BENIGN PAROXYSMAL POSITIONAL VERTIGO - Mydoctor.ca
BENIGN PAROXYSMAL POSITIONAL VERTIGO - Mydoctor.ca
BENIGN PAROXYSMAL POSITIONAL VERTIGO - Mydoctor.ca
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
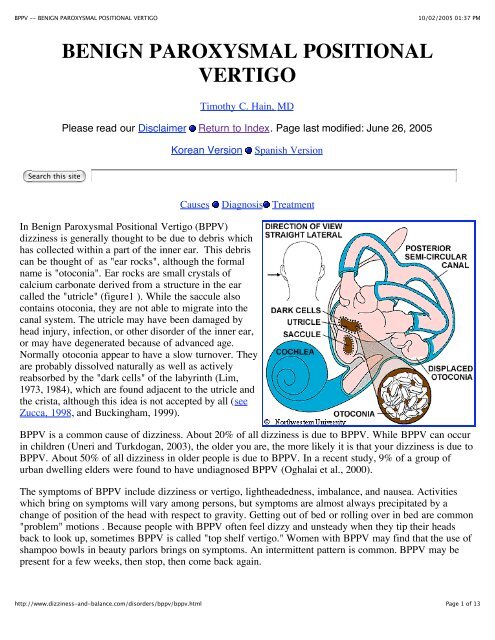
BPPV -- <strong>BENIGN</strong> <strong>PAROXYSMAL</strong> <strong>POSITIONAL</strong> <strong>VERTIGO</strong>10/02/2005 01:37 PMSupplemental material on the site CD: Animation of otoconia being displaced into posterior <strong>ca</strong>nalWHAT CAUSES BPPV?The most common <strong>ca</strong>use of BPPV in people under age 50 is head injury . There is also an association withmigraine (Ishiyama et al, 2000). In older people, the most common <strong>ca</strong>use is degeneration of the vestibularsystem of the inner ear. BPPV becomes much more common with advancing age (Froeling et al, 1991). Inhalf of all <strong>ca</strong>ses, BPPV is <strong>ca</strong>lled "idiopathic," which means it occurs for no known reason. Viruses affectingthe ear such as those <strong>ca</strong>using vestibular neuritis , minor strokes such as those involving anterior inferiorcerebellar artery (AICA) syndrome", and Meniere's disease are signifi<strong>ca</strong>nt but unusual <strong>ca</strong>uses. Oc<strong>ca</strong>sionallyBPPV follows surgery, where the <strong>ca</strong>use is felt to be a combination of a prolonged period of supinepositioning, or ear trauma when the surgery is to the inner ear (Ata<strong>ca</strong>n et al 2001). BPPV is also common inpersons who have been treated with ototoxic medi<strong>ca</strong>tions such as gentamicin (Black et al, 2004). Other<strong>ca</strong>uses of positional symptoms are discussed here.HOW IS THE DIAGNOSIS OF BPPV MADE?Your physician <strong>ca</strong>n make the diagnosis based on your history,findings on physi<strong>ca</strong>l examination, and the results of vestibular andauditory tests. Often, the diagnosis <strong>ca</strong>n be made with history andphysi<strong>ca</strong>l examination alone. The figure to the right illustrates theDix-Hallpike test. In this test, a person is brought from sitting to asupine position, with the head turned 45 degrees to one side andextended about 20 degrees backward. A positive Dix-Hallpike testsconsists of a burst of nystagmus (jumping of the eyes). The eyesjump upward as well as twist so that the top part of the eye jumpstoward the down side. Click here to see a movie of BPPVnystagmus. (13 meg download). The test <strong>ca</strong>n be made moresensitive by having the patient wear Frenzel goggles or a videogoggle. Most doctors that specialize in seeing dizzy patients havethese in their office.With respect to history, the key observation is that dizziness istriggered by lying down, or on rolling over in bed. Most otherconditions that have positional dizziness get worse on standingrather than lying down (e.g. orthostatic hypotension). There aresome rare conditions that have symptoms that resemble BPPV.Patients with certain types of central vertigo such as the spinocerebellar ataxias may have "bed spins" andprefer to sleep propped up in bed (Jen et al, 1998). These conditions <strong>ca</strong>n generally be detected on a <strong>ca</strong>refulneurologi<strong>ca</strong>l examination and also are generally accompanied by a family history of other persons withsimilar symptoms.Electronystagmography (ENG) testing may be needed to look for the characteristic nystagmus (jumping ofhttp://www.dizziness-and-balance.com/disorders/bppv/bppv.htmlPage 2 of 13
BPPV -- <strong>BENIGN</strong> <strong>PAROXYSMAL</strong> <strong>POSITIONAL</strong> <strong>VERTIGO</strong>10/02/2005 01:37 PMthe eyes) induced by the Dix-Hallpike test. It has been claimed that BPPV accompanied by unilateral lateral<strong>ca</strong>nal paralysis is suggestive of a vascular etiology (Kim et al, 1999). For diagnosis of BPPV withlaboratory tests, it is important to have the ENG test done by a laboratory that <strong>ca</strong>n measure verti<strong>ca</strong>l eyemovements. A magnetic resonance imaging (MRI) s<strong>ca</strong>n will be performed if a stroke or brain tumor issuspected. A rotatory chair test may be used for difficult diagnostic problems. It is possible but uncommon(5%) to have BPPV in both ears (bilateral BPPV).HOW IS BPPV TREATED?Wait it outOffice TreatmentHome TreatmentSurgi<strong>ca</strong>l TreatmentBPPV has often been described as "self-limiting" be<strong>ca</strong>use symptoms often subside or disappear within 2months of onset (Imai et al, 2005). BPPV is not intrinsi<strong>ca</strong>lly life-threatening. One <strong>ca</strong>n certainly opt to justwait it out.No active treatment (wait/see):If you decide to wait it out, certain modifi<strong>ca</strong>tions in your daily activities may be necessary to cope with yourdizziness. Use two or more pillows at night. Avoid sleeping on the "bad" side. In the morning, get up slowlyand sit on the edge of the bed for a minute. Avoid bending down to pick up things, and extending the head,such as to get something out of a <strong>ca</strong>binet. Be <strong>ca</strong>reful when at the dentist's office, the beauty parlor whenlying back having ones hair washed, when participating in sports activities and when you are lying flat onyour back.Symptoms tend to wax and wane. Motion sickness medi<strong>ca</strong>tions are sometimes helpful in controlling thenausea associated with BPPV but are otherwise rarely beneficial.As BPPV <strong>ca</strong>n last for much longer than 2 months, in our opinion, it is better to treat it activelyand be donewith it rather than taking the wait/see approach.OFFICE TREATMENT OF BPPV: The Epley and SemontManeuversThere are two treatments of BPPV that are usually performed inthe doctor's office. Both treatments are very effective, withroughly an 80% cure rate, according to a study by Herdman andothers (1993). If your doctor is unfamiliar with these treatments,you <strong>ca</strong>n find a list of knowledgeable clinicians from theVestibular Disorders Association (VEDA) .The maneuvers, named after their inventors, are both intended tohttp://www.dizziness-and-balance.com/disorders/bppv/bppv.htmlPage 3 of 13
BPPV -- <strong>BENIGN</strong> <strong>PAROXYSMAL</strong> <strong>POSITIONAL</strong> <strong>VERTIGO</strong>10/02/2005 01:37 PMmove debris or "ear rocks" out of the sensitive part of the ear(posterior <strong>ca</strong>nal) to a less sensitive lo<strong>ca</strong>tion. Each maneuver takesabout 15 minutes to complete. The Semont maneuver (also<strong>ca</strong>lled the "liberatory" maneuver) involves a procedure wherebythe patient is rapidly moved from lying on one side to lying onthe other (Levrat et al, 2003). It is a brisk maneuver that is notcurrently favored in the United States, but it is 90% effective after4 treatment sessions. In our opinion, it is equivalent to the Epleymaneuver as the head positioning is very similar, omitting only'C' from the figure to the right.The Epley maneuver is also <strong>ca</strong>lled the particle repositioning, <strong>ca</strong>nalith repositioning procedure, andmodified liberatory maneuver. It is illustrated in figure 2. Click here for a low bandwidth animation. Itinvolves sequential movement of the head into four positions, staying in each position for roughly 30seconds. The recurrence rate for BPPV after these maneuvers is about 30 percent at one year, and in someinstances a second treatment may be necessary.Variants: While some authors advo<strong>ca</strong>te use of vibration in the Epley maneuver, we have not found thisuseful in a study of our patients (Hain et al, 2000). Use of an antiemetic prior to the maneuver may behelpful if nausea is anticipated. Some authors suggest that position 'D' in the figure is not necessary (e.g.(Cohen et al. 1999; Cohen et al. 2004 ). In our opinion, this is a mistake as mathemati<strong>ca</strong>l modeling of BPPVsuggests that position 'D' is the most important position (Squires et al, 2004).When performing the Epley maneuver, <strong>ca</strong>ution is advised should neurologi<strong>ca</strong>l symptoms (for example,weakness, numbness, visual changes other than vertigo) occur. Oc<strong>ca</strong>sionally such symptoms are <strong>ca</strong>used bycompression of the vertebral arteries (Sakaguchi et al, 2003), and if one persists, a stroke could occur. If theexercises are being performed without medi<strong>ca</strong>l supervision, we advise stopping the exercises and consultinga physician. If the exercises are being supervised, given that the diagnosis of BPPV is well established, inmost <strong>ca</strong>ses we modify the maneuver so that the positions are attained with body movements rather than headmovements.After either of these maneuvers, you should be prepared to follow the instructions below, which are aimedat reducing the chance that debris might fall back into the sensitive back part of the ear.The "Gans" maneuver. This is a little used treatment maneuver, <strong>ca</strong>lled the "Gans maneuver by it'sinventor (R. Gans, Ph.D.), that is a hybrid between the Epley and Semont maneuvers. It incorporates thehead orientations to gravity of "B" and "D" in the Epley figure above, using the body positions of theSemont maneuver. There is too little published experience with this maneuver to say whether it is aseffective as the Epley/Semont but we suspect that it has the same effi<strong>ca</strong>cy, as it uses the same headpositions.Supplemental material on the site CD: Animation of Epley Maneuver.Note that this maneuver is done faster in the animation than in the clinic. Usually one allows 30 secondsbetween positions.http://www.dizziness-and-balance.com/disorders/bppv/bppv.htmlPage 4 of 13
BPPV -- <strong>BENIGN</strong> <strong>PAROXYSMAL</strong> <strong>POSITIONAL</strong> <strong>VERTIGO</strong>10/02/2005 01:37 PMwas 81%, compared to 37.% in placebo or untreated subjects. See here for the details.WHAT IF THE MANEUVERS DON'T WORK?These maneuvers are effective in about 80% of patients with BPPV. If you are among the other 20 percent,your doctor may wish you to proceed with the Brandt-Daroff exercises, as described below. If a maneuverworks but symptoms recur or the response is only partial (about 40% of the time according to Smouha,1997), another trial of the maneuver might be advised. The "habituation" exercises are also sometimesuseful in the situation where all other maneuvers (Epley, Semont, Brandt-Daroff) have been tried -- inessence these consist of a more intense and prolonged series of positional exercises. When all maneuvershave been tried, the diagnosis is clear, and symptoms are still intolerable, surgi<strong>ca</strong>l management (posterior<strong>ca</strong>nal plugging) may be offered.BPPV often recurs. About 1/3 of patients have a recurrence in the first year after treatment, and by fiveyears, about half of all patients have a recurrence (Hain et al, 2000; Nunez et al; 2000; Sakaida et al, 2003).If BPPV recurs, in our practice we usually retreat with one of the maneuvers above. While daily use ofBrandt-Daroff exercises would seem sensible, we did not find it to prevent recurrence (Helminski et al,2005).In some persons, the positional vertigo <strong>ca</strong>n be eliminated but imbalance persists. In these persons it may bereasonable to undertake a course of generic vestibular rehabilitation, as they may still need to compensatefor a changed utricular mass or a component of persistent vertigo <strong>ca</strong>used by cupulolithiasis. Conventionalvestibular rehabilitation has some effi<strong>ca</strong>cy, even without specific maneuvers. (Angeli, Hawley et al. 2003;Fujino et al ,1994) )HOME TREATMENT OF BPPV:BRANDT-DAROFF EXERCISESClick here for a low bandwidth animationThe Brandt-Daroff Exercises are a method oftreating BPPV, usually used when the officetreatment fails. They succeed in 95% of <strong>ca</strong>ses but aremore arduous than the office treatments. Theseexercises may take longer than the other maneuvers -- the response rate at one week is about 25% (Radkeet al, 1999). These exercises are performed in threesets per day for two weeks. In each set, one performsthe maneuver as shown five times.1 repetition = maneuver done to each side in turn(takes 2 minutes)Suggested Schedule forhttp://www.dizziness-and-balance.com/disorders/bppv/bppv.htmlPage 6 of 13
BPPV -- <strong>BENIGN</strong> <strong>PAROXYSMAL</strong> <strong>POSITIONAL</strong> <strong>VERTIGO</strong>10/02/2005 01:37 PMBrandt-Daroff exercisesTime Exercise DurationMorningNoonEvening5repetitions5repetitions5repetitions10minutes10minutes10minutesStart sitting upright (position 1). Then move into the side-lying position (position 2), with the head angledupward about halfway. An easy way to remember this is to imagine someone standing about 6 feet in frontof you, and just keep looking at their head at all times. Stay in the side-lying position for 30 seconds, oruntil the dizziness subsides if this is longer, then go back to the sitting position (position 3). Stay there for30 seconds, and then go to the opposite side (position 4) and follow the same routine.These exercises should be performed for two weeks, three times per day, or for three weeks, twice per day.This adds up to 52 sets in total. In most persons, complete relief from symptoms is obtained after 30 sets, orabout 10 days. In approximately 30 percent of patients, BPPV will recur within one year. If BPPV recurs,you may wish to add one 10-minute exercise to your daily routine (Amin et al, 1999). The Brandt-Daroffexercises as well as the Semont and Epley maneuvers are compared in an article by Brandt (1994), listed inthe reference section.When performing the Brandt-Daroff maneuver, <strong>ca</strong>ution is advised should neurologi<strong>ca</strong>l symptoms (i.e.weakness, numbness, visual changes other than vertigo) occur. Oc<strong>ca</strong>sionally such symptoms are <strong>ca</strong>used bycompression of the vertebral arteries (Sakaguchi et al, 2003). In this situation we advise not proceeding withthe exercises and consulting ones physician.Supplemental material on the site CD: Animation of Brandt-Daroff exercises. Note that this treatment maneuver is done faster in the animation than in actual use.Usually one allows 30 seconds between positions.Supplemental material on the site CD: Movie of Brandt-Daroff exercisesHOME EPLEY MANEUVERThe Epley and/or Semont maneuvers as described above <strong>ca</strong>n be done at home (Furman and Hain, 2004).For example, http://www.charite.de/ch/neuro/vertigo.html outlines a self-treatment Epley protocol. We mayrecommend the home-Epley to our patients who have a clear diagnosis. This procedure seems to be evenmore effective than the in-office procedure, perhaps be<strong>ca</strong>use it is repeated every night for a week.There are, however, several possible problems that may arise. If the diagnosis of BPPV has not beenconfirmed, one may be attempting to treat another condition (such as a brain tumor or stroke) withpositional exercises -- this is unlikely to be successful and may delay proper treatment. A second problem isthat the home-Epley requires knowledge of the "bad" side. Sometimes this <strong>ca</strong>n be tricky to establish.Compli<strong>ca</strong>tions such as conversion to another <strong>ca</strong>nal (see below) <strong>ca</strong>n occur during the Epley maneuver, whichare better handled in a doctor's office than at home. Finally, oc<strong>ca</strong>sionally during the Epley maneuverneurologi<strong>ca</strong>l symptoms are provoked due to compression of the vertebral arteries. In our opinion, it is saferhttp://www.dizziness-and-balance.com/disorders/bppv/bppv.htmlPage 7 of 13
BPPV -- <strong>BENIGN</strong> <strong>PAROXYSMAL</strong> <strong>POSITIONAL</strong> <strong>VERTIGO</strong>10/02/2005 01:37 PMto have the first Epley performed in a doctors office where appropriate action <strong>ca</strong>n be taken in thiseventuality.SURGICAL TREATMENT OF BPPV(POSTERIOR CANAL PLUGGING)If the exercises described above are ineffective incontrolling symptoms, symptoms have persisted for a yearor longer, and the diagnosis is very clear, a surgi<strong>ca</strong>lprocedure <strong>ca</strong>lled "posterior <strong>ca</strong>nal plugging" may berecommended. Canal plugging blocks most of theposterior <strong>ca</strong>nal's function without affecting the functionsof the other <strong>ca</strong>nals or parts of the ear. This procedureposes a small risk to hearing, but is effective in about 90%of individuals who have had no response to any othertreatment. Only about 1 percent of our BPPV patientseventually have this procedure done. Surgery should notbe considered until all three maneuvers/exercises (OfficeEpley, Office Semont, Home Epley) have been attemptedand failed. See the article by Parnes (1990, 1996) in the references for more information.There are several alternative surgeries. Dr Gacek (Syracuse, New York) has written extensively aboutsingular nerve section. Dr. Anthony (Houston, Texas), advo<strong>ca</strong>tes laser assisted posterior <strong>ca</strong>nal plugging. Itseems to us that these procedures, which require unusual amounts of surgi<strong>ca</strong>l skill, have little advantageover a conventional <strong>ca</strong>nal plugging procedure. Of course, it is always advisable when planning surgery toselect a surgeon who has had as wide an experience as possible.Compli<strong>ca</strong>tions are rare (Rizvi and Gauthier,2002)There are several surgi<strong>ca</strong>l procedures that we feel are inadvisable for the individual with intractableBPPV. Vestibular nerve section, while effective, eliminates more of the normal vestibular system than isnecessary. Similarly, transtympanic gentamicin treatment seems generally inappropriate. Labyrinthectomyand sacculotomy are also both generally inappropriate be<strong>ca</strong>use of reduction or loss of hearing expected withthese procedures.ATYPICAL BPPVLateral Canal BPPV, AnteriorCanal BPPV, Cupulolithiasis,Vestibulolithiasis, Multi<strong>ca</strong>nalpatternshttp://www.dizziness-and-balance.com/disorders/bppv/bppv.htmlPage 8 of 13
BPPV -- <strong>BENIGN</strong> <strong>PAROXYSMAL</strong> <strong>POSITIONAL</strong> <strong>VERTIGO</strong>10/02/2005 01:37 PMThere are several rarer variants of BPPVwhich may occur spontaneously as well asafter the Brandt-Daroff maneuvers orEpley/Semont maneuvers. They are mainlythought to be <strong>ca</strong>used by migration ofotoconial debris into <strong>ca</strong>nals other than theposterior <strong>ca</strong>nal, the anterior or lateral <strong>ca</strong>nal.It is also possible that some are due to otherconditions such as brainstem or cerebellar damage, but clini<strong>ca</strong>l experience suggests that this is very rare.There is presently no data reported as to the frequency and extent of these syndromes following treatmentprocedures. It is the author's estimate that they occur in roughly 5% of Epley maneuvers and about 10% ofthe time after the Brandt-Daroff exercises. In nearly all instances, with the exception of cupulolithiasis,these variants of BPPV following maneuvers resolve within a week without any special treatment, but whenthey do not, there are procedures available to treat them.In clini<strong>ca</strong>l practice, atypi<strong>ca</strong>l BPPV arising spontaneously is first treated with maneuvers as is typi<strong>ca</strong>l BPPV,and the special treatments as outlined below are entered into only after treatment failure. When atypi<strong>ca</strong>lBPPV follows the Epley, Semont or Brandt-Daroff maneuvers, specific exercises are generally begun assoon as the diagnosis is ascertained. In patients in whom the exercise treatment of atypi<strong>ca</strong>l BPPV fails,especially in situations where onset is spontaneous, additional diagnostic testing such as MRI s<strong>ca</strong>nning maybe indi<strong>ca</strong>ted. The reason for this is to look for other types of positional vertigo.Lateral <strong>ca</strong>nal BPPV is the most common atypi<strong>ca</strong>l BPPV variant, accounting for about 3-12 percent of <strong>ca</strong>ses(Korres et al, 2002; Hornibrook 2004). Many <strong>ca</strong>ses are seen as a consequence of an Epley maneuver. It isdiagnosed by a horizontal nystagmus that changes direction according to the ear that is down. More detailabout lateral <strong>ca</strong>nal BPPV as well as an illustration of a home exercise <strong>ca</strong>n be found hereAnterior <strong>ca</strong>nal BPPV is also rare, and a recent study suggested that it accounts for about 2% of <strong>ca</strong>ses ofBPPV (Korres et al, 2002). It is diagnosed by a positional nystagmus with components of downbeating andtorsional movement on taking up the Dix-Hallpike position, or a nystagmus that is upbeating and torsionalwhen sitting up from the Dix-Hallpike. There are a number of different suggestions in the literature aboutthe direction of the torsional quick phase in anterior <strong>ca</strong>nal BPPV. In our view, the nystagmus during theDix-Hallpike to one side is most likely due to excitation of the anterior <strong>ca</strong>nal on the opposite side. Thisshould <strong>ca</strong>use downbeating nystagmus as well as torsional nystagmus with a quick-phase towards thedisturbed ear. Thus the direction of the torsional component during the down-phase of the Dix-Hallpike tellsyou which is the bad ear. Anterior <strong>ca</strong>nal BPPV <strong>ca</strong>n be provoked from the opposite ear to the side of theDix-Hallpike maneuver -- in other words, if you get dizzy to the right side, the problem ear might be theleft. Some authors have suggested that be<strong>ca</strong>use the anterior <strong>ca</strong>nals are oriented so that parts are near thesaggital plane, anterior <strong>ca</strong>nal BPPV <strong>ca</strong>n be provoked with a Dix-Hallpike maneuver to either side as well asin the "head hanging" position (Bertholon et al, 2002). We have encountered a few patients who ONLYhave nystagmus in the head-hanging position. The upbeating nystagmus on sitting may be very persistent asthe debris settles on the cupula of the anterior <strong>ca</strong>nal. Anterior <strong>ca</strong>nal BPPV is probably rare be<strong>ca</strong>use theanterior <strong>ca</strong>nal is normally the highest part of the ear. Debris would naturally tend to fall out of the posteriorhalf of the anterior <strong>ca</strong>nal. From the geometry of the ear, it would seem likely that anterior <strong>ca</strong>nal BPPV mightoc<strong>ca</strong>sionally result as a compli<strong>ca</strong>tion of the Epley maneuver.Debris might also be temporarily lo<strong>ca</strong>ted in the common crus area, which is the shared <strong>ca</strong>nal between thehttp://www.dizziness-and-balance.com/disorders/bppv/bppv.htmlPage 9 of 13
BPPV -- <strong>BENIGN</strong> <strong>PAROXYSMAL</strong> <strong>POSITIONAL</strong> <strong>VERTIGO</strong>10/02/2005 01:37 PManterior and posterior <strong>ca</strong>nal. Should debris be present in the common cruse, one would expect a purelytorsional nystagmus. During the down phase of the Dix-Hallpike, when debris is falling backwards towardsthe ampulla, the torsional nystagmus should beat away from the bad ear. During the up phase of the Dix-Hallpike, when debris is moving towards the vestibule, the torsional nystagmus should beat towards the badear.In our clinic setting in Chi<strong>ca</strong>go, we have had the most success in treating anterior <strong>ca</strong>nal BPPV with a "deepDix-Hallpike". The idea is to invert the anterior <strong>ca</strong>nal, allow debris to fall to the "top" of the <strong>ca</strong>nal, and thenallow it to further migrate into the common crus and then vestibule.Cupulolithiasis is a condition in which debris is stuck to the cupula of a semicircular <strong>ca</strong>nal, rather thanbeing loose within the <strong>ca</strong>nal. Cupulolithiasis is not a treatment compli<strong>ca</strong>tion, but rather is part of thespectrum of BPPV. The mechanistic hypothesis is based on pathologi<strong>ca</strong>l findings of deposits on the cupulamade by Schuknecht and Ruby in three patients who had BPPV during their lives (Schuknecht 1969;Schuknecht et al. 1973). Moriarty and colleagues found similar deposits in 28% of 566 temporal bones(Moriarty et al. 1992). Schuknecht pointed out that cupulolithiasis hypothesis fails to explain the usualcharacteristic latency and burst pattern of BPPV nystagmus as well as remissions (Schuknecht et al. 1973).Rather, cupulolithiasis should result in a constant nystagmus. This pattern is sometimes seen (Smouha et al.1995). Cupulolithiasis might theoreti<strong>ca</strong>lly occur in any <strong>ca</strong>nal -- horizontal, anterior or verti<strong>ca</strong>l, each ofwhich might have it's own pattern of positional nystagmus. Some authors hold that both the cupulolithiasisand <strong>ca</strong>nalithiasis hypotheses may be correct (Brandt et al. 1994). If cupulolithiasis is suspected, it seemslogi<strong>ca</strong>l to treat with either the Epley with vibration, or alternatively, use the Semont maneuver. There are nostudies of cupulolithiasis to indi<strong>ca</strong>te which strategy is the most effective.Vestibulolithiasis is a hypotheti<strong>ca</strong>l condition in which debris is present on the vestibule-side of the cupula,rather than being on the <strong>ca</strong>nal side. For this theory, there is loose debris, close to but unattached to thecupula of the posterior <strong>ca</strong>nal, possibly in the vestibule or short arm of the semicircular <strong>ca</strong>nal. Pathologicstudies of BPPV have found roughly equal amounts of fixed debris on either side of the cupula (Moriarty etal. 1992), suggesting that loose debris might also be found on either side. For the vestibulolithiasismechanism, when the head is moved, stones or other debris might shift from vestibule to ampulla, or withinthe ampulla, impacting the cupula. This mechanism would be expected to resemble cupulolithiasis, having apersistent nystagmus, but with intermittency be<strong>ca</strong>use the debris is movable. Very little data is available as tothe frequency of this pattern, and no data is available regarding treatment.Multi<strong>ca</strong>nal patterns. If debris <strong>ca</strong>n get into one <strong>ca</strong>nal, why shouldn't it be able to get into more than one ? Itis common to find small amounts of horizontal nystagmus or contralateral downbeating nystagmus in aperson with classic posterior <strong>ca</strong>nal BPPV. While other explanations are possible, the most likely one is thatthere is debris in multiple <strong>ca</strong>nals. Gradually a literature is developing about these situations (Bertholon et al,2005).WHERE ARE BPPV EVALUATIONS AND TREATMENTSDONE?The Vestibular Disorders Association (VEDA) maintains a large and comprehensive list of doctors whohave indi<strong>ca</strong>ted a proficiency in treating BPPV. Please contact them to find a lo<strong>ca</strong>l treating doctor.http://www.dizziness-and-balance.com/disorders/bppv/bppv.htmlPage 10 of 13
BPPV -- <strong>BENIGN</strong> <strong>PAROXYSMAL</strong> <strong>POSITIONAL</strong> <strong>VERTIGO</strong>10/02/2005 01:37 PMAcknowledgementsMORE INFORMATIONLiterature-VEDA has recently published a patient-oriented book on BPPV.Supplemental material is available on the site CD:REFERENCES CONCERNING BPPV:Click here for recent, but possibly less relevant references.See also the following web pageshttp://www.charite.de/ch/neuro/vertigo.html -- This is a self-treatment Epley protocol.Search this sitePublished literature referred to above:Amin M, Giradi M, Neill M, Hughes LF, Konrad H. Effects of exercise on prevention of recurrenceof BPPV symptoms. ARO abstracts, 1999, #774Angeli, S. I., R. Hawley, et al. (2003). "Systematic approach to benign paroxysmal positional vertigoin the elderly." Otolaryngol Head Neck Surg 128(5): 719-25.ATACAN E, Sennaroglu L, Genc A, Kaya S. Benign paroxysmal positional vertigo afterstapedectomy. Laryngoscope 2001; 111: 1257-9.Bertholon, P., A. M. Bronstein, et al. (2002). "Positional down beating nystagmus in 50 patients:cerebellar disorders and possible anterior semicircular <strong>ca</strong>nalithiasis." J Neurol Neurosurg Psychiatry72(3): 366-72.BERTHOLON P, Chelikh L, Tringali S, Timoshenko A, et al. Combined horizontal and posterior<strong>ca</strong>nal benign paroxysmal positional vertigo in three patients with head trauma.Ann Otol Rhinol Laryngol 2005;114:105-10.Black FO, Pesznecker SC, Homer L, Stallings V. Benign paroxysmal positional nystagmus inhospitalized subjects receiving ototoxic medi<strong>ca</strong>tions. Otol Neurotol 2004: 25(3);353-8Brandt T, Daroff RB. Physi<strong>ca</strong>l therapy for benign paroxysmal positional vertigo. Arch Otolaryngol1980 Aug;106(8):484-485.Brandt T, Steddin S, Daroff RB. Therapy for benign paroxysmal positioning vertigo, revisited.Neurology 1994 May;44(5):796-800.Buckingham RA. Anatomi<strong>ca</strong>l and theoreti<strong>ca</strong>l observations on otolith repositioning for benignparoxysmal positional vertigo. Laryngoscope 109:717-722, 1999Cohen, H. S., et al. (1999). "Effi<strong>ca</strong>cy of treatments for posterior <strong>ca</strong>nal benign paroxysmal positionalvertigo." Laryngoscope 109(4): 584-90.Cohen, H. S., et al. (2004). "Treatment variations on the Epley maneuver for benign paroxysmalpositional vertigo." Am J Otolaryngol 25(1): 33-7.Epley JM. The <strong>ca</strong>nalith repositioning procedure: For treatment of benign paroxysmal positionalhttp://www.dizziness-and-balance.com/disorders/bppv/bppv.htmlPage 11 of 13