Universal Screening for Hearing Loss in Newborns - US Preventive ...
Universal Screening for Hearing Loss in Newborns - US Preventive ...
Universal Screening for Hearing Loss in Newborns - US Preventive ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
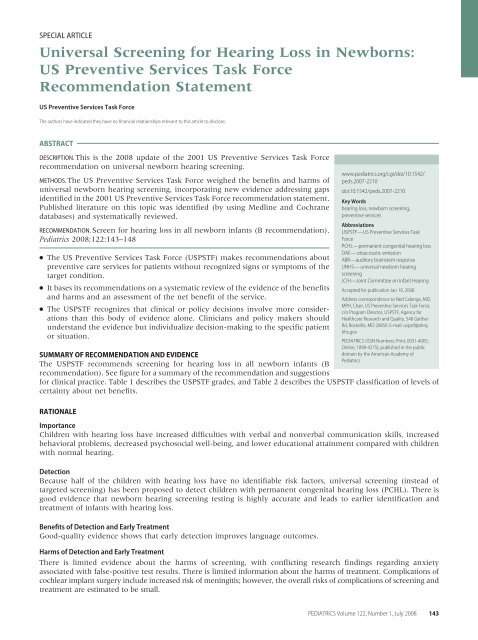
SPECIAL ARTICLE<strong>Universal</strong> <strong>Screen<strong>in</strong>g</strong> <strong>for</strong> <strong>Hear<strong>in</strong>g</strong> <strong>Loss</strong> <strong>in</strong> <strong>Newborns</strong>:<strong>US</strong> <strong>Preventive</strong> Services Task ForceRecommendation Statement<strong>US</strong> <strong>Preventive</strong> Services Task ForceThe authors have <strong>in</strong>dicated they have no f<strong>in</strong>ancial relationships relevant to this article to disclose.ABSTRACTDESCRIPTION. This is the 2008 update of the 2001 <strong>US</strong> <strong>Preventive</strong> Services Task Forcerecommendation on universal newborn hear<strong>in</strong>g screen<strong>in</strong>g.METHODS. The <strong>US</strong> <strong>Preventive</strong> Services Task Force weighed the benefits and harms ofuniversal newborn hear<strong>in</strong>g screen<strong>in</strong>g, <strong>in</strong>corporat<strong>in</strong>g new evidence address<strong>in</strong>g gapsidentified <strong>in</strong> the 2001 <strong>US</strong> <strong>Preventive</strong> Services Task Force recommendation statement.Published literature on this topic was identified (by us<strong>in</strong>g Medl<strong>in</strong>e and Cochranedatabases) and systematically reviewed.RECOMMENDATION. Screen <strong>for</strong> hear<strong>in</strong>g loss <strong>in</strong> all newborn <strong>in</strong>fants (B recommendation).Pediatrics 2008;122:143–148● The <strong>US</strong> <strong>Preventive</strong> Services Task Force (<strong>US</strong>PSTF) makes recommendations aboutpreventive care services <strong>for</strong> patients without recognized signs or symptoms of thetarget condition.● It bases its recommendations on a systematic review of the evidence of the benefitsand harms and an assessment of the net benefit of the service.● The <strong>US</strong>PSTF recognizes that cl<strong>in</strong>ical or policy decisions <strong>in</strong>volve more considerationsthan this body of evidence alone. Cl<strong>in</strong>icians and policy makers shouldunderstand the evidence but <strong>in</strong>dividualize decision-mak<strong>in</strong>g to the specific patientor situation.SUMMARY OF RECOMMENDATION AND EVIDENCEThe <strong>US</strong>PSTF recommends screen<strong>in</strong>g <strong>for</strong> hear<strong>in</strong>g loss <strong>in</strong> all newborn <strong>in</strong>fants (Brecommendation). See figure <strong>for</strong> a summary of the recommendation and suggestions<strong>for</strong> cl<strong>in</strong>ical practice. Table 1 describes the <strong>US</strong>PSTF grades, and Table 2 describes the <strong>US</strong>PSTF classification of levels ofcerta<strong>in</strong>ty about net benefits.RATIONALEImportanceChildren with hear<strong>in</strong>g loss have <strong>in</strong>creased difficulties with verbal and nonverbal communication skills, <strong>in</strong>creasedbehavioral problems, decreased psychosocial well-be<strong>in</strong>g, and lower educational atta<strong>in</strong>ment compared with childrenwith normal hear<strong>in</strong>g.DetectionBecause half of the children with hear<strong>in</strong>g loss have no identifiable risk factors, universal screen<strong>in</strong>g (<strong>in</strong>stead oftargeted screen<strong>in</strong>g) has been proposed to detect children with permanent congenital hear<strong>in</strong>g loss (PCHL). There isgood evidence that newborn hear<strong>in</strong>g screen<strong>in</strong>g test<strong>in</strong>g is highly accurate and leads to earlier identification andtreatment of <strong>in</strong>fants with hear<strong>in</strong>g loss.Benefits of Detection and Early TreatmentGood-quality evidence shows that early detection improves language outcomes.www.pediatrics.org/cgi/doi/10.1542/peds.2007-2210doi:10.1542/peds.2007-2210Key Wordshear<strong>in</strong>g loss, newborn screen<strong>in</strong>g,preventive servicesAbbreviations<strong>US</strong>PSTF—<strong>US</strong> <strong>Preventive</strong> Services TaskForcePCHL—permanent congenital hear<strong>in</strong>g lossOAE—otoacoustic emissionABR—auditory bra<strong>in</strong>stem responseUNHS—universal newborn hear<strong>in</strong>gscreen<strong>in</strong>gJCIH—Jo<strong>in</strong>t Committee on Infant <strong>Hear<strong>in</strong>g</strong>Accepted <strong>for</strong> publication Jan 10, 2008Address correspondence to Ned Calonge, MD,MPH, Chair, <strong>US</strong> <strong>Preventive</strong> Services Task Force,c/o Program Director, <strong>US</strong>PSTF, Agency <strong>for</strong>Healthcare Research and Quality, 540 GaitherRd, Rockville, MD 20850. E-mail: uspstf@ahrq.hhs.govPEDIATRICS (ISSN Numbers: Pr<strong>in</strong>t, 0031-4005;Onl<strong>in</strong>e, 1098-4275); published <strong>in</strong> the publicdoma<strong>in</strong> by the American Academy ofPediatricsHarms of Detection and Early TreatmentThere is limited evidence about the harms of screen<strong>in</strong>g, with conflict<strong>in</strong>g research f<strong>in</strong>d<strong>in</strong>gs regard<strong>in</strong>g anxietyassociated with false-positive test results. There is limited <strong>in</strong><strong>for</strong>mation about the harms of treatment. Complications ofcochlear implant surgery <strong>in</strong>clude <strong>in</strong>creased risk of men<strong>in</strong>gitis; however, the overall risks of complications of screen<strong>in</strong>g andtreatment are estimated to be small.PEDIATRICS Volume 122, Number 1, July 2008 143
<strong>Universal</strong> <strong>Screen<strong>in</strong>g</strong> <strong>for</strong> <strong>Hear<strong>in</strong>g</strong> <strong>Loss</strong> <strong>in</strong> <strong>Newborns</strong>:Cl<strong>in</strong>ical Summary of <strong>US</strong> <strong>Preventive</strong> Services Task Force RecommendationPopulationRecommendationAll <strong>Newborns</strong>Screen <strong>for</strong> hear<strong>in</strong>g loss <strong>in</strong> all newborn <strong>in</strong>fantsGrade: BThe prevalence of hear<strong>in</strong>g loss <strong>in</strong> newborn <strong>in</strong>fants with specific risk <strong>in</strong>dicators is 10 – 20 times higher than <strong>in</strong> the general population of newborns.Risk assessmentRisk <strong>in</strong>dicators associated with permanent bilateral congenital hear<strong>in</strong>g loss <strong>in</strong>clude:NICU admission <strong>for</strong> ≥ 2 dfamily history of hereditary childhood sensor<strong>in</strong>eural hear<strong>in</strong>g losscraniofacial abnormalitiescerta<strong>in</strong> congenital syndromes and <strong>in</strong>fectionsApproximately 50% of newborns with permanent bilateral congenital hear<strong>in</strong>g loss do not have any known risk <strong>in</strong>dicators.<strong>Screen<strong>in</strong>g</strong> tests<strong>Screen<strong>in</strong>g</strong> programs should be conducted by us<strong>in</strong>g a 1-step or 2-step validated protocol.A frequently-used 2-step screen<strong>in</strong>g process <strong>in</strong>volves otoacoustic emissions followed by auditory bra<strong>in</strong> stem response <strong>in</strong> newborns who fail the first test.Infants with positive screen<strong>in</strong>g test results should receive appropriate audiologic evaluation and follow-up after discharge.Procedures <strong>for</strong> screen<strong>in</strong>g and follow-up should be <strong>in</strong> place <strong>for</strong> newborns delivered at home, birth<strong>in</strong>g centers, or hospitals without hear<strong>in</strong>g screen<strong>in</strong>g facilities.Tim<strong>in</strong>g of screen<strong>in</strong>gAll <strong>in</strong>fants should have hear<strong>in</strong>g screen<strong>in</strong>g be<strong>for</strong>e 1 mo of age.Infants who do not pass the newborn screen<strong>in</strong>g should undergo audiologic and medical evaluation be<strong>for</strong>e 3 mo of age.TreatmentEarly <strong>in</strong>tervention services <strong>for</strong> hear<strong>in</strong>g-impaired <strong>in</strong>fants should meet the <strong>in</strong>dividualized needs of the <strong>in</strong>fant and family, <strong>in</strong>clud<strong>in</strong>g acquisition of communicationcompetence, social skills, emotional well-be<strong>in</strong>g, and positive self-esteem.Early <strong>in</strong>tervention comprises evaluation <strong>for</strong> amplification or sensory devices, surgical and medical evaluation, and communication assessment and therapy.Cochlear implants are usually considered <strong>for</strong> children with severe-to-profound hear<strong>in</strong>g loss only after <strong>in</strong>adequate response to hear<strong>in</strong>g aids.Other relevantrecommendationsfrom the <strong>US</strong>PSTFAdditional <strong>US</strong>PSTF recommendations regard<strong>in</strong>g screen<strong>in</strong>g tests <strong>for</strong> newborns can be accessed at www.ahrq.gov/cl<strong>in</strong>ic/cps3dix.htm#pediatric.For the full recommendation statement and support<strong>in</strong>g documents (<strong>in</strong>clud<strong>in</strong>g a summary of the evidence) please go to www.preventiveservices.ahrq.gov.FIGURECl<strong>in</strong>ical summary of <strong>US</strong>PSTF recommendation.<strong>US</strong>PSTF AssessmentThe <strong>US</strong>PSTF concludes that there is moderate certa<strong>in</strong>tythat the net benefit of screen<strong>in</strong>g all newborn <strong>in</strong>fants <strong>for</strong>hear<strong>in</strong>g loss is moderate.CLINICAL CONSIDERATIONSPatient Population Under ConsiderationThe patient population considered here <strong>in</strong>cludes allnewborn <strong>in</strong>fants.TABLE 1What the <strong>US</strong>PSTF Grades Mean and Suggestions <strong>for</strong> PracticeGrade Grade Def<strong>in</strong>itions Suggestions <strong>for</strong> PracticeAThe <strong>US</strong>PSTF recommends the service. There is high certa<strong>in</strong>ty that the net Offer/provide this service.benefit is substantial.BThe <strong>US</strong>PSTF recommends the service. There is high certa<strong>in</strong>ty that the net Offer/provide this service.benefit is moderate or there is moderate certa<strong>in</strong>ty that the net benefit ismoderate to substantial.CThe <strong>US</strong>PSTF recommends aga<strong>in</strong>st rout<strong>in</strong>ely provid<strong>in</strong>g the service. Theremay be considerations that support provid<strong>in</strong>g the service <strong>in</strong> an<strong>in</strong>dividual patient. There is moderate or high certa<strong>in</strong>ty that the netOffer/provide this service only if there are other considerations<strong>in</strong> support of the offer<strong>in</strong>g/provid<strong>in</strong>g the service <strong>in</strong> an<strong>in</strong>dividual patient.benefit is small.DThe <strong>US</strong>PSTF recommends aga<strong>in</strong>st the service. There is moderate or highcerta<strong>in</strong>ty that the service has no net benefit or that the harms outweighthe benefits.Discourage the use of this service.I statementThe <strong>US</strong>PSTF concludes that the current evidence is <strong>in</strong>sufficient to assess thebalance of benefits and harms of the service. Evidence is lack<strong>in</strong>g, of poorquality, or conflict<strong>in</strong>g, and the balance of benefits and harms cannot bedeterm<strong>in</strong>ed.Read “Cl<strong>in</strong>ical Considerations” <strong>in</strong> the <strong>US</strong>PSTF RecommendationStatement. If offered, patients should understand theuncerta<strong>in</strong>ty about the balance of benefits and harms.144 <strong>US</strong> PREVENTIVE SERVICES TASK FORCE
TABLE 2Level ofCerta<strong>in</strong>tyHighModerateLow<strong>US</strong>PSTF Levels of Certa<strong>in</strong>ty Regard<strong>in</strong>g Net BenefitDescriptionThe available evidence usually <strong>in</strong>cludes consistent results fromwell-designed, well-conducted studies <strong>in</strong> representativeprimary care populations. These studies assess theeffects of the preventive service on health outcomes.The conclusion, there<strong>for</strong>e, is unlikely to be stronglyaffected by the results of future studies.The available evidence is sufficient to determ<strong>in</strong>e the effects ofthe preventive service on health outcomes, butconfidence <strong>in</strong> the estimate is constra<strong>in</strong>ed by factorssuch as:the number, size, or quality of <strong>in</strong>dividual studies;<strong>in</strong>consistency of f<strong>in</strong>d<strong>in</strong>gs across <strong>in</strong>dividual studies;limited generalizability of f<strong>in</strong>d<strong>in</strong>gs to rout<strong>in</strong>e primary carepractice; orlack of coherence <strong>in</strong> the cha<strong>in</strong> of evidenceAs more <strong>in</strong><strong>for</strong>mation becomes available, the magnitude ordirection of the observed effect could change, and thechange may be large enough to alter the conclusion.The available evidence is <strong>in</strong>sufficient to assess effects onhealth outcomes. Evidence is <strong>in</strong>sufficient because of:the limited number or size of studies;important flaws <strong>in</strong> study design or methods;<strong>in</strong>consistency of f<strong>in</strong>d<strong>in</strong>gs across <strong>in</strong>dividual studies;gaps <strong>in</strong> the cha<strong>in</strong> of evidence;f<strong>in</strong>d<strong>in</strong>gs not generalizable to rout<strong>in</strong>e primary carepractice; ora lack of <strong>in</strong><strong>for</strong>mation on important health outcomesMore <strong>in</strong><strong>for</strong>mation may allow an estimation of effects on healthoutcomes.The <strong>US</strong>PSTF def<strong>in</strong>es certa<strong>in</strong>ty as “likelihood that the <strong>US</strong>PSTF assessment of the net benefit of apreventive service is correct.” The net benefit is def<strong>in</strong>ed as benefit m<strong>in</strong>us harm of the preventiveservice as implemented <strong>in</strong> a general, primary care population. The <strong>US</strong>PSTF assigns a certa<strong>in</strong>tylevel on the basis of the nature of the overall evidence available to assess the net benefit of apreventive service.Assessment of RiskRisk factors associated with a higher <strong>in</strong>cidence of permanentbilateral congenital hear<strong>in</strong>g loss <strong>in</strong>clude NICUadmission <strong>for</strong> 2 days, several congenital syndromes,family history of hereditary childhood sensor<strong>in</strong>euralhear<strong>in</strong>g loss, craniofacial abnormalities, and certa<strong>in</strong> congenital<strong>in</strong>fections. However, 50% of <strong>in</strong>fants with permanentbilateral congenital hear<strong>in</strong>g loss do not have anyknown risk factors.<strong>Screen<strong>in</strong>g</strong> Tests<strong>Screen<strong>in</strong>g</strong> programs should be conducted by us<strong>in</strong>g a 1-or 2-step validated protocol. A frequently used protocolrequires a 2-step screen<strong>in</strong>g process, which <strong>in</strong>cludes otoacousticemissions (OAEs) followed by auditory bra<strong>in</strong>stemresponse (ABR) <strong>in</strong> those who failed the first test.Equipment should be well ma<strong>in</strong>ta<strong>in</strong>ed, staff should bethoroughly tra<strong>in</strong>ed, and quality-control programsshould be <strong>in</strong> place to reduce avoidable false-positive testresults. Programs should develop protocols to ensurethat <strong>in</strong>fants with positive screen<strong>in</strong>g-test results receiveappropriate audiologic evaluation and follow-up afterdischarge. <strong>Newborns</strong> delivered at home, birth<strong>in</strong>g centers,or hospitals without hear<strong>in</strong>g screen<strong>in</strong>g facilitiesshould have some mechanism <strong>for</strong> referral <strong>for</strong> newbornhear<strong>in</strong>g screen<strong>in</strong>g, <strong>in</strong>clud<strong>in</strong>g track<strong>in</strong>g of follow-up.TreatmentEarly <strong>in</strong>tervention services <strong>for</strong> hear<strong>in</strong>g-impaired <strong>in</strong>fantsshould be designed to meet the <strong>in</strong>dividualized needs ofthe <strong>in</strong>fant and family, <strong>in</strong>clud<strong>in</strong>g acquisition of communicationcompetence, social skills, emotional well-be<strong>in</strong>g,and positive self-esteem. Early <strong>in</strong>tervention <strong>in</strong>cludesevaluation <strong>for</strong> amplification or sensory devices, surgicaland medical evaluation, and communication assessmentand therapy. In recent years, cochlear implants havebecome more available <strong>for</strong> appropriate candidates; thissurgery is usually considered <strong>in</strong> those with severe-toprofoundhear<strong>in</strong>g loss only after <strong>in</strong>adequate response tohear<strong>in</strong>g aids.<strong>Screen<strong>in</strong>g</strong> IntervalsAll <strong>in</strong>fants should have hear<strong>in</strong>g screen<strong>in</strong>g be<strong>for</strong>e 1month of age. Those <strong>in</strong>fants who do not pass the newbornscreen<strong>in</strong>g should undergo audiologic and medicalevaluation be<strong>for</strong>e 3 months of age <strong>for</strong> confirmatory test<strong>in</strong>g.Because of the elevated risk of hear<strong>in</strong>g loss <strong>in</strong> <strong>in</strong>fantswith risk <strong>in</strong>dicators, an expert panel has made a 2000recommendation that these children should undergo periodicmonitor<strong>in</strong>g <strong>for</strong> 3 years. 1OTHER CONSIDERATIONSImplementationThirty-n<strong>in</strong>e <strong>US</strong> states have enacted legislation related touniversal newborn hear<strong>in</strong>g screen<strong>in</strong>g (UNHS). Theselaws differ with respect to whether screen<strong>in</strong>g is mandatedor encouraged, how results are reported, and howscreen<strong>in</strong>g is funded.Research Needs/GapsAdditional studies detail<strong>in</strong>g the correlation betweenchildhood language scores and functional outcomes (eg,school atta<strong>in</strong>ment and social function<strong>in</strong>g) are needed.DISC<strong>US</strong>SIONBurden of DiseaseThe focus of UNHS programs is on congenital (as opposedto acquired or progressive) hear<strong>in</strong>g loss that maynot be detected <strong>in</strong> the newborn period. Accord<strong>in</strong>g to the2000 statement from the Jo<strong>in</strong>t Committee on Infant<strong>Hear<strong>in</strong>g</strong> (JCIH), hear<strong>in</strong>g screen<strong>in</strong>g should identify <strong>in</strong>fantsat risk <strong>for</strong> specifically def<strong>in</strong>ed hear<strong>in</strong>g loss that<strong>in</strong>terferes with development. The targeted hear<strong>in</strong>g loss<strong>for</strong> UNHS programs is permanent sensory or conductivehear<strong>in</strong>g loss averag<strong>in</strong>g 30 to 40 dB or more <strong>in</strong> the frequencyregion important <strong>for</strong> speech recognition (500–4000 Hz). 1 PCHL occurs <strong>in</strong> 1 to 3 per 1000 live births.The prevalence <strong>for</strong> PCHL is higher than <strong>for</strong> other conditionsscreened <strong>for</strong> <strong>in</strong> the newborn period. Children withhear<strong>in</strong>g loss may have difficulty learn<strong>in</strong>g grammar, wordorder, idiomatic expressions, and other <strong>for</strong>ms of verbalcommunication. 2 Delayed language and speech, low educationalatta<strong>in</strong>ment, <strong>in</strong>creased behavior problems, de-PEDIATRICS Volume 122, Number 1, July 2008 145
most negative emotions resolved after the child’s def<strong>in</strong>itivehear<strong>in</strong>g test. 2Evidence regard<strong>in</strong>g the harms of treatment is alsolimited. The have been few immediate complications ofsurgery reported <strong>in</strong> case series and case reports of cochlearimplant surgery <strong>in</strong> <strong>in</strong>fants; however, an <strong>in</strong>creasedrisk of men<strong>in</strong>gitis that may persist <strong>for</strong> several years afterimplantation has been reported. Note that these caseseries reflect the use of a no-longer-manufactured cochlearimplant. Furthermore, children with congenitalcochlear abnormalities may have a predisposition tomen<strong>in</strong>gitis regardless of the use of cochlear implants.The overall complications of screen<strong>in</strong>g and treatment areestimated to be small.Estimate of Magnitude of Net BenefitThere is good evidence that newborn hear<strong>in</strong>g-screen<strong>in</strong>gtest<strong>in</strong>g is highly accurate and leads to earlier identificationand treatment of <strong>in</strong>fants with hear<strong>in</strong>g loss. Withregard to the yield of screen<strong>in</strong>g 10 000 newborns <strong>for</strong>hear<strong>in</strong>g loss by us<strong>in</strong>g universal versus targeted screen<strong>in</strong>g,universal screen<strong>in</strong>g would yield 7 more cases diagnosedby 3 months of age (1 with risk factors and 6without known risk factors). The number needed toscreen to diagnose 1 case is 878 and 178 <strong>for</strong> UNHS andtargeted screen<strong>in</strong>g programs, respectively. The numberneeded to screen to diagnose 1 additional case by 3months of age is 1333 <strong>for</strong> UNHS. 2RECOMMENDATIONS OF OTHER GROUPSThe JCIH endorses early detection and <strong>in</strong>tervention <strong>for</strong><strong>in</strong>fants with hear<strong>in</strong>g loss through <strong>in</strong>tegrated, <strong>in</strong>terdiscipl<strong>in</strong>arystate and national systems of UNHS, evaluation,and family-centered <strong>in</strong>tervention. The JCIH 2000 positionstatement (and recently released 2007 statement)provides guidel<strong>in</strong>es that <strong>in</strong>clude UNHS soon after birth,be<strong>for</strong>e hospital discharge, or be<strong>for</strong>e 1 month of age;diagnosis of hear<strong>in</strong>g loss through audiologic and medicalevaluation be<strong>for</strong>e 3 months of age; and <strong>in</strong>terventionthrough <strong>in</strong>terdiscipl<strong>in</strong>ary programs <strong>for</strong> <strong>in</strong>fants with confirmedhear<strong>in</strong>g loss be<strong>for</strong>e 6 months. 1,11 The AmericanAcademy of Pediatrics Task Force on Newborn and Infant<strong>Hear<strong>in</strong>g</strong>, the National Institute on Deafness andOther Communication Disorders, and the Centers <strong>for</strong>Disease Control and Prevention Early <strong>Hear<strong>in</strong>g</strong> Detectionand Intervention Program support the JCIH recommendations.12–14 The American Academy of Audiology TaskForce on the Early Identification of <strong>Hear<strong>in</strong>g</strong> <strong>Loss</strong> agreesthat the use of support personnel <strong>in</strong> newborn hear<strong>in</strong>gscreen<strong>in</strong>gprograms is an appropriate and often necessarystrategy <strong>for</strong> achiev<strong>in</strong>g universal detection of congenitalhear<strong>in</strong>g loss. 15 The supervis<strong>in</strong>g audiologist shouldbe experienced <strong>in</strong> both the development and ma<strong>in</strong>tenanceof a UNHS program, <strong>in</strong>clud<strong>in</strong>g an understand<strong>in</strong>gof technology options.MEMBERS OF THE <strong>US</strong>PSTFMembers of the <strong>US</strong>PSTF at the time this recommendationwas f<strong>in</strong>alized were Ned Calonge, MD, MPH, <strong>US</strong>PSTFChair (Colorado Department of Public Health and Environment,Denver, CO); Diana B. Petitti, MD, MPH, <strong>US</strong>P-STF Vice-chair (Keck School of Medic<strong>in</strong>e, University ofSouthern Cali<strong>for</strong>nia, Sierra Madre, CA); Thomas G.DeWitt, MD (Children’s Hospital Medical Center, C<strong>in</strong>c<strong>in</strong>nati,OH); Leon Gordis, MD, MPH, DrPH (Johns Hopk<strong>in</strong>sBloomberg School of Public Health, Baltimore,MD); Kimberly D. Gregory, MD, MPH (Cedars-S<strong>in</strong>aiMedical Center, Los Angeles, CA); Russell Harris, MD,MPH (University of North Carol<strong>in</strong>a School of Medic<strong>in</strong>e,Chapel Hill, NC); George Isham, MD, MS (HealthPartners,M<strong>in</strong>neapolis, MN); Michael L. LeFevre, MD, MSPH(University of Missouri School of Medic<strong>in</strong>e, Columbia,MO); Carol Loveland-Cherry, PhD, RN (University ofMichigan School of Nurs<strong>in</strong>g, Ann Arbor, MI); Lucy N.Marion, PhD, RN (Medical College of Georgia, Augusta,GA); Virg<strong>in</strong>ia A. Moyer, MD, MPH (University of TexasHealth Science Center, Houston, TX); Judith K. Ockene,PhD (University of Massachusetts Medical School,Worcester, MA); George F. Sawaya, MD (University ofCali<strong>for</strong>nia, San Francisco, CA); Albert L. Siu, MD, MSPH(Mount S<strong>in</strong>ai Medical Center, New York, NY); Steven M.Teutsch, MD, MPH (Merck & Company, Inc, West Po<strong>in</strong>t,PA); and Barbara P. Yawn, MD, MSPH, MSc (OlmstedMedical Center, Rochester, MN). For a list of current task<strong>for</strong>ce members, go to www.ahrq.gov/cl<strong>in</strong>ic/uspstfab.htm.REFERENCES1. Jo<strong>in</strong>t Committee on Infant <strong>Hear<strong>in</strong>g</strong>; American Academy ofAudiology; American Academy of Pediatrics; AmericanSpeech-Language-<strong>Hear<strong>in</strong>g</strong> Association; Directors of Speechand <strong>Hear<strong>in</strong>g</strong> Programs <strong>in</strong> State Health and Welfare Agencies.Year 2000 position statement: pr<strong>in</strong>ciples and guidel<strong>in</strong>es <strong>for</strong>early hear<strong>in</strong>g detection and <strong>in</strong>tervention programs. Pediatrics.2000;106(4):798–8172. Nelson HD, Bougatsos C, Nygren P. <strong>Universal</strong> Newborn <strong>Hear<strong>in</strong>g</strong><strong>Screen<strong>in</strong>g</strong>: Systematic Review to Update the 2001 U.S.<strong>Preventive</strong> Services Task Force Recommendation. Pediatrics.2008;122(1):e266–e2763. Helfand M, Thompson DC, Davis RL, McPhillips H, Homer CJ,Lieu TL. Newborn hear<strong>in</strong>g screen<strong>in</strong>g. Rockville, MD: Agency<strong>for</strong> Healthcare Research and Quality; 2001. Systematic evidencereview No. 5; AHRQ publication 02-S001. Available at:www.ahrq.gov/cl<strong>in</strong>ic/serfiles.htm. Accessed July 17, 20074. Kennedy C, McCann D, Campbell MJ, Kimm L, Thornton R.<strong>Universal</strong> newborn screen<strong>in</strong>g <strong>for</strong> permanent childhood hear<strong>in</strong>gimpairment: an 8-year follow-up of a controlled trial. Lancet.2005;366(9486):660–6625. Wessex <strong>Universal</strong> Neonatal <strong>Hear<strong>in</strong>g</strong> <strong>Screen<strong>in</strong>g</strong> Trial Group.Controlled trial of universal neonatal screen<strong>in</strong>g <strong>for</strong> early identificationof permanent childhood hear<strong>in</strong>g impairment. Lancet.1998;352(9145):1957–19646. Kennedy CR, McCann DC, Campbell MJ, et al. Language abilityafter early detection of permanent childhood hear<strong>in</strong>g impairment.N Engl J Med. 2006;354(20):2131–21417. Wake M, Hughes EK, Poulakis Z, Coll<strong>in</strong>s C, Rickards FW.Outcomes of children with mild-profound congenital hear<strong>in</strong>gloss at 7 to 8 years: a population study. Ear Hear. 2004;25(1):1–88. Moeller MP. Early <strong>in</strong>tervention and language development <strong>in</strong>children who are deaf and hard of hear<strong>in</strong>g. Pediatrics. 2000;106(3). Available at: www.pediatrics.org/cgi/content/full/106/3/e43PEDIATRICS Volume 122, Number 1, July 2008 147
9. Calderon R, Naidu S. Further support of the benefits of earlyidentification and <strong>in</strong>tervention with children with hear<strong>in</strong>g loss.Volta Rev. 2000;100(4):53–8410. Kennedy CR. Controlled trial of universal neonatal screen<strong>in</strong>g<strong>for</strong> early identification of permanent childhood hear<strong>in</strong>gimpairment: coverage, positive predictive value, effect onmothers and <strong>in</strong>cremental yield. Wessex <strong>Universal</strong> Neonatal<strong>Screen<strong>in</strong>g</strong> Trial Group. Acta Paediatr Suppl. 1999:88(432):73–7511. American Academy of Pediatrics, Jo<strong>in</strong>t Committee on Infant<strong>Hear<strong>in</strong>g</strong>. Year 2007 position statement: pr<strong>in</strong>ciples and guidel<strong>in</strong>es<strong>for</strong> early hear<strong>in</strong>g detection and <strong>in</strong>tervention programs.Pediatrics. 2007;120(4):898–92112. American Academy of Pediatrics, Task Force on Newborn andInfant <strong>Hear<strong>in</strong>g</strong>. Newborn and <strong>in</strong>fant hear<strong>in</strong>g loss: detection and<strong>in</strong>tervention. Pediatrics. 1999;103(2):527–53013. Centers <strong>for</strong> Disease Control and Prevention. Infants tested <strong>for</strong>hear<strong>in</strong>g loss: United States [published correction appears <strong>in</strong>MMWR Morb Mortal Wkly Rep. 2003;42(49):1210]. MMWR MorbMortal Wkly Rep. 2003;52(41):981–98414. National Institutes of Health. Early identification of hear<strong>in</strong>gimpairment <strong>in</strong> <strong>in</strong>fants and young children. NIH Consens Statement.1993;11(1):1–2415. American Academy of Audiology. Considerations <strong>for</strong> the useof support personnel <strong>for</strong> newborn hear<strong>in</strong>g screen<strong>in</strong>g. Availableat: www.audiology.org/publications/documents/positions/InfantID/usp4nhs.htm. Accessed April 23, 2008148 <strong>US</strong> PREVENTIVE SERVICES TASK FORCE