Prucalopride - Regional Drug & Therapeutics Centre
Prucalopride - Regional Drug & Therapeutics Centre
Prucalopride - Regional Drug & Therapeutics Centre
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
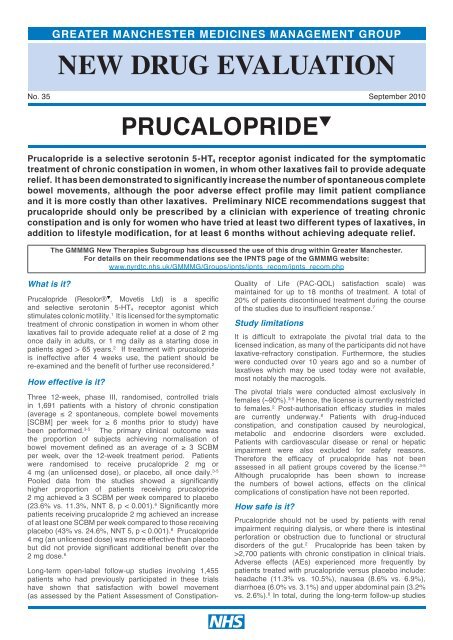
GREATER MANCHESTER MEDICINES MANAGEMENT GROUPNEW DRUG EVALUATIONNo. 35September 2010What is it?PRUCALOPRIDE q<strong>Prucalopride</strong> is a selective serotonin 5-HT 4 receptor agonist indicated for the symptomatictreatment of chronic constipation in women, in whom other laxatives fail to provide adequaterelief. It has been demonstrated to significantly increase the number of spontaneous completebowel movements, although the poor adverse effect profile may limit patient complianceand it is more costly than other laxatives. Preliminary NICE recommendations suggest thatprucalopride should only be prescribed by a clinician with experience of treating chronicconstipation and is only for women who have tried at least two different types of laxatives, inaddition to lifestyle modification, for at least 6 months without achieving adequate relief.The GMMMG New Therapies Subgroup has discussed the use of this drug within Greater Manchester.For details on their recommendations see the IPNTS page of the GMMMG website:www.nyrdtc.nhs.uk/GMMMG/Groups/ipnts/ipnts_recom/ipnts_recom.php<strong>Prucalopride</strong> (Resolor® q , Movetis Ltd) is a specificand selective serotonin 5-HT 4 receptor agonist whichstimulates colonic motility. 1 It is licensed for the symptomatictreatment of chronic constipation in women in whom otherlaxatives fail to provide adequate relief at a dose of 2 mgonce daily in adults, or 1 mg daily as a starting dose inpatients aged > 65 years. 2 If treatment with prucaloprideis ineffective after 4 weeks use, the patient should bere-examined and the benefit of further use reconsidered. 2How effective is it?Three 12-week, phase III, randomised, controlled trialsin 1,691 patients with a history of chronic constipation(average ≤ 2 spontaneous, complete bowel movements[SCBM] per week for ≥ 6 months prior to study) havebeen performed. 3-5 The primary clinical outcome wasthe proportion of subjects achieving normalisation ofbowel movement defined as an average of ≥ 3 SCBMper week, over the 12-week treatment period. Patientswere randomised to receive prucalopride 2 mg or4 mg (an unlicensed dose), or placebo, all once daily. 3-5Pooled data from the studies showed a significantlyhigher proportion of patients receiving prucalopride2 mg achieved ≥ 3 SCBM per week compared to placebo(23.6% vs. 11.3%, NNT 8, p < 0.001). 6 Significantly morepatients receiving prucalopride 2 mg achieved an increaseof at least one SCBM per week compared to those receivingplacebo (43% vs. 24.6%, NNT 5, p < 0.001). 6 <strong>Prucalopride</strong>4 mg (an unlicensed dose) was more effective than placebobut did not provide significant additional benefit over the2 mg dose. 6Long-term open-label follow-up studies involving 1,455patients who had previously participated in these trialshave shown that satisfaction with bowel movement(as assessed by the Patient Assessment of Constipation-nQuality of Life (PAC-QOL) satisfaction scale) wasmaintained for up to 18 months of treatment. A total of20% of patients discontinued treatment during the courseof the studies due to insufficient response. 7Study limitationsIt is difficult to extrapolate the pivotal trial data to thelicensed indication, as many of the participants did not havelaxative-refractory constipation. Furthermore, the studieswere conducted over 10 years ago and so a number oflaxatives which may be used today were not available,most notably the macrogols.The pivotal trials were conducted almost exclusively infemales (~90%). 3-5 Hence, the license is currently restrictedto females. 2 Post-authorisation efficacy studies in malesare currently underway. 8 Patients with drug-inducedconstipation, and constipation caused by neurological,metabolic and endocrine disorders were excluded.Patients with cardiovascular disease or renal or hepaticimpairment were also excluded for safety reasons.Therefore the efficacy of prucalopride has not beenassessed in all patient groups covered by the license. 3-5Although prucalopride has been shown to increasethe numbers of bowel actions, effects on the clinicalcomplications of constipation have not been reported.How safe is it?<strong>Prucalopride</strong> should not be used by patients with renalimpairment requiring dialysis, or where there is intestinalperforation or obstruction due to functional or structuraldisorders of the gut. 2 <strong>Prucalopride</strong> has been taken by>2,700 patients with chronic constipation in clinical trials.Adverse effects (AEs) experienced more frequently bypatients treated with prucalopride versus placebo include:headache (11.3% vs. 10.5%), nausea (8.6% vs. 6.9%),diarrhoea (6.0% vs. 3.1%) and upper abdominal pain (3.2%vs. 2.6%). 6 In total, during the long-term follow-up studies
the most frequent AEs which resulted in studydiscontinuation were abdominal pain (1.2%), diarrhoea(1.2%), headache (1.0%) and nausea (0.9%). 7All suspected adverse reactions to black triangle drugssuch as prucalopride should be reported to the MHRA viathe Yellow Card Scheme (www.yellowcard.gov.uk).What other options are there?The frequency of bowel actions varies in the healthypopulation and many people with infrequent bowel actionsdo not require medical intervention. UK guidelines currentlyrecommend the use of diet and lifestyle modificationsas a first line option in treating constipation, followed bythe introduction of various kinds of laxatives (bulk forming,stool softeners, osmotic or stimulating). 9-11 In severe casestreatment options include enemas, or surgical interventionssuch as sacral nerve stimulation.Economic ImpactA budgetary impact model supplied by Movetis estimatesthat approximately 296 per 100,000 women in the UKfail to achieve adequate relief with laxatives and aretherefore eligible for prucalopride treatment. Of these,approximately 88 per 100,000 would achieve normalisationof bowel frequency with symptomatic relief when treatedwith prucalopride, with a further 118 per 100,000 achievingan increase of ≥ 1 SCBM per week. Approximately 89per 100,000 are not expected to respond to prucalopride.Assuming 80% compliance this equates to an estimatedtotal cost including non-responders of >£113,000 per100,000 population. 8,12When should it be used?Preliminary NICE guidance suggests that prucaloprideshould only be considered in women who have beenmanaged by a clinician with experience of treating chronicconstipation. The women should have tried at least twodifferent types of laxative, and lifestyle modification, forat least six months, but have not had adequate relief. 9<strong>Prucalopride</strong> is not indicated for use in men or those agedless than 18 years. Final guidance on the use of prucalopridefor chronic constipation in women is expected to publishedin December 2010.How much does it cost?Cost of 28 days treatment (prices from eMIMs/<strong>Drug</strong> Tariff October 2010)<strong>Prucalopride</strong> 2mg daily£59.52<strong>Prucalopride</strong> 1mg daily£38.69Movicol sachets 3 daily£18.69Dicusate sodium 100mg capsules 5 dailyLactulose solution 15ml twice dailySenna 7.5mg tablets 2 twice dailyIspaghula husk 3.5g 6 sachets dailyBisacodyl 10mg od£8.96£5.39£4.80£3.43£1.83£0.00 £10.00 £20.00 £30.00 £40.00 £50.00 £60.00 £70.00N.B. Doses shown are for general comparison only and do not imply therapeutic equivalence. Average daily quantity (ADQ) values are used where available.The costs shown relate to the highest licensed dose for each drug, as it is assumed that this is the dose the patients will be receiving before treatment with prucaloprideis considered.references1. Frampton JE. <strong>Prucalopride</strong>. <strong>Drug</strong>s 2009;69:2463-76. ( R)2. Summary of Product Characteristics: Resolor 1 mg & 2 mg film-coatedtablets: Movetis Ltd. www.medicines.org.uk. Last updated 01/09/2010.3. Camilleri M et al. A placebo-controlled trial of prucalopride for severechronic constipation. N Engl J Med 2008;358:2344-54. (RCT)4. Quigley EM et al. Clinical trial: the efficacy, impact on quality of life, andsafety and tolerability of prucalopride in severe chronic constipation--a12-week, randomized, double-blind, placebo-controlled study. AlimentPharmacol Ther 2009;29:315-28. (RCT)5. Tack J et al. <strong>Prucalopride</strong> (Resolor) in the treatment of severe chronicconstipation in patients dissatisfied with laxatives. Gut 2009;58:357-65.(RCT)6. European Medicines Agency: CHMP Assessment Report for Resolor.EMEA/664892/2009. Accessed online: www.ema.europa.eu 12/07/2010.7. Camilleri M et al. Clinical trial: the efficacy of open lebel prucalopridetretament in patients with chronic constipation - follow-up of patients fromthe pivotal studies. Alimentary Pharmacology and <strong>Therapeutics</strong> 2010. (O)8.Personal communication with Movetis Ltd. 08/08/2010.9. National Institute for Health and Clinical Excellence. Constipation (women)- prucalopride: Appraisal Consultation Document. August 2010. Accessedonline: www.nice.org.uk 04/08/2010. (G)10. British National Formulary 59. Section 1.6: Laxatives.11. 11. NHS Clinical Knowledge Summaries: Constipation Management inAdults. Accessed online: www.cks.nhs.uk 12/07/2010. (G)12. National Institute for Health and Clinical Excellence. Constipation (women)- prucalopride: manufacturer submission August 2010. Accessed online:www.nice.org.uk 04/08/2010.KEYRCT – randomised controlled trial, G – guideline, O – open label, R – reviewPrepared by the <strong>Regional</strong> <strong>Drug</strong> and <strong>Therapeutics</strong> <strong>Centre</strong>Wolfson Unit, Claremont Place, Newcastle upon Tyne NE2 4HHTel: 0191 260 6188 Fax: 0191 260 6191Email: nyrdtc.rxsupp@nuth.nhs.uk Website: www.nyrdtc.nhs.uk/GMMMGthis document is intended for use by nhs healthcare professionals and cannot be used for commercial or marketing purposes.patient information on many topics can be accessed via nhs direct.