Endovascular stents for abdominal aortic aneurysms: a systematic ...
Endovascular stents for abdominal aortic aneurysms: a systematic ...
Endovascular stents for abdominal aortic aneurysms: a systematic ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
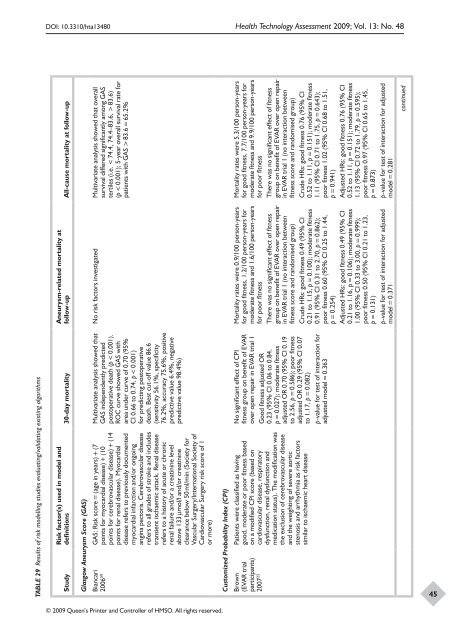
DOI: 10.3310/hta13480 Health Technology Assessment 2009; Vol. 13: No. 48TABLE 29 Results of risk modelling studies evaluating/validating existing algorithmsRisk factor(s) used in model anddefinitions 30-day mortalityAneurysm-related mortality atfollow-up All-cause mortality at follow-upStudyGlasgow Aneurysm Score (GAS)Multivariate analysis showed thatGAS independently predictedpostoperative death (p < 0.001).ROC curve showed GAS witharea under curve of 0.70 (95%CI 0.66 to 0.74, p < 0.001)<strong>for</strong> predicting postoperativedeath. Best cut-off value 86.6(sensitivity 56.1%, specificity76.2%, accuracy 75.6%, positivepredictive value 6.4%, negativepredictive value 98.4%)No risk factors investigated Multivariate analysis showed that overallsurvival differed significantly among GAStertiles (i.e. < 74.4, 74.4–83.6, > 83.6)(p < 0.001); 5-year overall survival rate <strong>for</strong>patients with GAS > 83.6 = 65.2%Biancari 2006 59 GAS: Risk score = (age in years) + (7points <strong>for</strong> myocardial disease) + (10points <strong>for</strong> cerebrovascular disease) + (14points <strong>for</strong> renal disease). Myocardialdisease refers to previously documentedmyocardial infarction and/or ongoingangina pectoris. Cerebrovascular diseaserefers to all grades of stroke and includestransient ischaemic attack. Renal diseaserefers to a history of acute or chronicrenal failure and/or a creatinine levelabove 133 µmol/l and/or creatinineclearance below 50 ml/min (Society <strong>for</strong>Vascular Surgery/International Society ofCardiovascular Surgery risk score of 1or more)Customized Probability Index (CPI)No significant effect of CPIfitness group on benefit of EVARover open repair in EVAR trial 1Good fitness adjusted OR0.23 (95% CI 0.06 to 0.84,p = 0.027); moderate fitnessadjusted OR 0.70 (95% CI 0.19to 2.56, p = 0.586); poor fitnessadjusted OR 0.29 (95% CI 0.07to 1.17, p = 0.082)p-value <strong>for</strong> test of interaction <strong>for</strong>adjusted model = 0.363Mortality rates were 0.9/100 person-years<strong>for</strong> good fitness, 1.2/100 person-years <strong>for</strong>moderate fitness and 1.6/100 person-years<strong>for</strong> poor fitnessThere was no significant effect of fitnessgroup on benefit of EVAR over open repairin EVAR trial 1 (no interaction betweenfitness score and randomised group)Crude HRs: good fitness 0.49 (95% CI0.21 to 1.15, p = 0.100); moderate fitness0.91 (95% CI 0.31 to 2.70, p = 0.862);poor fitness 0.60 (95% CI 0.25 to 1.44,p = 0.254)Adjusted HRs: good fitness 0.49 (95% CI0.21 to 1.16, p = 0.106); moderate fitness1.00 (95% CI 0.33 to 3.00, p = 0.999);poor fitness 0.50 (95% CI 0.21 to 1.23,p = 0.131)p-value <strong>for</strong> test of interaction <strong>for</strong> adjustedmodel = 0.371Mortality rates were 5.3/100 person-years<strong>for</strong> good fitness, 7.7/100 person-years <strong>for</strong>moderate fitness and 9.9/100 person-years<strong>for</strong> poor fitnessThere was no significant effect of fitnessgroup on benefit of EVAR over open repairin EVAR trial 1 (no interaction betweenfitness score and randomised group)Crude HRs: good fitness 0.76 (95% CI0.52 to 1.11, p = 0.151); moderate fitness1.11 (95% CI 0.71 to 1.75, p = 0.643);poor fitness 1.02 (95% CI 0.68 to 1.51,p = 0.941)Adjusted HRs: good fitness 0.76 (95% CI0.52 to 1.11, p = 0.151); moderate fitness1.13 (95% CI 0.72 to 1.79, p = 0.595);poor fitness 0.97 (95% CI 0.65 to 1.45,p = 0.873)p-value <strong>for</strong> test of interaction <strong>for</strong> adjustedmodel = 0.281continuedBrown (EVAR trial participants) 2007 23 Patients were classified as havinggood, moderate or poor fitness basedon a modified CPI score (based oncardiovascular disease, respiratorydysfunction, renal dysfunction andmedication status). The modification wasthe exclusion of cerebrovascular diseaseand the weighting of severe <strong>aortic</strong>stenosis and arrhythmia as risk factorssimilar to ischaemic heart disease45© 2009 Queen’s Printer and Controller of HMSO. All rights reserved.