Checklist for Development of a Care Plan - Long-Term Care Best ...
Checklist for Development of a Care Plan - Long-Term Care Best ...
Checklist for Development of a Care Plan - Long-Term Care Best ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
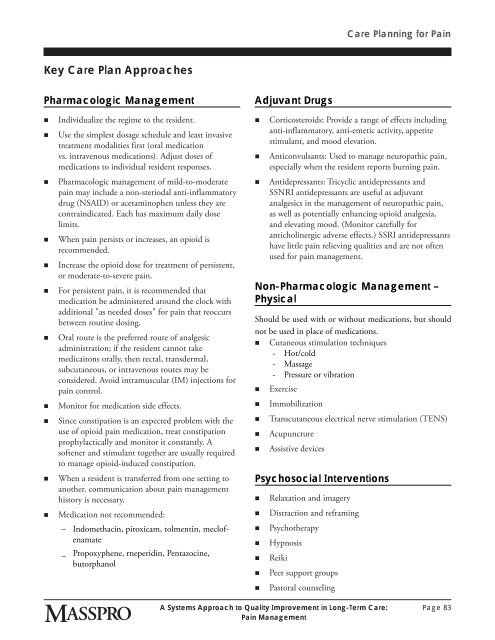
<strong>Care</strong> <strong>Plan</strong>ning <strong>for</strong> PainKey <strong>Care</strong> <strong>Plan</strong> ApproachesPharmacologic Management• Individualize the regime to the resident.• Use the simplest dosage schedule and least invasivetreatment modalities first (oral medicationvs. intravenous medications). Adjust doses <strong>of</strong>medications to individual resident responses.• Pharmacologic management <strong>of</strong> mild-to-moderatepain may include a non-steriodal anti-inflammatorydrug (NSAID) or acetaminophen unless they arecontraindicated. Each has maximum daily doselimits.• When pain persists or increases, an opioid isrecommended.• Increase the opioid dose <strong>for</strong> treatment <strong>of</strong> persistent,or moderate-to-severe pain.• For persistent pain, it is recommended thatmedication be administered around the clock withadditional "as needed doses" <strong>for</strong> pain that reoccursbetween routine dosing.• Oral route is the preferred route <strong>of</strong> analgesicadministration; if the resident cannot takemedicaitons orally, then rectal, transdermal,subcutaneous, or intravenous routes may beconsidered. Avoid intramuscular (IM) injections <strong>for</strong>pain control.• Monitor <strong>for</strong> medication side effects.• Since constipation is an expected problem with theuse <strong>of</strong> opioid pain medication, treat constipationprophylactically and monitor it constantly. As<strong>of</strong>tener and stimulant together are usually requiredto manage opioid-induced constipation.• When a resident is transferred from one setting toanother, communication about pain managementhistory is necessary.• Medication not recommended:– Indomethacin, piroxicam, tolmentin, mecl<strong>of</strong>enamate_ Propoxyphene, rneperidin, Pentazocine,butorphanolAdjuvant Drugs• Corticosteroids: Provide a range <strong>of</strong> effects includinganti-inflammatory, anti-emetic activity, appetitestimulant, and mood elevation.• Anticonvulsants: Used to manage neuropathic pain,especially when the resident reports burning pain.• Antidepressants: Tricyclic antidepressants andSSNRI antidepressants are useful as adjuvantanalgesics in the management <strong>of</strong> neuropathic pain,as well as potentially enhancing opioid analgesia,and elevating mood. (Monitor carefully <strong>for</strong>anticholinergic adverse effects.) SSRI antidepressantshave little pain relieving qualities and are not <strong>of</strong>tenused <strong>for</strong> pain management.Non-Pharmacologic Management –PhysicalShould be used with or without medications, but shouldnot be used in place <strong>of</strong> medications.• Cutaneous stimulation techniques- Hot/cold- Massage- Pressure or vibration• Exercise• Immobilization• Transcutaneous electrical nerve stimulation (TENS)• Acupuncture• Assistive devicesPsychosocial Interventions• Relaxation and imagery• Distraction and reframing• Psychotherapy• Hypnosis• Reiki• Peer support groups• Pastoral counselingA Systems Approach to Quality Improvement in <strong>Long</strong>-<strong>Term</strong> <strong>Care</strong>:Pain ManagementPage 83