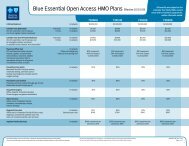
Key Benefits In-Network Out-of-Network Covered Services In ...
Key Benefits In-Network Out-of-Network Covered Services In ...
Key Benefits In-Network Out-of-Network Covered Services In ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
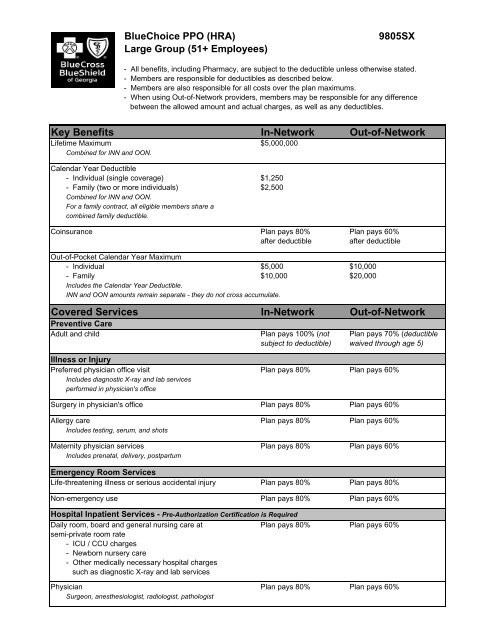
BlueChoice PPO (HRA)Large Group (51+ Employees)9805SX- All benefits, including Pharmacy, are subject to the deductible unless otherwise stated.- Members are responsible for deductibles as described below.- Members are also responsible for all costs over the plan maximums.- When using <strong>Out</strong>-<strong>of</strong>-<strong>Network</strong> providers, members may be responsible for any differencebetween the allowed amount and actual charges, as well as any deductibles.<strong>Key</strong> <strong>Benefits</strong> <strong>In</strong>-<strong>Network</strong> <strong>Out</strong>-<strong>of</strong>-<strong>Network</strong>Lifetime Maximum $5,000,000Combined for INN and OON.Calendar Year Deductible- <strong>In</strong>dividual (single coverage) $1,250- Family (two or more individuals) $2,500Combined for INN and OON.For a family contract, all eligible members share acombined family deductible.Coinsurance Plan pays 80% Plan pays 60%after deductibleafter deductible<strong>Out</strong>-<strong>of</strong>-Pocket Calendar Year Maximum- <strong>In</strong>dividual $5,000 $10,000- Family $10,000 $20,000<strong>In</strong>cludes the Calendar Year Deductible.INN and OON amounts remain separate - they do not cross accumulate.<strong>Covered</strong> <strong>Services</strong> <strong>In</strong>-<strong>Network</strong> <strong>Out</strong>-<strong>of</strong>-<strong>Network</strong>Preventive CareAdult and child Plan pays 100% (not Plan pays 70% (deductiblesubject to deductible) waived through age 5)Illness or <strong>In</strong>juryPreferred physician <strong>of</strong>fice visit Plan pays 80% Plan pays 60%<strong>In</strong>cludes diagnostic X-ray and lab servicesperformed in physician's <strong>of</strong>ficeSurgery in physician's <strong>of</strong>fice Plan pays 80% Plan pays 60%Allergy care Plan pays 80% Plan pays 60%<strong>In</strong>cludes testing, serum, and shotsMaternity physician services Plan pays 80% Plan pays 60%<strong>In</strong>cludes prenatal, delivery, postpartumEmergency Room <strong>Services</strong>Life-threatening illness or serious accidental injury Plan pays 80% Plan pays 80%Non-emergency use Plan pays 80% Plan pays 60%Hospital <strong>In</strong>patient <strong>Services</strong> - Pre-Authorization Certification is RequiredDaily room, board and general nursing care at Plan pays 80% Plan pays 60%semi-private room rate- ICU / CCU charges- Newborn nursery care- Other medically necessary hospital chargessuch as diagnostic X-ray and lab servicesPhysician Plan pays 80% Plan pays 60%Surgeon, anesthesiologist, radiologist, pathologist
BlueChoice PPO (HRA)9805SX<strong>Covered</strong> <strong>Services</strong> <strong>In</strong>-<strong>Network</strong> <strong>Out</strong>-<strong>of</strong>-<strong>Network</strong><strong>Out</strong>patient <strong>Services</strong>Facility / hospital charges Plan pays 80% Plan pays 60%<strong>In</strong>cluding diagnostic X-ray and lab servicesPhysician Plan pays 80% Plan pays 60%Surgeon, anesthesiologist, radiologist, pathologistTherapy <strong>Services</strong>Physical, occupational, chiropractic care, athletic trainers Plan pays 80% Plan pays 60%Visits per calendar year, combined specialties20 visitsVisits combined for INN and OONRespiratory therapy Plan pays 80% Plan pays 60%Visits per calendar year30 visitsVisits combined for INN and OONSpeech therapy Plan pays 80% Plan pays 60%Visits per calendar year20 visitsVisits combined for INN and OONRadiation therapy and chemotherapy Plan pays 80% Plan pays 60%Mental Health / Substance Abuse<strong>In</strong>patient Plan pays 80% Plan pays 60%<strong>Out</strong>patient Plan pays 80% Plan pays 60%Other <strong>Services</strong>Ambulance Plan pays 80% Plan pays 60%When medically necessaryHome health care Plan pays 80% Plan pays 60%Visits per calendar year120 visitsVisits combined for INN and OONHospice care Plan pays 100% Plan pays 100%$10,000 lifetime maximumSkilled nursing facility Plan pays 80% Plan pays 60%Days per calendar year30 daysDays combined for INN and OONPharmacyPrescription Drugs Plan pays 80% Plan pays 80%Unless otherwise indicated in the Certificate Booklet, each prescription has a 30-day supply limit.Members must file a claim for reimbursement when using an <strong>Out</strong>-<strong>of</strong>-<strong>Network</strong> pharmacy.For a full disclosure <strong>of</strong> all benefits, exclusions and limitations, refer to the Certificate Booklet.
Pre-Existing Condition Limitation and Credit for Prior CoverageUntil a member has had “creditable coverage” for 12 consecutive months, benefits for serviceshall not be available for any illness, injury or condition for which medical advice ortreatment was recommended by, or received from, a health care provider within sixmonths preceding the effective date <strong>of</strong> coverage (except maternity services, for whichthe pre-existing condition limitation is not applicable).Summary <strong>of</strong> Limitations and ExclusionsYour Certificate Booklet will provide you with complete benefit coverage information.Some key limitations and exclusions, however, are listed below:- Care or treatment that is not medically necessary- Cosmetic surgery, except to restore function altered by disease or trauma- Dental care and oral surgery; except for accidental injury to natural teethand limited treatment <strong>of</strong> TMJ.- Occupational related illness or injury- Routine physical examinations necessitated by employment, foreign travelor participation in school athletic programs- Smoking cessation products- Surgical or medical care for: artificial insemination, in-vitro fertilization,reversal <strong>of</strong> voluntary sterilization, radial keratotomy, learning disabilities,mental retardation, hyperkinetic syndrome or autistic disease <strong>of</strong> childhood- Treatment, drugs or supplies considered experimental or investigationalBlueCard ProgramBlueCard is a network partnership with all Blue Cross Blue Shield plans across thecountry. Through this cooperative arrangement, you receive participating providerdiscounts and more efficient processing <strong>of</strong> medical claims. This partnership also createsthe largest provider network in the U.S.See Certificate Booklet for Complete DetailsIt is important to keep in mind that this material is a brief outline<strong>of</strong> benefits and covered services and is not a contract. Please refer to yourCertificate Booklet Form # F-1681.801 (the contract) for a complete explanation<strong>of</strong> covered services, limitations and exclusions.For more information regarding our products and locating a provider, visit our Web Sitewww.bcbsga.com.
3350 Peachtree Road, NE Atlanta, Georgia 30326 1-800-441-2273<strong>In</strong>dependent Licensee <strong>of</strong> the Blue Cross Blue Shield Association® Registered Mark <strong>of</strong> the Blue Cross Blue Shield AssociationBEN0106 - eff 10/15/09 (MHPA updates)