(HMK) - DME Form - Blue Cross and Blue Shield of Montana
(HMK) - DME Form - Blue Cross and Blue Shield of Montana
(HMK) - DME Form - Blue Cross and Blue Shield of Montana
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
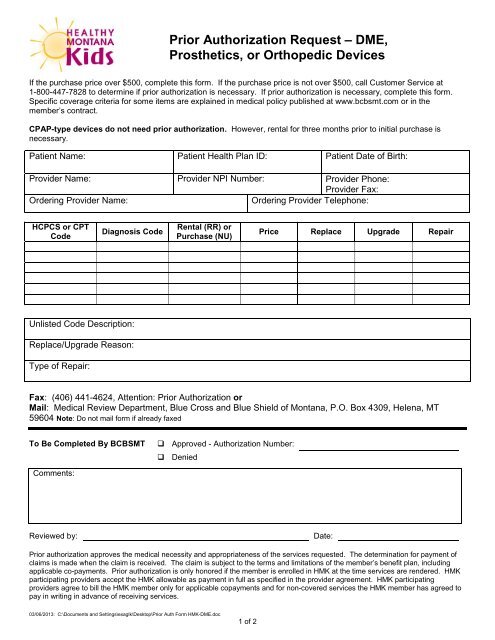
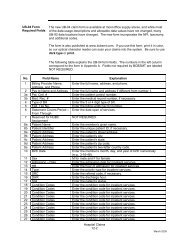
Prior Authorization Request – <strong>DME</strong>,Prosthetics, or Orthopedic DevicesIf the purchase price over $500, complete this form. If the purchase price is not over $500, call Customer Service at1-800-447-7828 to determine if prior authorization is necessary. If prior authorization is necessary, complete this form.Specific coverage criteria for some items are explained in medical policy published at www.bcbsmt.com or in themember’s contract.CPAP-type devices do not need prior authorization. However, rental for three months prior to initial purchase isnecessary.Patient Name: Patient Health Plan ID: Patient Date <strong>of</strong> Birth:Provider Name: Provider NPI Number: Provider Phone:Provider Fax:Ordering Provider Name:Ordering Provider Telephone:HCPCS or CPTCodeDiagnosis CodeRental (RR) orPurchase (NU)Price Replace Upgrade RepairUnlisted Code Description:Replace/Upgrade Reason:Type <strong>of</strong> Repair:Fax: (406) 441-4624, Attention: Prior Authorization orMail: Medical Review Department, <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Montana</strong>, P.O. Box 4309, Helena, MT59604 Note: Do not mail form if already faxedTo Be Completed By BCBSMT Approved - Authorization Number: DeniedComments:Reviewed by:Date:Prior authorization approves the medical necessity <strong>and</strong> appropriateness <strong>of</strong> the services requested. The determination for payment <strong>of</strong>claims is made when the claim is received. The claim is subject to the terms <strong>and</strong> limitations <strong>of</strong> the member’s benefit plan, includingapplicable co-payments. Prior authorization is only honored if the member is enrolled in <strong>HMK</strong> at the time services are rendered. <strong>HMK</strong>participating providers accept the <strong>HMK</strong> allowable as payment in full as specified in the provider agreement. <strong>HMK</strong> participatingproviders agree to bill the <strong>HMK</strong> member only for applicable copayments <strong>and</strong> for non-covered services the <strong>HMK</strong> member has agreed topay in writing in advance <strong>of</strong> receiving services.03/06/2013: C:\Documents <strong>and</strong> Settings\exaglk\Desktop\Prior Auth <strong>Form</strong> <strong>HMK</strong>-<strong>DME</strong>.doc1 <strong>of</strong> 2
Additional line itemsHCPCS or CPTCodeDiagnosis CodeRental (RR) orPurchase (NU)Price Replace Upgrade RepairUnlisted Code Description:Replace/Upgrade Reason:Type <strong>of</strong> Repair:Provider Participation NoticeHealthy <strong>Montana</strong> Kids (<strong>HMK</strong>) members are required to use <strong>HMK</strong> participating providers when seeking medical treatment<strong>and</strong> all providers involved with this procedure must be <strong>HMK</strong> participating providers. Call <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong><strong>Montana</strong> at 1-800-447-7828, Extension 6100, to enroll in the network prior to rendering services or to inquire aboutwhether the provider to whom you are referring an <strong>HMK</strong> member is an enrolled <strong>HMK</strong> participating provider.03/06/2013: C:\Documents <strong>and</strong> Settings\exaglk\Desktop\Prior Auth <strong>Form</strong> <strong>HMK</strong>-<strong>DME</strong>.doc2 <strong>of</strong> 2