February 2011 PDF - Thoracic Surgery News
February 2011 PDF - Thoracic Surgery News
February 2011 PDF - Thoracic Surgery News
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
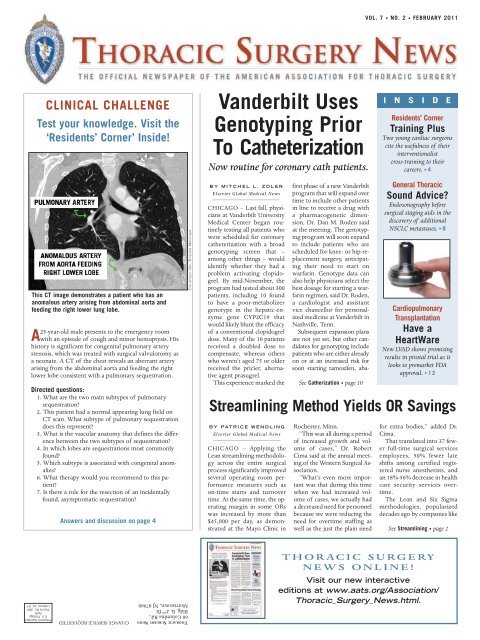
VOL. 7 • NO. 2 • FEBRUARY <strong>2011</strong>CLINICAL CHALLENGETest your knowledge. Visit the‘Residents’ Corner’ Inside!Vanderbilt UsesGenotyping PriorTo CatheterizationNow routine for coronary cath patients.I N S I D EResidents’ CornerTraining PlusTwo young cardiac surgeonscite the usefulness of theirinterventionalistcross-training to theircareers. • 4This CT image demonstrates a patient who has ananomalous artery arising from abdominal aorta andfeeding the right lower lung lobe.A25-year-old male presents to the emergency roomwith an episode of cough and minor hemoptysis. Hishistory is significant for congenital pulmonary arterystenosis, which was treated with surgical valvulotomy asa neonate. A CT of the chest reveals an aberrant arteryarising from the abdominal aorta and feeding the rightlower lobe consistent with a pulmonary sequestration.Directed questions:1. What are the two main subtypes of pulmonarysequestration?2. This patient had a normal appearing lung field onCT scan. What subtype of pulmonary sequestrationdoes this represent?3. What is the vascular anatomy that defines the differencebetween the two subtypes of sequestration?4. In which lobes are sequestrations most commonlyfound?5. Which subtype is associated with congenital anomalies?6. What therapy would you recommend to this patient?7. Is there a role for the resection of an incidentallyfound, asymptomatic sequestration?Answers and discussion on page 4COURTESY DR. STEVEN MENTZERBY MITCHEL L.ZOLERElsevier Global Medical <strong>News</strong>CHICAGO – Last fall, physiciansat Vanderbilt UniversityMedical Center began routinelytesting all patients whowere scheduled for coronarycatheterization with a broadgenotyping screen that –among other things – wouldidentify whether they had aproblem activating clopidogrel.By mid-November, theprogram had tested about 300patients, including 10 foundto have a poor-metabolizergenotype in the hepatic-enzymegene CYP2C19 thatwould likely blunt the efficacyof a conventional clopidogreldose. Many of the 10 patientsreceived a doubled dose tocompensate, whereas otherswho weren’t aged 75 or olderreceived the pricier, alternativeagent prasugrel.This experience marked theBY PATRICE WENDLINGElsevier Global Medical <strong>News</strong>CHICAGO – Applying theLean streamlining methodologyacross the entire surgicalprocess significantly improvedseveral operating room performancemeasures such ason-time starts and turnovertime. At the same time, the operatingmargin in some ORswas increased by more than$45,000 per day, as demonstratedat the Mayo Clinic infirst phase of a new Vanderbiltprogram that will expand overtime to include other patientsin line to receive a drug witha pharmacogenetic dimension,Dr. Dan M. Roden saidat the meeting. The genotypingprogram will soon expandto include patients who arescheduled for knee- or hip-replacementsurgery, anticipatingtheir need to start onwarfarin. Genotype data canalso help physicians select thebest dosage for starting a warfarinregimen, said Dr. Roden,a cardiologist and assistantvice chancellor for personalizedmedicine at Vanderbilt inNashville, Tenn.Subsequent expansion plansare not yet set, but other candidatesfor genotyping includepatients who are either alreadyon or at an increased risk forsoon starting tamoxifen, aba-See Catherization • page 10Streamlining Method Yields OR SavingsRochester, Minn.“This was all during a periodof increased growth and volumeof cases,” Dr. RobertCima said at the annual meeting.ofthe Western Surgical Association.“What’s even more importantwas that during this timewhen we had increased volumeof cases, we actually hada decreased need for personnelbecause we were reducing theneed for overtime staffing aswell as the just the plain needGeneral <strong>Thoracic</strong>Sound Advice?Endosonography beforesurgical staging aids in thediscovery of additionalNSCLC metastases. • 8CardiopulmonaryTransplantationHave aHeartWareNew LVAD shows promisingresults in pivotal trial as itlooks to premarket FDAapproval. • 12for extra bodies,” added Dr.Cima.That translated into 37 fewerfull-time surgical servicesemployees, 50% fewer lateshifts among certified registerednurse anesthetists, andan 18%-56% decrease in healthcare security services overtime.The Lean and Six Sigmamethodologies, popularizeddecades ago by companies likeSee Streamlining • page 2Presorted StandardU.S. PostagePAIDPermit No. 384Lebanon Jct. KYTHORACIC SURGERY NEWS CHANGE SERVICE REQUESTED60 Columbia Rd.,Bldg. B, 2 nd flr.Morristown, NJ 07960THORACIC SURGERYNEWS ONLINE!Visit our new interactiveeditions at www.aats.org/Association/<strong>Thoracic</strong>_<strong>Surgery</strong>_<strong>News</strong>.html.
2 NEWS FEBRUARY <strong>2011</strong> • THORACIC SURGERY NEWSGoing Lean for <strong>Surgery</strong>Streamlining • from page 1automobile maker Toyota as a way toeliminate wasteful steps and improveproductivity, have typically been appliedto a limited number of ORs or to specificoperations.The Mayo Clinic credits its success toapplying the methodology across theentire surgical process and in all 88 of itsmain ORs performing both in- and outpatientprocedures.“Multiple areas of redundantor non–value-added stepswere identified across the entireprocess flow that wouldnot have been identified witha focus on specific steps,” saidDr. Cima, a colorectal surgeonat the Mayo Clinic.First, a multidisciplinary leadershipteam developed a map ofthe surgical process from thedecision for surgery to leavingthe OR. The team analyzedeach step for personnel required,information process,and time expended. In all, 28systems and 14 points of delaywere identified, he said.Next, multidisciplinary teamswere formed and given 6months to redesign systemsaround five essential work streams: minimizingunplanned surgical volume variation,streamlining the preoperativeprocess, reducing nonoperative time, reducingredundant information collection,and engaging employees.“Specific goals were set for each specialty,”he said. “It was not ‘one size fitsall.’”Each work stream was tweaked tostandardize procedure descriptions, implementdedicated staggered surgerystart times, and develop a first-casescheduling checklist to eliminate barriersto on-time OR starts.When streamlining the preoperativeprocess, Dr. Cima said, the most importantthing is to start on time.AMERICAN ASSOCIATION FOR THORACIC SURGERYEditor Yolonda L. Colson, M.D., Ph.D.Associate Editor, General <strong>Thoracic</strong>Michael J. Liptay, M.D.Associate Editor, Adult Cardiac John G. Byrne, M.D.Associate Editor, Cardiopulmonary TransplantRichard N. (Robin) Pierson III, M.D.Associate Editor, Congenital Heart William G. Williams, M.D.Executive Director Elizabeth Dooley Crane, CAE, CMPAssociate Executive Director Cindy VerColenEditorial Associate Lisl K. JonesResident Editor Stephanie Mick, M.D.Resident Editor Christian Peyre, M.D.THORACIC SURGERY NEWS is the official newspaper of the American Associationfor <strong>Thoracic</strong> <strong>Surgery</strong> and provides the thoracic surgeon with timely andrelevant news and commentary about clinical developments and aboutthe impact of health care policy on the profession and on surgical practicetoday. Content for THORACIC SURGERY NEWS is provided by InternationalMedical <strong>News</strong> Group and Elsevier Global Medical <strong>News</strong>. Content for the<strong>News</strong> From the Association is provided by the American Association for<strong>Thoracic</strong> <strong>Surgery</strong>.The ideas and opinions expressed in THORACIC SURGERY NEWS do notnecessarily reflect those of the Association or the Publisher. TheAmerican Association for <strong>Thoracic</strong> <strong>Surgery</strong> and Elsevier Inc., will notassume responsibility for damages, loss, or claims of any kind arisingfrom or related to the information contained in this publication,including any claims related to the products, drugs, or servicesmentioned herein.“It is a collaborative effort,” said Dr. RobertCima of the Mayo Clinic.THORACIC SURGERY NEWSPOSTMASTER: Send changes of address (with old mailing label) toCirculation, THORACIC SURGERY NEWS, 60 B Columbia Rd., 2 nd flr.,Morristown, NJ 07960.The American Association for <strong>Thoracic</strong> <strong>Surgery</strong> headquarters islocated at 900 Cummings Center, Suite 221-U, Beverly, MA01915.THORACIC SURGERY NEWS (ISSN 1558-0156) is published bimonthly forthe American Association for <strong>Thoracic</strong> <strong>Surgery</strong> by Elsevier Inc., 60B Columbia Rd., 2 nd flr., Morristown, NJ 07960, 973-290-8200,fax 973-290-8250.Display Advertising Manager Betty Ann Gilchrist, 203-938-3156, fax 203-938-3570, bettyann@gilchristmedia.comClassified Sales Manager Robert Zwick 973-290-8226,fax 973-290-8250, r.zwick@elsevier.comCOURTESY MAYO FOUNDATION FOR MEDICAL EDUCATION AND RESEARCHThe hospital tried to get buy-in fromemployees by implementing OR briefingswith the OR team, creating a communicationcouncil to effectivelydisseminate information through alllevels of staff, and conducting a surveyto identify major drivers of employeeparticipation – many of which were notfinancial, Dr. Cima noted.Some of the drivers included promotionof shared goals, encouragementof continuous professionalgrowth, frequent recognition of individualemployee contributions, and executivedemonstration of values andcommitment to the project.Data collected before the interventionand 18 months afterward from thefirst three specialties tested showedthat on-time starts increased from 50%to 80% for thoracic surgery, from 64%to 92% for gynecologic surgery, andfrom 60% to 92% for general/colorectalsurgery.The differences were all significant (Pless than .05), he said.The percentage of operations performedpast 5 p.m. stayed relatively constantbefore and after interventionamong thoracic surgeons at 34% vs.36%, respectively. However, it decreasedsignificantly for gynecologic surgeons(from 42% to 36%) and general/colorectalsurgeons (from 37% to 31%) (Pless than .05 for both).The average nonoperative or turnovertime was reduced by 10-15 minutesamong the three specialties, or 25% forthoracic surgery, 43% for gynecologicsurgery, and 32% for general/colorectalsurgery, Dr. Cima said.Staff overtime was reduced by an averageof 17 minutes per month for thoracicsurgery (16%), 19 minutes forgynecologic surgery (18%), and 46 minutesfor general/colorectal surgery(53%).The financial impact of these improvementswas at times quite dramatic,he said.For example, the financial margin increased22% or $21,340 per OR/day forthoracic surgery, 16% or $24,570 perOR/day for gynecologic surgery, and55% and $47,700 per OR/day for general/colorectalsurgery.“Some people say this is a Hawthorneeffect . . . but this is sustainable and insome cases actually increases as theteams become more efficient,” he said,noting that positive improvements havenow been reported in nine separate specialties.Invited discussant Dr. R. StephenSmith called the project a “monumentaleffort,” but questioned whether themethodology is applicable to the averageworker in the average hospital.“Surgeons and others who toil in theoperating room are not analogous toToyota assembly line workers in Japan,”according to Dr. Smith, interim chair,department of surgery, Virginia TechCarilion School of Medicine inRoanoke.He also questioned how less affluentinstitutions could marshal the hospitalwideresources necessary to instituteLean/Six Sigma projects.Dr. Cima responded that the projectrequired very few resources, and thatAddress Changes Fax change of address (with old mailing label)to 973-290-8245 or e-mail change to subs@elsevier.comAdvertising Offices 60 B Columbia Rd., 2 nd flr., Morristown, NJ07960, 973-290-8200, fax 973-290-8250ELSEVIER SOCIETY NEWS GROUP, A DIVISION OFINTERNATIONAL MEDICAL NEWS GROUPPresident, IMNG Alan J. ImhoffDirector, ESNG Mark BrancaEditor in Chief Mary Jo M. DalesExecutive Editors Denise Fulton, Kathy ScarbeckManaging Editor Mark S. LesneyCirculation Analyst Barbara Cavallaro, 973-290-8253,b.cavallaro@elsevier.comExecutive Director, Operations Jim ChiccaDirector, Production and Manufacturing Yvonne Evans StrussProduction Manager Judi ShefferCreative Director Louise A. Koenigsmaller institutions actually may be in abetter position to implement Lean/SixSigma because they are less constrainedby bureaucracy.Dr. Cima acknowledged that the hospitalpopulation may be unique in itscommitment to the success of the overallinstitution, as opposed to individualproductivity, but added that there areadvantages for the employees to cometogether in smaller settings such as inambulatory, outpatient surgical practices.USING LEAN METHODOLOGY,THEFINANCIAL MARGIN INCREASEDBY 22% OR $21,340 PEROPERATING ROOM/DAY FORTHORACIC SURGERY.For example, surgeons may be able toreturn to the clinic earlier and see morecases if the surgical suite is run more efficiently.“One of the efforts that has to bebrought out to bring people together isto make sure everyone knows what theywant out of it and what they are willingto give up,” Dr. Cima said. “It is a collaborativeeffort.”During the discussion, Dr. TylerHughes, from Memorial Hospital inMcPherson, Kan., asked whether institutionscan survive if they don’t pushthrough these kinds of process improvements.“I would submit that any institutionthat doesn’t look at their processes – andnot just a step, but the whole process –will not be able to survive the next 10-15 years,” Dr. Cima responded.“The government is clearly sending asignal that efficiency, value, and safetyare the three main ways you’re going tosurvive.”The study was supported by the MayoClinic, department of surgery. Dr. Cimaand Dr. Smith reported no conflicts of interest.■EDITORIAL OFFICES 5635 Fishers Lane, Suite 6000, Rockville, MD 20852,240-221-4500, fax 240-221-2541. Letters to the Editor:aats@prri.com©Copyright <strong>2011</strong>, by the American Association for <strong>Thoracic</strong> <strong>Surgery</strong>
FEBRUARY <strong>2011</strong> • THORACIC SURGERY NEWS NEWS 3Never Say ‘Never’: Surgical Errors Remain a ConcernBY JEFFREY S.EISENBERGElsevier Global Medical <strong>News</strong>The following articles are featured fromthe <strong>February</strong> <strong>2011</strong> issue of the Journalof <strong>Thoracic</strong> and Cardiovascular <strong>Surgery</strong>.Presidential AddressWTSA 2010: BiggerJ. Scott MillikanEditorialJoint Council on <strong>Thoracic</strong> SurgicalEducation: An investment in our futureEdward D. VerrierAcquired Cardiovascular DiseaseMidterm results with thoracic endovascularaortic repair for chronictype B aortic dissection with associatedaneurysmCyrus J. Parsa,, Judson B.Williams,, SyamalD. Bhattacharya, et. al.The present study examines midtermresults with thoracic endovascular aorticrepair (TEVAR) for chronic (>2weeks) type B aortic dissection with associateddescending aneurysm. The resultsdemonstrate that TEVAR is safeand effective at midterm follow-up, althoughlonger-term followup is neededto determine the durability ofThe frequency of surgical complicationsinvolving a wrong site orwrong patient remains high, even inthe era of the Universal Protocol.The Joint Commission introduced theUniversal Protocol to ensure the correctpatient, site, and procedure. Although itbecame effective July 1, 2004, there stillexists a lack of data about the true incidenceof wrong-patient and wrong-siteoperations, called “never events,” accordingto new research.To determine the frequency, rootcauses, and outcomes of these neverevents, Dr. Philip F. Stahel of DenverHealth Medical Center and the Universityof Colorado School of Medicine,and colleagues performed a retrospectiveanalysis of the Colorado PhysicianInsurance Company’s (COPIC’s) comprehensivedatabase (Arch. Surg.2010;145:978-84).Dr. Stahel and his colleagues screened27,370 physician self-reported adverseoccurrences between Jan. 1, 2002, andJune 1, 2008. The researchers initiallyfound 119 wrong-site and 29 wrong-patientprocedures, but eliminated casesthey could not classify as being a factualwrong site or wrong patient. The finalanalysis consisted of 107 wrong-site and25 wrong-patient procedures.Analysis of root causes found errors in: Diagnosis, a root cause for 14 (56.0%)wrong-patient and 13 (12.1%) wrongsiteprocedures. Communication, resulted in 25 (100%)wrong-patient and 52 (48.6%) wrongsiteprocedures. Judgment, 2 (8.0%) wrong-patient and91 (85.0%) wrong-site procedures. Treatment, 22 (88.0%) wrong-patientand 9 (92.5%) wrong-site procedures.In addition, system issues were a rootcause in 21 (84.0%) wrong-patient proceduresand 78 (72.9%) wrong-site procedures.This category included time-outnot being performed in 77 (72%) wrongsitecases.Wrong-patient cases often were due toa mix-up of patients’ medical records, radiographs,and laboratory or biopsy samples,as well as errors in communication.Next, the researchers looked at outcomes,namely: Death, which occurred in 1 patient(0.9%) secondary to a wrong-site procedure. Significant harm, which occurred in 5(20%) wrong-patient and 38 (35.5%)wrong-site cases. Minimal harm or functional impairment,which occurred in 8 (32%)wrong-patient and 65 (60.7%) wrongsitecases. No-harm event, which occurred in 9(36%) wrong-patient and 3 (2.8%)wrong-site cases.The most frequent specialties involvedin wrong-patient procedures were internalmedicine (24.0% of cases) as well asfamily or general practice, pathology,urology, obstetrics-gynecology, and pediatrics(8.0% each). The most frequentspecialties involved in wrong-site occurrenceswere orthopedic surgery (22.4%of cases), general surgery (16.8%), andanesthesiology (12.1%).Overall, nonsurgical specialties wereTEVAR for this aortic pathology.involved in 14 (48.3%) wrong-patientand 29 (27.1%) wrong-site cases.“The findings from the present studyemphasize a continuing and concerningoccurrence of wrong-site and wrongpatientprocedures in the current era ofthe Universal Protocol, leading to frequentpatient harm and, rarely, patientdeath,” the researchers said. “Shockingly,nonsurgical disciplines equally contributeto patient injuries related towrong-site procedures.”The researchers believe these findingswarrant expansion of the Universal Protocolto nonsurgical specialties.COMMENTARYLimitations of the study include therestricted coverage of the COPIC databaseto about 6,000 physicians in Colorado;the potential for subjective bias indetermining root causes; and the designationof inadequate planning for theprocedure, which represents a genericcategory.Coauthors on the research analysis reportedthe following conflicts: Dr. Ted J.Clarke is the chief executive officer ofCOPIC; Dr. Jeffrey Varnell and Dr. AlanLembitz are employed by COPIC; andDr. Michael S. Victoroff and Dr. DennisJ. Boyle are consultants for COPIC. ■Universal Protocol is no magic wandAlthough compliance with theUniversal Protocol is important,“it is not the magic wand ofMerlin.” Consider: The UniversalProtocol has been in place since2004, yet Dr. Philip F. Stahel andcolleagues found that preventableerrors, or “never events,” exist atalarming rates. Further, the numberof wrong-site procedures thisstudy cites more likely reflect thenumber of errors reported ratherthan the actual rates of events. So,the number of wrong-site proceduresis probably much higher thanreflected here.Perhaps a more accurate measurementcomes from the complicationrates and safety culturescores under the National SurgicalQuality Improvement Program, orFeatured in the JTCVSCongenital Heart DiseaseStage II palliation of hypoplastic leftheart syndrome without cardiopulmonarybypassAnthony Azakie, Natalie C. Johnson, PetrosV. Anagnostopoulos, Sami M. Akram,Patrick McQuillen, and Anil SapruEarly outcomes for stage II palliation ofhypoplastic left heart syndrome withoutcardiopulmonary bypass were assessedby means of retrospectivereview of 20 infants who had off-pumpbidirectional cavopulmonary anastomosis.The approach is safe, effective,and did not require any conversions tocardiopulmonary bypass. There wereno unplanned reinterventions or hospitaldeaths.General <strong>Thoracic</strong> <strong>Surgery</strong>Refractory cervical esophagogastricanastomotic strictures: Managementand outcomesSamantha J. Davis, Lili Zhao, Andrew C.Chang, and Mark B. OrringerSelf-dilatation is a safe, convenient wayto manage recalcitrant cervical esophagogastricanastomotic strictures aftertranshiatal esophagectomy. This studyassessed quality of life and esophagealspecificoutcomes using patient surveys.Patients who have usedself-dilatation therapy report satisfactoryswallowing function and would useit again under similar circumstances.Evolving Technology/Basic ScienceTranscutaneous aortic valve implantationusing the axillary/subclavianaccess: Feasibility and early clinicaloutcomesThomas Modine, Jean Francois Obadia,Emmanuel Choukroun, et al.Prosthetic aortic valve implantation usinga subclavian arterial approach is aninteresting alternative to the femoralroute, even offering certain advantages.This initial study suggests that subclaviantransarterial aortic valve implantation,in selected high-risk patients, isfeasible and safe.TransplantationFactors associated with in-hospitalmortality in infants undergoing hearttransplantation in the United StatesRupali Gandhi, Christopher Almond,Tajinder P. Singh, Kimberlee Gauvreau,NSQIP. Safety culture scores reflectthe comfort level of hospital employeesabout speaking up aboutsafety concerns.To improve public reporting andbenchmarking, hospitals should berequired to publicly report theirNSQIP outcomes and culturescores.Finally, the Universal Protocol,while important, does not relievehospital systems from emphasizingindividual responsibility in preventingsurgical errors.MARTIN A. MAKARY, M.D., M.P.H.,is with the department of surgery atJohns Hopkins University, Baltimore.His remarks were made in anaccompanying commentary to thearticle. He has no conflicts to disclose.Gary Piercey, and Ravi R. ThiagarajanOf the 730 infants who underwenttheir primary HT between 1999 and2009, 11.2% did not survive to hospitaldischarge. Factors associated with earlymortality include CHD, ECMO support,mechanical ventilation, and renalfailure. Risk stratification among infantslisted for HT may improve decision-makingfor transplant eligibility,organ allocation, and posttransplant interventions.Perioperative ManagementDeep hypothermic circulatory arrestis not a risk factor for acute kidney injuryin thoracic aortic surgeryLars Englberger, Rakesh M. Suri, Kevin L.Greason, et al.The study investigated incidence(17.7%) and risk factors (increased age,elevated body mass index, hypertension,impaired left ventricular ejectionfraction, preoperative anemia, and cardiopulmonarybypass duration) ofacute kidney injury after elective thoracicaortic surgery. Deep hypothermiccirculatory arrest protects kidney function.Estimation of acute kidney injuryrisk requires multivariable prediction.
4 RESIDENTS' CORNER FEBRUARY <strong>2011</strong> • THORACIC SURGERY NEWSViews from Cross-TrainedCardiac Surgeons (Part 1)BY STEPHANIE MICK, M.D.Resident Associate Medical EditorAsession at the 2010 TranscatheterCardiovascular Therapeutics conferenceco-sponsored by TCT, theAmerican Association for <strong>Thoracic</strong><strong>Surgery</strong>, and the Society of <strong>Thoracic</strong>Surgeons centered on integrating cardiacsurgery and interventional cardiology.With such a shift being discussed, it isuseful to consider the perspectives of two“early adopters” of this way of thinking– Dr. Mathew Williams at New York PresbyterianHospital–Columbia and Dr.Michael Davidson at the Brigham andWomen’s Hospital. Both completed cardiacsurgery training and then went on topursue training in interventional cardiology.Each currently practices using ablend of techniques from both disciplines.At the time they pursued interventionalcardiology training, no formalizedtraining programs for cardiac surgeonsinterested in interventional techniquesexisted. But both had observed the emergenceof transcatheter valves.“I’ve always had a strong interest invalves,” said Dr. Davidson, “and it wasvery clear to me that transcatheter valvetechniques would play an incredibly largerole and that it was highly likely duringmy career that these would take a highprofilerole. To be a full participant, Icouldn’t just have cardiac surgical skillsbut would also need interventional skills,and not just for ‘cardiac surgical backup’or providing femoral access, but to reallybe a full participant – to understandthe technology and how to utilize it.”Dr. Williams and Dr. Davidson eachapproached interventional cardiologistsat their respective institutions to set uptheir training. Dr. Williams worked withDr. Martin Leon, a prominent interventionalcardiologist at Columbia and eventuallycompleted a year-long traditionalinterventional cardiology fellowship, “Idid everything the interventional cardiologyfellows did, except I also spent aday a week in the OR as well to keep upthose skills,” Dr. Williams said.Dr. Davidson worked with Dr. DonaldBaim, a pioneer in interventional cardiologythen at the Brigham, and did a yearlongfellowship from 2005 to 2006. “Ispent about 3 days a week in the cath laband 2 days a week in the OR so I couldkeep up my surgical skills. I did a lot ofdiagnostic catheterizations and assisted inPCI cases. Because of my interest invalves, I was also involved any time therewas a structural heart case such as mitral/aorticvalvuloplasties. I also made apoint of being involved in cases done byvascular surgeons (aortic, peripheral, renal,and carotid work) and spent sometime in the electrophysiology lab to gainexperience in trans-septal perforations.”The interventional cardiologists involved,Dr. Leon and Dr. Baim, were bothdescribed as very enthusiastic about thisinnovative training pathway. “It was somethingthat Marty [Leon] had alwaysthought was a great concept and had neverreally happened before then,” Dr.Williams said. Similarly, “Dr. Baim lovedthe idea; it really meshed well with hisworld view of how the specialties werechanging,” said Dr. Davidson, who addedthat “having that kind of high-altitudebackup was important and allowed me theair cover to pursue this sort of training.”After their interventional cardiologyfellowships, both men joined the staff attheir respective training institutions. Dr.Williams is on staff at Columbia in bothinterventional cardiology and cardiacsurgery. “I do a reasonable amount of independentPCI and perform the fullscope of interventional procedures – I’vejoined that group and take acute MI call.Our cardiologists have really embracedthis and are fantastic. I am in the hybridOR 4 days/week – not all of the cases Ido in this room are hybrids, but I docompletion angiograms on almost everyCABG that I do. I do hybrid coronaryrevascularization with PCI and surgery ina single setting. However, the majority ofmy work is valvular – including 4-8 transcathetervalves per month (eithertransapical or transfemoral). I also spendtime in the cath lab – I do the routine,catheter-only based procedures there.”Dr. Davidson is on staff in cardiacsurgery at the Brigham and does not performcoronary interventions. “I’m spendingthe majority of my time doingcardiac surgery with the emphasis beingon valves, but I am also a full participantin any structural heart disease cases goingon in interventional cardiology (e.g.transcatheter aortic valve). I also do myown cardiac catheterizations and so anygiven week, I have patients who come infor hybrid procedures. For instance a patientmay come in with mitral valve prolapseand I will schedule them for cardiaccatherization, possible stent and minimallyinvasive MVP in a single setting. Ispend about one day a week doingcatheter-based procedures and severaldays a week doing traditional surgery.Another thing that has occurred here isthat we’ve had a programmatic approachto this integrated practice. We have ajoint advanced valve and structural heartdisease clinic that I started with one ofmy interventional colleagues that hasnow branched out to involve more cardiologistsand more surgeons. In thisclinic, cardiac surgeons and interventionalcardiologists see patients jointly.”Dr. Davidson notes some of the benefitsof cross-training: “It allows me to bea greater participant in my patient’s care.For instance, I have patients sent to mewho have very complicated valve diseaseand we may put them through a fullworkup including catheterization to figureout what component of their symptomsis the valve disease and whatcomponent may be from other pathologies.It makes me more involved in diseasemanagement, not just doing thesurgeries as they come.”■(Part 2 of this article follows next month).Clinical Challenge: Key Points Definition:·Portion of lung parenchyma withabsence of normal bronchialcommunication with the tracheobronchialtree and systemicarterial blood supply. Two types:·Extralobar: mass of lung tissueseparate from normal lung withits own pleural investment. Venousdrainage and arterial supplyare systemic, not pulmonary inorigin·Intralobar: mass of abnormal lungtissue intimately related with normallung parenchyma with systemicarterial supply but normalpulmonary venous drainage Common presentation:·Recurrent, chronic pulmonary infections Arterial blood supply is alwayssystemic·Most commonly, arising from thedescending thoracic or abdominalBratu, I. The multiple facets of pulmonarysequestration. J Pediatric<strong>Surgery</strong>. 35(5):784-790, 2001.Mendeloff, EN. Sequestrations, CongenitalCystic Adenomatoid Malformations,and Congenital LobarEmphysema. J <strong>Thoracic</strong> and Cardiovascular<strong>Surgery</strong>. 16:209-214, 2004.Hamanaka, H. Surgical Treatment ofinfected intralobar pulmonary sequestration:a collective review of patientsolder than 50 years reported in the literature.Ann <strong>Thoracic</strong> and Cardiovascular<strong>Surgery</strong>. 13(5):331, 2007.aorta Most commonly located in thelower lobe but extralobar sequestrationshave been reported belowthe diaphragm as well Treatment:·Elective surgical resection·May need urgent/emergent resectionif significant hemoptysisor intrathoracic hemorrhage·Intralobar sequestrations oftenrequire lobectomy while extralobarresections can often be dissectedfree from normal lungparenchymaSelected References andAdditional Resources1. Intralobar and extralobar pulmonarysequestrations.2. Pryce type I sequestration classifiesa rare subtype characterized by anomaloussystemic arterial supply to anormal segment of lung.3. Both intralobar and extralobar sequestrationsare characterized bysystemic arterial inflow, most commonlyfrom the aorta. Intralobar sequestrationshave pulmonary venousreturn. In contrast, extralobar sequestrationshave systemic venousdrainage, most commonly via theazygous or hemiazygous venous system.4. Pulmonary sequestrations are mostcommonly found in the lower lobe,left side more common than right.Uncommonly, extralobar sequestrationscan be found outside of thechest cavity with reports of lesions belowthe diaphragm.5. Over half of patients with extralobarsequestrations have associatedcongenital anomalies. CommonStanton, M. Systemic review andmeta-analysis of the postnatal managementof congenital cystic lung lesions.J Pediatric Surg. 44(5): 1027,2009.Yamanaka, A. Anomalous systemic arterialsupply to normal basal segmentsof the left lower lobe. Ann<strong>Thoracic</strong> <strong>Surgery</strong>. 68(2): 332-8, 1999.TSDA Weekly Curriculum – “CongenitalLung Anomalies” www.tsda.org/documents/<strong>PDF</strong>/Weekly%20Curricula/Email%20Archive/06.10.10.pdfAnswers to the Clinical Challengeanomalies include congenital diaphragmatichernia, pericardial defects,other bronchopulmonaryforegut malformations and totalanomalous pulmonary venous return.Congenital anomalies are uncommonwith intralobar sequestrations.6. Resection of the sequestration withdirected ligation of the arterial feedingvessel.7. Asymptomatic sequestrationsshould be resected due to the potentialfor developing infection or hemorrhage,including aneurysmformation and rupture of the aberrantarterial vasculature. There are reportsthat suggest resection forsymptomatic disease, especially infection,is associated with a highermorbidity than resection for asymptomaticdisease.This challenge was contributed by Dr.Christian Peyre, resident associatemedical editor. Stay tuned for moreclinical challenges (Eds.).COURTESY DR. STEVEN MENTZER
FEBRUARY <strong>2011</strong> • THORACIC SURGERY NEWS GENERAL THORACIC 5Drug Resistance Triggers Lung Cancer TransformationBY PATRICE WENDLINGElsevier Global Medical <strong>News</strong>CHICAGO – A small study providescompelling data that both the genotypeand phenotype of non–small cell lungcancers can transform with acquired resistanceto tyrosine kinase inhibitors.Repeat tumor biopsies revealed thatthe histologic diagnosis of the tumorshifted from adenocarcinoma to smallcell lung cancer (SCLC) in 14% of 37consecutive patients with epidermalgrowth factor receptor (EGFR)-mutantnon–small cell lung cancer (NSCLC) andacquired tyrosine kinase inhibitor (TKI)resistance, Dr. Lecia Sequist said at theMultidisciplinary Syposium on <strong>Thoracic</strong>Oncology.The L858R mutationor E 19 deletionwas retained inall cases. In one patient,an additionalPIK3CA mutationwas seen onlywhen the tumorWe need to thinkvery carefullyabout doingmore repeatbiopsies in[NSCLC] patients.DR. SEQUISTshifted to SCLC.Although othergroups have documentedsporadictransformation,Dr. Sequist calledthe 14% transformationrate remarkable.“I thinkthis points to a broader conceptual modelof acquired resistance, and we need tothink very carefully about doing more repeatbiopsies in patients,” she said.EGFR-mutant NSCLC is highly sensitiveto EGFR TKI therapy, but acquiredresistance develops at about 9-12 monthsdue to T790M mutations in half of patientsand MET amplification in 10% to15%, said Dr. Sequist of MassachusettsGeneral Hospital Cancer Center, Boston.Although re-biopsy is not commonpractice, invited discussant Dr. MarkSocinski said it should be on the clinician’sradar because it can alter the therapeuticcourse of refractory disease andarguably the clinical benefit.“I think the message here is to considerre-biopsy more often in selected patientsuntil we have a better understanding ofthis one disease we call non–small lungcancer that we realize is an incrediblyheterogenous disease,” said Dr. Socinski,director of the thoracic oncology programat the Lineberger ComprehensiveCancer Center at the University of NorthCarolina–Chapel Hill.Among the five patients whose cancertransformed, two maintained a slow, indolentcourse after SCLC transformation,while three had a change aroundthe time of their biopsy to an explosivegrowth pattern more clinically reminiscentof SCLC, Dr. Sequist said. Four patientswere treated with SCLC-likechemotherapy regimens, and three respondedwith marked partial responses.Longitudinal data from fluorescent insitu hybridization analysis for MET andEGFR gene copy number suggest thatthe resistant tumor is distinct from theoriginal tumor and that MET amplificationlies in a distinct subpopulation of thecell and is selected out under pressurefrom TKI therapy, she said.Multiple biopsies over time also identifieda waxing and waning of genotypicand phenotypic findings in response toTKI therapy. This pattern was most pronouncedin a case that transformed fromEGFR TKI-sensitive adenocarcinoma toresistant SCLC while on erlotinib (Tarceva)for more than 1 year, switched backCREATED FOR SURGERYdesigned for comfortSurgiCam Pro Digital Video CameraRecord exactly what you see with this lightweightcamera designed for surgeryAll the features to help you see and feel your bestThe Exclusive SurgiTel Oakley LineThe best loupes, the best frames and themost frame choices; SurgiTel and Oakleyare your best choice for performance,comfort and style.to TKI-sensitive adenocarcinoma followingtreatment with chemotherapyand radiation and a 9- to 10-month breakfrom erlotinib, and then after a very successful,but short-lived re-response to erlotinib,shifted back to SCLC a secondtime upon clinical resistance.“It’s showing us that if you do repeatbiopsies, it can direct patients towardsclinical trials that they have a higher likelihoodof benefiting from,” she said.The population comprised 15 men/RXSHV[[+HDGOLJKWV&DPHUDVExcellent Postureand 22 women, median age 60 years. Allhad responded to either gefitinib (Iressa)or erlotinib, with a median of 18.4months of initial EGFR TKI therapy.The majority (81%) remained on TKI atthe time of repeat biopsy. Repeat biopsyshowed T790m mutations in 49%,PIK3CA in 5%, MET amplification in5%, and an unknown mechanism in30%, reported Dr. Sequist.Dr. Sequist and Dr. Socinski disclosedno relevant conflicts.■Other LoupesPoor PostureSurgiTel eliminated all of the neck pain thatI previously endured with other telescopes.Raymond L. Singer, MDDesigned for ComfortThe combination of SurgiTel’s lightweightoptics and Oakley’s “Three-Point” fitensures the highest level of comfortthroughout your work day.Patented Ergonomic DesignsDesigned for improving yourposture, SurgiTel patents providefor the best declination angle andoptical alignment.Compact Prism TelescopesSurgiTel’s patented Compact Prism Telescopes(3.0x-4.5x) are shorter and lighterthen traditional prism telescopes.www.surgitel.com800.959.0153
6 NEWS FROM THE AATS FEBRUARY <strong>2011</strong> • THORACIC SURGERY NEWSAttend the 91st Annual AATS Annual MeetingThe 91st AATS Annual MeetingMay 7 – 11, <strong>2011</strong>Pennsylvania Convention CenterPhiladelphia, PAThe <strong>2011</strong> AATS Annual Meeting isshaping up to be a superb program.We encourage those attendingthe Mitral Conclave, takingplace May 5 – 6, <strong>2011</strong>, to head toPhiladelphia from New York City afterthe Mitral Conclave concludes to participatein the Annual Meeting.Philadelphia is just a two hour ride bycar, one hour ride by train and an evenshorter plane ride from New York City.Maximize your time out of the OR byattending two superior CT-focusedCME programs in <strong>2011</strong> in the sameweek.The Annual Meeting features anumber of new programs in <strong>2011</strong>. Theinaugural “High Performance Teamsin the Operating Room: Using theNOTSS Program (“Non-TechnicalSkills for Surgeons”) to Improve Communication,Understanding and Performance”will focus on theunderlying human factors and nontechnicalskills which enable or hindersurgical performance. This interactiveprogram, taking place on Saturday,May 7 from 1:00 p.m. – 4:00 p.m., willprovide participants with an introductionto observational techniques and abehavior rating system to assist in theevaluation of the performance of surgeonsin the operating room.Audience participation will be augmentedby structured methods of analyzingbehavior and some initialtraining in identifying and discussingperformance in surgery. Chaired by SimonPatterson-Brown, George Youngson,CBE, PhD, and Steve Yule, MA,PhD, MSc, all of the Royal College ofSurgeons of Edinburgh, the course willaddress the needs of all surgical teammembers and was created based uponfeedback from our constituents.AATS Special Reception at theNational Constitution CenterTuesday, May 10, <strong>2011</strong>7:00 p.m. – 10:00 p.m.Reception Ticket Price: $75.00/personRound out your meeting experience byjoining your peers at the National ConstitutionCenter – America’s most interactivehistory museum. Located in astunning contemporary building justtwo blocks from the Liberty Bell andIndependence Hall, it is the only museumdevoted to the U.S. Constitutionand the story of “We, the People.”Opened in 2003, it has been dedicatedto increasing public understandingof the Constitution, its history, and itscontemporary relevance, through aninteractive, interpretive facility withinIndependence National Historic Parkand a program of national outreach, sothat “We the People” may better securethe Blessings of Liberty to ourselvesand our Posterity.Come join us for an historic eveningand enjoy the vistas of this beautifulcity!Reserve your space at the AATS AnnualMeeting, registerfor the High PerformanceTeams in theOperating Room andpurchase your ticket forthe Special Reception atwww.aats.org/annualmeeting/Registration-and-housing.Target AudienceThe AATS Annual Meeting is specificallydesigned to meet the educationalneeds of:• Cardiothoracic Surgeons• Physicians in related specialties includingCardiothoracic Anesthesia,Critical Care, Cardiology, Pulmonology,Radiology, Gastroenterology, <strong>Thoracic</strong>Oncology and Vascular <strong>Surgery</strong>• Fellows and Residents in Cardiothoracicand General Surgical trainingprograms• Nurses, Physician Assistants, Perfusionistsand Allied Health Professionalsinvolved in the care of cardiothoracicsurgical patients• Medical students with an interest incardiothoracic surgeryAATS Annual Meeting AccreditationThe American Association for <strong>Thoracic</strong><strong>Surgery</strong> is accredited by the AccreditationCouncil for Continuing MedicalEducation to provide continuing medicaleducation for physicians.This activity has been approved forAMA PRA Category 1 Credit(s).For additional information pleasevisit www.aats.org or contact:American Association for<strong>Thoracic</strong> <strong>Surgery</strong>900 Cummings CenterSuite 221-U, Beverly, MA, USA 01915Telephone: (978) 927-8330Fax: (978) 524-8890E-mail: meetings@aats.orgAATS Online AwardApplicationsNow Available at www.aats.org,Deadline July 1, <strong>2011</strong>David C. Sabiston ResearchScholarship 2012 – 2014 providesan opportunity for research,training, andexperience for NorthAmerican surgeons committedto pursuing anacademic career in cardiothoracicsurgery.• Research programmust be undertakenwithin the first threeyears after completionof an approved NorthAmerican cardiothoracicresidency.• Applications for the scholarshipmust be submitted duringthe candidate’s first two years inan academic position.• The scholarship will beginJuly 1, 2012 and conclude onJuly 1, 2014.• The Scholarship provides anannual stipend of $80,000 peryear paid to the host institutionfor direct salary support and relatedresearch expenses.Deadline: July 1, <strong>2011</strong>Evarts A. Graham MemorialTraveling Fellowship, 2012-2013 grants support for trainingof international surgeons whohave been regarded as havingthe potential for later internationalthoracic surgical leadership.• Candidate must be anon-North Americanwho plans a cardiothoracicsurgery trainingprogram in a NorthAmerican center andwho has not had extensive(exceeding a total ofsix months in duration)clinical training in NorthAmerica prior to submittingan application.• Candidate should have completedhis/her formal training ingeneral surgery and in thoracicand cardiovascular surgery, butshould not have reached a seniorposition.• The Fellowship provides astipend of US $75,000, a majorportion of which is intended forliving and travel expenses incurredwhen visiting other medicalcenters.Deadline: July 1, <strong>2011</strong>Attend <strong>2011</strong> Heart Valve Summit<strong>2011</strong> Heart Valve Summit:Medical, Surgical andInterventional Decision-MakingOctober 13 – 15, <strong>2011</strong>JW Marriott ChicagoChicago, ILProgram DirectorsDavid H. Adams, M.D.,F.A.C.C.Steven F. Bolling, M.D.,F.A.C.C.Robert O. Bonow, M.D.,M.A.C.C.Howard C. Herrmann,M.D., F.A.C.C.Nurse Planner: MicheleLangenfeld, R.N., M.S.PROGRAM OVERVIEWThe American Associationfor <strong>Thoracic</strong> <strong>Surgery</strong>(AATS) and the AmericanCollege of Cardiology Foundation(ACCF) have partneredonce again to bringyou the only educationalprogram that addressesvalvular heart disease froma cardiology and surgicalpoint-of-view, the <strong>2011</strong>Heart Valve Summit.Using an integrative approachto managing medical,surgical, andinterventional challenges invalvular heart disease, worldrenowned cardiologists andcardiac surgeons will provideyou with clinically relevantinformation on thecurrent and future directionsin valvular heart disease.This unique,interdisciplinary programwill include real world, interactivecase-based patientmanagement discussions, reviewof current practiceguidelines, and focusedbreakouts for cardiologists,cardiac surgeons, nurses,and physician assistants.TARGET AUDIENCECardiologists, interventionalcardiologists, cardiothoracicsurgeons, internists, nurses,physician assistants, and allhealth care professionals involvedin the evaluation, diagnosisand/ormanagement of patientswith valvular heart diseaseare strongly encouraged toattend this program.ACCREDITATION PhysiciansThe American Associationfor <strong>Thoracic</strong> <strong>Surgery</strong> is accreditedby the AccreditationCouncil for ContinuingMedical Education toprovide continuingmedical education for physicians.This activity has been approvedfor AMA PRA Category1 Credits. NursesThe American College ofCardiology Foundation isaccredited as a provider ofcontinuing nursing educationby the American NursesCredentialing Center’sCommission on Accreditation.Register today atwww.aats.org/valve to seefirst-hand why this programcontinually receives highrankingsand has been referredto as “one of the bestmeetings I have ever attended– practical, patient orientedand the lecturers reallyhad true clinical experience.”
A ATS 91STANNUAL MEETINGMay 7–11, <strong>2011</strong>Philadelphia, PA, USAPennsylvania Convention CenterAMERICAN ASSOCIATIONFOR THORCIC SURGERYRegister andReserve Housing atwww.aats.orgAATS/STS CARDIOTHORACIC CRITICAL CARESYMPOSIUMSunday, May 8, <strong>2011</strong> | 8:00 a.m. - 5:00 p.m.FeaturingNEWIN <strong>2011</strong>PHYSICIAN ASSISTANT/NURSE PRACTITIONER/PERFUSIONIST PROGRAMSaturday, May 7, <strong>2011</strong> | 8:00 a.m. - 5:00 p.m.Chair:Michael Argenziano, MD, Columbia UniversityTopics includes Percutaneous and hybrid approaches to coronary and valvulardisease, treatment of aortic disease, management of difficultchallenges in patient cares Advanced perfusion techniquess Cerebral and neuroprotection strategiess Advanced respiratory support and controversies in saphenousvein harvestingChairs:Nevin M. Katz, MD, Johns Hopkins UniversityMichael S. Mulligan, MD, University of Washington Medical CenterTopics include:s Optimal pharmacologic supports Management of arrhythmiass Protocols for severe LV dysfunctions Care of LVAD recipientss Principles of blood conservationAttend the symposium and learn how to implement new concepts,protocols and technology that make the recovery of patients fromCT surgery faster, safer and more comfortable.ICU OF THE FUTURE ©Sunday, May 8, <strong>2011</strong> – Tuesday, May 10, <strong>2011</strong>*During exhibit hoursAdvisors:Neil A. Halpern, MD, Memorial Sloan-Kettering Cancer CenterRobert L. Sladen, MD, Columbia UniversityNEWIN <strong>2011</strong>Participants will be able to see first hand what the future holds forcardiothoracic surgical critical care at the ICU of the Future display.Located on the exhibit floor between the Cardiac and the General<strong>Thoracic</strong> Operating Rooms of the Future, the CT ICU will showcasecutting edge equipment and the latest technological advancesin imaging, advanced information technology and critical caremedicine used in cardiothoracic surgical critical care.AATS Annual Meeting AccreditationThe American Association for <strong>Thoracic</strong> <strong>Surgery</strong> is accredited by the AccreditationCouncil for Continuing Medical Education to provide continuing medical educationfor physicians.The American Association for <strong>Thoracic</strong> <strong>Surgery</strong> designates this educational activityfor a maximum of 35 AMA PRA Category 1 Credits. Physicians should onlyclaim credit commensurate with the extent of their participation in the activity.This program will be submitted to the American Academy of Nurse Practitioners forcontinuing education credit.Conference organizers plan to request AAPA Category I CME credit from thePhysician Assistant Review Panel. Total number of approved credits yet to bedetermined.ICU Room, Adult Medical-Surgical ICUMemorial Sloan-Kettering Cancer Center, New York, NYWinner of the 2009 ICU Design Citation Award
10 ADULT CARDIAC FEBRUARY <strong>2011</strong> • THORACIC SURGERY NEWSGait Predicts Outcomes in Elderly Cardiac <strong>Surgery</strong>BY MARY ANN MOONElsevier Global Medical <strong>News</strong>Gait speed independently predictsboth major morbidityand mortality in elderly patientswho are about to undergocardiac surgery, according to aprospective, blinded study reportedin the Journal of theAmerican College of Cardiology.“This simple, rapid, and inexpensivetest effectively stratifiespatients beyond traditional estimatesof risk, which tend to be inaccuratein the elderly,” said Dr.Jonathan Afilalo of McGill University,Montreal, and his associates.Half the cardiac surgeries donein North America involve elderlypatients (aged at least 70 years),but scoring systems for estimatingoperative risk perform poorly inthis age group, “overestimatingmortality by as much as 250%,”they noted.Dr. Afilalo and his colleaguesperformed what they describedas the first study to test the valueof gait speed as a predictor ofpoor outcomes in elderly cardiacsurgery patients. The prospective,blinded study involved 131 patients(mean age, 76 years) whowere scheduled to undergo electivecoronary artery bypassand/or valve replacement or repairvia standard sternotomy atfour university-affiliated medicalcenters across Canada and theUnited States.Before surgery, the study subjectswere timed as they walked adistance of 5 meters in a well-lithallway; subjects were permittedto use an aid such as a cane orwalker if needed. A time of 6 secondsor longer was classified as aslow gait speed, whereas any timeunder 6 seconds was classified asa normal gait speed.The primary composite endpoint was in-hospital mortality orany of five major complications(stroke, renal failure, prolongedventilation, deep sternal woundinfection, and need for reoperation).In all, 60 patients (46%) werejudged to have slow gait speed beforesurgery. Interestingly, gaitspeed did not correlate with theSociety of <strong>Thoracic</strong> Surgeons’ riskscore, “suggesting that these wererepresenting distinct domains,”the investigators said.After surgery, 30 patients (23%)experienced the primary compositeend point.Slow gait speed was a strongand independent predictor, associatedwith a 3.17-fold increase inrisk of the primary end point.Moreover, adding gait speed to existingrisk prediction models improvedtheir performance in predictingwhich patients would experiencean adverse event andwhich patients would need “tobe discharged to a health care facilityfor ongoing medical care orrehabilitation.”Women with slow gait speedappeared to be at particularly highrisk for adverse outcomes.The study findings have threeclinical implications.“First, by refining risk predictionsin this challenging group,clinicians can have a more comprehensiveassessment of theirpatient and provide a more accurateestimate of risk to the patient,”Dr. Afilalo and hisassociates said (J. Am. Coll. Cardiol.2010;56:1668-76).Second, clinicians can better assesswhich elderly patients mighthave better success with less-invasivetechniques such as transcathetervalve implantation.And third, patients who werefound to have slow gait speedmight benefit from extra interventionsin the perioperative period,such as more intensivemonitoring, early mobilization,low-intensity exercise training,or planned discharge to a specializedrehabilitation facility,they said.The investigators reported nofinancial conflicts of interest. ■COMMENTARYAn Important New Toolfor CliniciansExisting risk-assessmenttools for elderlycardiac patients areinadequate, according toDr. Joseph C. ClevelandJr. “We must prepareourselves to face decisionsregarding treatmentoptions for thisexponentially growingsegment of our populationwith scant data toappropriately guide ourdecisions.”In this context, Dr. Afilaloand his associateshave given clinicians animportant, simple, and“extraordinarily cost-effective”tool, he wrote inan editorial accompanyingthe study (J. Am.Coll. Cardiol. 2010;56:1677-8). Assessing gaitspeed requires only anobserver, a stopwatch,and a well-lit hallway.He added that the investigatorsalso shouldbe commended for expandingthe list of adverseoutcomes beyondsimple mortality, “becausemany elderly peoplefear loss ofindependence as a fateworse than death.” Slowgait speed doubled thechances that a patientwould be discharged to ahealth care facility orwould have a prolongedhospital stay. “These dataare sorely needed whenfacing elderly patientsand counseling them,”Dr. Cleveland said.The researchers’ findingof an interaction betweenslow gait speedand female sex also is particularlyimportant. “Elderlywomen with slowgait speed had an eightfoldincrease in morbidityand mortality” andclearly represent a highrisksubgroup, he noted.JOSEPH C. CLEVELANDJR., M.D., is at theUniversity of ColoradoHealth Sciences Center,Denver.GenotypingCatherization • from page 1Dr. John McPherson (left) shown with Scyble VanCleve, the first patient at Vanderbilt to benefit from anew program using genetic information.cavir, azathioprine, 6-mercaptopurine, codeine,or “virtually any antidepressant or most antipsychotics,”Dr. Roden said in an interview.“In the long perspective, every 50-yearold”is a good bet to eventually receive at leastone drug for which a dosage adjustmentbased on genotype is warranted, but – stoppingshort of such global use right now – theVanderbilt program will instead graduallyphase in new groups of patients to the offerof genotyping.“Implementation is a huge challenge. Inmy opinion, this will only work with preemptiveimplementation. Electronic recordsare not just repositories of information, butare nimble enough to provide support at thetime of a prescription,” he said. “The way itought to work is, a physician prescribes adrug and the electronic system recognizes[that] the drug has a genetic element andgoes into the patient’s record and finds thegenotype information” to decide whether toflash a screen alert about the patient’s genotypeand the implications.The program, known as PREDICT (PharmacogenomicResource for Enhanced Decisionsin Care and Treatment) launched onSept. 15. It uses a genotyping panel sold onthe U.S. market by Illumina that screens for184 different genetic polymorphisms in 34genes that affect the absorption,distribution, metabolism, or excretionof various drugs.Test results get posted into therecord within a day of specimencollection.So far, Vanderbilt itself has completelyfunded the program, whichinvolved a year of planning and “ahuge amount of money,” said Dr.Roden, adding that the program isthe first of its kind worldwide.PREDICT is expected to improvepatient outcomes and its developershope to eventually convinceCOURTESY SUSAN URMYpayers to cover the cost.Dr. Roden stated that he is or hasbeen a consultant to several drugcompanies and has received royaltiesfrom Clinical Data Inc. ■New Troponin T Assay FindsSubclinical Cardiac ProblemsBY MARY ANN MOONElsevier Global Medical <strong>News</strong>The new, highly sensitive cardiactroponin T assay finds detectablelevels of the biomarker in25% of adults in the general populationwho would not be identifiedby the standard assay, and thatresult often correlates with cardiacstructural abnormalities, accordingto large cohort study.Elevated cardiac troponin T levelsalso correlated with all-causeand cardiovascular mortality, independentlyof other risk factors andeven in people thought to be at lowcardiovascular risk, said Dr. JamesA. de Lemos of the University ofTexas, Dallas, and his associates.The highly sensitive assay detectslevels of cardiac troponin Tthat are approximately one-tenth ofthe levels detectable with the standardassay. Dr. de Lemos and hiscolleagues examined the results ofthis assay in a general populationcohort of adults aged 30-65 yearsparticipating in the Dallas HeartStudy. The 3,546 subjects in thisrandom probability sample had detailedcardiovascular profiles.The prevalence of detectablecardiac troponin T by this highlysensitive assay was 25% in this multiethniccohort that included a highproportion of blacks and women.In contrast, the standard assayfound detectable levels in 0.7%.Higher levels of the biomarkeron the highly sensitive assay wereassociated with cardiac structuralabnormalities including left ventricularhypertrophy (both wallthickening and dilation) and leftventricular systolic dysfunction,even in subjects who were asymptomatic,had no known CVD, andwere classified as low-risk by theirFramingham Risk Scores.“Moreover, higher cardiac troponinT levels demonstrate[d] agraded association with all-causeand cardiovascular mortality, independentof traditional risk factors,renal function, and levels of otherbiomarkers” such as high-sensitivityC-reactive protein and N-terminalprohormone brain natriureticpeptide (JAMA 2010;304:2503-12).More research is needed to determineif routine use of the assaywould aid risk assessment in thegeneral population.■
FEBRUARY <strong>2011</strong> • THORACIC SURGERY NEWS CARDIOPULMONARY TRANSPLANTATION 11Strategy Nearly Doubles Lungs Suitable for TransplantProtective measures included lower tidal volumes,and continuous postive pressure during apnea tests.BY MARY ANN MOONElsevier Global Medical <strong>News</strong>Astrategy for protecting the lungs inpotential organ donors nearly doubledthe number of lungs that weresuitable for transplantation, accordingto a report in JAMA.The lung-protection strategy, which apparentlyforestalled much of the pulmonarydamage associated with braininjury and mechanical ventilation, had nodetrimental effects on other organs –hearts, livers, and kidneys – harvestedfrom the same donors for transplantation,said Dr. Luciana Mascia of the departmentsof anesthesia and intensive caremedicine at the University of Turin (Italy).Potential organ donors who have relativelynormal pulmonary function atthe time of brain death often showmarked declines in that function, so thatonly 15%-20% of these lungs are suitablefor transplantation when organ harvestingcommences.Dr. Mascia and her colleagues studied118 patients with brain death who werepotential organ donors and were beingtreated at 12 intensive care units (ICUs)in Italy and Spain between 2004 and2009. A total of 59 patients were randomlyassigned to undergo conventionallung ventilation techniques, and theother 59 were assigned to a strategy ofusing lower tidal volumes, higher positiveend-expiratory pressure (to preventatelectasis), a closed system for any trachealsuctioning, alveolar recruitmentmaneuvers after any ventilator disconnections,and continuous positive airwaypressure during apnea tests.After a mandatory 6-hour interval beforebrain death could be officially declared,there were 49 potential donors inthe conventional-care group and 51 inthe lung-protection group. The numberof patients who then were found to meetlung-donor eligibility criteria decreasedwith the conventional ventilation strategyby 29% to only 32 patients. In contrast,an increase to 56 patients met lungdonation criteria in the lung-protectiongroup, a significant difference.This means that of the original potentialdonors, only 54% in the conventional-caregroup met eligibility criteria,compared with 95% in the lung-protectiongroup, Dr. Mascia and her associatessaid (JAMA 2010;304:2620-7).The ultimate number of lungs thatwere successfully harvested was 27% ofthe conventional-care group (16 lungs),compared with 54% of the lung-protectiongroup (32 lungs), also a significantdifference.For the lung recipients, the medianICU length of stay was 12 days for patientswho received lungs from the conventional-caregroup and 8 days for thosewho received lungs from the lung-protectiongroup.Six-month survival was 69% for patientswho received lungs from the conventional-caregroup and 75% for thosewho received lungs from the lung-protectiongroup, a nonsignificant difference.The number of other organs harvesteddid not differ between the two studygroups, and 6-month survival of those recipientsalso did not differ significantly.The Protective Ventilatory Strategy inPotential Lung Donors Study (clinicaltrials.govID: NCT00260676) wasstopped after 118 patients were enrolled,because of termination of funding.“This study breaks important newground in providing a solid evidencebase for the care of potential organdonors and testing techniques of organpreservation,” said Dr. Mark S. Robertsin an accompanying editorial (JAMA2010;304:2643-4).The “profound” results showed that arelatively simple protection strategy doubledthe number of patients from whomtransplantable lungs could be harvested.Moreover, although the study samplewas small, there were no detrimental effectson transplant outcomes, either withthe lungs or with other donated organs,added Dr. Roberts of the department ofhealth policy and management at theUniversity of Pittsburgh School of PublicHealth.“Doubling [the lung] donation ratecould potentially meet steady-state demandas well as reduce waiting-list backlog,especially because each donor[potentially] provides organs for morethan 1 transplant,” he noted.“The study by Mascia et al. [also] providessobering evidence that conventionallung preservation practices, whichhave been used for many years, are remarkablyinefficient in their task,” Dr.Roberts added.This study was supported by the Ministerodella Salute Programma RicercaFinalizzata, the Regione Piemonte ProgrammaRicerca Finalizzata, and the Ministerodell’Universita Programma diRicerca di Interesse Nazionale. No financialconflicts of interest were reported. ■Grant WritingW orkshopMarch 4, <strong>2011</strong>Course Directors:David R. Jones, MDY. Joseph Woo, MDAmerican Association for <strong>Thoracic</strong> <strong>Surgery</strong>Bethesda Marriott, Bethesda, MDwww.aats.org
12 CARDIOPULMONARY TRANSPLANTATION FEBRUARY <strong>2011</strong> • THORACIC SURGERY NEWSThird-Generation LVAD Shows Good Efficacy, SafetyBY MITCHEL L.ZOLERElsevier Global Medical <strong>News</strong>CHICAGO – A third-generation, investigationalleft ventricular assist deviceperformed at least as well as current U.S. Food and Drug Administration-approvedLVAD devices on the market in a140-patient, pivotal, multicenter bridgeto-transplanttrial. Interim analysis alsosuggested important possible benefits,such as reduced rates of infections andbleeding during 6 months of follow-up..Based on results from the ADVANCE(Evaluation of the HeartWareVentricular Assist System forthe Treatment of AdvancedHeart Failure) study, Heart-Ware – the company developingthe new device – hasrequested pre-marketing approvalfrom the FDA for theHeartWare ventricular assistdevice (VAD) as a bridge totransplant in January. The continuous-flowHeartWare VADis small enough to be implantedin the pericardiumwith no need for creating asurgical pump pocket. Expertswho heard the new data cautionedthat although the resultsso far look encouraging in thisintermediate follow-up, the long-termdurability and performance of the newVAD needs to be assessed compared withthe current standard of care, primarily theHeartMate II device.“Implantation of the HeartWare VADpump in the pericardial space was associatedwith a very high probability ofsuccess at 180 days,” said Dr. Keith D.Aaronson at the scientific sessions. The92% of patients who received the Heart-Ware VAD and were either alive withtheir device or had received a heart transplantduring the 180 days after deviceplacement was “the highest rate ever reportedin any left VAD [LVAD] study,”said Dr. Aaronson, medical director ofthe heart failure program at the Universityof Michigan in Ann Arbor.The question of whether either theHeartWare or HeartMate III VAD has significantsurvival or risk profile advantageseither overall or in particular patientsubpopulations remains to be answered.“The only way to know for sure [whichdevice is better] is to compare them headto head.” A clinical trial now underwaycompares the two VADs as “destinationtherapy” for patients who are not consideredsuitable candidates to get a hearttransplant, he noted.“The HeartMate II has been a goodworkhorse. People know how to use itand are comfortable with it. When theHeartWare device comes out, peoplewill want to use it, and surgeons seem tolike the idea of implanting the device directlyin the heart. But [questions like]which is the best kind of VAD, where doyou put it, and what’s the best way to anticoagulatepatients [are] not clear. TheHeartMate VAD advances one piece ofthe puzzle, but the upcoming trials thatwill compare the VADs head to head willThe longer patientshave LVADs, themore you seeaortic insufficiency.Will the VADs differin this key issue?DR. JESSUPgive us a lot more answers,” commentedDr. Mariell L. Jessup, professor ofmedicine and medical director of theheart and vascular center at the Universityof Pennsylvania in Philadelphia.“This is the first successful completionof a bridge-to-transplant trial with a control”group of patients, noted Dr. LynneWarner Stevenson, professor of medicineand director of the cardiomyopathyand heart failure program at Brighamand Women’s Hospital in Boston. “Weall know that the bridge results are notthe same as the destination results.”The HeartWare VAD armof the study ran at 30 U.S.sites during August 2008–<strong>February</strong>2010. The researchersscreened 157 patients to find140 who met the enrollmentcriteria, including havingNew York Heart Associationclass IV heart failure and beinglisted for a heart transplant.Surgeons ultimatelyplaced the HeartWare VAD in137 patients. The control armincluded 499 U.S. patientswho received a commerciallyavailable LVAD during thesame period and were registeredin the INTERMACS (InteragencyRegistry for MechanicalAssisted Circulatory Support) system.By the first half of 2009, 94% of theseINTERMACS control patients received aHeartMate II as their LVAD, andthroughout the 18 months of the studyDr. Aaronson estimated that all but 3%-4% of the control patients received aHeartMate II. The average age of theVAD recipients was 53 years, and abouta quarter were women.After 180 days, 63% of the HeartWareVAD recipients remained alive with theirdevice in place, and 29% had received aheart transplant, 4% had their deviceswitched for another VAD, and 4% haddied. The overall 92% success rate in thisgroup was comparable with a 90% overallsuccess rate among the control patientsin the INTERMACS registry. Thesimilar rates in the two arms met the prespecifiedcriteria for noninferiority of thenew device. But the HeartWare VAD didnot show statistically significant superiorityto the control devices, either in anunadjusted analysis or after adjustment ina propensity analysis, Dr. Aaronson said.Mortality during the first 30 days followingdevice placement ran 1.4% inthe HeartWare group and 3.4% in thecontrol patients. The 1.4% perioperativerate in the HeartWare recipientswas “remarkable,” Dr. Aaronson said,and was “comparable to the rate in patientselectively receiving an aortic valvereplacement.”The HeartWare recipients also showedstatistically significant and clinicallymeaningful improvements in their qualityof life relatve to their own baseline.At 3 months after device placement, patients’average scores on the Kansas CityCardiomyopathy Questionnaire for clinicalsummary and overall summary hadrisen from a level consistent with severeThe HeartWare is smaller than other VADsand is implanted in the pericardium.heart failure at baseline to a level indicatingmild residual heart failure. AverageEuroQol 5D self-rating showed anincrease after 3 months of HeartWaresupport that was comparable with “whatis usually reported for heart transplantrecipients,” Dr. Aaronson said.The investigators compared adverseevents in the 140 HeartWare VAD recipientsto those seen in 281 patients who receivedthe HeartMate II VAD in amulticenter study done during 2005-2008,the trial that led to HeartMate II’s FDA approval(J. Am. Coll. Cardiol. 2009;54:312-21). In the HeartWare series, bleeding atgastrointestinal sites occurred at a rate of25% per patient-year, and bleeding requiringsurgery occurred in 27% per patient-year.In the HeartMate II series,bleeding requiring surgery occurred at arate of 45% per patient-year. Gastrointestinalbleeding was not separately reported.However, the 25% perpatient-year gastrointestinal-bleeding ratein the HeartWare patients was “relativelylow, about one-third the rate that’sbeen reported” by individual centers forpatients who received the HeartMate II,COMMENTARYDr. Aaronson said.“We need to know if there is a meaningfuldifference in the gastrointestinalbleeding, a key issue for all the nonpulsatileVADs,” Dr. Jessup said.Infection rates with the HeartWareVAD (39% per patient-year vs. 85%) andventricular arrythmias (13% per patientyearvs. 40% per patient-year) also ran“substantially lower” relative to theHeartMate II multicenter series.Ischemic stroke rates with the Heart-Ware VAD ran 11% per patient-year,similar to the 9% rate seen in the multicenterHeartMate II series. Hemorrhagicstroke occurred at the same rate(5% per patient-year) with both devices.Half of the 10 ischemic strokes in theHeartWare VAD recipients occurredduring the first 48 hours following deviceplacement. “We believe they weresurgically related; there is a clear learningcurve” for placing the HeartWareVAD, Dr. Aaronson said. In addition, henoted that 8 of the 10 patients who hadischemic strokes later recovered to“moderate disability.”With respect to long-term supportwith non-pulsatile VADs, a remaining“key issue” is aortic valve insufficiency,Dr. Jessup said. “No one talks about it inthese short-term trials, but you really seeaortic insufficiency in destination-treatmenttrials. The longer you see patients[with LVADs], the more you see themdeveloping hypertension and aortic insufficiency.Will there be a difference inthe VADs for aortic insufficiency?”The study was sponsored by Heart-Ware, the device developer. Dr. Aaronsonsaid that he has received researchsupport from HeartWare, Thoratec, andTerumo. Dr. Jessup is a consultant toMedtronic and a speaker on behalf ofBoston Scientific, and has received researchfunding from Scios. Dr. Stevensonhas been a consultant to Medtronic. ■Adverse-Event Edge for New LVAD?The early results using the Heart-Ware device as a bridge to transplantare at least as good asthose of the other LVADscurrently approved by theFDA. The main problemthat had dogged the applicationof LVADs has beentheir adverse effects. Thenew VAD appears to causeless infection, probably becauseit is smaller andneeds less dissection duringimplantation than do current devices.Placement and use of the newHeartWare device may also be associatedwith less bleeding.The new device is extremely attractivebecause it is small and simpleto place, and has no need for a“pump pocket.” There is hope thatthese factors will translate into improvedclinical benefit.My major concerns about the currentreport are that it involved no©HEARTWARE INC. CAUTION: INVESTIGATIONAL DEVICErandomization and no true controlgroup. In addition, the HeartWaredevice was linked with asignificant number ofstrokes. (There has beenhope that the innovativedesign of this new devicemight reduce bloodthrombogenicity.) In thedevice’s defense, many ofthe strokes occurred withinthe first 48 hours afterimplant, and up to 80%were recoverable. This issue mayalso relate to the type of anticoagulationused.Overall, this study represents alandmark in the long road of optimizingthe use of LVADs. I look forwardto seeing longer-term results.MAGDI H. YACOUB, M.D., is aprofessor of cardiothoracic surgery atImperial College London. He said hehad no disclosures.
<strong>2011</strong>American Associationfor <strong>Thoracic</strong> <strong>Surgery</strong>MAY 5-6, <strong>2011</strong>Sheraton Hotel & TowersNew York, New York, USAImmediately Preceding:AATS 91 st Annual MeetingMay 7-11, <strong>2011</strong>Philadelphia, PA, USAmitralconclavePROGRAM DIRECTORDavid H. Adams, MDPROGRAM committeeOttavio R. Alfieri, MDW. Randolph Chitwood, Jr., MDRobert A. Dion, MDA. Marc Gillinov, MDFriedrich W. Mohr, MDdecision makingOUTCOMESsurgical video sessionsREGISTER ONLINE AT:www.aats.org/mitralProgram Available OnlineAccreditation:The American Association for <strong>Thoracic</strong> <strong>Surgery</strong> is accredited by the Accreditation Council for Continuing Medical Education to provide continuingmedical education for physicians.The American Association for <strong>Thoracic</strong> <strong>Surgery</strong> designates this educational activity for a maximum of 17 AMA PRA Category 1 Credits.Physicians should only claim credit commensurate with the extent of their participation in the activity.
14 CONGENITAL HEART FEBRUARY <strong>2011</strong> • THORACIC SURGERY NEWSREV, Metras Beat Rastelli for TGA, VSD, and LVOTOBY MARK S.LESNEYElsevier Global Medical <strong>News</strong>Optimal surgical management of patientswith transposition of thegreat arteries, ventricular septal defect,and left ventricular outflow obstructionis still considered controversial.Although the Rastelli operation is themost commonly performed procedure,the Réparation à l’Etage Ventriculaireprocedure and Metras modificationyielded the best long-term results forboth survival and event-free survival, accordingto a retrospective study of 146patients who underwent surgery from1980 to 2008 in eight European hospitals.The multicenter study compared useand outcomes of several different surgicaloperations for transposition of thegreat arteries (TGA), ventricular septaldefect (VSD), and left ventricular outflowobstruction (LVOTO), according to a reportpublished in the European Journalof Cardio-thoracic <strong>Surgery</strong>.A total of 141 patients had TGA, VSD,and LVOTO; 5 patients had the TGAtype of double-outlet right ventricle(DORV) with LVOTO. Only those patientsfor whom the surgical methodchosen was equivalent to those for TGA,VSD, and LVOTO were included in thestudy; all other DORV types were excluded,according to Dr. Mark GerardHazekamp of Leids Universitair MedischCentrum, Leiden, the Netherlands, andhis colleagues from various Europeanuniversities on behalf of the EuropeanCongenital Heart Surgeons Association.The procedures investigated were theRastelli (82 patients), arterial (24) andatrial (5) switch operation with relief ofLVOTO, Réparation à l’Etage Ventriculaire(REV) procedure (7), and Metrasmodification (24), as well as the Nikaidoh(4). The type of surgery used has traditionallybeen different in different countries,they said, with the REV procedureand Metras modification mainly inFrance and the Rastelli procedure beingthe norm in most other countries.Patients had a median age at operationof 21.5 months (range 0.2-165.1 months)and a median weight of 10 kg (range 2.0-41.0 kg). Pulmonary stenosis was found in119 patients, while 27 had pulmonaryatresia. LVOTO was solely valvar in 24%of the patients, only subvalvar in 37% ofpatients, and multilevel in 39%.The location of the most importantVSD was known in 143 patients, withoutlet septum in 102, inlet septum in 14,trabecular septum in 3, and a combinationof the three in 24 patients. The greatmajority of the 140 patients for whomdata were available had great artery commitmentof the biggest VSD: to the aortain 60, the pulmonary artery in 32, anddoubly committed to both in 19. Only 29patients had noncommitment of one ofthe great arteries to the VSD.Overall postoperative survival was 92%at 1 month, 88% at 1 year, 88% at 10years, and 58% at 20 years. Events were[RASTELLI] REOPERATION ANDEVENT-FREE SURVIVAL RATESARE NOT SATISFACTORY, WITHEVENT-FREE SURVIVAL AT 10YEARS AT 24% TO 49%.followed as an outcome and were definedas death, reoperation, transcatheter intervention,or cardiac transplantation.The frequent necessity of reintervention(40.7% over follow-up) caused the overallevent-free survival to be lower: 85% at1 month, 80% at 1 year, 45% at 10 years,and 26% at 20 years (Euro. J. Cardiothorac.Surg. 2010;38:699-706).There were 41 surgical reinterventionsand 20 percutaneous procedures, with themost frequent cause of reoperation beingRVOT obstruction, including conduit failure(25.0%), followed by LVOT obstruction(7.9%), residual VSD closure (7.1%),and pulmonary artery plasty (4.3%).In multivariate analysis, age at the correctivesurgery, year of the operation,and type of operation were significantpredictors for reoperation and transcatheterintervention, in general, as wellas for RVOT reoperation/intervention.The younger the patient at the time ofoperation, the higher the risk of later reoperation,leading the researchers tospeculate that the more recent thesurgery, the less the probability that a patientwould undergo reoperation.Reoperation for RVOTO was mostcommon in patients with a Rastelli operation,according to the authors.“Although there are some differencesbetween Rastelli outcomes among differentgroups, the all-over rates of freedomfrom reoperation and, especially,event-free survival, are not satisfactorywith event-free survival rates at 10 yearsthat vary from 24% to 49%,” they said.“The Rastelli procedure was a significantindependent risk factor for re-operation,with the REV/Metras and theNikaidoh having the lowest re-interventionrates,” they wrote.They indicated more patients need tobe studied with longer follow-up, especiallyfor the Nikaidoh technique.The authors had no disclosures. ■
FEBRUARY <strong>2011</strong> • THORACIC SURGERY NEWS DEVICES, DRUGS & TRIALS 15E-Cadherin Levels Drive Entinostat Efficacy in NSCLCBY PATRICE WENDLINGElsevier Global Medical <strong>News</strong>CHICAGO – Patients with previously treated, advancednon–small cell lung cancer and high E-cadherinlevels derived greater benefit when the investigationalagent entinostat was added to erlotinib in a treatmentstrategy designed to overcome erlotinib resistance.The data from a placebo-controlled, phase II trial arenoteworthy because histone deacetylase inhibitors,such as entinostat, increase erlotinib sensitivity and preventor delay resistance, which inevitably occurs in patientswho are treated with erlotinib and otherepidermal growth factor receptor (EGFR) tyrosine kinaseinhibitors.In addition, patients with elevated E-cadherin levelsaccount for 40% of the overall NSCLC population,making it an attractive clinical biomarker for directingtherapy. These preliminary data suggest that “there maybe a subpopulation of patients for which entinostat mayhave the ability to overcome erlotinib resistance,” Dr.Robert Jotte said at the symposium, where he presentedthe findings at the Multidiciplinary Symposium on<strong>Thoracic</strong> Oncology..Among 132 unselected patients in the phase II EN-CORE 401 trial, outcomes were comparable for oralentinostat plus erlotinib (Tarceva) vs. erlotinib plusplacebo, with a nonsignificant median progressionfreesurvival difference of just 0.4 months and a medianoverall survival difference of 2.2 months, hereported.Among 26 patients who were identified as havinghigh E-cadherin levels, however, entinostat significantlyincreased overall survival, from 5.4 months withplacebo to 9.4 months (hazard ratio, 0.36; P = .03), saidDr. Jotte, director of thoracic oncology at the RockyMountain Cancer Centers in Denver.In contrast, 40 patients with low E-cadherin expressionwho received placebo survived a median of 7.0months, compared with 4.4 months with entinostat (P= .55; HR, 1.25).BY PATRICE WENDLINGElsevier Global Medical <strong>News</strong>CHICAGO – Bevacizumab maintenanceafter first-line chemotherapy foradvanced non–small cell lung cancer wasassociated with longer overall survival ina retrospective study of 403 patients whowere treated in outpatient communitysettings.Median NSCLC disease progressionwas 10.3 months among patients whocontinued on bevacizumab (Avastin) untildisease progression after they receivedfirst-line chemotherapy plus bevacizumab,compared with 6.5 months for thosewho discontinued the monoclonal antibodyafter chemotherapy.Median overall survival reached 20.9months vs. 10.2 months, respectively,Dr. Eric Nadler reported in a poster atthe Multidiciplinary Symosium on <strong>Thoracic</strong>Oncology.Although it is standard practice inclinical trials to continue bevacizumabuntil disease progression, recent assessmentsof treatment patterns in theUnited States have shown that bevacizumabis often discontinued whenchemotherapy ends. Price has been anissue, with the typical monthly cost ofMedian progression-free survival in the exploratorybiomarker analysis also trended in favor of high E-cadherinpatients who received entinostat vs. placebo (3.7months vs. 1.9 months), but the difference did not reachstatistical significance (HR, 0.55; P = .19).Median progression-free survival amonglow E-cadherin patients was similar at 1.7months with entinostat vs. 1.9 months withplacebo (HR, 1.36; P = .36), said Dr. Jotte.Invited discussant Dr. Pasi Jänne of theDana-Farber Cancer Institute in Boston, saidthat preclinical data showing that erlotiniband entinostat prevent the emergence of resistancein EGFR-mutant cell lines (Cell2010;141:69-80) provide a rationale for combiningthese agents. What isn’t clear iswhether entinostat would restore erlotinibsensitivity in cell lines with a KRAS mutationor EML4-ALK translocation.Dr. Jänne also observed that the currentdata contradict two other preclinical studiesand a subset analysis from the TRIBUTEtrial demonstrating that high E-cadherin expression isassociated with erlotinib sensitivity. In ENCORE 401,however, patients with high E-cadherin expressionwho were treated with erlotinib and placebo had ashorter median overall survival than did their counterpartswith low E-cadherin expression (5.4 monthsvs. 7.0 months).Discrepancies between these data and the phase IIdata need to be resolved before additional prospectivetrials of erlotinib/entinostat are undertaken, Dr. Jännesaid.Syndax Pharmaceuticals, which is developing entinostat,plans to evaluate the drug in combination witherlotinib in further randomized trials to be initiated in<strong>2011</strong> in selected NSCLC patients with high levels of E-cadherin, according to a statement by Syndax presidentand CEO Dr. Joanna Horobin.During a press conference at the meeting, Dr. FredHirsch, a professor of medicine with the University ofbevacizumab for advanced lung cancerplaced at about $8,800 in 2006. Only38% (or 154) of the 403 patients in thestudy received bevacizumab until diseaseprogression.The industry-sponsored study identifiedpatients with nonsquamous NSCLCfrom an electronic health records systemthat contains data from 884 communitybasedoncologists in US OncologyInc.–affiliated practices or clinics in 20states.Patients were treated from July 2006through June 2008, with 31% located inthe Southwest and 30% in the Southeast.In all, 37% of patients had private insurance,57% were covered by Medicare,and 6% had some other payer.The maintenance group tended tohave better pre- and postchemotherapyAdding entinostatincreased erlotinibsensitivity inresistant NSCLCpatients with highE-cadherin levels.DR. JOTTEColorado Cancer Center in Aurora, also cautioned thatan accepted standardized classification of E-cadherin expressionneeds to be established.In ENCORE 401, immunohistochemistry stainingvalues of +3 or greater were defined as highE-cadherin expression, and 0, +1, and +2were defined as low E-cadherin expression.In all, 132 patients who had progressed afterone or two prior chemotherapies forstage IIIB/IV NSCLC were randomized 1:1to erlotinib (150 mg once daily for 28 day)plus entinostat (10 mg on days 1 and 15 for28 days), or to erlotinib and placebo. Themajority was male (66%), had an ECOGperformance status of 0/1 (86%), had a historyof smoking (85%) and had adenocarcinomahistology (43%). Only 11 of 78patients who were tested had KRAS-mutanttumors.Entinostat/erlotinib was tolerable with nounexpected adverse events and a manageablesafety profile among evaluated patients,Dr. Jotte said.The most common grade 3/4 adverse event in eitherarm was fatigue, occurring in 16% of 63erlotinib/placebo patients and in 20% of 65 erlotinib/entinostatpatients. Fatal adverse events occurredin 25.4% of erlotinib/placebo patients vs. 18.5%of erlotinib/entinostat patients, with 43% of patientsin each arm discontinuing treatment because of adverseevents.The symposium was cosponsored by the American Societyof Clinical Oncology, the American Society for RadiationOncology, the International Association for theStudy of Lung Cancer, and the University of Chicago.Syndax Pharmaceuticals sponsored ENCORE 401.Dr. Jotte and his coauthors disclosed no conflicts ofinterest. Dr. Jänne disclosed financial relationshipswith AstraZeneca, Boehringer Ingelheim, Genentech,Pfizer, Roche, Gatekeeper Pharmaceuticals, andGenzyme.■Bevacizumab Maintenance Extended Lung Cancer SurvivalFOR THOSE ALIVE AND ALSOPROGRESSION FREE AT 18WEEKS, BEVACIZUMAB UNTILPROGRESSION WAS LINKED TO A46% REDUCED RISK OF DEATH.performance status scores and a greaternumber of completed chemotherapy cycles(median, six vs. four). Overall, 56%of the maintenance group and 39% ofthe no-maintenance group received asecond-line therapy.In order to control for survivorshipand selection bias, the researchers excludedthose patients who had diseaseprogression or death within 30 days oftheir chemotherapy completion; landmarkanalyses were conducted at 18,21, and 26 weeks from the initial treatment.Among those who were alive andprogression free at 18 weeks, bevacizumabmonotherapy until disease progressionwas associated with a 46%reduced risk of death (hazard ratio,0.54), reported Dr. Nadler of the TexasOncology–Baylor Sammons CancerCenter in Dallas.The association between bevacizumaband longer residual overall survival persistedamong patients who remainedprogression free and alive at 21 weeks(HR, 0.58) and 26 weeks (HR, 0.61).Bevacizumab monotherapy was foundto be associated with longer progression-freesurvival at 18 weeks (HR, 0.73),but the association was no longer observedat 21 weeks (HR, 0.82) and 26weeks (HR, 0.79).Although the nonrandomized natureof the study precludes making any conclusionsabout causality, the authors concludedthat the findings provide“significant insights into real-world patternsof care and associated outcomesand provide important evidence onwhich to base future comparative effectivenessresearch.”In a separate national survey of oncologists,Dr. Nadler and associates atTufts University in Boston reported that84% of oncologists say that patients’out-of-pocket spending influences treatmentrecommendations, even thoughonly 43% frequently or always discusscosts with patients.Among the 787 oncologists surveyed,79% favored more comparative effectivenessresearch and 80% supportedmore cost-effectiveness data, but only42% felt well prepared to interpret it(Health Aff. [Millwood] 2010;29:196-202).Genentech supported the study.Dr. Nadler reported no conflicts of interest.Three coauthors reported employmentwith Genentech and ownershipinterest in Roche Holdings.■
Get in the thick of itCovidien’s new black reloads enable surgeons tostaple into extra-thick tissue previously beyondthe indications of any MIS stapler.Innovating MoreSo You Can Do MoreTo learn more and request a demonstration ofTri-Staple Technology, visit www.tristaple.com.COVIDIEN, COVIDIEN with logo, and Covidien logo, are U.S. and/or internationally registered trademarks of Covidien AG.