Abdominal Wall Defects - Department of Surgery at SUNY ...
Abdominal Wall Defects - Department of Surgery at SUNY ...
Abdominal Wall Defects - Department of Surgery at SUNY ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
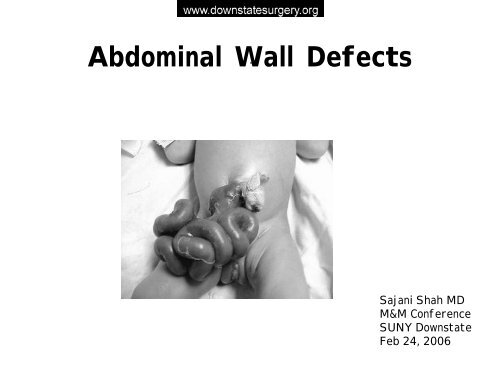
<strong>Abdominal</strong> <strong>Wall</strong> <strong>Defects</strong>-Sajani Shah MDM&M Conference<strong>SUNY</strong> Downst<strong>at</strong>eFeb 24, 2006
Case Present<strong>at</strong>ionHX: Pt is a 36 week gest<strong>at</strong>ional age maleborn via C-section Cdelivery with a dx <strong>of</strong>gastroschisis made on a pren<strong>at</strong>alultrasound <strong>at</strong> 15 weeks.M<strong>at</strong>ernal Hx: xx year old female G 0010,denies any medical problems.Meds:Tylenol for pain. Denies aspirin,ibupr<strong>of</strong>en or any OTC meds.Denies smoking or illicit drug use
Case Present<strong>at</strong>ionPE:Vitals: T 99 P 140 RR 45CVS:S1, S2 no murmurLungs:CTA B/LAbd:S<strong>of</strong>t, 4 cm defect to the right<strong>of</strong> the umbilical cordcontaining bowel. The bowel isthick, m<strong>at</strong>ted and edem<strong>at</strong>ous.Ext:no deformity
Hospital Course• Delivered via C-sectionC• Intub<strong>at</strong>ed with NGT Decompression• Saline soaked gauze wrapped aroundintestine.• OR for placement <strong>of</strong> spring loaded silo• Taken to NICU• IV Abx• IVF• Incub<strong>at</strong>or
• DOL#1• DOL#1-8• DOL#9-11• DOL#12Hospital CourseSurgical placement <strong>of</strong>spring loaded siloPlaced in incub<strong>at</strong>or, TPN,bowel reduction, mildlysed<strong>at</strong>ed11 Paralyzed baby. Freed upfilmy adhesion <strong>of</strong> bowel t<strong>of</strong>asciaTaken to OR. Silo removedand fascia closed withsilastic p<strong>at</strong>ch.
Hospital Course• DOL#44Taken back to OR forremoval <strong>of</strong> mesh andclosure <strong>of</strong> skinCurrently in NICU slowly toler<strong>at</strong>ing feeds
Gastroschisis
GastroschisisDefinition:• Deformity caused by involution <strong>of</strong> secondary umbilicalvein and results in a full thickness defect <strong>of</strong> theabdominal wall to the right <strong>of</strong> the umbilical cord.• Herni<strong>at</strong>ion <strong>of</strong> small bowel and large bowel• The loops <strong>of</strong> intestine lie uncovered in the amnioticfluid and become thickened, edem<strong>at</strong>ous and m<strong>at</strong>ted.
Gastroschisis•Incidence Incidence 1 in 10,000•Infrequent Infrequent congenital malform<strong>at</strong>ions•High High associ<strong>at</strong>ion prem<strong>at</strong>urity•Herni<strong>at</strong>ed Herni<strong>at</strong>ed contents rarely liver•Associ<strong>at</strong>ed cryptorchidism – 30%•Intestinal Intestinal <strong>at</strong>resia bowel common- 10%
Risk Factors• 4X more common in women < 20 years <strong>of</strong> age• Smoking• Stressed and undernourished mothers• Over the counter meds: Vasoactive propertiespseudoephedrine, aspirin, ephedrine• Multifactorial
Main Consequences <strong>of</strong>Gastroschisis• Perivisceritis• Short Gut Syndrome• Intestinal Atresia
Prevalence <strong>of</strong> Gastroschisis in the USPrevalence is calcul<strong>at</strong>ed by dividing the number <strong>of</strong>affected people by the total popul<strong>at</strong>ion.Prev. per 10,000 births• 0.00-1.4• 1.5-2.9• 3.0-4.4• 4.5+D<strong>at</strong>a from the Metropolitan Atlanta Congenital <strong>Defects</strong> Program, 2004.
Gastroschisis by Race5Prevalence per 10,00043210White Black Hispanic OtherRaceSource: 2003 Congenital Malform<strong>at</strong>ions Surveillance Report: A Report from theN<strong>at</strong>ional Birth <strong>Defects</strong> Prevention Network. Birth <strong>Defects</strong> Research (Part A):Clinical and Molecular Ter<strong>at</strong>ology. New York: Wiley-Liss; 2003.
Gastroschisis by M<strong>at</strong>ernal6AgePrevalence per 10,000543210=35M<strong>at</strong>ernal AgeSource: The Metropolitan Atlanta Congenital <strong>Defects</strong> Program, 2004.
Diagnosis <strong>of</strong> GastroschisisBefore BirthExcess amniotic fluidUltrasoundM<strong>at</strong>ernal serum alpha-fetoprotein levelselev<strong>at</strong>edAfter BirthVisible
Fetal Ultrasound
Tre<strong>at</strong>ment• Immedi<strong>at</strong>ely after birth exposedpart it wrapped in sterile salinesoaked gauze.• Tx: plastic “silo” slowlycompressed over the next week•Surgical closure <strong>of</strong> the defect .•Infants are feed TPN for 2-5weeks until normal bowel functionbegins
Postn<strong>at</strong>al Care• Consider<strong>at</strong>ion for third-space fluid losses• Nutrition- albumin• Risk <strong>of</strong> Infection- Antibiotics• Intestine <strong>of</strong>ten thickened:• Damage form amniotic fluid• Ischemia from constricting wall defect• Incub<strong>at</strong>or- temper<strong>at</strong>ure control• Respir<strong>at</strong>ory Compromise
Surgical Options for Tre<strong>at</strong>ment• Primary Closure• +/- Mesh• Staged closure with• Spring loaded Silo• Dacron reinforced Silastic Sheet- Sutured tomedial aspect <strong>of</strong> rectus fascia
Silo PlacementSilastic siloto conserve he<strong>at</strong>and prevent infection.
Surgical Managementfor Intestinal Atresia• Intestinal Atresia• Bowel placed into abdomen and plan for reoper<strong>at</strong>ion• Distal <strong>at</strong>resia perform a proximal diverting stoma• Proximal <strong>at</strong>resia- Nasogastric Decompression• Primary Anastomosis- not advised
Complic<strong>at</strong>ions• Deceased venous return• <strong>Abdominal</strong> Compartment Syndrome• Decreased Pulmonary Compliance• Renal Failure• Necrotizing Enterocolitis
“The Gentle Touch”• Tre<strong>at</strong>ed 52 babies with gastroschisis• Used “gentle touch” approach vs manual reduction• Fascial Closure 5.5 days vs 7 days• Feeding 11 to 24 days vs 12 to 30 days• TPN cess<strong>at</strong>ion in 23 days vs• Conclusions: Gravity reduction <strong>of</strong> intestine in babieswith gastroschisis is both gentle and effectiveJona JZ. The ‘gentle touch’ technique in the tre<strong>at</strong>ment <strong>of</strong> gastroschisis. J Pedi<strong>at</strong>ric Surg 2003;38:1036
“Gentle Touch” Protocol• Vaginal Delivery and ET Intub<strong>at</strong>ion• Gastric and Colonic Decompression• Broad Spectrum IV Abx• Sed<strong>at</strong>ion• Placement <strong>of</strong> Silo• Gravity Based Bowel reduction• Delayed Primary Fascial Closure• TPN until bowel function returnsJona JZ. The ‘gentle touch’ technique in the tre<strong>at</strong>ment <strong>of</strong> gastroschisis. J Pedi<strong>at</strong>ric Surg 2003; 38:1036
Omphalocele
Omphalocele• Incidence 2.5 in 10,000• Results from failure <strong>of</strong> normal embryonicregression <strong>of</strong> the mid-gut from the umbilicalstalk into the abdominal cavity.• Can include intestines liver or spleen coveredby a sac <strong>of</strong> parietal peritoneum and amnion-which can rupture• Herni<strong>at</strong>es into the base <strong>of</strong> the umbilical cord.
Embryology• 6 th wk – midgut loopelong<strong>at</strong>es and herni<strong>at</strong>es outthrough umbilical cord• Midgut rot<strong>at</strong>es 270 degrees• Returns to abdomen by 10 thwk• Anterior abdominal wallprogressively closes leavingonly umbilical ring
EtiologyThree Theories:1. Persistence <strong>of</strong> the primitive body stalk2. Failure <strong>of</strong> the bowel to return to theabdomen,3. Failure <strong>of</strong> complete l<strong>at</strong>eral-body foldmigr<strong>at</strong>ion and body wall closure
Omphalocele• Associ<strong>at</strong>ed Abnormalities in 60%• Cardiac, Renal, Limb and facial anomalies• Genetic Syndromes- Pentalogy <strong>of</strong> Cantrell,Beckwith-Wiedemann• Associ<strong>at</strong>ed with Trisomy 13, 14 , 15, and 18• Small Omphalocele without liver-Chromosomal abnormalities
Diagnosis• Ultrasound• M<strong>at</strong>ernal Serum AFP
• Most omphaloceles occur sporadically• Small Omphalocele < 5cm• Large Omphalocele >5cm :• Pulmonary Hypoplasia-High mortality
Evalu<strong>at</strong>ion• An amniocentesis for karyotype isperformed on all fetuses with ompahlocele• Search for other anomalies takes priorityover repair <strong>of</strong> omphalocele• Chest xray, echo, renal US• Pulmonary Hypoplasia may preclude closure
ASSOCIATED MALFORMATIONSWith Omphalocele•Upper Upper Midline Syndrome•Lower Lower Midline Syndrome•Beckwith-Wiedemann Syndrome
UPPER MIDLINE SYNDROME•Pentalogy <strong>of</strong> Cantrell•Sternal Sternal defect•Ectopia Ectopia cordis•Pericardial and cardiac defects•Diaphragm<strong>at</strong>ic defect•Omphalocele
LOWER MIDLINE SYNDROME•Vesiculointestinalfistula•Imperfor<strong>at</strong>e anus•Colonic Colonic agenesis•Bladder Bladder extrophy•Omphalocele
Som<strong>at</strong>ic GigantismHemihyperplasiaMacroglossiaVisceromegalyOmphaloceleEar creases/pitsHypoglycemiaTumoursBeckwith-Wiedemann SyndromeClinical Fe<strong>at</strong>ures
Surgical Repair• Small defects (
Surgical Repair• For moder<strong>at</strong>e to large defects (2 to 9 cm) place aDacron-reinforced reinforced silastic silo as a temporarycover for the bowel.• The silo can be reduced gradually over 3 to 7days in the intensive care unit, after which theinfant is returned to the oper<strong>at</strong>ing room for finalclosure <strong>of</strong> the abdominal wall
• Reducing a large defect or one th<strong>at</strong> containsliver can be done with Doppler ultrasoundguidance• Escharific<strong>at</strong>ion:extremely large (>10 cm) lesion or aprem<strong>at</strong>ure infant having respir<strong>at</strong>orydifficulties, a topical sclerosing agent can beused as a temporary measure until definitivetherapy can be performed on a more stablep<strong>at</strong>ient.
Prognosis• Gastroschisis: : Overall survival is 90%Low survival if associ<strong>at</strong>ed with intestinal <strong>at</strong>resia• Omphalocele: Mortality increased if associ<strong>at</strong>edwith chromosome syndrome or cardiac defect.Giant Omphalocele associ<strong>at</strong>ed with pulmonaryhypoplasia: worse prognosis
ConclusionsDefectDefect SizeUmbilical CordBowelAliment<strong>at</strong>ionAssocAnomaliesGastroschisisOpen2-5cmLeft <strong>of</strong> defectSerositis, edemaDelayed10%OmphaloceleMembraneCovered1-15cm15cmCenter <strong>of</strong>membraneNormalNormal60%
The End