chapter 6 biomechanics of the musculoskeletal system
chapter 6 biomechanics of the musculoskeletal system
chapter 6 biomechanics of the musculoskeletal system
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
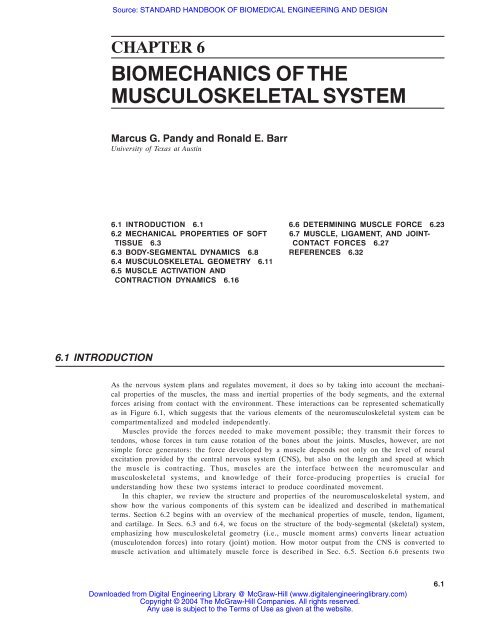
Source: STANDARD HANDBOOK OF BIOMEDICAL ENGINEERING AND DESIGNCHAPTER 6BIOMECHANICS OF THEMUSCULOSKELETAL SYSTEMMarcus G. Pandy and Ronald E. BarrUniversity <strong>of</strong> Texas at Austin6.1 INTRODUCTION 6.1 6.6 DETERMINING MUSCLE FORCE 6.236.2 MECHANICAL PROPERTIES OF SOFT 6.7 MUSCLE, LIGAMENT, AND JOINT-TISSUE 6.3 CONTACT FORCES 6.276.3 BODY-SEGMENTAL DYNAMICS 6.8 REFERENCES 6.326.4 MUSCULOSKELETAL GEOMETRY 6.116.5 MUSCLE ACTIVATION ANDCONTRACTION DYNAMICS 6.166.1 INTRODUCTIONAs <strong>the</strong> nervous <strong>system</strong> plans and regulates movement, it does so by taking into account <strong>the</strong> mechanicalproperties <strong>of</strong> <strong>the</strong> muscles, <strong>the</strong> mass and inertial properties <strong>of</strong> <strong>the</strong> body segments, and <strong>the</strong> externalforces arising from contact with <strong>the</strong> environment. These interactions can be represented schematicallyas in Figure 6.1, which suggests that <strong>the</strong> various elements <strong>of</strong> <strong>the</strong> neuro<strong>musculoskeletal</strong> <strong>system</strong> can becompartmentalized and modeled independently.Muscles provide <strong>the</strong> forces needed to make movement possible; <strong>the</strong>y transmit <strong>the</strong>ir forces totendons, whose forces in turn cause rotation <strong>of</strong> <strong>the</strong> bones about <strong>the</strong> joints. Muscles, however, are notsimple force generators: <strong>the</strong> force developed by a muscle depends not only on <strong>the</strong> level <strong>of</strong> neuralexcitation provided by <strong>the</strong> central nervous <strong>system</strong> (CNS), but also on <strong>the</strong> length and speed at which<strong>the</strong> muscle is contracting. Thus, muscles are <strong>the</strong> interface between <strong>the</strong> neuromuscular and<strong>musculoskeletal</strong> <strong>system</strong>s, and knowledge <strong>of</strong> <strong>the</strong>ir force-producing properties is crucial forunderstanding how <strong>the</strong>se two <strong>system</strong>s interact to produce coordinated movement.In this <strong>chapter</strong>, we review <strong>the</strong> structure and properties <strong>of</strong> <strong>the</strong> neuro<strong>musculoskeletal</strong> <strong>system</strong>, andshow how <strong>the</strong> various components <strong>of</strong> this <strong>system</strong> can be idealized and described in ma<strong>the</strong>maticalterms. Section 6.2 begins with an overview <strong>of</strong> <strong>the</strong> mechanical properties <strong>of</strong> muscle, tendon, ligament,and cartilage. In Secs. 6.3 and 6.4, we focus on <strong>the</strong> structure <strong>of</strong> <strong>the</strong> body-segmental (skeletal) <strong>system</strong>,emphasizing how <strong>musculoskeletal</strong> geometry (i.e., muscle moment arms) converts linear actuation(musculotendon forces) into rotary (joint) motion. How motor output from <strong>the</strong> CNS is converted tomuscle activation and ultimately muscle force is described in Sec. 6.5. Section 6.6 presents twoDownloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.6.1
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.2 MECHANICS OF THE HUMAN BODYFIGURE 6.1 Schematic diagram showing how <strong>the</strong> human neuro<strong>musculoskeletal</strong> <strong>system</strong> can be compartmentalizedfor modeling purposes.Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.3methods commonly used to determine <strong>musculoskeletal</strong> loading during human movement. Representative results <strong>of</strong> muscle, ligament, and joint-contact loading incurred during exercise and dailyactivity are given in Sec. 6.7.6.2 MECHANICAL PROPERTIES OF SOFT TISSUEWe focus our description <strong>of</strong> <strong>the</strong> mechanical properties <strong>of</strong> s<strong>of</strong>t tissue on muscle, tendon, ligament, andcartilage. The structure and properties <strong>of</strong> bone are treated elsewhere in this volume.FIGURE 6.2 Structural organization <strong>of</strong> skeletal muscle from macro- tomicrolevel. Whole muscle (a), bundles <strong>of</strong> my<strong>of</strong>ibrils (b), single my<strong>of</strong>ibril(c), sarcomere (d), and thick (myosin) filament and thin (actin)filament (e). All symbols are defined in <strong>the</strong> text. [Modified from Enoka(1994).]Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.4 MECHANICS OF THE HUMAN BODY6.2.1 MuscleGross Structure. Muscles are molecular machines that convert chemical energy into force. Individualmuscle fibers are connected toge<strong>the</strong>r by three levels <strong>of</strong> collagenous tissue: endomysium, whichsurrounds individual muscle fibers; perimysium, which collects bundles <strong>of</strong> fibers into fascicles; andepimysium, which encloses <strong>the</strong> entire muscle belly (Fig. 6.2a). This connective tissue matrix connectsmuscle fibers to tendon and ultimately to bone.FIGURE 6.3 Force versus length curve for muscle, (a) Isometric force versus length properties when muscle is fully activated.Total = active + passive. (b) Isometric force versus length properties when activation level is halved. (c) Muscle force versusstriation spacing curve. Symbols defined in text. [Modified from Zajac and Gordon (1989) and from A. M. Gordon, A. F. Huxley,and F. J. Julian, Journal <strong>of</strong> Physiology, vol. 184, 1966.]Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.5Whole muscles are composed <strong>of</strong> groups <strong>of</strong> muscle fibers, which vary from 1 to 400 mm in lengthand from 10 to 60 µm in diameter. Muscle fibers, in turn, are composed <strong>of</strong> groups <strong>of</strong> my<strong>of</strong>ibrils (Fig.6.2b), and each my<strong>of</strong>ibril is a series <strong>of</strong> sarcomeres added end to end (Fig. 6.2c). The sarcomere isboth <strong>the</strong> structural and functional unit <strong>of</strong> skeletal muscle. During contraction, <strong>the</strong> sarcomeres areshortened to about 70 percent <strong>of</strong> <strong>the</strong>ir uncontracted, resting length. Electron microscopy andbiochemical analysis have shown that each sarcomere contains two types <strong>of</strong> filaments: thick filaments,composed <strong>of</strong> myosin, and thin filaments, containing actin (Fig. 6.2d). Near <strong>the</strong> center <strong>of</strong> <strong>the</strong>sarcomere, thin filaments overlap with thick filaments to form <strong>the</strong> AI zone (Fig. 6.2e).In <strong>the</strong> discussion below, <strong>the</strong> force-length and force-velocity properties <strong>of</strong> muscle are assumed tobe scaled-up versions <strong>of</strong> <strong>the</strong> properties <strong>of</strong> muscle fibers, which in turn are assumed to be scaled-upversions <strong>of</strong> properties <strong>of</strong> sarcomeres.Force-Length Property. The steady-state property <strong>of</strong> muscle is defined by its isometric force-lengthcurve, which is obtained when activation and fiber length are both held constant. When a muscle isheld isometric and is fully activated, it develops a steady force. The difference in force developedwhen <strong>the</strong> muscle is activated and when <strong>the</strong> muscle is passive is called <strong>the</strong> active muscle force (Fig.6.3a). The region where active muscle force is generated is (nominally), whereis <strong>the</strong> length at which active muscle force peaks; that is, when ; is called muscle fiberresting length or optimal muscle fiber length and is <strong>the</strong> maximum isometric force developed by <strong>the</strong>muscle (Zajac and Gordon, 1989). In Fig. 6.3a passive muscle tissue bears no force at length . Theforce-length property <strong>of</strong> muscle tissue that is less than fully activated can be considered to be ascaled-down version <strong>of</strong> <strong>the</strong> one that is fully activated (Fig. 6.3b). Muscle tissue can be less than fullyactivated when some or all <strong>of</strong> its fibers are less than fully activated.The shape <strong>of</strong> <strong>the</strong> active force-length curve (Fig. 6.3) is explained by <strong>the</strong> experimental observationthat active muscle force varies with <strong>the</strong> amount <strong>of</strong> overlap between <strong>the</strong> thick and thin filaments withina sarcomere (see also “Mechanism <strong>of</strong> Muscle Contraction” in Sec. 6.5.2). The muscle force versusstriation spacing curve given in Fig. 6.3c shows that <strong>the</strong>re is minimal overlap <strong>of</strong> <strong>the</strong> thick and thinfilaments at a sarcomere length <strong>of</strong> 3.5 µm, whereas at a length <strong>of</strong> about 2.0 µm <strong>the</strong>re is maximumFIGURE 6.4 Force versus velocity curve for muscle when (a) muscle tissue is fully activated and (b) activation is halved. Symbols defined in text.[Modified from Zajac and Gordon (1989).]Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.6 MECHANICS OF THE HUMAN BODYFIGURE 6.5 Structural organization <strong>of</strong> tendon or ligament from macro- tomicrolevel. Modified from Enoka (1994).overlap between <strong>the</strong> cross-bridges. As sarcomere length decreases to 1.5 µm, <strong>the</strong> filaments slidefar<strong>the</strong>r over one ano<strong>the</strong>r, and <strong>the</strong> amount <strong>of</strong> filament overlap again decreases. Thus, muscle forcevaries with sarcomere length because <strong>of</strong> <strong>the</strong> change in <strong>the</strong> number <strong>of</strong> potential cross-bridgeattachments formed.Force-Velocity Property. When a constant load is applied to a fully activated muscle, <strong>the</strong> muscle willshorten (concentric contraction) if <strong>the</strong> applied load is less than <strong>the</strong> maximum isometric force developedby <strong>the</strong> muscle for <strong>the</strong> length at which <strong>the</strong> muscle is initially contracting. If <strong>the</strong> applied load isgreater than <strong>the</strong> muscle’s maximum isometric force at that length, <strong>the</strong>n <strong>the</strong> muscle will leng<strong>the</strong>n(eccentric contraction). From a set <strong>of</strong> length trajectories obtained by applying different loads toshortening and leng<strong>the</strong>ning muscle, an empirical force-velocity relation can be derived for anymuscle length l M (Fig. 6.4a). At <strong>the</strong> optimal fiber length , a maximum shortening velocity v max , canbe defined such that <strong>the</strong> muscle tissue cannot resist any load even when it is fully activated (Fig.6.4a). As with <strong>the</strong> force-length curve, it is commonly assumed that <strong>the</strong> force-velocity relation scalesproportionally with activation, although some studies have found that <strong>the</strong> maximum shorteningvelocity v max is also a function <strong>of</strong> muscle length (Fig. 6.4b).Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.7FIGURE 6.6 Force versus length curves for human medial patellar tendon, gracilis tendon, fascia latatendon, and <strong>the</strong> anterior cruciate ligament.6.2.2 Tendon and LigamentGross Structure. Tendon connects muscle to bone, whereas ligament connects bone to bone. The maindifference between <strong>the</strong> structure <strong>of</strong> tendon and ligament is <strong>the</strong> organization <strong>of</strong> <strong>the</strong> collagen fibril. Intendon, <strong>the</strong> fibrils are arranged longitudinally in parallel to maximize <strong>the</strong> resistance to tensile (pulling)forces exerted by muscle. In ligament, <strong>the</strong> fibrils are generally aligned in parallel with someoblique or spiral arrangements to accommodate forces applied in different directions.Tendons and ligaments are dense connective tissues that contain collagen, elastin, proteoglycans,water, and fibroblasts. Approximately 70 to 80 percent <strong>of</strong> <strong>the</strong> dry weight <strong>of</strong> tendon and ligamentconsists <strong>of</strong> Type I collagen, which is a fibrous protein. Whole tendon is composed <strong>of</strong> bundles <strong>of</strong>fascicles, each made up in turn <strong>of</strong> bundles <strong>of</strong> fibrils (Fig. 6.5). The collagen fibril is <strong>the</strong> basic loadbearingunit <strong>of</strong> tendon and ligament. The fibril consists <strong>of</strong> bundles <strong>of</strong> micr<strong>of</strong>ibrils held toge<strong>the</strong>r bybiochemical bonds (called cross-links) between <strong>the</strong> collagen molecules. Because <strong>the</strong>se cross-links bind<strong>the</strong> micr<strong>of</strong>ibrils toge<strong>the</strong>r, <strong>the</strong> number and state <strong>of</strong> <strong>the</strong> cross-links are thought to have a significanteffect on <strong>the</strong> strength <strong>of</strong> <strong>the</strong> connective tissue.Stress-Strain Property. When a tensile force is applied to tendon or ligament at its resting length, <strong>the</strong>tissue stretches. Figure 6.6 shows <strong>the</strong> force-length curves for three different muscle tendons and oneknee ligament found in humans. These data show that <strong>the</strong> medial patellar tendon is much strongerthan ei<strong>the</strong>r <strong>the</strong> gracilis or fascia lata tendons. Interestingly, <strong>the</strong> anterior cruciate ligament is alsostronger than <strong>the</strong> gracilis and fascia lata tendons, and is slightly more compliant as well.Force-length curves can be normalized to subtract out <strong>the</strong> effects <strong>of</strong> geometry; thus, force can benormalized by dividing by <strong>the</strong> cross-sectional area <strong>of</strong> a tissue, while length can be normalized bydividing by <strong>the</strong> initial length <strong>of</strong> <strong>the</strong> tendon or ligament. The resulting stress-strain curve displays threecharacteristic regions: <strong>the</strong> toe region, <strong>the</strong> linear region, and <strong>the</strong> failure region (Fig. 6.7). The toeregion corresponds to <strong>the</strong> initial part <strong>of</strong> <strong>the</strong> stress-strain curve and describes <strong>the</strong> mechanical behavior<strong>of</strong> <strong>the</strong> collagen fibers as <strong>the</strong>y are being stretched and straightened from <strong>the</strong> initial, resting zigzagpattern. The linear region describes <strong>the</strong> elastic behavior <strong>of</strong> <strong>the</strong> tissue, and <strong>the</strong> slope <strong>of</strong> <strong>the</strong> curve in thisregion represents <strong>the</strong> elastic modulus <strong>of</strong> <strong>the</strong> tendon or ligament. The failure region describes plasticchanges undergone by <strong>the</strong> tissue, where a small number <strong>of</strong> fibrils first rupture, followed by ultimatefailure <strong>of</strong> <strong>the</strong> whole tissue.Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.9FIGURE 6.8 Number <strong>of</strong> degrees <strong>of</strong> freedom (d<strong>of</strong>) <strong>of</strong> a joint. See text for explanation. [Modified from Zajac and Gordon (1989).]relative to <strong>the</strong> o<strong>the</strong>r (θ 1 , θ 2 , θ 3 in Fig. 6.8a), and 3 associated with <strong>the</strong> position <strong>of</strong> a point on onesegment relative to <strong>the</strong> o<strong>the</strong>r segment (x, y, z in Fig. 6.8a).In coordination studies, models <strong>of</strong> joints are kept as simple as possible. In studies <strong>of</strong> walking, forexample, <strong>the</strong> hip is <strong>of</strong>ten assumed to be a ball-and-socket joint, with <strong>the</strong> femur rotating relative to <strong>the</strong>pelvis only (Anderson and Pandy, 2001b). Thus, <strong>the</strong> position <strong>of</strong> <strong>the</strong> femur relative to <strong>the</strong> pelvis canbe described by three angles, as illustrated in Fig. 6.8b. In jumping, pedaling, and rising from a chair,<strong>the</strong> hip may even be assumed to be a simple hinge joint, in which case <strong>the</strong> position <strong>of</strong> <strong>the</strong> femurrelative to <strong>the</strong> pelvis is described by just one angle, as shown in Fig. 6.8c.Contact with <strong>the</strong> environment serves to constrain <strong>the</strong> motion <strong>of</strong> <strong>the</strong> body segments during a motortask. Consider <strong>the</strong> task <strong>of</strong> vertical jumping as illustrated in Fig. 6.9. Assuming that movement <strong>of</strong> <strong>the</strong>body segments is constrained to <strong>the</strong> sagittal plane, Figure 6.9a indicates that <strong>the</strong> motor task has 6 d<strong>of</strong>when <strong>the</strong> body is in <strong>the</strong> air (x p , y p , which specify <strong>the</strong> position <strong>of</strong> <strong>the</strong> metatarsals plus θ 1 , θ 2 , θ 3 , θ 4 , whichspecify <strong>the</strong> orientation <strong>of</strong> <strong>the</strong> foot, shank, thigh, and trunk, respectively). When <strong>the</strong> metatarsals touch<strong>the</strong> ground, only 4 generalized coordinates are needed to specify <strong>the</strong> position and orientation <strong>of</strong> <strong>the</strong>body segments relative to any point on <strong>the</strong> ground, and accordingly <strong>the</strong> motor task has only 4 d<strong>of</strong>(Figure 6.9b). Similarly, when <strong>the</strong> feet are flat on <strong>the</strong> ground, <strong>the</strong> number <strong>of</strong> generalized coordinatesand <strong>the</strong> number <strong>of</strong> d<strong>of</strong> are each correspondingly reduced by 1 (Fig. 6.9c).6.3.2 Equations <strong>of</strong> MotionOnce a set <strong>of</strong> generalized coordinates has been specified and a kinematic model <strong>of</strong> <strong>the</strong> motor taskhas been defined, <strong>the</strong> governing equations <strong>of</strong> motion for <strong>the</strong> motor task can be written. Thenumber <strong>of</strong> dynamical equations <strong>of</strong> motion is equal to <strong>the</strong> number <strong>of</strong> d<strong>of</strong> <strong>of</strong> <strong>the</strong> motor task; thus, if<strong>the</strong> number <strong>of</strong> d<strong>of</strong> changes during a motor task (see Fig. 6.9), so too will <strong>the</strong> structure <strong>of</strong> <strong>the</strong>equations <strong>of</strong> motion.Different methods are available to derive <strong>the</strong> dynamical equations <strong>of</strong> motion for a motor task. In<strong>the</strong> Newton-Euler method (Pandy and Berme, 1988), free-body diagrams are constructed to show <strong>the</strong>external forces and torques acting on each body segment. The relationships between forces and linearDownloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.10 MECHANICS OF THE HUMAN BODYFIGURE 6.9 Number <strong>of</strong> d<strong>of</strong> <strong>of</strong> a motor task such as landing from a vertical jump. [Modified from Zajac and Gordon (1989).]accelerations <strong>of</strong> <strong>the</strong> centers <strong>of</strong> mass <strong>of</strong> <strong>the</strong> segments are written according to Newton’s second law (ΣF= ma), and <strong>the</strong> relationships between torques and angular accelerations <strong>of</strong> <strong>the</strong> segments are writtenusing Ruler’s equation (ΣT = Iα).The Newton-Euler method is well suited to a recursive formulation <strong>of</strong> <strong>the</strong> kinematic and dynamicequations <strong>of</strong> motion (Pandy and Berme, 1988); however, its main disadvantage is that all <strong>of</strong> <strong>the</strong>intersegmental forces must be eliminated before <strong>the</strong> governing equations <strong>of</strong> motion can be formed. Inan alternative formulation <strong>of</strong> <strong>the</strong> dynamical equations <strong>of</strong> motion, Kane’s method (Kane andLevinson, 1985), which is also referred to as Lagrange’s form <strong>of</strong> D’Alembert’s principle, makesexplicit use <strong>of</strong> <strong>the</strong> fact that constraint forces do not contribute directly to <strong>the</strong> governing equations <strong>of</strong>motion. It has been shown that Kane’s formulation <strong>of</strong> <strong>the</strong> dynamical equations <strong>of</strong> motion iscomputationally more efficient than its counterpart, <strong>the</strong> Newton-Euler method (Kane and Levinson,1983).The governing equations <strong>of</strong> motion for any multijoint <strong>system</strong> can be expressed aswhere q, , = vectors <strong>of</strong> <strong>the</strong> generalized coordinates, velocities, accelerations, respectivelyM(q) = <strong>system</strong> mass matrixM(q) = vector <strong>of</strong> inertial forces and torquesC(q) 2= vector <strong>of</strong> centrifugal and Coriolis forces and torquesG(q) = vector <strong>of</strong> gravitational forces and torquesR(q) = matrix <strong>of</strong> muscle moment arms (see Sec. 6.4.3)F MT = vector <strong>of</strong> musculotendon forcesR(q)F MT = vector <strong>of</strong> musculotendon torquesE(q, ) = vector <strong>of</strong> external forces and torques applied to <strong>the</strong> bodyby <strong>the</strong> environment(6.1)Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.11If <strong>the</strong> number <strong>of</strong> d<strong>of</strong> <strong>of</strong> <strong>the</strong> motor task is greater than, say, 4, a computer is needed to obtain Eq. (6.1)explicitly. A number <strong>of</strong> commercial s<strong>of</strong>tware packages are available for this purpose includingAUTOLEV by On-Line Dynamics Inc., SD/FAST by Symbolic Dynamics Inc., ADAMS by MechanicalDynamics Inc., and DADS by CADSI.6.4 MUSCULOSKELETAL GEOMETRY6.4.1 Modeling <strong>the</strong> Paths <strong>of</strong> Musculotendinous ActuatorsTwo different methods are used to model <strong>the</strong> paths <strong>of</strong> musculotendinous actuators in <strong>the</strong> body: <strong>the</strong>straight-line method and <strong>the</strong> centroid-line method. In <strong>the</strong> straight-line method, <strong>the</strong> path <strong>of</strong> a musculotendinousactuator (muscle and tendon combined) is represented by a straight line joining <strong>the</strong>centroids <strong>of</strong> <strong>the</strong> tendon attachment sites (Jensen and Davy, 1975). Although this method is easy toimplement, it may not produce meaningful results when a muscle wraps around a bone or ano<strong>the</strong>rmuscle (see Fig. 6.10). In <strong>the</strong> centroid-line method, <strong>the</strong> path <strong>of</strong> <strong>the</strong> musculotendinous actuator isrepresented as a line passing through <strong>the</strong> locus <strong>of</strong> cross-sectional centroids <strong>of</strong> <strong>the</strong> actuator (Jensen andDavy, 1975). Although <strong>the</strong> actuator’s line <strong>of</strong> action is represented more accurately in this way, <strong>the</strong>centroid-line method can be difficult to apply because (1) it may not be possible to obtain <strong>the</strong>locations <strong>of</strong> <strong>the</strong> actuator’s cross-sectional centroids for even a single position <strong>of</strong> <strong>the</strong> body, and (2)even if an actuator’s centroid path is known for one position <strong>of</strong> <strong>the</strong> body, it is practically impossibleto determine how this path changes as body position changes.One way <strong>of</strong> addressing this problem is to introduce effective attachment sites or via points atspecific locations along <strong>the</strong> centroid path <strong>of</strong> <strong>the</strong> actuator. In this approach, <strong>the</strong> actuator’s line <strong>of</strong> actionis defined by ei<strong>the</strong>r straight-line segments or a combination <strong>of</strong> straight-line and curved-line segmentsbetween each set <strong>of</strong> via points (Brand et al., 1982; Delp et al., 1990). The via points remain fixedrelative to <strong>the</strong> bones even as <strong>the</strong> joints move, and muscle wrapping is taken into account by making<strong>the</strong> via points active or inactive, depending on <strong>the</strong> configuration <strong>of</strong> <strong>the</strong> joint. This method worksquite well when a muscle spans a 1-d<strong>of</strong> hinge joint, but it can lead to discontinuities in <strong>the</strong> calculatedvalues <strong>of</strong> moment arms when joints have more than 1 rotational d<strong>of</strong> (Fig. 6.10).6.4.2 Obstacle-Set MethodAn alternative approach, called <strong>the</strong> obstacle-set method, idealizes each musculotendinous actuator asa frictionless elastic band that can slide freely over <strong>the</strong> bones and o<strong>the</strong>r actuators as <strong>the</strong> configuration<strong>of</strong> <strong>the</strong> joint changes (Garner and Pandy, 2000). The musculotendinous path is defined by a series <strong>of</strong>straight-line and curved-line segments joined toge<strong>the</strong>r by via points, which may or may not be fixedrelative to <strong>the</strong> bones.To illustrate this method, consider <strong>the</strong> example shown in Fig. 6.11, where <strong>the</strong> path <strong>of</strong> <strong>the</strong> actuator isconstrained by a single obstacle, which is fixed to bone A. (An obstacle is defined as any regular-shapedrigid body that is used to model <strong>the</strong> shape <strong>of</strong> a constraining anatomical structure such as a bone orano<strong>the</strong>r muscle.) The actuator’s path is defined by <strong>the</strong> positions <strong>of</strong> <strong>the</strong> five fixed via points and <strong>the</strong>positions <strong>of</strong> <strong>the</strong> two obstacle via points. (A fixed via point remains fixed in a bone reference frame andis always active; an obstacle via point is not fixed in any reference frame, but is constrained to moveon <strong>the</strong> surface <strong>of</strong> an underlying obstacle.) Via points P 1 and P 2 are fixed to bone A, while S 1 , S 2 , and S 3are fixed to bone B. For a given configuration <strong>of</strong> <strong>the</strong> joint, <strong>the</strong> paths <strong>of</strong> all segments <strong>of</strong> <strong>the</strong> muscle areknown, except those between <strong>the</strong> bounding-fixed via points, P 2 and S 3 . The path <strong>of</strong> <strong>the</strong> actuator isknown once <strong>the</strong> positions <strong>of</strong> <strong>the</strong> obstacle via points Q and T have been found.Figure 6.12 shows a computational algorithm that can be used to model <strong>the</strong> centroid path <strong>of</strong> amusculotendinous actuator for a given configuration <strong>of</strong> <strong>the</strong> joints in <strong>the</strong> body. There are four steps in<strong>the</strong> computational algorithm. Given <strong>the</strong> relative positions <strong>of</strong> <strong>the</strong> bones, <strong>the</strong> locations <strong>of</strong> all fixed viaDownloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.12 MECHANICS OF THE HUMAN BODYFIGURE 6.10 (a) Comparison <strong>of</strong> moment arms for <strong>the</strong> long head <strong>of</strong> triceps obtained using <strong>the</strong>straight-line model (Straight), fixed-via-point model (Fixed), and <strong>the</strong> obstacle-set model(Obstacle). For each model, <strong>the</strong> moment arms were calculated over <strong>the</strong> full range <strong>of</strong> elbowflexion, with <strong>the</strong> humerus positioned alongside <strong>the</strong> torso in neutral rotation (solid lines) andin 45° internal rotation (dotted lines). (b) Expanded scale <strong>of</strong> <strong>the</strong> graph above, where <strong>the</strong>moment arms obtained using <strong>the</strong> fixed-via-point and obstacle-set models are shown near <strong>the</strong>elbow flexion angle where <strong>the</strong> muscle first begins to wrap around <strong>the</strong> obstacle (cylinder)placed at <strong>the</strong> elbow [see part (a)]. The fixed-via-point model produces a discontinuity inmoment arm when <strong>the</strong> shoulder is rotated 45° internally (Fixed, dotted line). [Modified fromGarner and Pandy (2000).]points are known and can be expressed in <strong>the</strong> obstacle reference frame (Fig. 6.12, Step 1). Thelocations <strong>of</strong> <strong>the</strong> remaining via points in <strong>the</strong> actuator’s path, <strong>the</strong> obstacle via points, can be calculatedusing one or more <strong>of</strong> <strong>the</strong> four different obstacle sets given in Appendices C to F in Garner and Pandy(2000) (Fig. 6.12, Step 2). Once <strong>the</strong> locations <strong>of</strong> <strong>the</strong> obstacle via points are known, a check is madeto determine whe<strong>the</strong>r any <strong>of</strong> <strong>the</strong>se points should be inactive (Fig. 6.12, Step 3). If an obstacle viapoint should be inactive, it is removed from <strong>the</strong> actuator’s path and <strong>the</strong> locations <strong>of</strong> <strong>the</strong> remainingDownloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.13FIGURE 6.11 Schematic <strong>of</strong> a hypo<strong>the</strong>tical muscle (a) represented by <strong>the</strong>obstacle-set model [(b) and (c)]. The muscle spans a single joint that connectsbones A and B. Reference frames attached to <strong>the</strong> bones are used todescribe <strong>the</strong> position and orientation <strong>of</strong> <strong>the</strong> bones relative to each o<strong>the</strong>r.At certain joint configurations, <strong>the</strong> muscle contacts <strong>the</strong> bones and causes<strong>the</strong> centroid path <strong>of</strong> <strong>the</strong> muscle to deviate from a straight line (a). Themuscle path is modeled by a total <strong>of</strong> seven via points; five <strong>of</strong> <strong>the</strong>se arefixed via points (P 1 , P 2 , S 1, S 2 , S 3 ); <strong>the</strong> remaining two are obstacle via points(Q, T), which move relative to <strong>the</strong> bones and <strong>the</strong> obstacle. Points P1 and S1are <strong>the</strong> origin and insertion <strong>of</strong> <strong>the</strong> muscle. Points P 2 and S 3 are boundingfixedvia points. The obstacle is shown as a shaded circle, which represents<strong>the</strong> cross section <strong>of</strong> a sphere or cylinder. An obstacle reference framepositions and orients <strong>the</strong> obstacle relative to <strong>the</strong> bones. The obstacle ismade larger than <strong>the</strong> cross sections <strong>of</strong> <strong>the</strong> bones in order to account for <strong>the</strong>thickness <strong>of</strong> <strong>the</strong> muscle belly. The obstacle set is defined by <strong>the</strong> obstacle,<strong>the</strong> four via points (P 2 , Q, T, S 3 ), and <strong>the</strong> segments <strong>of</strong> <strong>the</strong> muscle pathbetween <strong>the</strong> via points P 2 and S 3 . At some joint configurations, <strong>the</strong> musclepath can lose contact with <strong>the</strong> obstacle, and <strong>the</strong> obstacle via points <strong>the</strong>nbecome inactive (c). See Garner and Pandy (2000) for details <strong>of</strong> <strong>the</strong> obstacle-setmethod. [Modified from Garner and Pandy (2000).]obstacle via points are <strong>the</strong>n recomputed (Fig. 6.12, repeat Steps 2 and 3). Finally, <strong>the</strong> lengths <strong>of</strong> <strong>the</strong>segments between all <strong>of</strong> <strong>the</strong> active via points along <strong>the</strong> actuator’s path are computed (Fig. 6.12, Step 4).The computational algorithm shown in Fig. 6.12 was used to model <strong>the</strong> paths <strong>of</strong> <strong>the</strong> triceps brachiimuscle in <strong>the</strong> arm (Garner and Pandy, 2000). The muscle was separated into three segments: <strong>the</strong>Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.14 MECHANICS OF THE HUMAN BODYFIGURE 6.12 Flowchart <strong>of</strong> <strong>the</strong> obstacle-set algorithm. See text for details.Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.15medial, lateral, and long heads (Fig. 6.13). Themedial head [Fig. 6.13 (1)] and lateral head[Fig. 6.13 (3)] were each modeled by a singlecylinderobstacle set (not shown in Fig. 6.13).The long head [Fig. 6.13 (2)] was modeled by adouble-cylinder obstacle set as illustrated. Thelocations <strong>of</strong> <strong>the</strong> attachment sites <strong>of</strong> each musclesegment and <strong>the</strong> locations and orientations <strong>of</strong><strong>the</strong> obstacles were chosen to reproduce <strong>the</strong>centroid paths <strong>of</strong> each head as accurately aspossible. The geometry <strong>of</strong> <strong>the</strong> bones and <strong>the</strong>centroid paths <strong>of</strong> <strong>the</strong> muscle segments wereobtained from three-dimensional reconstructions<strong>of</strong> high-resolution medical images obtainedfrom <strong>the</strong> National Library <strong>of</strong> Medicine’s VisibleHuman Male dataset (Garner and Pandy, 2001).Because <strong>the</strong> path <strong>of</strong> a muscle is not improperlyconstrained by contact with neighboringmuscles and bones, <strong>the</strong> obstacle-set methodproduces not only accurate estimates <strong>of</strong> musclemoment arms, but also smooth moment armjointangle curves, as illustrated in Fig. 6.10.6.4.3 Muscle Moment ArmsMuscles develop forces and cause rotation <strong>of</strong> <strong>the</strong>bones about a joint. The tendency <strong>of</strong> a musculotendinousactuator to rotate a bone about a jointis described by <strong>the</strong> actuator’s moment arm. Twomethods are commonly used to measure <strong>the</strong> momentarm <strong>of</strong> an actuator—<strong>the</strong> geometric methodand <strong>the</strong> tendon excursion method.In <strong>the</strong> geometric method, a finite center <strong>of</strong>rotation is found by x-rays, computedtomography, or magnetic resonance imaging,and <strong>the</strong> moment arm is found by measuring <strong>the</strong>perpendicular distance from <strong>the</strong> joint center to<strong>the</strong> line <strong>of</strong> action <strong>of</strong> <strong>the</strong> muscle (Jensen andDavy, 1975). In <strong>the</strong> tendon excursion method,<strong>the</strong> change in length <strong>of</strong> <strong>the</strong> musculotendinousFIGURE 6.13 Posterolateral view <strong>of</strong> <strong>the</strong> obstacle-set modelused to represent <strong>the</strong> paths <strong>of</strong> <strong>the</strong> triceps brachii in a model <strong>of</strong><strong>the</strong> arm. The medial head (1) and lateral head (3) were eachmodeled by a single-cylinder obstacle set, which is not shownin <strong>the</strong> diagram. The long head (2) was modeled by a doublecylinderobstacle set as illustrated here. The locations <strong>of</strong> <strong>the</strong>attachment sites <strong>of</strong> <strong>the</strong> muscle and <strong>the</strong> locations and orientations<strong>of</strong> <strong>the</strong> obstacles were chosen to reproduce <strong>the</strong> centroidpaths <strong>of</strong> each portion <strong>of</strong> <strong>the</strong> modeled muscle. The geometry <strong>of</strong><strong>the</strong> bones and <strong>the</strong> centroid paths <strong>of</strong> <strong>the</strong> muscles were based onthree-dimensional reconstructions <strong>of</strong> high-resolution medicalimages obtained from <strong>the</strong> National Library <strong>of</strong> Medicine’sVisible Human Male dataset. [Modified from Garner andPandy (2000).]actu ator is measured as a function <strong>of</strong> <strong>the</strong> joint angle, and <strong>the</strong> moment arm is obtained by evaluating<strong>the</strong> slope <strong>of</strong> <strong>the</strong> actuator-length versus joint-angle curve over <strong>the</strong> full range <strong>of</strong> joint movement (Anet al., 1983).Consider two body segments, A and B, which articulate at a joint (Fig. 6.14). By considering <strong>the</strong>instantaneous power delivered by a musculotendinous actuator to body B, it can be shown that <strong>the</strong>moment arm <strong>of</strong> <strong>the</strong> actuator can be written as (Pandy, 1999):where F M = musculotendinous force directed from <strong>the</strong> effective insertion <strong>of</strong> <strong>the</strong> actuator on bodyB (point Q) to <strong>the</strong> effective origin <strong>of</strong> <strong>the</strong> actuator on body A (point P)= unit vector that specifies <strong>the</strong> direction <strong>of</strong> <strong>the</strong> angular velocity <strong>of</strong> body B in bodyA [i.e., parallel to <strong>the</strong> instantaneous axis <strong>of</strong> rotation (ISA) <strong>of</strong> body B relative tobody A](6.2)Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.16 MECHANICS OF THE HUMAN BODYr OQ = position vector directed from any point O on <strong>the</strong>ISA to any point Q on <strong>the</strong> line <strong>of</strong> action <strong>of</strong> <strong>the</strong>actuator between its origin and insertion sites= unit vector in <strong>the</strong> direction <strong>of</strong> <strong>the</strong> actuator forceF M (see Fig. 6.14)In Eq. (6.2), r M is <strong>the</strong> moment-arm vector, which is equal to <strong>the</strong>moment <strong>of</strong> <strong>the</strong> musculotendinous force per unit <strong>of</strong> musculotendinousforce. The direction <strong>of</strong> <strong>the</strong> moment-arm vector is along <strong>the</strong>instantaneous axis <strong>of</strong> rotation <strong>of</strong> <strong>the</strong> body B relative to body Awhose direction is described by <strong>the</strong> unit vector .In <strong>the</strong> tendon excursion method, Euler’s <strong>the</strong>orem on rotation isused to define an equivalent relation for <strong>the</strong> moment arm <strong>of</strong> amusculotendinous force. Thus, if every change in <strong>the</strong> relativeorientation <strong>of</strong> body A and body B can be produced by means <strong>of</strong> asimple rotation <strong>of</strong> B in A about <strong>the</strong> ISA, <strong>the</strong>n <strong>the</strong> moment arm <strong>of</strong>a musculotendinous force can also be written as (Pandy, 1999):(6.3)FIGURE 6.14 Two bodies, A and B,shown articulating at a joint. Body Ais fixed in an inertial reference frame,and body B moves relative to it. Thepath <strong>of</strong> a generic muscle is representedby <strong>the</strong> origin S on B, <strong>the</strong> insertion N onA, and three intermediate via points P,Q, and R. Q and R are via points arisingfrom contact <strong>of</strong> <strong>the</strong> muscle path withbody B. Via point P arises from contact<strong>of</strong> <strong>the</strong> muscle path with body A. TheISA <strong>of</strong> B relative to A is defined by <strong>the</strong>angular velocity vector <strong>of</strong> B in A ( A ω B ).[Modified from Pandy (1999).]where l M = length <strong>of</strong> <strong>the</strong> musculotendinous actuator between<strong>the</strong> effective origin and insertion sites (P to Qin Fig. 6.14)θ = angle associated with <strong>the</strong> simple rotation <strong>of</strong> bodyB about <strong>the</strong> ISA= total derivative <strong>of</strong> musculotendinous length withrespect to <strong>the</strong> angle <strong>of</strong> rotation θ <strong>of</strong>body B relative to body AEquations (6.2) and (6.3) have <strong>the</strong> same geometric interpretation:<strong>the</strong> moment arm <strong>of</strong> a muscle force r M , given ei<strong>the</strong>r by ·from Eq (6.2) or by dl M /dθ from Eq. (6.3), is equal to<strong>the</strong> perpendicular (shortest) distance between <strong>the</strong> ISA <strong>of</strong> B relativeto A and <strong>the</strong> line <strong>of</strong> action <strong>of</strong> <strong>the</strong> muscle force, multiplied by<strong>the</strong> sine <strong>of</strong> <strong>the</strong> angle between <strong>the</strong>se two lines (Pandy, 1999).6.5 MUSCLE ACTIVATION AND CONTRACTION DYNAMICS6.5.1 Muscle Activation DynamicsNeural Excitation <strong>of</strong> Muscle. Voluntary contraction <strong>of</strong> human muscle initiates in <strong>the</strong> frontal motorcortex <strong>of</strong> <strong>the</strong> brain, where impulses from large pyramidal cells travel downward through corticospinaltracts that lead out to peripheral muscles. These impulses from <strong>the</strong> motor cortex are called actionpotentials, and each impulse is associated with a single motor neuron. The principle structure <strong>of</strong> a motorneuron is shown in Fig. 6.15. The action potential initiates in <strong>the</strong> cell body, or soma, and travels downa long efferent trunk, called <strong>the</strong> axon, at a rate <strong>of</strong> about 80 to 120 m/s. The action potential waveformis <strong>the</strong> result <strong>of</strong> a voltage depolarization-repolarization phenomenon across <strong>the</strong> neuron cell membrane.The membrane ionic potential at rest is disturbed by a surrounding stimulus, and Na + ions are allowedto momentarily rush inside. An active transport mechanism, called <strong>the</strong> Na + -K + pump, quickly returns <strong>the</strong>Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.17transmembrane potential to rest. This sequence <strong>of</strong> events,which lasts about 1 ms, stimulates a succession <strong>of</strong> nerveimpulses or waves that eventually reach muscle tissue.When an impulse reaches <strong>the</strong> muscle, it conducts overmuscle tissue as a motor unit action potential (MUAP).Motor unit action potentials can have a variety <strong>of</strong> generalshapes (Fang et al., 1997), as depicted in Fig. 6.16.FIGURE 6.15 Motor neuron. (A) cell body, (B) axon,(C) neuromuscular junction, and (D) muscle fiber. Theaction potential travels downward, from <strong>the</strong> cell bodytowards <strong>the</strong> neuromuscular junction.FIGURE 6.16 Representative motor unit action potentials (MUAPs).(a) Change in shapes due to increase in stimulation, (b) Sequence <strong>of</strong>MUAPs during voluntary contraction. [Source: Fang et al., 1997.]The connecting site between <strong>the</strong> motor neuron and<strong>the</strong> muscle is called <strong>the</strong> neuromuscular junction. Onemotor neuron can have branches to many muscle fibers,and <strong>the</strong>se toge<strong>the</strong>r are called a motor unit. When<strong>the</strong> nerve impulse reaches <strong>the</strong> end <strong>of</strong> <strong>the</strong> nerve fiber, aneurotransmitter called acetylcholine is released into <strong>the</strong>motor end plate <strong>of</strong> <strong>the</strong> muscle. This in turn causes <strong>the</strong>release <strong>of</strong> Ca ++ ions deep into <strong>the</strong> muscle fiber. The presence<strong>of</strong> Ca ++ ions causes cross-bridges to be formed betweenactin and myosin filaments in <strong>the</strong> sarcomeres. The actin filaments slide inward along <strong>the</strong>myosin filaments, causing <strong>the</strong> muscle fiber to contract.In addition to cortical motor neurons, control <strong>of</strong> <strong>the</strong> musculosketal <strong>system</strong> also relies on afferentreceptors or sensory neurons that carry information from <strong>the</strong> periphery to <strong>the</strong> brain or spinal cord.The simplest nerve pathways lead directly from sensory neurons to motor neurons, and are known asreflex arcs. One such example is <strong>the</strong> withdrawal reflex. When skin receptors sense something is hot orsharp (a pin prick, for example), a sensory impulse is sent to <strong>the</strong> spinal cord, where an interneuronintegrates <strong>the</strong> information and relays it to a motor neuron. The motor neuron in turn transmits asignal to <strong>the</strong> appropriate flexor muscle, which contracts and thus completes <strong>the</strong> reflex loop.Muscle Electromyography. While motor unit action potentials form <strong>the</strong> cellular origin for muscleactivation, <strong>the</strong>y are normally not observable in routine clinical applications. The electromyogram(EMG) is <strong>the</strong> primary tool to study muscle activation in clinical and research settings using bothsurface and indwelling electrodes (Basmajian and DeLuca, 1985). The electromyogram is <strong>the</strong> summation<strong>of</strong> all motor unit action potentials at a given location during muscle contraction. Hence itrepresents a “gross” measure <strong>of</strong> <strong>the</strong> strength <strong>of</strong> a muscle contraction, since <strong>the</strong> number <strong>of</strong> musclefibers contracting is directly related to <strong>the</strong> number <strong>of</strong> motor units firing.Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.18 MECHANICS OF THE HUMAN BODYThe EMG appears as a random series <strong>of</strong> bursts that represent periods <strong>of</strong> muscle contraction andrelaxation. Figure 6.17 shows a series <strong>of</strong> EMG bursts. The EMG signal is acquired by both invasiveand noninvasive techniques. In invasive detection, a needle or fine wire is inserted directly into <strong>the</strong>muscle to a depth <strong>of</strong> several centimeters. In noninvasive techniques, also known as surfaceelectromyography, a recording electrode is pasted onto <strong>the</strong> skin approximately halfway between <strong>the</strong>muscle’s origin and insertion sites. In ei<strong>the</strong>r case, because <strong>of</strong> <strong>the</strong> low voltage <strong>of</strong> <strong>the</strong> EMG signal (100µV to several millivolts), some amplification <strong>of</strong> <strong>the</strong> signal is needed before it enters <strong>the</strong> digital datacollection <strong>system</strong>. In addition, to reduce unwanted noise in <strong>the</strong> signal, an analog filter with passband<strong>of</strong> 20 to 500 Hz should be used. This necessitates a typical digital sampling rate <strong>of</strong> 1000 Hz.Subsequent reduction <strong>of</strong> noise in <strong>the</strong> EMG signal can be handled computationally by digital filtering(Barr and Chan, 1986). A set <strong>of</strong> 16 recommendations for EMG acquisition and processing has beenpresented by DeLuca (1997).The EMG is analyzed in both <strong>the</strong> amplitude and frequency domains. For amplitude analysis, <strong>the</strong>most common processing technique is to compute a running root-mean-square (rms) <strong>of</strong> <strong>the</strong> signal.Over a short observational period T, <strong>the</strong> rms <strong>of</strong> <strong>the</strong> signal x(t) can be expressed as(6.4)In discrete form, over N contiguous samples, <strong>the</strong> rms can be expressed as:FIGURE 6.17 Two representative EMG bursts from <strong>the</strong> biceps muscle during an elbow flexion maneuver.Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.19(6.5)An alternative, but similar, approach to EMG amplitude analysis is to rectify and <strong>the</strong>n integrate <strong>the</strong>signal over <strong>the</strong> short period T (called integrated EMG, or IEMG). This approach has <strong>the</strong> advantage inthat a simple electronic circuit can be used and no numerical computation is necessary. In ei<strong>the</strong>r case,<strong>the</strong> objective is to obtain an estimation <strong>of</strong> <strong>the</strong> underlying muscle contraction force, which is roughlyproportional to <strong>the</strong> EMG rms or IEMG. In recent efforts to use <strong>the</strong> EMG signal as a myoelectric controlsignal (Evans et al., 1994), a three-stage digital processing approach has arisen; it is illustrated in Fig.6.18. The process consists <strong>of</strong> (1) band-pass filtering (20 to 200 Hz) <strong>of</strong> <strong>the</strong> signal, (2) fullwaverectification, and (3) low-pass filtering (10-Hz cut<strong>of</strong>f) to produce a smooth signal.In <strong>the</strong> frequency domain, <strong>the</strong> most common tool is to apply a fast Fourier transform (FFT) to <strong>the</strong>EMG signal. A typical result is shown in Fig. 6.19. One can see that most <strong>of</strong> <strong>the</strong> power in <strong>the</strong> signalis confined to <strong>the</strong> 20- to 200-Hz range, and that <strong>the</strong> center frequency or mean power point istypically below 100 Hz. One use <strong>of</strong> EMG frequency analysis is in <strong>the</strong> study <strong>of</strong> muscle fatigue. It hasbeen shown that as <strong>the</strong> muscle fatigues, <strong>the</strong> median power frequency <strong>of</strong> <strong>the</strong> EMG shifts downward(Big-land-Ritchie et al., 1983).Modeling Activation Dynamics. As noted is Sec. 6.5.1 (“Neural Excitation <strong>of</strong> Muscle”), musclecannot activate or relax instantaneously. The delay between excitation and activation (or <strong>the</strong> development<strong>of</strong> muscle force) is due mainly to <strong>the</strong> time taken for calcium pumped out <strong>of</strong> <strong>the</strong> sarcoplasmicreticulum to travel down <strong>the</strong> T-tubule <strong>system</strong> and bind to troponin (Ebashi and Endo, 1968). Thisdelay is <strong>of</strong>ten modeled as a first-order process (Zajac and Gordon 1989; Pandy et al., 1992):(6.6)where u represents <strong>the</strong> net neural drive to muscle and a m <strong>the</strong> activation level. O<strong>the</strong>r forms <strong>of</strong> thisrelation are also possible; for example, an equation that is linear in <strong>the</strong> control u has been used tosimulate jumping (Pandy et al., 1990) as well as pedaling (Raasch et al., 1997). Implicit in <strong>the</strong>formulation <strong>of</strong> Eq. (6.6) is <strong>the</strong> assumption that muscle activation depends only on a single variable u.O<strong>the</strong>r models assume that a depends on two inputs, u 1 and u 2 say, which represent <strong>the</strong> separate effects<strong>of</strong> recruitment and stimulation frequency (Hatze, 1978). In simulations <strong>of</strong> multijoint movement,whe<strong>the</strong>r or not both recruitment and stimulation frequency are incorporated in a model <strong>of</strong> excitationcontraction(activation) dynamics is probably not as important as <strong>the</strong> values assumed for <strong>the</strong> timeconstants τ rise and τ fall . Values <strong>of</strong> <strong>the</strong>se constants range from 12 to 20 ms for rise time, τ rise , and from24 to 200 ms for relaxation time, τ fall (Pandy, 2001). Changes in <strong>the</strong> values <strong>of</strong> τ rise and τ fall within <strong>the</strong>ranges indicated can have a significant effect on predictions <strong>of</strong> movement coordination (F. C. Andersonand M. G. Pandy, unpublished results).6.5.2 Muscle Contraction DynamicsMechanism <strong>of</strong> Muscle Contraction. Our understanding <strong>of</strong> how a muscle develops force is based on<strong>the</strong> sliding-filament <strong>the</strong>ory <strong>of</strong> contraction. This <strong>the</strong>ory, formulated by A. F. Huxley in 1957, proposesthat a muscle shortens or leng<strong>the</strong>ns because <strong>the</strong> thick and thin filaments slide past each o<strong>the</strong>r without<strong>the</strong> filaments <strong>the</strong>mselves changing length (Huxley, 1957). The central tenet <strong>of</strong> <strong>the</strong> <strong>the</strong>ory is thatadenosine triphosphate (ATP) dependent interactions between thick filaments (myosin proteins) andthin filaments (actin proteins) generate a force that causes <strong>the</strong> thin filaments to slide past <strong>the</strong> thickfilaments. The force is generated by <strong>the</strong> myosin heads <strong>of</strong> thick filaments, which form cross-bridges toactin thin filaments in <strong>the</strong> AI zone, where <strong>the</strong> two filaments overlap (see Fig. 6.2e). Subsequentstructural changes in <strong>the</strong>se cross-bridges cause <strong>the</strong> myosin heads to “walk” along an actin filament.Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.20 MECHANICS OF THE HUMAN BODYFIGURE 6.18 A method for processing EMG data for a myoelectric control signal, (a) <strong>the</strong> raw EMG data and (b) <strong>the</strong> signal afterbeing rectified and low pass filtered (10 Hz cut<strong>of</strong>f).Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.21FIGURE 6.19 The fast Fourier transform (FFT) <strong>of</strong> an EMG sample. Most <strong>of</strong> <strong>the</strong> signal power is in <strong>the</strong> 20- to 200-Hz range.The sliding-filament <strong>the</strong>ory correctly predicts that <strong>the</strong> force <strong>of</strong> contraction is proportional to <strong>the</strong>amount <strong>of</strong> overlap between <strong>the</strong> thick and thin filaments (see Fig. 6.3).To understand <strong>the</strong> mechanism <strong>of</strong> muscle contraction, consider Figure 6.20, which shows <strong>the</strong>various steps involved in <strong>the</strong> interaction between one myosin head and a thin filament, also <strong>of</strong>tenreferred to as <strong>the</strong> cross-bridge cycle. In <strong>the</strong> absence <strong>of</strong> ATP, a myosin head binds tightly to an actinfilament in a “rigor” state. When ATP binds (Step 1), it opens <strong>the</strong> cleft in <strong>the</strong> myosin head, whichweakens <strong>the</strong> interaction with <strong>the</strong> actin filament. The myosin head <strong>the</strong>n reacts with ATP (Step 2),causing a structural change in <strong>the</strong> head that moves it to a new position, closer to <strong>the</strong> end <strong>of</strong> <strong>the</strong> actinfilament, or Z disk, where it <strong>the</strong>n rebinds to <strong>the</strong> filament. Phosphate is <strong>the</strong>n released from <strong>the</strong> ATPbindingpocket on <strong>the</strong> myosin head (Step 3), and <strong>the</strong> head <strong>the</strong>n undergoes a second structural change,called <strong>the</strong> power stroke, which restores myosin to its rigor state. Because <strong>the</strong> myosin head is bound to<strong>the</strong> actin filament, this second structural change exerts a force that causes <strong>the</strong> myosin head to move<strong>the</strong> actin filament (Fig. 6.20).Modeling Contraction Dynamics. A. F. Huxley developed a mechanistic model to explain <strong>the</strong> structuralchanges at <strong>the</strong> sarcomere level that were seen under <strong>the</strong> electron microscope in <strong>the</strong> late 1940sand early 1950s. Because <strong>of</strong> its complexity, however, this (cross-bridge) model is rarely, if ever, usedin studies <strong>of</strong> coordination. Instead, an empirical model, proposed by A. V. Hill, is used in virtually allmodels <strong>of</strong> movement to account for <strong>the</strong> force-length and force-velocity properties <strong>of</strong> muscle (Hill,1938) (Fig. 6.21).In a Hill-type model, muscle’s force-producing properties are described by four parametersDownloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.22 MECHANICS OF THE HUMAN BODYFIGURE 6.20 Schematic diagram illustrating <strong>the</strong> mechanism <strong>of</strong> force development inmuscle. [Modified from Lodish et al. (2000).](Zajac, 1989): muscle’s peak isometric force and its corresponding fiber length andpennation angle (α), and <strong>the</strong> intrinsic shortening velocity <strong>of</strong> muscle (v max ). is usually obtained bymultiplying muscle’s physiological cross-sectional area by a generic value <strong>of</strong> specific tension. Values<strong>of</strong> optimal muscle fiber length, , and α, <strong>the</strong> angle at which muscle fibers insert on tendon when <strong>the</strong>fibers are at <strong>the</strong>ir optimal length, are almost always based on data obtained from cadaver dissections(Freiderich and Brand, 1990). v max is <strong>of</strong>ten assumed to be muscle independent; for example,simulations <strong>of</strong> jumping (Pandy et al., 1990), pedaling (Raasch et al., 1997), and walking (Andersonand Pandy, 2001b) assume a value <strong>of</strong> v max = 10 s -1 for all muscles, which models <strong>the</strong> summed effect<strong>of</strong> slow, intermediate, and fast fibers (Zajac, 1989). Very few studies have examined <strong>the</strong> sensitivity <strong>of</strong>model simulations to changes in v max , even though a change in <strong>the</strong> value <strong>of</strong> this parameter has beenfound to affect performance nearly as much as a change in <strong>the</strong> value <strong>of</strong> (Pandy, 1990).Tendon is usually represented as elastic (Pandy et al., 1990; Anderson and Pandy, 1993). Eventhough force varies nonlinearly with a change in length as tendon is stretched from its restingDownloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.23FIGURE 6.21 Schematic diagram <strong>of</strong> a model commonlyused to simulate musculotendon actuation. Eachmusculotendon actuator is represented as a three-elementmuscle in series with an elastic tendon. The mechanicalbehavior <strong>of</strong> muscle is described by a Hill-type contractileelement (CE) that models muscle’s force-length-velocityproperty, a series-elastic element (SEE) that modelsmuscle’s active stiffness, and a parallel-elastic element(PEE) that models muscle’s passive stiffness. The instantaneouslength <strong>of</strong> <strong>the</strong> actuator is determined by <strong>the</strong> length <strong>of</strong><strong>the</strong> muscle, <strong>the</strong> length <strong>of</strong> <strong>the</strong> tendon, and <strong>the</strong> pennationangle <strong>of</strong> <strong>the</strong> muscle. In this model <strong>the</strong> width <strong>of</strong> <strong>the</strong> muscleis assumed to remain constant as muscle length changes.[Modified from Zajac and Gordon (1989) and Pandy et al.(1990).]length (see Fig. 6.6), a linear force-length curve is sometimes used (Anderson and Pandy, 1993). Thissimplification will overestimate <strong>the</strong> amount <strong>of</strong> strain energy stored in tendon, but <strong>the</strong> effect onactuator performance is not likely to be significant, because tendon force is small in <strong>the</strong> region where<strong>the</strong> force-length curve is nonlinear. Values <strong>of</strong> <strong>the</strong> four muscle parameters plus tendon rest length fora number <strong>of</strong> musculotendinous actuators in <strong>the</strong> human arm and leg can be found in Garner andPandy (2001) and Anderson and Pandy (1999), respectively.For <strong>the</strong> actuator shown in Fig. 6.21, musculotendon dynamics is described by a single, nonlinear,differential equation that relates musculotendon force (F MT ), musculotendon length (l MT ),musculotendon shortening velocity (v MT ), and muscle activation (a m ) to <strong>the</strong> time rate <strong>of</strong> change inmusculotendon force:Given values <strong>of</strong> F MT , l MT , v MT , and a m at one instant in time, Eq. (6.7) can be integrated numerically t<strong>of</strong>ind musculotendon force at <strong>the</strong> next instant.(6.7)6.6 DETERMINING MUSCLE FORCE6.6.1 Muscle Forces and Joint TorquesThe torque <strong>of</strong> a musculotendinous force is equal to <strong>the</strong> magnitude <strong>of</strong> <strong>the</strong> actuator force F MT , multipliedby <strong>the</strong> moment arm <strong>of</strong> <strong>the</strong> actuator r MT . Thus, <strong>the</strong> torque exerted by actuator i about joint j is(6.8)Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.24 MECHANICS OF THE HUMAN BODYwhere can be found from ei<strong>the</strong>r Eq. (6.2) or Eq. (6.3). For a <strong>system</strong> with m actuators and n joints,<strong>the</strong> above relation can be expressed in matrix form [see also Eq. (6.1)]:(6.9)where r 11 is <strong>the</strong> moment arm <strong>of</strong> <strong>the</strong> actuator force that exerts a torque about joint 1, etc.6.6.2 Indeterminate Problem in BiomechanicsBoth agonist and antagonist muscles contribute (unequally) to <strong>the</strong> net torque developed about a joint.In fact, for any given joint in <strong>the</strong> body, <strong>the</strong>re are many more muscles crossing <strong>the</strong> joint than <strong>the</strong>re ared<strong>of</strong> prescribing joint movement. The knee, for example, has at most 6 d<strong>of</strong>, yet <strong>the</strong>re are at least 14muscles that actuate this joint. One consequence <strong>of</strong> this arrangement is that <strong>the</strong> force developed byeach muscle cannot be determined uniquely. Specifically, <strong>the</strong>re are more unknown musculotendinousactuator forces than net actuator torques exerted about <strong>the</strong> knee; that is, m > n in Eq. (6.9), whichmeans that <strong>the</strong> matrix <strong>of</strong> muscle moment arms is not square and <strong>the</strong>refore not invertible. This is <strong>the</strong>so-called indeterminate problem in <strong>biomechanics</strong>, and virtually all attempts to solve it are based on<strong>the</strong> application <strong>of</strong> optimization <strong>the</strong>ory (see also <strong>the</strong> Chap. 5 by Manal and Buchanan).6.6.3 Inverse-Dynamics MethodIn <strong>the</strong> inverse-dynamics method, noninvasive measurements <strong>of</strong> body motions (position, velocity, andacceleration <strong>of</strong> each segment) and external forces are used as inputs in Eq. (6.1) to calculate <strong>the</strong> netactuator torques exerted about each joint (see Fig. 6.22). This is a determinate problem because <strong>the</strong>number <strong>of</strong> net actuator torques is equal to <strong>the</strong> number <strong>of</strong> equations <strong>of</strong> motion <strong>of</strong> <strong>the</strong> <strong>system</strong>.Specifically, from Eq. (6.1), we can write(6.10)where Eq. (6.9) has been used to replace R(q)F MT with T MT (q) in Eq. (6.1). The right-hand side <strong>of</strong> Eq.(6.10) can be evaluated by noninvasive measurements <strong>of</strong> body motions (q, , ) and external forcesE(q, ). This means that all quantities on <strong>the</strong> left-hand side <strong>of</strong> Eq. (6.9) are known. The matrix <strong>of</strong>actuator moment arms on <strong>the</strong> right-hand side <strong>of</strong> Eq. (6.9) can also be evaluated if <strong>the</strong> origin andinsertion sites <strong>of</strong> each musculotendinous actuator and <strong>the</strong> relative positions <strong>of</strong> <strong>the</strong> body segments areknown at each instant during <strong>the</strong> movement (Sec. 6.4).However, Eq. (6.9) cannot be solved for <strong>the</strong> m actuator forces because m > n (i.e., <strong>the</strong> matrix <strong>of</strong>actuator moment arms is nonsquare). Static optimization <strong>the</strong>ory is usually used to solve thisindeterminate problem (Seireg and Arvikar, 1975; Hardt, 1978; Crowninshield and Brand, 1981).Here, a cost function is hypo<strong>the</strong>sized, and an optimal set <strong>of</strong> actuator forces is found, subject to <strong>the</strong>equality constraints defined by Eq. (6.9) plus additional inequality constraints that bound <strong>the</strong> values<strong>of</strong> <strong>the</strong> actuator forces. If, for example, actuator stress is to be minimized, <strong>the</strong>n <strong>the</strong> static optimizationproblem can be stated as follows (Seireg and Arvikar, 1975; Crowninshield and Brand, 1981): Find<strong>the</strong> set <strong>of</strong> actuator forces that minimizes <strong>the</strong> sum <strong>of</strong> <strong>the</strong> squares <strong>of</strong> actuator stresses:subject to <strong>the</strong> equality constraints(6.11)(6.12)Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.25FIGURE 6.22 Comparison <strong>of</strong> <strong>the</strong> forward- and inverse-dynamics methods for determining muscle forces during movement. Top:Body motions are <strong>the</strong> inputs and muscle forces are <strong>the</strong> outputs in inverse dynamics. Thus, measurements <strong>of</strong> body motions areused to calculate <strong>the</strong> net muscle torques exerted about <strong>the</strong> joints, from which muscle forces are determined using static optimization.Bottom: Muscle excitations are <strong>the</strong> inputs and body motions are <strong>the</strong> outputs in forward dynamics. Muscle force (F M ) isan intermediate product (i.e., output <strong>of</strong> <strong>the</strong> model for musculotendon dynamics).and <strong>the</strong> inequality constraints(6.13)is <strong>the</strong> peak isometric force developed by <strong>the</strong> ith musculotendinous actuator, a quantity that isdirectly proportional to <strong>the</strong> physiological cross-sectional area <strong>of</strong> <strong>the</strong> ith muscle. Equation (6.12)expresses <strong>the</strong> n relationships between <strong>the</strong> net actuator torques T MT , <strong>the</strong> matrix <strong>of</strong> actuator moment armsR(q), and <strong>the</strong> unknown actuator forces F MT . Equation (6.13) is a set <strong>of</strong> m equations that constrains <strong>the</strong>value <strong>of</strong> each actuator force to remain greater than zero and less than <strong>the</strong> peak isometric force <strong>of</strong> <strong>the</strong>actuator defined by <strong>the</strong> cross-sectional area <strong>of</strong> <strong>the</strong> muscle. Standard nonlinear programming algorithmscan be used to solve this problem [e.g., sequential quadratic programming (Powell, 1978)].6.6.4 Forward-Dynamics MethodEquations (6.1) and (6.7) can be combined to form a model <strong>of</strong> <strong>the</strong> <strong>musculoskeletal</strong> <strong>system</strong> in which<strong>the</strong> inputs are <strong>the</strong> muscle activation histories (a) and <strong>the</strong> outputs are <strong>the</strong> body motions (q, , ) (Fig.6.22). Measurements <strong>of</strong> muscle EMG and body motions can be used to calculate <strong>the</strong> time histories <strong>of</strong><strong>the</strong> musculotendinous forces during movement (H<strong>of</strong> et al., 1987; Buchanan et al., 1993). Alternatively,<strong>the</strong> goal <strong>of</strong> <strong>the</strong> motor task can be modeled and used, toge<strong>the</strong>r with dynamic optimization<strong>the</strong>ory, to calculate <strong>the</strong> pattern <strong>of</strong> muscle activations needed for optimal performance <strong>of</strong> <strong>the</strong> task(Hatze, 1976; Pandy et al., 1990; Raasch et al., 1997; Pandy, 2001). Thus, one reason why <strong>the</strong>forward-dynamics method is potentially more powerful for evaluating musculotendinous forces thanDownloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.26 MECHANICS OF THE HUMAN BODY<strong>the</strong> inverse-dynamics method is that <strong>the</strong> optimization is performed over a complete cycle <strong>of</strong> <strong>the</strong> task,not just at one instant at a time.If we consider once again <strong>the</strong> example <strong>of</strong> minimizing muscle stress (cf. Sec. 6.6.3), an analogousdynamic optimization problem may be posed as follows. Find <strong>the</strong> time histories <strong>of</strong> all actuator forcesthat minimize <strong>the</strong> sum <strong>of</strong> <strong>the</strong> squares <strong>of</strong> actuator stresses:(6.14)subject to <strong>the</strong> equality constraints given by <strong>the</strong> dynamical equations <strong>of</strong> motion [Eqs. (6.7) and (6.1),respectively]:andThe initial states <strong>of</strong> <strong>the</strong> <strong>system</strong>,(6.15)and any terminal and/or path constraints, must be satisfied additionally. The dynamic optimizationproblem formulated above is a two-point, boundary-value problem, which is <strong>of</strong>ten difficult to solve,particularly when <strong>the</strong> dimension <strong>of</strong> <strong>the</strong> <strong>system</strong> is large (i.e., when <strong>the</strong> <strong>system</strong> has many d<strong>of</strong> and manymuscles).A better approach involves parameterizing <strong>the</strong> input muscle activations (or controls) andconverting <strong>the</strong> dynamic optimization problem into a parameter optimization problem (Pandy et al.,1992). The procedure is as follows. First, an initial guess is assumed for <strong>the</strong> control variables a. The<strong>system</strong> dynamical equations [Eq. (6.7) and (6.1)] are <strong>the</strong>n integrated forward in time to evaluate <strong>the</strong>cost function in Eq. (6.14). Derivatives <strong>of</strong> <strong>the</strong> cost function and constraints are <strong>the</strong>n calculated andFIGURE 6.23 Computational algorithm used to solve dynamic optimization problems inhuman movement studies. The algorithm computes <strong>the</strong> muscle excitations (controls)needed to produce optimal performance (e.g., maximum jump height). The optimal controlsare found by parameter optimization.Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.27used to find a new set <strong>of</strong> controls that will improve <strong>the</strong> values <strong>of</strong> <strong>the</strong> cost function and <strong>the</strong> constraintsin <strong>the</strong> next iteration (see Fig. 6.23). The computational algorithm shown in Fig. 6.23 has been usedto find <strong>the</strong> optimal controls for vertical jumping (Anderson and Pandy, 1993), rising from a chair(Pandy et al., 1995), pedaling (Fregly and Zajac, 1996), and walking (Anderson and Pandy, 2001b).If accurate measurements <strong>of</strong> body motions and external forces are available, <strong>the</strong>n inversedynamics should be used to determine musculotendinous forces during movement, because thismethod is much less expensive computationally. If, instead, <strong>the</strong> goal is to study how changes in bodystructure affect function and performance <strong>of</strong> a motor task, <strong>the</strong>n <strong>the</strong> forward-dynamics method ispreferred, for measurements <strong>of</strong> body motions and external forces are a priori not available in thisinstance.6.7 MUSCLE, LIGAMENT, AND JOINT-CONTACT FORCESBecause muscle, ligament, and joint-contact forces cannot be measured noninvasively in vivo, estimates<strong>of</strong> <strong>the</strong>se quantities have been obtained by combining ma<strong>the</strong>matical models with ei<strong>the</strong>r <strong>the</strong>inverse-dynamics or <strong>the</strong> forward-dynamics approach (Sec. 6.6). Below we review <strong>the</strong> levels <strong>of</strong><strong>musculoskeletal</strong> loading incurred in <strong>the</strong> lower-limb during rehabilitation exercises, such as isokineticknee extension, as well as during daily activity such as gait.6.7.1 Knee Extension ExerciseThe quadriceps is <strong>the</strong> strongest muscle in <strong>the</strong> body. This can be demonstrated by performing anisometric knee-extension exercise. Here, <strong>the</strong> subject is seated comfortably in a Cybex or Biodexdynamometer with <strong>the</strong> torso and thigh strapped firmly to <strong>the</strong> seat. The hip is flexed to 60°, and <strong>the</strong>leg is strapped to <strong>the</strong> arm <strong>of</strong> <strong>the</strong> machine, which can be ei<strong>the</strong>r fixed or allowed to rotate at a constantangular velocity (see Fig. 6.24). Locking <strong>the</strong> machine arm in place allows <strong>the</strong> muscles crossing <strong>the</strong>FIGURE 6.24 Photograph and schematic diagram showing <strong>the</strong> arrangement commonly used when people perform a kneeextensionexercise on a Biodex or Cybex dynamometer. Notice that <strong>the</strong> strap fixed on <strong>the</strong> machine arm is attached distally (near<strong>the</strong> ankle) on <strong>the</strong> subject’s leg.Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.28 MECHANICS OF THE HUMAN BODYFIGURE 6.25 Muscle and knee-ligament forces incurred during a maximum isometricknee-extension exercise. The results were obtained from a two-dimensionalma<strong>the</strong>matical model <strong>of</strong> <strong>the</strong> knee joint, assuming <strong>the</strong> quadriceps musclesare fully activated and <strong>the</strong>re is no cocontraction in <strong>the</strong> flexor muscles <strong>of</strong> <strong>the</strong> knee(Shelburne and Pandy, 1997). The thick solid line represents <strong>the</strong> resultant forceacting in <strong>the</strong> quadriceps tendon. The thin lines are <strong>the</strong> forces transmitted to <strong>the</strong>cruciate ligaments (aAC, black solid line; pAC, black dashed line; aPC, graydashed line; pPC, gray solid line). The forces in <strong>the</strong> collateral ligaments are nearlyzero. [Modified from Shelburne and Pandy (1997).]knee to contract isometrically, because <strong>the</strong> knee angle is <strong>the</strong>n held fixed. Under <strong>the</strong>se conditions, <strong>the</strong>quadriceps muscles can exert up to 9500 N when fully activated. As shown in Fig. 6.25, peakisometric force is developed with <strong>the</strong> knee bent to 90°, and decreases as <strong>the</strong> knee is moved towardextension (Fig. 6.25, quads). Quadriceps force decreases as knee-flexion angle decreases because <strong>the</strong>muscle moves down <strong>the</strong> ascending limb <strong>of</strong> its force-length curve as <strong>the</strong> knee extends (see Fig. 6.3).Quadriceps force increases monotonically from full extension and 90° <strong>of</strong> flexion, but <strong>the</strong> forcesborne by <strong>the</strong> cruciate ligaments <strong>of</strong> <strong>the</strong> knee do not (Fig. 6.25, ACL). Calculations obtained from ama<strong>the</strong>matical model <strong>of</strong> <strong>the</strong> knee (Shelburne and Pandy, 1997; Pandy and Shelburne, 1997; Pandyand Sasaki, 1997) indicate that <strong>the</strong> ACL is loaded from full extension to 80° <strong>of</strong> flexion duringkneeextension exercise. The model calculations also show that <strong>the</strong> resultant force in <strong>the</strong> ACL reaches500 N at 20° <strong>of</strong> flexion, which is lower than <strong>the</strong> maximum strength <strong>of</strong> <strong>the</strong> human ACL (2000 N)(Noyes and Grood, 1976).The calculations show fur<strong>the</strong>r that load sharing within a ligament is not uniform. For example, <strong>the</strong>force borne by <strong>the</strong> anteromedial bundle <strong>of</strong> <strong>the</strong> ACL (aAC) increases from full extension to 20° <strong>of</strong>flexion, where peak force occurs, and aAC force <strong>the</strong>n decreases as <strong>the</strong> knee flexion increases (Figure6.25, aAC). The changing distribution <strong>of</strong> force within <strong>the</strong> ACL suggests that single-strandedreconstructions may not adequately meet <strong>the</strong> functional requirements <strong>of</strong> <strong>the</strong> natural ligament.For isokinetic exercise, in which <strong>the</strong> knee is made to move at a constant angular velocity,quadriceps force decreases as knee-extension speed increases. As <strong>the</strong> knee extends more quickly,quadriceps force decreases because <strong>the</strong> muscle shortens more quickly, and, from <strong>the</strong> force-velocityproperty, an increase in shortening velocity leads to less muscle force (see Fig. 6.4). As a result, ACLforce also decreases as knee-extension speed increases (Figure 6.26), because <strong>of</strong> <strong>the</strong> drop in shearforce applied to <strong>the</strong> leg by <strong>the</strong> quadriceps (via <strong>the</strong> patellar tendon) (Serpas et al., in press).Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.29FIGURE 6.26 Resultant force in <strong>the</strong> ACL for isometric (thick line) andisokinetic (30, 90, 180, and 300 deg/sec) knee-extension exercises. The resultswere obtained from a two-dimensional model <strong>of</strong> <strong>the</strong> knee joint, assuming<strong>the</strong> quadriceps are fully activated and <strong>the</strong>re is no cocontraction in <strong>the</strong>flexor muscles <strong>of</strong> <strong>the</strong> knee (Serpas et al., in press). The model results showthat exercises in <strong>the</strong> studied speed range can reduce <strong>the</strong> force in <strong>the</strong> ACL byas much as one-half. [Modified from Serpas et al. (in press).]The forces exerted between <strong>the</strong> femur and patella and between femur and tibia depend mainly on<strong>the</strong> geometry <strong>of</strong> <strong>the</strong> muscles that cross <strong>the</strong> knee. For maximum isometric extension peak forcestransmitted to <strong>the</strong> patell<strong>of</strong>emoral and tibi<strong>of</strong>emoral joints are around 11,000 N and 6500 N, respectively(i.e., 15.7 and 9.3 times body weight, respectively) (Fig. 6.27). As <strong>the</strong> knee moves fasterduring isokinetic extension exercise, joint-contact forces decrease in dire proportion to <strong>the</strong> drop inquadriceps force (T. Yanagawa and M. G. Pandy, unpublished results).FIGURE 6.27 Resultant forces acting between <strong>the</strong> femur and patella (PF)and between <strong>the</strong> femur and tibia (TF) during maximum isometric kneeextensionexercise. See Fig. 6.25 for details.Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.30 MECHANICS OF THE HUMAN BODYFIGURE 6.28 Forces generated by muscles spanning <strong>the</strong> hip, knee, and ankle (heavy black lines) during normal walking overlevel ground. The muscle forces were found by solving a dynamic optimization problem that minimized <strong>the</strong> amount <strong>of</strong> metabolicenergy consumed by <strong>the</strong> muscles in <strong>the</strong> body per meter walked. In <strong>the</strong> model used to simulate gait, <strong>the</strong> body was represented asa 10-segment, 23-d<strong>of</strong> articulated linkage, and was actuated by 54 musculotendinous units (Anderson, 1999; Anderson andPandy, 2001a; Anderson and Pandy, 2001b). The time scale is represented as a percentage <strong>of</strong> <strong>the</strong> gait cycle. The gray wavy linesare EMG data recorded from one subject, and are given to show that <strong>the</strong> timing <strong>of</strong> <strong>the</strong> muscle-force development is consistentwith <strong>the</strong> measured EMG activity <strong>of</strong> <strong>the</strong> muscles. The following gait cycle landmarks are demarcated by thin vertical lines:opposite toe-<strong>of</strong>f (OTO), opposite heel-strike (OHS), toe-<strong>of</strong>f (TO), and heel-strike (HS). The muscle-force plots are scaled to eachmuscle’s maximum isometric strength (e.g., peak isometric strength in vasti is 6865 N). Muscle abbreviations are as follows:erector spinae (ERSP), gluteus maximus (GMAX), gluteus medius (GMED), hamstrings (HAMS), vasti (VAS), gastrocnemius(GAS), soleus (SOL). [Modified from Anderson and Pandy (2001a).]Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.31FIGURE 6.29 Joint contact forces acting at <strong>the</strong> hip, knee, and ankleduring gait. The results were obtained by solving a dynamic optimizationproblem for normal walking (see Fig. 6.28 for details). [Modifiedfrom Anderson and Pandy (2001a).]The results <strong>of</strong> Fig. 6.25 to 6.27 have significant implications for <strong>the</strong> design <strong>of</strong> exercise regimensaimed at protecting injured or newly reconstructed knee ligaments. For maximum isolated contractions<strong>of</strong> <strong>the</strong> quadriceps, Fig. 6.25 shows that <strong>the</strong> ACL is loaded at all flex angles less than 80°.Quadriceps-streng<strong>the</strong>ning exercises should <strong>the</strong>refore be limited to flexion angles greater than 80° if<strong>the</strong> ACL is to be protected from load. In this region, however, very high contact forces can be appliedto <strong>the</strong> patella (Fig. 6.27), so limiting this exercise to large flexion angles may result in patell<strong>of</strong>emoralpain. This scenario, known as <strong>the</strong> “paradox <strong>of</strong> exercise,” is <strong>the</strong> reason why surgeons and physical<strong>the</strong>rapists now prescribe so-called closed-chain exercises, such as squatting, for streng<strong>the</strong>ning <strong>the</strong>quadriceps muscles subsequent to ACL reconstruction.6.7.2 GaitMuscle and joint loading are much lower during gait than during knee-extension exercise. Variousstudies have used inverse-dynamics or static optimization (Hardt, 1978; Crowninshield and Brand,1981; Glitsch and Baumann, 1997) and forward-dynamics or dynamic optimization (Davy and Audu,Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.32 MECHANICS OF THE HUMAN BODY1987; Yamaguchi and Zajac, 1990; Anderson and Pandy, 2001b) to estimate muscle forces duringnormal gait. There is general agreement in <strong>the</strong> results obtained from <strong>the</strong>se modeling studies.Analysis <strong>of</strong> a dynamic optimization solution has shown that <strong>the</strong> hip, knee, and ankle extensors are<strong>the</strong> prime movers <strong>of</strong> <strong>the</strong> lower limb during normal walking. Specifically, gluteus maximus and vastiprovide support against gravity during initial stance; gluteus medius provides most <strong>of</strong> <strong>the</strong> supportduring midstance; and soleus and gastrocnemius support and simultaneously propel <strong>the</strong> body forwardduring terminal stance (also known as push-<strong>of</strong>f) (Anderson, 1999; Anderson and Pandy, 2001a).The plantarflexors generate <strong>the</strong> largest forces <strong>of</strong> all <strong>the</strong> muscles in <strong>the</strong> leg during normal gait.Soleus and gastrocnemius, combined, produce peak forces <strong>of</strong> roughly 3000 N (or 4 times bodyweight) during <strong>the</strong> push-<strong>of</strong>f phase (Fig. 6.28, SOL and GAS prior to OHS). By comparison, <strong>the</strong> hipextensors, gluteus maximus, and gluteus medius combined produce peak forces that are slightly less(around 2500 N or 3.5 times body weight during initial stance) (Fig. 6.28, GMAXL, GMAXM,GMEDP, and GMEDA near OTO). Finally, <strong>the</strong> quadriceps, vasti, and rectus femoris combineddevelop peak forces that are barely 2 times body weight near <strong>the</strong> transition from double support tosingle support (Fig. 6.28, VAS and RF at OTO).Muscles dominate <strong>the</strong> forces transmitted to <strong>the</strong> bones for most activities <strong>of</strong> daily living. Thus, <strong>the</strong>loading histories applied at <strong>the</strong> ankle, knee, and hip are in close correspondence with <strong>the</strong> predictedactions <strong>of</strong> <strong>the</strong> muscles that cross each <strong>of</strong> <strong>the</strong>se joints (Fig. 6.29). For example, <strong>the</strong> peak forcetransmitted by <strong>the</strong> ankle is considerably higher than <strong>the</strong> peak forces transmitted by <strong>the</strong> hip or knee,which is consistent with <strong>the</strong> finding that <strong>the</strong> ankle plantarflexors develop <strong>the</strong> largest forces duringnormal gait (compare joint-contact force at ankle in Fig. 6.29 with forces produced by SOL and GASin Fig. 6.28). Similarly, peak hip-contact force is around 4 times body weight near OTO, whichresults from <strong>the</strong> actions <strong>of</strong> <strong>the</strong> hip extensors, gluteus maximus, and gluteus medius, at this time(compare joint-contact force at hip in Fig. 6.29 with forces developed by GMAXL, GMAXM,GMEDP, and GMEDA in Fig. 6.28). Finally, <strong>the</strong> peak articular-contact force transmitted by <strong>the</strong> tibi<strong>of</strong>emoraljoint at <strong>the</strong> knee is less than 3 times body weight for gait. This level <strong>of</strong> joint loading is muchlower than that estimated for knee-extension exercise, where forces approaching 10 times bodyweight have been predicted to act between <strong>the</strong> femur and tibia (Fig. 6.27).REFERENCESAn, K. N., Ueba, Y., Chao, E. Y., et al. (1983). “Tendon excursion and moment arm <strong>of</strong> index finger muscles,” Journal <strong>of</strong> Biomechanics,16:419–425.Anderson, F. C. (1999). “A dynamic optimization solution for a complete cycle <strong>of</strong> normal gait,” Ph.D. dissertation, University<strong>of</strong> Texas at Austin.Anderson, F. C., and Pandy, M. G. (2001b). “Dynamic optimization <strong>of</strong> human walking,” Journal <strong>of</strong> Biomechanical Engineering,123:381–390.Anderson, F. C., and Pandy, M. G. (2001 a). “Static and dynamic optimization solutions for gait are practically equivalent,”Journal <strong>of</strong> Biomechanics, 34:153—161.Anderson, F. C., and Pandy, M. G. (1999). “A dynamic optimization solution for vertical jumping in three dimensions.” ComputerMethods in Biomechanics and Biomedical Engineering, 2:201–231.Anderson, F. C., and Pandy, M. G. (1993). “Storage and utilization <strong>of</strong> elastic strain energy during jumping.” Journal <strong>of</strong> Biomechanics,26:1413–1427.Barr, R., and Chan, E. (1986). “Design and implementation <strong>of</strong> digital filters for biomedical signal processing,” Journal <strong>of</strong>Electrophysiological Techniques, 13:73–93.Basmajian, J., and DeLuca, C. (1985). Muscles Alive: Their Function Revealed by Electromyography, Williams and Wilkens,Baltimore.Bigland-Ritchie, R., Johansson, R., Lippold, O., et al. (1983). “Changes in motor neuron firing rates during sustained maximalvoluntary contractions,” Journal <strong>of</strong> Physiology, 340:335–346.Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEMBIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM 6.33Brand, R. A., Crowninshield, R. D., Wittstock, C. E., et al. (1982). “A model <strong>of</strong> lower extremity muscular anatomy,” Journal <strong>of</strong>Biomechanical Engineering, 104:304–310.Buchanan, T. S., Moniz, M. J., Dewald, J. P., and Rymer, W. Z. (1993). “Estimation <strong>of</strong> muscle forces about <strong>the</strong> wrist joint duringisometric tasks using an EMG coefficient method,” Journal <strong>of</strong> Biomechanics, 26:547–560.Butler, D. L., Grood, E. S., Noyes, F. R., and Zernicke, R. F. (1978). “Biomechanics <strong>of</strong> ligaments and tendons,” Exercise and SportSciences Reviews, 6:125–181.Crowninshield, R. D., and Brand, R. A. (1981). “A physiologically-based criterion <strong>of</strong> muscle force prediction in locomotion,”Journal <strong>of</strong> Biomechanics, 14:793–801.Davy, D. T., and Audu, M. L. (1987). “A dynamic optimization technique for predicting muscle forces in <strong>the</strong> swing phase <strong>of</strong> gait,”Journal <strong>of</strong> Biomechanics, 20:187–201.Delp, S. L., Loan, J. P., Hoy, M. G., Zajac, F. E., Topp, E. L., and Rosen, J. M. (1990). “An interactive graphicsbased model <strong>of</strong> <strong>the</strong> lowerextremity to study orthopaedic surgical procedures,” IEEE Transactions on Biomedical Engineering, 37:757–767.DeLuca, C. (1997). “The use <strong>of</strong> surface electromyography in <strong>biomechanics</strong>,” Journal <strong>of</strong> Applied Biomechanics, 13:135–163.Ebashi, S., and Endo, M. (1968). “Calcium ion and muscle contraction,” Progress in Biophysics and Molecular Biology, 18:125–183.Enoka, R. M. (1994). Neuromechanical Basis <strong>of</strong> Kinesiology, 2d ed., Human Kinetics, New York.Evans, H., Pan, Z., Parker, P., and Scott, R. (1994). “Signal processing for proportional myoelectric control,” IEEE Transactionson Biomedical Engineering, 41:207–211.Fang, J., Shahani, B., and Graupe, D. (1997). “Motor unit number estimation by spatial-temporal summation <strong>of</strong> single motor unitpotentials,” Muscle and Nerve, 20:461–468.Fregly, B. J., and Zajac, F. E. (1996). “A state-space analysis <strong>of</strong> mechanical energy generation, absorption, and transfer duringpedaling,” Journal <strong>of</strong> Biomechanics, 29:81–90.Friederich, J., and Brand, R. A. (1990). “Muscle fiber architecture in <strong>the</strong> human lower limb,” Journal <strong>of</strong> Biomechanics, 23:91–95.Garner, B. A., and Pandy, M. G. (2001). “Musculoskeletal model <strong>of</strong> <strong>the</strong> human arm based on <strong>the</strong> Visible Human Male dataset,”Computer Methods in Biomechanics and Biomedical Engineering, 4:93–126.Garner, B. A., and Pandy, M. G. (2000). “The obstacle-set method for representing muscle paths in <strong>musculoskeletal</strong> models,”Computer Methods in Biomechanics and Biomedical Engineering, 3:1–30.Glitsch, U., and Baumann, W. (1997). “The three-dimensional determination <strong>of</strong> internal loads in <strong>the</strong> lower extremity,” Journal<strong>of</strong> Biomechanics, 30:1123–1131.Hardt, D. E. (1978). “Determining muscle forces in <strong>the</strong> leg during human walking: An application and evaluation <strong>of</strong> optimizationmethods,” Journal <strong>of</strong> Biomechancal Engineering, 100:72–78.Hatze, H. (1978). “A general myocybernetic control model <strong>of</strong> skeletal muscle,” Biological Cybernetics, 28:143–157.Hatze, H. (1976). “The complete optimization <strong>of</strong> human motion,” Ma<strong>the</strong>matical Biosciences, 28:99–135.Hayes, W. C., and Bodine, A. J. (1978). “Flow-independent viscoelastic properties <strong>of</strong> articular cartilage matrix,” Journal <strong>of</strong>Biomechanics, 11:407–419.Hayes W. C., and Mockros, L. F. (1971). “Viscoelastic properties <strong>of</strong> human articular cartilage.” Journal <strong>of</strong> Applied Physiology,31:562–568.Hill, A. V. (1938). “The heat <strong>of</strong> shortening and <strong>the</strong> dynamic constants <strong>of</strong> muscle,” Proceedings <strong>of</strong> <strong>the</strong> Royal Society (London),Series B, 126:136–195.H<strong>of</strong>, A. L., Pronk, C. A. N., J. A. van Best, (1987). “Comparison between EMG to force processing and kinetic analysis for <strong>the</strong> calfmuscle moment in walking and stepping,” Journal <strong>of</strong> Biomechanics, 20:167–178,Hori, R. Y., Mockros, L. F. (1976). “Indention tests <strong>of</strong> human articular cartilage,” Journal <strong>of</strong> Applied Physiology, 31:562–568.Huxley, A. F. (1957). “Muscle structure and <strong>the</strong>ories <strong>of</strong> contraction,” Progress in Biophysics and Biophysical Chemistry, 7:255–318.Jensen, R. H., and Davy, D. T. (1975). “An investigation <strong>of</strong> muscle lines <strong>of</strong> action about <strong>the</strong> hip: A centroid line approach vs <strong>the</strong>straight line approach,” Journal <strong>of</strong> Biomechanics, 8:103–110.Kane, T. R., and Levinson, D. A. (1983). “The use <strong>of</strong> Kane’s dynamical equations in robotics,” International Journal <strong>of</strong> RoboticsResearch, 2:3–21.Kane, T. R., and Levinson, D. A. (1985). Dynamics: Theory and Applications, McGraw-Hill, New York.Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.
BIOMECHANICS OF THE MUSCULOSKELETAL SYSTEM6.34 MECHANICS OF THE HUMAN BODYKempson, G. E. (1980). The Joints and Synovial Fluid, Vol. 2, Chap. 5, pp. 177–238, Academic Press, New York.Lodish, H., Berk, A., Zipursky, S. L., et al. (2000). Molecular Cell Biology, 4th ed., W. H. Freeman and Company, New York.McMahon, T. A. (1984). Muscles, Reflexes, and Locomotion, Princeton University Press, New Jersey.Mak, A. F. (1986). “The apparent viscoelastic behavior <strong>of</strong> articular cartilage: The contributions from <strong>the</strong> intrinsic matrix viscoelasticityand interstitial fluid flow,” Journal <strong>of</strong> Biomechanical Engineering, 108:123–130.Mow, V. C., Holmes, M. H., and Lai, W. M. (1984). “Fluid transport and mechanical properties <strong>of</strong> articular cartilage: a review,”Journal <strong>of</strong> Biomechanics, 17:377–394.Noyes, F. R., and Grood, E. S. (1976). “The strength <strong>of</strong> <strong>the</strong> anterior cruciate ligament in humans and rhesus monkeys,” Journal<strong>of</strong> Bone and Joint Surgery, 58-A:1074–1082.Pandy, M. G. (2001). “Computer modeling and simulation <strong>of</strong> human movement,” Annual Review <strong>of</strong> Biomedical Engineering,3:245–273.Pandy, M. G. (1999). “Moment arm <strong>of</strong> a muscle force,” Exercise and Sport Sciences Reviews, 27:79–118.Pandy, M. G., and Sasaki, K. (1998). “A three-dimensional <strong>musculoskeletal</strong> model <strong>of</strong> <strong>the</strong> human knee joint. Part II: Analysis <strong>of</strong>ligament function.” Computer Methods in Biomechanics and Biomedical Engineering, 1:265–283.Pandy, M. G., Sasaki, K., and Kim, S. (1997). “A three-dimensional <strong>musculoskeletal</strong> model <strong>of</strong> <strong>the</strong> human knee joint. Part I:Theoretical construction.” Computer Methods in Biomechanics and Biomedical Engineering, 1: 87–108.Pandy, M. G., and Shelburne, K. B. (1997). “Dependence <strong>of</strong> cruciate-ligament loading on muscle forces and external load,”Journal <strong>of</strong> Biomechanics, 30:1015–1024.Pandy, M. G., Garner, B. A., and Anderson, F. C. (1995). “Optimal control <strong>of</strong> non-ballistic muscular movements: A constraintbasedperformance criterion for rising from a chair.” Journal <strong>of</strong> Biomechanical Engineering, 117: 15–26.Pandy, M. G., Anderson, F. C., and Hull, D. G. (1992). “A parameter optimization approach for <strong>the</strong> optimal control <strong>of</strong> large-scale<strong>musculoskeletal</strong> <strong>system</strong>s,” Journal <strong>of</strong> Biomechanical Engineering, 114:450–460.Pandy, M. G., and Zajac, F. E. (1991). “Optimal muscular coordination strategies for jumping,” Journal <strong>of</strong> Biomechanics, 24:1–10.Pandy, M. G., Zajac, F. E., Sim, E., and Levine, W. S. (1990). “An optimal control model for maximum-height human jumping.”Journal <strong>of</strong> Biomechanics, 23:1185–1198.Pandy, M. G. (1990). “An analytical framework for quantifying muscular action during human movement,” in Winters J. M., andWoo, S. L-Y. (eds.), Multiple Muscle Systems—Biomechanics and Movement Organization, Springer-Verlag, New York, pp.653—662.Pandy, M. G., and Berme, N. (1988). “A numerical method for simulating <strong>the</strong> dynamics <strong>of</strong> human walking,” Journal <strong>of</strong> Biomechanics,21:1043–1051.Powell, M. J. D. (1978). “A fast algorithm for nonlinearly constrained optimization calculations,” in Matson, G. A. (ed.): NumericalAnalysis: Lecture Notes in Ma<strong>the</strong>matics, Vol. 630, pp. 144–157, Springer-Verlag, New York.Raasch, C. C., Zajac, F. E., Ma, B., and Levine, W. S. (1997). Muscle coordination <strong>of</strong> maximum-speed pedaling. Journal <strong>of</strong>Biomechanics 6:595–602.Seireg, A., and Arvikar, R. J. (1973). “A ma<strong>the</strong>matical model for evaluation <strong>of</strong> forces in <strong>the</strong> lower extremities <strong>of</strong> <strong>the</strong> <strong>musculoskeletal</strong><strong>system</strong>,” Journal <strong>of</strong> Biomechanics, 6:313–326.Serpas, F., Yanagawa, T., and Pandy, M. G. (2002). “Forward-dynamics simulation <strong>of</strong> anterior cruciate ligament forces developedduring isokinetic dynamometry.” Computer Methods in Biomechanics and Biomedical Engineering, 5:33–43.Shelburne, K. B., and Pandy, M. G. (1998). “Determinants <strong>of</strong> cruciate-ligament loading during rehabilitation exercise,” ClinicalBiomechanics, 13:403–413.Shelburne, K. B., and Pandy, M. G. (1997). “A <strong>musculoskeletal</strong> model <strong>of</strong> <strong>the</strong> knee for evaluating ligament forces during isometriccontractions,” Journal <strong>of</strong> Biomechanics, 30:163–176.Yamaguchi, G. T., and Zajac, F. E. (1990). “Restoring unassisted natural gait to paraplegics via functional neuromuscular stimulation:A computer simulation study.” IEEE Transactions on Biomedical Engineering, 37: 886–902.Zajac, F. E. (1993). “Muscle coordination: a perspective,” Journal <strong>of</strong> Biomechanics, 26 (suppl. 1):109–124.Zajac F. E., and Gordon, M. E. (1989). “Determining muscle’s force and action in multi-articular movement,” Exercise and SportSciences Reviews, 17:187–230.Downloaded from Digital Engineering Library @ McGraw-Hill (www.digitalengineeringlibrary.com)Copyright © 2004 The McGraw-Hill Companies. All rights reserved.Any use is subject to <strong>the</strong> Terms <strong>of</strong> Use as given at <strong>the</strong> website.