Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
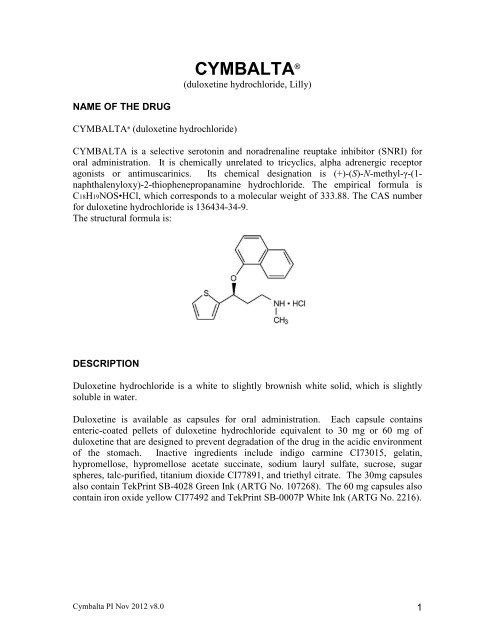
CYMBALTA ®(duloxetine hydrochloride, Lilly)NAME OF THE DRUGCYMBALTA ® (duloxetine hydrochloride)CYMBALTA is a selective serotonin and noradrenaline reuptake inhibitor (SNRI) fororal administration. It is chemically unrelated to tricyclics, alpha adrenergic receptoragonists or antimuscarinics. Its chemical designation is (+)-(S)-N-methyl-γ-(1-naphthalenyloxy)-2-thiophenepropanamine hydrochloride. The empirical formula isC18H19NOS•HCl, which corresponds to a molecular weight of 333.88. The CAS numberfor duloxetine hydrochloride is 136434-34-9.The structural formula is:DESCRIPTIONDuloxetine hydrochloride is a white to slightly brownish white solid, which is slightlysoluble in water.Duloxetine is available as capsules for oral administration. Each capsule containsenteric-coated pellets of duloxetine hydrochloride equivalent to 30 mg or 60 mg ofduloxetine that are designed to prevent degradation of the drug in the acidic environmentof the stomach. Inactive ingredients include indigo carmine CI73015, gelatin,hypromellose, hypromellose acetate succinate, sodium lauryl sulfate, sucrose, sugarspheres, talc-purified, titanium dioxide CI77891, and triethyl citrate. The 30mg capsulesalso contain TekPrint SB-4028 Green Ink (ARTG No. 107268). The 60 mg capsules alsocontain iron oxide yellow CI77492 and TekPrint SB-0007P White Ink (ARTG No. 2216).Cymbalta PI Nov 2012 v8.0 1
PHARMACOLOGYPharmacodynamicsDuloxetine is a selective serotonin and noradrenaline reuptake inhibitor, and weaklyinhibits dopamine uptake with no significant affinity for histaminergic, dopaminergic,cholinergic and adrenergic receptors.Although the mechanism of the antidepressant action of duloxetine in humans isunknown, it is believed to be related to its potentiation of serotonergic and noradrenergicactivity in the CNS. Duloxetine dose-dependently increased extracellular levels ofserotonin and noradrenaline in selected brain areas of animals, and neurochemical andbehavioural studies in animals indicate an enhancement of central serotonin andnoradrenaline neurotransmission. Duloxetine undergoes extensive metabolism, but themajor circulating metabolites have not been shown to contribute significantly to thepharmacologic activity of duloxetine. Duloxetine displayed analgesic activity in rodentmodels of persistent, inflammatory or neuropathic pain, but not acute or arthritic pain.PharmacokineticsAbsorptionIn humans, orally administered duloxetine hydrochloride is well absorbed with maximalplasma concentrations (Cmax) of duloxetine occurring 6 hours post dose. Food does notaffect the Cmax of duloxetine, however food can delay the time to reach peakconcentration from 6 to 10 hours and it marginally decreases the extent of absorption(AUC) by about 11%.Duloxetine plasma exposure increases in proportion to dose for doses up to 60 mg twice aday. Steady-state plasma concentrations are typically achieved after 3 days of dosing.Based upon AUC, multiple once daily doses of 60 mg produce steady-stateconcentrations that are approximately 1.5 times higher than that predicted from a 60 mgsingle dose. Average minimum and maximum steady-state concentrations for the 60 mgonce daily dose are 27.0 and 89.5 ng/mL, respectively. There is no clinically importantdifference in the pharmacokinetic parameters of morning and evening doses.DistributionFollowing oral administration, the apparent volume of distribution of duloxetine averages1640 L. Duloxetine is highly protein bound (>90%) to plasma proteins but proteinbinding is not affected by renal or hepatic impairment. Duloxetine binds to both albuminand α1-acid glycoprotein.MetabolismDuloxetine undergoes extensive metabolism. The 2 major metabolites found in plasmaand urine are the glucuronide conjugate of 4-hydroxy duloxetine, and the sulfateconjugate of 5-hydroxy, 6-methoxy duloxetine. Both CYP2D6 and CYP1A2 catalyse theformation of the initial oxidation steps to form 4-, 5-, and 6-hydroxy duloxetine. TheCymbalta PI Nov 2012 v8.0 2
metabolites circulating in plasma are in the conjugated form and are notpharmacologically active.ExcretionThe half-life of duloxetine (unchanged drug) is 12.1 hours. Apparent plasma clearance ofduloxetine after an oral dose is 101 L/hr. The majority (70%) of the duloxetine dose isrecovered in the urine as conjugated metabolites of oxidative metabolites of duloxetine.Approximately 20% of the dose is recovered in the faeces as unchanged drug,unconjugated metabolites, or unidentified compounds. Only trace (
CLINICAL TRIALSAcute treatment of depression:The efficacy of duloxetine has been evaluated in six double-blind, placebo-controlledacute Phase 3 studies of 8-9 weeks’ duration in 1978 adult outpatients (18 to 83 years)meeting the DSM-IV criteria for major depression at doses of 40 mg to 120 mg daily. Infour of these studies, duloxetine was significantly superior to placebo as measured by themean change in the 17 item Hamilton Depression Rating Scale (HAMD17) total scorefrom baseline to endpoint. Duloxetine doses in these four studies were:• 60 mg once daily (two studies)• 20 mg twice daily and 40 mg twice daily (one study)• 40 mg twice daily and 60 mg twice daily (one study)In the remaining two studies duloxetine showed numerically superior mean changecompared with placebo. The duloxetine doses in these two studies were:• 20 mg twice daily and 40 mg twice daily• 40 mg twice daily and 60 mg twice dailyIn both of these latter studies, the active comparator paroxetine also did not separatesignificantly from placebo on the primary outcome measure. Response (≥ 50% reductionin HAMD17 total score) and remission (HAMD17 total score ≤ 7) were also significantlyhigher with duloxetine compared with placebo in five out of six and three out of six acutestudies, respectively.While results were positive for improvement in the HAMD17 at a dose of 20 mg twicedaily in one of two studies, this dose did not demonstrate statistical superiority on anyother measure including response or remission.Table 1 HAMD17 Total, Response, and Remission Rates Placebo-ControlledDuloxetine 60 mg Once Daily StudiesPlacebo(n=115)HMBHaDuloxetine(n=121)P-Value 4Placebo(n=136)HMBHbDuloxetine(n=123)P-Value4HAMD17 -5.67 -9.47
evaluation of efficacy of duloxetine. HAMD17 Depressed Mood Item (Item 1), theAnxiety Subfactor of the HAMD17, the Patient Global Impressions (PGI) ImprovementScore, bodily pain as measured by Visual Analog Scale (VAS), and the Quality of Life inDepression rating scales were also examined. In the four studies where duloxetinedemonstrated statistical superiority over placebo as measured by improvement in theHAMD17 total score, results were also positive for the additional measures at doses of 60mg to 120 mg per day.In each study and in pooled data, the effectiveness of duloxetine was similar regardless ofage, gender or racial origin.Prevention of depressive relapse: Patients responding to 12 weeks of acute treatmentwith open-label duloxetine at a dose of 60 mg once daily were randomly assigned toeither duloxetine 60 mg once daily or placebo for a further 6 months (continuation phase)and time to relapse in each group was compared. Of 533 subjects who enrolled in thestudy, 278 responded and were randomised to duloxetine 60 mg once daily (n=136) orplacebo (n=142). The estimated probability of depressive relapse at 6 months for placebowas 38.3% and for duloxetine 60 mg once daily was 19.7% (p=0.004). During the 6-month continuation therapy phase of this study, 17.4% of duloxetine-treated patients metthe a priori-defined criteria for relapse compared with 28.5% on placebo (p=0.042).Of 88 patients who relapsed during the continuation phase, 87 received double-blindrescue therapy. The patients who relapsed on placebo (n=58) were treated withduloxetine at a dose of 60 mg once daily, and those relapsing on duloxetine 60 mg oncedaily (n=29) were treated with duloxetine 60 mg twice daily. Of those patients relapsingon placebo and treated with duloxetine 60 mg once daily, response (50% reduction inHAMD17 total score) occurred in 77% and remission (HAMD17 total score ≤ 7) occurredin 57% at the end of 12 further weeks of treatment. Of those patients who relapsed onduloxetine 60 mg once daily and who were treated with an increased dose of 60 mg twicedaily, 62% met response criteria and 38% met remission criteria.Use in elderly patients with depression: The efficacy and safety of duloxetine 60 mg oncedaily (n=207) and placebo (n=104) have been compared in the acute treatment (studyduration 8 weeks) of elderly patients with MDD (>65 years of age, mean age 72.9 years).Duloxetine treated patients experienced improvement in depressive symptoms, asassessed by the Geriatric Depression Scale, from week 1, with least-squares meanchanges from baseline to endpoint of -1.34 for placebo-treated patients and -4.07 forduloxetine-treated patients (p
Diabetic Peripheral Neuropathic PainThe efficacy of CYMBALTA for the management of neuropathic pain associated withdiabetic peripheral neuropathy was established in 2 randomised, 12-week, double-blind,placebo-controlled, fixed-dose studies in adult patients having diabetic peripheralneuropathic pain for at least 6 months The design of the two studies is summarised inTable 2.Table 2: Study Design of Clinical Trials Supporting Efficacy of Duloxetine in theTreatment of DPNPStudy Code Design Duration ofTreatmentHMAW-AcuteParallel, double-blind,randomised, placebocontrolledTreatment andDose12 Weeks DLX 20 mg QDDLX 60 mg QDDLX 60 mg BIDPBOHMAVa- AcuteParallel, double-blind,randomised, placebocontrolled12 weeks (plus 1week taper)52-week extensionDLX 60 mg QDDLX 60 mg BIDPBOBID = twice daily; QD = once daily; DLX = duloxetine; PBO = placeboPatients enrolled had Type I or II diabetes mellitus with a diagnosis of painful distalsymmetrical sensorimotor polyneuropathy for at least 6 months. The patients had abaseline pain score of ≥4 on an 11-point scale ranging from 0 (no pain) to 10 (worstpossible pain). Patients were permitted up to 4 g of paracetamol per day as needed forpain, in addition to CYMBALTA. Patients recorded their pain daily in a diary.Both studies compared duloxetine 60 mg once daily or 60 mg twice daily with placebo;one study additionally compared duloxetine 20 mg with placebo. A total of 457 patients(342 Cymbalta, 115 placebo) were enrolled in study HMAW-acute and a total of 334patients (226 Cymbalta, 108 placebo) were enrolled in study HMAVa-acute.The weekly average of the 24-hour average pain severity was the primary efficacymeasure for the assessment of duloxetine’s effectiveness in the treatment of DPNP.Duloxetine 60 mg once daily and duloxetine 60 mg twice daily were both statisticallysignificantly superior to placebo as assessed by the reduction from baseline in theprimary efficacy measure, 24-hour average pain severity, as shown in Table 3. Inaddition, duloxetine 60 mg once daily and duloxetine 60 mg twice daily were statisticallysignificant to placebo as assessed by response rate (whether measured by at least a 30%reduction or at least a 50% reduction in pain score from baseline). Evidence of efficacyfrom the primary efficacy measure is confirmed by comprehensive results from thesecondary pain and DPNP symptom measures.The secondary efficacy measures that supported the use of CYMBALTA in the treatmentof DPNP were: weekly averages of night pain and 24-hour worst pain from the dailyCymbalta PI Nov 2012 v8.0 6
diary, Brief Pain Inventory Severity and Interference (BPI Severity and Interference),Clinical Global Impressions of Severity (CGI-Severity), Patient Global Impression ofImprovement (PGI-Improvement) scale, and Sensory portion of the Short-form McGillpain questionnaire. In addition, measures of mood were employed in both placebocontrolledstudies to demonstrate changes of pain uncontaminated by duloxetine’s effecton mood.Table 3 Summary of Primary Efficacy in 12 week placebo controlled studiesStudy HMAVa-acute 1 Study HMAW-acute 2PBOn=106DLX60QDn=110DLX60BIDn=111PBOn=111DLX20QDn=111DLX60QDn=112 DLX60BIDn=109Mean Baseline 5.85 6.12 6.21 5.73 5.84 6.01 5.85Mean Change -1.39 -2.72P
Table 4 Summary of Primary Efficacy in acute placebo-controlled GAD studiesStudy/durationTreatment Group N Baseline Endpoint LSMeanChangep-valuevsplaceboHMBR Duloxetine 60 mg QD 165 25.05 12.32 -12.8
those receiving antidepressants. The average risk of such events in patients treated withan antidepressant was 4% compared with 2% of patients given placebo. There wasconsiderable variation in risk among the antidepressants, but there was a tendencytowards and increase for almost all antidepressants studied. The risk of suicidality wasmost consistently observed in the major depressive disorder trials, but there were signalsof risk arising from trials in other psychiatric indications (obsessive compulsive disorderand social anxiety disorder) as well. No suicides occurred in these trials. It is unknownwhether the suicidality risk in children and adolescent patients extends to use beyondseveral months. The nine antidepressant medications in the pooled analyses included fiveSSRIs (citalopram, fluoxetine, fluvoxamine, paroxetine, sertraline) and four non-SSRIs(bupropion, mirtazapine, nefazodone, venlafaxine).Symptoms of anxiety, agitation, panic attacks, insomnia, irritability, hostility(aggressiveness), impulsivity, akathisia (psychomotor restlessness), hypomania andmania have been reported in adults, adolescents and children being treated withantidepressants for major depressive disorder as well as for other indications, bothpsychiatric and nonpsychiatric. Although a causal link between the emergence of suchsymptoms and either worsening of depression and/or emergence of suicidal impulses hasnot been established, there is concern that such symptoms may be precursors of emergingsuicidality.Families and caregivers of children and adolescents being treated with antidepressants formajor depressive disorder or for any other condition (psychiatric or nonpsychiatric)should be informed about the need to monitor these patients for the emergence ofagitation, irritability, unusual changes in behaviour and other symptoms described above,as well as the emergence of suicidality, and to report such symptoms immediately tohealthcare providers. It is particularly important that monitoring be undertaken duringthe initial few months of antidepressant treatment or at times of dose increase ordecrease.Duloxetine hydrochloride is not indicated for use in patients under the age of 18.Although a causal role for duloxetine in inducing such events has not been established,some analyses from pooled studies of antidepressants in psychiatric disorders found anincreased risk for suicidal ideation and/or suicidal behaviors in pediatric and young adult(
transaminase elevations resulted in the discontinuation of 0.3% (82/27,229) ofCYMBALTA-treated patients. In these patients, the median time to detection of thetransaminase elevation was about two months. In placebo controlled trials in anyindication, elevations of alanine transaminase (ALT) to >3 times the upper limit ofnormal occurred in 1.1% (85/7632) of CYMBALTA-treated patients and in0.2% (13/5578) of placebo treated patients. In placebo-controlled studies using a fixeddose design, there was evidence of a dose-response relationship for ALT and ASTelevation of >3 times the upper limit of normal and >5 times the upper limit of normal,respectively.Postmarketing reports have described cases of hepatitis with abdominal pain,hepatomegaly and elevation of transaminase levels to more than twenty times the upperlimit of normal with or without jaundice, reflecting a mixed or hepatocellular pattern ofliver injury. Cases of cholestatic jaundice with minimal elevation of transaminase levelshave also been reported. Isolated cases of liver failure, including fatal cases, have beenreported. A majority of these cases have been reported in patients with past or currentrisk factors for liver injury, including alcohol abuse, hepatitis or exposure to drugs withknown adverse effects on the liver.The combination of transaminase elevations and elevated bilirubin, without evidence ofobstruction, is generally recognised as an important predictor of severe liver injury. Inclinical trials, 7 CYMBALTA patients had elevations of transaminases and bilirubin, but5 of 7 also had elevation of alkaline phosphatase, suggesting an obstructive process; inthese patients, in 3 of these 7 patients there was evidence of heavy alcohol use and thismay have contributed to the abnormalities seen.Postmarketing reports indicate that elevated transaminases, bilirubin and alkalinephosphatase have occurred in patients with chronic liver disease or cirrhosis.AlcoholBecause it is possible that duloxetine and alcohol may interact to cause liver injury or thatduloxetine may aggravate pre-existing liver disease, CYMBALTA should ordinarily notbe prescribed to patients with substantial alcohol use or evidence of chronic liver disease(see PRECAUTIONS – Hepatotoxicity)Bipolar DisorderA major depressive episode may be the initial presentation of bipolar disorder. It isgenerally believed that treating such an episode with an antidepressant alone can increasethe likelihood of precipitation of a mixed/manic episode in patients at risk of bipolardisorder. Prior to initiating treatment with an antidepressant, patients should beadequately screened to determine if they are at risk for bipolar disorder; such screeningshould include a detailed psychiatric history, including a family history of suicide, bipolardisorder, and depression.Cymbalta PI Nov 2012 v8.0 13
Activation of ManiaIn placebo-controlled trials in patients with major depressive disorder, activation ofhypomania or mania occurred in 0.1% of duloxetine treated patients and 0.1% of placebotreated patients. No activation of mania or hypomania was reported in DPNP or GADplacebo controlled trials. Activation of mania/hypomania has been reported in a smallproportion of patients with mood disorders who were treated with other marketed drugseffective in the treatment of major depressive disorder. As with these other drugs,duloxetine should be used cautiously in patients with a history of mania.SeizuresDuloxetine has not been systematically evaluated in patients with a seizure disorder. Inplacebo-controlled clinical trials, seizures/convulsions occurred in 0.03% (3/9445) ofpatients treated with duloxetine and 0.01% (1/6770) of patients with placebo. As withsimilar CNS active drugs, duloxetine should be used cautiously in patients with a historyof seizure disorder.MydriasisMydriasis has been reported in association with duloxetine. Caution should be exercisedin patients with raised intraocular pressure or those at risk of acute narrow-angleglaucoma.HyponatraemiaCases of hyponatremia (some with serum sodium lower than 110mmol/Liter) have beenreported very rarelywhen administering CYMBALTA. The majority of these casesoccurred in elderly patients, especially when coupled with a recent history of altered fluidbalance or conditions pre-disposing to altered fluid balance. Hyponatremia may presentwith nonspecific signs and symptoms (such as dizziness, weakness, nausea, vomiting,confusion, somnolence, and lethargy). Signs and symptoms associated with more severecases have included syncopal episodes, falls, and seizure. Caution is required in patientsat increased risk for hyponatraemia; such as elderly, cirrhotic, or dehydrated patients orpatients treated with diuretics. Hyponatraemia may be due to a syndrome of inappropriateanti-diuretic hormone secretion (SIADH).Abnormal BleedingSSRIs and SNRIs, including duloxetine, may increase the risk of bleeding events,including gastrointestinal bleeding (see ADVERSE REACTIONS). Therefore, caution isadvised in patients taking duloxetine concomitantly with anticoagulants and/or medicinalproducts known to affect platelet function (e.g., NSAIDs, aspirin) and in patients withknown bleeding tendencies.Use in Patients with Concomitant IllnessClinical experience with duloxetine in patients with concomitant systemic illnesses islimited. Caution is advisable in using duloxetine in patients with diseases or conditionsthat produce altered metabolism or haemodynamic responses.Duloxetine has not been systematically evaluated in patients with a recent history ofCymbalta PI Nov 2012 v8.0 14
myocardial infarction or unstable heart disease. Patients with these diagnoses weregenerally excluded from clinical studies during the product’s premarketing testing.However, evaluation of electrocardiograms (ECGs) of 321 patients who receivedduloxetine in placebo-controlled clinical trials indicated that duloxetine is not associatedwith the development of clinically significant ECG abnormalities (see PRECAUTIONS-Electrocardiogram Changes).Increased plasma concentrations of duloxetine occur in patients with end stage renaldisease (ESRD) and in patients with moderate hepatic impairment (seePharmacokinetics).Drug DependenceWhile duloxetine has not been systematically studied in humans for its potential forabuse, there was no indication of drug-seeking behaviour in the clinical trials. However,it is not possible to predict on the basis of premarketing experience the extent to which aCNS active drug will be misused, diverted, and/or abused once marketed. Consequently,physicians should carefully evaluate patients for a history of drug abuse and follow suchpatients closely, observing them for signs of misuse or abuse of duloxetine (e.g.development of tolerance, incrementation of dose, drug-seeking behaviour).Weight ChangesWeight changes do not appear to be clinically significant outcomes of treatment withduloxetine. In placebo-controlled clinical trials, patients treated with duloxetine for up to9-weeks experienced a mean weight loss of approximately 0.5 kg, compared with a meanweight gain of approximately 0.2 kg in placebo-treated patients.Renal ImpairmentDuloxetine Cmax and AUC values were approximately 2-fold higher in patients withESRD receiving chronic intermittent dialysis, compared with subjects with normal renalfunction. In contrast, the elimination half-life was similar in both groups. A lower doseshould be used for patients with ESRD (see DOSAGE AND ADMINISTRATION).Population pharmacokinetic analyses suggest that mild renal dysfunction has nosignificant effect on apparent plasma clearance of duloxetine.Blood PressureDuloxetine is associated with an increase in blood pressure in some patients. In placebocontrolledclinical trials duloxetine treatment was associated with small increases insystolic blood pressure averaging 2 mm Hg and small increases in diastolic bloodpressure averaging 0.5 mm Hg compared to placebo. Large, potentially clinicallysignificant, elevations in blood pressure do not appear to be more common withduloxetine than with placebo. In patients with known hypertension and/or other cardiacdisease, blood pressure monitoring is recommended as appropriate. CYMBALTA shouldbe used with caution in patients whose conditions could be compromised by an increasedheart rate or by an increase in blood pressure.Cymbalta PI Nov 2012 v8.0 15
Orthostatic Hypotension and SyncopeOrthostatic hypotension and syncope have been reported with therapeutic doses ofduloxetine. Syncope and hypotension tend to occur within the first week of therapy butcan occur at any time during duloxetine treatment, particularly after dose increases. Therisk of blood pressure decreases may be greater in patients taking concomitantmedications that induce orthostatic hypotension (such as antihypertensives) or are potentCYP1A2 inhibitors and in patients taking doses above 60 mg daily. Consideration shouldbe given to discontinuing CYMBALTA in patients who experience symptomaticorthostatic hypotension and/or syncope during therapy.Electrocardiogram ChangesECGs were obtained from 321 duloxetine-treated patients with MDD and 169 placebotreatedpatients in 8-week clinical trials. The rate-corrected QT interval in duloxetinetreatedpatients in an 8-week study did not differ from that seen in placebo-treatedpatients. In summary, the data suggest no arrhythmogenic potential with duloxetine. Noclinically significant differences were observed for QT, PR and QRS intervals betweenduloxetine-treated and placebo-treated patients.Discontinuing TreatmentAs with other drugs effective in the treatment of major depressive disorder, whendiscontinuing CYMBALTA after more than 1 week of therapy, it is generallyrecommended that the dose be tapered to minimise the risk of discontinuation symptoms(see DOSAGE AND ADMINISTRATION). The most commonly reported symptomsfollowing abrupt discontinuation of duloxetine in clinical trials have included dizziness,nausea, headache, paraesthesia, fatigue, vomiting, irritability, nightmares, insomnia,diarrhoea, anxiety, hyperhidrosis, vertigo, somnolence and myalgia.Serotonin SyndromeDevelopment of serotonin syndrome may occur in association with treatment with SSRlsand SNRls, particularly when given in combination with MAOls or other serotonergicagents. Symptoms and signs of serotonin syndrome include rapid onset of neuromuscularexcitation (hyperreflexia, incoordination, myoclonus, tremor), altered mental status(confusion, agitation, hypomania) and autonomic dysfunction (diaphoresis, diarrhoea,fever, shivering and rapidly fluctuating vital signs). Treatment with CYMBALTA shouldbe discontinued if such events occur and supportive symptomatic treatment initiated.Caution is advisable if CYMBALTA is used concomitantly with serotonergicantidepressants like SSRIs, SNRIs, tricyclic antidepressants like clomipramine oramitriptyline, St John’s Wort (Hypericum perforatum), triptans, tramadol, pethidine ortryptophan.Effect on Ability to Drive or Operate MachineryIn controlled studies duloxetine has not been shown to impair psychomotor performance,cognitive function or memory. However, as any psychoactive drug may impairCymbalta PI Nov 2012 v8.0 16
judgement, thinking or motor skills, and duloxetine may be associated with undesirableeffects such as sedation and dizziness, patients should be cautioned about their ability toperform potentially hazardous tasks until they are reasonably certain that duloxetinetherapy does not affect their ability to engage in such activities.Use in Patients aged ≥65 years of ageEvaluation of patients over the age of 65 who received duloxetine in clinical trialsrevealed no unusual pattern of adverse events relative to the clinical experience inyounger patients, but greater sensitivity of some older individuals cannot be ruled out.SSRIs and SNRIs, including CYMBALTA, have been associated with cases of clinicallysignificant hyponatraemia in elderly patients, who may be at greater risk for this adversereaction.Use in Children and Adolescents aged
maximum recommended dose. In rats receiving the maternotoxic dose of 45 mg/kg/dayduring organogenesis, there was increased preimplantation loss and resorptions, andreduced fetal weight.Oral administration of duloxetine to female rats prior to and throughout mating, gestationand lactation at doses of 30-45 mg/kg/day (2-3 times the maximum recommended humandose on a mg/m 2 basis) elicited maternal toxicity and reduced live birth indices, birthweight, and postnatal survival and growth of offspring, and altered some indices ofoffspring behaviour.Neonates exposed to serotonergic agents late in the third trimester have beenuncommonly reported to have clinical findings of respiratory distress, cyanosis, apnoea,seizures, temperature instability, feeding difficulty, vomiting, hypoglycaemia, hypotonia,hypertonia, hyperreflexia, tremor, jitteriness, irritability and constant crying. Such eventscan arise immediately upon delivery and are usually transient. The majority of cases haveoccurred either at birth or within a few days of birth. These features could be consistentwith either a direct effect of SSRIs and SNRIs or, possibly, a drug discontinuationsyndrome. When treating a pregnant woman with duloxetine during the third trimester,the physician should carefully consider the potential risks and benefits of treatment.The safety of duloxetine in human pregnancy has not been established and becauseanimal reproduction studies are not always predictive of human response, this drugshould be used during pregnancy only if the potential benefit justifies the potential risk.Use in LactationDuloxetine is excreted into the milk of lactating women. The estimated infant doseranges from approximately 0.1% to 0.3% of the maternal dose, normalised by bodyweight. Oral administration of duloxetine to female rats prior to and throughout mating,gestation and lactation was associated with maternal toxicity and adverse effects (see Usein Pregnancy). Administration of CYMBALTA to nursing mothers is not recommended.Labour and DeliveryThe effect of duloxetine on labour and delivery in humans is unknown.Interactions with Other DrugsDuloxetine is a SNRI with its primary effect on the CNS. Caution should be used when itis administered in combination with other centrally acting drugs and substances,especially those with a similar mechanism of action, including alcohol. Concurrent usewith other drugs with serotonergic activity (eg SNRIs, SSRIs, triptans or tramadol) mayresult in serotonin syndrome (see PRECAUTIONS).Although duloxetine does not increase the impairment of mental and motor skills causedby alcohol, use of CYMBALTA with substantial alcohol consumption may be associatedwith severe liver injury. Isolated cases of liver failure, including fatal cases, have beenreported (see PRECAUTIONS – Hepatotoxicity). CYMBALTA should only be used inexceptional circumstances with extreme caution in patients who consume substantialCymbalta PI Nov 2012 v8.0 18
amounts of alcohol.Drugs Metabolised by CYP1A2 – Although CYP1A2 is weakly inhibited byduloxetine in vitro, results of a clinical study show that the pharmacokinetics of aCYP1A2 substrate (theophylline) were not significantly affected by co-administrationwith duloxetine (60 mg twice daily). In vitro studies with human hepatocytesdemonstrated that duloxetine does not induce CYP1A2 activity. These studies suggestthat duloxetine is unlikely to have a clinically significant effect on the metabolism ofCYP1A2 substrates.Inhibitors of CYP1A2 - As CYP1A2 is involved in duloxetine metabolism,concomitant use of duloxetine with potent inhibitors of CYP1A2 will likely result inhigher concentrations of duloxetine. Fluvoxamine (100 mg once daily), a potentinhibitor of CYP1A2, decreased the apparent plasma clearance of duloxetine by about77%. CYMBALTA should not be used in combination with potent inhibitors ofCYP1A2 (e.g., fluvoxamine) (see CONTRAINDICATIONS).Drugs Metabolised by CYP2D6 - CYP2D6 is moderately inhibited by duloxetine(in common with tricyclic antidepressants and SSRIs). Duloxetine administered at 60mg twice daily caused a single 50 mg dose of desipramine (also metabolised throughCYP2D6) to have a 3-fold increase in the AUC. Duloxetine administered at 40 mgtwice daily increased steady-state AUC of tolterodine (2 mg twice daily) by 71% butdid not affect the pharmacokinetics of the 5-hydroxyl metabolite. Therefore, cautionshould be used if duloxetine is co-administered with medications that arepredominantly metabolised by the CYP2D6 system and which have a narrowtherapeutic index (e.g. tricyclic antidepressants such as nortriptyline and imipramine,phenothiazines, flecainide, propafenone). Because of the risk of serious ventriculararrhythmias and sudden death potentially associated with elevated plasmaconcentrations of thioridazine, CYMBALTA and thioridazine should not becoadministered.Inhibitors of CYP2D6 –An inhibitor of CYP2D6, paroxetine (20 mg once daily)decreased the oral clearance of duloxetine (40 mg once daily) by about 37%. BecauseCYP2D6 is involved in duloxetine metabolism, caution is advised if administeringduloxetine with inhibitors of CYP2D6 (e.g. SSRIs).Drugs Metabolised by CYP2C9 – Although clinical studies have not beenperformed, results of in vitro studies demonstrate that duloxetine does not inhibit theenzyme activity of CYP2C9.Drugs Metabolised by CYP3A – Although clinical studies have not beenperformed, results of in vitro studies demonstrate that duloxetine does not inhibit orinduce the catalytic activity of CYP3A.Antacids and H2 Antagonists – Co-administration of duloxetine with aluminiumandmagnesium-containing antacids or co-administration of duloxetine withCymbalta PI Nov 2012 v8.0 19
famotidine had no significant effect on the rate or extent of duloxetine absorption afteradministration of a40 mg oral dose.Drugs Highly Bound to Plasma Protein – Duloxetine is highly bound to plasmaprotein (>90%). Administration of duloxetine with another highly protein bound drugmay cause increased free concentrations of either duloxetine or the other drug.Monoamine Oxidase Inhibitors (MAOI) - Because duloxetine is an inhibitor ofboth serotonin and noradrenaline reuptake, it is recommended that duloxetine not beused in combination with an MAOI (see CONTRAINDICATIONS).St John’s Wort - In common with other antidepressants, concomitant administrationof duloxetine and the herbal remedy St John's Wort (Hypericum perforatum) is notrecommended.Warfarin and INR – Increases in INR have been reported when duloxetine was coadministeredwith warfarin.Drugs That Affect Gastric Acidity - CYMBALTA has an enteric coating thatresists dissolution until reaching a segment of the gastrointestinal tract where the pHexceeds 5.5. In extremely acidic conditions, CYMBALTA, unprotected by the entericcoating, may undergo hydrolysis to form naphthol. Caution is advised in usingCYMBALTA in patients with conditions that may slow gastric emptying (e.g., somediabetics). Drugs that raise the gastrointestinal pH may lead to an earlier release ofduloxetine. It is unknown whether the concomitant administration of proton pumpinhibitors affects duloxetine absorption.Effects on Laboratory TestsThere are no data available that shows that duloxetine has an effect on laboratory tests.ADVERSE REACTIONSClinical Trial DataThe data described below reflect exposure to duloxetine in placebo-controlled trials forMDD (N=2327), GAD (N=668) and DPNP (N=568). The population studied was 17 to89 years of age; 64.8%, 64.7% and 38.7%, female; and 85.5%, 77.6%, and 84.6%Caucasian for MDD, GAD and DPNP, respectively. Most patients received doses of atotal of 60 to 120 mg per day.Adverse Reactions Reported as Reasons for Discontinuation of Treatment inPlacebo-Controlled TrialsMajor Depressive Disorder — Approximately 9% (209/2327) of the patients whoreceived duloxetine in placebo-controlled trials for MDD discontinued treatment due toan adverse reaction, compared with 4.7% (68/1460) of the patients receiving placebo.Cymbalta PI Nov 2012 v8.0 20
Nausea (duloxetine 1.3%, placebo 0.5%) was the only common adverse reaction reportedas a reason for discontinuation and considered to be drug-related (i.e., discontinuationoccurring in at least 1% of the duloxetine-treated patients and at a rate of at least twicethat of placebo).Generalised Anxiety Disorder — Approximately 15.3% (102/668) of the patients whoreceived duloxetine in placebo-controlled trials for GAD discontinued treatment due toan adverse reaction, compared with 4.0% (20/495) for placebo. Common adversereactions reported as a reason for discontinuation and considered to be drug-related (asdefined above) included nausea (duloxetine 3.7%, placebo 0.2%), vomiting (duloxetine1.3%, placebo 0.0%), and dizziness (duloxetine 1.0%, placebo 0.2%).Diabetic Peripheral Neuropathic Pain — Approximately 14.3% (81/568) of the patientswho received duloxetine in placebo-controlled trials for DPNP discontinued treatmentdue to an adverse reaction, compared with 7.2% (16/223) for placebo. Common adversereactions reported as a reason for discontinuation and considered to be drug-related (asdefined above) were nausea (duloxetine 3.5%, placebo 0.4%), dizziness (duloxetine1.6%, placebo 0.4%), somnolence (duloxetine 1.6%, placebo 0.0%), and fatigue(duloxetine 1.1%, placebo 0.0%).Adverse Reactions Occurring at an Incidence of 2% or More Among Duloxetine-Treated Patients in Placebo-Controlled TrialsPooled MDD and GAD Trials — Table 5 gives the incidence of treatment-emergentadverse reactions in MDD and GAD placebo-controlled trials that occurred in 2% ormore of patients treated with duloxetine and with an incidence greater than placebo.Cymbalta PI Nov 2012 v8.0 21
Table 5: Treatment-Emergent Adverse Reactions: Incidence of 2% or More in MDD andGAD Placebo-Controlled TrialsPercentage of Patients Reporting ReactionSystem Organ Class / Adverse ReactionCymbalta(N=2995)Placebo(N=1955)Cardiac DisordersPalpitations 2^ 2Eye DisordersVision blurred 3 2Gastrointestinal DisordersNausea 25 9Dry mouth 15 6Diarrhea 10 7Constipation* 10 4Abdominal pain a 4 4Vomiting 5 2General Disorders and Administration SiteConditionsFatigue b 10 6InvestigationsWeight decreased* 2
abcdefghIjkAlso includes abdominal pain upper, abdominal pain lower, abdominal tenderness, abdominaldiscomfort, and gastrointestinal painAlso includes astheniaAlso includes anorexiaAlso includes hypersomnia and sedationAlso includes middle insomnia, early morning awakening, and initial insomniaAlso includes feeling jittery, nervousness, restlessness, tension, and psychomotor agitationAlso includes loss of libidoAlso includes anorgasmiaAlso includes nightmareMales patients onlyAlso includes ejaculation failure and ejaculation dysfunctionDiabetic Peripheral Neuropathic Pain — Table 6 gives the incidence oftreatment-emergent adverse events that occurred in 2% or more of patients treated withCymbalta in the premarketing acute phase of DPNP placebo-controlled trials (doses of20 to 120 mg/day) and with an incidence greater than placebo.Table 6: Treatment-Emergent Adverse Reactions Incidence of 2% or Morein DPNP Placebo-Controlled TrialsPercentage of Patients Reporting ReactionSystem Organ Class /Adverse ReactionCymbalta20 mg oncedaily(N=115)Cymbalta60 mg oncedaily(N=228)Cymbalta60 mg twicedaily(N=225)Placebo(N=223)Gastrointestinal DisordersNausea 14 22 30 9Constipation 5 11 15 3Diarrhea 13 11 7 6Dry mouth 5 7 12 4Vomiting 6 5 5 4Dyspepsia 4 4 4 3Loose stools 2 3 2 1General Disorders andAdministrationSite ConditionsFatigue 2 10 12 5Asthenia 2 4 8 1Pyrexia 2 1 3 1Infections and InfestationsNasopharyngitis 9 7 9 5Metabolism and Nutrition DisordersDecreased appetite 3 4 11
System Organ Class /Adverse ReactionPercentage of Patients Reporting ReactionCymbalta Cymbalta60 mg once 60 mg twicedaily daily(N=228) (N=225)Cymbalta20 mg oncedaily(N=115)Placebo(N=223)Nervous System DisordersSomnolence 7 15 21 5Headache 13 13 15 10Dizziness 6 14 17 6Tremor 0 1 5 0Psychiatric DisordersInsomnia 9 8 13 7Renal and Urinary DisordersPolyuria 3 1 5 2Reproductive System and BreastDisordersErectile dysfunction 1 0 1 4 0Respiratory, Thoracic andMediastinalDisordersCough 6 3 5 4Pharyngolaryngeal pain 3 1 6 1Skin and SubcutaneousTissue DisordersHyperhidrosis 6 6 8 21 Male patients only.The following additional adverse events were reported during placebo-controlled clinicaltrials of duloxetine for MDD or other indications in 8504 patients. Very common eventsare defined as those occurring in ≥10% of patients, common events are defined as thoseoccurring in ≥1% and
Gastrointestinal DisordersCommon: dyspepsia (including stomach discomfort), abdominal pain.Uncommon: eructation, gastroenteritis, stomatitis, halitosis, gastritis, flatulence,gastrointestinal haemorrhage, dysphagia.General Disorders and Administration Site ConditionsCommon: chills (including rigors).Uncommon: feeling abnormal, feeling hot and/or cold, malaise, thirst, falls (morecommon in the elderly (≥65 years old))..Rare: Gait disturbanceInfections and InfestationsUncommon: laryngitis.InvestigationsUncommon: blood pressure increased (including blood pressure systolic increased, bloodpressure diastolic increased), hepatic lab related findings (including alanineaminotransferase increased, hepatic enzyme increased, aspartate aminotransferaseincreased, liver function test abnormal, gamma-glutamyltransferase increased, bloodalkaline phosphatise increased, blood bilirubin increased), weight increased, bloodcholesterol increased.Duloxetine treatment in placebo-controlled clinical trials was associated with small meanincreases from baseline to endpoint in ALT, AST, CPK, and potassium; infrequent,transient, abnormal values were observed for these analytes in duloxetine-treated patients,compared with placebo-treated patients (see PRECAUTIONS).Metabolism and Nutrition DisordersUncommon: dehydration.Musculoskeletal and Connective Tissue DisordersCommon: musculoskeletal pain (including myalgia, neck pain), muscle spasm.Uncommon: muscle tightness (including musculoskeletal stiffness), muscle twitching.Nervous System DisordersVery common: headache (placebo rate was more than duloxetine rate in MDD trials).Common: lethargy, paraesthesia (including hypoaesthesia, hypoaesthesia facia andparasthesia oral).Uncommon: dysgeusia, disturbance in attention, dyskinesia, poor quality sleep.Rare: myoclonus.Psychiatric DisordersCommon: anxiety, sleep disorder, agitation (including feeling jittery, nervousness,restlessness, tension, psychomotor agitation).Uncommon: bruxism, disorientation (including confusional state), apathy, abnormaldreams (including nightmares).Cymbalta PI Nov 2012 v8.0 25
Renal and Urinary DisordersCommon: Urinary frequency.Uncommon: nocturia, urinary hesitation, urinary retention, dysuria, polyuria.Rare: urine odour abnormal, urine flow decreased.Reproductive System and Breast DisordersUncommon: ejaculation disorder (includes ejaculation dysfunction, ejaculation failure),sexual dysfunction, menopausal symptoms, testicular pain.Rare: Menstrual disorderRespiratory, Thoracic and Mediastinal DisordersCommon: yawning, oropharyngeal pain.Uncommon: throat tightnessSkin and Subcutaneous Tissue DisordersCommon: PruritusUncommon: night sweats, photosensitivity reaction, cold sweats, dermatitis contact,increased tendency to bruise.Vascular DisordersUncommon: flushing, peripheral coldness, orthostatic hypotension.Glucose Regulation—In three clinical trials of duloxetine for the treatment of diabeticneuropathic pain, the mean duration of diabetes was approximately 12 years, the meanbaseline fasting blood glucose was 176 mg/dL (9.78 mmol/L), and the mean baselinehaemoglobin A1c (HbA1c) was 7.81%. In the 12 week acute treatment phase of thesestudies, small increases in fasting blood glucose were observed in duloxetine-treatedpatients. HbA1c was stable in both duloxetine-treated and placebo-treated patients. Inthe extension phase of these studies, which lasted up to 52 weeks, there was an increasein HbA1c in both the duloxetine and routine care groups, but the mean increase was 0.3%greater in the duloxetine-treated group. There was also a small increase in fasting bloodglucose and in total cholesterol in duloxetine-treated patients while those laboratory testsshowed a slight decrease in the routine care group.Spontaneous DataThe following list of adverse drug reactions is based on post-marketing spontaneousreports involving use of duloxetine for any indication, and corresponding reporting rateshave been provided. Rare events are defined as those occurring in less than 1/1000patients; very rare events are those occurring in less than 1/10,000 patients.Endocrine disordersVery rare: Syndrome of inappropriate antidiuretic hormone (SIADH).Cardiac disordersVery rare: Supraventricular arrhythmia.Cymbalta PI Nov 2012 v8.0 26
Eye disordersVery rare: Glaucoma.Hepatobiliary disordersVery rare: Alanine aminotransferase (ALT) increased, alkaline phosphatase increased,aspartate aminotransferase (AST) increased, bilirubin increased.Very rare: Hepatitis, jaundice.Isolated cases of liver failure, including fatal cases, have been reported. A majority ofthese cases have been reported in patients with past or current risk factors for liver injury,including alcohol abuse, hepatitis or exposure to drugs with known adverse effects on theliver. (see PRECAUTIONS)Immune system disordersVery rare: Anaphylactic reaction, hypersensitivity.Metabolism and nutrition disordersVery rare: Hyponatraemia. Hyperglycaemia (reported especially in diabetic patients)Musculoskeletal and connective tissue disordersVery rare: Trismus.Nervous system disordersVery rare: Extrapyramidal disorder, paraesthia (including electric shock-like sensation)upon treatment discontinuation, serotonin syndrome, seizures, restless legs syndrome,seizures upon discontinuation.Psychiatric disordersRare: Hallucinations.Very rare: Mania, aggression and anger (particularly early in treatment or after treatmentdiscontinuations).Renal and urinary disordersRare: urinary retention.Reproductive system and breast disordersVery rare: Gynecological bleeding, galactorrhea, hyperprolactinemiaSkin and subcutaneous tissue disordersRare: Rash.Very rare: Angioneurotic oedema, Stevens-Johnson Syndrome, urticaria.Vascular disordersVery rare: Orthostatic hypotension (especially at the initiation of treatment), syncope(especially at initiation of treatment), hypertensive crisis.Cymbalta PI Nov 2012 v8.0 27
Adverse Events – causality not establishedVery rare cases of the following adverse events have been reported in post-marketingexperience, but no causal link between these events and duloxetine has been established.Abnormal bleeding events e.g. intracerebral, gastrointestinal; blood dyscrasias; cardiacevents e.g., myocardial infarction and ventricular arrhythmias; pancreatitis; renalimpairment; rhabdomyolysis; skin reactions especially in regards to subcutaneous tissuedisorderDiscontinuation SymptomsThe most commonly reported symptoms following abrupt or tapered discontinuation ofduloxetine in clinical trials have included dizziness, nausea, headache, paraesthesia,fatigue vomiting, irritability, nightmares, insomnia, diarrhoea, anxiety, hyperhidrosis,vertigo, somnolence and myalgia. (see PRECAUTIONS).DOSAGE AND ADMINISTRATIONMajor Depressive DisorderCYMBALTA should be administered for the treatment of major depressive disorder at adose of 60 mg once daily, with or without food. There is no adequate evidencesuggesting that patients not responding to 60 mg once daily will benefit from having theirdose increased.Diabetic Peripheral Neuropathic PainThe starting and maintenance dose of CYMBALTA in diabetic peripheral neuropathicpain is 60 mg once daily. As the progression of diabetic neuropathy is highly variableand management of pain is empirical, effectiveness of CYMBALTA should be assessedon an individual basis.Generalised Anxiety DisorderThe recommended starting dose of CYMBALTA in patients with generalized anxietydisorder is 30 mg once daily with or without food. The daily dose should be increased in30 mg increments until the minimum effective dose is achieved. The maximum dose is120 mg per day, given as 120 mg once daily. Doses above 120 mg have not beensystematically evaluated.Initial TolerabilityFor patients in whom initial tolerability may be a concern, such as treatment-naïvepatients or those with a history of adverse events with other medications, use of a lowerstarting dose such as 30 mg once daily for one week before increasing the dose to 60 mgonce daily should be considered. A dose of 30 mg once daily should be used in patientswith end stage renal disease (see below). In addition, clinical studies have shown thattaking CYMBALTA with food may improve initial tolerability.Discontinuation of treatmentWhen discontinuing CYMBALTA after more than one week of therapy it is generallyCymbalta PI Nov 2012 v8.0 28
ecommended that the dose be tapered to minimise the risk of discontinuation symptoms.As a general recommendation, the dose of CYMBALTA should be reduced by half oradministered on alternate days during a period of not less than two weeks. The preciseregimen followed should take into account the individual circumstances of the patient,such as duration of treatment, dose at discontinuation, etc.Renal ImpairmentA lower dose of 30 mg once daily should be used in patients with end stage renal disease(creatinine clearance < 30 mL/min) (see Pharmacokinetics).Hepatic ImpairmentCYMBALTA is contraindicated in patients with liver disease resulting in hepaticimpairment (see Pharmacokinetics).Patients aged ≥ 65 yearsNo dosage adjustment is recommended for elderly patients on the basis of age (seePharmacokinetics).Children and adolescents aged < 18 yearsDuloxetine is not indicated for use in patients under 18 years of age (seePRECAUTIONS)OVERDOSAGEOn the available evidence there is a wide margin of safety in overdose. In premarketingclinical trials, cases of acute ingestions up to 1400 mg, alone or in combination with otherdrugs, have been reported and have not been fatal. However in post marketingexperience, fatal outcomes have been reported for acute overdoses, primarily with mixedoverdoses, but also with duloxetine only, at doses as low as approximately 1000 mg. ..Signs and symptoms of overdose (most with mixed drugs) included serotonin syndrome,somnolence, vomiting and seizures.In animal studies, the major signs of overdose toxicity are related to the CNS and gastrointestinalsystems. Signs of toxicity include CNS effects such as tremors, clonicconvulsions, ataxia, emesis, and decreased appetite.Management of Overdose - No specific antidote is known, but if serotonin syndromeensues, specific treatment (such as with cyproheptadine and/or temperature control) maybe considered. An airway should be established. Monitoring of cardiac and vital signs isrecommended, along with appropriate symptomatic and supportive measures. Activatedcharcoal may be useful in limiting absorption. Duloxetine has a large volume ofdistribution and forced diuresis, haemoperfusion, and exchange perfusion are unlikely tobe beneficial.Contact your local Poisons Information Centre for information on the management ofoverdose with duloxetine.Cymbalta PI Nov 2012 v8.0 29
PRESENTATIONCapsules containing 30 mg and 60 mg duloxetine (as hydrochloride) in packs of 7 (starterpacks) and 28.The 30 mg capsule has an opaque white body and opaque blue cap imprinted with “9543”and “30 mg” using green ink.The 60 mg capsule has an opaque green body and opaque blue cap imprinted with “9542”and “60 mg” using white ink.Store below 25°CPoisons Schedule S4Name and Address of SponsorEli Lilly Australia Pty. Limited112 Wharf RoadWEST RYDE NSW 2114TGA Approval:15 July 2009Date of most recent amendment19 November 2012Cymbalta PI Nov 2012 v8.0 30