PullThrough Subcutaneous Pedicle Flap for an Anterior Auricular ...
PullThrough Subcutaneous Pedicle Flap for an Anterior Auricular ...
PullThrough Subcutaneous Pedicle Flap for an Anterior Auricular ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
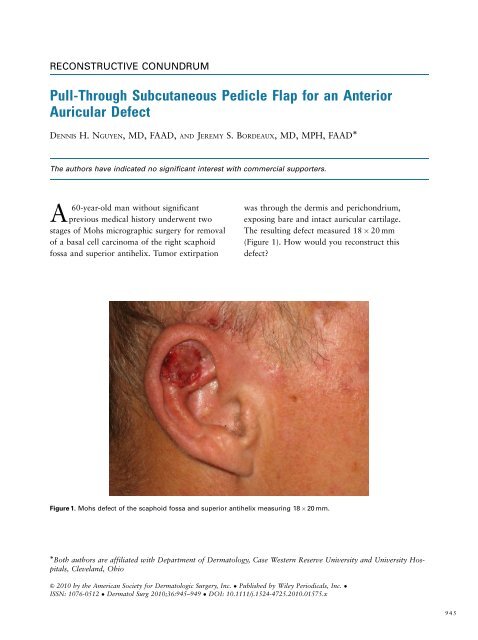
RECONSTRUCTIVE CONUNDRUMPull-Through <strong>Subcut<strong>an</strong>eous</strong> <strong>Pedicle</strong> <strong>Flap</strong> <strong>for</strong> <strong>an</strong> <strong>Anterior</strong><strong>Auricular</strong> DefectDENNIS H. NGUYEN, MD, FAAD, AND JEREMY S. BORDEAUX, MD, MPH, FAAD The authors have indicated no signific<strong>an</strong>t interest with commercial supporters.A60-year-old m<strong>an</strong> without signific<strong>an</strong>tprevious medical history underwent twostages of Mohs micrographic surgery <strong>for</strong> removalof a basal cell carcinoma of the right scaphoidfossa <strong>an</strong>d superior <strong>an</strong>tihelix. Tumor extirpationwas through the dermis <strong>an</strong>d perichondrium,exposing bare <strong>an</strong>d intact auricular cartilage.The resulting defect measured 18 20 mm(Figure 1). How would you reconstruct thisdefect?Figure 1. Mohs defect of the scaphoid fossa <strong>an</strong>d superior <strong>an</strong>tihelix measuring 18 20 mm. Both authors are affiliated with Department of Dermatology, Case Western Reserve University <strong>an</strong>d University Hospitals,Clevel<strong>an</strong>d, Ohio& 2010 by the Americ<strong>an</strong> Society <strong>for</strong> Dermatologic Surgery, Inc. Published by Wiley Periodicals, Inc. ISSN: 1076-0512 Dermatol Surg 2010;36:945–949 DOI: 10.1111/j.1524-4725.2010.01575.x945
PULL-THROUGH SUBCUTANEOUS PEDICLE FLAPResolutionExcision of cut<strong>an</strong>eous tumors of the ear <strong>an</strong>d theirsubsequent repair are commonly encountered inMohs micrographic surgery. A defect of the <strong>an</strong>teriorauricle presents a unique reconstructive dilemma inwhich specific concerns need to be addressed: Is the perichondrium intact? Is the cartilage intact? C<strong>an</strong> function (supporting glasses <strong>an</strong>d hearing aids)be maintained? Where c<strong>an</strong> skin be recruited from <strong>for</strong> the repair?In reviewing the options <strong>for</strong> this <strong>an</strong>terior auriculardefect, one could advocate <strong>for</strong> ‘‘nonrepair.’’ Secondintentionhealing is ideal <strong>for</strong> smaller, shallow defectsof concave surfaces such as the scaphoid fossa,conchal bowl, temple, or nasion/medial c<strong>an</strong>thus. Inthis case, there is little fear that contraction will altera free margin or signific<strong>an</strong>tly alter function, butbare cartilage is a suboptimal, avascular wound bedthat may need to be excised or per<strong>for</strong>ated throughto the opposing perichondrium to better supportre-epithelialization. Healing time c<strong>an</strong> be lengthy.A full-thickness skin graft is a remarkably hardyoption that c<strong>an</strong> be employed <strong>for</strong> this defect. Hairlessareas of the preauricular cheek or photo-protectedareas of the postauricular scalp are suitable donorsites that c<strong>an</strong> provide <strong>an</strong> acceptable color <strong>an</strong>d texturematch. For thin-skinned areas such as the scaphoidfossa, a split-thickness skin graft c<strong>an</strong> also be a viableoption. As in the case with second-intention healing,viability of the graft on bare cartilage may requireexcision or per<strong>for</strong>ation of the cartilage to facilitateimbibition <strong>an</strong>d inosculation from the opposing perichondrium.Signific<strong>an</strong>tly altering the cartilage toprepare <strong>for</strong> the graft may compromise the <strong>for</strong>m <strong>an</strong>drigidity of the auricle. In addition, seroma <strong>an</strong>dhematoma <strong>for</strong>mation under the graft may compromiseits viability. To ensure a vascular wound bed,delayed grafting is also <strong>an</strong> option but requiressufficient time <strong>for</strong> gr<strong>an</strong>ulation tissue to <strong>for</strong>m.Some authors have proposed a staged interpolation,pull-through flap <strong>for</strong> this kind of <strong>an</strong>terior auriculardefect. 1–3 Using the postauricular scalp, a cut<strong>an</strong>eousflap is incised <strong>an</strong>d pulled through a slit incision at thedistal portion of the <strong>an</strong>terior defect. The flap is inset<strong>an</strong>d allowed to take be<strong>for</strong>e being divided in a secondprocedure. This r<strong>an</strong>dom pattern flap probably derivesits vascular supply from tributaries of the posteriorauricular artery. Cosmetic outcome is usuallyexcellent.We propose that a postauricular scalp–to–<strong>an</strong>teriorauricle pull-through subcut<strong>an</strong>eous pedicle flapshould be considered <strong>for</strong> this defect of the scaphoidfossa <strong>an</strong>d <strong>an</strong>tihelix. Masson 4 first described this flap,which has been called the ‘‘revolving door’’ flap 5,6<strong>an</strong>d the ‘‘flip-flop’’ flap, 7 in the plastic surgery literaturein 1972 to describe the general movement ofthe pedicled flap. It is a versatile reconstructive optionthat has been applied to defects of the scaphoidfossa, <strong>an</strong>tihelix, <strong>an</strong>d conchal bowl. The flap’s mainadv<strong>an</strong>tages are that it c<strong>an</strong> be used <strong>for</strong> large defects<strong>an</strong>d uses skin that is protected <strong>an</strong>d well vascularized.Furthermore, it is per<strong>for</strong>med as a one-stageprocedure.In executing this flap, the auricle is reflected<strong>an</strong>teriorally, <strong>an</strong>d <strong>an</strong> area of donor skin is measured<strong>an</strong>d marked just posterior to the postauricular sulcus(Figure 2). This flap is incised as <strong>an</strong> isl<strong>an</strong>d thatFigure 2. <strong>Flap</strong> donor site marked.946DERMATOLOGIC SURGERY
NGUYEN AND BORDEAUXFigure 3. Slit excision through auricular cartilage.Figure 5. <strong>Flap</strong> set into the defect.maintains a subcut<strong>an</strong>eous pedicle that originatesfrom the postauricular sulcus. Reasonable hemostasisshould be obtained without compromising thevascular pedicle. Returning the auricle to its normal<strong>an</strong>atomical position, a slit excision at the proximalaspect of the defect is taken through the auricularcartilage <strong>an</strong>d to the base of the flap’s pedicle in thepostauricular sulcus (Figure 3). The excision shouldbe sufficient to accommodate the pedicle withoutvascular compromise; it may be necessary to excise a1- to 2-mm strip of cartilage to accomplish this.The flap <strong>an</strong>d its pedicle are pulled through theauricular excision (Figure 4) <strong>an</strong>d laid atop the defect(Figure 5). Without tension, torsion, or impingementof the pedicle, the flap should be well perfused.The flap is inset with fine nonabsorbablesuperficial sutures (Figure 6), <strong>an</strong>d the secondarydefect is easily closed primarily. A st<strong>an</strong>dard pressuredressing is applied, <strong>an</strong>d the patient is instructedto protect the area from trauma. Envisioningthe pages of a book c<strong>an</strong> be a helpful <strong>an</strong>alogy invisualizing the movement <strong>an</strong>d execution of thisrepair (Figure 7).In our patient, follow-up at 2 months revealed excellentaesthetic <strong>an</strong>d functional results of the primary(Figure 8) <strong>an</strong>d secondary (Figure 9) sites. Vascularsupply from tributaries of the posterior auricularartery contribute to the viability of this flap. 8Other authors have stated that neurologic function isFigure 4. The flap <strong>an</strong>d pedicle be<strong>for</strong>e being pulled throughthe excision.Figure 6. <strong>Flap</strong> sutured into place.36:6:JUNE 2010 947
PULL-THROUGH SUBCUTANEOUS PEDICLE FLAPFigure 9. The secondary site at the 2-month follow-up visit.maintained, <strong>an</strong>d indeed, our patient regainedminimal sensation at his flap site. 9 A potentialdrawback of this flap includes pullingback or ‘‘pinning’’ of the ear. Also, overm<strong>an</strong>ipulation<strong>an</strong>d incision of auricular cartilage may lead topain <strong>an</strong>d chondritis. Pain, if prolonged, c<strong>an</strong>be a symptom of subclinical infection, <strong>an</strong>d aprophylactic course of <strong>an</strong> appropriate <strong>an</strong>tibiotic,particularly in patients with diabetes mellitus,may be considered.Figure 7. (A) The ear c<strong>an</strong> be visualized as a leaflet between thepages of a book. With the defect on the <strong>an</strong>terior surface, a slitexcision is taken through the auricular cartilage. (B) The ear isreflected <strong>an</strong>teriorally, <strong>an</strong>d the flap is taken from the postauricularscalp. The subcut<strong>an</strong>eous pedicle is based in the postauricularsulcus. (C) The flap <strong>an</strong>d pedicle are pulled through theauricular excision, set into the defect, <strong>an</strong>d sutured into place.A subcut<strong>an</strong>eous, pull-through isl<strong>an</strong>d pedicle flap is<strong>an</strong> ideal <strong>an</strong>d versatile reconstructive choice <strong>for</strong>large defects of the <strong>an</strong>terior auricle that involveperichondrium.References1. Johnson T, Fader D. The staged retroauricular to auricular directpedicle (interpolation) flap <strong>for</strong> helical ear reconstruction. J AmAcad Dermatol 1997;37:975–8.2. Mellette J. Reconstruction of the ear. In: Lask G, Moy R, editors.Principles <strong>an</strong>d Techniques of Cut<strong>an</strong>eous Surgery. Los Angeles:McGraw-Hill; 1996. p. 369–74.3. Nguyen T. Staged cheek-to-nose <strong>an</strong>d auricular interpolation flaps.Dermatol Surg 2005;31:1034–45.4. Masson J. A simple isl<strong>an</strong>d flap <strong>for</strong> reconstruction of concha-helixdefects. Br J Plast Surg 1972;25:399–403.Figure 8. Two-month follow-up visit.5. Humphreys T, Goldberg L. The postauricular (revolvingdoor) isl<strong>an</strong>d pedicle flap revisited. Dermatol Surg 1996;22:148–50.948DERMATOLOGIC SURGERY
NGUYEN AND BORDEAUX6. Politi M, Robiony M. Anthelix-conchal reconstruction with postauricular‘‘revolving door’’ isl<strong>an</strong>d flap. Int J Oral Maxillofac Surg1995;24:340–1.7. Talmi Y, Horowitz Z, Bedrin L, Kronenberg J. <strong>Auricular</strong>reconstruction with a postauricular myocut<strong>an</strong>eous isl<strong>an</strong>dflap: flip-flop flap. Plast Reconstr Surg 1996;98:1191–9.8. Talmi Y, Liokumovitch P, Wolf M, et al. Anatomy of the postauricularisl<strong>an</strong>d ‘‘revolving door’’ flap (‘‘flip-flop’’ flap). Ann PlastSurg 1997;39:603–7.9. Turkasl<strong>an</strong> T, Kul Z, Isler C, Ozsoy Z. Reconstruction of the<strong>an</strong>terior surface of the ear using a postauricular pull-throughneurovascular isl<strong>an</strong>d flap. Ann Plast Surg 2006;56:609–13.Address correspondence <strong>an</strong>d reprint requests to: Dennis H.Nguyen, MD, Kaiser Perm<strong>an</strong>ente – R<strong>an</strong>cho CordovaMedical Officers, 10725 International Drive, 2nd Floor,Mohs Surgery, R<strong>an</strong>cho Cordova, CA 95670, ore-mail: dennguyen@gmail.com36:6:JUNE 2010 949