews• The Nurses and Midwives Council should weigh up <strong>the</strong>advantages <strong>of</strong> screening interviews held as a prerequisitefor registration post-qualification against detrimentaleffects on nurse morale.2. Raise <strong>the</strong> voices <strong>of</strong> health workersSharing <strong>of</strong> experience and common approaches• Encourage staff to meet with people from o<strong>the</strong>r healthcarefacilities to discuss solutions to common problems andcommunicate <strong>the</strong>m to sub-district level managers. Thesemanagers could also be encouraged to instigate similar forums.Speaking through pr<strong>of</strong>essional associations, unions andregulatory councils• Channel health worker concerns to <strong>the</strong> Ministry <strong>of</strong> Health,Government or Parliament through bodies that speak for<strong>the</strong>m, such as pr<strong>of</strong>essional organisations and trade unions.• Pr<strong>of</strong>essional associations and unions should do more tobring members toge<strong>the</strong>r, for instance at local generalmeetings, and make greater efforts to visit facilities and talkwith health workers so that <strong>the</strong> “right voices” can be takento <strong>the</strong> top. They should compile strong collective argumentsto improve conditions in <strong>the</strong> workplace, as well as addressingindividual grievances and traditional welfare issues.• The Health Workforce Advocacy Forum – Uganda (a coalition<strong>of</strong> health pr<strong>of</strong>essional associations, unions and health rightsorganisations) should expand its membership and continue itscampaign for a positive practice environment for health workers.3. Change public perceptions by influencing <strong>the</strong> media• Inform journalists about <strong>the</strong> obstacles to health workerrecruitment and discourage <strong>the</strong>m from writing sensationalistor negative stories in <strong>the</strong> media. Put complaints on locallanguage radio call-in shows into a wider context. Encourage<strong>the</strong> running <strong>of</strong> positive human interest features, such aspr<strong>of</strong>iles <strong>of</strong> individual health workers and <strong>the</strong> work <strong>the</strong>y do.Work with <strong>the</strong> Uganda Health Communication Alliance.• Improve <strong>the</strong> capacity <strong>of</strong> civil society and health workerorganisations to write press releases, hold press conferencesand build relationships with individual reporters and mediahouses, so <strong>the</strong> key campaign messages hit home.4. Build bridges between patient communities, healthcarefacilities and staffTransparency on drug availability• Use well-managed public opening <strong>of</strong> medicine deliveries tohelp convince communities that medicines are not in stock,and to counter accusations <strong>of</strong> <strong>the</strong>ft. Call on local notables,police or patients to witness <strong>the</strong> opening <strong>of</strong> boxes. Supportwith paperwork to show what has been ordered and delivered.• Ensure that local leaders are fully informed through regularmeetings about <strong>the</strong> demand for and supply <strong>of</strong> drugs andthat <strong>the</strong>y use this information responsibly.Connecting communities and facilities• Use opportunities to talk with people on <strong>the</strong>ir own groundand explain <strong>the</strong> problems health workers face, for instancethrough Village Health Teams, facility-based health workersproviding outreach immunisation services, and talks towomen awaiting prenatal checks.• Promote community dialogue meetings bringing toge<strong>the</strong>rservice users, local leaders and health unit managementteams. Increase funds to cover <strong>the</strong>se activities.• Invite top local politicians to spend time in facilitiesalongside staff to see what <strong>the</strong> work is really like.• Civil society organisations should continue <strong>the</strong>ir work tocreate common cause between health workers and patients.58
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersAppendix A: Sample detailsTable A.1Number <strong>of</strong> facilities and participants by regionKampala Central West South West North North East EastFacilities 3 1 5 1 4 1 3Participants 17 6 31 4 27 17 20Table A.2Level <strong>of</strong> facility by provider typeReferral Hospital General Hospital Health Centre IV Health Centre III TotalGovt Govt NFP* Private Govt NFP* Private Govt NFP* Private3 2 3 1 4 - - 2 2 118*NFP: Not-for-pr<strong>of</strong>itTable A.3Distribution <strong>of</strong> districts according to Ministry <strong>of</strong> Health hard-to-serve scoresVery hard- to-serve(score 55-100)Hard-to-serve(score 35-54)Medium hard-toserve(score 20-34)Somewhat hard-toserve(score 1-19)Not hard-toserve(score 0)TotalDistrictsMinistry 13 13 14 13 3 56Sample 2 2 2 1 1 8The sampling design aimed at a spread <strong>of</strong> districts in terms<strong>of</strong> how <strong>the</strong> Ministry <strong>of</strong> Health ranked <strong>the</strong>m as hard-to-serve.The Ministry’s scoring formula took into account degree <strong>of</strong>insecurity, measured by <strong>the</strong> proportion <strong>of</strong> <strong>the</strong> populationin internally displaced persons camps (50% <strong>of</strong> total score);distance from <strong>the</strong> capital, Kampala (10%); presence <strong>of</strong> socialamenities and utilities (bank, grid electricity, tarmac road anda tertiary education institution) (10%), and <strong>the</strong> proportion<strong>of</strong> approved staff positions appropriately filled with healthworkers (30%). 154 The formula was designed some years agowhen Uganda had only 56 districts and when insecurity wasgreater than at <strong>the</strong> time <strong>of</strong> this study. Researchers have notedsome anomalies in <strong>the</strong> scoring. 155 The scores were <strong>the</strong>reforeonly a guide to sampling decisions. Table A.3 shows that <strong>the</strong>sample under-represents districts that scored 1 to 19. 156154. Africa Health Workforce Observatory 2009155. Ministry <strong>of</strong> Health 2009a156. Based on Africa Health Workforce Observatory 2009, Annex 259
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersFigure 6Enrolled and registered nurse/midwife participants (n=74)25Comprehensive2021NurseMidwife15Nurse / midwife1410595 51080Enrolled2Registered60
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersAppendix B:Local government structures in UgandaLocal government is organised in five tiers from <strong>the</strong> village to <strong>the</strong> district, as outlined below. 157A village is <strong>the</strong> lowest political administrative unit. A village usually consists <strong>of</strong> between 50 and 70 householdsand 250 to 1,000 people. The 2002 Census found 44,000 villages. 158 Each village is run by a local council I (LCI)and is governed by a LCI chairman and nine o<strong>the</strong>r executive committee members.The parish, <strong>the</strong> next level up from <strong>the</strong> village, is made up <strong>of</strong> a number <strong>of</strong> villages. Each parish has a local council II (LCII)committee, made up <strong>of</strong> all <strong>the</strong> chairmen <strong>of</strong> <strong>the</strong> village LCIs in <strong>the</strong> parish. Each LCII elects, from among its members, anexecutive committee. LCIIs are largely involved in settling land distributions and mobilising <strong>the</strong> community for variousactivities. The parish is largely run by a parish chief, a government employee who provides technical leadership to <strong>the</strong> LCII.The sub-county is <strong>the</strong> next level up and is made up <strong>of</strong> a number <strong>of</strong> parishes. The sub-county is run by <strong>the</strong> sub-countychief on <strong>the</strong> technical side and by an elected local council III (LCIII) chairman and his or her executive committee. Thesub-county also has an LCIII council, a kind <strong>of</strong> parliament at that level, complete with a speaker and a deputy speaker.The council consists <strong>of</strong> elected councillors representing <strong>the</strong> parishes, o<strong>the</strong>r government <strong>of</strong>ficials involved in health,development and education, and NGO <strong>of</strong>ficials in <strong>the</strong> sub-county. In towns, a sub-county is called a division.A county is made up <strong>of</strong> several sub-counties. Each county is represented in <strong>the</strong> national parliament by an electedmember (an MP). In major towns, <strong>the</strong> equivalent <strong>of</strong> a county is a municipality (which is a set <strong>of</strong> divisions). LCIII executivecommittee members <strong>of</strong> all <strong>the</strong> sub-counties constitute <strong>the</strong> local council IV (LCIV). They <strong>the</strong>n elect an LCIV executivecommittee from among <strong>the</strong>mselves. These committees have limited powers, except in municipalities, which <strong>the</strong>y run.A district is led by an elected local council V (LCV) chairman and his executive. There is also an elected LCV council, withrepresentatives from <strong>the</strong> sub-counties and technical staff in <strong>the</strong> district. There are also district councillors representingspecial interest groups such as women, youth and disabled people. The council debates budgets, decisions and bylaws.On <strong>the</strong> technical side, <strong>the</strong> district is led by a chief administrative <strong>of</strong>ficer, appointed by central government. The districtalso has heads <strong>of</strong> various departments such as health, education, environment and planning, which are responsible forrelevant matters across <strong>the</strong> whole district.Uganda has an exceptionally high number <strong>of</strong> districts, <strong>the</strong> total having risen from 17 at independence in 1962 to 112in July 2010. In 2008, when its districts had grown to 79, Uganda stood fourth in <strong>the</strong> world in number <strong>of</strong> highest levelsub-national administrative units (ie districts). 159 Since <strong>the</strong> current president, Yoweri Museveni, came to power in 1986,78 districts have been created. It has been noted that bursts in district creation occurred around <strong>the</strong> times <strong>of</strong> presidentialelections in 1996, 2000 and 2006; 160 that pattern continued with fur<strong>the</strong>r districts created around <strong>the</strong> 2010 election.157. Drawing on Kavuma 2009158. Africa Health Workforce Observatory 2009159. Green 2008160. Green 200861
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersReferencesAchan J, Tibenderana J, Kyabayinze D, Mawejje H, Mugizi R,Mpeka B, Talisuna A, D’Alessandro U (2011) Case Management<strong>of</strong> Severe Malaria – A Forgotten Practice: Experiences fromHealth Facilities in Uganda, PLoS ONE 6, 3.Action Group for Health, Human Rights, and HIV/AIDS (AGHA)(2010) Civil Society Organisations Perspectives and Priorities:Health Sector Performance FY 2009-2010, Kampala: AGHA.Africa Health Workforce Observatory (2009) Human Resourcesfor Health Country Pr<strong>of</strong>ile: Uganda, Africa Health WorkforceObservatory.Awases M, Gbary A, Nyoni J and Chatora R (2004) Migration<strong>of</strong> Health Pr<strong>of</strong>essionals in Six Countries: A Syn<strong>the</strong>sis Report,Brazzaville: World Health Organisation Regional Office forAfrica, World Health Organisation.Azfar O, Livingston J and Meagher P (n.d.) Decentralization inUganda sticerd.lse.ac.uk/dps/decentralisation/Uganda.pdfBaguma, R (2010) Ugandans now richer, report says, NewVision, 26 October.Banerjee S, Faiz O, Rennie JA, Balyejjusa J and Walsh M (2005)Bridging <strong>the</strong> health gap in Uganda: <strong>the</strong> surgical role <strong>of</strong> <strong>the</strong>clinical <strong>of</strong>ficer, African Health Sciences, 5, 1, 86-89.Baryahirwa S (2010) The Uganda National Household Survey2009/2010, PowerPoint presentation, 26 October.Benavides, B (2009) Implementation <strong>of</strong> Performance SupportApproaches in Central America and Uganda, Chapel Hill, NC:The Capacity Project.Björkman M, and Svensson J (2007) Power to <strong>the</strong> People: Evidencefrom a Randomized Field Experiment <strong>of</strong> a Community-BasedMonitoring Project in Uganda, World Bank Policy ResearchWorking Paper No. 4268, Washington DC: World Bank.Burnham GM, Pariyo G, Galiwango E and Wabwire-Mangen F(2004) Discontinuation <strong>of</strong> cost sharing in Uganda, Bulletin <strong>of</strong><strong>the</strong> World Health Organisation, 82,187-195.Chaudhury N, Hammer J, Kremer M, Muralidharan K andRogers FH (2006) Missing in action: teacher and healthworker absence in developing countries, Journal <strong>of</strong> EconomicPerspectives, 20, 1, 91-116.Dal Poz M, Gupta N, Quain E and Soucat A (Eds) (2009)Handbook on Monitoring and Evaluation <strong>of</strong> Human Resourcesfor Health with Special Applications for Low- and Middle-Income Countries, USAID/World Bank/WHO.Dambisya YM (2004) ‘The fate and career destinations <strong>of</strong> doctorswho qualified at Uganda’s Makerere Medical School in 1984:retrospective cohort study’, British Medical Journal 329, 600–601.De Vries D, Blair G and Morgan K (2009) Evaluation <strong>of</strong> <strong>the</strong>Capacity Project’s Human Resources Information Systems(HRIS) Streng<strong>the</strong>ning Process in Swaziland, Uganda andRwanda, Chapel Hill, N.C: The Capacity Project.Dieleman M, Bwete V, Maniple E, Bakker M, Namaganda G,Odaga J and van der Wilt GJ (2007) ‘I believe that <strong>the</strong> staffhave reduced <strong>the</strong>ir closeness to patients’: an exploratory studyon <strong>the</strong> impact <strong>of</strong> HIV/AIDS on staff in four rural hospitals inUganda, BMC Health Services Research 7, 205.East, Central, and Sou<strong>the</strong>rn African Health Community (ECSA-HC)( 2010) Task Shifting in Uganda: Case Study. Washington,DC: Futures Group, Health Policy Initiative, Task Order 1.Emojong JA (2010) Museveni warns medical workers, DailyMonitor, 16 December.Ferrinho P, Omar MC, Fernandes M, Blaise P, Bugalho AMand Van Lerberghe W (2004) Pilfering for survival: how healthworkers use access to drugs as a coping strategy, HumanResources for Health, 2,4.Fonn S, Mtonga AS, Nkoloma HC, Bantebya KyomuhendoG, Dasilva L, Kaziliman E, Davis S and Dia F (2001) Healthproviders’ opinions on provider-client relations: results <strong>of</strong> amulti-country study to test Health Workers for Change, HealthPolicy and Planning, 16 (Suppl. 1), 19–23.Green E (2008) District Creation and Decentralisation in Uganda,Working Paper No. 24, Development as State-Making, Crisis StatesResearch Centre, London: LSE Development Studies Institute.Hagopian A, Zuyderduin A, Kyobutungi N and Yumkella F (2009)Job satisfaction and morale in <strong>the</strong> Ugandan health workforce,Health Affairs 28, 5, w863-w875.Harrowing J and Mill J (2010) Moral distress among Ugandannurses providing HIV care: a critical ethnography, InternationalJournal <strong>of</strong> Nursing Studies, 47, 6, 723-731.Harrowing J (2011) Compassion practice by Ugandan nurseswho provide HIV care, OJIN: The Online Journal <strong>of</strong> Issues inNursing, 16, 1, Man 5.62
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersHealth Workforce Advocacy Forum-Uganda (HWAF-U) (2010)Health workers call on each o<strong>the</strong>r to observe code <strong>of</strong> conductand ethics and on government to improve working conditions,Press Release 1 May, Kampala: HWAF-U.HEPS-Uganda (2010) Right to Essential Medicines: TrackingUganda’s Health Sector in Budgeting, Financing and Delivery<strong>of</strong> Essential Medicines, Kampala: HEPS-Uganda.Kapiriri L, Norheim OF and Heggenhougen K (2003) Publicparticipation in health planning and priority setting at <strong>the</strong> districtlevel in Uganda, Health Policy and Planning 2003, 18, 2, 205-213.Kavuma RM (2009) Explainer: Local government structuresin Uganda, The Guardian, http://www.guardian.co.uk/katine/2009/dec/14/local-government-explainerKaye D, Mwanika A, Burnham G, Chang LW, MbalindaSN, Okullo I, Nabirye RC, Muhwezi W, Oria O, Kijjambu S,Atuyambe L and Aryeija W (2011) The organization andimplementation <strong>of</strong> community-based education programsfor health worker training institutions in Uganda, BMCInternational Health and Human Rights, 11(Suppl 1), S4.Kidder J (2010) Streng<strong>the</strong>ning Health Unit ManagementCommittees in Uganda http://www.intrahealth.org/page/streng<strong>the</strong>ning-health-unit-management-committees-in-ugandaKiguli J, Ekirapa-Kiracho E, Okui O, Mutebi A, MacGregor H,Pariyo GW (2009) Increasing access to quality health care for<strong>the</strong> poor: community perceptions on quality care in Uganda,Patient Preference and Adherence, 3, 77-85.Kirunda KA (2011) Politicians stop playing games on <strong>the</strong> right tohealth, Daily Monitor, 16 February.Kiwanuka SN, Ekirapa EK, Peterson S, Okui O, Hafizur RahmanM, Peters D and Pariyo GW (2008) Access to and utilisation <strong>of</strong>health services for <strong>the</strong> poor in Uganda: a systematic review<strong>of</strong> available evidence, Transactions <strong>of</strong> <strong>the</strong> Royal Society forTropical Medicine and Hygiene, 102, 11, 1067-74.Konde-Lule J, Gitta S, Okuonzi, S and Matsiko C (2007) Accessto health care in rural Uganda, iHEA 2007 6 th World Congress:Explorations in Health Economics Paper.Ladu IM (2010) Health Service Commission wants doctors’salaries raised, The Monitor, 1 May.Mandelli A, Kyomuhangi LB and Scribner S (2005) Survey <strong>of</strong>Private Health Facilities in Uganda. Be<strong>the</strong>sda, MD: The Partnersfor Health Reformplus Project, Abt Associates Inc.Matsiko C (2010) Positive Practice Environments in Uganda:Enhancing health worker and health system performance,International Council <strong>of</strong> Nurses, International PharmaceuticalFederation, World Dental Federation, World MedicalAssociation, International Hospital Federation and WorldConfederation for Physical Therapy.McPake B, Asiimwe D, Mwesigye F, Ofumbi M, Ortenblad L,Streefland P and Turinde A (1999) Informal economic activities<strong>of</strong> health workers in Uganda: implications for quality andaccessibility <strong>of</strong> care, Social Science and Medicine 49, 7, 849-865.McPake B, Asiimwe D, Mwesigye F, Ofumbi M, Streefland P andTurinde A (2000) Coping strategies <strong>of</strong> health workers in Uganda,131-155 in P Ferrinho and W Van Lerberghe (eds) ProvidingHealth Care under Adverse Conditions: Health PersonnelPerformance and Individual Coping Strategies, Studies in HealthServices Organisation and Policy 16, Antwerp: ITG Press.Medicines and Health Service Delivery Monitoring Unit (2010)Annual Report 2010, Kampala: Medicines and Health ServiceDelivery Monitoring Unit.Ministry <strong>of</strong> Finance, Planning and Economic Development(2010) Millennium Development Goals Report for Uganda2010. Special <strong>the</strong>me: Accelerating progress towards improvingmaternal health, Kampala: Ministry <strong>of</strong> Finance, Planning andEconomic Development.Ministry <strong>of</strong> Health (2004) Health Sector Strategic Plan II2005/06 – 2009/2010 Volume II, Kampala: Ministry <strong>of</strong> Health.Ministry <strong>of</strong> Health (2006) Human Resources for Health Policy,Kampala: Ministry <strong>of</strong> Health.Ministry <strong>of</strong> Health (2008a) Pharmaceutical Situation Assessment– Level II, Health Facilities Survey in Uganda: Report <strong>of</strong> a surveyconducted July-August 2008, Kampala: Ministry <strong>of</strong> Health.Ministry <strong>of</strong> Health (2008b) Access to and Use <strong>of</strong> Medicines byHouseholds in Uganda: Report <strong>of</strong> a survey conducted 2008,Kampala: Ministry <strong>of</strong> Health.Ministry <strong>of</strong> Health (2009a) Uganda Health Workforce:Satisfaction and Intent to Stay among Current Health Workers,Chapel Hill, NC: The Capacity Project.Ministry <strong>of</strong> Health (2009b) Heath Sector Strategic Plan III:2010/11-2014/15 (draft)Ministry <strong>of</strong> Health (2009c) National Health Policy: Reducing povertythrough promoting people’s health, May 2009 Version, draft.Ministry <strong>of</strong> Health (2010a) The Second National HealthPolicy: Promoting People’s Health to Enhance Socio-economicDevelopment, Kampala: Uganda.63
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersMinistry <strong>of</strong> Health (2010b) Health Sector Strategic & InvestmentPlan: Promoting People’s Health to Enhance Socio-economicDevelopment 2010/11 – 2014/15, Kampala: Ministry <strong>of</strong> Health.Muhinda A, Mutumba A and Mugarura J (2008) Communityempowerment and participation in maternal health in Kamwengedistrict, Uganda, EQUINET PRA paper, Harare: EQUINET.Nabudere H, Asiimwe D and Mijumbi R (2010) Task shifting tooptimise <strong>the</strong> roles <strong>of</strong> health workers to improve <strong>the</strong> delivery <strong>of</strong>maternal and child healthcare, Kampala: REACH, Uganda TaskShifting Working Group.Nabyonga-Orem J, Karamagi H, Atuyambe L, Bagenda F,Okuonzi SA and Walker O (2008) Maintaining quality <strong>of</strong> healthservices after abolition <strong>of</strong> user fees: A Uganda case study, BMCHealth Services Research, 8,102.Nguyen L, Ropers S, Nderitu E, Zuyderduin A, Luboga S andHagopian A (2008) Intent to migrate among nursing students inUganda: measures <strong>of</strong> <strong>the</strong> brain drain in <strong>the</strong> next generation <strong>of</strong>health pr<strong>of</strong>essionals, Human Resources for Health, 6, 5.Oketcho V, Namaganda G and Matsiko C (2009) HumanResources for Health Planning In Uganda: Practice and Lessons,Uganda Capacity Program, IntraHealth International, Uganda.O’Neil ML and Paydos M (2008) Improving retention andperformance in civil society in Uganda, Human Resourcesfor Health, 6, 11.Onzubo P (2007) Turnover <strong>of</strong> health pr<strong>of</strong>essionals in <strong>the</strong>general hospitals in West Nile Region, Health Policy andDevelopment, 5, 1, 28-34.Open Society Initiative for East Africa (2010) Health rights arehuman rights: empowering local communities to demand qualityhealth services, Amplifying Voices: The Uganda Issue, 20-21.Republic <strong>of</strong> Uganda (2010) Annual Health Sector PerformanceReport Financial Year 2009/2010, Kampala: Ministry <strong>of</strong> Health.Ritchie J and Lewis J (2003) (eds) Qualitative Research Practice,London: Sage.Rutebemberawa E, Ekirapa-Kiracho E, Okui O, Walker D,Mutebi A and Pariyo G (2009) Lack <strong>of</strong> effective communicationbetween communities and hospitals in Uganda: a qualitativeexploration <strong>of</strong> missing links, BMC Health Services Research, 9, 146.Schmid B, Thomas E, Olivier J and Cochrane JR (2008) TheContribution <strong>of</strong> Religious Entities to Health in Sub-Saharan Africa.Study funded by <strong>the</strong> Bill & Melinda Gates Foundation. Unpublishedreport, ARHAP (Africa Religions for Health Assets Program).Schwalbach J, Abdula M, Adam Y and Khan Z (2000) GoodSamaritan or exploiter <strong>of</strong> illness? Coping strategies <strong>of</strong>Mozambican health care providers, 117-130 in P Ferrinhoand W Van Lerberghe (eds) Providing Health Care underAdverse Conditions: Health Personnel Performance andIndividual Coping Strategies, Studies in Health ServicesOrganisation and Policy 16, Antwerp: ITG Press.Senkabirwa A-M (2010) Over 800 nurses trek to work abroad,Daily Monitor, 29 September.Spero J and McQuide P (2011) Data show high level <strong>of</strong> attritionin Uganda. Prepared as a background document for The State<strong>of</strong> <strong>the</strong> World’s Midwifery 2011 http://www.unfpa.org/sowmy/resources/docs/background_papers/60_SperoMcQuide_UgandaAttrition.PDFSpero J, McQuide P and Matte R (2011) Tracking and monitoring<strong>the</strong> health workforce: a new human resources informationsystem (HRIS) in Uganda, Human Resources for Health, 9, 6.Stringhini S, Thomas S, Bidwell P, Mtui T and Mwisongo A (2009)Understanding informal payments in health care: motivation <strong>of</strong>health workers in Tanzania, Human Resources for Health, 7, 53.TARSC and HEPS (2011) Streng<strong>the</strong>ning Health Worker-CommunityInteractions through Health Literacy and Participatory Approaches,Uganda training workshop report, Harare: EQUINET.Uganda Bureau <strong>of</strong> Statistics (2002) Uganda Population and HousingCensus. Main Report, Kampala: Uganda Bureau <strong>of</strong> Statistics.Uganda Bureau <strong>of</strong> Statistics (2006) Uganda National HouseholdSurvey 2005/2006: Report on <strong>the</strong> Socio-economic Module,Kampala: Uganda Bureau <strong>of</strong> Statistics.Uganda Bureau <strong>of</strong> Statistics (2008) Report <strong>of</strong> <strong>the</strong> National ServiceDelivery Survey 2008, Kampala: Uganda Bureau <strong>of</strong> Statistics.Uganda Country Working Group (2010) Medicine Price MonitorUganda No 9 Apr-June 2010, Kampala: Uganda CountryWorking Group.Uganda Ministry <strong>of</strong> Health and The Capacity Project (2008)Mapping <strong>the</strong> Human Resources Management Processes inUganda, Chapel Hill, NC: The Capacity Project.Uganda National Health Users’/Consumers’ Organisation (2010)Establishing Incidence <strong>of</strong> Health Provider Absenteeism inBushenyi District, UNHCO: Kampala.UNFPA Uganda Country Office (2009) The State <strong>of</strong> MidwiferyTraining, Service and Practice in Uganda, Assessment Report,Kampala: UNFPA Uganda Country Office.64
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersUNFPA (2010) Evaluation <strong>of</strong> <strong>the</strong> Registered and EnrolledComprehensive Nurse Training Programs in Uganda: Terms<strong>of</strong> Reference, August, UNFPA.UNFPA (2011) The State <strong>of</strong> <strong>the</strong> World’s Midwifery 2011, UNFPA.United Nations Human Development Programme (2010)The Real Wealth <strong>of</strong> Nations: Pathways to Human Development,Human Development Report 2010, Basingstoke/New York:Palgrave Macmillan.Van Lerberghe W, Luck M, De Brouwere V, Kegels G and Ferrinho P(2000) Performance, working conditions and coping strategies:an introduction, 1-5 in P Ferrinho and W Van Lerberghe (eds)Providing Health Care under Adverse Conditions: Health PersonnelPerformance and Individual Coping Strategies, Studies in HealthServices Organisation and Policy 16, Antwerp: ITG Press.<strong>VSO</strong> (2011) Ugandan Health Workers Speak: The Rewards and<strong>the</strong> Realities, London: <strong>VSO</strong>.Womakuyu F (2010) Ambulance shortage in rural areas costingUgandan lives – report, New Vision, 16 December.World Bank (2010) Silent and Lethal: How quiet corruptionundermines Africa’s development efforts, An essay drawn from<strong>the</strong> Africa Development Indicators, World Bank.World Health Organisation (n.d) Global Atlas <strong>of</strong> <strong>the</strong> HealthWorkforce, Geneva: World Health Organisation www.who.int/globalatlas/autologin/hrh_login.asp.World Health Organisation (2006) The World Health Report 2006:Working Toge<strong>the</strong>r for Health, Geneva: World Health Organisation.World Health Organisation (2010) Achieving <strong>the</strong> health-relatedMDGs: It takes a workforce! http://www.who.int/hrh/workforce_mdgs/en/index.htmlZuyderduin A, Obuni JD and Mcquide PA (2010) Streng<strong>the</strong>ning<strong>the</strong> Uganda nurses’ and midwives’ association for a motivatedworkforce, International Nursing Review 57, 4, 419-425.65
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workersAnnex: Health worker topic guide1. Tell me why you decided to become a [----]Probe • Influences• Attraction <strong>of</strong> <strong>the</strong> pr<strong>of</strong>ession• Ambitions• Alternatives considered• Doubts2. What do you believe <strong>the</strong> [----] role is supposed to be?Prompt: Why do you think that?Probe • Influence <strong>of</strong> training, text books• Role models• Peers3. What words would you use to describe a good [----]?4. How does what you do in your work fit with your ideas <strong>of</strong> what <strong>the</strong> [----] role should be?Probe • Fit with work <strong>of</strong> nurses / doctors / clinical <strong>of</strong>ficers / nursing aides• Patients’ care needs• Constraints – staffing, equipment, drugs, work environment• O<strong>the</strong>r people’s attitudes5. What is good about being a [----] (in Uganda)?Probe • Material aspects – pay, housing, transport, etc• Uniform• Training, career prospects• Caring• O<strong>the</strong>r people’s opinion <strong>of</strong> you6. What helps make [----] feel good about <strong>the</strong>mselves?Probe • Praise• Gratitude• Respect• Achievement• Recognition• Status7. What is not so good about being a [----]? What are <strong>the</strong> challenges and difficulties?Probe • Pay• Hours <strong>of</strong> work, multiple jobs• Transport• Accommodation, facilities for self and family• Training, career prospects• Constraints – staffing, equipment, drugs, work environment• Pressure <strong>of</strong> work• Harassment, threats• Lack <strong>of</strong> respect – from colleagues, patients, public66
<strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: The lived experience and opinions <strong>of</strong> Ugandan health workers8. How does [specified difficulty] make [----] feel about <strong>the</strong>ir work? About <strong>the</strong>mselves?What words come up when <strong>the</strong>y talk about how <strong>the</strong>y feel? What do <strong>the</strong>y mean?Probe • Not respected• Not valued• Pressured / stressed• Demoralised / demotivated• Blamed9. We are interested in how health workers get by – how <strong>the</strong>y survive – in difficult conditions.Prompt • Managing to get enough money to survive on• Coping with family responsibilities• Dealing with frustrations• Coping with bad feelings10. What do you say to stories that criticise health workers?Prompt • Not turning up for work• Leaving <strong>the</strong> workplace to do o<strong>the</strong>r things• Taking away drugs or equipment• Taking money from patients• Talking harshly to patients11. If you had your time over again, would you still decide to become a [----]?Prompt • Are reasons for becoming a [----] still valid• Ever considered working as a [----] outside Uganda• Would consider working as a [----] outside Uganda in future12. What would you like to change about working as a [----]? And how might <strong>the</strong> change come about?Prompt • Things that realistically might be achieved13. What if anything might be done so that health workers have more <strong>of</strong> a say and are listened to?Prompt • Council• Association• Union• O<strong>the</strong>r advocacy organisations14. Is <strong>the</strong>re anything else that you would like to share with us about being a health worker?67
ISBN 978-1-903697-33-79 781903 697337Valuing Health Workers is <strong>VSO</strong>’s research and advocacyinitiative, which supports <strong>the</strong> achievement <strong>of</strong> <strong>the</strong>health-related Millennium Development Goals.Valuing Health Workers research is currently underwayin four countries. Following on from <strong>the</strong> research,advocacy strategies will be created, which will include<strong>the</strong> development <strong>of</strong> volunteer placements in civil societycoalitions, pr<strong>of</strong>essional associations and health ministries.<strong>VSO</strong> works with <strong>the</strong> Health Workforce Advocacy Initiative(HWAI). HWAI is <strong>the</strong> civil-society led network <strong>of</strong> <strong>the</strong>Global Health Workforce Alliance (GHWA) and engagesin evidence-based advocacy with <strong>the</strong> goal <strong>of</strong> enablingeveryone to access skilled, motivated and supported healthworkers who are part <strong>of</strong> well-functioning health systems.www.healthworkforce.info/HWAI/Welcome.html<strong>VSO</strong> works with Action for Global Health – a cross-Europeannetwork <strong>of</strong> health development organisations. The networkcalls on European Governments and <strong>the</strong> EuropeanCommission to act now to support developing countries toachieve <strong>the</strong> health-related Millennium Development Goals.www.actionforglobalhealth.euFor more information please contact:advocacy@vso.org.ukIf you would like to volunteer with <strong>VSO</strong> please visit:vsointernational.org/volunteerIn addition to this publication, <strong>the</strong> following researchand publications may also be <strong>of</strong> interest:• Participatory Advocacy: a Toolkit for Staff, Volunteersand Partners – this manual is an easily accessible guideto lobbying and campaigning, and can be used by healthactivists and o<strong>the</strong>r campaigners for social justice.• Ugandan Health Workers Speak: The Rewards and<strong>the</strong> Realities – a report <strong>of</strong> initial findings <strong>of</strong> <strong>the</strong>Valuing Health Workers research in Uganda.• Valuing Health Workers in Cambodia – a short briefingon <strong>the</strong> research approach in Cambodia.• Valuing Health Workers: Implementing SustainableInterventions to Improve Health Worker Motivation (Malawi)– a report drawing toge<strong>the</strong>r existing research in Malawi,and identifying recommendations to tackle <strong>the</strong> HRH crises.• Local Volunteering Responses to Health Care: Challengesand Lessons from Malawi, Mongolia and <strong>the</strong> Philippines– this report looks at how community volunteers can beinvolved in delivering health services.• Brain Gain: Making Health Worker Migration Work for Richand Poor Countries. <strong>VSO</strong> Briefing: <strong>the</strong> perspective from Africa.• The IMF, <strong>the</strong> Global Crisis and Human Resources for Health– this 2010 report, written with <strong>the</strong> Stop Aids Campaign andAction for Global Health, shows how <strong>the</strong> IMF is constraining<strong>the</strong> fiscal space for developing countries and impeding <strong>the</strong>recruitment <strong>of</strong> much-needed new health workers.• <strong>Our</strong> <strong>Side</strong> <strong>of</strong> <strong>the</strong> <strong>Story</strong>: Ugandan health workers speak up – areport on <strong>the</strong> rewards, challenges and recommendations for<strong>the</strong> future, from <strong>the</strong> perspective <strong>of</strong> Ugandan health workers.To access any <strong>of</strong> <strong>the</strong>se publications, please visit:www.vsointernational.org/healthCarlton House, 27a Carlton DrivePutney, London, SW15 2BS, UK+44 (0) 20 8780 7500www.vsointernational.org<strong>VSO</strong> is a registered charity inEngland and in Wales (313757)and in Scotland (SC039117).Published July 2012<strong>VSO</strong> Bahaginanwww.vsobahaginan.org.ph<strong>VSO</strong> Irelandwww.vso.ie<strong>VSO</strong> Jitoleewww.vsojitolee.org<strong>VSO</strong> Ne<strong>the</strong>rlandswww.vso.nl<strong>VSO</strong> UKwww.vso.org.uk