factors leading to conversion in laparoscopic cholecystectomy
factors leading to conversion in laparoscopic cholecystectomy
factors leading to conversion in laparoscopic cholecystectomy
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
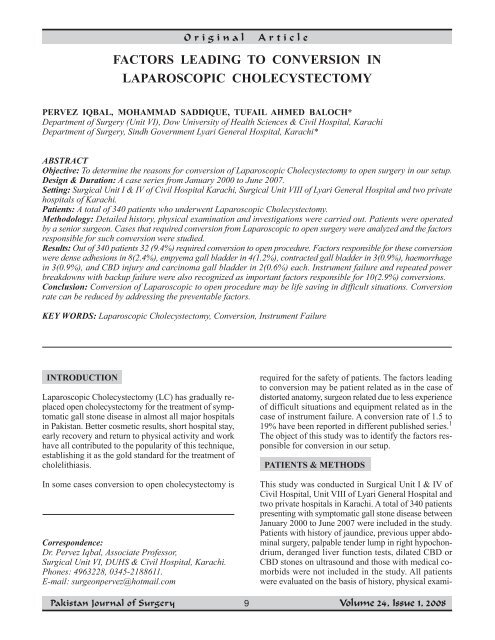
Orig<strong>in</strong>alArticleFACTORS LEADING TO CONVERSION INLAPAROSCOPIC CHOLECYSTECTOMYPERVEZ IQBAL, MOHAMMAD SADDIQUE, TUFAIL AHMED BALOCH*Department of Surgery (Unit VI), Dow University of Health Sciences & Civil Hospital, KarachiDepartment of Surgery, S<strong>in</strong>dh Government Lyari General Hospital, Karachi*ABSTRACTObjective: To determ<strong>in</strong>e the reasons for <strong>conversion</strong> of Laparoscopic Cholecystec<strong>to</strong>my <strong>to</strong> open surgery <strong>in</strong> our setup.Design & Duration: A case series from January 2000 <strong>to</strong> June 2007.Sett<strong>in</strong>g: Surgical Unit I & IV of Civil Hospital Karachi, Surgical Unit VIII of Lyari General Hospital and two privatehospitals of Karachi.Patients: A <strong>to</strong>tal of 340 patients who underwent Laparoscopic Cholecystec<strong>to</strong>my.Methodology: Detailed his<strong>to</strong>ry, physical exam<strong>in</strong>ation and <strong>in</strong>vestigations were carried out. Patients were operatedby a senior surgeon. Cases that required <strong>conversion</strong> from Laparoscopic <strong>to</strong> open surgery were analyzed and the <strong>fac<strong>to</strong>rs</strong>responsible for such <strong>conversion</strong> were studied.Results: Out of 340 patients 32 (9.4%) required <strong>conversion</strong> <strong>to</strong> open procedure. Fac<strong>to</strong>rs responsible for these <strong>conversion</strong>were dense adhesions <strong>in</strong> 8(2.4%), empyema gall bladder <strong>in</strong> 4(1.2%), contracted gall bladder <strong>in</strong> 3(0.9%), haemorrhage<strong>in</strong> 3(0.9%), and CBD <strong>in</strong>jury and carc<strong>in</strong>oma gall bladder <strong>in</strong> 2(0.6%) each. Instrument failure and repeated powerbreakdowns with backup failure were also recognized as important <strong>fac<strong>to</strong>rs</strong> responsible for 10(2.9%) <strong>conversion</strong>s.Conclusion: Conversion of Laparoscopic <strong>to</strong> open procedure may be life sav<strong>in</strong>g <strong>in</strong> difficult situations. Conversionrate can be reduced by address<strong>in</strong>g the preventable <strong>fac<strong>to</strong>rs</strong>.KEY WORDS: Laparoscopic Cholecystec<strong>to</strong>my, Conversion, Instrument FailureINTRODUCTIONLaparoscopic Cholecystec<strong>to</strong>my (LC) has gradually replacedopen cholecystec<strong>to</strong>my for the treatment of symp<strong>to</strong>maticgall s<strong>to</strong>ne disease <strong>in</strong> almost all major hospitals<strong>in</strong> Pakistan. Better cosmetic results, short hospital stay,early recovery and return <strong>to</strong> physical activity and workhave all contributed <strong>to</strong> the popularity of this technique,establish<strong>in</strong>g it as the gold standard for the treatment ofcholelithiasis.In some cases <strong>conversion</strong> <strong>to</strong> open cholecystec<strong>to</strong>my isCorrespondence:Dr. Pervez Iqbal, Associate Professor,Surgical Unit VI, DUHS & Civil Hospital, Karachi.Phones: 4963228, 0345-2188611.E-mail: surgeonpervez@hotmail.comrequired for the safety of patients. The <strong>fac<strong>to</strong>rs</strong> <strong>lead<strong>in</strong>g</strong><strong>to</strong> <strong>conversion</strong> may be patient related as <strong>in</strong> the case ofdis<strong>to</strong>rted ana<strong>to</strong>my, surgeon related due <strong>to</strong> less experienceof difficult situations and equipment related as <strong>in</strong> thecase of <strong>in</strong>strument failure. A <strong>conversion</strong> rate of 1.5 <strong>to</strong>19% have been reported <strong>in</strong> different published series. 1The object of this study was <strong>to</strong> identify the <strong>fac<strong>to</strong>rs</strong> responsiblefor <strong>conversion</strong> <strong>in</strong> our setup.PATIENTS & METHODSThis study was conducted <strong>in</strong> Surgical Unit I & IV ofCivil Hospital, Unit VIII of Lyari General Hospital andtwo private hospitals <strong>in</strong> Karachi. A <strong>to</strong>tal of 340 patientspresent<strong>in</strong>g with symp<strong>to</strong>matic gall s<strong>to</strong>ne disease betweenJanuary 2000 <strong>to</strong> June 2007 were <strong>in</strong>cluded <strong>in</strong> the study.Patients with his<strong>to</strong>ry of jaundice, previous upper abdom<strong>in</strong>alsurgery, palpable tender lump <strong>in</strong> right hypochondrium,deranged liver function tests, dilated CBD orCBD s<strong>to</strong>nes on ultrasound and those with medical comorbidswere not <strong>in</strong>cluded <strong>in</strong> the study. All patientswere evaluated on the basis of his<strong>to</strong>ry, physical exami-9Volume 24, Issue 1, 2008
Fac<strong>to</strong>rs <strong>lead<strong>in</strong>g</strong> <strong>to</strong> Conversion <strong>in</strong> Lap. Cholecystec<strong>to</strong>myP. Iqbal, M. Saddique, T. A. Balochnation, labora<strong>to</strong>ry <strong>in</strong>vestigations and ultrasound abdomen,and underwent classical <strong>laparoscopic</strong> cholecystec<strong>to</strong>my.Details of patients who underwent <strong>conversion</strong> <strong>to</strong>open operation were analyzed and the <strong>fac<strong>to</strong>rs</strong> responsiblenoted.RESULTSAmongst the 340 patients admitted for <strong>laparoscopic</strong>cholecystec<strong>to</strong>my 80(23.5%) were male and 260(76.5%)female, with an average age of 39 years (range 16 years<strong>to</strong> 62 years). Thirty two patients (9.41%) required <strong>conversion</strong><strong>to</strong> open procedure; <strong>in</strong> the rema<strong>in</strong><strong>in</strong>g cases the<strong>laparoscopic</strong> cholecystec<strong>to</strong>my was successfully completed.The reasons for <strong>conversion</strong> (Table I) <strong>in</strong>cluded denseadhesions <strong>in</strong> the region of gall bladder and Calot’s trianglemak<strong>in</strong>g dissection unsafe <strong>in</strong> 8(2.35%) cases,empyema gall bladder <strong>in</strong> 4(1.18%), failure <strong>to</strong> hold thecontracted thick-walled gall bladder <strong>in</strong> 3(0.88%) andhaemorrhage <strong>in</strong> 3(0.88%) patients. Two (0.59%) caseswith <strong>in</strong>jury <strong>to</strong> the CBD recognized dur<strong>in</strong>g surgery wereconverted <strong>to</strong> open procedure, as were 2(0.59%) patientswith <strong>in</strong>cidental f<strong>in</strong>d<strong>in</strong>g of carc<strong>in</strong>oma gall bladder. Instrumentfailure contributed <strong>to</strong> maximum number of <strong>conversion</strong>si.e. 10(2.94%). Instrument failure (Table II) <strong>in</strong>cludedfailure of light source <strong>in</strong> four cases, failure of thecamera <strong>in</strong> two and <strong>in</strong>suffla<strong>to</strong>r also <strong>in</strong> two cases. Repeateddisruption of power supply with backup failure wasalso responsible for two <strong>conversion</strong>s.DISCUSSIONWith grow<strong>in</strong>g experience of <strong>laparoscopic</strong> cholecystec<strong>to</strong>myand completion of the learn<strong>in</strong>g curve, the <strong>in</strong>dicationsfor LC have been extended, approach<strong>in</strong>g <strong>to</strong> tha<strong>to</strong>f open cholecystec<strong>to</strong>my depend<strong>in</strong>g upon the expertiseof the operat<strong>in</strong>g team. Complications of LC have beenm<strong>in</strong>imized <strong>to</strong> as low as 2-6%. 2 However, a substantialTable I. Reasons for Conversion (n=340)Reason for ConversionPresence of dense adhesionsEmpyema gall bladderContracted gall bladderHaemorrhageCBD InjuryCarc<strong>in</strong>oma gall bladderInstrument failureTotalNo.8433221032%2.351.180.880.880.590.592.949.41proportion of patients had <strong>to</strong> be converted from LC <strong>to</strong>open operation because of technical difficulty or <strong>in</strong>traoperativecomplications. 3-5 The <strong>conversion</strong> rate of LChas been reported <strong>in</strong> different studies as rang<strong>in</strong>g from2-15%. 6-8The importance of <strong>fac<strong>to</strong>rs</strong> predispos<strong>in</strong>g <strong>to</strong> <strong>conversion</strong>from <strong>laparoscopic</strong> <strong>to</strong> open cholecystec<strong>to</strong>my has beenemphasized <strong>in</strong> different studies 9-12 and studies havealso been conducted <strong>to</strong> address this important issue. 13The <strong>in</strong>cidence of <strong>conversion</strong> due <strong>to</strong> adhesions, empyemagall bladder and contracted gall bladder <strong>in</strong> our study issimilar <strong>to</strong> that of other <strong>in</strong>ternational studies. S<strong>in</strong>gh andOhri 14 <strong>in</strong> their study reported adhesions as the cause of<strong>conversion</strong> <strong>in</strong> 16.7% cases, empyema gall bladder <strong>in</strong>2.05% and contracted gall bladder <strong>in</strong> 1.4% cases.With more experience and technical advances, haemorrhageand CBD <strong>in</strong>juries are be<strong>in</strong>g <strong>in</strong>creas<strong>in</strong>gly managed<strong>laparoscopic</strong>ally. Similarly advances <strong>in</strong> diagnostic modalitieshave resulted <strong>in</strong> <strong>in</strong>creased preoperative diagnosisof carc<strong>in</strong>oma gall bladder. CBD s<strong>to</strong>nes can now alsobe managed by <strong>laparoscopic</strong> methods or ERCP.Conversion due <strong>to</strong> <strong>in</strong>strument failure has been reportedonly <strong>in</strong> earlier studies. 15 In our study it was an importantreason for <strong>conversion</strong> account<strong>in</strong>g for 10(2.9%) cases.Camera, <strong>in</strong>suffla<strong>to</strong>r and clip applica<strong>to</strong>r failure has beendocumented <strong>in</strong> a local study. 16 Search <strong>in</strong> local and <strong>in</strong>ternationalliterature revealed that <strong>conversion</strong> due <strong>to</strong> repeatedpower breakdown with backup failure has not beendocumented <strong>in</strong> any study. This new fac<strong>to</strong>r, endanger<strong>in</strong>gthe life of patients and threaten<strong>in</strong>g <strong>to</strong> damage the equipmenthas co<strong>in</strong>cided with power generation problemswhich the country is fac<strong>in</strong>g for the last one year.CONCLUSIONDur<strong>in</strong>g <strong>laparoscopic</strong> cholecystec<strong>to</strong>my operation <strong>conversion</strong><strong>to</strong> open surgery under difficult situation andconditions should not be delayed for the safety of patient.However certa<strong>in</strong> preventable <strong>fac<strong>to</strong>rs</strong> like <strong>in</strong>strumentfailure and power breakdown can be addressed by areliable backup.Table II. Instrument Failure (n=10)Cause of FailureLight sourceCameraInsuffla<strong>to</strong>rPower supplyNumber4222(%)1.180.590.590.5910Volume 24, Issue 1, 2008
Fac<strong>to</strong>rs <strong>lead<strong>in</strong>g</strong> <strong>to</strong> Conversion <strong>in</strong> Lap. Cholecystec<strong>to</strong>myP. Iqbal, M. Saddique, T. A. BalochREFERENCES1. Sikora SS, Kumar A, Saxena R, et al. LaparoscopicCholecystec<strong>to</strong>my - Can <strong>conversion</strong> be predicted?World J Surg 1995; 19: 858-60.2. Gadacz TR. Update on Laparoscopic Cholecystec<strong>to</strong>my,<strong>in</strong>clud<strong>in</strong>g a cl<strong>in</strong>ical pathway. Surg Cl<strong>in</strong> NorthAm 2000; 80: 1127-45.3. Krahenbuhl L, Sclabas G, Wente MN, et al. Incidence,risk <strong>fac<strong>to</strong>rs</strong> and prevention of biliary tract <strong>in</strong>juriesdur<strong>in</strong>g Laparoscopic Cholecystec<strong>to</strong>my <strong>in</strong> Switzerland.World J Surg 2001; 25: 1325-30.4. Merriam LT, Kanaan SA, Dawes LG, Angelos P,Prys<strong>to</strong>wsky JB, Rege RV, et al. Gangrenous cholecystitis:Analysis of risk <strong>fac<strong>to</strong>rs</strong> and experiencewith Laparoscopic Cholecystec<strong>to</strong>my. Surgery 1999;126: 680-6.5. Kumar A, Thombare MM, Sikora SS, Kapoor VK,Kaushik SP. Morbidity and mortality of LaparoscopicCholecystec<strong>to</strong>my <strong>in</strong> <strong>in</strong>stitutional setup. J LaparoendoscSurg 1996; 6: 393-7.6. Liv<strong>in</strong>gs<strong>to</strong>n EH, Rege RV. A nationwide study of<strong>conversion</strong> from Laparoscopic <strong>to</strong> Open Cholecystec<strong>to</strong>my.Am J Surg 2004; 188: 205-11.7. Kama NA, Kologlu M, Doganay M, Reis E, AtliM, Dolapei M. A risk score for <strong>conversion</strong> fromLaparoscopic <strong>to</strong> Open Cholecystec<strong>to</strong>my. Am J Surg2001; 181: 520-5.8. Rosen M, Brody F, Ponsky J. Predictive <strong>fac<strong>to</strong>rs</strong> forof <strong>conversion</strong> of Laparoscopic Cholecystec<strong>to</strong>my.Am J Surg 2002; 184: 254-8.9. Kologlu M, Tutuncu T, Yuksek YN, Gozalan U,Daglar G, Kama NA. Us<strong>in</strong>g a risk score for <strong>conversion</strong>from Laparoscopic <strong>to</strong> Open Cholecystec<strong>to</strong>my<strong>in</strong> resident tra<strong>in</strong><strong>in</strong>g. Surgery 2004;135:282-7.10. Hannan EL, Impera<strong>to</strong> PJ, Nenner RP, Starr H. Laparoscopicand Open Cholecystec<strong>to</strong>my <strong>in</strong> New YorkState: Mortality complications, and choice of procedure.Surgery 1999; 125: 223-31.11. Peters JH, Krailadsiri W, Incarbone R, BremnerCG, Froes E, Ireland AP, et al. Reasons for <strong>conversion</strong>from Laparoscopic <strong>to</strong> open <strong>in</strong> an urban teach<strong>in</strong>ghospital. Am J Surg 1994; 168: 555-9.12. Ross A, Gustafsson L, Krook H, Nordgren CE,Thorel A, Wall<strong>in</strong> G, et al. Laparoscopic Cholecystec<strong>to</strong>myversus M<strong>in</strong>i Laparo<strong>to</strong>my Cholecystec<strong>to</strong>my.Ann Surg 2001; 234: 741-9.13. Hammarstrom Lars-Erik. Prediction of unsuccessfulLaparoscopic Cholecystec<strong>to</strong>my. J Postgrad Med2005; 51: 21-2.14. S<strong>in</strong>gh Kuldip, Ohri Ashish. Laparoscopic Cholecystec<strong>to</strong>my- Is there a need <strong>to</strong> convert? J M<strong>in</strong> AccessSurg 2005; 1: 59-62.15. Ihasz M, Hung CM, Regoly-Merei J, Fazekas T,Ba<strong>to</strong>rfi J, Bal<strong>in</strong>t A, Zaborszky A, Posfai G. Complicationsof Laparoscopic Cholecystec<strong>to</strong>my <strong>in</strong> Hungary:A multicentre study of 13833 patients. Eur JSurg 1997; 163: 267-74.16. Jaffary SAA, Shamim MS, Raza SJ, Dastgir A.Instrument Failure: A Preventable cause of <strong>conversion</strong><strong>in</strong> Laparoscopic Cholecystec<strong>to</strong>my. Pak J Surg2007; 23: 92-5.11Volume 24, Issue 1, 2008