Implementing a community pharmacy minor ailment scheme
Implementing a community pharmacy minor ailment scheme
Implementing a community pharmacy minor ailment scheme
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Implementing</strong> a <strong>community</strong> <strong>pharmacy</strong> <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong><strong>Implementing</strong> a <strong>community</strong><strong>pharmacy</strong> <strong>minor</strong> <strong>ailment</strong><strong>scheme</strong>A practical toolkit for primary careorganisations and health professionalsThe National Pharmaceutical Association
contentsPage numberFORWARD 4INTRODUCTION 5• What is this toolkit? 5• How to use this toolkit 5• Who is this toolkit for? 5• Where do the ideas in this toolkit come from? 5GUIDE PRODUCTION 6POLICY AND CONTEXT 7• So what is a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>? 7• So why consider a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>? 7• References 9SUCCESSFUL CHANGE MANAGEMENT – WHAT DOES THEEVIDENCE BASE TELL US? 10STEPS TOWARDS IMPLEMENTATION 13CHAPTER ONE:Define a local strategy within the context of PCTpolicy and priorities 14CHAPTER TWO: Perform a needs assessment 16CHAPTER THREE: Develop the strategy with board level commitment 18CHAPTER FOUR:Develop and agree an action plan with timedmilestones for delivery 20CHAPTER FIVE: Pilot the <strong>scheme</strong> 26CHAPTER SIX: Implement the <strong>scheme</strong> 28• 6.1 Which GP practices and pharmacies should take partin the roll out? 29• 6.2Which <strong>minor</strong> <strong>ailment</strong>s and formulary drugs should becovered in the roll out? 31• 6.3 What type of training packages will be required? 33• 6.4 What about standard operating procedures? 351
Page number• 6.5 What about service level agreements? 36• 6.6 How should the <strong>scheme</strong> be publicised? 37• 6.7 How can patients access the <strong>scheme</strong>? 39• 6.8Do the patients have to see the pharmacist in a <strong>pharmacy</strong>consultation? 41• 6.9 How is information communicated to the GP practice 42• 6.10 How are the <strong>community</strong> pharmacists paid? 43• 6.11 How is patient expectation managed? 45• 6.12 What about clinical governance? 46CHAPTER SEVEN: Audit the <strong>scheme</strong> 49CHAPTER EIGHT: Build on the <strong>scheme</strong> 55A SUMMARY OF KEY MESSAGES FROM EXISTING SCHEMES 57LIST OF ABBREVIATIONS 59APPENDICES 61• Appendix 1:Example of recording form for collectingbaseline data 62• Appendix 2: Examples of project proposals / summaries 63• Appendix 3:Generic list of competencies for <strong>community</strong>pharmacies involved in providing a <strong>minor</strong> <strong>ailment</strong>service 73• Appendix 4: Examples of formularies 76Page number• Appendix 7: Example of <strong>pharmacy</strong> briefing 86• Appendix 8: Example of GP surgery protocol 87• Appendix 9: Examples of receptionist protocols 89• Appendix 10: Examples of <strong>pharmacy</strong> protocols 90• Appendix 11: Examples of service level agreements 92• Appendix 12: Examples of patient information 104• Appendix 13: Examples of how patients access the <strong>scheme</strong>s 105• Appendix 14: Examples of <strong>pharmacy</strong> prescription forms 106• Appendix 15: Examples of forms to communicate to the GP 109• Appendix 16: Examples of <strong>pharmacy</strong> claims forms 111• Appendix 17: Clinical governance implications forpharmacies providing a <strong>minor</strong> <strong>ailment</strong> service 114• Appendix 18: Generic checklist for establishing arobust clinical governance framework for <strong>minor</strong><strong>ailment</strong> <strong>scheme</strong>s 115• Appendix 19: Examples of Serious Untoward Incidentreporting forms 118• Appendix 20: Examples of patient surveys 121• Appendix 21: Examples of <strong>pharmacy</strong> record cards 126• Appendix 22: Examples of <strong>pharmacy</strong> monitoring forms 127• Appendix 23: Summary of the South Sefton PCT <strong>scheme</strong> 128• Appendix 5: Examples of formulary protocols 79• Appendix 6: Example of locum information 8323
forewordintroductionThis toolkit is a practical guide for health professionals and PCTs on how toimplement and monitor a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>. Research shows that up to 40%of GP time is taken up dealing with <strong>minor</strong> <strong>ailment</strong>s. However, the introduction of<strong>community</strong> <strong>pharmacy</strong> <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>s has been proven to transfer <strong>minor</strong><strong>ailment</strong> consultations from general practice to <strong>community</strong> <strong>pharmacy</strong> whichallows GPs to treat patients with more appropriate needs. There are real benefitsfor patients to get quicker expert advice in the <strong>pharmacy</strong> without having to makea GP appointment. Evaluations of existing <strong>scheme</strong>s have shown them to besafe, effective and well received by patients.A <strong>community</strong> <strong>pharmacy</strong> <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong> is where the <strong>community</strong>pharmacist supplies medication on the NHS from a limited formulary free ofcharge to patients who are exempt from prescription charges. Therefore, thepayment barrier is removed encouraging more patients to consult with theirpharmacist rather than with their GP for <strong>minor</strong> <strong>ailment</strong>s. For those who do payprescription charges, the <strong>scheme</strong>s promote the role of the pharmacist as amedicines expert and encourage the patient to consult the pharmacist for adviceon treating <strong>minor</strong> <strong>ailment</strong>s. There are numerous <strong>community</strong> <strong>pharmacy</strong> <strong>minor</strong><strong>ailment</strong> <strong>scheme</strong>s running in England and increasing interest among PCTs toconsider introducing one.With the publication of the new GMS contract, the Government consultation onchoice, responsiveness and equity in the NHS, plus the increasing pressure ofmore and more patients being treated in the <strong>community</strong>, now is the time for PCTsto explore all the options that will help to ease the burden on GP practices andimprove access in primary care.The toolkit has been developed by health professionals and PCT staff who havealready implemented successful <strong>scheme</strong>s. The toolkit provides useful guidance,practical tips and examples of paperwork from existing <strong>scheme</strong>s. If you areinterested in helping GP practices meet the targets in the new GMS contract,helping PCTs meet Government access targets, and developing local <strong>community</strong><strong>pharmacy</strong> services then this toolkit is essential reading and I highly recommendit to you.Dr Simon FraddChairmanDoctor Patient PartnershipWhat is this toolkit?This is a practical toolkit to help primary care trusts (PCTs) and healthprofessionals to implement, monitor and review a successful <strong>minor</strong> <strong>ailment</strong><strong>scheme</strong> based on the experience of established <strong>scheme</strong>s to date. This toolkit isnot meant to be used as a rigid framework for implementation, but is meant toprovide flexibility for PCTs to dip in and out of the toolkit in order to develop alocal <strong>scheme</strong> which has a strong local ownership. The toolkit provides key tipson how to influence change, project management, and lessons learnt fromexisting <strong>scheme</strong>s. It also includes examples of documentation from existing<strong>scheme</strong>s in order to help professionals to develop their own ideas. Examples ofdocumentation are also available on the National Pharmaceutical Associationwebsite at www.npa.co.uk (under ‘publications’ then ‘NHS ServiceDevelopment’) so that they can be downloaded and adapted for local use asrequired.How to use this toolkitThis toolkit is designed to take you through the steps of considering,implementing, monitoring and reviewing a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>. It identifies thekey areas that should be considered locally and provides supporting informationfrom existing <strong>scheme</strong>s to allow PCTs to build up a locally owned <strong>scheme</strong>. Eachsection includes as appropriate:Key pointsHow to influence changePractical tips from the existing <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>sFurther readingWho is this toolkit for?If you are interested in improving patient access and choice in primary care,developing local <strong>community</strong> <strong>pharmacy</strong> services, helping GP practices meettargets in the general medical service (GMS) contract and helping PCTs meetGovernment access targets then this toolkit is for you.Where do the ideas in this toolkit come from?This resource was developed in response to a call from PCTs and localpharmaceutical committees (LPCs) for a practical toolkit to stop themreinventing the wheel. The content is based on the experiences of successful<strong>scheme</strong>s to date, and has drawn on the expertise of national bodies andacademia.In addition, a recent report reviewed the evidence from existing <strong>scheme</strong>s in orderto inform discussions on a wider roll out of such <strong>scheme</strong>s 1 . The report called fora toolkit to assist PCTs in setting up <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>s to maximiseapplication of learning from current <strong>scheme</strong>s and avoid reinvention of the wheel.4 5
guide productionpolicy and contextThis guide was produced by:• Claire Jones, Assistant Head of NHS Service Development, NationalPharmaceutical Association. Email c.jones@npa.co.ukWith contributions from:• Alison Blenkinsopp, Professor of Practice of Pharmacy, Department ofMedicines Management, Keele University. Emaila.blenkinsopp@mema.keele.ac.uk• Ian Spencer, Director of Clinical Governance, Northumberland, Tyne &Wear Strategic Health Authority. Email ian.spencer@nhs.netIndividuals who provided details of their <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>sand who commented on the toolkit:• Alan Cummings, Community Pharmacy Advisor, South Sefton PCT. Emailalan.cummings@southsefton-pct.nhs.uk• Ian Spencer, Director of Clinical Governance, Northumberland, Tyne &Wear Strategic Health Authority. Email ian.spencer@nhs.net• Helen Hill, Community Pharmacy Adviser, Croydon PCT. Emailhelen.hill@croydonpct.nhs.uk• Laraine Tuplin, Head of Prescribing and Medicines Management, CentralDerby PCT. Email laraine.tuplin@centralderby-pct.nhs.uk• Peter Magirr, Community Pharmacy Facilitator, Sheffield CommunityPharmacy Development Unit. Email peter.magirr@sheffieldse-pct.nhs.uk• Susie Coates, Pharmacy Development Manager, Sheffield CommunityPharmacy Development Unit. Email susie.coates@sheffieldse-pct.nhs.uk• Marie Hancock, Medicines Management Scheme Facilitator, EastYorkshire PCT. Email marie.hancock@eypct.nhs.uk• Graham Hill, Professional Development Pharmacist, East Riding and HullLPC. Email ghill@tinyworld.co.uk• Jayne Parkinson, Medicines Management Scheme Facilitator, HartlepoolPCT. Email jayne.parkinson@hartlepoolpct.nhs.ukSo what is a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>?Patients are encouraged to consult the <strong>community</strong> pharmacist rather than theGP for a defined list of <strong>minor</strong> <strong>ailment</strong>s. Patients who are registered withparticipating GP practices and are exempt from NHS prescription chargesreceive treatment from an agreed local formulary free of charge.So why consider a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>?Between 100 and 150 million GP consultations per year are for conditions thatare potentially self-treatable 2 . In addition, the latest research from theProprietary Association of Great Britain (PAGB) shows that up to 40% of GP timeis taken up dealing with patients suffering from <strong>minor</strong> <strong>ailment</strong>s 3 .This comes at a time when it is more important than ever for GP practices to beable to free up time in order to improve access to patients with more complexconditions 4 . This is important if GP practices are to meet the various targets inthe new GMS contract 5 and to cope with the increasing pressure of more andmore patients being treated in the <strong>community</strong>.Minor <strong>ailment</strong> <strong>scheme</strong>s provide real benefits to patients in terms of increasingpatient access and choice in primary care. This is important when theGovernment is currently placing so much emphasis on increasing patient choice6 . In addition, evaluations of existing <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>s have shown themto be safe, effective and well received by patients.Improving access to primary care is also top of PCT priorities. The primary careaccess target in the NHS plan states that by the end of 2004 all patients will beable to see a GP within 48 hours 7 . This target is now one of the key performanceratings targets for PCTs that informs the annual star ratings 8 .Therefore why not consider implementing a <strong>community</strong> <strong>pharmacy</strong> <strong>minor</strong><strong>ailment</strong> <strong>scheme</strong>? Research shows that the management of self-limiting <strong>minor</strong><strong>ailment</strong>s can be successfully transferred from general practice to <strong>community</strong><strong>pharmacy</strong>, and that this transfer reduces GP workload in terms of the number of<strong>minor</strong> <strong>ailment</strong> consultations 2,9,10,11 . For example, in the Care at the Chemist<strong>scheme</strong> over one third of the GP practice workload for 12 <strong>minor</strong> <strong>ailment</strong>s wastransferred to <strong>community</strong> <strong>pharmacy</strong> over a 6 month period 2,9 . Evidence fromexisting <strong>scheme</strong>s also shows shifts in the <strong>minor</strong> <strong>ailment</strong> consultation workloadfrom GP practices to <strong>community</strong> <strong>pharmacy</strong>. For example, the <strong>scheme</strong> inNorthumberland, Tyne & Wear transferred 1000 consultations in the first 9months, and across South Sefton PCT (where the Care at the Chemist <strong>scheme</strong>was originally piloted) over 1000 consultations per month are currentlytransferred from general practice to <strong>community</strong> <strong>pharmacy</strong> 1 .Therefore, while the evidence does not show that <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>sactually free up GP time, it does show that <strong>minor</strong> <strong>ailment</strong> consultations aresuccessfully transferred to <strong>community</strong> <strong>pharmacy</strong> allowing improved accessto GP practices for patients with more complex conditions.6 7
eferencesMinor <strong>ailment</strong> <strong>scheme</strong>s could also potentially have an impact on waiting times inaccident and emergency (A&E) departments. Research has shown that<strong>community</strong> <strong>pharmacy</strong> could manage an estimated 8% of adult attendances toinner city A&E departments 12 .The key feature of existing <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>s is that the <strong>community</strong>pharmacist supplies the medication from a limited formulary and patientsexempt from prescription charges receive these medicines free of charge. Hencethe payment barrier is removed. Therefore if the PCT has an area of deprivation,it may be particularly beneficial to launch a <strong>scheme</strong> in that area since patients insocially disadvantaged areas are more likely to receive over the counter (OTC)medicines on prescription than patients in more affluent areas 13,14 . Indeed theNatPaCT competency framework on medicines management, <strong>pharmacy</strong> andprescribing states that PCTs should consider a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong> if there isa payment barrier to the use of <strong>community</strong> <strong>pharmacy</strong> 15 .As well as considering a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong> to improve access to GPpractices, and potentially A&E departments, PCTs should also consider that it ispart of their core business to develop <strong>community</strong> <strong>pharmacy</strong> services. This rolewill become increasingly important with the implementation of the new <strong>pharmacy</strong>contract 16 , the publication of the Vision for Pharmacy in the new NHS 17 , and thePharmacy in the Future target that by April 2004 every PCT will have a medicinesmanagement <strong>scheme</strong> in place 18 .In summary, GP practices and PCTs have ever increasing workloads and targetsto meet. A <strong>community</strong> <strong>pharmacy</strong> <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong> will help improve patientaccess to GP practices and support a number of PCT targets.1. Blenkinsopp & Noyce. Minor illness management in primary care: a reviewof <strong>community</strong> <strong>pharmacy</strong> NHS <strong>scheme</strong>s 2002. Available atwww.keele.ac.uk/depts/mm/Publications/publi.htm (then ‘Downloadreports’).2. Whittington. Community <strong>pharmacy</strong> management of <strong>minor</strong> conditions – the‘Care at the Chemist’ <strong>scheme</strong>. PJ 2001 266 425-432. Available atwww.pharmj.com.3. GPs recommend OTC medicines for 40% of <strong>minor</strong> <strong>ailment</strong> consultations.PharmaLife news Jul 2002. Available at www.pharmalife.co.uk.4. Making a difference: reducing burdens on GPs. Cabinet Office 2002.Available at www.cabinet-office.gov.uk/regulation/PublicSector/Index.htm.5. New GMS contract 2003: investing in general practice. BMA / NHS Confed2003. Available at www.bma.org.uk/ap.nsf/Content/ Home Public.6. Building on the best. Choice, responsiveness and equity nationalconsultation. DoH 2003. Available at www.doh.gov.uk/choiceconsultation/.7. The NHS plan: a plan for investment, a plan for reform. DoH 2000.Available at www.doh.gov.uk/nhsplan/.8. Performance ratings for NHS trusts in England. CHI 2003. Available atwww.chi.nhs.uk/.9. Hassell. Managing demand: transfer of management of self-limitingconditions from general practice to <strong>community</strong> pharmacists BMJ 2001 323146-147. Available at www.bmj.com.10. Schafheutle. Direct supply of medicines in Scotland – evaluation of a pilot<strong>scheme</strong>. Research Findings. Scottish Exec 2003. Available atwww.scotland.gov.uk.11. Sheehy & Jones. Direct supply of medicines in Scotland – extendedmonitoring of a pilot <strong>scheme</strong>. Research Findings. Scottish Exec 2003.Available at www.scotland.gov.uk.12. Bednall. Identification of patients attending Accident and Emergency whomay be suitable for treatment by a pharmacist. Fam Pract 2003 20 54-57.Available at www.fampra.oupjournals.org/.13. Johnson. A search for socio-economic influences in behaviour andattitudes to medicines available for self-medication and NHS prescription.IJPP 2001 9(suppl) R27. Available at www.pharmj.com.14. Evans. Do increasing levels of income deprivation have an effect on theprescribing of OTC medication? IJPP 2001 9(suppl) R69. Available atwww.pharmj.com.15. PCT competency framework: Medicines management, <strong>pharmacy</strong> andprescribing. NatPaCT 2003. Available at www.natpact.nhs.uk/.16. Framework for a new <strong>pharmacy</strong> contract. DoH 2003. Available atwww.doh.gov.uk/<strong>pharmacy</strong>framework/index.htm.17. A vision for <strong>pharmacy</strong> in the new NHS. DoH 2003. Available atwww.doh.gov.uk/<strong>pharmacy</strong>vision/index.htm.18. Pharmacy in the future: implementing the NHS plan. DoH 2000. Availableat www.doh.gov.uk/<strong>pharmacy</strong>future/index.htm.8 9
change managementSuccessful change management – what does the evidencebase tell us?Effective methodsIneffectivemethods• Passivedistribution ofguidelineswithoutexplanation orfollow-up.• Didacticeducationalmeetings (e.g.lectures).In order to successfully implement any change in service provision it is essentialto understand what interventions work to change practice. Described below is asummary of the evidence base for change management. This has also beenincorporated into the following chapters under the section ‘how to influencechange’.To drive the<strong>scheme</strong>To implementthe <strong>scheme</strong>Effective methods• Use national and local opinion leaders toendorse the change.• Identify local leaders who will champion thecause and act as change agents.• Ensure that sufficient resources, of time, moneyand skills, are in place.• Involve all key stakeholders at an early stage.• Be prepared to be pragmatic and flexible withinthe rigorous pre-planned framework forimplementation.• Start small and build incrementally.• Do not expect to change behaviour overnight.• Target the enthusiasts / innovators first.• Accept that individuals vary in their acceptanceof change (see ‘individuals and changemanagement’ on page 12*).• Improve the understanding of roles andrelationships between healthcare professionals.• Use what is already there (such as regular teammeetings, educational events, communicationforums, audit processes) and build on previouswork.• Use convincing arguments - changes are morelikely to be implemented if they are perceivedas being:1. Advantageous2. Compatible with what is already happening,with the presence of an acceptable firststep3. Simple4. Able to be tried out in instalments5. Effectively implemented in other practicesor settings.Ineffectivemethods• Passively gaininglocal consensuson the <strong>scheme</strong>.To educate thehealthcareprofessionalsinvolvedTo educate thepublicTo educate thepatientsTo disseminateinformationabout the<strong>scheme</strong>To feedbackresults of the<strong>scheme</strong>• Employ a number of variable methods.• Use interactive methods, e.g. participation ofhealth care providers in workshops that includediscussion or practice.• Utilise postgraduate education programmes.• Use educational outreach visits.• Use multi-disciplinary education programmeswhere appropriate.• Ensure that the following points areemphasised:1. The reason for the change in practice2. The published evidence base for the<strong>scheme</strong>3. The benefits to patients4. The benefits to frontline staff5. The sustainability of the <strong>scheme</strong>.• Use mass media campaigns.• Ensure that the reason for the change and thebenefits of the change are clearlycommunicated.• Use patient-specific reminders (manual orcomputerised).• Disseminate by active education interventions.• Undertake educational outreach visits.• Utilise audit and feedback with follow-upreviews to improve performance.• Feedback should be ongoing and alwaysincludes specific recommendations.• Passivedisseminationalone, e.g.publication inprofessionaljournals,presentation atmeetings andmailing ofeducationalmaterial.• General feedbackon currentbehaviour, thatdoes not includespecificrecommendations.10 11
implementation*Individuals and change managementIndividuals vary in their acceptance of change. Therefore in order to drive changeit is important to understand that individuals respond differently to the conceptof change. Five different types of individual have been defined in terms of theirresponse to change:Category of individualCharacteristicsAction required to changeSteps towards implementationThis toolkit has been written as a series of steps to consider when implementinga <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>. The steps have been presented in a logical order butare not meant as a rigid process which should be flexible depending on localneeds.InnovatorVenturesome; able tounderstand and applycomplex technicalknowledge; copes with ahigh degree of uncertaintyNone!The key steps are summarised below, and each step is thendescribed in more detail in the following pagesEarly adopterSuccessful adopters of newideas; are usually localopinion leadersMention the ideaDefine a local strategy within the context of PCT policy andprioritiesEarly majorityDeliberate before introducingchange; frequently interactswith peersShow working examplePerform a needs assessmentDevelop the strategy with board level commitmentLate majorityLaggardsSceptical; needs peerpressureIsolated; traditionalProve it!Change regulations orintroduce sanctionsDevelop and agree an action plan with timed milestones fordeliveryAdapted from:• Anon. Getting evidence into practice. EHC 1999 5(1) 1-16. Available atwww.york.ac.uk/inst/crd/ehcb.htm.• Cantrill. Improving quality in primary care: supporting pharmacists working in primarycare groups and trusts. NPC / NPCRDC 1999. Available at www.npc.co.uk/.• Wye & McClenahan. Getting better with evidence: experiences of putting evidence intopractice. Kings Fund / NHSE 2000. Available atwww.doh.gov.uk/research/london/getbtr.pdf.• Queensborough & Pruce. Managing antibiotic prescribing: audit handbook. NPC /RPSGB 2000. Available at www.npc.co.uk/.Pilot the <strong>scheme</strong>Implement the <strong>scheme</strong>Audit the <strong>scheme</strong>Build on the <strong>scheme</strong>12 13
chapter oneDefine a local strategy within the context of PCT policy andprioritiesIn order to start to define a local strategy to implement a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>consider:• Whether a local <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong> is actually needed. Minor <strong>ailment</strong><strong>scheme</strong>s provide real benefits to patients in terms of increasing patientaccess and choice in primary care. This is important when theGovernment is currently placing so much emphasis on increasing patientchoice. In addition, evaluations of existing <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>s haveshown them to be safe, effective and well received by patients. Theevidence base suggests that <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>s are particularlysuccessful in socially disadvantaged areas, and are particularly wellreceived by mothers with young children. Alternatively, GP practices mayonly have a problem with patient consultations for a particular selflimitingcondition e.g. headlice. In this case a <strong>community</strong> <strong>pharmacy</strong>patient group direction (PGD) for headlice may be more appropriate.• What the local drivers are for establishing such a <strong>scheme</strong> (see ‘Policyand context’ page 7).• That it is important that the PCT takes an integrated approach toconsider all services that treat <strong>minor</strong> <strong>ailment</strong>s across the PCT. Thereforethe PCT should consider how a <strong>community</strong> <strong>pharmacy</strong> <strong>minor</strong> <strong>ailment</strong><strong>scheme</strong> will fit in with nurse triage clinics in GP practices, NHS Direct,walk-in centres and independent nurse prescribers. The evaluation ofNHS Direct indicates that a substantial proportion of callers who wouldotherwise have seen the GP were diverted to ‘self-care’ but the overalleffect on GP workload was found to be minimal. The evaluation of walkincentres showed that patients do consult about <strong>minor</strong> <strong>ailment</strong>s but theeffect on GP workload was difficult to establish and 44% of patientssubsequently reconsulted their GP about the same problem. This is notthe case with <strong>community</strong> <strong>pharmacy</strong> <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>s where <strong>minor</strong><strong>ailment</strong> consultations are transferred from GP practices to <strong>community</strong><strong>pharmacy</strong>, and the reconsultation rate for the same condition is very low(approximately 5%).Key points• When considering the need for a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong> it is importantthat the PCT defines how <strong>minor</strong> <strong>ailment</strong>s are treated across the PCT,how a <strong>community</strong> <strong>pharmacy</strong> <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong> will fit in, and whatthe local drivers are for establishing such a <strong>scheme</strong>.Practical tipsThe local drivers for establishing the existing <strong>scheme</strong>s included:Primary care access targets: GPs in socially disadvantaged areas spending asignificant amount of time treating <strong>minor</strong> <strong>ailment</strong>s. One <strong>scheme</strong> stated thatGPs in small practices in inner city areas were overrun with requests forappointments for <strong>minor</strong> illness by patients unwilling to purchase medicines.GP and pharmacist dissatisfaction with the current system: patients unwillingto pay for medicines clogging up surgeries to ask for medication that thepharmacists have originally advised they needed.Under-use of pharmacists’ skills.Promoting better use of pharmacists skills as part of Pharmacy in the Future.Promoting better working relationships between GPs and <strong>community</strong>pharmacists, and building on the successes of previous prescribingmanagement <strong>scheme</strong>s.Developing patient empowerment for the treatment of <strong>minor</strong> <strong>ailment</strong>s.Note: Some <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>s target a specific patient population or aspecific set of conditions. For example, in Eastern Hull the <strong>minor</strong> <strong>ailment</strong><strong>scheme</strong> is aimed at children aged 3 and under who live in a sociallydisadvantaged area. It is a collaborative <strong>scheme</strong> run in partnership by SureStart Noddle Hill, East Riding and Hull LPC and Eastern Hull PCT. The driversto establish this <strong>scheme</strong> came from the LPC and Sure Start to improve thehealth of young children in this area. The <strong>scheme</strong> particularly focuses onparental education to increase parent’s confidence and ability to selfmedicate for their children.Further reading• Blenkinsopp. Models of <strong>minor</strong> illness management in primary care: A scoping study2003. Available at www.keele.ac.uk/depts/mm/Publications/publi.htm (then ‘Downloadreports’).• Blenkinsopp & Noyce. Minor illness management in primary care: a review of<strong>community</strong> <strong>pharmacy</strong> NHS <strong>scheme</strong>s 2002. Available atwww.keele.ac.uk/depts/mm/Publications/publi.htm (then ‘Download reports’).• Salisbury. The national evaluation of NHS walk-in centres. University of Bristol 2002.Available at www.epi.bris.ac.uk/wic.• Munro. Evaluation of NHS Direct first wave sites: Final report to the DoH. University ofSheffield 2001. Available at www.shef.ac.uk/uni/academic/R-Z/scharr/mcru/reports.htm.14 15
chapter twoPerform a needs assessmentAt this stage, both assessment of current service provision and assessment ofresource implications for the service development are required:Needs assessment of current service provisionNeeds assessment involves measuring the health needs in a population. Theprocess of needs assessment can also be used to establish baseline data for the<strong>scheme</strong>. Therefore it is important at this early stage to decide what the requiredoutcomes of the <strong>scheme</strong> are and then decide how these outcomes can bemonitored (see chapter 7 for further details). This will help to ensure that the datacollected provides a sound baseline for planning, monitoring, and auditingoutcomes so that the impact of the <strong>scheme</strong> can be assessed.As part of this needs assessment it is important to consider what currentsystems GP practices have in place already to deal with the treatment of <strong>minor</strong><strong>ailment</strong>s e.g. nurse triage.Assessment of the resource implications for providing the serviceIt is important to assess the financial, commissioning, training, IM&T andworkforce implications of the service development.For example:• Financial: does the PCT have the funds to finance the service? Are thesefunds sustainable? What is the PCT financial planning process?• Commissioning: what will the impact be on the PCT staff who willcommission and manage the service?• Training: what type of education and training programmes will need to bedeveloped?• IM&T: does the current technology support the service development, orwill new software packages need to be introduced?• Workforce: what are the staffing and workload implications for GPpractices and <strong>community</strong> pharmacies?Key points• The local needs assessment of current service provision should providebaseline data for monitoring the service (e.g. prescribing data), thereforethe aims of the <strong>scheme</strong> should be clearly defined at this stage.• Carefully assess the resource implications to the PCT, and to the healthprofessionals who will provide the service.How to influence change• Ensure that sufficient resources, of time, money and skills, are in place.• Use what is already there, and build on previous work.Practical tips: defining the aims of the <strong>scheme</strong>Listed below are the defined aims of two of the existing <strong>scheme</strong>s:Aims of the <strong>scheme</strong> in Central Derby PCT:To reduce the high prescribing of <strong>minor</strong> illness treatments by inner city GPs.To reduce the demand for GP consultations by patients with <strong>minor</strong> illness.To improve access to GPs for more seriously ill patients.To improve the use of <strong>community</strong> pharmacists for advice and treatment andraise their profile.To deal with the reluctance of patients exempt from prescriptions charges topurchase medicines.Aims of the <strong>scheme</strong> in Eastern Hull PCT:To increase parent education on health issues for children aged 3 and under.To provide support and build confidence of parents/guardians with regard toself-help and medication for children aged 3 and under.To supply in appropriate circumstances OTC medication free of charge totreat an acute episode of a recognised condition.To decrease the inappropriate use of OTC medication by supplying aminimum quantity to treat the acute episode only.Practical tips: collecting baseline dataConsider collecting baseline data on <strong>minor</strong> <strong>ailment</strong> consultations in GPpractices. Appendix 1 shows the form used by East Yorkshire PCT to collectsuch data.Refer to chapter 7 for ideas of which outcomes can be monitored.Further reading• Advice and resources from the Royal Pharmaceutical Society of Great Britain (RPSGB)clinical audit unit at www.rpsgb.org.uk.• Hooper & Longworth. Health needs assessment workbook. Health Development Agency2002. Available at www.hda-online.org.uk/.• Series of articles in the British Medical Journal in 1998 on health needs assessment. Forexample, Wilkinson. Assessment in primary care: practical issues and possibleapproaches. BMJ 1998 316 1524-1528. Available at www.bmj.com.• Porteous. Novel provision of <strong>pharmacy</strong> services to a deprived area: a pharmaceuticalneeds assessment. IJPP 2003 11 47-54. Available at www.pharmj.com.• Williams. A pharmaceutical needs assessment in a primary care setting. BJGP 2000 5095-99.16 17
chapter threeDevelop the strategy with board level commitmentThere should be board level commitment to the implementation andsustainability of a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>. The proposal for the servicedevelopment should ideally be put to the PCT executive committee (PEC) orboard in September / October to coincide with the PCT annual planning cycle.In most cases the detailed presentation will be made to the PEC since this is the‘engine room’ of the PCT, with the PCT board then ratifying the decision of thePEC to move forward with the <strong>scheme</strong>.At this stage, ensure that the local opinion leaders are fully engaged with drivingthe process forward. Ideally, a local leader on the PCT board and PEC should beidentified.In order to present a convincing case to the PCT, the following points should beaddressed:• A description of what a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong> is and what it sets out toachieve.• How the <strong>scheme</strong> will fit in with other local initiatives to improve accessand meet PCT targets, e.g. as part of Advanced Access Initiatives. Astrategy for the implementation of a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong> will be mostuseful if it is seen in the wider context of improving access for patients.For example, how will the <strong>scheme</strong> fit in with treatment provided by walkincentres, or nurse triage clinics in GP practices? In addition describehow the <strong>scheme</strong> will help to support the implementation of the new GMScontract by improving access to GP practices or becoming part of thePCT’s integrated out-of-hours strategy.• The evidence base for the <strong>scheme</strong>: both published papers and examplesof successful <strong>scheme</strong>s in other areas should be included.• Results of the local needs assessment.• The benefits to patients.• The benefits to front line staff.• How the service will be piloted. It is always best to start small and thenbuild upon the <strong>scheme</strong> once it is running smoothly. Get the localinnovators to agree to pilot the service.• How the service will be developed. A strategy for the implementation of a<strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong> will be most useful if it is developed collaborativelyby health professionals and PCT managers, with input from patients.• How the service will be managed.• A description of the resource implications of the service.• How the service will be rolled out across the PCT.• How the service will be monitored and improved upon.• How learning will be shared and disseminated.How to influence change• Use national and local opinion leaders to endorse the service.• Identify local leaders who will champion the cause and act as changeagents.• Use convincing arguments - changes are more likely to be implementedif they are perceived as being:1. Advantageous2. Compatible with what is already happening, with the presence ofan acceptable first step3. Simple4. Able to be tried out in instalments5. Effectively implemented in other practices or settings.• Start small and build incrementally.• Target the enthusiasts / innovators first to pilot the <strong>scheme</strong>.Practical tipsA local opinion leader is essential to drive the service. Individuals who drovethe existing <strong>scheme</strong>s included:Locality pharmacistsCommunity <strong>pharmacy</strong> advisersPCT pharmaceutical advisersCommunity <strong>pharmacy</strong> facilitatorsPharmacy development managersLPC professional development pharmacistsGP practices in areas of social deprivationDirectors of primary careAppendix 2 shows briefings, summaries and PEC papers from the Croydon,South Sefton and Hartlepool <strong>scheme</strong>s.Further reading• Tann & Blenkinsopp. Understanding innovation in <strong>community</strong> <strong>pharmacy</strong> 2003. Availableat www.rpsgb.org.uk (then ‘Practice Research’).Key points• Ideally, present a paper to the PCT in September / October to coincidewith the PCT annual planning cycle.• Identify the local opinion leaders to drive the change.• Identify the local innovators to pilot the service.18 19
chapter fourDevelop and agree an action plan with timed milestones fordeliveryAll <strong>scheme</strong>s must have clear and specific objectives and be properly planned. Itis easy to feel overwhelmed at this stage therefore devise an action plan brokendown into small implementation steps. Each implementation step should have atimed milestone for delivery. Everyone involved in the <strong>scheme</strong> should be awareof the milestones.The action plan should include:1. Resources required: for example, each stage of the action plan shouldbe costed with a contingency reserve in place.2. Timescales and deadlines that must be met: each stage of the planshould include milestones with dates for completion. All stages of theaction plan should be monitored against agreed milestones andoutcomes. The implementation timetable in the action plan should belinked into the planning cycle of the PCT.3. How the <strong>scheme</strong> will be monitored, how the results will be fed back toall participants, and how action will be taken as a result.Everyone on the working group should be clear what the <strong>scheme</strong> is and what itsets out to achieve.The first role of the working group is to draw up and agree the action plan for theimplementation of the <strong>scheme</strong>. This approach will increase the commitment ofthe local stakeholders on the working group. Successful implementation of a<strong>scheme</strong>, even if developed successfully elsewhere, requires professionals tohave ownership of the process and outcomes locally.When drawing up the action plan, particularly concentrate on:• The steps within the timetable for implementation which will take themost time and/or resources so that these steps can be tackled first.• Identifying any problems or barriers to implementation at an early stageand developing plans to deal with them. Barriers to change can beformidable but implementation programmes can be successful if theyuse proven interventions. Use the ‘successful change management’section on page 10 as a checklist to ensure that all the evidence basedinterventions are being utilised in the action plan for <strong>scheme</strong>implementation.Practical responsibility for <strong>scheme</strong> implementation should rest with one namedindividual lead, acting on the guidance of a local working group. This lead shouldhave local credibility with the visible backing of the PCT chief executive. Inaddition, the implementation of the action plan will only be successful if there isa visible, high-level support and awareness within the PCT. The commitment ofthe chief executive, senior managers and non-executive directors will ensure thatimplementation is supported and fully integrated into the organisations way ofworking. Early links should also be formed with the finance and clinicalgovernance departments.The established <strong>scheme</strong>s found that some common concerns were raised 1 . Thetable below describes these concerns and how to address them.Patients might decide to consult the GP The Care at the Chemist evaluation showedThe working group should include all the relevant stakeholders, and be properlyanyway in addition to the pharmacist that there was no significant difference in reattendingthe GP surgery for the sameconsultation.funded to ensure that all key stakeholders can attend. To ensure that all keycondition within 14 days following astakeholders are included consider:pharmacist consultation or a GP• Who will be directly involved with providing the service? For example, itconsultation.is equally important to include receptionists as well as GPs, and counterEvidence from the evaluations of existingassistants as well as <strong>community</strong> pharmacists. If the <strong>scheme</strong> is to be<strong>scheme</strong>s indicates that there is littleduplication of service, with the majority ofpiloted involve the innovators who will pilot the service. Consider<strong>pharmacy</strong> consultations substituting for GPinvolving individuals at both ends of the ‘change spectrum’ (see page 12)consultations. Reconsultation rates with thein order to gain a broad perspective of the potential barriers toGP for the same condition appear to be veryimplementation.low.• Who the service will impact upon? Involving patients is essential inplanning services. Involve patients that are most likely to be affected bythe service, for example mothers of young children and the elderly.Section 11 of the Health and Social Care Act requires PCTs to consultwith patients upon service developments,• Who needs to be involved in making the changes to the service? Forexample, area managers from multiple <strong>pharmacy</strong> stores, practicemanagers from GP surgeries, PCT personnel who will be involved inadministering the service, the PCT communications lead, local opinionleaders to drive the change.• Who may have something else to contribute? For example, the <strong>community</strong>pharmacist clinical governance facilitator, independent nurse prescribers, arepresentative from the LPC, local medical committee (LMC), etc.20 21ConcernPharmacists might refer patients to the GPfollowing the <strong>pharmacy</strong> consultation.How to address the concernIn the Care at the Chemist <strong>scheme</strong> only3.6% of patients were referred back to GP inthe <strong>scheme</strong>’s ‘rapid referral’ mechanism.
Concern (continued)Patients who would not otherwise havemade an appointment to see the GP mightuse the <strong>scheme</strong>, creating additionalconsultations.Legal liability arising from receptionists’decisions about who to refer to the<strong>pharmacy</strong>.The occurrence of potentially serious events.In addition, concerns have been raised in relation to the effects on prescribingcosts 1 .ConcernHow to address the concern (continued)In terms of referral into <strong>pharmacy</strong> <strong>scheme</strong>s,some <strong>scheme</strong>s have opted for referral onlyafter a request to the practice by telephoneor visit for a GP appointment. This modelprovides the highest level of reassurance thatthe <strong>pharmacy</strong> consultation substitutes for aGP appointment but has the potentialdrawback of involving practice staff inadditional work (see section 6.7).In the evaluation of the Sheffield <strong>scheme</strong>patients were asked what they would havedone had the <strong>pharmacy</strong> <strong>scheme</strong> not beenavailable and 88% said they would haveconsulted their GP.Receptionists are not making clinicaldecisions. They are showing patients the listof symptoms covered by the <strong>scheme</strong> andoffering them a choice of seeing thepharmacist.Establishing a local adverse event reportingsystem as part of the clinical governanceframework for the <strong>scheme</strong> will ensure thatcommon problems are identified.How to address the concernOnce the action plan has been completed by the working group, it should bewidely consulted on and then approved by the PEC.Once agreed, the implementation timetable should be widely publicised.Progress against the milestones in the action plan should also be publicised sothat all the relevant people are kept informed.Therefore consider:• Who needs to receive the publicised action plan to begin to raise localawareness.• How local awareness of the planned <strong>scheme</strong> will be raised, e.g. pressreleases to the local media (see section 6.6).Key points• Nominate a local lead who should be responsible for implementing,monitoring and feeding back on the <strong>scheme</strong>.• Involve all key stakeholders in the planning and implementation process.Consider the funding that will be needed to get all stakeholders roundthe table.• Draw up and agree an action plan with timed milestones for delivery.• Identify any problems or barriers to implementation at an early stage anddevelop plans to deal with them.• Consider which steps within the timetable for implementation will takethe most time and/or resources so that these steps can be tackled first.• Link the implementation timetable in the action plan into the planningcycle of the PCT.• Consult widely on the action plan.• Publicise the implementation timetable and progress made towards theactions points in it.The public may abuse <strong>pharmacy</strong> <strong>scheme</strong>s byusing several pharmacies to obtain freemedicines.People who previously purchased OTCmedicines may stop doing so and switch tothe <strong>scheme</strong>.Voluntary patient registration with a specific<strong>community</strong> pharmacist for the purposes ofthe <strong>scheme</strong>, with a notification to thepatients GP will reassure those concernedabout abuse of the system by use of multiplepharmacies.Evidence from existing <strong>scheme</strong>s indicatesthat key user groups are children and peopleexempt from prescription charges on thegrounds of low income.How to influence change• Involve all key stakeholders at an early stage.• Be prepared to be pragmatic and flexible within the rigorous pre-plannedframework for implementation.• Accept that individuals vary in their acceptance of change.• Improve the understanding of the roles and relationships betweenhealthcare professionals.Pharmacists may prescribe more than GPswould for the same <strong>ailment</strong>.The Care at the Chemist <strong>scheme</strong> showedthat pharmacist and GP treatment costs peritem were similar during the study at £1.75.22 23
Practical tipsTop tips from the existing <strong>scheme</strong>s include:Involve all key stakeholders from the beginningKey stakeholders to include on the working group are: doctors, practicenurses, receptionists, practice managers, LPC, LMC, <strong>community</strong>pharmacists, medicines counter assistants, PCT pharmacists (includingprescribing advisers, <strong>community</strong> <strong>pharmacy</strong> facilitators), patients and patientrepresentative groups, representatives from the area medicines managementcommittee. It is particularly important to involve reception staff.Other stakeholders have included academia, the pharmaceutical industry(e.g. PAGB), and representatives from local initiatives (e.g. Health ActionZone or Sure Start).Consult widely on the <strong>scheme</strong> and action plan for implementationRegular communication and updates to all about the progress of <strong>scheme</strong>implementation is essential. For example:Croydon held a launch evening and two road shows in local GP practices toraise awareness of the <strong>scheme</strong>.East Yorkshire held face to face meetings with <strong>community</strong> pharmacists andGPs.Get all the concerns on the table at the beginningInitial barriers to establishing the existing <strong>scheme</strong>s included:Gaining agreement for the process, and the systems to put in place toimplement <strong>scheme</strong>.Initial <strong>minor</strong> teething problems in establishing administrative arrangementsfor reimbursement.Gaining agreement on which <strong>ailment</strong>s would be covered.Concerns from <strong>community</strong> pharmacists including: consistency of approachfrom different pharmacists, patients getting lots of medicines from severalpharmacies and abuse of the system.Concerns from GPs including: concerns they would be liable for anythingthat went wrong, GPs insisting that the <strong>scheme</strong> should not just be a supplyfunction but also an opportunity for pharmacists to better educate patientson self care.Lack of robust data on which to forecast activity and cost, leading to alimited budget and a delayed implementation.Lack of sustainable funding for the <strong>scheme</strong>.Getting sufficient publicity about the <strong>scheme</strong> to the people who would use it.South Sefton consulted on the <strong>scheme</strong> by attending various meetings andpresenting plans for the <strong>scheme</strong>.The Sheffield Community Pharmacy Development Unit held eveningmeetings for pharmacists and undertook practice visits to GPs.Northumberland, Tyne & Wear consulted mainly by stakeholder participationon the project board, but also gave numerous presentations on the <strong>scheme</strong>.Identify funding (note: the majority of existing <strong>scheme</strong>s now have recurrentfunding for the <strong>scheme</strong>):Topslice from the PCT drugs budgetPCT unified budgetPCT <strong>pharmacy</strong> development budgetPCT access fundPharmaceutical industryHealth Action Zone moniesSure Start moniesNew Deal monies24 25
chapter fivePilot the <strong>scheme</strong>Implementation should start with a pilot phase. This will help to address anyoperational problems, and will provide reassurance to staff that the new systemis not set in stone. Agree which health professionals will pilot the <strong>scheme</strong>, howthey will be trained, and how their compliance with local protocols will beassessed. Also agree on how the pilot phase will be evaluated, how long it willlast, and how results of the pilot phase will be fed back to all stakeholders.There are several ways of identifying pilot sites, for example:• Innovative GP practices and <strong>community</strong> pharmacies that will be willingto try something new.• GP practices and <strong>community</strong> pharmacies that are located in the areas ofgreatest need for the service.• By identifying a set of competencies that are required to run the service.These competencies could then be used to select suitable individuals.Appendix 3 describes an example of a core competency framework for<strong>community</strong> pharmacies providing a <strong>minor</strong> <strong>ailment</strong>s <strong>scheme</strong>.Also, consider whether only a small selection of <strong>minor</strong> <strong>ailment</strong>s should bepiloted. The choice of conditions will be determined from the results of the needsassessment. For example, the Care at the Chemist research showed that, beforethe <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong> was introduced, about 80% of GP <strong>minor</strong> <strong>ailment</strong>consultations were for headlice. Some <strong>scheme</strong>s simply considered from theneeds assessment which conditions presented a high volume to GP practicesbut a low risk if transferred to pharmacies.Key points• Implementation should start with a pilot phase in order to address anyoperational problems.• Agree the scope of the pilot, e.g. which health professionals will beinvolved, how many <strong>minor</strong> <strong>ailment</strong>s will be included, how long the pilotwill last, how the pilot will be evaluated and how the results will be fedback to all stakeholders.How to influence change• Start small and build incrementally.• Target the enthusiasts / innovators first.• Use convincing arguments - changes are more likely to be implementedif they are perceived as being:1. Advantageous2. Compatible with what is already happening, with the presence ofan acceptable first step3. Simple4. Able to be tried out in instalments5. Effectively implemented in other practices or settings.Practical tipsEast Yorkshire piloted eight <strong>minor</strong> <strong>ailment</strong>s in one GP practice in an area ofsocial deprivation in September 2000.In Eastern Hull, three medical conditions in children aged 3 and under werecovered for the first twelve months of the <strong>scheme</strong>. These were temperature,aches and pains; nasal congestion and nappy rash. A limited formulary ofparacetamol sugar free elixir 120mg/5ml (50ml), conotrane cream (100g) andpseudoephedrine elixir 30mg/5ml was used.Croydon chose to pilot their <strong>scheme</strong> in two wards with different deprivationlevels (as measured by Jarman scores) in order to compare the uptake of the<strong>scheme</strong> in a socially disadvantaged v a more affluent area. All GP practicesand pharmacies in these areas took part. The pilot clearly showed that thepatient uptake of the <strong>scheme</strong> was far greater in the socially disadvantagedarea, with 83% of all the vouchers issued being cashed in the sociallydisadvantaged area in 2001-2002.The following <strong>minor</strong> <strong>ailment</strong>s were piloted after discussions with localstakeholder groups: athletes foot, back pain, cough, diarrhea, fever,headache, headlice, soft tissue injury, sore throat, vaginal thrush, viral upperrespiratory tract infection, hayfever, allergic rhinitis and allergies.In Northumberland, Tyne & Wear, GP practices in the three health authoritiesin the Tyne & Wear area were mailed with details of the project and invited toapply to participate. Applications were assessed against the followingcriteria:1. one practice in each of the three health authority areas2. practice population (the aim was to achieve population coverage of25,000)3. relative deprivation4. perceived organisational capacity of the practice to implement andcomply with reporting framework and training5. willingness of local pharmacists to participate.Final approval was withheld until appropriate <strong>pharmacy</strong> participation wasconfirmed.Based on local morbidity data and seasonality the <strong>scheme</strong> was launched inthe month of December to treat upper respiratory infections andgastrointestinal symptoms.Further reading• For competencies for pharmacists working in primary care: Anon. PCT responsibilitiesaround prescribing and medicines management: a scoping and support guide. NPC2003. Available at www.npc.co.uk.• For useful ideas on consultation areas: Anon. Community <strong>pharmacy</strong> medicinesmanagement: a resource pack for <strong>community</strong> pharmacists. The <strong>community</strong> <strong>pharmacy</strong>medicines management project 2003. Available at www.medicinesmanagement.org.uk/.• For good practice guidance on implementing a protocol: Anon. Protocol-based care.Modernisation Agency 2002. Available atwww.modern.nhs.uk/scripts/default.asp?site_id=53.26 27
chapter sixImplement the <strong>scheme</strong>In order to implement the <strong>scheme</strong>, there are a number of key areas to considerwhich are described below. These areas should all be included in theimplementation action plan with an assessment of the resources needed andtimed milestones for delivery.These areas have been presented in a logical order but are not meant as a rigidprocess which should be flexible depending on local needs.The areas are summarised below, and each area is then described in more detailin the following pages:6.1 Which GP practices and pharmacies should take part in the roll out?6.2 Which <strong>minor</strong> <strong>ailment</strong>s and formulary drugs should be covered in the rollout?6.3 What type of training packages will be required?6.4 What about standard operating procedures?6.5 What about service level agreements?6.6 How should the <strong>scheme</strong> be publicised?6.7 How can patients access the <strong>scheme</strong>?6.8 Do the patients have to see the pharmacist in a <strong>pharmacy</strong> consultation?6.9 How is information communicated to the GP practice?6.10 How are the <strong>community</strong> pharmacists paid?6.11 How is patient expectation managed?6.12 What about clinical governance?6.1 Which GP practices and pharmacies should take part in theroll out?Once the results of the pilot have been fed back to the working group, and anyoperational teething problems have been sorted out, the working group shoulddecide the criteria for roll out of the <strong>scheme</strong> across the PCT.There are several ways of identifying sites to roll out the service, for example:• Opening up the <strong>scheme</strong> to all GP practices and <strong>community</strong> pharmacistsin the PCT.• Targeting GP practices and <strong>community</strong> pharmacies that are located inthe areas of greatest need for the service.• Identifying a set of competencies that are required to run the service.Appendix 3 describes an example of a core competency framework for<strong>community</strong> pharmacies providing a <strong>minor</strong> <strong>ailment</strong>s <strong>scheme</strong>.Key points• The working group should decide the criteria for roll out of the <strong>scheme</strong>.How to influence change• Do not expect change overnight.• Accept that individuals vary in their acceptance of change.• Improve the understanding of roles and relationships between healthcareprofessionals.• Use convincing arguments - changes are more likely to be implementedif they are perceived as being:1. Advantageous2. Compatible with what is already happening, with the presence ofan acceptable first step3. Simple4. Able to be tried out in instalments5. Effectively implemented in other practices or settings.28 29
Practical tipsEast Yorkshire expanded its <strong>scheme</strong> from eight to twenty <strong>minor</strong> <strong>ailment</strong>sfollowing its pilot <strong>scheme</strong>. The <strong>scheme</strong> started in one GP practice in an areaof social deprivation in September 2000 and was then expanded in June2003 to three GP practices in socially disadvantaged areas with an existinggood relationship with the <strong>community</strong> pharmacist.Croydon’s pilot used two wards with different deprivation levels (as measuredby Jarman scores) in order to compare the uptake of the <strong>scheme</strong> in a sociallydisadvantaged v a more affluent area. All GP practices and pharmacies inthese areas took part. Following the success of the project in the sociallydisadvantaged area the <strong>scheme</strong> was rolled out to other GP practices basedon their Jarman score for deprivation and also the prescribing of drugs oflimited clinical value.When the Care of the Chemist <strong>scheme</strong> was rolled out in South Sefton PCT itwas open to all in that PCT. But it was most successful where:1. The <strong>pharmacy</strong> participated actively in the <strong>scheme</strong>2. The GP practice had systems in place to refer patients to the <strong>scheme</strong>even when busy3. The <strong>pharmacy</strong> and GP practice staff worked together to make the<strong>scheme</strong> work.Central Derby rolled out the <strong>scheme</strong> to GPs where access was a problemwhich was mainly single handed GPs who were located in inner city, highethnic population areas. Community pharmacies were then chosen in thesame area.In the Sheffield Community Pharmacy Development Unit <strong>scheme</strong> the PCTdecided which GP practices were recruited into the <strong>scheme</strong>. Pharmacieswere then recruited according to co-location with a participating GP practice.Further reading• Anon. PCT responsibilities around prescribing and medicines management: a scopingand support guide. NPC 2003. Available at www.npc.co.uk.• Anon. Community <strong>pharmacy</strong> medicines management: a resource pack for <strong>community</strong>pharmacists. The <strong>community</strong> <strong>pharmacy</strong> medicines management project 2003. Availableat www.medicinesmanagement.org.uk/.6.2 Which <strong>minor</strong> <strong>ailment</strong>s and formulary drugs should becovered in the roll out?The range of <strong>minor</strong> <strong>ailment</strong>s and the formulary of drugs for the roll out should beinformed by the results of the pilot and following consultation with allstakeholders on these results.Selection of <strong>ailment</strong>s for inclusion in the <strong>scheme</strong>, formulary content andestablishment of proof of eligibility for access to the <strong>scheme</strong> appear to beeffective ways of controlling usage and costs of the <strong>scheme</strong> 1 . Therefore therange of <strong>minor</strong> <strong>ailment</strong>s and the drugs formulary should be considered carefully.Most <strong>scheme</strong>s focus on respiratory, gastrointestinal and skin <strong>ailment</strong>s 1 . Thethree criteria set by the Care at the Chemist <strong>scheme</strong> have been used by other<strong>scheme</strong>s to select the range of <strong>minor</strong> <strong>ailment</strong>s:• A high presentation rate of <strong>ailment</strong> to local GP practices• GPs willing to transfer the management to the <strong>community</strong> pharmacist• OTC non-blacklisted medicines available for treatment.Experience from existing <strong>scheme</strong>s shows the importance of <strong>community</strong>pharmacists being able to supply the same medicines as local GPs might usuallyprescribe. This ensures that patients are supplied with the same productswhether they consult the GP or the pharmacist. However, overly restrictivegeneric formularies for <strong>pharmacy</strong> supply can result in some patients revertingback to GP consultations to obtain a ‘better’ medicine 1 .As well as deciding on the list of formulary drugs, consideration should be givento what guidelines and advice should be included in the formulary, e.g. inclusionand exclusion criteria for treatment with the drug, when to refer to the GP, etc.Appendix 4 and 5 provide examples of formulary lists and details of formularies.The transferability of consultations from the GP to the pharmacist is variable andpatients find pharmacist consultation more acceptable for some symptoms thanothers. Reasons for not choosing a <strong>pharmacy</strong> consultation include co-existingconditions, the need for reassurance and the belief that an antibiotic is needed.In the Care at the Chemist <strong>scheme</strong>, the highest rates of transfer from the GP tothe <strong>scheme</strong> were for headlice and vaginal thrush, and the lowest was forearache 1 .Key points• Decide on the number of <strong>minor</strong> <strong>ailment</strong>s, the formulary drugs used totreat those <strong>ailment</strong>s (which ideally should only be those also availableon prescription), and what information the formulary should contain.• Selection of <strong>ailment</strong>s for inclusion in the <strong>scheme</strong>, formulary content andestablishment of proof of eligibility for access to the <strong>scheme</strong> appear tobe effective ways of controlling usage and costs of the <strong>scheme</strong>.30 31
6.5 What about service level agreements?Service level agreements (SLAs) should be drawn up for pharmacies and GPpractices to support corporate governance arrangements in the PCT.Practical tipsAppendix 11 contains examples of SLAs from existing <strong>scheme</strong>s.Further reading• Anon. Evidence based commissioning for PCTs: a directory. DoH 2003. Available atwww.doh.gov.uk/pricare/pctdirectory.pdf.• Anon. Service level agreement guidance. DoH 2003. Available atwww.doh.gov.uk/nhsfinancialreforms/sla.htm.6.6 How should the <strong>scheme</strong> be publicised?Before the <strong>scheme</strong> is publicised ensure that NHS Direct has all therelevant details of the <strong>scheme</strong> so that it can refer callers appropriately.One of the roles of the working group within the implementation action planshould be to prepare a communications plan for the <strong>scheme</strong>. This plan will helpto:• Identify the audience: e.g. patients and service users, staff involved inthe <strong>scheme</strong>, PCT staff including the chief executive, senior managersand non-executive directors.• Agree themes and messages: to ensure the messages are clear, simple,precise, concise and relevant to users.• Identify and develop tools: e.g. patient information leaflets, posters,presentations, newsletters, regular reports to the board, information inthe PCT annual report, on the PCT website, and in the PCT patientprospectus.• Implement and receive responses as part of the monitoring process.• Review effectiveness of the communications plan.The PCT communications lead should be a key member of the PCT workinggroup in order to bring their local media contacts and expertise to the table. Apunchy press release which offers photo opportunities should be considered tograb media attention.In terms of specifically advertising the <strong>scheme</strong> to the public, the more active thepromotion is the greater the transfer rates of <strong>minor</strong> <strong>ailment</strong> consultations fromGP practices to <strong>community</strong> pharmacies will be. Raising public awareness of theavailability of the <strong>scheme</strong> and changing patient behaviour take time to show theireffects and it may take 1-2 years before <strong>scheme</strong>s reach saturation in terms ofpotential uptake 1 . Schemes have generally used the local media (particularlylocal radio) with great success.Publicity for <strong>scheme</strong>s through posters in GP surgeries and pharmacies, the useof patient information leaflets, and endorsement by GPs have all shown to raisepublic awareness of existing <strong>scheme</strong>s 1 .Displaying a poster at practice reception and use of a patient card at receptionwith the list of conditions covered by the <strong>scheme</strong> will help practice staff to referpatients.Active promotion of the <strong>scheme</strong> by GPs can be undertaken at the end ofconsultations for <strong>minor</strong> <strong>ailment</strong>s. This approach should be encouraged sinceendorsement of the <strong>scheme</strong> by GPs is key 1 . It is essential that all GPs aresupportive of the <strong>scheme</strong> and give positive messages to patients about the<strong>scheme</strong>, since some <strong>scheme</strong>s have found that patients feel they are eitherreceiving a “second rate service” by getting a <strong>pharmacy</strong> consultation instead ofa GP consultation, or are being “fobbed off” by the GP practice.36 37
Key points• The working group should prepare a communications plan for the<strong>scheme</strong> which will help to identify the audience, agree the keymessages, and identify how information will be disseminated.• The more active the promotion of the <strong>scheme</strong> to the public is, thegreater the transfer rates of <strong>minor</strong> <strong>ailment</strong> consultations from GPpractices to <strong>community</strong> pharmacies will be.• Endorsement of the <strong>scheme</strong> by GPs is essential.• Experience from existing <strong>scheme</strong>s shows that changing patientbehaviour takes at least several months and that publicity andendorsement by GPs are key accelerators of uptake.• The PCT communications lead should be a key member of the PCTworking group in order to bring their local media contacts and expertiseto the table. Schemes have generally used the local media (particularlylocal radio) with great success.• A punchy press release which offers photo opportunities should beconsidered to grab media attention.• Before the <strong>scheme</strong> is publicised ensure that NHS Direct has all therelevant details of the <strong>scheme</strong> so that it can refer callers appropriately.How to influence change• Use mass media campaigns.• Ensure that the reason for the change and the benefits of the change areclearly communicated.Practical tipsAll the established <strong>scheme</strong>s agree that a wide ranging publicity <strong>scheme</strong> iskey to the success of the <strong>scheme</strong>. Publicity has included:• Information slips stapled to repeat prescriptions.• Posters and patient information leaflets in GP surgeries.• Advertising in libraries, in shopping centres, and on bus stops.• Newspaper articles.The PCT communications lead should be included on the PCT workinggroup to ensure maximum coverage of the <strong>scheme</strong> in the local media.Appendix 12 contains examples of patient information.Further reading• Anon. Toolkit for producing patient information. DoH 2003. Available atwww.doh.gov.uk/nhsidentity/toolkit-patientinfo.htm.6.7 How can patients access the <strong>scheme</strong>?The <strong>scheme</strong>s are generally available to patients who are exempt from payingprescription charges.During the Care at the Chemist study patients were referred into <strong>scheme</strong> by theGP practice only and the practice faxed a form through to <strong>pharmacy</strong> to informthe <strong>pharmacy</strong> of each patient they were referring.The established <strong>scheme</strong>s now mostly use a mixture of GP referral (e.g. patientcollects a voucher from the practice) and patients self-referring directly to a<strong>pharmacy</strong> with the <strong>pharmacy</strong> first checking that the patient is eligible:SchemeSouth SeftonNorthumberland, Tyne & WearCroydonCentral DerbySheffieldEastern HullEast YorkshireReferral methodSelf referral to the <strong>pharmacy</strong>, GP surgery referralSelf referral to the <strong>pharmacy</strong>, GP surgery referralGP surgery referral (voucher <strong>scheme</strong>)Self referral to the <strong>pharmacy</strong>, GP surgery referralSelf referral to the <strong>pharmacy</strong>, GP surgery referralSelf referral to the <strong>pharmacy</strong>Self referral to the <strong>pharmacy</strong>Establishing proof of patient eligibility for access to the <strong>scheme</strong> is an effectiveway of controlling usage and costs of the <strong>scheme</strong>. For example, the GP practicesupplying a voucher to the patient, or the <strong>pharmacy</strong> checking the eligibility ofpatients who self refer.The effects of <strong>scheme</strong>s on practice staff workload are dependent on themechanisms used to refer patients to <strong>community</strong> pharmacies. While individualreferral by practice staff provides direct evidence of substitution for GPconsultation it also increases staff workload. There is, therefore, a trade offbetween ensuring that the pharmacist consultation substitutes for a GPconsultation by patients being referred to the <strong>scheme</strong> by the GP practice vminimising additional workload for practice staff.A possible solution is for PCTs to consider a system where patients voluntarilyregister with the <strong>pharmacy</strong> of their choice for the purposes of using the <strong>scheme</strong>,with the <strong>pharmacy</strong> informing the patients GP of the registration. This would notaffect patients’ free choice of <strong>pharmacy</strong> for dispensing and other services, wouldenable maximum usage while minimising additional work for practice staff, andwould help to ensure that the PCT is contributing to the patient choice agenda.Key points• There is a trade off between ensuring that the pharmacist consultationsubstitutes for a GP consultation by patients being referred to the<strong>scheme</strong> by the GP practice v minimising additional workload forpractice staff.38 39
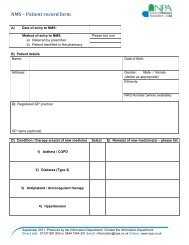
Practical tipsIn Croydon patients collect a voucher from the GP surgery.In Central Derby patients have a booklet issued either by the surgery or the<strong>pharmacy</strong> once patient eligibility has been checked. Patients can then selfrefer with the booklet to any <strong>pharmacy</strong> in <strong>scheme</strong>.In East Yorkshire the <strong>scheme</strong> began with patients collecting a referral slipfrom the GP surgery and presenting this to <strong>community</strong> pharmacist. Nowpatients can self refer to any <strong>pharmacy</strong>. The pharmacist and patientcomplete a form detailing patient and <strong>pharmacy</strong> details, nature of the <strong>minor</strong><strong>ailment</strong> and outcome of the consultation. A top copy is sent to the PCT, asecond copy to the practice and a third copy is kept by the <strong>pharmacy</strong>. Thepatient gives written consent to the PCT for having details of theirconsultation recorded in this way.In Eastern Hull the parent / guardian completes a Sure Start RegistrationForm in the <strong>pharmacy</strong> in order to access the <strong>scheme</strong>. This is then forwardedby the <strong>pharmacy</strong> to Sure Start. The <strong>pharmacy</strong> then adds the patient detailsto their Patient Log and allocates a patient code to the patient. This isrecorded on the Sure Start Registration Form and in the Personal ChildHealth Record. The parents / guardians must prove that the patient is a childaged 3 and under, and that the patient’s home address is within thecatchment area for the <strong>scheme</strong>.6.8 Do the patients have to see the pharmacist in a <strong>pharmacy</strong>consultation?Consideration should be given as to whether the local written protocols shouldstipulate that the pharmacist handles all <strong>minor</strong> <strong>ailment</strong> consultations under the<strong>scheme</strong>.There is a varying approach in the established <strong>scheme</strong>s as to whether thepharmacist and/or the trained medicines counter assistant can see the patientunder the <strong>scheme</strong>.Practical tipsCroydon, East Yorkshire, and Sheffield all stipulate that patients must see the<strong>community</strong> pharmacist since the PCT is paying for a <strong>community</strong> pharmacistconsultation.Central Derby, Eastern Hull, South Sefton and Northumberland, Tyne & Weardo not specify that the patient must be seen by the pharmacist. The SouthSefton <strong>scheme</strong> specifies that the <strong>pharmacy</strong> must follow it’s own standardoperating procedures for the treatment of <strong>minor</strong> <strong>ailment</strong>s. In Northumberland,Tyne & Wear counter staff can initiate the consultation and obtain as muchinformation from the patient as possible but the ‘prescription’ must be signedby the pharmacist. In Eastern Hull, counter staff are fully involved in theservice and provide advice or refer on when appropriate.In South Sefton patients register with a <strong>pharmacy</strong> in a number of ways:1. Possessing an FP10 bearing the name of a south Sefton GP2. Possessing a repeat slip bearing the name of a south Sefton GP3. A record on the <strong>pharmacy</strong> patient medication record (PMR) showingregistration with a south Sefton GP4. Referral form from the surgery5. Verbal referral from the surgery. The pharmacist must then phone thesurgery to confirm.The <strong>pharmacy</strong> then issues the patient with a Care at the Chemist Passport.This can be used to access the <strong>scheme</strong> in any participating <strong>pharmacy</strong>.In Sheffield the pharmacist must satisfy themselves that the patient isregistered at a participating surgery - this can be via documentation providedunder the <strong>scheme</strong>, but in many cases the <strong>pharmacy</strong> PMR can confirm thepractice that the patient attends. Patients present at any <strong>pharmacy</strong> operatingthe <strong>scheme</strong> and request the service. The <strong>pharmacy</strong> notes the patient’sdoctor in all cases and this information is audited. As on an FP10 form, thepatient signs to confirm their prescription charge exempt status.In Northumberland, Tyne & Wear patients obtain an information leaflet whichcontains a voucher. Exemption status is checked by the pharmacist toensure patients are exempt from prescription charges. The prescription formthat the pharmacists use includes a declaration of exemption that must besigned by the patient or their representative.Appendix 13-14 includes examples of patient registration forms, vouchersand <strong>pharmacy</strong> prescription forms.40 41
6.9 How is information communicated to the GP practice?There are two reasons why information could be communicated back to a GPpractice:• The pharmacist needs to urgently refer a patient to a GP.• The pharmacist sends the GP practice information on patientattendances at the <strong>pharmacy</strong> so that the GP can record this in thepatient notes.There must be a robust mechanism for the pharmacist to quickly referappropriate patients to their GP. This is particularly important when <strong>scheme</strong>sallow patients to self refer to a <strong>pharmacy</strong>.The majority of the existing <strong>scheme</strong>s cover this aspect within their standardoperating procedures (section 6.4), and use a <strong>pharmacy</strong> referral fax back form tothe GP practice.Practical tipsAppendix 15 includes examples of urgent <strong>pharmacy</strong> referral forms andrecords of <strong>pharmacy</strong> supply for GP practices.6.10 How are the <strong>community</strong> pharmacists paid?In the existing <strong>scheme</strong>s, remuneration is usually based on a ‘prescription’ writtenby the <strong>community</strong> pharmacist which includes patient details and treatmentsupplied.Pharmacists usually submit these ‘prescriptions’ to the PCT on a monthly basiswith a summary sheet of items supplied.Currently <strong>scheme</strong>s use a mixture of fee per item of service and banded feestructures, the latter being less work intensive for PCTs.All <strong>scheme</strong>s reimburse costs of treatment supplied for each item.PCT finance staff generally carry out data entry and arrange for payments to bemade. Paying the <strong>community</strong> pharmacists to provide the <strong>scheme</strong> is one of themost time consuming elements of the <strong>scheme</strong> for the PCT. For example, in theCroydon <strong>scheme</strong> an administrative assistant spends 1.5-2 days to processapproximately 560 consultation vouchers 1 .Ways to make the process less time consuming include:• Using a banded fee structure for payment.• The possibility of the Prescription Pricing Authority (PPA) administeringpayments the same way they do for FP10s. This may become a realityonce <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>s are viewed as one of the supplementaryservices in the new <strong>pharmacy</strong> contract. This would also ensure that thePCT had a ready made source of auditable data for the <strong>scheme</strong>, i.e.PACT data.• Using already established mechanisms in the PCT for administeringpayment to pharmacies, e.g. payment systems for services to carehomes, etc. However a method a data collection is still needed for auditpurposes.When considering payments to <strong>community</strong> pharmacists, it is also important that:• The LPC is involved at an early stage.• The issue of VAT is considered at an early stage. There is no clear cutnational policy on this issue, however Customs and Excise are likely totreat the professional fees for <strong>minor</strong> <strong>ailment</strong>s services as being VATexempt, but the supply of medicines under these <strong>scheme</strong>s as beingsubject to VAT. There is discretion at local level amongst Customs andExcise offices in terms of deciding what constitutes a VAT exemptprofessional service, therefore PCTs and contractors should discuss thespecifics of the service with their local office at an early stage.Key points• Consider what data are required from the pharmacies for payment andaudit purposes, how payments will be administered, and how oftenpayments will be made.• Consider the issue of VAT at an early stage.• Involve the LPC in the negotiations.42 43
Practical tips: remuneration structuresSchemeRemuneration structureSouth Sefton £500 annually for up to 400 items then £500per additional 300 itemsNorthumberland, Tyne & Wear £3.00 consultation fee from 1 st April 2003(prior to that was £1.50 consultation fee)6.11 How is patient expectation managed?Managing patient expectation of the <strong>scheme</strong> is very important. For example,some patients may expect:• To jump the queue in order to see the pharmacist immediately.• A 10 minute consultation from the pharmacist as they would from the GP.• To be examined by the pharmacist in the same way that a GP would.• Free prescriptions even though they are non-exempt.The patient information that accompanies the <strong>scheme</strong> should ideally address theabove points in order to manage patient expectation.CroydonCentral DerbySheffield CommunityPharmacy Development UnitEastern HullEast YorkshireA sliding scale related to workload:1 – 20 consultations £1021 – 40 consultations £2041 – 60 consultations £3061 – 80 consultations £4081 – 100 consultations £50100 + consultations £60£50 retainer then£2.50 consultation fee£2.50 consultation fee, plus further monthly feeof £20 paid in each month in which more than10 patients are seen.£1500 annual retainer£50 annual retainer then£2.00 consultation feeIt is also essential that local GPs endorse the <strong>scheme</strong> so that patients gainconfidence in the <strong>scheme</strong>.Key points• The patient information for the <strong>scheme</strong> should aim to manage patientexpectation.• GPs must endorse the <strong>scheme</strong> to encourage use by patients.Practical tipsAll the established <strong>scheme</strong>s expect patients to wait their turn in the‘prescription queue’.In Croydon pharmacists have been asked to train their counter staff that thevoucher is equivalent to a prescription.In South Sefton the patient passport and leaflets explain that in busy periodsthey may have to wait to see the pharmacist. The leaflet also explains thatpatients cannot demand medication and that the pharmacist must besatisfied that there is a need for medication.Appendix 16 contains examples of <strong>pharmacy</strong> claim forms.44 45
6.12 What about clinical governance?What is clinical governance?The Department of Health (DoH) defines clinical governance as “a frameworkthrough which NHS organisations are accountable for continuously improvingthe quality of their services and safeguarding high standards of care bycreating an environment in which excellence in clinical care can flourish”.The Royal Pharmaceutical Society of Great Britain (RPSGB) breaks clinicalgovernance into several elements:1. Clear lines of responsibility and accountability for the overall quality ofclinical care – all professionals are individually responsible for thequality of care they deliver.2. A comprehensive programme of quality improvement activities:Clinical auditContinuing professional development (CPD)Evidence based practiceResearch and developmentEffective monitoring of clinical care3. Policies aimed at managing risks – managing risk is essentially a twostageprocess:Risk assessment – which areas have the highest possibility of goingwrong? And which of those have the highest possibility of doingharm?Risk management – how can we reduce the likelihood of amistake?4. Procedures to identify and remedy poor performance – audit willhighlight sub-standard performance as will individual performanceappraisal.The Commission for Health Improvement (CHI) clinical governance reviewsfocus on the patient experience, strategic management capacity, healthimprovement and securing service delivery, together with the sevencomponents of clinical governance which are:1. patient, service user, carer and public involvement2. risk management3. clinical audit4. staffing and management5. education and training6. clinical effectiveness7. use of information.Note: from April 2004 the work currently undertaken by CHI will transfer tothe new inspection body, CHAI (Commission for Healthcare Audit andInspection).In order to ensure that the <strong>scheme</strong> has a robust clinical governance frameworkearly links should be formed with the clinical governance team, particularly the<strong>community</strong> <strong>pharmacy</strong> clinical governance facilitator.For any new service, there are a number of clinical governance elements for boththe PCT and the pharmacies providing the service to consider. For example, thestandards in part three ‘service specifications’ of Medicines Ethics and Practicestates that when providing any professional service pharmacists should ensurethat the tenets of clinical governance are followed:• That an identifiable pharmacist is accountable for all activitiesundertaken.• That they and staff providing services are suitably trained and competentto perform the tasks required.• That any necessary equipment and suitable facilities are available for theprovision of the service, and that these are maintained in good order.• That risk assessment and management procedures have been identifiedand are followed (for example, a complaints procedure in place, strictadherence to service protocols, robust patient referral systems).• That adequate records are maintained to enable the service to bemonitored (therefore <strong>community</strong> pharmacists must understand theimportance of recording their interventions).Professional IndemnityIt is essential that all extended role activities of <strong>community</strong> pharmacists arecovered by professional indemnity insurance. The Chemists DefenceAssociation (CDA) at the NPA will endeavour to provide cover to all itsmembers and their employees and any person or persons who may beengaged by members to provide a service or services. It is important that fulldetails of any <strong>scheme</strong>s are forwarded to CDA before commencement. Thiswill enable a risk evaluation to be calculated before confirmation is given thatcover will be provided. Contact CDA for further details at cda@npa.co.uk.A local mechanism to capture serious untoward incidents is an important part ofany clinical governance framework for a new service, particularly when theservice is delivered through a number of GP practices and pharmacies in a PCT.If the PCT does not establish a common reporting mechanism then it will not beable to identify (and remedy) common problems.Appendix 17 describes, in practical terms, what a robust clinical governanceframework is likely to mean for participating pharmacies.Appendix 18 contains a generic PCT checklist for establishing a robust clinicalgovernance framework for <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>s. This checklist could be usedto inform CHI clinical governance reviews.Key points• A robust clinical framework for the <strong>scheme</strong> is essential. The PCT shoulddevelop a checklist to ensure that a robust framework is established.Clinical governance is an essential element of any service in the NHS. It isimportant to be able to demonstrate the quality of a service, manage the riskswithin the service and to continually monitor a service to ensure that standardsare maintained or to improve the service where failures or lapses are identified.46 47
chapter sevenPractical tipsSeveral <strong>scheme</strong>s have established serious incident reporting frameworks aspart of the <strong>scheme</strong>, for example in Northumberland, Tyne & Wear (however,to date no adverse incidents have occurred).Appendix 19 contains examples of these local reporting mechanisms.Further reading• Further information on CHI clinical governance reviews at www.chi.nhs.uk/.• Anon. Clinical governance in <strong>community</strong> <strong>pharmacy</strong>: guidelines on good practice for theNHS. DoH 2001. Available atwww.doh.gov.uk/clinicalgovernance/<strong>community</strong><strong>pharmacy</strong>.htm.• Anon. Achieving excellence in <strong>pharmacy</strong> through clinical governance. RPSGB 1999.Available at www.rpsgb.org.uk/practice/clingov.htm.• Anon. Beyond the baseline: the role of clinical governance facilitators working with<strong>community</strong> pharmacists. RPSGB 2003. Available atwww.rpsgb.org.uk/practice/clingov.htm.• Anon. <strong>Implementing</strong> clinical governance in <strong>community</strong> <strong>pharmacy</strong> (in England): a localdevelopment plan. NPA 2002. Available at www.npa.co.uk.• Anon. PCT competency frameworks. NatPaCT 2003. Available at www.natpact.nhs.uk/.Audit the <strong>scheme</strong>Audit is the method used to monitor and continually improve the quality ofservices, hence it underpins the clinical governance framework.Figure 1 describes the audit cycle and Figure 2 describes the key points toconsider when designing an audit.Figure 1: The audit cycle• Select the topic• Set the criteria and standards. The criteria are what are beingmeasured, e.g. the number of people who visited the <strong>pharmacy</strong> fortreatment of their <strong>minor</strong> <strong>ailment</strong> who would have visited the GP practiceinstead. The standard describes the level of care to be achieved foreach criteria, e.g. 80% of people who attended the <strong>pharmacy</strong> wouldhave visited their GP instead• Set data collection rules• Collect the data• Analyse the data• Agree and implement change as necessary: there must be acommitment to change practice where the results of the audit showthat improvements should be made. This is where a lot of audits gowrong – the change process is poorly thought through or omittedentirely• Monitor progress by repeating the cycle.Adapted from:• Queensborough & Pruce. Managing antibiotic prescribing: audit handbook. NPC /RPSGB 2000. Available at www.npc.co.uk/.Figure 2: Designing the auditWhen designing the audit consider the following points:Who should be involved?The working group should be involved in developing and approving the audit.This step will help to increase the commitment of all participants.Consider who can advise on the process of audit. For example, nationalsources of advice (e.g. RPSGB clinical audit unit), local sources of advice(e.g. local clinical effectiveness unit).Clarify the audit question, criteria and standardsIdeally the audit question should help to support a PCT target. For examplethe audit question could be ‘How many patients using a <strong>minor</strong> <strong>ailment</strong><strong>scheme</strong> would have gone to see the GP instead?’The criteria would then be the number of people who visited the <strong>pharmacy</strong>for treatment of their <strong>minor</strong> <strong>ailment</strong> who would have visited the GP practiceinstead. The standard can then be set, for example 80% of people whoattended the <strong>pharmacy</strong> would have visited their GP instead.48 49
Information collectionWhat information will be collected? See monitoring outcomes on page 51.How will information be collected? Carefully considered data collectionmethods can simplify the audit process.Who will collect it? Does the PCT have experienced audit facilitators or dataclerks that can help?What should the sample size be?It may be more appropriate to use a sample to audit certain aspects of theservice, e.g. patient satisfaction. Discuss with local experts in audit the mostappropriate sample size to achieve a representative outcome. Not using toolarge a sample will also minimise effort and use of resources.What resources will be needed?Resources including finance, personnel and time should be identified.Do all the relevant healthcare professionals agree to taking part in theaudit?Taking part in audit could be one of the requirements in the local SLA.It essential that the health professionals required to collect the audit dataappreciate the benefits of audit and are provided with feedback on the auditdata.Monitoring implementation and outcomesAdapted from:• Cox & Mynors. Project evaluation toolkit. Medicines Partnership 2003. Available atwww.medicines-partnership.org.The objectives of the <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong> should be specific, measurable andachievable. The measures used to assess the impact of the <strong>scheme</strong> shouldrelate directly to these objectives.Examples of poor objectives include:• To increase patient satisfaction (not specific – satisfaction of what?)• To improve links between GPs and pharmacists (not measurable - howdo you measure links?)• To reduce GP consultations for <strong>minor</strong> <strong>ailment</strong>s by 90% (is thisachievable?)Collecting dataA quantitative approach will lead to outcomes that provide numerical data e.g.PACT data analysis across the PCT.A qualitative approach will lead to outcomes that provide verbal data, e.g. indepthinterview with a small sample of patients, in-depth questionnaire with asmall sample of <strong>community</strong> pharmacists and GPs. If questionnaires or interviewsare used they should include a mixture of closed and open questions. It iscommon practice to ask a number of closed questions first and then one or twoopen questions at the end.Have confidentiality arrangements been considered?Caldicott and data protection principles need to be adhered to. Consult withthe PCT Caldicott guardian, and the local research ethics committee (LREC).Type of questionDescriptionExampleShould the audit be piloted?It may be more appropriate to pilot the audit first as part of the <strong>scheme</strong> pilot.This will ensure that the question is easily understood and results inconsistent responses. Testing the data collection forms for consistency ofcompletion will result in a more valid data collection process.Adapted from:• Queensborough & Pruce. Managing antibiotic prescribing: audit handbook. NPC /RPSGB 2000. Available at www.npc.co.uk/.• Cox & Mynors. Project evaluation toolkit. Medicines Partnership 2003. Available atwww.medicines-partnership.org.ClosedPeople have a limitedchoice of responses,making it easier toquantify the data.How satisfied were youwith the service that the<strong>community</strong> pharmacistprovided? (please tickonly one):• Very satisfied• Fairly satisfied• Neutral• Fairly unsatisfied• Very unsatisfiedOpenAre much more difficultto quantify but sincerespondents will answerin their own words theyusually provide moredetailed information ofpeoples’ views.What other medicineswould you like yourpharmacist to provide?50 51
Which variables could be measured?Measurable variables fall into three main categories:InputsWhat your intervention involves and how it modifies standard patient care, forexample:The nature of the intervention and who it involves, e.g.• The number and type of patients involved: patient’s age, patient’sgender, the reason they are exempt from prescription charges, the <strong>minor</strong><strong>ailment</strong> they have.• How long the patient: professional interaction is.• How patients learned about the <strong>scheme</strong>.• What information was given to the patients during the <strong>pharmacy</strong>consultation.The cost of the interventionIt is very important to measure the costs of the intervention, for two reasons:• To evaluate the costs compared to the benefits.• To assess how feasible it would be to put the <strong>scheme</strong> into practice inother sites.OutputsThe immediate impact of the <strong>scheme</strong> on the patients and professionals, forexample:Patient and professional satisfaction with the <strong>scheme</strong>• When assessing satisfaction, it is better to ask multiple questions abouttheir satisfaction with different aspects of the intervention, rather thanjust one question about their overall satisfaction. Consider questionsaround the advantages and disadvantages of the new <strong>scheme</strong> comparedwith previous care.Level of prescribing• For example PACT data analysis.OutcomesThe longer term consequences of the <strong>scheme</strong> on health outcomes and cost, forexample:To assess patients changes in the use of services and the effect on the pattern ofconsultations• Number of GP visits, attendances at A&E.Key points• The working group should be involved in developing and approving theaudit. This step will help to increase the commitment of all participants.• The objectives of the <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong> should be specific,measurable and achievable. The measures used to assess the impact ofthe <strong>scheme</strong> should relate directly to these objectives. Consider whetherthese measures should be quantitative or qualitative or a mixture ofboth.• It essential that the health professionals required to collect the auditdata appreciate the benefits of audit and are provided with feedback onthe audit data.• There must be a commitment to change practice where the results ofthe audit show that improvements should be made.Practical tipsThere are a number of tools that can be used to collect data about a<strong>scheme</strong>, e.g. data from:Pharmacy prescription forms (appendix 14)Pharmacy claim forms (appendix 16)Surveys (appendix 20)Pharmacy record cards (appendix 21)Pharmacy monitoring forms (appendix 22)In the existing <strong>scheme</strong>s, the following data is collected for auditing andmonitoring purposes:Central DerbyQuantitativePACT data analysis: monitoring the number of items prescribed by GPpractices per quarter a year before the <strong>scheme</strong> started, and comparing it toquarterly PACT data analysis once the <strong>scheme</strong> had begun.QualitativeSurveys of GP, receptionist and pharmacist views.Eastern HullQuantitativeNumber of children aged 3 and under registered in the <strong>scheme</strong>.Pharmacy consultations per month: number and pattern.QualitativeSurvey of GP views: a focus group discussion was arranged to get feedbackfrom GPs in the area. This group work led to changes to the list of conditionscovered and medication supplied.Survey of <strong>pharmacy</strong> staff views: a meeting was arranged to look back overthe first 12 months of the <strong>scheme</strong> with pharmacists and their staff.52 53
chapter eightNorthumberland, Tyne & WearQuantitativePACT data analysis (prescribing cost and volume)Consultation ratesSupply of OTC medicinesQualitativeViews of professionals and patients: a key question in the patient survey isasking patients what they would have done if the <strong>scheme</strong> didn’t exist. This isa key question since it is important to determine whether the <strong>scheme</strong> ischanging patient behaviour. To date, over 80% of patients surveyed inNorthumberland, Tyne & Wear would have gone to see the GP instead.Sheffield Community Pharmacy Development UnitQuantitativePharmacy consultations: number and patternReferral routesMedicines prescribed by the pharmacistQualitativeViews of GPs, pharmacists and patientsFurther reading• Advice and resources from the RPSGB clinical audit unit at www.rpsgb.org.uk.• Queensborough & Pruce. Managing antibiotic prescribing: audit handbook. NPC /RPSGB 2000. Available at www.npc.co.uk/.• Cox & Mynors. Project evaluation toolkit. Medicines Partnership 2003. Available atwww.medicines-partnership.org.Build on the <strong>scheme</strong>In order to build on the success of a <strong>scheme</strong>:• Regular feedback should be supplied on the outcomes and progress ofthe <strong>scheme</strong>.• Patient education about the treatment of <strong>minor</strong> <strong>ailment</strong>s should beongoing in order to empower patients to take more responsibility for theirhealth.Regular feedbackThe reason for the variable effectiveness of audit and feedback is that often littleeffort is put into the all important change aspect of audit. The results of the auditwill identify whether there is a problem that needs addressing, but many peoplethink that audit ends after the data collection. The real work starts once the datacollection is complete.There is also no point in collecting and analysing data if the results are notpublicised and the learning shared. Mechanisms for feedback include:• Regular monitoring reports presented at board level• Public meetings• Newsletters• Local professional committees• PCT website• Local newspapers.Patient empowermentOngoing patient education about the treatment of <strong>minor</strong> <strong>ailment</strong>s is key toachieving sustainability of the <strong>scheme</strong>, and to making a real impact on patientcare.Key points• Feedback on achievements is important: changes made to improve the<strong>scheme</strong> should be publicised.• The key to achieving sustainability of the <strong>scheme</strong> and having a realimpact is to build on patient education and empowerment.How to influence change• Utilise audit and feedback with follow-up reviews to improveperformance.• Feedback should be ongoing and always includes specificrecommendations.54 55
summaryPractical tipsThe 14 month evaluation report from the Sheffield <strong>scheme</strong> is available todownload on the National Pharmaceutical Association website atwww.npa.co.uk. This is an excellent example of how a <strong>scheme</strong> can beevaluated, how the results can be presented and how an evaluation reportcan be written.Further reading• Advice and resources from the RPSGB clinical audit unit at www.rpsgb.org.uk.• Queensborough & Pruce. Managing antibiotic prescribing: audit handbook. NPC /RPSGB 2000. Available at www.npc.co.uk/.• Cox & Mynors. Project evaluation toolkit. Medicines Partnership 2003. Available atwww.medicines-partnership.org.• For further information on the Expert Patient Programme go towww.doh.gov.uk/cmo/progress/expertpatient/index.htm.A summary of key messages from existing <strong>scheme</strong>sStarting the <strong>scheme</strong>The key is to start small, learn the lessons and build. For example:• Start with 8-10 <strong>minor</strong> <strong>ailment</strong>s• Start in areas of deprivation• Start with one committed GP practice• Start with the <strong>minor</strong> <strong>ailment</strong>s that will produce the most dramatic transferof care from GP practices• Ensure there is a local champion who will drive the <strong>scheme</strong>. This personis not necessarily the project lead.Local ownershipLocal ownership of the <strong>scheme</strong> is very important:• Devise locally agreed <strong>minor</strong> illness protocols• Approach the GP practices and <strong>community</strong> pharmacists in person andget them involved from the start. Provide a lunch time meeting (withfood) so that everyone can have their say and feel they have someownership of the <strong>scheme</strong>.Education• Get all <strong>community</strong> pharmacists up to speed before starting• Brief GP surgeries one at a time.Communication• To stop patients feeling ‘fobbed off’ with a ‘second rate service’ it isessential that GPs are on board and giving positive messages about the<strong>scheme</strong>.AdvertisingGood publicity is key to making the <strong>scheme</strong> successful:• Develop high quality posters and leaflets• Clear branding of all leaflets and posters is important• Produce printed patient information leaflets that conform with DOHguidelines.• Advertise the <strong>scheme</strong> everywhere to ensure the target audience isreached. For example, libraries, newspapers, bill boards, schools.56 57
abbreviationsRunning the <strong>scheme</strong>• Ensure that a named individual is responsible and accountable for themanagement of the service – ideally this should be a project manager• Try to keep the paperwork for pharmacies as simple as possible• Ensure payments are made to the pharmacies on time• Ensure there is a very clear and unambiguous protocol and that it isbacked up with high quality paperwork and systems for processing theservice• Identify sustainable funding.List of abbreviationsA&E: Accident and emergencyCHAI: Commission for Healthcare Audit and InspectionCHI: Commission for Health ImprovementCPD: Continuing professional developmentAppendix 23 summarises the process followed in South Sefton PCTfollowing the Care at the Chemist <strong>scheme</strong>.As an example, the full set of protocols from the Hartlepool <strong>minor</strong> <strong>ailment</strong><strong>scheme</strong> is available to download from the NPA website at www.npa.co.uk.CPPE:DoH:GMS:LMC:LPC:LREC:NatPaCT:NPC:OTC:PAGB:PCT:PEC:PGD:PMR:POM:PPA:RPSGB:SHA:SLA:Centre for Pharmacy Postgraduate EducationDepartment of HealthGeneral medical servicesLocal medical committeeLocal pharmaceutical committeeLocal research ethics committeeNational Primary and Care Trust Development ProgrammeNational Prescribing CentreOver the counterProprietary Association of Great BritainPrimary Care TrustPCT executive committeePatient group directionPatient medication recordPrescription only medicinePrescription Pricing AuthorityRoyal Pharmaceutical Society of Great BritainStrategic Health AuthorityService level agreement58 59
appendices• Appendix 1:• Appendix 2:• Appendix 3:• Appendix 4:• Appendix 5:• Appendix 6:• Appendix 7:• Appendix 8:• Appendix 9:Example of recording form for collecting baseline dataExamples of project proposals / summariesGeneric list of competencies for <strong>community</strong> pharmaciesinvolved in providing a <strong>minor</strong> <strong>ailment</strong> serviceExamples of formulariesExamples of formulary protocolsExample of locum informationExample of <strong>pharmacy</strong> briefingExample of GP surgery protocolExamples of receptionist protocol• Appendix 10: Examples of <strong>pharmacy</strong> protocols• Appendix 11: Examples of service level agreements• Appendix 12: Examples of patient information• Appendix 13: Examples of how patients access the <strong>scheme</strong>s• Appendix 14: Examples of <strong>pharmacy</strong> prescription forms• Appendix 15: Examples of forms to communicate to the GP• Appendix 16: Examples of <strong>pharmacy</strong> claims forms• Appendix 17: Clinical governance implications for pharmaciesproviding a <strong>minor</strong> <strong>ailment</strong> service• Appendix 18: Generic checklist for establishing a robust clinicalgovernance framework for <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>s• Appendix 19: Examples of Serious Untoward Incident reporting forms• Appendix 20: Examples of patient surveys• Appendix 21: Examples of <strong>pharmacy</strong> record cards• Appendix 22: Examples of <strong>pharmacy</strong> monitoring forms• Appendix 23: Summary of the South Sefton PCT <strong>scheme</strong>DisclaimerThe National Pharmaceutical Association is not responsible for thecontent of the information contained within the appendices.6061
appendix 1appendix 2Example of recording form for collecting baseline dataEast Yorkshire PCTMINOR AILMENTS BASELINE DATAGP Receptionist NurseWeek Day Hayfever Headlice Sore throat Headache Cough / ColdMondayTuesdayWednesdayThursdayFridayExamples of project proposals / summariesPage 63-72 contains proposals, summaries and PEC papers fromCroydon, South Sefton and Hartlepool, respectively.Croydon Health AuthorityMinor Ailment ProjectProposal for joint working between General Practice and CommunityPharmacy on Minor Ailments1. Introduction and backgrounda) Doctors, pharmacists and nurses often see patients with <strong>minor</strong><strong>ailment</strong>s leading to various types of information and treatmentbeing given. It has been estimated that 40% of all GPconsultations are for <strong>minor</strong> <strong>ailment</strong>s. This puts a considerable timeburden on practice staff. A reduction of this burden could beachieved by transferring these consultations from the surgery tothe <strong>pharmacy</strong>.b) Exemption from prescription charges means that a visit to the GPis a matter of necessity for those whose income cannot stretch tothe cost of over the counter medicines for <strong>minor</strong> <strong>ailment</strong>s.2. Aim of this proposala) It is proposed to develop a <strong>scheme</strong> to offer a referral to a<strong>community</strong> pharmacist for eligible patients of a practice whocontact that practice with specific <strong>minor</strong> <strong>ailment</strong>s.b) The <strong>scheme</strong> should include:• Co-ordination and agreement of local policy on the treatment of<strong>minor</strong> <strong>ailment</strong>s.• Promotion of the <strong>scheme</strong> to all patients of the participatingpractice, who visit or telephone the surgery for repeat prescriptionsor ‘urgent’ same day appointments associated with the specified<strong>minor</strong> <strong>ailment</strong>s.• A reduction in the time between onset and treatment of symptoms,i.e. faster for patients.• A reduction in GP consultations should reduce surgery workloadbecause appropriate patients are re-directed to <strong>community</strong>pharmacies.• Development of the role of the pharmacist.• Two-way referral procedure.• Exploring the use of a voucher for the supply of medicines.6263
3. The objectivesa) Developing the quality and range of services in primary care by theprovision of a new service in Croydon.b) To investigate the viability of the use of <strong>community</strong> pharmacies tosupply medicines by the use of a medicines voucher.4. Pilot projecta) Initially surgeries located in New Addington and Shirley and thesurrounding pharmacies will be invited to participate in the project.5. Potential benefitsa) The clients of such a <strong>scheme</strong> should be able to access theappropriate treatment with the greatest confidence and leastwaiting time.b) The client will have access to uniform advice and treatmentindependent of whether they see the GP, practice nurse or<strong>community</strong> pharmacist.c) An agreed referral system would identify those patients in need ofthe greatest help.d) A closer professional relationship between practice staff andpharmacists should lead to sharing of experience and knowledgefor the benefit of all.e) Education of patients about self-care and the accessibility of<strong>community</strong> pharmacies for advice.f) A reduction in GP consultations for <strong>minor</strong> <strong>ailment</strong>s by theappropriate referral of patients to <strong>community</strong> pharmacists.6. Evaluationa) Minimal evaluation will be undertaken due to the comprehensivereports that have been published by Sefton Health Authority. Aone-week record of activity for baseline data will be collected.During the pilot project a structured interview will be arranged witha representative of each of the following groups:• GP• Pharmacist• Practice manager• Nurse practitioner• Receptionist• Pharmacy healthcare staff• Patient.7. Developing the proposala) A steering group for this project comprising representatives fromCroydon Health Authority, the LPC, practice staff and PCGpharmacists.• Pharmaceutical Adviser• Community Pharmacy Adviser• GP• PCG principal pharmacist• LPC representative• Practice manager• Practice nurse• Pharmacy representative• Walk-in centre lead nurseb) The success of the project depends upon the support of all thoselisted above.8. Proposed reimbursement and feesa) Overall project budget is £10,000 for six months only.b) Nine pharmacies are located within the proposed project areas.c) Project retention fee.d) A project retention fee of £200 will be paid to all <strong>community</strong>pharmacies that participate in the pilot project.d) Quarterly workload consultation fee.Croydon Health Authority on the receipt of the completed medicinevouchers will pay a fee quarterly in arrears to all participatingpharmacies; this will be on a sliding scale related to the workloadof the <strong>minor</strong> <strong>ailment</strong> project.1 – 20 consultations £10 61 – 80 consultations £4021 – 40 consultations £20 81 – 100 consultations £5041 – 60 consultations £30 100 + consultations £60e) Reimbursement of the drug cost.The completed vouchers are to be submitted to Croydon HealthAuthority monthly no later than five working days after the end ofthe month.a) Reimbursement will be the retail value of the original packs on theformulary or the cost of the item from the Drug Tariff price orChemist and Druggist price (worked up to a retail value bymultiplying by 1.7625).f) Prescription charge payments.Where a prescription charge has been received from a client a deductionwill be made against the total amount that is reimbursable.These proposals relate to the <strong>minor</strong> <strong>ailment</strong> project. When the Walk-inCentre is running they will be issuing vouchers for redemption in<strong>community</strong> pharmacies. These vouchers will be reimbursed at the retaildrug cost only.6465
A comparison of <strong>community</strong> pharmacist and GP management of<strong>minor</strong> <strong>ailment</strong>s: A feasibility studyBrief Summary for Sefton Health AuthorityRecent health policy has demonstrated support for transferring themanagement of <strong>minor</strong> <strong>ailment</strong>s away from GPs to other health careprofessionals. This is largely due to the perceived high level of selftreatableconditions being managed by GPs. Previous research hasdemonstrated that <strong>community</strong> pharmacists can and do manage <strong>minor</strong><strong>ailment</strong>s. However, patients exempt from the prescription charge areunable or unwilling to utilise the <strong>community</strong> <strong>pharmacy</strong> as they receivemedicines free from their GP. This study explores whether a shift inpatient demand for the pharmacist rather than the GP occurs when thisfinancial incentive is removed, with pharmacists providing medicines freeof charge to prescription exempt patients.The evaluation involved interviews with patients and practitioners toprovide insights into the acceptability of such a service. Those patientswho had utilised the <strong>pharmacy</strong> service were satisfied with theirconsultation. Interviewees were asked whether there were any acute, selflimitingconditions that they would prefer to consult the GP about. Manyfelt it depended on previous experience and the severity of the illness,with patients more likely to consult the GP with children, with symptomsthey had not previously experienced or where the severity of thesymptoms suggested something more serious. The GPs were positiveabout <strong>community</strong> pharmacists providing this type of service butsuggested there was still a role for GPs as <strong>community</strong> pharmacists maynot be able to meet all the patient’s needs. The <strong>community</strong> pharmacistsfelt that it was a good <strong>scheme</strong> for <strong>pharmacy</strong> and for patients, as they hadthe necessary skills to manage <strong>minor</strong> <strong>ailment</strong>s.In August 1999 the ‘Care at the Chemist’ trial was established as part of a10-month feasibility study to explore whether and to what extent anumber of different self-limiting conditions could be transferred fromgeneral practitioner to <strong>community</strong> pharmacist management. The trialinvolves one general medical practice and eight <strong>community</strong> pharmaciesranging from small independents to large multiples, in a sociallydisadvantaged area of Merseyside. Twelve conditions have been included,from coughs and colds to thrush. Under the trial the <strong>community</strong>pharmacist is able to advise patients on treatment and ‘prescribe’ suitableproducts from an agreed formulary. This model of service delivery isunique in that patients who are exempt from prescription chargescontinue to receive their medicines free when accessing treatmentthrough the <strong>pharmacy</strong>.Baseline data on GP management of <strong>minor</strong> <strong>ailment</strong>s and data from thetrial were analysed to address a number of questions. Data from the 16-week baseline period indicated that <strong>minor</strong> <strong>ailment</strong> consultationsaccounted for 8.9% of the GPs total caseload. The trial was evaluated forsix months during which 38% of all recorded <strong>minor</strong> <strong>ailment</strong> contacts weretransferred to the participating <strong>community</strong> pharmacies. While the trial didnot have an effect on the total number of consultations seen by the GPs,the composition of the caseload changed with significantly less <strong>minor</strong><strong>ailment</strong> consultations during the trial period (accounting for 6.6% of totalcaseload). There were no significant differences in re-consultation within14 days between those patients who initially consulted a GP and thosewho consulted the <strong>community</strong> pharmacist. There were differences in the<strong>minor</strong> <strong>ailment</strong>s seen by the different practitioners, with <strong>community</strong>pharmacists dealing with the majority of head lice (83%) and vaginalthrush (80%) consultations and GPs dealing with the majority of earache(88%), cough (88%) and upper respiratory tract infections (82%). Therewere some differences in patient characteristics, the average age ofpatients consulting a <strong>community</strong> pharmacist was 4 years younger thanthose consulting a GP (17.8 years compared to 21.8 years).6667
Hartlepool Primary Care TrustCommunity Pharmacy Minor Ailments SchemePurposeThe purpose of this paper is to provide a progress report on theCommunity Pharmacy Minor Ailments Scheme Pilot and to giveconsideration to commissioning the service across Hartlepool with effectfrom December 2003.BackgroundBetween 100 and 150 million GP consultations per year are for conditionsthat are potentially self-treatable (Lancet 343:1373-5), emergencyappointments are taken up by patients with <strong>minor</strong> <strong>ailment</strong>s and each GP’sworkload could be reduced by up to 16 consultations a day if selfmedicationwere encouraged in certain <strong>minor</strong> <strong>ailment</strong>s (Blenkinsopp A(2003)~ Community Pharmacy Minor Ailments Scheme).A Minor Ailments Scheme means transfer of patient care (under agreedprotocols) for a given number of conditions from the GP to the patient’schosen <strong>pharmacy</strong> so that• Access to treatment for patients is quicker and easier• GPs spend more time with those patients who really need to seethem• Medicines are used more appropriatelyBy establishing a Minor Ailments Scheme patients get quicker, easier andmore appropriate access to the support they need to look afterthemselves and GPs spend less time on conditions for which their input isnot needed.Such a <strong>scheme</strong> would help meet national targets around:• Primary Care Access• Helping patients get the best from their medicines• Improved patient choice and experience- service redesign aroundthe patient• Workforce modernisation agenda- specifically aims around ensuringhigh quality services and getting the most from professionals• Pharmacy in the FutureAnd local targets around:• Medicines Management Services (MMS) Collaborative objectives tobetter utilise the Community Pharmacists• Provision of medicines management services in environmentsconvenient to the patient• Wasted MedicinesCurrent PositionA six month Minor Ailments Scheme pilot commenced in May 2003 attwo of the MMS Collaborative practices (combined population of 21,500patients) utilising the five geographically nearest <strong>community</strong> pharmaciesto offer advice and/or treatment for 12 agreed <strong>minor</strong> <strong>ailment</strong>s.Patients exempt from NHS prescription charges are not charged for anytreatment required via the <strong>scheme</strong>.The service specification, agreed by the Prescribing Sub-committee andratified by the Clinical Governance Committee, includes• A well defined set of locally agreed <strong>ailment</strong>s• Simple evidence-based treatment protocols• Mechanisms to establish patient eligibility onto the <strong>scheme</strong>• An agreed medicines formulary• Agreed interventions from the pharmacist by way of advice, supplyor referral back to the GP• Documentation including incident reporting and complaintsprocedures.Following expressions of interest from neighbouring Primary Care Trusts,this service specification has been shared with Derwentside, Durham andChester i.e. Street, Langbaurgh and Middlesborough. A similar <strong>scheme</strong> isalready in operation at Easington PCT.Audit and Evaluation of the pilotQualitative evaluationQualitative evaluation included attitudinal surveys for patients, GPs,Practice Staff and Pharmacists.Interim evaluation shows that the majority of patients were referred to the<strong>scheme</strong> by their practice at the point when the patient was queryingappointment availability so it can confidently be reported that all practicereferrals in to the <strong>scheme</strong> would have resulted in a Nurse or GPconsultation. This can be supported by the patient survey which showsthat 94% patients treated via the <strong>scheme</strong> said that they would have madean appointment with their GP had the <strong>scheme</strong> not been available. Due todemand these appointment slots were refilled which means transferringthese patients to the <strong>pharmacy</strong> did not reduce the GP’s workload, theydid however improve access to the GP for other patients.The majority (81%) of patients had no need to visit their GP after receivingtreatment via the <strong>scheme</strong> which indicates successful treatment outcomesand the potential for moving the treatment of <strong>minor</strong> <strong>ailment</strong>s from the GPpractice to <strong>community</strong> <strong>pharmacy</strong>.6869
16% patients who did consult their GP gave two main reasons for thesecond consultation• 6% were unhappy about the 7 day treatment length for hay fever• 10% were unhappy with the treatment available for sore throatsPatient, GP and Pharmacist evaluation requested expanding the <strong>scheme</strong>to include the treatment of threadworm.Quantitative evaluation239 patients were treated during the first 12 weeks of the <strong>scheme</strong> and theaverage number of items per consultation was 1.18 with an average costper consultation of £6.10 (which includes the consultation fee).The nearest comparable data available for GP prescribing states that theaverage cost per GP prescribed item is £10.42 (DoH, Statistical BulletinJune 2002- Prescriptions dispensed in the Community), but this includesall prescribed medicines and not solely those used for the treatment of<strong>minor</strong> <strong>ailment</strong>s.It is fair to say that utilising the pharmacist to treat these <strong>minor</strong> <strong>ailment</strong>sappears to be cost-effective and offer good value for money.The pilot reimbursed the <strong>pharmacy</strong> at an agreed recommended retailprice for the medicine and paid a consultation fee of £1.50 per patient.Evaluation shows that this retail price was often higher than the <strong>pharmacy</strong>would charge for a sale of the same product given the large choice ofdifferent brands of the same medication. On the other hand, the £1.50consultation fee was considered to be a poor reflection of theprofessional time taken during the consultation and completing therequired documentation.Evaluation resultsFrom evaluation, amendments made to the pilot <strong>scheme</strong> include:• The treatment for Hay fever increased to 30 days supply• The treatment for sore throat extended to include dispersibleaspirin as an analgesic gargle• A protocol for the treatment of threadworm added to the servicespecification• Amendments to the payment scheduleDrug costs: Over the counter packs only to be supplied atChemist and Druggist cost price plus VATFee: £2.50 per consultationThese amendments will go to the Clinical Governance Sub-committee forratification prior to submission to the Professional and ExecutiveCommittee.FundingThe pilot was funded from MMS Collaborative monies.3 month ForecastEvaluation AnnualCostsTotal costs for 12 Minor Ailments in 2 GP practices(21,500 patients) £1,800 £7,200Total costs for 12 Minor Ailments across the PCT £29,000Annual prescribing costs for inclusion of threadworm £1,000Total £30,000The total cost of the pilot was £1,800 for the first 3 months which equatesto £7.2k annually. The pilot was available to approx 25% Hartlepoolpatients so roll out across the PCT is estimated at £29k.Extending the pilot to include the treatment of threadworm would add anadditional cost of £1k (Epact.net, GP prescribing data for financial year2002-2003)The total annual forecast for a Hartlepool Primary Care Trust MinorAilments Scheme is £30k.0.25 WTE Grade 4 Admin Support will be required to support the <strong>scheme</strong>at a cost of approx £4 -£5k which could be incorporated into the newPrimary Care Structure and has not been included in the estimatedforecast for the <strong>scheme</strong>.3 month ForecastEvaluation AnnualNumber ofConsultationsNumber of consultations for the 12 Minor Ailmentsfrom patients from the 2 GP practices (21,500 patients) 239 956Forecast number of consultations for 12 MinorAilments across the PCT 3824Additional forecast number of consultations fortreatment of threadworm 150Expected number of consultations 3974Extrapolating data from interim evaluation means the Primary Care Trustwould expect approx 4,000 consultations to be made via the <strong>scheme</strong>annually at a cost of £10k (£2.50 <strong>pharmacy</strong> consultation fee)Promotion and marketing of the <strong>scheme</strong> during the pilot was limited sincethe <strong>scheme</strong> was only available to patients from the two pilot practices.7071
appendix 3This meant that self-referral was a small percentage of the totalconsultations. With a PCT roll out programme and promotional campaign,transfer into the <strong>scheme</strong> is expected to be greater than during the pilot somay exceed 4,000 consultations per year. This would therefore increasethe consultation costs above £10k. This will be monitored by thePrescribing Sub-committee.4,000 consultations equates to approximately 0.7 WTE GP time saved.Options for consideration by the Professional and Executive Committeeare to:• Top slice £20k from the Prescribing Budget recognising the transferof prescribing costs from the GP to the <strong>minor</strong> <strong>ailment</strong>s <strong>scheme</strong> andsupport the <strong>scheme</strong> with £10k from monies for Primary CareAccess targets to cover consultation fees and administration costs• Include the funding of a Minor Ailments Scheme in the LocalDelivery Plan 2004/05 to support Primary Care Trust activitiesaround accessFor this financial year 2003/04, £11.5k (33% of the annual cost) willprovide the <strong>scheme</strong> across the Primary Care Trust from December 2003until March 2004. This equates to £6.5k prescribing fees and £5kconsultation and administration costs.Spread or roll-out of the <strong>scheme</strong>If funding is secured Practice staff, GPs and Pharmacists will be invited toa ‘spread’ event for training around the process of the <strong>scheme</strong> and thedocumentation/administration involved.A publicity campaign will be organised to raise awareness of the <strong>scheme</strong>to the people in Hartlepool using posters, patient information leaflets andlocal media.RecommendationsThe Professional and Executive Committee is requested to:• Note the detail in the Community Pharmacy Minor AilmentsScheme service specification• Receive the interim evaluation of the <strong>scheme</strong>• Consider the <strong>scheme</strong> for funding for December 2003 to March2004 and the following financial year 2004/05.Jayne ParkinsonProject Facilitator MMS Collaborative29 th September 2003Generic list of competencies for <strong>community</strong> pharmaciesinvolved in providing a <strong>minor</strong> <strong>ailment</strong> serviceThis is an example of a core competency framework which defines ingeneric terms the competencies that <strong>community</strong> pharmacists have, orneed to develop, to offer a <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>.Competency frameworks can be used to assist in recruiting <strong>community</strong>pharmacies to provide extended services, for performance review, and toidentify training and development needs of <strong>community</strong> <strong>pharmacy</strong> staffproviding extended services.Core competency framework for <strong>community</strong> pharmacists providingextended servicesAdapted from:• Anon. Community <strong>pharmacy</strong> medicines management: a resource pack for<strong>community</strong> pharmacists. The <strong>community</strong> <strong>pharmacy</strong> medicines managementproject 2003. Available at www.medicinesmanagement.org.uk/.Competence in information managementThe <strong>pharmacy</strong> will:• establish and maintain appropriate sources of information about<strong>minor</strong> <strong>ailment</strong>s and their treatment.• operate a protocol(s) for the sale of non-prescription medicines.• establish and maintain information on other local services relevantto the treatment of <strong>minor</strong> <strong>ailment</strong>s.• make a written record of the <strong>minor</strong> <strong>ailment</strong> consultation.• record the outcome of the <strong>minor</strong> <strong>ailment</strong> consultation in the PMR,as appropriate.• correctly process documentation of the <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>.• provide appropriate records for audit and evaluation purposes.Competence in communicationThe <strong>pharmacy</strong> will:• elicit key information for the treatment of <strong>minor</strong> <strong>ailment</strong>s by the useof appropriate questions.• provide information and advice in a manner appropriate to theneeds of the patient.Competence in problem-solvingThe <strong>pharmacy</strong> will:• recognise and define actual or potential problems in the patient’sdrug therapy, life style or quality of life related to the treatment ofthat <strong>minor</strong> <strong>ailment</strong>.• identify the best option for the treatment of the <strong>minor</strong> <strong>ailment</strong>,based on appropriate evidence and sound analysis, and takingaccount of the patient’s wishes.7273
• when necessary refer the patient to a more appropriate source ofhelp or information.• take responsibility for, and accept the outcomes of, own profferedadvice or decisions for <strong>minor</strong> <strong>ailment</strong>s.Competence in working with othersThe <strong>pharmacy</strong> will:• contribute to the <strong>scheme</strong> in accordance with the law, with theRPSGB Code of Ethics and with other relevant codes of conduct orpractice, including systems for clinical governance.• respect and observe patient confidentiality.• negotiate successfully with GPs and their staff if any problemsarise.• operate across the <strong>community</strong> <strong>pharmacy</strong>: primary care interface insupport of the management of <strong>minor</strong> <strong>ailment</strong>s.• behave in a manner which instils confidence of others involved inthe treatment of <strong>minor</strong> <strong>ailment</strong>s, especially the patient.• support, collaborate with, delegate to, and supervise other teammembers in an appropriate manner for the treatment of <strong>minor</strong><strong>ailment</strong>s.• use knowledge and skills effectively to help the learning of otherteam members about the treatment of <strong>minor</strong> <strong>ailment</strong>s.• encourage the patient to ask questions about his/her condition andtreatment.• explain clearly to the patient the benefits of and rationale for his/herproposed medicine.• identify factors which might discourage or prevent the patient fromtaking the medication regimen and seek to remove or amelioratethose factors by simple practical measures or suggestions of aclinical or non-clinical nature.Competence in achieving a healthier lifestyle and higher quality of lifeThe <strong>pharmacy</strong> will:• help the patient to recognise any clear need for change in his/herlifestyle for reduced risk of ill-health.• use opportunities to promote and support the patient’s healthierlifestyle.Competence in personal skills developmentThe <strong>pharmacy</strong> will:• recognise personal and professional limitations in respect of <strong>minor</strong><strong>ailment</strong>s.• identify and prioritise the <strong>pharmacy</strong> staffs’ learning anddevelopment needs for <strong>minor</strong> <strong>ailment</strong>s management.• develop plans with learning objectives to meet identified needs forthe treatment of <strong>minor</strong> <strong>ailment</strong>s.• use learning and development opportunities, including those of andfrom work-based experience, in support of <strong>minor</strong> <strong>ailment</strong>smanagement.• records learning activities relevant to <strong>minor</strong> <strong>ailment</strong>s management.• evaluate if learning objectives were met and identify further learningneeds for <strong>minor</strong> <strong>ailment</strong>s management.• apply learning to practice of <strong>minor</strong> <strong>ailment</strong>s management.Competence in achieving concordance in drug therapyThe <strong>pharmacy</strong> will:• elicit, listen to, respect and reflect the patient’s perceptions ofhis/her condition and addresses his/her concerns about his/hermedicines or about taking them.7475
appendix 4Examples of formulariesNote: in addition to the example below from Croydon the followingformulary lists can be downloaded from the National PharmaceuticalAssociation website at www.npa.co.uk :• South Sefton PCT• Northumberland, Tyne & Wear SHACroydon Primary Care Trust Formulary – For Minor Ailment ReferralsViral upper respiratory tract infection• Paracetamol tablets (32 tablets)• Paracetamol liquid (Calpol suspension 70ml)• Ibuprofen tablets 200mg (24 tablets)• Ibuprofen tablets 400mg (24 tablets)• Ibuprofen suspension• Xylometazoline nasal drops 0.1% (Otrivine brand)• Xylometazoline nasal drops 0.05% (Otrivine brand)• Xylometazoline nasal spray 0.1% (Otrivine brand)• Pseudoephedrine tablets (Sudafed 12 tablets)• Pseudoephedrine liquid (Sudafed 100ml)• Saline nasal drops (1 x 10ml)• Menthol and eucalyptus inhalation (1 x 100ml)Cough• Pholcodine linctus (200ml SF when necessary)• Simple linctus (100 or 200ml SF when necessary)• Simple linctus paed (100 or 200ml SF when necessary)• Ammonia and ipecacuanha mixture (500ml or smaller if you canobtain it)Fever• Paracetamol tablets (32 tablets)• Paracetamol liquid (Calpol suspension 70ml)• Ibuprofen tablets 200mg (24 tablets)• Ibuprofen tablets 400mg (24 tablets)Hayfever• Chlorphenamine (Chlorpheniramine) tablets (30 tablets Piriton))• Chlorphenamine (Chlorpheniramine ) liquid 1 x 150ml• Loratidine tablets (1x 7 Clarityn tablets)• Sodium cromoglycate eye drops 1 x 5ml (Opticrom drops)• Beclomethasone nasal spray 1 x 100 dose (Beconase nasal spray)Diarrhoea & vomiting• Loperamide capsules (Imodium capsules 1 x 8)• Oral re-hydration therapy 1 x 6 sachets (Dioralyte sachets 1 x 6 anyflavour)Headache• Paracetamol tablets (32 tablets)• Paracetamol liquid (Calpol suspension 1 x 70ml)• Ibuprofen tablets 200mg (24 tablets)• Ibuprofen tablets 400mg (24 tablets)• Paracetamol and codeine tablets (Co-codamol 32 tablets)Back pain• Paracetamol tablets (32 tablets)• Ibuprofen tablets 200mg (24 tablets)• Ibuprofen tablets 400mg (24 tablets)Soft tissue injury• Paracetamol tablets (32 tablets)• Ibuprofen tablets 200mg (24 tablets)• Ibuprofen tablets 400mg (24 tablets)• Tubular bandage (Tubigrip 0.5m Sizes B, C, D, E, F & G)Sore throat• Soluble Paracetamol tablets (Panadol 20 tablets)• Ibuprofen tablets 200mg (24 tablets)• Ibuprofen tablets 400mg (24 tablets)• Ultra Chloraseptic spray (1 x 15ml)Athlete’s foot• Miconazole cream 1 x 30g (Daktarin cream 1 x 30g)• Clotrimazole solution 1 x 20ml (Canesten solution)Head lice• Suleo M lotion (1 x 50ml)• Derbac M solution (1 x 50ml)• Lyclear crème rinse (1 x 59ml)7677
appendix 5Vaginal thrush• Clotrimazole pessary (1 x original pack) (Canestan 1)• Clotrimazole 1% cream (1 x 20g) (Canestan)• Clotrimazole combi (1 x original pack) (Canestan)• Fluconazole capsule (1 capsule) (Diflucan 1)• Clotrimazole Once cream (1 x 5g) (Canestan)Examples of formulary protocolsNote: in addition to the protocols from Central Derby and Croydon onpage 80-82 the following <strong>community</strong> <strong>pharmacy</strong> protocols can bedownloaded from the National Pharmaceutical Association website atwww.npa.co.uk :Contact dermatitis, bites and stings• Hydrocortisone cream 1% (1 x 15g)CroydonAtheletes footCentral DerbyCoughSheffield CommunityPharmacy DevelopmentUnitTeething and mouth ulcers• Bonjela (1 x 15g)Bites and stingsViral URTIContact dermatitisDiarrhoeaCoughFeverHayfeverHeadacheHeadliceMouth ulcersSoft tissueNon traumatic back painSore throatSore throatHeadache/earache/temperatureNasal congestionHayfeverHeadliceIndigestion/heartburn/tummy upsetDiarrhoeaCoughSore throatHeadache/earache/temperatureNasal congestionHayfeverHeadliceIndigestion/heartburn/tummy upsetDiarrhoeaConstipationThrushTeethingVaginal thrush7879
Croydon primary care trust viral URT infection protocolCroydon primary care trust headlice protocolDefinitionHow common is it?Description of symptomsAdvice to be givenOTC medicationCold and Influenza• Very common. Children are more at riskto developing upper respiratory tractinfections.• There are over 1000 types of cold virus 1 .• A collection of symptoms including cough(dry or productive) with or without pain ortemperature.• Runny or blocked nasal cavity.• Give palliative treatment for symptoms.• Rest if symptoms are severe.• Drink plenty of non-alcoholic fluids.Paracetamol tabs or liquid, Ibuprofen tabs,Xylometazoline (
appendix 6Pharmacy FirstExample of locum informationCentral Derby Primary Care TrustCONSTIPATIONDefinition/CriteriaIncreased difficulty and reduced frequency of bowel evacuation compared to normalCriteria for INCLUSIONSignificant variation from normal bowel evacuation which has not improved followingadjustments to diet and other lifestyle activities (see below)Criteria for conditional EXCLUSIONPatients currently receiving laxatives as part of their regular medication. Pharmacistsshould exercise their professional judgment to implement dosage alteration to existinglaxative regimeAction for excluded patients & non-complying patientsReferral to General PractitionerReferral to Health Visitor for Children and BabiesRecommended Treatments, Route and Legal status. Frequency of administration& maximum dosageSenna tabs (20) po P 2 onFybogel (10) po P 1 bdFollow-up & adviceRegular doses of laxatives are rarely required and can cause a “lazy” bowelConsider alteration to diet to prevent the occurrence of further events eg.increasedfibreAnd fluid intake and increased physical activity if appropriateSenna should not be used in pregnancySide effects and their managementIf dosage is too large, griping and diarrhoea may resultSenna may colour the urine yellow or redWhen & how to refer to GPConditional referral:• If constipation persists beyond one week, consult the GP• If more than one request per monthConsider supply, but patient should be advised to make an appointment to seethe GP:• Patients taking medication with recognised constipating effectsCare at theChemistLOCUM GUIDEThe Care at the Chemist <strong>scheme</strong> allowsparticipating pharmacies to supplycertain medication on a <strong>pharmacy</strong>prescription form to patients registeredwith a South Sefton GP.The <strong>pharmacy</strong> may supply any of themedication listed in the formulary forthose stated conditions. The medicationmay only be supplied in accordance withits OTC product licence.Medication may not be supplied for anyother condition other than thoselisted even though the product islicensed for such use.Normal Prescription Charges andExemptions Apply8283
Please ensure that• The patient has a Care at the Chemist Passportor is issued with one once registration with aparticipating Bootle and Litherland GP has beenconfirmed.• The prescription form is completed on BOTHsides.• An entry is made onto the Monthly Claims Form.Passports ??How ??To use the <strong>scheme</strong> the patientmust have a passport, or be issuedwith one. It acts as a record cardand lists the medication suppliedthrough the <strong>scheme</strong>You can supply any of themedication listed for any of theconditions. Label medication as if itwere being supplied on FP10 andensure a record is made in thePMRThe yellowbookNormalprescriptionexemptionsand chargesapply• An entry into the Care at the Chemist Passportis made.• Any prescription levy is collected.• Any medication supplied is labeled in the normalway.When not tosupply ??There are no real limits on thefrequency of supply. Use yourprofessional judgment. Generally ifthe medication has been suppliedon two previous occasions in thelast month, referral may berequired. Obvious exemptionsinclude hay fever medicines.Don’t supplythrough the<strong>scheme</strong> if youwouldn’t sellthe product !What is it ??For further information contactAlan Cummings on 0151 920 5056Over ViewThe <strong>scheme</strong> provides treatment forcertain <strong>ailment</strong>s from pharmaciesas if they were on an FP10See monthlyclaims formPaperwork ??Each patient should have apassport.Any passports issued must berecorded on the log form. At eachsupply make an entry on/in• The PMR• The Passport• Monthly claim formIt looks like alot but it’squite simple.Pleaseensure it iscompleted orpayment willnot be made.Who ??Any patient registered with aparticipating South Sefton GPA list hasbeen faxed tothe <strong>pharmacy</strong>Where ??When ??Any participating <strong>pharmacy</strong>Any time the <strong>pharmacy</strong> is open. Noneed to see a GP firstYou’re inone !Complete the FPPharm (Both sides)84 85
appendix 7appendix 8Example of <strong>pharmacy</strong> briefingExample of GP surgery protocolCARE AT THE CHEMISTCommon QuestionsQ. Who can use the service?A. Any patient registered with any South Sefton PCT GP. This includeschildren and the elderly. Children under 16 must be issued with their ownpassport and the parent/guardian must sign on their behalf. The parent orguardian must accompany the child on each occasion they wish toaccess the <strong>scheme</strong>.Q. What medicines can I use to treat which <strong>ailment</strong>s?A. The list of medicines and <strong>ailment</strong>s will change from time to time.These are detailed on the monthly claims form. No other <strong>ailment</strong> istreatable through the <strong>scheme</strong> even if a suitable medicine is available foranother condition.Q. Does the patient have to pay for advice only if they pay aprescription charge?A. No. Simply complete the reverse of the prescription as normal. Write“advice only” in amount paid box. This will still count towards the totalnumber of items dispensed in a month. No levy will be deducted.Q. Can patients demand the medicines available for the conditionstreatable?A. No. You are under no obligation to supply any of the productsavailable if you feel they are inappropriate for a particular patient or youthink a referral is required.Q. How much will I be paid?A. Payments will be £1.50 per item supplied. If advice only is given then£1.50 will be paid. You will be reimbursed your drug costs at DT or C+Dprice, less a discount of 8% + VAT. A container fee of 4p per item will alsobe paid.Croydon Primary Care TrustSurgery Procedure for using the Minor Ailment Pharmacist AdviceRequestNote: Only medicines on the agreed list can be written on the voucher.• Individually numbered vouchers, in pads of 50, will be distributed tothe participating Surgeries. The vouchers will be white (top copy)and yellow (bottom copy) in colour.• The top copy of the completed voucher will given to the patient, theduplicate copy will be stored, in the appropriate locked place, bythe Surgery for reference and audit purposes.1. Role of the referring person• Complete the name, address and date of birth for the person youare giving the voucher to.• Complete the sections requesting your name the GP practice andthe date of referral.• Ensure that the patient is aware that the pharmacist will need toask some questions of the patient to satisfy their professionalobligations regarding the selection of an appropriate treatment.• Hand the top copy of the voucher to the patient and file the bottomcopy in the appropriate locked place. When the pad of vouchersare not in use they should be stored in a locked/secure place.• Inform the patient that only certain pharmacies in CroydonPrimary Care Trust area can supply the medicines on thevoucher.• Ensure that the patient realises that the voucher has to bepresented at the <strong>pharmacy</strong> within five days of the date of issue.If a voucher is presented to the <strong>pharmacy</strong> that is more than 5 daysold then the pharmacist will refer the patient back to the surgery. Ifthe patient doesn’t wish to do this, the pharmacist may sell thepatient a suitable product.• The pharmacist will complete the point of dispensing check onexemption from prescription charges as they do for all other NHSprescriptions. If evidence cannot be shown the medicine will stillbe provided free of charge and checks will be made at a laterstage. Please remind patients that they will need to show evidenceof their exemption from prescription charges at the <strong>pharmacy</strong>.• If the patient has to pay a prescription charge the pharmacist maysell the medicine to the patient if it is cheaper. The Voucher will stillbe returned to the PCT for auditing purposes and payment of theconsultation fee.• Please ignore all non-shaded sections on the voucher as these arefor the pharmacist to use.8687
appendix 9• The Community pharmacist may contact you to clarify any details onthe Voucher if this is needed.• If you have any questions about how to use the vouchers pleasecontact Helen Hill or Rena Amin at Croydon PCT on Tel 020 84013900 in the first instance.• To obtain a further supply of vouchers please contact Ian Murie(details as above).2. Role of the PCT / co-ordinator in processing completed vouchers.• Check that the voucher has been completed satisfactorily andobtain any missing information.• Agree the appropriate reimbursements to the pharmacist in eachcase and make arrangements for payment.Examples of receptionist protocolsNote: in addition to the protocol from Central Derby below the followingreceptionist protocols can be downloaded from the NationalPharmaceutical Association website at www.npa.co.uk :• Sheffield Community Pharmacy Development UnitPharmacy FirstCentral Derby Primary Care TrustReception ProtocolThis protocol is for use by all persons dealing with requests forappointments and/or prescriptions either by the patient in person or bytelephone.For patients making an appointment by telephone or in person1. If the patient is telephoning a request ask patient verbally if it is forone of the <strong>minor</strong> illnesses included in the <strong>scheme</strong>.2. If the patient is presenting in person show them the laminated list ofincluded illnesses asking if it is for one of the listed illnesses.3. Inform them that there is a new <strong>scheme</strong> in operation called PharmacyFirst. Patients can be referred to a local <strong>pharmacy</strong> for advice and amedicine rather than waiting for an appointment. If the patient isexempt from prescription charges then the medicines will be free. Ifthe patient pays for prescriptions the patient can go to the <strong>pharmacy</strong>and purchase a medicine in the normal way (this will usually be lessthan a prescription charge).4. If the patient is present and accepts transfer into the <strong>scheme</strong> pleasecomplete a booklet with their details and the practice stamp and askthem to present this at the <strong>pharmacy</strong>. Patients who pay for theirmedication will not need a booklet. For patients who go to the<strong>pharmacy</strong> following a telephone request, if they are not known to the<strong>pharmacy</strong> they will need to prove that they are eligible for the <strong>scheme</strong>by taking some form of identification and proof of GP registration withthem. Each patient should receive a Pharmacy First informationleaflet.5. Following transfer into Pharmacy First it is good practice to record inthe patient’s notes or computer record.6. If a patient refuses transfer into Pharmacy First an appointmentshould be made for them with the Doctor in the usual manner.For patients self-referring at the PharmacyThe pharmacist is required to confirm their identification and registrationwith your surgery. If the pharmacist does not know the patient or have aprevious prescription record for them then they may ring the surgery tocheck their registration. Please cooperate with these requests.Rapid referralOn some occasions the Pharmacist may consider that the patient needsto be seen by a doctor. The urgency will depend on the symptoms. Inthese circumstances the Pharmacist will ring to make an appointment onthe patient’s behalf or advise the patient to make an appointment.Sometimes if the surgery is closed the Pharmacist may advise the patientto call the emergency number or go straight to A & E.8889
appendix 10Examples of <strong>pharmacy</strong> protocolsNote: in addition to the protocol below from Croydon the followingprotocols can be downloaded from the National PharmaceuticalAssociation website at www.npa.co.uk :• Eastern Hull PCTCroydon Primary Care TrustPharmacy Procedures for handling the Minor Ailment PharmacistAdvice RequestNote: Only medicines listed on the Minor Ailments Formulary can besupplied using this form.• Individually numbered vouchers, in pads of 50, will be distributed tothe participating Surgeries. The vouchers will be white in colour.• The top copy of the completed voucher will be given to the client, theduplicate copy will be stored by the Surgery for reference and auditpurposes.• The referring person will complete the shaded section of the form.Please ask the client to complete the right hand side of the voucheras they would normally. If they are not willing to show evidence ofexemption or are unable to produce the evidence, then mark it as“evidence of exemption not seen”.Role of the pharmacist• The client presenting a Minor Ailment Pharmacist Advice Requestmust be seen by the Pharmacist.• Ensure that the voucher has been presented at the <strong>pharmacy</strong> withinfive days of the date of issue. If a voucher is presented that is morethan 5 days old refer the client back to the Surgery. If the client iswilling you could also sell them an appropriate item. Please take theVoucher from the client and mark it as received but out of date andreturn to the Primary Care Trust (PCT) as normal.• During the consultation with the client complete the symptomsreported section. After an agreement has been reached about thetreatment for the client complete the next section on the voucher.• If a medicine is to be supplied via the voucher complete the nextsection detailing its name and quantity (refer to the Formulary if indoubt as these are the only medicines that will be reimbursed).• Ask the client to sign the declaration on the right hand side of theTreatment Voucher. Reimbursement of the pharmacist for the cost ofthe product will be dependent on the submission of a fully completedvoucher and declaration.• The point of dispensing check on exemption should be completed asit is for all other NHS prescription forms. If evidence cannot beshown the medicine should still be provided free of charge. Mark oneof the boxes on the bottom right hand side of the Treatment Voucherto declare whether evidence of exemption has been seen.• If the client has to pay a prescription charge take this money or sellthe medicine to the patient if it is cheaper. If you sell an item pleasemark the paid box with the exact amount that the client paid. Thetreatment Voucher will need to be returned to the Finance DepartmentCroydon PCT for auditing purposes even if the patient purchases anitem over the counter.• Please complete the lower parts of the voucher by adding your name,signature, <strong>pharmacy</strong> stamp and date of supply and ask the patient tosign to say they have received the medication or advice.• Guidance from the RPSGB indicates that the Voucher should behandled the same as sales of [P] medicines, therefore you shouldensure that you carry out all of your professional responsibilities. Thepharmacist should see all clients presenting a Voucher. Please handlethe Voucher in the same way that you would a prescription for thepurposes of dispensing and counselling the client. When handingover the item please ask them to sign the declaration on the left-handside to say they have received the medication.• Return the Treatment Vouchers to the Finance Department at CroydonPCT by the 10 th day of the month proceeding the month in which thesupply was made.• If it is required the patient can be rapidly referred back to the surgeryusing the Rapid Referral Request Form. It is essential that the timescale for the referral is completed on the form.• If you have any further questions regarding the administration of theTreatment Vouchers in the Community Pharmacy please contactHelen Hill or Rena Amin at Croydon PCT on Telephone 020 8401 3900• To request a further supply of the referral to surgery forms pleasecontact Helen Hill (details as above).Role of the <strong>pharmacy</strong> assistants• To alert the pharmacist that the client is presenting a Minor AilmentPharmacist Advice Request form that can only be dealt with by thepharmacist.Role of the PCT / co-ordinator in processing completed vouchers• Check that the voucher has been completed satisfactorily and obtainany missing information.• Agree the appropriate reimbursements to the pharmacist in each caseand make arrangements for payment.• Reimbursement will be the cost of an item from the Drug Tariff price(worked up to a retail value by multiplying by 1.7625) or the Chemistand Druggist price for branded items on the agreed list.9091
appendix 11Examples of service level agreementsNote: in addition to the service level agreements from Central Derby, EastYorkshire and Newcastle on page 93-103 the following agreements canbe downloaded from the National Pharmaceutical Association website atwww.npa.co.uk :• South Sefton PCT• Sheffield Community Pharmacy Development UnitPharmacy FirstCentral Derby Primary Care TrustService Specification1. Introduction1.1 This service is available to all patients exempt from prescriptioncharges registered with the surgeries participating in the <strong>scheme</strong>.Patients are at liberty to refuse this service. Patients who pay fortheir prescriptions should be referred to a <strong>pharmacy</strong> to purchasemedicines in the usual way.1.2 The service is only available for the identified <strong>minor</strong> illnesses.1.3 Only Community Pharmacies who are committed to making staffavailable to provide the service and who have successfullycompleted the appropriate training will be included in PharmacyFirst, for the treatment of <strong>minor</strong> illness service with Central DerbyPrimary Care Trust.2. Transfer of care2.1 Patients presenting with identified symptoms at the GP surgerywill be offered transfer into this service. Patients may also selfrefer.2.2 Patients presenting at a participating Community Pharmacyregistered with a participating GP will receive the service level ofcare as laid out in this specification.2.3 Patients wishing to access the service must present identificationand reasonable proof of registration with a participating practice.This can bea NHS cardb Pharmacy Card appropriately stamped by practice or a<strong>pharmacy</strong>c Be registered on <strong>pharmacy</strong> PMS system and known to thepharmacist.2.4 If registration with a participating practice is in doubt the patientwill not be eligible for this <strong>scheme</strong> and they will be advised toaccess medical care through the normal channels.3. Duties of participating surgeries3.1 All patients requesting appointments (either immediately or on anappointment basis) for symptoms matching the criteria identifiedcan be offered transfer into the service.3.2 Patients presenting in person, accepting transfer should be issuedwith a booklet stamped by the practice for presentation at aparticipating Community Pharmacy, a service information leafletand a list of participating Pharmacies.9293
3.3 Patients accepting transfer by phone will be advised to takeevidence of identity and registration to one of the participatingpharmacies. In the absence of an NHS card or <strong>pharmacy</strong> card the<strong>pharmacy</strong> may telephone the surgery to confirm registration.3.4 All surgeries should co-operate and liaise with CommunityPharmacists to activate the rapid referral procedure whenrequired.3.5 All participating GP surgeries should display official posters andprovide leaflets promoting the service.3.6 For patients under the age of 16 the parent/guardian can accepttransfer into the <strong>scheme</strong> on behalf of the patient.3.7 Practices may decide on their own restrictions and referral criteriabut must make this known to the service coordinator.4. Duties of participating accredited <strong>community</strong> pharmacists4.1 Patients should only be accepted into the service if thepharmacist can confirm their identity and has reasonable proofof registration with a participating GP.4.2 All participating Pharmacies will provide a professionalconsultation service for patients registered with participatingGPs who present with one of the specified conditions.4.3 The Pharmacist or appropriate member of staff will assess thepatient’s condition. The consultation will consist of4.3.1 Patient assessment by qualified member of staff4.3.2 Provision of advice4.3.3 Provision of a medication, only if necessary, from theagreed formulary appropriate to the patients condition4.3.4 Either complete a new <strong>pharmacy</strong> card or make an entryonto existing Card. Patients should be encouraged tohold only one card4.3.5 FPPharm (pharmacists prescription) shall be completed.4.4 Normal rules of patient confidentiality apply.4.5 The Pharmacist should ensure that the patient has completedand signed the declaration of exemption of Prescription charges(on reverse of FPPharm).4.6 It is appropriate to record the supply on the Pharmacy PMRsystem.4.7 Implementation of the rapid referral process if symptoms meetagreed criteria4.8 If a patient presents more than twice within any month withthe same symptoms the patients should be referred to theirsurgery, and unless the symptoms meet the criteria for a rapidreferral the patients should be advised to make an appointmentin the normal manner. The pharmacist should mark the card tothis effect.4.9 If the pharmacist suspects that the patient and/or parent isabusing the <strong>scheme</strong> they should alert the PCT pharmacist orservice co-ordinator.4.10 Pharmacies will be required to complete a monthly summarysheet for each participating surgery and submit the FPPharmsattached to this sheet.4.11 Rapid referral procedure- If the patient presents withsymptoms indicating the need for an immediate consultationwith the GP, the pharmacist should ring the surgery and make anappointment for the patient within the appropriate time frame.If the surgery is closed and/or the symptoms are sufficientlysevere the patient should be advised to contact the on-calldoctor or attend A & E immediately.5. Service funding and payment mechanismThe Pharmacy will be paid according to the following schedule5.1 Annual retainer fee £50.005.2 Fee per consultation £2.505.3 Drug costs at drug tariff/agreed cost pricesThe summary recording forms with relevant FPPharms attached shouldbe returned to the PCT office as soon as possible after the end of themonth. Payments will be made to the participating <strong>pharmacy</strong> by chequeor BACS approximately two weeks later. Pharmacists are advised toretain a copy of the summary forms. Retaining copies of the FPPharms isoptional.6. Monitoring and evaluationParticipating pharmacies and surgeries will be expected to participate inmonitoring and evaluation to show:6.1 Changes to GP prescribing data both costs and volume6.2 Cost and volume of Pharmacy prescribing6.3 Impact on GP appointments and time6.4 Attitudinal survey ofa GPsb Receptionistsc Pharmacistsd Patients9495
East Yorkshire Primary Care TrustService Level AgreementForTreatment of Minor Ailments by a Community Pharmacy usingThe Pharmacy Link Scheme1. Parties to the AgreementThis agreement is between:5.3 Payment MethodPayment will be paid monthly in arrears (on receipt of acompleted monthly summary and white copies of the patientforms) by BACS from the PCT direct into the bank account of the<strong>pharmacy</strong>.BankAddress……………………………………………….....…………… (“The Pharmacy”)And East Yorkshire Primary Care Trust (“The PCT”)Sort CodeAccount Number2. Purpose of the AgreementThis agreement relates to a <strong>scheme</strong> for the supply of medicines and/oradvice using The Pharmacy Link Scheme. The PCT will manage the<strong>scheme</strong> subject to the provisions of paragraph 4 (“Obligations of thePharmacy and PCT”).3. Agreement Period3.1 The agreement will commence on 16 th June 2003 and extend fora period of 9 months.3.2 It will be subject to renewal if agreed by all parties.3.3 The agreement may be terminated, without penalty, if thePharmacy or PCT give the other party three months notice inwriting.4. Obligations of the Pharmacy and PCT4.1 The Pharmacy must provide the service in accordance with theService Specification (Page 4 of Pharmacy Link OperationalProcedure)4.2 The PCT will manage the <strong>scheme</strong> in accordance with the ServiceSpecification.5. Terms and Fees5.1 Payment for Consultation and Drug ReimbursementAn annual retainer fee of £50 will be paid.A £2 Consultation fee will be paid for each consultation at thePharmacy.5.2 Payment for Medicines SuppliedThe Pharmacy will be reimbursed for medicines supplied at thedrug tariff or cost price plus VAT as detailed in operationalprocedure dated June 2003.5.4 Payment TermsA fully completed monthly summary sheet (with white copies ofthe prescription sheets attached) must be submitted monthly bythe Pharmacy to Marie Hancock, MMS Facilitator at EastYorkshire PCT, Health House, Willerby, Hull who will makepayments from PCT funds as appropriate.6. Confidentiality6.1 The Pharmacists and their staff must not disclose to any personother than a person authorised by the PCT any informationacquired by them in connection with this Agreement.6.2 Without prejudice to the generality of Clause 6.1, the Pharmacistand their staff must not disclose to any person other than aperson authorised by the PCT, any information acquired by themin connection with the provision of the services hereunder whichconcerns:the PCT, its staff or procedures;the identity of any patient;the medical condition of or the treatment received by any patient.7. Indemnity7.1 The Pharmacy shall be liable for, and shall indemnify the PCT, itsofficers, employees and agents against any liability, loss, claim orproceedings arising under statute or at common law inconsequences of this Agreement.7.2 The Pharmacy shall maintain insurance of a minimum of £5 millionin respect of public liability and personal indemnity against anyclaims, whatsoever which may arise out of the terms andconditions and obligations of this Agreement and will at all timesduring the period of this Agreement be a member of a recognisedprofessional organisation. The PCT will have the right to seedocumentary evidence of the foregoing including policy renewal9697
eceipts prior to commencement of this Agreement or at anystage during the period of this Agreement. If the Pharmacy failsto maintain adequate insurance, or is no longer a member of anappropriate professional organisation (for whatever reason), thisAgreement may be terminated by the PCT without prejudice toany other rights and remedies available.8. Tax Liabilities8.1 It is hereby declared that it is the intention of the parties that thePharmacy shall have the status of a self-employed person andshall be responsible for all Income Tax liabilities and NationalInsurance or similar contributions in respect of his fees.9. Termination9.1 This Agreement may be terminated by either party as provided byClause 3.3 provided always that the PCT may terminate orsuspend this Agreement forthwith if there are reasonable groundsfor concern including, but not limited to, malpractice, negligenceor fraud on the part of the Pharmacy.9.2 If events occur which could not have been reasonably foreseenand are of such substance to effect the ability of either party tomeet their obligations, then joint negotiations will be undertakento consider the future provision of services or to terminate thisAgreement without prejudice to the generality of Clause 7 and 9.1hereof.10. Standard of Service10.1 The services hereunder shall be provided in accordance with thisAgreement and, except in emergencies, the Pharmacy shall notdeviate from this Agreement without the prior written consent ofthe PCT.10.2 In addition to any more specific obligations imposed by theterms of this Agreement it shall be the duty of the Pharmacy toprovide the services hereunder to a standard, which is in allrespects to the reasonable satisfaction of the PCT. The standardand quality of service will be of paramount importance to thePCT in managing this Agreement.11. Transfer and sub-contracting11.1 Neither party may assign the whole nor any part of thisAgreement, save that the PCT may assign (where not otherwisefacilitated under operation of law) where the PCT or part is takenover by another health service body.11.2 The <strong>pharmacy</strong> must not sub-contract the supply of serviceshereunder without the PCT’s previous consent in writing.12. Staff12.1 The Pharmacy shall in respect of all persons employed orseeking to be employed by the Pharmacy (whether in and aboutthe provision of the services hereunder or otherwise) complywith each and every provision of law including those whichprohibit discrimination in relation to employment on the groundsof sex, colour, race, ethnic or national origin or religion.13. Audit13.1 The Pharmacy must allow the PCT’s internal and othernominated auditors access to all or any papers relating to thisAgreement for the purposes of audit.14. Data Protection14.1 The Pharmacy must protect personal data in accordance withprovisions and the principles of the Data Protection Act 1998and must ensure the reliability of their staff who have access tothe data.14.2 The Pharmacy must indemnify the PCT against all claims andproceedings and/or liability, loss, costs and expenses incurred inconnection therewith made or brought by any person in respectof any loss, damage or distress caused to that person by thedisclosure of any personal data by the Pharmacy, its staff oragents.14.3 ‘Personal Data’ has the same meaning as in the Data ProtectionAct 1998, Section 1 (1).15. Complaints15.1 The <strong>pharmacy</strong> will be required to have a system for the handlingof complaints. All complaints received must be fed back in atimely fashion to the PCT complaints officer.16. Insurance16.1 If the <strong>scheme</strong> is extended in the future to include Patient GroupDirectives ( PGDs ) additional cover will be required.17 Publicity17.1 The Pharmacy must not advertise or publicly announce that it issupplying the services hereunder to the PCT without the priorwritten consent of the PCT.9899
Signed for and on behalf of the PharmacySignature ………………………………………………….Date ………………….............Designation ……………………………………………….Signed for and on behalf of the PCTSignature ………………………………………………….Date ………………….............Standard Service Agreement (for GP practices)Agreement Title Promoting patient care through empowerment andspeed of access for <strong>minor</strong> <strong>ailment</strong>sReference number1. Purchaser and providerThis agreement is between Newcastle Primary Care Trust (the Purchaser)of Benfield Road, Newcastle upon Tyne, NE6 4PF and ______________(the Provider) of _______________________________.The agreement will commence May 2003 and terminate on 31 st March2004.2. ObjectivesThe objectives of the service are:To identify effective ways of promoting self-care for <strong>minor</strong> <strong>ailment</strong>s inareas of social disadvantage.DesignationHead of Prescribing & Medicines ManagementThe modernisation of services relating to over the counter purchase ofmedicines.To reduce inequities in access to and speed of access to health servicesin line with the ‘National plan for the New NHS’ and ‘Pharmacy in theFuture’.3. Service detailsThe services to be delivered are:Members of the primary care team to participate in training to ensurepatients receive the same standard of information regarding the project.Triage of patients to identify those with gastro-intestinal symptoms, upperrespiratory tract infections, hayfever and thrush or cystitis in women.These patients to be given a patient information leaflet and directed totheir pharmacist rather than be given a prescription. Other conditions willbe added as appropriate.Data collection to identify which leaflets were handed out and to whichgroup of patients.Evaluation of the project, skill mix and training requirements to beprovided to the project manager via questionnaire and/or structuredinterview.The service will be delivered at the practice premises.100101
4. Activity levels/outputs/quality standardsA data collection form will be provided to the practice. The practice mustrecord the details of all patients who receive a patient information leaflet,together with the numbers of the tokens within the leaflet. Thisinformation is necessary to audit the distribution of leaflets andsubsequent reimbursement of tokens.5. Monitoring arrangementsData collection forms must be returned to the Project Manager, NewcastlePrimary Care Trust, on a monthly basis. Forms must be received at thePCT by the 10 th of the month.Staff will be required to participate in an evaluation questionnaire toassess staff perception of the project. The Project Manager will arrangeinterviews at a mutually convenient time.6. Review procedures and frequencyA review of the project progress will take place in October. A furtherreview will take place at the end of March 2004.7. Other conditionsThere must be sufficient publicity of the project to the practice’sregistered patients. Material to support publicity will be provided by theproject team.10. AuthorisationAuthorised on behalf of Newcastle Primary Care Trust:Name(print):………………………………………………………………………….......Position:…………………………………………………………………………..Signed:…………………………………………….Authorised on behalf of the Provider by:Date:……………………Name(print):………………………………………………………………………….......Position:…………………………………………………………………………..Signed:…………………………………………….Date:……………………8. Resolution of disputesDisputes will be referred to the project Advisory Group. In the event ofcontinued dispute, the Primary Care Trust management group willconsider the appropriate course of action.9. Cessation of agreementNotice period – one month for either party.It is expressly stated that this agreement does not commit the PrimaryCare Trust to future funding of the service described, once the agreementterminates.102103
appendix 12appendix 13Examples of patient informationExamples of how patients access the <strong>scheme</strong>sNote: in addition to the patient information from Central Derby below thefollowing leaflets can be downloaded from the National PharmaceuticalAssociation website at www.npa.co.uk :• Croydon PCT• Central Derby PCT• South Sefton PCT• Sheffield Community Pharmacy Development Unit• Northumberland, Tyne & Wear SHANote: in addition to the South Sefton registration form below the followingcan be downloaded from the National Pharmaceutical Associationwebsite at www.npa.co.uk :• Sheffield Community Pharmacy Development Unit registration form• South Sefton PCT patient flowchartCare at the Chemist Registration FormPharmacy FirstCentral Derby Primary Care TrustDid you want to see your doctor about oneof these………………NameDate of BirthSignature .............................................AddressCoughSore ThroatHeadache, Earache, orTemperatureBlocked NoseHay FeverHead LiceIndigestion, Heartburn orTummy UpsetDiarrhoeaConstipationThen talk to the receptionist about a new<strong>scheme</strong> that is working in this surgeryThe above named person is registered at this surgery as a patient ofDr…………………. and is eligible to receive treatment under the“Care at the Chemist Scheme”Signed…………………………………....Date…………........Take this form to one of the pharmacieslisted overleaf.The pharmacist will issue you with a“Care at the Chemist Passport”This will enable you to receive thetreatment available under the <strong>scheme</strong>without going back to the doctor’ssurgery.104105
appendix 14Examples of <strong>pharmacy</strong> prescription formsFPPharm (pharmacists prescription)Note: in addition to the <strong>pharmacy</strong> prescription from Central Derby onpage 107-108 the following forms can be downloaded from the NationalPharmaceutical Association website at www.npa.co.uk:• Croydon PCT• East Yorkshire PCT• Sefton PCT patient passport• Sheffield Community Pharmacy Development Unit• Northumberland, Tyne & Wear SHAOnly to be completed if the patient is exempt from prescriptioncharges and has signed the declaration overleafPharmacy Stamp Patients name . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .Patients Address . . . . . . . . . . . . . . . . . . . . . . . . . . . . .NHS no (if known) . . . . . . . . . . . . . . . . . . . . . . . . . . . .Date of Birth . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .GPs name . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .GPs address . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .I supplied the above patient with the following items (please tick the appropriate boxes):Product suppliedTickProduct suppliedTick1 200ml Simple Linctus or200ml Simple Linctus S.F. or100ml Simple Paed Linctus or7 32 Paracetamol Tabs or32 Soluble Aspirin 300mg Tabs or48 Ibuprofen 200mg Tabs or100ml Ibuprofen Susp or150ml Paracetamol Susp SF120mg/5mlor100ml Paracetamol Susp SF250mg/5ml2 100ml Menthol and Euc Inh. or1 Xylometazoline Nasal Spray or1 Xylometazoline Paed Drops or10ml Sod Chloride Nasal Drops or12 Pseudoephedrine Tabs or24 Pseudoephedrine Tabs or8 50ml Malathion alcoholic Liquid or200ml Malathion alcoholic Liquid or50ml Malathion Aqueous Liquid or200ml Malathion Aqueous Liquid or59ml Permethrin Cream Rinse100ml Pseudoephedrine Elixir3 30 Loratadine 10mg Tabs or90 Chlorpheniramine 4mg Tabs or30 chlorpheniramine 4mg Tabs or60ml Loratadine Syrup or9 200ml Mag Trisil Mist. or200ml Gaviscon Liq or20 Gaviscon Tabs150ml Chlorpheniramine Syrup4 1 Sod. Cromoglycate Eye Drops (5ml)and/or1 Beclomethasone Nasal Spray (1801 20 Senna Tabs or0 10 Fybogel Sachetsdose)5 12 Loperamide Capsules1 Rapid referral procedure implemented16 Advice only given - no medicationnecessary12Signature of Pharmacist………………………………………Date…………….106 107
appendix 15Pharmacy FirstCentral Derby Primary Care TrustDeclaration of exemptionTo be completed by the patientThe patient does not pay because:Examples of forms to communicate to the GPNote: in addition to the example from Croydon on page 110 the followingpaperwork can be downloaded from the National PharmaceuticalAssociation website at www.npa.co.uk:• Eastern Hull PCT record of <strong>pharmacy</strong> supply form which the GPpractice enters into the patient record.• South Sefton PCT rapid referral form.• Sheffield Community Pharmacy Development Unit rapid referralform.A X is under 16 years of ageB X is 16, 17 or 18 and in full-time educationC X is 60 years of age or overD X has a maternity exemption certificateE X has a medical exemption certificateF X has a prescription prepayment certificateL X is named on a current HC2 charge certificateH X gets income supportK X gets income based jobseeker’s allowanceM X Holds a Working Families’ Tax Credit exemption certificateor gets full WFTC or WFTC reduced by £70 or lessN X Holds a Disabled Persons’ Tax Credit exemption certificateor gets full DPTC or DPTC reduced by £70 or lessI am the patient patient’s representativeTo be completed by the Patient/patients representativeI received ……....(insert number) of medicines from this <strong>pharmacy</strong>Signed: ………………………….....................Date: ………………………..Was evidence of exemption seen? Yes No108109
appendix 16Croydon Primary Care TrustExamples of <strong>pharmacy</strong> claims formsNameAddressMinor Ailment Rapid Referral RequestGP SurgeryReferring PersonNote: in addition to the example from Central Derby on page 112-113 thefollowing <strong>pharmacy</strong> claims forms can be downloaded from the NationalPharmaceutical Association website at www.npa.co.uk :• Northumberland, Tyne & Wear SHA• South Sefton PCTDoBDate of ReferralSymptoms ReportedReason for referralWas a medicine supplied? YES/NO(Please give details)How soon does the patient require theappointment? (please delete)Immediately (Pharmacist to phonesurgery to arrange)Appointment Time__________________Appointment Date__________________Next available routine appointment.Routine appointment in ___ days/weekstimeName of Pharmacist doing referral (Block Capitals)Pharmacy StampPharmacists signatureDate referred110111
Monthly Summary sheetPlease complete a separate sheet for each GP practiceMonth………………………....................................Doctors……………………………………………….I declare that for the month of …………….…the following was suppliedPharmacy FirstCentral Derby Primary Care TrustPharmacy stampCost per No. of Total Cost per No. of Totalitem (£) items cost item (£) items cost200ml Simple Linctus 0.54 32 Paracetamol Tabs 0.25200ml Simple Linctus S.F. 0.63 32 Soluble Aspirin 300mg Tabs 0.30100ml Simple Paed Linctus 0.37 48 Ibuprofen 200mg Tabs 0.85100ml Menthol and Euc Inhalation 0.56 100ml Ibuprofen Susp 1.701 Xylometazoline Nasal Spray 1.78 150ml Paracetamol Susp SF 120mg/5ml 0.551 Xylometazoline Paed Nasal Drops 1.59 100ml Paracetamol Susp SF 250mg/5ml 0.6510ml Sod Chloride Nasal Drops 0.99 50ml Malathion Alcoholic Liquid 2.2212 Pseudoephedrine Tabs 1.14 200ml Malathion Alcoholic Liquid 5.4224 Pseudoephedrine Tabs 1.94 50ml Malathion Aqueous Liquid 2.22Cost per No. of Total Cost per No. of Totalitem (£) items cost item (£) items cost100ml Pseudoephedrine Elixir 1.40 200ml Malathion Aqueous liquid 5.4230 Loratadine 10mg Tabs 4.71 59ml Permethrin Crème Rinse 2.2630 Chlorpheniramine 4mg Tabs 0.90 200ml Mag Trisil Mist. 0.4290 Chlorpheniramine 4mg Tabs 2.70 12 Loperamide Capsules 1.9760ml Loratadine Syrup 3.98 200ml Gaviscon Liq 2.22150ml Chlorpheniramine Syrup 2.16 20 Gaviscon Tabs 0.755ml Sod. Cromoglycate Eye Drops 2.44 20 Senna Tabs 1.361 Beclomethasone Nasal Spray 3.56 10 Fybogel sachets 1.29Advice only given - no medication 2.50 Rapid referral procedure implemented 2.50necessaryTotals TotalsGrand total (sum of column 4 and 8) = + VAT =Number of Consultations (no. of Rx forms) = … x 2.50Total payment expected =Please attach this form to the prescription forms for this surgery and submit to the PCTSigned.................................................................. Date............................Pharmacists name...............................................112 113
appendix 17appendix 18Clinical governance implications for pharmacies providinga <strong>minor</strong> <strong>ailment</strong> serviceThe pharmacist and the <strong>pharmacy</strong> staff should be clinically competent inthe treatment of the <strong>minor</strong> <strong>ailment</strong>s included in the <strong>scheme</strong>. It is throughcontinuing education and CPD that this competency can be maintained.As the <strong>pharmacy</strong> manager / owner may not be present at the <strong>pharmacy</strong>every day, they must ensure that all support staff, including part-time andlocum pharmacists are fully briefed on the services being provided. Staffappraisals should be conducted regularly to ensure personal developmentfor the staff and adequate training should be provided to them. Aninduction period for locum pharmacists would be advisable.Pharmacists should have relevant sources of references in the <strong>pharmacy</strong>which should be available to all appropriate staff. The <strong>pharmacy</strong> shouldbe equipped with up to date computerised PMR facilities. A facility torecord interventions, conversations with prescribers, carers and patientsshould ideally be available on the PMR. All support staff should befamiliar with the PMR and associated programmes.Standard operating procedures related to the safe operation of the<strong>pharmacy</strong> should be written so that support staff, particularly part-timeand locum pharmacists, are aware of the standards to which they areexpected to perform. The procedures should include error and near missreporting.The staff and responsible pharmacist should be able to reflect on theirpractice, and continually endeavour to improve their practice. Thepharmacist should regularly perform an audit cycle on procedures toensure robustness and enable continuous improvement.The practice in the <strong>pharmacy</strong> should reflect the safety, confidentiality andviews of patients.Adapted from:• Anon. Community <strong>pharmacy</strong> medicines management: a resource pack for<strong>community</strong> pharmacists. The <strong>community</strong> <strong>pharmacy</strong> medicines managementproject 2003. Available at www.medicinesmanagement.org.uk/.Generic checklist for establishing a robust clinicalgovernance framework for <strong>minor</strong> <strong>ailment</strong> <strong>scheme</strong>sQuality improvement• Integration of the <strong>scheme</strong> with PCT service planning and other keystrategic elements including controls assurance and IM&T.• Appropriate priorities for quality improvement through the <strong>scheme</strong>identified within the PCT Local Development Plan.• Commitment to, and leadership for, the <strong>scheme</strong> at board level.• Required support for the <strong>scheme</strong> (project lead, budget, etc).• A <strong>scheme</strong> working group with appropriate awareness andexpertise.• Involvement of patients and users in planning and monitoring the<strong>scheme</strong>.Communication and partnership• Effectiveness of communication, within the PCT, at spreadinginformation about the <strong>scheme</strong>, to ensure there is awareness at alllevels about: priorities and importance, roles and responsibilities,sharing and acting on lessons learnt.• The extent to which the PCT and local GP practices and<strong>community</strong> pharmacists work in partnership, in respect to the<strong>scheme</strong>, including close working on both planning and servicedelivery, and operational joint working to provide seamlessservices.• Arrangements to address issues of fair access to the <strong>scheme</strong> forpeople with a diversity of needs, taking into consideration thepopulation profile (e.g. ethnic diversity, age structure).Risk management• An effective risk management strategy for the <strong>scheme</strong>.• Awareness of the significance of risk management issues by thoseresponsible for leading on it.• Systems of collecting and bringing together information from riskmanagement activities.• Promotion of an open, blame-free culture for reporting risks.• Policies and systems for risk assessments, complaintsmanagement, near misses and critical incidents that enables riskissues to be reported and learning to be shared.• Evidence of shared learning and of organisational improvementsresulting from risk issues.• The Caldicott framework readily available for handling andprotecting patient information.• Staff appropriately trained in risk management issues.• Actual evidence of risks and how well these are managed inrelation to: staff competence, clinical record keeping, prescribing,drug administration and supply, and extended / enhanced roles.114115
IM&T• Incorporation of the <strong>scheme</strong> into the strategic planning for IM&Tdevelopment.• Identification of the information requirements of the PCT and localpractices.• Use of information to assess the health and pharmaceutical careneeds of the population.• Use of information to address inequality issues.• The extent to which the PCT and local practices are monitoringdata quality and taking steps to continually improve it.• The extent to which the PCT has established systems andprocedures for data recording, collection and analysis betweenpractices.• The extent to which established information sources are used toinform commissioning behaviour of the PCT.• How the PCT uses information to monitor and improve the deliveryof care within local practices.Education, training and CPD• The presence of a CPD strategy across each organisation involvedin managing and providing the service.Complaints management• There is a policy and system for complaints management aroundthe <strong>scheme</strong>.• Processes for monitoring and reviewing complaints are in place.Adapted from:• Anon. Modernising medicines management: a guide to achieving benefits forpatients, professionals and the NHS. NPC / NPCRDC 2002. Available atwww.npc.co.uk/Patient user and public involvement• The effectiveness of mechanisms for user involvement in theplanning and monitoring of the <strong>scheme</strong>, such as: publicconsultation exercises, lay representation on the steering group.• Use of validated instruments to test the views of service users.• The extent to which issues around access and support for peoplewith disabilities has been addressed.• The extent to which access to, and the quality of, services providedout-of-hours has been evaluated.• The extent to which the pharmaceutical needs of patients fromdiverse cultural backgrounds are understood and provision made.Clinical effectiveness / research• The extent to which there is dissemination of research findings onsuch <strong>scheme</strong>s.• Evidence that the <strong>scheme</strong> and clinical governance agenda link to,and inform, clinical audit.• The extent to which the <strong>scheme</strong> actually results in sustainedchange and improvements to patient care at local level.• The extent to which the impact of the <strong>scheme</strong> is assessed andunderstood by the PCT.• The extent to which the <strong>scheme</strong> is monitored against agreed plans,fed back to staff, and used to improve audit activity.116117
appendix 19Examples of Serious Untoward Incident event reportingformsPages 118-120 contain examples of Incident Reporting Forms fromHartepool and Northumberland, Tyne & Wear.Newcastle and North TynesideHealth AuthorityHAZ/PAGB self-care projectReport of adverse incidentNewcastle and North TynesideHealth AuthorityHAZ/PAGB self-care projectReporting of adverse incidentsStrictly confidentialReporter detailsName and addressIt is important that the project Management Group is made aware of anyproblems that may be experienced in the pilot sites.Tel no. Date: Signature:Whilst it will, of course, be necessary to address any complaints locallywithin the practice as part of the NHS Complaints Procedures, I would begrateful if you would arrange for a copy of the adverse incident proformato be forwarded to me as a matter of urgency to enable us to monitorimplementation and identify any common problems.Patient detailsPlease provide an identifier to allow confidential follow up of the incidentTo maintain patient confidentiality, the proforma provides for a patientidentifier to be provided. I would be obliged if you would maintain arecord of the identifier to enable me to follow up specific incidents withthe practice.Incident reportThere will, no doubt, be a number of issues that come to light as we rolloutthe initiative and I would be pleased to receive any comments thatyou wish to forward to me.Dr Ian SpencerHead of Primary Care Development22 November 2000Please continue overleaf if necessaryPlease forward to:Dr Ian Spencer, Head of Primary Care DevelopmentNewcastle and North Tyneside Health AuthorityBenfield Road, Newcastle upon Tyne, NE6 4PFOffice use onlyIncident code:118 119
appendix 20PharmacyCodeHartlepool Primary Care TrustWhatHappened?Incident Reporting FormExamples of patient surveysNote: in addition to the patient survey below from Northumberland Tyneand Wear, the following surveys for patients, receptionists and GPs canbe downloaded from the National Pharmaceutical Association website atwww.npa.co.uk:• East Yorkshire PCT.LocationDate & TimeTyne and Wear Health Action ZoneSelf-care <strong>scheme</strong>Equipment InvolvedIndividuals/Agencies notifiedWe would be grateful for your views about why you chose to have anappointment with your GP rather than use the self-care <strong>scheme</strong>. Pleasecomplete the following questionnaire as fully as possible and return it tous in the stamped addressed envelope given to you.Please note, your response is anonymous and confidential and will haveno affect on your future treatment.What ‘harm’ / potential harm did it cause, e.g. <strong>pharmacy</strong>; patient; or staff?Thank you for your response.Question 1Why did you choose to see the GP?Please tick all that apply.Record of IncidentKey Lessons?Why did it happen (contributory factors)?I wanted reassurance from the GP [ ]I thought I needed a prescription medicine [ ]I was not confident that the pharmacistcould help [ ]There is a lack of confidentiality in <strong>pharmacy</strong> [ ]I didn’t understand the <strong>scheme</strong> [ ]I was not prepared to discuss my symptomswith the practice’s receptionist [ ]I think this is the GP’s job [ ]This is not the pharmacist’s job [ ]Changes plannedPlease add anything else in the space below.Please post or email to: Jayne.parkinson@hartlepoolpct.nhs.ukor contact 01429 287072Please retain a copy of this form in the Practice/Pharmacy120 121
Question 2Did the GP give you a prescription, a self care leaflet, both or adviceonly?Prescription [ ]Self care leaflet [ ]Both [ ]Advice only [ ]Question 3Would you use the self care <strong>scheme</strong> the next time you have a <strong>minor</strong><strong>ailment</strong> covered by the <strong>scheme</strong>?Yes [ ]No [ ]If not, why not?Question 4What would persuade you to use the self care <strong>scheme</strong> in the future?Please tick all that apply.Nothing [ ]Having to wait for an appointment with the GP [ ]Better understanding of the <strong>scheme</strong> [ ]Privacy at the <strong>pharmacy</strong> [ ]More confidence in the pharmacist [ ]Please add anything else in the space below.Please add any further comments which have not been covered bythe questionnaire, in the space below.Tyne and Wear Health Action ZoneSelf-care <strong>scheme</strong>We would be grateful for your views about the self-care <strong>scheme</strong> whichyou have used today. Please complete the following questionnaire as fullyas possible and return it to us in the stamped addressed envelope givento you.Please note, your response is anonymous and confidential and will haveno affect on your future treatment.Thank you for your response.Question 1What do you think of the <strong>scheme</strong> overall, taking into considerationeverything you know about it?Please tick that which applies.Excellent [ ]Very good [ ]Quite good [ ]Not particularly good [ ]Not very good at all [ ]Question 2What are the main things you liked about the <strong>scheme</strong>, if any?Please tick all that apply.I don’t have to wait to see the GP [ ]I can get medical advice without going to thesurgery [ ]I can treat myself sooner [ ]I can get medicine free without seeing the GP [ ]I don’t need to see GP for <strong>minor</strong> complaint [ ]The pharmacist will tell me if I need to seethe GP [ ]Please add anything else in the space below.Thank you again for taking the time to complete this questionnaire.122123
Question 3What are the things you don’t like about the <strong>scheme</strong>, if any?Please tick all that apply.I can’t speak to the pharmacist in confidence [ ]I am unsure if I have received the correcttreatment [ ]The leaflet should be available fromthe <strong>pharmacy</strong> [ ]I felt as though I was being pushed to see thepharmacist [ ]I don’t trust the pharmacist as much asthe doctor in this situation [ ]The pharmacist can’t examine me [ ]Please add anything else in the space below.Question 4Here are some statements which other people have made about the<strong>scheme</strong>. Please indicate the extent to which you share that view bycircling the number which most closely matches your opinion.1 = I strongly share that view2 = I share that view to some extent3 = I don’t really share that view4 = I don’t share that view at allIt saved me time 1 2 3 4I was just as happy to be given anover the counter medicine 1 2 3 4I want to get the medicines I need in thecheapest way possible 1 2 3 4I generally prefer to see the doctor whenit’s about my children 1 2 3 4I wanted to see the doctor because Iwanted to be reassured that it wasn’ttoo serious 1 2 3 4The leaflet was very clear and easyto read 1 2 3 4I will keep the leaflet in case somethingsimilar happens again 1 2 3 4Question 5Would you recommend the <strong>scheme</strong> to someone else?Yes [ ]No [ ]If not, why not?Question 6Would you use the self-care <strong>scheme</strong> again in the future?Yes [ ]No [ ]If not, why not?Please add any further comments, which have not been covered bythe questionnaire, below.Next time something similar happens, I’dbe happy to go straight to thepharmacist but only if they can give mefree medicines 1 2 3 4Next time something similar happens,I’d be happy to go straight to thepharmacist, even if I have to pay for themedicines 1 2 3 4Thank you again for taking the time to complete this questionnaire.124125
appendix 21appendix 22Examples of <strong>pharmacy</strong> record cardsNote: in addition to the example below from Central Derby the following<strong>pharmacy</strong> record cards can be downloaded from the NationalPharmaceutical Association website at www.npa.co.uk :• Sheffield Community Pharmacy Development UnitPharmacy record CardPharmacy FirstCentral Derby Primary Care TrustPatients name…………………………………Address ………………………………….Date of Birth………………………………….NHS number (if known)…….………………..Pharmacy stampDate and Presenting symptoms Medication supplied PharmacyPharmacists (Circle all appropriate symptoms) / Action taken stampsignature1 Nasal symptoms/cough/sorethroat/temperature/hayfever/constipation/diarrhoea/dyspepsia/headliceExamples of <strong>pharmacy</strong> monitoring formsNote: in addition to the form from Northumberland, Tyne & Wear belowthe following forms can be downloaded from the National PharmaceuticalAssociation website at www.npa.co.uk :• Eastern Hull PCT <strong>pharmacy</strong> visit recordThe SurgeryNewcastle and North TynesideHealth AuthorityHAZ/PAGB self-care projectData Collection FormDATE OF TOKEN NUMBERS AGE GENDERISSUE (E.G. CA0001&2) (M/F)2 Nasal symptoms/cough/sorethroat/temperature/hayfever/constipation/diarrhoea/dyspepsia/headlice3 Nasal symptoms/cough/sorethroat/temperature/hayfever/constipation/diarrhoea/dyspepsia/headlice4 Nasal symptoms/cough/sorethroat/temperature/hayfever/constipation/diarrhoea/dyspepsia/headlice5 Nasal symptoms/cough/sorethroat/temperature/hayfever/constipation/diarrhoea/dyspepsia/headlice6 Nasal symptoms/cough/sorethroat/temperature/hayfever/constipation/diarrhoea/dyspepsia/headlice126127
appendix 23Summary of the South Sefton PCT <strong>scheme</strong>The studyThe Care at Chemist <strong>scheme</strong> involved 1 GP practice, 8 pharmacies and12 <strong>minor</strong> <strong>ailment</strong>s over a 10 month study period.The pilotLessons learned from the pilot included:• Start small and expand when established• Engaged enthusiastic pharmacists first.Strategy for roll outTo ensure a successful roll out:• Get interested parties on board• Get all <strong>community</strong> pharmacists up to speed before starting• Brief GP practices and train staff one at a time• One surgery at a time should ‘go live’.Solutions to problems• Central agency to price prescriptions and do most of administration• Steering committee developed new formulary to reflect PCT wideneeds• New formulary more evidence based• Compromise on some items of doubtful value as demand existed• Reluctant GPs patients initially excluded from <strong>scheme</strong>• PCT accepted costs of <strong>scheme</strong> were better than alternatives i.e.over burdened GPs.The current situationThe South Sefton PCT <strong>scheme</strong> now covers all patients registered in theSouth Sefton area. Plans for even further roll out include:• Wider publicity planned• Closer working with neighbouring PCTs• Expanded formulary to include POMs using PGD.A project manager• A facilitator was used 1 day per week to train surgery and<strong>pharmacy</strong> staff• Facilitator was a <strong>community</strong> pharmacist who was already involvedin the <strong>scheme</strong> as part of the pilot• Facilitator was used to “trouble shoot” in the first few months ofPCT wide <strong>scheme</strong>.Rolling out the <strong>scheme</strong> across the PCT• LMC and LPC consulted to ensure support• An invitation to participate issued to all GPs and pharmacies• Further invitation followed by telephone call was sent toprofessionals not responding• Visits to those who had questions and concerns.Problems encountered• Formulary did not reflect PCT wide prescribing• Pricing arrangements needed to change due to higher volume• Cost of administration greatly increased• Concerns from GP over liability• Formulary contained items of doubtful value, i.e. not evidencebased• Funding.128129
The National Pharmaceutical Association LimitedMallinson House, 38-42 St. Peter’s Street, St. Albans, Herts AL1 3NPTelephone: 01727 832161 Fax: 01727 840858 Website: www.npa.co.ukDECEMBER 2003