PPO PLANS - Aetna Medicare
PPO PLANS - Aetna Medicare
PPO PLANS - Aetna Medicare
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
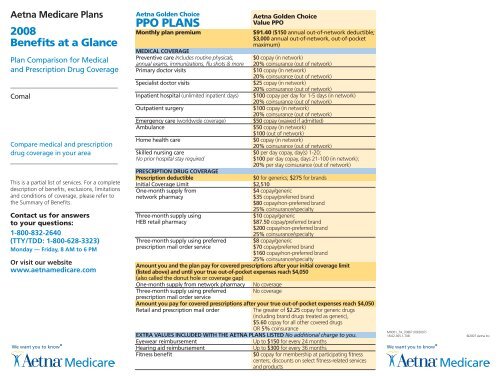
<strong>Aetna</strong> <strong>Medicare</strong> Plans2008Benefits at a GlancePlan Comparison for Medicaland Prescription Drug CoverageComalCompare medical and prescriptiondrug coverage in your areaThis is a partial list of services. For a completedescription of benefits, exclusions, limitationsand conditions of coverage, please refer tothe Summary of Benefits.Contact us for answersto your questions:1-800-832-2640(TTY/TDD: 1-800-628-3323)Monday — Friday, 8 AM to 6 PMOr visit our websitewww.aetnamedicare.com<strong>Aetna</strong> Golden Choice<strong>PPO</strong> <strong>PLANS</strong>Monthly plan premiumMedical CoveragePreventive care Includes routine physicals,annual exams, immunizations, flu shots & morePrimary doctor visits<strong>Aetna</strong> Golden ChoiceValue <strong>PPO</strong>$91.40 ($150 annual out-of-network deductible;$3,000 annual out-of-network, out-of-pocketmaximum)$0 copay (in network)20% coinsurance (out of network)$10 copay (in network)20% coinsurance (out of network)Specialist doctor visits$25 copay (in network)20% coinsurance (out of network)Inpatient hospital (unlimited inpatient days) $100 copay per day for 1-5 days (in network)20% coinsurance (out of network)Outpatient surgery$100 copay (in network)20% coinsurance (out of network)Emergency care (worldwide coverage) $50 copay (waived if admitted)Ambulance$50 copay (in network)$100 (out of network)Home health care$0 copay (in network)20% coinsurance (out of network)Skilled nursing care$0 per day copay, day(s) 1-20;No prior hospital stay required$100 per day copay, days 21-100 (in network);20% per stay coinsurance (out of network)Prescription Drug CoveragePrescription deductible$0 for generics; $275 for brandsInitial Coverage Limit $2,510One-month supply fromnetwork pharmacyThree-month supply usingHEB retail pharmacyThree-month supply using preferredprescription mail order service$4 copay/generic$35 copay/preferred brand$80 copay/non-preferred brand25% coinsurance/specialty$10 copay/generic$87.50 copay/preferred brand$200 copay/non-preferred brand25% coinsurance/specialty$8 copay/generic$70 copay/preferred brand$160 copay/non-preferred brand25% coinsurance/specialtyAmount you and the plan pay for covered prescriptions after your initial coverage limit(listed above) and until your true out-of-pocket expenses reach $4,050(also called the donut hole or coverage gap)One-month supply from network pharmacy No coverageThree-month supply using preferred No coverageprescription mail order serviceAmount you pay for covered prescriptions after your true out-of-pocket expenses reach $4,050Retail and prescription mail orderThe greater of $2.25 copay for generic drugs(including brand drugs treated as generic),$5.60 copay for all other covered drugsOR 5% coinsuranceExtra values included with the <strong>Aetna</strong> plans listed No additional charge to you.Eyewear reimbursementHearing aid reimbursementFitness benefitUp to $150 for every 24 monthsUp to $300 for every 36 months$0 copay for membership at participating fitnesscenters; discounts on select fitness-related servicesand productsM0001_7A_70867 (09/2007)18.02.365.1-TX8©2007 <strong>Aetna</strong> Inc.
Access to Thousands of Hospitals,Doctors and SpecialistsThe <strong>Aetna</strong> Golden <strong>Medicare</strong> Plan and <strong>Aetna</strong>Golden Choice Plan provide you with accessto a large number of top doctors and hospitals— locally or around the country where theseplans are available. So even if you are travelingor away from home, if an <strong>Aetna</strong> Golden<strong>Medicare</strong> Plan or <strong>Aetna</strong> Golden Choice Plannetwork provider is available, you’ll payyour low in-network cost sharing*. Findinga provider is easy. Search online at www.aetnamedicare.com or call Member Servicesto get help locating a provider in your area.*HMO members may be required to enrollin the U.S. Travel Advantage Program priorto seeking care out of their service area.See your plan materials for details.More Options in Your AreaThere may be additional options available.Please contact an <strong>Aetna</strong> <strong>Medicare</strong> Specialistto review the plans in your area.All-in-One <strong>Medicare</strong> PlanCoverage has its AdvantagesWhen you enroll in a plan listed, you get one<strong>Aetna</strong> <strong>Medicare</strong> member identification (ID)card and one phone number to call if youneed help. Plus, our plans do not requirea lot of complicated paperwork or claimforms. Using your medical coverage, havinga prescription filled, or taking advantageof the discounts and extra values our plansoffer is simple.Wide Flexibility in ChoosingProvidersWith the <strong>Aetna</strong> Golden Choice Plan, youhave the freedom to choose to use eithernetwork providers at lower out-of-pocketcosts, or out-of-network at a highercost-sharing level. Save more with alower copayment when you select aprimary care physician (PCP) from the<strong>Aetna</strong> Golden Choice network.Remember that you are covered when youaccess care outside the <strong>Aetna</strong> network, butthere are higher out-of-pocket costs that youmay have to pay. For example, after you havemet your annual deductible, you will continueto pay coinsurance when you visit out ofnetwork providers. Once you reach the annualcoinsurance maximum amount, coveredservices will be paid at 100%. Certain serviceslike your deductible, <strong>Medicare</strong> prescriptiondrug benefits, eyewear, hearing aids,and any optional benefits do not applytowards the annual maximum coinsuranceamount. Please review the Summary ofBenefits for more information.Benefits coverage is provided by <strong>Aetna</strong> Health Inc.,<strong>Aetna</strong> Health of California Inc. and/or <strong>Aetna</strong> Healthof Illinois Inc., which are <strong>Medicare</strong> Advantageorganizations with a <strong>Medicare</strong> contract and benefits,limitations, service areas and premiums are subjectto change on January 1 of each year.This material is for informational purposes only. Notall health services are covered. See plan documentsfor a complete description of benefits, exclusions,limitations and conditions of coverage. Plan featuresand availability may vary by location and are subjectto change. <strong>Aetna</strong> receives rebates from drugmanufacturers that may be taken into account indetermining <strong>Aetna</strong>’s Preferred Drug List. Rebatesdo not reduce the amount a member pays thepharmacy for covered prescriptions. Pharmacy clinicalprograms such as pre-certification, step therapy, andquantity limits may apply to your prescription drugcoverage. Providers are independent contractorsand are not agents of <strong>Aetna</strong>. Provider participationmay change without notice. <strong>Aetna</strong> does not providecare or guarantee access to health services. Healthinformation programs provide general healthinformation and are not a substitute for diagnosisor treatment by a physician or other health careprofessional. Discount programs provide access todiscounted prices and are not insured benefits.You must be entitled to <strong>Medicare</strong> Part A andcontinue to pay your Part B premium and Part A, ifapplicable.For the <strong>Aetna</strong> Golden <strong>Medicare</strong> Plan: You mustuse network providers except for emergent care orout-of-area urgent care/renal dialysis.For the <strong>Aetna</strong> Golden Choice Plan: Higher costsapply for out-of-network services. Precertification, orprior approval of coverage, is requested for certainservices. Providers must be licensed and eligibleto receive payment under the federal <strong>Medicare</strong>program.While this material is believed to be accurate as ofthe print date, it is subject to change.Translation of this material into another languagemay be available. For assistance, please callMember Services at 1-800-832-2640 (TTY/TDD:1-800-628-3323), Monday through Friday, 8 a.m.to 6 p.m.Puede estar disponsible la traduccion de estematerial en otro idioma. Por favor, para ayuda llamea Servicios al Miembro al 1-800-832-2640 (TTY/TDD:1-800-628-3323), de Lunes a Viernes de 8 a.m.to 6 p.m.



![[PDF] Directory - Aetna Medicare](https://img.yumpu.com/50361210/1/190x247/pdf-directory-aetna-medicare.jpg?quality=85)