CHAPTER 38 QUIZ - SDMiramarEmt
CHAPTER 38 QUIZ - SDMiramarEmt
CHAPTER 38 QUIZ - SDMiramarEmt
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Handout <strong>38</strong>-2 (continued)You are at the home of a family with a 10-month-old child. The father explains he called because the childhad a seizure that lasted about a minute. The child appears flushed. You touch her skin, which is extremelyhot to the touch. The father says the child has been running a fever all day. He put her to bed about anhour ago. About 10 or 15 minutes ago he heard a crash in the infant’s room and went to investigate. Whenhe entered, the child was convulsing in the crib. That’s when he called 911.5. What is likely to be the cause of the problem?6. What emergency care would you provide?©2010 by Pearson Education, Inc.Prehospital Emergency Care, 9th Ed.<strong>CHAPTER</strong> <strong>38</strong>Pediatrics
Handout <strong>38</strong>-3Student’s Name<strong>CHAPTER</strong> <strong>38</strong> REVIEWWrite the word or words that best complete each sentence in the space provided.1. During the assessment and treatment of a young child, you will, if possible, want the child to sit inthe ______________________________ ______________________________.2. When opening a child’s airway, it is important not to ______________________________ thechild’s neck.3. Use ______________________________ ______________________________ alternating with______________________________ ______________________________ to clear a complete airwayobstruction in an infant 1-year-old or younger.4. In infants and children, the ______________________________ system is usually an early indicator ofother medical problems.5. For infants and young children who are frightened by the oxygen mask, provide oxygen using the______________________________ technique.6. For infants and children, provide artificial ventilations at a minimum rate of______________________________ breaths per minute.7. Diarrhea and/or vomiting, dehydration, infection, abdominal injuries, and blood loss are commoncauses of ______________________________ in infants and children.8. Because children have a large surface area in proportion to their body mass, they are especiallyprone to ______________________________.9. Fever, epilepsy, meningitis, drug overdose, hypoglycemia, head trauma, and decreased levels ofoxygen can bring on ______________________________ in children.10. If a pediatric patient has a seizure and there is no possibility of spinal injury, position the patient______________________________ ______________________________ ______________________________.11. In the case of a submersion, assume that ____________________________________________________________ has occurred and fully immobilize the child.12. The diagnosis of SIDS is made ______________________________.13. Inflation of the abdominal compartment of the PASG with a pediatric patient may compromise______________________________.(continued)©2010 by Pearson Education, Inc.Prehospital Emergency Care, 9th Ed.<strong>CHAPTER</strong> <strong>38</strong>Pediatrics
Handout <strong>38</strong>-3 (continued)14. Cases of ______________________________ trauma exceed those of ______________________________trauma in infants and children.15. When dealing with suspected foreign body airway obstruction in an infant or a child, never perform______________________________ ______________________________ ______________________________.16. If you suspect abuse as the cause of injury with a child trauma patient, do not______________________________ the caregivers about abuse or ______________________________ them.17. If there is bleeding in a pediatric patient with a central intravenous line, your emergency care willconsist of ______________________________ ______________________________ to the device and______________________________ the patient.18. Pediatric calls are among the most ______________________________ for EMTs.19. For children with special airway needs, the most common problems that EMS will encounter arewith ______________________________ tubes, ____________________________________________________________, central lines, and feeding tubes.20. ______________________________ tubes are placed into the stomach to assist with feeding.©2010 by Pearson Education, Inc.Prehospital Emergency Care, 9th Ed.<strong>CHAPTER</strong> <strong>38</strong>Pediatrics
Handout <strong>38</strong>-4Student’s NamePEDIATRICS: TRUE OR FALSEIndicate if the following statements are true or false by writing T or F in the space provided.__________________________________________________________________________________________1. The term “toddler” refers to a child between 2 and 4 years old.2. Modesty and body image are very important issues for school-age children.3. With children, padding under the shoulders is often necessary to maintain an openairway during immobilization to a spine board.4. Because children have a smaller blood volume than adults, issues of blood loss are lessserious in those patients.5. Determining the cause of respiratory distress in a pediatric patient is an important part ofan EMT’s assessment.6. Provide an initial series of six back blows to any infant or child patient suffering a partialairway obstruction.7. Capillary refill can be a useful tool in assessing circulation in pediatric patients.8. Infants and children need a respiratory tidal volume of approximately 10 mL/kg.9. In a pediatric patient with a foreign body airway obstruction, perform a “blind” fingersweep of the oral cavity if back blows do not dislodge the obstruction.__________10. Seizures that last longer than 10 minutes or recur without interruption represent a truemedical emergency.__________11. To assess an unresponsive child, give him or her a gentle shake.__________12. With any infant or child poisoning patient, administer activated charcoal once youdetermine that the airway is open.__________13. A sunken fontanelle is a sign of dehydration in an infant.__________14. A drop in blood pressure is a late sign of shock in children.__________15. With submersion patients in whom normal breathing is restored, deterioration can stilltake place from minutes to hours after the event.__________16. Explaining to parents that SIDS is a relatively common occurrence is one way the EMTcan help them cope with the loss of a child.__________17. With child patients, slow delivery of ventilations and cricoid pressure can help reducegastric distension.(continued)©2010 by Pearson Education, Inc.Prehospital Emergency Care, 9th Ed.<strong>CHAPTER</strong> <strong>38</strong>Pediatrics
Handout <strong>38</strong>-4 (continued)__________18. Use a single leg of the PASG to control serious bleeding in an infant.__________19. Never ask a suspected victim of child abuse to explain the circumstances of an incidentwhile the possible abuser is present.__________20. CISD is one way EMTs can defuse the stress created by dealing with pediatricemergencies.©2010 by Pearson Education, Inc.Prehospital Emergency Care, 9th Ed.<strong>CHAPTER</strong> <strong>38</strong>Pediatrics
Handout <strong>38</strong>-5Student’s NamePEDIATRICS: LISTING1. List at least five signs of respiratory distress in pediatric patients.2. List the emergency care steps for a child with fever and seizures.3. List the basic emergency care steps for the pediatric trauma patient.4. List four signs of possible child abuse.©2010 by Pearson Education, Inc.Prehospital Emergency Care, 9th Ed.<strong>CHAPTER</strong> <strong>38</strong>Pediatrics
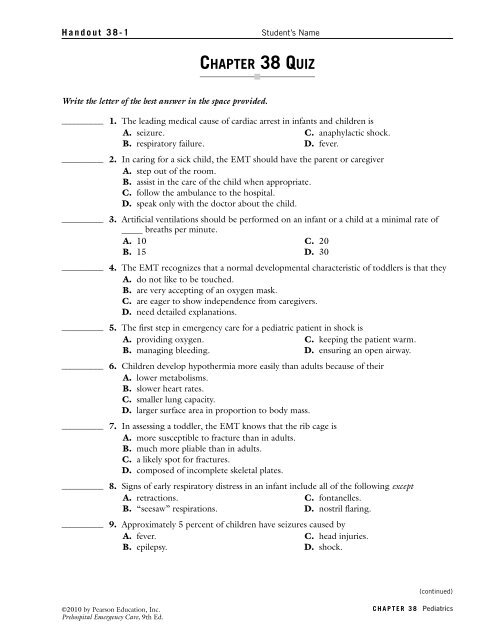
<strong>CHAPTER</strong> <strong>38</strong> ANSWER KEYHANDOUT <strong>38</strong>-1: Chapter <strong>38</strong> Quiz1. B 5. D 9. A 13. A2. B 6. D 10. D 14. C3. C 7. B 11. C 15. C4. A 8. C 12. B 16. BHANDOUT <strong>38</strong>-2: In the Field1. The child is likely in the early stages of shock(hypoperfusion) from infection and hypovolemia.2. Ensure an open airway. Provide oxygen at 15 litersper minute by nonrebreather mask and be preparedto provide positive-pressure ventilations. Keep thechild warm. Expedite transport.3. The child may be suffering from poisoning.4. Establish and maintain an airway. Be prepared tosuction. Provide high-flow, high-concentrationoxygen and be prepared to provide positive-pressureventilation with supplemental oxygen as needed.Expedite transport. Perform a rapid traumaassessment.5. The child may have suffered a febrile seizure.6. Maintain the airway and provide oxygen at 15 litersper minute by nonrebreather mask. (Providepositive-pressure ventilation, if necessary.) Lower theinfant’s body temperature. Be alert for possiblevomiting and the need to suction. Transport.HANDOUT <strong>38</strong>-3: Chapter <strong>38</strong> Review1. parent’s (caregiver’s) lap2. hyperextend3. back blows, chest thrusts4. respiratory5. “blow-by”6. 207. shock (hypoperfusion)8. hypothermia9. seizures10. on his side11. spinal injury12. postmortem13. respirations14. blunt, penetrating15. blind finger sweeps16. question, accuse17. applying pressure, transporting18. stressful19. tracheostomy, mechanical ventilators20. GastrostomyHANDOUT <strong>38</strong>-4: Pediatrics: True or False1. F 6. F 11. F 16. F2. T 7. T 12. F 17. T3. T 8. T 13. T 18. F4. F 9. F 14. T 19. T5. F 10. T 15. T 20. THANDOUT <strong>38</strong>-5: Pediatrics: Listing1. Any five: nasal flaring, retractions; neck muscle use;“seesaw” respirations; breathing noises such asstridor, wheezing, or grunting; breathing rate abovenormal for child’s age. Additional: cyanosis,decreased muscle tone, poor peripheral perfusion,altered mental status, head bobbing.2. Establish and maintain an airway. Protect patientfrom injury. Suction secretions for no longer than5–10 seconds at a time. Provide positive-pressureventilations with supplemental oxygen at 20/minuteif breathing is inadequate; administer oxygen;consider blow-by oxygen in very young children.Remove clothing and cool by fanning or spongingwith tepid water. Consider advanced life supporttransport. Ongoing assessment every 5 minutes.3. Establish and maintain in-line spinal stabilization andopen the airway using the jaw-thrust maneuver.Suction as necessary, no more than 5–10 seconds at atime. Provide oxygen by nonrebreather mask at 15liters per minute or provide positive-pressureventilation with supplemental oxygen for inadequatebreathing. Provide occlusive dressings for any openwound to the chest. Cover any eviscerations withmoist, sterile gauze dressing and secure. Providecomplete spinal immobilization. Consider request forALS support. Apply PASG if pelvic injury issuspected and local protocols direct. Transport.Splint fractures and dress open wounds. Performongoing assessment every 5 minutes.4. Any four of the following: multiple abrasions,lacerations, incisions, bruises, broken bones; multipleinjuries or bruises in various stages of healing;injuries on both sides or both front and back ofchild’s body; unusual wounds; a fearful child; injuriesto the genitalia; injuries to spinal cord and brainwhen child is violently shaken; situations in whichthe injuries are not consistent with the story; lack ofadult supervision; untreated chronic illness;malnourishment; delay in reporting injuries.©2010 by Pearson Education, Inc.Prehospital Emergency Care, 9th Ed.<strong>CHAPTER</strong> <strong>38</strong>Pediatrics