perio study guide.pdf
perio study guide.pdf
perio study guide.pdf
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
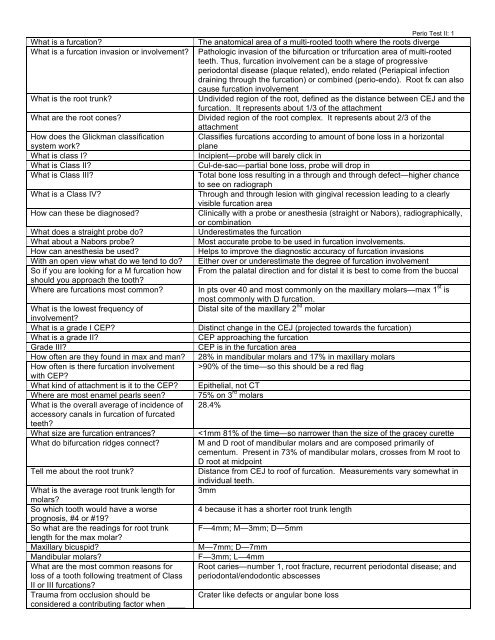
What is a furcation?What is a furcation invasion or involvement?What is the root trunk?What are the root cones?How does the Glickman classificationsystem work?What is class I?What is Class II?What is Class III?What is a Class IV?How can these be diagnosed?What does a straight probe do?What about a Nabors probe?How can anesthesia be used?With an open view what do we tend to do?So if you are looking for a M furcation howshould you approach the tooth?Where are furcations most common?What is the lowest frequency ofinvolvement?What is a grade I CEP?What is a grade II?Grade III?How often are they found in max and man?How often is there furcation involvementwith CEP?What kind of attachment is it to the CEP?Where are most enamel pearls seen?What is the overall average of incidence ofaccessory canals in furcation of furcatedteeth?What size are furcation entrances?What do bifurcation ridges connect?Tell me about the root trunk?What is the average root trunk length formolars?So which tooth would have a worseprognosis, #4 or #19?So what are the readings for root trunklength for the max molar?Maxillary bicuspid?Mandibular molars?What are the most common reasons forloss of a tooth following treatment of ClassII or III furcations?Trauma from occlusion should beconsidered a contributing factor when ____Perio Test II: 1The anatomical area of a multi-rooted tooth where the roots divergePathologic invasion of the bifurcation or trifurcation area of multi-rootedteeth. Thus, furcation involvement can be a stage of progressive<strong>perio</strong>dontal disease (plaque related), endo related (Periapical infectiondraining through the furcation) or combined (<strong>perio</strong>-endo). Root fx can alsocause furcation involvementUndivided region of the root, defined as the distance between CEJ and thefurcation. It represents about 1/3 of the attachmentDivided region of the root complex. It represents about 2/3 of theattachmentClassifies furcations according to amount of bone loss in a horizontalplaneIncipient—probe will barely click inCul-de-sac—partial bone loss, probe will drop inTotal bone loss resulting in a through and through defect—higher chanceto see on radiographThrough and through lesion with gingival recession leading to a clearlyvisible furcation areaClinically with a probe or anesthesia (straight or Nabors), radiographically,or combinationUnderestimates the furcationMost accurate probe to be used in furcation involvements.Helps to improve the diagnostic accuracy of furcation invasionsEither over or underestimate the degree of furcation involvementFrom the palatal direction and for distal it is best to come from the buccalIn pts over 40 and most commonly on the maxillary molars—max 1 st ismost commonly with D furcation.Distal site of the maxillary 2 nd molarDistinct change in the CEJ (projected towards the furcation)CEP approaching the furcationCEP is in the furcation area28% in mandibular molars and 17% in maxillary molars>90% of the time—so this should be a red flagEpithelial, not CT75% on 3 rd molars28.4%
or _____ are seen?Does a maxillary bicuspid with furcationinvolved have a good prognosis?How do you treat these?Very poor because the furca is so far apicalPerio Test II: 2SRP, access flap surgery, <strong>guide</strong>d tissue regeneration and or bone graft;root amputation—DB most common; tunneling; bicuspidization (mandmolars), and implants4/22/08: PERIODONTAL PLASTIC SURGERYWhere is the zone of the greatest amount of keratinized tissue?• On the facial it is greater in the anterior and less in the posterior• On the lingual it is greater posterior to anterior• Overall, lower lingual has the greatest bandWhat is the most imp factor to determine the prognosis of the tooth?• Attachment lossWhat determines the gingival contour?• Interdental space—remember greater scalloping in the anterior than posterior d/t more spaceWhat tooth has the greatest dehiscence (#1 thinnest site of bone on a tooth) in the mouth?• MB root of the upper 1 st molarWhat is in all sensitivity toothpaste?• Potassium nitrateRoot coverage predictability is correlated to the presence or absence of interdental boneWhat happens when you take piece of tissue and place from donor site of palate to the recipient site?• Will get keratinized tissue—epithelialization comes from lateral margins because all the epithelium in the graftsloughsunderlying tissue gives its nutrition (REMEMBER there are NO blood vessels in the epithelium).What determines whether or not it is keratinized?• Site of originWhere does the coating reside?• In the connective tissue—important b/c it is the basis for root coverageKnow the miller classifications!Class I—marginal recession not extending to the MGJ; NO loss of interdental bone or soft tissue; possible toobtain 100% coverage of exposed rootClass II—marginal recession extends to or beyond the MGJ; NO loss of interdental bone or soft tissue;possible to obtain 100% coverage of exposed rootClass III—marginal tissue extend to or beyond the MGJ; loss of interdental bone and or soft tissue is apicalto CEJ, but coronal to the most apical extent of the recession; possible to obtain partial coverage of exposedroot (50-75%)Class IV—marginal tissue extends to or beyond the MGJ; loss of interdental tissues extends to apical extentof the recession; not possible to obtain any significant degree of root coverageWhat is the determinant of root coverage?• The amount of interdental boneHow much keratinized tissue do you need?• In presence of good OH you could get away with little to no keratinized tissue, w/o good OH lots of controversyTake tissue from anywhere and the epithelium will disintegrate!Easy to correct B width, difficult to correct Height!
28% know this %, why is it important• % of accessory canals found in furcations overallPerio Test II: 3What is the etiology of furcations?• Bacterial plaque in a susceptible hostWhen looking for a furcation on the mesial, which direction is it best to come from?• PalatalWhen looking for a furcation on the distal, which direction is it best to come from?• BuccalWhich furcation is involved the most?• M of maxillary 1 st molar, remember the mesial is the most common and this is where you would probe if youcould only probe one spaceWhy is the mesial the most involved when facial of the mand 1 st is just as short?• Facial of the lower 1 st molar is also just as short, but you can clean that much better because it is not aninterproximal area (which is not cleaned by a toothbrush)With the M furcation you can probe from which direction?• The palatal directionMUCOGINGIVAL PROBLEMSWhen do mucogingival problems result?When there has been a loss of attached and or keratinized tissues tosuch an extent that the remaining tissue is considered clinicallyinadequateHow much is enough when it comes to keratinized If pt has good OH, they can keep areas of little to no keratinized tissuetissue?healthy, but if poor OH it is up in the air as to how much is enoughHow do you diagnose localized gingivalVisual, measurement of the amount of attached and keratinizedrecession?mucosa, use of probe to determine level of the mucogingival junction,and muscle and frenulum pull on marginal gingivaWhat are etiologic and or predisposing factors? Inadequate attached gingiva, malposed teeth (affects the amount ofscalloping), tooth brushing technique, chronic inflammation, iatrogenic(restorative), iatrogenic (ortho), factitious injury, high frenulumattachment, alveolar housing and eruption pattern, smoking/smokelesstobacco use—always put in the same place, ortho treatment—maymove tooth too far, and substance abuse (cocaine)What are Miller’s classifications of gingivalrecession?What are treatment options?What is the etiology of localized ridge defects?What are the classifications of alveolar ridgeClass I—marginal recession not extending to the MGJ; NO loss ofinterdental bone or soft tissue; possible to obtain 100% coverageof exposed rootClass II—marginal recession extends to or beyond the MGJ; NO lossof interdental bone or soft tissue; possible to obtain 100%coverage of exposed rootClass III—marginal tissue extend to or beyond the MGJ; loss ofinterdental bone and or soft tissue is apical to CEJ, but coronal tothe most apical extent of the recession; possible to obtain partialcoverage of exposed root (50-75%)Class IV—marginal tissue extends to or beyond the MGJ; loss ofinterdental tissues extends to apical extent of the recession; notpossible to obtain any significant degree of root coverageFree autogenous gingival graft (FGG)—severed from donor,connective tissue graft (<strong>perio</strong>plastic surgery), semi-lunar incision+coronal repositioned flap (Tarnow); FGG + coronal repositioning ofkeratinized gingivaResorption of alveolar ridge following traumatic tooth extraction,developmental defects, advanced <strong>perio</strong>dontal disease, excessive ridgeresorption over time, and acute traumaClass I—facial-lingual defect with ridge exhibiting collapse towards the
Perio Test II: 4defects?lingual (usually) or facial (rarely)Class II—coronal-apical defect with ridge exhibiting loss vertical.Height most difficult to correctClass III—combination defect (commonly seen in anterior sextants)What are the treatment options?Gingival only graft, connective tissue graft, or barrier membranes+osseous graftingFURCATIONS• What is Furcation involvement?o Pathologic involvement of bone in Furcation area. Loss of attachment and bone involvement• Why do you need a classification system?o Determines prognosis of tooth• What makes furcations difficult?o Pts cannot clean well (proxy brush)• What is the problem with straight probes?o Underestimate Furcation• What if you don’t have complete Furcation visualization?o Tend to overclassify, because you can’t see• When you are looking for furcations where do you look?o Know anatomy and place probe where furcation would be• Diagnosis is best determined by?o Probeo Radiographo Bone sounding• Where is the most common place for a furcation to develop?o Max 1 st molar on distal furcation• Where is the least common place for furcation to develop?o Distal max 2 nd molar• What are the contributory factorso Anatomic Cervical enamel projections Enamel pearls Accessory canals Furcation entrance Rootform Bifurcation ridges Root trunko Supervised neglecto Trauma from occlusion• If you see a CEP what should you look for? (asked 2 times)o Furcation involvement• If you have a tooth that had RCT but has a furcation what is wrong?o Accessory canal• What feature of furcations makes them progress more?o The are larger than most curette, and we can’t get in there and clean themo This is why we flap for access• How far on the root trunk can we get until we are in the furcation?
Perio Test II: 5o• From above chart, what is the worse prognosis, 6 mm attachment loss on max molar or max bicuspid?o Max molar, less distance to furcation• What is better to avoid furcation involvement, long root trunk or short root trunk?o Long root trunk• How does furcation involvement effect the long term prognosis of a tooth?o Poor long term prognosis (31%-44% loss rate after 20 years)• What are the most common causes of Class II or Class II furcations?a. Root cariesb. Root fracture (if endo treated)c. Recurrent <strong>perio</strong>dontal diseased. Periodontal/endodontic abscess• Why would you do enameloplasty on a furcation area?o Makes it bigger to be able to clean effectively• How do you treat furcation teeth?o Scaling and rt planningo Osteo-dentin-ameloplasty (better access)o Access flap surgery-open scaling and root planningo Guided tissue regeneration and/or bone grafto Root amputationo Tunneling (cause root carries)o Bicuspidization (cut molar in half)o Cavitron (more narrow and reaches in furcation)• What could cause a breakdown of furcation bone that is NOT <strong>perio</strong>dontal disease?o Trauma from occlusiono Crater like defects or angular bone loss• What feature of the furcation involvement of a maxillary bicuspid makes its prognosis so poor?o Furca is so far apical• What are 2 causes of furcation involvement that do not start from <strong>perio</strong>dontal disease?o Traumatic occlusiono Accessory canal (endo-<strong>perio</strong> lesion)o Super-eruptionMUCOGINGIVAL PROBLEMS• Mucogingival surgery = peri-plastic surgery• How much attached gingiva is enough?o Research: over an 8 year <strong>perio</strong>d, people with good oral hygiene and 1 mm attachment, have a 92% chance of notlosing attachmento Therefore,
Perio Test II: 6o Interproximal bone• Purpose of the free gingival graft?o Increase the thickness of keratinized tissue not to cover roots (connective tissue grafts cover roots)• What happens when you graft tissue?o Epithelium disintegrates, and bare CT remainso Epithelium later will regenerateo Therefore, graft must include CT• So where is the DNA coding that determines what the epithelium type of covering will be produced?o In the connective tissue• Are there any blood vessels in epitheliumo No• What are the advantages of thick grafts?o Plenty of CT for forming epitheliumo Less shrinkage• What has better color match, free gingival graft or CT graft?o Ct graftMucogingival Problems26Apr05Describe the trend of attached gingiva in the mouth.Facial: widest in anterior, narrowest in posterior;Lingual: widest in posterior, narrowest in anteriorT/F: Less than 1mm of attached gingiva is adequate for T, if inflammation if controlledhealth.A patient taking procardia has a pocket depth of 8mm; but as 2mm; procardia will likely give you a pseudopocket;you withdraw your probe, a click is felt at 6mm. What is the the click was the CEJ.attachement loss?Name 234 ways to mess up an RPD.Name as many etiologic and/or predisposing factors forlocalized gingival recession.Describe the 4 Miller classes of gingival recession.(MGJ = mucogingival junction, b/st = bone & softtissue)Describe the possible root coverage that can be obtained foreach Miller class of gingival recession.What determines the tissue of a graft?Which with have primary contraction: thick or thin?Forget it…expect disappointmentInadequate attached gingiva, malposed teeth, toothbrushing with Mac’s pencil, chronic inflammation,iatrogenic (restorative), iatrogenic (ortho), iatrogenic(uhoh), factitious injury (chewing on Mac’s pencil whilehe was taking this test), high frenulum attachment,alveolar housing and eruption pattern, tobacco use,cocaine useI: marginal recession not to MGJ, no loss ofinterdental b/stII: marg recession to/past MGJ, no loss of interdentalb/stIII: marg recession to/past MGJ, loss of inderdentalb/stapical to CEJ but coronal to most apical extent ofrecessionIV: marg recession to/past MGJ, loss of interdentalb/st toThe most apical extent of recessionI: 100%, II: 100%, III: 50-75%, IV: 0%The underlying connective tissue at the source of thegraftThick (more initial shrinkage); thin = secondarycontraction due to shrinking in the mouthDescribe the Glickman classification system of furcationdefects.Which class is the only time to do GTR?What are the two components of GTR?What instrument provides reproducible and validinformation about furcation involvement?Cl I: btn 1&2mm, feel catch but not seen on rad;Cl II: >2mm, cul-de-sac, may be on rad or not;Cl III: total bone loss resulting in a through-and-through,may see on rad;Cl IV: through-and-through that is visible due torecessionII (GTR is <strong>guide</strong>d tissue regeneration)Bone graft and collagen membraneNabers probe
According to Ross, what is the most common site offurcation involvement?Maxillary molars (max 1 st distal)Perio Test II: 7
Perio Test II: 8According to Hirshfeld &Wasserman, what is the orderof frequency of occurrence of furcation involvement?Describe the 3 grades of cervical enamel projections(ceps)According to Masters and Hoskins, what is theprevalence of ceps in the molars? What is therelationship of ceps and mandibular molar furcationinvolvement?Where are enamel pearls usually found?Give the %s of accessory canals in each molar.How often is the furcation entrance narrower than astandard Gracey currette in 1 st molars?How often do mandibular molars have bifurcationridges?Give all root trunk average lengths in mm.What is the general ratio of attachment loss toattachment surface area?What factor should be considered as a contributingfactor when crater-like defects or angular bone loss isencountered?T/F: Trauma from occlusion can cause attachment loss.Name 5 indications for root resection.Name 3 contraindications for root resection.1 st molars, 2 nd molars, Maxillary 1 st bicuspidsI: distinct change in the cej projected toward thefurcation; II: cep approaches the furcation; III: cep is inthe furcation area28.6% of mandibular molars, 17% of maxillary molars;>90% of isolated mandibular molars with furcationinvolvement had ceps75% of them are found on 3 rd molars36% of Mx1stM, 32% of mn1stM, 24% mn2ndM, 12% ofMx2ndM {U, -4,-8,-12)58%73%MxM: f=4, m=4, d=5; MxPM: m&d=7;mnM: f=3, l=4(n)mm = 7(n)%Trauma from occlusionF; <strong>perio</strong> disease must already be in place for traumafrom occlusion to cause attachment lossClass II or III FI; severe bone loss involving one or moreroots; root fracture, perforation, resorption, deep rootcaries; root proximity with adjacent teeth; failed endo orinorperable/calcified canalsInadequate bone support on the remaining roots orunfavorable anatomical factors (long root trunk, fusedroots); significant discrepancies in adjacentinterproximal bone height; remaining roots can’t berestored/treated w/ endo